[11] In this patient, the negative results of the rubber series kit obviated the need to repeat the test.
\\r\\n\\r\\nMany known allergens, such as those commonly found in cosmetic products, are not included in patch testing kits. Thus, referral to a specialist for customized patch testing would be useful to confirm the diagnosis in this patient.
\\r\\n\\r\\nAn open application test, also known as a "repeat open application test," is performed after a mildly positive patch test to determine whether the reaction is clinically significant.[13] The allergen in question is openly and repeatedly applied to a small area of the skin, which is observed for a reaction at regular intervals within the first hour of testing and after 3-4 days.[14] This test is most appropriate for "leave-on" consumer products suspected to contain low-level contact allergens.
\\r\\n\\r\\nA skin biopsy can exclude other conditions, such as psoriasis. The histologic finding of spongiotic dermatitis is an important clue to the diagnosis of allergic contact dermatitis.[15] Because the offending agent had been identified in this patient, a skin biopsy was not necessary.\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 492331,\n \"questionText\": \"Of the following tests, which would best help to confirm this patient's diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"A 38-Year-Old Radiology Technician With a Blistering, Itchy Rash\"\n },\n {\n \"authors\": \"Melba Estrella, MD; Alan Snyder; John Plante; Dirk M. Elston, MD\",\n \"content\": [],\n \"date\": \"November 15, 2024\",\n \"figures\": [],\n \"markdown\": \"# A 38-Year-Old Radiology Technician With a Blistering, Itchy Rash\\n\\n **Authors:** Melba Estrella, MD; Alan Snyder; John Plante; Dirk M. Elston, MD \\n **Date:** November 15, 2024\\n\\n ## Content\\n\\n \\n\\n ## Figures\\n\\n \\n*Page 6 of 6*\",\n \"pagination\": {\n \"current_page\": 6,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1535601,\n \"choiceText\": \"Natural latex proteins\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535602,\n \"choiceText\": \"Synthetic latex polymers\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535603,\n \"choiceText\": \"Rubber manufacturing accelerators\",\n \"correct\": true,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535604,\n \"choiceText\": \"Bleached rubber compounds\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Patients can become sensitized to components found in natural rubber (latex) or synthetic rubber; however, they are more likely to become sensitized to the chemicals used in the process of rubber manufacturing, particularly accelerator agents.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 492330,\n \"questionText\": \"Which of the following is most likely to cause allergic contact dermatitis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1535605,\n \"choiceText\": \"Repeat patch testing using a rubber series kit\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535606,\n \"choiceText\": \"Perform patch testing using samples of the patient's underwear\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535607,\n \"choiceText\": \"Perform a repeat open application test\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535608,\n \"choiceText\": \"Perform a punch biopsy\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\\r\\nIf allergy remains strongly suspected despite a negative baseline series patch test, a rubber series kit is warranted to avoid false-negative results.[11] In this patient, the negative results of the rubber series kit obviated the need to repeat the test.
\\r\\n\\r\\nMany known allergens, such as those commonly found in cosmetic products, are not included in patch testing kits. Thus, referral to a specialist for customized patch testing would be useful to confirm the diagnosis in this patient.
\\r\\n\\r\\nAn open application test, also known as a "repeat open application test," is performed after a mildly positive patch test to determine whether the reaction is clinically significant.[13] The allergen in question is openly and repeatedly applied to a small area of the skin, which is observed for a reaction at regular intervals within the first hour of testing and after 3-4 days.[14] This test is most appropriate for "leave-on" consumer products suspected to contain low-level contact allergens.
\\r\\n\\r\\nA skin biopsy can exclude other conditions, such as psoriasis. The histologic finding of spongiotic dermatitis is an important clue to the diagnosis of allergic contact dermatitis.[15] Because the offending agent had been identified in this patient, a skin biopsy was not necessary.\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 492331,\n \"questionText\": \"Of the following tests, which would best help to confirm this patient's diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"A 38-Year-Old Radiology Technician With a Blistering, Itchy Rash\"\n }\n]"},"questions":{"kind":"list like","value":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1535597,"choiceText":"Herpes simplex virus infection","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1535598,"choiceText":"Atopic dermatitis","correct":false,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1535599,"choiceText":"Plaque psoriasis","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1535600,"choiceText":"Contact dermatitis","correct":true,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"","displayOrder":1,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":492329,"questionText":"On the basis of these findings only, which of the following is the most likely diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1535601,"choiceText":"Natural latex proteins","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1535602,"choiceText":"Synthetic latex polymers","correct":false,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1535603,"choiceText":"Rubber manufacturing accelerators","correct":true,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1535604,"choiceText":"Bleached rubber compounds","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Patients can become sensitized to components found in natural rubber (latex) or synthetic rubber; however, they are more likely to become sensitized to the chemicals used in the process of rubber manufacturing, particularly accelerator agents.","displayOrder":2,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":492330,"questionText":"Which of the following is most likely to cause allergic contact dermatitis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1535605,"choiceText":"Repeat patch testing using a rubber series kit","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1535606,"choiceText":"Perform patch testing using samples of the patient's underwear","correct":true,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1535607,"choiceText":"Perform a repeat open application test","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1535608,"choiceText":"Perform a punch biopsy","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"\r\nIf allergy remains strongly suspected despite a negative baseline series patch test, a rubber series kit is warranted to avoid false-negative results.[11] In this patient, the negative results of the rubber series kit obviated the need to repeat the test.
\r\n\r\nMany known allergens, such as those commonly found in cosmetic products, are not included in patch testing kits. Thus, referral to a specialist for customized patch testing would be useful to confirm the diagnosis in this patient.
\r\n\r\nAn open application test, also known as a "repeat open application test," is performed after a mildly positive patch test to determine whether the reaction is clinically significant.[13] The allergen in question is openly and repeatedly applied to a small area of the skin, which is observed for a reaction at regular intervals within the first hour of testing and after 3-4 days.[14] This test is most appropriate for "leave-on" consumer products suspected to contain low-level contact allergens.
\r\n\r\nA skin biopsy can exclude other conditions, such as psoriasis. The histologic finding of spongiotic dermatitis is an important clue to the diagnosis of allergic contact dermatitis.[15] Because the offending agent had been identified in this patient, a skin biopsy was not necessary.","displayOrder":3,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":492331,"questionText":"Of the following tests, which would best help to confirm this patient's diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"string":"[\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1535597,\n \"choiceText\": \"Herpes simplex virus infection\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535598,\n \"choiceText\": \"Atopic dermatitis\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535599,\n \"choiceText\": \"Plaque psoriasis\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535600,\n \"choiceText\": \"Contact dermatitis\",\n \"correct\": true,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\",\n \"displayOrder\": 1,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 492329,\n \"questionText\": \"On the basis of these findings only, which of the following is the most likely diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1535601,\n \"choiceText\": \"Natural latex proteins\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535602,\n \"choiceText\": \"Synthetic latex polymers\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535603,\n \"choiceText\": \"Rubber manufacturing accelerators\",\n \"correct\": true,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535604,\n \"choiceText\": \"Bleached rubber compounds\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Patients can become sensitized to components found in natural rubber (latex) or synthetic rubber; however, they are more likely to become sensitized to the chemicals used in the process of rubber manufacturing, particularly accelerator agents.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 492330,\n \"questionText\": \"Which of the following is most likely to cause allergic contact dermatitis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1535605,\n \"choiceText\": \"Repeat patch testing using a rubber series kit\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535606,\n \"choiceText\": \"Perform patch testing using samples of the patient's underwear\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535607,\n \"choiceText\": \"Perform a repeat open application test\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535608,\n \"choiceText\": \"Perform a punch biopsy\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\\r\\nIf allergy remains strongly suspected despite a negative baseline series patch test, a rubber series kit is warranted to avoid false-negative results.[11] In this patient, the negative results of the rubber series kit obviated the need to repeat the test.
\\r\\n\\r\\nMany known allergens, such as those commonly found in cosmetic products, are not included in patch testing kits. Thus, referral to a specialist for customized patch testing would be useful to confirm the diagnosis in this patient.
\\r\\n\\r\\nAn open application test, also known as a "repeat open application test," is performed after a mildly positive patch test to determine whether the reaction is clinically significant.[13] The allergen in question is openly and repeatedly applied to a small area of the skin, which is observed for a reaction at regular intervals within the first hour of testing and after 3-4 days.[14] This test is most appropriate for "leave-on" consumer products suspected to contain low-level contact allergens.
\\r\\n\\r\\nA skin biopsy can exclude other conditions, such as psoriasis. The histologic finding of spongiotic dermatitis is an important clue to the diagnosis of allergic contact dermatitis.[15] Because the offending agent had been identified in this patient, a skin biopsy was not necessary.\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 492331,\n \"questionText\": \"Of the following tests, which would best help to confirm this patient's diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n]"}}},{"rowIdx":297,"cells":{"article_id":{"kind":"string","value":"842258"},"url":{"kind":"string","value":"/viewarticle/842258"},"article_data":{"kind":"list like","value":[{"authors":"Winston W. Tan, MD; Matthew Tan","content":["Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.","A 63-year-old woman presents with a chronic cough. She was in her usual state of health until 3 months ago, when she developed a dry cough with fever. She was initially treated with antibiotics for 2 weeks. The cough improved, and the fever resolved. However, the dry cough returned.","The patient reports recent several instances of hemoptysis, as well as a 5-lb weight loss that she attributes to her recent diet change and exercise. She also describes chest pain, shortness of breath, dyspnea, and significant lower back pain.","Her medical history is significant for hypertension and diabetes. Her family history includes a father who had congestive heart failure at age 73 years. The patient gets her eyes checked regularly. She has never seen a pulmonary specialist. She reports aches and pains that vary, depending on how much physical activity she gets. She has had a hysterectomy. She is married and denies smoking, although she reports a history of continued secondhand smoke exposure."],"date":"October 16, 2020","figures":[],"markdown":"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\n\n **Authors:** Winston W. Tan, MD; Matthew Tan \n **Date:** October 16, 2020\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 63-year-old woman presents with a chronic cough. She was in her usual state of health until 3 months ago, when she developed a dry cough with fever. She was initially treated with antibiotics for 2 weeks. The cough improved, and the fever resolved. However, the dry cough returned.\nThe patient reports recent several instances of hemoptysis, as well as a 5-lb weight loss that she attributes to her recent diet change and exercise. She also describes chest pain, shortness of breath, dyspnea, and significant lower back pain.\nHer medical history is significant for hypertension and diabetes. Her family history includes a father who had congestive heart failure at age 73 years. The patient gets her eyes checked regularly. She has never seen a pulmonary specialist. She reports aches and pains that vary, depending on how much physical activity she gets. She has had a hysterectomy. She is married and denies smoking, although she reports a history of continued secondhand smoke exposure.\n\n ## Figures\n\n \n*Page 1 of 6*","pagination":{"current_page":1,"total_pages":6},"questionnaire":[],"title":"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old"},{"authors":"Winston W. Tan, MD; Matthew Tan","content":["Physical examination reveals the following:","Blood pressure: 124/58 mm Hg","Temperature: 98.3°F (36.8°C)","Heart rate: 85 beats/min","Examination of her neck reveals enlarged supraclavicular lymph nodes. Examination of her breasts reveals no distinct nodules, lumps, discharge, skin retraction, or axillary adenopathy. Her abdomen is soft, benign, and nontender. Neurologically, cranial nerves II through XII are grossly intact.","Upon evaluation of the lungs, wheezing and atelectasis are observed. Increased work of breathing is also noted. A chest radiograph is subsequently ordered."],"date":"October 16, 2020","figures":[],"markdown":"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\n\n **Authors:** Winston W. Tan, MD; Matthew Tan \n **Date:** October 16, 2020\n\n ## Content\n\n Physical examination reveals the following:\nBlood pressure: 124/58 mm Hg\nTemperature: 98.3°F (36.8°C)\nHeart rate: 85 beats/min\nExamination of her neck reveals enlarged supraclavicular lymph nodes. Examination of her breasts reveals no distinct nodules, lumps, discharge, skin retraction, or axillary adenopathy. Her abdomen is soft, benign, and nontender. Neurologically, cranial nerves II through XII are grossly intact.\nUpon evaluation of the lungs, wheezing and atelectasis are observed. Increased work of breathing is also noted. A chest radiograph is subsequently ordered.\n\n ## Figures\n\n \n*Page 2 of 6*","pagination":{"current_page":2,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":831357,"choiceText":"Sarcoidosis","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831359,"choiceText":"Lung cancer","correct":true,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831361,"choiceText":"Tuberculosis","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831363,"choiceText":"Pneumonia \r\n","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"","displayOrder":1,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":261411,"questionText":"Based only on these findings, which of the following is the most likely diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old"},{"authors":"Winston W. Tan, MD; Matthew Tan","content":["Lung cancer is often insidious, failing to produce clear symptoms until advanced disease. A high index of suspicion is required to properly identify this disease in most patients. In this case, weight loss, hemoptysis, and a history of secondhand smoke exposure, along with a low-grade fever and irregularities upon lung evaluation, warranted an investigation for lung cancer. Subsequently, CT revealed a 1.3-cm left upper lobe complex nodule (Figure 1).","Figure 1.","The patient underwent a left upper lobectomy with mediastinal lymph node dissection for a 1.5-cm poorly differentiated squamous cancer of lung, with 1 (station 5) of 18 lymph nodes positive with a microscopic focus of cancer. She was subsequently treated with adjuvant chemoradiation therapy, consisting of cisplatin and docetaxel concurrent with radiation. However, chemotherapy was stopped after a few doses owing to complications.","The patient later developed a seizure and was hospitalized; MRI of the brain was negative for metastatic disease but suggested possible temporal lobe inflammation. Her cerebrospinal fluid was positive for herpes. She was started on phenytoin and valacyclovir.","She completed radiation therapy to 6120 cGy. Additional planned chemotherapy was delayed owing to the patient's debility. She also experienced an outbreak of shingles. Serial follow-up every 4 months showed that disease was in complete remission, with a stable postradiation residual scar in the left lung.","Figure 2.","Figure 3.","Six years later, CT revealed a new enhancing mass in the medial right upper lobe (adjacent to the mediastinum) that was suspicious for metastatic or new primary lung cancer (Figure 2). A brain scan was negative for metastases. PET revealed uptake in the expected area and indeterminate uptake in a right hilar node (Figure 3), but was otherwise negative. Pulmonary function tests revealed showed an FEV1 of 1.45 L, or 65% of predicted. The diffusing capacity of the lung for carbon monoxide (DLCO) was 42%. Saturation was normal at rest but decreased to 92% with exercise.","Endobronchial ultrasonography did not reveal any specific abnormality. The mucosa was friable. A right hilar lymph node was sampled, but no lymphoid elements were obtained. Nothing specific for the tumor area was seen.","Figure 4.","A CT-guided biopsy was nondiagnostic. Surgical exploration yielded a small cell carcinoma that was unresectable owing to mediastinal invasion and bleeding (Figure 4). The patient started palliative chemotherapy with carboplatin/etoposide, with etoposide given orally on days 2 and 3. She completed four cycles of this chemotherapy and tolerated chemotherapy well overall.","Follow-up CT showed minimal residual density in the area of the prior lesion. As a result of excellent response, she was referred for proton therapy, because standard radiation was not feasible owing to prior dosing.","Induction chemotherapy was followed by consolidation radiation. The patient subsequently underwent proton radiation to the residual chest mass. She experienced a seizure; she was dehydrated, and was started on anticonvulsant and became stable. MRI of the brain revealed an area of right anterior temporal encephalomalacia. She is doing well currently and is under active surveillance for her cancer."],"date":"October 16, 2020","figures":[{"caption":"Figure 1.","image_url":"https://img.medscapestatic.com/article/842/258/842258-Thumb1a.png"},{"caption":"Figure 2.","image_url":"https://img.medscapestatic.com/article/842/258/842258-Thumb2a.png"},{"caption":"Figure 3.","image_url":"https://img.medscapestatic.com/article/842/258/842258-Thumb3a.png"},{"caption":"Figure 4.","image_url":"https://img.medscapestatic.com/article/842/258/842258-Thumb4a.png"}],"markdown":"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\n\n **Authors:** Winston W. Tan, MD; Matthew Tan \n **Date:** October 16, 2020\n\n ## Content\n\n Lung cancer is often insidious, failing to produce clear symptoms until advanced disease. A high index of suspicion is required to properly identify this disease in most patients. In this case, weight loss, hemoptysis, and a history of secondhand smoke exposure, along with a low-grade fever and irregularities upon lung evaluation, warranted an investigation for lung cancer. Subsequently, CT revealed a 1.3-cm left upper lobe complex nodule (Figure 1).\nFigure 1.\nThe patient underwent a left upper lobectomy with mediastinal lymph node dissection for a 1.5-cm poorly differentiated squamous cancer of lung, with 1 (station 5) of 18 lymph nodes positive with a microscopic focus of cancer. She was subsequently treated with adjuvant chemoradiation therapy, consisting of cisplatin and docetaxel concurrent with radiation. However, chemotherapy was stopped after a few doses owing to complications.\nThe patient later developed a seizure and was hospitalized; MRI of the brain was negative for metastatic disease but suggested possible temporal lobe inflammation. Her cerebrospinal fluid was positive for herpes. She was started on phenytoin and valacyclovir.\nShe completed radiation therapy to 6120 cGy. Additional planned chemotherapy was delayed owing to the patient's debility. She also experienced an outbreak of shingles. Serial follow-up every 4 months showed that disease was in complete remission, with a stable postradiation residual scar in the left lung.\nFigure 2.\nFigure 3.\nSix years later, CT revealed a new enhancing mass in the medial right upper lobe (adjacent to the mediastinum) that was suspicious for metastatic or new primary lung cancer (Figure 2). A brain scan was negative for metastases. PET revealed uptake in the expected area and indeterminate uptake in a right hilar node (Figure 3), but was otherwise negative. Pulmonary function tests revealed showed an FEV1 of 1.45 L, or 65% of predicted. The diffusing capacity of the lung for carbon monoxide (DLCO) was 42%. Saturation was normal at rest but decreased to 92% with exercise.\nEndobronchial ultrasonography did not reveal any specific abnormality. The mucosa was friable. A right hilar lymph node was sampled, but no lymphoid elements were obtained. Nothing specific for the tumor area was seen.\nFigure 4.\nA CT-guided biopsy was nondiagnostic. Surgical exploration yielded a small cell carcinoma that was unresectable owing to mediastinal invasion and bleeding (Figure 4). The patient started palliative chemotherapy with carboplatin/etoposide, with etoposide given orally on days 2 and 3. She completed four cycles of this chemotherapy and tolerated chemotherapy well overall.\nFollow-up CT showed minimal residual density in the area of the prior lesion. As a result of excellent response, she was referred for proton therapy, because standard radiation was not feasible owing to prior dosing.\nInduction chemotherapy was followed by consolidation radiation. The patient subsequently underwent proton radiation to the residual chest mass. She experienced a seizure; she was dehydrated, and was started on anticonvulsant and became stable. MRI of the brain revealed an area of right anterior temporal encephalomalacia. She is doing well currently and is under active surveillance for her cancer.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4.** \n \n\n\n*Page 3 of 6*","pagination":{"current_page":3,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":831357,"choiceText":"Sarcoidosis","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831359,"choiceText":"Lung cancer","correct":true,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831361,"choiceText":"Tuberculosis","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831363,"choiceText":"Pneumonia \r\n","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"","displayOrder":1,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":261411,"questionText":"Based only on these findings, which of the following is the most likely diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old"},{"authors":"Winston W. Tan, MD; Matthew Tan","content":["Non-small cell lung cancer accounts for approximately 85% of all lung cancers. Histologically, it is divided into adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Patients with non-small cell lung cancer require a complete staging work-up to evaluate the extent of disease because stage plays a major role in determining the choice of treatment.[1]","The patient in this case has the typical presentation of chronic cough. Typically, a cough that is initially thought to be an infection is noted. A chronic cough without improvement of symptoms despite treatment for infection should prompt further evaluation for potential lung mass. CT of the chest is often used as a diagnostic tool to clarify the suspicion of a lung mass.[2]","Because of the importance of stage in the therapeutic decision-making process, all patients must undergo proper staging of disease. A complete staging work-up should be performed to evaluate the extent of disease. In the United States, the standard staging work-up includes the following:","CT of the chest and upper abdomen","Complete blood count with differential","Serum chemistry studies, including creatinine, electrolytes, and calcium","Alkaline phosphate","Aspartate aminotransferase","Pulmonary function testing","Mediastinoscopy (if surgical resection is considered)","The information obtained from these tests guides additional testing (eg, imaging studies). Invasive staging procedures (eg, mediastinoscopy, mediastinotomy) may be required to assess mediastinal lymph nodes in patients who may undergo surgical resection. PET may be useful in detecting affected nodes, which may influence decisions about operability.","Paraneoplastic syndromes are more likely to occur in small cell lung cancer than in non-small cell lung cancer. Patients are at risk for the following:","Cushing syndrome","Lambert-Eaton myasthenic syndrome (Onset of proximal lower-extremity weakness is gradual; proximal upper-extremity weakness is usually less noticeable; the syndrome may be worse in the morning and improve during the day; although extraocular muscle involvement is uncommon, ptosis is often found)","Hypercalcemia (usually occurs with squamous cell carcinoma)","Syndrome of inappropriate antidiuretic hormone secretion","Enlargement of the extremities and painful, swollen joints (hypertrophic osteoarthropathy)"],"date":"October 16, 2020","figures":[],"markdown":"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\n\n **Authors:** Winston W. Tan, MD; Matthew Tan \n **Date:** October 16, 2020\n\n ## Content\n\n Non-small cell lung cancer accounts for approximately 85% of all lung cancers. Histologically, it is divided into adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Patients with non-small cell lung cancer require a complete staging work-up to evaluate the extent of disease because stage plays a major role in determining the choice of treatment.[1]\nThe patient in this case has the typical presentation of chronic cough. Typically, a cough that is initially thought to be an infection is noted. A chronic cough without improvement of symptoms despite treatment for infection should prompt further evaluation for potential lung mass. CT of the chest is often used as a diagnostic tool to clarify the suspicion of a lung mass.[2]\nBecause of the importance of stage in the therapeutic decision-making process, all patients must undergo proper staging of disease. A complete staging work-up should be performed to evaluate the extent of disease. In the United States, the standard staging work-up includes the following:\nCT of the chest and upper abdomen\nComplete blood count with differential\nSerum chemistry studies, including creatinine, electrolytes, and calcium\nAlkaline phosphate\nAspartate aminotransferase\nPulmonary function testing\nMediastinoscopy (if surgical resection is considered)\nThe information obtained from these tests guides additional testing (eg, imaging studies). Invasive staging procedures (eg, mediastinoscopy, mediastinotomy) may be required to assess mediastinal lymph nodes in patients who may undergo surgical resection. PET may be useful in detecting affected nodes, which may influence decisions about operability.\nParaneoplastic syndromes are more likely to occur in small cell lung cancer than in non-small cell lung cancer. Patients are at risk for the following:\nCushing syndrome\nLambert-Eaton myasthenic syndrome (Onset of proximal lower-extremity weakness is gradual; proximal upper-extremity weakness is usually less noticeable; the syndrome may be worse in the morning and improve during the day; although extraocular muscle involvement is uncommon, ptosis is often found)\nHypercalcemia (usually occurs with squamous cell carcinoma)\nSyndrome of inappropriate antidiuretic hormone secretion\nEnlargement of the extremities and painful, swollen joints (hypertrophic osteoarthropathy)\n\n ## Figures\n\n \n*Page 4 of 6*","pagination":{"current_page":4,"total_pages":6},"questionnaire":[],"title":"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old"},{"authors":"Winston W. Tan, MD; Matthew Tan","content":["The standard treatment for stage I and II disease is surgical resection. In stage IIIA, chemotherapy is indicated, as is surgical resection in selected patients. Standard treatment of stage IIIb is chemoradiation. Stage IV requires cisplatin-based chemotherapy or surgical resection if a solitary metastatic lesion with resectable primary tumor is present.[3,4,5]","This patient underwent resection of the cancer. Owing to her residual disease and because her lymph nodes were positive, she was treated with chemoradiation. Surgical resection is the primary modality of treatment for early stage non-small cell lung cancer.[6]","Close surveillance of patients with cancer should be the standard after completion of therapy. This patient had a contralateral hilar recurrence 6 years later. When a patient has a recurrence, it must be determined whether it is the same cancer or another primary cancer. This patient had another primary cancer, specifically small cell cancer of the lung. Biopsy must be done of a new recurrence, because it could be an entirely different cancer.","Approximately 60%-70% of patients with small cell lung cancer have clinically disseminated or extensive disease at presentation. Extensive-stage small cell lung cancer is incurable. When given combination chemotherapy, patients with extensive-stage disease have a complete response rate of more than 20% and a median survival longer than 7 months; however, only 2% are alive at 5 years.","For individuals with limited-stage disease that is treated with combination chemotherapy plus chest radiation, a complete response rate of 80% and survival of 17 months have been reported; 12%-15% of patients are alive at 5 years.[1]","Recommendations from the National Comprehensive Cancer Network (NCCN) regarding cancer surveillance in survivors of non-small cell lung cancer include the following:","History and physical examination, and chest CT with or without contrast, every 6-12 months for 2 years, then history and physical examination and noncontrast chest CT annually","Assessment of smoking status at each visit, with counseling and referral for smoking cessation as needed","Other NCCN recommendations for long-term follow-up care include the following:","Immunization: Annual influenza vaccination, pneumococcal vaccination with revaccination as appropriate, herpes zoster vaccination","Counseling regarding health promotion and wellness (eg, regular physical activity, healthy diet)","Routine health monitoring","Several important points should be remembered:","Persistent cough despite treatment should prompt further diagnostic testing for lung mass.","Nonsmokers can develop lung cancer.","Neurologic symptoms in patients with lung cancer do not always mean brain metastasis. Although brain metastasis should be ruled out, other causes could be found, such as encephalomalacia.","Biopsy of recurrent cancer should be redone, especially if the time to recurrence is more than a few years. A separate cancer can be found in a patient previously cured of their cancer.","Several factors may increase the likelihood of a primary cancer resulting in a secondary cancer. A \"field effect\" is noted in certain types of cancers, particularly in the areas of respiratory tract. In smokers, this is especially true in such areas as the head and neck, throat, laryngeal, esophageal area, and tongue. Because the body's immune system is vulnerable to the development of the first cancer, it may be more susceptible to the development of a second cancer."],"date":"October 16, 2020","figures":[],"markdown":"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\n\n **Authors:** Winston W. Tan, MD; Matthew Tan \n **Date:** October 16, 2020\n\n ## Content\n\n The standard treatment for stage I and II disease is surgical resection. In stage IIIA, chemotherapy is indicated, as is surgical resection in selected patients. Standard treatment of stage IIIb is chemoradiation. Stage IV requires cisplatin-based chemotherapy or surgical resection if a solitary metastatic lesion with resectable primary tumor is present.[3,4,5]\nThis patient underwent resection of the cancer. Owing to her residual disease and because her lymph nodes were positive, she was treated with chemoradiation. Surgical resection is the primary modality of treatment for early stage non-small cell lung cancer.[6]\nClose surveillance of patients with cancer should be the standard after completion of therapy. This patient had a contralateral hilar recurrence 6 years later. When a patient has a recurrence, it must be determined whether it is the same cancer or another primary cancer. This patient had another primary cancer, specifically small cell cancer of the lung. Biopsy must be done of a new recurrence, because it could be an entirely different cancer.\nApproximately 60%-70% of patients with small cell lung cancer have clinically disseminated or extensive disease at presentation. Extensive-stage small cell lung cancer is incurable. When given combination chemotherapy, patients with extensive-stage disease have a complete response rate of more than 20% and a median survival longer than 7 months; however, only 2% are alive at 5 years.\nFor individuals with limited-stage disease that is treated with combination chemotherapy plus chest radiation, a complete response rate of 80% and survival of 17 months have been reported; 12%-15% of patients are alive at 5 years.[1]\nRecommendations from the National Comprehensive Cancer Network (NCCN) regarding cancer surveillance in survivors of non-small cell lung cancer include the following:\nHistory and physical examination, and chest CT with or without contrast, every 6-12 months for 2 years, then history and physical examination and noncontrast chest CT annually\nAssessment of smoking status at each visit, with counseling and referral for smoking cessation as needed\nOther NCCN recommendations for long-term follow-up care include the following:\nImmunization: Annual influenza vaccination, pneumococcal vaccination with revaccination as appropriate, herpes zoster vaccination\nCounseling regarding health promotion and wellness (eg, regular physical activity, healthy diet)\nRoutine health monitoring\nSeveral important points should be remembered:\nPersistent cough despite treatment should prompt further diagnostic testing for lung mass.\nNonsmokers can develop lung cancer.\nNeurologic symptoms in patients with lung cancer do not always mean brain metastasis. Although brain metastasis should be ruled out, other causes could be found, such as encephalomalacia.\nBiopsy of recurrent cancer should be redone, especially if the time to recurrence is more than a few years. A separate cancer can be found in a patient previously cured of their cancer.\nSeveral factors may increase the likelihood of a primary cancer resulting in a secondary cancer. A \"field effect\" is noted in certain types of cancers, particularly in the areas of respiratory tract. In smokers, this is especially true in such areas as the head and neck, throat, laryngeal, esophageal area, and tongue. Because the body's immune system is vulnerable to the development of the first cancer, it may be more susceptible to the development of a second cancer.\n\n ## Figures\n\n \n*Page 5 of 6*","pagination":{"current_page":5,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":831365,"choiceText":"Adenocarcinoma","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831367,"choiceText":"Squamous cell carcinoma","correct":true,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831369,"choiceText":"Large-cell carcinoma","correct":false,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831371,"choiceText":"None of the above\r\n","correct":false,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"The most common metabolic abnormality associated with non-small cell lung cancer is hypercalcemia, which usually occurs with squamous cell carcinoma and results from secretion of parathyroid hormone-related peptide by the tumor. This can be distinguished from hyperparathyroidism by confirmation of normal serum parathyroid hormone levels.","displayOrder":2,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":261413,"questionText":"Which of the following is most commonly associated with hypercalcemia in patients with non-small cell lung cancer?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":831373,"choiceText":"Smoke exposure","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831375,"choiceText":"Family history","correct":false,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831377,"choiceText":"Poor diet","correct":true,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831379,"choiceText":"Chemical exposure","correct":false,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Smoking is the most well-recognized risk factor for lung cancer. Even secondhand exposure carries a significant risk. In addition, exposure to certain gases (eg, radon), asbestos, and other chemicals may increase the risk for lung cancer. Likewise, a family history of lung cancer increases risk for the disease.","displayOrder":3,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":261415,"questionText":"Which of the following is not considered a primary risk factor for lung cancer?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old"},{"authors":"Winston W. Tan, MD; Matthew Tan","content":[],"date":"October 16, 2020","figures":[],"markdown":"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\n\n **Authors:** Winston W. Tan, MD; Matthew Tan \n **Date:** October 16, 2020\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*","pagination":{"current_page":6,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":831365,"choiceText":"Adenocarcinoma","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831367,"choiceText":"Squamous cell carcinoma","correct":true,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831369,"choiceText":"Large-cell carcinoma","correct":false,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831371,"choiceText":"None of the above\r\n","correct":false,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"The most common metabolic abnormality associated with non-small cell lung cancer is hypercalcemia, which usually occurs with squamous cell carcinoma and results from secretion of parathyroid hormone-related peptide by the tumor. This can be distinguished from hyperparathyroidism by confirmation of normal serum parathyroid hormone levels.","displayOrder":2,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":261413,"questionText":"Which of the following is most commonly associated with hypercalcemia in patients with non-small cell lung cancer?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":831373,"choiceText":"Smoke exposure","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831375,"choiceText":"Family history","correct":false,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831377,"choiceText":"Poor diet","correct":true,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831379,"choiceText":"Chemical exposure","correct":false,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Smoking is the most well-recognized risk factor for lung cancer. Even secondhand exposure carries a significant risk. In addition, exposure to certain gases (eg, radon), asbestos, and other chemicals may increase the risk for lung cancer. Likewise, a family history of lung cancer increases risk for the disease.","displayOrder":3,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":261415,"questionText":"Which of the following is not considered a primary risk factor for lung cancer?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old"}],"string":"[\n {\n \"authors\": \"Winston W. Tan, MD; Matthew Tan\",\n \"content\": [\n \"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\",\n \"A 63-year-old woman presents with a chronic cough. She was in her usual state of health until 3 months ago, when she developed a dry cough with fever. She was initially treated with antibiotics for 2 weeks. The cough improved, and the fever resolved. However, the dry cough returned.\",\n \"The patient reports recent several instances of hemoptysis, as well as a 5-lb weight loss that she attributes to her recent diet change and exercise. She also describes chest pain, shortness of breath, dyspnea, and significant lower back pain.\",\n \"Her medical history is significant for hypertension and diabetes. Her family history includes a father who had congestive heart failure at age 73 years. The patient gets her eyes checked regularly. She has never seen a pulmonary specialist. She reports aches and pains that vary, depending on how much physical activity she gets. She has had a hysterectomy. She is married and denies smoking, although she reports a history of continued secondhand smoke exposure.\"\n ],\n \"date\": \"October 16, 2020\",\n \"figures\": [],\n \"markdown\": \"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\\n\\n **Authors:** Winston W. Tan, MD; Matthew Tan \\n **Date:** October 16, 2020\\n\\n ## Content\\n\\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\\nA 63-year-old woman presents with a chronic cough. She was in her usual state of health until 3 months ago, when she developed a dry cough with fever. She was initially treated with antibiotics for 2 weeks. The cough improved, and the fever resolved. However, the dry cough returned.\\nThe patient reports recent several instances of hemoptysis, as well as a 5-lb weight loss that she attributes to her recent diet change and exercise. She also describes chest pain, shortness of breath, dyspnea, and significant lower back pain.\\nHer medical history is significant for hypertension and diabetes. Her family history includes a father who had congestive heart failure at age 73 years. The patient gets her eyes checked regularly. She has never seen a pulmonary specialist. She reports aches and pains that vary, depending on how much physical activity she gets. She has had a hysterectomy. She is married and denies smoking, although she reports a history of continued secondhand smoke exposure.\\n\\n ## Figures\\n\\n \\n*Page 1 of 6*\",\n \"pagination\": {\n \"current_page\": 1,\n \"total_pages\": 6\n },\n \"questionnaire\": [],\n \"title\": \"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\"\n },\n {\n \"authors\": \"Winston W. Tan, MD; Matthew Tan\",\n \"content\": [\n \"Physical examination reveals the following:\",\n \"Blood pressure: 124/58 mm Hg\",\n \"Temperature: 98.3°F (36.8°C)\",\n \"Heart rate: 85 beats/min\",\n \"Examination of her neck reveals enlarged supraclavicular lymph nodes. Examination of her breasts reveals no distinct nodules, lumps, discharge, skin retraction, or axillary adenopathy. Her abdomen is soft, benign, and nontender. Neurologically, cranial nerves II through XII are grossly intact.\",\n \"Upon evaluation of the lungs, wheezing and atelectasis are observed. Increased work of breathing is also noted. A chest radiograph is subsequently ordered.\"\n ],\n \"date\": \"October 16, 2020\",\n \"figures\": [],\n \"markdown\": \"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\\n\\n **Authors:** Winston W. Tan, MD; Matthew Tan \\n **Date:** October 16, 2020\\n\\n ## Content\\n\\n Physical examination reveals the following:\\nBlood pressure: 124/58 mm Hg\\nTemperature: 98.3°F (36.8°C)\\nHeart rate: 85 beats/min\\nExamination of her neck reveals enlarged supraclavicular lymph nodes. Examination of her breasts reveals no distinct nodules, lumps, discharge, skin retraction, or axillary adenopathy. Her abdomen is soft, benign, and nontender. Neurologically, cranial nerves II through XII are grossly intact.\\nUpon evaluation of the lungs, wheezing and atelectasis are observed. Increased work of breathing is also noted. A chest radiograph is subsequently ordered.\\n\\n ## Figures\\n\\n \\n*Page 2 of 6*\",\n \"pagination\": {\n \"current_page\": 2,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 831357,\n \"choiceText\": \"Sarcoidosis\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831359,\n \"choiceText\": \"Lung cancer\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831361,\n \"choiceText\": \"Tuberculosis\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831363,\n \"choiceText\": \"Pneumonia \\r\\n\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\",\n \"displayOrder\": 1,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 261411,\n \"questionText\": \"Based only on these findings, which of the following is the most likely diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\"\n },\n {\n \"authors\": \"Winston W. Tan, MD; Matthew Tan\",\n \"content\": [\n \"Lung cancer is often insidious, failing to produce clear symptoms until advanced disease. A high index of suspicion is required to properly identify this disease in most patients. In this case, weight loss, hemoptysis, and a history of secondhand smoke exposure, along with a low-grade fever and irregularities upon lung evaluation, warranted an investigation for lung cancer. Subsequently, CT revealed a 1.3-cm left upper lobe complex nodule (Figure 1).\",\n \"Figure 1.\",\n \"The patient underwent a left upper lobectomy with mediastinal lymph node dissection for a 1.5-cm poorly differentiated squamous cancer of lung, with 1 (station 5) of 18 lymph nodes positive with a microscopic focus of cancer. She was subsequently treated with adjuvant chemoradiation therapy, consisting of cisplatin and docetaxel concurrent with radiation. However, chemotherapy was stopped after a few doses owing to complications.\",\n \"The patient later developed a seizure and was hospitalized; MRI of the brain was negative for metastatic disease but suggested possible temporal lobe inflammation. Her cerebrospinal fluid was positive for herpes. She was started on phenytoin and valacyclovir.\",\n \"She completed radiation therapy to 6120 cGy. Additional planned chemotherapy was delayed owing to the patient's debility. She also experienced an outbreak of shingles. Serial follow-up every 4 months showed that disease was in complete remission, with a stable postradiation residual scar in the left lung.\",\n \"Figure 2.\",\n \"Figure 3.\",\n \"Six years later, CT revealed a new enhancing mass in the medial right upper lobe (adjacent to the mediastinum) that was suspicious for metastatic or new primary lung cancer (Figure 2). A brain scan was negative for metastases. PET revealed uptake in the expected area and indeterminate uptake in a right hilar node (Figure 3), but was otherwise negative. Pulmonary function tests revealed showed an FEV1 of 1.45 L, or 65% of predicted. The diffusing capacity of the lung for carbon monoxide (DLCO) was 42%. Saturation was normal at rest but decreased to 92% with exercise.\",\n \"Endobronchial ultrasonography did not reveal any specific abnormality. The mucosa was friable. A right hilar lymph node was sampled, but no lymphoid elements were obtained. Nothing specific for the tumor area was seen.\",\n \"Figure 4.\",\n \"A CT-guided biopsy was nondiagnostic. Surgical exploration yielded a small cell carcinoma that was unresectable owing to mediastinal invasion and bleeding (Figure 4). The patient started palliative chemotherapy with carboplatin/etoposide, with etoposide given orally on days 2 and 3. She completed four cycles of this chemotherapy and tolerated chemotherapy well overall.\",\n \"Follow-up CT showed minimal residual density in the area of the prior lesion. As a result of excellent response, she was referred for proton therapy, because standard radiation was not feasible owing to prior dosing.\",\n \"Induction chemotherapy was followed by consolidation radiation. The patient subsequently underwent proton radiation to the residual chest mass. She experienced a seizure; she was dehydrated, and was started on anticonvulsant and became stable. MRI of the brain revealed an area of right anterior temporal encephalomalacia. She is doing well currently and is under active surveillance for her cancer.\"\n ],\n \"date\": \"October 16, 2020\",\n \"figures\": [\n {\n \"caption\": \"Figure 1.\",\n \"image_url\": \"https://img.medscapestatic.com/article/842/258/842258-Thumb1a.png\"\n },\n {\n \"caption\": \"Figure 2.\",\n \"image_url\": \"https://img.medscapestatic.com/article/842/258/842258-Thumb2a.png\"\n },\n {\n \"caption\": \"Figure 3.\",\n \"image_url\": \"https://img.medscapestatic.com/article/842/258/842258-Thumb3a.png\"\n },\n {\n \"caption\": \"Figure 4.\",\n \"image_url\": \"https://img.medscapestatic.com/article/842/258/842258-Thumb4a.png\"\n }\n ],\n \"markdown\": \"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\\n\\n **Authors:** Winston W. Tan, MD; Matthew Tan \\n **Date:** October 16, 2020\\n\\n ## Content\\n\\n Lung cancer is often insidious, failing to produce clear symptoms until advanced disease. A high index of suspicion is required to properly identify this disease in most patients. In this case, weight loss, hemoptysis, and a history of secondhand smoke exposure, along with a low-grade fever and irregularities upon lung evaluation, warranted an investigation for lung cancer. Subsequently, CT revealed a 1.3-cm left upper lobe complex nodule (Figure 1).\\nFigure 1.\\nThe patient underwent a left upper lobectomy with mediastinal lymph node dissection for a 1.5-cm poorly differentiated squamous cancer of lung, with 1 (station 5) of 18 lymph nodes positive with a microscopic focus of cancer. She was subsequently treated with adjuvant chemoradiation therapy, consisting of cisplatin and docetaxel concurrent with radiation. However, chemotherapy was stopped after a few doses owing to complications.\\nThe patient later developed a seizure and was hospitalized; MRI of the brain was negative for metastatic disease but suggested possible temporal lobe inflammation. Her cerebrospinal fluid was positive for herpes. She was started on phenytoin and valacyclovir.\\nShe completed radiation therapy to 6120 cGy. Additional planned chemotherapy was delayed owing to the patient's debility. She also experienced an outbreak of shingles. Serial follow-up every 4 months showed that disease was in complete remission, with a stable postradiation residual scar in the left lung.\\nFigure 2.\\nFigure 3.\\nSix years later, CT revealed a new enhancing mass in the medial right upper lobe (adjacent to the mediastinum) that was suspicious for metastatic or new primary lung cancer (Figure 2). A brain scan was negative for metastases. PET revealed uptake in the expected area and indeterminate uptake in a right hilar node (Figure 3), but was otherwise negative. Pulmonary function tests revealed showed an FEV1 of 1.45 L, or 65% of predicted. The diffusing capacity of the lung for carbon monoxide (DLCO) was 42%. Saturation was normal at rest but decreased to 92% with exercise.\\nEndobronchial ultrasonography did not reveal any specific abnormality. The mucosa was friable. A right hilar lymph node was sampled, but no lymphoid elements were obtained. Nothing specific for the tumor area was seen.\\nFigure 4.\\nA CT-guided biopsy was nondiagnostic. Surgical exploration yielded a small cell carcinoma that was unresectable owing to mediastinal invasion and bleeding (Figure 4). The patient started palliative chemotherapy with carboplatin/etoposide, with etoposide given orally on days 2 and 3. She completed four cycles of this chemotherapy and tolerated chemotherapy well overall.\\nFollow-up CT showed minimal residual density in the area of the prior lesion. As a result of excellent response, she was referred for proton therapy, because standard radiation was not feasible owing to prior dosing.\\nInduction chemotherapy was followed by consolidation radiation. The patient subsequently underwent proton radiation to the residual chest mass. She experienced a seizure; she was dehydrated, and was started on anticonvulsant and became stable. MRI of the brain revealed an area of right anterior temporal encephalomalacia. She is doing well currently and is under active surveillance for her cancer.\\n\\n ## Figures\\n\\n **Figure 1.** \\n \\n\\n**Figure 2.** \\n \\n\\n**Figure 3.** \\n \\n\\n**Figure 4.** \\n \\n\\n\\n*Page 3 of 6*\",\n \"pagination\": {\n \"current_page\": 3,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 831357,\n \"choiceText\": \"Sarcoidosis\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831359,\n \"choiceText\": \"Lung cancer\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831361,\n \"choiceText\": \"Tuberculosis\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831363,\n \"choiceText\": \"Pneumonia \\r\\n\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\",\n \"displayOrder\": 1,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 261411,\n \"questionText\": \"Based only on these findings, which of the following is the most likely diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\"\n },\n {\n \"authors\": \"Winston W. Tan, MD; Matthew Tan\",\n \"content\": [\n \"Non-small cell lung cancer accounts for approximately 85% of all lung cancers. Histologically, it is divided into adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Patients with non-small cell lung cancer require a complete staging work-up to evaluate the extent of disease because stage plays a major role in determining the choice of treatment.[1]\",\n \"The patient in this case has the typical presentation of chronic cough. Typically, a cough that is initially thought to be an infection is noted. A chronic cough without improvement of symptoms despite treatment for infection should prompt further evaluation for potential lung mass. CT of the chest is often used as a diagnostic tool to clarify the suspicion of a lung mass.[2]\",\n \"Because of the importance of stage in the therapeutic decision-making process, all patients must undergo proper staging of disease. A complete staging work-up should be performed to evaluate the extent of disease. In the United States, the standard staging work-up includes the following:\",\n \"CT of the chest and upper abdomen\",\n \"Complete blood count with differential\",\n \"Serum chemistry studies, including creatinine, electrolytes, and calcium\",\n \"Alkaline phosphate\",\n \"Aspartate aminotransferase\",\n \"Pulmonary function testing\",\n \"Mediastinoscopy (if surgical resection is considered)\",\n \"The information obtained from these tests guides additional testing (eg, imaging studies). Invasive staging procedures (eg, mediastinoscopy, mediastinotomy) may be required to assess mediastinal lymph nodes in patients who may undergo surgical resection. PET may be useful in detecting affected nodes, which may influence decisions about operability.\",\n \"Paraneoplastic syndromes are more likely to occur in small cell lung cancer than in non-small cell lung cancer. Patients are at risk for the following:\",\n \"Cushing syndrome\",\n \"Lambert-Eaton myasthenic syndrome (Onset of proximal lower-extremity weakness is gradual; proximal upper-extremity weakness is usually less noticeable; the syndrome may be worse in the morning and improve during the day; although extraocular muscle involvement is uncommon, ptosis is often found)\",\n \"Hypercalcemia (usually occurs with squamous cell carcinoma)\",\n \"Syndrome of inappropriate antidiuretic hormone secretion\",\n \"Enlargement of the extremities and painful, swollen joints (hypertrophic osteoarthropathy)\"\n ],\n \"date\": \"October 16, 2020\",\n \"figures\": [],\n \"markdown\": \"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\\n\\n **Authors:** Winston W. Tan, MD; Matthew Tan \\n **Date:** October 16, 2020\\n\\n ## Content\\n\\n Non-small cell lung cancer accounts for approximately 85% of all lung cancers. Histologically, it is divided into adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Patients with non-small cell lung cancer require a complete staging work-up to evaluate the extent of disease because stage plays a major role in determining the choice of treatment.[1]\\nThe patient in this case has the typical presentation of chronic cough. Typically, a cough that is initially thought to be an infection is noted. A chronic cough without improvement of symptoms despite treatment for infection should prompt further evaluation for potential lung mass. CT of the chest is often used as a diagnostic tool to clarify the suspicion of a lung mass.[2]\\nBecause of the importance of stage in the therapeutic decision-making process, all patients must undergo proper staging of disease. A complete staging work-up should be performed to evaluate the extent of disease. In the United States, the standard staging work-up includes the following:\\nCT of the chest and upper abdomen\\nComplete blood count with differential\\nSerum chemistry studies, including creatinine, electrolytes, and calcium\\nAlkaline phosphate\\nAspartate aminotransferase\\nPulmonary function testing\\nMediastinoscopy (if surgical resection is considered)\\nThe information obtained from these tests guides additional testing (eg, imaging studies). Invasive staging procedures (eg, mediastinoscopy, mediastinotomy) may be required to assess mediastinal lymph nodes in patients who may undergo surgical resection. PET may be useful in detecting affected nodes, which may influence decisions about operability.\\nParaneoplastic syndromes are more likely to occur in small cell lung cancer than in non-small cell lung cancer. Patients are at risk for the following:\\nCushing syndrome\\nLambert-Eaton myasthenic syndrome (Onset of proximal lower-extremity weakness is gradual; proximal upper-extremity weakness is usually less noticeable; the syndrome may be worse in the morning and improve during the day; although extraocular muscle involvement is uncommon, ptosis is often found)\\nHypercalcemia (usually occurs with squamous cell carcinoma)\\nSyndrome of inappropriate antidiuretic hormone secretion\\nEnlargement of the extremities and painful, swollen joints (hypertrophic osteoarthropathy)\\n\\n ## Figures\\n\\n \\n*Page 4 of 6*\",\n \"pagination\": {\n \"current_page\": 4,\n \"total_pages\": 6\n },\n \"questionnaire\": [],\n \"title\": \"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\"\n },\n {\n \"authors\": \"Winston W. Tan, MD; Matthew Tan\",\n \"content\": [\n \"The standard treatment for stage I and II disease is surgical resection. In stage IIIA, chemotherapy is indicated, as is surgical resection in selected patients. Standard treatment of stage IIIb is chemoradiation. Stage IV requires cisplatin-based chemotherapy or surgical resection if a solitary metastatic lesion with resectable primary tumor is present.[3,4,5]\",\n \"This patient underwent resection of the cancer. Owing to her residual disease and because her lymph nodes were positive, she was treated with chemoradiation. Surgical resection is the primary modality of treatment for early stage non-small cell lung cancer.[6]\",\n \"Close surveillance of patients with cancer should be the standard after completion of therapy. This patient had a contralateral hilar recurrence 6 years later. When a patient has a recurrence, it must be determined whether it is the same cancer or another primary cancer. This patient had another primary cancer, specifically small cell cancer of the lung. Biopsy must be done of a new recurrence, because it could be an entirely different cancer.\",\n \"Approximately 60%-70% of patients with small cell lung cancer have clinically disseminated or extensive disease at presentation. Extensive-stage small cell lung cancer is incurable. When given combination chemotherapy, patients with extensive-stage disease have a complete response rate of more than 20% and a median survival longer than 7 months; however, only 2% are alive at 5 years.\",\n \"For individuals with limited-stage disease that is treated with combination chemotherapy plus chest radiation, a complete response rate of 80% and survival of 17 months have been reported; 12%-15% of patients are alive at 5 years.[1]\",\n \"Recommendations from the National Comprehensive Cancer Network (NCCN) regarding cancer surveillance in survivors of non-small cell lung cancer include the following:\",\n \"History and physical examination, and chest CT with or without contrast, every 6-12 months for 2 years, then history and physical examination and noncontrast chest CT annually\",\n \"Assessment of smoking status at each visit, with counseling and referral for smoking cessation as needed\",\n \"Other NCCN recommendations for long-term follow-up care include the following:\",\n \"Immunization: Annual influenza vaccination, pneumococcal vaccination with revaccination as appropriate, herpes zoster vaccination\",\n \"Counseling regarding health promotion and wellness (eg, regular physical activity, healthy diet)\",\n \"Routine health monitoring\",\n \"Several important points should be remembered:\",\n \"Persistent cough despite treatment should prompt further diagnostic testing for lung mass.\",\n \"Nonsmokers can develop lung cancer.\",\n \"Neurologic symptoms in patients with lung cancer do not always mean brain metastasis. Although brain metastasis should be ruled out, other causes could be found, such as encephalomalacia.\",\n \"Biopsy of recurrent cancer should be redone, especially if the time to recurrence is more than a few years. A separate cancer can be found in a patient previously cured of their cancer.\",\n \"Several factors may increase the likelihood of a primary cancer resulting in a secondary cancer. A \\\"field effect\\\" is noted in certain types of cancers, particularly in the areas of respiratory tract. In smokers, this is especially true in such areas as the head and neck, throat, laryngeal, esophageal area, and tongue. Because the body's immune system is vulnerable to the development of the first cancer, it may be more susceptible to the development of a second cancer.\"\n ],\n \"date\": \"October 16, 2020\",\n \"figures\": [],\n \"markdown\": \"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\\n\\n **Authors:** Winston W. Tan, MD; Matthew Tan \\n **Date:** October 16, 2020\\n\\n ## Content\\n\\n The standard treatment for stage I and II disease is surgical resection. In stage IIIA, chemotherapy is indicated, as is surgical resection in selected patients. Standard treatment of stage IIIb is chemoradiation. Stage IV requires cisplatin-based chemotherapy or surgical resection if a solitary metastatic lesion with resectable primary tumor is present.[3,4,5]\\nThis patient underwent resection of the cancer. Owing to her residual disease and because her lymph nodes were positive, she was treated with chemoradiation. Surgical resection is the primary modality of treatment for early stage non-small cell lung cancer.[6]\\nClose surveillance of patients with cancer should be the standard after completion of therapy. This patient had a contralateral hilar recurrence 6 years later. When a patient has a recurrence, it must be determined whether it is the same cancer or another primary cancer. This patient had another primary cancer, specifically small cell cancer of the lung. Biopsy must be done of a new recurrence, because it could be an entirely different cancer.\\nApproximately 60%-70% of patients with small cell lung cancer have clinically disseminated or extensive disease at presentation. Extensive-stage small cell lung cancer is incurable. When given combination chemotherapy, patients with extensive-stage disease have a complete response rate of more than 20% and a median survival longer than 7 months; however, only 2% are alive at 5 years.\\nFor individuals with limited-stage disease that is treated with combination chemotherapy plus chest radiation, a complete response rate of 80% and survival of 17 months have been reported; 12%-15% of patients are alive at 5 years.[1]\\nRecommendations from the National Comprehensive Cancer Network (NCCN) regarding cancer surveillance in survivors of non-small cell lung cancer include the following:\\nHistory and physical examination, and chest CT with or without contrast, every 6-12 months for 2 years, then history and physical examination and noncontrast chest CT annually\\nAssessment of smoking status at each visit, with counseling and referral for smoking cessation as needed\\nOther NCCN recommendations for long-term follow-up care include the following:\\nImmunization: Annual influenza vaccination, pneumococcal vaccination with revaccination as appropriate, herpes zoster vaccination\\nCounseling regarding health promotion and wellness (eg, regular physical activity, healthy diet)\\nRoutine health monitoring\\nSeveral important points should be remembered:\\nPersistent cough despite treatment should prompt further diagnostic testing for lung mass.\\nNonsmokers can develop lung cancer.\\nNeurologic symptoms in patients with lung cancer do not always mean brain metastasis. Although brain metastasis should be ruled out, other causes could be found, such as encephalomalacia.\\nBiopsy of recurrent cancer should be redone, especially if the time to recurrence is more than a few years. A separate cancer can be found in a patient previously cured of their cancer.\\nSeveral factors may increase the likelihood of a primary cancer resulting in a secondary cancer. A \\\"field effect\\\" is noted in certain types of cancers, particularly in the areas of respiratory tract. In smokers, this is especially true in such areas as the head and neck, throat, laryngeal, esophageal area, and tongue. Because the body's immune system is vulnerable to the development of the first cancer, it may be more susceptible to the development of a second cancer.\\n\\n ## Figures\\n\\n \\n*Page 5 of 6*\",\n \"pagination\": {\n \"current_page\": 5,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 831365,\n \"choiceText\": \"Adenocarcinoma\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831367,\n \"choiceText\": \"Squamous cell carcinoma\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831369,\n \"choiceText\": \"Large-cell carcinoma\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831371,\n \"choiceText\": \"None of the above\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"The most common metabolic abnormality associated with non-small cell lung cancer is hypercalcemia, which usually occurs with squamous cell carcinoma and results from secretion of parathyroid hormone-related peptide by the tumor. This can be distinguished from hyperparathyroidism by confirmation of normal serum parathyroid hormone levels.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 261413,\n \"questionText\": \"Which of the following is most commonly associated with hypercalcemia in patients with non-small cell lung cancer?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 831373,\n \"choiceText\": \"Smoke exposure\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831375,\n \"choiceText\": \"Family history\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831377,\n \"choiceText\": \"Poor diet\",\n \"correct\": true,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831379,\n \"choiceText\": \"Chemical exposure\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Smoking is the most well-recognized risk factor for lung cancer. Even secondhand exposure carries a significant risk. In addition, exposure to certain gases (eg, radon), asbestos, and other chemicals may increase the risk for lung cancer. Likewise, a family history of lung cancer increases risk for the disease.\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 261415,\n \"questionText\": \"Which of the following is not considered a primary risk factor for lung cancer?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\"\n },\n {\n \"authors\": \"Winston W. Tan, MD; Matthew Tan\",\n \"content\": [],\n \"date\": \"October 16, 2020\",\n \"figures\": [],\n \"markdown\": \"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\\n\\n **Authors:** Winston W. Tan, MD; Matthew Tan \\n **Date:** October 16, 2020\\n\\n ## Content\\n\\n \\n\\n ## Figures\\n\\n \\n*Page 6 of 6*\",\n \"pagination\": {\n \"current_page\": 6,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 831365,\n \"choiceText\": \"Adenocarcinoma\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831367,\n \"choiceText\": \"Squamous cell carcinoma\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831369,\n \"choiceText\": \"Large-cell carcinoma\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831371,\n \"choiceText\": \"None of the above\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"The most common metabolic abnormality associated with non-small cell lung cancer is hypercalcemia, which usually occurs with squamous cell carcinoma and results from secretion of parathyroid hormone-related peptide by the tumor. This can be distinguished from hyperparathyroidism by confirmation of normal serum parathyroid hormone levels.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 261413,\n \"questionText\": \"Which of the following is most commonly associated with hypercalcemia in patients with non-small cell lung cancer?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 831373,\n \"choiceText\": \"Smoke exposure\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831375,\n \"choiceText\": \"Family history\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831377,\n \"choiceText\": \"Poor diet\",\n \"correct\": true,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831379,\n \"choiceText\": \"Chemical exposure\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Smoking is the most well-recognized risk factor for lung cancer. Even secondhand exposure carries a significant risk. In addition, exposure to certain gases (eg, radon), asbestos, and other chemicals may increase the risk for lung cancer. Likewise, a family history of lung cancer increases risk for the disease.\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 261415,\n \"questionText\": \"Which of the following is not considered a primary risk factor for lung cancer?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\"\n }\n]"},"questions":{"kind":"list like","value":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":831357,"choiceText":"Sarcoidosis","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831359,"choiceText":"Lung cancer","correct":true,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831361,"choiceText":"Tuberculosis","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831363,"choiceText":"Pneumonia \r\n","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"","displayOrder":1,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":261411,"questionText":"Based only on these findings, which of the following is the most likely diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":831365,"choiceText":"Adenocarcinoma","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831367,"choiceText":"Squamous cell carcinoma","correct":true,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831369,"choiceText":"Large-cell carcinoma","correct":false,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831371,"choiceText":"None of the above\r\n","correct":false,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"The most common metabolic abnormality associated with non-small cell lung cancer is hypercalcemia, which usually occurs with squamous cell carcinoma and results from secretion of parathyroid hormone-related peptide by the tumor. This can be distinguished from hyperparathyroidism by confirmation of normal serum parathyroid hormone levels.","displayOrder":2,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":261413,"questionText":"Which of the following is most commonly associated with hypercalcemia in patients with non-small cell lung cancer?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":831373,"choiceText":"Smoke exposure","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831375,"choiceText":"Family history","correct":false,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831377,"choiceText":"Poor diet","correct":true,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831379,"choiceText":"Chemical exposure","correct":false,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Smoking is the most well-recognized risk factor for lung cancer. Even secondhand exposure carries a significant risk. In addition, exposure to certain gases (eg, radon), asbestos, and other chemicals may increase the risk for lung cancer. Likewise, a family history of lung cancer increases risk for the disease.","displayOrder":3,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":261415,"questionText":"Which of the following is not considered a primary risk factor for lung cancer?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"string":"[\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 831357,\n \"choiceText\": \"Sarcoidosis\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831359,\n \"choiceText\": \"Lung cancer\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831361,\n \"choiceText\": \"Tuberculosis\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831363,\n \"choiceText\": \"Pneumonia \\r\\n\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\",\n \"displayOrder\": 1,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 261411,\n \"questionText\": \"Based only on these findings, which of the following is the most likely diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 831365,\n \"choiceText\": \"Adenocarcinoma\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831367,\n \"choiceText\": \"Squamous cell carcinoma\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831369,\n \"choiceText\": \"Large-cell carcinoma\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831371,\n \"choiceText\": \"None of the above\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"The most common metabolic abnormality associated with non-small cell lung cancer is hypercalcemia, which usually occurs with squamous cell carcinoma and results from secretion of parathyroid hormone-related peptide by the tumor. This can be distinguished from hyperparathyroidism by confirmation of normal serum parathyroid hormone levels.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 261413,\n \"questionText\": \"Which of the following is most commonly associated with hypercalcemia in patients with non-small cell lung cancer?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 831373,\n \"choiceText\": \"Smoke exposure\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831375,\n \"choiceText\": \"Family history\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831377,\n \"choiceText\": \"Poor diet\",\n \"correct\": true,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831379,\n \"choiceText\": \"Chemical exposure\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Smoking is the most well-recognized risk factor for lung cancer. Even secondhand exposure carries a significant risk. In addition, exposure to certain gases (eg, radon), asbestos, and other chemicals may increase the risk for lung cancer. Likewise, a family history of lung cancer increases risk for the disease.\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 261415,\n \"questionText\": \"Which of the following is not considered a primary risk factor for lung cancer?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n]"}}},{"rowIdx":298,"cells":{"article_id":{"kind":"string","value":"938423"},"url":{"kind":"string","value":"/viewarticle/938423"},"article_data":{"kind":"list like","value":[{"authors":"Timothy D. Murphy, MD","content":["Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us .","A 5-year-old girl with a long-standing history of severe asthma and eczema presented to a pediatric pulmonary and sleep medicine clinic. Her asthma was stabilized with an inhaled corticosteroid (fluticasone, 88 µg, inhaled twice daily), albuterol sulfate (180 µg, inhaled as needed), and ipratropium bromide (34 µg, inhaled as needed). Her skin condition improved with a moderately aggressive regimen of hydrating bleach baths, moisturizing lotions, nonsedating antihistamines, and as-needed use of topical hydrocortisone or triamcinolone, pimecrolimus, and mupirocin.","Her asthma remained stable for a year but then progressed to the extent that the dosage of inhaled fluticasone was increased to 220 µg twice daily. Bronchoscopy revealed only mild bronchomalacia of the left mainstem bronchus (Figure 1), diffuse mild inflammation, and increased secretions.","Figure 1.","Montelukast (5 mg daily) and nasal fluticasone (50 µg) were added to her regimen. In addition, diphenhydramine (25 mg) was prescribed to be used as needed for excessive itchiness, eczema flares, and allergic asthma flares.","The patient remained well and was followed up in the clinic approximately every 3 months, owing to the complexity of her condition. After 6 months, significant weight gain and an increasing body mass index (BMI) were noted. She met with a dietitian, who recommended weight loss strategies. From the age of 7-8 years, the patient demonstrated a modest weight loss from the changes in her diet. However, symptoms of fatigue, excessive daytime sleepiness (EDS), and inattention in school developed over a 1- to 2-month period, and her weight started to increase rapidly despite the dietary intervention.","Her daytime sleepiness seemed to be progressive, and she would fall asleep suddenly even when she wanted to be awake. Concerned about the emerging symptoms of inattention, autistic features, fatigue, and sleepiness, the girl's parents are seeking further medical advice."],"date":"October 09, 2020","figures":[{"caption":"Figure 1.","image_url":"https://img.medscapestatic.com/article/938/423/938423-Thumb1.jpg"}],"markdown":"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\n\n **Authors:** Timothy D. Murphy, MD \n **Date:** October 09, 2020\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us .\nA 5-year-old girl with a long-standing history of severe asthma and eczema presented to a pediatric pulmonary and sleep medicine clinic. Her asthma was stabilized with an inhaled corticosteroid (fluticasone, 88 µg, inhaled twice daily), albuterol sulfate (180 µg, inhaled as needed), and ipratropium bromide (34 µg, inhaled as needed). Her skin condition improved with a moderately aggressive regimen of hydrating bleach baths, moisturizing lotions, nonsedating antihistamines, and as-needed use of topical hydrocortisone or triamcinolone, pimecrolimus, and mupirocin.\nHer asthma remained stable for a year but then progressed to the extent that the dosage of inhaled fluticasone was increased to 220 µg twice daily. Bronchoscopy revealed only mild bronchomalacia of the left mainstem bronchus (Figure 1), diffuse mild inflammation, and increased secretions.\nFigure 1.\nMontelukast (5 mg daily) and nasal fluticasone (50 µg) were added to her regimen. In addition, diphenhydramine (25 mg) was prescribed to be used as needed for excessive itchiness, eczema flares, and allergic asthma flares.\nThe patient remained well and was followed up in the clinic approximately every 3 months, owing to the complexity of her condition. After 6 months, significant weight gain and an increasing body mass index (BMI) were noted. She met with a dietitian, who recommended weight loss strategies. From the age of 7-8 years, the patient demonstrated a modest weight loss from the changes in her diet. However, symptoms of fatigue, excessive daytime sleepiness (EDS), and inattention in school developed over a 1- to 2-month period, and her weight started to increase rapidly despite the dietary intervention.\nHer daytime sleepiness seemed to be progressive, and she would fall asleep suddenly even when she wanted to be awake. Concerned about the emerging symptoms of inattention, autistic features, fatigue, and sleepiness, the girl's parents are seeking further medical advice.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 1 of 6*","pagination":{"current_page":1,"total_pages":6},"questionnaire":[],"title":"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma"},{"authors":"Timothy D. Murphy, MD","content":["The patient has fallen asleep at school nearly every day for the past 1-2 months and falls into a deep sleep unless she is kept active. At home, she is taking more naps during the day, falling asleep in the car, and struggling with schoolwork. Her grades have dropped significantly over the past few months. Her parents report that she does not awaken during the night. No snoring, choking, snorting, gasping, or apnea is noted. She sleeps an average of 9-10 hours per night but is restless and tosses and turns frequently in her sleep.","Her family history is notable for obesity, obstructive sleep apnea (OSA) that requires continuous positive airway pressure (CPAP) in her father, and narcolepsy in an uncle and a grandfather.","On physical examination, she has mild to moderate obesity (BMI of 23.89 kg/m2 [the 98th percentile for age]) and enlarged tonsils (2-3+). She has difficulty with focusing and staying awake in the clinic.","She is referred to a pediatric otolaryngologist for consideration of nocturnal polysomnography (NPSG) or an adenotonsillectomy. The otolaryngologist notes that she has not tolerated nasal fluticasone well, that she is a chronic mouth breather, and that her tonsils are enlarged (3+). An NPSG is ordered to help clarify matters.","The NPSG demonstrates the following:","A respiratory disturbance index and an apnea-hypopnea index (AHI) of 6.2 per hour","Sleep latency of 0.5 minutes and rapid eye movement (REM) latency of 0.5 minutes","A sleep efficiency of 87.5%","18.2% of total sleep time in stage N1, 36.4% in N2, 29.9% in N3, and 15.5% in REM sleep","An arousal index of 18.6","A periodic leg movement index of 6.3","Multiple periods of wakefulness scattered throughout the night and six REM periods"],"date":"October 09, 2020","figures":[],"markdown":"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\n\n **Authors:** Timothy D. Murphy, MD \n **Date:** October 09, 2020\n\n ## Content\n\n The patient has fallen asleep at school nearly every day for the past 1-2 months and falls into a deep sleep unless she is kept active. At home, she is taking more naps during the day, falling asleep in the car, and struggling with schoolwork. Her grades have dropped significantly over the past few months. Her parents report that she does not awaken during the night. No snoring, choking, snorting, gasping, or apnea is noted. She sleeps an average of 9-10 hours per night but is restless and tosses and turns frequently in her sleep.\nHer family history is notable for obesity, obstructive sleep apnea (OSA) that requires continuous positive airway pressure (CPAP) in her father, and narcolepsy in an uncle and a grandfather.\nOn physical examination, she has mild to moderate obesity (BMI of 23.89 kg/m2 [the 98th percentile for age]) and enlarged tonsils (2-3+). She has difficulty with focusing and staying awake in the clinic.\nShe is referred to a pediatric otolaryngologist for consideration of nocturnal polysomnography (NPSG) or an adenotonsillectomy. The otolaryngologist notes that she has not tolerated nasal fluticasone well, that she is a chronic mouth breather, and that her tonsils are enlarged (3+). An NPSG is ordered to help clarify matters.\nThe NPSG demonstrates the following:\nA respiratory disturbance index and an apnea-hypopnea index (AHI) of 6.2 per hour\nSleep latency of 0.5 minutes and rapid eye movement (REM) latency of 0.5 minutes\nA sleep efficiency of 87.5%\n18.2% of total sleep time in stage N1, 36.4% in N2, 29.9% in N3, and 15.5% in REM sleep\nAn arousal index of 18.6\nA periodic leg movement index of 6.3\nMultiple periods of wakefulness scattered throughout the night and six REM periods\n\n ## Figures\n\n \n*Page 2 of 6*","pagination":{"current_page":2,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1529064,"choiceText":"Behavioral insomnia of childhood\r\n","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529065,"choiceText":"Pediatric chronic obstructive pulmonary disease","correct":false,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529066,"choiceText":"Delayed sleep phase disorder","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529067,"choiceText":"Narcolepsy","correct":true,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"","displayOrder":1,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":490073,"questionText":"On the basis of these findings only, what is the most likely diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma"},{"authors":"Timothy D. Murphy, MD","content":["This case is very challenging because the patient had the findings of and met the criteria for OSA, periodic limb movement disorder (PLMD)/restless legs syndrome (RLS), and hypersomnolence. She also had several historical findings that were highly suggestive of narcolepsy with cataplexy. These included a strong family history of narcolepsy, a history of the sudden onset of sleep and greatly increased sleep pressure, and rapid weight gain. A critical finding was a nocturnal sleep-onset REM sleep period (SOREMP). A nocturnal SOREMP (defined as REM sleep within 15 minutes of falling asleep) has a very high specificity for narcolepsy with cataplexy in adults and children.[1,2] However, the importance of the nocturnal SOREMP was not initially noted in her evaluation and management.","OSA and PLMD were initially diagnosed, and the otolaryngologist performed an adenotonsillectomy. The patient returned to the pediatric pulmonary and sleep medicine clinic after the procedure. At 3 weeks after the surgery, her somnolence improved very little. She had been gaining weight more rapidly and symptoms of apparent instability in her asthma were noted.","Further history-taking revealed a complex set of interactions around eating (some involved her father catering to her desire for higher-carbohydrate foods), increased sedentary behavior, and a history suggestive of vocal cord dysfunction. She was having \"asthma attacks\" characterized by rapid onset with inspiratory stridor and rapid resolution at the onset of activity. Her family was willing to make changes in their diet and to encourage activity, and they sought help for the vocal cord dysfunction from a speech and language pathologist.","Despite these measures, her weight gain rapidly progressed and the daytime fatigue and sleepiness continued. The pediatrician referred her to the neurologist who had interpreted the first NPSG. His history presented a differential diagnosis of narcolepsy, primary hypersomnolence, persistent OSA, and PLMD. He recommended a second NPSG with a multiple sleep latency test (MSLT), to be done immediately following the NPSG to assess her sleepiness more formally. His history documented that she felt as if she was \"going to fall\" when she laughed. He also noted that her father had OSA (treated with CPAP) and that she had an uncle and a grandfather with narcolepsy.","The second NPSG revealed the following:","A respiratory disturbance index of 1.4 (improved)","Sleep latency of 2.5 minutes and REM latency of 68.5 minutes","A sleep efficiency of 68.3%","31.6% of total sleep time in stage N1, 43.8% in N2, 20% in N3, and 4.6% in REM sleep","An arousal index of 23.5 (increased)","A periodic leg movement index of 5.9 (slightly lower)","\"3 REM periods, 2 of them were very brief,\" and a period of wakefulness after sleep onset of 180.5 minutes (increased)","The MSLT showed a mean sleep latency calculated at 9.5 minutes and no sleep onset–associated REM sleep (REM sleep within 20 minutes of sleep onset).","The neurologist provisionally diagnosed narcolepsy (vs hypersomnolence). He prescribed methylphenidate and then gradually increased the dose. Despite slightly improved daytime alertness, the patient started to develop more classic findings of cataplexy. The patient's mother brought her back to the pediatric pulmonary and sleep medicine clinic. Methylphenidate was discontinued and therapy with modafinil was initiated.","When the patient was 9 years old, sodium oxybate was added to her regimen and her condition finally stabilized. Her therapy was complicated by the treatment of her inattention with dextroamphetamine and levoamphetamine (Adderall) and the effects of all of her therapy on her weight. Her rapid weight gain was followed by an equally rapid weight loss, and these changes finally settled into her currently stable pattern of tracking around the 75th percentile after starting sodium oxybate (Figure 2).","Figure 2."],"date":"October 09, 2020","figures":[{"caption":"Figure 2.","image_url":"https://img.medscapestatic.com/article/938/423/938423-Thumb2.jpg"}],"markdown":"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\n\n **Authors:** Timothy D. Murphy, MD \n **Date:** October 09, 2020\n\n ## Content\n\n This case is very challenging because the patient had the findings of and met the criteria for OSA, periodic limb movement disorder (PLMD)/restless legs syndrome (RLS), and hypersomnolence. She also had several historical findings that were highly suggestive of narcolepsy with cataplexy. These included a strong family history of narcolepsy, a history of the sudden onset of sleep and greatly increased sleep pressure, and rapid weight gain. A critical finding was a nocturnal sleep-onset REM sleep period (SOREMP). A nocturnal SOREMP (defined as REM sleep within 15 minutes of falling asleep) has a very high specificity for narcolepsy with cataplexy in adults and children.[1,2] However, the importance of the nocturnal SOREMP was not initially noted in her evaluation and management.\nOSA and PLMD were initially diagnosed, and the otolaryngologist performed an adenotonsillectomy. The patient returned to the pediatric pulmonary and sleep medicine clinic after the procedure. At 3 weeks after the surgery, her somnolence improved very little. She had been gaining weight more rapidly and symptoms of apparent instability in her asthma were noted.\nFurther history-taking revealed a complex set of interactions around eating (some involved her father catering to her desire for higher-carbohydrate foods), increased sedentary behavior, and a history suggestive of vocal cord dysfunction. She was having \"asthma attacks\" characterized by rapid onset with inspiratory stridor and rapid resolution at the onset of activity. Her family was willing to make changes in their diet and to encourage activity, and they sought help for the vocal cord dysfunction from a speech and language pathologist.\nDespite these measures, her weight gain rapidly progressed and the daytime fatigue and sleepiness continued. The pediatrician referred her to the neurologist who had interpreted the first NPSG. His history presented a differential diagnosis of narcolepsy, primary hypersomnolence, persistent OSA, and PLMD. He recommended a second NPSG with a multiple sleep latency test (MSLT), to be done immediately following the NPSG to assess her sleepiness more formally. His history documented that she felt as if she was \"going to fall\" when she laughed. He also noted that her father had OSA (treated with CPAP) and that she had an uncle and a grandfather with narcolepsy.\nThe second NPSG revealed the following:\nA respiratory disturbance index of 1.4 (improved)\nSleep latency of 2.5 minutes and REM latency of 68.5 minutes\nA sleep efficiency of 68.3%\n31.6% of total sleep time in stage N1, 43.8% in N2, 20% in N3, and 4.6% in REM sleep\nAn arousal index of 23.5 (increased)\nA periodic leg movement index of 5.9 (slightly lower)\n\"3 REM periods, 2 of them were very brief,\" and a period of wakefulness after sleep onset of 180.5 minutes (increased)\nThe MSLT showed a mean sleep latency calculated at 9.5 minutes and no sleep onset–associated REM sleep (REM sleep within 20 minutes of sleep onset).\nThe neurologist provisionally diagnosed narcolepsy (vs hypersomnolence). He prescribed methylphenidate and then gradually increased the dose. Despite slightly improved daytime alertness, the patient started to develop more classic findings of cataplexy. The patient's mother brought her back to the pediatric pulmonary and sleep medicine clinic. Methylphenidate was discontinued and therapy with modafinil was initiated.\nWhen the patient was 9 years old, sodium oxybate was added to her regimen and her condition finally stabilized. Her therapy was complicated by the treatment of her inattention with dextroamphetamine and levoamphetamine (Adderall) and the effects of all of her therapy on her weight. Her rapid weight gain was followed by an equally rapid weight loss, and these changes finally settled into her currently stable pattern of tracking around the 75th percentile after starting sodium oxybate (Figure 2).\nFigure 2.\n\n ## Figures\n\n **Figure 2.** \n \n\n\n*Page 3 of 6*","pagination":{"current_page":3,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1529064,"choiceText":"Behavioral insomnia of childhood\r\n","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529065,"choiceText":"Pediatric chronic obstructive pulmonary disease","correct":false,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529066,"choiceText":"Delayed sleep phase disorder","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529067,"choiceText":"Narcolepsy","correct":true,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"","displayOrder":1,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":490073,"questionText":"On the basis of these findings only, what is the most likely diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma"},{"authors":"Timothy D. Murphy, MD","content":["This case illustrates some of the challenges facing clinicians who care for a \"sleepy child.\" In the evolution of this child's care, multiple diagnoses were made and treated. The failure of her symptoms to respond to treatment resulted in further evaluation (and reevaluation of the data), which finally led to the diagnosis (narcolepsy with cataplexy) and her ultimate improvement and stabilization.","Hypersomnolence may be primary or it may be secondary to a poor night's sleep. The most common conditions seen in a pediatric sleep clinic that might lead to daytime sleepiness include sleep apnea, behavioral insomnia of childhood, restless sleeping (or, when more extreme, pediatric RLS), and delayed sleep phase disorder (DSPD). The latter is much more common in teenagers, with a prevalence of up to 7% in this age group.[3] However, youths with daytime hypersomnolence due to DSPD do not typically fall asleep easily at bedtime, as this patient did. Moreover, DSPD is unusual in an 8-year-old.","An insufficient quantity of sleep can usually be diagnosed on the basis of the history alone, but actigraphy is occasionally used when the history does not exclude difficulty in falling asleep or a circadian rhythm sleep-wake disorder.[4] Actigraphy was not included in this patient's workup.","Pediatric RLS is primarily diagnosed on the basis of history, but the use of strict criteria (which include that the child \"relates a description in his or her own words\" of leg discomfort) may lead to missing the diagnosis in children who can benefit from treatment but are unable to verbalize their feelings. Suboptimal levels of serum ferritin are associated with restless sleep in children, as is improvement with iron therapy. The use of dopaminergic medications typically requires a higher standard for the diagnosis of RLS and a failure to respond to iron therapy.[5,6] Published data regarding autism and attention-deficit/hyperactivity disorder (ADHD) increasingly suggest complex links between iron metabolism and brain function, including during sleep.[7,8] This patient's movements in bed and her behavioral and learning struggles led to the investigation of her iron stores and ferritin levels and a trial of treatment for RLS.","Hypersomnolence is associated with OSA more commonly in adults than in children. \"Hyperactivity\" or symptoms of ADHD are more frequently observed in children with OSA, although some sleepiness is still noted.[9] Most sleep centers consider an obstructive AHI of fewer than 1 event per hour (some use a threshold of 1.5) to be normal.[10] More pragmatically, the absolute score is useful in choosing a diagnostic billing code, but clinical decision-making also factors in the age of the patient and the severity of observed symptoms, considered formally or as a gestalt.[11]","This patient had a positive AHI, which is diagnostic of OSA, and underwent adenotonsillectomy without significant improvement. She was also treated with iron and vitamin C, without significant changes in her daytime sleepiness or her apparent sleep quality. Furthermore, her clinical care was complicated by the MSLT result, which documented hypersomnolence but not narcolepsy.","The diagnosis of narcolepsy was based primarily on clinical factors. Despite the positive AHI, snoring, leg movements, and low ferritin level, her condition did not improve after the adenotonsillectomy and iron therapy. As her case progressed, she developed more classic symptoms of cataplexy, such as feeling as if she would fall with laughter and falling asleep rapidly in conjunction with strong emotions. These findings, along with the rapid weight gain, pointed toward the diagnosis.","Some confusion along the path toward a diagnosis is common in narcolepsy. Comorbidities, including PLMD, RLS, and OSA, may be found in association with narcolepsy and can delay the diagnosis,[12] as certainly happened in this patient.","Narcolepsy affects about 1 in 2000 people. Two types are recognized: type 1 narcolepsy (previously referred to as narcolepsy with cataplexy) and type 2 narcolepsy (narcolepsy without cataplexy). Type 1 narcolepsy is considered an adult diagnosis by many pediatricians, but it frequently develops during adolescence, and onset after age 40 years is uncommon. Children may first present with a resumption of prolonged naps rather than prolonged nighttime sleep; nocturnal sleep is often somewhat disturbed initially. Cataplexy, multiple short naps during the day, hypnagogic hallucinations, and sleep-onset REM periods may be absent in young children, and repeated NPSGs and MSLTs over months to years may be required to make the diagnosis.","Although a retrospective analysis of sleep histories often reveals hypersomnolence for years prior to the diagnosis, it can be easily missed in the first decade of life.[13] Type 1 narcolepsy is caused by the loss of orexin neuropeptides, which are mediators of central nervous system (CNS) control of energy metabolism and maintenance of sleep-wake states. Rapid weight gain and precocious puberty can occur in children with type 1 narcolepsy. This patient's rapid weight gain started to make more sense once the diagnosis was made.[14]","In type 1 narcolepsy, the lack of consistent REM sleep at night leads to the intrusion of REM sleep features into the waking state. The diagnostic features include the tetrad of daytime sleepiness, cataplexy, hypnagogic hallucinations, and sleep paralysis. Specific questioning is usually required to elicit the history; only cataplexy is specific for narcolepsy. Patients often present initially with hypersomnolence alone, and other diagnostic findings may emerge over time.","The etiology of narcolepsy is unclear. The lack of orexin may be related to autoimmune disease or infectious diseases. Most patients with type 1 narcolepsy have HLA DQB1 (0602 allele), the gene complex that encodes for proteins on the surface of T cells. Additionally, some infections (most notably H1N1 influenza, as well as some vaccines for it) are associated with clusters of type 1 narcolepsy and reduced orexin levels.[15,16,17] However, measurement of cerebrospinal fluid (CSF) levels of orexin is not required to make the diagnosis of narcolepsy.","The diagnosis of type 1 narcolepsy can be clinically made in a child with a clear history of cataplexy, EDS, and an otherwise normal neurologic examination. In the absence of cataplexy, an NPSG followed by an MSLT can be used to make the diagnosis of narcolepsy. \"Secondary narcolepsy\" in the setting of CNS diseases such as hypothalamic tumors or arteriovenous malformations, following cerebrovascular accidents, or in association with multiple sclerosis or Niemann-Pick disease type C has been reported, but alternative causes of narcolepsy are vanishingly rare in childhood. The primary challenge is to rule out other sleep disorders causing the EDS; as in this patient, that may be difficult."],"date":"October 09, 2020","figures":[],"markdown":"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\n\n **Authors:** Timothy D. Murphy, MD \n **Date:** October 09, 2020\n\n ## Content\n\n This case illustrates some of the challenges facing clinicians who care for a \"sleepy child.\" In the evolution of this child's care, multiple diagnoses were made and treated. The failure of her symptoms to respond to treatment resulted in further evaluation (and reevaluation of the data), which finally led to the diagnosis (narcolepsy with cataplexy) and her ultimate improvement and stabilization.\nHypersomnolence may be primary or it may be secondary to a poor night's sleep. The most common conditions seen in a pediatric sleep clinic that might lead to daytime sleepiness include sleep apnea, behavioral insomnia of childhood, restless sleeping (or, when more extreme, pediatric RLS), and delayed sleep phase disorder (DSPD). The latter is much more common in teenagers, with a prevalence of up to 7% in this age group.[3] However, youths with daytime hypersomnolence due to DSPD do not typically fall asleep easily at bedtime, as this patient did. Moreover, DSPD is unusual in an 8-year-old.\nAn insufficient quantity of sleep can usually be diagnosed on the basis of the history alone, but actigraphy is occasionally used when the history does not exclude difficulty in falling asleep or a circadian rhythm sleep-wake disorder.[4] Actigraphy was not included in this patient's workup.\nPediatric RLS is primarily diagnosed on the basis of history, but the use of strict criteria (which include that the child \"relates a description in his or her own words\" of leg discomfort) may lead to missing the diagnosis in children who can benefit from treatment but are unable to verbalize their feelings. Suboptimal levels of serum ferritin are associated with restless sleep in children, as is improvement with iron therapy. The use of dopaminergic medications typically requires a higher standard for the diagnosis of RLS and a failure to respond to iron therapy.[5,6] Published data regarding autism and attention-deficit/hyperactivity disorder (ADHD) increasingly suggest complex links between iron metabolism and brain function, including during sleep.[7,8] This patient's movements in bed and her behavioral and learning struggles led to the investigation of her iron stores and ferritin levels and a trial of treatment for RLS.\nHypersomnolence is associated with OSA more commonly in adults than in children. \"Hyperactivity\" or symptoms of ADHD are more frequently observed in children with OSA, although some sleepiness is still noted.[9] Most sleep centers consider an obstructive AHI of fewer than 1 event per hour (some use a threshold of 1.5) to be normal.[10] More pragmatically, the absolute score is useful in choosing a diagnostic billing code, but clinical decision-making also factors in the age of the patient and the severity of observed symptoms, considered formally or as a gestalt.[11]\nThis patient had a positive AHI, which is diagnostic of OSA, and underwent adenotonsillectomy without significant improvement. She was also treated with iron and vitamin C, without significant changes in her daytime sleepiness or her apparent sleep quality. Furthermore, her clinical care was complicated by the MSLT result, which documented hypersomnolence but not narcolepsy.\nThe diagnosis of narcolepsy was based primarily on clinical factors. Despite the positive AHI, snoring, leg movements, and low ferritin level, her condition did not improve after the adenotonsillectomy and iron therapy. As her case progressed, she developed more classic symptoms of cataplexy, such as feeling as if she would fall with laughter and falling asleep rapidly in conjunction with strong emotions. These findings, along with the rapid weight gain, pointed toward the diagnosis.\nSome confusion along the path toward a diagnosis is common in narcolepsy. Comorbidities, including PLMD, RLS, and OSA, may be found in association with narcolepsy and can delay the diagnosis,[12] as certainly happened in this patient.\nNarcolepsy affects about 1 in 2000 people. Two types are recognized: type 1 narcolepsy (previously referred to as narcolepsy with cataplexy) and type 2 narcolepsy (narcolepsy without cataplexy). Type 1 narcolepsy is considered an adult diagnosis by many pediatricians, but it frequently develops during adolescence, and onset after age 40 years is uncommon. Children may first present with a resumption of prolonged naps rather than prolonged nighttime sleep; nocturnal sleep is often somewhat disturbed initially. Cataplexy, multiple short naps during the day, hypnagogic hallucinations, and sleep-onset REM periods may be absent in young children, and repeated NPSGs and MSLTs over months to years may be required to make the diagnosis.\nAlthough a retrospective analysis of sleep histories often reveals hypersomnolence for years prior to the diagnosis, it can be easily missed in the first decade of life.[13] Type 1 narcolepsy is caused by the loss of orexin neuropeptides, which are mediators of central nervous system (CNS) control of energy metabolism and maintenance of sleep-wake states. Rapid weight gain and precocious puberty can occur in children with type 1 narcolepsy. This patient's rapid weight gain started to make more sense once the diagnosis was made.[14]\nIn type 1 narcolepsy, the lack of consistent REM sleep at night leads to the intrusion of REM sleep features into the waking state. The diagnostic features include the tetrad of daytime sleepiness, cataplexy, hypnagogic hallucinations, and sleep paralysis. Specific questioning is usually required to elicit the history; only cataplexy is specific for narcolepsy. Patients often present initially with hypersomnolence alone, and other diagnostic findings may emerge over time.\nThe etiology of narcolepsy is unclear. The lack of orexin may be related to autoimmune disease or infectious diseases. Most patients with type 1 narcolepsy have HLA DQB1 (0602 allele), the gene complex that encodes for proteins on the surface of T cells. Additionally, some infections (most notably H1N1 influenza, as well as some vaccines for it) are associated with clusters of type 1 narcolepsy and reduced orexin levels.[15,16,17] However, measurement of cerebrospinal fluid (CSF) levels of orexin is not required to make the diagnosis of narcolepsy.\nThe diagnosis of type 1 narcolepsy can be clinically made in a child with a clear history of cataplexy, EDS, and an otherwise normal neurologic examination. In the absence of cataplexy, an NPSG followed by an MSLT can be used to make the diagnosis of narcolepsy. \"Secondary narcolepsy\" in the setting of CNS diseases such as hypothalamic tumors or arteriovenous malformations, following cerebrovascular accidents, or in association with multiple sclerosis or Niemann-Pick disease type C has been reported, but alternative causes of narcolepsy are vanishingly rare in childhood. The primary challenge is to rule out other sleep disorders causing the EDS; as in this patient, that may be difficult.\n\n ## Figures\n\n \n*Page 4 of 6*","pagination":{"current_page":4,"total_pages":6},"questionnaire":[],"title":"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma"},{"authors":"Timothy D. Murphy, MD","content":["The treatment of narcolepsy focuses first on attempts to reduce the EDS pharmacologically; timed naps or increased time in bed is not usually sufficient to reduce the EDS. Although many medications have been used to treat EDS, clinicians typically start with caffeine (usually inadequate) and then move to stronger stimulants, such as methylphenidate or amphetamine and dextroamphetamine in combination.","Failure of these agents might then lead to the use of modafinil (prescription without the failure of other therapies is often difficult). Monitoring of response and fairly frequent visits are required at this point. A selective serotonin reuptake inhibitor, such as fluoxetine, is often added to the regimen of patients with classic cataplexy. As was the case for this patient, the use of medications that might affect mood, attention, learning, and sleep requires close attention and collaboration between specialists in sleep medicine, neurology, and behavioral and general pediatrics.","In some patients, including this patient, sodium oxybate (gamma-hydroxybutyrate [GHB]) is required to treat the cataplexy and to lead to better daytime functioning.[18] The exact mechanism of action is unknown, but the evening dosing of GHB is associated with improved REM sleep at night, perhaps relieving the intrusion of REM during daytime wake periods associated with type 1 narcolepsy. Unfortunately, GHB is associated with abuse — it is often called the \"date rape drug\" — and is now tightly regulated. Prescription in the United States is limited to one US pharmacy, and a sleep physician is typically required to obtain and use this medication.","The finding of EDS requires exploration of nocturnal problems with sleep, including RLS, OSA, and behavioral insomnia that affects daytime functioning. Narcolepsy can be diagnosed as the cause of EDS on the basis of careful history-taking as well as the results of an NPSG and an MSLT."],"date":"October 09, 2020","figures":[],"markdown":"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\n\n **Authors:** Timothy D. Murphy, MD \n **Date:** October 09, 2020\n\n ## Content\n\n The treatment of narcolepsy focuses first on attempts to reduce the EDS pharmacologically; timed naps or increased time in bed is not usually sufficient to reduce the EDS. Although many medications have been used to treat EDS, clinicians typically start with caffeine (usually inadequate) and then move to stronger stimulants, such as methylphenidate or amphetamine and dextroamphetamine in combination.\nFailure of these agents might then lead to the use of modafinil (prescription without the failure of other therapies is often difficult). Monitoring of response and fairly frequent visits are required at this point. A selective serotonin reuptake inhibitor, such as fluoxetine, is often added to the regimen of patients with classic cataplexy. As was the case for this patient, the use of medications that might affect mood, attention, learning, and sleep requires close attention and collaboration between specialists in sleep medicine, neurology, and behavioral and general pediatrics.\nIn some patients, including this patient, sodium oxybate (gamma-hydroxybutyrate [GHB]) is required to treat the cataplexy and to lead to better daytime functioning.[18] The exact mechanism of action is unknown, but the evening dosing of GHB is associated with improved REM sleep at night, perhaps relieving the intrusion of REM during daytime wake periods associated with type 1 narcolepsy. Unfortunately, GHB is associated with abuse — it is often called the \"date rape drug\" — and is now tightly regulated. Prescription in the United States is limited to one US pharmacy, and a sleep physician is typically required to obtain and use this medication.\nThe finding of EDS requires exploration of nocturnal problems with sleep, including RLS, OSA, and behavioral insomnia that affects daytime functioning. Narcolepsy can be diagnosed as the cause of EDS on the basis of careful history-taking as well as the results of an NPSG and an MSLT.\n\n ## Figures\n\n \n*Page 5 of 6*","pagination":{"current_page":5,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1529068,"choiceText":"Narcolepsy without cataplexy (type 2 narcolepsy) is associated with increased orexin neuropeptide levels","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529069,"choiceText":"Childhood narcolepsy is characterized by multiple brief naps during the day","correct":false,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529070,"choiceText":"Narcolepsy is associated with the loss of orexin neuropeptides","correct":true,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529071,"choiceText":"Measurement of orexin levels in the CSF is required for the diagnosis of narcolepsy","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Levels of orexin neuropeptides in the CNS are reduced, not increased, in all forms of narcolepsy. Children more frequently present with prolonged daytime sleep, and multiple naps are typically seen in older patients. The diagnosis can be made by a careful history-taking that documents cataplexy, which is explained only by type 1 narcolepsy. Measurement of CSF levels of orexin is usually related to research only and typically is not used clinically in diagnosing narcolepsy.","displayOrder":2,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":490074,"questionText":"Which of the following is most accurate regarding narcolepsy in children?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1529072,"choiceText":"Timed or planned naps to reduce sleep pressure, and amphetamine and dextroamphetamine for stimulant therapy during the day\r\n","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529073,"choiceText":"Modafinil as a daytime stimulant, fluoxetine for cataplexy, and sodium oxybate to improve REM efficiency","correct":true,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529074,"choiceText":"Caffeine as a morning stimulant and sodium oxybate (gamma-hydroxybutyrate [GHB]) used at night to consolidate non-REM sleep","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529075,"choiceText":"Methylphenidate to reduce cataplexy, fluoxetine to reduce depressive symptoms, and sodium oxybate to prolong REM latency","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Caffeine is usually an inadequate stimulant for patients with narcolepsy. The daytime use of methylphenidate or amphetamine and dextroamphetamine in combination does not adequately reduce cataplexy and does not address the problem with REM sleep at night. Modafinil is a more reliable daytime stimulant, and fluoxetine helps reduce cataplexy. The use of sodium oxybate in the evening in divided doses is intended to consolidate REM sleep and may reduce REM latency; non-REM sleep is not related to the daytime difficulties associated with narcolepsy.","displayOrder":3,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":490075,"questionText":"Which of the following is typically required in the treatment of type 1 narcolepsy?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma"},{"authors":"Timothy D. Murphy, MD","content":[],"date":"October 09, 2020","figures":[],"markdown":"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\n\n **Authors:** Timothy D. Murphy, MD \n **Date:** October 09, 2020\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*","pagination":{"current_page":6,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1529068,"choiceText":"Narcolepsy without cataplexy (type 2 narcolepsy) is associated with increased orexin neuropeptide levels","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529069,"choiceText":"Childhood narcolepsy is characterized by multiple brief naps during the day","correct":false,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529070,"choiceText":"Narcolepsy is associated with the loss of orexin neuropeptides","correct":true,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529071,"choiceText":"Measurement of orexin levels in the CSF is required for the diagnosis of narcolepsy","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Levels of orexin neuropeptides in the CNS are reduced, not increased, in all forms of narcolepsy. Children more frequently present with prolonged daytime sleep, and multiple naps are typically seen in older patients. The diagnosis can be made by a careful history-taking that documents cataplexy, which is explained only by type 1 narcolepsy. Measurement of CSF levels of orexin is usually related to research only and typically is not used clinically in diagnosing narcolepsy.","displayOrder":2,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":490074,"questionText":"Which of the following is most accurate regarding narcolepsy in children?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1529072,"choiceText":"Timed or planned naps to reduce sleep pressure, and amphetamine and dextroamphetamine for stimulant therapy during the day\r\n","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529073,"choiceText":"Modafinil as a daytime stimulant, fluoxetine for cataplexy, and sodium oxybate to improve REM efficiency","correct":true,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529074,"choiceText":"Caffeine as a morning stimulant and sodium oxybate (gamma-hydroxybutyrate [GHB]) used at night to consolidate non-REM sleep","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529075,"choiceText":"Methylphenidate to reduce cataplexy, fluoxetine to reduce depressive symptoms, and sodium oxybate to prolong REM latency","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Caffeine is usually an inadequate stimulant for patients with narcolepsy. The daytime use of methylphenidate or amphetamine and dextroamphetamine in combination does not adequately reduce cataplexy and does not address the problem with REM sleep at night. Modafinil is a more reliable daytime stimulant, and fluoxetine helps reduce cataplexy. The use of sodium oxybate in the evening in divided doses is intended to consolidate REM sleep and may reduce REM latency; non-REM sleep is not related to the daytime difficulties associated with narcolepsy.","displayOrder":3,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":490075,"questionText":"Which of the following is typically required in the treatment of type 1 narcolepsy?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma"}],"string":"[\n {\n \"authors\": \"Timothy D. Murphy, MD\",\n \"content\": [\n \"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us .\",\n \"A 5-year-old girl with a long-standing history of severe asthma and eczema presented to a pediatric pulmonary and sleep medicine clinic. Her asthma was stabilized with an inhaled corticosteroid (fluticasone, 88 µg, inhaled twice daily), albuterol sulfate (180 µg, inhaled as needed), and ipratropium bromide (34 µg, inhaled as needed). Her skin condition improved with a moderately aggressive regimen of hydrating bleach baths, moisturizing lotions, nonsedating antihistamines, and as-needed use of topical hydrocortisone or triamcinolone, pimecrolimus, and mupirocin.\",\n \"Her asthma remained stable for a year but then progressed to the extent that the dosage of inhaled fluticasone was increased to 220 µg twice daily. Bronchoscopy revealed only mild bronchomalacia of the left mainstem bronchus (Figure 1), diffuse mild inflammation, and increased secretions.\",\n \"Figure 1.\",\n \"Montelukast (5 mg daily) and nasal fluticasone (50 µg) were added to her regimen. In addition, diphenhydramine (25 mg) was prescribed to be used as needed for excessive itchiness, eczema flares, and allergic asthma flares.\",\n \"The patient remained well and was followed up in the clinic approximately every 3 months, owing to the complexity of her condition. After 6 months, significant weight gain and an increasing body mass index (BMI) were noted. She met with a dietitian, who recommended weight loss strategies. From the age of 7-8 years, the patient demonstrated a modest weight loss from the changes in her diet. However, symptoms of fatigue, excessive daytime sleepiness (EDS), and inattention in school developed over a 1- to 2-month period, and her weight started to increase rapidly despite the dietary intervention.\",\n \"Her daytime sleepiness seemed to be progressive, and she would fall asleep suddenly even when she wanted to be awake. Concerned about the emerging symptoms of inattention, autistic features, fatigue, and sleepiness, the girl's parents are seeking further medical advice.\"\n ],\n \"date\": \"October 09, 2020\",\n \"figures\": [\n {\n \"caption\": \"Figure 1.\",\n \"image_url\": \"https://img.medscapestatic.com/article/938/423/938423-Thumb1.jpg\"\n }\n ],\n \"markdown\": \"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\\n\\n **Authors:** Timothy D. Murphy, MD \\n **Date:** October 09, 2020\\n\\n ## Content\\n\\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us .\\nA 5-year-old girl with a long-standing history of severe asthma and eczema presented to a pediatric pulmonary and sleep medicine clinic. Her asthma was stabilized with an inhaled corticosteroid (fluticasone, 88 µg, inhaled twice daily), albuterol sulfate (180 µg, inhaled as needed), and ipratropium bromide (34 µg, inhaled as needed). Her skin condition improved with a moderately aggressive regimen of hydrating bleach baths, moisturizing lotions, nonsedating antihistamines, and as-needed use of topical hydrocortisone or triamcinolone, pimecrolimus, and mupirocin.\\nHer asthma remained stable for a year but then progressed to the extent that the dosage of inhaled fluticasone was increased to 220 µg twice daily. Bronchoscopy revealed only mild bronchomalacia of the left mainstem bronchus (Figure 1), diffuse mild inflammation, and increased secretions.\\nFigure 1.\\nMontelukast (5 mg daily) and nasal fluticasone (50 µg) were added to her regimen. In addition, diphenhydramine (25 mg) was prescribed to be used as needed for excessive itchiness, eczema flares, and allergic asthma flares.\\nThe patient remained well and was followed up in the clinic approximately every 3 months, owing to the complexity of her condition. After 6 months, significant weight gain and an increasing body mass index (BMI) were noted. She met with a dietitian, who recommended weight loss strategies. From the age of 7-8 years, the patient demonstrated a modest weight loss from the changes in her diet. However, symptoms of fatigue, excessive daytime sleepiness (EDS), and inattention in school developed over a 1- to 2-month period, and her weight started to increase rapidly despite the dietary intervention.\\nHer daytime sleepiness seemed to be progressive, and she would fall asleep suddenly even when she wanted to be awake. Concerned about the emerging symptoms of inattention, autistic features, fatigue, and sleepiness, the girl's parents are seeking further medical advice.\\n\\n ## Figures\\n\\n **Figure 1.** \\n \\n\\n\\n*Page 1 of 6*\",\n \"pagination\": {\n \"current_page\": 1,\n \"total_pages\": 6\n },\n \"questionnaire\": [],\n \"title\": \"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\"\n },\n {\n \"authors\": \"Timothy D. Murphy, MD\",\n \"content\": [\n \"The patient has fallen asleep at school nearly every day for the past 1-2 months and falls into a deep sleep unless she is kept active. At home, she is taking more naps during the day, falling asleep in the car, and struggling with schoolwork. Her grades have dropped significantly over the past few months. Her parents report that she does not awaken during the night. No snoring, choking, snorting, gasping, or apnea is noted. She sleeps an average of 9-10 hours per night but is restless and tosses and turns frequently in her sleep.\",\n \"Her family history is notable for obesity, obstructive sleep apnea (OSA) that requires continuous positive airway pressure (CPAP) in her father, and narcolepsy in an uncle and a grandfather.\",\n \"On physical examination, she has mild to moderate obesity (BMI of 23.89 kg/m2 [the 98th percentile for age]) and enlarged tonsils (2-3+). She has difficulty with focusing and staying awake in the clinic.\",\n \"She is referred to a pediatric otolaryngologist for consideration of nocturnal polysomnography (NPSG) or an adenotonsillectomy. The otolaryngologist notes that she has not tolerated nasal fluticasone well, that she is a chronic mouth breather, and that her tonsils are enlarged (3+). An NPSG is ordered to help clarify matters.\",\n \"The NPSG demonstrates the following:\",\n \"A respiratory disturbance index and an apnea-hypopnea index (AHI) of 6.2 per hour\",\n \"Sleep latency of 0.5 minutes and rapid eye movement (REM) latency of 0.5 minutes\",\n \"A sleep efficiency of 87.5%\",\n \"18.2% of total sleep time in stage N1, 36.4% in N2, 29.9% in N3, and 15.5% in REM sleep\",\n \"An arousal index of 18.6\",\n \"A periodic leg movement index of 6.3\",\n \"Multiple periods of wakefulness scattered throughout the night and six REM periods\"\n ],\n \"date\": \"October 09, 2020\",\n \"figures\": [],\n \"markdown\": \"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\\n\\n **Authors:** Timothy D. Murphy, MD \\n **Date:** October 09, 2020\\n\\n ## Content\\n\\n The patient has fallen asleep at school nearly every day for the past 1-2 months and falls into a deep sleep unless she is kept active. At home, she is taking more naps during the day, falling asleep in the car, and struggling with schoolwork. Her grades have dropped significantly over the past few months. Her parents report that she does not awaken during the night. No snoring, choking, snorting, gasping, or apnea is noted. She sleeps an average of 9-10 hours per night but is restless and tosses and turns frequently in her sleep.\\nHer family history is notable for obesity, obstructive sleep apnea (OSA) that requires continuous positive airway pressure (CPAP) in her father, and narcolepsy in an uncle and a grandfather.\\nOn physical examination, she has mild to moderate obesity (BMI of 23.89 kg/m2 [the 98th percentile for age]) and enlarged tonsils (2-3+). She has difficulty with focusing and staying awake in the clinic.\\nShe is referred to a pediatric otolaryngologist for consideration of nocturnal polysomnography (NPSG) or an adenotonsillectomy. The otolaryngologist notes that she has not tolerated nasal fluticasone well, that she is a chronic mouth breather, and that her tonsils are enlarged (3+). An NPSG is ordered to help clarify matters.\\nThe NPSG demonstrates the following:\\nA respiratory disturbance index and an apnea-hypopnea index (AHI) of 6.2 per hour\\nSleep latency of 0.5 minutes and rapid eye movement (REM) latency of 0.5 minutes\\nA sleep efficiency of 87.5%\\n18.2% of total sleep time in stage N1, 36.4% in N2, 29.9% in N3, and 15.5% in REM sleep\\nAn arousal index of 18.6\\nA periodic leg movement index of 6.3\\nMultiple periods of wakefulness scattered throughout the night and six REM periods\\n\\n ## Figures\\n\\n \\n*Page 2 of 6*\",\n \"pagination\": {\n \"current_page\": 2,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1529064,\n \"choiceText\": \"Behavioral insomnia of childhood\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529065,\n \"choiceText\": \"Pediatric chronic obstructive pulmonary disease\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529066,\n \"choiceText\": \"Delayed sleep phase disorder\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529067,\n \"choiceText\": \"Narcolepsy\",\n \"correct\": true,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\",\n \"displayOrder\": 1,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 490073,\n \"questionText\": \"On the basis of these findings only, what is the most likely diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\"\n },\n {\n \"authors\": \"Timothy D. Murphy, MD\",\n \"content\": [\n \"This case is very challenging because the patient had the findings of and met the criteria for OSA, periodic limb movement disorder (PLMD)/restless legs syndrome (RLS), and hypersomnolence. She also had several historical findings that were highly suggestive of narcolepsy with cataplexy. These included a strong family history of narcolepsy, a history of the sudden onset of sleep and greatly increased sleep pressure, and rapid weight gain. A critical finding was a nocturnal sleep-onset REM sleep period (SOREMP). A nocturnal SOREMP (defined as REM sleep within 15 minutes of falling asleep) has a very high specificity for narcolepsy with cataplexy in adults and children.[1,2] However, the importance of the nocturnal SOREMP was not initially noted in her evaluation and management.\",\n \"OSA and PLMD were initially diagnosed, and the otolaryngologist performed an adenotonsillectomy. The patient returned to the pediatric pulmonary and sleep medicine clinic after the procedure. At 3 weeks after the surgery, her somnolence improved very little. She had been gaining weight more rapidly and symptoms of apparent instability in her asthma were noted.\",\n \"Further history-taking revealed a complex set of interactions around eating (some involved her father catering to her desire for higher-carbohydrate foods), increased sedentary behavior, and a history suggestive of vocal cord dysfunction. She was having \\\"asthma attacks\\\" characterized by rapid onset with inspiratory stridor and rapid resolution at the onset of activity. Her family was willing to make changes in their diet and to encourage activity, and they sought help for the vocal cord dysfunction from a speech and language pathologist.\",\n \"Despite these measures, her weight gain rapidly progressed and the daytime fatigue and sleepiness continued. The pediatrician referred her to the neurologist who had interpreted the first NPSG. His history presented a differential diagnosis of narcolepsy, primary hypersomnolence, persistent OSA, and PLMD. He recommended a second NPSG with a multiple sleep latency test (MSLT), to be done immediately following the NPSG to assess her sleepiness more formally. His history documented that she felt as if she was \\\"going to fall\\\" when she laughed. He also noted that her father had OSA (treated with CPAP) and that she had an uncle and a grandfather with narcolepsy.\",\n \"The second NPSG revealed the following:\",\n \"A respiratory disturbance index of 1.4 (improved)\",\n \"Sleep latency of 2.5 minutes and REM latency of 68.5 minutes\",\n \"A sleep efficiency of 68.3%\",\n \"31.6% of total sleep time in stage N1, 43.8% in N2, 20% in N3, and 4.6% in REM sleep\",\n \"An arousal index of 23.5 (increased)\",\n \"A periodic leg movement index of 5.9 (slightly lower)\",\n \"\\\"3 REM periods, 2 of them were very brief,\\\" and a period of wakefulness after sleep onset of 180.5 minutes (increased)\",\n \"The MSLT showed a mean sleep latency calculated at 9.5 minutes and no sleep onset–associated REM sleep (REM sleep within 20 minutes of sleep onset).\",\n \"The neurologist provisionally diagnosed narcolepsy (vs hypersomnolence). He prescribed methylphenidate and then gradually increased the dose. Despite slightly improved daytime alertness, the patient started to develop more classic findings of cataplexy. The patient's mother brought her back to the pediatric pulmonary and sleep medicine clinic. Methylphenidate was discontinued and therapy with modafinil was initiated.\",\n \"When the patient was 9 years old, sodium oxybate was added to her regimen and her condition finally stabilized. Her therapy was complicated by the treatment of her inattention with dextroamphetamine and levoamphetamine (Adderall) and the effects of all of her therapy on her weight. Her rapid weight gain was followed by an equally rapid weight loss, and these changes finally settled into her currently stable pattern of tracking around the 75th percentile after starting sodium oxybate (Figure 2).\",\n \"Figure 2.\"\n ],\n \"date\": \"October 09, 2020\",\n \"figures\": [\n {\n \"caption\": \"Figure 2.\",\n \"image_url\": \"https://img.medscapestatic.com/article/938/423/938423-Thumb2.jpg\"\n }\n ],\n \"markdown\": \"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\\n\\n **Authors:** Timothy D. Murphy, MD \\n **Date:** October 09, 2020\\n\\n ## Content\\n\\n This case is very challenging because the patient had the findings of and met the criteria for OSA, periodic limb movement disorder (PLMD)/restless legs syndrome (RLS), and hypersomnolence. She also had several historical findings that were highly suggestive of narcolepsy with cataplexy. These included a strong family history of narcolepsy, a history of the sudden onset of sleep and greatly increased sleep pressure, and rapid weight gain. A critical finding was a nocturnal sleep-onset REM sleep period (SOREMP). A nocturnal SOREMP (defined as REM sleep within 15 minutes of falling asleep) has a very high specificity for narcolepsy with cataplexy in adults and children.[1,2] However, the importance of the nocturnal SOREMP was not initially noted in her evaluation and management.\\nOSA and PLMD were initially diagnosed, and the otolaryngologist performed an adenotonsillectomy. The patient returned to the pediatric pulmonary and sleep medicine clinic after the procedure. At 3 weeks after the surgery, her somnolence improved very little. She had been gaining weight more rapidly and symptoms of apparent instability in her asthma were noted.\\nFurther history-taking revealed a complex set of interactions around eating (some involved her father catering to her desire for higher-carbohydrate foods), increased sedentary behavior, and a history suggestive of vocal cord dysfunction. She was having \\\"asthma attacks\\\" characterized by rapid onset with inspiratory stridor and rapid resolution at the onset of activity. Her family was willing to make changes in their diet and to encourage activity, and they sought help for the vocal cord dysfunction from a speech and language pathologist.\\nDespite these measures, her weight gain rapidly progressed and the daytime fatigue and sleepiness continued. The pediatrician referred her to the neurologist who had interpreted the first NPSG. His history presented a differential diagnosis of narcolepsy, primary hypersomnolence, persistent OSA, and PLMD. He recommended a second NPSG with a multiple sleep latency test (MSLT), to be done immediately following the NPSG to assess her sleepiness more formally. His history documented that she felt as if she was \\\"going to fall\\\" when she laughed. He also noted that her father had OSA (treated with CPAP) and that she had an uncle and a grandfather with narcolepsy.\\nThe second NPSG revealed the following:\\nA respiratory disturbance index of 1.4 (improved)\\nSleep latency of 2.5 minutes and REM latency of 68.5 minutes\\nA sleep efficiency of 68.3%\\n31.6% of total sleep time in stage N1, 43.8% in N2, 20% in N3, and 4.6% in REM sleep\\nAn arousal index of 23.5 (increased)\\nA periodic leg movement index of 5.9 (slightly lower)\\n\\\"3 REM periods, 2 of them were very brief,\\\" and a period of wakefulness after sleep onset of 180.5 minutes (increased)\\nThe MSLT showed a mean sleep latency calculated at 9.5 minutes and no sleep onset–associated REM sleep (REM sleep within 20 minutes of sleep onset).\\nThe neurologist provisionally diagnosed narcolepsy (vs hypersomnolence). He prescribed methylphenidate and then gradually increased the dose. Despite slightly improved daytime alertness, the patient started to develop more classic findings of cataplexy. The patient's mother brought her back to the pediatric pulmonary and sleep medicine clinic. Methylphenidate was discontinued and therapy with modafinil was initiated.\\nWhen the patient was 9 years old, sodium oxybate was added to her regimen and her condition finally stabilized. Her therapy was complicated by the treatment of her inattention with dextroamphetamine and levoamphetamine (Adderall) and the effects of all of her therapy on her weight. Her rapid weight gain was followed by an equally rapid weight loss, and these changes finally settled into her currently stable pattern of tracking around the 75th percentile after starting sodium oxybate (Figure 2).\\nFigure 2.\\n\\n ## Figures\\n\\n **Figure 2.** \\n \\n\\n\\n*Page 3 of 6*\",\n \"pagination\": {\n \"current_page\": 3,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1529064,\n \"choiceText\": \"Behavioral insomnia of childhood\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529065,\n \"choiceText\": \"Pediatric chronic obstructive pulmonary disease\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529066,\n \"choiceText\": \"Delayed sleep phase disorder\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529067,\n \"choiceText\": \"Narcolepsy\",\n \"correct\": true,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\",\n \"displayOrder\": 1,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 490073,\n \"questionText\": \"On the basis of these findings only, what is the most likely diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\"\n },\n {\n \"authors\": \"Timothy D. Murphy, MD\",\n \"content\": [\n \"This case illustrates some of the challenges facing clinicians who care for a \\\"sleepy child.\\\" In the evolution of this child's care, multiple diagnoses were made and treated. The failure of her symptoms to respond to treatment resulted in further evaluation (and reevaluation of the data), which finally led to the diagnosis (narcolepsy with cataplexy) and her ultimate improvement and stabilization.\",\n \"Hypersomnolence may be primary or it may be secondary to a poor night's sleep. The most common conditions seen in a pediatric sleep clinic that might lead to daytime sleepiness include sleep apnea, behavioral insomnia of childhood, restless sleeping (or, when more extreme, pediatric RLS), and delayed sleep phase disorder (DSPD). The latter is much more common in teenagers, with a prevalence of up to 7% in this age group.[3] However, youths with daytime hypersomnolence due to DSPD do not typically fall asleep easily at bedtime, as this patient did. Moreover, DSPD is unusual in an 8-year-old.\",\n \"An insufficient quantity of sleep can usually be diagnosed on the basis of the history alone, but actigraphy is occasionally used when the history does not exclude difficulty in falling asleep or a circadian rhythm sleep-wake disorder.[4] Actigraphy was not included in this patient's workup.\",\n \"Pediatric RLS is primarily diagnosed on the basis of history, but the use of strict criteria (which include that the child \\\"relates a description in his or her own words\\\" of leg discomfort) may lead to missing the diagnosis in children who can benefit from treatment but are unable to verbalize their feelings. Suboptimal levels of serum ferritin are associated with restless sleep in children, as is improvement with iron therapy. The use of dopaminergic medications typically requires a higher standard for the diagnosis of RLS and a failure to respond to iron therapy.[5,6] Published data regarding autism and attention-deficit/hyperactivity disorder (ADHD) increasingly suggest complex links between iron metabolism and brain function, including during sleep.[7,8] This patient's movements in bed and her behavioral and learning struggles led to the investigation of her iron stores and ferritin levels and a trial of treatment for RLS.\",\n \"Hypersomnolence is associated with OSA more commonly in adults than in children. \\\"Hyperactivity\\\" or symptoms of ADHD are more frequently observed in children with OSA, although some sleepiness is still noted.[9] Most sleep centers consider an obstructive AHI of fewer than 1 event per hour (some use a threshold of 1.5) to be normal.[10] More pragmatically, the absolute score is useful in choosing a diagnostic billing code, but clinical decision-making also factors in the age of the patient and the severity of observed symptoms, considered formally or as a gestalt.[11]\",\n \"This patient had a positive AHI, which is diagnostic of OSA, and underwent adenotonsillectomy without significant improvement. She was also treated with iron and vitamin C, without significant changes in her daytime sleepiness or her apparent sleep quality. Furthermore, her clinical care was complicated by the MSLT result, which documented hypersomnolence but not narcolepsy.\",\n \"The diagnosis of narcolepsy was based primarily on clinical factors. Despite the positive AHI, snoring, leg movements, and low ferritin level, her condition did not improve after the adenotonsillectomy and iron therapy. As her case progressed, she developed more classic symptoms of cataplexy, such as feeling as if she would fall with laughter and falling asleep rapidly in conjunction with strong emotions. These findings, along with the rapid weight gain, pointed toward the diagnosis.\",\n \"Some confusion along the path toward a diagnosis is common in narcolepsy. Comorbidities, including PLMD, RLS, and OSA, may be found in association with narcolepsy and can delay the diagnosis,[12] as certainly happened in this patient.\",\n \"Narcolepsy affects about 1 in 2000 people. Two types are recognized: type 1 narcolepsy (previously referred to as narcolepsy with cataplexy) and type 2 narcolepsy (narcolepsy without cataplexy). Type 1 narcolepsy is considered an adult diagnosis by many pediatricians, but it frequently develops during adolescence, and onset after age 40 years is uncommon. Children may first present with a resumption of prolonged naps rather than prolonged nighttime sleep; nocturnal sleep is often somewhat disturbed initially. Cataplexy, multiple short naps during the day, hypnagogic hallucinations, and sleep-onset REM periods may be absent in young children, and repeated NPSGs and MSLTs over months to years may be required to make the diagnosis.\",\n \"Although a retrospective analysis of sleep histories often reveals hypersomnolence for years prior to the diagnosis, it can be easily missed in the first decade of life.[13] Type 1 narcolepsy is caused by the loss of orexin neuropeptides, which are mediators of central nervous system (CNS) control of energy metabolism and maintenance of sleep-wake states. Rapid weight gain and precocious puberty can occur in children with type 1 narcolepsy. This patient's rapid weight gain started to make more sense once the diagnosis was made.[14]\",\n \"In type 1 narcolepsy, the lack of consistent REM sleep at night leads to the intrusion of REM sleep features into the waking state. The diagnostic features include the tetrad of daytime sleepiness, cataplexy, hypnagogic hallucinations, and sleep paralysis. Specific questioning is usually required to elicit the history; only cataplexy is specific for narcolepsy. Patients often present initially with hypersomnolence alone, and other diagnostic findings may emerge over time.\",\n \"The etiology of narcolepsy is unclear. The lack of orexin may be related to autoimmune disease or infectious diseases. Most patients with type 1 narcolepsy have HLA DQB1 (0602 allele), the gene complex that encodes for proteins on the surface of T cells. Additionally, some infections (most notably H1N1 influenza, as well as some vaccines for it) are associated with clusters of type 1 narcolepsy and reduced orexin levels.[15,16,17] However, measurement of cerebrospinal fluid (CSF) levels of orexin is not required to make the diagnosis of narcolepsy.\",\n \"The diagnosis of type 1 narcolepsy can be clinically made in a child with a clear history of cataplexy, EDS, and an otherwise normal neurologic examination. In the absence of cataplexy, an NPSG followed by an MSLT can be used to make the diagnosis of narcolepsy. \\\"Secondary narcolepsy\\\" in the setting of CNS diseases such as hypothalamic tumors or arteriovenous malformations, following cerebrovascular accidents, or in association with multiple sclerosis or Niemann-Pick disease type C has been reported, but alternative causes of narcolepsy are vanishingly rare in childhood. The primary challenge is to rule out other sleep disorders causing the EDS; as in this patient, that may be difficult.\"\n ],\n \"date\": \"October 09, 2020\",\n \"figures\": [],\n \"markdown\": \"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\\n\\n **Authors:** Timothy D. Murphy, MD \\n **Date:** October 09, 2020\\n\\n ## Content\\n\\n This case illustrates some of the challenges facing clinicians who care for a \\\"sleepy child.\\\" In the evolution of this child's care, multiple diagnoses were made and treated. The failure of her symptoms to respond to treatment resulted in further evaluation (and reevaluation of the data), which finally led to the diagnosis (narcolepsy with cataplexy) and her ultimate improvement and stabilization.\\nHypersomnolence may be primary or it may be secondary to a poor night's sleep. The most common conditions seen in a pediatric sleep clinic that might lead to daytime sleepiness include sleep apnea, behavioral insomnia of childhood, restless sleeping (or, when more extreme, pediatric RLS), and delayed sleep phase disorder (DSPD). The latter is much more common in teenagers, with a prevalence of up to 7% in this age group.[3] However, youths with daytime hypersomnolence due to DSPD do not typically fall asleep easily at bedtime, as this patient did. Moreover, DSPD is unusual in an 8-year-old.\\nAn insufficient quantity of sleep can usually be diagnosed on the basis of the history alone, but actigraphy is occasionally used when the history does not exclude difficulty in falling asleep or a circadian rhythm sleep-wake disorder.[4] Actigraphy was not included in this patient's workup.\\nPediatric RLS is primarily diagnosed on the basis of history, but the use of strict criteria (which include that the child \\\"relates a description in his or her own words\\\" of leg discomfort) may lead to missing the diagnosis in children who can benefit from treatment but are unable to verbalize their feelings. Suboptimal levels of serum ferritin are associated with restless sleep in children, as is improvement with iron therapy. The use of dopaminergic medications typically requires a higher standard for the diagnosis of RLS and a failure to respond to iron therapy.[5,6] Published data regarding autism and attention-deficit/hyperactivity disorder (ADHD) increasingly suggest complex links between iron metabolism and brain function, including during sleep.[7,8] This patient's movements in bed and her behavioral and learning struggles led to the investigation of her iron stores and ferritin levels and a trial of treatment for RLS.\\nHypersomnolence is associated with OSA more commonly in adults than in children. \\\"Hyperactivity\\\" or symptoms of ADHD are more frequently observed in children with OSA, although some sleepiness is still noted.[9] Most sleep centers consider an obstructive AHI of fewer than 1 event per hour (some use a threshold of 1.5) to be normal.[10] More pragmatically, the absolute score is useful in choosing a diagnostic billing code, but clinical decision-making also factors in the age of the patient and the severity of observed symptoms, considered formally or as a gestalt.[11]\\nThis patient had a positive AHI, which is diagnostic of OSA, and underwent adenotonsillectomy without significant improvement. She was also treated with iron and vitamin C, without significant changes in her daytime sleepiness or her apparent sleep quality. Furthermore, her clinical care was complicated by the MSLT result, which documented hypersomnolence but not narcolepsy.\\nThe diagnosis of narcolepsy was based primarily on clinical factors. Despite the positive AHI, snoring, leg movements, and low ferritin level, her condition did not improve after the adenotonsillectomy and iron therapy. As her case progressed, she developed more classic symptoms of cataplexy, such as feeling as if she would fall with laughter and falling asleep rapidly in conjunction with strong emotions. These findings, along with the rapid weight gain, pointed toward the diagnosis.\\nSome confusion along the path toward a diagnosis is common in narcolepsy. Comorbidities, including PLMD, RLS, and OSA, may be found in association with narcolepsy and can delay the diagnosis,[12] as certainly happened in this patient.\\nNarcolepsy affects about 1 in 2000 people. Two types are recognized: type 1 narcolepsy (previously referred to as narcolepsy with cataplexy) and type 2 narcolepsy (narcolepsy without cataplexy). Type 1 narcolepsy is considered an adult diagnosis by many pediatricians, but it frequently develops during adolescence, and onset after age 40 years is uncommon. Children may first present with a resumption of prolonged naps rather than prolonged nighttime sleep; nocturnal sleep is often somewhat disturbed initially. Cataplexy, multiple short naps during the day, hypnagogic hallucinations, and sleep-onset REM periods may be absent in young children, and repeated NPSGs and MSLTs over months to years may be required to make the diagnosis.\\nAlthough a retrospective analysis of sleep histories often reveals hypersomnolence for years prior to the diagnosis, it can be easily missed in the first decade of life.[13] Type 1 narcolepsy is caused by the loss of orexin neuropeptides, which are mediators of central nervous system (CNS) control of energy metabolism and maintenance of sleep-wake states. Rapid weight gain and precocious puberty can occur in children with type 1 narcolepsy. This patient's rapid weight gain started to make more sense once the diagnosis was made.[14]\\nIn type 1 narcolepsy, the lack of consistent REM sleep at night leads to the intrusion of REM sleep features into the waking state. The diagnostic features include the tetrad of daytime sleepiness, cataplexy, hypnagogic hallucinations, and sleep paralysis. Specific questioning is usually required to elicit the history; only cataplexy is specific for narcolepsy. Patients often present initially with hypersomnolence alone, and other diagnostic findings may emerge over time.\\nThe etiology of narcolepsy is unclear. The lack of orexin may be related to autoimmune disease or infectious diseases. Most patients with type 1 narcolepsy have HLA DQB1 (0602 allele), the gene complex that encodes for proteins on the surface of T cells. Additionally, some infections (most notably H1N1 influenza, as well as some vaccines for it) are associated with clusters of type 1 narcolepsy and reduced orexin levels.[15,16,17] However, measurement of cerebrospinal fluid (CSF) levels of orexin is not required to make the diagnosis of narcolepsy.\\nThe diagnosis of type 1 narcolepsy can be clinically made in a child with a clear history of cataplexy, EDS, and an otherwise normal neurologic examination. In the absence of cataplexy, an NPSG followed by an MSLT can be used to make the diagnosis of narcolepsy. \\\"Secondary narcolepsy\\\" in the setting of CNS diseases such as hypothalamic tumors or arteriovenous malformations, following cerebrovascular accidents, or in association with multiple sclerosis or Niemann-Pick disease type C has been reported, but alternative causes of narcolepsy are vanishingly rare in childhood. The primary challenge is to rule out other sleep disorders causing the EDS; as in this patient, that may be difficult.\\n\\n ## Figures\\n\\n \\n*Page 4 of 6*\",\n \"pagination\": {\n \"current_page\": 4,\n \"total_pages\": 6\n },\n \"questionnaire\": [],\n \"title\": \"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\"\n },\n {\n \"authors\": \"Timothy D. Murphy, MD\",\n \"content\": [\n \"The treatment of narcolepsy focuses first on attempts to reduce the EDS pharmacologically; timed naps or increased time in bed is not usually sufficient to reduce the EDS. Although many medications have been used to treat EDS, clinicians typically start with caffeine (usually inadequate) and then move to stronger stimulants, such as methylphenidate or amphetamine and dextroamphetamine in combination.\",\n \"Failure of these agents might then lead to the use of modafinil (prescription without the failure of other therapies is often difficult). Monitoring of response and fairly frequent visits are required at this point. A selective serotonin reuptake inhibitor, such as fluoxetine, is often added to the regimen of patients with classic cataplexy. As was the case for this patient, the use of medications that might affect mood, attention, learning, and sleep requires close attention and collaboration between specialists in sleep medicine, neurology, and behavioral and general pediatrics.\",\n \"In some patients, including this patient, sodium oxybate (gamma-hydroxybutyrate [GHB]) is required to treat the cataplexy and to lead to better daytime functioning.[18] The exact mechanism of action is unknown, but the evening dosing of GHB is associated with improved REM sleep at night, perhaps relieving the intrusion of REM during daytime wake periods associated with type 1 narcolepsy. Unfortunately, GHB is associated with abuse — it is often called the \\\"date rape drug\\\" — and is now tightly regulated. Prescription in the United States is limited to one US pharmacy, and a sleep physician is typically required to obtain and use this medication.\",\n \"The finding of EDS requires exploration of nocturnal problems with sleep, including RLS, OSA, and behavioral insomnia that affects daytime functioning. Narcolepsy can be diagnosed as the cause of EDS on the basis of careful history-taking as well as the results of an NPSG and an MSLT.\"\n ],\n \"date\": \"October 09, 2020\",\n \"figures\": [],\n \"markdown\": \"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\\n\\n **Authors:** Timothy D. Murphy, MD \\n **Date:** October 09, 2020\\n\\n ## Content\\n\\n The treatment of narcolepsy focuses first on attempts to reduce the EDS pharmacologically; timed naps or increased time in bed is not usually sufficient to reduce the EDS. Although many medications have been used to treat EDS, clinicians typically start with caffeine (usually inadequate) and then move to stronger stimulants, such as methylphenidate or amphetamine and dextroamphetamine in combination.\\nFailure of these agents might then lead to the use of modafinil (prescription without the failure of other therapies is often difficult). Monitoring of response and fairly frequent visits are required at this point. A selective serotonin reuptake inhibitor, such as fluoxetine, is often added to the regimen of patients with classic cataplexy. As was the case for this patient, the use of medications that might affect mood, attention, learning, and sleep requires close attention and collaboration between specialists in sleep medicine, neurology, and behavioral and general pediatrics.\\nIn some patients, including this patient, sodium oxybate (gamma-hydroxybutyrate [GHB]) is required to treat the cataplexy and to lead to better daytime functioning.[18] The exact mechanism of action is unknown, but the evening dosing of GHB is associated with improved REM sleep at night, perhaps relieving the intrusion of REM during daytime wake periods associated with type 1 narcolepsy. Unfortunately, GHB is associated with abuse — it is often called the \\\"date rape drug\\\" — and is now tightly regulated. Prescription in the United States is limited to one US pharmacy, and a sleep physician is typically required to obtain and use this medication.\\nThe finding of EDS requires exploration of nocturnal problems with sleep, including RLS, OSA, and behavioral insomnia that affects daytime functioning. Narcolepsy can be diagnosed as the cause of EDS on the basis of careful history-taking as well as the results of an NPSG and an MSLT.\\n\\n ## Figures\\n\\n \\n*Page 5 of 6*\",\n \"pagination\": {\n \"current_page\": 5,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1529068,\n \"choiceText\": \"Narcolepsy without cataplexy (type 2 narcolepsy) is associated with increased orexin neuropeptide levels\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529069,\n \"choiceText\": \"Childhood narcolepsy is characterized by multiple brief naps during the day\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529070,\n \"choiceText\": \"Narcolepsy is associated with the loss of orexin neuropeptides\",\n \"correct\": true,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529071,\n \"choiceText\": \"Measurement of orexin levels in the CSF is required for the diagnosis of narcolepsy\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Levels of orexin neuropeptides in the CNS are reduced, not increased, in all forms of narcolepsy. Children more frequently present with prolonged daytime sleep, and multiple naps are typically seen in older patients. The diagnosis can be made by a careful history-taking that documents cataplexy, which is explained only by type 1 narcolepsy. Measurement of CSF levels of orexin is usually related to research only and typically is not used clinically in diagnosing narcolepsy.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 490074,\n \"questionText\": \"Which of the following is most accurate regarding narcolepsy in children?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1529072,\n \"choiceText\": \"Timed or planned naps to reduce sleep pressure, and amphetamine and dextroamphetamine for stimulant therapy during the day\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529073,\n \"choiceText\": \"Modafinil as a daytime stimulant, fluoxetine for cataplexy, and sodium oxybate to improve REM efficiency\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529074,\n \"choiceText\": \"Caffeine as a morning stimulant and sodium oxybate (gamma-hydroxybutyrate [GHB]) used at night to consolidate non-REM sleep\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529075,\n \"choiceText\": \"Methylphenidate to reduce cataplexy, fluoxetine to reduce depressive symptoms, and sodium oxybate to prolong REM latency\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Caffeine is usually an inadequate stimulant for patients with narcolepsy. The daytime use of methylphenidate or amphetamine and dextroamphetamine in combination does not adequately reduce cataplexy and does not address the problem with REM sleep at night. Modafinil is a more reliable daytime stimulant, and fluoxetine helps reduce cataplexy. The use of sodium oxybate in the evening in divided doses is intended to consolidate REM sleep and may reduce REM latency; non-REM sleep is not related to the daytime difficulties associated with narcolepsy.\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 490075,\n \"questionText\": \"Which of the following is typically required in the treatment of type 1 narcolepsy?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\"\n },\n {\n \"authors\": \"Timothy D. Murphy, MD\",\n \"content\": [],\n \"date\": \"October 09, 2020\",\n \"figures\": [],\n \"markdown\": \"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\\n\\n **Authors:** Timothy D. Murphy, MD \\n **Date:** October 09, 2020\\n\\n ## Content\\n\\n \\n\\n ## Figures\\n\\n \\n*Page 6 of 6*\",\n \"pagination\": {\n \"current_page\": 6,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1529068,\n \"choiceText\": \"Narcolepsy without cataplexy (type 2 narcolepsy) is associated with increased orexin neuropeptide levels\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529069,\n \"choiceText\": \"Childhood narcolepsy is characterized by multiple brief naps during the day\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529070,\n \"choiceText\": \"Narcolepsy is associated with the loss of orexin neuropeptides\",\n \"correct\": true,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529071,\n \"choiceText\": \"Measurement of orexin levels in the CSF is required for the diagnosis of narcolepsy\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Levels of orexin neuropeptides in the CNS are reduced, not increased, in all forms of narcolepsy. Children more frequently present with prolonged daytime sleep, and multiple naps are typically seen in older patients. The diagnosis can be made by a careful history-taking that documents cataplexy, which is explained only by type 1 narcolepsy. Measurement of CSF levels of orexin is usually related to research only and typically is not used clinically in diagnosing narcolepsy.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 490074,\n \"questionText\": \"Which of the following is most accurate regarding narcolepsy in children?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1529072,\n \"choiceText\": \"Timed or planned naps to reduce sleep pressure, and amphetamine and dextroamphetamine for stimulant therapy during the day\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529073,\n \"choiceText\": \"Modafinil as a daytime stimulant, fluoxetine for cataplexy, and sodium oxybate to improve REM efficiency\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529074,\n \"choiceText\": \"Caffeine as a morning stimulant and sodium oxybate (gamma-hydroxybutyrate [GHB]) used at night to consolidate non-REM sleep\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529075,\n \"choiceText\": \"Methylphenidate to reduce cataplexy, fluoxetine to reduce depressive symptoms, and sodium oxybate to prolong REM latency\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Caffeine is usually an inadequate stimulant for patients with narcolepsy. The daytime use of methylphenidate or amphetamine and dextroamphetamine in combination does not adequately reduce cataplexy and does not address the problem with REM sleep at night. Modafinil is a more reliable daytime stimulant, and fluoxetine helps reduce cataplexy. The use of sodium oxybate in the evening in divided doses is intended to consolidate REM sleep and may reduce REM latency; non-REM sleep is not related to the daytime difficulties associated with narcolepsy.\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 490075,\n \"questionText\": \"Which of the following is typically required in the treatment of type 1 narcolepsy?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\"\n }\n]"},"questions":{"kind":"list like","value":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1529064,"choiceText":"Behavioral insomnia of childhood\r\n","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529065,"choiceText":"Pediatric chronic obstructive pulmonary disease","correct":false,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529066,"choiceText":"Delayed sleep phase disorder","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529067,"choiceText":"Narcolepsy","correct":true,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"","displayOrder":1,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":490073,"questionText":"On the basis of these findings only, what is the most likely diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1529068,"choiceText":"Narcolepsy without cataplexy (type 2 narcolepsy) is associated with increased orexin neuropeptide levels","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529069,"choiceText":"Childhood narcolepsy is characterized by multiple brief naps during the day","correct":false,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529070,"choiceText":"Narcolepsy is associated with the loss of orexin neuropeptides","correct":true,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529071,"choiceText":"Measurement of orexin levels in the CSF is required for the diagnosis of narcolepsy","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Levels of orexin neuropeptides in the CNS are reduced, not increased, in all forms of narcolepsy. Children more frequently present with prolonged daytime sleep, and multiple naps are typically seen in older patients. The diagnosis can be made by a careful history-taking that documents cataplexy, which is explained only by type 1 narcolepsy. Measurement of CSF levels of orexin is usually related to research only and typically is not used clinically in diagnosing narcolepsy.","displayOrder":2,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":490074,"questionText":"Which of the following is most accurate regarding narcolepsy in children?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1529072,"choiceText":"Timed or planned naps to reduce sleep pressure, and amphetamine and dextroamphetamine for stimulant therapy during the day\r\n","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529073,"choiceText":"Modafinil as a daytime stimulant, fluoxetine for cataplexy, and sodium oxybate to improve REM efficiency","correct":true,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529074,"choiceText":"Caffeine as a morning stimulant and sodium oxybate (gamma-hydroxybutyrate [GHB]) used at night to consolidate non-REM sleep","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529075,"choiceText":"Methylphenidate to reduce cataplexy, fluoxetine to reduce depressive symptoms, and sodium oxybate to prolong REM latency","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Caffeine is usually an inadequate stimulant for patients with narcolepsy. The daytime use of methylphenidate or amphetamine and dextroamphetamine in combination does not adequately reduce cataplexy and does not address the problem with REM sleep at night. Modafinil is a more reliable daytime stimulant, and fluoxetine helps reduce cataplexy. The use of sodium oxybate in the evening in divided doses is intended to consolidate REM sleep and may reduce REM latency; non-REM sleep is not related to the daytime difficulties associated with narcolepsy.","displayOrder":3,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":490075,"questionText":"Which of the following is typically required in the treatment of type 1 narcolepsy?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"string":"[\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1529064,\n \"choiceText\": \"Behavioral insomnia of childhood\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529065,\n \"choiceText\": \"Pediatric chronic obstructive pulmonary disease\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529066,\n \"choiceText\": \"Delayed sleep phase disorder\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529067,\n \"choiceText\": \"Narcolepsy\",\n \"correct\": true,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\",\n \"displayOrder\": 1,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 490073,\n \"questionText\": \"On the basis of these findings only, what is the most likely diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1529068,\n \"choiceText\": \"Narcolepsy without cataplexy (type 2 narcolepsy) is associated with increased orexin neuropeptide levels\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529069,\n \"choiceText\": \"Childhood narcolepsy is characterized by multiple brief naps during the day\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529070,\n \"choiceText\": \"Narcolepsy is associated with the loss of orexin neuropeptides\",\n \"correct\": true,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529071,\n \"choiceText\": \"Measurement of orexin levels in the CSF is required for the diagnosis of narcolepsy\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Levels of orexin neuropeptides in the CNS are reduced, not increased, in all forms of narcolepsy. Children more frequently present with prolonged daytime sleep, and multiple naps are typically seen in older patients. The diagnosis can be made by a careful history-taking that documents cataplexy, which is explained only by type 1 narcolepsy. Measurement of CSF levels of orexin is usually related to research only and typically is not used clinically in diagnosing narcolepsy.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 490074,\n \"questionText\": \"Which of the following is most accurate regarding narcolepsy in children?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1529072,\n \"choiceText\": \"Timed or planned naps to reduce sleep pressure, and amphetamine and dextroamphetamine for stimulant therapy during the day\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529073,\n \"choiceText\": \"Modafinil as a daytime stimulant, fluoxetine for cataplexy, and sodium oxybate to improve REM efficiency\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529074,\n \"choiceText\": \"Caffeine as a morning stimulant and sodium oxybate (gamma-hydroxybutyrate [GHB]) used at night to consolidate non-REM sleep\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529075,\n \"choiceText\": \"Methylphenidate to reduce cataplexy, fluoxetine to reduce depressive symptoms, and sodium oxybate to prolong REM latency\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Caffeine is usually an inadequate stimulant for patients with narcolepsy. The daytime use of methylphenidate or amphetamine and dextroamphetamine in combination does not adequately reduce cataplexy and does not address the problem with REM sleep at night. Modafinil is a more reliable daytime stimulant, and fluoxetine helps reduce cataplexy. The use of sodium oxybate in the evening in divided doses is intended to consolidate REM sleep and may reduce REM latency; non-REM sleep is not related to the daytime difficulties associated with narcolepsy.\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 490075,\n \"questionText\": \"Which of the following is typically required in the treatment of type 1 narcolepsy?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n]"}}},{"rowIdx":299,"cells":{"article_id":{"kind":"string","value":"904350"},"url":{"kind":"string","value":"/viewarticle/904350"},"article_data":{"kind":"list like","value":[{"authors":"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO","content":["Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.","A 49-year-old man with a significant medical history of alcohol abuse, tobacco dependence, and pancreatitis presents to the emergency department (ED) with abdominal pain that has lasted for 3 days. The abdominal pain has been intermittent, achy, and located in the periumbilical region. Associated symptoms have included nausea and vomiting, with several episodes of watery, brown diarrhea.","The patient reports a history of alcohol abuse, stating that he has ingested at least 1 pint a day since he was a teenager. He states that this pain feels different from the pain associated with his last bout of pancreatitis."],"date":"October 02, 2020","figures":[],"markdown":"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\n\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \n **Date:** October 02, 2020\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 49-year-old man with a significant medical history of alcohol abuse, tobacco dependence, and pancreatitis presents to the emergency department (ED) with abdominal pain that has lasted for 3 days. The abdominal pain has been intermittent, achy, and located in the periumbilical region. Associated symptoms have included nausea and vomiting, with several episodes of watery, brown diarrhea.\nThe patient reports a history of alcohol abuse, stating that he has ingested at least 1 pint a day since he was a teenager. He states that this pain feels different from the pain associated with his last bout of pancreatitis.\n\n ## Figures\n\n \n*Page 1 of 6*","pagination":{"current_page":1,"total_pages":6},"questionnaire":[],"title":"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old"},{"authors":"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO","content":["Upon arrival to the ED, the patient has a temperature of 97.9°F (36.6°C), a heart rate of 91 beats/min, a respiratory rate of 23 breaths/min, blood pressure of 113/85 mm Hg, and 98% saturation on room air.","Upon physical examination, he appears uncomfortable and is lying on his right side; he is slightly diaphoretic, with dry oral mucosa. Abdominal examination reveals a soft abdomen with apparent tenderness to palpation in the epigastric and periumbilical region, with minimal left upper-quadrant pain. His abdominal pain appears out of proportion to the physical examination findings.","His laboratory values are as follows:","White blood cell count: 13,000 cells/µL (reference range, 4,000-11,000 cells/µL)","Hemoglobin level: 14.1 g/dL (reference range, 13.5-17.5 g/dL)","Hematocrit: 39% (reference range, 41%-50%)","Platelet count: 506,000 cells/µL (reference range, 150,000-400,000 cells/µL)","Aspartate aminotransferase level: 126 U/L (reference range, 6-34 IU/L)","Alanine aminotransferase level: 81 U/L (reference range, 7-55 U/L)","Amylase level: 125 U/L (reference range, 30-110 U/L)","Lipase level: 419 U/L (reference range, 0-160 U/L)","Gamma glutamyltransferase level: 58 U/L (reference range, 8-38 U/L)","Lactate dehydrogenase level: 175 U/L (reference range, 140-280 U/L)","Lactic acid level: 0.7 mmol/L (reference range, 0.5-2.2 mmol/L)","Glucose level: 102 mg/dL (reference range, <100 mg/dL)","Rectal examination findings are negative for occult blood. All other laboratory values are unremarkable, including alcohol level. Subsequent CT of the abdomen/pelvis with intravenous contrast was performed (Figures 1-3).","Figure 1.","Figure 2.","Figure 3."],"date":"October 02, 2020","figures":[{"caption":"Figure 1.","image_url":"https://img.medscapestatic.com/article/904/350/904350-Thumb1.png"},{"caption":"Figure 2.","image_url":"https://img.medscapestatic.com/article/904/350/904350-Thumb2.png"},{"caption":"Figure 3.","image_url":"https://img.medscapestatic.com/article/904/350/904350-Thumb3.png"}],"markdown":"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\n\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \n **Date:** October 02, 2020\n\n ## Content\n\n Upon arrival to the ED, the patient has a temperature of 97.9°F (36.6°C), a heart rate of 91 beats/min, a respiratory rate of 23 breaths/min, blood pressure of 113/85 mm Hg, and 98% saturation on room air.\nUpon physical examination, he appears uncomfortable and is lying on his right side; he is slightly diaphoretic, with dry oral mucosa. Abdominal examination reveals a soft abdomen with apparent tenderness to palpation in the epigastric and periumbilical region, with minimal left upper-quadrant pain. His abdominal pain appears out of proportion to the physical examination findings.\nHis laboratory values are as follows:\nWhite blood cell count: 13,000 cells/µL (reference range, 4,000-11,000 cells/µL)\nHemoglobin level: 14.1 g/dL (reference range, 13.5-17.5 g/dL)\nHematocrit: 39% (reference range, 41%-50%)\nPlatelet count: 506,000 cells/µL (reference range, 150,000-400,000 cells/µL)\nAspartate aminotransferase level: 126 U/L (reference range, 6-34 IU/L)\nAlanine aminotransferase level: 81 U/L (reference range, 7-55 U/L)\nAmylase level: 125 U/L (reference range, 30-110 U/L)\nLipase level: 419 U/L (reference range, 0-160 U/L)\nGamma glutamyltransferase level: 58 U/L (reference range, 8-38 U/L)\nLactate dehydrogenase level: 175 U/L (reference range, 140-280 U/L)\nLactic acid level: 0.7 mmol/L (reference range, 0.5-2.2 mmol/L)\nGlucose level: 102 mg/dL (reference range, <100 mg/dL)\nRectal examination findings are negative for occult blood. All other laboratory values are unremarkable, including alcohol level. Subsequent CT of the abdomen/pelvis with intravenous contrast was performed (Figures 1-3).\nFigure 1.\nFigure 2.\nFigure 3.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n\n*Page 2 of 6*","pagination":{"current_page":2,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1281940,"choiceText":"Splenic vein thrombosis","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281942,"choiceText":"Superior mesenteric vein thrombosis","correct":true,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281944,"choiceText":"Mesenteric arterial thrombosis","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281946,"choiceText":"Septic pylephlebitis\r\n","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"","displayOrder":1,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":408509,"questionText":"Based only on these findings, which of the following is the most likely diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old"},{"authors":"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO","content":["Acute mesenteric vein thrombosis (MVT) is a rare but extremely important cause of mesenteric intestinal ischemia. In this patient, CT of the abdomen/pelvis with intravenous contrast revealed a filling defect that was consistent with acute thrombosis within the superior mesenteric vein (SMV), which extends approximately 3 cm cephalad to the portosplenic confluence. Other associated findings on these images included peripancreatic fat stranding and peripancreatic fluid consistent with acute pancreatitis (Figures 1-3).","Figure 1.","Figure 2.","Figure 3.","Pancreatitis results in a vast spectrum of both arterial and venous complications. The vascular complications involved in pancreatitis are major causes of morbidity and mortality. The venous complications result from thrombosis of the splenic vein and, less commonly, the portal vein and the SMV, as seen in the patient in this case. Prompt recognition is of paramount importance and requires a high index of clinical suspicion because aggressive therapy and anticoagulation can limit progression of the potential devastating consequences.","Patients with acute pancreatitis can present with portal vein thrombosis, splenic vein thrombosis, or (less commonly) superior MVT. Clinical research has shown that an isolated venous thrombosis to only the SMV, without simultaneous involvement of either the portal vein or the splenic vein, is rare. This vascular complication is important because of the increased risk for mesenteric ischemia and bowel infarction if not recognized.[1]","MVT is considered a rare condition, with only 1 case per 5000-15000 inpatient admissions per year; it accounts for roughly 6%-9% of all cases of acute mesenteric ischemia.[2] In a systematic review of 3692 patients from 1966 to 2002, MVT was the cause of acute mesenteric ischemia in about 3% of patients.[3]"],"date":"October 02, 2020","figures":[{"caption":"Figure 1.","image_url":"https://img.medscapestatic.com/article/904/350/904350-Thumb1.png"},{"caption":"Figure 2.","image_url":"https://img.medscapestatic.com/article/904/350/904350-Thumb2.png"},{"caption":"Figure 3.","image_url":"https://img.medscapestatic.com/article/904/350/904350-Thumb3.png"}],"markdown":"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\n\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \n **Date:** October 02, 2020\n\n ## Content\n\n Acute mesenteric vein thrombosis (MVT) is a rare but extremely important cause of mesenteric intestinal ischemia. In this patient, CT of the abdomen/pelvis with intravenous contrast revealed a filling defect that was consistent with acute thrombosis within the superior mesenteric vein (SMV), which extends approximately 3 cm cephalad to the portosplenic confluence. Other associated findings on these images included peripancreatic fat stranding and peripancreatic fluid consistent with acute pancreatitis (Figures 1-3).\nFigure 1.\nFigure 2.\nFigure 3.\nPancreatitis results in a vast spectrum of both arterial and venous complications. The vascular complications involved in pancreatitis are major causes of morbidity and mortality. The venous complications result from thrombosis of the splenic vein and, less commonly, the portal vein and the SMV, as seen in the patient in this case. Prompt recognition is of paramount importance and requires a high index of clinical suspicion because aggressive therapy and anticoagulation can limit progression of the potential devastating consequences.\nPatients with acute pancreatitis can present with portal vein thrombosis, splenic vein thrombosis, or (less commonly) superior MVT. Clinical research has shown that an isolated venous thrombosis to only the SMV, without simultaneous involvement of either the portal vein or the splenic vein, is rare. This vascular complication is important because of the increased risk for mesenteric ischemia and bowel infarction if not recognized.[1]\nMVT is considered a rare condition, with only 1 case per 5000-15000 inpatient admissions per year; it accounts for roughly 6%-9% of all cases of acute mesenteric ischemia.[2] In a systematic review of 3692 patients from 1966 to 2002, MVT was the cause of acute mesenteric ischemia in about 3% of patients.[3]\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n\n*Page 3 of 6*","pagination":{"current_page":3,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1281940,"choiceText":"Splenic vein thrombosis","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281942,"choiceText":"Superior mesenteric vein thrombosis","correct":true,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281944,"choiceText":"Mesenteric arterial thrombosis","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281946,"choiceText":"Septic pylephlebitis\r\n","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"","displayOrder":1,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":408509,"questionText":"Based only on these findings, which of the following is the most likely diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old"},{"authors":"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO","content":["Many risk factors for MVT are recognized, including direct injury (eg, abdominal trauma, splenectomy, intra-abdominal inflammatory processes), venous congestion/stasis (eg, congestive heart failure, portal hypertension, cirrhosis), and hypercoagulable conditions (eg, protein C/S deficiency, antithrombin III deficiency, factor V Leiden mutation, pancreatic/colon carcinoma, oral contraceptive use, polycythemia vera, heparin-induced thrombocytopenia, lupus anticoagulant/anti-phospholipid syndrome).[4] In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.[5]","Acute occlusion of the mesenteric vein results in increased resistance within the mesenteric venous bed, leading to decreased perfusion pressure.[3] As flow stagnates in the mesenteric vein, increased venous pressure results in an efflux of fluid into the tissues, leading to bowel-wall edema. If the clinical progression continues, venous return from the bowel wall is completely occluded, and the end result is bowel ischemia.[3] Integrity of the bowel mucosa is lost and bacteria can translocate, leading to lactic acidosis, sepsis, multiorgan failure, and eventually death.[2]","MVT can occur acutely, subacutely, or chronically. The clinical features vary, depending on the location of the thrombus within the splanchnic vasculature.[3] Acute MVT, similar to other forms of acute mesenteric ischemia, presents most often as a colicky periumbilical pain that is often out of proportion to the physical examination findings. However, the onset of venous thrombosis, compared with arterial thrombosis, is often less sudden and dull, with as many as 75% of patients presenting after 2 days of abdominal pain.[3]","Alternatively, chronic mesenteric venous thrombosis often presents with portal hypertension and variceal hemorrhage.[2] In general, peritoneal signs are absent, unless the venous thrombosis goes untreated and the bowel becomes ischemic, in which case peritoneal signs develop.","In a retrospective study, 31 patients diagnosed with MVT from 1985-1999 were reviewed.[4] Approximately 84% of patients presented with abdominal pain, with 16% presenting with peritoneal signs. Common overall symptoms included diarrhea (42%), nausea and vomiting (32%), lower gastrointestinal bleeding (19%), fatigue (16%), and upper gastrointestinal bleeding (10%). Furthermore, only 22 patients were initially treated with heparin. Five patients were found to have peritonitis and underwent exploratory laparotomy, with the ultimate goal to prevent or limit gangrenous bowel, with an additional five patients later undergoing surgery for the development of ischemic bowel. Seven of the 31 patients died within 30 days, secondary to complications from infarcted bowel and multisystemic organ failure. Overall, 19 of the 24 survivors were treated with long-term anticoagulation, with 88% of those surviving long-term.","Differentiating between ischemia secondary to MVT and ischemia secondary to a mesenteric arterial thrombosis is important. MVT presents in the setting of thrombophilia or an inflammatory abdominal process, whereas mesenteric arterial ischemia presents in the setting of cardiac disease, low-flow states, and atrial fibrillation.[1] Similar to all forms of mesenteric ischemia, no clinical features are specific to MVT. As such, a clinician must have a high index of suspicion in order to make an early diagnosis and avoid the complications of an undiagnosed MVT."],"date":"October 02, 2020","figures":[],"markdown":"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\n\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \n **Date:** October 02, 2020\n\n ## Content\n\n Many risk factors for MVT are recognized, including direct injury (eg, abdominal trauma, splenectomy, intra-abdominal inflammatory processes), venous congestion/stasis (eg, congestive heart failure, portal hypertension, cirrhosis), and hypercoagulable conditions (eg, protein C/S deficiency, antithrombin III deficiency, factor V Leiden mutation, pancreatic/colon carcinoma, oral contraceptive use, polycythemia vera, heparin-induced thrombocytopenia, lupus anticoagulant/anti-phospholipid syndrome).[4] In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.[5]\nAcute occlusion of the mesenteric vein results in increased resistance within the mesenteric venous bed, leading to decreased perfusion pressure.[3] As flow stagnates in the mesenteric vein, increased venous pressure results in an efflux of fluid into the tissues, leading to bowel-wall edema. If the clinical progression continues, venous return from the bowel wall is completely occluded, and the end result is bowel ischemia.[3] Integrity of the bowel mucosa is lost and bacteria can translocate, leading to lactic acidosis, sepsis, multiorgan failure, and eventually death.[2]\nMVT can occur acutely, subacutely, or chronically. The clinical features vary, depending on the location of the thrombus within the splanchnic vasculature.[3] Acute MVT, similar to other forms of acute mesenteric ischemia, presents most often as a colicky periumbilical pain that is often out of proportion to the physical examination findings. However, the onset of venous thrombosis, compared with arterial thrombosis, is often less sudden and dull, with as many as 75% of patients presenting after 2 days of abdominal pain.[3]\nAlternatively, chronic mesenteric venous thrombosis often presents with portal hypertension and variceal hemorrhage.[2] In general, peritoneal signs are absent, unless the venous thrombosis goes untreated and the bowel becomes ischemic, in which case peritoneal signs develop.\nIn a retrospective study, 31 patients diagnosed with MVT from 1985-1999 were reviewed.[4] Approximately 84% of patients presented with abdominal pain, with 16% presenting with peritoneal signs. Common overall symptoms included diarrhea (42%), nausea and vomiting (32%), lower gastrointestinal bleeding (19%), fatigue (16%), and upper gastrointestinal bleeding (10%). Furthermore, only 22 patients were initially treated with heparin. Five patients were found to have peritonitis and underwent exploratory laparotomy, with the ultimate goal to prevent or limit gangrenous bowel, with an additional five patients later undergoing surgery for the development of ischemic bowel. Seven of the 31 patients died within 30 days, secondary to complications from infarcted bowel and multisystemic organ failure. Overall, 19 of the 24 survivors were treated with long-term anticoagulation, with 88% of those surviving long-term.\nDifferentiating between ischemia secondary to MVT and ischemia secondary to a mesenteric arterial thrombosis is important. MVT presents in the setting of thrombophilia or an inflammatory abdominal process, whereas mesenteric arterial ischemia presents in the setting of cardiac disease, low-flow states, and atrial fibrillation.[1] Similar to all forms of mesenteric ischemia, no clinical features are specific to MVT. As such, a clinician must have a high index of suspicion in order to make an early diagnosis and avoid the complications of an undiagnosed MVT.\n\n ## Figures\n\n \n*Page 4 of 6*","pagination":{"current_page":4,"total_pages":6},"questionnaire":[],"title":"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old"},{"authors":"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO","content":["Treatment for MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal exams. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence. If evidence of clinical deterioration and bowel infarction is present, surgical intervention is necessary. Broad-spectrum antibiotics are generally reserved for the setting of pylephlebitis, septic thrombophlebitis, and sepsis secondary to bacterial translocation from an infarcted bowel.[2]","Initiation of anticoagulation remains the cornerstone of treatment and should not be delayed.[6]Research has shown that once a patient is transitioned to oral anticoagulation, treatment should continue for 3-6 months, unless a thrombophilia has been diagnosed. After anticoagulation, most MVTs partially or completely recanalize, with one study showing recanalization in 80% of patients who received anticoagulation.[7] However, the recurrence rate has been reported at 15%.","Acute MVT carries a better prognosis than acute mesenteric ischemia. In one systematic review of nearly 3700 cases of acute mesenteric ischemia from 1966 to 2002, the mortality rate of those patients with MVT was 44%, compared with as much as 89% for those patients with advancement to mesenteric ischemia.[8] However, with increasing physician awareness, the use of contrast-enhanced CT to investigate abdominal pain in combination with anticoagulation has improved outcomes in these patients. In more modern studies, the mortality rate of acute MVT is down to 20%, with the most common cause of death being sepsis and multiorgan failure.[8]","In conclusion, acute superior MVT is a rare but important cause of mesenteric intestinal ischemia. It requires a high index of clinical suspicion. Rapid recognition and aggressive therapy are of extreme importance in order to prevent ischemic and infarcted bowel, sepsis, multiorgan failure, and eventual death. The 49-year-old man in this case had nonnecrotizing, alcohol-induced acute pancreatitis, complicated by acute superior MVT.","The patient in this case was eventually transitioned to rivaroxaban and discharged on day 4. Since his discharge, he has entered into alcohol rehabilitation and remains compliant with his anticoagulation."],"date":"October 02, 2020","figures":[],"markdown":"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\n\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \n **Date:** October 02, 2020\n\n ## Content\n\n Treatment for MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal exams. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence. If evidence of clinical deterioration and bowel infarction is present, surgical intervention is necessary. Broad-spectrum antibiotics are generally reserved for the setting of pylephlebitis, septic thrombophlebitis, and sepsis secondary to bacterial translocation from an infarcted bowel.[2]\nInitiation of anticoagulation remains the cornerstone of treatment and should not be delayed.[6]Research has shown that once a patient is transitioned to oral anticoagulation, treatment should continue for 3-6 months, unless a thrombophilia has been diagnosed. After anticoagulation, most MVTs partially or completely recanalize, with one study showing recanalization in 80% of patients who received anticoagulation.[7] However, the recurrence rate has been reported at 15%.\nAcute MVT carries a better prognosis than acute mesenteric ischemia. In one systematic review of nearly 3700 cases of acute mesenteric ischemia from 1966 to 2002, the mortality rate of those patients with MVT was 44%, compared with as much as 89% for those patients with advancement to mesenteric ischemia.[8] However, with increasing physician awareness, the use of contrast-enhanced CT to investigate abdominal pain in combination with anticoagulation has improved outcomes in these patients. In more modern studies, the mortality rate of acute MVT is down to 20%, with the most common cause of death being sepsis and multiorgan failure.[8]\nIn conclusion, acute superior MVT is a rare but important cause of mesenteric intestinal ischemia. It requires a high index of clinical suspicion. Rapid recognition and aggressive therapy are of extreme importance in order to prevent ischemic and infarcted bowel, sepsis, multiorgan failure, and eventual death. The 49-year-old man in this case had nonnecrotizing, alcohol-induced acute pancreatitis, complicated by acute superior MVT.\nThe patient in this case was eventually transitioned to rivaroxaban and discharged on day 4. Since his discharge, he has entered into alcohol rehabilitation and remains compliant with his anticoagulation.\n\n ## Figures\n\n \n*Page 5 of 6*","pagination":{"current_page":5,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1281948,"choiceText":"Pancreatic and inflammatory bowel disease","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281950,"choiceText":"Portal hypertension","correct":false,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281952,"choiceText":"Factor V Leiden mutation","correct":false,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281954,"choiceText":"Splenectomy","correct":false,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281956,"choiceText":"Gastric sleeve","correct":false,"displayOrder":5,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281958,"choiceText":"All of the above\r\n","correct":true,"displayOrder":6,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"MVT has many associated risk factors, including direct injury, venous congestive/stasis, and hypercoagulable conditions. The patient in this case had an extensive history of alcohol abuse and pancreatitis. In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.","displayOrder":2,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":408511,"questionText":"Which of the following is considered a risk factor for the development of MVT?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1281960,"choiceText":"Broad-spectrum antibiotic use is contraindicated at this point","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281962,"choiceText":"Surgical consultation is unnecessary at this point","correct":false,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281964,"choiceText":"Anticoagulation should be delayed until further investigation is done","correct":false,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281966,"choiceText":"Bowel rest and fluid resuscitation should be promptly initiated","correct":true,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Treatment of MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal examinations. In this particular case, the patient is septic and has evidence of an intra-abdominal source in the setting of SMV thrombosis. If evidence suggests clinical deterioration and bowel infarction, surgical intervention is necessary.
\r\n\r\nIn this case, the patient has voluntary guarding and an elevated lactic acid level, making an emergent surgical consult necessary. Broad-spectrum antibiotics are generally reserved for patients with pylephlebitis, those with septic thrombophlebitis, and those with sepsis secondary to bacterial translocation from an infarcted bowel.\r\n
\r\nInitiation of anticoagulation remains the cornerstone of treatment and should not be delayed. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence.\r\n","displayOrder":3,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":408513,"questionText":"A 53-year-old man with a significant medical history of pancreatitis presents to the ED with nausea, vomiting, and abdominal pain. His vital signs are notable for a heart rate of 113 beats/min, respiratory rate of 24 breaths/min, and a blood pressure of 96/50 mm Hg, with a temperature of 101.3°F (38.5°C). Abdominal examination reveals diffuse tenderness to palpation with voluntary guarding. Laboratory values are notable for a lactic acid level of 4.6 mmol/L, neutrophil-predominant leukocytosis of 19 × 109 cells/L, and a lipase level of 459 U/L. CT of the abdomen/pelvis reveals superior MVT. \r\n
\r\nWhich of the following is accurate regarding his treatment?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old"},{"authors":"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO","content":[],"date":"October 02, 2020","figures":[],"markdown":"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\n\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \n **Date:** October 02, 2020\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*","pagination":{"current_page":6,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1281948,"choiceText":"Pancreatic and inflammatory bowel disease","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281950,"choiceText":"Portal hypertension","correct":false,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281952,"choiceText":"Factor V Leiden mutation","correct":false,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281954,"choiceText":"Splenectomy","correct":false,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281956,"choiceText":"Gastric sleeve","correct":false,"displayOrder":5,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281958,"choiceText":"All of the above\r\n","correct":true,"displayOrder":6,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"MVT has many associated risk factors, including direct injury, venous congestive/stasis, and hypercoagulable conditions. The patient in this case had an extensive history of alcohol abuse and pancreatitis. In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.","displayOrder":2,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":408511,"questionText":"Which of the following is considered a risk factor for the development of MVT?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1281960,"choiceText":"Broad-spectrum antibiotic use is contraindicated at this point","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281962,"choiceText":"Surgical consultation is unnecessary at this point","correct":false,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281964,"choiceText":"Anticoagulation should be delayed until further investigation is done","correct":false,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281966,"choiceText":"Bowel rest and fluid resuscitation should be promptly initiated","correct":true,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Treatment of MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal examinations. In this particular case, the patient is septic and has evidence of an intra-abdominal source in the setting of SMV thrombosis. If evidence suggests clinical deterioration and bowel infarction, surgical intervention is necessary.
\r\n\r\nIn this case, the patient has voluntary guarding and an elevated lactic acid level, making an emergent surgical consult necessary. Broad-spectrum antibiotics are generally reserved for patients with pylephlebitis, those with septic thrombophlebitis, and those with sepsis secondary to bacterial translocation from an infarcted bowel.\r\n
\r\nInitiation of anticoagulation remains the cornerstone of treatment and should not be delayed. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence.\r\n","displayOrder":3,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":408513,"questionText":"A 53-year-old man with a significant medical history of pancreatitis presents to the ED with nausea, vomiting, and abdominal pain. His vital signs are notable for a heart rate of 113 beats/min, respiratory rate of 24 breaths/min, and a blood pressure of 96/50 mm Hg, with a temperature of 101.3°F (38.5°C). Abdominal examination reveals diffuse tenderness to palpation with voluntary guarding. Laboratory values are notable for a lactic acid level of 4.6 mmol/L, neutrophil-predominant leukocytosis of 19 × 109 cells/L, and a lipase level of 459 U/L. CT of the abdomen/pelvis reveals superior MVT. \r\n
\r\nWhich of the following is accurate regarding his treatment?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old"}],"string":"[\n {\n \"authors\": \"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO\",\n \"content\": [\n \"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\",\n \"A 49-year-old man with a significant medical history of alcohol abuse, tobacco dependence, and pancreatitis presents to the emergency department (ED) with abdominal pain that has lasted for 3 days. The abdominal pain has been intermittent, achy, and located in the periumbilical region. Associated symptoms have included nausea and vomiting, with several episodes of watery, brown diarrhea.\",\n \"The patient reports a history of alcohol abuse, stating that he has ingested at least 1 pint a day since he was a teenager. He states that this pain feels different from the pain associated with his last bout of pancreatitis.\"\n ],\n \"date\": \"October 02, 2020\",\n \"figures\": [],\n \"markdown\": \"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\\n\\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \\n **Date:** October 02, 2020\\n\\n ## Content\\n\\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\\nA 49-year-old man with a significant medical history of alcohol abuse, tobacco dependence, and pancreatitis presents to the emergency department (ED) with abdominal pain that has lasted for 3 days. The abdominal pain has been intermittent, achy, and located in the periumbilical region. Associated symptoms have included nausea and vomiting, with several episodes of watery, brown diarrhea.\\nThe patient reports a history of alcohol abuse, stating that he has ingested at least 1 pint a day since he was a teenager. He states that this pain feels different from the pain associated with his last bout of pancreatitis.\\n\\n ## Figures\\n\\n \\n*Page 1 of 6*\",\n \"pagination\": {\n \"current_page\": 1,\n \"total_pages\": 6\n },\n \"questionnaire\": [],\n \"title\": \"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\"\n },\n {\n \"authors\": \"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO\",\n \"content\": [\n \"Upon arrival to the ED, the patient has a temperature of 97.9°F (36.6°C), a heart rate of 91 beats/min, a respiratory rate of 23 breaths/min, blood pressure of 113/85 mm Hg, and 98% saturation on room air.\",\n \"Upon physical examination, he appears uncomfortable and is lying on his right side; he is slightly diaphoretic, with dry oral mucosa. Abdominal examination reveals a soft abdomen with apparent tenderness to palpation in the epigastric and periumbilical region, with minimal left upper-quadrant pain. His abdominal pain appears out of proportion to the physical examination findings.\",\n \"His laboratory values are as follows:\",\n \"White blood cell count: 13,000 cells/µL (reference range, 4,000-11,000 cells/µL)\",\n \"Hemoglobin level: 14.1 g/dL (reference range, 13.5-17.5 g/dL)\",\n \"Hematocrit: 39% (reference range, 41%-50%)\",\n \"Platelet count: 506,000 cells/µL (reference range, 150,000-400,000 cells/µL)\",\n \"Aspartate aminotransferase level: 126 U/L (reference range, 6-34 IU/L)\",\n \"Alanine aminotransferase level: 81 U/L (reference range, 7-55 U/L)\",\n \"Amylase level: 125 U/L (reference range, 30-110 U/L)\",\n \"Lipase level: 419 U/L (reference range, 0-160 U/L)\",\n \"Gamma glutamyltransferase level: 58 U/L (reference range, 8-38 U/L)\",\n \"Lactate dehydrogenase level: 175 U/L (reference range, 140-280 U/L)\",\n \"Lactic acid level: 0.7 mmol/L (reference range, 0.5-2.2 mmol/L)\",\n \"Glucose level: 102 mg/dL (reference range, <100 mg/dL)\",\n \"Rectal examination findings are negative for occult blood. All other laboratory values are unremarkable, including alcohol level. Subsequent CT of the abdomen/pelvis with intravenous contrast was performed (Figures 1-3).\",\n \"Figure 1.\",\n \"Figure 2.\",\n \"Figure 3.\"\n ],\n \"date\": \"October 02, 2020\",\n \"figures\": [\n {\n \"caption\": \"Figure 1.\",\n \"image_url\": \"https://img.medscapestatic.com/article/904/350/904350-Thumb1.png\"\n },\n {\n \"caption\": \"Figure 2.\",\n \"image_url\": \"https://img.medscapestatic.com/article/904/350/904350-Thumb2.png\"\n },\n {\n \"caption\": \"Figure 3.\",\n \"image_url\": \"https://img.medscapestatic.com/article/904/350/904350-Thumb3.png\"\n }\n ],\n \"markdown\": \"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\\n\\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \\n **Date:** October 02, 2020\\n\\n ## Content\\n\\n Upon arrival to the ED, the patient has a temperature of 97.9°F (36.6°C), a heart rate of 91 beats/min, a respiratory rate of 23 breaths/min, blood pressure of 113/85 mm Hg, and 98% saturation on room air.\\nUpon physical examination, he appears uncomfortable and is lying on his right side; he is slightly diaphoretic, with dry oral mucosa. Abdominal examination reveals a soft abdomen with apparent tenderness to palpation in the epigastric and periumbilical region, with minimal left upper-quadrant pain. His abdominal pain appears out of proportion to the physical examination findings.\\nHis laboratory values are as follows:\\nWhite blood cell count: 13,000 cells/µL (reference range, 4,000-11,000 cells/µL)\\nHemoglobin level: 14.1 g/dL (reference range, 13.5-17.5 g/dL)\\nHematocrit: 39% (reference range, 41%-50%)\\nPlatelet count: 506,000 cells/µL (reference range, 150,000-400,000 cells/µL)\\nAspartate aminotransferase level: 126 U/L (reference range, 6-34 IU/L)\\nAlanine aminotransferase level: 81 U/L (reference range, 7-55 U/L)\\nAmylase level: 125 U/L (reference range, 30-110 U/L)\\nLipase level: 419 U/L (reference range, 0-160 U/L)\\nGamma glutamyltransferase level: 58 U/L (reference range, 8-38 U/L)\\nLactate dehydrogenase level: 175 U/L (reference range, 140-280 U/L)\\nLactic acid level: 0.7 mmol/L (reference range, 0.5-2.2 mmol/L)\\nGlucose level: 102 mg/dL (reference range, <100 mg/dL)\\nRectal examination findings are negative for occult blood. All other laboratory values are unremarkable, including alcohol level. Subsequent CT of the abdomen/pelvis with intravenous contrast was performed (Figures 1-3).\\nFigure 1.\\nFigure 2.\\nFigure 3.\\n\\n ## Figures\\n\\n **Figure 1.** \\n \\n\\n**Figure 2.** \\n \\n\\n**Figure 3.** \\n \\n\\n\\n*Page 2 of 6*\",\n \"pagination\": {\n \"current_page\": 2,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1281940,\n \"choiceText\": \"Splenic vein thrombosis\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281942,\n \"choiceText\": \"Superior mesenteric vein thrombosis\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281944,\n \"choiceText\": \"Mesenteric arterial thrombosis\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281946,\n \"choiceText\": \"Septic pylephlebitis\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\",\n \"displayOrder\": 1,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 408509,\n \"questionText\": \"Based only on these findings, which of the following is the most likely diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\"\n },\n {\n \"authors\": \"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO\",\n \"content\": [\n \"Acute mesenteric vein thrombosis (MVT) is a rare but extremely important cause of mesenteric intestinal ischemia. In this patient, CT of the abdomen/pelvis with intravenous contrast revealed a filling defect that was consistent with acute thrombosis within the superior mesenteric vein (SMV), which extends approximately 3 cm cephalad to the portosplenic confluence. Other associated findings on these images included peripancreatic fat stranding and peripancreatic fluid consistent with acute pancreatitis (Figures 1-3).\",\n \"Figure 1.\",\n \"Figure 2.\",\n \"Figure 3.\",\n \"Pancreatitis results in a vast spectrum of both arterial and venous complications. The vascular complications involved in pancreatitis are major causes of morbidity and mortality. The venous complications result from thrombosis of the splenic vein and, less commonly, the portal vein and the SMV, as seen in the patient in this case. Prompt recognition is of paramount importance and requires a high index of clinical suspicion because aggressive therapy and anticoagulation can limit progression of the potential devastating consequences.\",\n \"Patients with acute pancreatitis can present with portal vein thrombosis, splenic vein thrombosis, or (less commonly) superior MVT. Clinical research has shown that an isolated venous thrombosis to only the SMV, without simultaneous involvement of either the portal vein or the splenic vein, is rare. This vascular complication is important because of the increased risk for mesenteric ischemia and bowel infarction if not recognized.[1]\",\n \"MVT is considered a rare condition, with only 1 case per 5000-15000 inpatient admissions per year; it accounts for roughly 6%-9% of all cases of acute mesenteric ischemia.[2] In a systematic review of 3692 patients from 1966 to 2002, MVT was the cause of acute mesenteric ischemia in about 3% of patients.[3]\"\n ],\n \"date\": \"October 02, 2020\",\n \"figures\": [\n {\n \"caption\": \"Figure 1.\",\n \"image_url\": \"https://img.medscapestatic.com/article/904/350/904350-Thumb1.png\"\n },\n {\n \"caption\": \"Figure 2.\",\n \"image_url\": \"https://img.medscapestatic.com/article/904/350/904350-Thumb2.png\"\n },\n {\n \"caption\": \"Figure 3.\",\n \"image_url\": \"https://img.medscapestatic.com/article/904/350/904350-Thumb3.png\"\n }\n ],\n \"markdown\": \"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\\n\\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \\n **Date:** October 02, 2020\\n\\n ## Content\\n\\n Acute mesenteric vein thrombosis (MVT) is a rare but extremely important cause of mesenteric intestinal ischemia. In this patient, CT of the abdomen/pelvis with intravenous contrast revealed a filling defect that was consistent with acute thrombosis within the superior mesenteric vein (SMV), which extends approximately 3 cm cephalad to the portosplenic confluence. Other associated findings on these images included peripancreatic fat stranding and peripancreatic fluid consistent with acute pancreatitis (Figures 1-3).\\nFigure 1.\\nFigure 2.\\nFigure 3.\\nPancreatitis results in a vast spectrum of both arterial and venous complications. The vascular complications involved in pancreatitis are major causes of morbidity and mortality. The venous complications result from thrombosis of the splenic vein and, less commonly, the portal vein and the SMV, as seen in the patient in this case. Prompt recognition is of paramount importance and requires a high index of clinical suspicion because aggressive therapy and anticoagulation can limit progression of the potential devastating consequences.\\nPatients with acute pancreatitis can present with portal vein thrombosis, splenic vein thrombosis, or (less commonly) superior MVT. Clinical research has shown that an isolated venous thrombosis to only the SMV, without simultaneous involvement of either the portal vein or the splenic vein, is rare. This vascular complication is important because of the increased risk for mesenteric ischemia and bowel infarction if not recognized.[1]\\nMVT is considered a rare condition, with only 1 case per 5000-15000 inpatient admissions per year; it accounts for roughly 6%-9% of all cases of acute mesenteric ischemia.[2] In a systematic review of 3692 patients from 1966 to 2002, MVT was the cause of acute mesenteric ischemia in about 3% of patients.[3]\\n\\n ## Figures\\n\\n **Figure 1.** \\n \\n\\n**Figure 2.** \\n \\n\\n**Figure 3.** \\n \\n\\n\\n*Page 3 of 6*\",\n \"pagination\": {\n \"current_page\": 3,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1281940,\n \"choiceText\": \"Splenic vein thrombosis\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281942,\n \"choiceText\": \"Superior mesenteric vein thrombosis\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281944,\n \"choiceText\": \"Mesenteric arterial thrombosis\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281946,\n \"choiceText\": \"Septic pylephlebitis\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\",\n \"displayOrder\": 1,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 408509,\n \"questionText\": \"Based only on these findings, which of the following is the most likely diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\"\n },\n {\n \"authors\": \"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO\",\n \"content\": [\n \"Many risk factors for MVT are recognized, including direct injury (eg, abdominal trauma, splenectomy, intra-abdominal inflammatory processes), venous congestion/stasis (eg, congestive heart failure, portal hypertension, cirrhosis), and hypercoagulable conditions (eg, protein C/S deficiency, antithrombin III deficiency, factor V Leiden mutation, pancreatic/colon carcinoma, oral contraceptive use, polycythemia vera, heparin-induced thrombocytopenia, lupus anticoagulant/anti-phospholipid syndrome).[4] In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.[5]\",\n \"Acute occlusion of the mesenteric vein results in increased resistance within the mesenteric venous bed, leading to decreased perfusion pressure.[3] As flow stagnates in the mesenteric vein, increased venous pressure results in an efflux of fluid into the tissues, leading to bowel-wall edema. If the clinical progression continues, venous return from the bowel wall is completely occluded, and the end result is bowel ischemia.[3] Integrity of the bowel mucosa is lost and bacteria can translocate, leading to lactic acidosis, sepsis, multiorgan failure, and eventually death.[2]\",\n \"MVT can occur acutely, subacutely, or chronically. The clinical features vary, depending on the location of the thrombus within the splanchnic vasculature.[3] Acute MVT, similar to other forms of acute mesenteric ischemia, presents most often as a colicky periumbilical pain that is often out of proportion to the physical examination findings. However, the onset of venous thrombosis, compared with arterial thrombosis, is often less sudden and dull, with as many as 75% of patients presenting after 2 days of abdominal pain.[3]\",\n \"Alternatively, chronic mesenteric venous thrombosis often presents with portal hypertension and variceal hemorrhage.[2] In general, peritoneal signs are absent, unless the venous thrombosis goes untreated and the bowel becomes ischemic, in which case peritoneal signs develop.\",\n \"In a retrospective study, 31 patients diagnosed with MVT from 1985-1999 were reviewed.[4] Approximately 84% of patients presented with abdominal pain, with 16% presenting with peritoneal signs. Common overall symptoms included diarrhea (42%), nausea and vomiting (32%), lower gastrointestinal bleeding (19%), fatigue (16%), and upper gastrointestinal bleeding (10%). Furthermore, only 22 patients were initially treated with heparin. Five patients were found to have peritonitis and underwent exploratory laparotomy, with the ultimate goal to prevent or limit gangrenous bowel, with an additional five patients later undergoing surgery for the development of ischemic bowel. Seven of the 31 patients died within 30 days, secondary to complications from infarcted bowel and multisystemic organ failure. Overall, 19 of the 24 survivors were treated with long-term anticoagulation, with 88% of those surviving long-term.\",\n \"Differentiating between ischemia secondary to MVT and ischemia secondary to a mesenteric arterial thrombosis is important. MVT presents in the setting of thrombophilia or an inflammatory abdominal process, whereas mesenteric arterial ischemia presents in the setting of cardiac disease, low-flow states, and atrial fibrillation.[1] Similar to all forms of mesenteric ischemia, no clinical features are specific to MVT. As such, a clinician must have a high index of suspicion in order to make an early diagnosis and avoid the complications of an undiagnosed MVT.\"\n ],\n \"date\": \"October 02, 2020\",\n \"figures\": [],\n \"markdown\": \"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\\n\\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \\n **Date:** October 02, 2020\\n\\n ## Content\\n\\n Many risk factors for MVT are recognized, including direct injury (eg, abdominal trauma, splenectomy, intra-abdominal inflammatory processes), venous congestion/stasis (eg, congestive heart failure, portal hypertension, cirrhosis), and hypercoagulable conditions (eg, protein C/S deficiency, antithrombin III deficiency, factor V Leiden mutation, pancreatic/colon carcinoma, oral contraceptive use, polycythemia vera, heparin-induced thrombocytopenia, lupus anticoagulant/anti-phospholipid syndrome).[4] In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.[5]\\nAcute occlusion of the mesenteric vein results in increased resistance within the mesenteric venous bed, leading to decreased perfusion pressure.[3] As flow stagnates in the mesenteric vein, increased venous pressure results in an efflux of fluid into the tissues, leading to bowel-wall edema. If the clinical progression continues, venous return from the bowel wall is completely occluded, and the end result is bowel ischemia.[3] Integrity of the bowel mucosa is lost and bacteria can translocate, leading to lactic acidosis, sepsis, multiorgan failure, and eventually death.[2]\\nMVT can occur acutely, subacutely, or chronically. The clinical features vary, depending on the location of the thrombus within the splanchnic vasculature.[3] Acute MVT, similar to other forms of acute mesenteric ischemia, presents most often as a colicky periumbilical pain that is often out of proportion to the physical examination findings. However, the onset of venous thrombosis, compared with arterial thrombosis, is often less sudden and dull, with as many as 75% of patients presenting after 2 days of abdominal pain.[3]\\nAlternatively, chronic mesenteric venous thrombosis often presents with portal hypertension and variceal hemorrhage.[2] In general, peritoneal signs are absent, unless the venous thrombosis goes untreated and the bowel becomes ischemic, in which case peritoneal signs develop.\\nIn a retrospective study, 31 patients diagnosed with MVT from 1985-1999 were reviewed.[4] Approximately 84% of patients presented with abdominal pain, with 16% presenting with peritoneal signs. Common overall symptoms included diarrhea (42%), nausea and vomiting (32%), lower gastrointestinal bleeding (19%), fatigue (16%), and upper gastrointestinal bleeding (10%). Furthermore, only 22 patients were initially treated with heparin. Five patients were found to have peritonitis and underwent exploratory laparotomy, with the ultimate goal to prevent or limit gangrenous bowel, with an additional five patients later undergoing surgery for the development of ischemic bowel. Seven of the 31 patients died within 30 days, secondary to complications from infarcted bowel and multisystemic organ failure. Overall, 19 of the 24 survivors were treated with long-term anticoagulation, with 88% of those surviving long-term.\\nDifferentiating between ischemia secondary to MVT and ischemia secondary to a mesenteric arterial thrombosis is important. MVT presents in the setting of thrombophilia or an inflammatory abdominal process, whereas mesenteric arterial ischemia presents in the setting of cardiac disease, low-flow states, and atrial fibrillation.[1] Similar to all forms of mesenteric ischemia, no clinical features are specific to MVT. As such, a clinician must have a high index of suspicion in order to make an early diagnosis and avoid the complications of an undiagnosed MVT.\\n\\n ## Figures\\n\\n \\n*Page 4 of 6*\",\n \"pagination\": {\n \"current_page\": 4,\n \"total_pages\": 6\n },\n \"questionnaire\": [],\n \"title\": \"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\"\n },\n {\n \"authors\": \"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO\",\n \"content\": [\n \"Treatment for MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal exams. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence. If evidence of clinical deterioration and bowel infarction is present, surgical intervention is necessary. Broad-spectrum antibiotics are generally reserved for the setting of pylephlebitis, septic thrombophlebitis, and sepsis secondary to bacterial translocation from an infarcted bowel.[2]\",\n \"Initiation of anticoagulation remains the cornerstone of treatment and should not be delayed.[6]Research has shown that once a patient is transitioned to oral anticoagulation, treatment should continue for 3-6 months, unless a thrombophilia has been diagnosed. After anticoagulation, most MVTs partially or completely recanalize, with one study showing recanalization in 80% of patients who received anticoagulation.[7] However, the recurrence rate has been reported at 15%.\",\n \"Acute MVT carries a better prognosis than acute mesenteric ischemia. In one systematic review of nearly 3700 cases of acute mesenteric ischemia from 1966 to 2002, the mortality rate of those patients with MVT was 44%, compared with as much as 89% for those patients with advancement to mesenteric ischemia.[8] However, with increasing physician awareness, the use of contrast-enhanced CT to investigate abdominal pain in combination with anticoagulation has improved outcomes in these patients. In more modern studies, the mortality rate of acute MVT is down to 20%, with the most common cause of death being sepsis and multiorgan failure.[8]\",\n \"In conclusion, acute superior MVT is a rare but important cause of mesenteric intestinal ischemia. It requires a high index of clinical suspicion. Rapid recognition and aggressive therapy are of extreme importance in order to prevent ischemic and infarcted bowel, sepsis, multiorgan failure, and eventual death. The 49-year-old man in this case had nonnecrotizing, alcohol-induced acute pancreatitis, complicated by acute superior MVT.\",\n \"The patient in this case was eventually transitioned to rivaroxaban and discharged on day 4. Since his discharge, he has entered into alcohol rehabilitation and remains compliant with his anticoagulation.\"\n ],\n \"date\": \"October 02, 2020\",\n \"figures\": [],\n \"markdown\": \"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\\n\\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \\n **Date:** October 02, 2020\\n\\n ## Content\\n\\n Treatment for MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal exams. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence. If evidence of clinical deterioration and bowel infarction is present, surgical intervention is necessary. Broad-spectrum antibiotics are generally reserved for the setting of pylephlebitis, septic thrombophlebitis, and sepsis secondary to bacterial translocation from an infarcted bowel.[2]\\nInitiation of anticoagulation remains the cornerstone of treatment and should not be delayed.[6]Research has shown that once a patient is transitioned to oral anticoagulation, treatment should continue for 3-6 months, unless a thrombophilia has been diagnosed. After anticoagulation, most MVTs partially or completely recanalize, with one study showing recanalization in 80% of patients who received anticoagulation.[7] However, the recurrence rate has been reported at 15%.\\nAcute MVT carries a better prognosis than acute mesenteric ischemia. In one systematic review of nearly 3700 cases of acute mesenteric ischemia from 1966 to 2002, the mortality rate of those patients with MVT was 44%, compared with as much as 89% for those patients with advancement to mesenteric ischemia.[8] However, with increasing physician awareness, the use of contrast-enhanced CT to investigate abdominal pain in combination with anticoagulation has improved outcomes in these patients. In more modern studies, the mortality rate of acute MVT is down to 20%, with the most common cause of death being sepsis and multiorgan failure.[8]\\nIn conclusion, acute superior MVT is a rare but important cause of mesenteric intestinal ischemia. It requires a high index of clinical suspicion. Rapid recognition and aggressive therapy are of extreme importance in order to prevent ischemic and infarcted bowel, sepsis, multiorgan failure, and eventual death. The 49-year-old man in this case had nonnecrotizing, alcohol-induced acute pancreatitis, complicated by acute superior MVT.\\nThe patient in this case was eventually transitioned to rivaroxaban and discharged on day 4. Since his discharge, he has entered into alcohol rehabilitation and remains compliant with his anticoagulation.\\n\\n ## Figures\\n\\n \\n*Page 5 of 6*\",\n \"pagination\": {\n \"current_page\": 5,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1281948,\n \"choiceText\": \"Pancreatic and inflammatory bowel disease\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281950,\n \"choiceText\": \"Portal hypertension\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281952,\n \"choiceText\": \"Factor V Leiden mutation\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281954,\n \"choiceText\": \"Splenectomy\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281956,\n \"choiceText\": \"Gastric sleeve\",\n \"correct\": false,\n \"displayOrder\": 5,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281958,\n \"choiceText\": \"All of the above\\r\\n\",\n \"correct\": true,\n \"displayOrder\": 6,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"MVT has many associated risk factors, including direct injury, venous congestive/stasis, and hypercoagulable conditions. The patient in this case had an extensive history of alcohol abuse and pancreatitis. In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 408511,\n \"questionText\": \"Which of the following is considered a risk factor for the development of MVT?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1281960,\n \"choiceText\": \"Broad-spectrum antibiotic use is contraindicated at this point\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281962,\n \"choiceText\": \"Surgical consultation is unnecessary at this point\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281964,\n \"choiceText\": \"Anticoagulation should be delayed until further investigation is done\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281966,\n \"choiceText\": \"Bowel rest and fluid resuscitation should be promptly initiated\",\n \"correct\": true,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Treatment of MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal examinations. In this particular case, the patient is septic and has evidence of an intra-abdominal source in the setting of SMV thrombosis. If evidence suggests clinical deterioration and bowel infarction, surgical intervention is necessary.
\\r\\n\\r\\nIn this case, the patient has voluntary guarding and an elevated lactic acid level, making an emergent surgical consult necessary. Broad-spectrum antibiotics are generally reserved for patients with pylephlebitis, those with septic thrombophlebitis, and those with sepsis secondary to bacterial translocation from an infarcted bowel.\\r\\n
\\r\\nInitiation of anticoagulation remains the cornerstone of treatment and should not be delayed. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence.\\r\\n\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 408513,\n \"questionText\": \"A 53-year-old man with a significant medical history of pancreatitis presents to the ED with nausea, vomiting, and abdominal pain. His vital signs are notable for a heart rate of 113 beats/min, respiratory rate of 24 breaths/min, and a blood pressure of 96/50 mm Hg, with a temperature of 101.3°F (38.5°C). Abdominal examination reveals diffuse tenderness to palpation with voluntary guarding. Laboratory values are notable for a lactic acid level of 4.6 mmol/L, neutrophil-predominant leukocytosis of 19 × 109 cells/L, and a lipase level of 459 U/L. CT of the abdomen/pelvis reveals superior MVT. \\r\\n
\\r\\nWhich of the following is accurate regarding his treatment?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\"\n },\n {\n \"authors\": \"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO\",\n \"content\": [],\n \"date\": \"October 02, 2020\",\n \"figures\": [],\n \"markdown\": \"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\\n\\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \\n **Date:** October 02, 2020\\n\\n ## Content\\n\\n \\n\\n ## Figures\\n\\n \\n*Page 6 of 6*\",\n \"pagination\": {\n \"current_page\": 6,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1281948,\n \"choiceText\": \"Pancreatic and inflammatory bowel disease\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281950,\n \"choiceText\": \"Portal hypertension\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281952,\n \"choiceText\": \"Factor V Leiden mutation\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281954,\n \"choiceText\": \"Splenectomy\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281956,\n \"choiceText\": \"Gastric sleeve\",\n \"correct\": false,\n \"displayOrder\": 5,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281958,\n \"choiceText\": \"All of the above\\r\\n\",\n \"correct\": true,\n \"displayOrder\": 6,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"MVT has many associated risk factors, including direct injury, venous congestive/stasis, and hypercoagulable conditions. The patient in this case had an extensive history of alcohol abuse and pancreatitis. In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 408511,\n \"questionText\": \"Which of the following is considered a risk factor for the development of MVT?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1281960,\n \"choiceText\": \"Broad-spectrum antibiotic use is contraindicated at this point\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281962,\n \"choiceText\": \"Surgical consultation is unnecessary at this point\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281964,\n \"choiceText\": \"Anticoagulation should be delayed until further investigation is done\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281966,\n \"choiceText\": \"Bowel rest and fluid resuscitation should be promptly initiated\",\n \"correct\": true,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Treatment of MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal examinations. In this particular case, the patient is septic and has evidence of an intra-abdominal source in the setting of SMV thrombosis. If evidence suggests clinical deterioration and bowel infarction, surgical intervention is necessary.
\\r\\n\\r\\nIn this case, the patient has voluntary guarding and an elevated lactic acid level, making an emergent surgical consult necessary. Broad-spectrum antibiotics are generally reserved for patients with pylephlebitis, those with septic thrombophlebitis, and those with sepsis secondary to bacterial translocation from an infarcted bowel.\\r\\n
\\r\\nInitiation of anticoagulation remains the cornerstone of treatment and should not be delayed. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence.\\r\\n\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 408513,\n \"questionText\": \"A 53-year-old man with a significant medical history of pancreatitis presents to the ED with nausea, vomiting, and abdominal pain. His vital signs are notable for a heart rate of 113 beats/min, respiratory rate of 24 breaths/min, and a blood pressure of 96/50 mm Hg, with a temperature of 101.3°F (38.5°C). Abdominal examination reveals diffuse tenderness to palpation with voluntary guarding. Laboratory values are notable for a lactic acid level of 4.6 mmol/L, neutrophil-predominant leukocytosis of 19 × 109 cells/L, and a lipase level of 459 U/L. CT of the abdomen/pelvis reveals superior MVT. \\r\\n
\\r\\nWhich of the following is accurate regarding his treatment?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\"\n }\n]"},"questions":{"kind":"list like","value":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1281940,"choiceText":"Splenic vein thrombosis","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281942,"choiceText":"Superior mesenteric vein thrombosis","correct":true,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281944,"choiceText":"Mesenteric arterial thrombosis","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281946,"choiceText":"Septic pylephlebitis\r\n","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"","displayOrder":1,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":408509,"questionText":"Based only on these findings, which of the following is the most likely diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1281948,"choiceText":"Pancreatic and inflammatory bowel disease","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281950,"choiceText":"Portal hypertension","correct":false,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281952,"choiceText":"Factor V Leiden mutation","correct":false,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281954,"choiceText":"Splenectomy","correct":false,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281956,"choiceText":"Gastric sleeve","correct":false,"displayOrder":5,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281958,"choiceText":"All of the above\r\n","correct":true,"displayOrder":6,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"MVT has many associated risk factors, including direct injury, venous congestive/stasis, and hypercoagulable conditions. The patient in this case had an extensive history of alcohol abuse and pancreatitis. In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.","displayOrder":2,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":408511,"questionText":"Which of the following is considered a risk factor for the development of MVT?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1281960,"choiceText":"Broad-spectrum antibiotic use is contraindicated at this point","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281962,"choiceText":"Surgical consultation is unnecessary at this point","correct":false,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281964,"choiceText":"Anticoagulation should be delayed until further investigation is done","correct":false,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281966,"choiceText":"Bowel rest and fluid resuscitation should be promptly initiated","correct":true,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Treatment of MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal examinations. In this particular case, the patient is septic and has evidence of an intra-abdominal source in the setting of SMV thrombosis. If evidence suggests clinical deterioration and bowel infarction, surgical intervention is necessary.
\r\n\r\nIn this case, the patient has voluntary guarding and an elevated lactic acid level, making an emergent surgical consult necessary. Broad-spectrum antibiotics are generally reserved for patients with pylephlebitis, those with septic thrombophlebitis, and those with sepsis secondary to bacterial translocation from an infarcted bowel.\r\n
\r\nInitiation of anticoagulation remains the cornerstone of treatment and should not be delayed. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence.\r\n","displayOrder":3,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":408513,"questionText":"A 53-year-old man with a significant medical history of pancreatitis presents to the ED with nausea, vomiting, and abdominal pain. His vital signs are notable for a heart rate of 113 beats/min, respiratory rate of 24 breaths/min, and a blood pressure of 96/50 mm Hg, with a temperature of 101.3°F (38.5°C). Abdominal examination reveals diffuse tenderness to palpation with voluntary guarding. Laboratory values are notable for a lactic acid level of 4.6 mmol/L, neutrophil-predominant leukocytosis of 19 × 109 cells/L, and a lipase level of 459 U/L. CT of the abdomen/pelvis reveals superior MVT. \r\n
\r\nWhich of the following is accurate regarding his treatment?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"string":"[\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1281940,\n \"choiceText\": \"Splenic vein thrombosis\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281942,\n \"choiceText\": \"Superior mesenteric vein thrombosis\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281944,\n \"choiceText\": \"Mesenteric arterial thrombosis\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281946,\n \"choiceText\": \"Septic pylephlebitis\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\",\n \"displayOrder\": 1,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 408509,\n \"questionText\": \"Based only on these findings, which of the following is the most likely diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1281948,\n \"choiceText\": \"Pancreatic and inflammatory bowel disease\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281950,\n \"choiceText\": \"Portal hypertension\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281952,\n \"choiceText\": \"Factor V Leiden mutation\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281954,\n \"choiceText\": \"Splenectomy\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281956,\n \"choiceText\": \"Gastric sleeve\",\n \"correct\": false,\n \"displayOrder\": 5,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281958,\n \"choiceText\": \"All of the above\\r\\n\",\n \"correct\": true,\n \"displayOrder\": 6,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"MVT has many associated risk factors, including direct injury, venous congestive/stasis, and hypercoagulable conditions. The patient in this case had an extensive history of alcohol abuse and pancreatitis. In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 408511,\n \"questionText\": \"Which of the following is considered a risk factor for the development of MVT?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1281960,\n \"choiceText\": \"Broad-spectrum antibiotic use is contraindicated at this point\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281962,\n \"choiceText\": \"Surgical consultation is unnecessary at this point\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281964,\n \"choiceText\": \"Anticoagulation should be delayed until further investigation is done\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281966,\n \"choiceText\": \"Bowel rest and fluid resuscitation should be promptly initiated\",\n \"correct\": true,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Treatment of MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal examinations. In this particular case, the patient is septic and has evidence of an intra-abdominal source in the setting of SMV thrombosis. If evidence suggests clinical deterioration and bowel infarction, surgical intervention is necessary.
\\r\\n\\r\\nIn this case, the patient has voluntary guarding and an elevated lactic acid level, making an emergent surgical consult necessary. Broad-spectrum antibiotics are generally reserved for patients with pylephlebitis, those with septic thrombophlebitis, and those with sepsis secondary to bacterial translocation from an infarcted bowel.\\r\\n
\\r\\nInitiation of anticoagulation remains the cornerstone of treatment and should not be delayed. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence.\\r\\n\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 408513,\n \"questionText\": \"A 53-year-old man with a significant medical history of pancreatitis presents to the ED with nausea, vomiting, and abdominal pain. His vital signs are notable for a heart rate of 113 beats/min, respiratory rate of 24 breaths/min, and a blood pressure of 96/50 mm Hg, with a temperature of 101.3°F (38.5°C). Abdominal examination reveals diffuse tenderness to palpation with voluntary guarding. Laboratory values are notable for a lactic acid level of 4.6 mmol/L, neutrophil-predominant leukocytosis of 19 × 109 cells/L, and a lipase level of 459 U/L. CT of the abdomen/pelvis reveals superior MVT. \\r\\n
\\r\\nWhich of the following is accurate regarding his treatment?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n]"}}}],"truncated":false,"partial":false},"paginationData":{"pageIndex":2,"numItemsPerPage":100,"numTotalItems":508,"offset":200,"length":100}},"jwt":"eyJhbGciOiJFZERTQSJ9.eyJyZWFkIjp0cnVlLCJwZXJtaXNzaW9ucyI6eyJyZXBvLmNvbnRlbnQucmVhZCI6dHJ1ZX0sImlhdCI6MTc0NjQyMzU3OSwic3ViIjoiL2RhdGFzZXRzL2hsbGovbWVkc2NhcGUiLCJleHAiOjE3NDY0MjcxNzksImlzcyI6Imh0dHBzOi8vaHVnZ2luZ2ZhY2UuY28ifQ.sinwUiCqQrlj8AQMez_vGuBfK6e-N0uXfATqAeB2npmIes5b-ZDMbCSY11kWjYUhJ2YG13BYU-Vl85sUvFmMCQ","displayUrls":true},"discussionsStats":{"closed":0,"open":1,"total":1},"fullWidth":true,"hasGatedAccess":true,"hasFullAccess":true,"isEmbedded":false,"savedQueries":{"community":[],"user":[]}}">
\\r\\n\\r\\nMany known allergens, such as those commonly found in cosmetic products, are not included in patch testing kits. Thus, referral to a specialist for customized patch testing would be useful to confirm the diagnosis in this patient.
\\r\\n\\r\\nAn open application test, also known as a "repeat open application test," is performed after a mildly positive patch test to determine whether the reaction is clinically significant.[13] The allergen in question is openly and repeatedly applied to a small area of the skin, which is observed for a reaction at regular intervals within the first hour of testing and after 3-4 days.[14] This test is most appropriate for "leave-on" consumer products suspected to contain low-level contact allergens.
\\r\\n\\r\\nA skin biopsy can exclude other conditions, such as psoriasis. The histologic finding of spongiotic dermatitis is an important clue to the diagnosis of allergic contact dermatitis.[15] Because the offending agent had been identified in this patient, a skin biopsy was not necessary.\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 492331,\n \"questionText\": \"Of the following tests, which would best help to confirm this patient's diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"A 38-Year-Old Radiology Technician With a Blistering, Itchy Rash\"\n },\n {\n \"authors\": \"Melba Estrella, MD; Alan Snyder; John Plante; Dirk M. Elston, MD\",\n \"content\": [],\n \"date\": \"November 15, 2024\",\n \"figures\": [],\n \"markdown\": \"# A 38-Year-Old Radiology Technician With a Blistering, Itchy Rash\\n\\n **Authors:** Melba Estrella, MD; Alan Snyder; John Plante; Dirk M. Elston, MD \\n **Date:** November 15, 2024\\n\\n ## Content\\n\\n \\n\\n ## Figures\\n\\n \\n*Page 6 of 6*\",\n \"pagination\": {\n \"current_page\": 6,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1535601,\n \"choiceText\": \"Natural latex proteins\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535602,\n \"choiceText\": \"Synthetic latex polymers\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535603,\n \"choiceText\": \"Rubber manufacturing accelerators\",\n \"correct\": true,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535604,\n \"choiceText\": \"Bleached rubber compounds\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Patients can become sensitized to components found in natural rubber (latex) or synthetic rubber; however, they are more likely to become sensitized to the chemicals used in the process of rubber manufacturing, particularly accelerator agents.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 492330,\n \"questionText\": \"Which of the following is most likely to cause allergic contact dermatitis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1535605,\n \"choiceText\": \"Repeat patch testing using a rubber series kit\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535606,\n \"choiceText\": \"Perform patch testing using samples of the patient's underwear\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535607,\n \"choiceText\": \"Perform a repeat open application test\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535608,\n \"choiceText\": \"Perform a punch biopsy\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\\r\\nIf allergy remains strongly suspected despite a negative baseline series patch test, a rubber series kit is warranted to avoid false-negative results.[11] In this patient, the negative results of the rubber series kit obviated the need to repeat the test.
\\r\\n\\r\\nMany known allergens, such as those commonly found in cosmetic products, are not included in patch testing kits. Thus, referral to a specialist for customized patch testing would be useful to confirm the diagnosis in this patient.
\\r\\n\\r\\nAn open application test, also known as a "repeat open application test," is performed after a mildly positive patch test to determine whether the reaction is clinically significant.[13] The allergen in question is openly and repeatedly applied to a small area of the skin, which is observed for a reaction at regular intervals within the first hour of testing and after 3-4 days.[14] This test is most appropriate for "leave-on" consumer products suspected to contain low-level contact allergens.
\\r\\n\\r\\nA skin biopsy can exclude other conditions, such as psoriasis. The histologic finding of spongiotic dermatitis is an important clue to the diagnosis of allergic contact dermatitis.[15] Because the offending agent had been identified in this patient, a skin biopsy was not necessary.\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 492331,\n \"questionText\": \"Of the following tests, which would best help to confirm this patient's diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"A 38-Year-Old Radiology Technician With a Blistering, Itchy Rash\"\n }\n]"},"questions":{"kind":"list like","value":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1535597,"choiceText":"Herpes simplex virus infection","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1535598,"choiceText":"Atopic dermatitis","correct":false,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1535599,"choiceText":"Plaque psoriasis","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1535600,"choiceText":"Contact dermatitis","correct":true,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"","displayOrder":1,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":492329,"questionText":"On the basis of these findings only, which of the following is the most likely diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1535601,"choiceText":"Natural latex proteins","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1535602,"choiceText":"Synthetic latex polymers","correct":false,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1535603,"choiceText":"Rubber manufacturing accelerators","correct":true,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1535604,"choiceText":"Bleached rubber compounds","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Patients can become sensitized to components found in natural rubber (latex) or synthetic rubber; however, they are more likely to become sensitized to the chemicals used in the process of rubber manufacturing, particularly accelerator agents.","displayOrder":2,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":492330,"questionText":"Which of the following is most likely to cause allergic contact dermatitis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1535605,"choiceText":"Repeat patch testing using a rubber series kit","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1535606,"choiceText":"Perform patch testing using samples of the patient's underwear","correct":true,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1535607,"choiceText":"Perform a repeat open application test","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1535608,"choiceText":"Perform a punch biopsy","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"\r\nIf allergy remains strongly suspected despite a negative baseline series patch test, a rubber series kit is warranted to avoid false-negative results.[11] In this patient, the negative results of the rubber series kit obviated the need to repeat the test.
\r\n\r\nMany known allergens, such as those commonly found in cosmetic products, are not included in patch testing kits. Thus, referral to a specialist for customized patch testing would be useful to confirm the diagnosis in this patient.
\r\n\r\nAn open application test, also known as a "repeat open application test," is performed after a mildly positive patch test to determine whether the reaction is clinically significant.[13] The allergen in question is openly and repeatedly applied to a small area of the skin, which is observed for a reaction at regular intervals within the first hour of testing and after 3-4 days.[14] This test is most appropriate for "leave-on" consumer products suspected to contain low-level contact allergens.
\r\n\r\nA skin biopsy can exclude other conditions, such as psoriasis. The histologic finding of spongiotic dermatitis is an important clue to the diagnosis of allergic contact dermatitis.[15] Because the offending agent had been identified in this patient, a skin biopsy was not necessary.","displayOrder":3,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":492331,"questionText":"Of the following tests, which would best help to confirm this patient's diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"string":"[\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1535597,\n \"choiceText\": \"Herpes simplex virus infection\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535598,\n \"choiceText\": \"Atopic dermatitis\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535599,\n \"choiceText\": \"Plaque psoriasis\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535600,\n \"choiceText\": \"Contact dermatitis\",\n \"correct\": true,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\",\n \"displayOrder\": 1,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 492329,\n \"questionText\": \"On the basis of these findings only, which of the following is the most likely diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1535601,\n \"choiceText\": \"Natural latex proteins\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535602,\n \"choiceText\": \"Synthetic latex polymers\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535603,\n \"choiceText\": \"Rubber manufacturing accelerators\",\n \"correct\": true,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535604,\n \"choiceText\": \"Bleached rubber compounds\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Patients can become sensitized to components found in natural rubber (latex) or synthetic rubber; however, they are more likely to become sensitized to the chemicals used in the process of rubber manufacturing, particularly accelerator agents.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 492330,\n \"questionText\": \"Which of the following is most likely to cause allergic contact dermatitis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1535605,\n \"choiceText\": \"Repeat patch testing using a rubber series kit\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535606,\n \"choiceText\": \"Perform patch testing using samples of the patient's underwear\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535607,\n \"choiceText\": \"Perform a repeat open application test\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1535608,\n \"choiceText\": \"Perform a punch biopsy\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\\r\\nIf allergy remains strongly suspected despite a negative baseline series patch test, a rubber series kit is warranted to avoid false-negative results.[11] In this patient, the negative results of the rubber series kit obviated the need to repeat the test.
\\r\\n\\r\\nMany known allergens, such as those commonly found in cosmetic products, are not included in patch testing kits. Thus, referral to a specialist for customized patch testing would be useful to confirm the diagnosis in this patient.
\\r\\n\\r\\nAn open application test, also known as a "repeat open application test," is performed after a mildly positive patch test to determine whether the reaction is clinically significant.[13] The allergen in question is openly and repeatedly applied to a small area of the skin, which is observed for a reaction at regular intervals within the first hour of testing and after 3-4 days.[14] This test is most appropriate for "leave-on" consumer products suspected to contain low-level contact allergens.
\\r\\n\\r\\nA skin biopsy can exclude other conditions, such as psoriasis. The histologic finding of spongiotic dermatitis is an important clue to the diagnosis of allergic contact dermatitis.[15] Because the offending agent had been identified in this patient, a skin biopsy was not necessary.\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 492331,\n \"questionText\": \"Of the following tests, which would best help to confirm this patient's diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n]"}}},{"rowIdx":297,"cells":{"article_id":{"kind":"string","value":"842258"},"url":{"kind":"string","value":"/viewarticle/842258"},"article_data":{"kind":"list like","value":[{"authors":"Winston W. Tan, MD; Matthew Tan","content":["Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.","A 63-year-old woman presents with a chronic cough. She was in her usual state of health until 3 months ago, when she developed a dry cough with fever. She was initially treated with antibiotics for 2 weeks. The cough improved, and the fever resolved. However, the dry cough returned.","The patient reports recent several instances of hemoptysis, as well as a 5-lb weight loss that she attributes to her recent diet change and exercise. She also describes chest pain, shortness of breath, dyspnea, and significant lower back pain.","Her medical history is significant for hypertension and diabetes. Her family history includes a father who had congestive heart failure at age 73 years. The patient gets her eyes checked regularly. She has never seen a pulmonary specialist. She reports aches and pains that vary, depending on how much physical activity she gets. She has had a hysterectomy. She is married and denies smoking, although she reports a history of continued secondhand smoke exposure."],"date":"October 16, 2020","figures":[],"markdown":"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\n\n **Authors:** Winston W. Tan, MD; Matthew Tan \n **Date:** October 16, 2020\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 63-year-old woman presents with a chronic cough. She was in her usual state of health until 3 months ago, when she developed a dry cough with fever. She was initially treated with antibiotics for 2 weeks. The cough improved, and the fever resolved. However, the dry cough returned.\nThe patient reports recent several instances of hemoptysis, as well as a 5-lb weight loss that she attributes to her recent diet change and exercise. She also describes chest pain, shortness of breath, dyspnea, and significant lower back pain.\nHer medical history is significant for hypertension and diabetes. Her family history includes a father who had congestive heart failure at age 73 years. The patient gets her eyes checked regularly. She has never seen a pulmonary specialist. She reports aches and pains that vary, depending on how much physical activity she gets. She has had a hysterectomy. She is married and denies smoking, although she reports a history of continued secondhand smoke exposure.\n\n ## Figures\n\n \n*Page 1 of 6*","pagination":{"current_page":1,"total_pages":6},"questionnaire":[],"title":"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old"},{"authors":"Winston W. Tan, MD; Matthew Tan","content":["Physical examination reveals the following:","Blood pressure: 124/58 mm Hg","Temperature: 98.3°F (36.8°C)","Heart rate: 85 beats/min","Examination of her neck reveals enlarged supraclavicular lymph nodes. Examination of her breasts reveals no distinct nodules, lumps, discharge, skin retraction, or axillary adenopathy. Her abdomen is soft, benign, and nontender. Neurologically, cranial nerves II through XII are grossly intact.","Upon evaluation of the lungs, wheezing and atelectasis are observed. Increased work of breathing is also noted. A chest radiograph is subsequently ordered."],"date":"October 16, 2020","figures":[],"markdown":"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\n\n **Authors:** Winston W. Tan, MD; Matthew Tan \n **Date:** October 16, 2020\n\n ## Content\n\n Physical examination reveals the following:\nBlood pressure: 124/58 mm Hg\nTemperature: 98.3°F (36.8°C)\nHeart rate: 85 beats/min\nExamination of her neck reveals enlarged supraclavicular lymph nodes. Examination of her breasts reveals no distinct nodules, lumps, discharge, skin retraction, or axillary adenopathy. Her abdomen is soft, benign, and nontender. Neurologically, cranial nerves II through XII are grossly intact.\nUpon evaluation of the lungs, wheezing and atelectasis are observed. Increased work of breathing is also noted. A chest radiograph is subsequently ordered.\n\n ## Figures\n\n \n*Page 2 of 6*","pagination":{"current_page":2,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":831357,"choiceText":"Sarcoidosis","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831359,"choiceText":"Lung cancer","correct":true,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831361,"choiceText":"Tuberculosis","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831363,"choiceText":"Pneumonia \r\n","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"","displayOrder":1,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":261411,"questionText":"Based only on these findings, which of the following is the most likely diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old"},{"authors":"Winston W. Tan, MD; Matthew Tan","content":["Lung cancer is often insidious, failing to produce clear symptoms until advanced disease. A high index of suspicion is required to properly identify this disease in most patients. In this case, weight loss, hemoptysis, and a history of secondhand smoke exposure, along with a low-grade fever and irregularities upon lung evaluation, warranted an investigation for lung cancer. Subsequently, CT revealed a 1.3-cm left upper lobe complex nodule (Figure 1).","Figure 1.","The patient underwent a left upper lobectomy with mediastinal lymph node dissection for a 1.5-cm poorly differentiated squamous cancer of lung, with 1 (station 5) of 18 lymph nodes positive with a microscopic focus of cancer. She was subsequently treated with adjuvant chemoradiation therapy, consisting of cisplatin and docetaxel concurrent with radiation. However, chemotherapy was stopped after a few doses owing to complications.","The patient later developed a seizure and was hospitalized; MRI of the brain was negative for metastatic disease but suggested possible temporal lobe inflammation. Her cerebrospinal fluid was positive for herpes. She was started on phenytoin and valacyclovir.","She completed radiation therapy to 6120 cGy. Additional planned chemotherapy was delayed owing to the patient's debility. She also experienced an outbreak of shingles. Serial follow-up every 4 months showed that disease was in complete remission, with a stable postradiation residual scar in the left lung.","Figure 2.","Figure 3.","Six years later, CT revealed a new enhancing mass in the medial right upper lobe (adjacent to the mediastinum) that was suspicious for metastatic or new primary lung cancer (Figure 2). A brain scan was negative for metastases. PET revealed uptake in the expected area and indeterminate uptake in a right hilar node (Figure 3), but was otherwise negative. Pulmonary function tests revealed showed an FEV1 of 1.45 L, or 65% of predicted. The diffusing capacity of the lung for carbon monoxide (DLCO) was 42%. Saturation was normal at rest but decreased to 92% with exercise.","Endobronchial ultrasonography did not reveal any specific abnormality. The mucosa was friable. A right hilar lymph node was sampled, but no lymphoid elements were obtained. Nothing specific for the tumor area was seen.","Figure 4.","A CT-guided biopsy was nondiagnostic. Surgical exploration yielded a small cell carcinoma that was unresectable owing to mediastinal invasion and bleeding (Figure 4). The patient started palliative chemotherapy with carboplatin/etoposide, with etoposide given orally on days 2 and 3. She completed four cycles of this chemotherapy and tolerated chemotherapy well overall.","Follow-up CT showed minimal residual density in the area of the prior lesion. As a result of excellent response, she was referred for proton therapy, because standard radiation was not feasible owing to prior dosing.","Induction chemotherapy was followed by consolidation radiation. The patient subsequently underwent proton radiation to the residual chest mass. She experienced a seizure; she was dehydrated, and was started on anticonvulsant and became stable. MRI of the brain revealed an area of right anterior temporal encephalomalacia. She is doing well currently and is under active surveillance for her cancer."],"date":"October 16, 2020","figures":[{"caption":"Figure 1.","image_url":"https://img.medscapestatic.com/article/842/258/842258-Thumb1a.png"},{"caption":"Figure 2.","image_url":"https://img.medscapestatic.com/article/842/258/842258-Thumb2a.png"},{"caption":"Figure 3.","image_url":"https://img.medscapestatic.com/article/842/258/842258-Thumb3a.png"},{"caption":"Figure 4.","image_url":"https://img.medscapestatic.com/article/842/258/842258-Thumb4a.png"}],"markdown":"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\n\n **Authors:** Winston W. Tan, MD; Matthew Tan \n **Date:** October 16, 2020\n\n ## Content\n\n Lung cancer is often insidious, failing to produce clear symptoms until advanced disease. A high index of suspicion is required to properly identify this disease in most patients. In this case, weight loss, hemoptysis, and a history of secondhand smoke exposure, along with a low-grade fever and irregularities upon lung evaluation, warranted an investigation for lung cancer. Subsequently, CT revealed a 1.3-cm left upper lobe complex nodule (Figure 1).\nFigure 1.\nThe patient underwent a left upper lobectomy with mediastinal lymph node dissection for a 1.5-cm poorly differentiated squamous cancer of lung, with 1 (station 5) of 18 lymph nodes positive with a microscopic focus of cancer. She was subsequently treated with adjuvant chemoradiation therapy, consisting of cisplatin and docetaxel concurrent with radiation. However, chemotherapy was stopped after a few doses owing to complications.\nThe patient later developed a seizure and was hospitalized; MRI of the brain was negative for metastatic disease but suggested possible temporal lobe inflammation. Her cerebrospinal fluid was positive for herpes. She was started on phenytoin and valacyclovir.\nShe completed radiation therapy to 6120 cGy. Additional planned chemotherapy was delayed owing to the patient's debility. She also experienced an outbreak of shingles. Serial follow-up every 4 months showed that disease was in complete remission, with a stable postradiation residual scar in the left lung.\nFigure 2.\nFigure 3.\nSix years later, CT revealed a new enhancing mass in the medial right upper lobe (adjacent to the mediastinum) that was suspicious for metastatic or new primary lung cancer (Figure 2). A brain scan was negative for metastases. PET revealed uptake in the expected area and indeterminate uptake in a right hilar node (Figure 3), but was otherwise negative. Pulmonary function tests revealed showed an FEV1 of 1.45 L, or 65% of predicted. The diffusing capacity of the lung for carbon monoxide (DLCO) was 42%. Saturation was normal at rest but decreased to 92% with exercise.\nEndobronchial ultrasonography did not reveal any specific abnormality. The mucosa was friable. A right hilar lymph node was sampled, but no lymphoid elements were obtained. Nothing specific for the tumor area was seen.\nFigure 4.\nA CT-guided biopsy was nondiagnostic. Surgical exploration yielded a small cell carcinoma that was unresectable owing to mediastinal invasion and bleeding (Figure 4). The patient started palliative chemotherapy with carboplatin/etoposide, with etoposide given orally on days 2 and 3. She completed four cycles of this chemotherapy and tolerated chemotherapy well overall.\nFollow-up CT showed minimal residual density in the area of the prior lesion. As a result of excellent response, she was referred for proton therapy, because standard radiation was not feasible owing to prior dosing.\nInduction chemotherapy was followed by consolidation radiation. The patient subsequently underwent proton radiation to the residual chest mass. She experienced a seizure; she was dehydrated, and was started on anticonvulsant and became stable. MRI of the brain revealed an area of right anterior temporal encephalomalacia. She is doing well currently and is under active surveillance for her cancer.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4.** \n \n\n\n*Page 3 of 6*","pagination":{"current_page":3,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":831357,"choiceText":"Sarcoidosis","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831359,"choiceText":"Lung cancer","correct":true,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831361,"choiceText":"Tuberculosis","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831363,"choiceText":"Pneumonia \r\n","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"","displayOrder":1,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":261411,"questionText":"Based only on these findings, which of the following is the most likely diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old"},{"authors":"Winston W. Tan, MD; Matthew Tan","content":["Non-small cell lung cancer accounts for approximately 85% of all lung cancers. Histologically, it is divided into adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Patients with non-small cell lung cancer require a complete staging work-up to evaluate the extent of disease because stage plays a major role in determining the choice of treatment.[1]","The patient in this case has the typical presentation of chronic cough. Typically, a cough that is initially thought to be an infection is noted. A chronic cough without improvement of symptoms despite treatment for infection should prompt further evaluation for potential lung mass. CT of the chest is often used as a diagnostic tool to clarify the suspicion of a lung mass.[2]","Because of the importance of stage in the therapeutic decision-making process, all patients must undergo proper staging of disease. A complete staging work-up should be performed to evaluate the extent of disease. In the United States, the standard staging work-up includes the following:","CT of the chest and upper abdomen","Complete blood count with differential","Serum chemistry studies, including creatinine, electrolytes, and calcium","Alkaline phosphate","Aspartate aminotransferase","Pulmonary function testing","Mediastinoscopy (if surgical resection is considered)","The information obtained from these tests guides additional testing (eg, imaging studies). Invasive staging procedures (eg, mediastinoscopy, mediastinotomy) may be required to assess mediastinal lymph nodes in patients who may undergo surgical resection. PET may be useful in detecting affected nodes, which may influence decisions about operability.","Paraneoplastic syndromes are more likely to occur in small cell lung cancer than in non-small cell lung cancer. Patients are at risk for the following:","Cushing syndrome","Lambert-Eaton myasthenic syndrome (Onset of proximal lower-extremity weakness is gradual; proximal upper-extremity weakness is usually less noticeable; the syndrome may be worse in the morning and improve during the day; although extraocular muscle involvement is uncommon, ptosis is often found)","Hypercalcemia (usually occurs with squamous cell carcinoma)","Syndrome of inappropriate antidiuretic hormone secretion","Enlargement of the extremities and painful, swollen joints (hypertrophic osteoarthropathy)"],"date":"October 16, 2020","figures":[],"markdown":"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\n\n **Authors:** Winston W. Tan, MD; Matthew Tan \n **Date:** October 16, 2020\n\n ## Content\n\n Non-small cell lung cancer accounts for approximately 85% of all lung cancers. Histologically, it is divided into adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Patients with non-small cell lung cancer require a complete staging work-up to evaluate the extent of disease because stage plays a major role in determining the choice of treatment.[1]\nThe patient in this case has the typical presentation of chronic cough. Typically, a cough that is initially thought to be an infection is noted. A chronic cough without improvement of symptoms despite treatment for infection should prompt further evaluation for potential lung mass. CT of the chest is often used as a diagnostic tool to clarify the suspicion of a lung mass.[2]\nBecause of the importance of stage in the therapeutic decision-making process, all patients must undergo proper staging of disease. A complete staging work-up should be performed to evaluate the extent of disease. In the United States, the standard staging work-up includes the following:\nCT of the chest and upper abdomen\nComplete blood count with differential\nSerum chemistry studies, including creatinine, electrolytes, and calcium\nAlkaline phosphate\nAspartate aminotransferase\nPulmonary function testing\nMediastinoscopy (if surgical resection is considered)\nThe information obtained from these tests guides additional testing (eg, imaging studies). Invasive staging procedures (eg, mediastinoscopy, mediastinotomy) may be required to assess mediastinal lymph nodes in patients who may undergo surgical resection. PET may be useful in detecting affected nodes, which may influence decisions about operability.\nParaneoplastic syndromes are more likely to occur in small cell lung cancer than in non-small cell lung cancer. Patients are at risk for the following:\nCushing syndrome\nLambert-Eaton myasthenic syndrome (Onset of proximal lower-extremity weakness is gradual; proximal upper-extremity weakness is usually less noticeable; the syndrome may be worse in the morning and improve during the day; although extraocular muscle involvement is uncommon, ptosis is often found)\nHypercalcemia (usually occurs with squamous cell carcinoma)\nSyndrome of inappropriate antidiuretic hormone secretion\nEnlargement of the extremities and painful, swollen joints (hypertrophic osteoarthropathy)\n\n ## Figures\n\n \n*Page 4 of 6*","pagination":{"current_page":4,"total_pages":6},"questionnaire":[],"title":"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old"},{"authors":"Winston W. Tan, MD; Matthew Tan","content":["The standard treatment for stage I and II disease is surgical resection. In stage IIIA, chemotherapy is indicated, as is surgical resection in selected patients. Standard treatment of stage IIIb is chemoradiation. Stage IV requires cisplatin-based chemotherapy or surgical resection if a solitary metastatic lesion with resectable primary tumor is present.[3,4,5]","This patient underwent resection of the cancer. Owing to her residual disease and because her lymph nodes were positive, she was treated with chemoradiation. Surgical resection is the primary modality of treatment for early stage non-small cell lung cancer.[6]","Close surveillance of patients with cancer should be the standard after completion of therapy. This patient had a contralateral hilar recurrence 6 years later. When a patient has a recurrence, it must be determined whether it is the same cancer or another primary cancer. This patient had another primary cancer, specifically small cell cancer of the lung. Biopsy must be done of a new recurrence, because it could be an entirely different cancer.","Approximately 60%-70% of patients with small cell lung cancer have clinically disseminated or extensive disease at presentation. Extensive-stage small cell lung cancer is incurable. When given combination chemotherapy, patients with extensive-stage disease have a complete response rate of more than 20% and a median survival longer than 7 months; however, only 2% are alive at 5 years.","For individuals with limited-stage disease that is treated with combination chemotherapy plus chest radiation, a complete response rate of 80% and survival of 17 months have been reported; 12%-15% of patients are alive at 5 years.[1]","Recommendations from the National Comprehensive Cancer Network (NCCN) regarding cancer surveillance in survivors of non-small cell lung cancer include the following:","History and physical examination, and chest CT with or without contrast, every 6-12 months for 2 years, then history and physical examination and noncontrast chest CT annually","Assessment of smoking status at each visit, with counseling and referral for smoking cessation as needed","Other NCCN recommendations for long-term follow-up care include the following:","Immunization: Annual influenza vaccination, pneumococcal vaccination with revaccination as appropriate, herpes zoster vaccination","Counseling regarding health promotion and wellness (eg, regular physical activity, healthy diet)","Routine health monitoring","Several important points should be remembered:","Persistent cough despite treatment should prompt further diagnostic testing for lung mass.","Nonsmokers can develop lung cancer.","Neurologic symptoms in patients with lung cancer do not always mean brain metastasis. Although brain metastasis should be ruled out, other causes could be found, such as encephalomalacia.","Biopsy of recurrent cancer should be redone, especially if the time to recurrence is more than a few years. A separate cancer can be found in a patient previously cured of their cancer.","Several factors may increase the likelihood of a primary cancer resulting in a secondary cancer. A \"field effect\" is noted in certain types of cancers, particularly in the areas of respiratory tract. In smokers, this is especially true in such areas as the head and neck, throat, laryngeal, esophageal area, and tongue. Because the body's immune system is vulnerable to the development of the first cancer, it may be more susceptible to the development of a second cancer."],"date":"October 16, 2020","figures":[],"markdown":"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\n\n **Authors:** Winston W. Tan, MD; Matthew Tan \n **Date:** October 16, 2020\n\n ## Content\n\n The standard treatment for stage I and II disease is surgical resection. In stage IIIA, chemotherapy is indicated, as is surgical resection in selected patients. Standard treatment of stage IIIb is chemoradiation. Stage IV requires cisplatin-based chemotherapy or surgical resection if a solitary metastatic lesion with resectable primary tumor is present.[3,4,5]\nThis patient underwent resection of the cancer. Owing to her residual disease and because her lymph nodes were positive, she was treated with chemoradiation. Surgical resection is the primary modality of treatment for early stage non-small cell lung cancer.[6]\nClose surveillance of patients with cancer should be the standard after completion of therapy. This patient had a contralateral hilar recurrence 6 years later. When a patient has a recurrence, it must be determined whether it is the same cancer or another primary cancer. This patient had another primary cancer, specifically small cell cancer of the lung. Biopsy must be done of a new recurrence, because it could be an entirely different cancer.\nApproximately 60%-70% of patients with small cell lung cancer have clinically disseminated or extensive disease at presentation. Extensive-stage small cell lung cancer is incurable. When given combination chemotherapy, patients with extensive-stage disease have a complete response rate of more than 20% and a median survival longer than 7 months; however, only 2% are alive at 5 years.\nFor individuals with limited-stage disease that is treated with combination chemotherapy plus chest radiation, a complete response rate of 80% and survival of 17 months have been reported; 12%-15% of patients are alive at 5 years.[1]\nRecommendations from the National Comprehensive Cancer Network (NCCN) regarding cancer surveillance in survivors of non-small cell lung cancer include the following:\nHistory and physical examination, and chest CT with or without contrast, every 6-12 months for 2 years, then history and physical examination and noncontrast chest CT annually\nAssessment of smoking status at each visit, with counseling and referral for smoking cessation as needed\nOther NCCN recommendations for long-term follow-up care include the following:\nImmunization: Annual influenza vaccination, pneumococcal vaccination with revaccination as appropriate, herpes zoster vaccination\nCounseling regarding health promotion and wellness (eg, regular physical activity, healthy diet)\nRoutine health monitoring\nSeveral important points should be remembered:\nPersistent cough despite treatment should prompt further diagnostic testing for lung mass.\nNonsmokers can develop lung cancer.\nNeurologic symptoms in patients with lung cancer do not always mean brain metastasis. Although brain metastasis should be ruled out, other causes could be found, such as encephalomalacia.\nBiopsy of recurrent cancer should be redone, especially if the time to recurrence is more than a few years. A separate cancer can be found in a patient previously cured of their cancer.\nSeveral factors may increase the likelihood of a primary cancer resulting in a secondary cancer. A \"field effect\" is noted in certain types of cancers, particularly in the areas of respiratory tract. In smokers, this is especially true in such areas as the head and neck, throat, laryngeal, esophageal area, and tongue. Because the body's immune system is vulnerable to the development of the first cancer, it may be more susceptible to the development of a second cancer.\n\n ## Figures\n\n \n*Page 5 of 6*","pagination":{"current_page":5,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":831365,"choiceText":"Adenocarcinoma","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831367,"choiceText":"Squamous cell carcinoma","correct":true,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831369,"choiceText":"Large-cell carcinoma","correct":false,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831371,"choiceText":"None of the above\r\n","correct":false,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"The most common metabolic abnormality associated with non-small cell lung cancer is hypercalcemia, which usually occurs with squamous cell carcinoma and results from secretion of parathyroid hormone-related peptide by the tumor. This can be distinguished from hyperparathyroidism by confirmation of normal serum parathyroid hormone levels.","displayOrder":2,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":261413,"questionText":"Which of the following is most commonly associated with hypercalcemia in patients with non-small cell lung cancer?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":831373,"choiceText":"Smoke exposure","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831375,"choiceText":"Family history","correct":false,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831377,"choiceText":"Poor diet","correct":true,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831379,"choiceText":"Chemical exposure","correct":false,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Smoking is the most well-recognized risk factor for lung cancer. Even secondhand exposure carries a significant risk. In addition, exposure to certain gases (eg, radon), asbestos, and other chemicals may increase the risk for lung cancer. Likewise, a family history of lung cancer increases risk for the disease.","displayOrder":3,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":261415,"questionText":"Which of the following is not considered a primary risk factor for lung cancer?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old"},{"authors":"Winston W. Tan, MD; Matthew Tan","content":[],"date":"October 16, 2020","figures":[],"markdown":"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\n\n **Authors:** Winston W. Tan, MD; Matthew Tan \n **Date:** October 16, 2020\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*","pagination":{"current_page":6,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":831365,"choiceText":"Adenocarcinoma","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831367,"choiceText":"Squamous cell carcinoma","correct":true,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831369,"choiceText":"Large-cell carcinoma","correct":false,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831371,"choiceText":"None of the above\r\n","correct":false,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"The most common metabolic abnormality associated with non-small cell lung cancer is hypercalcemia, which usually occurs with squamous cell carcinoma and results from secretion of parathyroid hormone-related peptide by the tumor. This can be distinguished from hyperparathyroidism by confirmation of normal serum parathyroid hormone levels.","displayOrder":2,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":261413,"questionText":"Which of the following is most commonly associated with hypercalcemia in patients with non-small cell lung cancer?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":831373,"choiceText":"Smoke exposure","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831375,"choiceText":"Family history","correct":false,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831377,"choiceText":"Poor diet","correct":true,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831379,"choiceText":"Chemical exposure","correct":false,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Smoking is the most well-recognized risk factor for lung cancer. Even secondhand exposure carries a significant risk. In addition, exposure to certain gases (eg, radon), asbestos, and other chemicals may increase the risk for lung cancer. Likewise, a family history of lung cancer increases risk for the disease.","displayOrder":3,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":261415,"questionText":"Which of the following is not considered a primary risk factor for lung cancer?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old"}],"string":"[\n {\n \"authors\": \"Winston W. Tan, MD; Matthew Tan\",\n \"content\": [\n \"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\",\n \"A 63-year-old woman presents with a chronic cough. She was in her usual state of health until 3 months ago, when she developed a dry cough with fever. She was initially treated with antibiotics for 2 weeks. The cough improved, and the fever resolved. However, the dry cough returned.\",\n \"The patient reports recent several instances of hemoptysis, as well as a 5-lb weight loss that she attributes to her recent diet change and exercise. She also describes chest pain, shortness of breath, dyspnea, and significant lower back pain.\",\n \"Her medical history is significant for hypertension and diabetes. Her family history includes a father who had congestive heart failure at age 73 years. The patient gets her eyes checked regularly. She has never seen a pulmonary specialist. She reports aches and pains that vary, depending on how much physical activity she gets. She has had a hysterectomy. She is married and denies smoking, although she reports a history of continued secondhand smoke exposure.\"\n ],\n \"date\": \"October 16, 2020\",\n \"figures\": [],\n \"markdown\": \"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\\n\\n **Authors:** Winston W. Tan, MD; Matthew Tan \\n **Date:** October 16, 2020\\n\\n ## Content\\n\\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\\nA 63-year-old woman presents with a chronic cough. She was in her usual state of health until 3 months ago, when she developed a dry cough with fever. She was initially treated with antibiotics for 2 weeks. The cough improved, and the fever resolved. However, the dry cough returned.\\nThe patient reports recent several instances of hemoptysis, as well as a 5-lb weight loss that she attributes to her recent diet change and exercise. She also describes chest pain, shortness of breath, dyspnea, and significant lower back pain.\\nHer medical history is significant for hypertension and diabetes. Her family history includes a father who had congestive heart failure at age 73 years. The patient gets her eyes checked regularly. She has never seen a pulmonary specialist. She reports aches and pains that vary, depending on how much physical activity she gets. She has had a hysterectomy. She is married and denies smoking, although she reports a history of continued secondhand smoke exposure.\\n\\n ## Figures\\n\\n \\n*Page 1 of 6*\",\n \"pagination\": {\n \"current_page\": 1,\n \"total_pages\": 6\n },\n \"questionnaire\": [],\n \"title\": \"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\"\n },\n {\n \"authors\": \"Winston W. Tan, MD; Matthew Tan\",\n \"content\": [\n \"Physical examination reveals the following:\",\n \"Blood pressure: 124/58 mm Hg\",\n \"Temperature: 98.3°F (36.8°C)\",\n \"Heart rate: 85 beats/min\",\n \"Examination of her neck reveals enlarged supraclavicular lymph nodes. Examination of her breasts reveals no distinct nodules, lumps, discharge, skin retraction, or axillary adenopathy. Her abdomen is soft, benign, and nontender. Neurologically, cranial nerves II through XII are grossly intact.\",\n \"Upon evaluation of the lungs, wheezing and atelectasis are observed. Increased work of breathing is also noted. A chest radiograph is subsequently ordered.\"\n ],\n \"date\": \"October 16, 2020\",\n \"figures\": [],\n \"markdown\": \"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\\n\\n **Authors:** Winston W. Tan, MD; Matthew Tan \\n **Date:** October 16, 2020\\n\\n ## Content\\n\\n Physical examination reveals the following:\\nBlood pressure: 124/58 mm Hg\\nTemperature: 98.3°F (36.8°C)\\nHeart rate: 85 beats/min\\nExamination of her neck reveals enlarged supraclavicular lymph nodes. Examination of her breasts reveals no distinct nodules, lumps, discharge, skin retraction, or axillary adenopathy. Her abdomen is soft, benign, and nontender. Neurologically, cranial nerves II through XII are grossly intact.\\nUpon evaluation of the lungs, wheezing and atelectasis are observed. Increased work of breathing is also noted. A chest radiograph is subsequently ordered.\\n\\n ## Figures\\n\\n \\n*Page 2 of 6*\",\n \"pagination\": {\n \"current_page\": 2,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 831357,\n \"choiceText\": \"Sarcoidosis\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831359,\n \"choiceText\": \"Lung cancer\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831361,\n \"choiceText\": \"Tuberculosis\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831363,\n \"choiceText\": \"Pneumonia \\r\\n\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\",\n \"displayOrder\": 1,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 261411,\n \"questionText\": \"Based only on these findings, which of the following is the most likely diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\"\n },\n {\n \"authors\": \"Winston W. Tan, MD; Matthew Tan\",\n \"content\": [\n \"Lung cancer is often insidious, failing to produce clear symptoms until advanced disease. A high index of suspicion is required to properly identify this disease in most patients. In this case, weight loss, hemoptysis, and a history of secondhand smoke exposure, along with a low-grade fever and irregularities upon lung evaluation, warranted an investigation for lung cancer. Subsequently, CT revealed a 1.3-cm left upper lobe complex nodule (Figure 1).\",\n \"Figure 1.\",\n \"The patient underwent a left upper lobectomy with mediastinal lymph node dissection for a 1.5-cm poorly differentiated squamous cancer of lung, with 1 (station 5) of 18 lymph nodes positive with a microscopic focus of cancer. She was subsequently treated with adjuvant chemoradiation therapy, consisting of cisplatin and docetaxel concurrent with radiation. However, chemotherapy was stopped after a few doses owing to complications.\",\n \"The patient later developed a seizure and was hospitalized; MRI of the brain was negative for metastatic disease but suggested possible temporal lobe inflammation. Her cerebrospinal fluid was positive for herpes. She was started on phenytoin and valacyclovir.\",\n \"She completed radiation therapy to 6120 cGy. Additional planned chemotherapy was delayed owing to the patient's debility. She also experienced an outbreak of shingles. Serial follow-up every 4 months showed that disease was in complete remission, with a stable postradiation residual scar in the left lung.\",\n \"Figure 2.\",\n \"Figure 3.\",\n \"Six years later, CT revealed a new enhancing mass in the medial right upper lobe (adjacent to the mediastinum) that was suspicious for metastatic or new primary lung cancer (Figure 2). A brain scan was negative for metastases. PET revealed uptake in the expected area and indeterminate uptake in a right hilar node (Figure 3), but was otherwise negative. Pulmonary function tests revealed showed an FEV1 of 1.45 L, or 65% of predicted. The diffusing capacity of the lung for carbon monoxide (DLCO) was 42%. Saturation was normal at rest but decreased to 92% with exercise.\",\n \"Endobronchial ultrasonography did not reveal any specific abnormality. The mucosa was friable. A right hilar lymph node was sampled, but no lymphoid elements were obtained. Nothing specific for the tumor area was seen.\",\n \"Figure 4.\",\n \"A CT-guided biopsy was nondiagnostic. Surgical exploration yielded a small cell carcinoma that was unresectable owing to mediastinal invasion and bleeding (Figure 4). The patient started palliative chemotherapy with carboplatin/etoposide, with etoposide given orally on days 2 and 3. She completed four cycles of this chemotherapy and tolerated chemotherapy well overall.\",\n \"Follow-up CT showed minimal residual density in the area of the prior lesion. As a result of excellent response, she was referred for proton therapy, because standard radiation was not feasible owing to prior dosing.\",\n \"Induction chemotherapy was followed by consolidation radiation. The patient subsequently underwent proton radiation to the residual chest mass. She experienced a seizure; she was dehydrated, and was started on anticonvulsant and became stable. MRI of the brain revealed an area of right anterior temporal encephalomalacia. She is doing well currently and is under active surveillance for her cancer.\"\n ],\n \"date\": \"October 16, 2020\",\n \"figures\": [\n {\n \"caption\": \"Figure 1.\",\n \"image_url\": \"https://img.medscapestatic.com/article/842/258/842258-Thumb1a.png\"\n },\n {\n \"caption\": \"Figure 2.\",\n \"image_url\": \"https://img.medscapestatic.com/article/842/258/842258-Thumb2a.png\"\n },\n {\n \"caption\": \"Figure 3.\",\n \"image_url\": \"https://img.medscapestatic.com/article/842/258/842258-Thumb3a.png\"\n },\n {\n \"caption\": \"Figure 4.\",\n \"image_url\": \"https://img.medscapestatic.com/article/842/258/842258-Thumb4a.png\"\n }\n ],\n \"markdown\": \"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\\n\\n **Authors:** Winston W. Tan, MD; Matthew Tan \\n **Date:** October 16, 2020\\n\\n ## Content\\n\\n Lung cancer is often insidious, failing to produce clear symptoms until advanced disease. A high index of suspicion is required to properly identify this disease in most patients. In this case, weight loss, hemoptysis, and a history of secondhand smoke exposure, along with a low-grade fever and irregularities upon lung evaluation, warranted an investigation for lung cancer. Subsequently, CT revealed a 1.3-cm left upper lobe complex nodule (Figure 1).\\nFigure 1.\\nThe patient underwent a left upper lobectomy with mediastinal lymph node dissection for a 1.5-cm poorly differentiated squamous cancer of lung, with 1 (station 5) of 18 lymph nodes positive with a microscopic focus of cancer. She was subsequently treated with adjuvant chemoradiation therapy, consisting of cisplatin and docetaxel concurrent with radiation. However, chemotherapy was stopped after a few doses owing to complications.\\nThe patient later developed a seizure and was hospitalized; MRI of the brain was negative for metastatic disease but suggested possible temporal lobe inflammation. Her cerebrospinal fluid was positive for herpes. She was started on phenytoin and valacyclovir.\\nShe completed radiation therapy to 6120 cGy. Additional planned chemotherapy was delayed owing to the patient's debility. She also experienced an outbreak of shingles. Serial follow-up every 4 months showed that disease was in complete remission, with a stable postradiation residual scar in the left lung.\\nFigure 2.\\nFigure 3.\\nSix years later, CT revealed a new enhancing mass in the medial right upper lobe (adjacent to the mediastinum) that was suspicious for metastatic or new primary lung cancer (Figure 2). A brain scan was negative for metastases. PET revealed uptake in the expected area and indeterminate uptake in a right hilar node (Figure 3), but was otherwise negative. Pulmonary function tests revealed showed an FEV1 of 1.45 L, or 65% of predicted. The diffusing capacity of the lung for carbon monoxide (DLCO) was 42%. Saturation was normal at rest but decreased to 92% with exercise.\\nEndobronchial ultrasonography did not reveal any specific abnormality. The mucosa was friable. A right hilar lymph node was sampled, but no lymphoid elements were obtained. Nothing specific for the tumor area was seen.\\nFigure 4.\\nA CT-guided biopsy was nondiagnostic. Surgical exploration yielded a small cell carcinoma that was unresectable owing to mediastinal invasion and bleeding (Figure 4). The patient started palliative chemotherapy with carboplatin/etoposide, with etoposide given orally on days 2 and 3. She completed four cycles of this chemotherapy and tolerated chemotherapy well overall.\\nFollow-up CT showed minimal residual density in the area of the prior lesion. As a result of excellent response, she was referred for proton therapy, because standard radiation was not feasible owing to prior dosing.\\nInduction chemotherapy was followed by consolidation radiation. The patient subsequently underwent proton radiation to the residual chest mass. She experienced a seizure; she was dehydrated, and was started on anticonvulsant and became stable. MRI of the brain revealed an area of right anterior temporal encephalomalacia. She is doing well currently and is under active surveillance for her cancer.\\n\\n ## Figures\\n\\n **Figure 1.** \\n \\n\\n**Figure 2.** \\n \\n\\n**Figure 3.** \\n \\n\\n**Figure 4.** \\n \\n\\n\\n*Page 3 of 6*\",\n \"pagination\": {\n \"current_page\": 3,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 831357,\n \"choiceText\": \"Sarcoidosis\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831359,\n \"choiceText\": \"Lung cancer\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831361,\n \"choiceText\": \"Tuberculosis\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831363,\n \"choiceText\": \"Pneumonia \\r\\n\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\",\n \"displayOrder\": 1,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 261411,\n \"questionText\": \"Based only on these findings, which of the following is the most likely diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\"\n },\n {\n \"authors\": \"Winston W. Tan, MD; Matthew Tan\",\n \"content\": [\n \"Non-small cell lung cancer accounts for approximately 85% of all lung cancers. Histologically, it is divided into adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Patients with non-small cell lung cancer require a complete staging work-up to evaluate the extent of disease because stage plays a major role in determining the choice of treatment.[1]\",\n \"The patient in this case has the typical presentation of chronic cough. Typically, a cough that is initially thought to be an infection is noted. A chronic cough without improvement of symptoms despite treatment for infection should prompt further evaluation for potential lung mass. CT of the chest is often used as a diagnostic tool to clarify the suspicion of a lung mass.[2]\",\n \"Because of the importance of stage in the therapeutic decision-making process, all patients must undergo proper staging of disease. A complete staging work-up should be performed to evaluate the extent of disease. In the United States, the standard staging work-up includes the following:\",\n \"CT of the chest and upper abdomen\",\n \"Complete blood count with differential\",\n \"Serum chemistry studies, including creatinine, electrolytes, and calcium\",\n \"Alkaline phosphate\",\n \"Aspartate aminotransferase\",\n \"Pulmonary function testing\",\n \"Mediastinoscopy (if surgical resection is considered)\",\n \"The information obtained from these tests guides additional testing (eg, imaging studies). Invasive staging procedures (eg, mediastinoscopy, mediastinotomy) may be required to assess mediastinal lymph nodes in patients who may undergo surgical resection. PET may be useful in detecting affected nodes, which may influence decisions about operability.\",\n \"Paraneoplastic syndromes are more likely to occur in small cell lung cancer than in non-small cell lung cancer. Patients are at risk for the following:\",\n \"Cushing syndrome\",\n \"Lambert-Eaton myasthenic syndrome (Onset of proximal lower-extremity weakness is gradual; proximal upper-extremity weakness is usually less noticeable; the syndrome may be worse in the morning and improve during the day; although extraocular muscle involvement is uncommon, ptosis is often found)\",\n \"Hypercalcemia (usually occurs with squamous cell carcinoma)\",\n \"Syndrome of inappropriate antidiuretic hormone secretion\",\n \"Enlargement of the extremities and painful, swollen joints (hypertrophic osteoarthropathy)\"\n ],\n \"date\": \"October 16, 2020\",\n \"figures\": [],\n \"markdown\": \"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\\n\\n **Authors:** Winston W. Tan, MD; Matthew Tan \\n **Date:** October 16, 2020\\n\\n ## Content\\n\\n Non-small cell lung cancer accounts for approximately 85% of all lung cancers. Histologically, it is divided into adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Patients with non-small cell lung cancer require a complete staging work-up to evaluate the extent of disease because stage plays a major role in determining the choice of treatment.[1]\\nThe patient in this case has the typical presentation of chronic cough. Typically, a cough that is initially thought to be an infection is noted. A chronic cough without improvement of symptoms despite treatment for infection should prompt further evaluation for potential lung mass. CT of the chest is often used as a diagnostic tool to clarify the suspicion of a lung mass.[2]\\nBecause of the importance of stage in the therapeutic decision-making process, all patients must undergo proper staging of disease. A complete staging work-up should be performed to evaluate the extent of disease. In the United States, the standard staging work-up includes the following:\\nCT of the chest and upper abdomen\\nComplete blood count with differential\\nSerum chemistry studies, including creatinine, electrolytes, and calcium\\nAlkaline phosphate\\nAspartate aminotransferase\\nPulmonary function testing\\nMediastinoscopy (if surgical resection is considered)\\nThe information obtained from these tests guides additional testing (eg, imaging studies). Invasive staging procedures (eg, mediastinoscopy, mediastinotomy) may be required to assess mediastinal lymph nodes in patients who may undergo surgical resection. PET may be useful in detecting affected nodes, which may influence decisions about operability.\\nParaneoplastic syndromes are more likely to occur in small cell lung cancer than in non-small cell lung cancer. Patients are at risk for the following:\\nCushing syndrome\\nLambert-Eaton myasthenic syndrome (Onset of proximal lower-extremity weakness is gradual; proximal upper-extremity weakness is usually less noticeable; the syndrome may be worse in the morning and improve during the day; although extraocular muscle involvement is uncommon, ptosis is often found)\\nHypercalcemia (usually occurs with squamous cell carcinoma)\\nSyndrome of inappropriate antidiuretic hormone secretion\\nEnlargement of the extremities and painful, swollen joints (hypertrophic osteoarthropathy)\\n\\n ## Figures\\n\\n \\n*Page 4 of 6*\",\n \"pagination\": {\n \"current_page\": 4,\n \"total_pages\": 6\n },\n \"questionnaire\": [],\n \"title\": \"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\"\n },\n {\n \"authors\": \"Winston W. Tan, MD; Matthew Tan\",\n \"content\": [\n \"The standard treatment for stage I and II disease is surgical resection. In stage IIIA, chemotherapy is indicated, as is surgical resection in selected patients. Standard treatment of stage IIIb is chemoradiation. Stage IV requires cisplatin-based chemotherapy or surgical resection if a solitary metastatic lesion with resectable primary tumor is present.[3,4,5]\",\n \"This patient underwent resection of the cancer. Owing to her residual disease and because her lymph nodes were positive, she was treated with chemoradiation. Surgical resection is the primary modality of treatment for early stage non-small cell lung cancer.[6]\",\n \"Close surveillance of patients with cancer should be the standard after completion of therapy. This patient had a contralateral hilar recurrence 6 years later. When a patient has a recurrence, it must be determined whether it is the same cancer or another primary cancer. This patient had another primary cancer, specifically small cell cancer of the lung. Biopsy must be done of a new recurrence, because it could be an entirely different cancer.\",\n \"Approximately 60%-70% of patients with small cell lung cancer have clinically disseminated or extensive disease at presentation. Extensive-stage small cell lung cancer is incurable. When given combination chemotherapy, patients with extensive-stage disease have a complete response rate of more than 20% and a median survival longer than 7 months; however, only 2% are alive at 5 years.\",\n \"For individuals with limited-stage disease that is treated with combination chemotherapy plus chest radiation, a complete response rate of 80% and survival of 17 months have been reported; 12%-15% of patients are alive at 5 years.[1]\",\n \"Recommendations from the National Comprehensive Cancer Network (NCCN) regarding cancer surveillance in survivors of non-small cell lung cancer include the following:\",\n \"History and physical examination, and chest CT with or without contrast, every 6-12 months for 2 years, then history and physical examination and noncontrast chest CT annually\",\n \"Assessment of smoking status at each visit, with counseling and referral for smoking cessation as needed\",\n \"Other NCCN recommendations for long-term follow-up care include the following:\",\n \"Immunization: Annual influenza vaccination, pneumococcal vaccination with revaccination as appropriate, herpes zoster vaccination\",\n \"Counseling regarding health promotion and wellness (eg, regular physical activity, healthy diet)\",\n \"Routine health monitoring\",\n \"Several important points should be remembered:\",\n \"Persistent cough despite treatment should prompt further diagnostic testing for lung mass.\",\n \"Nonsmokers can develop lung cancer.\",\n \"Neurologic symptoms in patients with lung cancer do not always mean brain metastasis. Although brain metastasis should be ruled out, other causes could be found, such as encephalomalacia.\",\n \"Biopsy of recurrent cancer should be redone, especially if the time to recurrence is more than a few years. A separate cancer can be found in a patient previously cured of their cancer.\",\n \"Several factors may increase the likelihood of a primary cancer resulting in a secondary cancer. A \\\"field effect\\\" is noted in certain types of cancers, particularly in the areas of respiratory tract. In smokers, this is especially true in such areas as the head and neck, throat, laryngeal, esophageal area, and tongue. Because the body's immune system is vulnerable to the development of the first cancer, it may be more susceptible to the development of a second cancer.\"\n ],\n \"date\": \"October 16, 2020\",\n \"figures\": [],\n \"markdown\": \"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\\n\\n **Authors:** Winston W. Tan, MD; Matthew Tan \\n **Date:** October 16, 2020\\n\\n ## Content\\n\\n The standard treatment for stage I and II disease is surgical resection. In stage IIIA, chemotherapy is indicated, as is surgical resection in selected patients. Standard treatment of stage IIIb is chemoradiation. Stage IV requires cisplatin-based chemotherapy or surgical resection if a solitary metastatic lesion with resectable primary tumor is present.[3,4,5]\\nThis patient underwent resection of the cancer. Owing to her residual disease and because her lymph nodes were positive, she was treated with chemoradiation. Surgical resection is the primary modality of treatment for early stage non-small cell lung cancer.[6]\\nClose surveillance of patients with cancer should be the standard after completion of therapy. This patient had a contralateral hilar recurrence 6 years later. When a patient has a recurrence, it must be determined whether it is the same cancer or another primary cancer. This patient had another primary cancer, specifically small cell cancer of the lung. Biopsy must be done of a new recurrence, because it could be an entirely different cancer.\\nApproximately 60%-70% of patients with small cell lung cancer have clinically disseminated or extensive disease at presentation. Extensive-stage small cell lung cancer is incurable. When given combination chemotherapy, patients with extensive-stage disease have a complete response rate of more than 20% and a median survival longer than 7 months; however, only 2% are alive at 5 years.\\nFor individuals with limited-stage disease that is treated with combination chemotherapy plus chest radiation, a complete response rate of 80% and survival of 17 months have been reported; 12%-15% of patients are alive at 5 years.[1]\\nRecommendations from the National Comprehensive Cancer Network (NCCN) regarding cancer surveillance in survivors of non-small cell lung cancer include the following:\\nHistory and physical examination, and chest CT with or without contrast, every 6-12 months for 2 years, then history and physical examination and noncontrast chest CT annually\\nAssessment of smoking status at each visit, with counseling and referral for smoking cessation as needed\\nOther NCCN recommendations for long-term follow-up care include the following:\\nImmunization: Annual influenza vaccination, pneumococcal vaccination with revaccination as appropriate, herpes zoster vaccination\\nCounseling regarding health promotion and wellness (eg, regular physical activity, healthy diet)\\nRoutine health monitoring\\nSeveral important points should be remembered:\\nPersistent cough despite treatment should prompt further diagnostic testing for lung mass.\\nNonsmokers can develop lung cancer.\\nNeurologic symptoms in patients with lung cancer do not always mean brain metastasis. Although brain metastasis should be ruled out, other causes could be found, such as encephalomalacia.\\nBiopsy of recurrent cancer should be redone, especially if the time to recurrence is more than a few years. A separate cancer can be found in a patient previously cured of their cancer.\\nSeveral factors may increase the likelihood of a primary cancer resulting in a secondary cancer. A \\\"field effect\\\" is noted in certain types of cancers, particularly in the areas of respiratory tract. In smokers, this is especially true in such areas as the head and neck, throat, laryngeal, esophageal area, and tongue. Because the body's immune system is vulnerable to the development of the first cancer, it may be more susceptible to the development of a second cancer.\\n\\n ## Figures\\n\\n \\n*Page 5 of 6*\",\n \"pagination\": {\n \"current_page\": 5,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 831365,\n \"choiceText\": \"Adenocarcinoma\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831367,\n \"choiceText\": \"Squamous cell carcinoma\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831369,\n \"choiceText\": \"Large-cell carcinoma\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831371,\n \"choiceText\": \"None of the above\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"The most common metabolic abnormality associated with non-small cell lung cancer is hypercalcemia, which usually occurs with squamous cell carcinoma and results from secretion of parathyroid hormone-related peptide by the tumor. This can be distinguished from hyperparathyroidism by confirmation of normal serum parathyroid hormone levels.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 261413,\n \"questionText\": \"Which of the following is most commonly associated with hypercalcemia in patients with non-small cell lung cancer?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 831373,\n \"choiceText\": \"Smoke exposure\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831375,\n \"choiceText\": \"Family history\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831377,\n \"choiceText\": \"Poor diet\",\n \"correct\": true,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831379,\n \"choiceText\": \"Chemical exposure\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Smoking is the most well-recognized risk factor for lung cancer. Even secondhand exposure carries a significant risk. In addition, exposure to certain gases (eg, radon), asbestos, and other chemicals may increase the risk for lung cancer. Likewise, a family history of lung cancer increases risk for the disease.\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 261415,\n \"questionText\": \"Which of the following is not considered a primary risk factor for lung cancer?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\"\n },\n {\n \"authors\": \"Winston W. Tan, MD; Matthew Tan\",\n \"content\": [],\n \"date\": \"October 16, 2020\",\n \"figures\": [],\n \"markdown\": \"# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\\n\\n **Authors:** Winston W. Tan, MD; Matthew Tan \\n **Date:** October 16, 2020\\n\\n ## Content\\n\\n \\n\\n ## Figures\\n\\n \\n*Page 6 of 6*\",\n \"pagination\": {\n \"current_page\": 6,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 831365,\n \"choiceText\": \"Adenocarcinoma\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831367,\n \"choiceText\": \"Squamous cell carcinoma\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831369,\n \"choiceText\": \"Large-cell carcinoma\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831371,\n \"choiceText\": \"None of the above\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"The most common metabolic abnormality associated with non-small cell lung cancer is hypercalcemia, which usually occurs with squamous cell carcinoma and results from secretion of parathyroid hormone-related peptide by the tumor. This can be distinguished from hyperparathyroidism by confirmation of normal serum parathyroid hormone levels.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 261413,\n \"questionText\": \"Which of the following is most commonly associated with hypercalcemia in patients with non-small cell lung cancer?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 831373,\n \"choiceText\": \"Smoke exposure\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831375,\n \"choiceText\": \"Family history\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831377,\n \"choiceText\": \"Poor diet\",\n \"correct\": true,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831379,\n \"choiceText\": \"Chemical exposure\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Smoking is the most well-recognized risk factor for lung cancer. Even secondhand exposure carries a significant risk. In addition, exposure to certain gases (eg, radon), asbestos, and other chemicals may increase the risk for lung cancer. Likewise, a family history of lung cancer increases risk for the disease.\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 261415,\n \"questionText\": \"Which of the following is not considered a primary risk factor for lung cancer?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\"\n }\n]"},"questions":{"kind":"list like","value":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":831357,"choiceText":"Sarcoidosis","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831359,"choiceText":"Lung cancer","correct":true,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831361,"choiceText":"Tuberculosis","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831363,"choiceText":"Pneumonia \r\n","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"","displayOrder":1,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":261411,"questionText":"Based only on these findings, which of the following is the most likely diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":831365,"choiceText":"Adenocarcinoma","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831367,"choiceText":"Squamous cell carcinoma","correct":true,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831369,"choiceText":"Large-cell carcinoma","correct":false,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831371,"choiceText":"None of the above\r\n","correct":false,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"The most common metabolic abnormality associated with non-small cell lung cancer is hypercalcemia, which usually occurs with squamous cell carcinoma and results from secretion of parathyroid hormone-related peptide by the tumor. This can be distinguished from hyperparathyroidism by confirmation of normal serum parathyroid hormone levels.","displayOrder":2,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":261413,"questionText":"Which of the following is most commonly associated with hypercalcemia in patients with non-small cell lung cancer?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":831373,"choiceText":"Smoke exposure","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831375,"choiceText":"Family history","correct":false,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831377,"choiceText":"Poor diet","correct":true,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":831379,"choiceText":"Chemical exposure","correct":false,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Smoking is the most well-recognized risk factor for lung cancer. Even secondhand exposure carries a significant risk. In addition, exposure to certain gases (eg, radon), asbestos, and other chemicals may increase the risk for lung cancer. Likewise, a family history of lung cancer increases risk for the disease.","displayOrder":3,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":261415,"questionText":"Which of the following is not considered a primary risk factor for lung cancer?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"string":"[\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 831357,\n \"choiceText\": \"Sarcoidosis\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831359,\n \"choiceText\": \"Lung cancer\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831361,\n \"choiceText\": \"Tuberculosis\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831363,\n \"choiceText\": \"Pneumonia \\r\\n\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\",\n \"displayOrder\": 1,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 261411,\n \"questionText\": \"Based only on these findings, which of the following is the most likely diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 831365,\n \"choiceText\": \"Adenocarcinoma\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831367,\n \"choiceText\": \"Squamous cell carcinoma\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831369,\n \"choiceText\": \"Large-cell carcinoma\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831371,\n \"choiceText\": \"None of the above\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"The most common metabolic abnormality associated with non-small cell lung cancer is hypercalcemia, which usually occurs with squamous cell carcinoma and results from secretion of parathyroid hormone-related peptide by the tumor. This can be distinguished from hyperparathyroidism by confirmation of normal serum parathyroid hormone levels.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 261413,\n \"questionText\": \"Which of the following is most commonly associated with hypercalcemia in patients with non-small cell lung cancer?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 831373,\n \"choiceText\": \"Smoke exposure\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831375,\n \"choiceText\": \"Family history\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831377,\n \"choiceText\": \"Poor diet\",\n \"correct\": true,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 831379,\n \"choiceText\": \"Chemical exposure\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Smoking is the most well-recognized risk factor for lung cancer. Even secondhand exposure carries a significant risk. In addition, exposure to certain gases (eg, radon), asbestos, and other chemicals may increase the risk for lung cancer. Likewise, a family history of lung cancer increases risk for the disease.\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 261415,\n \"questionText\": \"Which of the following is not considered a primary risk factor for lung cancer?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n]"}}},{"rowIdx":298,"cells":{"article_id":{"kind":"string","value":"938423"},"url":{"kind":"string","value":"/viewarticle/938423"},"article_data":{"kind":"list like","value":[{"authors":"Timothy D. Murphy, MD","content":["Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us .","A 5-year-old girl with a long-standing history of severe asthma and eczema presented to a pediatric pulmonary and sleep medicine clinic. Her asthma was stabilized with an inhaled corticosteroid (fluticasone, 88 µg, inhaled twice daily), albuterol sulfate (180 µg, inhaled as needed), and ipratropium bromide (34 µg, inhaled as needed). Her skin condition improved with a moderately aggressive regimen of hydrating bleach baths, moisturizing lotions, nonsedating antihistamines, and as-needed use of topical hydrocortisone or triamcinolone, pimecrolimus, and mupirocin.","Her asthma remained stable for a year but then progressed to the extent that the dosage of inhaled fluticasone was increased to 220 µg twice daily. Bronchoscopy revealed only mild bronchomalacia of the left mainstem bronchus (Figure 1), diffuse mild inflammation, and increased secretions.","Figure 1.","Montelukast (5 mg daily) and nasal fluticasone (50 µg) were added to her regimen. In addition, diphenhydramine (25 mg) was prescribed to be used as needed for excessive itchiness, eczema flares, and allergic asthma flares.","The patient remained well and was followed up in the clinic approximately every 3 months, owing to the complexity of her condition. After 6 months, significant weight gain and an increasing body mass index (BMI) were noted. She met with a dietitian, who recommended weight loss strategies. From the age of 7-8 years, the patient demonstrated a modest weight loss from the changes in her diet. However, symptoms of fatigue, excessive daytime sleepiness (EDS), and inattention in school developed over a 1- to 2-month period, and her weight started to increase rapidly despite the dietary intervention.","Her daytime sleepiness seemed to be progressive, and she would fall asleep suddenly even when she wanted to be awake. Concerned about the emerging symptoms of inattention, autistic features, fatigue, and sleepiness, the girl's parents are seeking further medical advice."],"date":"October 09, 2020","figures":[{"caption":"Figure 1.","image_url":"https://img.medscapestatic.com/article/938/423/938423-Thumb1.jpg"}],"markdown":"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\n\n **Authors:** Timothy D. Murphy, MD \n **Date:** October 09, 2020\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us .\nA 5-year-old girl with a long-standing history of severe asthma and eczema presented to a pediatric pulmonary and sleep medicine clinic. Her asthma was stabilized with an inhaled corticosteroid (fluticasone, 88 µg, inhaled twice daily), albuterol sulfate (180 µg, inhaled as needed), and ipratropium bromide (34 µg, inhaled as needed). Her skin condition improved with a moderately aggressive regimen of hydrating bleach baths, moisturizing lotions, nonsedating antihistamines, and as-needed use of topical hydrocortisone or triamcinolone, pimecrolimus, and mupirocin.\nHer asthma remained stable for a year but then progressed to the extent that the dosage of inhaled fluticasone was increased to 220 µg twice daily. Bronchoscopy revealed only mild bronchomalacia of the left mainstem bronchus (Figure 1), diffuse mild inflammation, and increased secretions.\nFigure 1.\nMontelukast (5 mg daily) and nasal fluticasone (50 µg) were added to her regimen. In addition, diphenhydramine (25 mg) was prescribed to be used as needed for excessive itchiness, eczema flares, and allergic asthma flares.\nThe patient remained well and was followed up in the clinic approximately every 3 months, owing to the complexity of her condition. After 6 months, significant weight gain and an increasing body mass index (BMI) were noted. She met with a dietitian, who recommended weight loss strategies. From the age of 7-8 years, the patient demonstrated a modest weight loss from the changes in her diet. However, symptoms of fatigue, excessive daytime sleepiness (EDS), and inattention in school developed over a 1- to 2-month period, and her weight started to increase rapidly despite the dietary intervention.\nHer daytime sleepiness seemed to be progressive, and she would fall asleep suddenly even when she wanted to be awake. Concerned about the emerging symptoms of inattention, autistic features, fatigue, and sleepiness, the girl's parents are seeking further medical advice.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 1 of 6*","pagination":{"current_page":1,"total_pages":6},"questionnaire":[],"title":"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma"},{"authors":"Timothy D. Murphy, MD","content":["The patient has fallen asleep at school nearly every day for the past 1-2 months and falls into a deep sleep unless she is kept active. At home, she is taking more naps during the day, falling asleep in the car, and struggling with schoolwork. Her grades have dropped significantly over the past few months. Her parents report that she does not awaken during the night. No snoring, choking, snorting, gasping, or apnea is noted. She sleeps an average of 9-10 hours per night but is restless and tosses and turns frequently in her sleep.","Her family history is notable for obesity, obstructive sleep apnea (OSA) that requires continuous positive airway pressure (CPAP) in her father, and narcolepsy in an uncle and a grandfather.","On physical examination, she has mild to moderate obesity (BMI of 23.89 kg/m2 [the 98th percentile for age]) and enlarged tonsils (2-3+). She has difficulty with focusing and staying awake in the clinic.","She is referred to a pediatric otolaryngologist for consideration of nocturnal polysomnography (NPSG) or an adenotonsillectomy. The otolaryngologist notes that she has not tolerated nasal fluticasone well, that she is a chronic mouth breather, and that her tonsils are enlarged (3+). An NPSG is ordered to help clarify matters.","The NPSG demonstrates the following:","A respiratory disturbance index and an apnea-hypopnea index (AHI) of 6.2 per hour","Sleep latency of 0.5 minutes and rapid eye movement (REM) latency of 0.5 minutes","A sleep efficiency of 87.5%","18.2% of total sleep time in stage N1, 36.4% in N2, 29.9% in N3, and 15.5% in REM sleep","An arousal index of 18.6","A periodic leg movement index of 6.3","Multiple periods of wakefulness scattered throughout the night and six REM periods"],"date":"October 09, 2020","figures":[],"markdown":"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\n\n **Authors:** Timothy D. Murphy, MD \n **Date:** October 09, 2020\n\n ## Content\n\n The patient has fallen asleep at school nearly every day for the past 1-2 months and falls into a deep sleep unless she is kept active. At home, she is taking more naps during the day, falling asleep in the car, and struggling with schoolwork. Her grades have dropped significantly over the past few months. Her parents report that she does not awaken during the night. No snoring, choking, snorting, gasping, or apnea is noted. She sleeps an average of 9-10 hours per night but is restless and tosses and turns frequently in her sleep.\nHer family history is notable for obesity, obstructive sleep apnea (OSA) that requires continuous positive airway pressure (CPAP) in her father, and narcolepsy in an uncle and a grandfather.\nOn physical examination, she has mild to moderate obesity (BMI of 23.89 kg/m2 [the 98th percentile for age]) and enlarged tonsils (2-3+). She has difficulty with focusing and staying awake in the clinic.\nShe is referred to a pediatric otolaryngologist for consideration of nocturnal polysomnography (NPSG) or an adenotonsillectomy. The otolaryngologist notes that she has not tolerated nasal fluticasone well, that she is a chronic mouth breather, and that her tonsils are enlarged (3+). An NPSG is ordered to help clarify matters.\nThe NPSG demonstrates the following:\nA respiratory disturbance index and an apnea-hypopnea index (AHI) of 6.2 per hour\nSleep latency of 0.5 minutes and rapid eye movement (REM) latency of 0.5 minutes\nA sleep efficiency of 87.5%\n18.2% of total sleep time in stage N1, 36.4% in N2, 29.9% in N3, and 15.5% in REM sleep\nAn arousal index of 18.6\nA periodic leg movement index of 6.3\nMultiple periods of wakefulness scattered throughout the night and six REM periods\n\n ## Figures\n\n \n*Page 2 of 6*","pagination":{"current_page":2,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1529064,"choiceText":"Behavioral insomnia of childhood\r\n","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529065,"choiceText":"Pediatric chronic obstructive pulmonary disease","correct":false,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529066,"choiceText":"Delayed sleep phase disorder","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529067,"choiceText":"Narcolepsy","correct":true,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"","displayOrder":1,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":490073,"questionText":"On the basis of these findings only, what is the most likely diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma"},{"authors":"Timothy D. Murphy, MD","content":["This case is very challenging because the patient had the findings of and met the criteria for OSA, periodic limb movement disorder (PLMD)/restless legs syndrome (RLS), and hypersomnolence. She also had several historical findings that were highly suggestive of narcolepsy with cataplexy. These included a strong family history of narcolepsy, a history of the sudden onset of sleep and greatly increased sleep pressure, and rapid weight gain. A critical finding was a nocturnal sleep-onset REM sleep period (SOREMP). A nocturnal SOREMP (defined as REM sleep within 15 minutes of falling asleep) has a very high specificity for narcolepsy with cataplexy in adults and children.[1,2] However, the importance of the nocturnal SOREMP was not initially noted in her evaluation and management.","OSA and PLMD were initially diagnosed, and the otolaryngologist performed an adenotonsillectomy. The patient returned to the pediatric pulmonary and sleep medicine clinic after the procedure. At 3 weeks after the surgery, her somnolence improved very little. She had been gaining weight more rapidly and symptoms of apparent instability in her asthma were noted.","Further history-taking revealed a complex set of interactions around eating (some involved her father catering to her desire for higher-carbohydrate foods), increased sedentary behavior, and a history suggestive of vocal cord dysfunction. She was having \"asthma attacks\" characterized by rapid onset with inspiratory stridor and rapid resolution at the onset of activity. Her family was willing to make changes in their diet and to encourage activity, and they sought help for the vocal cord dysfunction from a speech and language pathologist.","Despite these measures, her weight gain rapidly progressed and the daytime fatigue and sleepiness continued. The pediatrician referred her to the neurologist who had interpreted the first NPSG. His history presented a differential diagnosis of narcolepsy, primary hypersomnolence, persistent OSA, and PLMD. He recommended a second NPSG with a multiple sleep latency test (MSLT), to be done immediately following the NPSG to assess her sleepiness more formally. His history documented that she felt as if she was \"going to fall\" when she laughed. He also noted that her father had OSA (treated with CPAP) and that she had an uncle and a grandfather with narcolepsy.","The second NPSG revealed the following:","A respiratory disturbance index of 1.4 (improved)","Sleep latency of 2.5 minutes and REM latency of 68.5 minutes","A sleep efficiency of 68.3%","31.6% of total sleep time in stage N1, 43.8% in N2, 20% in N3, and 4.6% in REM sleep","An arousal index of 23.5 (increased)","A periodic leg movement index of 5.9 (slightly lower)","\"3 REM periods, 2 of them were very brief,\" and a period of wakefulness after sleep onset of 180.5 minutes (increased)","The MSLT showed a mean sleep latency calculated at 9.5 minutes and no sleep onset–associated REM sleep (REM sleep within 20 minutes of sleep onset).","The neurologist provisionally diagnosed narcolepsy (vs hypersomnolence). He prescribed methylphenidate and then gradually increased the dose. Despite slightly improved daytime alertness, the patient started to develop more classic findings of cataplexy. The patient's mother brought her back to the pediatric pulmonary and sleep medicine clinic. Methylphenidate was discontinued and therapy with modafinil was initiated.","When the patient was 9 years old, sodium oxybate was added to her regimen and her condition finally stabilized. Her therapy was complicated by the treatment of her inattention with dextroamphetamine and levoamphetamine (Adderall) and the effects of all of her therapy on her weight. Her rapid weight gain was followed by an equally rapid weight loss, and these changes finally settled into her currently stable pattern of tracking around the 75th percentile after starting sodium oxybate (Figure 2).","Figure 2."],"date":"October 09, 2020","figures":[{"caption":"Figure 2.","image_url":"https://img.medscapestatic.com/article/938/423/938423-Thumb2.jpg"}],"markdown":"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\n\n **Authors:** Timothy D. Murphy, MD \n **Date:** October 09, 2020\n\n ## Content\n\n This case is very challenging because the patient had the findings of and met the criteria for OSA, periodic limb movement disorder (PLMD)/restless legs syndrome (RLS), and hypersomnolence. She also had several historical findings that were highly suggestive of narcolepsy with cataplexy. These included a strong family history of narcolepsy, a history of the sudden onset of sleep and greatly increased sleep pressure, and rapid weight gain. A critical finding was a nocturnal sleep-onset REM sleep period (SOREMP). A nocturnal SOREMP (defined as REM sleep within 15 minutes of falling asleep) has a very high specificity for narcolepsy with cataplexy in adults and children.[1,2] However, the importance of the nocturnal SOREMP was not initially noted in her evaluation and management.\nOSA and PLMD were initially diagnosed, and the otolaryngologist performed an adenotonsillectomy. The patient returned to the pediatric pulmonary and sleep medicine clinic after the procedure. At 3 weeks after the surgery, her somnolence improved very little. She had been gaining weight more rapidly and symptoms of apparent instability in her asthma were noted.\nFurther history-taking revealed a complex set of interactions around eating (some involved her father catering to her desire for higher-carbohydrate foods), increased sedentary behavior, and a history suggestive of vocal cord dysfunction. She was having \"asthma attacks\" characterized by rapid onset with inspiratory stridor and rapid resolution at the onset of activity. Her family was willing to make changes in their diet and to encourage activity, and they sought help for the vocal cord dysfunction from a speech and language pathologist.\nDespite these measures, her weight gain rapidly progressed and the daytime fatigue and sleepiness continued. The pediatrician referred her to the neurologist who had interpreted the first NPSG. His history presented a differential diagnosis of narcolepsy, primary hypersomnolence, persistent OSA, and PLMD. He recommended a second NPSG with a multiple sleep latency test (MSLT), to be done immediately following the NPSG to assess her sleepiness more formally. His history documented that she felt as if she was \"going to fall\" when she laughed. He also noted that her father had OSA (treated with CPAP) and that she had an uncle and a grandfather with narcolepsy.\nThe second NPSG revealed the following:\nA respiratory disturbance index of 1.4 (improved)\nSleep latency of 2.5 minutes and REM latency of 68.5 minutes\nA sleep efficiency of 68.3%\n31.6% of total sleep time in stage N1, 43.8% in N2, 20% in N3, and 4.6% in REM sleep\nAn arousal index of 23.5 (increased)\nA periodic leg movement index of 5.9 (slightly lower)\n\"3 REM periods, 2 of them were very brief,\" and a period of wakefulness after sleep onset of 180.5 minutes (increased)\nThe MSLT showed a mean sleep latency calculated at 9.5 minutes and no sleep onset–associated REM sleep (REM sleep within 20 minutes of sleep onset).\nThe neurologist provisionally diagnosed narcolepsy (vs hypersomnolence). He prescribed methylphenidate and then gradually increased the dose. Despite slightly improved daytime alertness, the patient started to develop more classic findings of cataplexy. The patient's mother brought her back to the pediatric pulmonary and sleep medicine clinic. Methylphenidate was discontinued and therapy with modafinil was initiated.\nWhen the patient was 9 years old, sodium oxybate was added to her regimen and her condition finally stabilized. Her therapy was complicated by the treatment of her inattention with dextroamphetamine and levoamphetamine (Adderall) and the effects of all of her therapy on her weight. Her rapid weight gain was followed by an equally rapid weight loss, and these changes finally settled into her currently stable pattern of tracking around the 75th percentile after starting sodium oxybate (Figure 2).\nFigure 2.\n\n ## Figures\n\n **Figure 2.** \n \n\n\n*Page 3 of 6*","pagination":{"current_page":3,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1529064,"choiceText":"Behavioral insomnia of childhood\r\n","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529065,"choiceText":"Pediatric chronic obstructive pulmonary disease","correct":false,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529066,"choiceText":"Delayed sleep phase disorder","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529067,"choiceText":"Narcolepsy","correct":true,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"","displayOrder":1,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":490073,"questionText":"On the basis of these findings only, what is the most likely diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma"},{"authors":"Timothy D. Murphy, MD","content":["This case illustrates some of the challenges facing clinicians who care for a \"sleepy child.\" In the evolution of this child's care, multiple diagnoses were made and treated. The failure of her symptoms to respond to treatment resulted in further evaluation (and reevaluation of the data), which finally led to the diagnosis (narcolepsy with cataplexy) and her ultimate improvement and stabilization.","Hypersomnolence may be primary or it may be secondary to a poor night's sleep. The most common conditions seen in a pediatric sleep clinic that might lead to daytime sleepiness include sleep apnea, behavioral insomnia of childhood, restless sleeping (or, when more extreme, pediatric RLS), and delayed sleep phase disorder (DSPD). The latter is much more common in teenagers, with a prevalence of up to 7% in this age group.[3] However, youths with daytime hypersomnolence due to DSPD do not typically fall asleep easily at bedtime, as this patient did. Moreover, DSPD is unusual in an 8-year-old.","An insufficient quantity of sleep can usually be diagnosed on the basis of the history alone, but actigraphy is occasionally used when the history does not exclude difficulty in falling asleep or a circadian rhythm sleep-wake disorder.[4] Actigraphy was not included in this patient's workup.","Pediatric RLS is primarily diagnosed on the basis of history, but the use of strict criteria (which include that the child \"relates a description in his or her own words\" of leg discomfort) may lead to missing the diagnosis in children who can benefit from treatment but are unable to verbalize their feelings. Suboptimal levels of serum ferritin are associated with restless sleep in children, as is improvement with iron therapy. The use of dopaminergic medications typically requires a higher standard for the diagnosis of RLS and a failure to respond to iron therapy.[5,6] Published data regarding autism and attention-deficit/hyperactivity disorder (ADHD) increasingly suggest complex links between iron metabolism and brain function, including during sleep.[7,8] This patient's movements in bed and her behavioral and learning struggles led to the investigation of her iron stores and ferritin levels and a trial of treatment for RLS.","Hypersomnolence is associated with OSA more commonly in adults than in children. \"Hyperactivity\" or symptoms of ADHD are more frequently observed in children with OSA, although some sleepiness is still noted.[9] Most sleep centers consider an obstructive AHI of fewer than 1 event per hour (some use a threshold of 1.5) to be normal.[10] More pragmatically, the absolute score is useful in choosing a diagnostic billing code, but clinical decision-making also factors in the age of the patient and the severity of observed symptoms, considered formally or as a gestalt.[11]","This patient had a positive AHI, which is diagnostic of OSA, and underwent adenotonsillectomy without significant improvement. She was also treated with iron and vitamin C, without significant changes in her daytime sleepiness or her apparent sleep quality. Furthermore, her clinical care was complicated by the MSLT result, which documented hypersomnolence but not narcolepsy.","The diagnosis of narcolepsy was based primarily on clinical factors. Despite the positive AHI, snoring, leg movements, and low ferritin level, her condition did not improve after the adenotonsillectomy and iron therapy. As her case progressed, she developed more classic symptoms of cataplexy, such as feeling as if she would fall with laughter and falling asleep rapidly in conjunction with strong emotions. These findings, along with the rapid weight gain, pointed toward the diagnosis.","Some confusion along the path toward a diagnosis is common in narcolepsy. Comorbidities, including PLMD, RLS, and OSA, may be found in association with narcolepsy and can delay the diagnosis,[12] as certainly happened in this patient.","Narcolepsy affects about 1 in 2000 people. Two types are recognized: type 1 narcolepsy (previously referred to as narcolepsy with cataplexy) and type 2 narcolepsy (narcolepsy without cataplexy). Type 1 narcolepsy is considered an adult diagnosis by many pediatricians, but it frequently develops during adolescence, and onset after age 40 years is uncommon. Children may first present with a resumption of prolonged naps rather than prolonged nighttime sleep; nocturnal sleep is often somewhat disturbed initially. Cataplexy, multiple short naps during the day, hypnagogic hallucinations, and sleep-onset REM periods may be absent in young children, and repeated NPSGs and MSLTs over months to years may be required to make the diagnosis.","Although a retrospective analysis of sleep histories often reveals hypersomnolence for years prior to the diagnosis, it can be easily missed in the first decade of life.[13] Type 1 narcolepsy is caused by the loss of orexin neuropeptides, which are mediators of central nervous system (CNS) control of energy metabolism and maintenance of sleep-wake states. Rapid weight gain and precocious puberty can occur in children with type 1 narcolepsy. This patient's rapid weight gain started to make more sense once the diagnosis was made.[14]","In type 1 narcolepsy, the lack of consistent REM sleep at night leads to the intrusion of REM sleep features into the waking state. The diagnostic features include the tetrad of daytime sleepiness, cataplexy, hypnagogic hallucinations, and sleep paralysis. Specific questioning is usually required to elicit the history; only cataplexy is specific for narcolepsy. Patients often present initially with hypersomnolence alone, and other diagnostic findings may emerge over time.","The etiology of narcolepsy is unclear. The lack of orexin may be related to autoimmune disease or infectious diseases. Most patients with type 1 narcolepsy have HLA DQB1 (0602 allele), the gene complex that encodes for proteins on the surface of T cells. Additionally, some infections (most notably H1N1 influenza, as well as some vaccines for it) are associated with clusters of type 1 narcolepsy and reduced orexin levels.[15,16,17] However, measurement of cerebrospinal fluid (CSF) levels of orexin is not required to make the diagnosis of narcolepsy.","The diagnosis of type 1 narcolepsy can be clinically made in a child with a clear history of cataplexy, EDS, and an otherwise normal neurologic examination. In the absence of cataplexy, an NPSG followed by an MSLT can be used to make the diagnosis of narcolepsy. \"Secondary narcolepsy\" in the setting of CNS diseases such as hypothalamic tumors or arteriovenous malformations, following cerebrovascular accidents, or in association with multiple sclerosis or Niemann-Pick disease type C has been reported, but alternative causes of narcolepsy are vanishingly rare in childhood. The primary challenge is to rule out other sleep disorders causing the EDS; as in this patient, that may be difficult."],"date":"October 09, 2020","figures":[],"markdown":"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\n\n **Authors:** Timothy D. Murphy, MD \n **Date:** October 09, 2020\n\n ## Content\n\n This case illustrates some of the challenges facing clinicians who care for a \"sleepy child.\" In the evolution of this child's care, multiple diagnoses were made and treated. The failure of her symptoms to respond to treatment resulted in further evaluation (and reevaluation of the data), which finally led to the diagnosis (narcolepsy with cataplexy) and her ultimate improvement and stabilization.\nHypersomnolence may be primary or it may be secondary to a poor night's sleep. The most common conditions seen in a pediatric sleep clinic that might lead to daytime sleepiness include sleep apnea, behavioral insomnia of childhood, restless sleeping (or, when more extreme, pediatric RLS), and delayed sleep phase disorder (DSPD). The latter is much more common in teenagers, with a prevalence of up to 7% in this age group.[3] However, youths with daytime hypersomnolence due to DSPD do not typically fall asleep easily at bedtime, as this patient did. Moreover, DSPD is unusual in an 8-year-old.\nAn insufficient quantity of sleep can usually be diagnosed on the basis of the history alone, but actigraphy is occasionally used when the history does not exclude difficulty in falling asleep or a circadian rhythm sleep-wake disorder.[4] Actigraphy was not included in this patient's workup.\nPediatric RLS is primarily diagnosed on the basis of history, but the use of strict criteria (which include that the child \"relates a description in his or her own words\" of leg discomfort) may lead to missing the diagnosis in children who can benefit from treatment but are unable to verbalize their feelings. Suboptimal levels of serum ferritin are associated with restless sleep in children, as is improvement with iron therapy. The use of dopaminergic medications typically requires a higher standard for the diagnosis of RLS and a failure to respond to iron therapy.[5,6] Published data regarding autism and attention-deficit/hyperactivity disorder (ADHD) increasingly suggest complex links between iron metabolism and brain function, including during sleep.[7,8] This patient's movements in bed and her behavioral and learning struggles led to the investigation of her iron stores and ferritin levels and a trial of treatment for RLS.\nHypersomnolence is associated with OSA more commonly in adults than in children. \"Hyperactivity\" or symptoms of ADHD are more frequently observed in children with OSA, although some sleepiness is still noted.[9] Most sleep centers consider an obstructive AHI of fewer than 1 event per hour (some use a threshold of 1.5) to be normal.[10] More pragmatically, the absolute score is useful in choosing a diagnostic billing code, but clinical decision-making also factors in the age of the patient and the severity of observed symptoms, considered formally or as a gestalt.[11]\nThis patient had a positive AHI, which is diagnostic of OSA, and underwent adenotonsillectomy without significant improvement. She was also treated with iron and vitamin C, without significant changes in her daytime sleepiness or her apparent sleep quality. Furthermore, her clinical care was complicated by the MSLT result, which documented hypersomnolence but not narcolepsy.\nThe diagnosis of narcolepsy was based primarily on clinical factors. Despite the positive AHI, snoring, leg movements, and low ferritin level, her condition did not improve after the adenotonsillectomy and iron therapy. As her case progressed, she developed more classic symptoms of cataplexy, such as feeling as if she would fall with laughter and falling asleep rapidly in conjunction with strong emotions. These findings, along with the rapid weight gain, pointed toward the diagnosis.\nSome confusion along the path toward a diagnosis is common in narcolepsy. Comorbidities, including PLMD, RLS, and OSA, may be found in association with narcolepsy and can delay the diagnosis,[12] as certainly happened in this patient.\nNarcolepsy affects about 1 in 2000 people. Two types are recognized: type 1 narcolepsy (previously referred to as narcolepsy with cataplexy) and type 2 narcolepsy (narcolepsy without cataplexy). Type 1 narcolepsy is considered an adult diagnosis by many pediatricians, but it frequently develops during adolescence, and onset after age 40 years is uncommon. Children may first present with a resumption of prolonged naps rather than prolonged nighttime sleep; nocturnal sleep is often somewhat disturbed initially. Cataplexy, multiple short naps during the day, hypnagogic hallucinations, and sleep-onset REM periods may be absent in young children, and repeated NPSGs and MSLTs over months to years may be required to make the diagnosis.\nAlthough a retrospective analysis of sleep histories often reveals hypersomnolence for years prior to the diagnosis, it can be easily missed in the first decade of life.[13] Type 1 narcolepsy is caused by the loss of orexin neuropeptides, which are mediators of central nervous system (CNS) control of energy metabolism and maintenance of sleep-wake states. Rapid weight gain and precocious puberty can occur in children with type 1 narcolepsy. This patient's rapid weight gain started to make more sense once the diagnosis was made.[14]\nIn type 1 narcolepsy, the lack of consistent REM sleep at night leads to the intrusion of REM sleep features into the waking state. The diagnostic features include the tetrad of daytime sleepiness, cataplexy, hypnagogic hallucinations, and sleep paralysis. Specific questioning is usually required to elicit the history; only cataplexy is specific for narcolepsy. Patients often present initially with hypersomnolence alone, and other diagnostic findings may emerge over time.\nThe etiology of narcolepsy is unclear. The lack of orexin may be related to autoimmune disease or infectious diseases. Most patients with type 1 narcolepsy have HLA DQB1 (0602 allele), the gene complex that encodes for proteins on the surface of T cells. Additionally, some infections (most notably H1N1 influenza, as well as some vaccines for it) are associated with clusters of type 1 narcolepsy and reduced orexin levels.[15,16,17] However, measurement of cerebrospinal fluid (CSF) levels of orexin is not required to make the diagnosis of narcolepsy.\nThe diagnosis of type 1 narcolepsy can be clinically made in a child with a clear history of cataplexy, EDS, and an otherwise normal neurologic examination. In the absence of cataplexy, an NPSG followed by an MSLT can be used to make the diagnosis of narcolepsy. \"Secondary narcolepsy\" in the setting of CNS diseases such as hypothalamic tumors or arteriovenous malformations, following cerebrovascular accidents, or in association with multiple sclerosis or Niemann-Pick disease type C has been reported, but alternative causes of narcolepsy are vanishingly rare in childhood. The primary challenge is to rule out other sleep disorders causing the EDS; as in this patient, that may be difficult.\n\n ## Figures\n\n \n*Page 4 of 6*","pagination":{"current_page":4,"total_pages":6},"questionnaire":[],"title":"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma"},{"authors":"Timothy D. Murphy, MD","content":["The treatment of narcolepsy focuses first on attempts to reduce the EDS pharmacologically; timed naps or increased time in bed is not usually sufficient to reduce the EDS. Although many medications have been used to treat EDS, clinicians typically start with caffeine (usually inadequate) and then move to stronger stimulants, such as methylphenidate or amphetamine and dextroamphetamine in combination.","Failure of these agents might then lead to the use of modafinil (prescription without the failure of other therapies is often difficult). Monitoring of response and fairly frequent visits are required at this point. A selective serotonin reuptake inhibitor, such as fluoxetine, is often added to the regimen of patients with classic cataplexy. As was the case for this patient, the use of medications that might affect mood, attention, learning, and sleep requires close attention and collaboration between specialists in sleep medicine, neurology, and behavioral and general pediatrics.","In some patients, including this patient, sodium oxybate (gamma-hydroxybutyrate [GHB]) is required to treat the cataplexy and to lead to better daytime functioning.[18] The exact mechanism of action is unknown, but the evening dosing of GHB is associated with improved REM sleep at night, perhaps relieving the intrusion of REM during daytime wake periods associated with type 1 narcolepsy. Unfortunately, GHB is associated with abuse — it is often called the \"date rape drug\" — and is now tightly regulated. Prescription in the United States is limited to one US pharmacy, and a sleep physician is typically required to obtain and use this medication.","The finding of EDS requires exploration of nocturnal problems with sleep, including RLS, OSA, and behavioral insomnia that affects daytime functioning. Narcolepsy can be diagnosed as the cause of EDS on the basis of careful history-taking as well as the results of an NPSG and an MSLT."],"date":"October 09, 2020","figures":[],"markdown":"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\n\n **Authors:** Timothy D. Murphy, MD \n **Date:** October 09, 2020\n\n ## Content\n\n The treatment of narcolepsy focuses first on attempts to reduce the EDS pharmacologically; timed naps or increased time in bed is not usually sufficient to reduce the EDS. Although many medications have been used to treat EDS, clinicians typically start with caffeine (usually inadequate) and then move to stronger stimulants, such as methylphenidate or amphetamine and dextroamphetamine in combination.\nFailure of these agents might then lead to the use of modafinil (prescription without the failure of other therapies is often difficult). Monitoring of response and fairly frequent visits are required at this point. A selective serotonin reuptake inhibitor, such as fluoxetine, is often added to the regimen of patients with classic cataplexy. As was the case for this patient, the use of medications that might affect mood, attention, learning, and sleep requires close attention and collaboration between specialists in sleep medicine, neurology, and behavioral and general pediatrics.\nIn some patients, including this patient, sodium oxybate (gamma-hydroxybutyrate [GHB]) is required to treat the cataplexy and to lead to better daytime functioning.[18] The exact mechanism of action is unknown, but the evening dosing of GHB is associated with improved REM sleep at night, perhaps relieving the intrusion of REM during daytime wake periods associated with type 1 narcolepsy. Unfortunately, GHB is associated with abuse — it is often called the \"date rape drug\" — and is now tightly regulated. Prescription in the United States is limited to one US pharmacy, and a sleep physician is typically required to obtain and use this medication.\nThe finding of EDS requires exploration of nocturnal problems with sleep, including RLS, OSA, and behavioral insomnia that affects daytime functioning. Narcolepsy can be diagnosed as the cause of EDS on the basis of careful history-taking as well as the results of an NPSG and an MSLT.\n\n ## Figures\n\n \n*Page 5 of 6*","pagination":{"current_page":5,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1529068,"choiceText":"Narcolepsy without cataplexy (type 2 narcolepsy) is associated with increased orexin neuropeptide levels","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529069,"choiceText":"Childhood narcolepsy is characterized by multiple brief naps during the day","correct":false,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529070,"choiceText":"Narcolepsy is associated with the loss of orexin neuropeptides","correct":true,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529071,"choiceText":"Measurement of orexin levels in the CSF is required for the diagnosis of narcolepsy","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Levels of orexin neuropeptides in the CNS are reduced, not increased, in all forms of narcolepsy. Children more frequently present with prolonged daytime sleep, and multiple naps are typically seen in older patients. The diagnosis can be made by a careful history-taking that documents cataplexy, which is explained only by type 1 narcolepsy. Measurement of CSF levels of orexin is usually related to research only and typically is not used clinically in diagnosing narcolepsy.","displayOrder":2,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":490074,"questionText":"Which of the following is most accurate regarding narcolepsy in children?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1529072,"choiceText":"Timed or planned naps to reduce sleep pressure, and amphetamine and dextroamphetamine for stimulant therapy during the day\r\n","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529073,"choiceText":"Modafinil as a daytime stimulant, fluoxetine for cataplexy, and sodium oxybate to improve REM efficiency","correct":true,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529074,"choiceText":"Caffeine as a morning stimulant and sodium oxybate (gamma-hydroxybutyrate [GHB]) used at night to consolidate non-REM sleep","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529075,"choiceText":"Methylphenidate to reduce cataplexy, fluoxetine to reduce depressive symptoms, and sodium oxybate to prolong REM latency","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Caffeine is usually an inadequate stimulant for patients with narcolepsy. The daytime use of methylphenidate or amphetamine and dextroamphetamine in combination does not adequately reduce cataplexy and does not address the problem with REM sleep at night. Modafinil is a more reliable daytime stimulant, and fluoxetine helps reduce cataplexy. The use of sodium oxybate in the evening in divided doses is intended to consolidate REM sleep and may reduce REM latency; non-REM sleep is not related to the daytime difficulties associated with narcolepsy.","displayOrder":3,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":490075,"questionText":"Which of the following is typically required in the treatment of type 1 narcolepsy?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma"},{"authors":"Timothy D. Murphy, MD","content":[],"date":"October 09, 2020","figures":[],"markdown":"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\n\n **Authors:** Timothy D. Murphy, MD \n **Date:** October 09, 2020\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*","pagination":{"current_page":6,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1529068,"choiceText":"Narcolepsy without cataplexy (type 2 narcolepsy) is associated with increased orexin neuropeptide levels","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529069,"choiceText":"Childhood narcolepsy is characterized by multiple brief naps during the day","correct":false,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529070,"choiceText":"Narcolepsy is associated with the loss of orexin neuropeptides","correct":true,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529071,"choiceText":"Measurement of orexin levels in the CSF is required for the diagnosis of narcolepsy","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Levels of orexin neuropeptides in the CNS are reduced, not increased, in all forms of narcolepsy. Children more frequently present with prolonged daytime sleep, and multiple naps are typically seen in older patients. The diagnosis can be made by a careful history-taking that documents cataplexy, which is explained only by type 1 narcolepsy. Measurement of CSF levels of orexin is usually related to research only and typically is not used clinically in diagnosing narcolepsy.","displayOrder":2,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":490074,"questionText":"Which of the following is most accurate regarding narcolepsy in children?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1529072,"choiceText":"Timed or planned naps to reduce sleep pressure, and amphetamine and dextroamphetamine for stimulant therapy during the day\r\n","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529073,"choiceText":"Modafinil as a daytime stimulant, fluoxetine for cataplexy, and sodium oxybate to improve REM efficiency","correct":true,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529074,"choiceText":"Caffeine as a morning stimulant and sodium oxybate (gamma-hydroxybutyrate [GHB]) used at night to consolidate non-REM sleep","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529075,"choiceText":"Methylphenidate to reduce cataplexy, fluoxetine to reduce depressive symptoms, and sodium oxybate to prolong REM latency","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Caffeine is usually an inadequate stimulant for patients with narcolepsy. The daytime use of methylphenidate or amphetamine and dextroamphetamine in combination does not adequately reduce cataplexy and does not address the problem with REM sleep at night. Modafinil is a more reliable daytime stimulant, and fluoxetine helps reduce cataplexy. The use of sodium oxybate in the evening in divided doses is intended to consolidate REM sleep and may reduce REM latency; non-REM sleep is not related to the daytime difficulties associated with narcolepsy.","displayOrder":3,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":490075,"questionText":"Which of the following is typically required in the treatment of type 1 narcolepsy?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma"}],"string":"[\n {\n \"authors\": \"Timothy D. Murphy, MD\",\n \"content\": [\n \"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us .\",\n \"A 5-year-old girl with a long-standing history of severe asthma and eczema presented to a pediatric pulmonary and sleep medicine clinic. Her asthma was stabilized with an inhaled corticosteroid (fluticasone, 88 µg, inhaled twice daily), albuterol sulfate (180 µg, inhaled as needed), and ipratropium bromide (34 µg, inhaled as needed). Her skin condition improved with a moderately aggressive regimen of hydrating bleach baths, moisturizing lotions, nonsedating antihistamines, and as-needed use of topical hydrocortisone or triamcinolone, pimecrolimus, and mupirocin.\",\n \"Her asthma remained stable for a year but then progressed to the extent that the dosage of inhaled fluticasone was increased to 220 µg twice daily. Bronchoscopy revealed only mild bronchomalacia of the left mainstem bronchus (Figure 1), diffuse mild inflammation, and increased secretions.\",\n \"Figure 1.\",\n \"Montelukast (5 mg daily) and nasal fluticasone (50 µg) were added to her regimen. In addition, diphenhydramine (25 mg) was prescribed to be used as needed for excessive itchiness, eczema flares, and allergic asthma flares.\",\n \"The patient remained well and was followed up in the clinic approximately every 3 months, owing to the complexity of her condition. After 6 months, significant weight gain and an increasing body mass index (BMI) were noted. She met with a dietitian, who recommended weight loss strategies. From the age of 7-8 years, the patient demonstrated a modest weight loss from the changes in her diet. However, symptoms of fatigue, excessive daytime sleepiness (EDS), and inattention in school developed over a 1- to 2-month period, and her weight started to increase rapidly despite the dietary intervention.\",\n \"Her daytime sleepiness seemed to be progressive, and she would fall asleep suddenly even when she wanted to be awake. Concerned about the emerging symptoms of inattention, autistic features, fatigue, and sleepiness, the girl's parents are seeking further medical advice.\"\n ],\n \"date\": \"October 09, 2020\",\n \"figures\": [\n {\n \"caption\": \"Figure 1.\",\n \"image_url\": \"https://img.medscapestatic.com/article/938/423/938423-Thumb1.jpg\"\n }\n ],\n \"markdown\": \"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\\n\\n **Authors:** Timothy D. Murphy, MD \\n **Date:** October 09, 2020\\n\\n ## Content\\n\\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us .\\nA 5-year-old girl with a long-standing history of severe asthma and eczema presented to a pediatric pulmonary and sleep medicine clinic. Her asthma was stabilized with an inhaled corticosteroid (fluticasone, 88 µg, inhaled twice daily), albuterol sulfate (180 µg, inhaled as needed), and ipratropium bromide (34 µg, inhaled as needed). Her skin condition improved with a moderately aggressive regimen of hydrating bleach baths, moisturizing lotions, nonsedating antihistamines, and as-needed use of topical hydrocortisone or triamcinolone, pimecrolimus, and mupirocin.\\nHer asthma remained stable for a year but then progressed to the extent that the dosage of inhaled fluticasone was increased to 220 µg twice daily. Bronchoscopy revealed only mild bronchomalacia of the left mainstem bronchus (Figure 1), diffuse mild inflammation, and increased secretions.\\nFigure 1.\\nMontelukast (5 mg daily) and nasal fluticasone (50 µg) were added to her regimen. In addition, diphenhydramine (25 mg) was prescribed to be used as needed for excessive itchiness, eczema flares, and allergic asthma flares.\\nThe patient remained well and was followed up in the clinic approximately every 3 months, owing to the complexity of her condition. After 6 months, significant weight gain and an increasing body mass index (BMI) were noted. She met with a dietitian, who recommended weight loss strategies. From the age of 7-8 years, the patient demonstrated a modest weight loss from the changes in her diet. However, symptoms of fatigue, excessive daytime sleepiness (EDS), and inattention in school developed over a 1- to 2-month period, and her weight started to increase rapidly despite the dietary intervention.\\nHer daytime sleepiness seemed to be progressive, and she would fall asleep suddenly even when she wanted to be awake. Concerned about the emerging symptoms of inattention, autistic features, fatigue, and sleepiness, the girl's parents are seeking further medical advice.\\n\\n ## Figures\\n\\n **Figure 1.** \\n \\n\\n\\n*Page 1 of 6*\",\n \"pagination\": {\n \"current_page\": 1,\n \"total_pages\": 6\n },\n \"questionnaire\": [],\n \"title\": \"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\"\n },\n {\n \"authors\": \"Timothy D. Murphy, MD\",\n \"content\": [\n \"The patient has fallen asleep at school nearly every day for the past 1-2 months and falls into a deep sleep unless she is kept active. At home, she is taking more naps during the day, falling asleep in the car, and struggling with schoolwork. Her grades have dropped significantly over the past few months. Her parents report that she does not awaken during the night. No snoring, choking, snorting, gasping, or apnea is noted. She sleeps an average of 9-10 hours per night but is restless and tosses and turns frequently in her sleep.\",\n \"Her family history is notable for obesity, obstructive sleep apnea (OSA) that requires continuous positive airway pressure (CPAP) in her father, and narcolepsy in an uncle and a grandfather.\",\n \"On physical examination, she has mild to moderate obesity (BMI of 23.89 kg/m2 [the 98th percentile for age]) and enlarged tonsils (2-3+). She has difficulty with focusing and staying awake in the clinic.\",\n \"She is referred to a pediatric otolaryngologist for consideration of nocturnal polysomnography (NPSG) or an adenotonsillectomy. The otolaryngologist notes that she has not tolerated nasal fluticasone well, that she is a chronic mouth breather, and that her tonsils are enlarged (3+). An NPSG is ordered to help clarify matters.\",\n \"The NPSG demonstrates the following:\",\n \"A respiratory disturbance index and an apnea-hypopnea index (AHI) of 6.2 per hour\",\n \"Sleep latency of 0.5 minutes and rapid eye movement (REM) latency of 0.5 minutes\",\n \"A sleep efficiency of 87.5%\",\n \"18.2% of total sleep time in stage N1, 36.4% in N2, 29.9% in N3, and 15.5% in REM sleep\",\n \"An arousal index of 18.6\",\n \"A periodic leg movement index of 6.3\",\n \"Multiple periods of wakefulness scattered throughout the night and six REM periods\"\n ],\n \"date\": \"October 09, 2020\",\n \"figures\": [],\n \"markdown\": \"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\\n\\n **Authors:** Timothy D. Murphy, MD \\n **Date:** October 09, 2020\\n\\n ## Content\\n\\n The patient has fallen asleep at school nearly every day for the past 1-2 months and falls into a deep sleep unless she is kept active. At home, she is taking more naps during the day, falling asleep in the car, and struggling with schoolwork. Her grades have dropped significantly over the past few months. Her parents report that she does not awaken during the night. No snoring, choking, snorting, gasping, or apnea is noted. She sleeps an average of 9-10 hours per night but is restless and tosses and turns frequently in her sleep.\\nHer family history is notable for obesity, obstructive sleep apnea (OSA) that requires continuous positive airway pressure (CPAP) in her father, and narcolepsy in an uncle and a grandfather.\\nOn physical examination, she has mild to moderate obesity (BMI of 23.89 kg/m2 [the 98th percentile for age]) and enlarged tonsils (2-3+). She has difficulty with focusing and staying awake in the clinic.\\nShe is referred to a pediatric otolaryngologist for consideration of nocturnal polysomnography (NPSG) or an adenotonsillectomy. The otolaryngologist notes that she has not tolerated nasal fluticasone well, that she is a chronic mouth breather, and that her tonsils are enlarged (3+). An NPSG is ordered to help clarify matters.\\nThe NPSG demonstrates the following:\\nA respiratory disturbance index and an apnea-hypopnea index (AHI) of 6.2 per hour\\nSleep latency of 0.5 minutes and rapid eye movement (REM) latency of 0.5 minutes\\nA sleep efficiency of 87.5%\\n18.2% of total sleep time in stage N1, 36.4% in N2, 29.9% in N3, and 15.5% in REM sleep\\nAn arousal index of 18.6\\nA periodic leg movement index of 6.3\\nMultiple periods of wakefulness scattered throughout the night and six REM periods\\n\\n ## Figures\\n\\n \\n*Page 2 of 6*\",\n \"pagination\": {\n \"current_page\": 2,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1529064,\n \"choiceText\": \"Behavioral insomnia of childhood\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529065,\n \"choiceText\": \"Pediatric chronic obstructive pulmonary disease\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529066,\n \"choiceText\": \"Delayed sleep phase disorder\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529067,\n \"choiceText\": \"Narcolepsy\",\n \"correct\": true,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\",\n \"displayOrder\": 1,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 490073,\n \"questionText\": \"On the basis of these findings only, what is the most likely diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\"\n },\n {\n \"authors\": \"Timothy D. Murphy, MD\",\n \"content\": [\n \"This case is very challenging because the patient had the findings of and met the criteria for OSA, periodic limb movement disorder (PLMD)/restless legs syndrome (RLS), and hypersomnolence. She also had several historical findings that were highly suggestive of narcolepsy with cataplexy. These included a strong family history of narcolepsy, a history of the sudden onset of sleep and greatly increased sleep pressure, and rapid weight gain. A critical finding was a nocturnal sleep-onset REM sleep period (SOREMP). A nocturnal SOREMP (defined as REM sleep within 15 minutes of falling asleep) has a very high specificity for narcolepsy with cataplexy in adults and children.[1,2] However, the importance of the nocturnal SOREMP was not initially noted in her evaluation and management.\",\n \"OSA and PLMD were initially diagnosed, and the otolaryngologist performed an adenotonsillectomy. The patient returned to the pediatric pulmonary and sleep medicine clinic after the procedure. At 3 weeks after the surgery, her somnolence improved very little. She had been gaining weight more rapidly and symptoms of apparent instability in her asthma were noted.\",\n \"Further history-taking revealed a complex set of interactions around eating (some involved her father catering to her desire for higher-carbohydrate foods), increased sedentary behavior, and a history suggestive of vocal cord dysfunction. She was having \\\"asthma attacks\\\" characterized by rapid onset with inspiratory stridor and rapid resolution at the onset of activity. Her family was willing to make changes in their diet and to encourage activity, and they sought help for the vocal cord dysfunction from a speech and language pathologist.\",\n \"Despite these measures, her weight gain rapidly progressed and the daytime fatigue and sleepiness continued. The pediatrician referred her to the neurologist who had interpreted the first NPSG. His history presented a differential diagnosis of narcolepsy, primary hypersomnolence, persistent OSA, and PLMD. He recommended a second NPSG with a multiple sleep latency test (MSLT), to be done immediately following the NPSG to assess her sleepiness more formally. His history documented that she felt as if she was \\\"going to fall\\\" when she laughed. He also noted that her father had OSA (treated with CPAP) and that she had an uncle and a grandfather with narcolepsy.\",\n \"The second NPSG revealed the following:\",\n \"A respiratory disturbance index of 1.4 (improved)\",\n \"Sleep latency of 2.5 minutes and REM latency of 68.5 minutes\",\n \"A sleep efficiency of 68.3%\",\n \"31.6% of total sleep time in stage N1, 43.8% in N2, 20% in N3, and 4.6% in REM sleep\",\n \"An arousal index of 23.5 (increased)\",\n \"A periodic leg movement index of 5.9 (slightly lower)\",\n \"\\\"3 REM periods, 2 of them were very brief,\\\" and a period of wakefulness after sleep onset of 180.5 minutes (increased)\",\n \"The MSLT showed a mean sleep latency calculated at 9.5 minutes and no sleep onset–associated REM sleep (REM sleep within 20 minutes of sleep onset).\",\n \"The neurologist provisionally diagnosed narcolepsy (vs hypersomnolence). He prescribed methylphenidate and then gradually increased the dose. Despite slightly improved daytime alertness, the patient started to develop more classic findings of cataplexy. The patient's mother brought her back to the pediatric pulmonary and sleep medicine clinic. Methylphenidate was discontinued and therapy with modafinil was initiated.\",\n \"When the patient was 9 years old, sodium oxybate was added to her regimen and her condition finally stabilized. Her therapy was complicated by the treatment of her inattention with dextroamphetamine and levoamphetamine (Adderall) and the effects of all of her therapy on her weight. Her rapid weight gain was followed by an equally rapid weight loss, and these changes finally settled into her currently stable pattern of tracking around the 75th percentile after starting sodium oxybate (Figure 2).\",\n \"Figure 2.\"\n ],\n \"date\": \"October 09, 2020\",\n \"figures\": [\n {\n \"caption\": \"Figure 2.\",\n \"image_url\": \"https://img.medscapestatic.com/article/938/423/938423-Thumb2.jpg\"\n }\n ],\n \"markdown\": \"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\\n\\n **Authors:** Timothy D. Murphy, MD \\n **Date:** October 09, 2020\\n\\n ## Content\\n\\n This case is very challenging because the patient had the findings of and met the criteria for OSA, periodic limb movement disorder (PLMD)/restless legs syndrome (RLS), and hypersomnolence. She also had several historical findings that were highly suggestive of narcolepsy with cataplexy. These included a strong family history of narcolepsy, a history of the sudden onset of sleep and greatly increased sleep pressure, and rapid weight gain. A critical finding was a nocturnal sleep-onset REM sleep period (SOREMP). A nocturnal SOREMP (defined as REM sleep within 15 minutes of falling asleep) has a very high specificity for narcolepsy with cataplexy in adults and children.[1,2] However, the importance of the nocturnal SOREMP was not initially noted in her evaluation and management.\\nOSA and PLMD were initially diagnosed, and the otolaryngologist performed an adenotonsillectomy. The patient returned to the pediatric pulmonary and sleep medicine clinic after the procedure. At 3 weeks after the surgery, her somnolence improved very little. She had been gaining weight more rapidly and symptoms of apparent instability in her asthma were noted.\\nFurther history-taking revealed a complex set of interactions around eating (some involved her father catering to her desire for higher-carbohydrate foods), increased sedentary behavior, and a history suggestive of vocal cord dysfunction. She was having \\\"asthma attacks\\\" characterized by rapid onset with inspiratory stridor and rapid resolution at the onset of activity. Her family was willing to make changes in their diet and to encourage activity, and they sought help for the vocal cord dysfunction from a speech and language pathologist.\\nDespite these measures, her weight gain rapidly progressed and the daytime fatigue and sleepiness continued. The pediatrician referred her to the neurologist who had interpreted the first NPSG. His history presented a differential diagnosis of narcolepsy, primary hypersomnolence, persistent OSA, and PLMD. He recommended a second NPSG with a multiple sleep latency test (MSLT), to be done immediately following the NPSG to assess her sleepiness more formally. His history documented that she felt as if she was \\\"going to fall\\\" when she laughed. He also noted that her father had OSA (treated with CPAP) and that she had an uncle and a grandfather with narcolepsy.\\nThe second NPSG revealed the following:\\nA respiratory disturbance index of 1.4 (improved)\\nSleep latency of 2.5 minutes and REM latency of 68.5 minutes\\nA sleep efficiency of 68.3%\\n31.6% of total sleep time in stage N1, 43.8% in N2, 20% in N3, and 4.6% in REM sleep\\nAn arousal index of 23.5 (increased)\\nA periodic leg movement index of 5.9 (slightly lower)\\n\\\"3 REM periods, 2 of them were very brief,\\\" and a period of wakefulness after sleep onset of 180.5 minutes (increased)\\nThe MSLT showed a mean sleep latency calculated at 9.5 minutes and no sleep onset–associated REM sleep (REM sleep within 20 minutes of sleep onset).\\nThe neurologist provisionally diagnosed narcolepsy (vs hypersomnolence). He prescribed methylphenidate and then gradually increased the dose. Despite slightly improved daytime alertness, the patient started to develop more classic findings of cataplexy. The patient's mother brought her back to the pediatric pulmonary and sleep medicine clinic. Methylphenidate was discontinued and therapy with modafinil was initiated.\\nWhen the patient was 9 years old, sodium oxybate was added to her regimen and her condition finally stabilized. Her therapy was complicated by the treatment of her inattention with dextroamphetamine and levoamphetamine (Adderall) and the effects of all of her therapy on her weight. Her rapid weight gain was followed by an equally rapid weight loss, and these changes finally settled into her currently stable pattern of tracking around the 75th percentile after starting sodium oxybate (Figure 2).\\nFigure 2.\\n\\n ## Figures\\n\\n **Figure 2.** \\n \\n\\n\\n*Page 3 of 6*\",\n \"pagination\": {\n \"current_page\": 3,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1529064,\n \"choiceText\": \"Behavioral insomnia of childhood\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529065,\n \"choiceText\": \"Pediatric chronic obstructive pulmonary disease\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529066,\n \"choiceText\": \"Delayed sleep phase disorder\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529067,\n \"choiceText\": \"Narcolepsy\",\n \"correct\": true,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\",\n \"displayOrder\": 1,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 490073,\n \"questionText\": \"On the basis of these findings only, what is the most likely diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\"\n },\n {\n \"authors\": \"Timothy D. Murphy, MD\",\n \"content\": [\n \"This case illustrates some of the challenges facing clinicians who care for a \\\"sleepy child.\\\" In the evolution of this child's care, multiple diagnoses were made and treated. The failure of her symptoms to respond to treatment resulted in further evaluation (and reevaluation of the data), which finally led to the diagnosis (narcolepsy with cataplexy) and her ultimate improvement and stabilization.\",\n \"Hypersomnolence may be primary or it may be secondary to a poor night's sleep. The most common conditions seen in a pediatric sleep clinic that might lead to daytime sleepiness include sleep apnea, behavioral insomnia of childhood, restless sleeping (or, when more extreme, pediatric RLS), and delayed sleep phase disorder (DSPD). The latter is much more common in teenagers, with a prevalence of up to 7% in this age group.[3] However, youths with daytime hypersomnolence due to DSPD do not typically fall asleep easily at bedtime, as this patient did. Moreover, DSPD is unusual in an 8-year-old.\",\n \"An insufficient quantity of sleep can usually be diagnosed on the basis of the history alone, but actigraphy is occasionally used when the history does not exclude difficulty in falling asleep or a circadian rhythm sleep-wake disorder.[4] Actigraphy was not included in this patient's workup.\",\n \"Pediatric RLS is primarily diagnosed on the basis of history, but the use of strict criteria (which include that the child \\\"relates a description in his or her own words\\\" of leg discomfort) may lead to missing the diagnosis in children who can benefit from treatment but are unable to verbalize their feelings. Suboptimal levels of serum ferritin are associated with restless sleep in children, as is improvement with iron therapy. The use of dopaminergic medications typically requires a higher standard for the diagnosis of RLS and a failure to respond to iron therapy.[5,6] Published data regarding autism and attention-deficit/hyperactivity disorder (ADHD) increasingly suggest complex links between iron metabolism and brain function, including during sleep.[7,8] This patient's movements in bed and her behavioral and learning struggles led to the investigation of her iron stores and ferritin levels and a trial of treatment for RLS.\",\n \"Hypersomnolence is associated with OSA more commonly in adults than in children. \\\"Hyperactivity\\\" or symptoms of ADHD are more frequently observed in children with OSA, although some sleepiness is still noted.[9] Most sleep centers consider an obstructive AHI of fewer than 1 event per hour (some use a threshold of 1.5) to be normal.[10] More pragmatically, the absolute score is useful in choosing a diagnostic billing code, but clinical decision-making also factors in the age of the patient and the severity of observed symptoms, considered formally or as a gestalt.[11]\",\n \"This patient had a positive AHI, which is diagnostic of OSA, and underwent adenotonsillectomy without significant improvement. She was also treated with iron and vitamin C, without significant changes in her daytime sleepiness or her apparent sleep quality. Furthermore, her clinical care was complicated by the MSLT result, which documented hypersomnolence but not narcolepsy.\",\n \"The diagnosis of narcolepsy was based primarily on clinical factors. Despite the positive AHI, snoring, leg movements, and low ferritin level, her condition did not improve after the adenotonsillectomy and iron therapy. As her case progressed, she developed more classic symptoms of cataplexy, such as feeling as if she would fall with laughter and falling asleep rapidly in conjunction with strong emotions. These findings, along with the rapid weight gain, pointed toward the diagnosis.\",\n \"Some confusion along the path toward a diagnosis is common in narcolepsy. Comorbidities, including PLMD, RLS, and OSA, may be found in association with narcolepsy and can delay the diagnosis,[12] as certainly happened in this patient.\",\n \"Narcolepsy affects about 1 in 2000 people. Two types are recognized: type 1 narcolepsy (previously referred to as narcolepsy with cataplexy) and type 2 narcolepsy (narcolepsy without cataplexy). Type 1 narcolepsy is considered an adult diagnosis by many pediatricians, but it frequently develops during adolescence, and onset after age 40 years is uncommon. Children may first present with a resumption of prolonged naps rather than prolonged nighttime sleep; nocturnal sleep is often somewhat disturbed initially. Cataplexy, multiple short naps during the day, hypnagogic hallucinations, and sleep-onset REM periods may be absent in young children, and repeated NPSGs and MSLTs over months to years may be required to make the diagnosis.\",\n \"Although a retrospective analysis of sleep histories often reveals hypersomnolence for years prior to the diagnosis, it can be easily missed in the first decade of life.[13] Type 1 narcolepsy is caused by the loss of orexin neuropeptides, which are mediators of central nervous system (CNS) control of energy metabolism and maintenance of sleep-wake states. Rapid weight gain and precocious puberty can occur in children with type 1 narcolepsy. This patient's rapid weight gain started to make more sense once the diagnosis was made.[14]\",\n \"In type 1 narcolepsy, the lack of consistent REM sleep at night leads to the intrusion of REM sleep features into the waking state. The diagnostic features include the tetrad of daytime sleepiness, cataplexy, hypnagogic hallucinations, and sleep paralysis. Specific questioning is usually required to elicit the history; only cataplexy is specific for narcolepsy. Patients often present initially with hypersomnolence alone, and other diagnostic findings may emerge over time.\",\n \"The etiology of narcolepsy is unclear. The lack of orexin may be related to autoimmune disease or infectious diseases. Most patients with type 1 narcolepsy have HLA DQB1 (0602 allele), the gene complex that encodes for proteins on the surface of T cells. Additionally, some infections (most notably H1N1 influenza, as well as some vaccines for it) are associated with clusters of type 1 narcolepsy and reduced orexin levels.[15,16,17] However, measurement of cerebrospinal fluid (CSF) levels of orexin is not required to make the diagnosis of narcolepsy.\",\n \"The diagnosis of type 1 narcolepsy can be clinically made in a child with a clear history of cataplexy, EDS, and an otherwise normal neurologic examination. In the absence of cataplexy, an NPSG followed by an MSLT can be used to make the diagnosis of narcolepsy. \\\"Secondary narcolepsy\\\" in the setting of CNS diseases such as hypothalamic tumors or arteriovenous malformations, following cerebrovascular accidents, or in association with multiple sclerosis or Niemann-Pick disease type C has been reported, but alternative causes of narcolepsy are vanishingly rare in childhood. The primary challenge is to rule out other sleep disorders causing the EDS; as in this patient, that may be difficult.\"\n ],\n \"date\": \"October 09, 2020\",\n \"figures\": [],\n \"markdown\": \"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\\n\\n **Authors:** Timothy D. Murphy, MD \\n **Date:** October 09, 2020\\n\\n ## Content\\n\\n This case illustrates some of the challenges facing clinicians who care for a \\\"sleepy child.\\\" In the evolution of this child's care, multiple diagnoses were made and treated. The failure of her symptoms to respond to treatment resulted in further evaluation (and reevaluation of the data), which finally led to the diagnosis (narcolepsy with cataplexy) and her ultimate improvement and stabilization.\\nHypersomnolence may be primary or it may be secondary to a poor night's sleep. The most common conditions seen in a pediatric sleep clinic that might lead to daytime sleepiness include sleep apnea, behavioral insomnia of childhood, restless sleeping (or, when more extreme, pediatric RLS), and delayed sleep phase disorder (DSPD). The latter is much more common in teenagers, with a prevalence of up to 7% in this age group.[3] However, youths with daytime hypersomnolence due to DSPD do not typically fall asleep easily at bedtime, as this patient did. Moreover, DSPD is unusual in an 8-year-old.\\nAn insufficient quantity of sleep can usually be diagnosed on the basis of the history alone, but actigraphy is occasionally used when the history does not exclude difficulty in falling asleep or a circadian rhythm sleep-wake disorder.[4] Actigraphy was not included in this patient's workup.\\nPediatric RLS is primarily diagnosed on the basis of history, but the use of strict criteria (which include that the child \\\"relates a description in his or her own words\\\" of leg discomfort) may lead to missing the diagnosis in children who can benefit from treatment but are unable to verbalize their feelings. Suboptimal levels of serum ferritin are associated with restless sleep in children, as is improvement with iron therapy. The use of dopaminergic medications typically requires a higher standard for the diagnosis of RLS and a failure to respond to iron therapy.[5,6] Published data regarding autism and attention-deficit/hyperactivity disorder (ADHD) increasingly suggest complex links between iron metabolism and brain function, including during sleep.[7,8] This patient's movements in bed and her behavioral and learning struggles led to the investigation of her iron stores and ferritin levels and a trial of treatment for RLS.\\nHypersomnolence is associated with OSA more commonly in adults than in children. \\\"Hyperactivity\\\" or symptoms of ADHD are more frequently observed in children with OSA, although some sleepiness is still noted.[9] Most sleep centers consider an obstructive AHI of fewer than 1 event per hour (some use a threshold of 1.5) to be normal.[10] More pragmatically, the absolute score is useful in choosing a diagnostic billing code, but clinical decision-making also factors in the age of the patient and the severity of observed symptoms, considered formally or as a gestalt.[11]\\nThis patient had a positive AHI, which is diagnostic of OSA, and underwent adenotonsillectomy without significant improvement. She was also treated with iron and vitamin C, without significant changes in her daytime sleepiness or her apparent sleep quality. Furthermore, her clinical care was complicated by the MSLT result, which documented hypersomnolence but not narcolepsy.\\nThe diagnosis of narcolepsy was based primarily on clinical factors. Despite the positive AHI, snoring, leg movements, and low ferritin level, her condition did not improve after the adenotonsillectomy and iron therapy. As her case progressed, she developed more classic symptoms of cataplexy, such as feeling as if she would fall with laughter and falling asleep rapidly in conjunction with strong emotions. These findings, along with the rapid weight gain, pointed toward the diagnosis.\\nSome confusion along the path toward a diagnosis is common in narcolepsy. Comorbidities, including PLMD, RLS, and OSA, may be found in association with narcolepsy and can delay the diagnosis,[12] as certainly happened in this patient.\\nNarcolepsy affects about 1 in 2000 people. Two types are recognized: type 1 narcolepsy (previously referred to as narcolepsy with cataplexy) and type 2 narcolepsy (narcolepsy without cataplexy). Type 1 narcolepsy is considered an adult diagnosis by many pediatricians, but it frequently develops during adolescence, and onset after age 40 years is uncommon. Children may first present with a resumption of prolonged naps rather than prolonged nighttime sleep; nocturnal sleep is often somewhat disturbed initially. Cataplexy, multiple short naps during the day, hypnagogic hallucinations, and sleep-onset REM periods may be absent in young children, and repeated NPSGs and MSLTs over months to years may be required to make the diagnosis.\\nAlthough a retrospective analysis of sleep histories often reveals hypersomnolence for years prior to the diagnosis, it can be easily missed in the first decade of life.[13] Type 1 narcolepsy is caused by the loss of orexin neuropeptides, which are mediators of central nervous system (CNS) control of energy metabolism and maintenance of sleep-wake states. Rapid weight gain and precocious puberty can occur in children with type 1 narcolepsy. This patient's rapid weight gain started to make more sense once the diagnosis was made.[14]\\nIn type 1 narcolepsy, the lack of consistent REM sleep at night leads to the intrusion of REM sleep features into the waking state. The diagnostic features include the tetrad of daytime sleepiness, cataplexy, hypnagogic hallucinations, and sleep paralysis. Specific questioning is usually required to elicit the history; only cataplexy is specific for narcolepsy. Patients often present initially with hypersomnolence alone, and other diagnostic findings may emerge over time.\\nThe etiology of narcolepsy is unclear. The lack of orexin may be related to autoimmune disease or infectious diseases. Most patients with type 1 narcolepsy have HLA DQB1 (0602 allele), the gene complex that encodes for proteins on the surface of T cells. Additionally, some infections (most notably H1N1 influenza, as well as some vaccines for it) are associated with clusters of type 1 narcolepsy and reduced orexin levels.[15,16,17] However, measurement of cerebrospinal fluid (CSF) levels of orexin is not required to make the diagnosis of narcolepsy.\\nThe diagnosis of type 1 narcolepsy can be clinically made in a child with a clear history of cataplexy, EDS, and an otherwise normal neurologic examination. In the absence of cataplexy, an NPSG followed by an MSLT can be used to make the diagnosis of narcolepsy. \\\"Secondary narcolepsy\\\" in the setting of CNS diseases such as hypothalamic tumors or arteriovenous malformations, following cerebrovascular accidents, or in association with multiple sclerosis or Niemann-Pick disease type C has been reported, but alternative causes of narcolepsy are vanishingly rare in childhood. The primary challenge is to rule out other sleep disorders causing the EDS; as in this patient, that may be difficult.\\n\\n ## Figures\\n\\n \\n*Page 4 of 6*\",\n \"pagination\": {\n \"current_page\": 4,\n \"total_pages\": 6\n },\n \"questionnaire\": [],\n \"title\": \"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\"\n },\n {\n \"authors\": \"Timothy D. Murphy, MD\",\n \"content\": [\n \"The treatment of narcolepsy focuses first on attempts to reduce the EDS pharmacologically; timed naps or increased time in bed is not usually sufficient to reduce the EDS. Although many medications have been used to treat EDS, clinicians typically start with caffeine (usually inadequate) and then move to stronger stimulants, such as methylphenidate or amphetamine and dextroamphetamine in combination.\",\n \"Failure of these agents might then lead to the use of modafinil (prescription without the failure of other therapies is often difficult). Monitoring of response and fairly frequent visits are required at this point. A selective serotonin reuptake inhibitor, such as fluoxetine, is often added to the regimen of patients with classic cataplexy. As was the case for this patient, the use of medications that might affect mood, attention, learning, and sleep requires close attention and collaboration between specialists in sleep medicine, neurology, and behavioral and general pediatrics.\",\n \"In some patients, including this patient, sodium oxybate (gamma-hydroxybutyrate [GHB]) is required to treat the cataplexy and to lead to better daytime functioning.[18] The exact mechanism of action is unknown, but the evening dosing of GHB is associated with improved REM sleep at night, perhaps relieving the intrusion of REM during daytime wake periods associated with type 1 narcolepsy. Unfortunately, GHB is associated with abuse — it is often called the \\\"date rape drug\\\" — and is now tightly regulated. Prescription in the United States is limited to one US pharmacy, and a sleep physician is typically required to obtain and use this medication.\",\n \"The finding of EDS requires exploration of nocturnal problems with sleep, including RLS, OSA, and behavioral insomnia that affects daytime functioning. Narcolepsy can be diagnosed as the cause of EDS on the basis of careful history-taking as well as the results of an NPSG and an MSLT.\"\n ],\n \"date\": \"October 09, 2020\",\n \"figures\": [],\n \"markdown\": \"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\\n\\n **Authors:** Timothy D. Murphy, MD \\n **Date:** October 09, 2020\\n\\n ## Content\\n\\n The treatment of narcolepsy focuses first on attempts to reduce the EDS pharmacologically; timed naps or increased time in bed is not usually sufficient to reduce the EDS. Although many medications have been used to treat EDS, clinicians typically start with caffeine (usually inadequate) and then move to stronger stimulants, such as methylphenidate or amphetamine and dextroamphetamine in combination.\\nFailure of these agents might then lead to the use of modafinil (prescription without the failure of other therapies is often difficult). Monitoring of response and fairly frequent visits are required at this point. A selective serotonin reuptake inhibitor, such as fluoxetine, is often added to the regimen of patients with classic cataplexy. As was the case for this patient, the use of medications that might affect mood, attention, learning, and sleep requires close attention and collaboration between specialists in sleep medicine, neurology, and behavioral and general pediatrics.\\nIn some patients, including this patient, sodium oxybate (gamma-hydroxybutyrate [GHB]) is required to treat the cataplexy and to lead to better daytime functioning.[18] The exact mechanism of action is unknown, but the evening dosing of GHB is associated with improved REM sleep at night, perhaps relieving the intrusion of REM during daytime wake periods associated with type 1 narcolepsy. Unfortunately, GHB is associated with abuse — it is often called the \\\"date rape drug\\\" — and is now tightly regulated. Prescription in the United States is limited to one US pharmacy, and a sleep physician is typically required to obtain and use this medication.\\nThe finding of EDS requires exploration of nocturnal problems with sleep, including RLS, OSA, and behavioral insomnia that affects daytime functioning. Narcolepsy can be diagnosed as the cause of EDS on the basis of careful history-taking as well as the results of an NPSG and an MSLT.\\n\\n ## Figures\\n\\n \\n*Page 5 of 6*\",\n \"pagination\": {\n \"current_page\": 5,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1529068,\n \"choiceText\": \"Narcolepsy without cataplexy (type 2 narcolepsy) is associated with increased orexin neuropeptide levels\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529069,\n \"choiceText\": \"Childhood narcolepsy is characterized by multiple brief naps during the day\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529070,\n \"choiceText\": \"Narcolepsy is associated with the loss of orexin neuropeptides\",\n \"correct\": true,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529071,\n \"choiceText\": \"Measurement of orexin levels in the CSF is required for the diagnosis of narcolepsy\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Levels of orexin neuropeptides in the CNS are reduced, not increased, in all forms of narcolepsy. Children more frequently present with prolonged daytime sleep, and multiple naps are typically seen in older patients. The diagnosis can be made by a careful history-taking that documents cataplexy, which is explained only by type 1 narcolepsy. Measurement of CSF levels of orexin is usually related to research only and typically is not used clinically in diagnosing narcolepsy.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 490074,\n \"questionText\": \"Which of the following is most accurate regarding narcolepsy in children?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1529072,\n \"choiceText\": \"Timed or planned naps to reduce sleep pressure, and amphetamine and dextroamphetamine for stimulant therapy during the day\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529073,\n \"choiceText\": \"Modafinil as a daytime stimulant, fluoxetine for cataplexy, and sodium oxybate to improve REM efficiency\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529074,\n \"choiceText\": \"Caffeine as a morning stimulant and sodium oxybate (gamma-hydroxybutyrate [GHB]) used at night to consolidate non-REM sleep\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529075,\n \"choiceText\": \"Methylphenidate to reduce cataplexy, fluoxetine to reduce depressive symptoms, and sodium oxybate to prolong REM latency\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Caffeine is usually an inadequate stimulant for patients with narcolepsy. The daytime use of methylphenidate or amphetamine and dextroamphetamine in combination does not adequately reduce cataplexy and does not address the problem with REM sleep at night. Modafinil is a more reliable daytime stimulant, and fluoxetine helps reduce cataplexy. The use of sodium oxybate in the evening in divided doses is intended to consolidate REM sleep and may reduce REM latency; non-REM sleep is not related to the daytime difficulties associated with narcolepsy.\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 490075,\n \"questionText\": \"Which of the following is typically required in the treatment of type 1 narcolepsy?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\"\n },\n {\n \"authors\": \"Timothy D. Murphy, MD\",\n \"content\": [],\n \"date\": \"October 09, 2020\",\n \"figures\": [],\n \"markdown\": \"# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\\n\\n **Authors:** Timothy D. Murphy, MD \\n **Date:** October 09, 2020\\n\\n ## Content\\n\\n \\n\\n ## Figures\\n\\n \\n*Page 6 of 6*\",\n \"pagination\": {\n \"current_page\": 6,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1529068,\n \"choiceText\": \"Narcolepsy without cataplexy (type 2 narcolepsy) is associated with increased orexin neuropeptide levels\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529069,\n \"choiceText\": \"Childhood narcolepsy is characterized by multiple brief naps during the day\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529070,\n \"choiceText\": \"Narcolepsy is associated with the loss of orexin neuropeptides\",\n \"correct\": true,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529071,\n \"choiceText\": \"Measurement of orexin levels in the CSF is required for the diagnosis of narcolepsy\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Levels of orexin neuropeptides in the CNS are reduced, not increased, in all forms of narcolepsy. Children more frequently present with prolonged daytime sleep, and multiple naps are typically seen in older patients. The diagnosis can be made by a careful history-taking that documents cataplexy, which is explained only by type 1 narcolepsy. Measurement of CSF levels of orexin is usually related to research only and typically is not used clinically in diagnosing narcolepsy.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 490074,\n \"questionText\": \"Which of the following is most accurate regarding narcolepsy in children?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1529072,\n \"choiceText\": \"Timed or planned naps to reduce sleep pressure, and amphetamine and dextroamphetamine for stimulant therapy during the day\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529073,\n \"choiceText\": \"Modafinil as a daytime stimulant, fluoxetine for cataplexy, and sodium oxybate to improve REM efficiency\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529074,\n \"choiceText\": \"Caffeine as a morning stimulant and sodium oxybate (gamma-hydroxybutyrate [GHB]) used at night to consolidate non-REM sleep\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529075,\n \"choiceText\": \"Methylphenidate to reduce cataplexy, fluoxetine to reduce depressive symptoms, and sodium oxybate to prolong REM latency\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Caffeine is usually an inadequate stimulant for patients with narcolepsy. The daytime use of methylphenidate or amphetamine and dextroamphetamine in combination does not adequately reduce cataplexy and does not address the problem with REM sleep at night. Modafinil is a more reliable daytime stimulant, and fluoxetine helps reduce cataplexy. The use of sodium oxybate in the evening in divided doses is intended to consolidate REM sleep and may reduce REM latency; non-REM sleep is not related to the daytime difficulties associated with narcolepsy.\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 490075,\n \"questionText\": \"Which of the following is typically required in the treatment of type 1 narcolepsy?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\"\n }\n]"},"questions":{"kind":"list like","value":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1529064,"choiceText":"Behavioral insomnia of childhood\r\n","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529065,"choiceText":"Pediatric chronic obstructive pulmonary disease","correct":false,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529066,"choiceText":"Delayed sleep phase disorder","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529067,"choiceText":"Narcolepsy","correct":true,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"","displayOrder":1,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":490073,"questionText":"On the basis of these findings only, what is the most likely diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1529068,"choiceText":"Narcolepsy without cataplexy (type 2 narcolepsy) is associated with increased orexin neuropeptide levels","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529069,"choiceText":"Childhood narcolepsy is characterized by multiple brief naps during the day","correct":false,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529070,"choiceText":"Narcolepsy is associated with the loss of orexin neuropeptides","correct":true,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529071,"choiceText":"Measurement of orexin levels in the CSF is required for the diagnosis of narcolepsy","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Levels of orexin neuropeptides in the CNS are reduced, not increased, in all forms of narcolepsy. Children more frequently present with prolonged daytime sleep, and multiple naps are typically seen in older patients. The diagnosis can be made by a careful history-taking that documents cataplexy, which is explained only by type 1 narcolepsy. Measurement of CSF levels of orexin is usually related to research only and typically is not used clinically in diagnosing narcolepsy.","displayOrder":2,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":490074,"questionText":"Which of the following is most accurate regarding narcolepsy in children?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1529072,"choiceText":"Timed or planned naps to reduce sleep pressure, and amphetamine and dextroamphetamine for stimulant therapy during the day\r\n","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529073,"choiceText":"Modafinil as a daytime stimulant, fluoxetine for cataplexy, and sodium oxybate to improve REM efficiency","correct":true,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529074,"choiceText":"Caffeine as a morning stimulant and sodium oxybate (gamma-hydroxybutyrate [GHB]) used at night to consolidate non-REM sleep","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1529075,"choiceText":"Methylphenidate to reduce cataplexy, fluoxetine to reduce depressive symptoms, and sodium oxybate to prolong REM latency","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Caffeine is usually an inadequate stimulant for patients with narcolepsy. The daytime use of methylphenidate or amphetamine and dextroamphetamine in combination does not adequately reduce cataplexy and does not address the problem with REM sleep at night. Modafinil is a more reliable daytime stimulant, and fluoxetine helps reduce cataplexy. The use of sodium oxybate in the evening in divided doses is intended to consolidate REM sleep and may reduce REM latency; non-REM sleep is not related to the daytime difficulties associated with narcolepsy.","displayOrder":3,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":490075,"questionText":"Which of the following is typically required in the treatment of type 1 narcolepsy?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"string":"[\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1529064,\n \"choiceText\": \"Behavioral insomnia of childhood\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529065,\n \"choiceText\": \"Pediatric chronic obstructive pulmonary disease\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529066,\n \"choiceText\": \"Delayed sleep phase disorder\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529067,\n \"choiceText\": \"Narcolepsy\",\n \"correct\": true,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\",\n \"displayOrder\": 1,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 490073,\n \"questionText\": \"On the basis of these findings only, what is the most likely diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1529068,\n \"choiceText\": \"Narcolepsy without cataplexy (type 2 narcolepsy) is associated with increased orexin neuropeptide levels\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529069,\n \"choiceText\": \"Childhood narcolepsy is characterized by multiple brief naps during the day\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529070,\n \"choiceText\": \"Narcolepsy is associated with the loss of orexin neuropeptides\",\n \"correct\": true,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529071,\n \"choiceText\": \"Measurement of orexin levels in the CSF is required for the diagnosis of narcolepsy\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Levels of orexin neuropeptides in the CNS are reduced, not increased, in all forms of narcolepsy. Children more frequently present with prolonged daytime sleep, and multiple naps are typically seen in older patients. The diagnosis can be made by a careful history-taking that documents cataplexy, which is explained only by type 1 narcolepsy. Measurement of CSF levels of orexin is usually related to research only and typically is not used clinically in diagnosing narcolepsy.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 490074,\n \"questionText\": \"Which of the following is most accurate regarding narcolepsy in children?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1529072,\n \"choiceText\": \"Timed or planned naps to reduce sleep pressure, and amphetamine and dextroamphetamine for stimulant therapy during the day\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529073,\n \"choiceText\": \"Modafinil as a daytime stimulant, fluoxetine for cataplexy, and sodium oxybate to improve REM efficiency\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529074,\n \"choiceText\": \"Caffeine as a morning stimulant and sodium oxybate (gamma-hydroxybutyrate [GHB]) used at night to consolidate non-REM sleep\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1529075,\n \"choiceText\": \"Methylphenidate to reduce cataplexy, fluoxetine to reduce depressive symptoms, and sodium oxybate to prolong REM latency\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Caffeine is usually an inadequate stimulant for patients with narcolepsy. The daytime use of methylphenidate or amphetamine and dextroamphetamine in combination does not adequately reduce cataplexy and does not address the problem with REM sleep at night. Modafinil is a more reliable daytime stimulant, and fluoxetine helps reduce cataplexy. The use of sodium oxybate in the evening in divided doses is intended to consolidate REM sleep and may reduce REM latency; non-REM sleep is not related to the daytime difficulties associated with narcolepsy.\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 490075,\n \"questionText\": \"Which of the following is typically required in the treatment of type 1 narcolepsy?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n]"}}},{"rowIdx":299,"cells":{"article_id":{"kind":"string","value":"904350"},"url":{"kind":"string","value":"/viewarticle/904350"},"article_data":{"kind":"list like","value":[{"authors":"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO","content":["Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.","A 49-year-old man with a significant medical history of alcohol abuse, tobacco dependence, and pancreatitis presents to the emergency department (ED) with abdominal pain that has lasted for 3 days. The abdominal pain has been intermittent, achy, and located in the periumbilical region. Associated symptoms have included nausea and vomiting, with several episodes of watery, brown diarrhea.","The patient reports a history of alcohol abuse, stating that he has ingested at least 1 pint a day since he was a teenager. He states that this pain feels different from the pain associated with his last bout of pancreatitis."],"date":"October 02, 2020","figures":[],"markdown":"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\n\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \n **Date:** October 02, 2020\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 49-year-old man with a significant medical history of alcohol abuse, tobacco dependence, and pancreatitis presents to the emergency department (ED) with abdominal pain that has lasted for 3 days. The abdominal pain has been intermittent, achy, and located in the periumbilical region. Associated symptoms have included nausea and vomiting, with several episodes of watery, brown diarrhea.\nThe patient reports a history of alcohol abuse, stating that he has ingested at least 1 pint a day since he was a teenager. He states that this pain feels different from the pain associated with his last bout of pancreatitis.\n\n ## Figures\n\n \n*Page 1 of 6*","pagination":{"current_page":1,"total_pages":6},"questionnaire":[],"title":"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old"},{"authors":"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO","content":["Upon arrival to the ED, the patient has a temperature of 97.9°F (36.6°C), a heart rate of 91 beats/min, a respiratory rate of 23 breaths/min, blood pressure of 113/85 mm Hg, and 98% saturation on room air.","Upon physical examination, he appears uncomfortable and is lying on his right side; he is slightly diaphoretic, with dry oral mucosa. Abdominal examination reveals a soft abdomen with apparent tenderness to palpation in the epigastric and periumbilical region, with minimal left upper-quadrant pain. His abdominal pain appears out of proportion to the physical examination findings.","His laboratory values are as follows:","White blood cell count: 13,000 cells/µL (reference range, 4,000-11,000 cells/µL)","Hemoglobin level: 14.1 g/dL (reference range, 13.5-17.5 g/dL)","Hematocrit: 39% (reference range, 41%-50%)","Platelet count: 506,000 cells/µL (reference range, 150,000-400,000 cells/µL)","Aspartate aminotransferase level: 126 U/L (reference range, 6-34 IU/L)","Alanine aminotransferase level: 81 U/L (reference range, 7-55 U/L)","Amylase level: 125 U/L (reference range, 30-110 U/L)","Lipase level: 419 U/L (reference range, 0-160 U/L)","Gamma glutamyltransferase level: 58 U/L (reference range, 8-38 U/L)","Lactate dehydrogenase level: 175 U/L (reference range, 140-280 U/L)","Lactic acid level: 0.7 mmol/L (reference range, 0.5-2.2 mmol/L)","Glucose level: 102 mg/dL (reference range, <100 mg/dL)","Rectal examination findings are negative for occult blood. All other laboratory values are unremarkable, including alcohol level. Subsequent CT of the abdomen/pelvis with intravenous contrast was performed (Figures 1-3).","Figure 1.","Figure 2.","Figure 3."],"date":"October 02, 2020","figures":[{"caption":"Figure 1.","image_url":"https://img.medscapestatic.com/article/904/350/904350-Thumb1.png"},{"caption":"Figure 2.","image_url":"https://img.medscapestatic.com/article/904/350/904350-Thumb2.png"},{"caption":"Figure 3.","image_url":"https://img.medscapestatic.com/article/904/350/904350-Thumb3.png"}],"markdown":"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\n\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \n **Date:** October 02, 2020\n\n ## Content\n\n Upon arrival to the ED, the patient has a temperature of 97.9°F (36.6°C), a heart rate of 91 beats/min, a respiratory rate of 23 breaths/min, blood pressure of 113/85 mm Hg, and 98% saturation on room air.\nUpon physical examination, he appears uncomfortable and is lying on his right side; he is slightly diaphoretic, with dry oral mucosa. Abdominal examination reveals a soft abdomen with apparent tenderness to palpation in the epigastric and periumbilical region, with minimal left upper-quadrant pain. His abdominal pain appears out of proportion to the physical examination findings.\nHis laboratory values are as follows:\nWhite blood cell count: 13,000 cells/µL (reference range, 4,000-11,000 cells/µL)\nHemoglobin level: 14.1 g/dL (reference range, 13.5-17.5 g/dL)\nHematocrit: 39% (reference range, 41%-50%)\nPlatelet count: 506,000 cells/µL (reference range, 150,000-400,000 cells/µL)\nAspartate aminotransferase level: 126 U/L (reference range, 6-34 IU/L)\nAlanine aminotransferase level: 81 U/L (reference range, 7-55 U/L)\nAmylase level: 125 U/L (reference range, 30-110 U/L)\nLipase level: 419 U/L (reference range, 0-160 U/L)\nGamma glutamyltransferase level: 58 U/L (reference range, 8-38 U/L)\nLactate dehydrogenase level: 175 U/L (reference range, 140-280 U/L)\nLactic acid level: 0.7 mmol/L (reference range, 0.5-2.2 mmol/L)\nGlucose level: 102 mg/dL (reference range, <100 mg/dL)\nRectal examination findings are negative for occult blood. All other laboratory values are unremarkable, including alcohol level. Subsequent CT of the abdomen/pelvis with intravenous contrast was performed (Figures 1-3).\nFigure 1.\nFigure 2.\nFigure 3.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n\n*Page 2 of 6*","pagination":{"current_page":2,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1281940,"choiceText":"Splenic vein thrombosis","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281942,"choiceText":"Superior mesenteric vein thrombosis","correct":true,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281944,"choiceText":"Mesenteric arterial thrombosis","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281946,"choiceText":"Septic pylephlebitis\r\n","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"","displayOrder":1,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":408509,"questionText":"Based only on these findings, which of the following is the most likely diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old"},{"authors":"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO","content":["Acute mesenteric vein thrombosis (MVT) is a rare but extremely important cause of mesenteric intestinal ischemia. In this patient, CT of the abdomen/pelvis with intravenous contrast revealed a filling defect that was consistent with acute thrombosis within the superior mesenteric vein (SMV), which extends approximately 3 cm cephalad to the portosplenic confluence. Other associated findings on these images included peripancreatic fat stranding and peripancreatic fluid consistent with acute pancreatitis (Figures 1-3).","Figure 1.","Figure 2.","Figure 3.","Pancreatitis results in a vast spectrum of both arterial and venous complications. The vascular complications involved in pancreatitis are major causes of morbidity and mortality. The venous complications result from thrombosis of the splenic vein and, less commonly, the portal vein and the SMV, as seen in the patient in this case. Prompt recognition is of paramount importance and requires a high index of clinical suspicion because aggressive therapy and anticoagulation can limit progression of the potential devastating consequences.","Patients with acute pancreatitis can present with portal vein thrombosis, splenic vein thrombosis, or (less commonly) superior MVT. Clinical research has shown that an isolated venous thrombosis to only the SMV, without simultaneous involvement of either the portal vein or the splenic vein, is rare. This vascular complication is important because of the increased risk for mesenteric ischemia and bowel infarction if not recognized.[1]","MVT is considered a rare condition, with only 1 case per 5000-15000 inpatient admissions per year; it accounts for roughly 6%-9% of all cases of acute mesenteric ischemia.[2] In a systematic review of 3692 patients from 1966 to 2002, MVT was the cause of acute mesenteric ischemia in about 3% of patients.[3]"],"date":"October 02, 2020","figures":[{"caption":"Figure 1.","image_url":"https://img.medscapestatic.com/article/904/350/904350-Thumb1.png"},{"caption":"Figure 2.","image_url":"https://img.medscapestatic.com/article/904/350/904350-Thumb2.png"},{"caption":"Figure 3.","image_url":"https://img.medscapestatic.com/article/904/350/904350-Thumb3.png"}],"markdown":"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\n\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \n **Date:** October 02, 2020\n\n ## Content\n\n Acute mesenteric vein thrombosis (MVT) is a rare but extremely important cause of mesenteric intestinal ischemia. In this patient, CT of the abdomen/pelvis with intravenous contrast revealed a filling defect that was consistent with acute thrombosis within the superior mesenteric vein (SMV), which extends approximately 3 cm cephalad to the portosplenic confluence. Other associated findings on these images included peripancreatic fat stranding and peripancreatic fluid consistent with acute pancreatitis (Figures 1-3).\nFigure 1.\nFigure 2.\nFigure 3.\nPancreatitis results in a vast spectrum of both arterial and venous complications. The vascular complications involved in pancreatitis are major causes of morbidity and mortality. The venous complications result from thrombosis of the splenic vein and, less commonly, the portal vein and the SMV, as seen in the patient in this case. Prompt recognition is of paramount importance and requires a high index of clinical suspicion because aggressive therapy and anticoagulation can limit progression of the potential devastating consequences.\nPatients with acute pancreatitis can present with portal vein thrombosis, splenic vein thrombosis, or (less commonly) superior MVT. Clinical research has shown that an isolated venous thrombosis to only the SMV, without simultaneous involvement of either the portal vein or the splenic vein, is rare. This vascular complication is important because of the increased risk for mesenteric ischemia and bowel infarction if not recognized.[1]\nMVT is considered a rare condition, with only 1 case per 5000-15000 inpatient admissions per year; it accounts for roughly 6%-9% of all cases of acute mesenteric ischemia.[2] In a systematic review of 3692 patients from 1966 to 2002, MVT was the cause of acute mesenteric ischemia in about 3% of patients.[3]\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n\n*Page 3 of 6*","pagination":{"current_page":3,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1281940,"choiceText":"Splenic vein thrombosis","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281942,"choiceText":"Superior mesenteric vein thrombosis","correct":true,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281944,"choiceText":"Mesenteric arterial thrombosis","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281946,"choiceText":"Septic pylephlebitis\r\n","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"","displayOrder":1,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":408509,"questionText":"Based only on these findings, which of the following is the most likely diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old"},{"authors":"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO","content":["Many risk factors for MVT are recognized, including direct injury (eg, abdominal trauma, splenectomy, intra-abdominal inflammatory processes), venous congestion/stasis (eg, congestive heart failure, portal hypertension, cirrhosis), and hypercoagulable conditions (eg, protein C/S deficiency, antithrombin III deficiency, factor V Leiden mutation, pancreatic/colon carcinoma, oral contraceptive use, polycythemia vera, heparin-induced thrombocytopenia, lupus anticoagulant/anti-phospholipid syndrome).[4] In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.[5]","Acute occlusion of the mesenteric vein results in increased resistance within the mesenteric venous bed, leading to decreased perfusion pressure.[3] As flow stagnates in the mesenteric vein, increased venous pressure results in an efflux of fluid into the tissues, leading to bowel-wall edema. If the clinical progression continues, venous return from the bowel wall is completely occluded, and the end result is bowel ischemia.[3] Integrity of the bowel mucosa is lost and bacteria can translocate, leading to lactic acidosis, sepsis, multiorgan failure, and eventually death.[2]","MVT can occur acutely, subacutely, or chronically. The clinical features vary, depending on the location of the thrombus within the splanchnic vasculature.[3] Acute MVT, similar to other forms of acute mesenteric ischemia, presents most often as a colicky periumbilical pain that is often out of proportion to the physical examination findings. However, the onset of venous thrombosis, compared with arterial thrombosis, is often less sudden and dull, with as many as 75% of patients presenting after 2 days of abdominal pain.[3]","Alternatively, chronic mesenteric venous thrombosis often presents with portal hypertension and variceal hemorrhage.[2] In general, peritoneal signs are absent, unless the venous thrombosis goes untreated and the bowel becomes ischemic, in which case peritoneal signs develop.","In a retrospective study, 31 patients diagnosed with MVT from 1985-1999 were reviewed.[4] Approximately 84% of patients presented with abdominal pain, with 16% presenting with peritoneal signs. Common overall symptoms included diarrhea (42%), nausea and vomiting (32%), lower gastrointestinal bleeding (19%), fatigue (16%), and upper gastrointestinal bleeding (10%). Furthermore, only 22 patients were initially treated with heparin. Five patients were found to have peritonitis and underwent exploratory laparotomy, with the ultimate goal to prevent or limit gangrenous bowel, with an additional five patients later undergoing surgery for the development of ischemic bowel. Seven of the 31 patients died within 30 days, secondary to complications from infarcted bowel and multisystemic organ failure. Overall, 19 of the 24 survivors were treated with long-term anticoagulation, with 88% of those surviving long-term.","Differentiating between ischemia secondary to MVT and ischemia secondary to a mesenteric arterial thrombosis is important. MVT presents in the setting of thrombophilia or an inflammatory abdominal process, whereas mesenteric arterial ischemia presents in the setting of cardiac disease, low-flow states, and atrial fibrillation.[1] Similar to all forms of mesenteric ischemia, no clinical features are specific to MVT. As such, a clinician must have a high index of suspicion in order to make an early diagnosis and avoid the complications of an undiagnosed MVT."],"date":"October 02, 2020","figures":[],"markdown":"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\n\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \n **Date:** October 02, 2020\n\n ## Content\n\n Many risk factors for MVT are recognized, including direct injury (eg, abdominal trauma, splenectomy, intra-abdominal inflammatory processes), venous congestion/stasis (eg, congestive heart failure, portal hypertension, cirrhosis), and hypercoagulable conditions (eg, protein C/S deficiency, antithrombin III deficiency, factor V Leiden mutation, pancreatic/colon carcinoma, oral contraceptive use, polycythemia vera, heparin-induced thrombocytopenia, lupus anticoagulant/anti-phospholipid syndrome).[4] In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.[5]\nAcute occlusion of the mesenteric vein results in increased resistance within the mesenteric venous bed, leading to decreased perfusion pressure.[3] As flow stagnates in the mesenteric vein, increased venous pressure results in an efflux of fluid into the tissues, leading to bowel-wall edema. If the clinical progression continues, venous return from the bowel wall is completely occluded, and the end result is bowel ischemia.[3] Integrity of the bowel mucosa is lost and bacteria can translocate, leading to lactic acidosis, sepsis, multiorgan failure, and eventually death.[2]\nMVT can occur acutely, subacutely, or chronically. The clinical features vary, depending on the location of the thrombus within the splanchnic vasculature.[3] Acute MVT, similar to other forms of acute mesenteric ischemia, presents most often as a colicky periumbilical pain that is often out of proportion to the physical examination findings. However, the onset of venous thrombosis, compared with arterial thrombosis, is often less sudden and dull, with as many as 75% of patients presenting after 2 days of abdominal pain.[3]\nAlternatively, chronic mesenteric venous thrombosis often presents with portal hypertension and variceal hemorrhage.[2] In general, peritoneal signs are absent, unless the venous thrombosis goes untreated and the bowel becomes ischemic, in which case peritoneal signs develop.\nIn a retrospective study, 31 patients diagnosed with MVT from 1985-1999 were reviewed.[4] Approximately 84% of patients presented with abdominal pain, with 16% presenting with peritoneal signs. Common overall symptoms included diarrhea (42%), nausea and vomiting (32%), lower gastrointestinal bleeding (19%), fatigue (16%), and upper gastrointestinal bleeding (10%). Furthermore, only 22 patients were initially treated with heparin. Five patients were found to have peritonitis and underwent exploratory laparotomy, with the ultimate goal to prevent or limit gangrenous bowel, with an additional five patients later undergoing surgery for the development of ischemic bowel. Seven of the 31 patients died within 30 days, secondary to complications from infarcted bowel and multisystemic organ failure. Overall, 19 of the 24 survivors were treated with long-term anticoagulation, with 88% of those surviving long-term.\nDifferentiating between ischemia secondary to MVT and ischemia secondary to a mesenteric arterial thrombosis is important. MVT presents in the setting of thrombophilia or an inflammatory abdominal process, whereas mesenteric arterial ischemia presents in the setting of cardiac disease, low-flow states, and atrial fibrillation.[1] Similar to all forms of mesenteric ischemia, no clinical features are specific to MVT. As such, a clinician must have a high index of suspicion in order to make an early diagnosis and avoid the complications of an undiagnosed MVT.\n\n ## Figures\n\n \n*Page 4 of 6*","pagination":{"current_page":4,"total_pages":6},"questionnaire":[],"title":"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old"},{"authors":"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO","content":["Treatment for MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal exams. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence. If evidence of clinical deterioration and bowel infarction is present, surgical intervention is necessary. Broad-spectrum antibiotics are generally reserved for the setting of pylephlebitis, septic thrombophlebitis, and sepsis secondary to bacterial translocation from an infarcted bowel.[2]","Initiation of anticoagulation remains the cornerstone of treatment and should not be delayed.[6]Research has shown that once a patient is transitioned to oral anticoagulation, treatment should continue for 3-6 months, unless a thrombophilia has been diagnosed. After anticoagulation, most MVTs partially or completely recanalize, with one study showing recanalization in 80% of patients who received anticoagulation.[7] However, the recurrence rate has been reported at 15%.","Acute MVT carries a better prognosis than acute mesenteric ischemia. In one systematic review of nearly 3700 cases of acute mesenteric ischemia from 1966 to 2002, the mortality rate of those patients with MVT was 44%, compared with as much as 89% for those patients with advancement to mesenteric ischemia.[8] However, with increasing physician awareness, the use of contrast-enhanced CT to investigate abdominal pain in combination with anticoagulation has improved outcomes in these patients. In more modern studies, the mortality rate of acute MVT is down to 20%, with the most common cause of death being sepsis and multiorgan failure.[8]","In conclusion, acute superior MVT is a rare but important cause of mesenteric intestinal ischemia. It requires a high index of clinical suspicion. Rapid recognition and aggressive therapy are of extreme importance in order to prevent ischemic and infarcted bowel, sepsis, multiorgan failure, and eventual death. The 49-year-old man in this case had nonnecrotizing, alcohol-induced acute pancreatitis, complicated by acute superior MVT.","The patient in this case was eventually transitioned to rivaroxaban and discharged on day 4. Since his discharge, he has entered into alcohol rehabilitation and remains compliant with his anticoagulation."],"date":"October 02, 2020","figures":[],"markdown":"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\n\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \n **Date:** October 02, 2020\n\n ## Content\n\n Treatment for MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal exams. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence. If evidence of clinical deterioration and bowel infarction is present, surgical intervention is necessary. Broad-spectrum antibiotics are generally reserved for the setting of pylephlebitis, septic thrombophlebitis, and sepsis secondary to bacterial translocation from an infarcted bowel.[2]\nInitiation of anticoagulation remains the cornerstone of treatment and should not be delayed.[6]Research has shown that once a patient is transitioned to oral anticoagulation, treatment should continue for 3-6 months, unless a thrombophilia has been diagnosed. After anticoagulation, most MVTs partially or completely recanalize, with one study showing recanalization in 80% of patients who received anticoagulation.[7] However, the recurrence rate has been reported at 15%.\nAcute MVT carries a better prognosis than acute mesenteric ischemia. In one systematic review of nearly 3700 cases of acute mesenteric ischemia from 1966 to 2002, the mortality rate of those patients with MVT was 44%, compared with as much as 89% for those patients with advancement to mesenteric ischemia.[8] However, with increasing physician awareness, the use of contrast-enhanced CT to investigate abdominal pain in combination with anticoagulation has improved outcomes in these patients. In more modern studies, the mortality rate of acute MVT is down to 20%, with the most common cause of death being sepsis and multiorgan failure.[8]\nIn conclusion, acute superior MVT is a rare but important cause of mesenteric intestinal ischemia. It requires a high index of clinical suspicion. Rapid recognition and aggressive therapy are of extreme importance in order to prevent ischemic and infarcted bowel, sepsis, multiorgan failure, and eventual death. The 49-year-old man in this case had nonnecrotizing, alcohol-induced acute pancreatitis, complicated by acute superior MVT.\nThe patient in this case was eventually transitioned to rivaroxaban and discharged on day 4. Since his discharge, he has entered into alcohol rehabilitation and remains compliant with his anticoagulation.\n\n ## Figures\n\n \n*Page 5 of 6*","pagination":{"current_page":5,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1281948,"choiceText":"Pancreatic and inflammatory bowel disease","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281950,"choiceText":"Portal hypertension","correct":false,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281952,"choiceText":"Factor V Leiden mutation","correct":false,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281954,"choiceText":"Splenectomy","correct":false,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281956,"choiceText":"Gastric sleeve","correct":false,"displayOrder":5,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281958,"choiceText":"All of the above\r\n","correct":true,"displayOrder":6,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"MVT has many associated risk factors, including direct injury, venous congestive/stasis, and hypercoagulable conditions. The patient in this case had an extensive history of alcohol abuse and pancreatitis. In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.","displayOrder":2,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":408511,"questionText":"Which of the following is considered a risk factor for the development of MVT?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1281960,"choiceText":"Broad-spectrum antibiotic use is contraindicated at this point","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281962,"choiceText":"Surgical consultation is unnecessary at this point","correct":false,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281964,"choiceText":"Anticoagulation should be delayed until further investigation is done","correct":false,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281966,"choiceText":"Bowel rest and fluid resuscitation should be promptly initiated","correct":true,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Treatment of MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal examinations. In this particular case, the patient is septic and has evidence of an intra-abdominal source in the setting of SMV thrombosis. If evidence suggests clinical deterioration and bowel infarction, surgical intervention is necessary.
\r\n\r\nIn this case, the patient has voluntary guarding and an elevated lactic acid level, making an emergent surgical consult necessary. Broad-spectrum antibiotics are generally reserved for patients with pylephlebitis, those with septic thrombophlebitis, and those with sepsis secondary to bacterial translocation from an infarcted bowel.\r\n
\r\nInitiation of anticoagulation remains the cornerstone of treatment and should not be delayed. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence.\r\n","displayOrder":3,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":408513,"questionText":"A 53-year-old man with a significant medical history of pancreatitis presents to the ED with nausea, vomiting, and abdominal pain. His vital signs are notable for a heart rate of 113 beats/min, respiratory rate of 24 breaths/min, and a blood pressure of 96/50 mm Hg, with a temperature of 101.3°F (38.5°C). Abdominal examination reveals diffuse tenderness to palpation with voluntary guarding. Laboratory values are notable for a lactic acid level of 4.6 mmol/L, neutrophil-predominant leukocytosis of 19 × 109 cells/L, and a lipase level of 459 U/L. CT of the abdomen/pelvis reveals superior MVT. \r\n
\r\nWhich of the following is accurate regarding his treatment?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old"},{"authors":"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO","content":[],"date":"October 02, 2020","figures":[],"markdown":"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\n\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \n **Date:** October 02, 2020\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*","pagination":{"current_page":6,"total_pages":6},"questionnaire":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1281948,"choiceText":"Pancreatic and inflammatory bowel disease","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281950,"choiceText":"Portal hypertension","correct":false,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281952,"choiceText":"Factor V Leiden mutation","correct":false,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281954,"choiceText":"Splenectomy","correct":false,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281956,"choiceText":"Gastric sleeve","correct":false,"displayOrder":5,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281958,"choiceText":"All of the above\r\n","correct":true,"displayOrder":6,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"MVT has many associated risk factors, including direct injury, venous congestive/stasis, and hypercoagulable conditions. The patient in this case had an extensive history of alcohol abuse and pancreatitis. In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.","displayOrder":2,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":408511,"questionText":"Which of the following is considered a risk factor for the development of MVT?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1281960,"choiceText":"Broad-spectrum antibiotic use is contraindicated at this point","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281962,"choiceText":"Surgical consultation is unnecessary at this point","correct":false,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281964,"choiceText":"Anticoagulation should be delayed until further investigation is done","correct":false,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281966,"choiceText":"Bowel rest and fluid resuscitation should be promptly initiated","correct":true,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Treatment of MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal examinations. In this particular case, the patient is septic and has evidence of an intra-abdominal source in the setting of SMV thrombosis. If evidence suggests clinical deterioration and bowel infarction, surgical intervention is necessary.
\r\n\r\nIn this case, the patient has voluntary guarding and an elevated lactic acid level, making an emergent surgical consult necessary. Broad-spectrum antibiotics are generally reserved for patients with pylephlebitis, those with septic thrombophlebitis, and those with sepsis secondary to bacterial translocation from an infarcted bowel.\r\n
\r\nInitiation of anticoagulation remains the cornerstone of treatment and should not be delayed. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence.\r\n","displayOrder":3,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":408513,"questionText":"A 53-year-old man with a significant medical history of pancreatitis presents to the ED with nausea, vomiting, and abdominal pain. His vital signs are notable for a heart rate of 113 beats/min, respiratory rate of 24 breaths/min, and a blood pressure of 96/50 mm Hg, with a temperature of 101.3°F (38.5°C). Abdominal examination reveals diffuse tenderness to palpation with voluntary guarding. Laboratory values are notable for a lactic acid level of 4.6 mmol/L, neutrophil-predominant leukocytosis of 19 × 109 cells/L, and a lipase level of 459 U/L. CT of the abdomen/pelvis reveals superior MVT. \r\n
\r\nWhich of the following is accurate regarding his treatment?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"title":"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old"}],"string":"[\n {\n \"authors\": \"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO\",\n \"content\": [\n \"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\",\n \"A 49-year-old man with a significant medical history of alcohol abuse, tobacco dependence, and pancreatitis presents to the emergency department (ED) with abdominal pain that has lasted for 3 days. The abdominal pain has been intermittent, achy, and located in the periumbilical region. Associated symptoms have included nausea and vomiting, with several episodes of watery, brown diarrhea.\",\n \"The patient reports a history of alcohol abuse, stating that he has ingested at least 1 pint a day since he was a teenager. He states that this pain feels different from the pain associated with his last bout of pancreatitis.\"\n ],\n \"date\": \"October 02, 2020\",\n \"figures\": [],\n \"markdown\": \"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\\n\\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \\n **Date:** October 02, 2020\\n\\n ## Content\\n\\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\\nA 49-year-old man with a significant medical history of alcohol abuse, tobacco dependence, and pancreatitis presents to the emergency department (ED) with abdominal pain that has lasted for 3 days. The abdominal pain has been intermittent, achy, and located in the periumbilical region. Associated symptoms have included nausea and vomiting, with several episodes of watery, brown diarrhea.\\nThe patient reports a history of alcohol abuse, stating that he has ingested at least 1 pint a day since he was a teenager. He states that this pain feels different from the pain associated with his last bout of pancreatitis.\\n\\n ## Figures\\n\\n \\n*Page 1 of 6*\",\n \"pagination\": {\n \"current_page\": 1,\n \"total_pages\": 6\n },\n \"questionnaire\": [],\n \"title\": \"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\"\n },\n {\n \"authors\": \"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO\",\n \"content\": [\n \"Upon arrival to the ED, the patient has a temperature of 97.9°F (36.6°C), a heart rate of 91 beats/min, a respiratory rate of 23 breaths/min, blood pressure of 113/85 mm Hg, and 98% saturation on room air.\",\n \"Upon physical examination, he appears uncomfortable and is lying on his right side; he is slightly diaphoretic, with dry oral mucosa. Abdominal examination reveals a soft abdomen with apparent tenderness to palpation in the epigastric and periumbilical region, with minimal left upper-quadrant pain. His abdominal pain appears out of proportion to the physical examination findings.\",\n \"His laboratory values are as follows:\",\n \"White blood cell count: 13,000 cells/µL (reference range, 4,000-11,000 cells/µL)\",\n \"Hemoglobin level: 14.1 g/dL (reference range, 13.5-17.5 g/dL)\",\n \"Hematocrit: 39% (reference range, 41%-50%)\",\n \"Platelet count: 506,000 cells/µL (reference range, 150,000-400,000 cells/µL)\",\n \"Aspartate aminotransferase level: 126 U/L (reference range, 6-34 IU/L)\",\n \"Alanine aminotransferase level: 81 U/L (reference range, 7-55 U/L)\",\n \"Amylase level: 125 U/L (reference range, 30-110 U/L)\",\n \"Lipase level: 419 U/L (reference range, 0-160 U/L)\",\n \"Gamma glutamyltransferase level: 58 U/L (reference range, 8-38 U/L)\",\n \"Lactate dehydrogenase level: 175 U/L (reference range, 140-280 U/L)\",\n \"Lactic acid level: 0.7 mmol/L (reference range, 0.5-2.2 mmol/L)\",\n \"Glucose level: 102 mg/dL (reference range, <100 mg/dL)\",\n \"Rectal examination findings are negative for occult blood. All other laboratory values are unremarkable, including alcohol level. Subsequent CT of the abdomen/pelvis with intravenous contrast was performed (Figures 1-3).\",\n \"Figure 1.\",\n \"Figure 2.\",\n \"Figure 3.\"\n ],\n \"date\": \"October 02, 2020\",\n \"figures\": [\n {\n \"caption\": \"Figure 1.\",\n \"image_url\": \"https://img.medscapestatic.com/article/904/350/904350-Thumb1.png\"\n },\n {\n \"caption\": \"Figure 2.\",\n \"image_url\": \"https://img.medscapestatic.com/article/904/350/904350-Thumb2.png\"\n },\n {\n \"caption\": \"Figure 3.\",\n \"image_url\": \"https://img.medscapestatic.com/article/904/350/904350-Thumb3.png\"\n }\n ],\n \"markdown\": \"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\\n\\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \\n **Date:** October 02, 2020\\n\\n ## Content\\n\\n Upon arrival to the ED, the patient has a temperature of 97.9°F (36.6°C), a heart rate of 91 beats/min, a respiratory rate of 23 breaths/min, blood pressure of 113/85 mm Hg, and 98% saturation on room air.\\nUpon physical examination, he appears uncomfortable and is lying on his right side; he is slightly diaphoretic, with dry oral mucosa. Abdominal examination reveals a soft abdomen with apparent tenderness to palpation in the epigastric and periumbilical region, with minimal left upper-quadrant pain. His abdominal pain appears out of proportion to the physical examination findings.\\nHis laboratory values are as follows:\\nWhite blood cell count: 13,000 cells/µL (reference range, 4,000-11,000 cells/µL)\\nHemoglobin level: 14.1 g/dL (reference range, 13.5-17.5 g/dL)\\nHematocrit: 39% (reference range, 41%-50%)\\nPlatelet count: 506,000 cells/µL (reference range, 150,000-400,000 cells/µL)\\nAspartate aminotransferase level: 126 U/L (reference range, 6-34 IU/L)\\nAlanine aminotransferase level: 81 U/L (reference range, 7-55 U/L)\\nAmylase level: 125 U/L (reference range, 30-110 U/L)\\nLipase level: 419 U/L (reference range, 0-160 U/L)\\nGamma glutamyltransferase level: 58 U/L (reference range, 8-38 U/L)\\nLactate dehydrogenase level: 175 U/L (reference range, 140-280 U/L)\\nLactic acid level: 0.7 mmol/L (reference range, 0.5-2.2 mmol/L)\\nGlucose level: 102 mg/dL (reference range, <100 mg/dL)\\nRectal examination findings are negative for occult blood. All other laboratory values are unremarkable, including alcohol level. Subsequent CT of the abdomen/pelvis with intravenous contrast was performed (Figures 1-3).\\nFigure 1.\\nFigure 2.\\nFigure 3.\\n\\n ## Figures\\n\\n **Figure 1.** \\n \\n\\n**Figure 2.** \\n \\n\\n**Figure 3.** \\n \\n\\n\\n*Page 2 of 6*\",\n \"pagination\": {\n \"current_page\": 2,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1281940,\n \"choiceText\": \"Splenic vein thrombosis\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281942,\n \"choiceText\": \"Superior mesenteric vein thrombosis\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281944,\n \"choiceText\": \"Mesenteric arterial thrombosis\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281946,\n \"choiceText\": \"Septic pylephlebitis\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\",\n \"displayOrder\": 1,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 408509,\n \"questionText\": \"Based only on these findings, which of the following is the most likely diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\"\n },\n {\n \"authors\": \"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO\",\n \"content\": [\n \"Acute mesenteric vein thrombosis (MVT) is a rare but extremely important cause of mesenteric intestinal ischemia. In this patient, CT of the abdomen/pelvis with intravenous contrast revealed a filling defect that was consistent with acute thrombosis within the superior mesenteric vein (SMV), which extends approximately 3 cm cephalad to the portosplenic confluence. Other associated findings on these images included peripancreatic fat stranding and peripancreatic fluid consistent with acute pancreatitis (Figures 1-3).\",\n \"Figure 1.\",\n \"Figure 2.\",\n \"Figure 3.\",\n \"Pancreatitis results in a vast spectrum of both arterial and venous complications. The vascular complications involved in pancreatitis are major causes of morbidity and mortality. The venous complications result from thrombosis of the splenic vein and, less commonly, the portal vein and the SMV, as seen in the patient in this case. Prompt recognition is of paramount importance and requires a high index of clinical suspicion because aggressive therapy and anticoagulation can limit progression of the potential devastating consequences.\",\n \"Patients with acute pancreatitis can present with portal vein thrombosis, splenic vein thrombosis, or (less commonly) superior MVT. Clinical research has shown that an isolated venous thrombosis to only the SMV, without simultaneous involvement of either the portal vein or the splenic vein, is rare. This vascular complication is important because of the increased risk for mesenteric ischemia and bowel infarction if not recognized.[1]\",\n \"MVT is considered a rare condition, with only 1 case per 5000-15000 inpatient admissions per year; it accounts for roughly 6%-9% of all cases of acute mesenteric ischemia.[2] In a systematic review of 3692 patients from 1966 to 2002, MVT was the cause of acute mesenteric ischemia in about 3% of patients.[3]\"\n ],\n \"date\": \"October 02, 2020\",\n \"figures\": [\n {\n \"caption\": \"Figure 1.\",\n \"image_url\": \"https://img.medscapestatic.com/article/904/350/904350-Thumb1.png\"\n },\n {\n \"caption\": \"Figure 2.\",\n \"image_url\": \"https://img.medscapestatic.com/article/904/350/904350-Thumb2.png\"\n },\n {\n \"caption\": \"Figure 3.\",\n \"image_url\": \"https://img.medscapestatic.com/article/904/350/904350-Thumb3.png\"\n }\n ],\n \"markdown\": \"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\\n\\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \\n **Date:** October 02, 2020\\n\\n ## Content\\n\\n Acute mesenteric vein thrombosis (MVT) is a rare but extremely important cause of mesenteric intestinal ischemia. In this patient, CT of the abdomen/pelvis with intravenous contrast revealed a filling defect that was consistent with acute thrombosis within the superior mesenteric vein (SMV), which extends approximately 3 cm cephalad to the portosplenic confluence. Other associated findings on these images included peripancreatic fat stranding and peripancreatic fluid consistent with acute pancreatitis (Figures 1-3).\\nFigure 1.\\nFigure 2.\\nFigure 3.\\nPancreatitis results in a vast spectrum of both arterial and venous complications. The vascular complications involved in pancreatitis are major causes of morbidity and mortality. The venous complications result from thrombosis of the splenic vein and, less commonly, the portal vein and the SMV, as seen in the patient in this case. Prompt recognition is of paramount importance and requires a high index of clinical suspicion because aggressive therapy and anticoagulation can limit progression of the potential devastating consequences.\\nPatients with acute pancreatitis can present with portal vein thrombosis, splenic vein thrombosis, or (less commonly) superior MVT. Clinical research has shown that an isolated venous thrombosis to only the SMV, without simultaneous involvement of either the portal vein or the splenic vein, is rare. This vascular complication is important because of the increased risk for mesenteric ischemia and bowel infarction if not recognized.[1]\\nMVT is considered a rare condition, with only 1 case per 5000-15000 inpatient admissions per year; it accounts for roughly 6%-9% of all cases of acute mesenteric ischemia.[2] In a systematic review of 3692 patients from 1966 to 2002, MVT was the cause of acute mesenteric ischemia in about 3% of patients.[3]\\n\\n ## Figures\\n\\n **Figure 1.** \\n \\n\\n**Figure 2.** \\n \\n\\n**Figure 3.** \\n \\n\\n\\n*Page 3 of 6*\",\n \"pagination\": {\n \"current_page\": 3,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1281940,\n \"choiceText\": \"Splenic vein thrombosis\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281942,\n \"choiceText\": \"Superior mesenteric vein thrombosis\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281944,\n \"choiceText\": \"Mesenteric arterial thrombosis\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281946,\n \"choiceText\": \"Septic pylephlebitis\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\",\n \"displayOrder\": 1,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 408509,\n \"questionText\": \"Based only on these findings, which of the following is the most likely diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\"\n },\n {\n \"authors\": \"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO\",\n \"content\": [\n \"Many risk factors for MVT are recognized, including direct injury (eg, abdominal trauma, splenectomy, intra-abdominal inflammatory processes), venous congestion/stasis (eg, congestive heart failure, portal hypertension, cirrhosis), and hypercoagulable conditions (eg, protein C/S deficiency, antithrombin III deficiency, factor V Leiden mutation, pancreatic/colon carcinoma, oral contraceptive use, polycythemia vera, heparin-induced thrombocytopenia, lupus anticoagulant/anti-phospholipid syndrome).[4] In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.[5]\",\n \"Acute occlusion of the mesenteric vein results in increased resistance within the mesenteric venous bed, leading to decreased perfusion pressure.[3] As flow stagnates in the mesenteric vein, increased venous pressure results in an efflux of fluid into the tissues, leading to bowel-wall edema. If the clinical progression continues, venous return from the bowel wall is completely occluded, and the end result is bowel ischemia.[3] Integrity of the bowel mucosa is lost and bacteria can translocate, leading to lactic acidosis, sepsis, multiorgan failure, and eventually death.[2]\",\n \"MVT can occur acutely, subacutely, or chronically. The clinical features vary, depending on the location of the thrombus within the splanchnic vasculature.[3] Acute MVT, similar to other forms of acute mesenteric ischemia, presents most often as a colicky periumbilical pain that is often out of proportion to the physical examination findings. However, the onset of venous thrombosis, compared with arterial thrombosis, is often less sudden and dull, with as many as 75% of patients presenting after 2 days of abdominal pain.[3]\",\n \"Alternatively, chronic mesenteric venous thrombosis often presents with portal hypertension and variceal hemorrhage.[2] In general, peritoneal signs are absent, unless the venous thrombosis goes untreated and the bowel becomes ischemic, in which case peritoneal signs develop.\",\n \"In a retrospective study, 31 patients diagnosed with MVT from 1985-1999 were reviewed.[4] Approximately 84% of patients presented with abdominal pain, with 16% presenting with peritoneal signs. Common overall symptoms included diarrhea (42%), nausea and vomiting (32%), lower gastrointestinal bleeding (19%), fatigue (16%), and upper gastrointestinal bleeding (10%). Furthermore, only 22 patients were initially treated with heparin. Five patients were found to have peritonitis and underwent exploratory laparotomy, with the ultimate goal to prevent or limit gangrenous bowel, with an additional five patients later undergoing surgery for the development of ischemic bowel. Seven of the 31 patients died within 30 days, secondary to complications from infarcted bowel and multisystemic organ failure. Overall, 19 of the 24 survivors were treated with long-term anticoagulation, with 88% of those surviving long-term.\",\n \"Differentiating between ischemia secondary to MVT and ischemia secondary to a mesenteric arterial thrombosis is important. MVT presents in the setting of thrombophilia or an inflammatory abdominal process, whereas mesenteric arterial ischemia presents in the setting of cardiac disease, low-flow states, and atrial fibrillation.[1] Similar to all forms of mesenteric ischemia, no clinical features are specific to MVT. As such, a clinician must have a high index of suspicion in order to make an early diagnosis and avoid the complications of an undiagnosed MVT.\"\n ],\n \"date\": \"October 02, 2020\",\n \"figures\": [],\n \"markdown\": \"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\\n\\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \\n **Date:** October 02, 2020\\n\\n ## Content\\n\\n Many risk factors for MVT are recognized, including direct injury (eg, abdominal trauma, splenectomy, intra-abdominal inflammatory processes), venous congestion/stasis (eg, congestive heart failure, portal hypertension, cirrhosis), and hypercoagulable conditions (eg, protein C/S deficiency, antithrombin III deficiency, factor V Leiden mutation, pancreatic/colon carcinoma, oral contraceptive use, polycythemia vera, heparin-induced thrombocytopenia, lupus anticoagulant/anti-phospholipid syndrome).[4] In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.[5]\\nAcute occlusion of the mesenteric vein results in increased resistance within the mesenteric venous bed, leading to decreased perfusion pressure.[3] As flow stagnates in the mesenteric vein, increased venous pressure results in an efflux of fluid into the tissues, leading to bowel-wall edema. If the clinical progression continues, venous return from the bowel wall is completely occluded, and the end result is bowel ischemia.[3] Integrity of the bowel mucosa is lost and bacteria can translocate, leading to lactic acidosis, sepsis, multiorgan failure, and eventually death.[2]\\nMVT can occur acutely, subacutely, or chronically. The clinical features vary, depending on the location of the thrombus within the splanchnic vasculature.[3] Acute MVT, similar to other forms of acute mesenteric ischemia, presents most often as a colicky periumbilical pain that is often out of proportion to the physical examination findings. However, the onset of venous thrombosis, compared with arterial thrombosis, is often less sudden and dull, with as many as 75% of patients presenting after 2 days of abdominal pain.[3]\\nAlternatively, chronic mesenteric venous thrombosis often presents with portal hypertension and variceal hemorrhage.[2] In general, peritoneal signs are absent, unless the venous thrombosis goes untreated and the bowel becomes ischemic, in which case peritoneal signs develop.\\nIn a retrospective study, 31 patients diagnosed with MVT from 1985-1999 were reviewed.[4] Approximately 84% of patients presented with abdominal pain, with 16% presenting with peritoneal signs. Common overall symptoms included diarrhea (42%), nausea and vomiting (32%), lower gastrointestinal bleeding (19%), fatigue (16%), and upper gastrointestinal bleeding (10%). Furthermore, only 22 patients were initially treated with heparin. Five patients were found to have peritonitis and underwent exploratory laparotomy, with the ultimate goal to prevent or limit gangrenous bowel, with an additional five patients later undergoing surgery for the development of ischemic bowel. Seven of the 31 patients died within 30 days, secondary to complications from infarcted bowel and multisystemic organ failure. Overall, 19 of the 24 survivors were treated with long-term anticoagulation, with 88% of those surviving long-term.\\nDifferentiating between ischemia secondary to MVT and ischemia secondary to a mesenteric arterial thrombosis is important. MVT presents in the setting of thrombophilia or an inflammatory abdominal process, whereas mesenteric arterial ischemia presents in the setting of cardiac disease, low-flow states, and atrial fibrillation.[1] Similar to all forms of mesenteric ischemia, no clinical features are specific to MVT. As such, a clinician must have a high index of suspicion in order to make an early diagnosis and avoid the complications of an undiagnosed MVT.\\n\\n ## Figures\\n\\n \\n*Page 4 of 6*\",\n \"pagination\": {\n \"current_page\": 4,\n \"total_pages\": 6\n },\n \"questionnaire\": [],\n \"title\": \"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\"\n },\n {\n \"authors\": \"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO\",\n \"content\": [\n \"Treatment for MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal exams. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence. If evidence of clinical deterioration and bowel infarction is present, surgical intervention is necessary. Broad-spectrum antibiotics are generally reserved for the setting of pylephlebitis, septic thrombophlebitis, and sepsis secondary to bacterial translocation from an infarcted bowel.[2]\",\n \"Initiation of anticoagulation remains the cornerstone of treatment and should not be delayed.[6]Research has shown that once a patient is transitioned to oral anticoagulation, treatment should continue for 3-6 months, unless a thrombophilia has been diagnosed. After anticoagulation, most MVTs partially or completely recanalize, with one study showing recanalization in 80% of patients who received anticoagulation.[7] However, the recurrence rate has been reported at 15%.\",\n \"Acute MVT carries a better prognosis than acute mesenteric ischemia. In one systematic review of nearly 3700 cases of acute mesenteric ischemia from 1966 to 2002, the mortality rate of those patients with MVT was 44%, compared with as much as 89% for those patients with advancement to mesenteric ischemia.[8] However, with increasing physician awareness, the use of contrast-enhanced CT to investigate abdominal pain in combination with anticoagulation has improved outcomes in these patients. In more modern studies, the mortality rate of acute MVT is down to 20%, with the most common cause of death being sepsis and multiorgan failure.[8]\",\n \"In conclusion, acute superior MVT is a rare but important cause of mesenteric intestinal ischemia. It requires a high index of clinical suspicion. Rapid recognition and aggressive therapy are of extreme importance in order to prevent ischemic and infarcted bowel, sepsis, multiorgan failure, and eventual death. The 49-year-old man in this case had nonnecrotizing, alcohol-induced acute pancreatitis, complicated by acute superior MVT.\",\n \"The patient in this case was eventually transitioned to rivaroxaban and discharged on day 4. Since his discharge, he has entered into alcohol rehabilitation and remains compliant with his anticoagulation.\"\n ],\n \"date\": \"October 02, 2020\",\n \"figures\": [],\n \"markdown\": \"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\\n\\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \\n **Date:** October 02, 2020\\n\\n ## Content\\n\\n Treatment for MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal exams. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence. If evidence of clinical deterioration and bowel infarction is present, surgical intervention is necessary. Broad-spectrum antibiotics are generally reserved for the setting of pylephlebitis, septic thrombophlebitis, and sepsis secondary to bacterial translocation from an infarcted bowel.[2]\\nInitiation of anticoagulation remains the cornerstone of treatment and should not be delayed.[6]Research has shown that once a patient is transitioned to oral anticoagulation, treatment should continue for 3-6 months, unless a thrombophilia has been diagnosed. After anticoagulation, most MVTs partially or completely recanalize, with one study showing recanalization in 80% of patients who received anticoagulation.[7] However, the recurrence rate has been reported at 15%.\\nAcute MVT carries a better prognosis than acute mesenteric ischemia. In one systematic review of nearly 3700 cases of acute mesenteric ischemia from 1966 to 2002, the mortality rate of those patients with MVT was 44%, compared with as much as 89% for those patients with advancement to mesenteric ischemia.[8] However, with increasing physician awareness, the use of contrast-enhanced CT to investigate abdominal pain in combination with anticoagulation has improved outcomes in these patients. In more modern studies, the mortality rate of acute MVT is down to 20%, with the most common cause of death being sepsis and multiorgan failure.[8]\\nIn conclusion, acute superior MVT is a rare but important cause of mesenteric intestinal ischemia. It requires a high index of clinical suspicion. Rapid recognition and aggressive therapy are of extreme importance in order to prevent ischemic and infarcted bowel, sepsis, multiorgan failure, and eventual death. The 49-year-old man in this case had nonnecrotizing, alcohol-induced acute pancreatitis, complicated by acute superior MVT.\\nThe patient in this case was eventually transitioned to rivaroxaban and discharged on day 4. Since his discharge, he has entered into alcohol rehabilitation and remains compliant with his anticoagulation.\\n\\n ## Figures\\n\\n \\n*Page 5 of 6*\",\n \"pagination\": {\n \"current_page\": 5,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1281948,\n \"choiceText\": \"Pancreatic and inflammatory bowel disease\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281950,\n \"choiceText\": \"Portal hypertension\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281952,\n \"choiceText\": \"Factor V Leiden mutation\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281954,\n \"choiceText\": \"Splenectomy\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281956,\n \"choiceText\": \"Gastric sleeve\",\n \"correct\": false,\n \"displayOrder\": 5,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281958,\n \"choiceText\": \"All of the above\\r\\n\",\n \"correct\": true,\n \"displayOrder\": 6,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"MVT has many associated risk factors, including direct injury, venous congestive/stasis, and hypercoagulable conditions. The patient in this case had an extensive history of alcohol abuse and pancreatitis. In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 408511,\n \"questionText\": \"Which of the following is considered a risk factor for the development of MVT?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1281960,\n \"choiceText\": \"Broad-spectrum antibiotic use is contraindicated at this point\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281962,\n \"choiceText\": \"Surgical consultation is unnecessary at this point\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281964,\n \"choiceText\": \"Anticoagulation should be delayed until further investigation is done\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281966,\n \"choiceText\": \"Bowel rest and fluid resuscitation should be promptly initiated\",\n \"correct\": true,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Treatment of MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal examinations. In this particular case, the patient is septic and has evidence of an intra-abdominal source in the setting of SMV thrombosis. If evidence suggests clinical deterioration and bowel infarction, surgical intervention is necessary.
\\r\\n\\r\\nIn this case, the patient has voluntary guarding and an elevated lactic acid level, making an emergent surgical consult necessary. Broad-spectrum antibiotics are generally reserved for patients with pylephlebitis, those with septic thrombophlebitis, and those with sepsis secondary to bacterial translocation from an infarcted bowel.\\r\\n
\\r\\nInitiation of anticoagulation remains the cornerstone of treatment and should not be delayed. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence.\\r\\n\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 408513,\n \"questionText\": \"A 53-year-old man with a significant medical history of pancreatitis presents to the ED with nausea, vomiting, and abdominal pain. His vital signs are notable for a heart rate of 113 beats/min, respiratory rate of 24 breaths/min, and a blood pressure of 96/50 mm Hg, with a temperature of 101.3°F (38.5°C). Abdominal examination reveals diffuse tenderness to palpation with voluntary guarding. Laboratory values are notable for a lactic acid level of 4.6 mmol/L, neutrophil-predominant leukocytosis of 19 × 109 cells/L, and a lipase level of 459 U/L. CT of the abdomen/pelvis reveals superior MVT. \\r\\n
\\r\\nWhich of the following is accurate regarding his treatment?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\"\n },\n {\n \"authors\": \"Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO\",\n \"content\": [],\n \"date\": \"October 02, 2020\",\n \"figures\": [],\n \"markdown\": \"# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\\n\\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \\n **Date:** October 02, 2020\\n\\n ## Content\\n\\n \\n\\n ## Figures\\n\\n \\n*Page 6 of 6*\",\n \"pagination\": {\n \"current_page\": 6,\n \"total_pages\": 6\n },\n \"questionnaire\": [\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1281948,\n \"choiceText\": \"Pancreatic and inflammatory bowel disease\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281950,\n \"choiceText\": \"Portal hypertension\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281952,\n \"choiceText\": \"Factor V Leiden mutation\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281954,\n \"choiceText\": \"Splenectomy\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281956,\n \"choiceText\": \"Gastric sleeve\",\n \"correct\": false,\n \"displayOrder\": 5,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281958,\n \"choiceText\": \"All of the above\\r\\n\",\n \"correct\": true,\n \"displayOrder\": 6,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"MVT has many associated risk factors, including direct injury, venous congestive/stasis, and hypercoagulable conditions. The patient in this case had an extensive history of alcohol abuse and pancreatitis. In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 408511,\n \"questionText\": \"Which of the following is considered a risk factor for the development of MVT?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1281960,\n \"choiceText\": \"Broad-spectrum antibiotic use is contraindicated at this point\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281962,\n \"choiceText\": \"Surgical consultation is unnecessary at this point\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281964,\n \"choiceText\": \"Anticoagulation should be delayed until further investigation is done\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281966,\n \"choiceText\": \"Bowel rest and fluid resuscitation should be promptly initiated\",\n \"correct\": true,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Treatment of MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal examinations. In this particular case, the patient is septic and has evidence of an intra-abdominal source in the setting of SMV thrombosis. If evidence suggests clinical deterioration and bowel infarction, surgical intervention is necessary.
\\r\\n\\r\\nIn this case, the patient has voluntary guarding and an elevated lactic acid level, making an emergent surgical consult necessary. Broad-spectrum antibiotics are generally reserved for patients with pylephlebitis, those with septic thrombophlebitis, and those with sepsis secondary to bacterial translocation from an infarcted bowel.\\r\\n
\\r\\nInitiation of anticoagulation remains the cornerstone of treatment and should not be delayed. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence.\\r\\n\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 408513,\n \"questionText\": \"A 53-year-old man with a significant medical history of pancreatitis presents to the ED with nausea, vomiting, and abdominal pain. His vital signs are notable for a heart rate of 113 beats/min, respiratory rate of 24 breaths/min, and a blood pressure of 96/50 mm Hg, with a temperature of 101.3°F (38.5°C). Abdominal examination reveals diffuse tenderness to palpation with voluntary guarding. Laboratory values are notable for a lactic acid level of 4.6 mmol/L, neutrophil-predominant leukocytosis of 19 × 109 cells/L, and a lipase level of 459 U/L. CT of the abdomen/pelvis reveals superior MVT. \\r\\n
\\r\\nWhich of the following is accurate regarding his treatment?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n ],\n \"title\": \"Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\"\n }\n]"},"questions":{"kind":"list like","value":[{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1281940,"choiceText":"Splenic vein thrombosis","correct":false,"displayOrder":1,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281942,"choiceText":"Superior mesenteric vein thrombosis","correct":true,"displayOrder":2,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281944,"choiceText":"Mesenteric arterial thrombosis","correct":false,"displayOrder":3,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281946,"choiceText":"Septic pylephlebitis\r\n","correct":false,"displayOrder":4,"explanation":"","hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"","displayOrder":1,"displayType":1,"horizontal":false,"introduction":"","matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":408509,"questionText":"Based only on these findings, which of the following is the most likely diagnosis?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1281948,"choiceText":"Pancreatic and inflammatory bowel disease","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281950,"choiceText":"Portal hypertension","correct":false,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281952,"choiceText":"Factor V Leiden mutation","correct":false,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281954,"choiceText":"Splenectomy","correct":false,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281956,"choiceText":"Gastric sleeve","correct":false,"displayOrder":5,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281958,"choiceText":"All of the above\r\n","correct":true,"displayOrder":6,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"MVT has many associated risk factors, including direct injury, venous congestive/stasis, and hypercoagulable conditions. The patient in this case had an extensive history of alcohol abuse and pancreatitis. In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.","displayOrder":2,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":408511,"questionText":"Which of the following is considered a risk factor for the development of MVT?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false},{"answered":false,"answeredCorrectly":false,"branch":false,"choices":[{"branchPath":null,"choiceId":1281960,"choiceText":"Broad-spectrum antibiotic use is contraindicated at this point","correct":false,"displayOrder":1,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281962,"choiceText":"Surgical consultation is unnecessary at this point","correct":false,"displayOrder":2,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281964,"choiceText":"Anticoagulation should be delayed until further investigation is done","correct":false,"displayOrder":3,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"},{"branchPath":null,"choiceId":1281966,"choiceText":"Bowel rest and fluid resuscitation should be promptly initiated","correct":true,"displayOrder":4,"explanation":null,"hideLabel":false,"selected":false,"totalAbsoluteResponseCount":0,"totalResponses":"0"}],"discussion":"Treatment of MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal examinations. In this particular case, the patient is septic and has evidence of an intra-abdominal source in the setting of SMV thrombosis. If evidence suggests clinical deterioration and bowel infarction, surgical intervention is necessary.
\r\n\r\nIn this case, the patient has voluntary guarding and an elevated lactic acid level, making an emergent surgical consult necessary. Broad-spectrum antibiotics are generally reserved for patients with pylephlebitis, those with septic thrombophlebitis, and those with sepsis secondary to bacterial translocation from an infarcted bowel.\r\n
\r\nInitiation of anticoagulation remains the cornerstone of treatment and should not be delayed. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence.\r\n","displayOrder":3,"displayType":1,"horizontal":false,"introduction":null,"matrixQuestions":[],"mutuallyExclusive":false,"poll":true,"professions":[],"questionId":408513,"questionText":"A 53-year-old man with a significant medical history of pancreatitis presents to the ED with nausea, vomiting, and abdominal pain. His vital signs are notable for a heart rate of 113 beats/min, respiratory rate of 24 breaths/min, and a blood pressure of 96/50 mm Hg, with a temperature of 101.3°F (38.5°C). Abdominal examination reveals diffuse tenderness to palpation with voluntary guarding. Laboratory values are notable for a lactic acid level of 4.6 mmol/L, neutrophil-predominant leukocytosis of 19 × 109 cells/L, and a lipase level of 459 U/L. CT of the abdomen/pelvis reveals superior MVT. \r\n
\r\nWhich of the following is accurate regarding his treatment?","questionTypeId":1,"required":false,"responseText":null,"score":false,"showAnsTable":true,"showQuestion":true,"showResult":true,"specialties":[],"totalResponses":0,"viewResults":false}],"string":"[\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1281940,\n \"choiceText\": \"Splenic vein thrombosis\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281942,\n \"choiceText\": \"Superior mesenteric vein thrombosis\",\n \"correct\": true,\n \"displayOrder\": 2,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281944,\n \"choiceText\": \"Mesenteric arterial thrombosis\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281946,\n \"choiceText\": \"Septic pylephlebitis\\r\\n\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": \"\",\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"\",\n \"displayOrder\": 1,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": \"\",\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 408509,\n \"questionText\": \"Based only on these findings, which of the following is the most likely diagnosis?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1281948,\n \"choiceText\": \"Pancreatic and inflammatory bowel disease\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281950,\n \"choiceText\": \"Portal hypertension\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281952,\n \"choiceText\": \"Factor V Leiden mutation\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281954,\n \"choiceText\": \"Splenectomy\",\n \"correct\": false,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281956,\n \"choiceText\": \"Gastric sleeve\",\n \"correct\": false,\n \"displayOrder\": 5,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281958,\n \"choiceText\": \"All of the above\\r\\n\",\n \"correct\": true,\n \"displayOrder\": 6,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"MVT has many associated risk factors, including direct injury, venous congestive/stasis, and hypercoagulable conditions. The patient in this case had an extensive history of alcohol abuse and pancreatitis. In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.\",\n \"displayOrder\": 2,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 408511,\n \"questionText\": \"Which of the following is considered a risk factor for the development of MVT?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n },\n {\n \"answered\": false,\n \"answeredCorrectly\": false,\n \"branch\": false,\n \"choices\": [\n {\n \"branchPath\": null,\n \"choiceId\": 1281960,\n \"choiceText\": \"Broad-spectrum antibiotic use is contraindicated at this point\",\n \"correct\": false,\n \"displayOrder\": 1,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281962,\n \"choiceText\": \"Surgical consultation is unnecessary at this point\",\n \"correct\": false,\n \"displayOrder\": 2,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281964,\n \"choiceText\": \"Anticoagulation should be delayed until further investigation is done\",\n \"correct\": false,\n \"displayOrder\": 3,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n },\n {\n \"branchPath\": null,\n \"choiceId\": 1281966,\n \"choiceText\": \"Bowel rest and fluid resuscitation should be promptly initiated\",\n \"correct\": true,\n \"displayOrder\": 4,\n \"explanation\": null,\n \"hideLabel\": false,\n \"selected\": false,\n \"totalAbsoluteResponseCount\": 0,\n \"totalResponses\": \"0\"\n }\n ],\n \"discussion\": \"Treatment of MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal examinations. In this particular case, the patient is septic and has evidence of an intra-abdominal source in the setting of SMV thrombosis. If evidence suggests clinical deterioration and bowel infarction, surgical intervention is necessary.
\\r\\n\\r\\nIn this case, the patient has voluntary guarding and an elevated lactic acid level, making an emergent surgical consult necessary. Broad-spectrum antibiotics are generally reserved for patients with pylephlebitis, those with septic thrombophlebitis, and those with sepsis secondary to bacterial translocation from an infarcted bowel.\\r\\n
\\r\\nInitiation of anticoagulation remains the cornerstone of treatment and should not be delayed. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence.\\r\\n\",\n \"displayOrder\": 3,\n \"displayType\": 1,\n \"horizontal\": false,\n \"introduction\": null,\n \"matrixQuestions\": [],\n \"mutuallyExclusive\": false,\n \"poll\": true,\n \"professions\": [],\n \"questionId\": 408513,\n \"questionText\": \"A 53-year-old man with a significant medical history of pancreatitis presents to the ED with nausea, vomiting, and abdominal pain. His vital signs are notable for a heart rate of 113 beats/min, respiratory rate of 24 breaths/min, and a blood pressure of 96/50 mm Hg, with a temperature of 101.3°F (38.5°C). Abdominal examination reveals diffuse tenderness to palpation with voluntary guarding. Laboratory values are notable for a lactic acid level of 4.6 mmol/L, neutrophil-predominant leukocytosis of 19 × 109 cells/L, and a lipase level of 459 U/L. CT of the abdomen/pelvis reveals superior MVT. \\r\\n
\\r\\nWhich of the following is accurate regarding his treatment?\",\n \"questionTypeId\": 1,\n \"required\": false,\n \"responseText\": null,\n \"score\": false,\n \"showAnsTable\": true,\n \"showQuestion\": true,\n \"showResult\": true,\n \"specialties\": [],\n \"totalResponses\": 0,\n \"viewResults\": false\n }\n]"}}}],"truncated":false,"partial":false},"paginationData":{"pageIndex":2,"numItemsPerPage":100,"numTotalItems":508,"offset":200,"length":100}},"jwt":"eyJhbGciOiJFZERTQSJ9.eyJyZWFkIjp0cnVlLCJwZXJtaXNzaW9ucyI6eyJyZXBvLmNvbnRlbnQucmVhZCI6dHJ1ZX0sImlhdCI6MTc0NjQyMzU3OSwic3ViIjoiL2RhdGFzZXRzL2hsbGovbWVkc2NhcGUiLCJleHAiOjE3NDY0MjcxNzksImlzcyI6Imh0dHBzOi8vaHVnZ2luZ2ZhY2UuY28ifQ.sinwUiCqQrlj8AQMez_vGuBfK6e-N0uXfATqAeB2npmIes5b-ZDMbCSY11kWjYUhJ2YG13BYU-Vl85sUvFmMCQ","displayUrls":true},"discussionsStats":{"closed":0,"open":1,"total":1},"fullWidth":true,"hasGatedAccess":true,"hasFullAccess":true,"isEmbedded":false,"savedQueries":{"community":[],"user":[]}}">
article_id
stringlengths 6
7
| url
stringlengths 19
20
| article_data
listlengths 1
7
| questions
listlengths 0
5
|
|---|---|---|---|
743272 | /viewarticle/743272 | [
{
"authors": "Linda A. Dultz, MD, MPH; Karina L. Vivar; Suzanne MacFarland; MaryAnn Hopkins, MD, MPhil",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to recognize accurately. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 38-year-old woman presents with a 2-year history of an abdominal wall mass that has recently enlarged in size. She reports unusual sensations of soreness and pain in her abdomen associated with the mass. The symptoms are predominantly premenstrual and have progressed to the point of debilitation. She has not noticed any other masses or lesions on her body. Three years prior to presentation, the patient began experiencing menorrhagia and dysmenorrhea.",
"The patient's gynecologic history is significant for menarche at age 10 years, an elective abortion at age 18 years, and an ectopic pregnancy treated by left salpingectomy at age 25 years. She has never taken hormonal contraception. She underwent ovarian stimulation and uterine preparation for in vitro fertilization (IVF) at age 25 years. The patient received leuprolide prior to ovarian stimulation; she also received progesterone to ameliorate menopausal symptoms associated with leuprolide. Ovarian stimulation was achieved and was followed by successful egg retrieval. The patient later had 4 transvaginal IVF embryo transfers, resulting in 3 pregnancies and 4 children. Her first 2 children were born via normal spontaneous vaginal deliveries when the patient was aged 26 years and 28 years. At age 30 years, she gave birth to twins, one via normal spontaneous vaginal delivery and the other via cesarean delivery because of failure to progress. No unusual findings were noted at the time of cesarean delivery.",
"The patient has had no other surgeries. She has no other significant medical history. She does not have any allergies and, at presentation, she is not on any medications. She has not had any recent weight loss, fevers, or chills."
],
"date": "January 17, 2023",
"figures": [],
"markdown": "# A Mother of Four With Menstruation Issues and Debilitating Pain\n\n **Authors:** Linda A. Dultz, MD, MPH; Karina L. Vivar; Suzanne MacFarland; MaryAnn Hopkins, MD, MPhil \n **Date:** January 17, 2023\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to recognize accurately. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 38-year-old woman presents with a 2-year history of an abdominal wall mass that has recently enlarged in size. She reports unusual sensations of soreness and pain in her abdomen associated with the mass. The symptoms are predominantly premenstrual and have progressed to the point of debilitation. She has not noticed any other masses or lesions on her body. Three years prior to presentation, the patient began experiencing menorrhagia and dysmenorrhea.\nThe patient's gynecologic history is significant for menarche at age 10 years, an elective abortion at age 18 years, and an ectopic pregnancy treated by left salpingectomy at age 25 years. She has never taken hormonal contraception. She underwent ovarian stimulation and uterine preparation for in vitro fertilization (IVF) at age 25 years. The patient received leuprolide prior to ovarian stimulation; she also received progesterone to ameliorate menopausal symptoms associated with leuprolide. Ovarian stimulation was achieved and was followed by successful egg retrieval. The patient later had 4 transvaginal IVF embryo transfers, resulting in 3 pregnancies and 4 children. Her first 2 children were born via normal spontaneous vaginal deliveries when the patient was aged 26 years and 28 years. At age 30 years, she gave birth to twins, one via normal spontaneous vaginal delivery and the other via cesarean delivery because of failure to progress. No unusual findings were noted at the time of cesarean delivery.\nThe patient has had no other surgeries. She has no other significant medical history. She does not have any allergies and, at presentation, she is not on any medications. She has not had any recent weight loss, fevers, or chills.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A Mother of Four With Menstruation Issues and Debilitating Pain"
},
{
"authors": "Linda A. Dultz, MD, MPH; Karina L. Vivar; Suzanne MacFarland; MaryAnn Hopkins, MD, MPhil",
"content": [
"Upon initial examination, her temperature is 97.6°F (36.4°C), blood pressure is 126/83 mm Hg, heart rate is 67 beats/min, respiratory rate is 12 breaths/min, and oxygen saturation is 99% on room air. She has a firm, nonmobile, nonpulsatile, ill-defined, tender mass palpated to the left of her umbilicus. The mass is remote from her prior surgical incisions. The remainder of her examination, including the pelvic examination, is unremarkable.",
"The preoperative laboratory findings are within normal limits. An MRI demonstrates a 3.2 × 2.4 × 1.8 cm mass within the left abdominal rectus muscle, which deforms the posterior rectus fascia. The radiologic features are interpreted as being most compatible with abdominal wall fibromatosis. The patient is offered surgical excision. Intraoperatively, the mass is excised from within the musculature of the rectus without disturbing the posterior rectus fascia. Grossly, the mass is found to be 3.7 × 3.3 × 1.4 cm and composed of tan-yellow, soft, lobular, fibrous adipose tissue. Histologic sections are shown (Figures 1 and 2).",
"Figure 1.",
"Figure 2."
],
"date": "January 17, 2023",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/742/478/742478-thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/742/478/742478-thumb2.png"
}
],
"markdown": "# A Mother of Four With Menstruation Issues and Debilitating Pain\n\n **Authors:** Linda A. Dultz, MD, MPH; Karina L. Vivar; Suzanne MacFarland; MaryAnn Hopkins, MD, MPhil \n **Date:** January 17, 2023\n\n ## Content\n\n Upon initial examination, her temperature is 97.6°F (36.4°C), blood pressure is 126/83 mm Hg, heart rate is 67 beats/min, respiratory rate is 12 breaths/min, and oxygen saturation is 99% on room air. She has a firm, nonmobile, nonpulsatile, ill-defined, tender mass palpated to the left of her umbilicus. The mass is remote from her prior surgical incisions. The remainder of her examination, including the pelvic examination, is unremarkable.\nThe preoperative laboratory findings are within normal limits. An MRI demonstrates a 3.2 × 2.4 × 1.8 cm mass within the left abdominal rectus muscle, which deforms the posterior rectus fascia. The radiologic features are interpreted as being most compatible with abdominal wall fibromatosis. The patient is offered surgical excision. Intraoperatively, the mass is excised from within the musculature of the rectus without disturbing the posterior rectus fascia. Grossly, the mass is found to be 3.7 × 3.3 × 1.4 cm and composed of tan-yellow, soft, lobular, fibrous adipose tissue. Histologic sections are shown (Figures 1 and 2).\nFigure 1.\nFigure 2.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 407467,
"choiceText": "Desmoid tumor\r\n",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407468,
"choiceText": "Lipoma",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407469,
"choiceText": "Endometriosis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407470,
"choiceText": "Synovial sarcoma",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 119298,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Mother of Four With Menstruation Issues and Debilitating Pain"
},
{
"authors": "Linda A. Dultz, MD, MPH; Karina L. Vivar; Suzanne MacFarland; MaryAnn Hopkins, MD, MPhil",
"content": [
"The diagnosis of endometriosis was confirmed by histology of the surgical specimen and was consistent with the patient’s clinical history of premenstrual pain exacerbation. The histologic sections showed irregular endometrial glands and stroma interspersed within muscular and other soft tissue (Figure 1). The glands were lined by columnar epithelium surrounded by endometrial stromal tissue. Evidence of hemorrhage and hemosiderin-laden macrophages were observed, consistent with menstrual cycle changes (Figure 2).",
"Figure 1.",
"Figure 2.",
"The presence of cholesterol clefts and giant cells also suggested past hemorrhage. The glandular tissue was estrogen-receptor positive, further supporting a uterine endometrial origin. The diagnosis of endometriosis was made on the basis of the typical histologic appearance.",
"First described in 1860, endometriosis continues to be a benign but debilitating disease that burdens millions of women each year. It is a chronic gynecologic disorder whose principal manifestations are chronic pain and infertility. Pelvic endometriosis is the presence of endometrial glands and stromal tissue outside of the uterine cavity but confined to the pelvis. Extrapelvic endometriosis refers to endometrial tissue found anywhere in the body outside of the pelvic cavity.[1,2] Although the pathophysiology of endometriosis is poorly understood, several theories have been proposed.",
"The first and best supported is the implantation theory, which suggests that endometrial tissue passes through the fallopian tubes in a retrograde fashion to attach and proliferate at ectopic sites in the peritoneal cavity. This theory has been observed in menstruating females during laparoscopic surgery, as well as in animal models mimicking retrograde flow. These studies have not only demonstrated retrograde flow, but they support the idea that sloughed endometrial cells can reimplant and survive outside the pelvic cavity.[3]",
"A second proposed theory is the direct extension theory, which states that endometriosis results from direct invasion of ectopic endometrium through the uterine musculature. However, studies have thus far failed to show a connection between direct invasion and ectopic endometrial implants.[3] A third theory, the lymphatic/vascular metastases theory, suggests that endometrial cells can metastasize through lymphatic and hematogenous routes. This theory has been supported by a few studies demonstrating endometrial tissue in pelvic lymph nodes and findings of endometrial tissue in uterine blood vessels.[3] Other theories have also been proposed, including coelomic metaplasia, but the most evidence seems to support the implantation theory."
],
"date": "January 17, 2023",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/742/478/742478-thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/742/478/742478-thumb2.png"
}
],
"markdown": "# A Mother of Four With Menstruation Issues and Debilitating Pain\n\n **Authors:** Linda A. Dultz, MD, MPH; Karina L. Vivar; Suzanne MacFarland; MaryAnn Hopkins, MD, MPhil \n **Date:** January 17, 2023\n\n ## Content\n\n The diagnosis of endometriosis was confirmed by histology of the surgical specimen and was consistent with the patient’s clinical history of premenstrual pain exacerbation. The histologic sections showed irregular endometrial glands and stroma interspersed within muscular and other soft tissue (Figure 1). The glands were lined by columnar epithelium surrounded by endometrial stromal tissue. Evidence of hemorrhage and hemosiderin-laden macrophages were observed, consistent with menstrual cycle changes (Figure 2).\nFigure 1.\nFigure 2.\nThe presence of cholesterol clefts and giant cells also suggested past hemorrhage. The glandular tissue was estrogen-receptor positive, further supporting a uterine endometrial origin. The diagnosis of endometriosis was made on the basis of the typical histologic appearance.\nFirst described in 1860, endometriosis continues to be a benign but debilitating disease that burdens millions of women each year. It is a chronic gynecologic disorder whose principal manifestations are chronic pain and infertility. Pelvic endometriosis is the presence of endometrial glands and stromal tissue outside of the uterine cavity but confined to the pelvis. Extrapelvic endometriosis refers to endometrial tissue found anywhere in the body outside of the pelvic cavity.[1,2] Although the pathophysiology of endometriosis is poorly understood, several theories have been proposed.\nThe first and best supported is the implantation theory, which suggests that endometrial tissue passes through the fallopian tubes in a retrograde fashion to attach and proliferate at ectopic sites in the peritoneal cavity. This theory has been observed in menstruating females during laparoscopic surgery, as well as in animal models mimicking retrograde flow. These studies have not only demonstrated retrograde flow, but they support the idea that sloughed endometrial cells can reimplant and survive outside the pelvic cavity.[3]\nA second proposed theory is the direct extension theory, which states that endometriosis results from direct invasion of ectopic endometrium through the uterine musculature. However, studies have thus far failed to show a connection between direct invasion and ectopic endometrial implants.[3] A third theory, the lymphatic/vascular metastases theory, suggests that endometrial cells can metastasize through lymphatic and hematogenous routes. This theory has been supported by a few studies demonstrating endometrial tissue in pelvic lymph nodes and findings of endometrial tissue in uterine blood vessels.[3] Other theories have also been proposed, including coelomic metaplasia, but the most evidence seems to support the implantation theory.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 407467,
"choiceText": "Desmoid tumor\r\n",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407468,
"choiceText": "Lipoma",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407469,
"choiceText": "Endometriosis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407470,
"choiceText": "Synovial sarcoma",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 119298,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Mother of Four With Menstruation Issues and Debilitating Pain"
},
{
"authors": "Linda A. Dultz, MD, MPH; Karina L. Vivar; Suzanne MacFarland; MaryAnn Hopkins, MD, MPhil",
"content": [
"The estimated prevalence of endometriosis is 10% in the general population, and it is a leading cause of gynecologic-related hospitalization.[4,5] The true prevalence of endometriosis is most likely underestimated because the disease can be asymptomatic or manifest only minimal symptoms and can be difficult to diagnose without surgery.[2]",
"Several clinical features are commonly seen in patients with endometriosis, including age between 30 and 40 years, nulliparity, and involuntary infertility. They also may have dysmenorrhea, dyspareunia, and the classic symptom, pelvic pain.[2] Pain and infertility are the most common sequelae of this disease and can cause devastating effects on the physical, mental, and social well-being of affected women.[6]",
"Due to a lack of sufficient studies, the true prevalence of extrapelvic endometriosis remains unknown. Extrapelvic endometriosis has been reported in the gastrointestinal tract,[7] appendix,[8] inguinal canal,[9] liver,[10] lung,[11] umbilicus,[12] cesarean scar,[13] and rectus abdominus.[1] Cases have also been reported of abdominal wall endometriosis following needle introduction from amniocentesis.[14,15]",
"Blanco and colleagues[16] noted a 4% prevalence of abdominal wall endometriosis in a retrospective study of 297 patients with endometriosis. Common clinical symptoms for these cases of endometriosis included a palpable mass, dyspareunia, menorrhagia, and dysmenorrhea.",
"The initial workup of possible extrapelvic endometriosis should include a detailed history and physical examination, consideration of various imaging modalities (ultrasonography, MRI, CT scanning), and/or fine-needle aspiration (FNA).",
"FNA of an endometriotic mass demonstrates the tubular and spindle-shaped stromal cells seen in endometriosis. Endometrial glands with endometrial stroma can also be appreciated on hematoxylin-eosin stained specimens.[17] Imaging modalities used to help determine the extent of endometriotic masses for surgery include ultrasonography, CT scanning, and MRI. Classic endometriosis demonstrates low-level homogeneous internal echoes on ultrasonography and is found in 95% of cases.[18] CT scanning of these masses is nonspecific, with findings including simple to complex cystic structures and contrast enhancement due to vascularity and hemorrhagic components.[19] MRI is the most specific modality because it can detect hemorrhagic nodules containing degenerated blood product, with T2-weighted images showing progressive loss of signal in the dependent portion of the lesion as a result of accumulation of chronic blood products from cyclic bleeding.[20]"
],
"date": "January 17, 2023",
"figures": [],
"markdown": "# A Mother of Four With Menstruation Issues and Debilitating Pain\n\n **Authors:** Linda A. Dultz, MD, MPH; Karina L. Vivar; Suzanne MacFarland; MaryAnn Hopkins, MD, MPhil \n **Date:** January 17, 2023\n\n ## Content\n\n The estimated prevalence of endometriosis is 10% in the general population, and it is a leading cause of gynecologic-related hospitalization.[4,5] The true prevalence of endometriosis is most likely underestimated because the disease can be asymptomatic or manifest only minimal symptoms and can be difficult to diagnose without surgery.[2]\nSeveral clinical features are commonly seen in patients with endometriosis, including age between 30 and 40 years, nulliparity, and involuntary infertility. They also may have dysmenorrhea, dyspareunia, and the classic symptom, pelvic pain.[2] Pain and infertility are the most common sequelae of this disease and can cause devastating effects on the physical, mental, and social well-being of affected women.[6]\nDue to a lack of sufficient studies, the true prevalence of extrapelvic endometriosis remains unknown. Extrapelvic endometriosis has been reported in the gastrointestinal tract,[7] appendix,[8] inguinal canal,[9] liver,[10] lung,[11] umbilicus,[12] cesarean scar,[13] and rectus abdominus.[1] Cases have also been reported of abdominal wall endometriosis following needle introduction from amniocentesis.[14,15]\nBlanco and colleagues[16] noted a 4% prevalence of abdominal wall endometriosis in a retrospective study of 297 patients with endometriosis. Common clinical symptoms for these cases of endometriosis included a palpable mass, dyspareunia, menorrhagia, and dysmenorrhea.\nThe initial workup of possible extrapelvic endometriosis should include a detailed history and physical examination, consideration of various imaging modalities (ultrasonography, MRI, CT scanning), and/or fine-needle aspiration (FNA).\nFNA of an endometriotic mass demonstrates the tubular and spindle-shaped stromal cells seen in endometriosis. Endometrial glands with endometrial stroma can also be appreciated on hematoxylin-eosin stained specimens.[17] Imaging modalities used to help determine the extent of endometriotic masses for surgery include ultrasonography, CT scanning, and MRI. Classic endometriosis demonstrates low-level homogeneous internal echoes on ultrasonography and is found in 95% of cases.[18] CT scanning of these masses is nonspecific, with findings including simple to complex cystic structures and contrast enhancement due to vascularity and hemorrhagic components.[19] MRI is the most specific modality because it can detect hemorrhagic nodules containing degenerated blood product, with T2-weighted images showing progressive loss of signal in the dependent portion of the lesion as a result of accumulation of chronic blood products from cyclic bleeding.[20]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A Mother of Four With Menstruation Issues and Debilitating Pain"
},
{
"authors": "Linda A. Dultz, MD, MPH; Karina L. Vivar; Suzanne MacFarland; MaryAnn Hopkins, MD, MPhil",
"content": [
"The mainstay of treatment for endometriosis includes medical and/or surgical treatment.[6] Medical therapies consist most commonly of the use of nonsteroidal anti-inflammatory drugs (NSAIDs), progestogens, oral contraceptive pills, or gonadotropin-releasing hormone (GnRH) agonists. Sustained progestins work by atrophying the glands, whereas GnRH analogs suppress endogenous estrogen.",
"Surgical procedures can also be performed, either as first-line management or when patients are refractory to medical therapy. Treatment options may include laparoscopic or open excision with fulguration, or laser ablation of endometriosis, resection of rectovaginal nodules, lysis of adhesions, and/or interruption of nerve pathways to obtain pain relief.[21] Recurrence of symptoms is common in up to 60% of patients despite surgical efforts, and postoperative medical therapy is normally continued with a GnRH agonist, danazol, or combined oral contraceptives.[21]",
"The role of IVF leading to worsening of endometriosis is currently under investigation and is controversial in nature. Whether ovarian stimulation leads to progression of disease in these patients due to the unopposed estrogen is unclear. Several case reports and retrospective studies have presented data for both sides of the argument.[22,23,24,25] In a review article by Dechaud and colleagues,[26] the authors conceded that more data need to be obtained to conclusively determine whether IVF plays a role in the worsening of endometriosis.",
"In this case, the patient had no known history of pelvic endometriosis, but because her symptoms increased with her menstrual cycles, the diagnosis could be suspected prior to surgery. The patient underwent surgery without complications and was discharged to home the same day. She has done well postoperatively and remains pain-free. Because she had an isolated nodule and has not had any return of her pain symptoms, she remains off medical therapy."
],
"date": "January 17, 2023",
"figures": [],
"markdown": "# A Mother of Four With Menstruation Issues and Debilitating Pain\n\n **Authors:** Linda A. Dultz, MD, MPH; Karina L. Vivar; Suzanne MacFarland; MaryAnn Hopkins, MD, MPhil \n **Date:** January 17, 2023\n\n ## Content\n\n The mainstay of treatment for endometriosis includes medical and/or surgical treatment.[6] Medical therapies consist most commonly of the use of nonsteroidal anti-inflammatory drugs (NSAIDs), progestogens, oral contraceptive pills, or gonadotropin-releasing hormone (GnRH) agonists. Sustained progestins work by atrophying the glands, whereas GnRH analogs suppress endogenous estrogen.\nSurgical procedures can also be performed, either as first-line management or when patients are refractory to medical therapy. Treatment options may include laparoscopic or open excision with fulguration, or laser ablation of endometriosis, resection of rectovaginal nodules, lysis of adhesions, and/or interruption of nerve pathways to obtain pain relief.[21] Recurrence of symptoms is common in up to 60% of patients despite surgical efforts, and postoperative medical therapy is normally continued with a GnRH agonist, danazol, or combined oral contraceptives.[21]\nThe role of IVF leading to worsening of endometriosis is currently under investigation and is controversial in nature. Whether ovarian stimulation leads to progression of disease in these patients due to the unopposed estrogen is unclear. Several case reports and retrospective studies have presented data for both sides of the argument.[22,23,24,25] In a review article by Dechaud and colleagues,[26] the authors conceded that more data need to be obtained to conclusively determine whether IVF plays a role in the worsening of endometriosis.\nIn this case, the patient had no known history of pelvic endometriosis, but because her symptoms increased with her menstrual cycles, the diagnosis could be suspected prior to surgery. The patient underwent surgery without complications and was discharged to home the same day. She has done well postoperatively and remains pain-free. Because she had an isolated nodule and has not had any return of her pain symptoms, she remains off medical therapy.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 407471,
"choiceText": "Ultrasound",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407472,
"choiceText": "Positron emission tomography (PET) scanning",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407473,
"choiceText": "CT scan",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407474,
"choiceText": "MRI",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Of the imaging modalities listed, MRI is the most specific to diagnose an endometrioma. It can detect hemorrhagic nodules containing degenerated blood product with T2-weighted images showing progressive loss of signal in the dependent portion of the lesion as a result of accumulation of chronic blood products from cyclic bleeding. FNA can also be attempted, although its sensitivity and specificity are unclear. However, if positive, FNA demonstrates the tubular and spindle-shaped stromal cells seen in endometriosis. Endometrial glands with endometrial stroma can also be appreciated on hematoxylin-eosin-stained specimens. CT scanning is nonspecific for the diagnosis of endometriosis and can cause confusion over benign vs malignant tumors. Characteristics of endometriosis also widely vary on ultrasound and can appear cystic (simple or complex) or can present as a solid mass which can confuse the diagnosis. PET scanning does not currently have a well-recognized role in the diagnosis of endometriosis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 119299,
"questionText": "A 36-year-old woman presents with a palpable mass directly underneath a prior cesarean-delivery scar. She states that she has a history of endometriosis and has noticed that the mass becomes larger and more painful with her menses.<br><br>\r\nWhich of the following imaging tests is the most specific modality for the diagnosis of endometrioma?\r\n",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 407475,
"choiceText": "Dysuria",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407476,
"choiceText": "Weight gain",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407477,
"choiceText": "Dysmenorrhea",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407478,
"choiceText": "Breast tenderness",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Endometriosis classically presents with menorrhagia and dysmenorrhea. Depending on the location of the endometrioma, an associated palpable mass may be present that enlarges and becomes increasingly tender with a patient's menstrual cycle.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 119300,
"questionText": "A 32-year-old woman states that she cannot become pregnant after trying for 2 years. Which of the following is more likely to indicate that she may have endometriosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Mother of Four With Menstruation Issues and Debilitating Pain"
},
{
"authors": "Linda A. Dultz, MD, MPH; Karina L. Vivar; Suzanne MacFarland; MaryAnn Hopkins, MD, MPhil",
"content": [],
"date": "January 17, 2023",
"figures": [],
"markdown": "# A Mother of Four With Menstruation Issues and Debilitating Pain\n\n **Authors:** Linda A. Dultz, MD, MPH; Karina L. Vivar; Suzanne MacFarland; MaryAnn Hopkins, MD, MPhil \n **Date:** January 17, 2023\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 407471,
"choiceText": "Ultrasound",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407472,
"choiceText": "Positron emission tomography (PET) scanning",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407473,
"choiceText": "CT scan",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407474,
"choiceText": "MRI",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Of the imaging modalities listed, MRI is the most specific to diagnose an endometrioma. It can detect hemorrhagic nodules containing degenerated blood product with T2-weighted images showing progressive loss of signal in the dependent portion of the lesion as a result of accumulation of chronic blood products from cyclic bleeding. FNA can also be attempted, although its sensitivity and specificity are unclear. However, if positive, FNA demonstrates the tubular and spindle-shaped stromal cells seen in endometriosis. Endometrial glands with endometrial stroma can also be appreciated on hematoxylin-eosin-stained specimens. CT scanning is nonspecific for the diagnosis of endometriosis and can cause confusion over benign vs malignant tumors. Characteristics of endometriosis also widely vary on ultrasound and can appear cystic (simple or complex) or can present as a solid mass which can confuse the diagnosis. PET scanning does not currently have a well-recognized role in the diagnosis of endometriosis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 119299,
"questionText": "A 36-year-old woman presents with a palpable mass directly underneath a prior cesarean-delivery scar. She states that she has a history of endometriosis and has noticed that the mass becomes larger and more painful with her menses.<br><br>\r\nWhich of the following imaging tests is the most specific modality for the diagnosis of endometrioma?\r\n",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 407475,
"choiceText": "Dysuria",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407476,
"choiceText": "Weight gain",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407477,
"choiceText": "Dysmenorrhea",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407478,
"choiceText": "Breast tenderness",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Endometriosis classically presents with menorrhagia and dysmenorrhea. Depending on the location of the endometrioma, an associated palpable mass may be present that enlarges and becomes increasingly tender with a patient's menstrual cycle.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 119300,
"questionText": "A 32-year-old woman states that she cannot become pregnant after trying for 2 years. Which of the following is more likely to indicate that she may have endometriosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Mother of Four With Menstruation Issues and Debilitating Pain"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 407467,
"choiceText": "Desmoid tumor\r\n",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407468,
"choiceText": "Lipoma",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407469,
"choiceText": "Endometriosis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407470,
"choiceText": "Synovial sarcoma",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 119298,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 407471,
"choiceText": "Ultrasound",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407472,
"choiceText": "Positron emission tomography (PET) scanning",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407473,
"choiceText": "CT scan",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407474,
"choiceText": "MRI",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Of the imaging modalities listed, MRI is the most specific to diagnose an endometrioma. It can detect hemorrhagic nodules containing degenerated blood product with T2-weighted images showing progressive loss of signal in the dependent portion of the lesion as a result of accumulation of chronic blood products from cyclic bleeding. FNA can also be attempted, although its sensitivity and specificity are unclear. However, if positive, FNA demonstrates the tubular and spindle-shaped stromal cells seen in endometriosis. Endometrial glands with endometrial stroma can also be appreciated on hematoxylin-eosin-stained specimens. CT scanning is nonspecific for the diagnosis of endometriosis and can cause confusion over benign vs malignant tumors. Characteristics of endometriosis also widely vary on ultrasound and can appear cystic (simple or complex) or can present as a solid mass which can confuse the diagnosis. PET scanning does not currently have a well-recognized role in the diagnosis of endometriosis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 119299,
"questionText": "A 36-year-old woman presents with a palpable mass directly underneath a prior cesarean-delivery scar. She states that she has a history of endometriosis and has noticed that the mass becomes larger and more painful with her menses.<br><br>\r\nWhich of the following imaging tests is the most specific modality for the diagnosis of endometrioma?\r\n",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 407475,
"choiceText": "Dysuria",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407476,
"choiceText": "Weight gain",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407477,
"choiceText": "Dysmenorrhea",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 407478,
"choiceText": "Breast tenderness",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Endometriosis classically presents with menorrhagia and dysmenorrhea. Depending on the location of the endometrioma, an associated palpable mass may be present that enlarges and becomes increasingly tender with a patient's menstrual cycle.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 119300,
"questionText": "A 32-year-old woman states that she cannot become pregnant after trying for 2 years. Which of the following is more likely to indicate that she may have endometriosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
877716 | /viewarticle/877716 | [
{
"authors": "Shah Azmoon, MD; Matthew Budoff, MD; David Atkinson, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"An 18-month-old girl is brought to a pediatrician by her parents with a history of intermittent episodes of nighttime diaphoresis and agitation. The patient's medical history is significant for viral cardiomyopathy that was diagnosed when the child was aged 9 months. At that time, the patient had been taken to a local emergency department (ED) in her native country of the Philippines for chronic cough and worsening shortness of breath. Routine chest radiography was performed, which showed the presence of cardiomegaly; a two-dimensional echocardiogram further revealed dilated cardiomyopathy, with a left ventricular ejection fraction of approximately 20% and a left ventricular thrombus. The patient was diagnosed with cardiomyopathy presumed to be secondary to viral myocarditis, and her family was informed that the infant would need to be on long-term digoxin and captopril.",
"The following year, the patient and her family immigrated to the United States. As a result of financial constraints, the patient's family has not received any medication nor have they been able to seek medical care for the child in several months. No family history of significant disease, maternal radiation exposure, or intake of teratogenic drugs is noted."
],
"date": "January 17, 2023",
"figures": [],
"markdown": "# Pediatric Case Challenge: Alarming Symptoms in a Toddler Who Had Myocarditis and Recently Immigrated\n\n **Authors:** Shah Azmoon, MD; Matthew Budoff, MD; David Atkinson, MD \n **Date:** January 17, 2023\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nAn 18-month-old girl is brought to a pediatrician by her parents with a history of intermittent episodes of nighttime diaphoresis and agitation. The patient's medical history is significant for viral cardiomyopathy that was diagnosed when the child was aged 9 months. At that time, the patient had been taken to a local emergency department (ED) in her native country of the Philippines for chronic cough and worsening shortness of breath. Routine chest radiography was performed, which showed the presence of cardiomegaly; a two-dimensional echocardiogram further revealed dilated cardiomyopathy, with a left ventricular ejection fraction of approximately 20% and a left ventricular thrombus. The patient was diagnosed with cardiomyopathy presumed to be secondary to viral myocarditis, and her family was informed that the infant would need to be on long-term digoxin and captopril.\nThe following year, the patient and her family immigrated to the United States. As a result of financial constraints, the patient's family has not received any medication nor have they been able to seek medical care for the child in several months. No family history of significant disease, maternal radiation exposure, or intake of teratogenic drugs is noted.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Pediatric Case Challenge: Alarming Symptoms in a Toddler Who Had Myocarditis and Recently Immigrated"
},
{
"authors": "Shah Azmoon, MD; Matthew Budoff, MD; David Atkinson, MD",
"content": [
"Upon physical examination, the patient is in no apparent distress. The child is not cyanotic, and she is noted to be in the 50th percentile for height and weight. Her vital signs, including an oxygen saturation level of 98% while breathing room air, are all normal. The cardiac examination reveals a visible and lateralized point of maximal intensity, a normal rate and rhythm, a fourth heart sound, and a II/VI holosystolic blowing murmur of mitral regurgitation. Her breath sounds are clear bilaterally. No hepatomegaly is noted on the abdominal examination, and symmetric normal amplitude pulses are found in all extremities.",
"Chest radiography is performed (images not available) that is significant for cardiomegaly, without any evidence of acute venous congestion. An electrocardiogram (ECG; tracing not available) reveals sinus tachycardia, Q waves in leads I and aVL, and inferior ST-segment depression with T-wave inversion that is suggestive of ischemia in the inferolateral distribution with repolarization abnormalities.",
"The pediatrician refers the patient to the pediatric ED of an affiliated hospital, where an initial transthoracic echocardiogram (TTE) reveals a dilated left ventricle with an ejection fraction of 15%, the presence of a left ventricular thrombus and spontaneous contrast, and a small pericardial effusion. The patient is admitted for anticoagulation therapy and further workup of her cardiomyopathy, which includes a gallium scan with an unremarkable result and mildly elevated pulmonary artery (PA) pressures detected on right heart catheterization. A repeat TTE obtained during the course of the admission shows resolution of the thrombus and an ejection fraction of approximately 25%; however, the TTE is not able to appreciate the continuous course of the coronaries.",
"The patient is referred for cardiac CT angiography (CCTA) for better delineation of her coronary anatomy. The CCTA images are obtained using low-dose protocols, with an estimated radiation dose of 1 millisievert (Figure 1, Figure 2).",
"Figure 1",
"Figure 2"
],
"date": "January 17, 2023",
"figures": [
{
"caption": "Figure 1",
"image_url": "https://img.medscapestatic.com/article/877/716/877716-Thumb1.png"
},
{
"caption": "Figure 2",
"image_url": "https://img.medscapestatic.com/article/877/716/877716-Thumb2.png"
}
],
"markdown": "# Pediatric Case Challenge: Alarming Symptoms in a Toddler Who Had Myocarditis and Recently Immigrated\n\n **Authors:** Shah Azmoon, MD; Matthew Budoff, MD; David Atkinson, MD \n **Date:** January 17, 2023\n\n ## Content\n\n Upon physical examination, the patient is in no apparent distress. The child is not cyanotic, and she is noted to be in the 50th percentile for height and weight. Her vital signs, including an oxygen saturation level of 98% while breathing room air, are all normal. The cardiac examination reveals a visible and lateralized point of maximal intensity, a normal rate and rhythm, a fourth heart sound, and a II/VI holosystolic blowing murmur of mitral regurgitation. Her breath sounds are clear bilaterally. No hepatomegaly is noted on the abdominal examination, and symmetric normal amplitude pulses are found in all extremities.\nChest radiography is performed (images not available) that is significant for cardiomegaly, without any evidence of acute venous congestion. An electrocardiogram (ECG; tracing not available) reveals sinus tachycardia, Q waves in leads I and aVL, and inferior ST-segment depression with T-wave inversion that is suggestive of ischemia in the inferolateral distribution with repolarization abnormalities.\nThe pediatrician refers the patient to the pediatric ED of an affiliated hospital, where an initial transthoracic echocardiogram (TTE) reveals a dilated left ventricle with an ejection fraction of 15%, the presence of a left ventricular thrombus and spontaneous contrast, and a small pericardial effusion. The patient is admitted for anticoagulation therapy and further workup of her cardiomyopathy, which includes a gallium scan with an unremarkable result and mildly elevated pulmonary artery (PA) pressures detected on right heart catheterization. A repeat TTE obtained during the course of the admission shows resolution of the thrombus and an ejection fraction of approximately 25%; however, the TTE is not able to appreciate the continuous course of the coronaries.\nThe patient is referred for cardiac CT angiography (CCTA) for better delineation of her coronary anatomy. The CCTA images are obtained using low-dose protocols, with an estimated radiation dose of 1 millisievert (Figure 1, Figure 2).\nFigure 1\nFigure 2\n\n ## Figures\n\n **Figure 1** \n \n\n**Figure 2** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1082812,
"choiceText": "Pulmonary vein anomaly",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082814,
"choiceText": "Left atrial thrombus",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082816,
"choiceText": "Anomalous coronary artery",
"correct": true,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082818,
"choiceText": "Aortic aneurysm",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": null,
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 342991,
"questionText": "What is the condition demonstrated by the CCTA images?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Pediatric Case Challenge: Alarming Symptoms in a Toddler Who Had Myocarditis and Recently Immigrated"
},
{
"authors": "Shah Azmoon, MD; Matthew Budoff, MD; David Atkinson, MD",
"content": [
"The images provided demonstrate a left main coronary artery arising anomalously from the PA, a condition referred to as Bland-White-Garland syndrome or anomalous left coronary artery originating from the PA (ALCAPA), and a significantly dilated left ventricle (Figure 1, Figure 3).[1]",
"Figure 1",
"Figure 3",
"Coronary arteries originating anomalously from the PA have been documented as far back as the 1800s.[2,3] Although most coronary artery anomalies arise from the aorta, less than 0.4% of patients with congenital cardiac anomalies have coronary vessels that originate from the PA (approximately 1 in 300,000 live births in the United States).[4]",
"Coronary vessel formation begins at approximately 32 days' gestation. Abnormal division of the conotruncus into the aorta and PA or abnormal involution and persistence of an endothelial bud on a pulmonary sinus may lead to an aberrant connection to the developing coronary artery. In 1933, Bland, White, and Garland diagnosed the syndrome of early progressive heart failure associated with anomalous origin of the coronary arteries arising from the PA in a 3-month-old child at autopsy.[5] The anomaly is most often a single left coronary artery rather than a right coronary artery. In some instances, the left circumflex artery and the left anterior descending artery may also have separate origins from the PA.[6]",
"Although the clinical presentation may vary depending on the coronary artery involved, as well as its size and distribution, in most cases significant hemodynamic compromise is present, with ensuing myocardial ischemia and progressive ischemic cardiomyopathy. If left untreated, mortality has been reported to be as high as 90% within the first year of life.[6] Prompt diagnosis and treatment are necessary in cases in which both the left and right coronary arteries arise from the PA (a less common variant of Bland-White-Garland syndrome) because the condition is not compatible with survival.",
"The symptoms of angina in an infant may include feeding intolerance, irritability or respiratory distress when crying, diaphoresis, pallor, failure to thrive, and even shock. Early symptoms may temporarily be masked by the presence of large collateral vessels. Rarely, the onset of symptoms in children may include precordial pain, dyspnea and tachypnea, shortness of breath, exertional chest pain, syncope, and even sudden cardiac death. Upon the normalization of physiologically elevated neonatal pulmonary vascular resistance in the first 4-6 weeks of infancy, the low perfusion pressures and low oxygen saturation characteristic of the PA lead to myocardial ischemia and progressive cardiomyopathy.",
"Demand ischemia caused by anomalous coronary arteries from the PA is not noted prenatally because the parallel circulatory system provides relatively equivalent oxygen concentrations and pressures between the aorta and main PA through the patent ductus arteriosus (PDA). With the formation of a collateral blood supply between the right and left coronary systems, the symptom onset may be delayed; however, coronary steal phenomenon may occur as a result of the higher-pressure collateral vessels and retrograde flow into the PA from the anomalous coronary artery, should collaterals arise from normal coronary arteries. [7] If left untreated, coronary steal will exacerbate the symptoms of heart failure and accelerate the complications associated with ischemia, cardiomyopathy, and pulmonary hypertension."
],
"date": "January 17, 2023",
"figures": [
{
"caption": "Figure 1",
"image_url": "https://img.medscapestatic.com/article/877/716/877716-Thumb1.png"
},
{
"caption": "Figure 3",
"image_url": "https://img.medscapestatic.com/article/877/716/877716-Thumb3.png"
}
],
"markdown": "# Pediatric Case Challenge: Alarming Symptoms in a Toddler Who Had Myocarditis and Recently Immigrated\n\n **Authors:** Shah Azmoon, MD; Matthew Budoff, MD; David Atkinson, MD \n **Date:** January 17, 2023\n\n ## Content\n\n The images provided demonstrate a left main coronary artery arising anomalously from the PA, a condition referred to as Bland-White-Garland syndrome or anomalous left coronary artery originating from the PA (ALCAPA), and a significantly dilated left ventricle (Figure 1, Figure 3).[1]\nFigure 1\nFigure 3\nCoronary arteries originating anomalously from the PA have been documented as far back as the 1800s.[2,3] Although most coronary artery anomalies arise from the aorta, less than 0.4% of patients with congenital cardiac anomalies have coronary vessels that originate from the PA (approximately 1 in 300,000 live births in the United States).[4]\nCoronary vessel formation begins at approximately 32 days' gestation. Abnormal division of the conotruncus into the aorta and PA or abnormal involution and persistence of an endothelial bud on a pulmonary sinus may lead to an aberrant connection to the developing coronary artery. In 1933, Bland, White, and Garland diagnosed the syndrome of early progressive heart failure associated with anomalous origin of the coronary arteries arising from the PA in a 3-month-old child at autopsy.[5] The anomaly is most often a single left coronary artery rather than a right coronary artery. In some instances, the left circumflex artery and the left anterior descending artery may also have separate origins from the PA.[6]\nAlthough the clinical presentation may vary depending on the coronary artery involved, as well as its size and distribution, in most cases significant hemodynamic compromise is present, with ensuing myocardial ischemia and progressive ischemic cardiomyopathy. If left untreated, mortality has been reported to be as high as 90% within the first year of life.[6] Prompt diagnosis and treatment are necessary in cases in which both the left and right coronary arteries arise from the PA (a less common variant of Bland-White-Garland syndrome) because the condition is not compatible with survival.\nThe symptoms of angina in an infant may include feeding intolerance, irritability or respiratory distress when crying, diaphoresis, pallor, failure to thrive, and even shock. Early symptoms may temporarily be masked by the presence of large collateral vessels. Rarely, the onset of symptoms in children may include precordial pain, dyspnea and tachypnea, shortness of breath, exertional chest pain, syncope, and even sudden cardiac death. Upon the normalization of physiologically elevated neonatal pulmonary vascular resistance in the first 4-6 weeks of infancy, the low perfusion pressures and low oxygen saturation characteristic of the PA lead to myocardial ischemia and progressive cardiomyopathy.\nDemand ischemia caused by anomalous coronary arteries from the PA is not noted prenatally because the parallel circulatory system provides relatively equivalent oxygen concentrations and pressures between the aorta and main PA through the patent ductus arteriosus (PDA). With the formation of a collateral blood supply between the right and left coronary systems, the symptom onset may be delayed; however, coronary steal phenomenon may occur as a result of the higher-pressure collateral vessels and retrograde flow into the PA from the anomalous coronary artery, should collaterals arise from normal coronary arteries. [7] If left untreated, coronary steal will exacerbate the symptoms of heart failure and accelerate the complications associated with ischemia, cardiomyopathy, and pulmonary hypertension.\n\n ## Figures\n\n **Figure 1** \n \n\n**Figure 3** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1082812,
"choiceText": "Pulmonary vein anomaly",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082814,
"choiceText": "Left atrial thrombus",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082816,
"choiceText": "Anomalous coronary artery",
"correct": true,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082818,
"choiceText": "Aortic aneurysm",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": null,
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 342991,
"questionText": "What is the condition demonstrated by the CCTA images?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Pediatric Case Challenge: Alarming Symptoms in a Toddler Who Had Myocarditis and Recently Immigrated"
},
{
"authors": "Shah Azmoon, MD; Matthew Budoff, MD; David Atkinson, MD",
"content": [
"In patients with ALCAPA, a chest x-ray may demonstrate cardiomegaly with or without pulmonary vascular congestion; however, this is not diagnostic. Left ventricular hypertrophy, abnormalities of repolarization detected as ST-segment depression, and/or inversion in the inferior and lateral leads may be noted on ECG, as well as wide, deep Q waves in the lateral leads and poor R wave progression. Left ventricular dysfunction, mitral regurgitation or mitral annular dilation, and wall motion abnormalities in the setting of left heart dilatation may be seen on TTE. Enlargement of the proximal right coronary artery may reflect the development of extensive collateralization.",
"Although most cases may be diagnosed with echocardiography, echocardiography alone may be inadequate for establishing the diagnosis because the close course of the anomalous coronary vessel to the aortic sinus may create a false impression of normal anatomic origin. The use of color-flow Doppler ultrasonography has largely eliminated the need for cardiac catheterization by providing significantly increased diagnostic accuracy. Although it is dependent on PA pressures and the development of collateral vessels, abnormal retrograde anomalous coronary flow can be clearly demonstrated with color-flow Doppler ultrasonography. If the anomalous coronary artery arises from a branch PA, however, the diagnosis may be difficult to make using echocardiography, even when enhanced with Doppler techniques.",
"Although retrograde flow into the PA is most often directed in an unusual orientation, improper diagnosis of a PDA shunt or a coronary-cameral fistula may be erroneously made. Lack of collateralization may also make identification by selective right coronary arteriography or aortography difficult in the catheterization laboratory. The use of transesophageal echocardiography is seldom necessary in infants.",
"Although cardiac catheterization has traditionally been used as the criterion standard for diagnosing coronary artery anomalies, the angular restriction of angiographic projections and the limitations inherent in its planar imaging nature may render conventional angiography less useful for creating a clear anatomic picture when compared with newer imaging modalities. Conventional angiography is also invasive and carries a morbidity and mortality rate of 1.5% and 0.15%, respectively (especially in children).[1]",
"With progressive improvement in both the resolution and technical specifications, as well as multiplanar reconstruction with maximum intensity projections and volume rendering, CCTA may be an adequate alternative diagnostic tool for detecting coronary anomalies. Although in younger patients a short investigation time and minimal follow-up using CCTA as a diagnostic modality provides practical usefulness, multiangle assessment using three-dimensional reconstruction can provide optimal vessel projection for evaluating surgical intervention; therefore, repeated exposure to radiation and contrast required for conventional angiography is minimized."
],
"date": "January 17, 2023",
"figures": [],
"markdown": "# Pediatric Case Challenge: Alarming Symptoms in a Toddler Who Had Myocarditis and Recently Immigrated\n\n **Authors:** Shah Azmoon, MD; Matthew Budoff, MD; David Atkinson, MD \n **Date:** January 17, 2023\n\n ## Content\n\n In patients with ALCAPA, a chest x-ray may demonstrate cardiomegaly with or without pulmonary vascular congestion; however, this is not diagnostic. Left ventricular hypertrophy, abnormalities of repolarization detected as ST-segment depression, and/or inversion in the inferior and lateral leads may be noted on ECG, as well as wide, deep Q waves in the lateral leads and poor R wave progression. Left ventricular dysfunction, mitral regurgitation or mitral annular dilation, and wall motion abnormalities in the setting of left heart dilatation may be seen on TTE. Enlargement of the proximal right coronary artery may reflect the development of extensive collateralization.\nAlthough most cases may be diagnosed with echocardiography, echocardiography alone may be inadequate for establishing the diagnosis because the close course of the anomalous coronary vessel to the aortic sinus may create a false impression of normal anatomic origin. The use of color-flow Doppler ultrasonography has largely eliminated the need for cardiac catheterization by providing significantly increased diagnostic accuracy. Although it is dependent on PA pressures and the development of collateral vessels, abnormal retrograde anomalous coronary flow can be clearly demonstrated with color-flow Doppler ultrasonography. If the anomalous coronary artery arises from a branch PA, however, the diagnosis may be difficult to make using echocardiography, even when enhanced with Doppler techniques.\nAlthough retrograde flow into the PA is most often directed in an unusual orientation, improper diagnosis of a PDA shunt or a coronary-cameral fistula may be erroneously made. Lack of collateralization may also make identification by selective right coronary arteriography or aortography difficult in the catheterization laboratory. The use of transesophageal echocardiography is seldom necessary in infants.\nAlthough cardiac catheterization has traditionally been used as the criterion standard for diagnosing coronary artery anomalies, the angular restriction of angiographic projections and the limitations inherent in its planar imaging nature may render conventional angiography less useful for creating a clear anatomic picture when compared with newer imaging modalities. Conventional angiography is also invasive and carries a morbidity and mortality rate of 1.5% and 0.15%, respectively (especially in children).[1]\nWith progressive improvement in both the resolution and technical specifications, as well as multiplanar reconstruction with maximum intensity projections and volume rendering, CCTA may be an adequate alternative diagnostic tool for detecting coronary anomalies. Although in younger patients a short investigation time and minimal follow-up using CCTA as a diagnostic modality provides practical usefulness, multiangle assessment using three-dimensional reconstruction can provide optimal vessel projection for evaluating surgical intervention; therefore, repeated exposure to radiation and contrast required for conventional angiography is minimized.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Pediatric Case Challenge: Alarming Symptoms in a Toddler Who Had Myocarditis and Recently Immigrated"
},
{
"authors": "Shah Azmoon, MD; Matthew Budoff, MD; David Atkinson, MD",
"content": [
"More than 35 years after ALCAPA was described by Bland, White, and Garland, Sabiston and colleagues[8] first showed that retrograde flow into the PA via an anomalous coronary artery could be effectively treated by ligation of the anomalous coronary artery at the junction of the PA and direct anastomosis of the anomalous coronary artery from the PA to the aorta. Surgical correction is necessary to avoid further strain on the heart and progressive cardiomyopathy.",
"As described by Takeuchi and colleagues[9] in 1979, the creation of an intrapulmonary aortocoronary tunnel may be required in young patients with anomalous coronary arteries that are in positions not suitable for direct transfer. This procedure, however, may result in tunnel stenosis, aortic regurgitation, or PA stenosis.[10] When significant cardiac dysfunction is present, an evaluation for cardiac transplantation may be necessary. The prognosis after surgical correction is usually good, with improvement of global left ventricular dysfunction or mitral regurgitation; however, patients are still susceptible to atheromatous and nonatheromatous coronary stenoses.",
"Because of the delay in diagnosis and the history of significant cardiomyopathy, the patient in this case was referred to a nearby transplantation hospital and underwent a cardiac transplantation. At 2 years posttransplant, significant improvement in the patient's symptoms was noted; however, the patient and her family moved out of state shortly thereafter and were lost to follow-up. With this case of ALCAPA, the authors hope to draw attention to the need for suspicion and early recognition of coronary artery anomalies when presented with clinical symptoms of heart failure or ischemia in infants."
],
"date": "January 17, 2023",
"figures": [],
"markdown": "# Pediatric Case Challenge: Alarming Symptoms in a Toddler Who Had Myocarditis and Recently Immigrated\n\n **Authors:** Shah Azmoon, MD; Matthew Budoff, MD; David Atkinson, MD \n **Date:** January 17, 2023\n\n ## Content\n\n More than 35 years after ALCAPA was described by Bland, White, and Garland, Sabiston and colleagues[8] first showed that retrograde flow into the PA via an anomalous coronary artery could be effectively treated by ligation of the anomalous coronary artery at the junction of the PA and direct anastomosis of the anomalous coronary artery from the PA to the aorta. Surgical correction is necessary to avoid further strain on the heart and progressive cardiomyopathy.\nAs described by Takeuchi and colleagues[9] in 1979, the creation of an intrapulmonary aortocoronary tunnel may be required in young patients with anomalous coronary arteries that are in positions not suitable for direct transfer. This procedure, however, may result in tunnel stenosis, aortic regurgitation, or PA stenosis.[10] When significant cardiac dysfunction is present, an evaluation for cardiac transplantation may be necessary. The prognosis after surgical correction is usually good, with improvement of global left ventricular dysfunction or mitral regurgitation; however, patients are still susceptible to atheromatous and nonatheromatous coronary stenoses.\nBecause of the delay in diagnosis and the history of significant cardiomyopathy, the patient in this case was referred to a nearby transplantation hospital and underwent a cardiac transplantation. At 2 years posttransplant, significant improvement in the patient's symptoms was noted; however, the patient and her family moved out of state shortly thereafter and were lost to follow-up. With this case of ALCAPA, the authors hope to draw attention to the need for suspicion and early recognition of coronary artery anomalies when presented with clinical symptoms of heart failure or ischemia in infants.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1082828,
"choiceText": "Precordial pain",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082830,
"choiceText": "Dyspnea",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082832,
"choiceText": "Syncope",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082834,
"choiceText": "Tachypnea ",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082836,
"choiceText": "Feeding intolerance ",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The symptoms of angina in an infant may include feeding intolerance, irritability or respiratory distress when crying, diaphoresis, pallor, failure to thrive, and even shock. Early symptoms may temporarily be masked by the presence of large collateral vessels. Rarely, the onset of symptoms in children may include precordial pain, dyspnea and tachypnea, shortness of breath, exertional chest pain, <a href=\"http://emedicine.medscape.com/article/811669-overview\">syncope</a>, and even <a href=\"http://emedicine.medscape.com/article/151907-overview\">sudden cardiac death</a>.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 342995,
"questionText": "Of these symptoms associated with angina in infancy, which is more common?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1082864,
"choiceText": "Right ventricular dilation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082866,
"choiceText": "Right ventricular hypertrophy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082868,
"choiceText": "Enlargement of the proximal left coronary artery",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082870,
"choiceText": "Mitral regurgitation ",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082872,
"choiceText": "ST-segment elevation",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": " In patients with <a href=\"http://emedicine.medscape.com/article/893290-overview\">ALCAPA</a>, a chest x-ray may demonstrate cardiomegaly with or without pulmonary vascular congestion; however, this is not diagnostic. Left ventricular hypertrophy, abnormalities of repolarization detected as ST-segment depression, and/or inversion in the inferior and lateral leads may be noted on ECG, as well as wide, deep Q waves in the lateral leads and poor R wave progression. <br/><br/>\r\nLeft ventricular dysfunction, <a href=\"http://emedicine.medscape.com/article/155618-overview\">mitral regurgitation</a> or mitral annular dilation, and wall motion abnormalities in the setting of left heart dilatation may be seen on TTE. Enlargement of the proximal right coronary artery may reflect the development of extensive collateralization.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 343003,
"questionText": "Which of the following is more commonly associated with ALCAPA?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Pediatric Case Challenge: Alarming Symptoms in a Toddler Who Had Myocarditis and Recently Immigrated"
},
{
"authors": "Shah Azmoon, MD; Matthew Budoff, MD; David Atkinson, MD",
"content": [],
"date": "January 17, 2023",
"figures": [],
"markdown": "# Pediatric Case Challenge: Alarming Symptoms in a Toddler Who Had Myocarditis and Recently Immigrated\n\n **Authors:** Shah Azmoon, MD; Matthew Budoff, MD; David Atkinson, MD \n **Date:** January 17, 2023\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1082828,
"choiceText": "Precordial pain",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082830,
"choiceText": "Dyspnea",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082832,
"choiceText": "Syncope",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082834,
"choiceText": "Tachypnea ",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082836,
"choiceText": "Feeding intolerance ",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The symptoms of angina in an infant may include feeding intolerance, irritability or respiratory distress when crying, diaphoresis, pallor, failure to thrive, and even shock. Early symptoms may temporarily be masked by the presence of large collateral vessels. Rarely, the onset of symptoms in children may include precordial pain, dyspnea and tachypnea, shortness of breath, exertional chest pain, <a href=\"http://emedicine.medscape.com/article/811669-overview\">syncope</a>, and even <a href=\"http://emedicine.medscape.com/article/151907-overview\">sudden cardiac death</a>.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 342995,
"questionText": "Of these symptoms associated with angina in infancy, which is more common?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1082864,
"choiceText": "Right ventricular dilation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082866,
"choiceText": "Right ventricular hypertrophy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082868,
"choiceText": "Enlargement of the proximal left coronary artery",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082870,
"choiceText": "Mitral regurgitation ",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082872,
"choiceText": "ST-segment elevation",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": " In patients with <a href=\"http://emedicine.medscape.com/article/893290-overview\">ALCAPA</a>, a chest x-ray may demonstrate cardiomegaly with or without pulmonary vascular congestion; however, this is not diagnostic. Left ventricular hypertrophy, abnormalities of repolarization detected as ST-segment depression, and/or inversion in the inferior and lateral leads may be noted on ECG, as well as wide, deep Q waves in the lateral leads and poor R wave progression. <br/><br/>\r\nLeft ventricular dysfunction, <a href=\"http://emedicine.medscape.com/article/155618-overview\">mitral regurgitation</a> or mitral annular dilation, and wall motion abnormalities in the setting of left heart dilatation may be seen on TTE. Enlargement of the proximal right coronary artery may reflect the development of extensive collateralization.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 343003,
"questionText": "Which of the following is more commonly associated with ALCAPA?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Pediatric Case Challenge: Alarming Symptoms in a Toddler Who Had Myocarditis and Recently Immigrated"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1082812,
"choiceText": "Pulmonary vein anomaly",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082814,
"choiceText": "Left atrial thrombus",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082816,
"choiceText": "Anomalous coronary artery",
"correct": true,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082818,
"choiceText": "Aortic aneurysm",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": null,
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 342991,
"questionText": "What is the condition demonstrated by the CCTA images?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1082828,
"choiceText": "Precordial pain",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082830,
"choiceText": "Dyspnea",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082832,
"choiceText": "Syncope",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082834,
"choiceText": "Tachypnea ",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082836,
"choiceText": "Feeding intolerance ",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The symptoms of angina in an infant may include feeding intolerance, irritability or respiratory distress when crying, diaphoresis, pallor, failure to thrive, and even shock. Early symptoms may temporarily be masked by the presence of large collateral vessels. Rarely, the onset of symptoms in children may include precordial pain, dyspnea and tachypnea, shortness of breath, exertional chest pain, <a href=\"http://emedicine.medscape.com/article/811669-overview\">syncope</a>, and even <a href=\"http://emedicine.medscape.com/article/151907-overview\">sudden cardiac death</a>.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 342995,
"questionText": "Of these symptoms associated with angina in infancy, which is more common?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1082864,
"choiceText": "Right ventricular dilation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082866,
"choiceText": "Right ventricular hypertrophy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082868,
"choiceText": "Enlargement of the proximal left coronary artery",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082870,
"choiceText": "Mitral regurgitation ",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1082872,
"choiceText": "ST-segment elevation",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": " In patients with <a href=\"http://emedicine.medscape.com/article/893290-overview\">ALCAPA</a>, a chest x-ray may demonstrate cardiomegaly with or without pulmonary vascular congestion; however, this is not diagnostic. Left ventricular hypertrophy, abnormalities of repolarization detected as ST-segment depression, and/or inversion in the inferior and lateral leads may be noted on ECG, as well as wide, deep Q waves in the lateral leads and poor R wave progression. <br/><br/>\r\nLeft ventricular dysfunction, <a href=\"http://emedicine.medscape.com/article/155618-overview\">mitral regurgitation</a> or mitral annular dilation, and wall motion abnormalities in the setting of left heart dilatation may be seen on TTE. Enlargement of the proximal right coronary artery may reflect the development of extensive collateralization.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 343003,
"questionText": "Which of the following is more commonly associated with ALCAPA?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
984951 | /viewarticle/984951 | [
{
"authors": "Jonathan Katz, MD; Shivani Garg, MD, MS",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 46-year-old woman (G1P1) with a history of congenital splenomegaly and thrombocytopenia, who follows up with the hematology service, presents to the hospital as a transfer for worsening lung infiltrates. The patient also has a history of asthma, bipolar disorder, migraines, and recurrent lower-extremity deep venous thrombosis (DVT), with two positive tests for lupus anticoagulant (12 weeks apart) while taking apixaban.",
"She initially presented to another hospital with several days of worsening fatigue and fevers. At the other hospital, she underwent chest imaging, which demonstrated right-sided multifocal patchy ground glass opacities and a right-sided multiloculated effusion. Antibiotic therapy was started, and her symptoms improved; however, repeated CT showed new left upper lobe infiltrates with stable right lung findings. The new findings prompted her transfer for further workup and evaluation.",
"The patient notes that she has experienced several weeks of poor appetite and intermittent abdominal pain associated with her fevers and fatigue. She has a 6-month history of oral ulcers and a 2-year history of bilateral hand, wrist, and elbow pain, with intermittent swelling, erythema, and stiffness that has progressed for the past 6 months. The remainder of her review of systems is notable for Raynaud phenomenon and a history of photosensitivity, which manifests as profound fatigue after sun exposure.",
"Before her hospitalization, the patient had sought medical attention for her abdominal pain. At that visit, a CT scan showed new trace perisplenic fluid and laboratory results demonstrated leukopenia with thrombocytopenia, for which she underwent a bone biopsy several days before her current presentation. The results of the biopsy are pending.",
"She has no family history of rheumatologic or pulmonary disease. She works as a teaching assistant, and her social history is notable for rare alcohol use and a 30–pack-year smoking history."
],
"date": "January 09, 2023",
"figures": [],
"markdown": "# Internal Medicine Case Challenge: A Teacher’s Assistant With Bipolar Disorder Has Lung Problems\n\n **Authors:** Jonathan Katz, MD; Shivani Garg, MD, MS \n **Date:** January 09, 2023\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 46-year-old woman (G1P1) with a history of congenital splenomegaly and thrombocytopenia, who follows up with the hematology service, presents to the hospital as a transfer for worsening lung infiltrates. The patient also has a history of asthma, bipolar disorder, migraines, and recurrent lower-extremity deep venous thrombosis (DVT), with two positive tests for lupus anticoagulant (12 weeks apart) while taking apixaban.\nShe initially presented to another hospital with several days of worsening fatigue and fevers. At the other hospital, she underwent chest imaging, which demonstrated right-sided multifocal patchy ground glass opacities and a right-sided multiloculated effusion. Antibiotic therapy was started, and her symptoms improved; however, repeated CT showed new left upper lobe infiltrates with stable right lung findings. The new findings prompted her transfer for further workup and evaluation.\nThe patient notes that she has experienced several weeks of poor appetite and intermittent abdominal pain associated with her fevers and fatigue. She has a 6-month history of oral ulcers and a 2-year history of bilateral hand, wrist, and elbow pain, with intermittent swelling, erythema, and stiffness that has progressed for the past 6 months. The remainder of her review of systems is notable for Raynaud phenomenon and a history of photosensitivity, which manifests as profound fatigue after sun exposure.\nBefore her hospitalization, the patient had sought medical attention for her abdominal pain. At that visit, a CT scan showed new trace perisplenic fluid and laboratory results demonstrated leukopenia with thrombocytopenia, for which she underwent a bone biopsy several days before her current presentation. The results of the biopsy are pending.\nShe has no family history of rheumatologic or pulmonary disease. She works as a teaching assistant, and her social history is notable for rare alcohol use and a 30–pack-year smoking history.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Internal Medicine Case Challenge: A Teacher’s Assistant With Bipolar Disorder Has Lung Problems"
},
{
"authors": "Jonathan Katz, MD; Shivani Garg, MD, MS",
"content": [
"The patient's vital signs are stable, and no hypoxia is noted. The physical examination reveals oral ulcerations. Her heart rate and rhythm are regular. Decreased breath sounds are noted in the right lower lobe, along with crackles in the left posterior lung fields. The musculoskeletal examination is notable for swelling of the bilateral wrists and the right proximal interphalangeal and left metacarpophalangeal joints, with significant associated erythema. The neurologic examination shows that the patient is alert and oriented to herself, place, and time, with an appropriate affect. She has no gross neurologic deficits.",
"Given her presentation, a broad workup is pursued. The laboratory investigation reveals a white blood cell count of 6100 cells/µL (reference range, 3800-10,500 cells/µL), a hemoglobin level of 9.4 g/dL (reference range, 11.6-15.6 g/dL), and a platelet count of 115,000 cells/µL (reference range, 160,000-370,000 cells/µL). The basic metabolic panel is notable for a slightly elevated serum creatinine level of 0.93 mg/dL (reference range, 0.5-1.1 mg/dL). The patient's previous baseline level was 0.8 mg/dL.",
"The workup for inflammatory disease reveals a high C-reactive protein level of 14.1 mg/dL (reference range, 0.0-1.0 mg/dL) and an elevated erythrocyte sedimentation rate of 41 mm/h (reference range, 0-20 mm/h). Antibody testing shows these values:",
"Antinuclear antibody: 1:640 homogeneous (reference range, negative)",
"Double-stranded DNA (dsDNA): > 200 IU (> 200 IU, strong positive)",
"Antineutrophil cytoplasmic antibodies (ANCA): Positive (atypical ANCA pattern)",
"Smith antibody: 32 U (20-39 U, weak positive)",
"Complement component 3 (C3): 39 mg/dL (reference range, 83-193 mg/dL)",
"Complement component 4 (C4): 6 mg/dL (reference range, 15-57 mg/dL)",
"Testing for myeloperoxidase and proteinase 3 antibodies is negative. Testing for cardiolipin antibodies and beta-2 glycoprotein antibodies is negative, and lupus anticoagulant testing is positive (while the patient is on anticoagulation). She has a history of positive testing for lupus anticoagulant in the past, along with recurrent DVT, for which she was taking apixaban before this admission.",
"An infectious disease workup, including blood and sputum cultures, reveals few pseudomonads on sputum culture. Her antibiotic coverage is broadened, and she undergoes thoracentesis, with results indicative of an exudative effusion.",
"Upon serial blood testing over several days, her laboratory results demonstrate worsening kidney function, with a serum creatinine level of 1.78 mg/dL, now without azotemia. Additionally, a significant drop in platelet count is noted, with a nadir at 67,000 cells/µL. Her hemoglobin level also decreased and now is 7.7 g/dL. A concern for hemolysis is raised. Additional laboratory studies reveal:",
"Total bilirubin level: 0.3 mg/dL (reference range, 0.3-1.0 mg/dL)",
"Lactate dehydrogenase level: 297 U/dL (reference range, 125-220 U/dL)",
"Positive direct Coombs immunoglobulin G (IgG) test",
"Haptoglobin level: 282 mg/dL (reference range, 35-250 mg/dL)",
"Partial thromboplastin time: 88.2 sec (reference range, 28-38 sec)",
"Because of the elevated creatinine level, additional urine studies are ordered, which reveal no blood or blood cells, but a dipstick test is positive for protein. Further quantification reveals a urine protein-to-creatinine ratio of 0.42. Given the patient's presentation, a concern for kidney injury due to lupus, antiphospholipid syndrome (APS), thrombotic thrombocytopenic purpura (TTP), or tubulointerstitial nephritis is raised. Thus, she undergoes renal biopsy, which reveals acute thrombotic microangiopathy (TMA) with focal cortical necrosis, along with glomeruli with few segmental mesangial electron-dense deposits. These findings are consistent with class I lupus nephritis and TMA."
],
"date": "January 09, 2023",
"figures": [],
"markdown": "# Internal Medicine Case Challenge: A Teacher’s Assistant With Bipolar Disorder Has Lung Problems\n\n **Authors:** Jonathan Katz, MD; Shivani Garg, MD, MS \n **Date:** January 09, 2023\n\n ## Content\n\n The patient's vital signs are stable, and no hypoxia is noted. The physical examination reveals oral ulcerations. Her heart rate and rhythm are regular. Decreased breath sounds are noted in the right lower lobe, along with crackles in the left posterior lung fields. The musculoskeletal examination is notable for swelling of the bilateral wrists and the right proximal interphalangeal and left metacarpophalangeal joints, with significant associated erythema. The neurologic examination shows that the patient is alert and oriented to herself, place, and time, with an appropriate affect. She has no gross neurologic deficits.\nGiven her presentation, a broad workup is pursued. The laboratory investigation reveals a white blood cell count of 6100 cells/µL (reference range, 3800-10,500 cells/µL), a hemoglobin level of 9.4 g/dL (reference range, 11.6-15.6 g/dL), and a platelet count of 115,000 cells/µL (reference range, 160,000-370,000 cells/µL). The basic metabolic panel is notable for a slightly elevated serum creatinine level of 0.93 mg/dL (reference range, 0.5-1.1 mg/dL). The patient's previous baseline level was 0.8 mg/dL.\nThe workup for inflammatory disease reveals a high C-reactive protein level of 14.1 mg/dL (reference range, 0.0-1.0 mg/dL) and an elevated erythrocyte sedimentation rate of 41 mm/h (reference range, 0-20 mm/h). Antibody testing shows these values:\nAntinuclear antibody: 1:640 homogeneous (reference range, negative)\nDouble-stranded DNA (dsDNA): > 200 IU (> 200 IU, strong positive)\nAntineutrophil cytoplasmic antibodies (ANCA): Positive (atypical ANCA pattern)\nSmith antibody: 32 U (20-39 U, weak positive)\nComplement component 3 (C3): 39 mg/dL (reference range, 83-193 mg/dL)\nComplement component 4 (C4): 6 mg/dL (reference range, 15-57 mg/dL)\nTesting for myeloperoxidase and proteinase 3 antibodies is negative. Testing for cardiolipin antibodies and beta-2 glycoprotein antibodies is negative, and lupus anticoagulant testing is positive (while the patient is on anticoagulation). She has a history of positive testing for lupus anticoagulant in the past, along with recurrent DVT, for which she was taking apixaban before this admission.\nAn infectious disease workup, including blood and sputum cultures, reveals few pseudomonads on sputum culture. Her antibiotic coverage is broadened, and she undergoes thoracentesis, with results indicative of an exudative effusion.\nUpon serial blood testing over several days, her laboratory results demonstrate worsening kidney function, with a serum creatinine level of 1.78 mg/dL, now without azotemia. Additionally, a significant drop in platelet count is noted, with a nadir at 67,000 cells/µL. Her hemoglobin level also decreased and now is 7.7 g/dL. A concern for hemolysis is raised. Additional laboratory studies reveal:\nTotal bilirubin level: 0.3 mg/dL (reference range, 0.3-1.0 mg/dL)\nLactate dehydrogenase level: 297 U/dL (reference range, 125-220 U/dL)\nPositive direct Coombs immunoglobulin G (IgG) test\nHaptoglobin level: 282 mg/dL (reference range, 35-250 mg/dL)\nPartial thromboplastin time: 88.2 sec (reference range, 28-38 sec)\nBecause of the elevated creatinine level, additional urine studies are ordered, which reveal no blood or blood cells, but a dipstick test is positive for protein. Further quantification reveals a urine protein-to-creatinine ratio of 0.42. Given the patient's presentation, a concern for kidney injury due to lupus, antiphospholipid syndrome (APS), thrombotic thrombocytopenic purpura (TTP), or tubulointerstitial nephritis is raised. Thus, she undergoes renal biopsy, which reveals acute thrombotic microangiopathy (TMA) with focal cortical necrosis, along with glomeruli with few segmental mesangial electron-dense deposits. These findings are consistent with class I lupus nephritis and TMA.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1751269,
"choiceText": "Lupus nephritis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751270,
"choiceText": "Interstitial nephritis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751271,
"choiceText": "Antiphospholipid syndrome nephropathy",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751272,
"choiceText": "Thrombotic thrombocytopenic purpura",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 565693,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Internal Medicine Case Challenge: A Teacher’s Assistant With Bipolar Disorder Has Lung Problems"
},
{
"authors": "Jonathan Katz, MD; Shivani Garg, MD, MS",
"content": [
"The patient in this case has signs and symptoms of an underlying connective tissue disease. Her antibody profile and her symptoms suggest a diagnosis of systemic lupus erythematosus (SLE); therefore, lupus nephritis is an important consideration for the cause of her renal injury. However, the absence of hematuria in the urine studies, which is typically present in approximately 80% of cases of lupus nephritis, should prompt a broader differential for the etiology of her renal injury.[1]",
"This patient has a history of clots, which raises the concern for APS, specifically APS nephropathy. Additionally, with her worsening anemia, suspected SLE, and drug exposures, both interstitial nephritis and TTP should be considered in the differential as well.",
"Ultimately, biopsy is required to distinguish between these diagnoses. This patient's renal biopsy that demonstrates acute TMA is the key histologic finding. The otherwise normal-appearing glomeruli and lack of cellular infiltrates and scarring make the biopsy findings consistent with class Ib lupus nephritis, which is the classification for normal glomeruli with the presence of dense deposits on electron microscopy and is not associated with the degree of renal injury seen in this case.[2] Thus, the cause of her renal injury is most likely related to the microangiopathy observed on the biopsy. In the context of her history of clots, this finding makes a diagnosis of APS nephropathy, occurring in the setting of new-onset SLE, the most likely cause of her worsening renal function.",
"APS nephropathy is one of the most common renal manifestations of APS and refers to noninflammatory occlusion of the small vessels in the kidneys. Among patients with a diagnosis of SLE, up to 40% also have antiphospholipid antibodies and upward of 50% of these patients develop APS, which is characterized by a clotting event or an obstetric event.[3,4] APS nephropathy occurs in approximately 65% of patients with SLE APS, and the presentation can vary from generally asymptomatic with proteinuria to severe hypertension, nephrotic-range proteinuria, and active urinary sediment.[4]"
],
"date": "January 09, 2023",
"figures": [],
"markdown": "# Internal Medicine Case Challenge: A Teacher’s Assistant With Bipolar Disorder Has Lung Problems\n\n **Authors:** Jonathan Katz, MD; Shivani Garg, MD, MS \n **Date:** January 09, 2023\n\n ## Content\n\n The patient in this case has signs and symptoms of an underlying connective tissue disease. Her antibody profile and her symptoms suggest a diagnosis of systemic lupus erythematosus (SLE); therefore, lupus nephritis is an important consideration for the cause of her renal injury. However, the absence of hematuria in the urine studies, which is typically present in approximately 80% of cases of lupus nephritis, should prompt a broader differential for the etiology of her renal injury.[1]\nThis patient has a history of clots, which raises the concern for APS, specifically APS nephropathy. Additionally, with her worsening anemia, suspected SLE, and drug exposures, both interstitial nephritis and TTP should be considered in the differential as well.\nUltimately, biopsy is required to distinguish between these diagnoses. This patient's renal biopsy that demonstrates acute TMA is the key histologic finding. The otherwise normal-appearing glomeruli and lack of cellular infiltrates and scarring make the biopsy findings consistent with class Ib lupus nephritis, which is the classification for normal glomeruli with the presence of dense deposits on electron microscopy and is not associated with the degree of renal injury seen in this case.[2] Thus, the cause of her renal injury is most likely related to the microangiopathy observed on the biopsy. In the context of her history of clots, this finding makes a diagnosis of APS nephropathy, occurring in the setting of new-onset SLE, the most likely cause of her worsening renal function.\nAPS nephropathy is one of the most common renal manifestations of APS and refers to noninflammatory occlusion of the small vessels in the kidneys. Among patients with a diagnosis of SLE, up to 40% also have antiphospholipid antibodies and upward of 50% of these patients develop APS, which is characterized by a clotting event or an obstetric event.[3,4] APS nephropathy occurs in approximately 65% of patients with SLE APS, and the presentation can vary from generally asymptomatic with proteinuria to severe hypertension, nephrotic-range proteinuria, and active urinary sediment.[4]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1751269,
"choiceText": "Lupus nephritis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751270,
"choiceText": "Interstitial nephritis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751271,
"choiceText": "Antiphospholipid syndrome nephropathy",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751272,
"choiceText": "Thrombotic thrombocytopenic purpura",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 565693,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Internal Medicine Case Challenge: A Teacher’s Assistant With Bipolar Disorder Has Lung Problems"
},
{
"authors": "Jonathan Katz, MD; Shivani Garg, MD, MS",
"content": [
"Identifying the correct diagnosis has therapeutic implications, as acute thrombotic APS nephropathy warrants a specific anticoagulation regimen with warfarin, according to the 2021 Kidney Disease: Improving Global Outcomes (KDIGO) guidelines.[5,6] If not treated, it can lead to kidney failure. APS nephropathy should be considered in the differential diagnosis when patients present with kidney impairment, proteinuria, and high blood pressure, with or without a lupus diagnosis.",
"Diagnosis of APS nephropathy requires renal biopsy because in the early stages, it cannot be distinguished from lupus nephritis. Among patients with preexisting lupus nephritis, between 1% and 14% have coexisting APS nephropathy,[4] and up to 40% of those with SLE who test positive for antiphospholipid antibodies have APS nephropathy.[6] Upon biopsy, the early lesions of APS nephropathy often have the pathologic characteristics of TMA, as observed in the patient in this case. An example is shown in the figure below.",
"Figure 1.",
"Patients with a history of SLE and APS nephropathy have a higher rate of arterial thrombotic complications than those without such a history.[6] The antibody phenotype of APS has important prognostic implications, because patients with a history of triple positivity (two positive serum IgG antiphospholipid antibody test results, along with one positive functional plasma lupus anticoagulant test result) should receive anticoagulation with warfarin or heparin. Studies have demonstrated a higher rate of recurrent thrombotic events in patients treated with other anticoagulants.[7] In cases of catastrophic antiphospholipid syndrome (CAPS), anticoagulants, in addition to corticosteroids and intravenous immunoglobulin, are used for treatment; however, immunosuppression outside of CAPS is controversial without other indications and would not be indicated for treatment of TMA in this case.",
"A clinical diagnosis of TMA is an important consideration in the differential diagnosis because it carries potential therapeutic implications. TMA is both a clinical syndrome and a histologic definition (the latter demonstrated in the biopsy in this case). The clinical syndrome of TMA is a broad category and encompasses both primary and secondary causes. Manifestations include evidence of microangiopathic hemolytic anemia, thrombocytopenia, and end-organ injury. The histopathologic component demonstrates occlusive thrombus formation with characteristic abnormalities in the endothelium and vessel wall.[8]",
"Causes of primary TMA refer to causes that are either genetic or acquired; these include primary TTP and complement-mediated hemolytic-uremic syndrome. TTP can be hereditary or acquired and is related to severe deficiencies of ADAMTS13 (due to autoantibody formation against the protein or acquired genetic abnormalities), which separates it from the other causes of TMA. The diagnosis of TTP ultimately hinges on testing of ADAMTS13 activity, because the clinical presentation can vary from nonspecific findings to substantial neurologic deficits. Mortality ranges between 5% and 16%,[9] which makes a timely diagnosis crucial for the initiation of emergent plasma exchange therapy, a mainstay of TTP treatment.[8,9,10] Patients with SLE or APS nephropathy can have evidence of systemic TMA. Complement-mediated TMA may require complement inhibition with eculizumab in addition to anticoagulation and immunosuppression and is important to consider in the differential diagnosis.",
"The other diagnosis to consider is acute interstitial nephritis (AIN). AIN can be drug-induced (occurring in more than 75% of cases) or related to other conditions, including autoimmune disorders (10%-15% of cases).[11] The criterion standard for the diagnosis of interstitial nephritis is renal biopsy, which demonstrates an infiltrate of inflammatory cells within the renal interstitium. This is often associated with edema and sparing of the glomeruli and blood vessels. Figure 2 shows interstitial nephritis in a different patient.",
"Figure 2.",
"Urinalysis typically demonstrates proteinuria, pyuria, and hematuria, although red cell casts are rare. Eosinophiluria is classically associated with AIN. The absence of the finding does not exclude the diagnosis, and its overall utility is limited; studies have demonstrated a positive predictive value of 38% and a negative predictive value of 74%.[12]"
],
"date": "January 09, 2023",
"figures": [],
"markdown": "# Internal Medicine Case Challenge: A Teacher’s Assistant With Bipolar Disorder Has Lung Problems\n\n **Authors:** Jonathan Katz, MD; Shivani Garg, MD, MS \n **Date:** January 09, 2023\n\n ## Content\n\n Identifying the correct diagnosis has therapeutic implications, as acute thrombotic APS nephropathy warrants a specific anticoagulation regimen with warfarin, according to the 2021 Kidney Disease: Improving Global Outcomes (KDIGO) guidelines.[5,6] If not treated, it can lead to kidney failure. APS nephropathy should be considered in the differential diagnosis when patients present with kidney impairment, proteinuria, and high blood pressure, with or without a lupus diagnosis.\nDiagnosis of APS nephropathy requires renal biopsy because in the early stages, it cannot be distinguished from lupus nephritis. Among patients with preexisting lupus nephritis, between 1% and 14% have coexisting APS nephropathy,[4] and up to 40% of those with SLE who test positive for antiphospholipid antibodies have APS nephropathy.[6] Upon biopsy, the early lesions of APS nephropathy often have the pathologic characteristics of TMA, as observed in the patient in this case. An example is shown in the figure below.\nFigure 1.\nPatients with a history of SLE and APS nephropathy have a higher rate of arterial thrombotic complications than those without such a history.[6] The antibody phenotype of APS has important prognostic implications, because patients with a history of triple positivity (two positive serum IgG antiphospholipid antibody test results, along with one positive functional plasma lupus anticoagulant test result) should receive anticoagulation with warfarin or heparin. Studies have demonstrated a higher rate of recurrent thrombotic events in patients treated with other anticoagulants.[7] In cases of catastrophic antiphospholipid syndrome (CAPS), anticoagulants, in addition to corticosteroids and intravenous immunoglobulin, are used for treatment; however, immunosuppression outside of CAPS is controversial without other indications and would not be indicated for treatment of TMA in this case.\nA clinical diagnosis of TMA is an important consideration in the differential diagnosis because it carries potential therapeutic implications. TMA is both a clinical syndrome and a histologic definition (the latter demonstrated in the biopsy in this case). The clinical syndrome of TMA is a broad category and encompasses both primary and secondary causes. Manifestations include evidence of microangiopathic hemolytic anemia, thrombocytopenia, and end-organ injury. The histopathologic component demonstrates occlusive thrombus formation with characteristic abnormalities in the endothelium and vessel wall.[8]\nCauses of primary TMA refer to causes that are either genetic or acquired; these include primary TTP and complement-mediated hemolytic-uremic syndrome. TTP can be hereditary or acquired and is related to severe deficiencies of ADAMTS13 (due to autoantibody formation against the protein or acquired genetic abnormalities), which separates it from the other causes of TMA. The diagnosis of TTP ultimately hinges on testing of ADAMTS13 activity, because the clinical presentation can vary from nonspecific findings to substantial neurologic deficits. Mortality ranges between 5% and 16%,[9] which makes a timely diagnosis crucial for the initiation of emergent plasma exchange therapy, a mainstay of TTP treatment.[8,9,10] Patients with SLE or APS nephropathy can have evidence of systemic TMA. Complement-mediated TMA may require complement inhibition with eculizumab in addition to anticoagulation and immunosuppression and is important to consider in the differential diagnosis.\nThe other diagnosis to consider is acute interstitial nephritis (AIN). AIN can be drug-induced (occurring in more than 75% of cases) or related to other conditions, including autoimmune disorders (10%-15% of cases).[11] The criterion standard for the diagnosis of interstitial nephritis is renal biopsy, which demonstrates an infiltrate of inflammatory cells within the renal interstitium. This is often associated with edema and sparing of the glomeruli and blood vessels. Figure 2 shows interstitial nephritis in a different patient.\nFigure 2.\nUrinalysis typically demonstrates proteinuria, pyuria, and hematuria, although red cell casts are rare. Eosinophiluria is classically associated with AIN. The absence of the finding does not exclude the diagnosis, and its overall utility is limited; studies have demonstrated a positive predictive value of 38% and a negative predictive value of 74%.[12]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Internal Medicine Case Challenge: A Teacher’s Assistant With Bipolar Disorder Has Lung Problems"
},
{
"authors": "Jonathan Katz, MD; Shivani Garg, MD, MS",
"content": [
"The treatment of AIN involves removal of the offending agent (when drug-induced) or treatment of the underlying disorder. Although the evidence for empirical corticosteroid therapy for AIN (for drug-induced cases or cases of unknown etiology) has lacked large randomized, controlled trials, empirical use has been supported by small case studies.[12,13]",
"In conclusion, APS nephropathy is an important cause of renal dysfunction and is a key consideration in the differential for renal injury in both patients with and those without SLE. The diagnosis requires renal biopsy to distinguish it from other causes, including lupus nephritis, and treatment is dependent on the APS antibody profile. Patients with triple-positive APS require anticoagulation with warfarin and heparin. APS can present with associated TMA, and in treatment-refractory cases, APS TMA may require complement-specific therapies in addition to immunosuppression to treat the underlying disease process.",
"For the patient in this case, treatment with corticosteroids, mycophenolate, and hydroxychloroquine was started. The results of ADAMTS13 testing were within normal limits. She had a significant past medical history for positive lupus anticoagulant tests (12 weeks apart) with recurrent DVT; however, she did not receive a formal diagnosis of APS. Given her past medical history, lupus anticoagulant positivity, recurrent DVT, and now acute TMA in the kidneys, formal diagnoses of APS and acute APS nephropathy were confirmed. Thus, her regimen was transitioned at discharge to warfarin for long-term anticoagulation."
],
"date": "January 09, 2023",
"figures": [],
"markdown": "# Internal Medicine Case Challenge: A Teacher’s Assistant With Bipolar Disorder Has Lung Problems\n\n **Authors:** Jonathan Katz, MD; Shivani Garg, MD, MS \n **Date:** January 09, 2023\n\n ## Content\n\n The treatment of AIN involves removal of the offending agent (when drug-induced) or treatment of the underlying disorder. Although the evidence for empirical corticosteroid therapy for AIN (for drug-induced cases or cases of unknown etiology) has lacked large randomized, controlled trials, empirical use has been supported by small case studies.[12,13]\nIn conclusion, APS nephropathy is an important cause of renal dysfunction and is a key consideration in the differential for renal injury in both patients with and those without SLE. The diagnosis requires renal biopsy to distinguish it from other causes, including lupus nephritis, and treatment is dependent on the APS antibody profile. Patients with triple-positive APS require anticoagulation with warfarin and heparin. APS can present with associated TMA, and in treatment-refractory cases, APS TMA may require complement-specific therapies in addition to immunosuppression to treat the underlying disease process.\nFor the patient in this case, treatment with corticosteroids, mycophenolate, and hydroxychloroquine was started. The results of ADAMTS13 testing were within normal limits. She had a significant past medical history for positive lupus anticoagulant tests (12 weeks apart) with recurrent DVT; however, she did not receive a formal diagnosis of APS. Given her past medical history, lupus anticoagulant positivity, recurrent DVT, and now acute TMA in the kidneys, formal diagnoses of APS and acute APS nephropathy were confirmed. Thus, her regimen was transitioned at discharge to warfarin for long-term anticoagulation.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1751274,
"choiceText": "ADAMTS13 activity testing",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751275,
"choiceText": "dsDNA antibody testing",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751276,
"choiceText": "C3/C4 testing",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751277,
"choiceText": "Both dsDNA antibody testing and C3/C4 testing",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nADAMTS13 activity testing should be included in her workup. Secondary causes of TMA need to be excluded because a positive workup would necessitate a change in her therapy.\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 565694,
"questionText": "A 68-year-old woman with a history of recurrent DVT and lupus anticoagulant positivity (APS) and a new diagnosis of SLE is admitted with worsening renal function. The laboratory investigation is notable for concurrent worsening anemia, thrombocytopenia, and an elevated total bilirubin level with a positive Coombs test. She undergoes renal biopsy, and intravenous methylprednisolone is started, in addition to hydroxychloroquine and mycophenolate mofetil. Which is the most helpful test to include in her workup to assist with differential diagnoses?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1751278,
"choiceText": "Aspirin",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751279,
"choiceText": "Warfarin",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751280,
"choiceText": "Rivaroxaban",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751281,
"choiceText": "No anticoagulation is needed",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "According to the 2021 KDIGO guidelines, patients with a history of triple positivity (two positive serum IgG antiphospholipid antibody test results and one positive functional plasma lupus anticoagulant test result) should receive warfarin therapy for anticoagulation regardless of a history of DVT.<sup>[6]</sup> Patients who do not achieve an international normalized ratio goal of 2-3 despite compliance could be considered for apixaban therapy, although supporting data are limited.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 565695,
"questionText": "The results of the aforementioned patient's ADAMTS13 activity testing are negative. Her dsDNA antibody level is elevated, and her C3 and C4 levels are low. Further testing reveals positive results for lupus anticoagulant, cardiolipin antibody, and beta-2 glycoprotein antibody. Renal biopsy findings are consistent with a diagnosis of APS nephropathy. Heparin is started for anticoagulation. What is the most appropriate regimen to transition to at discharge?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Internal Medicine Case Challenge: A Teacher’s Assistant With Bipolar Disorder Has Lung Problems"
},
{
"authors": "Jonathan Katz, MD; Shivani Garg, MD, MS",
"content": [
"Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult."
],
"date": "January 09, 2023",
"figures": [],
"markdown": "# Internal Medicine Case Challenge: A Teacher’s Assistant With Bipolar Disorder Has Lung Problems\n\n **Authors:** Jonathan Katz, MD; Shivani Garg, MD, MS \n **Date:** January 09, 2023\n\n ## Content\n\n Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult.\n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1751274,
"choiceText": "ADAMTS13 activity testing",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751275,
"choiceText": "dsDNA antibody testing",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751276,
"choiceText": "C3/C4 testing",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751277,
"choiceText": "Both dsDNA antibody testing and C3/C4 testing",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nADAMTS13 activity testing should be included in her workup. Secondary causes of TMA need to be excluded because a positive workup would necessitate a change in her therapy.\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 565694,
"questionText": "A 68-year-old woman with a history of recurrent DVT and lupus anticoagulant positivity (APS) and a new diagnosis of SLE is admitted with worsening renal function. The laboratory investigation is notable for concurrent worsening anemia, thrombocytopenia, and an elevated total bilirubin level with a positive Coombs test. She undergoes renal biopsy, and intravenous methylprednisolone is started, in addition to hydroxychloroquine and mycophenolate mofetil. Which is the most helpful test to include in her workup to assist with differential diagnoses?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1751278,
"choiceText": "Aspirin",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751279,
"choiceText": "Warfarin",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751280,
"choiceText": "Rivaroxaban",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751281,
"choiceText": "No anticoagulation is needed",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "According to the 2021 KDIGO guidelines, patients with a history of triple positivity (two positive serum IgG antiphospholipid antibody test results and one positive functional plasma lupus anticoagulant test result) should receive warfarin therapy for anticoagulation regardless of a history of DVT.<sup>[6]</sup> Patients who do not achieve an international normalized ratio goal of 2-3 despite compliance could be considered for apixaban therapy, although supporting data are limited.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 565695,
"questionText": "The results of the aforementioned patient's ADAMTS13 activity testing are negative. Her dsDNA antibody level is elevated, and her C3 and C4 levels are low. Further testing reveals positive results for lupus anticoagulant, cardiolipin antibody, and beta-2 glycoprotein antibody. Renal biopsy findings are consistent with a diagnosis of APS nephropathy. Heparin is started for anticoagulation. What is the most appropriate regimen to transition to at discharge?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Internal Medicine Case Challenge: A Teacher’s Assistant With Bipolar Disorder Has Lung Problems"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1751269,
"choiceText": "Lupus nephritis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751270,
"choiceText": "Interstitial nephritis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751271,
"choiceText": "Antiphospholipid syndrome nephropathy",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751272,
"choiceText": "Thrombotic thrombocytopenic purpura",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 565693,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1751274,
"choiceText": "ADAMTS13 activity testing",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751275,
"choiceText": "dsDNA antibody testing",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751276,
"choiceText": "C3/C4 testing",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751277,
"choiceText": "Both dsDNA antibody testing and C3/C4 testing",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nADAMTS13 activity testing should be included in her workup. Secondary causes of TMA need to be excluded because a positive workup would necessitate a change in her therapy.\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 565694,
"questionText": "A 68-year-old woman with a history of recurrent DVT and lupus anticoagulant positivity (APS) and a new diagnosis of SLE is admitted with worsening renal function. The laboratory investigation is notable for concurrent worsening anemia, thrombocytopenia, and an elevated total bilirubin level with a positive Coombs test. She undergoes renal biopsy, and intravenous methylprednisolone is started, in addition to hydroxychloroquine and mycophenolate mofetil. Which is the most helpful test to include in her workup to assist with differential diagnoses?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1751278,
"choiceText": "Aspirin",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751279,
"choiceText": "Warfarin",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751280,
"choiceText": "Rivaroxaban",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751281,
"choiceText": "No anticoagulation is needed",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "According to the 2021 KDIGO guidelines, patients with a history of triple positivity (two positive serum IgG antiphospholipid antibody test results and one positive functional plasma lupus anticoagulant test result) should receive warfarin therapy for anticoagulation regardless of a history of DVT.<sup>[6]</sup> Patients who do not achieve an international normalized ratio goal of 2-3 despite compliance could be considered for apixaban therapy, although supporting data are limited.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 565695,
"questionText": "The results of the aforementioned patient's ADAMTS13 activity testing are negative. Her dsDNA antibody level is elevated, and her C3 and C4 levels are low. Further testing reveals positive results for lupus anticoagulant, cardiolipin antibody, and beta-2 glycoprotein antibody. Renal biopsy findings are consistent with a diagnosis of APS nephropathy. Heparin is started for anticoagulation. What is the most appropriate regimen to transition to at discharge?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
984950 | /viewarticle/984950 | [
{
"authors": "Heidi Moawad, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 27-year-old man reports recent balance problems and several episodes of bladder incontinence. He is a factory assembly worker and has no difficulty using his hands for repetitive tasks at work; however, he feels off balance when he walks. He says that he is not dizzy. He explains that his legs feel stiff, and it seems as if he is going to fall. He has had at least three episodes of bladder incontinence on different occasions. All the episodes occurred during the day, when he already knew that he needed to urinate but had not had a break to use the toilet.",
"He says that he has been healthy and athletic and did well in school. He went to a vocational program during his last year of school and has done well in his job, with no complaints or interpersonal issues. He lives with his parents and his younger brother. His parents are healthy, and he has a maternal uncle who uses a wheelchair as the result of a work injury.",
"He drinks a few beers each week and does not smoke. He played on a community baseball team a year ago, but he does not think he would be able to play at the local community level with his current balance problems and leg stiffness."
],
"date": "January 09, 2023",
"figures": [],
"markdown": "# A 27-Year-Old Factory Worker With Incontinence and Imbalance\n\n **Authors:** Heidi Moawad, MD \n **Date:** January 09, 2023\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 27-year-old man reports recent balance problems and several episodes of bladder incontinence. He is a factory assembly worker and has no difficulty using his hands for repetitive tasks at work; however, he feels off balance when he walks. He says that he is not dizzy. He explains that his legs feel stiff, and it seems as if he is going to fall. He has had at least three episodes of bladder incontinence on different occasions. All the episodes occurred during the day, when he already knew that he needed to urinate but had not had a break to use the toilet.\nHe says that he has been healthy and athletic and did well in school. He went to a vocational program during his last year of school and has done well in his job, with no complaints or interpersonal issues. He lives with his parents and his younger brother. His parents are healthy, and he has a maternal uncle who uses a wheelchair as the result of a work injury.\nHe drinks a few beers each week and does not smoke. He played on a community baseball team a year ago, but he does not think he would be able to play at the local community level with his current balance problems and leg stiffness.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A 27-Year-Old Factory Worker With Incontinence and Imbalance"
},
{
"authors": "Heidi Moawad, MD",
"content": [
"Upon physical examination, the patient appears thin and is in no acute distress. He is alert and cooperative, and his mental status examination is normal. His vital signs are also normal.",
"Upon neurologic examination, he has brisk reflexes of his lower extremities with upgoing toes and normal reflexes of his upper extremities. His strength is 5/5 in all four extremities with some spasticity, which is worse in his lower extremities. The coordination examination is normal, with intact finger to nose and rapid alternating movements. His sensory examination is normal to light touch, pinprick, vibration, and temperature. The cranial nerve examination is completely normal, with no nystagmus and normal pupils and facial movements.",
"Upon systemic examination, the patient has a normal heart rhythm and clear, regular breathing sounds. The abdominal examination is normal, with no tenderness. His skin appears normal.",
"A complete blood cell count and electrolyte values are normal. Lumbar spine MRI shows demyelination of the lateral dorsal columns at several levels, on both the right and left sides.",
"His physician orders measurement of plasma very long-chain fatty acid (VLCFA) levels. The patient's C26:0 level (a VLCFA) is 2.00 μmol/L (reference range, < 1.46 μmol/L). After evaluating the VLCFA levels, his physician orders a morning cortisol level, which is 102 nmol/L (reference range, 130-640 nmol/L), and an adrenocorticotropic hormone level, which is 97 pmol/L (reference range, ≤ 11 pmol/L)."
],
"date": "January 09, 2023",
"figures": [],
"markdown": "# A 27-Year-Old Factory Worker With Incontinence and Imbalance\n\n **Authors:** Heidi Moawad, MD \n **Date:** January 09, 2023\n\n ## Content\n\n Upon physical examination, the patient appears thin and is in no acute distress. He is alert and cooperative, and his mental status examination is normal. His vital signs are also normal.\nUpon neurologic examination, he has brisk reflexes of his lower extremities with upgoing toes and normal reflexes of his upper extremities. His strength is 5/5 in all four extremities with some spasticity, which is worse in his lower extremities. The coordination examination is normal, with intact finger to nose and rapid alternating movements. His sensory examination is normal to light touch, pinprick, vibration, and temperature. The cranial nerve examination is completely normal, with no nystagmus and normal pupils and facial movements.\nUpon systemic examination, the patient has a normal heart rhythm and clear, regular breathing sounds. The abdominal examination is normal, with no tenderness. His skin appears normal.\nA complete blood cell count and electrolyte values are normal. Lumbar spine MRI shows demyelination of the lateral dorsal columns at several levels, on both the right and left sides.\nHis physician orders measurement of plasma very long-chain fatty acid (VLCFA) levels. The patient's C26:0 level (a VLCFA) is 2.00 μmol/L (reference range, < 1.46 μmol/L). After evaluating the VLCFA levels, his physician orders a morning cortisol level, which is 102 nmol/L (reference range, 130-640 nmol/L), and an adrenocorticotropic hormone level, which is 97 pmol/L (reference range, ≤ 11 pmol/L).\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1751149,
"choiceText": "Multiple sclerosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751150,
"choiceText": "Familial hypercholesterolemia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751151,
"choiceText": "Adrenomyeloneuropathy",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751152,
"choiceText": "Adrenoleukodystrophy",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 565660,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 27-Year-Old Factory Worker With Incontinence and Imbalance"
},
{
"authors": "Heidi Moawad, MD",
"content": [
"This patient has adrenomyeloneuropathy. His age of onset is older and his symptom severity is milder than the pattern seen with adrenoleukodystrophy. Although he has demyelination and an age of onset that is consistent with multiple sclerosis (MS), his changes in very low-density lipoprotein and adrenal hormone laboratory values are not typically observed in patients with MS. He has a familial disorder; however, familial hypercholesterolemia causes different blood test findings (high cholesterol levels) without neurologic symptoms.",
"This young man's maternal uncle was also suspected to have adrenomyeloneuropathy; his wheelchair dependence could be due to his disease, in that an injury may have caused a sudden decline in neurologic function. The patient and his uncle were later tested, and both had the same mutation in the ABCD1 gene on their X chromosome. Further testing of the uncle showed a few areas of white-matter demyelination on his brain MRI scan, as well as adrenal insufficiency.",
"Adrenomyeloneuropathy is a demyelinating condition that primarily affects the spinal cord and adrenal glands. It is an X-linked recessive disorder caused by a change in the ABCD1 gene on the X chromosome.[1] Several different alterations in this gene have been identified in association with the disease. The condition is usually inherited, but sporadic cases can occur as well. It is a rare disorder, and because it is caused by a mutation on the X chromosome, it is generally diagnosed in males. Females can develop the condition, although it is much less common.",
"The genetic defect results in an abnormality of a transporter protein that normally transports VLCFAs in the course of their breakdown process. The transporter protein deficiency leads to a buildup of VLCFAs. This accumulation is believed to produce inflammation and demyelination of white matter in the central nervous system, as well as damage to the adrenal glands and the testicles. It is not known how long it takes for the metabolic changes and the inflammatory process to cause permanent tissue damage."
],
"date": "January 09, 2023",
"figures": [],
"markdown": "# A 27-Year-Old Factory Worker With Incontinence and Imbalance\n\n **Authors:** Heidi Moawad, MD \n **Date:** January 09, 2023\n\n ## Content\n\n This patient has adrenomyeloneuropathy. His age of onset is older and his symptom severity is milder than the pattern seen with adrenoleukodystrophy. Although he has demyelination and an age of onset that is consistent with multiple sclerosis (MS), his changes in very low-density lipoprotein and adrenal hormone laboratory values are not typically observed in patients with MS. He has a familial disorder; however, familial hypercholesterolemia causes different blood test findings (high cholesterol levels) without neurologic symptoms.\nThis young man's maternal uncle was also suspected to have adrenomyeloneuropathy; his wheelchair dependence could be due to his disease, in that an injury may have caused a sudden decline in neurologic function. The patient and his uncle were later tested, and both had the same mutation in the ABCD1 gene on their X chromosome. Further testing of the uncle showed a few areas of white-matter demyelination on his brain MRI scan, as well as adrenal insufficiency.\nAdrenomyeloneuropathy is a demyelinating condition that primarily affects the spinal cord and adrenal glands. It is an X-linked recessive disorder caused by a change in the ABCD1 gene on the X chromosome.[1] Several different alterations in this gene have been identified in association with the disease. The condition is usually inherited, but sporadic cases can occur as well. It is a rare disorder, and because it is caused by a mutation on the X chromosome, it is generally diagnosed in males. Females can develop the condition, although it is much less common.\nThe genetic defect results in an abnormality of a transporter protein that normally transports VLCFAs in the course of their breakdown process. The transporter protein deficiency leads to a buildup of VLCFAs. This accumulation is believed to produce inflammation and demyelination of white matter in the central nervous system, as well as damage to the adrenal glands and the testicles. It is not known how long it takes for the metabolic changes and the inflammatory process to cause permanent tissue damage.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1751149,
"choiceText": "Multiple sclerosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751150,
"choiceText": "Familial hypercholesterolemia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751151,
"choiceText": "Adrenomyeloneuropathy",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751152,
"choiceText": "Adrenoleukodystrophy",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 565660,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 27-Year-Old Factory Worker With Incontinence and Imbalance"
},
{
"authors": "Heidi Moawad, MD",
"content": [
"The demyelinating changes result in neurologic impairment, manifested as irreversible weakness, ataxia, spasticity, and bladder incontinence. The adrenal insufficiency causes hypotension and electrolyte abnormalities, and the testicular involvement causes sexual dysfunction, and possibly infertility as well. Some patients also have mild or moderate peripheral neuropathy, which can cause sensory and motor symptoms. This is believed to be caused by the same process of demyelination.[2]",
"Adrenomyeloneuropathy has a widely heterogeneous presentation: Some males develop effects that include severe weakness, motor spasticity, gait abnormalities, and seizures, whereas others may have only mild sensory or motor changes.[3] Heterozygous females generally are asymptomatic or may have mild symptoms. The age of onset is typically in the third or fourth decades of life, with a slow progression.",
"The genetic defect and the pathogenesis of adrenomyeloneuropathy are identical to those of cerebral adrenoleukodystrophy. The latter begins during childhood and causes rapid neurologic deterioration, vision loss, seizures, and early death. Figure 1 is an MRI scan that shows adrenoleukodystrophy in a different patient.",
"Figure 1.",
"It is not clear why some children who have the mutation develop symptoms early in life with cerebral involvement and rapid progression, whereas others develop symptoms later in life without cerebral involvement and a slower progression. In fact, adrenomyeloneuropathy is considered a phenotypic variation of adrenoleukodystrophy.[4] Other phenotypes of the same genetic defect include an adult-onset cerebral disorder and an Addison-only variant.",
"Young men with a diagnosis of adrenomyeloneuropathy may have a normal lifespan, especially if they receive medical care to prevent the complications associated with neurologic impairment. An estimated 50% of these patients have mild to moderate cerebral involvement and may develop cognitive decline or vision changes, but they typically do not have as severe a decline as boys whose symptoms begin in early childhood. Infant screening for the genetic defect is standard in several states throughout the United States; however, it is not possible to predict whether a young child with the defect will have a milder or more serious form of the disorder.[5]",
"Upon physical examination, patients generally have spastic paraparesis by the time they begin to notice their symptoms. Patients may also have motor weakness, sensory changes, or evidence of cerebral involvement noted upon physical examination. Some conditions commonly considered in the differential diagnosis include MS, muscular dystrophy, myopathy, and peripheral neuropathy.",
"Patients may have evidence of demyelination or axonal degeneration in the corticospinal tract regions of the lumbar and thoracic spinal cord, which is visible on MRI. Electromyography and nerve conduction studies may show nonspecific signs of peripheral neuropathy, which are not likely to help in the diagnosis. Muscle or nerve biopsy would not be expected to show changes or to be diagnostic.",
"VLCFA levels may be elevated on a blood test, and adrenal hormone levels may be low. Genetic testing is diagnostic. Patients who have a family history of the condition or who screened positive before symptom onset might have a more rapid diagnosis owing to a high level of clinical suspicion. However, there can be a delay in ordering these tests because adrenomyeloneuropathy is not common. The incidence of adrenoleukodystrophy ranges from 1:15,000 to 1:20,000, and the approximate incidence of the adrenomyeloneuropathy phenotype is 1:42,000.[6]",
"No effective treatment for either manifestation of the condition has been established. Early stem cell transplantation has been used with some success. The mechanism for the possible efficacy of stem cell transplantation is not well understood; it appears to have an effect on demyelination in this setting.[6] Gene therapy is currently being investigated as an option. Stem cell transplantation and gene therapy are both intended to be curative, whereas other treatments are used to relieve symptoms and must be continued throughout a patient's life.",
"Figure 2. Stem cell."
],
"date": "January 09, 2023",
"figures": [],
"markdown": "# A 27-Year-Old Factory Worker With Incontinence and Imbalance\n\n **Authors:** Heidi Moawad, MD \n **Date:** January 09, 2023\n\n ## Content\n\n The demyelinating changes result in neurologic impairment, manifested as irreversible weakness, ataxia, spasticity, and bladder incontinence. The adrenal insufficiency causes hypotension and electrolyte abnormalities, and the testicular involvement causes sexual dysfunction, and possibly infertility as well. Some patients also have mild or moderate peripheral neuropathy, which can cause sensory and motor symptoms. This is believed to be caused by the same process of demyelination.[2]\nAdrenomyeloneuropathy has a widely heterogeneous presentation: Some males develop effects that include severe weakness, motor spasticity, gait abnormalities, and seizures, whereas others may have only mild sensory or motor changes.[3] Heterozygous females generally are asymptomatic or may have mild symptoms. The age of onset is typically in the third or fourth decades of life, with a slow progression.\nThe genetic defect and the pathogenesis of adrenomyeloneuropathy are identical to those of cerebral adrenoleukodystrophy. The latter begins during childhood and causes rapid neurologic deterioration, vision loss, seizures, and early death. Figure 1 is an MRI scan that shows adrenoleukodystrophy in a different patient.\nFigure 1.\nIt is not clear why some children who have the mutation develop symptoms early in life with cerebral involvement and rapid progression, whereas others develop symptoms later in life without cerebral involvement and a slower progression. In fact, adrenomyeloneuropathy is considered a phenotypic variation of adrenoleukodystrophy.[4] Other phenotypes of the same genetic defect include an adult-onset cerebral disorder and an Addison-only variant.\nYoung men with a diagnosis of adrenomyeloneuropathy may have a normal lifespan, especially if they receive medical care to prevent the complications associated with neurologic impairment. An estimated 50% of these patients have mild to moderate cerebral involvement and may develop cognitive decline or vision changes, but they typically do not have as severe a decline as boys whose symptoms begin in early childhood. Infant screening for the genetic defect is standard in several states throughout the United States; however, it is not possible to predict whether a young child with the defect will have a milder or more serious form of the disorder.[5]\nUpon physical examination, patients generally have spastic paraparesis by the time they begin to notice their symptoms. Patients may also have motor weakness, sensory changes, or evidence of cerebral involvement noted upon physical examination. Some conditions commonly considered in the differential diagnosis include MS, muscular dystrophy, myopathy, and peripheral neuropathy.\nPatients may have evidence of demyelination or axonal degeneration in the corticospinal tract regions of the lumbar and thoracic spinal cord, which is visible on MRI. Electromyography and nerve conduction studies may show nonspecific signs of peripheral neuropathy, which are not likely to help in the diagnosis. Muscle or nerve biopsy would not be expected to show changes or to be diagnostic.\nVLCFA levels may be elevated on a blood test, and adrenal hormone levels may be low. Genetic testing is diagnostic. Patients who have a family history of the condition or who screened positive before symptom onset might have a more rapid diagnosis owing to a high level of clinical suspicion. However, there can be a delay in ordering these tests because adrenomyeloneuropathy is not common. The incidence of adrenoleukodystrophy ranges from 1:15,000 to 1:20,000, and the approximate incidence of the adrenomyeloneuropathy phenotype is 1:42,000.[6]\nNo effective treatment for either manifestation of the condition has been established. Early stem cell transplantation has been used with some success. The mechanism for the possible efficacy of stem cell transplantation is not well understood; it appears to have an effect on demyelination in this setting.[6] Gene therapy is currently being investigated as an option. Stem cell transplantation and gene therapy are both intended to be curative, whereas other treatments are used to relieve symptoms and must be continued throughout a patient's life.\nFigure 2. Stem cell.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A 27-Year-Old Factory Worker With Incontinence and Imbalance"
},
{
"authors": "Heidi Moawad, MD",
"content": [
"Steroid replacement treats the adrenal dysfunction and is not expected to have any effect on the neurologic symptoms or disease process. Muscle relaxants, physical therapy, and intrathecal baclofen are used to manage spastic paraparesis, which the young man in this case appears to be developing.",
"Functional electrical stimulation has been examined as a potential symptomatic treatment for this condition. One small study showed that this treatment, which uses externally applied electrical stimulation to induce functional movement in weak muscles, can benefit some patients with adrenomyeloneuropathy who have difficulty walking. The treatment helped maintain walking speed, at least for the 2-year study duration.[7]",
"Dietary modification with Lorenzo's oil has not proved effective in reversing the disease. This supplement contains erucic acid and oleic acid, which normalize the VLCFA levels in the blood but do not improve symptoms in patients with adrenomyeloneuropathy or adrenoleukodystrophy. The lack of improvement despite normalization of the VLCFA levels suggests that the disease involves neuronal death in addition to the demyelination.",
"The duration of the effects of central nervous system demyelination can vary. The effects of demyelination are usually partially reversible with MS, but they are permanent and progressive with adrenomyeloneuropathy and cerebral adrenoleukodystrophy.",
"The patient in this case was treated with physical therapy for his balance problems, and he had bladder physical therapy to manage and prevent incontinence. These treatments were both effective, and he did not have any further neurologic decline. He required ongoing treatment for adrenal insufficiency with steroid hormones, with occasional dosing adjustments."
],
"date": "January 09, 2023",
"figures": [],
"markdown": "# A 27-Year-Old Factory Worker With Incontinence and Imbalance\n\n **Authors:** Heidi Moawad, MD \n **Date:** January 09, 2023\n\n ## Content\n\n Steroid replacement treats the adrenal dysfunction and is not expected to have any effect on the neurologic symptoms or disease process. Muscle relaxants, physical therapy, and intrathecal baclofen are used to manage spastic paraparesis, which the young man in this case appears to be developing.\nFunctional electrical stimulation has been examined as a potential symptomatic treatment for this condition. One small study showed that this treatment, which uses externally applied electrical stimulation to induce functional movement in weak muscles, can benefit some patients with adrenomyeloneuropathy who have difficulty walking. The treatment helped maintain walking speed, at least for the 2-year study duration.[7]\nDietary modification with Lorenzo's oil has not proved effective in reversing the disease. This supplement contains erucic acid and oleic acid, which normalize the VLCFA levels in the blood but do not improve symptoms in patients with adrenomyeloneuropathy or adrenoleukodystrophy. The lack of improvement despite normalization of the VLCFA levels suggests that the disease involves neuronal death in addition to the demyelination.\nThe duration of the effects of central nervous system demyelination can vary. The effects of demyelination are usually partially reversible with MS, but they are permanent and progressive with adrenomyeloneuropathy and cerebral adrenoleukodystrophy.\nThe patient in this case was treated with physical therapy for his balance problems, and he had bladder physical therapy to manage and prevent incontinence. These treatments were both effective, and he did not have any further neurologic decline. He required ongoing treatment for adrenal insufficiency with steroid hormones, with occasional dosing adjustments.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1751153,
"choiceText": "It can cause inflammatory damage to the lateral columns in the spinal cord",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751154,
"choiceText": "The condition could predispose to an injury, and additional physical limitations may result from the injury",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751155,
"choiceText": "An injury may trigger demyelination of the central nervous system",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751156,
"choiceText": "It could precipitate an alteration of the <i>ABCD1</i> gene",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "An injury would not be expected to exacerbate the underlying disease process. The changes that occur with adrenomyeloneuropathy are caused by a distinct pathologic process, and an injury would not be expected to trigger a genetic change, inflammatory damage, or demyelination. <br><br>\r\nSometimes the effects of adrenomyeloneuropathy may be subtle, which could predispose a patient to an injury. Furthermore, injuries can temporarily or permanently worsen a patient's overall physical abilities, potentially resulting in more pronounced physical disability.\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 565661,
"questionText": "Which of these would best explain how a work injury could be associated with physical function in a patient with adrenomyeloneuropathy?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1751157,
"choiceText": "Patients can start steroid treatment when asymptomatic",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751158,
"choiceText": "Patients can initiate physical therapy before symptom onset ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751159,
"choiceText": "Patients can begin a treatment algorithm involving gene therapy",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751160,
"choiceText": "Patients can be regularly assessed for development of early signs of motor changes",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nScreening for the genetic defect that causes phenotypic variations of adrenoleukodystrophy can identify patients who could eventually develop symptoms. Patients would not benefit from steroid treatment unless they experience dysfunction of the adrenal gland. Similarly, physical therapy would not be beneficial unless motor deficits develop. <br><br>\r\nPatients who have the genetic defect and who do not develop early-onset adrenoleukodystrophy could be followed up with frequent medical examinations to identify early signs of motor changes characteristic of adrenomyeloneuropathy. They may be provided with education about early symptoms so that they can seek medical attention if symptoms develop. There is not an established algorithm regarding treatment with stem cell transplant or gene therapy. Conditions identified by infant genetic screening do not always have a clear-cut treatment algorithm.\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 565662,
"questionText": "What is the benefit of screening for adrenoleukodystrophy?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 27-Year-Old Factory Worker With Incontinence and Imbalance"
},
{
"authors": "Heidi Moawad, MD",
"content": [
"Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult."
],
"date": "January 09, 2023",
"figures": [],
"markdown": "# A 27-Year-Old Factory Worker With Incontinence and Imbalance\n\n **Authors:** Heidi Moawad, MD \n **Date:** January 09, 2023\n\n ## Content\n\n Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult.\n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1751153,
"choiceText": "It can cause inflammatory damage to the lateral columns in the spinal cord",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751154,
"choiceText": "The condition could predispose to an injury, and additional physical limitations may result from the injury",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751155,
"choiceText": "An injury may trigger demyelination of the central nervous system",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751156,
"choiceText": "It could precipitate an alteration of the <i>ABCD1</i> gene",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "An injury would not be expected to exacerbate the underlying disease process. The changes that occur with adrenomyeloneuropathy are caused by a distinct pathologic process, and an injury would not be expected to trigger a genetic change, inflammatory damage, or demyelination. <br><br>\r\nSometimes the effects of adrenomyeloneuropathy may be subtle, which could predispose a patient to an injury. Furthermore, injuries can temporarily or permanently worsen a patient's overall physical abilities, potentially resulting in more pronounced physical disability.\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 565661,
"questionText": "Which of these would best explain how a work injury could be associated with physical function in a patient with adrenomyeloneuropathy?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1751157,
"choiceText": "Patients can start steroid treatment when asymptomatic",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751158,
"choiceText": "Patients can initiate physical therapy before symptom onset ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751159,
"choiceText": "Patients can begin a treatment algorithm involving gene therapy",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751160,
"choiceText": "Patients can be regularly assessed for development of early signs of motor changes",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nScreening for the genetic defect that causes phenotypic variations of adrenoleukodystrophy can identify patients who could eventually develop symptoms. Patients would not benefit from steroid treatment unless they experience dysfunction of the adrenal gland. Similarly, physical therapy would not be beneficial unless motor deficits develop. <br><br>\r\nPatients who have the genetic defect and who do not develop early-onset adrenoleukodystrophy could be followed up with frequent medical examinations to identify early signs of motor changes characteristic of adrenomyeloneuropathy. They may be provided with education about early symptoms so that they can seek medical attention if symptoms develop. There is not an established algorithm regarding treatment with stem cell transplant or gene therapy. Conditions identified by infant genetic screening do not always have a clear-cut treatment algorithm.\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 565662,
"questionText": "What is the benefit of screening for adrenoleukodystrophy?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 27-Year-Old Factory Worker With Incontinence and Imbalance"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1751149,
"choiceText": "Multiple sclerosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751150,
"choiceText": "Familial hypercholesterolemia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751151,
"choiceText": "Adrenomyeloneuropathy",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751152,
"choiceText": "Adrenoleukodystrophy",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 565660,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1751153,
"choiceText": "It can cause inflammatory damage to the lateral columns in the spinal cord",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751154,
"choiceText": "The condition could predispose to an injury, and additional physical limitations may result from the injury",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751155,
"choiceText": "An injury may trigger demyelination of the central nervous system",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751156,
"choiceText": "It could precipitate an alteration of the <i>ABCD1</i> gene",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "An injury would not be expected to exacerbate the underlying disease process. The changes that occur with adrenomyeloneuropathy are caused by a distinct pathologic process, and an injury would not be expected to trigger a genetic change, inflammatory damage, or demyelination. <br><br>\r\nSometimes the effects of adrenomyeloneuropathy may be subtle, which could predispose a patient to an injury. Furthermore, injuries can temporarily or permanently worsen a patient's overall physical abilities, potentially resulting in more pronounced physical disability.\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 565661,
"questionText": "Which of these would best explain how a work injury could be associated with physical function in a patient with adrenomyeloneuropathy?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1751157,
"choiceText": "Patients can start steroid treatment when asymptomatic",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751158,
"choiceText": "Patients can initiate physical therapy before symptom onset ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751159,
"choiceText": "Patients can begin a treatment algorithm involving gene therapy",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1751160,
"choiceText": "Patients can be regularly assessed for development of early signs of motor changes",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nScreening for the genetic defect that causes phenotypic variations of adrenoleukodystrophy can identify patients who could eventually develop symptoms. Patients would not benefit from steroid treatment unless they experience dysfunction of the adrenal gland. Similarly, physical therapy would not be beneficial unless motor deficits develop. <br><br>\r\nPatients who have the genetic defect and who do not develop early-onset adrenoleukodystrophy could be followed up with frequent medical examinations to identify early signs of motor changes characteristic of adrenomyeloneuropathy. They may be provided with education about early symptoms so that they can seek medical attention if symptoms develop. There is not an established algorithm regarding treatment with stem cell transplant or gene therapy. Conditions identified by infant genetic screening do not always have a clear-cut treatment algorithm.\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 565662,
"questionText": "What is the benefit of screening for adrenoleukodystrophy?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
724047 | /viewarticle/724047 | [
{
"authors": "Jansen Tiongson, MD; Lisa Chan, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to recognize accurately. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"The emergency department (ED) receives a paramedic call reporting a 10-minute estimated time of arrival for a 17-year-old boy who was found in cardiac arrest after a blow to the chest. The patient has regained spontaneous circulation and is currently awake and alert. A rhythm strip faxed to the ED before the patient's arrival shows ventricular fibrillation, with subsequent conversion to a normal sinus rhythm after defibrillation with 200 J (Figure 1).",
"Figure 1.",
"The prehospital personnel further report that the patient, a center outfielder for a local baseball team, was trying to catch a baseball when one of his teammates accidentally ran into him, elbowing him in the middle of his chest. The patient immediately dropped to the ground, was unresponsive, and showed no spontaneous movement.",
"His coach immediately initiated cardiopulmonary resuscitation (CPR) after no pulses were palpated. The paramedics arrived 5 minutes later and, as noted on the rhythm strip, found the patient to be in ventricular fibrillation. One 200-J countershock was administered converting the ventricular fibrillation to a normal sinus rhythm. The patient slowly regained consciousness. He was confused initially and was amnestic to the event.",
"Upon arrival at the ED, the patient reports mild anterior chest-wall pain but no shortness of breath, palpitations, weakness, or feelings of confusion. He states that he has never before fainted. The patient and his mother report no significant past medical or family history, including any arrhythmias, unexplained sudden deaths, or cardiac structural diseases. He states that he does not have a lower exercise tolerance than his teammates and does not smoke, drink, use medications, abuse illicit substances, or engage in doping practices."
],
"date": "December 16, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/724/047/724047-thumb1.png"
}
],
"markdown": "# Cardio Case Challenge: A 17-Year-Old in Cardiac Arrest After Collision Playing Sports\n\n **Authors:** Jansen Tiongson, MD; Lisa Chan, MD \n **Date:** December 16, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to recognize accurately. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nThe emergency department (ED) receives a paramedic call reporting a 10-minute estimated time of arrival for a 17-year-old boy who was found in cardiac arrest after a blow to the chest. The patient has regained spontaneous circulation and is currently awake and alert. A rhythm strip faxed to the ED before the patient's arrival shows ventricular fibrillation, with subsequent conversion to a normal sinus rhythm after defibrillation with 200 J (Figure 1).\nFigure 1.\nThe prehospital personnel further report that the patient, a center outfielder for a local baseball team, was trying to catch a baseball when one of his teammates accidentally ran into him, elbowing him in the middle of his chest. The patient immediately dropped to the ground, was unresponsive, and showed no spontaneous movement.\nHis coach immediately initiated cardiopulmonary resuscitation (CPR) after no pulses were palpated. The paramedics arrived 5 minutes later and, as noted on the rhythm strip, found the patient to be in ventricular fibrillation. One 200-J countershock was administered converting the ventricular fibrillation to a normal sinus rhythm. The patient slowly regained consciousness. He was confused initially and was amnestic to the event.\nUpon arrival at the ED, the patient reports mild anterior chest-wall pain but no shortness of breath, palpitations, weakness, or feelings of confusion. He states that he has never before fainted. The patient and his mother report no significant past medical or family history, including any arrhythmias, unexplained sudden deaths, or cardiac structural diseases. He states that he does not have a lower exercise tolerance than his teammates and does not smoke, drink, use medications, abuse illicit substances, or engage in doping practices.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Cardio Case Challenge: A 17-Year-Old in Cardiac Arrest After Collision Playing Sports"
},
{
"authors": "Jansen Tiongson, MD; Lisa Chan, MD",
"content": [
"Upon physical examination, the primary survey of his airway, breathing, and circulation is unremarkable. The patient has a blood pressure of 130/71 mm Hg and a heart rate of 106 beats/min, with a normal rhythm. His respirations are 28-30 breaths/min. The initial oxygen saturation is 83% while the patient is breathing room air, but it corrects to 98% with a non-rebreather mask. Soon after, his saturation improves to 99% with a 2-L nasal cannula.",
"His mentation is normal, and he is alert, with a Glasgow coma scale rating of 15. The skin examination reveals mild ecchymosis just anterior to his sternum. The lungs are clear to auscultation bilaterally, and the cardiac examination reveals a regular rate, with normal S1 and S2 heart sounds and no clicks, gallops, rubs, or murmurs. The abdominal and neurologic examinations are unremarkable. No hyperflexibility or marfanoid appearance is noted.",
"The patient is placed on a cardiac monitor upon arrival at the ED. A 12-lead electrocardiogram (ECG) reveals sinus tachycardia at a rate of 110 beats/min, with mild right-axis deviation. The QRS complex, QT interval, ST/T waves, and P waves are all normal (Figure 2). A portable, upright chest x-ray shows no signs of fractures, widening of the mediastinum, cardiomegaly, effusion, or pneumothorax (Figure 3).",
"Figure 2.",
"Figure 3.",
"A complete blood count is normal except for a mildly elevated white blood cell count of 13.6 ×103/µL (13.6 ×109/L). A metabolic panel is normal, including normal potassium and magnesium findings. The initial troponin I level is 0.04 ng/mL (0.04 µg/L; normal range, 0.02-0.04 ng/mL; indeterminate range, 0.05-0.30 ng/mL). A urine drug screen is negative. Computed tomography of the chest (Figure 4) is remarkable only for mild pulmonary and periportal edema.",
"Figure 4.",
"The patient is admitted to the pediatric intensive care unit (PICU) for continuous cardiac monitoring and cardiology consultation. An echocardiogram ordered in the ED is to be done in the PICU."
],
"date": "December 16, 2022",
"figures": [
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/thumbnail_library/724047-Thumb2rev.jpg"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/724/047/724047-thumb3.png"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/724/047/724047-thumb4.png"
}
],
"markdown": "# Cardio Case Challenge: A 17-Year-Old in Cardiac Arrest After Collision Playing Sports\n\n **Authors:** Jansen Tiongson, MD; Lisa Chan, MD \n **Date:** December 16, 2022\n\n ## Content\n\n Upon physical examination, the primary survey of his airway, breathing, and circulation is unremarkable. The patient has a blood pressure of 130/71 mm Hg and a heart rate of 106 beats/min, with a normal rhythm. His respirations are 28-30 breaths/min. The initial oxygen saturation is 83% while the patient is breathing room air, but it corrects to 98% with a non-rebreather mask. Soon after, his saturation improves to 99% with a 2-L nasal cannula.\nHis mentation is normal, and he is alert, with a Glasgow coma scale rating of 15. The skin examination reveals mild ecchymosis just anterior to his sternum. The lungs are clear to auscultation bilaterally, and the cardiac examination reveals a regular rate, with normal S1 and S2 heart sounds and no clicks, gallops, rubs, or murmurs. The abdominal and neurologic examinations are unremarkable. No hyperflexibility or marfanoid appearance is noted.\nThe patient is placed on a cardiac monitor upon arrival at the ED. A 12-lead electrocardiogram (ECG) reveals sinus tachycardia at a rate of 110 beats/min, with mild right-axis deviation. The QRS complex, QT interval, ST/T waves, and P waves are all normal (Figure 2). A portable, upright chest x-ray shows no signs of fractures, widening of the mediastinum, cardiomegaly, effusion, or pneumothorax (Figure 3).\nFigure 2.\nFigure 3.\nA complete blood count is normal except for a mildly elevated white blood cell count of 13.6 ×103/µL (13.6 ×109/L). A metabolic panel is normal, including normal potassium and magnesium findings. The initial troponin I level is 0.04 ng/mL (0.04 µg/L; normal range, 0.02-0.04 ng/mL; indeterminate range, 0.05-0.30 ng/mL). A urine drug screen is negative. Computed tomography of the chest (Figure 4) is remarkable only for mild pulmonary and periportal edema.\nFigure 4.\nThe patient is admitted to the pediatric intensive care unit (PICU) for continuous cardiac monitoring and cardiology consultation. An echocardiogram ordered in the ED is to be done in the PICU.\n\n ## Figures\n\n **Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 349495,
"choiceText": "Hypertrophic cardiomyopathy",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349496,
"choiceText": "Myocardial infarction",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349497,
"choiceText": "Commotio cordis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349498,
"choiceText": "Long-QT syndrome",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 99156,
"questionText": "Based on only these findings, which most likely led to this patient's cardiac arrest?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Cardio Case Challenge: A 17-Year-Old in Cardiac Arrest After Collision Playing Sports"
},
{
"authors": "Jansen Tiongson, MD; Lisa Chan, MD",
"content": [
"Commotio cordis (which is Latin for \"disturbance of the heart\") is, in essence, a concussion of the heart. Initially described as early as 1857, it is defined as an instantaneous cardiac arrest produced by a witnessed, nonpenetrating blow to the chest, in the absence of preexisting heart disease or identifiable morphologic injury to the sternum, ribs, chest wall, or heart. Commotio cordis is a diagnosis of exclusion. Other causes, such as myocardial infarction, electrolyte abnormality, long-QT syndrome, and hypertrophic obstructive cardiomyopathy (HOCM), must first be ruled out with examinations such as serial assessment of cardiac biomarkers and electrocardiography, electrolyte level testing, and echocardiography.[1,2]",
"Commotio cordis is believed to be underreported and underrecognized. Less than 30 cases are reported each year.[2] The vast majority of cases (95%) occur in boys. The mean age is 15 years, with few cases reported in individuals older than 20 years. This may be due to the fact that protection of the heart by subcutaneous fat, muscle bulk, and fully ossified ribs all become more common in adulthood.[2,3]"
],
"date": "December 16, 2022",
"figures": [],
"markdown": "# Cardio Case Challenge: A 17-Year-Old in Cardiac Arrest After Collision Playing Sports\n\n **Authors:** Jansen Tiongson, MD; Lisa Chan, MD \n **Date:** December 16, 2022\n\n ## Content\n\n Commotio cordis (which is Latin for \"disturbance of the heart\") is, in essence, a concussion of the heart. Initially described as early as 1857, it is defined as an instantaneous cardiac arrest produced by a witnessed, nonpenetrating blow to the chest, in the absence of preexisting heart disease or identifiable morphologic injury to the sternum, ribs, chest wall, or heart. Commotio cordis is a diagnosis of exclusion. Other causes, such as myocardial infarction, electrolyte abnormality, long-QT syndrome, and hypertrophic obstructive cardiomyopathy (HOCM), must first be ruled out with examinations such as serial assessment of cardiac biomarkers and electrocardiography, electrolyte level testing, and echocardiography.[1,2]\nCommotio cordis is believed to be underreported and underrecognized. Less than 30 cases are reported each year.[2] The vast majority of cases (95%) occur in boys. The mean age is 15 years, with few cases reported in individuals older than 20 years. This may be due to the fact that protection of the heart by subcutaneous fat, muscle bulk, and fully ossified ribs all become more common in adulthood.[2,3]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 349495,
"choiceText": "Hypertrophic cardiomyopathy",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349496,
"choiceText": "Myocardial infarction",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349497,
"choiceText": "Commotio cordis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349498,
"choiceText": "Long-QT syndrome",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 99156,
"questionText": "Based on only these findings, which most likely led to this patient's cardiac arrest?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Cardio Case Challenge: A 17-Year-Old in Cardiac Arrest After Collision Playing Sports"
},
{
"authors": "Jansen Tiongson, MD; Lisa Chan, MD",
"content": [
"A review of data from the US Commotio Cordis Registry (USCCR), in Minneapolis, Minnesota revealed that most cases were caused by a blow to the chest from an object used during an organized youth sporting event.[2] A baseball accounted for 53 of the cases, with a softball and a hockey puck the next most frequent, at 14 and 10 cases, respectively. Other documented sporting cases have been caused by blows delivered by body parts, such as an elbow, knee, foot, or fist hitting the anterior chest wall (5-6 cases of each).",
"Daily activities, including parent-child discipline (5 cases), and even a fall from monkey bars (1 case), can also lead to commotio cordis. Regardless of the mechanism, impacts resulting in commotio cordis are typically of low energy and velocity.[1,4] The victim may collapse immediately after the blow, but in as many as 50% of cases, a short delay occurs between the impact and collapse.",
"In 1930, George Schlomka was the first to describe the factors that can lead to arrhythmia after a moderate precordial impact. He believed that the force, location, and type of object causing the impact determined the type of injury and the subsequent risk for arrhythmia.[2] The force transmitted to the heart is directly related to the hardness of the striking object. Madias and colleagues[4] reported that the threshold speed of impact at which a standard baseball can cause ventricular fibrillation is between 25 and 30 miles per hour. However, when the speed is over 50 miles per hour, the likelihood of ventricular fibrillation actually decreases, although the possibility of myocardial contusion becomes greater. Furthermore, the authors stated that the impact must be directly over the heart near or just to the left of the sternum in order to instigate ventricular fibrillation. Impact on the center of the heart induced ventricular fibrillation in 30% of reported cases, compared with 13% and 4% at the left ventricular base and apex, respectively.[4]",
"The use of a standard baseball leads to the incidence rate reported above, but if the core of the ball is softer, then the rate for ventricular fibrillation drops. Link and colleagues[5] reported that changes to the cores of baseballs to make them softer led to a decrease in the rate of ventricular fibrillation with commotio cordis from 70% to 19%. As such, the use of safety baseballs with rubber cores of different degrees of hardness has been advocated to reduce the risk for such traumatic injury in young athletes.[3,5]",
"Not all impacts to the anterior chest lead to the ventricular fibrillation observed in commotio cordis. The impact must be delivered 10-30 milliseconds before the peak of the T wave in the cardiac cycle (Figure 5) in order to induce ventricular fibrillation.",
"Figure 5.",
"Induction is probably secondary to the activation of potassium-carrying ion channels via mechanoelectric coupling. The activation of these ion channels generates an inward current, thus locally augmenting repolarization and resulting in premature ventricular depolarization and the initiation of unstable ventricular arrhythmias. If impact occurs during other portions of the cardiac cycle, different conduction disturbances, such as heart block, bundle branch block, or transient ST segment elevation, may be induced.[2,4,5]"
],
"date": "December 16, 2022",
"figures": [
{
"caption": "Figure 5.",
"image_url": "https://img.medscapestatic.com/article/724/047/724047-thumb5.png"
}
],
"markdown": "# Cardio Case Challenge: A 17-Year-Old in Cardiac Arrest After Collision Playing Sports\n\n **Authors:** Jansen Tiongson, MD; Lisa Chan, MD \n **Date:** December 16, 2022\n\n ## Content\n\n A review of data from the US Commotio Cordis Registry (USCCR), in Minneapolis, Minnesota revealed that most cases were caused by a blow to the chest from an object used during an organized youth sporting event.[2] A baseball accounted for 53 of the cases, with a softball and a hockey puck the next most frequent, at 14 and 10 cases, respectively. Other documented sporting cases have been caused by blows delivered by body parts, such as an elbow, knee, foot, or fist hitting the anterior chest wall (5-6 cases of each).\nDaily activities, including parent-child discipline (5 cases), and even a fall from monkey bars (1 case), can also lead to commotio cordis. Regardless of the mechanism, impacts resulting in commotio cordis are typically of low energy and velocity.[1,4] The victim may collapse immediately after the blow, but in as many as 50% of cases, a short delay occurs between the impact and collapse.\nIn 1930, George Schlomka was the first to describe the factors that can lead to arrhythmia after a moderate precordial impact. He believed that the force, location, and type of object causing the impact determined the type of injury and the subsequent risk for arrhythmia.[2] The force transmitted to the heart is directly related to the hardness of the striking object. Madias and colleagues[4] reported that the threshold speed of impact at which a standard baseball can cause ventricular fibrillation is between 25 and 30 miles per hour. However, when the speed is over 50 miles per hour, the likelihood of ventricular fibrillation actually decreases, although the possibility of myocardial contusion becomes greater. Furthermore, the authors stated that the impact must be directly over the heart near or just to the left of the sternum in order to instigate ventricular fibrillation. Impact on the center of the heart induced ventricular fibrillation in 30% of reported cases, compared with 13% and 4% at the left ventricular base and apex, respectively.[4]\nThe use of a standard baseball leads to the incidence rate reported above, but if the core of the ball is softer, then the rate for ventricular fibrillation drops. Link and colleagues[5] reported that changes to the cores of baseballs to make them softer led to a decrease in the rate of ventricular fibrillation with commotio cordis from 70% to 19%. As such, the use of safety baseballs with rubber cores of different degrees of hardness has been advocated to reduce the risk for such traumatic injury in young athletes.[3,5]\nNot all impacts to the anterior chest lead to the ventricular fibrillation observed in commotio cordis. The impact must be delivered 10-30 milliseconds before the peak of the T wave in the cardiac cycle (Figure 5) in order to induce ventricular fibrillation.\nFigure 5.\nInduction is probably secondary to the activation of potassium-carrying ion channels via mechanoelectric coupling. The activation of these ion channels generates an inward current, thus locally augmenting repolarization and resulting in premature ventricular depolarization and the initiation of unstable ventricular arrhythmias. If impact occurs during other portions of the cardiac cycle, different conduction disturbances, such as heart block, bundle branch block, or transient ST segment elevation, may be induced.[2,4,5]\n\n ## Figures\n\n **Figure 5.** \n \n\n\n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Cardio Case Challenge: A 17-Year-Old in Cardiac Arrest After Collision Playing Sports"
},
{
"authors": "Jansen Tiongson, MD; Lisa Chan, MD",
"content": [
"Regardless of the cause, if a young athlete goes into sudden cardiac arrest, CPR should be implemented immediately. Among sports-related cases of commotio cordis documented in the USCCR, 15% of patients survived. When CPR was instituted within 3 minutes of the impact, 68% of patients survived; however, if CPR was delayed by more than 3 minutes, only 3% of patients survived. Animal studies have shown that CPR instituted within the first 3 minutes of injury can increase survival rate by up to 25%. Concomitantly, early use of an automatic external defibrillator (AED) device has been proven to increase survival rates. With an AED recognizing ventricular fibrillation at a sensitivity of 98% and a specificity of 100%, defibrillation within the first 3 minutes can increase the survival rate by an additional 50% or more in animal models, yielding a survival rate of 46% at 4 minutes and 25% at 6 minutes. The USCCR has recommended that all athletic venues have an accessible AED. Preventive measures for commotio cordis include parental education, softer baseballs, and protective padding of an athlete's precordium.[1,4] Secondary prevention may involve avoidance of certain sports until at least age 18 years.",
"While the patient in this case was in the PICU, he was placed on continuous cardiac monitoring for 24 hours, and no incident of arrhythmia was noted. An echocardiogram revealed a normal left ventricular systolic ejection fraction, with no structural abnormalities, valvular disease, or hypertrophy. A repeat 12-lead ECG showed no changes from the previous one, and subsequently, the serial troponin measurements decreased from 0.25 to 0.04 ng/mL. A pediatric cardiologist consultation was unrevealing. The patient was transferred to the pediatric floor the next day, and he was discharged 2 days after initial admission, with no signs of postarrest sequelae. His final diagnosis was commotio cordis."
],
"date": "December 16, 2022",
"figures": [],
"markdown": "# Cardio Case Challenge: A 17-Year-Old in Cardiac Arrest After Collision Playing Sports\n\n **Authors:** Jansen Tiongson, MD; Lisa Chan, MD \n **Date:** December 16, 2022\n\n ## Content\n\n Regardless of the cause, if a young athlete goes into sudden cardiac arrest, CPR should be implemented immediately. Among sports-related cases of commotio cordis documented in the USCCR, 15% of patients survived. When CPR was instituted within 3 minutes of the impact, 68% of patients survived; however, if CPR was delayed by more than 3 minutes, only 3% of patients survived. Animal studies have shown that CPR instituted within the first 3 minutes of injury can increase survival rate by up to 25%. Concomitantly, early use of an automatic external defibrillator (AED) device has been proven to increase survival rates. With an AED recognizing ventricular fibrillation at a sensitivity of 98% and a specificity of 100%, defibrillation within the first 3 minutes can increase the survival rate by an additional 50% or more in animal models, yielding a survival rate of 46% at 4 minutes and 25% at 6 minutes. The USCCR has recommended that all athletic venues have an accessible AED. Preventive measures for commotio cordis include parental education, softer baseballs, and protective padding of an athlete's precordium.[1,4] Secondary prevention may involve avoidance of certain sports until at least age 18 years.\nWhile the patient in this case was in the PICU, he was placed on continuous cardiac monitoring for 24 hours, and no incident of arrhythmia was noted. An echocardiogram revealed a normal left ventricular systolic ejection fraction, with no structural abnormalities, valvular disease, or hypertrophy. A repeat 12-lead ECG showed no changes from the previous one, and subsequently, the serial troponin measurements decreased from 0.25 to 0.04 ng/mL. A pediatric cardiologist consultation was unrevealing. The patient was transferred to the pediatric floor the next day, and he was discharged 2 days after initial admission, with no signs of postarrest sequelae. His final diagnosis was commotio cordis.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 349499,
"choiceText": "Performance of an immediate precordial thump",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349500,
"choiceText": "Use of an automated external defibrillator (AED) within 3 minutes of impact",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349501,
"choiceText": "Initiation of cardiopulmonary resuscitation (CPR) within 10 minutes of impact",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349502,
"choiceText": "Intubation and mechanical ventilation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Among sports-related cases of commotio cordis documented in the US Commotio Cordis Registry (USCCR), 15% of patients survived. When CPR was instituted within 3 minutes of the impact, 68% of patients survived; however, if CPR was delayed by more than 3 minutes, only 3% of patients survived. Animal studies have shown that CPR instituted within the first 3 minutes of injury can increase survival rate by up to 25%. Concomitantly, early use of an AED device has been proven to increase survival rates. With an AED recognizing ventricular fibrillation at a sensitivity of 98% and a specificity of 100%, defibrillation within the first 3 minutes can increase the survival rate by an additional 50% or more in animal models, yielding a survival rate of 46% at 4 minutes and 25% at 6 minutes. The USCCR has recommended that all athletic venues have an accessible AED.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 99157,
"questionText": "A 15-year-old boy collapses while practicing with his school baseball team. The boy was attempting to catch a ball thrown at him; he missed, and the ball struck him in the chest. He collapsed after the blow and was unresponsive. Which is most likely to improve the chances of survival in this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 349511,
"choiceText": "A small elevation in his cardiac enzymes but otherwise normal findings",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349512,
"choiceText": "Abnormal echocardiography revealing an enlarged heart",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349513,
"choiceText": "A QT interval of 520 ms on his electrocardiogram",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349514,
"choiceText": " A chest x-ray demonstrating an R-sided pneumothorax",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Commotio cordis is a diagnosis of exclusion in that other causes, such as substance abuse, myocardial infarction, electrolyte abnormality, prolonged QT syndrome, and hypertrophic obstructive cardiomyopathy, must first be ruled out with examinations such as urine drug screens, serial assessment of cardiac biomarkers and ECGs, electrolyte level testing, and echocardiography.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 99160,
"questionText": "The patient above is resuscitated. Which is most likely to be found during a subsequent examination?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Cardio Case Challenge: A 17-Year-Old in Cardiac Arrest After Collision Playing Sports"
},
{
"authors": "Jansen Tiongson, MD; Lisa Chan, MD",
"content": [],
"date": "December 16, 2022",
"figures": [],
"markdown": "# Cardio Case Challenge: A 17-Year-Old in Cardiac Arrest After Collision Playing Sports\n\n **Authors:** Jansen Tiongson, MD; Lisa Chan, MD \n **Date:** December 16, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 349499,
"choiceText": "Performance of an immediate precordial thump",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349500,
"choiceText": "Use of an automated external defibrillator (AED) within 3 minutes of impact",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349501,
"choiceText": "Initiation of cardiopulmonary resuscitation (CPR) within 10 minutes of impact",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349502,
"choiceText": "Intubation and mechanical ventilation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Among sports-related cases of commotio cordis documented in the US Commotio Cordis Registry (USCCR), 15% of patients survived. When CPR was instituted within 3 minutes of the impact, 68% of patients survived; however, if CPR was delayed by more than 3 minutes, only 3% of patients survived. Animal studies have shown that CPR instituted within the first 3 minutes of injury can increase survival rate by up to 25%. Concomitantly, early use of an AED device has been proven to increase survival rates. With an AED recognizing ventricular fibrillation at a sensitivity of 98% and a specificity of 100%, defibrillation within the first 3 minutes can increase the survival rate by an additional 50% or more in animal models, yielding a survival rate of 46% at 4 minutes and 25% at 6 minutes. The USCCR has recommended that all athletic venues have an accessible AED.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 99157,
"questionText": "A 15-year-old boy collapses while practicing with his school baseball team. The boy was attempting to catch a ball thrown at him; he missed, and the ball struck him in the chest. He collapsed after the blow and was unresponsive. Which is most likely to improve the chances of survival in this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 349511,
"choiceText": "A small elevation in his cardiac enzymes but otherwise normal findings",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349512,
"choiceText": "Abnormal echocardiography revealing an enlarged heart",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349513,
"choiceText": "A QT interval of 520 ms on his electrocardiogram",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349514,
"choiceText": " A chest x-ray demonstrating an R-sided pneumothorax",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Commotio cordis is a diagnosis of exclusion in that other causes, such as substance abuse, myocardial infarction, electrolyte abnormality, prolonged QT syndrome, and hypertrophic obstructive cardiomyopathy, must first be ruled out with examinations such as urine drug screens, serial assessment of cardiac biomarkers and ECGs, electrolyte level testing, and echocardiography.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 99160,
"questionText": "The patient above is resuscitated. Which is most likely to be found during a subsequent examination?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Cardio Case Challenge: A 17-Year-Old in Cardiac Arrest After Collision Playing Sports"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 349495,
"choiceText": "Hypertrophic cardiomyopathy",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349496,
"choiceText": "Myocardial infarction",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349497,
"choiceText": "Commotio cordis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349498,
"choiceText": "Long-QT syndrome",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 99156,
"questionText": "Based on only these findings, which most likely led to this patient's cardiac arrest?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 349499,
"choiceText": "Performance of an immediate precordial thump",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349500,
"choiceText": "Use of an automated external defibrillator (AED) within 3 minutes of impact",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349501,
"choiceText": "Initiation of cardiopulmonary resuscitation (CPR) within 10 minutes of impact",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349502,
"choiceText": "Intubation and mechanical ventilation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Among sports-related cases of commotio cordis documented in the US Commotio Cordis Registry (USCCR), 15% of patients survived. When CPR was instituted within 3 minutes of the impact, 68% of patients survived; however, if CPR was delayed by more than 3 minutes, only 3% of patients survived. Animal studies have shown that CPR instituted within the first 3 minutes of injury can increase survival rate by up to 25%. Concomitantly, early use of an AED device has been proven to increase survival rates. With an AED recognizing ventricular fibrillation at a sensitivity of 98% and a specificity of 100%, defibrillation within the first 3 minutes can increase the survival rate by an additional 50% or more in animal models, yielding a survival rate of 46% at 4 minutes and 25% at 6 minutes. The USCCR has recommended that all athletic venues have an accessible AED.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 99157,
"questionText": "A 15-year-old boy collapses while practicing with his school baseball team. The boy was attempting to catch a ball thrown at him; he missed, and the ball struck him in the chest. He collapsed after the blow and was unresponsive. Which is most likely to improve the chances of survival in this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 349511,
"choiceText": "A small elevation in his cardiac enzymes but otherwise normal findings",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349512,
"choiceText": "Abnormal echocardiography revealing an enlarged heart",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349513,
"choiceText": "A QT interval of 520 ms on his electrocardiogram",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 349514,
"choiceText": " A chest x-ray demonstrating an R-sided pneumothorax",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Commotio cordis is a diagnosis of exclusion in that other causes, such as substance abuse, myocardial infarction, electrolyte abnormality, prolonged QT syndrome, and hypertrophic obstructive cardiomyopathy, must first be ruled out with examinations such as urine drug screens, serial assessment of cardiac biomarkers and ECGs, electrolyte level testing, and echocardiography.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 99160,
"questionText": "The patient above is resuscitated. Which is most likely to be found during a subsequent examination?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
729899 | /viewarticle/729899 | [
{
"authors": "Abraham A. Ayantunde, MB BS, FRCS; George G. Araklitis, MB BS, BSc",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to recognize accurately. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 21-year-old man presents to the emergency department with a 10-hour history of epigastric pain that is radiating to his chest. The pain is constant, localized, and sharp in nature.",
"He was at what he describes as a \"wild party\" the previous night. He states that he drank alcoholic beverages but did not use any illicit drugs. He has no associated nausea, vomiting, or indigestion. He has not experienced this pain in the past. The patient provides no history of shortness of breath, palpitations, or syncope. He has no history of trauma to the epigastrium. He does not remember anything that may be causing his symptoms but states that his memories of the night are hazy.",
"His past medical history is significant for an appendectomy 9 years ago and surgery for a deviated nasal septum 11 months ago. He is not currently on any regular medication. He has no history of allergies. His family history is negative for any cardiac or abdominal pathology. He smokes approximately 1 pack of cigarettes a day and binge-drinks alcohol at weekend parties."
],
"date": "December 14, 2022",
"figures": [],
"markdown": "# A 21-Year-Old Man With Epigastric Pain After a Wild Party\n\n **Authors:** Abraham A. Ayantunde, MB BS, FRCS; George G. Araklitis, MB BS, BSc \n **Date:** December 14, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to recognize accurately. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 21-year-old man presents to the emergency department with a 10-hour history of epigastric pain that is radiating to his chest. The pain is constant, localized, and sharp in nature.\nHe was at what he describes as a \"wild party\" the previous night. He states that he drank alcoholic beverages but did not use any illicit drugs. He has no associated nausea, vomiting, or indigestion. He has not experienced this pain in the past. The patient provides no history of shortness of breath, palpitations, or syncope. He has no history of trauma to the epigastrium. He does not remember anything that may be causing his symptoms but states that his memories of the night are hazy.\nHis past medical history is significant for an appendectomy 9 years ago and surgery for a deviated nasal septum 11 months ago. He is not currently on any regular medication. He has no history of allergies. His family history is negative for any cardiac or abdominal pathology. He smokes approximately 1 pack of cigarettes a day and binge-drinks alcohol at weekend parties.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A 21-Year-Old Man With Epigastric Pain After a Wild Party"
},
{
"authors": "Abraham A. Ayantunde, MB BS, FRCS; George G. Araklitis, MB BS, BSc",
"content": [
"Upon examination, he appears to be alert, comfortable, and in no acute distress. He is well oriented to person, time, and place. His vital signs reveal a heart rate of 76 beats/min, a respiratory rate of 18 breaths/min, and an O2 saturation of 97% on room air. His temperature is normal. His respiratory and cardiovascular examinations reveal no abnormal findings.",
"The abdominal examination reveals no abnormal findings on inspection, except for a well-healed appendectomy scar; otherwise, the abdomen is scaphoid and without any discoloration, bruises, or visible abnormalities. Palpation reveals a slightly tender but otherwise soft epigastrium, with positive bowel sounds and no evidence of guarding or rebound tenderness. No masses or organomegaly are appreciated, and the abdomen is resonant to percussion, with the absence of a fluid wave or shifting dullness. The spleen and liver margins are normal, and the kidneys are not palpable.",
"Neurologic examination is grossly normal with equal power, tone, and bulk in both upper and lower extremities bilaterally, normal reflexes, and intact cranial nerves. His mental status examination findings are normal.",
"Laboratory investigations reveal a hemoglobin count of 16.9 g/dL (reference range, 13.8-17.g/dL) and a white blood cell count of 7.8 × 103/μL (reference range, 4.5-11 × 103/μL). Urea and electrolytes are within normal limits, and no derangement of liver function is noted. Serum amylase findings are normal. A chest x-ray shows clear lung fields, a normal heart size, and no evidence of air under the diaphragm; however, the chest and abdominal x-rays do reveal a radio-opaque shadow in the central lower chest/epigastrium region (Figure 1).",
"Figure 1.",
"Electrocardiography shows a sinus rhythm with no evidence of ischemic changes. The patient is instructed to take nothing orally and is placed on intravenous fluids. His symptoms are persistent, and a repeat chest and abdominal x-ray at 12 hours postadmission shows that the previously seen shadow has not changed position. The decision to intervene endoscopically is made."
],
"date": "December 14, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/729/522/729522-thumb1.png"
}
],
"markdown": "# A 21-Year-Old Man With Epigastric Pain After a Wild Party\n\n **Authors:** Abraham A. Ayantunde, MB BS, FRCS; George G. Araklitis, MB BS, BSc \n **Date:** December 14, 2022\n\n ## Content\n\n Upon examination, he appears to be alert, comfortable, and in no acute distress. He is well oriented to person, time, and place. His vital signs reveal a heart rate of 76 beats/min, a respiratory rate of 18 breaths/min, and an O2 saturation of 97% on room air. His temperature is normal. His respiratory and cardiovascular examinations reveal no abnormal findings.\nThe abdominal examination reveals no abnormal findings on inspection, except for a well-healed appendectomy scar; otherwise, the abdomen is scaphoid and without any discoloration, bruises, or visible abnormalities. Palpation reveals a slightly tender but otherwise soft epigastrium, with positive bowel sounds and no evidence of guarding or rebound tenderness. No masses or organomegaly are appreciated, and the abdomen is resonant to percussion, with the absence of a fluid wave or shifting dullness. The spleen and liver margins are normal, and the kidneys are not palpable.\nNeurologic examination is grossly normal with equal power, tone, and bulk in both upper and lower extremities bilaterally, normal reflexes, and intact cranial nerves. His mental status examination findings are normal.\nLaboratory investigations reveal a hemoglobin count of 16.9 g/dL (reference range, 13.8-17.g/dL) and a white blood cell count of 7.8 × 103/μL (reference range, 4.5-11 × 103/μL). Urea and electrolytes are within normal limits, and no derangement of liver function is noted. Serum amylase findings are normal. A chest x-ray shows clear lung fields, a normal heart size, and no evidence of air under the diaphragm; however, the chest and abdominal x-rays do reveal a radio-opaque shadow in the central lower chest/epigastrium region (Figure 1).\nFigure 1.\nElectrocardiography shows a sinus rhythm with no evidence of ischemic changes. The patient is instructed to take nothing orally and is placed on intravenous fluids. His symptoms are persistent, and a repeat chest and abdominal x-ray at 12 hours postadmission shows that the previously seen shadow has not changed position. The decision to intervene endoscopically is made.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 369595,
"choiceText": "External monitoring device",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369596,
"choiceText": "Radiologic artifact",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369597,
"choiceText": "Foreign-body ingestion",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369598,
"choiceText": "An implanted medical device",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 106001,
"questionText": "What abnormality is seen on the x-ray?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 21-Year-Old Man With Epigastric Pain After a Wild Party"
},
{
"authors": "Abraham A. Ayantunde, MB BS, FRCS; George G. Araklitis, MB BS, BSc",
"content": [
"In this case, the chest and upper abdominal x-rays revealed that the patient had ingested a foreign body, which appeared to be lodged at the gastroesophageal junction. No radiologic or clinical evidence suggested air in the mediastinum or under the diaphragm, which ruled out an upper gastrointestinal perforation.",
"The patient admitted to uncapping the bottles of alcoholic beverages with his teeth. He had accidently swallowed one such metallic bottle cap that, having impacted at the gastroesophageal junction, was responsible for his symptoms (Figure 2).",
"Figure 2.",
"The patient's own inebriation probably caused him to swallow the foreign body and was also the reason why he could not remember swallowing it. The patient did not report any recent problems with swallowing solids or liquids; however, he had not tried ingesting any solid food since the occurrence of the incident. A common symptom of total luminal obstruction is the inability to swallow one's own secretions. This was not the case here, and presumably some fluids were able to bypass the obstruction.",
"Gastrointestinal foreign objects are either ingested (intentionally or accidently) or inserted rectally. They are encountered in all age groups but are more commonly seen in children between 6 months and 6 years of age.[1] In adults, they are found more frequently in those with psychiatric or behavioral problems, and, as in this case, in cases of alcohol intoxication.[1] Foreign-body ingestion may also occur accidently in patients who have dental prostheses. In the United States, approximately 1,500-1,600 deaths occur annually due to foreign-body ingestion or insertion.[2]",
"A wide variety of foreign objects may be found in the gastrointestinal tract; a review of foreign bodies found in the gastrointestinal tract of patients who presented to the emergency department in London showed that the most common objects were coins (18.4%), aerosol caps (rectally; 10.5%), metal blades (10.5%), and AA batteries (7.9%).[2] Disc batteries are especially dangerous if ingested because they can cause caustic injury and quickly result in tissue necrosis and esophageal perforation. Intentional gastrointestinal foreign-body ingestion and insertion are more common than accidental occurrence in the adult population."
],
"date": "December 14, 2022",
"figures": [
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/729/522/729522-thumb2.png"
}
],
"markdown": "# A 21-Year-Old Man With Epigastric Pain After a Wild Party\n\n **Authors:** Abraham A. Ayantunde, MB BS, FRCS; George G. Araklitis, MB BS, BSc \n **Date:** December 14, 2022\n\n ## Content\n\n In this case, the chest and upper abdominal x-rays revealed that the patient had ingested a foreign body, which appeared to be lodged at the gastroesophageal junction. No radiologic or clinical evidence suggested air in the mediastinum or under the diaphragm, which ruled out an upper gastrointestinal perforation.\nThe patient admitted to uncapping the bottles of alcoholic beverages with his teeth. He had accidently swallowed one such metallic bottle cap that, having impacted at the gastroesophageal junction, was responsible for his symptoms (Figure 2).\nFigure 2.\nThe patient's own inebriation probably caused him to swallow the foreign body and was also the reason why he could not remember swallowing it. The patient did not report any recent problems with swallowing solids or liquids; however, he had not tried ingesting any solid food since the occurrence of the incident. A common symptom of total luminal obstruction is the inability to swallow one's own secretions. This was not the case here, and presumably some fluids were able to bypass the obstruction.\nGastrointestinal foreign objects are either ingested (intentionally or accidently) or inserted rectally. They are encountered in all age groups but are more commonly seen in children between 6 months and 6 years of age.[1] In adults, they are found more frequently in those with psychiatric or behavioral problems, and, as in this case, in cases of alcohol intoxication.[1] Foreign-body ingestion may also occur accidently in patients who have dental prostheses. In the United States, approximately 1,500-1,600 deaths occur annually due to foreign-body ingestion or insertion.[2]\nA wide variety of foreign objects may be found in the gastrointestinal tract; a review of foreign bodies found in the gastrointestinal tract of patients who presented to the emergency department in London showed that the most common objects were coins (18.4%), aerosol caps (rectally; 10.5%), metal blades (10.5%), and AA batteries (7.9%).[2] Disc batteries are especially dangerous if ingested because they can cause caustic injury and quickly result in tissue necrosis and esophageal perforation. Intentional gastrointestinal foreign-body ingestion and insertion are more common than accidental occurrence in the adult population.\n\n ## Figures\n\n **Figure 2.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 369595,
"choiceText": "External monitoring device",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369596,
"choiceText": "Radiologic artifact",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369597,
"choiceText": "Foreign-body ingestion",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369598,
"choiceText": "An implanted medical device",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 106001,
"questionText": "What abnormality is seen on the x-ray?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 21-Year-Old Man With Epigastric Pain After a Wild Party"
},
{
"authors": "Abraham A. Ayantunde, MB BS, FRCS; George G. Araklitis, MB BS, BSc",
"content": [
"The diagnosis of foreign body ingestion is usually made on the basis of the patient history and appropriate imaging; however, making the diagnosis can be difficult because most patients who ingest foreign objects are either children or those in whom a proper history-taking would prove challenging (such as psychiatric patients or intoxicated patients). These patients may only present after the onset of symptoms such as choking, pain, refusal to eat, vomiting, wheezing, or respiratory distress.[1] Examination may reveal swelling, erythema, tenderness, or crepitus in the neck; additionally, the abdomen may also show signs of obstruction or peritonitis secondary to perforation.[1]",
"Past studies have shown that most patients present with no clinical signs or symptoms, with a small proportion presenting with abdominal pain.[2] Radiologic investigations are used to localize the object. X-rays can identify most foreign objects and free air in the mediastinum or peritoneum.[2] A lateral x-ray may help identify multiple foreign bodies, such as coins, or it may help differentiate a coin from a disc battery.[1,3] Serial x-rays over a period of time may show the progress of the foreign body through the gastrointestinal tract if the object is small, has no sharp edges, and the patient is stable. Some objects, such as fish bone, plastic, or glass, are more difficult to see on x-rays.[1] A CT scan or contrast study may help locate more difficult objects.[1]",
"The risks of a foreign body in the alimentary canal include impaction, perforation, obstruction, erosion, and fistulation anywhere along the gastrointestinal tract. Rounded and/or smooth objects, such as coins, pass more easily than sharp objects.[3] Anatomically, the esophagus is one of the narrowest sections of the gastrointestinal tract,[3] which makes it a common site of foreign-object impaction. Other common sites include the pyloric channel and ileocecal valve. The esophagus is about 7.9-9.4 in (20-24 cm) long, starting 5.5-6.3 in (14-16 cm) distal to the incisor teeth[4] at the upper esophageal sphincter. This is the narrowest part of gastrointestinal tract. It is formed by the cricopharyngeal fibers of the constrictor muscles of the pharynx.[4] Distally, the esophagus also narrows at sites where it is indented by the aorta, the left main bronchus, and the heart[4]; these are also sites for potential foreign-body impaction. The most common site of foreign-body impaction is at the level of the thoracic inlet,[1] followed by the gastroesophageal junction.[3]",
"Once an object passes through the esophagus into the stomach, the risk of it lodging somewhere along the rest of the alimentary canal is relatively small, even for sharp objects.[1,3] Sharp objects that have passed into the stomach, however, still pose a 35% risk for complication, and most authorities recommend that removal be attempted.[7] A Chinese study showed that 84.5% of 439 patients with foreign-body ingestion had the object lodged in the esophagus, with most in the upper esophagus.[5]",
"Management of patients with ingested foreign bodies depends on the age and clinical condition of the patient as well as the size, shape, and nature of the object (eg, sharp, corrosive, or poisonous[1]) and the site at which the foreign body is lodged. Foreign objects should not remain in the esophagus for more than 24 hours from the time of presentation to the emergency department.[1] Endoscopy should usually be performed within that timeframe.",
"Most foreign bodies pass through the gastrointestinal tract without requiring intervention, whereas 10%-20% of foreign bodies require nonoperative intervention and less than 1% require surgery (eg, laparotomy).[5] Upper gastrointestinal endoscopy can be used to remove the foreign body. Initial attempts to dislodge a food bolus are usually made with ingestion of a carbonated beverage or via intravenous glucagon; however, this is not done with foreign-body ingestions. Ingested foreign body is the second most common indication for emergency endoscopy (gastrointestinal bleeding is the first).[5]",
"During endoscopy, forceps are more successful in removing sharp objects, while the basket is more successful in removing blunt objects, such as coins or a food bolus.[5] An overtube or protector hood should be used to avoid puncture of the esophagus and/or aspiration upon withdrawal. Failure of endoscopic removal usually means that the foreign body in question is a bone, with 76.5% of cases being fish bone,[5] usually in the upper esophagus.[5] The potential for luminal abnormalities that result in obstruction is important to remember. An esophageal stricture, achalasia, esophageal diverticula, and eosinophilic esophagitis are common pathologies that are found at follow-up endoscopy.",
"An American study concluded that adopting a conservative approach in the asymptomatic patient allowed spontaneous passage of nearly all swallowed foreign objects.[6] This study did not include corrosive objects or those stuck in the esophagus. Narcotic packets concealed internally for drug trafficking should be allowed to progress through the gastrointestinal tract naturally.[1] If removal becomes a necessity because of obstruction or rupture of the packet contents, endoscopic removal should not be attempted because of the risk for iatrogenic rupture and leakage of the drug packets, leaving surgical intervention as the only choice.[1]"
],
"date": "December 14, 2022",
"figures": [],
"markdown": "# A 21-Year-Old Man With Epigastric Pain After a Wild Party\n\n **Authors:** Abraham A. Ayantunde, MB BS, FRCS; George G. Araklitis, MB BS, BSc \n **Date:** December 14, 2022\n\n ## Content\n\n The diagnosis of foreign body ingestion is usually made on the basis of the patient history and appropriate imaging; however, making the diagnosis can be difficult because most patients who ingest foreign objects are either children or those in whom a proper history-taking would prove challenging (such as psychiatric patients or intoxicated patients). These patients may only present after the onset of symptoms such as choking, pain, refusal to eat, vomiting, wheezing, or respiratory distress.[1] Examination may reveal swelling, erythema, tenderness, or crepitus in the neck; additionally, the abdomen may also show signs of obstruction or peritonitis secondary to perforation.[1]\nPast studies have shown that most patients present with no clinical signs or symptoms, with a small proportion presenting with abdominal pain.[2] Radiologic investigations are used to localize the object. X-rays can identify most foreign objects and free air in the mediastinum or peritoneum.[2] A lateral x-ray may help identify multiple foreign bodies, such as coins, or it may help differentiate a coin from a disc battery.[1,3] Serial x-rays over a period of time may show the progress of the foreign body through the gastrointestinal tract if the object is small, has no sharp edges, and the patient is stable. Some objects, such as fish bone, plastic, or glass, are more difficult to see on x-rays.[1] A CT scan or contrast study may help locate more difficult objects.[1]\nThe risks of a foreign body in the alimentary canal include impaction, perforation, obstruction, erosion, and fistulation anywhere along the gastrointestinal tract. Rounded and/or smooth objects, such as coins, pass more easily than sharp objects.[3] Anatomically, the esophagus is one of the narrowest sections of the gastrointestinal tract,[3] which makes it a common site of foreign-object impaction. Other common sites include the pyloric channel and ileocecal valve. The esophagus is about 7.9-9.4 in (20-24 cm) long, starting 5.5-6.3 in (14-16 cm) distal to the incisor teeth[4] at the upper esophageal sphincter. This is the narrowest part of gastrointestinal tract. It is formed by the cricopharyngeal fibers of the constrictor muscles of the pharynx.[4] Distally, the esophagus also narrows at sites where it is indented by the aorta, the left main bronchus, and the heart[4]; these are also sites for potential foreign-body impaction. The most common site of foreign-body impaction is at the level of the thoracic inlet,[1] followed by the gastroesophageal junction.[3]\nOnce an object passes through the esophagus into the stomach, the risk of it lodging somewhere along the rest of the alimentary canal is relatively small, even for sharp objects.[1,3] Sharp objects that have passed into the stomach, however, still pose a 35% risk for complication, and most authorities recommend that removal be attempted.[7] A Chinese study showed that 84.5% of 439 patients with foreign-body ingestion had the object lodged in the esophagus, with most in the upper esophagus.[5]\nManagement of patients with ingested foreign bodies depends on the age and clinical condition of the patient as well as the size, shape, and nature of the object (eg, sharp, corrosive, or poisonous[1]) and the site at which the foreign body is lodged. Foreign objects should not remain in the esophagus for more than 24 hours from the time of presentation to the emergency department.[1] Endoscopy should usually be performed within that timeframe.\nMost foreign bodies pass through the gastrointestinal tract without requiring intervention, whereas 10%-20% of foreign bodies require nonoperative intervention and less than 1% require surgery (eg, laparotomy).[5] Upper gastrointestinal endoscopy can be used to remove the foreign body. Initial attempts to dislodge a food bolus are usually made with ingestion of a carbonated beverage or via intravenous glucagon; however, this is not done with foreign-body ingestions. Ingested foreign body is the second most common indication for emergency endoscopy (gastrointestinal bleeding is the first).[5]\nDuring endoscopy, forceps are more successful in removing sharp objects, while the basket is more successful in removing blunt objects, such as coins or a food bolus.[5] An overtube or protector hood should be used to avoid puncture of the esophagus and/or aspiration upon withdrawal. Failure of endoscopic removal usually means that the foreign body in question is a bone, with 76.5% of cases being fish bone,[5] usually in the upper esophagus.[5] The potential for luminal abnormalities that result in obstruction is important to remember. An esophageal stricture, achalasia, esophageal diverticula, and eosinophilic esophagitis are common pathologies that are found at follow-up endoscopy.\nAn American study concluded that adopting a conservative approach in the asymptomatic patient allowed spontaneous passage of nearly all swallowed foreign objects.[6] This study did not include corrosive objects or those stuck in the esophagus. Narcotic packets concealed internally for drug trafficking should be allowed to progress through the gastrointestinal tract naturally.[1] If removal becomes a necessity because of obstruction or rupture of the packet contents, endoscopic removal should not be attempted because of the risk for iatrogenic rupture and leakage of the drug packets, leaving surgical intervention as the only choice.[1]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A 21-Year-Old Man With Epigastric Pain After a Wild Party"
},
{
"authors": "Abraham A. Ayantunde, MB BS, FRCS; George G. Araklitis, MB BS, BSc",
"content": [
"To summarize, any esophageal foreign-body obstruction should be treated endoscopically within 24 hours. Disc batteries pose the highest risk for caustic injury and perforation. Luminal abnormalities must be excluded at the site of obstruction, usually through follow-up endoscopy. More variation is observed in practice with respect to the management of a foreign body that has reached the stomach. Some centers take a liberal wait-and-watch approach for passage of even large (0.8-2 in [2-5 cm] oval or 2.4-3.9 in [6-10 cm] long) and sharp objects. Most endoscopists, however, attempt removal of foreign-body obstructions larger than 0.8 in (2 cm) in circular diameter and/or more than 2.4 in (6 cm) long, as these are deemed unlikely to pass the pyloric channel and duodenal sweep, respectively.",
"Sharp objects that remain in the stomach still carry a small but significant risk for complication if left untreated, and regulatory bodies generally recommend that they be removed endoscopically if possible.[8]",
"The patient in this case was observed for 12 hours. His symptoms did not resolve and he continued to have epigastric and chest pain. Repeat x-rays of the chest and abdomen revealed that the foreign body had not moved from the gastroesophageal junction. An emergency esophagogastroduodenoscopy was performed to retrieve the bottle cap within 24 hours of the patient presenting to the ED. The metallic bottle cap was visualized at the gastroesophageal junction, and it was pushed down into the gastric cardia before retrieval. No other endoscopic abnormality of the upper gastrointestinal tract was noted apart from associated gastritis.",
"Initial attempts at retrieval of the bottle cap with the large biopsy forceps failed because the cap dropped back into the stomach upon reaching into the gastroesophageal junction. It was successfully removed with a basket net. The patient was later discharged from the hospital and warned about the dangers of uncapping bottles with his teeth."
],
"date": "December 14, 2022",
"figures": [],
"markdown": "# A 21-Year-Old Man With Epigastric Pain After a Wild Party\n\n **Authors:** Abraham A. Ayantunde, MB BS, FRCS; George G. Araklitis, MB BS, BSc \n **Date:** December 14, 2022\n\n ## Content\n\n To summarize, any esophageal foreign-body obstruction should be treated endoscopically within 24 hours. Disc batteries pose the highest risk for caustic injury and perforation. Luminal abnormalities must be excluded at the site of obstruction, usually through follow-up endoscopy. More variation is observed in practice with respect to the management of a foreign body that has reached the stomach. Some centers take a liberal wait-and-watch approach for passage of even large (0.8-2 in [2-5 cm] oval or 2.4-3.9 in [6-10 cm] long) and sharp objects. Most endoscopists, however, attempt removal of foreign-body obstructions larger than 0.8 in (2 cm) in circular diameter and/or more than 2.4 in (6 cm) long, as these are deemed unlikely to pass the pyloric channel and duodenal sweep, respectively.\nSharp objects that remain in the stomach still carry a small but significant risk for complication if left untreated, and regulatory bodies generally recommend that they be removed endoscopically if possible.[8]\nThe patient in this case was observed for 12 hours. His symptoms did not resolve and he continued to have epigastric and chest pain. Repeat x-rays of the chest and abdomen revealed that the foreign body had not moved from the gastroesophageal junction. An emergency esophagogastroduodenoscopy was performed to retrieve the bottle cap within 24 hours of the patient presenting to the ED. The metallic bottle cap was visualized at the gastroesophageal junction, and it was pushed down into the gastric cardia before retrieval. No other endoscopic abnormality of the upper gastrointestinal tract was noted apart from associated gastritis.\nInitial attempts at retrieval of the bottle cap with the large biopsy forceps failed because the cap dropped back into the stomach upon reaching into the gastroesophageal junction. It was successfully removed with a basket net. The patient was later discharged from the hospital and warned about the dangers of uncapping bottles with his teeth.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 369599,
"choiceText": "Conservative management",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369600,
"choiceText": "Lateral x-ray",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369601,
"choiceText": "Serial x-rays",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369602,
"choiceText": "Endoscopic retrieval ",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369603,
"choiceText": "Surgery ",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The next step is a lateral x-ray because the mother does not know what the child swallowed. In this case, the need arises to differentiate between commonly ingested circular foreign bodies such as coins and corrosive disc batteries. This also helps to ascertain the position of the foreign body in the esophagus. Once a coin has been identified, conservative management can be used.</p><p>Serial x-rays should be taken to establish whether the coin has passed through the narrowest part of the gastrointestinal tract (the esophagus). If the coin remains in the esophagus, endoscopy must be considered within 24 hours after first presenting to the hospital for the object's removal in order to avoid the risk for esophageal pressure necrosis and perforation. Surgery is a very rare management option for an uncommon failure of endoscopic retrieval.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 106002,
"questionText": "A concerned mother presents with her 1-year-old child, who she believes swallowed an unknown object 35 minutes earlier. An initial single plain chest x-ray in the anteroposterior view shows a circular object in the esophagus. Which should be the next step in the management of this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 369604,
"choiceText": "Upper esophagus",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369605,
"choiceText": "Middle esophagus",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369606,
"choiceText": "Lower esophagus",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369607,
"choiceText": "Gastroesophageal junction",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369608,
"choiceText": "Pyloric sphincter ",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Foreign objects most commonly become lodged at the narrowest part of the gastrointestinal tract, which is in the upper esophagus at the level of the thoracic inlet. The next most common site is the gastroesophageal junction. Once a foreign object enters the stomach, the chance of it being lodged anywhere along the rest of the gastrointestinal tract is relatively small. Rarely, sharp, long, or large objects can get stuck at the pylorus, the duodenal sweep, or at the ileocecal valve. Such a situation requires intervention.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 106003,
"questionText": "A 21-year-old man with recently diagnosed schizophrenia presents with his parents. For the past hour he has been complaining of pain in his upper abdomen. He admits to swallowing coins. If the patient undergoes endoscopic retrieval of the coin, where is it most likely to be found in the gastrointestinal tract?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 21-Year-Old Man With Epigastric Pain After a Wild Party"
},
{
"authors": "Abraham A. Ayantunde, MB BS, FRCS; George G. Araklitis, MB BS, BSc",
"content": [],
"date": "December 14, 2022",
"figures": [],
"markdown": "# A 21-Year-Old Man With Epigastric Pain After a Wild Party\n\n **Authors:** Abraham A. Ayantunde, MB BS, FRCS; George G. Araklitis, MB BS, BSc \n **Date:** December 14, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 369599,
"choiceText": "Conservative management",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369600,
"choiceText": "Lateral x-ray",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369601,
"choiceText": "Serial x-rays",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369602,
"choiceText": "Endoscopic retrieval ",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369603,
"choiceText": "Surgery ",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The next step is a lateral x-ray because the mother does not know what the child swallowed. In this case, the need arises to differentiate between commonly ingested circular foreign bodies such as coins and corrosive disc batteries. This also helps to ascertain the position of the foreign body in the esophagus. Once a coin has been identified, conservative management can be used.</p><p>Serial x-rays should be taken to establish whether the coin has passed through the narrowest part of the gastrointestinal tract (the esophagus). If the coin remains in the esophagus, endoscopy must be considered within 24 hours after first presenting to the hospital for the object's removal in order to avoid the risk for esophageal pressure necrosis and perforation. Surgery is a very rare management option for an uncommon failure of endoscopic retrieval.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 106002,
"questionText": "A concerned mother presents with her 1-year-old child, who she believes swallowed an unknown object 35 minutes earlier. An initial single plain chest x-ray in the anteroposterior view shows a circular object in the esophagus. Which should be the next step in the management of this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 369604,
"choiceText": "Upper esophagus",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369605,
"choiceText": "Middle esophagus",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369606,
"choiceText": "Lower esophagus",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369607,
"choiceText": "Gastroesophageal junction",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369608,
"choiceText": "Pyloric sphincter ",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Foreign objects most commonly become lodged at the narrowest part of the gastrointestinal tract, which is in the upper esophagus at the level of the thoracic inlet. The next most common site is the gastroesophageal junction. Once a foreign object enters the stomach, the chance of it being lodged anywhere along the rest of the gastrointestinal tract is relatively small. Rarely, sharp, long, or large objects can get stuck at the pylorus, the duodenal sweep, or at the ileocecal valve. Such a situation requires intervention.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 106003,
"questionText": "A 21-year-old man with recently diagnosed schizophrenia presents with his parents. For the past hour he has been complaining of pain in his upper abdomen. He admits to swallowing coins. If the patient undergoes endoscopic retrieval of the coin, where is it most likely to be found in the gastrointestinal tract?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 21-Year-Old Man With Epigastric Pain After a Wild Party"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 369595,
"choiceText": "External monitoring device",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369596,
"choiceText": "Radiologic artifact",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369597,
"choiceText": "Foreign-body ingestion",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369598,
"choiceText": "An implanted medical device",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 106001,
"questionText": "What abnormality is seen on the x-ray?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 369599,
"choiceText": "Conservative management",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369600,
"choiceText": "Lateral x-ray",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369601,
"choiceText": "Serial x-rays",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369602,
"choiceText": "Endoscopic retrieval ",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369603,
"choiceText": "Surgery ",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The next step is a lateral x-ray because the mother does not know what the child swallowed. In this case, the need arises to differentiate between commonly ingested circular foreign bodies such as coins and corrosive disc batteries. This also helps to ascertain the position of the foreign body in the esophagus. Once a coin has been identified, conservative management can be used.</p><p>Serial x-rays should be taken to establish whether the coin has passed through the narrowest part of the gastrointestinal tract (the esophagus). If the coin remains in the esophagus, endoscopy must be considered within 24 hours after first presenting to the hospital for the object's removal in order to avoid the risk for esophageal pressure necrosis and perforation. Surgery is a very rare management option for an uncommon failure of endoscopic retrieval.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 106002,
"questionText": "A concerned mother presents with her 1-year-old child, who she believes swallowed an unknown object 35 minutes earlier. An initial single plain chest x-ray in the anteroposterior view shows a circular object in the esophagus. Which should be the next step in the management of this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 369604,
"choiceText": "Upper esophagus",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369605,
"choiceText": "Middle esophagus",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369606,
"choiceText": "Lower esophagus",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369607,
"choiceText": "Gastroesophageal junction",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 369608,
"choiceText": "Pyloric sphincter ",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Foreign objects most commonly become lodged at the narrowest part of the gastrointestinal tract, which is in the upper esophagus at the level of the thoracic inlet. The next most common site is the gastroesophageal junction. Once a foreign object enters the stomach, the chance of it being lodged anywhere along the rest of the gastrointestinal tract is relatively small. Rarely, sharp, long, or large objects can get stuck at the pylorus, the duodenal sweep, or at the ileocecal valve. Such a situation requires intervention.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 106003,
"questionText": "A 21-year-old man with recently diagnosed schizophrenia presents with his parents. For the past hour he has been complaining of pain in his upper abdomen. He admits to swallowing coins. If the patient undergoes endoscopic retrieval of the coin, where is it most likely to be found in the gastrointestinal tract?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
984871 | /viewarticle/984871 | [
{
"authors": "Vivian Vega, MD; Antonia Fernandez, MD; Simon S. Rabinowitz, MD, PhD; Meredith E. Pittman, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 19-year-old who received a diagnosis of ileocolonic Crohn's disease at age 5 years is referred by his primary pediatrician after laboratory studies performed at his annual visit revealed dyslipidemia and elevated liver enzyme levels. A fasting lipid panel demonstrated an elevated total cholesterol level of 232 mg/dL (reference range, < 170 mg/dL), a triglyceride level of 125 mg/dL (reference range, 40-163 mg/dL), and a low-density lipoprotein cholesterol level of 114 mg/dL (reference range, < 100 mg/dL). His aspartate aminotransferase (AST) level was 192 U/L (reference range, 0-35 U/L), alanine aminotransferase (ALT) level was 149 U/L (reference range, 7-56 U/L), total bilirubin level was 0.9 mg/dL (reference range, 0.3-1.0 mg/dL), and alkaline phosphatase (ALP) level was 534 U/L (reference range, 44-147 U/L).",
"The patient reports that he has been completely asymptomatic. At the time of the pandemic, he had not followed up with his physicians for 4 years and had stopped taking all of his medications.",
"His most recent gastroenterology visit before the current one was 5 years prior. At that time, he had decided to stop taking 6-mercaptopurine and mesalamine for about 1 year. Laboratory studies performed at that visit revealed that his AST and ALT levels were slightly increased to the upper limits of normal, and the plan was to repeat them at the next visit.",
"During the current visit, he once again reports that he has had no symptoms, including nighttime bowel movements, diarrhea, hematochezia, tenesmus, abdominal pain, icteric sclerae, rash, oral ulcers, and generalized pruritus. He passes a painless, formed bowel movement daily, with no blood.",
"The patient attends college full time as an honor student and works part time. He is sexually active with a female partner and consistently uses condoms. He denies the use of alcohol, tobacco products, vaping, and prescription or illicit drugs, including over-the-counter, internet, and health food store medications."
],
"date": "December 12, 2022",
"figures": [],
"markdown": "# A 19-Year-Old With Hypercholesterolemia, Transaminitis, and IBD\n\n **Authors:** Vivian Vega, MD; Antonia Fernandez, MD; Simon S. Rabinowitz, MD, PhD; Meredith E. Pittman, MD \n **Date:** December 12, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 19-year-old who received a diagnosis of ileocolonic Crohn's disease at age 5 years is referred by his primary pediatrician after laboratory studies performed at his annual visit revealed dyslipidemia and elevated liver enzyme levels. A fasting lipid panel demonstrated an elevated total cholesterol level of 232 mg/dL (reference range, < 170 mg/dL), a triglyceride level of 125 mg/dL (reference range, 40-163 mg/dL), and a low-density lipoprotein cholesterol level of 114 mg/dL (reference range, < 100 mg/dL). His aspartate aminotransferase (AST) level was 192 U/L (reference range, 0-35 U/L), alanine aminotransferase (ALT) level was 149 U/L (reference range, 7-56 U/L), total bilirubin level was 0.9 mg/dL (reference range, 0.3-1.0 mg/dL), and alkaline phosphatase (ALP) level was 534 U/L (reference range, 44-147 U/L).\nThe patient reports that he has been completely asymptomatic. At the time of the pandemic, he had not followed up with his physicians for 4 years and had stopped taking all of his medications.\nHis most recent gastroenterology visit before the current one was 5 years prior. At that time, he had decided to stop taking 6-mercaptopurine and mesalamine for about 1 year. Laboratory studies performed at that visit revealed that his AST and ALT levels were slightly increased to the upper limits of normal, and the plan was to repeat them at the next visit.\nDuring the current visit, he once again reports that he has had no symptoms, including nighttime bowel movements, diarrhea, hematochezia, tenesmus, abdominal pain, icteric sclerae, rash, oral ulcers, and generalized pruritus. He passes a painless, formed bowel movement daily, with no blood.\nThe patient attends college full time as an honor student and works part time. He is sexually active with a female partner and consistently uses condoms. He denies the use of alcohol, tobacco products, vaping, and prescription or illicit drugs, including over-the-counter, internet, and health food store medications.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A 19-Year-Old With Hypercholesterolemia, Transaminitis, and IBD"
},
{
"authors": "Vivian Vega, MD; Antonia Fernandez, MD; Simon S. Rabinowitz, MD, PhD; Meredith E. Pittman, MD",
"content": [
"Upon examination, the patient is well-developed and well-nourished and is in no acute distress. His vital signs include a temperature of 98.5 °F (36.9 °C), a heart rate of 88 beats/min, a respiration rate of 16 breaths/min, a blood pressure of 102/63 mm Hg, and an oxygen saturation of 98% on room air. His weight is 143 lb (65 kg), his height is 5 ft 5 in (1.65 m), and his body mass index is 23.9.",
"His head is normocephalic and shows no evidence of trauma. The sclerae are anicteric. The mucous membranes are pink and moist, and no oral ulcers are noted. There are no dermatologic lesions, erythema, or jaundice. The patient has good airway entry bilaterally and no increased work of breathing. His heart rate and rhythm are regular, heart sounds are normal, no murmurs are detected, and distal pulses are intact.",
"His abdomen is soft, nontender, and not distended; bowel sounds are normal. No palpable masses are detected. His spleen is not palpable. His liver is slightly enlarged with a smooth liver edge, which is neither tender nor firm. No costovertebral angle tenderness is noted, and no perianal lesions are found. The results of his neurologic examination are grossly normal.",
"The patient's inflammatory markers are elevated. His erythrocyte sedimentation rate is 41 mm/h (reference range, 0-15 mm/h), his C-reactive protein level is 8 mg/L (reference range, < 10.0 mg/L), and his fecal calprotectin level is higher than 2000 µg/g (reference range, 50-120 µg/g). A repeat comprehensive metabolic panel and lipid profile confirm the earlier results obtained at the visit to his pediatrician.",
"Colonoscopy shows chronic active colitis from the cecum to the descending colon, without evidence of significant inflammation in the sigmoid or rectum. Results of magnetic resonance enterography of his abdomen and pelvis demonstrate normal small and large bowel signals, without focal dilation or strictures. The liver is enlarged to 18.8 cm, with a normal background and no focal lesions. The extrahepatic biliary duct system is unremarkable.",
"Serology results for hepatitis viruses A, B, and C; ceruloplasmin; alpha 1 antitrypsin; anti–smooth muscle antibody; antinuclear antibody (ANA); and antimitochondrial antibody are all negative. Lysosomal acid lipase (LAL) activity is borderline low but higher than what would be observed in true LAL deficiency."
],
"date": "December 12, 2022",
"figures": [],
"markdown": "# A 19-Year-Old With Hypercholesterolemia, Transaminitis, and IBD\n\n **Authors:** Vivian Vega, MD; Antonia Fernandez, MD; Simon S. Rabinowitz, MD, PhD; Meredith E. Pittman, MD \n **Date:** December 12, 2022\n\n ## Content\n\n Upon examination, the patient is well-developed and well-nourished and is in no acute distress. His vital signs include a temperature of 98.5 °F (36.9 °C), a heart rate of 88 beats/min, a respiration rate of 16 breaths/min, a blood pressure of 102/63 mm Hg, and an oxygen saturation of 98% on room air. His weight is 143 lb (65 kg), his height is 5 ft 5 in (1.65 m), and his body mass index is 23.9.\nHis head is normocephalic and shows no evidence of trauma. The sclerae are anicteric. The mucous membranes are pink and moist, and no oral ulcers are noted. There are no dermatologic lesions, erythema, or jaundice. The patient has good airway entry bilaterally and no increased work of breathing. His heart rate and rhythm are regular, heart sounds are normal, no murmurs are detected, and distal pulses are intact.\nHis abdomen is soft, nontender, and not distended; bowel sounds are normal. No palpable masses are detected. His spleen is not palpable. His liver is slightly enlarged with a smooth liver edge, which is neither tender nor firm. No costovertebral angle tenderness is noted, and no perianal lesions are found. The results of his neurologic examination are grossly normal.\nThe patient's inflammatory markers are elevated. His erythrocyte sedimentation rate is 41 mm/h (reference range, 0-15 mm/h), his C-reactive protein level is 8 mg/L (reference range, < 10.0 mg/L), and his fecal calprotectin level is higher than 2000 µg/g (reference range, 50-120 µg/g). A repeat comprehensive metabolic panel and lipid profile confirm the earlier results obtained at the visit to his pediatrician.\nColonoscopy shows chronic active colitis from the cecum to the descending colon, without evidence of significant inflammation in the sigmoid or rectum. Results of magnetic resonance enterography of his abdomen and pelvis demonstrate normal small and large bowel signals, without focal dilation or strictures. The liver is enlarged to 18.8 cm, with a normal background and no focal lesions. The extrahepatic biliary duct system is unremarkable.\nSerology results for hepatitis viruses A, B, and C; ceruloplasmin; alpha 1 antitrypsin; anti–smooth muscle antibody; antinuclear antibody (ANA); and antimitochondrial antibody are all negative. Lysosomal acid lipase (LAL) activity is borderline low but higher than what would be observed in true LAL deficiency.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1747031,
"choiceText": "Hepatitis B virus infection",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747032,
"choiceText": "Autoimmune hepatitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747033,
"choiceText": "Primary biliary cholangitis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747034,
"choiceText": "Primary sclerosing cholangitis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747035,
"choiceText": "Lysosomal acid lipase deficiency",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 564328,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 19-Year-Old With Hypercholesterolemia, Transaminitis, and IBD"
},
{
"authors": "Vivian Vega, MD; Antonia Fernandez, MD; Simon S. Rabinowitz, MD, PhD; Meredith E. Pittman, MD",
"content": [
"In addition to primary sclerosing cholangitis (PSC), the diagnostic considerations in a young adult with inflammatory bowel disease (IBD), elevated liver enzymes, and hyperlipidemia include hepatitis B virus infection, autoimmune hepatitis, primary biliary cholangitis, and LAL deficiency.[1] Viral hepatitis should always be considered in a sexually active teenager or young adult with an abrupt increase in aminotransferases levels.[2] Most patients in this age group would also have cholestasis. The patient in this case had negative serology results for hepatitis B.",
"Autoimmune hepatitis is a chronic hepatocellular disease caused by a loss of tolerance to hepatocyte-specific autoantigens. The disease is characterized by elevated levels of aminotransferases, nonspecific autoantibodies, and immunoglobulin (Ig) G. Autoimmune hepatitis has a female predilection and occurs in both children and adults worldwide among all ethnicities and races.[3] It should be considered in the differential diagnosis of all patients who present with acute or chronic liver disease, including acute liver failure in previously asymptomatic patients.[4] Autoimmune hepatitis has been described in patients with IBD; however, in the patient in this case, testing for ANA and anti–smooth muscle antibodies was negative.[3,4]",
"Primary biliary cholangitis, also known as primary biliary cirrhosis, is an autoimmune disorder that usually presents with increased ALP and serum IgM levels, along with antimitochondrial antibodies. Patients with primary biliary cholangitis may present with typical biliary pattern symptoms (jaundice, pruritus, abdominal pain, and fatigue), although up to half are asymptomatic. The disorder has been described in patients with IBD but is more commonly seen in women and usually affects middle-aged women. The serologic marker for primary biliary cholangitis is the presence of antimitochondrial antibodies. This diagnosis is unlikely in the patient in this case, given that he is male and testing for antimitochondrial antibodies was negative.[5]",
"LAL deficiency is an autosomal-recessive lysosomal storage disease. The various forms of LAL deficiency have different severities, ranging from cases with early mortality within the first months of life to mild asymptomatic forms in adulthood. Infants with early-onset LAL deficiency usually present with acute illness and failure to thrive. Lysosomal acid lipase is a nonredundant enzyme that hydrolyzes triglycerides and cholesteryl esters. In patients who lack this enzyme, cholesteryl esters and triglycerides progressively accumulate in the lysosomes of hepatocytes and macrophages, inducing organ damage over time. Patients with LAL deficiency typically have low serum levels of lysosomal acid lipase. In the patient in this case, the activity was borderline low but higher than what would be seen in true LAL deficiency.[6,7]"
],
"date": "December 12, 2022",
"figures": [],
"markdown": "# A 19-Year-Old With Hypercholesterolemia, Transaminitis, and IBD\n\n **Authors:** Vivian Vega, MD; Antonia Fernandez, MD; Simon S. Rabinowitz, MD, PhD; Meredith E. Pittman, MD \n **Date:** December 12, 2022\n\n ## Content\n\n In addition to primary sclerosing cholangitis (PSC), the diagnostic considerations in a young adult with inflammatory bowel disease (IBD), elevated liver enzymes, and hyperlipidemia include hepatitis B virus infection, autoimmune hepatitis, primary biliary cholangitis, and LAL deficiency.[1] Viral hepatitis should always be considered in a sexually active teenager or young adult with an abrupt increase in aminotransferases levels.[2] Most patients in this age group would also have cholestasis. The patient in this case had negative serology results for hepatitis B.\nAutoimmune hepatitis is a chronic hepatocellular disease caused by a loss of tolerance to hepatocyte-specific autoantigens. The disease is characterized by elevated levels of aminotransferases, nonspecific autoantibodies, and immunoglobulin (Ig) G. Autoimmune hepatitis has a female predilection and occurs in both children and adults worldwide among all ethnicities and races.[3] It should be considered in the differential diagnosis of all patients who present with acute or chronic liver disease, including acute liver failure in previously asymptomatic patients.[4] Autoimmune hepatitis has been described in patients with IBD; however, in the patient in this case, testing for ANA and anti–smooth muscle antibodies was negative.[3,4]\nPrimary biliary cholangitis, also known as primary biliary cirrhosis, is an autoimmune disorder that usually presents with increased ALP and serum IgM levels, along with antimitochondrial antibodies. Patients with primary biliary cholangitis may present with typical biliary pattern symptoms (jaundice, pruritus, abdominal pain, and fatigue), although up to half are asymptomatic. The disorder has been described in patients with IBD but is more commonly seen in women and usually affects middle-aged women. The serologic marker for primary biliary cholangitis is the presence of antimitochondrial antibodies. This diagnosis is unlikely in the patient in this case, given that he is male and testing for antimitochondrial antibodies was negative.[5]\nLAL deficiency is an autosomal-recessive lysosomal storage disease. The various forms of LAL deficiency have different severities, ranging from cases with early mortality within the first months of life to mild asymptomatic forms in adulthood. Infants with early-onset LAL deficiency usually present with acute illness and failure to thrive. Lysosomal acid lipase is a nonredundant enzyme that hydrolyzes triglycerides and cholesteryl esters. In patients who lack this enzyme, cholesteryl esters and triglycerides progressively accumulate in the lysosomes of hepatocytes and macrophages, inducing organ damage over time. Patients with LAL deficiency typically have low serum levels of lysosomal acid lipase. In the patient in this case, the activity was borderline low but higher than what would be seen in true LAL deficiency.[6,7]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1747031,
"choiceText": "Hepatitis B virus infection",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747032,
"choiceText": "Autoimmune hepatitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747033,
"choiceText": "Primary biliary cholangitis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747034,
"choiceText": "Primary sclerosing cholangitis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747035,
"choiceText": "Lysosomal acid lipase deficiency",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 564328,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 19-Year-Old With Hypercholesterolemia, Transaminitis, and IBD"
},
{
"authors": "Vivian Vega, MD; Antonia Fernandez, MD; Simon S. Rabinowitz, MD, PhD; Meredith E. Pittman, MD",
"content": [
"On the basis of the information provided by the history, physical examination, laboratory studies, colonoscopy, and magnetic resonance studies, a definitive diagnosis could not be made without knowing the liver histology. Thus, a liver biopsy was performed.",
"The liver biopsy was significant for bile duct epithelial damage and increased fibrosis with an \"onion skinning\" pattern (Figure). A few bile ducts showed evidence of mild periductal fibrosis. The biopsy also revealed mild hepatocellular cholestasis and lobular parenchyma with no evidence of steatosis or necroinflammatory activity. CK7 immunostaining highlighted extensive biliary-type metaplasia of the periportal hepatocytes and mild ductal perforation. Iron and periodic acid-Schiff-diastase stains were negative. All of the changes described are consistent with small-duct PSC.",
"Figure. (A) Histologic features of bile duct epithelial damage are present, including overlapping ductular nuclei, loss of nuclei, nuclear vacuolization, and increased fibrosis with an \"onion skinning\" pattern that is atypical for a small portal tract of this size. (B) The presence of numerous ductlike structures at the periphery of the portal tract also suggests an underlying biliary injury. (C) Cytokeratin 7 darkly stains native bile ducts within the portal tract but also highlights an increased number of \"intermediate phenotype\" cells at the periphery of the portal tract. (D) These cells are increased in cholestatic disorders. A trichrome stain demonstrates expansion of the portal tract with early nodular formation, consistent with a chronic disease process.",
"After the biopsy findings were reviewed, further investigation was performed for other potential causes of cholangitis, such as IgG4 cholangiopathy or primary biliary cholangitis. Tests for IgG4, anticardiolipin antibody, and antimitochondrial antibody were negative. CA 19-9 and carcinoembryonic antigen baseline values were obtained for surveillance of cholangiocarcinoma.",
"In patients with primary biliary cholangitis, liver biopsy characteristically shows nonsuppurative cholangitis and mild to moderate portal inflammation. Granulomatous destruction of bile ducts may be present. Primary biliary cholangitis is unlikely in the patient in this case, given that his liver biopsy did not show these findings. Instead, he had the characteristic findings of small-duct PSC.[5]",
"In patients with autoimmune hepatitis, liver biopsy reveals interface hepatitis (piecemeal necrosis). Biopsy results in this patient were not consistent with the typical findings in autoimmune hepatitis. Liver biopsy in patients with LAL deficiency shows evidence of steatosis, often accompanied by fibrosis and cirrhosis. This patient did not have evidence of steatosis on biopsy.[6,7]",
"PSC is a chronic cholestatic liver disease of uncertain etiology that is characterized by inflammation and fibrosis, leading to multifocal biliary strictures.[8] It is closely associated with IBD, primarily ulcerative colitis, but cases related to Crohn's disease have been described. In 90% of cases, PSC involves larger bile ducts that are noted on magnetic resonance studies. The remaining 10% of patients require liver biopsy to evaluate the smaller ductules.[9] Large-ductular PSC typically progresses from biliary fibrosis to cirrhosis, end-stage liver disease, and/or cholangiocarcinoma.[10]",
"PSC is insidious, with a very gradual onset of disease manifestations.[8] About half of patients do not have symptoms and receive a diagnosis only after the results of liver function tests are abnormal.[11] The most frequent signs at diagnosis are hepatomegaly and splenomegaly. If symptoms are present, the most common are abdominal pain, pruritus, jaundice, and fatigue.[11]",
"Two types of PSC are recognized: large duct and small duct.[11] Both feature biochemical evidence of cholestasis. Large-duct PSC has cholangiographic findings of one or more of these within large- or medium-sized bile ducts[9]:",
"Focal stricturing of bile ducts",
"Dominant stricture of common bile duct",
"Saccular dilation of bile ducts",
"Beaded appearance of bile ducts",
"Pruning appearance of the distal bile duct branches",
"In contrast, cholangiographic findings in patients with small-duct PSC are normal.[12] Histologic features that characterize definitive small-duct PSC include periductal fibrosis/onion skinning around interlobular bile ducts or smaller profiles. Some hepatologists believe that the diagnosis of small-duct PSC requires three or more of these liver histology criteria[1,9,13]:",
"Periductal edema",
"Periductal concentric inflammation",
"Bile duct epithelial injury",
"Ductular reaction",
"Neutrophils in the bile ducts",
"About two thirds of patients with PSC also have IBD. Most commonly, patients have ulcerative colitis with pancolonic involvement, but those with PSC can have Crohn's disease. A disease distribution that features a right-sided predominance with subtle ileal inflammation (\"backwash\" ileitis) and rectal sparing has been described.[9,10,14]"
],
"date": "December 12, 2022",
"figures": [],
"markdown": "# A 19-Year-Old With Hypercholesterolemia, Transaminitis, and IBD\n\n **Authors:** Vivian Vega, MD; Antonia Fernandez, MD; Simon S. Rabinowitz, MD, PhD; Meredith E. Pittman, MD \n **Date:** December 12, 2022\n\n ## Content\n\n On the basis of the information provided by the history, physical examination, laboratory studies, colonoscopy, and magnetic resonance studies, a definitive diagnosis could not be made without knowing the liver histology. Thus, a liver biopsy was performed.\nThe liver biopsy was significant for bile duct epithelial damage and increased fibrosis with an \"onion skinning\" pattern (Figure). A few bile ducts showed evidence of mild periductal fibrosis. The biopsy also revealed mild hepatocellular cholestasis and lobular parenchyma with no evidence of steatosis or necroinflammatory activity. CK7 immunostaining highlighted extensive biliary-type metaplasia of the periportal hepatocytes and mild ductal perforation. Iron and periodic acid-Schiff-diastase stains were negative. All of the changes described are consistent with small-duct PSC.\nFigure. (A) Histologic features of bile duct epithelial damage are present, including overlapping ductular nuclei, loss of nuclei, nuclear vacuolization, and increased fibrosis with an \"onion skinning\" pattern that is atypical for a small portal tract of this size. (B) The presence of numerous ductlike structures at the periphery of the portal tract also suggests an underlying biliary injury. (C) Cytokeratin 7 darkly stains native bile ducts within the portal tract but also highlights an increased number of \"intermediate phenotype\" cells at the periphery of the portal tract. (D) These cells are increased in cholestatic disorders. A trichrome stain demonstrates expansion of the portal tract with early nodular formation, consistent with a chronic disease process.\nAfter the biopsy findings were reviewed, further investigation was performed for other potential causes of cholangitis, such as IgG4 cholangiopathy or primary biliary cholangitis. Tests for IgG4, anticardiolipin antibody, and antimitochondrial antibody were negative. CA 19-9 and carcinoembryonic antigen baseline values were obtained for surveillance of cholangiocarcinoma.\nIn patients with primary biliary cholangitis, liver biopsy characteristically shows nonsuppurative cholangitis and mild to moderate portal inflammation. Granulomatous destruction of bile ducts may be present. Primary biliary cholangitis is unlikely in the patient in this case, given that his liver biopsy did not show these findings. Instead, he had the characteristic findings of small-duct PSC.[5]\nIn patients with autoimmune hepatitis, liver biopsy reveals interface hepatitis (piecemeal necrosis). Biopsy results in this patient were not consistent with the typical findings in autoimmune hepatitis. Liver biopsy in patients with LAL deficiency shows evidence of steatosis, often accompanied by fibrosis and cirrhosis. This patient did not have evidence of steatosis on biopsy.[6,7]\nPSC is a chronic cholestatic liver disease of uncertain etiology that is characterized by inflammation and fibrosis, leading to multifocal biliary strictures.[8] It is closely associated with IBD, primarily ulcerative colitis, but cases related to Crohn's disease have been described. In 90% of cases, PSC involves larger bile ducts that are noted on magnetic resonance studies. The remaining 10% of patients require liver biopsy to evaluate the smaller ductules.[9] Large-ductular PSC typically progresses from biliary fibrosis to cirrhosis, end-stage liver disease, and/or cholangiocarcinoma.[10]\nPSC is insidious, with a very gradual onset of disease manifestations.[8] About half of patients do not have symptoms and receive a diagnosis only after the results of liver function tests are abnormal.[11] The most frequent signs at diagnosis are hepatomegaly and splenomegaly. If symptoms are present, the most common are abdominal pain, pruritus, jaundice, and fatigue.[11]\nTwo types of PSC are recognized: large duct and small duct.[11] Both feature biochemical evidence of cholestasis. Large-duct PSC has cholangiographic findings of one or more of these within large- or medium-sized bile ducts[9]:\nFocal stricturing of bile ducts\nDominant stricture of common bile duct\nSaccular dilation of bile ducts\nBeaded appearance of bile ducts\nPruning appearance of the distal bile duct branches\nIn contrast, cholangiographic findings in patients with small-duct PSC are normal.[12] Histologic features that characterize definitive small-duct PSC include periductal fibrosis/onion skinning around interlobular bile ducts or smaller profiles. Some hepatologists believe that the diagnosis of small-duct PSC requires three or more of these liver histology criteria[1,9,13]:\nPeriductal edema\nPeriductal concentric inflammation\nBile duct epithelial injury\nDuctular reaction\nNeutrophils in the bile ducts\nAbout two thirds of patients with PSC also have IBD. Most commonly, patients have ulcerative colitis with pancolonic involvement, but those with PSC can have Crohn's disease. A disease distribution that features a right-sided predominance with subtle ileal inflammation (\"backwash\" ileitis) and rectal sparing has been described.[9,10,14]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A 19-Year-Old With Hypercholesterolemia, Transaminitis, and IBD"
},
{
"authors": "Vivian Vega, MD; Antonia Fernandez, MD; Simon S. Rabinowitz, MD, PhD; Meredith E. Pittman, MD",
"content": [
"PSC has a highly variable natural history, and predicting which patients will progress to end-stage liver disease or cholangiocarcinoma is difficult. Studies have shown that the mean time from diagnosis to death or liver transplant ranges from 10 to 22 years.[1] Mortality in patients with PSC is four times higher than in the general population. Despite the harsh prognosis, a proportion of patients may never need a liver transplant. However, any patient with PSC should be assessed for IBD with a total colonoscopy with biopsies, as the combination of PSC and IBD increases the risk for colorectal cancer.[9]",
"Factors that are associated with a good prognosis include younger age at diagnosis, female sex, small-duct disease, Crohn's disease (as opposed to ulcerative colitis), and a normal or mildly elevated ALP level. Poor prognostic factors include extensive intrahepatic and/or extrahepatic biliary involvement, liver synthetic dysfunction or portal hypertension, severe parenchymal fibrosis or cirrhosis, and jaundice.[1,9]",
"After the diagnosis was established in this case, the patient and his family were informed that currently no medical treatment is available that is proven to alter the progression of small-duct PSC. Several drugs have been attempted that are currently used for other cholestatic liver diseases, such as ursodeoxycholic acid and anti–tumor necrosis factor (anti-TNF) drugs, which are frequently used for IBD.[15] Treatment with ursodeoxycholic acid does not alter disease progression, with no differences for patients when death, liver transplantation, or the development of large-duct PSC are compared. The use of anti-TNF drugs, such as adalimumab and infliximab, has been described in patients who also have IBD. After much discussion with the patient and his family, it was decided to start adalimumab, ursodeoxycholic acid, and cholestyramine, with close follow-up including colonic and liver histology."
],
"date": "December 12, 2022",
"figures": [],
"markdown": "# A 19-Year-Old With Hypercholesterolemia, Transaminitis, and IBD\n\n **Authors:** Vivian Vega, MD; Antonia Fernandez, MD; Simon S. Rabinowitz, MD, PhD; Meredith E. Pittman, MD \n **Date:** December 12, 2022\n\n ## Content\n\n PSC has a highly variable natural history, and predicting which patients will progress to end-stage liver disease or cholangiocarcinoma is difficult. Studies have shown that the mean time from diagnosis to death or liver transplant ranges from 10 to 22 years.[1] Mortality in patients with PSC is four times higher than in the general population. Despite the harsh prognosis, a proportion of patients may never need a liver transplant. However, any patient with PSC should be assessed for IBD with a total colonoscopy with biopsies, as the combination of PSC and IBD increases the risk for colorectal cancer.[9]\nFactors that are associated with a good prognosis include younger age at diagnosis, female sex, small-duct disease, Crohn's disease (as opposed to ulcerative colitis), and a normal or mildly elevated ALP level. Poor prognostic factors include extensive intrahepatic and/or extrahepatic biliary involvement, liver synthetic dysfunction or portal hypertension, severe parenchymal fibrosis or cirrhosis, and jaundice.[1,9]\nAfter the diagnosis was established in this case, the patient and his family were informed that currently no medical treatment is available that is proven to alter the progression of small-duct PSC. Several drugs have been attempted that are currently used for other cholestatic liver diseases, such as ursodeoxycholic acid and anti–tumor necrosis factor (anti-TNF) drugs, which are frequently used for IBD.[15] Treatment with ursodeoxycholic acid does not alter disease progression, with no differences for patients when death, liver transplantation, or the development of large-duct PSC are compared. The use of anti-TNF drugs, such as adalimumab and infliximab, has been described in patients who also have IBD. After much discussion with the patient and his family, it was decided to start adalimumab, ursodeoxycholic acid, and cholestyramine, with close follow-up including colonic and liver histology.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1747036,
"choiceText": "Decreased bilirubin levels",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747037,
"choiceText": "Abnormalities on magnetic resonance cholangiopancreatography or endoscopic retrograde cholangiopancreatography",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747038,
"choiceText": "ALP levels in the lower reference range",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747039,
"choiceText": "Periductal fibrosis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Small-duct PSC is characterized by the findings of cholestasis on the chemistry panel, including elevations in bilirubin, gamma-glutamyl transferase, and/or ALP. Some of the histologic findings of PSC include periductal fibrosis, which is described as onion skinning around the interlobular bile ducts, and smaller profiles. Other histologic findings include periductal concentric inflammation, bile duct epithelial injury, ductular reaction, and the presence of neutrophils in the bile duct. If a magnetic resonance cholangiopancreatography or an endoscopic retrograde cholangiopancreatography is performed, the study will not show evidence of cholangiographic abnormalities.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 564329,
"questionText": "Which is most consistent with small-duct PSC?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1747040,
"choiceText": "Extensive intrahepatic or extrahepatic biliary involvement",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747041,
"choiceText": "Cirrhosis with portal hypertension",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747042,
"choiceText": "Small-duct disease",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747043,
"choiceText": "Evidence of liver synthetic dysfunction",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Extensive intrahepatic or extrahepatic biliary involvement, cirrhosis with portal hypertension, and evidence of liver synthetic dysfunction all indicate advanced liver disease. Other adverse prognostic factors are dominant strictures, recurrent cholangitis, and ulcerative colitis (as opposed to Crohn's disease). Favorable prognostic factors are younger age at diagnosis, female sex, mildly elevated or normal ALP concentration (whether or not the patient is given ursodeoxycholic acid), small-duct disease, and PSC with features of autoimmune hepatitis (a worse prognosis than classic autoimmune hepatitis but a better prognosis than classic PSC).<sup>[11]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 564330,
"questionText": "Which of these factors is associated with the best prognosis in PSC?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 19-Year-Old With Hypercholesterolemia, Transaminitis, and IBD"
},
{
"authors": "Vivian Vega, MD; Antonia Fernandez, MD; Simon S. Rabinowitz, MD, PhD; Meredith E. Pittman, MD",
"content": [
"Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult."
],
"date": "December 12, 2022",
"figures": [],
"markdown": "# A 19-Year-Old With Hypercholesterolemia, Transaminitis, and IBD\n\n **Authors:** Vivian Vega, MD; Antonia Fernandez, MD; Simon S. Rabinowitz, MD, PhD; Meredith E. Pittman, MD \n **Date:** December 12, 2022\n\n ## Content\n\n Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult.\n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1747036,
"choiceText": "Decreased bilirubin levels",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747037,
"choiceText": "Abnormalities on magnetic resonance cholangiopancreatography or endoscopic retrograde cholangiopancreatography",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747038,
"choiceText": "ALP levels in the lower reference range",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747039,
"choiceText": "Periductal fibrosis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Small-duct PSC is characterized by the findings of cholestasis on the chemistry panel, including elevations in bilirubin, gamma-glutamyl transferase, and/or ALP. Some of the histologic findings of PSC include periductal fibrosis, which is described as onion skinning around the interlobular bile ducts, and smaller profiles. Other histologic findings include periductal concentric inflammation, bile duct epithelial injury, ductular reaction, and the presence of neutrophils in the bile duct. If a magnetic resonance cholangiopancreatography or an endoscopic retrograde cholangiopancreatography is performed, the study will not show evidence of cholangiographic abnormalities.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 564329,
"questionText": "Which is most consistent with small-duct PSC?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1747040,
"choiceText": "Extensive intrahepatic or extrahepatic biliary involvement",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747041,
"choiceText": "Cirrhosis with portal hypertension",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747042,
"choiceText": "Small-duct disease",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747043,
"choiceText": "Evidence of liver synthetic dysfunction",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Extensive intrahepatic or extrahepatic biliary involvement, cirrhosis with portal hypertension, and evidence of liver synthetic dysfunction all indicate advanced liver disease. Other adverse prognostic factors are dominant strictures, recurrent cholangitis, and ulcerative colitis (as opposed to Crohn's disease). Favorable prognostic factors are younger age at diagnosis, female sex, mildly elevated or normal ALP concentration (whether or not the patient is given ursodeoxycholic acid), small-duct disease, and PSC with features of autoimmune hepatitis (a worse prognosis than classic autoimmune hepatitis but a better prognosis than classic PSC).<sup>[11]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 564330,
"questionText": "Which of these factors is associated with the best prognosis in PSC?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 19-Year-Old With Hypercholesterolemia, Transaminitis, and IBD"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1747031,
"choiceText": "Hepatitis B virus infection",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747032,
"choiceText": "Autoimmune hepatitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747033,
"choiceText": "Primary biliary cholangitis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747034,
"choiceText": "Primary sclerosing cholangitis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747035,
"choiceText": "Lysosomal acid lipase deficiency",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 564328,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1747036,
"choiceText": "Decreased bilirubin levels",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747037,
"choiceText": "Abnormalities on magnetic resonance cholangiopancreatography or endoscopic retrograde cholangiopancreatography",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747038,
"choiceText": "ALP levels in the lower reference range",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747039,
"choiceText": "Periductal fibrosis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Small-duct PSC is characterized by the findings of cholestasis on the chemistry panel, including elevations in bilirubin, gamma-glutamyl transferase, and/or ALP. Some of the histologic findings of PSC include periductal fibrosis, which is described as onion skinning around the interlobular bile ducts, and smaller profiles. Other histologic findings include periductal concentric inflammation, bile duct epithelial injury, ductular reaction, and the presence of neutrophils in the bile duct. If a magnetic resonance cholangiopancreatography or an endoscopic retrograde cholangiopancreatography is performed, the study will not show evidence of cholangiographic abnormalities.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 564329,
"questionText": "Which is most consistent with small-duct PSC?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1747040,
"choiceText": "Extensive intrahepatic or extrahepatic biliary involvement",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747041,
"choiceText": "Cirrhosis with portal hypertension",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747042,
"choiceText": "Small-duct disease",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1747043,
"choiceText": "Evidence of liver synthetic dysfunction",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Extensive intrahepatic or extrahepatic biliary involvement, cirrhosis with portal hypertension, and evidence of liver synthetic dysfunction all indicate advanced liver disease. Other adverse prognostic factors are dominant strictures, recurrent cholangitis, and ulcerative colitis (as opposed to Crohn's disease). Favorable prognostic factors are younger age at diagnosis, female sex, mildly elevated or normal ALP concentration (whether or not the patient is given ursodeoxycholic acid), small-duct disease, and PSC with features of autoimmune hepatitis (a worse prognosis than classic autoimmune hepatitis but a better prognosis than classic PSC).<sup>[11]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 564330,
"questionText": "Which of these factors is associated with the best prognosis in PSC?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
882400 | /viewarticle/882400 | [
{
"authors": "Noah Gudel, DO; Lisa M. Rock, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 51-year-old woman presents with severe abdominal pain. She states that the pain started 9 months ago and occurs about every 3-4 weeks, with each episode lasting 2-3 days at a time. She describes the pain as \"excruciating\" when it occurs, causing her to double over, and it is diffuse across the abdomen. Although no episodes of emesis have occurred, severe nausea is associated with the pain.",
"The patient cannot cite any alleviating or aggravating factors. The pain does not improve after a bowel movement, and she has noticed no changes in her bowel habits. The pain has not affected her appetite, and she denies having fever, chills, melena, or hematochezia.",
"The patient has not experienced any recent weight loss. Her medical history is significant for gastroesophageal reflux disease, irritable bowel syndrome, bilateral ovarian cysts, and depression. Her medications include esomeprazole, aspirin, bupropion, and alprazolam, as needed. She is also taking acetaminophen/hydrocodone as needed for abdominal pain.",
"The patient's surgical history is significant for a vaginal hysterectomy. The family and social histories are noncontributory.",
"The patient notes that in the past 9 months, she has had CT of the abdomen and pelvis, as well as colonoscopy; the results of both studies were unremarkable at that time (except for the previously diagnosed ovarian cysts)."
],
"date": "December 07, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: Excruciating Abdominal Pain in a Woman Taking Benzodiazepines and Narcotics\n\n **Authors:** Noah Gudel, DO; Lisa M. Rock, MD \n **Date:** December 07, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 51-year-old woman presents with severe abdominal pain. She states that the pain started 9 months ago and occurs about every 3-4 weeks, with each episode lasting 2-3 days at a time. She describes the pain as \"excruciating\" when it occurs, causing her to double over, and it is diffuse across the abdomen. Although no episodes of emesis have occurred, severe nausea is associated with the pain.\nThe patient cannot cite any alleviating or aggravating factors. The pain does not improve after a bowel movement, and she has noticed no changes in her bowel habits. The pain has not affected her appetite, and she denies having fever, chills, melena, or hematochezia.\nThe patient has not experienced any recent weight loss. Her medical history is significant for gastroesophageal reflux disease, irritable bowel syndrome, bilateral ovarian cysts, and depression. Her medications include esomeprazole, aspirin, bupropion, and alprazolam, as needed. She is also taking acetaminophen/hydrocodone as needed for abdominal pain.\nThe patient's surgical history is significant for a vaginal hysterectomy. The family and social histories are noncontributory.\nThe patient notes that in the past 9 months, she has had CT of the abdomen and pelvis, as well as colonoscopy; the results of both studies were unremarkable at that time (except for the previously diagnosed ovarian cysts).\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Gastro Case Challenge: Excruciating Abdominal Pain in a Woman Taking Benzodiazepines and Narcotics"
},
{
"authors": "Noah Gudel, DO; Lisa M. Rock, MD",
"content": [
"The physical examination reveals an overweight white woman in no acute distress. Her weight is 190 lb (86.2 kg), and her height is 5'5\" (1.65 m). Her body mass index is 31.6.",
"The patient's oral temperature is 98.4°F (36.9°C). Her blood pressure is 138/88 mm Hg; her pulse is regular, at 75 beats/min; and her heart sounds are normal, without any murmurs, rubs, or gallops. The patient's respirations are 14 breaths/min and unlabored, and her lungs are clear to auscultation.",
"Examination of the head and neck is unremarkable. Abdominal examination reveals a nontender and nondistended abdomen, with normal bowel sounds. No rebound, rigidity, or guarding is noted, and no masses are palpated. A rectal examination is not performed. The extremities exhibit normal range of motion, and no clubbing, cyanosis, or edema is observed.",
"The patient states that several days prior, she had an episode of pain and went to the emergency department (ED) to be examined. Laboratory analysis included urinalysis, complete blood cell count with differential, complete metabolic panel, amylase, and lipase; all values were within normal limits. Abdominal and pelvic CT were repeated during the recent ED visit, and she was told that the preliminary interpretation was \"normal.\" She has brought the official interpretation of her CT scan as well as the films themselves (Figures 1 and 2).",
"Figure 1.",
"Figure 2."
],
"date": "December 07, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/882/400/882400-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/882/400/882400-Thumb2.png"
}
],
"markdown": "# Gastro Case Challenge: Excruciating Abdominal Pain in a Woman Taking Benzodiazepines and Narcotics\n\n **Authors:** Noah Gudel, DO; Lisa M. Rock, MD \n **Date:** December 07, 2022\n\n ## Content\n\n The physical examination reveals an overweight white woman in no acute distress. Her weight is 190 lb (86.2 kg), and her height is 5'5\" (1.65 m). Her body mass index is 31.6.\nThe patient's oral temperature is 98.4°F (36.9°C). Her blood pressure is 138/88 mm Hg; her pulse is regular, at 75 beats/min; and her heart sounds are normal, without any murmurs, rubs, or gallops. The patient's respirations are 14 breaths/min and unlabored, and her lungs are clear to auscultation.\nExamination of the head and neck is unremarkable. Abdominal examination reveals a nontender and nondistended abdomen, with normal bowel sounds. No rebound, rigidity, or guarding is noted, and no masses are palpated. A rectal examination is not performed. The extremities exhibit normal range of motion, and no clubbing, cyanosis, or edema is observed.\nThe patient states that several days prior, she had an episode of pain and went to the emergency department (ED) to be examined. Laboratory analysis included urinalysis, complete blood cell count with differential, complete metabolic panel, amylase, and lipase; all values were within normal limits. Abdominal and pelvic CT were repeated during the recent ED visit, and she was told that the preliminary interpretation was \"normal.\" She has brought the official interpretation of her CT scan as well as the films themselves (Figures 1 and 2).\nFigure 1.\nFigure 2.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1116010,
"choiceText": "Primary epiploic appendagitis",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116012,
"choiceText": "Acute omental infarction",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116014,
"choiceText": "Mesenteric panniculitis\r\n",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116016,
"choiceText": "Appendicitis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353691,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: Excruciating Abdominal Pain in a Woman Taking Benzodiazepines and Narcotics"
},
{
"authors": "Noah Gudel, DO; Lisa M. Rock, MD",
"content": [
"An area of increased attenuation within the mesenteric fat in the right upper quadrant surrounding an area of diminished attenuation was noted, arising from the transverse colon (Figures 3 and 4).",
"Figure 3.",
"Figure 4.",
"The findings were consistent with a diagnosis of epiploic appendagitis. The epiploic appendages (variably termed \"appendices epiploicae\") are pedunculated adipose projections from the serosal surface of the colon. They appear in the fifth month of fetal life, and each appendage contains a venule and one or two arterioles branching off of the vasa recta.[1,2] They are multiple (up to 100) and form two rows that parallel the anterior and posterior taenia coli and run from the cecum to the rectosigmoid junction; they are most prominent along the descending and sigmoid colon.[1,3]",
"Each epiploic appendage is approximately 1-2 cm thick and 0.5-5 cm in length,[1,4] with an average length of 3 cm (although appendages as long as 15 cm have been reported).[5] They are frequently found in association with colonic diverticula and are only visible on diagnostic imaging when surrounded by inflammatory fluid.[4]",
"The term \"primary epiploic appendagitis\" is reserved for cases resulting from spontaneous torsion, thrombosis, ischemia, or inflammation of an epiploic appendage.[1,2,3] Two central factors contribute to the appendages' propensity for torsion, followed by ischemia and/or infarction: They are freely mobile and they have a limited blood supply, consisting of two narrow end arteries and one tortuous vein passing through a narrow pedicle base.[3]",
"The sequence of clinical events is similar to that of appendicitis—namely, an obstruction of some sort, followed by ischemia, thrombosis, and, finally, necrosis. The signs of torsion and necrosis are rarely seen during laparotomy.[6]",
"Secondary epiploic appendagitis is caused by inflammation that extends from adjacent structures (as in diverticulitis, appendicitis, or cholecystitis).[2,3]",
"Vesalius was the first to recognize the appendices epiploicae in 1543, but their potential significance was not recognized until 1853, when Virchow proposed that their detachment may be a source of loose intraperitoneal bodies.[5,7,8] These loose appendages may calcify and may be later seen as incidental findings on diagnostic imaging or laparoscopy; when found reattached to intraperitoneal organs, these epiploic appendages are known as \"parasitized appendices epiploicae.\"[8]",
"The exact role of these appendages is not known, although there are various plausible theories as to their function. Epiploic appendages may protect and cushion the colon, like a small omentum; they may act as a blood depository during colonic vessel contraction; they may store fat; and they may even have a role in absorption and the immune response.[1,9,10] They are also used in surgery to protect suture lines and close perforations.[10]"
],
"date": "December 07, 2022",
"figures": [
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/882/400/882400-Thumb3.png"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/882/400/882400-Thumb4.png"
}
],
"markdown": "# Gastro Case Challenge: Excruciating Abdominal Pain in a Woman Taking Benzodiazepines and Narcotics\n\n **Authors:** Noah Gudel, DO; Lisa M. Rock, MD \n **Date:** December 07, 2022\n\n ## Content\n\n An area of increased attenuation within the mesenteric fat in the right upper quadrant surrounding an area of diminished attenuation was noted, arising from the transverse colon (Figures 3 and 4).\nFigure 3.\nFigure 4.\nThe findings were consistent with a diagnosis of epiploic appendagitis. The epiploic appendages (variably termed \"appendices epiploicae\") are pedunculated adipose projections from the serosal surface of the colon. They appear in the fifth month of fetal life, and each appendage contains a venule and one or two arterioles branching off of the vasa recta.[1,2] They are multiple (up to 100) and form two rows that parallel the anterior and posterior taenia coli and run from the cecum to the rectosigmoid junction; they are most prominent along the descending and sigmoid colon.[1,3]\nEach epiploic appendage is approximately 1-2 cm thick and 0.5-5 cm in length,[1,4] with an average length of 3 cm (although appendages as long as 15 cm have been reported).[5] They are frequently found in association with colonic diverticula and are only visible on diagnostic imaging when surrounded by inflammatory fluid.[4]\nThe term \"primary epiploic appendagitis\" is reserved for cases resulting from spontaneous torsion, thrombosis, ischemia, or inflammation of an epiploic appendage.[1,2,3] Two central factors contribute to the appendages' propensity for torsion, followed by ischemia and/or infarction: They are freely mobile and they have a limited blood supply, consisting of two narrow end arteries and one tortuous vein passing through a narrow pedicle base.[3]\nThe sequence of clinical events is similar to that of appendicitis—namely, an obstruction of some sort, followed by ischemia, thrombosis, and, finally, necrosis. The signs of torsion and necrosis are rarely seen during laparotomy.[6]\nSecondary epiploic appendagitis is caused by inflammation that extends from adjacent structures (as in diverticulitis, appendicitis, or cholecystitis).[2,3]\nVesalius was the first to recognize the appendices epiploicae in 1543, but their potential significance was not recognized until 1853, when Virchow proposed that their detachment may be a source of loose intraperitoneal bodies.[5,7,8] These loose appendages may calcify and may be later seen as incidental findings on diagnostic imaging or laparoscopy; when found reattached to intraperitoneal organs, these epiploic appendages are known as \"parasitized appendices epiploicae.\"[8]\nThe exact role of these appendages is not known, although there are various plausible theories as to their function. Epiploic appendages may protect and cushion the colon, like a small omentum; they may act as a blood depository during colonic vessel contraction; they may store fat; and they may even have a role in absorption and the immune response.[1,9,10] They are also used in surgery to protect suture lines and close perforations.[10]\n\n ## Figures\n\n **Figure 3.** \n \n\n**Figure 4.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1116010,
"choiceText": "Primary epiploic appendagitis",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116012,
"choiceText": "Acute omental infarction",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116014,
"choiceText": "Mesenteric panniculitis\r\n",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116016,
"choiceText": "Appendicitis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353691,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: Excruciating Abdominal Pain in a Woman Taking Benzodiazepines and Narcotics"
},
{
"authors": "Noah Gudel, DO; Lisa M. Rock, MD",
"content": [
"The sigmoid and the cecum are the most common sites of appendagitis, with the former more frequently affected.[11] Because the appendages tend to be larger in the sigmoid, epiploic appendagitis and its accompanying symptoms are most often experienced in the left lower quadrant. However, at least one case is known of a patient with a massive sigmoid that extended into the right iliac fossa who presented with pain in the right lower quadrant.[1] Also, at least one reported case details epiploic appendagitis located within an inguinal hernia sac.[12]",
"Primary epiploic appendagitis is most often mistaken for diverticulitis and appendicitis, depending on the location (diverticulitis in cases of left lower-quadrant pain and appendicitis in cases of right lower-quadrant pain). Of note, primary epiploic appendagitis was the final diagnosis made in 2%-7% of abdominal CT scans that were performed to rule out diverticulitis, and in 1% of CT scans that looked for appendicitis.[13,14] The pain may also mimic that of a hernia, renal or ureteric colic, omental infarction, acute cholecystitis, and pelvic inflammatory disease.[15]",
"The rarity of primary epiploic appendagitis is evidenced by the fact that Sand and colleagues[1] were only able to include 10 patients in their study over 3 years, despite conducting their investigation in an urban academic surgical ED. Although it can present at any age, epiploic appendagitis most commonly presents in the fifth decade of life; it has a slight male preponderance.[1,3,16]",
"Whether or not this condition is more common in overweight or patients with obesity is controversial; multiple studies support either view. The literature does support an increased incidence in overweight or obese patients.[2,12,17] Hanson and Kam[18] reported that epiploic appendagitis is more common not only in patients with obesity, but also in those who have recently lost weight. Strenuous exercise or physical labor by the unaccustomed patient is often recorded as the inciting event.[9,19,20]",
"A patient with epiploic appendagitis generally presents with an acute onset of sharp, localized, nonmigratory abdominal pain, most often in the left lower quadrant (as detailed above). The pain may be aggravated by movement, deep breathing, or coughing.[2] In contrast to other acute abdominal processes (appendicitis, diverticulitis), patients do not generally present with fever, anorexia, nausea, or vomiting. Typically, laboratory study values, including a complete blood cell count, complete metabolic profile, and urinalysis, are within normal limits; however, some patients may have mild leukocytosis.[1,2] Sand and colleagues[1] reported an elevated C-reactive protein (CRP) level in two out of 10 patients in their case series, and hypothesized that the necrosis of epiploic appendagitis triggers an inflammatory response, thereby elevating the CRP level.",
"Before the advent and common use of CT, the diagnosis of primary epiploic appendagitis was made by exploratory laparotomy, wherein the inflamed appendage was then ligated and excised.[21] Proper identification of this condition using radiologic studies, specifically abdominal and pelvic CT, may prevent unnecessary surgical exploration and its associated costs and complications. A study by Rao and colleagues[22] revealed that the average cost per misdiagnosed patient in this situation was $4117.",
"On CT, epiploic appendagitis is represented by a round or oval lesion, typically 2-4 cm in diameter, in close apposition to the colonic wall. More than one half of these cases are located in the sigmoid colon. Surrounded by periappendageal and pericolic fat stranding, the attenuation of the lesion itself is similar to that of fat, but there is often a thin rim of increased density. A central section of hyperattenuation representing an area of venous thrombosis may be intermittently present.[1,4] The proximal colonic wall is not normally thickened, which helps differentiate this condition from diverticulitis; however, the adjacent visceral peritoneum may occasionally be thickened.[1]",
"Identifying epiploic appendagitis with ultrasonography is generally difficult, but the appendage has been described as an oval, hyperechoic, noncompressible mass with a fine hypoechoic rim at the point of maximal tenderness, adjacent to the colon. On color Doppler ultrasonography, lack of central blood flow is observed; this is an important differentiating factor from appendicitis, which would demonstrate increased blood flow.[1,20,23,24]",
"MRI is not typically performed in this patient population; however, epiploic appendagitis can certainly be identified on MRI. T1- and T2-weighted images demonstrate a focal lesion, with a signal intensity similar to that of fat. The addition of contrast to T1-weighted imaging demonstrates a fatty lesion with rim enhancement.[25]",
"Radiologic changes can persist for weeks,[20] but they generally resolve within 6 months of the acute episode.[4]"
],
"date": "December 07, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: Excruciating Abdominal Pain in a Woman Taking Benzodiazepines and Narcotics\n\n **Authors:** Noah Gudel, DO; Lisa M. Rock, MD \n **Date:** December 07, 2022\n\n ## Content\n\n The sigmoid and the cecum are the most common sites of appendagitis, with the former more frequently affected.[11] Because the appendages tend to be larger in the sigmoid, epiploic appendagitis and its accompanying symptoms are most often experienced in the left lower quadrant. However, at least one case is known of a patient with a massive sigmoid that extended into the right iliac fossa who presented with pain in the right lower quadrant.[1] Also, at least one reported case details epiploic appendagitis located within an inguinal hernia sac.[12]\nPrimary epiploic appendagitis is most often mistaken for diverticulitis and appendicitis, depending on the location (diverticulitis in cases of left lower-quadrant pain and appendicitis in cases of right lower-quadrant pain). Of note, primary epiploic appendagitis was the final diagnosis made in 2%-7% of abdominal CT scans that were performed to rule out diverticulitis, and in 1% of CT scans that looked for appendicitis.[13,14] The pain may also mimic that of a hernia, renal or ureteric colic, omental infarction, acute cholecystitis, and pelvic inflammatory disease.[15]\nThe rarity of primary epiploic appendagitis is evidenced by the fact that Sand and colleagues[1] were only able to include 10 patients in their study over 3 years, despite conducting their investigation in an urban academic surgical ED. Although it can present at any age, epiploic appendagitis most commonly presents in the fifth decade of life; it has a slight male preponderance.[1,3,16]\nWhether or not this condition is more common in overweight or patients with obesity is controversial; multiple studies support either view. The literature does support an increased incidence in overweight or obese patients.[2,12,17] Hanson and Kam[18] reported that epiploic appendagitis is more common not only in patients with obesity, but also in those who have recently lost weight. Strenuous exercise or physical labor by the unaccustomed patient is often recorded as the inciting event.[9,19,20]\nA patient with epiploic appendagitis generally presents with an acute onset of sharp, localized, nonmigratory abdominal pain, most often in the left lower quadrant (as detailed above). The pain may be aggravated by movement, deep breathing, or coughing.[2] In contrast to other acute abdominal processes (appendicitis, diverticulitis), patients do not generally present with fever, anorexia, nausea, or vomiting. Typically, laboratory study values, including a complete blood cell count, complete metabolic profile, and urinalysis, are within normal limits; however, some patients may have mild leukocytosis.[1,2] Sand and colleagues[1] reported an elevated C-reactive protein (CRP) level in two out of 10 patients in their case series, and hypothesized that the necrosis of epiploic appendagitis triggers an inflammatory response, thereby elevating the CRP level.\nBefore the advent and common use of CT, the diagnosis of primary epiploic appendagitis was made by exploratory laparotomy, wherein the inflamed appendage was then ligated and excised.[21] Proper identification of this condition using radiologic studies, specifically abdominal and pelvic CT, may prevent unnecessary surgical exploration and its associated costs and complications. A study by Rao and colleagues[22] revealed that the average cost per misdiagnosed patient in this situation was $4117.\nOn CT, epiploic appendagitis is represented by a round or oval lesion, typically 2-4 cm in diameter, in close apposition to the colonic wall. More than one half of these cases are located in the sigmoid colon. Surrounded by periappendageal and pericolic fat stranding, the attenuation of the lesion itself is similar to that of fat, but there is often a thin rim of increased density. A central section of hyperattenuation representing an area of venous thrombosis may be intermittently present.[1,4] The proximal colonic wall is not normally thickened, which helps differentiate this condition from diverticulitis; however, the adjacent visceral peritoneum may occasionally be thickened.[1]\nIdentifying epiploic appendagitis with ultrasonography is generally difficult, but the appendage has been described as an oval, hyperechoic, noncompressible mass with a fine hypoechoic rim at the point of maximal tenderness, adjacent to the colon. On color Doppler ultrasonography, lack of central blood flow is observed; this is an important differentiating factor from appendicitis, which would demonstrate increased blood flow.[1,20,23,24]\nMRI is not typically performed in this patient population; however, epiploic appendagitis can certainly be identified on MRI. T1- and T2-weighted images demonstrate a focal lesion, with a signal intensity similar to that of fat. The addition of contrast to T1-weighted imaging demonstrates a fatty lesion with rim enhancement.[25]\nRadiologic changes can persist for weeks,[20] but they generally resolve within 6 months of the acute episode.[4]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Gastro Case Challenge: Excruciating Abdominal Pain in a Woman Taking Benzodiazepines and Narcotics"
},
{
"authors": "Noah Gudel, DO; Lisa M. Rock, MD",
"content": [
"Conservative management with anti-inflammatory medications and pain control are the mainstays of treatment for primary epiploic appendagitis.[1] The patient's symptoms usually regress within 1-2 weeks, although as noted, radiologic changes may persist.[1,12] Potential complications that have been reported include adhesions, local abscess formation, intussusception, intraperitoneal loose bodies, bowel obstruction, and peritonitis.[4,11]",
"Sand and colleagues[1] suggested that surgical intervention is preferable to expectant management, because four out of 10 patients in their study had multiple episodes before their initial presentation, and early surgery would (in theory) prevent complications, such as adhesions and abscess formation. They also noted that clinicians must consider the potential adverse effects associated with the multiple CT scans that are likely to be ordered for follow-up on these conservatively managed patients.[1]",
"In the case presented here, the patient opted for conservative treatment, with over-the-counter nonsteroidal anti-inflammatory medications and expectant management. The patient was counseled to follow up in 3 months for possible repeat CT and clinical evaluation. If clinical symptoms or radiologic findings persist, laparoscopy may be considered."
],
"date": "December 07, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: Excruciating Abdominal Pain in a Woman Taking Benzodiazepines and Narcotics\n\n **Authors:** Noah Gudel, DO; Lisa M. Rock, MD \n **Date:** December 07, 2022\n\n ## Content\n\n Conservative management with anti-inflammatory medications and pain control are the mainstays of treatment for primary epiploic appendagitis.[1] The patient's symptoms usually regress within 1-2 weeks, although as noted, radiologic changes may persist.[1,12] Potential complications that have been reported include adhesions, local abscess formation, intussusception, intraperitoneal loose bodies, bowel obstruction, and peritonitis.[4,11]\nSand and colleagues[1] suggested that surgical intervention is preferable to expectant management, because four out of 10 patients in their study had multiple episodes before their initial presentation, and early surgery would (in theory) prevent complications, such as adhesions and abscess formation. They also noted that clinicians must consider the potential adverse effects associated with the multiple CT scans that are likely to be ordered for follow-up on these conservatively managed patients.[1]\nIn the case presented here, the patient opted for conservative treatment, with over-the-counter nonsteroidal anti-inflammatory medications and expectant management. The patient was counseled to follow up in 3 months for possible repeat CT and clinical evaluation. If clinical symptoms or radiologic findings persist, laparoscopy may be considered.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1116018,
"choiceText": "An intraperitoneal infectious process",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116020,
"choiceText": "Twisting, stretching, or kinking of the appendages, with impairment of the blood supply",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116022,
"choiceText": "Detachment of the epiploic appendages",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116024,
"choiceText": "Fecaliths\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Possible etiologies of primary epiploic appendagitis include spontaneous torsion, thrombosis, ischemia, or inflammation of an epiploic appendage. An intraperitoneal inflammatory or infectious process that spreads to the appendages, causing appendagitis, is termed \"secondary epiploic appendagitis.\" Neither detachment of the appendages themselves nor fecaliths are involved in the pathophysiology of primary epiploic appendagitis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353693,
"questionText": "Which is involved in the pathogenesis of primary epiploic appendagitis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1116026,
"choiceText": "Elevated CRP level",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116028,
"choiceText": "Anorexia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116030,
"choiceText": "Abdominal pain",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116032,
"choiceText": "Fever\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The most consistent symptom associated with epiploic appendagitis is sharp, localized, nonmigratory abdominal pain. An elevated CRP level may occasionally be associated with primary epiploic appendagitis; however, such symptoms as fever and anorexia are usually absent.<br><br>\r\nCorrect identification of the entity avoids unnecessary surgery and the associated morbidity and cost. However, certain persistent or recurrent cases might benefit from laparoscopic removal of the chronically inflamed appendage. ",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353695,
"questionText": "Which is most consistently associated with primary epiploic appendagitis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: Excruciating Abdominal Pain in a Woman Taking Benzodiazepines and Narcotics"
},
{
"authors": "Noah Gudel, DO; Lisa M. Rock, MD",
"content": [],
"date": "December 07, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: Excruciating Abdominal Pain in a Woman Taking Benzodiazepines and Narcotics\n\n **Authors:** Noah Gudel, DO; Lisa M. Rock, MD \n **Date:** December 07, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1116018,
"choiceText": "An intraperitoneal infectious process",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116020,
"choiceText": "Twisting, stretching, or kinking of the appendages, with impairment of the blood supply",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116022,
"choiceText": "Detachment of the epiploic appendages",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116024,
"choiceText": "Fecaliths\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Possible etiologies of primary epiploic appendagitis include spontaneous torsion, thrombosis, ischemia, or inflammation of an epiploic appendage. An intraperitoneal inflammatory or infectious process that spreads to the appendages, causing appendagitis, is termed \"secondary epiploic appendagitis.\" Neither detachment of the appendages themselves nor fecaliths are involved in the pathophysiology of primary epiploic appendagitis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353693,
"questionText": "Which is involved in the pathogenesis of primary epiploic appendagitis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1116026,
"choiceText": "Elevated CRP level",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116028,
"choiceText": "Anorexia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116030,
"choiceText": "Abdominal pain",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116032,
"choiceText": "Fever\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The most consistent symptom associated with epiploic appendagitis is sharp, localized, nonmigratory abdominal pain. An elevated CRP level may occasionally be associated with primary epiploic appendagitis; however, such symptoms as fever and anorexia are usually absent.<br><br>\r\nCorrect identification of the entity avoids unnecessary surgery and the associated morbidity and cost. However, certain persistent or recurrent cases might benefit from laparoscopic removal of the chronically inflamed appendage. ",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353695,
"questionText": "Which is most consistently associated with primary epiploic appendagitis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: Excruciating Abdominal Pain in a Woman Taking Benzodiazepines and Narcotics"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1116010,
"choiceText": "Primary epiploic appendagitis",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116012,
"choiceText": "Acute omental infarction",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116014,
"choiceText": "Mesenteric panniculitis\r\n",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116016,
"choiceText": "Appendicitis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353691,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1116018,
"choiceText": "An intraperitoneal infectious process",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116020,
"choiceText": "Twisting, stretching, or kinking of the appendages, with impairment of the blood supply",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116022,
"choiceText": "Detachment of the epiploic appendages",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116024,
"choiceText": "Fecaliths\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Possible etiologies of primary epiploic appendagitis include spontaneous torsion, thrombosis, ischemia, or inflammation of an epiploic appendage. An intraperitoneal inflammatory or infectious process that spreads to the appendages, causing appendagitis, is termed \"secondary epiploic appendagitis.\" Neither detachment of the appendages themselves nor fecaliths are involved in the pathophysiology of primary epiploic appendagitis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353693,
"questionText": "Which is involved in the pathogenesis of primary epiploic appendagitis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1116026,
"choiceText": "Elevated CRP level",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116028,
"choiceText": "Anorexia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116030,
"choiceText": "Abdominal pain",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1116032,
"choiceText": "Fever\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The most consistent symptom associated with epiploic appendagitis is sharp, localized, nonmigratory abdominal pain. An elevated CRP level may occasionally be associated with primary epiploic appendagitis; however, such symptoms as fever and anorexia are usually absent.<br><br>\r\nCorrect identification of the entity avoids unnecessary surgery and the associated morbidity and cost. However, certain persistent or recurrent cases might benefit from laparoscopic removal of the chronically inflamed appendage. ",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353695,
"questionText": "Which is most consistently associated with primary epiploic appendagitis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
888178 | /viewarticle/888178 | [
{
"authors": "Janice Verham, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 19-year-old has developed a loculated pleural effusion after a percutaneous pigtail catheter was inserted into the right side of his chest 5 weeks after polytrauma from multiple gunshot wounds. Minimal output from the chest tube prompted interventional radiology to begin daily tissue plasminogen activator (tPA) administration through the pigtail catheter 2 days ago.",
"The patient describes diffuse right-sided chest pain and shortness of breath secondary to pain after the second administration of tPA. He has no leg pain, fevers, chills, or cough."
],
"date": "December 06, 2022",
"figures": [],
"markdown": "# A Teenager Shot Multiple Times Develops Further Complications\n\n **Authors:** Janice Verham, MD \n **Date:** December 06, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 19-year-old has developed a loculated pleural effusion after a percutaneous pigtail catheter was inserted into the right side of his chest 5 weeks after polytrauma from multiple gunshot wounds. Minimal output from the chest tube prompted interventional radiology to begin daily tissue plasminogen activator (tPA) administration through the pigtail catheter 2 days ago.\nThe patient describes diffuse right-sided chest pain and shortness of breath secondary to pain after the second administration of tPA. He has no leg pain, fevers, chills, or cough.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A Teenager Shot Multiple Times Develops Further Complications"
},
{
"authors": "Janice Verham, MD",
"content": [
"Upon evaluation, the patient's vital signs include a temperature of 96.4°F (35.8°C), pulse of 150 beats/min, blood pressure of 115/74 mm Hg, respiratory rate of 34 breaths/min, and saturation of 96% on room air. He is a thin young man sitting up comfortably in bed. He is alert and oriented. His respiratory examination is notable for mildly decreased breath sounds on the right, and his cardiac examination is significant for tachycardia.",
"The patient's pigtail catheter is in place; the dressings are clean, dry, and intact; and approximately 75 mL of serosanguinous output from the chest tube is noted over 12 hours. The patient's bilateral lower extremities demonstrate no edema and are soft. He has a negative Homan sign bilaterally.",
"EKG reveals sinus tachycardia with no Q waves or T-wave abnormalities. Ultrasonography of the patient's bilateral lower extremities reveals no evidence of venous occlusion.",
"Laboratory analysis reveals negative troponin findings (< 0.04 ng/mL), worsening anemia (decrease in hemoglobin level from 8 g/dL to 6 g/dL over 12 hours), and stable elevated leukocytosis (white blood cell count of 19 × 109 cells/L).",
"A chest radiograph reveals an acute increase in density in the right chest at the pigtail catheter site compared with prior imaging (Figure 1).",
"Figure 1.",
"The CT scan one day after chest pain is reported indicates an expanding, loculated right pleural effusion with high-density material and layering. The pigtail catheter is in the anterior superior portion of the fluid collection (Figures 2 and 3).",
"Figure 2.",
"Figure 3."
],
"date": "December 06, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/888/178/888178-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/888/178/888178-Thumb2.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/888/178/888178-Thumb3.png"
}
],
"markdown": "# A Teenager Shot Multiple Times Develops Further Complications\n\n **Authors:** Janice Verham, MD \n **Date:** December 06, 2022\n\n ## Content\n\n Upon evaluation, the patient's vital signs include a temperature of 96.4°F (35.8°C), pulse of 150 beats/min, blood pressure of 115/74 mm Hg, respiratory rate of 34 breaths/min, and saturation of 96% on room air. He is a thin young man sitting up comfortably in bed. He is alert and oriented. His respiratory examination is notable for mildly decreased breath sounds on the right, and his cardiac examination is significant for tachycardia.\nThe patient's pigtail catheter is in place; the dressings are clean, dry, and intact; and approximately 75 mL of serosanguinous output from the chest tube is noted over 12 hours. The patient's bilateral lower extremities demonstrate no edema and are soft. He has a negative Homan sign bilaterally.\nEKG reveals sinus tachycardia with no Q waves or T-wave abnormalities. Ultrasonography of the patient's bilateral lower extremities reveals no evidence of venous occlusion.\nLaboratory analysis reveals negative troponin findings (< 0.04 ng/mL), worsening anemia (decrease in hemoglobin level from 8 g/dL to 6 g/dL over 12 hours), and stable elevated leukocytosis (white blood cell count of 19 × 109 cells/L).\nA chest radiograph reveals an acute increase in density in the right chest at the pigtail catheter site compared with prior imaging (Figure 1).\nFigure 1.\nThe CT scan one day after chest pain is reported indicates an expanding, loculated right pleural effusion with high-density material and layering. The pigtail catheter is in the anterior superior portion of the fluid collection (Figures 2 and 3).\nFigure 2.\nFigure 3.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1154934,
"choiceText": "Dissecting aortic aneurysm",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154936,
"choiceText": "Pulmonary embolism",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154938,
"choiceText": "Hemothorax",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154940,
"choiceText": "Empyema",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154942,
"choiceText": "Pneumothorax",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154944,
"choiceText": "Disseminated intravascular coagulation",
"correct": false,
"displayOrder": 6,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154946,
"choiceText": "Exudative pleural effusion",
"correct": false,
"displayOrder": 7,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 366897,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Teenager Shot Multiple Times Develops Further Complications"
},
{
"authors": "Janice Verham, MD",
"content": [
"The differential diagnosis in this patient was initially broad, after a primary symptom of pleuritic chest pain associated with shortness of breath, tachypnea, and tachycardia. However, the patient's acutely worsening anemia and chest radiography provided a clear diagnosis of hemothorax.",
"Hemothorax is an accumulation of blood in the pleural space, which may occur spontaneously or secondary to blunt or penetrating trauma. Injured lung parenchyma from fractured ribs is the main cause of bleeding from blunt trauma; however, in rare cases, injury to the intercostal arteries, cardiac injury, and pulmonary hilar are sources of bleeding that should be considered.",
"The source of bleeding is important because it guides the physician as to how to manage the bleeding. For example, lung parenchyma often stop bleeding without additional intervention, whereas bleeding from the pressurized arterial system (eg, lacerated intercostal arteries) often requires intervention.[1]",
"Spontaneous hemothorax may also occur, although it is significantly less common. Causes of spontaneous hemothorax include rupture of pleural adhesions, neoplasms, metastasis, and systemic anticoagulant therapy.[2] Because spontaneous causes are less likely, a thorough work-up for chest pain and/or shortness of breath is always indicated.",
"Physical examination findings for hemothorax may include absent or decreased breath sounds. With the assistance of imaging, a tracheal deviation, blunting of the costophrenic angle, or complete opacification of the pleural cavity may be visualized. However, a hemothorax is usually not visible on a chest x-ray until a minimum of 200 mL of fluid is present in the pleural cavity. With a smaller fluid collection, lateral chest radiography is indicated because that view allows visualization of smaller collections.[3] CT is frequently used owing to its higher sensitivity compared with chest radiography in diagnosing hemothorax.[4]",
"Ultrasonography is increasingly used as part of the evaluation for hemothorax; a Focused Assessment with Sonography in Trauma (FAST) scan is widely considered the criterion standard for an initial trauma evaluation and is as sensitive and specific as chest radiography.[5,6] Given that ultrasonography may already be part of the trauma team evaluation, its use can save time in the workup and diagnosis of hemothorax."
],
"date": "December 06, 2022",
"figures": [],
"markdown": "# A Teenager Shot Multiple Times Develops Further Complications\n\n **Authors:** Janice Verham, MD \n **Date:** December 06, 2022\n\n ## Content\n\n The differential diagnosis in this patient was initially broad, after a primary symptom of pleuritic chest pain associated with shortness of breath, tachypnea, and tachycardia. However, the patient's acutely worsening anemia and chest radiography provided a clear diagnosis of hemothorax.\nHemothorax is an accumulation of blood in the pleural space, which may occur spontaneously or secondary to blunt or penetrating trauma. Injured lung parenchyma from fractured ribs is the main cause of bleeding from blunt trauma; however, in rare cases, injury to the intercostal arteries, cardiac injury, and pulmonary hilar are sources of bleeding that should be considered.\nThe source of bleeding is important because it guides the physician as to how to manage the bleeding. For example, lung parenchyma often stop bleeding without additional intervention, whereas bleeding from the pressurized arterial system (eg, lacerated intercostal arteries) often requires intervention.[1]\nSpontaneous hemothorax may also occur, although it is significantly less common. Causes of spontaneous hemothorax include rupture of pleural adhesions, neoplasms, metastasis, and systemic anticoagulant therapy.[2] Because spontaneous causes are less likely, a thorough work-up for chest pain and/or shortness of breath is always indicated.\nPhysical examination findings for hemothorax may include absent or decreased breath sounds. With the assistance of imaging, a tracheal deviation, blunting of the costophrenic angle, or complete opacification of the pleural cavity may be visualized. However, a hemothorax is usually not visible on a chest x-ray until a minimum of 200 mL of fluid is present in the pleural cavity. With a smaller fluid collection, lateral chest radiography is indicated because that view allows visualization of smaller collections.[3] CT is frequently used owing to its higher sensitivity compared with chest radiography in diagnosing hemothorax.[4]\nUltrasonography is increasingly used as part of the evaluation for hemothorax; a Focused Assessment with Sonography in Trauma (FAST) scan is widely considered the criterion standard for an initial trauma evaluation and is as sensitive and specific as chest radiography.[5,6] Given that ultrasonography may already be part of the trauma team evaluation, its use can save time in the workup and diagnosis of hemothorax.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1154934,
"choiceText": "Dissecting aortic aneurysm",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154936,
"choiceText": "Pulmonary embolism",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154938,
"choiceText": "Hemothorax",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154940,
"choiceText": "Empyema",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154942,
"choiceText": "Pneumothorax",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154944,
"choiceText": "Disseminated intravascular coagulation",
"correct": false,
"displayOrder": 6,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154946,
"choiceText": "Exudative pleural effusion",
"correct": false,
"displayOrder": 7,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 366897,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Teenager Shot Multiple Times Develops Further Complications"
},
{
"authors": "Janice Verham, MD",
"content": [
"In this specific case, the cause of hemothorax was unique because it was attributed to intrathoracic tPA administration for a loculated pleural effusion. Intrathoracic hemorrhage is a rare but acknowledged complication of tPA administration.[7] The patient had a prior hemothorax secondary to multiple rib fractures, which may have increased his risk for bleeding.",
"A case report found that a patient with previous rib fractures developed a hemothorax after fibrinolytic therapy for empyema that required two thoracotomies.[8] This suggests that clinicians should have an increased awareness when using fibrinolytic therapy in the setting of recent trauma. In addition, patients receiving therapeutic anticoagulation, or who are coagulopathic from other causes (including liver disease) at the time of intrapleural fibrinolytic therapy, may be at increased risk for pleural hemorrhages.[7]",
"After diagnosis of a hemothorax, the next logical step is determining the proper management. Tube thoracostomy (chest tube) is the placement of a tube to drain air or fluid from the pleural cavity. Placement of a chest tube may be performed via the Seldinger technique or a classic surgical technique, which is used more often in a trauma setting. The size of chest tube is measured in the unit French (Fr), which is equivalent to 0.33 mm and refers to the diameter of the outside of a cylindrical tube.[9]",
"The optimal chest tube size has been thoroughly studied, with recent data suggesting that use of large-bore (> 14 Fr) chest tubes is not correlated with improved outcomes.[10] The use of smaller-caliber catheters is associated with decreased pain and lower risk for damage to surrounding structures.[11] Although many physicians still advocate for the insertion of a large-bore (32-40 Fr) chest tube for acute hemothorax, a study by the trauma group at University of Arizona suggests that use of 14-Fr pigtail catheters had higher drainage output and decreased the number of days with a chest tube in place, without an increased rate of failed attempts or complications related to tube insertion.[12]",
"Although it is debated, most physicians drain the pleural cavity via placement of a chest tube if the hemothorax is > 500 mL.[1] Massive hemothorax, which is defined as > 1500 mL or > 200 mL/hr for 2-4 hours in the pleural space, typically occurs in trauma patients.[13] The source of the bleeding in massive hemothorax is either a pulmonary vascular or an arterial source. Because neither cause is likely to stop without additional intervention, operative exploration is the criterion standard.[1]",
"Complications of chest tube thoracostomy include infection, empyema, and lung injury; the incidence rate of other, more rare complications is reportedly as high as 20%.[14] Algorithms are useful in guiding treatment once a chest tube is placed.[15]",
"Infectious complications, including empyema and pneumonia, are the most common complications after chest tube drainage of hemothorax. Although some providers use prophylactic antibiotics, this practice is highly controversial because large-scale reviews suggest insufficient evidence to support this routine practice.[16] Other systematic reviews suggest a decreased risk for empyema and infectious complications with antibiotic prophylaxis in patients with penetrating chest injuries, but not in those with blunt chest trauma.[16]"
],
"date": "December 06, 2022",
"figures": [],
"markdown": "# A Teenager Shot Multiple Times Develops Further Complications\n\n **Authors:** Janice Verham, MD \n **Date:** December 06, 2022\n\n ## Content\n\n In this specific case, the cause of hemothorax was unique because it was attributed to intrathoracic tPA administration for a loculated pleural effusion. Intrathoracic hemorrhage is a rare but acknowledged complication of tPA administration.[7] The patient had a prior hemothorax secondary to multiple rib fractures, which may have increased his risk for bleeding.\nA case report found that a patient with previous rib fractures developed a hemothorax after fibrinolytic therapy for empyema that required two thoracotomies.[8] This suggests that clinicians should have an increased awareness when using fibrinolytic therapy in the setting of recent trauma. In addition, patients receiving therapeutic anticoagulation, or who are coagulopathic from other causes (including liver disease) at the time of intrapleural fibrinolytic therapy, may be at increased risk for pleural hemorrhages.[7]\nAfter diagnosis of a hemothorax, the next logical step is determining the proper management. Tube thoracostomy (chest tube) is the placement of a tube to drain air or fluid from the pleural cavity. Placement of a chest tube may be performed via the Seldinger technique or a classic surgical technique, which is used more often in a trauma setting. The size of chest tube is measured in the unit French (Fr), which is equivalent to 0.33 mm and refers to the diameter of the outside of a cylindrical tube.[9]\nThe optimal chest tube size has been thoroughly studied, with recent data suggesting that use of large-bore (> 14 Fr) chest tubes is not correlated with improved outcomes.[10] The use of smaller-caliber catheters is associated with decreased pain and lower risk for damage to surrounding structures.[11] Although many physicians still advocate for the insertion of a large-bore (32-40 Fr) chest tube for acute hemothorax, a study by the trauma group at University of Arizona suggests that use of 14-Fr pigtail catheters had higher drainage output and decreased the number of days with a chest tube in place, without an increased rate of failed attempts or complications related to tube insertion.[12]\nAlthough it is debated, most physicians drain the pleural cavity via placement of a chest tube if the hemothorax is > 500 mL.[1] Massive hemothorax, which is defined as > 1500 mL or > 200 mL/hr for 2-4 hours in the pleural space, typically occurs in trauma patients.[13] The source of the bleeding in massive hemothorax is either a pulmonary vascular or an arterial source. Because neither cause is likely to stop without additional intervention, operative exploration is the criterion standard.[1]\nComplications of chest tube thoracostomy include infection, empyema, and lung injury; the incidence rate of other, more rare complications is reportedly as high as 20%.[14] Algorithms are useful in guiding treatment once a chest tube is placed.[15]\nInfectious complications, including empyema and pneumonia, are the most common complications after chest tube drainage of hemothorax. Although some providers use prophylactic antibiotics, this practice is highly controversial because large-scale reviews suggest insufficient evidence to support this routine practice.[16] Other systematic reviews suggest a decreased risk for empyema and infectious complications with antibiotic prophylaxis in patients with penetrating chest injuries, but not in those with blunt chest trauma.[16]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A Teenager Shot Multiple Times Develops Further Complications"
},
{
"authors": "Janice Verham, MD",
"content": [
"Retained hemothorax (a residual hemothorax despite tube thoracostomy placement) has been reported in as many as 17% of patients.[17] A retained hemothorax increases the risk for empyema, as well as prolonging hospital stay and increasing hospital charges.[18,19]",
"The management of retained hemothorax includes observation, second chest tube placement, intrapleural fibrinolytic therapy, and video-assisted thoracoscopic surgery (VATS). Observation is more likely to be successful if the retained hemothorax is < 300 mL.[20] Placement of a second chest tube may be beneficial in the presence of a poorly placed initial tube thoracostomy; however, surgical intervention with VATS within 5-7 days after the initial injury decreases conversion to open surgery, empyema formation, and length of hospital stay.[21]",
"Although fibrinolytic therapy is another option, its disadvantages include prolonged hospital stay for the administration of fibrinolysis (3-7 days of infusion). VATS has been shown to decrease the risk for empyema, reduce hospital stay, and decrease the need for open surgery compared with fibrinolytic therapy.[22] A longer duration between development of hemothorax and VATS increases the need for conversion to thoracotomy and prolongs hospitalization, which may be indicated regardless, especially for difficult empyema evacuation or decortication.[23] In the setting of massive hemothorax or ongoing bleeding, open thoracotomy is the procedure of choice.[24] During surgery, bleeding can be controlled at the source, and the hemothorax can be evacuated.",
"The most feared complications associated with chest tube placement are reexpansion pulmonary edema and vagus nerve irritation. Reexpansion pulmonary edema can have a mortality rate as high as 20%.[24] Although the exact cause is unclear, reexpansion pulmonary edema is thought to be due to sudden and excessive endothelial permeability in the ipsilateral lung.[25] Another severe complication, vagus nerve irritation, has been known to cause sudden death via excess parasympathetic stimulation and bradycardia that causes a fatal arrhythmia.[26,27]",
"Although these complications may cause a physician to hesitate in placing a chest tube, waiting to place one is also associated with risks. By delaying placement of a thoracostomy tube or incompletely evacuating a hemothorax, a fibrothorax may develop, which effectively \"traps\" the lung and prevents full expansion."
],
"date": "December 06, 2022",
"figures": [],
"markdown": "# A Teenager Shot Multiple Times Develops Further Complications\n\n **Authors:** Janice Verham, MD \n **Date:** December 06, 2022\n\n ## Content\n\n Retained hemothorax (a residual hemothorax despite tube thoracostomy placement) has been reported in as many as 17% of patients.[17] A retained hemothorax increases the risk for empyema, as well as prolonging hospital stay and increasing hospital charges.[18,19]\nThe management of retained hemothorax includes observation, second chest tube placement, intrapleural fibrinolytic therapy, and video-assisted thoracoscopic surgery (VATS). Observation is more likely to be successful if the retained hemothorax is < 300 mL.[20] Placement of a second chest tube may be beneficial in the presence of a poorly placed initial tube thoracostomy; however, surgical intervention with VATS within 5-7 days after the initial injury decreases conversion to open surgery, empyema formation, and length of hospital stay.[21]\nAlthough fibrinolytic therapy is another option, its disadvantages include prolonged hospital stay for the administration of fibrinolysis (3-7 days of infusion). VATS has been shown to decrease the risk for empyema, reduce hospital stay, and decrease the need for open surgery compared with fibrinolytic therapy.[22] A longer duration between development of hemothorax and VATS increases the need for conversion to thoracotomy and prolongs hospitalization, which may be indicated regardless, especially for difficult empyema evacuation or decortication.[23] In the setting of massive hemothorax or ongoing bleeding, open thoracotomy is the procedure of choice.[24] During surgery, bleeding can be controlled at the source, and the hemothorax can be evacuated.\nThe most feared complications associated with chest tube placement are reexpansion pulmonary edema and vagus nerve irritation. Reexpansion pulmonary edema can have a mortality rate as high as 20%.[24] Although the exact cause is unclear, reexpansion pulmonary edema is thought to be due to sudden and excessive endothelial permeability in the ipsilateral lung.[25] Another severe complication, vagus nerve irritation, has been known to cause sudden death via excess parasympathetic stimulation and bradycardia that causes a fatal arrhythmia.[26,27]\nAlthough these complications may cause a physician to hesitate in placing a chest tube, waiting to place one is also associated with risks. By delaying placement of a thoracostomy tube or incompletely evacuating a hemothorax, a fibrothorax may develop, which effectively \"traps\" the lung and prevents full expansion.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1154948,
"choiceText": "Transfer to the intensive care unit",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154950,
"choiceText": "Transfusion with packed red blood cells",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154952,
"choiceText": "Transfusion with platelets",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154954,
"choiceText": "Place pigtail catheter to water seal",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The patient in this case is probably symptomatic owing to acute anemia secondary to blood loss. Volume resuscitation is the most important next step for him. Although transfer to an intensive care unit should be considered, this will not immediately help the patient. Transfusing platelets would increase his volume but would not address the deficits. The patient's chest tube is probably clogged, given the low output and volume of blood seen on a chest x-ray. Placing the chest tube to water-seal would probably have no impact on his symptoms.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 366899,
"questionText": "Which of the following is the next step in management for a patient with hemothorax, such as the one described in the case above?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1154956,
"choiceText": "Addition of a second chest tube",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154958,
"choiceText": "VATS",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154960,
"choiceText": "Thoracotomy",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154962,
"choiceText": "Injection of fibrin-thrombin sealant through pigtail catheter",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Because this patient now has a loculated parapneumonic effusion coupled with hemothorax, VATS is indicated. The addition of a second chest tube may be helpful in removing the hemothorax, but it would not address the patient's loculated parapneumonic effusion. Thoracotomy may be necessary if the surgeon is unable to address the source of bleeding and perform adequate evacuation of the loculated effusion. Although fibrin-thrombin sealant has been documented as a way of managing pleural hemorrhage, it was applied directly to the pleural cavity during thoracotomy and not through a pigtail catheter. <br><br>\r\n\r\nThe patient in this case received a total of 3 units of packed red blood cells the night and day after his episode of tachycardia. Two days after his pain started, he underwent VATS, during which a large amount of old clot was found, evacuated, and sent for culture. No active bleeding was found, the pleural cavity was irrigated and the lung was reinflated under direct vision. The patient tolerated the procedure well, and cultures remained negative.<br><br>\r\n\r\n\r\nFive days after the procedure, the patient developed right upper-lobe collapse, presumably due to a mucus plug. Chest physical therapy was started. With an aggressive pulmonary toilet, the patient improved and was discharged home 2 weeks after VATS.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 366901,
"questionText": "Which of the following is the definitive treatment for the patient described in the case above?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Teenager Shot Multiple Times Develops Further Complications"
},
{
"authors": "Janice Verham, MD",
"content": [],
"date": "December 06, 2022",
"figures": [],
"markdown": "# A Teenager Shot Multiple Times Develops Further Complications\n\n **Authors:** Janice Verham, MD \n **Date:** December 06, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1154948,
"choiceText": "Transfer to the intensive care unit",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154950,
"choiceText": "Transfusion with packed red blood cells",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154952,
"choiceText": "Transfusion with platelets",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154954,
"choiceText": "Place pigtail catheter to water seal",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The patient in this case is probably symptomatic owing to acute anemia secondary to blood loss. Volume resuscitation is the most important next step for him. Although transfer to an intensive care unit should be considered, this will not immediately help the patient. Transfusing platelets would increase his volume but would not address the deficits. The patient's chest tube is probably clogged, given the low output and volume of blood seen on a chest x-ray. Placing the chest tube to water-seal would probably have no impact on his symptoms.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 366899,
"questionText": "Which of the following is the next step in management for a patient with hemothorax, such as the one described in the case above?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1154956,
"choiceText": "Addition of a second chest tube",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154958,
"choiceText": "VATS",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154960,
"choiceText": "Thoracotomy",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154962,
"choiceText": "Injection of fibrin-thrombin sealant through pigtail catheter",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Because this patient now has a loculated parapneumonic effusion coupled with hemothorax, VATS is indicated. The addition of a second chest tube may be helpful in removing the hemothorax, but it would not address the patient's loculated parapneumonic effusion. Thoracotomy may be necessary if the surgeon is unable to address the source of bleeding and perform adequate evacuation of the loculated effusion. Although fibrin-thrombin sealant has been documented as a way of managing pleural hemorrhage, it was applied directly to the pleural cavity during thoracotomy and not through a pigtail catheter. <br><br>\r\n\r\nThe patient in this case received a total of 3 units of packed red blood cells the night and day after his episode of tachycardia. Two days after his pain started, he underwent VATS, during which a large amount of old clot was found, evacuated, and sent for culture. No active bleeding was found, the pleural cavity was irrigated and the lung was reinflated under direct vision. The patient tolerated the procedure well, and cultures remained negative.<br><br>\r\n\r\n\r\nFive days after the procedure, the patient developed right upper-lobe collapse, presumably due to a mucus plug. Chest physical therapy was started. With an aggressive pulmonary toilet, the patient improved and was discharged home 2 weeks after VATS.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 366901,
"questionText": "Which of the following is the definitive treatment for the patient described in the case above?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Teenager Shot Multiple Times Develops Further Complications"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1154934,
"choiceText": "Dissecting aortic aneurysm",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154936,
"choiceText": "Pulmonary embolism",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154938,
"choiceText": "Hemothorax",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154940,
"choiceText": "Empyema",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154942,
"choiceText": "Pneumothorax",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154944,
"choiceText": "Disseminated intravascular coagulation",
"correct": false,
"displayOrder": 6,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154946,
"choiceText": "Exudative pleural effusion",
"correct": false,
"displayOrder": 7,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 366897,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1154948,
"choiceText": "Transfer to the intensive care unit",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154950,
"choiceText": "Transfusion with packed red blood cells",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154952,
"choiceText": "Transfusion with platelets",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154954,
"choiceText": "Place pigtail catheter to water seal",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The patient in this case is probably symptomatic owing to acute anemia secondary to blood loss. Volume resuscitation is the most important next step for him. Although transfer to an intensive care unit should be considered, this will not immediately help the patient. Transfusing platelets would increase his volume but would not address the deficits. The patient's chest tube is probably clogged, given the low output and volume of blood seen on a chest x-ray. Placing the chest tube to water-seal would probably have no impact on his symptoms.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 366899,
"questionText": "Which of the following is the next step in management for a patient with hemothorax, such as the one described in the case above?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1154956,
"choiceText": "Addition of a second chest tube",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154958,
"choiceText": "VATS",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154960,
"choiceText": "Thoracotomy",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1154962,
"choiceText": "Injection of fibrin-thrombin sealant through pigtail catheter",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Because this patient now has a loculated parapneumonic effusion coupled with hemothorax, VATS is indicated. The addition of a second chest tube may be helpful in removing the hemothorax, but it would not address the patient's loculated parapneumonic effusion. Thoracotomy may be necessary if the surgeon is unable to address the source of bleeding and perform adequate evacuation of the loculated effusion. Although fibrin-thrombin sealant has been documented as a way of managing pleural hemorrhage, it was applied directly to the pleural cavity during thoracotomy and not through a pigtail catheter. <br><br>\r\n\r\nThe patient in this case received a total of 3 units of packed red blood cells the night and day after his episode of tachycardia. Two days after his pain started, he underwent VATS, during which a large amount of old clot was found, evacuated, and sent for culture. No active bleeding was found, the pleural cavity was irrigated and the lung was reinflated under direct vision. The patient tolerated the procedure well, and cultures remained negative.<br><br>\r\n\r\n\r\nFive days after the procedure, the patient developed right upper-lobe collapse, presumably due to a mucus plug. Chest physical therapy was started. With an aggressive pulmonary toilet, the patient improved and was discharged home 2 weeks after VATS.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 366901,
"questionText": "Which of the following is the definitive treatment for the patient described in the case above?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
913911 | /viewarticle/913911 | [
{
"authors": "Sumaira Nabi, MBBS; Shahzad Ahmed, MBBS; Mazhar Badshah, MBBS",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 20-year-old woman presents with a 2-week history of bilateral flank pain and episodic vomiting. In addition, she has malar angiofibromas on her face, a leathery patch of skin on her lower back, and periungual fibromas on her fingers and toes (Figures 1-4).",
"Figure 1.",
"Figure 2.",
"Figure 3.",
"Figure 4.",
"She has no history of fever, dysuria, polyuria, hematuria, or urinary urgency. She was diagnosed with epilepsy in early childhood and has taken multiple antiepileptic drugs, with variable control. She is currently taking oral levetiracetam (500 mg three times per day) and oral carbamazepine (400 mg three times per day). She is single and unemployed. She is a nonsmoker and denies substance abuse. Her family history is noncontributory."
],
"date": "November 29, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/913/911/913911-fig1-thumb.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/913/911/913911-fig2-thumb.jpg"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/913/911/913911-fig3-thumb.jpg"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/913/911/913911-fig4-thumb.jpg"
}
],
"markdown": "# Fingernail, Toenail Changes and Flank Pain in a 20-Year-Old\n\n **Authors:** Sumaira Nabi, MBBS; Shahzad Ahmed, MBBS; Mazhar Badshah, MBBS \n **Date:** November 29, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 20-year-old woman presents with a 2-week history of bilateral flank pain and episodic vomiting. In addition, she has malar angiofibromas on her face, a leathery patch of skin on her lower back, and periungual fibromas on her fingers and toes (Figures 1-4).\nFigure 1.\nFigure 2.\nFigure 3.\nFigure 4.\nShe has no history of fever, dysuria, polyuria, hematuria, or urinary urgency. She was diagnosed with epilepsy in early childhood and has taken multiple antiepileptic drugs, with variable control. She is currently taking oral levetiracetam (500 mg three times per day) and oral carbamazepine (400 mg three times per day). She is single and unemployed. She is a nonsmoker and denies substance abuse. Her family history is noncontributory.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4.** \n \n\n\n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Fingernail, Toenail Changes and Flank Pain in a 20-Year-Old"
},
{
"authors": "Sumaira Nabi, MBBS; Shahzad Ahmed, MBBS; Mazhar Badshah, MBBS",
"content": [
"Upon clinical examination, the patient is an alert young woman oriented to time, place, and person. Her vital signs include an oral temperature of 98.6°F (37°C), a regular pulse of 76 beats/min, and a blood pressure of 110/70 mm Hg. Her respiratory rate is 16 breaths/minute. Her Glasgow Coma Score is 15/15, and her higher mental functions are intact.",
"Upon neurologic examination, her cranial nerves are intact and symmetrical. She has no signs of meningeal irritation, pyramidal weakness, or incoordination. Her abdomen is soft, with flank fullness. She has bimanually palpable, nontender, cystic to firm masses extending from the hypochondrium to the lumber region on both sides. Her bowel sounds are audible. Precordial examination reveals normal heart sounds. Auscultation of the lung fields shows normal vesicular breathing.",
"Laboratory analysis includes a complete blood cell count that reveals anemia, with a hemoglobin level of 10 mg/dL. The remainder of the patient's cell counts and erythrocyte sedimentation rate are within the reference range. Her liver function test results, renal function test results, serum glucose levels, ECG findings, echocardiography findings, and chest radiography findings are unremarkable. Urine examination reveals albuminuria and microscopic hematuria.",
"Contrast-enhanced CT of the abdomen reveals kidneys replaced by heterogeneously enhancing large, well-defined lobulated mass lesions, with variable proportions of soft tissue and fat density areas as well as angioid tissues consistent with bilateral renal angiomyolipomas (Figures 5 and 6). The right side lesion measures 11 cm x 10 cm; the left side lesion measures 7 cm x 5 cm. The remainder of the viscera are normal.",
"Figure 5.",
"Figure 6.",
"Intravenous urography reveals an almost nonfunctioning right kidney and a left kidney with near-normal function. Non–contrast-enhanced CT of the brain reveals subependymal calcified nodules in the distribution of bilateral lateral ventricles (Figure 7).",
"Figure 7."
],
"date": "November 29, 2022",
"figures": [
{
"caption": "Figure 5.",
"image_url": "https://img.medscapestatic.com/article/913/911/913911-fig5-thumb.jpg"
},
{
"caption": "Figure 6.",
"image_url": "https://img.medscapestatic.com/article/913/911/913911-fig6-thumb.jpg"
},
{
"caption": "Figure 7.",
"image_url": "https://img.medscapestatic.com/article/913/911/913911-fig7-thumb.jpg"
}
],
"markdown": "# Fingernail, Toenail Changes and Flank Pain in a 20-Year-Old\n\n **Authors:** Sumaira Nabi, MBBS; Shahzad Ahmed, MBBS; Mazhar Badshah, MBBS \n **Date:** November 29, 2022\n\n ## Content\n\n Upon clinical examination, the patient is an alert young woman oriented to time, place, and person. Her vital signs include an oral temperature of 98.6°F (37°C), a regular pulse of 76 beats/min, and a blood pressure of 110/70 mm Hg. Her respiratory rate is 16 breaths/minute. Her Glasgow Coma Score is 15/15, and her higher mental functions are intact.\nUpon neurologic examination, her cranial nerves are intact and symmetrical. She has no signs of meningeal irritation, pyramidal weakness, or incoordination. Her abdomen is soft, with flank fullness. She has bimanually palpable, nontender, cystic to firm masses extending from the hypochondrium to the lumber region on both sides. Her bowel sounds are audible. Precordial examination reveals normal heart sounds. Auscultation of the lung fields shows normal vesicular breathing.\nLaboratory analysis includes a complete blood cell count that reveals anemia, with a hemoglobin level of 10 mg/dL. The remainder of the patient's cell counts and erythrocyte sedimentation rate are within the reference range. Her liver function test results, renal function test results, serum glucose levels, ECG findings, echocardiography findings, and chest radiography findings are unremarkable. Urine examination reveals albuminuria and microscopic hematuria.\nContrast-enhanced CT of the abdomen reveals kidneys replaced by heterogeneously enhancing large, well-defined lobulated mass lesions, with variable proportions of soft tissue and fat density areas as well as angioid tissues consistent with bilateral renal angiomyolipomas (Figures 5 and 6). The right side lesion measures 11 cm x 10 cm; the left side lesion measures 7 cm x 5 cm. The remainder of the viscera are normal.\nFigure 5.\nFigure 6.\nIntravenous urography reveals an almost nonfunctioning right kidney and a left kidney with near-normal function. Non–contrast-enhanced CT of the brain reveals subependymal calcified nodules in the distribution of bilateral lateral ventricles (Figure 7).\nFigure 7.\n\n ## Figures\n\n **Figure 5.** \n \n\n**Figure 6.** \n \n\n**Figure 7.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1365792,
"choiceText": "Tuberous sclerosis",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365794,
"choiceText": "Neurofibromatosis type 1",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365796,
"choiceText": "Neurofibromatosis type 2",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365798,
"choiceText": "Sturge-Weber syndrome",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 435879,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Fingernail, Toenail Changes and Flank Pain in a 20-Year-Old"
},
{
"authors": "Sumaira Nabi, MBBS; Shahzad Ahmed, MBBS; Mazhar Badshah, MBBS",
"content": [
"This patient was diagnosed with tuberous sclerosis (TS) with renal angiomyolipomas. Also referred to as \"tuberous sclerosis complex,\" TS is an inherited (autosomal dominant) neurocutaneous disorder. It was first described in 1880 by Bourneville and is also known as \"Bourneville disease.\" It is characterized by multisystem involvement, including the brain, skin, eyes, heart, lung, liver, and kidneys in different combinations with varying severity.[1] In the United States, 1 in 6000 newborns is affected; worldwide, 2 million people are estimated to have TS.[2]",
"TS is caused by mutations of the TSC1 gene on chromosome 9 and the TSC2 gene on chromosome 16, which encode for the proteins hamartin and tuberin, respectively.[3,4] These proteins are tumor suppressors and regulate cell division, growth, and differentiation.",
"TS is characterized by the development of various benign tumors in different organ systems of the body. The phenotypic expression varies greatly. Almost all patients have one or more of the characteristic skin lesions.[5] The typical dermatologic features include ash-leaf macules; these are elliptical, 0.5-2 cm in size, hypopigmented, and most commonly found on the trunk and lower extremities. These lesions may be present at birth. Angiofibromas, previously called \"adenoma sebaceum,\" typically involve the malar aspects of the face, as is seen in the patient in this case (Figure 1).",
"Figure 1.",
"These erythematous lesions have an increased growth during puberty and are sometimes misdiagnosed as acne. Shagreen patches have an orange peel or leathery texture. These connective tissue hamartomas are often seen in children aged 2-6 years and are located over the lower trunk, as was seen in this case (Figure 2). Periungual and subungual fibromas develop later on and occur more commonly on the toenails (Figures 3 and 4).[6]",
"Figure 2.",
"Figure 3.",
"Figure 4.",
"Brain lesions typical of TS include cortical tubers; subependymal nodules; subependymal giant cell astrocytoma (SEGA); and dysplastic, dysmyelinated white-matter lesions. Subependymal nodules are areas of rounded hypertrophic tissue and are usually seen as discrete or confluent calcified spots on CT scans of the brain. They are distributed along the walls of the lateral ventricles. These nodules and cortical tubers are visualized in nearly 90% of patients on MRI of the brain; SEGAs are seen in 5%-20% of cases.[7,8] The severity of neurologic manifestations is proportional to the burden of radiologic disease. Symptoms include seizures, mental retardation, and behavioral dysfunction. Seizures are encountered in almost 90% of cases and are typically difficult to treat.[9]",
"Renal involvement is common. Angiomyolipoma is the most common renal manifestation and is seen in 50%-80% cases, including the patient in this case (Figures 5 and 6).[9]",
"Figure 5.",
"Figure 6.",
"Angiomyolipomas may arise from the renal cortex or medulla. They are benign and are usually bilateral and multiple. An increase in the size of angiomyolipomas leads to pain and can cause hematuria and disturbance of renal function. Other lesions include benign cysts, lymphangiomas, and renal cell carcinoma.[9] Eye involvement may be retinal (astrocytic hamartomas) and nonretinal (coloboma, eyelid angiofibroma, nonparalytic strabismus, refractive errors, papilledema).[10]",
"Multiple skeletal manifestations are recognized, including sclerotic lesions; scoliosis; and bone cysts in metatarsals, metacarpals, and phalanges.[11] The most characteristic cardiovascular feature is rhabdomyoma,[12] which is found on echocardiography in approximately 50% of patients with TS. Rhabdomyomas can lead to valvular dysfunction, outflow obstruction, cardiomyopathy, and cardiac arrhythmias. Coarctation of the aorta and aortic aneurysm have also been documented. Pulmonary manifestations of TS include a cystic lung disease known as lymphangioleiomyomatosis (LAM). LAM presents with dyspnea and pneumothorax. Rarely, liver leiomyomas or adenomas may be present."
],
"date": "November 29, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/913/911/913911-fig1-thumb.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/913/911/913911-fig2-thumb.jpg"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/913/911/913911-fig3-thumb.jpg"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/913/911/913911-fig4-thumb.jpg"
},
{
"caption": "Figure 5.",
"image_url": "https://img.medscapestatic.com/article/913/911/913911-fig5-thumb.jpg"
},
{
"caption": "Figure 6.",
"image_url": "https://img.medscapestatic.com/article/913/911/913911-fig6-thumb.jpg"
}
],
"markdown": "# Fingernail, Toenail Changes and Flank Pain in a 20-Year-Old\n\n **Authors:** Sumaira Nabi, MBBS; Shahzad Ahmed, MBBS; Mazhar Badshah, MBBS \n **Date:** November 29, 2022\n\n ## Content\n\n This patient was diagnosed with tuberous sclerosis (TS) with renal angiomyolipomas. Also referred to as \"tuberous sclerosis complex,\" TS is an inherited (autosomal dominant) neurocutaneous disorder. It was first described in 1880 by Bourneville and is also known as \"Bourneville disease.\" It is characterized by multisystem involvement, including the brain, skin, eyes, heart, lung, liver, and kidneys in different combinations with varying severity.[1] In the United States, 1 in 6000 newborns is affected; worldwide, 2 million people are estimated to have TS.[2]\nTS is caused by mutations of the TSC1 gene on chromosome 9 and the TSC2 gene on chromosome 16, which encode for the proteins hamartin and tuberin, respectively.[3,4] These proteins are tumor suppressors and regulate cell division, growth, and differentiation.\nTS is characterized by the development of various benign tumors in different organ systems of the body. The phenotypic expression varies greatly. Almost all patients have one or more of the characteristic skin lesions.[5] The typical dermatologic features include ash-leaf macules; these are elliptical, 0.5-2 cm in size, hypopigmented, and most commonly found on the trunk and lower extremities. These lesions may be present at birth. Angiofibromas, previously called \"adenoma sebaceum,\" typically involve the malar aspects of the face, as is seen in the patient in this case (Figure 1).\nFigure 1.\nThese erythematous lesions have an increased growth during puberty and are sometimes misdiagnosed as acne. Shagreen patches have an orange peel or leathery texture. These connective tissue hamartomas are often seen in children aged 2-6 years and are located over the lower trunk, as was seen in this case (Figure 2). Periungual and subungual fibromas develop later on and occur more commonly on the toenails (Figures 3 and 4).[6]\nFigure 2.\nFigure 3.\nFigure 4.\nBrain lesions typical of TS include cortical tubers; subependymal nodules; subependymal giant cell astrocytoma (SEGA); and dysplastic, dysmyelinated white-matter lesions. Subependymal nodules are areas of rounded hypertrophic tissue and are usually seen as discrete or confluent calcified spots on CT scans of the brain. They are distributed along the walls of the lateral ventricles. These nodules and cortical tubers are visualized in nearly 90% of patients on MRI of the brain; SEGAs are seen in 5%-20% of cases.[7,8] The severity of neurologic manifestations is proportional to the burden of radiologic disease. Symptoms include seizures, mental retardation, and behavioral dysfunction. Seizures are encountered in almost 90% of cases and are typically difficult to treat.[9]\nRenal involvement is common. Angiomyolipoma is the most common renal manifestation and is seen in 50%-80% cases, including the patient in this case (Figures 5 and 6).[9]\nFigure 5.\nFigure 6.\nAngiomyolipomas may arise from the renal cortex or medulla. They are benign and are usually bilateral and multiple. An increase in the size of angiomyolipomas leads to pain and can cause hematuria and disturbance of renal function. Other lesions include benign cysts, lymphangiomas, and renal cell carcinoma.[9] Eye involvement may be retinal (astrocytic hamartomas) and nonretinal (coloboma, eyelid angiofibroma, nonparalytic strabismus, refractive errors, papilledema).[10]\nMultiple skeletal manifestations are recognized, including sclerotic lesions; scoliosis; and bone cysts in metatarsals, metacarpals, and phalanges.[11] The most characteristic cardiovascular feature is rhabdomyoma,[12] which is found on echocardiography in approximately 50% of patients with TS. Rhabdomyomas can lead to valvular dysfunction, outflow obstruction, cardiomyopathy, and cardiac arrhythmias. Coarctation of the aorta and aortic aneurysm have also been documented. Pulmonary manifestations of TS include a cystic lung disease known as lymphangioleiomyomatosis (LAM). LAM presents with dyspnea and pneumothorax. Rarely, liver leiomyomas or adenomas may be present.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4.** \n \n\n**Figure 5.** \n \n\n**Figure 6.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1365792,
"choiceText": "Tuberous sclerosis",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365794,
"choiceText": "Neurofibromatosis type 1",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365796,
"choiceText": "Neurofibromatosis type 2",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365798,
"choiceText": "Sturge-Weber syndrome",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 435879,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Fingernail, Toenail Changes and Flank Pain in a 20-Year-Old"
},
{
"authors": "Sumaira Nabi, MBBS; Shahzad Ahmed, MBBS; Mazhar Badshah, MBBS",
"content": [
"The diagnosis of TS is based on clinical evaluation, laboratory findings, and genetic test results. A thorough history of symptoms associated with TS should be elicited. A detailed family history is important. Obtaining a three-generation family history is recommended by international guidelines.[13] A detailed and careful physical examination should be performed, with skin and neurologic systems thoroughly examined. Characteristic dermatologic manifestations of TS should be assessed, including ash-leaf macules, facial fibroadenomas, shagreen patches, and periungual fibromas.",
"Meticulous neurologic examination and ophthalmic evaluation should be done. MRI of the brain should be performed to detect cortical tubers, subependymal nodules, SEGAs, or cerebral white-matter changes. EEG should be obtained in patients with TS who have epilepsy. Ultrasonography and CT of the abdomen are recommended to screen for renal angiomyolipomas or cysts. Echocardiography, CT of the chest, and bone radiography may be performed, depending on the history and physical examination findings.",
"In 2012, criteria for the diagnosis of TS were published by the International Tuberous Sclerosis Complex Consensus Conference.[13] These include 11 major and six minor features.",
"Major features include the following:",
"Hypomelanotic macules (three or more, at least 5 mm in diameter)",
"Angiofibromas (three or more) or fibrous cephalic plaque",
"Ungual fibromas (two or more)",
"Shagreen patches",
"Multiple retinal hamartomas",
"Cortical dysplasias",
"Subependymal nodules",
"SEGA",
"Cardiac rhabdomyoma",
"LAM",
"Angiomyolipomas (two)",
"Minor features include the following:",
"\"Confetti\" skin lesions",
"Dental enamel pits (more than three)",
"Intraoral fibromas (two or more)",
"Retinal achromic patches",
"Multiple renal cysts",
"Nonrenal hamartomas",
"The presence of two major features, or one major feature with two minor features, is considered a definitive diagnosis. Possible diagnosis includes either one major feature or two minor features.",
"The classic Vogt triad of seizures, mental retardation, and adenoma sebaceum has become obsolete. Many patients have normal intellect. Molecular genetic testing for gene mutations may be required, although the clinical signature is generally vivid enough for confirmation of the diagnosis. In some patients with TS, no mutation is present on molecular genetic testing."
],
"date": "November 29, 2022",
"figures": [],
"markdown": "# Fingernail, Toenail Changes and Flank Pain in a 20-Year-Old\n\n **Authors:** Sumaira Nabi, MBBS; Shahzad Ahmed, MBBS; Mazhar Badshah, MBBS \n **Date:** November 29, 2022\n\n ## Content\n\n The diagnosis of TS is based on clinical evaluation, laboratory findings, and genetic test results. A thorough history of symptoms associated with TS should be elicited. A detailed family history is important. Obtaining a three-generation family history is recommended by international guidelines.[13] A detailed and careful physical examination should be performed, with skin and neurologic systems thoroughly examined. Characteristic dermatologic manifestations of TS should be assessed, including ash-leaf macules, facial fibroadenomas, shagreen patches, and periungual fibromas.\nMeticulous neurologic examination and ophthalmic evaluation should be done. MRI of the brain should be performed to detect cortical tubers, subependymal nodules, SEGAs, or cerebral white-matter changes. EEG should be obtained in patients with TS who have epilepsy. Ultrasonography and CT of the abdomen are recommended to screen for renal angiomyolipomas or cysts. Echocardiography, CT of the chest, and bone radiography may be performed, depending on the history and physical examination findings.\nIn 2012, criteria for the diagnosis of TS were published by the International Tuberous Sclerosis Complex Consensus Conference.[13] These include 11 major and six minor features.\nMajor features include the following:\nHypomelanotic macules (three or more, at least 5 mm in diameter)\nAngiofibromas (three or more) or fibrous cephalic plaque\nUngual fibromas (two or more)\nShagreen patches\nMultiple retinal hamartomas\nCortical dysplasias\nSubependymal nodules\nSEGA\nCardiac rhabdomyoma\nLAM\nAngiomyolipomas (two)\nMinor features include the following:\n\"Confetti\" skin lesions\nDental enamel pits (more than three)\nIntraoral fibromas (two or more)\nRetinal achromic patches\nMultiple renal cysts\nNonrenal hamartomas\nThe presence of two major features, or one major feature with two minor features, is considered a definitive diagnosis. Possible diagnosis includes either one major feature or two minor features.\nThe classic Vogt triad of seizures, mental retardation, and adenoma sebaceum has become obsolete. Many patients have normal intellect. Molecular genetic testing for gene mutations may be required, although the clinical signature is generally vivid enough for confirmation of the diagnosis. In some patients with TS, no mutation is present on molecular genetic testing.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Fingernail, Toenail Changes and Flank Pain in a 20-Year-Old"
},
{
"authors": "Sumaira Nabi, MBBS; Shahzad Ahmed, MBBS; Mazhar Badshah, MBBS",
"content": [
"Management is directed at manifestations. Treatment of epilepsy in patients with TS is difficult and often requires polytherapy. Depending on the type of seizures, appropriate and adequate antiepileptics should be prescribed. Nearly 63% cases of epilepsy in TS are medically refractory.[14] A ketogenic diet or vagus nerve stimulation are options for these patients.[15]",
"Treatment options for brain tumors associated with TS include surgical resection or medical therapy with mammalian target of rapamycin (mTOR) inhibitors, such as everolimus.[16] If present, renal, pulmonary, and cardiac disease require referral and management by relevant specialists. The prognosis varies and depends on the number and severity of organ systems involved. It is a progressive disorder, and complications lead to morbidity and mortality. Status epilepticus, SEGA, and renal disease are the most common causes of death.",
"In this case, the patient's antiepileptic medication was adjusted, and she was referred to a urology specialist, who is helping to plan a right-sided nephrectomy."
],
"date": "November 29, 2022",
"figures": [],
"markdown": "# Fingernail, Toenail Changes and Flank Pain in a 20-Year-Old\n\n **Authors:** Sumaira Nabi, MBBS; Shahzad Ahmed, MBBS; Mazhar Badshah, MBBS \n **Date:** November 29, 2022\n\n ## Content\n\n Management is directed at manifestations. Treatment of epilepsy in patients with TS is difficult and often requires polytherapy. Depending on the type of seizures, appropriate and adequate antiepileptics should be prescribed. Nearly 63% cases of epilepsy in TS are medically refractory.[14] A ketogenic diet or vagus nerve stimulation are options for these patients.[15]\nTreatment options for brain tumors associated with TS include surgical resection or medical therapy with mammalian target of rapamycin (mTOR) inhibitors, such as everolimus.[16] If present, renal, pulmonary, and cardiac disease require referral and management by relevant specialists. The prognosis varies and depends on the number and severity of organ systems involved. It is a progressive disorder, and complications lead to morbidity and mortality. Status epilepticus, SEGA, and renal disease are the most common causes of death.\nIn this case, the patient's antiepileptic medication was adjusted, and she was referred to a urology specialist, who is helping to plan a right-sided nephrectomy.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1365800,
"choiceText": "Face",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365802,
"choiceText": "Upper extremities",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365804,
"choiceText": "Trunk and lower extremities",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365806,
"choiceText": "Hands",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365808,
"choiceText": "Chest",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Almost all patients have one or more of the characteristic skin lesions. The typical dermatologic features include ash-leaf macules; these are elliptical, 0.5-2 cm in size, hypopigmented, and most commonly found on the trunk and lower extremities. These lesions may be present at birth.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 435881,
"questionText": "Ash-leaf macules associated with TS are most commonly found where?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1365810,
"choiceText": "Renal cell carcinoma",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365812,
"choiceText": "Glomerulonephritis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365814,
"choiceText": "Renal cysts",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365816,
"choiceText": "Angiomyolipoma",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365818,
"choiceText": "Light chain nephropathy",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Renal involvement is frequently seen in TS. Angiomyolipoma is the most common renal manifestation and is seen in 50%-80% cases.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 435883,
"questionText": "Which is the most common renal manifestation of TS",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Fingernail, Toenail Changes and Flank Pain in a 20-Year-Old"
},
{
"authors": "Sumaira Nabi, MBBS; Shahzad Ahmed, MBBS; Mazhar Badshah, MBBS",
"content": [],
"date": "November 29, 2022",
"figures": [],
"markdown": "# Fingernail, Toenail Changes and Flank Pain in a 20-Year-Old\n\n **Authors:** Sumaira Nabi, MBBS; Shahzad Ahmed, MBBS; Mazhar Badshah, MBBS \n **Date:** November 29, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1365800,
"choiceText": "Face",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365802,
"choiceText": "Upper extremities",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365804,
"choiceText": "Trunk and lower extremities",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365806,
"choiceText": "Hands",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365808,
"choiceText": "Chest",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Almost all patients have one or more of the characteristic skin lesions. The typical dermatologic features include ash-leaf macules; these are elliptical, 0.5-2 cm in size, hypopigmented, and most commonly found on the trunk and lower extremities. These lesions may be present at birth.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 435881,
"questionText": "Ash-leaf macules associated with TS are most commonly found where?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1365810,
"choiceText": "Renal cell carcinoma",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365812,
"choiceText": "Glomerulonephritis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365814,
"choiceText": "Renal cysts",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365816,
"choiceText": "Angiomyolipoma",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365818,
"choiceText": "Light chain nephropathy",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Renal involvement is frequently seen in TS. Angiomyolipoma is the most common renal manifestation and is seen in 50%-80% cases.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 435883,
"questionText": "Which is the most common renal manifestation of TS",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Fingernail, Toenail Changes and Flank Pain in a 20-Year-Old"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1365792,
"choiceText": "Tuberous sclerosis",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365794,
"choiceText": "Neurofibromatosis type 1",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365796,
"choiceText": "Neurofibromatosis type 2",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365798,
"choiceText": "Sturge-Weber syndrome",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 435879,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1365800,
"choiceText": "Face",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365802,
"choiceText": "Upper extremities",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365804,
"choiceText": "Trunk and lower extremities",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365806,
"choiceText": "Hands",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365808,
"choiceText": "Chest",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Almost all patients have one or more of the characteristic skin lesions. The typical dermatologic features include ash-leaf macules; these are elliptical, 0.5-2 cm in size, hypopigmented, and most commonly found on the trunk and lower extremities. These lesions may be present at birth.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 435881,
"questionText": "Ash-leaf macules associated with TS are most commonly found where?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1365810,
"choiceText": "Renal cell carcinoma",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365812,
"choiceText": "Glomerulonephritis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365814,
"choiceText": "Renal cysts",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365816,
"choiceText": "Angiomyolipoma",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1365818,
"choiceText": "Light chain nephropathy",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Renal involvement is frequently seen in TS. Angiomyolipoma is the most common renal manifestation and is seen in 50%-80% cases.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 435883,
"questionText": "Which is the most common renal manifestation of TS",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
983918 | /viewarticle/983918 | [
{
"authors": "Malgorzata K. Nowakowska, BS; Saira George, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"An 80-year-old man presents to a dermatology clinic for skin screening and treatment of large \"golden\" patches on his chest and shoulders. The yellow-orange patches are asymptomatic but have steadily deepened in color and have progressed in extent. After his wife first noticed the patches 6 months ago, he was evaluated by a dermatologist and underwent a punch biopsy of a representative patch. On the basis of the biopsy finding of foamy, lipid-laden macrophages in the dermis, he was told the plaques were a skin finding seen in patients with underlying lipid disorders.",
"His medical history is significant for hypercholesterolemia that has been well controlled on atorvastatin (10 mg daily), which he has taken for over 20 years. He also has hypertension, which is managed with valsartan (160 mg daily). His dermatologic history is significant only for actinic keratoses and cutaneous squamous cell carcinomas. He has no significant family history of illness.",
"He has no new medications, supplements, or exposures related to the onset of his skin changes and has been in his usual state of health, with no recent illnesses. He has never smoked cigarettes or used smokeless tobacco. He occasionally smokes cigars. His current alcohol use consists of about one standard drink per day. On a review of systems, he reports only mild fatigue with no fevers, chills, night sweats, weight loss, or malaise."
],
"date": "November 22, 2022",
"figures": [],
"markdown": "# Dermatology Case Challenge: Colorful Skin Patches on a Man With Fatigue Who Smokes Cigars\n\n **Authors:** Malgorzata K. Nowakowska, BS; Saira George, MD \n **Date:** November 22, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nAn 80-year-old man presents to a dermatology clinic for skin screening and treatment of large \"golden\" patches on his chest and shoulders. The yellow-orange patches are asymptomatic but have steadily deepened in color and have progressed in extent. After his wife first noticed the patches 6 months ago, he was evaluated by a dermatologist and underwent a punch biopsy of a representative patch. On the basis of the biopsy finding of foamy, lipid-laden macrophages in the dermis, he was told the plaques were a skin finding seen in patients with underlying lipid disorders.\nHis medical history is significant for hypercholesterolemia that has been well controlled on atorvastatin (10 mg daily), which he has taken for over 20 years. He also has hypertension, which is managed with valsartan (160 mg daily). His dermatologic history is significant only for actinic keratoses and cutaneous squamous cell carcinomas. He has no significant family history of illness.\nHe has no new medications, supplements, or exposures related to the onset of his skin changes and has been in his usual state of health, with no recent illnesses. He has never smoked cigarettes or used smokeless tobacco. He occasionally smokes cigars. His current alcohol use consists of about one standard drink per day. On a review of systems, he reports only mild fatigue with no fevers, chills, night sweats, weight loss, or malaise.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Dermatology Case Challenge: Colorful Skin Patches on a Man With Fatigue Who Smokes Cigars"
},
{
"authors": "Malgorzata K. Nowakowska, BS; Saira George, MD",
"content": [
"Upon physical examination, the patient appears relaxed and comfortable. His vital signs include a temperature of 98.1 °F (36.7 °C), a blood pressure of 145/65 mm Hg, a heart rate of 62 beats/min, and a respiration rate of 18 breaths/min.",
"Examination of the skin reveals diffuse, symmetric yellow-orange thin plaques involving the upper torso and upper arms (Figure 1 and Figure 2). He has no mucosal involvement. Sclera, conjunctiva, and eyelids are clear, without signs of jaundice.",
"Figure 1.",
"Figure 2.",
"The bloodwork results are notable for normal total, low-density lipoprotein, and high-density lipoprotein cholesterol levels and triglyceride levels. A complete blood cell count is unremarkable, except for mild anemia (hemoglobin level, 12.7 g/dL; reference range, 13.8-17.2 g/dL) and mild thrombocytopenia (127,000 cells/μL; reference range, 150,000-450,000 cells/μL). Serum electrophoresis and immunofixation are ordered and show an M protein level of 3.0 g/dL (reference range, 0.57-2.63 g/dL) and an immunoglobulin G (IgG) kappa monoclonal gammopathy.",
"The patient is referred to the hematology-oncology service. After an extensive workup of his monoclonal gammopathy, including a bone marrow biopsy and a bone survey, he is found to have smoldering multiple myeloma."
],
"date": "November 22, 2022",
"figures": [],
"markdown": "# Dermatology Case Challenge: Colorful Skin Patches on a Man With Fatigue Who Smokes Cigars\n\n **Authors:** Malgorzata K. Nowakowska, BS; Saira George, MD \n **Date:** November 22, 2022\n\n ## Content\n\n Upon physical examination, the patient appears relaxed and comfortable. His vital signs include a temperature of 98.1 °F (36.7 °C), a blood pressure of 145/65 mm Hg, a heart rate of 62 beats/min, and a respiration rate of 18 breaths/min.\nExamination of the skin reveals diffuse, symmetric yellow-orange thin plaques involving the upper torso and upper arms (Figure 1 and Figure 2). He has no mucosal involvement. Sclera, conjunctiva, and eyelids are clear, without signs of jaundice.\nFigure 1.\nFigure 2.\nThe bloodwork results are notable for normal total, low-density lipoprotein, and high-density lipoprotein cholesterol levels and triglyceride levels. A complete blood cell count is unremarkable, except for mild anemia (hemoglobin level, 12.7 g/dL; reference range, 13.8-17.2 g/dL) and mild thrombocytopenia (127,000 cells/μL; reference range, 150,000-450,000 cells/μL). Serum electrophoresis and immunofixation are ordered and show an M protein level of 3.0 g/dL (reference range, 0.57-2.63 g/dL) and an immunoglobulin G (IgG) kappa monoclonal gammopathy.\nThe patient is referred to the hematology-oncology service. After an extensive workup of his monoclonal gammopathy, including a bone marrow biopsy and a bone survey, he is found to have smoldering multiple myeloma.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1739571,
"choiceText": "Cutaneous sarcoidosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739572,
"choiceText": "Carotenemia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739573,
"choiceText": "Normolipemic plane xanthoma",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739574,
"choiceText": "Lipoid proteinosis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739575,
"choiceText": "Necrobiotic xanthogranuloma",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 561773,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Dermatology Case Challenge: Colorful Skin Patches on a Man With Fatigue Who Smokes Cigars"
},
{
"authors": "Malgorzata K. Nowakowska, BS; Saira George, MD",
"content": [
"Widespread large yellow-orange patches and plaques on the torso, shoulders, and upper arms, accompanied by the histologic finding of lipid-laden macrophages, or \"foam cells,\" are a characteristic presentation of diffuse normolipemic plane xanthomas. Carotenemia presents with a generalized yellow skin discoloration due to excess levels of beta-carotene, most commonly from excessive dietary intake of beta-carotene–rich vegetables. Lipoid proteinosis is a rare autosomal recessive genodermatosis that presents during the first year of life with mucocutaneous and visceral findings related to the deposition of amorphous hyaline material. Necrobiotic xanthogranuloma is a multisystemic histiocytic condition in which yellow-orange papules or plaques most commonly involve the periorbital skin. The protean manifestations of cutaneous sarcoidosis can include yellow-orange papules or plaques, but histologic examination of these lesions typically reveals the noncaseating granulomas typical of the disorder.",
"Cutaneous xanthomas represent lipid deposition in the skin.[1] The word xanthoma is derived from the Greek word xanthos, meaning yellow, and refers to the distinctive hue of most lesions. Scavenging macrophages that phagocytose and oxidize lipids give rise to the characteristic histologic finding of xanthomas: lipid-laden macrophages, or \"foam cells,\" in the dermis.[2] Additional inflammatory cells, extracellular lipids, and fibrosis may also be present, to varying degrees. The exact mechanisms that lead to lipid deposition in the skin and the formation of xanthomas are not yet fully known but are thought to differ among the various subtypes of xanthomas.[3]"
],
"date": "November 22, 2022",
"figures": [],
"markdown": "# Dermatology Case Challenge: Colorful Skin Patches on a Man With Fatigue Who Smokes Cigars\n\n **Authors:** Malgorzata K. Nowakowska, BS; Saira George, MD \n **Date:** November 22, 2022\n\n ## Content\n\n Widespread large yellow-orange patches and plaques on the torso, shoulders, and upper arms, accompanied by the histologic finding of lipid-laden macrophages, or \"foam cells,\" are a characteristic presentation of diffuse normolipemic plane xanthomas. Carotenemia presents with a generalized yellow skin discoloration due to excess levels of beta-carotene, most commonly from excessive dietary intake of beta-carotene–rich vegetables. Lipoid proteinosis is a rare autosomal recessive genodermatosis that presents during the first year of life with mucocutaneous and visceral findings related to the deposition of amorphous hyaline material. Necrobiotic xanthogranuloma is a multisystemic histiocytic condition in which yellow-orange papules or plaques most commonly involve the periorbital skin. The protean manifestations of cutaneous sarcoidosis can include yellow-orange papules or plaques, but histologic examination of these lesions typically reveals the noncaseating granulomas typical of the disorder.\nCutaneous xanthomas represent lipid deposition in the skin.[1] The word xanthoma is derived from the Greek word xanthos, meaning yellow, and refers to the distinctive hue of most lesions. Scavenging macrophages that phagocytose and oxidize lipids give rise to the characteristic histologic finding of xanthomas: lipid-laden macrophages, or \"foam cells,\" in the dermis.[2] Additional inflammatory cells, extracellular lipids, and fibrosis may also be present, to varying degrees. The exact mechanisms that lead to lipid deposition in the skin and the formation of xanthomas are not yet fully known but are thought to differ among the various subtypes of xanthomas.[3]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1739571,
"choiceText": "Cutaneous sarcoidosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739572,
"choiceText": "Carotenemia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739573,
"choiceText": "Normolipemic plane xanthoma",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739574,
"choiceText": "Lipoid proteinosis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739575,
"choiceText": "Necrobiotic xanthogranuloma",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 561773,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Dermatology Case Challenge: Colorful Skin Patches on a Man With Fatigue Who Smokes Cigars"
},
{
"authors": "Malgorzata K. Nowakowska, BS; Saira George, MD",
"content": [
"Xanthomas often develop in association with hyperlipidemia. In hyperlipidemic states, the elevated level or abnormal composition of lipoproteins in the blood is thought to result in lipoprotein extravasation and deposition in the skin.[2,4] Both primary hyperlipidemia (arising from genetic disorders of lipid metabolism) and secondary hyperlipidemia (caused by medications or disease states such as diabetes, cholestasis, and nephrotic syndrome) can result in xanthoma formation.[2,5]",
"Eruptive xanthomas present as a widespread eruption of small red-yellow papules, with a predilection for the hands, buttocks, and extensor surfaces of the extremities. They are associated with hypertriglyceridemia and can be secondary to alcohol abuse; diabetes; obesity; and certain medications, such as oral retinoids, protease inhibitors, olanzapine, prednisone, cyclosporine, and estrogen replacement.[4] Tuberous xanthomas are yellow-pink indurated papulonodules that typically form over the tuberosities of joints, such as at the elbows and knees. Tendinous xanthomas are smooth, firm nodules that involve the Achilles tendon or extensor tendons of the hands, elbows, and knees. Both tuberous xanthomas and tendinous xanthomas are associated with familial hyperlipidemias, particularly types II and III.[6] Verruciform xanthomas, which are small, warty-appearing papules that usually involve the mouth and genitals, are not associated with hyperlipidemia but are thought to result from epithelial lipids released by local trauma.[7]",
"Plane xanthomas are yellow to orange patches or plaques that most commonly involve the eyelid, neck, upper torso, interdigital areas, and palms.[3] More than 50% of cases of plane xanthomas are associated with a primary or secondary hyperlipidemia.[8] The most commonly encountered type of xanthoma is xanthelasma palpebrarum, a localized plane xanthoma of the eyelid. Patients with xanthelasma have been found to have higher serum levels of total cholesterol and apolipoprotein B (a risk marker of atherosclerosis) than do normal control patients.[9] Other plane xanthomas are pathognomonic of certain hereditary lipid disorders. Xanthomas of the creases of the palm (xanthoma striatum palmare) are seen almost exclusively in familial dysbetalipoproteinemia.[10] Interdigital plane xanthomas, most commonly arising between the thumb and index finger, are strongly indicative of homozygous familial hypercholesterolemia.[11]",
"Diffuse normolipemic plane xanthomas, as seen in the patient in this case, are widespread large yellow-orange patches or plaques that favor the neck, upper torso, and shoulders. Palpebral involvement can also occur. The clinical significance of diffuse normolipemic plane xanthomas is their association with paraproteinemias, most commonly multiple myeloma.[12] Normolipemic plane xanthomas can also be seen with other hematologic or lymphoproliferative disorders, including monoclonal gammopathy of undetermined significance, Waldenström macroglobulinemia, leukemias (such as chronic myelomonocytic leukemia and chronic myeloid leukemia), B-cell lymphoma, and Castleman disease.[12,13,14,15] The development of xanthomas in association with hematologic disorders is thought to result from the presence of an abnormal serum protein that binds lipoproteins to form complexes that aggregate in the skin.[13]",
"Because xanthomas are frequently associated with primary and secondary lipid disorders, the initial workup should include a fasting serum lipid panel, measurement of fasting glucose and hemoglobin 1c, and renal and liver function tests.[3] In patients who present with diffuse normolipemic plane xanthomas, a careful evaluation for hematologic and lymphoproliferative disorders should be performed, owing to the association of this subtype with underlying hematologic disorders. Because the development of normolipemic plane xanthomas can precede an associated hematologic disease by months to years, monitoring should be ongoing.[3,13,16] The workup should include a complete blood cell count and serum and urine protein electrophoresis with immunofixation. If a paraproteinemia is detected, referral to a hematologist or an oncologist for further evaluation and management is indicated."
],
"date": "November 22, 2022",
"figures": [],
"markdown": "# Dermatology Case Challenge: Colorful Skin Patches on a Man With Fatigue Who Smokes Cigars\n\n **Authors:** Malgorzata K. Nowakowska, BS; Saira George, MD \n **Date:** November 22, 2022\n\n ## Content\n\n Xanthomas often develop in association with hyperlipidemia. In hyperlipidemic states, the elevated level or abnormal composition of lipoproteins in the blood is thought to result in lipoprotein extravasation and deposition in the skin.[2,4] Both primary hyperlipidemia (arising from genetic disorders of lipid metabolism) and secondary hyperlipidemia (caused by medications or disease states such as diabetes, cholestasis, and nephrotic syndrome) can result in xanthoma formation.[2,5]\nEruptive xanthomas present as a widespread eruption of small red-yellow papules, with a predilection for the hands, buttocks, and extensor surfaces of the extremities. They are associated with hypertriglyceridemia and can be secondary to alcohol abuse; diabetes; obesity; and certain medications, such as oral retinoids, protease inhibitors, olanzapine, prednisone, cyclosporine, and estrogen replacement.[4] Tuberous xanthomas are yellow-pink indurated papulonodules that typically form over the tuberosities of joints, such as at the elbows and knees. Tendinous xanthomas are smooth, firm nodules that involve the Achilles tendon or extensor tendons of the hands, elbows, and knees. Both tuberous xanthomas and tendinous xanthomas are associated with familial hyperlipidemias, particularly types II and III.[6] Verruciform xanthomas, which are small, warty-appearing papules that usually involve the mouth and genitals, are not associated with hyperlipidemia but are thought to result from epithelial lipids released by local trauma.[7]\nPlane xanthomas are yellow to orange patches or plaques that most commonly involve the eyelid, neck, upper torso, interdigital areas, and palms.[3] More than 50% of cases of plane xanthomas are associated with a primary or secondary hyperlipidemia.[8] The most commonly encountered type of xanthoma is xanthelasma palpebrarum, a localized plane xanthoma of the eyelid. Patients with xanthelasma have been found to have higher serum levels of total cholesterol and apolipoprotein B (a risk marker of atherosclerosis) than do normal control patients.[9] Other plane xanthomas are pathognomonic of certain hereditary lipid disorders. Xanthomas of the creases of the palm (xanthoma striatum palmare) are seen almost exclusively in familial dysbetalipoproteinemia.[10] Interdigital plane xanthomas, most commonly arising between the thumb and index finger, are strongly indicative of homozygous familial hypercholesterolemia.[11]\nDiffuse normolipemic plane xanthomas, as seen in the patient in this case, are widespread large yellow-orange patches or plaques that favor the neck, upper torso, and shoulders. Palpebral involvement can also occur. The clinical significance of diffuse normolipemic plane xanthomas is their association with paraproteinemias, most commonly multiple myeloma.[12] Normolipemic plane xanthomas can also be seen with other hematologic or lymphoproliferative disorders, including monoclonal gammopathy of undetermined significance, Waldenström macroglobulinemia, leukemias (such as chronic myelomonocytic leukemia and chronic myeloid leukemia), B-cell lymphoma, and Castleman disease.[12,13,14,15] The development of xanthomas in association with hematologic disorders is thought to result from the presence of an abnormal serum protein that binds lipoproteins to form complexes that aggregate in the skin.[13]\nBecause xanthomas are frequently associated with primary and secondary lipid disorders, the initial workup should include a fasting serum lipid panel, measurement of fasting glucose and hemoglobin 1c, and renal and liver function tests.[3] In patients who present with diffuse normolipemic plane xanthomas, a careful evaluation for hematologic and lymphoproliferative disorders should be performed, owing to the association of this subtype with underlying hematologic disorders. Because the development of normolipemic plane xanthomas can precede an associated hematologic disease by months to years, monitoring should be ongoing.[3,13,16] The workup should include a complete blood cell count and serum and urine protein electrophoresis with immunofixation. If a paraproteinemia is detected, referral to a hematologist or an oncologist for further evaluation and management is indicated.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Dermatology Case Challenge: Colorful Skin Patches on a Man With Fatigue Who Smokes Cigars"
},
{
"authors": "Malgorzata K. Nowakowska, BS; Saira George, MD",
"content": [
"The management of xanthomas is generally directed toward treatment of an underlying disease if present. Although xanthomas associated with hyperlipidemia often improve with correction of the lipid disorder, diffuse normolipemic xanthomas may persist even with the treatment of an underlying condition. A number of surgical and destructive treatments for xanthomas, ranging from simple excision to laser ablation, have been tried and may be feasible, depending on the distribution, size, and number of the lesions.[17]",
"After multiple myeloma was detected in the patient in this case, chemotherapy was scheduled. Because normolipemic plane xanthomas were observed before other manifestations of his disease, the multiple myeloma was detected early, and his prognosis is good. The appearance of the xanthomas improved with treatment of the underlying disease.",
"In summary, although xanthomas are often associated with lipid disorders, diffuse normolipemic plane xanthoma is a rare variant that most commonly develops in patients with hematologic disorders. A diagnosis of normolipemic plane xanthomas should prompt assessment and ongoing monitoring for an underlying hematologic or lymphoproliferative disease."
],
"date": "November 22, 2022",
"figures": [],
"markdown": "# Dermatology Case Challenge: Colorful Skin Patches on a Man With Fatigue Who Smokes Cigars\n\n **Authors:** Malgorzata K. Nowakowska, BS; Saira George, MD \n **Date:** November 22, 2022\n\n ## Content\n\n The management of xanthomas is generally directed toward treatment of an underlying disease if present. Although xanthomas associated with hyperlipidemia often improve with correction of the lipid disorder, diffuse normolipemic xanthomas may persist even with the treatment of an underlying condition. A number of surgical and destructive treatments for xanthomas, ranging from simple excision to laser ablation, have been tried and may be feasible, depending on the distribution, size, and number of the lesions.[17]\nAfter multiple myeloma was detected in the patient in this case, chemotherapy was scheduled. Because normolipemic plane xanthomas were observed before other manifestations of his disease, the multiple myeloma was detected early, and his prognosis is good. The appearance of the xanthomas improved with treatment of the underlying disease.\nIn summary, although xanthomas are often associated with lipid disorders, diffuse normolipemic plane xanthoma is a rare variant that most commonly develops in patients with hematologic disorders. A diagnosis of normolipemic plane xanthomas should prompt assessment and ongoing monitoring for an underlying hematologic or lymphoproliferative disease.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1739581,
"choiceText": "Waldenström macroglobulinemia",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739582,
"choiceText": "Hepatic cholestasis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739583,
"choiceText": "Multiple myeloma",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739584,
"choiceText": "Monoclonal gammopathy of undetermined significance",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739585,
"choiceText": "Lymphoma",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Unlike many other types of xanthomas, diffuse normolipemic plane xanthomas are not principally associated with underlying primary or secondary lipid disorders, such as may be seen with hepatic cholestasis. Instead, they are associated with hematologic or lymphoproliferative disorders, including monoclonal gammopathy of undetermined significance, multiple myeloma, Waldenström macroglobulinemia, myelodysplastic syndrome, chronic myelomonocytic leukemia, B-cell lymphoma, and Castleman disease.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 561779,
"questionText": "Which condition is <i>least </i>likely to be associated with diffuse normolipemic plane xanthomas?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1739630,
"choiceText": "Bacterial cultures",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739631,
"choiceText": "Liver biopsy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739632,
"choiceText": "Cerebrospinal fluid studies",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739633,
"choiceText": "Serum protein electrophoresis and immunofixation",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739634,
"choiceText": "Vitamin D level measurement",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "For patients who present with diffuse normolipemic plane xanthomas, a complete blood cell count and serum and urine protein electrophoresis with immunofixation should be performed for the initial evaluation, with continued monitoring for an associated hematologic cancer.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 561794,
"questionText": "Which test should be ordered for patients who present with diffuse normolipemic plane xanthomas?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Dermatology Case Challenge: Colorful Skin Patches on a Man With Fatigue Who Smokes Cigars"
},
{
"authors": "Malgorzata K. Nowakowska, BS; Saira George, MD",
"content": [
"Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult."
],
"date": "November 22, 2022",
"figures": [],
"markdown": "# Dermatology Case Challenge: Colorful Skin Patches on a Man With Fatigue Who Smokes Cigars\n\n **Authors:** Malgorzata K. Nowakowska, BS; Saira George, MD \n **Date:** November 22, 2022\n\n ## Content\n\n Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult.\n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1739581,
"choiceText": "Waldenström macroglobulinemia",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739582,
"choiceText": "Hepatic cholestasis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739583,
"choiceText": "Multiple myeloma",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739584,
"choiceText": "Monoclonal gammopathy of undetermined significance",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739585,
"choiceText": "Lymphoma",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Unlike many other types of xanthomas, diffuse normolipemic plane xanthomas are not principally associated with underlying primary or secondary lipid disorders, such as may be seen with hepatic cholestasis. Instead, they are associated with hematologic or lymphoproliferative disorders, including monoclonal gammopathy of undetermined significance, multiple myeloma, Waldenström macroglobulinemia, myelodysplastic syndrome, chronic myelomonocytic leukemia, B-cell lymphoma, and Castleman disease.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 561779,
"questionText": "Which condition is <i>least </i>likely to be associated with diffuse normolipemic plane xanthomas?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1739630,
"choiceText": "Bacterial cultures",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739631,
"choiceText": "Liver biopsy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739632,
"choiceText": "Cerebrospinal fluid studies",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739633,
"choiceText": "Serum protein electrophoresis and immunofixation",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739634,
"choiceText": "Vitamin D level measurement",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "For patients who present with diffuse normolipemic plane xanthomas, a complete blood cell count and serum and urine protein electrophoresis with immunofixation should be performed for the initial evaluation, with continued monitoring for an associated hematologic cancer.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 561794,
"questionText": "Which test should be ordered for patients who present with diffuse normolipemic plane xanthomas?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Dermatology Case Challenge: Colorful Skin Patches on a Man With Fatigue Who Smokes Cigars"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1739571,
"choiceText": "Cutaneous sarcoidosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739572,
"choiceText": "Carotenemia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739573,
"choiceText": "Normolipemic plane xanthoma",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739574,
"choiceText": "Lipoid proteinosis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739575,
"choiceText": "Necrobiotic xanthogranuloma",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 561773,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1739581,
"choiceText": "Waldenström macroglobulinemia",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739582,
"choiceText": "Hepatic cholestasis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739583,
"choiceText": "Multiple myeloma",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739584,
"choiceText": "Monoclonal gammopathy of undetermined significance",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739585,
"choiceText": "Lymphoma",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Unlike many other types of xanthomas, diffuse normolipemic plane xanthomas are not principally associated with underlying primary or secondary lipid disorders, such as may be seen with hepatic cholestasis. Instead, they are associated with hematologic or lymphoproliferative disorders, including monoclonal gammopathy of undetermined significance, multiple myeloma, Waldenström macroglobulinemia, myelodysplastic syndrome, chronic myelomonocytic leukemia, B-cell lymphoma, and Castleman disease.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 561779,
"questionText": "Which condition is <i>least </i>likely to be associated with diffuse normolipemic plane xanthomas?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1739630,
"choiceText": "Bacterial cultures",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739631,
"choiceText": "Liver biopsy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739632,
"choiceText": "Cerebrospinal fluid studies",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739633,
"choiceText": "Serum protein electrophoresis and immunofixation",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1739634,
"choiceText": "Vitamin D level measurement",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "For patients who present with diffuse normolipemic plane xanthomas, a complete blood cell count and serum and urine protein electrophoresis with immunofixation should be performed for the initial evaluation, with continued monitoring for an associated hematologic cancer.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 561794,
"questionText": "Which test should be ordered for patients who present with diffuse normolipemic plane xanthomas?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
885566 | /viewarticle/885566 | [
{
"authors": "Vimon Seriburi, MD; Ann F. Fisher, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 73-year-old woman presents to the emergency department (ED) with fever, chills, and night sweats. Approximately 3 weeks ago, she was hospitalized for hematochezia and fever; urine cultures from that hospitalization had grown Escherichia coli, and the blood cultures were positive for Serratia marcescens.",
"The workup during that initial hospitalization also included transthoracic echocardiography that revealed no valvular abnormalities; noncontrast abdominal CT, which failed to demonstrate any intra-abdominal pathology; and colonoscopy, which was positive only for polyps. At the time of discharge, the hematochezia was suspected to have been caused by several large external hemorrhoids that were noted on the physical examination as a diagnosis of exclusion. Repeat blood cultures were performed, and they were negative for growth. The patient was discharged to home to complete a 2-week course of levofloxacin after sensitivities from the initial set of cultures were confirmed.",
"At today's presentation to the ED (3 days after finishing her course of levofloxacin), the patient states that over the past 24 hours, the fever and chills have returned. She denies any rectal bleeding, dizziness, headache, chest pain, hematemesis, abdominal pain, melena, dysuria, or recent weight change. Her medical history includes hypertension; abdominal aortic aneurysm with bilateral iliac artery occlusive disease, treated by aortobifemoral bypass grafting 6 years ago; coronary artery disease, treated with coronary artery bypass grafting 1 year ago; diabetes; chronic renal insufficiency; and diverticulosis. She has an 80–pack-year history of smoking, and she currently continues to smoke. The review of systems is notable only for a chronic cough."
],
"date": "November 14, 2022",
"figures": [],
"markdown": "# Emergency Med Case Challenge: Hemorrhoids, Urinary and Blood Infections in a Woman With Rigors\n\n **Authors:** Vimon Seriburi, MD; Ann F. Fisher, MD \n **Date:** November 14, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 73-year-old woman presents to the emergency department (ED) with fever, chills, and night sweats. Approximately 3 weeks ago, she was hospitalized for hematochezia and fever; urine cultures from that hospitalization had grown Escherichia coli, and the blood cultures were positive for Serratia marcescens.\nThe workup during that initial hospitalization also included transthoracic echocardiography that revealed no valvular abnormalities; noncontrast abdominal CT, which failed to demonstrate any intra-abdominal pathology; and colonoscopy, which was positive only for polyps. At the time of discharge, the hematochezia was suspected to have been caused by several large external hemorrhoids that were noted on the physical examination as a diagnosis of exclusion. Repeat blood cultures were performed, and they were negative for growth. The patient was discharged to home to complete a 2-week course of levofloxacin after sensitivities from the initial set of cultures were confirmed.\nAt today's presentation to the ED (3 days after finishing her course of levofloxacin), the patient states that over the past 24 hours, the fever and chills have returned. She denies any rectal bleeding, dizziness, headache, chest pain, hematemesis, abdominal pain, melena, dysuria, or recent weight change. Her medical history includes hypertension; abdominal aortic aneurysm with bilateral iliac artery occlusive disease, treated by aortobifemoral bypass grafting 6 years ago; coronary artery disease, treated with coronary artery bypass grafting 1 year ago; diabetes; chronic renal insufficiency; and diverticulosis. She has an 80–pack-year history of smoking, and she currently continues to smoke. The review of systems is notable only for a chronic cough.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Emergency Med Case Challenge: Hemorrhoids, Urinary and Blood Infections in a Woman With Rigors"
},
{
"authors": "Vimon Seriburi, MD; Ann F. Fisher, MD",
"content": [
"The physical examination demonstrates a toxic-appearing elderly woman who is actively experiencing rigors, with a temperature of 103°F (39.4°C) and a heart rate of 104 beats/min. Her blood pressure is stable at 120/86 mm Hg. She has pulse oxygenation of 97% while breathing room air. Distant and regular heart sounds are heard, but no murmur is noted.",
"The lung examination is unremarkable except for an occasional wheeze. The abdomen is soft and nontender, with positive normoactive bowel sounds and no apparent organomegaly. She has a well-healed midline abdominal incision from her prior surgery. The rectal examination reveals several nontender external hemorrhoids, with no evidence of recent bleeding. Guaiac testing of the stool is strongly positive.",
"Her laboratory findings are notable for a white blood cell count of 23.7 × 103 cells/µL, with 98% neutrophils and 12% bands; a hemoglobin level of 8.2 g/dL; and a hematocrit of 24.6%. At the time of discharge approximately 2 weeks ago, her baseline hemoglobin level was 10 g/dL and baseline hematocrit was 29.4%. The creatinine level is 1.8 mg/dL (reference range, 0.59-1.04 mg/dL). Liver aminotransferase values are within normal limits. Urinalysis is unremarkable.",
"Chest radiography reveals clear lung fields. Given the patient's relatively recent history of colonic instrumentation, repeat abdominal CT is performed, this time with both oral and intravenous contrast (Figure 1).",
"Figure 1.",
"To help in making the diagnosis, additional information from the hospitalization is presented here. Two sets of blood cultures were obtained in the ED, at the time of initial presentation, several hours apart, and the two cultures were noted to be positive for different organisms: alpha-hemolytic Streptococcus and Candida glabrata. In addition, repeat echocardiography was again negative for vegetations."
],
"date": "November 14, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/885/566/885566-Thumb1.png"
}
],
"markdown": "# Emergency Med Case Challenge: Hemorrhoids, Urinary and Blood Infections in a Woman With Rigors\n\n **Authors:** Vimon Seriburi, MD; Ann F. Fisher, MD \n **Date:** November 14, 2022\n\n ## Content\n\n The physical examination demonstrates a toxic-appearing elderly woman who is actively experiencing rigors, with a temperature of 103°F (39.4°C) and a heart rate of 104 beats/min. Her blood pressure is stable at 120/86 mm Hg. She has pulse oxygenation of 97% while breathing room air. Distant and regular heart sounds are heard, but no murmur is noted.\nThe lung examination is unremarkable except for an occasional wheeze. The abdomen is soft and nontender, with positive normoactive bowel sounds and no apparent organomegaly. She has a well-healed midline abdominal incision from her prior surgery. The rectal examination reveals several nontender external hemorrhoids, with no evidence of recent bleeding. Guaiac testing of the stool is strongly positive.\nHer laboratory findings are notable for a white blood cell count of 23.7 × 103 cells/µL, with 98% neutrophils and 12% bands; a hemoglobin level of 8.2 g/dL; and a hematocrit of 24.6%. At the time of discharge approximately 2 weeks ago, her baseline hemoglobin level was 10 g/dL and baseline hematocrit was 29.4%. The creatinine level is 1.8 mg/dL (reference range, 0.59-1.04 mg/dL). Liver aminotransferase values are within normal limits. Urinalysis is unremarkable.\nChest radiography reveals clear lung fields. Given the patient's relatively recent history of colonic instrumentation, repeat abdominal CT is performed, this time with both oral and intravenous contrast (Figure 1).\nFigure 1.\nTo help in making the diagnosis, additional information from the hospitalization is presented here. Two sets of blood cultures were obtained in the ED, at the time of initial presentation, several hours apart, and the two cultures were noted to be positive for different organisms: alpha-hemolytic Streptococcus and Candida glabrata. In addition, repeat echocardiography was again negative for vegetations.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136578,
"choiceText": "Diverticulitis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136580,
"choiceText": "Aortoenteric fistula",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136582,
"choiceText": "Urinary tract infection",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136584,
"choiceText": "Bacterial endocarditis\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360613,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Emergency Med Case Challenge: Hemorrhoids, Urinary and Blood Infections in a Woman With Rigors"
},
{
"authors": "Vimon Seriburi, MD; Ann F. Fisher, MD",
"content": [
"Recurrent bacteremia and bleeding secondary to an aortoenteric fistula (AEF) were diagnosed in this patient. AEFs are rare clinical entities that often result in fatal exsanguination if not recognized early. Gastrointestinal (GI) bleeding in a patient with a known or repaired abdominal aortic aneurysm should be considered secondary to an AEF until proven otherwise.",
"On the basis of this patient's symptoms and presentation, bacterial endocarditis, pneumonia, urinary tract infection, and intra-abdominal infection are reasonable differential diagnoses. However, because of an otherwise unremarkable workup and suspicion of an intra-abdominal infectious process (given the recent colonoscopy and the patient's history of an abdominal aortic aneurysm repair), abdominal CT was performed. The scan suggested the diagnosis of AEF (Figure 1); it demonstrated an aorta that was intimately associated with the third portion of the duodenum and, furthermore, a small air bubble at the interface of the aorta and duodenum.",
"Figure 1.",
"Other findings on the CT scan that were suggestive of AEF included fat stranding and fluid around the aortic graft and loss of normal tissue planes between the duodenum and the aortic graft.",
"Another nonradiographic clue to the diagnosis of AEF was the fact that the various blood cultures were positive for multiple different organisms. A previous blood culture had grown S marcescens, and one set of the current blood cultures grew Streptococcus viridans, a common colonizer of the oral and GI tracts.",
"In addition, the patient had evidence of fungemia, with C glabrata on the second set of blood cultures from the current hospitalization. The diagnosis of AEF was definitively confirmed by esophagogastroduodenoscopy, which revealed ulceration into part of the aortic graft (the white patch seen in Figure 2), visualized about 100 mm distal to the pyloric bulb.[1,2,3,4]",
"Figure 2.",
"AEF was first described in 1839 in a patient with a pulsatile abdominal mass and bloody stool who died suddenly. At autopsy, the jejunum was noted to have adhered to the \"aneurysmal bag and that sac has ulcerated in the intestine.\"[5] Since then, two types of AEFs have been described: primary and secondary."
],
"date": "November 14, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/885/566/885566-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/885/566/885566-Thumb2.png"
}
],
"markdown": "# Emergency Med Case Challenge: Hemorrhoids, Urinary and Blood Infections in a Woman With Rigors\n\n **Authors:** Vimon Seriburi, MD; Ann F. Fisher, MD \n **Date:** November 14, 2022\n\n ## Content\n\n Recurrent bacteremia and bleeding secondary to an aortoenteric fistula (AEF) were diagnosed in this patient. AEFs are rare clinical entities that often result in fatal exsanguination if not recognized early. Gastrointestinal (GI) bleeding in a patient with a known or repaired abdominal aortic aneurysm should be considered secondary to an AEF until proven otherwise.\nOn the basis of this patient's symptoms and presentation, bacterial endocarditis, pneumonia, urinary tract infection, and intra-abdominal infection are reasonable differential diagnoses. However, because of an otherwise unremarkable workup and suspicion of an intra-abdominal infectious process (given the recent colonoscopy and the patient's history of an abdominal aortic aneurysm repair), abdominal CT was performed. The scan suggested the diagnosis of AEF (Figure 1); it demonstrated an aorta that was intimately associated with the third portion of the duodenum and, furthermore, a small air bubble at the interface of the aorta and duodenum.\nFigure 1.\nOther findings on the CT scan that were suggestive of AEF included fat stranding and fluid around the aortic graft and loss of normal tissue planes between the duodenum and the aortic graft.\nAnother nonradiographic clue to the diagnosis of AEF was the fact that the various blood cultures were positive for multiple different organisms. A previous blood culture had grown S marcescens, and one set of the current blood cultures grew Streptococcus viridans, a common colonizer of the oral and GI tracts.\nIn addition, the patient had evidence of fungemia, with C glabrata on the second set of blood cultures from the current hospitalization. The diagnosis of AEF was definitively confirmed by esophagogastroduodenoscopy, which revealed ulceration into part of the aortic graft (the white patch seen in Figure 2), visualized about 100 mm distal to the pyloric bulb.[1,2,3,4]\nFigure 2.\nAEF was first described in 1839 in a patient with a pulsatile abdominal mass and bloody stool who died suddenly. At autopsy, the jejunum was noted to have adhered to the \"aneurysmal bag and that sac has ulcerated in the intestine.\"[5] Since then, two types of AEFs have been described: primary and secondary.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136578,
"choiceText": "Diverticulitis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136580,
"choiceText": "Aortoenteric fistula",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136582,
"choiceText": "Urinary tract infection",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136584,
"choiceText": "Bacterial endocarditis\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360613,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Emergency Med Case Challenge: Hemorrhoids, Urinary and Blood Infections in a Woman With Rigors"
},
{
"authors": "Vimon Seriburi, MD; Ann F. Fisher, MD",
"content": [
"Primary AEFs are caused by spontaneous erosion of the aorta into the GI tract. As many as 83% of these cases are associated with abdominal aortic atherosclerotic aneurysms, with a mean diameter of 6.2 cm. Other causes of AEFs include infection (often with tuberculosis or syphilis), cancer, radiation therapy, and foreign body ingestion. Evidence of GI bleeding is observed in 94% of cases, abdominal or back pain is seen in 46% of cases, and a pulsating mass is found in 17% of cases. The classic triad of GI hemorrhage, abdominal pain, and pulsating abdominal mass is present only in 11% of cases.",
"Classically, AEF initially presents with a minor so-called \"herald\" bleed, which is followed in hours, days, or weeks by catastrophic hemorrhage. This may be the result of a thrombus providing a tamponade effect on the small fistula, which eventually is dislodged when the fistula expands or is removed at the time of endoscopy (resulting in massive exsanguination directly from the aorta into the small intestine).[1,3,4]",
"Secondary AEFs are a late complication of aortic graft replacement used to treat aneurysms or aortoiliac occlusive disease.[3] Before 1960, the most common cause of AEFs was aortic aneurysm, followed by infectious aortitis (as mentioned above). Currently, erosion into the intestine by prosthetic vascular grafts has become a common cause, with an incidence of up to 4%.[4] This type of fistula may occur in two different forms:",
"A graft-enteric fistula (GEF) is a communication between the bowel and the disrupted graft/aorta anastomotic site. Most GEFs develop at the proximal aortic suture line, with the distal duodenum involved in approximately 75% of the cases.",
"A graft-enteric erosion (GEE) is a breakdown of the enteric wall overlying the graft, resulting in bathing of the graft by enteric contents and chronic graft infection without direct involvement of the suture line (less common).",
"A 20-year retrospective review of 443 patients with secondary AEFs extrapolated that the mean onset of symptoms after the procedure was 65 months (ranging from 3 days to 27 years) for GEF and 33 months (ranging from 45 days to 5 years) for GEE.[6]",
"AEF is difficult to diagnose preoperatively because no diagnostic modality with good sensitivity or specificity is available. Patients are usually evaluated by initial upper GI endoscopy, to rule out upper GI bleeding, with a resultant 25% detection rate. Endoscopy should include the entire duodenum because most AEFs occur at the level of the third and fourth portions of the duodenum. In the setting of upper GI bleeding and anemia, bleeding sources from peptic ulcer, postpolypectomy sites, diverticulosis, neoplasm, and angiodysplasia should also be considered in the differential diagnosis.",
"Clinicians should have a high index of suspicion in EGDs that show no pathologies except for a clot in the duodenum in patients with GI bleeding and a history of previous aortic aneurysm repair or aortobifemoral bypass grafting. Other diagnostic tools include CT scanning with intravenous contrast (61% detection rate) and arteriography (26% detection rate). Only one half of patients with AEF develop positive blood cultures, and one half of those positive cultures yield mixed gram-negative, gram-positive, and fungal organisms.[3,4,7]"
],
"date": "November 14, 2022",
"figures": [],
"markdown": "# Emergency Med Case Challenge: Hemorrhoids, Urinary and Blood Infections in a Woman With Rigors\n\n **Authors:** Vimon Seriburi, MD; Ann F. Fisher, MD \n **Date:** November 14, 2022\n\n ## Content\n\n Primary AEFs are caused by spontaneous erosion of the aorta into the GI tract. As many as 83% of these cases are associated with abdominal aortic atherosclerotic aneurysms, with a mean diameter of 6.2 cm. Other causes of AEFs include infection (often with tuberculosis or syphilis), cancer, radiation therapy, and foreign body ingestion. Evidence of GI bleeding is observed in 94% of cases, abdominal or back pain is seen in 46% of cases, and a pulsating mass is found in 17% of cases. The classic triad of GI hemorrhage, abdominal pain, and pulsating abdominal mass is present only in 11% of cases.\nClassically, AEF initially presents with a minor so-called \"herald\" bleed, which is followed in hours, days, or weeks by catastrophic hemorrhage. This may be the result of a thrombus providing a tamponade effect on the small fistula, which eventually is dislodged when the fistula expands or is removed at the time of endoscopy (resulting in massive exsanguination directly from the aorta into the small intestine).[1,3,4]\nSecondary AEFs are a late complication of aortic graft replacement used to treat aneurysms or aortoiliac occlusive disease.[3] Before 1960, the most common cause of AEFs was aortic aneurysm, followed by infectious aortitis (as mentioned above). Currently, erosion into the intestine by prosthetic vascular grafts has become a common cause, with an incidence of up to 4%.[4] This type of fistula may occur in two different forms:\nA graft-enteric fistula (GEF) is a communication between the bowel and the disrupted graft/aorta anastomotic site. Most GEFs develop at the proximal aortic suture line, with the distal duodenum involved in approximately 75% of the cases.\nA graft-enteric erosion (GEE) is a breakdown of the enteric wall overlying the graft, resulting in bathing of the graft by enteric contents and chronic graft infection without direct involvement of the suture line (less common).\nA 20-year retrospective review of 443 patients with secondary AEFs extrapolated that the mean onset of symptoms after the procedure was 65 months (ranging from 3 days to 27 years) for GEF and 33 months (ranging from 45 days to 5 years) for GEE.[6]\nAEF is difficult to diagnose preoperatively because no diagnostic modality with good sensitivity or specificity is available. Patients are usually evaluated by initial upper GI endoscopy, to rule out upper GI bleeding, with a resultant 25% detection rate. Endoscopy should include the entire duodenum because most AEFs occur at the level of the third and fourth portions of the duodenum. In the setting of upper GI bleeding and anemia, bleeding sources from peptic ulcer, postpolypectomy sites, diverticulosis, neoplasm, and angiodysplasia should also be considered in the differential diagnosis.\nClinicians should have a high index of suspicion in EGDs that show no pathologies except for a clot in the duodenum in patients with GI bleeding and a history of previous aortic aneurysm repair or aortobifemoral bypass grafting. Other diagnostic tools include CT scanning with intravenous contrast (61% detection rate) and arteriography (26% detection rate). Only one half of patients with AEF develop positive blood cultures, and one half of those positive cultures yield mixed gram-negative, gram-positive, and fungal organisms.[3,4,7]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Emergency Med Case Challenge: Hemorrhoids, Urinary and Blood Infections in a Woman With Rigors"
},
{
"authors": "Vimon Seriburi, MD; Ann F. Fisher, MD",
"content": [
"Once the diagnosis of AEF is confirmed, removal of the infected graft, repair of the fistula, and revascularization are imperative. A herald hemorrhage should be viewed as an opportunity for prompt surgical intervention, because only about 50% of patients will survive the first 24 hours after the initial bleeding.",
"Open surgical repair of an AEF is technically demanding, and it is often associated with high morbidity and mortality. Options for revascularization include extra-anatomical bypass with an axillobifemoral bypass, neoaortic replacement using the deep veins of the lower extremity, and aortic replacement with either cadaveric human allografts or antibiotic-soaked prosthetic grafts. Evolving strategies for the treatment of aortoenteric fistulas through endovascular methods should be used only in the most unstable patients, and these methods should only be viewed as temporizing measures to more definitive open surgical repair. The optimal surveillance strategy after repair of an AEF has not been established because of the difficulty in tracking long-term follow-ups.",
"Data regarding the duration and choice of antibiotic therapy are also limited. So far, recommendations for treatment are largely based on experience with bacterial endocarditis. In general, antibiotics should be given for 4-6 weeks postoperatively in patients with positive blood cultures.[2,3,8,9]",
"In this case, once the patient's aortoduodenal fistula was confirmed, she underwent emergent laparotomy for repair. An opening was found in the retrobulbar region of the duodenum, which was adherent to the aorta. Gross contamination of the graft with duodenal contents was noted. The infected aortobifemoral bypass was removed, and a new rifampin-soaked thermoplastic resin bifurcated graft was placed. The aortoduodenal fistula was simultaneously closed.",
"Multiple cultures of the old graft grew Candida albicans and C glabrata. The patient completed a 6-week course of piperacillin/tazobactam for the Streptococcus bacteremia and caspofungin for the Candida fungemia. Her hospital course was complicated by multiple nosocomial infections; however, her anemia eventually improved, and she was discharged to a short-term rehabilitation facility 2 months after surgery."
],
"date": "November 14, 2022",
"figures": [],
"markdown": "# Emergency Med Case Challenge: Hemorrhoids, Urinary and Blood Infections in a Woman With Rigors\n\n **Authors:** Vimon Seriburi, MD; Ann F. Fisher, MD \n **Date:** November 14, 2022\n\n ## Content\n\n Once the diagnosis of AEF is confirmed, removal of the infected graft, repair of the fistula, and revascularization are imperative. A herald hemorrhage should be viewed as an opportunity for prompt surgical intervention, because only about 50% of patients will survive the first 24 hours after the initial bleeding.\nOpen surgical repair of an AEF is technically demanding, and it is often associated with high morbidity and mortality. Options for revascularization include extra-anatomical bypass with an axillobifemoral bypass, neoaortic replacement using the deep veins of the lower extremity, and aortic replacement with either cadaveric human allografts or antibiotic-soaked prosthetic grafts. Evolving strategies for the treatment of aortoenteric fistulas through endovascular methods should be used only in the most unstable patients, and these methods should only be viewed as temporizing measures to more definitive open surgical repair. The optimal surveillance strategy after repair of an AEF has not been established because of the difficulty in tracking long-term follow-ups.\nData regarding the duration and choice of antibiotic therapy are also limited. So far, recommendations for treatment are largely based on experience with bacterial endocarditis. In general, antibiotics should be given for 4-6 weeks postoperatively in patients with positive blood cultures.[2,3,8,9]\nIn this case, once the patient's aortoduodenal fistula was confirmed, she underwent emergent laparotomy for repair. An opening was found in the retrobulbar region of the duodenum, which was adherent to the aorta. Gross contamination of the graft with duodenal contents was noted. The infected aortobifemoral bypass was removed, and a new rifampin-soaked thermoplastic resin bifurcated graft was placed. The aortoduodenal fistula was simultaneously closed.\nMultiple cultures of the old graft grew Candida albicans and C glabrata. The patient completed a 6-week course of piperacillin/tazobactam for the Streptococcus bacteremia and caspofungin for the Candida fungemia. Her hospital course was complicated by multiple nosocomial infections; however, her anemia eventually improved, and she was discharged to a short-term rehabilitation facility 2 months after surgery.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136586,
"choiceText": "2-4 weeks",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136588,
"choiceText": "4-6 weeks",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136590,
"choiceText": "6-8 weeks",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136592,
"choiceText": "8-10 weeks",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136594,
"choiceText": "10-12 weeks\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Data regarding the duration and choice of antibiotic therapy are limited. So far, recommendations for treatment are largely based on experience with bacterial endocarditis. In general, antibiotics should be given for 4-6 weeks postoperatively in patients with positive blood cultures.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360615,
"questionText": "What is the recommended duration of antibiotic therapy for a patient with AEF after the removal of an infected bypass graft?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136596,
"choiceText": "Abdominal aortic aneurysm",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136598,
"choiceText": "Syphilitic aortitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136600,
"choiceText": "Tuberculous aortitis\r\n",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136602,
"choiceText": "Peptic ulcer disease",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136604,
"choiceText": "Radiation therapy",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Primary AEFs are caused by spontaneous erosion of the aorta into the GI tract. As many as 83% of these cases are associated with abdominal aortic atherosclerotic aneurysms, with a mean diameter of 6.2 cm. Other causes of AEFs include infection (often with tuberculosis or syphilis), cancer, radiation therapy, and foreign body ingestion. ",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360617,
"questionText": "Which etiology of primary AEF formation is most common?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Emergency Med Case Challenge: Hemorrhoids, Urinary and Blood Infections in a Woman With Rigors"
},
{
"authors": "Vimon Seriburi, MD; Ann F. Fisher, MD",
"content": [],
"date": "November 14, 2022",
"figures": [],
"markdown": "# Emergency Med Case Challenge: Hemorrhoids, Urinary and Blood Infections in a Woman With Rigors\n\n **Authors:** Vimon Seriburi, MD; Ann F. Fisher, MD \n **Date:** November 14, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136586,
"choiceText": "2-4 weeks",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136588,
"choiceText": "4-6 weeks",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136590,
"choiceText": "6-8 weeks",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136592,
"choiceText": "8-10 weeks",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136594,
"choiceText": "10-12 weeks\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Data regarding the duration and choice of antibiotic therapy are limited. So far, recommendations for treatment are largely based on experience with bacterial endocarditis. In general, antibiotics should be given for 4-6 weeks postoperatively in patients with positive blood cultures.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360615,
"questionText": "What is the recommended duration of antibiotic therapy for a patient with AEF after the removal of an infected bypass graft?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136596,
"choiceText": "Abdominal aortic aneurysm",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136598,
"choiceText": "Syphilitic aortitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136600,
"choiceText": "Tuberculous aortitis\r\n",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136602,
"choiceText": "Peptic ulcer disease",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136604,
"choiceText": "Radiation therapy",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Primary AEFs are caused by spontaneous erosion of the aorta into the GI tract. As many as 83% of these cases are associated with abdominal aortic atherosclerotic aneurysms, with a mean diameter of 6.2 cm. Other causes of AEFs include infection (often with tuberculosis or syphilis), cancer, radiation therapy, and foreign body ingestion. ",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360617,
"questionText": "Which etiology of primary AEF formation is most common?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Emergency Med Case Challenge: Hemorrhoids, Urinary and Blood Infections in a Woman With Rigors"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136578,
"choiceText": "Diverticulitis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136580,
"choiceText": "Aortoenteric fistula",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136582,
"choiceText": "Urinary tract infection",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136584,
"choiceText": "Bacterial endocarditis\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360613,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136586,
"choiceText": "2-4 weeks",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136588,
"choiceText": "4-6 weeks",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136590,
"choiceText": "6-8 weeks",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136592,
"choiceText": "8-10 weeks",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136594,
"choiceText": "10-12 weeks\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Data regarding the duration and choice of antibiotic therapy are limited. So far, recommendations for treatment are largely based on experience with bacterial endocarditis. In general, antibiotics should be given for 4-6 weeks postoperatively in patients with positive blood cultures.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360615,
"questionText": "What is the recommended duration of antibiotic therapy for a patient with AEF after the removal of an infected bypass graft?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136596,
"choiceText": "Abdominal aortic aneurysm",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136598,
"choiceText": "Syphilitic aortitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136600,
"choiceText": "Tuberculous aortitis\r\n",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136602,
"choiceText": "Peptic ulcer disease",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136604,
"choiceText": "Radiation therapy",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Primary AEFs are caused by spontaneous erosion of the aorta into the GI tract. As many as 83% of these cases are associated with abdominal aortic atherosclerotic aneurysms, with a mean diameter of 6.2 cm. Other causes of AEFs include infection (often with tuberculosis or syphilis), cancer, radiation therapy, and foreign body ingestion. ",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360617,
"questionText": "Which etiology of primary AEF formation is most common?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
983148 | /viewarticle/983148 | [
{
"authors": "Kristine M. Lohr, MD, MS; Muhammad Sohail Khan, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"Six months ago, a 58-year-old woman presented with a 1-year history of bilateral sternoclavicular joint swelling and stiffness. She reported mild pain and stiffness of her shoulders and upper back as well as 1-2 hours of morning stiffness that lessened by the end of the day. Ibuprofen provided partial relief. Working out also helped alleviate her symptoms; however, the affected joints became sorer. Although she noted dryness in her eyes upon waking up in the morning, she did not use artificial tears regularly.",
"She presents for follow-up 6 months later. The bilateral sternoclavicular joint pain and swelling resolved completely with the use of nonsteroidal anti-inflammatory drugs (NSAIDs). However, she reports worsening of her bilateral shoulder pain, with restriction of range of motion. She cannot abduct her left shoulder beyond 30-40 degrees. The patient had no previous restriction of range of motion. She also has significant bilateral knee pain and stiffness, especially in the morning, as well as morning stiffness in her lower back and sacroiliac joints that increases by evening. She notes partial relief with ibuprofen 200 mg twice daily and acetaminophen once daily.",
"Her family history is negative for any significant autoimmune diseases. She has no family history of psoriasis. She does not smoke tobacco, drink alcohol, or use illicit drugs. She has no history of prior surgeries. The results of a recent colonoscopy were normal. The patient was previously healthy before her current symptoms developed, and she has no significant past medical history. A detailed review of system is negative for any history of seizures, strokes, Raynaud phenomenon, dry mouth, mouth sores, nausea, vomiting, breathing problems, or heart disorders."
],
"date": "November 10, 2022",
"figures": [],
"markdown": "# Morning Stiffness, Dry Eyes, Back Pain in a Fit 58-Year-Old\n\n **Authors:** Kristine M. Lohr, MD, MS; Muhammad Sohail Khan, MD \n **Date:** November 10, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nSix months ago, a 58-year-old woman presented with a 1-year history of bilateral sternoclavicular joint swelling and stiffness. She reported mild pain and stiffness of her shoulders and upper back as well as 1-2 hours of morning stiffness that lessened by the end of the day. Ibuprofen provided partial relief. Working out also helped alleviate her symptoms; however, the affected joints became sorer. Although she noted dryness in her eyes upon waking up in the morning, she did not use artificial tears regularly.\nShe presents for follow-up 6 months later. The bilateral sternoclavicular joint pain and swelling resolved completely with the use of nonsteroidal anti-inflammatory drugs (NSAIDs). However, she reports worsening of her bilateral shoulder pain, with restriction of range of motion. She cannot abduct her left shoulder beyond 30-40 degrees. The patient had no previous restriction of range of motion. She also has significant bilateral knee pain and stiffness, especially in the morning, as well as morning stiffness in her lower back and sacroiliac joints that increases by evening. She notes partial relief with ibuprofen 200 mg twice daily and acetaminophen once daily.\nHer family history is negative for any significant autoimmune diseases. She has no family history of psoriasis. She does not smoke tobacco, drink alcohol, or use illicit drugs. She has no history of prior surgeries. The results of a recent colonoscopy were normal. The patient was previously healthy before her current symptoms developed, and she has no significant past medical history. A detailed review of system is negative for any history of seizures, strokes, Raynaud phenomenon, dry mouth, mouth sores, nausea, vomiting, breathing problems, or heart disorders.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Morning Stiffness, Dry Eyes, Back Pain in a Fit 58-Year-Old"
},
{
"authors": "Kristine M. Lohr, MD, MS; Muhammad Sohail Khan, MD",
"content": [
"At the current office visit, the patient's vital signs are normal. Six months ago, bilateral tender and hypertrophied bony sternoclavicular joints were noted. The remainder of the physical examination was otherwise unremarkable. By the time of the current office visit, the bilateral sternoclavicular joint swelling has resolved. A new finding is that shoulder abduction is limited to 30-40 degrees. Results of the occiput-to-wall distance test and the chest expansion and Schober tests are normal at the current visit and were normal on the prior visit.",
"Laboratory tests at the first office visit revealed:",
"Antinuclear antibody (ANA) level: Positive ANA of 1:160 with a nucleolar pattern (reference range, negative)",
"Serum interferon-gamma release assay (QuantiFERON): Negative (reference range, negative)",
"Hepatitis panel: Negative (reference range, negative)",
"C-reactive protein (CRP) level: 13.9 mg/L (reference range, < 10.0 mg/L)",
"Rheumatoid factor level: Negative (reference range, negative)",
"Anti–cyclic citrullinated peptide (anti-CCP) antibody level: Negative (reference range, negative)",
"Erythrocyte sedimentation rate (ESR): 84 mm/h (reference range, 1-20 mm/h for women)",
"At the initial office visit, a radiograph of the sacroiliac joint was unremarkable, without any erosion (Figure 1). A radiograph of the left shoulder showed mild glenohumeral and acromioclavicular joint osteoarthrosis (Figure 2). A radiograph of the knees revealed mild patellofemoral compartment osteoarthrosis bilaterally, with small to moderate suprapatellar effusions.",
"Figure 1.",
"Figure 2.",
"Laboratory studies at the current office visit show:",
"Human leukocyte antigen B27 (HLA B27) level: Negative (reference range, negative)",
"Anti-DNA antibody, anti-Smith antibody immunoglobulin (Ig)–G, anti-SSA 52 and 60 IgG, and anti-SSB IgG levels: Negative (reference range, negative)",
"C3 complement level: Normal (reference range, 80-160 mg/dL)",
"C4 complement level: Normal (reference range, 15-45 mg/dL)",
"A synovial biopsy from the right sternoclavicular joint reveals benign cartilage with cystic degeneration but no infection or inflammation.",
"An MRI shows grossly symmetric periarticular edema about the bilateral sacroiliac joints, most pronounced on the inferior iliac sides (Figure 3). Associated mild erosion is noted along the iliac side. Overall, the findings are most suggestive of active sacroiliitis. No ankylosis of the sacroiliac joint is noted.",
"Figure 3.",
"An MRI of the left shoulder reveals extensive supraspinatus and infraspinatus bursal-sided fraying, with articular-sided low-grade fraying and/or tearing of the supraspinatus and infraspinatus proximal to the footprint. In addition, multifocal intrasubstance tearing of the infraspinatus footprint is noted. A moderate amount of fluid is present in the subacromial-subdeltoid bursa. The scan also shows moderate to severe acromioclavicular joint osteoarthrosis, with a laterally downsloping acromion, and mild glenohumeral osteoarthrosis. Labral degeneration, with extensive maceration and fraying of the mid-anterior to anteroinferior labrum, is present."
],
"date": "November 10, 2022",
"figures": [],
"markdown": "# Morning Stiffness, Dry Eyes, Back Pain in a Fit 58-Year-Old\n\n **Authors:** Kristine M. Lohr, MD, MS; Muhammad Sohail Khan, MD \n **Date:** November 10, 2022\n\n ## Content\n\n At the current office visit, the patient's vital signs are normal. Six months ago, bilateral tender and hypertrophied bony sternoclavicular joints were noted. The remainder of the physical examination was otherwise unremarkable. By the time of the current office visit, the bilateral sternoclavicular joint swelling has resolved. A new finding is that shoulder abduction is limited to 30-40 degrees. Results of the occiput-to-wall distance test and the chest expansion and Schober tests are normal at the current visit and were normal on the prior visit.\nLaboratory tests at the first office visit revealed:\nAntinuclear antibody (ANA) level: Positive ANA of 1:160 with a nucleolar pattern (reference range, negative)\nSerum interferon-gamma release assay (QuantiFERON): Negative (reference range, negative)\nHepatitis panel: Negative (reference range, negative)\nC-reactive protein (CRP) level: 13.9 mg/L (reference range, < 10.0 mg/L)\nRheumatoid factor level: Negative (reference range, negative)\nAnti–cyclic citrullinated peptide (anti-CCP) antibody level: Negative (reference range, negative)\nErythrocyte sedimentation rate (ESR): 84 mm/h (reference range, 1-20 mm/h for women)\nAt the initial office visit, a radiograph of the sacroiliac joint was unremarkable, without any erosion (Figure 1). A radiograph of the left shoulder showed mild glenohumeral and acromioclavicular joint osteoarthrosis (Figure 2). A radiograph of the knees revealed mild patellofemoral compartment osteoarthrosis bilaterally, with small to moderate suprapatellar effusions.\nFigure 1.\nFigure 2.\nLaboratory studies at the current office visit show:\nHuman leukocyte antigen B27 (HLA B27) level: Negative (reference range, negative)\nAnti-DNA antibody, anti-Smith antibody immunoglobulin (Ig)–G, anti-SSA 52 and 60 IgG, and anti-SSB IgG levels: Negative (reference range, negative)\nC3 complement level: Normal (reference range, 80-160 mg/dL)\nC4 complement level: Normal (reference range, 15-45 mg/dL)\nA synovial biopsy from the right sternoclavicular joint reveals benign cartilage with cystic degeneration but no infection or inflammation.\nAn MRI shows grossly symmetric periarticular edema about the bilateral sacroiliac joints, most pronounced on the inferior iliac sides (Figure 3). Associated mild erosion is noted along the iliac side. Overall, the findings are most suggestive of active sacroiliitis. No ankylosis of the sacroiliac joint is noted.\nFigure 3.\nAn MRI of the left shoulder reveals extensive supraspinatus and infraspinatus bursal-sided fraying, with articular-sided low-grade fraying and/or tearing of the supraspinatus and infraspinatus proximal to the footprint. In addition, multifocal intrasubstance tearing of the infraspinatus footprint is noted. A moderate amount of fluid is present in the subacromial-subdeltoid bursa. The scan also shows moderate to severe acromioclavicular joint osteoarthrosis, with a laterally downsloping acromion, and mild glenohumeral osteoarthrosis. Labral degeneration, with extensive maceration and fraying of the mid-anterior to anteroinferior labrum, is present.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1737896,
"choiceText": "Reactive arthritis ",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737897,
"choiceText": "Ankylosing spondylitis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737898,
"choiceText": "Psoriatic arthritis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737899,
"choiceText": "Spondylitis associated with inflammatory bowel disease",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737900,
"choiceText": "Synovitis, acne, pustulosis, hyperostosis, osteitis (SAPHO) syndrome",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 561247,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Morning Stiffness, Dry Eyes, Back Pain in a Fit 58-Year-Old"
},
{
"authors": "Kristine M. Lohr, MD, MS; Muhammad Sohail Khan, MD",
"content": [
"The history of the present illness and the physical examination show that the patient has bilaterally tender sternoclavicular joints, along with bony hypertrophy, which is obvious to the naked eye. At the first office visit, 6 months earlier, she also had mild bilateral acromioclavicular joint tenderness. An initial trial of NSAIDs resulted in complete resolution of the sternoclavicular joint swelling. However, the patient developed worsening symptoms of shoulder pain and restriction of range of motion, and MRI findings suggested sacroiliitis. She also had involvement of the peripheral joints, including the left shoulder. The elevated CRP and ESR levels indicate the presence of an inflammatory disease.",
"The dramatic improvement in this patient's symptoms and joint swelling with the use of NSAIDs makes ankylosing spondylitis the most probable diagnosis. In addition, the MRI of the sacroiliac joints revealed findings suggestive of sacroiliitis, which support this diagnosis. However, this patient's presentation was atypical from the standpoint of the usual progression of ankylosing spondylitis. Typically, the progression takes 4-9 years from the onset of inflammatory back pain until the development of definite radiographic sacroiliitis.",
"Axial spondyloarthropathy is a chronic, systemic inflammatory disease that affects the sacroiliac joints, spine, and occasionally peripheral joints. Sacroiliitis that is evident on plain radiographs is characteristic of ankylosing spondylitis, which is the more advanced presentation of the disease. Patients who have axial spondyloarthropathy without clear sacroiliitis on plain radiography usually have inflammation detected on MRI. These patients are said to have a \"nonradiographic\" axial spondyloarthropathy, which may or may not progress over time to definite radiographic sacroiliitis. The Assessment of SpondyloArthritis International Society (ASAS) classification criteria were developed for patients with back pain for more than 3 months and age of onset younger than 45 years in order to identify early disease (ie, no clear sacroiliitis on radiographs). These criteria have a sensitivity of 83% and a specificity of 84% for a patient with axial spondyloarthropathy.",
"The clinical manifestations of axial spondyloarthropathy usually begin in late adolescence or early adulthood; onset after age 45 years is highly uncommon. It occurs slightly more often in men than in women (2:1). Patients with axial spondyloarthropathy usually present with low back pain and prolonged morning (and often nocturnal) stiffness, which improves with movement and exercise. Buttock pain may initially alternate from side to side before becoming persistent. Physical examination reveals decreased spinal mobility and sometimes enthesitis, scleral injection/photophobia (uveitis/iritis) and, in advanced disease, loss of lordosis, exaggerated kyphosis, and reduced chest expansion due to costovertebral joint involvement. Axial spondyloarthropathy is often more difficult to diagnose early in women as a result of less pronounced clinical features, atypical presentations (peripheral arthritis, cervical spine disease), and possibly slower development of radiographic changes.",
"Approximately 30% of patients with axial spondyloarthropathy develop a peripheral arthritis. The hips and shoulders (girdle joints) are involved most commonly. Of note, hip involvement in axial spondyloarthropathy is associated with a poor prognosis. Rarely, arthritis of the sternoclavicular, temporomandibular, cricoarytenoid joints, or the symphysis pubis occurs. Involvement of the thoracic costovertebral, sternocostal, and manubriosternal joints may cause chest pain that is worsened by coughing or sneezing."
],
"date": "November 10, 2022",
"figures": [],
"markdown": "# Morning Stiffness, Dry Eyes, Back Pain in a Fit 58-Year-Old\n\n **Authors:** Kristine M. Lohr, MD, MS; Muhammad Sohail Khan, MD \n **Date:** November 10, 2022\n\n ## Content\n\n The history of the present illness and the physical examination show that the patient has bilaterally tender sternoclavicular joints, along with bony hypertrophy, which is obvious to the naked eye. At the first office visit, 6 months earlier, she also had mild bilateral acromioclavicular joint tenderness. An initial trial of NSAIDs resulted in complete resolution of the sternoclavicular joint swelling. However, the patient developed worsening symptoms of shoulder pain and restriction of range of motion, and MRI findings suggested sacroiliitis. She also had involvement of the peripheral joints, including the left shoulder. The elevated CRP and ESR levels indicate the presence of an inflammatory disease.\nThe dramatic improvement in this patient's symptoms and joint swelling with the use of NSAIDs makes ankylosing spondylitis the most probable diagnosis. In addition, the MRI of the sacroiliac joints revealed findings suggestive of sacroiliitis, which support this diagnosis. However, this patient's presentation was atypical from the standpoint of the usual progression of ankylosing spondylitis. Typically, the progression takes 4-9 years from the onset of inflammatory back pain until the development of definite radiographic sacroiliitis.\nAxial spondyloarthropathy is a chronic, systemic inflammatory disease that affects the sacroiliac joints, spine, and occasionally peripheral joints. Sacroiliitis that is evident on plain radiographs is characteristic of ankylosing spondylitis, which is the more advanced presentation of the disease. Patients who have axial spondyloarthropathy without clear sacroiliitis on plain radiography usually have inflammation detected on MRI. These patients are said to have a \"nonradiographic\" axial spondyloarthropathy, which may or may not progress over time to definite radiographic sacroiliitis. The Assessment of SpondyloArthritis International Society (ASAS) classification criteria were developed for patients with back pain for more than 3 months and age of onset younger than 45 years in order to identify early disease (ie, no clear sacroiliitis on radiographs). These criteria have a sensitivity of 83% and a specificity of 84% for a patient with axial spondyloarthropathy.\nThe clinical manifestations of axial spondyloarthropathy usually begin in late adolescence or early adulthood; onset after age 45 years is highly uncommon. It occurs slightly more often in men than in women (2:1). Patients with axial spondyloarthropathy usually present with low back pain and prolonged morning (and often nocturnal) stiffness, which improves with movement and exercise. Buttock pain may initially alternate from side to side before becoming persistent. Physical examination reveals decreased spinal mobility and sometimes enthesitis, scleral injection/photophobia (uveitis/iritis) and, in advanced disease, loss of lordosis, exaggerated kyphosis, and reduced chest expansion due to costovertebral joint involvement. Axial spondyloarthropathy is often more difficult to diagnose early in women as a result of less pronounced clinical features, atypical presentations (peripheral arthritis, cervical spine disease), and possibly slower development of radiographic changes.\nApproximately 30% of patients with axial spondyloarthropathy develop a peripheral arthritis. The hips and shoulders (girdle joints) are involved most commonly. Of note, hip involvement in axial spondyloarthropathy is associated with a poor prognosis. Rarely, arthritis of the sternoclavicular, temporomandibular, cricoarytenoid joints, or the symphysis pubis occurs. Involvement of the thoracic costovertebral, sternocostal, and manubriosternal joints may cause chest pain that is worsened by coughing or sneezing.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1737896,
"choiceText": "Reactive arthritis ",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737897,
"choiceText": "Ankylosing spondylitis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737898,
"choiceText": "Psoriatic arthritis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737899,
"choiceText": "Spondylitis associated with inflammatory bowel disease",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737900,
"choiceText": "Synovitis, acne, pustulosis, hyperostosis, osteitis (SAPHO) syndrome",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 561247,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Morning Stiffness, Dry Eyes, Back Pain in a Fit 58-Year-Old"
},
{
"authors": "Kristine M. Lohr, MD, MS; Muhammad Sohail Khan, MD",
"content": [
"Extra-articular/extraskeletal manifestations of axial spondyloarthropathy/ankylosing spondylitis include:[1]",
"Cardiac: Aortic insufficiency (2%-6%), ascending aortitis, and other manifestations, such as conduction abnormalities (3%-5%), diastolic dysfunction, pericarditis, and ischemic heart disease (30%)",
"Neurologic: Atlantoaxial (C1-2) subluxation (2%), cauda equina syndrome from spinal arachnoiditis, traumatic spinal fractures with myelopathy (C5-6, C6-7 most commonly), ossification of the posterior longitudinal ligament with spinal stenosis",
"Kidney: Secondary amyloidosis, IgA nephropathy (5%), chronic prostatitis",
"Skin: Psoriasis (10%) and, to a lesser extent, erythema nodosum, keratoderma blennorrhagicum, and pyoderma gangrenosum",
"Pulmonary: Upper lobe fibrosis, restrictive changes",
"Ocular: Acute anterior uveitis (20%-30%)",
"Discitis or spondylodiscitis (Andersson lesions)",
"In addition, 30%-60% of patients have asymptomatic microscopic colitis or Crohn's disease–like lesions in their terminal ileum and colon, although overt inflammatory bowel disease occurs in only 7% of patients with axial spondyloarthropathy. Patients with peripheral arthritis are more likely to have colitis lesions.",
"In the differential diagnosis of axial spondyloarthropathy/ankylosing spondylitis, other conditions to consider include:",
"Psoriatic arthritis",
"Reactive arthritis",
"Arthritis related to inflammatory bowel disease",
"SAPHO syndrome",
"The patient in this case did not have any personal history or physical examination findings of psoriasis. Her family history was also negative for psoriasis.",
"The onset of reactive arthritis is usually acute. Patients typically present with an asymmetric oligoarthritis, usually 1-4 weeks after the inciting infection. In at least half of patients, all symptoms resolve in less than 6 months; in most patients, symptoms resolve within 1 year. It would be atypical for reactive arthritis to persist and worsen over the course of 18 months, as this patient's symptoms did.",
"The patient does not have any history suggestive of inflammatory bowel disease. Moreover, the results of a recent colonoscopy were normal. Finally, she does not have typical stigmata of SAPHO syndrome: synovitis, acne, pustulosis, hyperostosis, or osteitis.",
"The prevalence of spondyloarthritis (SpA) reported worldwide widely varies, depending on the genetic background in the country or region under study and, to a certain extent, on the criteria used by the surveyors. The prevalence rate for SpA is about 0.9%-1.7%; peripheral SpA accounts for approximately 25% of the total.[1] Reactive arthritis is the least common form of SpA.",
"The major clinical features that differentiate SpA from other forms of arthritis are the distribution and type of musculoskeletal manifestations and certain extra-articular features. Patients with axial SpA characteristically have chronic low back pain. Patients with peripheral SpA can exhibit peripheral musculoskeletal features, which include dactylitis (sausage digits), enthesitis (heel pain and/or swelling), and peripheral arthritis (as the patient in this case had). Patients with peripheral SpA may experience one or more of these peripheral manifestations concurrently or in the past. Patients can also have both axial and peripheral manifestations. Certain extramusculoskeletal manifestations can be associated with the musculoskeletal features seen in SpA, including uveitis, psoriasis, features of inflammatory bowel diseases, and others. Reactive arthritis is sometimes associated with genital lesions. Atypical presentations can include radiographically negative SpA or rapid progression of the disease (as occurred in the patient in this case).",
"Three physical examination tests are used to assess the severity of sacroiliac and spinal joint involvement in axial spondyloarthropathy:",
"Occiput-to-wall test",
"Chest expansion test",
"Schober test (modified)",
"The occiput-to-wall test assesses the exaggerated kyphosis in more advanced disease. Normally, with the heels and scapulae touching the wall, the occiput should also touch the wall. The distance from the occiput to the wall represents the magnitude of thoracic/cervical involvement. The tragus-to-wall test could also be used.",
"The chest expansion test detects limited chest mobility. It is measured at the xiphisternum. Normal chest expansion varies by age and possibly sex, although it is usually abnormal if < 2.5 cm and normal if ≥ 5 cm.",
"The Schober test (modified) detects limitation of forward flexion of the lumbar spine. Place a mark at the level of the posterior superior iliac spine (dimples of Venus) and another 10 cm above in the midline. With the patient in maximal forward spinal flexion with straight knees, the distance measured between the marks should increase from 10 cm to ≥ 14.5 cm in a young adult man. Other spinal mobility tests will show diminution in lateral flexion and spinal rotation, illustrating that the patient has a global loss of spinal mobility. Lateral flexion is measured by having the patient stand with heels and back against the wall and hands flat on the lateral thighs. The patient bends sideways toward the floor without bending the knees or lifting heels. The difference in the distance of the middle finger between neutral position and maximal lateral flexion is recorded and averaged for the left and right sides.",
"Imaging studies that are usually helpful in the diagnosis of spondyloarthropathies include axial radiographs, radiographs of peripheral joints, MRI of the sacroiliac joints, and MRI of the spine."
],
"date": "November 10, 2022",
"figures": [],
"markdown": "# Morning Stiffness, Dry Eyes, Back Pain in a Fit 58-Year-Old\n\n **Authors:** Kristine M. Lohr, MD, MS; Muhammad Sohail Khan, MD \n **Date:** November 10, 2022\n\n ## Content\n\n Extra-articular/extraskeletal manifestations of axial spondyloarthropathy/ankylosing spondylitis include:[1]\nCardiac: Aortic insufficiency (2%-6%), ascending aortitis, and other manifestations, such as conduction abnormalities (3%-5%), diastolic dysfunction, pericarditis, and ischemic heart disease (30%)\nNeurologic: Atlantoaxial (C1-2) subluxation (2%), cauda equina syndrome from spinal arachnoiditis, traumatic spinal fractures with myelopathy (C5-6, C6-7 most commonly), ossification of the posterior longitudinal ligament with spinal stenosis\nKidney: Secondary amyloidosis, IgA nephropathy (5%), chronic prostatitis\nSkin: Psoriasis (10%) and, to a lesser extent, erythema nodosum, keratoderma blennorrhagicum, and pyoderma gangrenosum\nPulmonary: Upper lobe fibrosis, restrictive changes\nOcular: Acute anterior uveitis (20%-30%)\nDiscitis or spondylodiscitis (Andersson lesions)\nIn addition, 30%-60% of patients have asymptomatic microscopic colitis or Crohn's disease–like lesions in their terminal ileum and colon, although overt inflammatory bowel disease occurs in only 7% of patients with axial spondyloarthropathy. Patients with peripheral arthritis are more likely to have colitis lesions.\nIn the differential diagnosis of axial spondyloarthropathy/ankylosing spondylitis, other conditions to consider include:\nPsoriatic arthritis\nReactive arthritis\nArthritis related to inflammatory bowel disease\nSAPHO syndrome\nThe patient in this case did not have any personal history or physical examination findings of psoriasis. Her family history was also negative for psoriasis.\nThe onset of reactive arthritis is usually acute. Patients typically present with an asymmetric oligoarthritis, usually 1-4 weeks after the inciting infection. In at least half of patients, all symptoms resolve in less than 6 months; in most patients, symptoms resolve within 1 year. It would be atypical for reactive arthritis to persist and worsen over the course of 18 months, as this patient's symptoms did.\nThe patient does not have any history suggestive of inflammatory bowel disease. Moreover, the results of a recent colonoscopy were normal. Finally, she does not have typical stigmata of SAPHO syndrome: synovitis, acne, pustulosis, hyperostosis, or osteitis.\nThe prevalence of spondyloarthritis (SpA) reported worldwide widely varies, depending on the genetic background in the country or region under study and, to a certain extent, on the criteria used by the surveyors. The prevalence rate for SpA is about 0.9%-1.7%; peripheral SpA accounts for approximately 25% of the total.[1] Reactive arthritis is the least common form of SpA.\nThe major clinical features that differentiate SpA from other forms of arthritis are the distribution and type of musculoskeletal manifestations and certain extra-articular features. Patients with axial SpA characteristically have chronic low back pain. Patients with peripheral SpA can exhibit peripheral musculoskeletal features, which include dactylitis (sausage digits), enthesitis (heel pain and/or swelling), and peripheral arthritis (as the patient in this case had). Patients with peripheral SpA may experience one or more of these peripheral manifestations concurrently or in the past. Patients can also have both axial and peripheral manifestations. Certain extramusculoskeletal manifestations can be associated with the musculoskeletal features seen in SpA, including uveitis, psoriasis, features of inflammatory bowel diseases, and others. Reactive arthritis is sometimes associated with genital lesions. Atypical presentations can include radiographically negative SpA or rapid progression of the disease (as occurred in the patient in this case).\nThree physical examination tests are used to assess the severity of sacroiliac and spinal joint involvement in axial spondyloarthropathy:\nOcciput-to-wall test\nChest expansion test\nSchober test (modified)\nThe occiput-to-wall test assesses the exaggerated kyphosis in more advanced disease. Normally, with the heels and scapulae touching the wall, the occiput should also touch the wall. The distance from the occiput to the wall represents the magnitude of thoracic/cervical involvement. The tragus-to-wall test could also be used.\nThe chest expansion test detects limited chest mobility. It is measured at the xiphisternum. Normal chest expansion varies by age and possibly sex, although it is usually abnormal if < 2.5 cm and normal if ≥ 5 cm.\nThe Schober test (modified) detects limitation of forward flexion of the lumbar spine. Place a mark at the level of the posterior superior iliac spine (dimples of Venus) and another 10 cm above in the midline. With the patient in maximal forward spinal flexion with straight knees, the distance measured between the marks should increase from 10 cm to ≥ 14.5 cm in a young adult man. Other spinal mobility tests will show diminution in lateral flexion and spinal rotation, illustrating that the patient has a global loss of spinal mobility. Lateral flexion is measured by having the patient stand with heels and back against the wall and hands flat on the lateral thighs. The patient bends sideways toward the floor without bending the knees or lifting heels. The difference in the distance of the middle finger between neutral position and maximal lateral flexion is recorded and averaged for the left and right sides.\nImaging studies that are usually helpful in the diagnosis of spondyloarthropathies include axial radiographs, radiographs of peripheral joints, MRI of the sacroiliac joints, and MRI of the spine.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Morning Stiffness, Dry Eyes, Back Pain in a Fit 58-Year-Old"
},
{
"authors": "Kristine M. Lohr, MD, MS; Muhammad Sohail Khan, MD",
"content": [
"An anteroposterior projection of the pelvis (AP pelvis) is often sufficient to evaluate the inferior aspects of the sacroiliac joints. The Ferguson view (AP with the tube angled 25-40 degrees cephalad) counteracts the overlap of the sacrum with the ilium, enabling a full view of the sacroiliac joint. This view is recognized because the symphysis pubis overlaps the sacrum.",
"MRI of the pelvis with T1 sequences is used for evaluation of ankylosis, erosions, backfill, and fatty metaplasia, and short T1 inversion recovery sequences are used for evaluation of osteitis/inflammation. Semicoronal views are included to visualize the sacroiliac joints along their full length. Pelvis MRI identifies 95% of patients with axial SpA/ankylosing spondylitis. Only 5% of patients require lumbar spine MRI owing to normal pelvis MRI.",
"The radiographic changes of axial SpA are predominantly seen in the axial skeleton (sacroiliac, apophyseal, discovertebral, and costovertebral) as well as at sites of enthesopathy (\"whiskering\" of the iliac crest, greater tuberosities of the humerus, ischial tuberosities, femoral trochanters, calcaneus, and vertebral spinous processes). Sacroiliitis is usually bilateral and symmetric. Initially, it involves the synovial-lined lower two thirds of the sacroiliac joint. The earliest radiographic change is minimal erosion of the iliac side of the sacroiliac joint, where the cartilage is thinner and has clefts, or sclerosis. Progression of the erosive process may result in moderate to significant erosions, sclerosis, widening, narrowing, or partial ankylosis of the sacroiliac joint space, eventually followed by complete bony ankylosis or fusion of the joint",
"Axial spondyloarthritis has no cure. Treatment focuses on control of inflammatory symptoms and participation in an exercise program to minimize deformity and disability.",
"For most patients with axial spondyloarthropathy, an NSAID is used as initial therapy rather than a biologic agent. Two weeks of NSAID therapy is considered an adequate trial. For those who do not respond to NSAIDs, tumor necrosis factor (TNF) inhibitors can be considered. For patients who fail to respond to TNF inhibitors, interleukin-17 (IL-17) inhibitors or Janus kinase (JAK) inhibitors can be used.",
"A TNF inhibitor was prescribed for the patient in this case. Within 6 months, she showed dramatic improvement in her joint pain and range of motion symptoms."
],
"date": "November 10, 2022",
"figures": [],
"markdown": "# Morning Stiffness, Dry Eyes, Back Pain in a Fit 58-Year-Old\n\n **Authors:** Kristine M. Lohr, MD, MS; Muhammad Sohail Khan, MD \n **Date:** November 10, 2022\n\n ## Content\n\n An anteroposterior projection of the pelvis (AP pelvis) is often sufficient to evaluate the inferior aspects of the sacroiliac joints. The Ferguson view (AP with the tube angled 25-40 degrees cephalad) counteracts the overlap of the sacrum with the ilium, enabling a full view of the sacroiliac joint. This view is recognized because the symphysis pubis overlaps the sacrum.\nMRI of the pelvis with T1 sequences is used for evaluation of ankylosis, erosions, backfill, and fatty metaplasia, and short T1 inversion recovery sequences are used for evaluation of osteitis/inflammation. Semicoronal views are included to visualize the sacroiliac joints along their full length. Pelvis MRI identifies 95% of patients with axial SpA/ankylosing spondylitis. Only 5% of patients require lumbar spine MRI owing to normal pelvis MRI.\nThe radiographic changes of axial SpA are predominantly seen in the axial skeleton (sacroiliac, apophyseal, discovertebral, and costovertebral) as well as at sites of enthesopathy (\"whiskering\" of the iliac crest, greater tuberosities of the humerus, ischial tuberosities, femoral trochanters, calcaneus, and vertebral spinous processes). Sacroiliitis is usually bilateral and symmetric. Initially, it involves the synovial-lined lower two thirds of the sacroiliac joint. The earliest radiographic change is minimal erosion of the iliac side of the sacroiliac joint, where the cartilage is thinner and has clefts, or sclerosis. Progression of the erosive process may result in moderate to significant erosions, sclerosis, widening, narrowing, or partial ankylosis of the sacroiliac joint space, eventually followed by complete bony ankylosis or fusion of the joint\nAxial spondyloarthritis has no cure. Treatment focuses on control of inflammatory symptoms and participation in an exercise program to minimize deformity and disability.\nFor most patients with axial spondyloarthropathy, an NSAID is used as initial therapy rather than a biologic agent. Two weeks of NSAID therapy is considered an adequate trial. For those who do not respond to NSAIDs, tumor necrosis factor (TNF) inhibitors can be considered. For patients who fail to respond to TNF inhibitors, interleukin-17 (IL-17) inhibitors or Janus kinase (JAK) inhibitors can be used.\nA TNF inhibitor was prescribed for the patient in this case. Within 6 months, she showed dramatic improvement in her joint pain and range of motion symptoms.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1737905,
"choiceText": "High-dose NSAID therapy for 2 weeks is considered an adequate trial",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737906,
"choiceText": "A trial with at least four different NSAIDs is recommended prior to more aggressive therapy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737907,
"choiceText": "NSAIDs have been proven to cure the disease if used for more than 10 years, with close monitoring of side effects",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737908,
"choiceText": "TNF inhibitors have no role in the treatment of spondyloarthropathy",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "To date, axial spondyloarthritis has no cure. For most patients, management consists of control of inflammatory symptoms and participation in an exercise program to minimize deformity and disability.<sup>[2]</sup>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 561249,
"questionText": "Which statement is most accurate regarding NSAID therapy for patients with axial spondyloarthritis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1737921,
"choiceText": "Concomitant therapy with methotrexate is highly recommended to prevent drug failure",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737922,
"choiceText": "Secukinumab and ixekizumab have no role in the treatment of the ankylosing spondyloarthropathies",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737923,
"choiceText": "TNF inhibitors are highly effective in reducing the inflammatory component of axial SpA, including peripheral synovitis, enthesitis, and uveitis, and in improving spinal mobility and function and overall quality of life",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737924,
"choiceText": "Sulfasalazine and methotrexate are highly effective in treating sacroiliitis, spondylitis, and enthesitis, according to most studies",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "TNF inhibitors are the first-line choice for biologic treatment if NSAID treatment provides an inadequate response. IL-17 inhibitors may be used in patients who fail treatment with TNF inhibitors.</br></br>\r\nTNF inhibitors reduce the inflammatory component of axial SpA and improve quality of life. Coadministration of low-dose methotrexate with TNF inhibitors is not recommended nor is a strict treat-to-target strategy or discontinuation or tapering of biologics in patients with stable disease.<sup>[2]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 561251,
"questionText": "Regarding the treatment of the ankylosing spondyloarthropathies, which statement is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Morning Stiffness, Dry Eyes, Back Pain in a Fit 58-Year-Old"
},
{
"authors": "Kristine M. Lohr, MD, MS; Muhammad Sohail Khan, MD",
"content": [
"Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult."
],
"date": "November 10, 2022",
"figures": [],
"markdown": "# Morning Stiffness, Dry Eyes, Back Pain in a Fit 58-Year-Old\n\n **Authors:** Kristine M. Lohr, MD, MS; Muhammad Sohail Khan, MD \n **Date:** November 10, 2022\n\n ## Content\n\n Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult.\n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1737905,
"choiceText": "High-dose NSAID therapy for 2 weeks is considered an adequate trial",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737906,
"choiceText": "A trial with at least four different NSAIDs is recommended prior to more aggressive therapy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737907,
"choiceText": "NSAIDs have been proven to cure the disease if used for more than 10 years, with close monitoring of side effects",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737908,
"choiceText": "TNF inhibitors have no role in the treatment of spondyloarthropathy",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "To date, axial spondyloarthritis has no cure. For most patients, management consists of control of inflammatory symptoms and participation in an exercise program to minimize deformity and disability.<sup>[2]</sup>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 561249,
"questionText": "Which statement is most accurate regarding NSAID therapy for patients with axial spondyloarthritis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1737921,
"choiceText": "Concomitant therapy with methotrexate is highly recommended to prevent drug failure",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737922,
"choiceText": "Secukinumab and ixekizumab have no role in the treatment of the ankylosing spondyloarthropathies",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737923,
"choiceText": "TNF inhibitors are highly effective in reducing the inflammatory component of axial SpA, including peripheral synovitis, enthesitis, and uveitis, and in improving spinal mobility and function and overall quality of life",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737924,
"choiceText": "Sulfasalazine and methotrexate are highly effective in treating sacroiliitis, spondylitis, and enthesitis, according to most studies",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "TNF inhibitors are the first-line choice for biologic treatment if NSAID treatment provides an inadequate response. IL-17 inhibitors may be used in patients who fail treatment with TNF inhibitors.</br></br>\r\nTNF inhibitors reduce the inflammatory component of axial SpA and improve quality of life. Coadministration of low-dose methotrexate with TNF inhibitors is not recommended nor is a strict treat-to-target strategy or discontinuation or tapering of biologics in patients with stable disease.<sup>[2]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 561251,
"questionText": "Regarding the treatment of the ankylosing spondyloarthropathies, which statement is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Morning Stiffness, Dry Eyes, Back Pain in a Fit 58-Year-Old"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1737896,
"choiceText": "Reactive arthritis ",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737897,
"choiceText": "Ankylosing spondylitis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737898,
"choiceText": "Psoriatic arthritis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737899,
"choiceText": "Spondylitis associated with inflammatory bowel disease",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737900,
"choiceText": "Synovitis, acne, pustulosis, hyperostosis, osteitis (SAPHO) syndrome",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 561247,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1737905,
"choiceText": "High-dose NSAID therapy for 2 weeks is considered an adequate trial",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737906,
"choiceText": "A trial with at least four different NSAIDs is recommended prior to more aggressive therapy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737907,
"choiceText": "NSAIDs have been proven to cure the disease if used for more than 10 years, with close monitoring of side effects",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737908,
"choiceText": "TNF inhibitors have no role in the treatment of spondyloarthropathy",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "To date, axial spondyloarthritis has no cure. For most patients, management consists of control of inflammatory symptoms and participation in an exercise program to minimize deformity and disability.<sup>[2]</sup>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 561249,
"questionText": "Which statement is most accurate regarding NSAID therapy for patients with axial spondyloarthritis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1737921,
"choiceText": "Concomitant therapy with methotrexate is highly recommended to prevent drug failure",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737922,
"choiceText": "Secukinumab and ixekizumab have no role in the treatment of the ankylosing spondyloarthropathies",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737923,
"choiceText": "TNF inhibitors are highly effective in reducing the inflammatory component of axial SpA, including peripheral synovitis, enthesitis, and uveitis, and in improving spinal mobility and function and overall quality of life",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1737924,
"choiceText": "Sulfasalazine and methotrexate are highly effective in treating sacroiliitis, spondylitis, and enthesitis, according to most studies",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "TNF inhibitors are the first-line choice for biologic treatment if NSAID treatment provides an inadequate response. IL-17 inhibitors may be used in patients who fail treatment with TNF inhibitors.</br></br>\r\nTNF inhibitors reduce the inflammatory component of axial SpA and improve quality of life. Coadministration of low-dose methotrexate with TNF inhibitors is not recommended nor is a strict treat-to-target strategy or discontinuation or tapering of biologics in patients with stable disease.<sup>[2]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 561251,
"questionText": "Regarding the treatment of the ankylosing spondyloarthropathies, which statement is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
882771 | /viewarticle/882771 | [
{
"authors": "Nail Alouch, MD; Doina Ivan, MD; Phyu P. Aung, MD, PhD; Victor G. Prieto, MD, PhD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 76-year-old man with a medical history of multiple cutaneous basal cell carcinomas presents with a lesion on his right lateral lower eyelid. The lesion was noted by an optometrist approximately 8 months ago, during a routine eye examination. It appeared to be slow-growing. The clinical impression was basal cell carcinoma. The lesion was biopsied at an outside facility, and the patient was referred for further workup.",
"His medical history includes hypertension; multiple basal cell carcinomas of the face, trunk, and extremities; prostate cancer (prostatectomy and radiation therapy about 13 years ago); removal of a synovial cyst on the lower spine; cervical disk surgery; and hernia repair. The patient takes aspirin (81 mg daily) and lisinopril (5 mg daily). He has no known drug allergies. His family history is noncontributory.",
"The patient works in construction. He smoked one pack of cigarettes per day for about 23 years and has recently reduced this to smoking six or seven cigarettes per day. He consumes approximately two alcoholic drinks per day and has no history of illicit drug use."
],
"date": "November 02, 2022",
"figures": [],
"markdown": "# Oncology Case Challenge: A Construction Worker Who Drinks Daily Has an Eyelid Lesion\n\n **Authors:** Nail Alouch, MD; Doina Ivan, MD; Phyu P. Aung, MD, PhD; Victor G. Prieto, MD, PhD \n **Date:** November 02, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 76-year-old man with a medical history of multiple cutaneous basal cell carcinomas presents with a lesion on his right lateral lower eyelid. The lesion was noted by an optometrist approximately 8 months ago, during a routine eye examination. It appeared to be slow-growing. The clinical impression was basal cell carcinoma. The lesion was biopsied at an outside facility, and the patient was referred for further workup.\nHis medical history includes hypertension; multiple basal cell carcinomas of the face, trunk, and extremities; prostate cancer (prostatectomy and radiation therapy about 13 years ago); removal of a synovial cyst on the lower spine; cervical disk surgery; and hernia repair. The patient takes aspirin (81 mg daily) and lisinopril (5 mg daily). He has no known drug allergies. His family history is noncontributory.\nThe patient works in construction. He smoked one pack of cigarettes per day for about 23 years and has recently reduced this to smoking six or seven cigarettes per day. He consumes approximately two alcoholic drinks per day and has no history of illicit drug use.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Oncology Case Challenge: A Construction Worker Who Drinks Daily Has an Eyelid Lesion"
},
{
"authors": "Nail Alouch, MD; Doina Ivan, MD; Phyu P. Aung, MD, PhD; Victor G. Prieto, MD, PhD",
"content": [
"Upon physical examination, the lesion is erythematous and measures 6 mm in diameter, with a central scar from the prior biopsy site (performed at an outside facility). The physical examination, including ophthalmic examination, is otherwise unremarkable.",
"Laboratory studies, including complete blood cell count, glucose level, metabolic panel, electrolyte levels, lactate dehydrogenase level, and coagulation studies, are within normal ranges. Imaging studies are negative for metastatic disease and other significant findings.",
"A skin shave and subsequent resection are performed at an outside institution and reveal a predominantly intraepidermal proliferation of basophilic atypical cells (Figure 1). The cells are single or arranged in nests and are noted at all levels of the epidermis, with prominent pagetoid upward migration (Figure 2). The cells are round to oval, with scant cytoplasm, and the nuclei are hyperchromatic, with nuclear molding and inconspicuous nucleoli (Figure 3). No invasion of the atypical cells into the dermis is noted.",
"Figure 1.",
"Figure 2.",
"Figure 3.",
"Immunohistochemical studies reveal that the atypical cells are diffusely positive for cytokeratin 20 (Figure 4), high-molecular-weight cytokeratin, synaptophysin (Figure 5), and BerEp4. The atypical cells are negative for CK5/6 (Figure 6), S100 protein, melan-A, carcinoembryonic antigen, and CD45.",
"Figure 4.",
"Figure 5.",
"Figure 6.."
],
"date": "November 02, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/882/771/882771-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/882/771/882771-Thumb2.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/882/771/882771-Thumb3.png"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/882/771/882771-Thumb4.png"
},
{
"caption": "Figure 5.",
"image_url": "https://img.medscapestatic.com/article/882/771/882771-Thumb5.png"
},
{
"caption": "Figure 6..",
"image_url": "https://img.medscapestatic.com/article/882/771/882771-Thumb6.png"
}
],
"markdown": "# Oncology Case Challenge: A Construction Worker Who Drinks Daily Has an Eyelid Lesion\n\n **Authors:** Nail Alouch, MD; Doina Ivan, MD; Phyu P. Aung, MD, PhD; Victor G. Prieto, MD, PhD \n **Date:** November 02, 2022\n\n ## Content\n\n Upon physical examination, the lesion is erythematous and measures 6 mm in diameter, with a central scar from the prior biopsy site (performed at an outside facility). The physical examination, including ophthalmic examination, is otherwise unremarkable.\nLaboratory studies, including complete blood cell count, glucose level, metabolic panel, electrolyte levels, lactate dehydrogenase level, and coagulation studies, are within normal ranges. Imaging studies are negative for metastatic disease and other significant findings.\nA skin shave and subsequent resection are performed at an outside institution and reveal a predominantly intraepidermal proliferation of basophilic atypical cells (Figure 1). The cells are single or arranged in nests and are noted at all levels of the epidermis, with prominent pagetoid upward migration (Figure 2). The cells are round to oval, with scant cytoplasm, and the nuclei are hyperchromatic, with nuclear molding and inconspicuous nucleoli (Figure 3). No invasion of the atypical cells into the dermis is noted.\nFigure 1.\nFigure 2.\nFigure 3.\nImmunohistochemical studies reveal that the atypical cells are diffusely positive for cytokeratin 20 (Figure 4), high-molecular-weight cytokeratin, synaptophysin (Figure 5), and BerEp4. The atypical cells are negative for CK5/6 (Figure 6), S100 protein, melan-A, carcinoembryonic antigen, and CD45.\nFigure 4.\nFigure 5.\nFigure 6..\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4.** \n \n\n**Figure 5.** \n \n\n**Figure 6..** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1117520,
"choiceText": "Melanoma in situ",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117522,
"choiceText": "Squamous cell carcinoma in situ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117524,
"choiceText": "Extramammary Paget disease\r\n",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117526,
"choiceText": "Merkel cell carcinoma in situ",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117528,
"choiceText": "Cutaneous T-cell lymphoma",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 354187,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Oncology Case Challenge: A Construction Worker Who Drinks Daily Has an Eyelid Lesion"
},
{
"authors": "Nail Alouch, MD; Doina Ivan, MD; Phyu P. Aung, MD, PhD; Victor G. Prieto, MD, PhD",
"content": [
"Merkel cell carcinoma is an uncommon malignant skin tumor. The origin of this tumor is controversial. It was first described by Toker in 1972. The tumor was called \"trabecular carcinoma,\" and it was thought to arise from the eccrine cells.",
"In 1978, Tang and Toker[1] examined these tumors using electron microscopy. They identified cytoplasmic neurosecretory granules in the tumor cells, which led them to suggest that these tumors are derived from the neural crest and are of neuroendocrine nature and differentiation. Thus, they suggested that these tumors arise from the known normal neuroendocrine cells of the skin: Merkel cells. Some authors have proposed the possibility of pluripotent stem cells as the cells of origin.[2,3,4] Currently, these tumors are called \"Merkel cell carcinomas\" or \"primary cutaneous neuroendocrine carcinomas.\"",
"Merkel cell carcinoma is an aggressive cancer. It typically presents as a rapidly growing, painless, red-violaceous papule, plaque, or nodule on sun-exposed skin. It is more common in white elderly persons, with a slight male predilection. The skin of the head and neck region is the most commonly involved, followed by the upper extremities. The clinical features can be summarized with the acronym AEIOU (asymptomatic/painless, expanding rapidly, immune suppression, older than 50 years, ultraviolet-exposed skin in a fair-skinned individual).[5]",
"Merkel cell carcinoma is a high-grade tumor with a relatively high rate of metastasis. The vast majority of tumors involve the dermis. As many as 41% of cases of Merkel cell carcinoma cases can be associated with other skin lesions, including actinic keratosis, squamous cell carcinoma (in situ and invasive), basal cell carcinoma, and melanoma.[2,6,7,8,9,10] These associations, along with the tendency of these tumors to occur in sun-exposed skin, suggest solar irradiation damage as an etiology for Merkel cell carcinoma."
],
"date": "November 02, 2022",
"figures": [],
"markdown": "# Oncology Case Challenge: A Construction Worker Who Drinks Daily Has an Eyelid Lesion\n\n **Authors:** Nail Alouch, MD; Doina Ivan, MD; Phyu P. Aung, MD, PhD; Victor G. Prieto, MD, PhD \n **Date:** November 02, 2022\n\n ## Content\n\n Merkel cell carcinoma is an uncommon malignant skin tumor. The origin of this tumor is controversial. It was first described by Toker in 1972. The tumor was called \"trabecular carcinoma,\" and it was thought to arise from the eccrine cells.\nIn 1978, Tang and Toker[1] examined these tumors using electron microscopy. They identified cytoplasmic neurosecretory granules in the tumor cells, which led them to suggest that these tumors are derived from the neural crest and are of neuroendocrine nature and differentiation. Thus, they suggested that these tumors arise from the known normal neuroendocrine cells of the skin: Merkel cells. Some authors have proposed the possibility of pluripotent stem cells as the cells of origin.[2,3,4] Currently, these tumors are called \"Merkel cell carcinomas\" or \"primary cutaneous neuroendocrine carcinomas.\"\nMerkel cell carcinoma is an aggressive cancer. It typically presents as a rapidly growing, painless, red-violaceous papule, plaque, or nodule on sun-exposed skin. It is more common in white elderly persons, with a slight male predilection. The skin of the head and neck region is the most commonly involved, followed by the upper extremities. The clinical features can be summarized with the acronym AEIOU (asymptomatic/painless, expanding rapidly, immune suppression, older than 50 years, ultraviolet-exposed skin in a fair-skinned individual).[5]\nMerkel cell carcinoma is a high-grade tumor with a relatively high rate of metastasis. The vast majority of tumors involve the dermis. As many as 41% of cases of Merkel cell carcinoma cases can be associated with other skin lesions, including actinic keratosis, squamous cell carcinoma (in situ and invasive), basal cell carcinoma, and melanoma.[2,6,7,8,9,10] These associations, along with the tendency of these tumors to occur in sun-exposed skin, suggest solar irradiation damage as an etiology for Merkel cell carcinoma.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1117520,
"choiceText": "Melanoma in situ",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117522,
"choiceText": "Squamous cell carcinoma in situ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117524,
"choiceText": "Extramammary Paget disease\r\n",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117526,
"choiceText": "Merkel cell carcinoma in situ",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117528,
"choiceText": "Cutaneous T-cell lymphoma",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 354187,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Oncology Case Challenge: A Construction Worker Who Drinks Daily Has an Eyelid Lesion"
},
{
"authors": "Nail Alouch, MD; Doina Ivan, MD; Phyu P. Aung, MD, PhD; Victor G. Prieto, MD, PhD",
"content": [
"Epidermal involvement by Merkel cell carcinoma is uncommon. It was first noted in 1980 by Sidhu and colleagues.[11]The authors described the presence of the neoplastic cells in the overlying epithelium in two of the seven reported cases. In 1993, Smith and colleagues[2] found the intraepidermal component in 11 of 132 cases (8.3%).[2] Of these 11 cases, only one had pure intraepidermal carcinoma without dermal tumor. The remaining 10 cases had both dermal and epidermal elements. Walsh[6] described the presence of at least focal epidermotropism in eight of 27 cases (30%).",
"Pure epidermal Merkel cell carcinoma (Merkel cell carcinoma in situ) without a dermal component is exceedingly rare. Most reported patients with pure epidermal Merkel cell carcinoma also had other skin lesions, such as actinic keratosis, squamous cell carcinoma in situ, and trichilemmal cyst.[3,4,12,13,14] Owing to this association, the epidermal component of Merkel cell carcinoma was overlooked or misdiagnosed (usually as squamous cell carcinoma in situ) in some cases.[2]",
"As mentioned above, Merkel cell carcinoma is aggressive, with a high frequency of metastasis to regional lymph nodes and distant organs. When intraepidermal Merkel cell carcinoma is recognized on skin biopsy, ruling out an invasive component, which can be sometimes minimal, is important. The absence of invasion on a representative biopsy does not establish the diagnosis of pure intraepidermal Merkel cell carcinoma (Merkel cell carcinoma in situ). The rarity of this entity makes it more likely for an intraepithelial lesion to be a nonsampled invasive Merkel cell carcinoma than a pure epidermal Merkel cell carcinoma. Thus, when no invasion is seen on biopsy, examining additional sections to rule out an invasive component is recommended.",
"Conventional Merkel cell carcinoma is usually treated with wide local excision with potential sentinel lymph node dissection. Owing to the rarity of Merkel cell carcinoma in situ and the possibility of a nonsampled invasive involvement, pure epidermal Merkel cell carcinoma (Merkel cell carcinoma in situ) is usually managed as conventional Merkel cell carcinoma.",
"The histologic features of Merkel cell carcinoma include small, poorly differentiated round cells with hyperchromatic nuclei, nuclear molding, inconspicuous nucleoli, and scant cytoplasm. The cells can be organized in nests, sheets, and sometimes single cells. Mitotic figures and apoptotic bodies are common. When the tumor is present in the epidermis, the cells demonstrate histologic features similar to those of standard, dermal Merkel cell carcinoma. In addition, the cells may also show pagetoid upward migration of the atypical cells[5,9,12]; Pautrier-like microabscesses[15]; and squamous, glandular, or adnexal differentiation.[3,6]These features are usually seen in other lesions, such as adnexal or squamous cell carcinoma; therefore, recognizing them is important to avoid misdiagnosis.",
"Histologically, the differential diagnosis for the epidermal Merkel cell carcinoma is broad; it includes such lesions as melanoma in situ, squamous cell carcinoma in situ, Paget disease (mammary and extramammary), sebaceous gland carcinoma, Langerhans cell histiocytosis, and cutaneous T-cell lymphoma. The differential diagnosis also includes benign conditions, such as Toker cell hyperplasia, pagetoid dyskeratosis, and clear cell papulosis (which is an artifactual phenomenon). Immunohistochemical studies are essential in characterizing these lesions and rendering the correct diagnosis.",
"Immunohistochemically, Merkel cell carcinoma cells typically express neuroendocrine markers, such as synaptophysin, chromogranin, and neuron-specific enolase. The cells also demonstrate the characteristic perinuclear dot-like staining pattern for cytokeratin 20 (in most cases) and pancytokeratin markers, as well as for some of the neuroendocrine markers."
],
"date": "November 02, 2022",
"figures": [],
"markdown": "# Oncology Case Challenge: A Construction Worker Who Drinks Daily Has an Eyelid Lesion\n\n **Authors:** Nail Alouch, MD; Doina Ivan, MD; Phyu P. Aung, MD, PhD; Victor G. Prieto, MD, PhD \n **Date:** November 02, 2022\n\n ## Content\n\n Epidermal involvement by Merkel cell carcinoma is uncommon. It was first noted in 1980 by Sidhu and colleagues.[11]The authors described the presence of the neoplastic cells in the overlying epithelium in two of the seven reported cases. In 1993, Smith and colleagues[2] found the intraepidermal component in 11 of 132 cases (8.3%).[2] Of these 11 cases, only one had pure intraepidermal carcinoma without dermal tumor. The remaining 10 cases had both dermal and epidermal elements. Walsh[6] described the presence of at least focal epidermotropism in eight of 27 cases (30%).\nPure epidermal Merkel cell carcinoma (Merkel cell carcinoma in situ) without a dermal component is exceedingly rare. Most reported patients with pure epidermal Merkel cell carcinoma also had other skin lesions, such as actinic keratosis, squamous cell carcinoma in situ, and trichilemmal cyst.[3,4,12,13,14] Owing to this association, the epidermal component of Merkel cell carcinoma was overlooked or misdiagnosed (usually as squamous cell carcinoma in situ) in some cases.[2]\nAs mentioned above, Merkel cell carcinoma is aggressive, with a high frequency of metastasis to regional lymph nodes and distant organs. When intraepidermal Merkel cell carcinoma is recognized on skin biopsy, ruling out an invasive component, which can be sometimes minimal, is important. The absence of invasion on a representative biopsy does not establish the diagnosis of pure intraepidermal Merkel cell carcinoma (Merkel cell carcinoma in situ). The rarity of this entity makes it more likely for an intraepithelial lesion to be a nonsampled invasive Merkel cell carcinoma than a pure epidermal Merkel cell carcinoma. Thus, when no invasion is seen on biopsy, examining additional sections to rule out an invasive component is recommended.\nConventional Merkel cell carcinoma is usually treated with wide local excision with potential sentinel lymph node dissection. Owing to the rarity of Merkel cell carcinoma in situ and the possibility of a nonsampled invasive involvement, pure epidermal Merkel cell carcinoma (Merkel cell carcinoma in situ) is usually managed as conventional Merkel cell carcinoma.\nThe histologic features of Merkel cell carcinoma include small, poorly differentiated round cells with hyperchromatic nuclei, nuclear molding, inconspicuous nucleoli, and scant cytoplasm. The cells can be organized in nests, sheets, and sometimes single cells. Mitotic figures and apoptotic bodies are common. When the tumor is present in the epidermis, the cells demonstrate histologic features similar to those of standard, dermal Merkel cell carcinoma. In addition, the cells may also show pagetoid upward migration of the atypical cells[5,9,12]; Pautrier-like microabscesses[15]; and squamous, glandular, or adnexal differentiation.[3,6]These features are usually seen in other lesions, such as adnexal or squamous cell carcinoma; therefore, recognizing them is important to avoid misdiagnosis.\nHistologically, the differential diagnosis for the epidermal Merkel cell carcinoma is broad; it includes such lesions as melanoma in situ, squamous cell carcinoma in situ, Paget disease (mammary and extramammary), sebaceous gland carcinoma, Langerhans cell histiocytosis, and cutaneous T-cell lymphoma. The differential diagnosis also includes benign conditions, such as Toker cell hyperplasia, pagetoid dyskeratosis, and clear cell papulosis (which is an artifactual phenomenon). Immunohistochemical studies are essential in characterizing these lesions and rendering the correct diagnosis.\nImmunohistochemically, Merkel cell carcinoma cells typically express neuroendocrine markers, such as synaptophysin, chromogranin, and neuron-specific enolase. The cells also demonstrate the characteristic perinuclear dot-like staining pattern for cytokeratin 20 (in most cases) and pancytokeratin markers, as well as for some of the neuroendocrine markers.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Oncology Case Challenge: A Construction Worker Who Drinks Daily Has an Eyelid Lesion"
},
{
"authors": "Nail Alouch, MD; Doina Ivan, MD; Phyu P. Aung, MD, PhD; Victor G. Prieto, MD, PhD",
"content": [
"Melanoma in situ represents an intraepidermal proliferation of atypical melanocytes. The cells usually have abundant cytoplasm with melanin pigment and intranuclear pseudoinclusions. On immunohistochemistry, the neoplastic cells express melanocytic markers, including S100 protein, melan-A, HMB45 antigen, and SOX10, and are negative for cytokeratin. As a possible pitfall, numerous melanomas may express neuroendocrine markers.",
"Squamous cell carcinoma in situ reveals more epithelioid cells with desmosomes between the tumor cells. The cells express squamous cell markers, such as high-molecular-weight cytokeratins (eg, CK5/6), p40, and p63, and are negative for neuroendocrine markers and cytokeratin 20. Remembering that squamous carcinoma in situ and Merkel cell carcinoma can be concurrent is important.",
"In extramammary Paget disease, the atypical cells are thought to arise from intraepidermal sweat gland cells and demonstrate glandular features, including abundant basophilic cytoplasm, which can be highlighted by periodic acid-Schiff with diastase and mucin special stains. The cells express cytokeratin 7, carcinoembryonic antigen, and variably epithelial membranous antigen. Secondary extramammary Paget disease from the genitourinary tract may express also CK20, but not with a dot-like pattern.",
"Sebaceous carcinoma cells have multiple cytoplasmic vacuoles that contain lipid droplets and nuclear scalloping. The intracytoplasmic lipid droplets can be highlighted with an adipophilin stain. The cells are also negative for cytokeratin 20 and the neuroendocrine markers.",
"One substantial differential diagnosis is cutaneous T-cell lymphoma. Histologically, the infiltrating lymphocytes typically have clear cytoplasm and marked atypia. The cells express general lymphocytic markers (such as CD45) and T-lymphocytic markers, such as CD3 and CD4 (or CD8). The atypical lymphocytes are immunonegative for all cytokeratin and neuroendocrine markers.",
"The main treatment for cutaneous lymphoma is chemotherapy-based without surgical intervention. Therefore, recognizing cutaneous lymphoma is crucial to avoid unnecessary surgical procedure and provide the appropriate treatment.",
"Some important points to be remembered include the following:",
"Pure epidermal Merkel cell carcinoma (Merkel cell carcinoma in situ) is rare.",
"Identification of epidermal Merkel cell carcinoma should prompt reexcision for evaluation of a possible dermal component.",
"Immunohistochemistry is essential for histologic diagnosis. Depending on the morphology and location, the recommended panel includes cytokeratin 20; adipophilin; and squamous, neuroendocrine, melanocytic, glandular, and lymphocytic immunohistochemical markers.",
"Merkel cell carcinoma in situ can coexist with other skin lesions (especially squamous cell carcinoma in situ and actinic keratosis).",
"The patient in this case underwent wide local excision with two-stage tarsal conjunctival flap (Hughes flap procedure), without sentinel lymph node sampling. The patient is still alive without evidence of recurrence or metastatic disease after 18 months of follow-up."
],
"date": "November 02, 2022",
"figures": [],
"markdown": "# Oncology Case Challenge: A Construction Worker Who Drinks Daily Has an Eyelid Lesion\n\n **Authors:** Nail Alouch, MD; Doina Ivan, MD; Phyu P. Aung, MD, PhD; Victor G. Prieto, MD, PhD \n **Date:** November 02, 2022\n\n ## Content\n\n Melanoma in situ represents an intraepidermal proliferation of atypical melanocytes. The cells usually have abundant cytoplasm with melanin pigment and intranuclear pseudoinclusions. On immunohistochemistry, the neoplastic cells express melanocytic markers, including S100 protein, melan-A, HMB45 antigen, and SOX10, and are negative for cytokeratin. As a possible pitfall, numerous melanomas may express neuroendocrine markers.\nSquamous cell carcinoma in situ reveals more epithelioid cells with desmosomes between the tumor cells. The cells express squamous cell markers, such as high-molecular-weight cytokeratins (eg, CK5/6), p40, and p63, and are negative for neuroendocrine markers and cytokeratin 20. Remembering that squamous carcinoma in situ and Merkel cell carcinoma can be concurrent is important.\nIn extramammary Paget disease, the atypical cells are thought to arise from intraepidermal sweat gland cells and demonstrate glandular features, including abundant basophilic cytoplasm, which can be highlighted by periodic acid-Schiff with diastase and mucin special stains. The cells express cytokeratin 7, carcinoembryonic antigen, and variably epithelial membranous antigen. Secondary extramammary Paget disease from the genitourinary tract may express also CK20, but not with a dot-like pattern.\nSebaceous carcinoma cells have multiple cytoplasmic vacuoles that contain lipid droplets and nuclear scalloping. The intracytoplasmic lipid droplets can be highlighted with an adipophilin stain. The cells are also negative for cytokeratin 20 and the neuroendocrine markers.\nOne substantial differential diagnosis is cutaneous T-cell lymphoma. Histologically, the infiltrating lymphocytes typically have clear cytoplasm and marked atypia. The cells express general lymphocytic markers (such as CD45) and T-lymphocytic markers, such as CD3 and CD4 (or CD8). The atypical lymphocytes are immunonegative for all cytokeratin and neuroendocrine markers.\nThe main treatment for cutaneous lymphoma is chemotherapy-based without surgical intervention. Therefore, recognizing cutaneous lymphoma is crucial to avoid unnecessary surgical procedure and provide the appropriate treatment.\nSome important points to be remembered include the following:\nPure epidermal Merkel cell carcinoma (Merkel cell carcinoma in situ) is rare.\nIdentification of epidermal Merkel cell carcinoma should prompt reexcision for evaluation of a possible dermal component.\nImmunohistochemistry is essential for histologic diagnosis. Depending on the morphology and location, the recommended panel includes cytokeratin 20; adipophilin; and squamous, neuroendocrine, melanocytic, glandular, and lymphocytic immunohistochemical markers.\nMerkel cell carcinoma in situ can coexist with other skin lesions (especially squamous cell carcinoma in situ and actinic keratosis).\nThe patient in this case underwent wide local excision with two-stage tarsal conjunctival flap (Hughes flap procedure), without sentinel lymph node sampling. The patient is still alive without evidence of recurrence or metastatic disease after 18 months of follow-up.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1117530,
"choiceText": "Epidermal Merkel cell carcinoma is common and can be seen in about 75% of Merkel cell carcinoma cases",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117532,
"choiceText": "Merkel cell carcinoma commonly affects the trunk",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117534,
"choiceText": "The presence of squamous cell carcinoma in situ or actinic keratosis adjacent to epidermal Merkel cell carcinoma is rare",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117536,
"choiceText": "Histologically, epidermal Merkel cell carcinoma has atypical cells with hyperchromatic nuclei, nuclear pseudoinclusions, and abundant pigmented cytoplasm",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117538,
"choiceText": "Epidermal Merkel cell carcinoma can demonstrate pagetoid upward migration, Pautrier-like microabscesses, and squamous or glandular differentiation",
"correct": true,
"displayOrder": 5,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The vast majority of Merkel cell carcinomas involve the dermis. Epidermal involvement with Merkel cell carcinoma is uncommon and ranges from 8% to 30% of the reported cases. The most common location of Merkel cell carcinoma is the head and neck, followed by the upper extremities. This raises the likelihood of a role of sun/ultraviolet light exposure as an etiology for Merkel cell carcinoma. Therefore, Merkel cell carcinomas are commonly associated with other skin lesions, mostly squamous cell carcinoma in situ and actinic keratosis. <br><br>\r\n\r\nThe histologic features of Merkel cell carcinoma are small cells with hyperchromatic nuclei with scant cytoplasm and increased mitotic activity. Epidermal Merkel cell carcinoma can present as a diffuse proliferation of atypical small hyperchromatic cells between the epidermal keratinocytes. However, it can demonstrate other features that may mimic or be mistaken for other entities. Some of these features include pagetoid upward migration, which is commonly seen in melanoma in situ; Pautrier-like microabscesses, which are noted in cutaneous T-cell lymphomas; squamous differentiation, which can be mistaken as squamous cell carcinoma; and glandular differentiation, which can raise the possibility of Paget disease or extramammary Paget disease.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 354189,
"questionText": "Which of the following statements about Merkel cell carcinoma is accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1117540,
"choiceText": "CD45",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117542,
"choiceText": "CK7",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117544,
"choiceText": "Synaptophysin",
"correct": true,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117546,
"choiceText": "Melan-A",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117548,
"choiceText": "p40\r\n",
"correct": false,
"displayOrder": 5,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Merkel cell carcinoma is usually positive for CK20 (perinuclear dot-like pattern) and neuroendocrine markers, such as synaptophysin, chromogranin and neuron-specific enolase. Neuroendocrine markers are not sensitive for Merkel cell carcinoma, but patchy or focal staining can be seen in most cases; it is considered most specific. <br><br>\r\n\r\nCD45 is a general lymphocytic marker. It stains the lymphocytes in cutaneous lymphoma and the normal inflammatory lymphocytes. CK7 is one of the cytokeratin stains commonly present in nonkeratinizing epithelia and is generally used for glandular differentiation. In skin specimens, CK7 is helpful to distinguish the tumors arising from the adnexal structures, such as Paget disease and extramammary Paget disease. CK7 expression can be seen in in about one third of Merkel cell carcinoma cases.<br><br>\r\n\r\nMelan-A is one of the melanocytic markers and is used to highlight the intraepidermal and dermal melanocytes. It is helpful to differentiate melanoma (invasive and in situ) from other lesions.\r\n<br><br>\r\np40 is a sensitive nuclear maker for normal and malignant squamous cells. It is positive in squamous cell carcinomas and basal cell carcinomas of the skin. In cases with atypical epidermal proliferation, p40 is helpful to distinguish whether the atypical cells are of squamous (diffusely labeling of normal and atypical cells) or nonsquamous differentiation (labeling only the normal epidermal cells and not the atypical cells). ",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 354191,
"questionText": "Which of the following immunohistochemical studies is most specific for diagnosing Merkel cell carcinoma?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Oncology Case Challenge: A Construction Worker Who Drinks Daily Has an Eyelid Lesion"
},
{
"authors": "Nail Alouch, MD; Doina Ivan, MD; Phyu P. Aung, MD, PhD; Victor G. Prieto, MD, PhD",
"content": [],
"date": "November 02, 2022",
"figures": [],
"markdown": "# Oncology Case Challenge: A Construction Worker Who Drinks Daily Has an Eyelid Lesion\n\n **Authors:** Nail Alouch, MD; Doina Ivan, MD; Phyu P. Aung, MD, PhD; Victor G. Prieto, MD, PhD \n **Date:** November 02, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1117530,
"choiceText": "Epidermal Merkel cell carcinoma is common and can be seen in about 75% of Merkel cell carcinoma cases",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117532,
"choiceText": "Merkel cell carcinoma commonly affects the trunk",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117534,
"choiceText": "The presence of squamous cell carcinoma in situ or actinic keratosis adjacent to epidermal Merkel cell carcinoma is rare",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117536,
"choiceText": "Histologically, epidermal Merkel cell carcinoma has atypical cells with hyperchromatic nuclei, nuclear pseudoinclusions, and abundant pigmented cytoplasm",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117538,
"choiceText": "Epidermal Merkel cell carcinoma can demonstrate pagetoid upward migration, Pautrier-like microabscesses, and squamous or glandular differentiation",
"correct": true,
"displayOrder": 5,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The vast majority of Merkel cell carcinomas involve the dermis. Epidermal involvement with Merkel cell carcinoma is uncommon and ranges from 8% to 30% of the reported cases. The most common location of Merkel cell carcinoma is the head and neck, followed by the upper extremities. This raises the likelihood of a role of sun/ultraviolet light exposure as an etiology for Merkel cell carcinoma. Therefore, Merkel cell carcinomas are commonly associated with other skin lesions, mostly squamous cell carcinoma in situ and actinic keratosis. <br><br>\r\n\r\nThe histologic features of Merkel cell carcinoma are small cells with hyperchromatic nuclei with scant cytoplasm and increased mitotic activity. Epidermal Merkel cell carcinoma can present as a diffuse proliferation of atypical small hyperchromatic cells between the epidermal keratinocytes. However, it can demonstrate other features that may mimic or be mistaken for other entities. Some of these features include pagetoid upward migration, which is commonly seen in melanoma in situ; Pautrier-like microabscesses, which are noted in cutaneous T-cell lymphomas; squamous differentiation, which can be mistaken as squamous cell carcinoma; and glandular differentiation, which can raise the possibility of Paget disease or extramammary Paget disease.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 354189,
"questionText": "Which of the following statements about Merkel cell carcinoma is accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1117540,
"choiceText": "CD45",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117542,
"choiceText": "CK7",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117544,
"choiceText": "Synaptophysin",
"correct": true,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117546,
"choiceText": "Melan-A",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117548,
"choiceText": "p40\r\n",
"correct": false,
"displayOrder": 5,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Merkel cell carcinoma is usually positive for CK20 (perinuclear dot-like pattern) and neuroendocrine markers, such as synaptophysin, chromogranin and neuron-specific enolase. Neuroendocrine markers are not sensitive for Merkel cell carcinoma, but patchy or focal staining can be seen in most cases; it is considered most specific. <br><br>\r\n\r\nCD45 is a general lymphocytic marker. It stains the lymphocytes in cutaneous lymphoma and the normal inflammatory lymphocytes. CK7 is one of the cytokeratin stains commonly present in nonkeratinizing epithelia and is generally used for glandular differentiation. In skin specimens, CK7 is helpful to distinguish the tumors arising from the adnexal structures, such as Paget disease and extramammary Paget disease. CK7 expression can be seen in in about one third of Merkel cell carcinoma cases.<br><br>\r\n\r\nMelan-A is one of the melanocytic markers and is used to highlight the intraepidermal and dermal melanocytes. It is helpful to differentiate melanoma (invasive and in situ) from other lesions.\r\n<br><br>\r\np40 is a sensitive nuclear maker for normal and malignant squamous cells. It is positive in squamous cell carcinomas and basal cell carcinomas of the skin. In cases with atypical epidermal proliferation, p40 is helpful to distinguish whether the atypical cells are of squamous (diffusely labeling of normal and atypical cells) or nonsquamous differentiation (labeling only the normal epidermal cells and not the atypical cells). ",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 354191,
"questionText": "Which of the following immunohistochemical studies is most specific for diagnosing Merkel cell carcinoma?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Oncology Case Challenge: A Construction Worker Who Drinks Daily Has an Eyelid Lesion"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1117520,
"choiceText": "Melanoma in situ",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117522,
"choiceText": "Squamous cell carcinoma in situ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117524,
"choiceText": "Extramammary Paget disease\r\n",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117526,
"choiceText": "Merkel cell carcinoma in situ",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117528,
"choiceText": "Cutaneous T-cell lymphoma",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 354187,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1117530,
"choiceText": "Epidermal Merkel cell carcinoma is common and can be seen in about 75% of Merkel cell carcinoma cases",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117532,
"choiceText": "Merkel cell carcinoma commonly affects the trunk",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117534,
"choiceText": "The presence of squamous cell carcinoma in situ or actinic keratosis adjacent to epidermal Merkel cell carcinoma is rare",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117536,
"choiceText": "Histologically, epidermal Merkel cell carcinoma has atypical cells with hyperchromatic nuclei, nuclear pseudoinclusions, and abundant pigmented cytoplasm",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117538,
"choiceText": "Epidermal Merkel cell carcinoma can demonstrate pagetoid upward migration, Pautrier-like microabscesses, and squamous or glandular differentiation",
"correct": true,
"displayOrder": 5,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The vast majority of Merkel cell carcinomas involve the dermis. Epidermal involvement with Merkel cell carcinoma is uncommon and ranges from 8% to 30% of the reported cases. The most common location of Merkel cell carcinoma is the head and neck, followed by the upper extremities. This raises the likelihood of a role of sun/ultraviolet light exposure as an etiology for Merkel cell carcinoma. Therefore, Merkel cell carcinomas are commonly associated with other skin lesions, mostly squamous cell carcinoma in situ and actinic keratosis. <br><br>\r\n\r\nThe histologic features of Merkel cell carcinoma are small cells with hyperchromatic nuclei with scant cytoplasm and increased mitotic activity. Epidermal Merkel cell carcinoma can present as a diffuse proliferation of atypical small hyperchromatic cells between the epidermal keratinocytes. However, it can demonstrate other features that may mimic or be mistaken for other entities. Some of these features include pagetoid upward migration, which is commonly seen in melanoma in situ; Pautrier-like microabscesses, which are noted in cutaneous T-cell lymphomas; squamous differentiation, which can be mistaken as squamous cell carcinoma; and glandular differentiation, which can raise the possibility of Paget disease or extramammary Paget disease.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 354189,
"questionText": "Which of the following statements about Merkel cell carcinoma is accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1117540,
"choiceText": "CD45",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117542,
"choiceText": "CK7",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117544,
"choiceText": "Synaptophysin",
"correct": true,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117546,
"choiceText": "Melan-A",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1117548,
"choiceText": "p40\r\n",
"correct": false,
"displayOrder": 5,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Merkel cell carcinoma is usually positive for CK20 (perinuclear dot-like pattern) and neuroendocrine markers, such as synaptophysin, chromogranin and neuron-specific enolase. Neuroendocrine markers are not sensitive for Merkel cell carcinoma, but patchy or focal staining can be seen in most cases; it is considered most specific. <br><br>\r\n\r\nCD45 is a general lymphocytic marker. It stains the lymphocytes in cutaneous lymphoma and the normal inflammatory lymphocytes. CK7 is one of the cytokeratin stains commonly present in nonkeratinizing epithelia and is generally used for glandular differentiation. In skin specimens, CK7 is helpful to distinguish the tumors arising from the adnexal structures, such as Paget disease and extramammary Paget disease. CK7 expression can be seen in in about one third of Merkel cell carcinoma cases.<br><br>\r\n\r\nMelan-A is one of the melanocytic markers and is used to highlight the intraepidermal and dermal melanocytes. It is helpful to differentiate melanoma (invasive and in situ) from other lesions.\r\n<br><br>\r\np40 is a sensitive nuclear maker for normal and malignant squamous cells. It is positive in squamous cell carcinomas and basal cell carcinomas of the skin. In cases with atypical epidermal proliferation, p40 is helpful to distinguish whether the atypical cells are of squamous (diffusely labeling of normal and atypical cells) or nonsquamous differentiation (labeling only the normal epidermal cells and not the atypical cells). ",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 354191,
"questionText": "Which of the following immunohistochemical studies is most specific for diagnosing Merkel cell carcinoma?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
889517 | /viewarticle/889517 | [
{
"authors": "Faizah Siddique, MD; Herbert S. Diamond, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 22-year-old man presents to the emergency department after collapsing on a college football field about 45 minutes earlier, after doing several 50-yard sprints. He describes aching pain in his muscles and feeling weak and lightheaded. He is not sure whether he lost consciousness. He felt dizzy and was confused after the event. No seizure activity was observed.",
"The patient says that he felt well that afternoon, when he began the first training session for his football team. The temperature on the football field was 90°F, with 85% humidity. He was sweating profusely.",
"The patient has not had recurrent syncope. He maintains an active lifestyle and is on his college football team; however, he admits to having been out of shape and having gained weight over the summer.",
"The patient's past medical history is notable for a left ankle sprain. He does not smoke or use illicit drugs. He drinks alcohol socially, typically limiting his intake to four beers on the weekend; however, he has not had a drink in over 2 weeks. He has no allergies, and his family history is notable for diabetes and hypertension. He is not on any prescription medication or over-the-counter supplements. The patient has no relevant history of recent travel, illness, or sick contacts."
],
"date": "November 01, 2022",
"figures": [],
"markdown": "# A 22-Year-Old Football Player Who Collapsed Has Urine Changes\n\n **Authors:** Faizah Siddique, MD; Herbert S. Diamond, MD \n **Date:** November 01, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 22-year-old man presents to the emergency department after collapsing on a college football field about 45 minutes earlier, after doing several 50-yard sprints. He describes aching pain in his muscles and feeling weak and lightheaded. He is not sure whether he lost consciousness. He felt dizzy and was confused after the event. No seizure activity was observed.\nThe patient says that he felt well that afternoon, when he began the first training session for his football team. The temperature on the football field was 90°F, with 85% humidity. He was sweating profusely.\nThe patient has not had recurrent syncope. He maintains an active lifestyle and is on his college football team; however, he admits to having been out of shape and having gained weight over the summer.\nThe patient's past medical history is notable for a left ankle sprain. He does not smoke or use illicit drugs. He drinks alcohol socially, typically limiting his intake to four beers on the weekend; however, he has not had a drink in over 2 weeks. He has no allergies, and his family history is notable for diabetes and hypertension. He is not on any prescription medication or over-the-counter supplements. The patient has no relevant history of recent travel, illness, or sick contacts.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A 22-Year-Old Football Player Who Collapsed Has Urine Changes"
},
{
"authors": "Faizah Siddique, MD; Herbert S. Diamond, MD",
"content": [
"The patient is examined in the emergency department approximately 1 hour after the episode. His vital signs include a temperature of 99.5°F (37.5°C), a blood pressure of 116/74 mm Hg, and a heart rate of 110 beats/min. His weight is 250 lb (113.4 kg), and his height is 6 feet 2 inches (1.88 m). He is muscular but has obesity. He is in no discomfort. He has a regular heart rhythm, and no murmurs or bruits are auscultated.",
"The patient's lung and abdominal examination findings are normal. His cranial nerves are intact. His proximal upper-extremity muscle examination reveals bulky muscles with 4/5 strength; the remainder of his examination findings are normal. His muscles are tender and doughy. He has normal sensation to light touch, pinprick, cold, and vibration. His deep tendon reflexes are 2+. Finger-to-nose test findings are normal. The Romberg sign is negative. His gait is normal. His neuromuscular examination findings are otherwise normal.",
"Initial laboratory test results reveal a hemoglobin level of 14.5 g/dL (reference range, 13.8-17.2 g/dL), a hematocrit of 49% (reference range, 41% to 50%), and a white blood cell count of 11,200/mcl (reference range, 4,500-11,000/mcl), with 72% neutrophils and no bands. A renal electrolyte panel reveals a creatinine level of 1.7 mg/dL (reference range, 0.7-1.3 mg/dL), a sodium level of 135 mmol/L (reference range, 135-145 mmol/L), and a potassium level of 4.9 mmol/L (reference range, 3.6-5.2 mmol/L). His creatin phosphokinase level is 12,976 IU/L (reference range, 20-200 IU/L). The remainder of his basic metabolic panel findings, including calcium, magnesium, and phosphorus levels, are normal.",
"The urinalysis is positive for blood, but no red cells are found. Urine drug screen results are negative. The patient's urine is dark (Figure).",
"Figure.",
"CT of the head and MRI of the brain are both normal. An ECG is notable for sinus tachycardia. The EEG findings are normal. Electromyography and nerve conduction study findings are normal."
],
"date": "November 01, 2022",
"figures": [
{
"caption": "Figure.",
"image_url": "https://img.medscapestatic.com/article/889/517/889517-Thumb1.jpg"
}
],
"markdown": "# A 22-Year-Old Football Player Who Collapsed Has Urine Changes\n\n **Authors:** Faizah Siddique, MD; Herbert S. Diamond, MD \n **Date:** November 01, 2022\n\n ## Content\n\n The patient is examined in the emergency department approximately 1 hour after the episode. His vital signs include a temperature of 99.5°F (37.5°C), a blood pressure of 116/74 mm Hg, and a heart rate of 110 beats/min. His weight is 250 lb (113.4 kg), and his height is 6 feet 2 inches (1.88 m). He is muscular but has obesity. He is in no discomfort. He has a regular heart rhythm, and no murmurs or bruits are auscultated.\nThe patient's lung and abdominal examination findings are normal. His cranial nerves are intact. His proximal upper-extremity muscle examination reveals bulky muscles with 4/5 strength; the remainder of his examination findings are normal. His muscles are tender and doughy. He has normal sensation to light touch, pinprick, cold, and vibration. His deep tendon reflexes are 2+. Finger-to-nose test findings are normal. The Romberg sign is negative. His gait is normal. His neuromuscular examination findings are otherwise normal.\nInitial laboratory test results reveal a hemoglobin level of 14.5 g/dL (reference range, 13.8-17.2 g/dL), a hematocrit of 49% (reference range, 41% to 50%), and a white blood cell count of 11,200/mcl (reference range, 4,500-11,000/mcl), with 72% neutrophils and no bands. A renal electrolyte panel reveals a creatinine level of 1.7 mg/dL (reference range, 0.7-1.3 mg/dL), a sodium level of 135 mmol/L (reference range, 135-145 mmol/L), and a potassium level of 4.9 mmol/L (reference range, 3.6-5.2 mmol/L). His creatin phosphokinase level is 12,976 IU/L (reference range, 20-200 IU/L). The remainder of his basic metabolic panel findings, including calcium, magnesium, and phosphorus levels, are normal.\nThe urinalysis is positive for blood, but no red cells are found. Urine drug screen results are negative. The patient's urine is dark (Figure).\nFigure.\nCT of the head and MRI of the brain are both normal. An ECG is notable for sinus tachycardia. The EEG findings are normal. Electromyography and nerve conduction study findings are normal.\n\n ## Figures\n\n **Figure.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1163814,
"choiceText": "Intravascular hemolysis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163816,
"choiceText": "Septicemia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163818,
"choiceText": "Heat stroke or exercise-induced rhabdomyolysis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163820,
"choiceText": "Polymyositis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163822,
"choiceText": "Genetic dystrophy-induced rhabdomyolysis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 369877,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 22-Year-Old Football Player Who Collapsed Has Urine Changes"
},
{
"authors": "Faizah Siddique, MD; Herbert S. Diamond, MD",
"content": [
"Rhabdomyolysis is extensive muscle injury. The muscle damage results in release of creatine kinase into the blood stream. Rhabdomyolysis symptoms can range from asymptomatic muscle enzyme elevation to acute kidney failure and muscle pain.",
"The rhabdomyolysis diagnosis in this patient was based on the marked elevation of creatine kinase levels and the dark urine that was positive for blood in the absence of red blood cells, along with his muscle pain and tenderness. The attribution to exercise with or without heat stroke is based on the history of vigorous exercise on a hot, humid day in a deconditioned and obese patient.",
"Intravascular hemolysis may produce dark urine that is positive for blood but not the marked elevation in creatine phosphokinase level, muscle pain, and tenderness. Genetic causes are unlikely, given the lack of prior episodes despite vigorous exercise. No evidence suggests sepsis.",
"Rhabdomyolysis has many causes, including the following[1,2]:",
"Trauma or muscle hypoxia, such as crush syndrome",
"Exertion related to strenuous or vigorous exercise especially with heat stroke",
"Genetic disorders",
"Infections primarily viral infection",
"Metabolic and electrolyte disturbances",
"Prescription medications, such as statins",
"Illicit drugs (eg, cocaine, heroin)",
"Trauma is the most common cause of rhabdomyolysis,[3] occurring in as many as 85% of patients with traumatic injuries. Between 10% and 50% of patients with rhabdomyolysis develop acute renal failure.[2,4] In critically ill patients, mortality can be as high as 59% with acute renal failure.[4,5]"
],
"date": "November 01, 2022",
"figures": [],
"markdown": "# A 22-Year-Old Football Player Who Collapsed Has Urine Changes\n\n **Authors:** Faizah Siddique, MD; Herbert S. Diamond, MD \n **Date:** November 01, 2022\n\n ## Content\n\n Rhabdomyolysis is extensive muscle injury. The muscle damage results in release of creatine kinase into the blood stream. Rhabdomyolysis symptoms can range from asymptomatic muscle enzyme elevation to acute kidney failure and muscle pain.\nThe rhabdomyolysis diagnosis in this patient was based on the marked elevation of creatine kinase levels and the dark urine that was positive for blood in the absence of red blood cells, along with his muscle pain and tenderness. The attribution to exercise with or without heat stroke is based on the history of vigorous exercise on a hot, humid day in a deconditioned and obese patient.\nIntravascular hemolysis may produce dark urine that is positive for blood but not the marked elevation in creatine phosphokinase level, muscle pain, and tenderness. Genetic causes are unlikely, given the lack of prior episodes despite vigorous exercise. No evidence suggests sepsis.\nRhabdomyolysis has many causes, including the following[1,2]:\nTrauma or muscle hypoxia, such as crush syndrome\nExertion related to strenuous or vigorous exercise especially with heat stroke\nGenetic disorders\nInfections primarily viral infection\nMetabolic and electrolyte disturbances\nPrescription medications, such as statins\nIllicit drugs (eg, cocaine, heroin)\nTrauma is the most common cause of rhabdomyolysis,[3] occurring in as many as 85% of patients with traumatic injuries. Between 10% and 50% of patients with rhabdomyolysis develop acute renal failure.[2,4] In critically ill patients, mortality can be as high as 59% with acute renal failure.[4,5]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1163814,
"choiceText": "Intravascular hemolysis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163816,
"choiceText": "Septicemia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163818,
"choiceText": "Heat stroke or exercise-induced rhabdomyolysis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163820,
"choiceText": "Polymyositis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163822,
"choiceText": "Genetic dystrophy-induced rhabdomyolysis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 369877,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 22-Year-Old Football Player Who Collapsed Has Urine Changes"
},
{
"authors": "Faizah Siddique, MD; Herbert S. Diamond, MD",
"content": [
"Rhabdomyolysis is often diagnosed on the basis of creatine kinase levels at least five times the upper limit of normal.[2] According to recommendations by the American College of Cardiology; the American Heart Association; and the National Heart, Lung, and Blood Institute, for rhabdomyolysis occurring in patients on lipid-lowering therapy, rhabdomyolysis is defined as a creatine kinase level more than 10 times the upper limit of normal.[6] Levels are often considerably higher.",
"Recurrent cases of rhabdomyolysis without any precipitating trauma or exertion should raise suspicion of a genetic defect in metabolism. Defects in glycogen, lipid, mitochondria, and purine metabolism can cause rhabdomyolysis. Muscle biopsies should be obtained in these patients, with appropriate staining for diagnosis.",
"The mechanism of muscle cell destruction is direct injury to the muscle cell membrane, depletion of cellular energy due to hypoxia, or electrolyte disturbances that affect the sodium/potassium pump in the cell. Muscle injury results in leakage of extracellular calcium into the intracellular space, which eventually leads to muscle cell death and necrosis.[3] Once cellular necrosis occurs, cellular products, such as myoglobin, potassium, and creatine kinase, escape into the blood. Acute renal failure can result from massive deposition of muscle enzymes and myoglobin in the renal tubules.[3] Previous studies have suggested that acute renal failure can result from hypovolemia and aciduria.[3]",
"Rhabdomyolysis can occur at any age but is more frequent in individuals older than 60 years or younger than 10 years.[2] The risk for rhabdomyolysis is higher in those with a body mass index > 40 kg/m2. Patients with sickle cell anemia may be at higher risk for exertional rhabdomyolysis.[7]",
"The most common symptoms are muscle weakness, myalgia, and dark-colored urine.[3] Severe cases of rhabdomyolysis can cause oliguria or even anuria. Cardiovascular symptoms can include cardiac arrhythmias or cardiac arrest; these often stem from severe electrolyte abnormalities.[2] Hypokalemia during strenuous physical activity can increase the risk for rhabdomyolysis, owing to low potassium levels restricting muscle vasodilation.[3] Asymptomatic elevations in creatine kinase levels can also occur. Myoglobulinemia and myoglobinuria may occur after strenuous physical activity.[3]",
"The diagnosis is established by checking serum creatine kinase levels. Urinalysis may reveal pigmented granular casts and a dark reddish-brown supernatant.[1] Urine dipstick reveals positive results for blood but no red cells, owing to the presence of myoglobin. Serum creatinine levels may be elevated. Other causes of dark tea-colored urine include hemoglobinuria, porphyria, bile pigments, food (eg, beets), and drugs (eg, rifampin, chloroquine).[1]",
"Complications of acute rhabdomyolysis include multiple electrolyte abnormalities (eg, hypocalcemia, hypercalcemia, hyperphosphatemia, hyperkalemia). The latter may require treatment. The most serious complication is acute renal failure. A large retrospective cohort study suggested that morbidity and mortality often depends on the underlying cause of rhabdomyolysis, with higher rates of in-hospital mortality or requirement of renal replacement therapy in patients with compartment syndrome, sepsis, neuroleptic malignant syndrome, cardiac arrest, and certain surgeries.[4]"
],
"date": "November 01, 2022",
"figures": [],
"markdown": "# A 22-Year-Old Football Player Who Collapsed Has Urine Changes\n\n **Authors:** Faizah Siddique, MD; Herbert S. Diamond, MD \n **Date:** November 01, 2022\n\n ## Content\n\n Rhabdomyolysis is often diagnosed on the basis of creatine kinase levels at least five times the upper limit of normal.[2] According to recommendations by the American College of Cardiology; the American Heart Association; and the National Heart, Lung, and Blood Institute, for rhabdomyolysis occurring in patients on lipid-lowering therapy, rhabdomyolysis is defined as a creatine kinase level more than 10 times the upper limit of normal.[6] Levels are often considerably higher.\nRecurrent cases of rhabdomyolysis without any precipitating trauma or exertion should raise suspicion of a genetic defect in metabolism. Defects in glycogen, lipid, mitochondria, and purine metabolism can cause rhabdomyolysis. Muscle biopsies should be obtained in these patients, with appropriate staining for diagnosis.\nThe mechanism of muscle cell destruction is direct injury to the muscle cell membrane, depletion of cellular energy due to hypoxia, or electrolyte disturbances that affect the sodium/potassium pump in the cell. Muscle injury results in leakage of extracellular calcium into the intracellular space, which eventually leads to muscle cell death and necrosis.[3] Once cellular necrosis occurs, cellular products, such as myoglobin, potassium, and creatine kinase, escape into the blood. Acute renal failure can result from massive deposition of muscle enzymes and myoglobin in the renal tubules.[3] Previous studies have suggested that acute renal failure can result from hypovolemia and aciduria.[3]\nRhabdomyolysis can occur at any age but is more frequent in individuals older than 60 years or younger than 10 years.[2] The risk for rhabdomyolysis is higher in those with a body mass index > 40 kg/m2. Patients with sickle cell anemia may be at higher risk for exertional rhabdomyolysis.[7]\nThe most common symptoms are muscle weakness, myalgia, and dark-colored urine.[3] Severe cases of rhabdomyolysis can cause oliguria or even anuria. Cardiovascular symptoms can include cardiac arrhythmias or cardiac arrest; these often stem from severe electrolyte abnormalities.[2] Hypokalemia during strenuous physical activity can increase the risk for rhabdomyolysis, owing to low potassium levels restricting muscle vasodilation.[3] Asymptomatic elevations in creatine kinase levels can also occur. Myoglobulinemia and myoglobinuria may occur after strenuous physical activity.[3]\nThe diagnosis is established by checking serum creatine kinase levels. Urinalysis may reveal pigmented granular casts and a dark reddish-brown supernatant.[1] Urine dipstick reveals positive results for blood but no red cells, owing to the presence of myoglobin. Serum creatinine levels may be elevated. Other causes of dark tea-colored urine include hemoglobinuria, porphyria, bile pigments, food (eg, beets), and drugs (eg, rifampin, chloroquine).[1]\nComplications of acute rhabdomyolysis include multiple electrolyte abnormalities (eg, hypocalcemia, hypercalcemia, hyperphosphatemia, hyperkalemia). The latter may require treatment. The most serious complication is acute renal failure. A large retrospective cohort study suggested that morbidity and mortality often depends on the underlying cause of rhabdomyolysis, with higher rates of in-hospital mortality or requirement of renal replacement therapy in patients with compartment syndrome, sepsis, neuroleptic malignant syndrome, cardiac arrest, and certain surgeries.[4]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A 22-Year-Old Football Player Who Collapsed Has Urine Changes"
},
{
"authors": "Faizah Siddique, MD; Herbert S. Diamond, MD",
"content": [
"The primary treatment for rhabdomyolysis is rapid initiation of intravenous (IV) fluids within 6 hours of admission.[3,8] No consensus guidelines suggest a specific type of fluid. Experimental studies have suggested benefit when mannitol is administered after IV saline resuscitation.[3] Alkalinization of urine with sodium bicarbonate may reduce the risk for renal damage.[3]",
"The patient was started on IV normal saline. At the time of discharge, his creatine kinase level had decreased to 1222 IU/L. His potassium level, which was checked 2 hours after IV fluid administration, was 3.9 mEq/L. With the seemingly popular rise of strenuous exercise programs, counseling patients regarding adequate hydration to reduce the risk for exercise-induced rhabdomyolysis is important.[9]"
],
"date": "November 01, 2022",
"figures": [],
"markdown": "# A 22-Year-Old Football Player Who Collapsed Has Urine Changes\n\n **Authors:** Faizah Siddique, MD; Herbert S. Diamond, MD \n **Date:** November 01, 2022\n\n ## Content\n\n The primary treatment for rhabdomyolysis is rapid initiation of intravenous (IV) fluids within 6 hours of admission.[3,8] No consensus guidelines suggest a specific type of fluid. Experimental studies have suggested benefit when mannitol is administered after IV saline resuscitation.[3] Alkalinization of urine with sodium bicarbonate may reduce the risk for renal damage.[3]\nThe patient was started on IV normal saline. At the time of discharge, his creatine kinase level had decreased to 1222 IU/L. His potassium level, which was checked 2 hours after IV fluid administration, was 3.9 mEq/L. With the seemingly popular rise of strenuous exercise programs, counseling patients regarding adequate hydration to reduce the risk for exercise-induced rhabdomyolysis is important.[9]\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1163824,
"choiceText": "Discontinue any causative medication, such as statins",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163826,
"choiceText": "Start IV fluids immediately",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163828,
"choiceText": "Perform ECG to evaluate for potassium toxicity",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163830,
"choiceText": "Perform muscle biopsy ",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163832,
"choiceText": "Administer mannitol\r\n",
"correct": false,
"displayOrder": 5,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Although discontinuing any offending agent is important, many patients are not due for their next dose of medication until many hours later. In the immediate setting, starting IV fluids can reduce the risk for renal damage and electrolyte complications. Serial ECGs are indicated to evaluate for potassium toxicity; however, IV fluid administration comes first. Mannitol may be useful as an addition to intravenous fluids if signs of renal failure are present and not quickly reversed. Muscle biopsy is not indicated.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 369879,
"questionText": "Which of the following is the best initial step in the management of rhabdomyolysis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1163834,
"choiceText": "Administration of bicarbonate",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163836,
"choiceText": "Vigorous hydration and electrolyte replacement",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163838,
"choiceText": "Use of a fan to enhance cooling though evaporation",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163840,
"choiceText": "Administration of mannitol",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Vigorous hydration to replace fluid loss is the best preventive measure. Use of bicarbonate or mannitol is not recommended. Evaporation does not occur readily when the humidity exceeds 75%. ",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 369881,
"questionText": "What is the best approach to preventing rhabdomyolysis with vigorous exercise in hot humid weather?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 22-Year-Old Football Player Who Collapsed Has Urine Changes"
},
{
"authors": "Faizah Siddique, MD; Herbert S. Diamond, MD",
"content": [],
"date": "November 01, 2022",
"figures": [],
"markdown": "# A 22-Year-Old Football Player Who Collapsed Has Urine Changes\n\n **Authors:** Faizah Siddique, MD; Herbert S. Diamond, MD \n **Date:** November 01, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1163824,
"choiceText": "Discontinue any causative medication, such as statins",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163826,
"choiceText": "Start IV fluids immediately",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163828,
"choiceText": "Perform ECG to evaluate for potassium toxicity",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163830,
"choiceText": "Perform muscle biopsy ",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163832,
"choiceText": "Administer mannitol\r\n",
"correct": false,
"displayOrder": 5,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Although discontinuing any offending agent is important, many patients are not due for their next dose of medication until many hours later. In the immediate setting, starting IV fluids can reduce the risk for renal damage and electrolyte complications. Serial ECGs are indicated to evaluate for potassium toxicity; however, IV fluid administration comes first. Mannitol may be useful as an addition to intravenous fluids if signs of renal failure are present and not quickly reversed. Muscle biopsy is not indicated.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 369879,
"questionText": "Which of the following is the best initial step in the management of rhabdomyolysis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1163834,
"choiceText": "Administration of bicarbonate",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163836,
"choiceText": "Vigorous hydration and electrolyte replacement",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163838,
"choiceText": "Use of a fan to enhance cooling though evaporation",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163840,
"choiceText": "Administration of mannitol",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Vigorous hydration to replace fluid loss is the best preventive measure. Use of bicarbonate or mannitol is not recommended. Evaporation does not occur readily when the humidity exceeds 75%. ",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 369881,
"questionText": "What is the best approach to preventing rhabdomyolysis with vigorous exercise in hot humid weather?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 22-Year-Old Football Player Who Collapsed Has Urine Changes"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1163814,
"choiceText": "Intravascular hemolysis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163816,
"choiceText": "Septicemia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163818,
"choiceText": "Heat stroke or exercise-induced rhabdomyolysis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163820,
"choiceText": "Polymyositis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163822,
"choiceText": "Genetic dystrophy-induced rhabdomyolysis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 369877,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1163824,
"choiceText": "Discontinue any causative medication, such as statins",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163826,
"choiceText": "Start IV fluids immediately",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163828,
"choiceText": "Perform ECG to evaluate for potassium toxicity",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163830,
"choiceText": "Perform muscle biopsy ",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163832,
"choiceText": "Administer mannitol\r\n",
"correct": false,
"displayOrder": 5,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Although discontinuing any offending agent is important, many patients are not due for their next dose of medication until many hours later. In the immediate setting, starting IV fluids can reduce the risk for renal damage and electrolyte complications. Serial ECGs are indicated to evaluate for potassium toxicity; however, IV fluid administration comes first. Mannitol may be useful as an addition to intravenous fluids if signs of renal failure are present and not quickly reversed. Muscle biopsy is not indicated.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 369879,
"questionText": "Which of the following is the best initial step in the management of rhabdomyolysis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1163834,
"choiceText": "Administration of bicarbonate",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163836,
"choiceText": "Vigorous hydration and electrolyte replacement",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163838,
"choiceText": "Use of a fan to enhance cooling though evaporation",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1163840,
"choiceText": "Administration of mannitol",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Vigorous hydration to replace fluid loss is the best preventive measure. Use of bicarbonate or mannitol is not recommended. Evaporation does not occur readily when the humidity exceeds 75%. ",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 369881,
"questionText": "What is the best approach to preventing rhabdomyolysis with vigorous exercise in hot humid weather?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
871259 | /viewarticle/871259 | [
{
"authors": "Tiffany Kwok, BHSc; Benjamin Barankin, MD, FRCPC",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us",
"A 45-year-old woman presents to the emergency department (ED) with a 2-day history of an acute-onset, mildly pruritic rash. The rash started in her axillae and groin and has since progressed to the rest of her body. She then developed a fever.",
"She was diagnosed with pneumonia 4 days ago and has been taking azithromycin since that time. She was previously in good health, and her past medical history and family history are negative for psoriasis, arthritis, and other significant medical conditions. She has no known history of drug allergies. She does not smoke and drinks an average of two glasses of wine each week. She is a teacher, and she has two young children at home."
],
"date": "October 21, 2022",
"figures": [],
"markdown": "# A 45-Year-Old Teacher With a Groin Rash That Is Spreading\n\n **Authors:** Tiffany Kwok, BHSc; Benjamin Barankin, MD, FRCPC \n **Date:** October 21, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us\nA 45-year-old woman presents to the emergency department (ED) with a 2-day history of an acute-onset, mildly pruritic rash. The rash started in her axillae and groin and has since progressed to the rest of her body. She then developed a fever.\nShe was diagnosed with pneumonia 4 days ago and has been taking azithromycin since that time. She was previously in good health, and her past medical history and family history are negative for psoriasis, arthritis, and other significant medical conditions. She has no known history of drug allergies. She does not smoke and drinks an average of two glasses of wine each week. She is a teacher, and she has two young children at home.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A 45-Year-Old Teacher With a Groin Rash That Is Spreading"
},
{
"authors": "Tiffany Kwok, BHSc; Benjamin Barankin, MD, FRCPC",
"content": [
"Upon physical examination, the patient appears to be in no acute distress. Her vital signs include a temperature of 102° F (38.9° C), a pulse rate of 88 beats/min, a blood pressure of 124/76 mm Hg, and a respiratory rate of 16 breaths/min. Fine crackles are auscultated in the left lower lung field. A complete skin examination reveals hundreds of nonfollicular pustules on erythematous bases diffusely spread over her face, trunk, axillae, groin, arms, and legs (see Figure below). The lesions are without any crust or scale. No lesions are observed on her palms, soles, or mucous membranes. The remainder of the physical examination is unremarkable.",
"Figure.",
"Laboratory tests are obtained. The white blood cell count is elevated at 16 × 109 cells/L (reference range, 4.3-10.8 × 109 cells/L), with a moderately elevated total neutrophil count of 14 × 109 cells/L (reference range, 1.3-6.7 × 109 mg/L) and a slightly elevated eosinophil count of 0.37 × 109 cells/L (normal range, 0.0-0.3 × 109 cells/L). The C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) are also elevated, at 84 mg/L (reference range, < 10 mg/L) and 34 mm/hr (normal range, 0-19 mm/hr), respectively.",
"Blood cultures are positive for Mycoplasma pneumoniae but negative for additional bacteria or fungi. Culture and Gram stain of several pustules are obtained and are negative. A punch biopsy of a pustule on her leg is performed. The histology shows spongiform subcorneal pustules, edema of the papillary dermis, marked perivascular infiltration of neutrophils, and exocytosis of a few eosinophils."
],
"date": "October 21, 2022",
"figures": [
{
"caption": "Figure.",
"image_url": "https://img.medscapestatic.com/article/871/259/871259-Thumb1.jpg"
}
],
"markdown": "# A 45-Year-Old Teacher With a Groin Rash That Is Spreading\n\n **Authors:** Tiffany Kwok, BHSc; Benjamin Barankin, MD, FRCPC \n **Date:** October 21, 2022\n\n ## Content\n\n Upon physical examination, the patient appears to be in no acute distress. Her vital signs include a temperature of 102° F (38.9° C), a pulse rate of 88 beats/min, a blood pressure of 124/76 mm Hg, and a respiratory rate of 16 breaths/min. Fine crackles are auscultated in the left lower lung field. A complete skin examination reveals hundreds of nonfollicular pustules on erythematous bases diffusely spread over her face, trunk, axillae, groin, arms, and legs (see Figure below). The lesions are without any crust or scale. No lesions are observed on her palms, soles, or mucous membranes. The remainder of the physical examination is unremarkable.\nFigure.\nLaboratory tests are obtained. The white blood cell count is elevated at 16 × 109 cells/L (reference range, 4.3-10.8 × 109 cells/L), with a moderately elevated total neutrophil count of 14 × 109 cells/L (reference range, 1.3-6.7 × 109 mg/L) and a slightly elevated eosinophil count of 0.37 × 109 cells/L (normal range, 0.0-0.3 × 109 cells/L). The C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) are also elevated, at 84 mg/L (reference range, < 10 mg/L) and 34 mm/hr (normal range, 0-19 mm/hr), respectively.\nBlood cultures are positive for Mycoplasma pneumoniae but negative for additional bacteria or fungi. Culture and Gram stain of several pustules are obtained and are negative. A punch biopsy of a pustule on her leg is performed. The histology shows spongiform subcorneal pustules, edema of the papillary dermis, marked perivascular infiltration of neutrophils, and exocytosis of a few eosinophils.\n\n ## Figures\n\n **Figure.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1031076,
"choiceText": "Acute generalized exanthematous pustulosis",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031078,
"choiceText": "Leukocytoclastic vasculitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031080,
"choiceText": "Pustular psoriasis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031082,
"choiceText": "Subcorneal pustular dermatosis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031084,
"choiceText": "Toxic epidermal necrolysis\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 326309,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 45-Year-Old Teacher With a Groin Rash That Is Spreading"
},
{
"authors": "Tiffany Kwok, BHSc; Benjamin Barankin, MD, FRCPC",
"content": [
"Acute generalized exanthematous pustulosis (AGEP) is a cutaneous eruption in which dozens to hundreds of sterile nonfollicular pustules on edematous and erythematous bases appear acutely on the skin. Dermatologic symptoms are almost always accompanied by fever and neutrophilic leukocytosis. Usually linked to drug intake, most reactions resolve rapidly and spontaneously after discontinuation of the responsible drug.",
"AGEP is unusual, and no good estimate of its incidence is available. Registries of AGEP cases reported mostly in Europe have found that this entity affects individuals of all ages (6-85 years), with no significant predilection for sex.[1,2] Ninety percent of cases have been associated with drug ingestion, namely beta-lactam drugs and macrolides (as with our patient).[1,2,3,4] Other implicated drug classes include antimycotics, calcium-channel blockers, mercury, nonsteroidal anti-inflammatory drugs (NSAIDs), carbamazepine, and acetaminophen.",
"Of note, AGEP has not been commonly attributed to sulfonamides, a frequent cause of other cutaneous drug reactions. Reactions to viral infections, such as enteroviruses and parvovirus B19, have also been noted in many cases.[1,2,4,5] One study found that patients with AGEP eruptions were more likely to have human leukocyte antigen haplotypes B51 (HLA-B51), DR11 (HLA-DR11), and DQ3 (HLA-DQ3).[6]",
"The pathogenesis of AGEP is unknown, but it may be linked with type III and IV hypersensitivity reactions. The association with type IV hypersensitivity may explain the delayed reaction in some cases, whereby patients have either used the offending drug in the past with no problems or they have used the drug for 1-3 weeks before symptoms appear. Previous research has noted an association with neutrophil-promoting cytokines interleukin (IL)-3 and IL-8, released by T cells. AGEP shows a high rate of concordance with lymphocyte transformation tests and positive patch testing to an offending drug. Another possible mechanism involves the offending drug or infection producing antigen-antibody complexes that activate the complement system, which causes neutrophil chemotaxis.[3,4]",
"Clinically, an acute onset of reaction (average time to reaction, 2.5 days; range, 3 hours to over 3 weeks) occurs after drug ingestion, first manifesting as an edematous erythema, which may cause burning or pruritus. Shortly after, dozens to hundreds of sterile nonfollicular pustules arise in the folds of the skin, later generalizing to the rest of the body. A fever above 100.4° F (38° C) develops soon after the appearance of the pustules."
],
"date": "October 21, 2022",
"figures": [],
"markdown": "# A 45-Year-Old Teacher With a Groin Rash That Is Spreading\n\n **Authors:** Tiffany Kwok, BHSc; Benjamin Barankin, MD, FRCPC \n **Date:** October 21, 2022\n\n ## Content\n\n Acute generalized exanthematous pustulosis (AGEP) is a cutaneous eruption in which dozens to hundreds of sterile nonfollicular pustules on edematous and erythematous bases appear acutely on the skin. Dermatologic symptoms are almost always accompanied by fever and neutrophilic leukocytosis. Usually linked to drug intake, most reactions resolve rapidly and spontaneously after discontinuation of the responsible drug.\nAGEP is unusual, and no good estimate of its incidence is available. Registries of AGEP cases reported mostly in Europe have found that this entity affects individuals of all ages (6-85 years), with no significant predilection for sex.[1,2] Ninety percent of cases have been associated with drug ingestion, namely beta-lactam drugs and macrolides (as with our patient).[1,2,3,4] Other implicated drug classes include antimycotics, calcium-channel blockers, mercury, nonsteroidal anti-inflammatory drugs (NSAIDs), carbamazepine, and acetaminophen.\nOf note, AGEP has not been commonly attributed to sulfonamides, a frequent cause of other cutaneous drug reactions. Reactions to viral infections, such as enteroviruses and parvovirus B19, have also been noted in many cases.[1,2,4,5] One study found that patients with AGEP eruptions were more likely to have human leukocyte antigen haplotypes B51 (HLA-B51), DR11 (HLA-DR11), and DQ3 (HLA-DQ3).[6]\nThe pathogenesis of AGEP is unknown, but it may be linked with type III and IV hypersensitivity reactions. The association with type IV hypersensitivity may explain the delayed reaction in some cases, whereby patients have either used the offending drug in the past with no problems or they have used the drug for 1-3 weeks before symptoms appear. Previous research has noted an association with neutrophil-promoting cytokines interleukin (IL)-3 and IL-8, released by T cells. AGEP shows a high rate of concordance with lymphocyte transformation tests and positive patch testing to an offending drug. Another possible mechanism involves the offending drug or infection producing antigen-antibody complexes that activate the complement system, which causes neutrophil chemotaxis.[3,4]\nClinically, an acute onset of reaction (average time to reaction, 2.5 days; range, 3 hours to over 3 weeks) occurs after drug ingestion, first manifesting as an edematous erythema, which may cause burning or pruritus. Shortly after, dozens to hundreds of sterile nonfollicular pustules arise in the folds of the skin, later generalizing to the rest of the body. A fever above 100.4° F (38° C) develops soon after the appearance of the pustules.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1031076,
"choiceText": "Acute generalized exanthematous pustulosis",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031078,
"choiceText": "Leukocytoclastic vasculitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031080,
"choiceText": "Pustular psoriasis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031082,
"choiceText": "Subcorneal pustular dermatosis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031084,
"choiceText": "Toxic epidermal necrolysis\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 326309,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 45-Year-Old Teacher With a Groin Rash That Is Spreading"
},
{
"authors": "Tiffany Kwok, BHSc; Benjamin Barankin, MD, FRCPC",
"content": [
"Roujeau and colleagues[5] established five hallmark features of AGEP after a 1991 retrospective review of 63 cases, which have been widely used to form a working definition; however, this list of features is not considered diagnostic because its specificity remains to be tested. Sidoroff and coworkers[1] further elaborated on this list, creating a more detailed scoring system as a result of an analysis of up to 150 additional patients in Europe. The hallmark criteria of AGEP are [5]:",
"Dozens of small, nonfollicular pustules on widespread edematous erythema",
"Histopathology showing spongiform subcorneal and/or intraepidermal pustules, marked edema of papillary dermis, and perivascular infiltrates with neutrophils and exocytosis of some eosinophils",
"Fever > 100.4° F (38° C)",
"Blood neutrophil counts > 7 × 109 cells/L",
"Acute evolution with spontaneous resolution of pustules in less than 15 days",
"Less common presentations of AGEP may include confluence of pustules with a positive Nikolsky sign, marked edema of the face, purpuric lesions on the legs, and target lesions similar to those observed in Stevens-Johnson syndrome.",
"Many cutaneous diseases or reactions may cause pustular eruptions and mimic AGEP. Pustular conditions such as acne, bacterial folliculitis, dermatophyte infections, varicella, and localized pustular contact dermatitis can be differentiated from AGEP when considering clinical features and associated laboratory test results. Entities that are often challenging to differentiate from AGEP include pustular psoriasis, subcorneal pustular dermatosis, drug hypersensitivity syndrome, and toxic epidermal necrolysis (TEN). In particular, controversy has surrounded the differentiation of AGEP and pustular psoriasis, but Sidoroff and colleagues[3] compiled differences between AGEP and pustular psoriasis (Table).",
"Differences Between AGEP and Pustular Psoriasis",
"AGEP",
"Pustular Psoriasis",
"History of psoriasis",
"Possible",
"Mostly",
"Distribution pattern",
"Predominance in the folds",
"More generalized",
"Duration of pustules",
"Shorter",
"Longer",
"Duration of fever",
"Shorter",
"Longer",
"History of drug reaction",
"Usual",
"Uncommon",
"Recent drug administration",
"Very frequent",
"Less frequent",
"Arthritis",
"Rare",
"~30%",
"Histology",
"Spongiform subcorneal and/or intraepidermal pustules, edema of papillary dermis, vasculitis, exocytosis of eosinophils, and single-cell necrosis of keratinocytes",
"Subcorneal and/or intraepidermal pustules, papillomatosis, and acanthosis",
"Of note, almost all individuals who present with pustular psoriasis have a history of psoriasis. Although several cases of AGEP have occurred in individuals with psoriasis, lack of a personal and family history of psoriasis should generally point the clinician away from a diagnosis of pustular psoriasis. Subcorneal pustular dermatosis, or Sneddon-Wilkinson disease, is typically characterized by larger flaccid blisters with a more gradual onset. Drug hypersensitivity syndrome often shows an acute pustular eruption and fever, as well as lymphadenopathy, eosinophilia, and systemic symptoms (such as hepatitis, nephritis, pneumonitis, and myocarditis) not seen in AGEP.",
"Finally, the confluence of pustules and atypical target lesions seen in AGEP may mimic a positive Nikolsky sign and may suggest a diagnosis of TEN; however, mucous membrane involvement is more pronounced and epidermal detachment is deeper in cases of TEN. The histologic findings, discussed later, show significant differences between these entities, and they can be used to confirm the diagnosis.",
"AGEP is often a combined clinical and histologic diagnosis. A biopsy of a pustule and blood counts should always be conducted in patients with suspected AGEP. Classic histology findings will show spongiform subcorneal and/or intraepidermal pustules with papillary edema, although nonspongiform variants and absence of papillary edema have been noted in past cases. Blood counts will show leukocytosis, particularly blood neutrophil levels greater than 7 × 109 cells/L (reference range, 1.3-6.7 × 109 cells/L), and, less commonly, eosinophilia (reference range, 0.0-0.3 × 109 cells/L). The leukocytosis peaks on day 4 and persists for approximately 12 days. Hypoalbuminemia, hypocalcemia, mild transaminitis, prerenal azotemia, and increased ESR have all been described in patients with AGEP. Testing for these findings is not particularly useful, however, because their presence is very nonspecific, which renders these findings nondiagnostic."
],
"date": "October 21, 2022",
"figures": [],
"markdown": "# A 45-Year-Old Teacher With a Groin Rash That Is Spreading\n\n **Authors:** Tiffany Kwok, BHSc; Benjamin Barankin, MD, FRCPC \n **Date:** October 21, 2022\n\n ## Content\n\n Roujeau and colleagues[5] established five hallmark features of AGEP after a 1991 retrospective review of 63 cases, which have been widely used to form a working definition; however, this list of features is not considered diagnostic because its specificity remains to be tested. Sidoroff and coworkers[1] further elaborated on this list, creating a more detailed scoring system as a result of an analysis of up to 150 additional patients in Europe. The hallmark criteria of AGEP are [5]:\nDozens of small, nonfollicular pustules on widespread edematous erythema\nHistopathology showing spongiform subcorneal and/or intraepidermal pustules, marked edema of papillary dermis, and perivascular infiltrates with neutrophils and exocytosis of some eosinophils\nFever > 100.4° F (38° C)\nBlood neutrophil counts > 7 × 109 cells/L\nAcute evolution with spontaneous resolution of pustules in less than 15 days\nLess common presentations of AGEP may include confluence of pustules with a positive Nikolsky sign, marked edema of the face, purpuric lesions on the legs, and target lesions similar to those observed in Stevens-Johnson syndrome.\nMany cutaneous diseases or reactions may cause pustular eruptions and mimic AGEP. Pustular conditions such as acne, bacterial folliculitis, dermatophyte infections, varicella, and localized pustular contact dermatitis can be differentiated from AGEP when considering clinical features and associated laboratory test results. Entities that are often challenging to differentiate from AGEP include pustular psoriasis, subcorneal pustular dermatosis, drug hypersensitivity syndrome, and toxic epidermal necrolysis (TEN). In particular, controversy has surrounded the differentiation of AGEP and pustular psoriasis, but Sidoroff and colleagues[3] compiled differences between AGEP and pustular psoriasis (Table).\nDifferences Between AGEP and Pustular Psoriasis\nAGEP\nPustular Psoriasis\nHistory of psoriasis\nPossible\nMostly\nDistribution pattern\nPredominance in the folds\nMore generalized\nDuration of pustules\nShorter\nLonger\nDuration of fever\nShorter\nLonger\nHistory of drug reaction\nUsual\nUncommon\nRecent drug administration\nVery frequent\nLess frequent\nArthritis\nRare\n~30%\nHistology\nSpongiform subcorneal and/or intraepidermal pustules, edema of papillary dermis, vasculitis, exocytosis of eosinophils, and single-cell necrosis of keratinocytes\nSubcorneal and/or intraepidermal pustules, papillomatosis, and acanthosis\nOf note, almost all individuals who present with pustular psoriasis have a history of psoriasis. Although several cases of AGEP have occurred in individuals with psoriasis, lack of a personal and family history of psoriasis should generally point the clinician away from a diagnosis of pustular psoriasis. Subcorneal pustular dermatosis, or Sneddon-Wilkinson disease, is typically characterized by larger flaccid blisters with a more gradual onset. Drug hypersensitivity syndrome often shows an acute pustular eruption and fever, as well as lymphadenopathy, eosinophilia, and systemic symptoms (such as hepatitis, nephritis, pneumonitis, and myocarditis) not seen in AGEP.\nFinally, the confluence of pustules and atypical target lesions seen in AGEP may mimic a positive Nikolsky sign and may suggest a diagnosis of TEN; however, mucous membrane involvement is more pronounced and epidermal detachment is deeper in cases of TEN. The histologic findings, discussed later, show significant differences between these entities, and they can be used to confirm the diagnosis.\nAGEP is often a combined clinical and histologic diagnosis. A biopsy of a pustule and blood counts should always be conducted in patients with suspected AGEP. Classic histology findings will show spongiform subcorneal and/or intraepidermal pustules with papillary edema, although nonspongiform variants and absence of papillary edema have been noted in past cases. Blood counts will show leukocytosis, particularly blood neutrophil levels greater than 7 × 109 cells/L (reference range, 1.3-6.7 × 109 cells/L), and, less commonly, eosinophilia (reference range, 0.0-0.3 × 109 cells/L). The leukocytosis peaks on day 4 and persists for approximately 12 days. Hypoalbuminemia, hypocalcemia, mild transaminitis, prerenal azotemia, and increased ESR have all been described in patients with AGEP. Testing for these findings is not particularly useful, however, because their presence is very nonspecific, which renders these findings nondiagnostic.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A 45-Year-Old Teacher With a Groin Rash That Is Spreading"
},
{
"authors": "Tiffany Kwok, BHSc; Benjamin Barankin, MD, FRCPC",
"content": [
"The provocation method is the most definitive way to investigate potential offending drugs, but it is usually avoided because of the risk for an increasingly severe eruption posed to the patient. As a result of a questionable association with T cells, patch testing may have a limited role in the diagnosis of AGEP and the determination of the offending drug. Some patients with AGEP have positive prick-test findings for the drug to which they reacted. These methods are not diagnostic, though, and most patients with AGEP do not display positive patch or prick tests. Blood cultures for bacteria and fungi as well as bacterial swabs of the pustules are negative for microbes, which is useful in ruling out an infectious etiology. In vitro studies, such as the macrophage migration inhibition factor and mast-cell degranulation tests, have helped to detect causative drugs in AGEP, although they are seldom performed in a clinical setting.",
"AGEP is a benign disease following a self-limited course. Pustules resolve spontaneously within 4-10 days and are often followed by a characteristic postpustular pinpoint desquamation. The prognosis of AGEP is excellent, although the uncommon superinfection is a potentially serious complication.[3]",
"Drug-induced AGEP responds well to discontinuation of the offending drug, and skin changes will diminish and eventually resolve completely, often within 14 days. Management includes topical corticosteroids, antihistamines, and antipyretics to relieve symptoms. Less commonly, systemic steroids may be employed if the symptoms are severe.",
"The patient in the case was found to have azithromycin-induced AGEP. Upon discontinuation of the drug, her skin eruption completely cleared within 5 days, and her fever and neutrophilia diminished. She was treated with mild topical steroids and emollients to ease her pruritus."
],
"date": "October 21, 2022",
"figures": [],
"markdown": "# A 45-Year-Old Teacher With a Groin Rash That Is Spreading\n\n **Authors:** Tiffany Kwok, BHSc; Benjamin Barankin, MD, FRCPC \n **Date:** October 21, 2022\n\n ## Content\n\n The provocation method is the most definitive way to investigate potential offending drugs, but it is usually avoided because of the risk for an increasingly severe eruption posed to the patient. As a result of a questionable association with T cells, patch testing may have a limited role in the diagnosis of AGEP and the determination of the offending drug. Some patients with AGEP have positive prick-test findings for the drug to which they reacted. These methods are not diagnostic, though, and most patients with AGEP do not display positive patch or prick tests. Blood cultures for bacteria and fungi as well as bacterial swabs of the pustules are negative for microbes, which is useful in ruling out an infectious etiology. In vitro studies, such as the macrophage migration inhibition factor and mast-cell degranulation tests, have helped to detect causative drugs in AGEP, although they are seldom performed in a clinical setting.\nAGEP is a benign disease following a self-limited course. Pustules resolve spontaneously within 4-10 days and are often followed by a characteristic postpustular pinpoint desquamation. The prognosis of AGEP is excellent, although the uncommon superinfection is a potentially serious complication.[3]\nDrug-induced AGEP responds well to discontinuation of the offending drug, and skin changes will diminish and eventually resolve completely, often within 14 days. Management includes topical corticosteroids, antihistamines, and antipyretics to relieve symptoms. Less commonly, systemic steroids may be employed if the symptoms are severe.\nThe patient in the case was found to have azithromycin-induced AGEP. Upon discontinuation of the drug, her skin eruption completely cleared within 5 days, and her fever and neutrophilia diminished. She was treated with mild topical steroids and emollients to ease her pruritus.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1031086,
"choiceText": "Enterovirus",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031088,
"choiceText": "Mercury",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031090,
"choiceText": "Parvovirus B19",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031092,
"choiceText": "Penicillin V",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031094,
"choiceText": "Sulfasalazine\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Beta-lactams (eg, penicillin V) are the most common causes of AGEP. Enterovirus, mercury, and parvovirus B19 have all been implicated in some instances of AGEP but are not as common. Although sulfonamides (eg, sulfasalazine) are implicated in many cutaneous drug reactions, they are a very uncommon cause of AGEP.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 326311,
"questionText": "Which of these is the most common trigger for AGEP?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1031096,
"choiceText": "Oral erosions",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031098,
"choiceText": "Leukopenia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031100,
"choiceText": "Fever",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031102,
"choiceText": "Neutropenia",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031104,
"choiceText": "Persistence of rash longer than a month after discontinuation of responsible drug",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "AGEP is a cutaneous eruption in which dozens to hundreds of sterile nonfollicular pustules on edematous and erythematous bases appear acutely on the skin. Dermatologic symptoms are almost always accompanied by fever and neutrophilic leukocytosis. Usually linked to drug intake, most reactions resolve rapidly and spontaneously after discontinuation of the responsible drug.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 326313,
"questionText": "Which is more commonly associated with AGEP?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 45-Year-Old Teacher With a Groin Rash That Is Spreading"
},
{
"authors": "Tiffany Kwok, BHSc; Benjamin Barankin, MD, FRCPC",
"content": [],
"date": "October 21, 2022",
"figures": [],
"markdown": "# A 45-Year-Old Teacher With a Groin Rash That Is Spreading\n\n **Authors:** Tiffany Kwok, BHSc; Benjamin Barankin, MD, FRCPC \n **Date:** October 21, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1031086,
"choiceText": "Enterovirus",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031088,
"choiceText": "Mercury",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031090,
"choiceText": "Parvovirus B19",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031092,
"choiceText": "Penicillin V",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031094,
"choiceText": "Sulfasalazine\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Beta-lactams (eg, penicillin V) are the most common causes of AGEP. Enterovirus, mercury, and parvovirus B19 have all been implicated in some instances of AGEP but are not as common. Although sulfonamides (eg, sulfasalazine) are implicated in many cutaneous drug reactions, they are a very uncommon cause of AGEP.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 326311,
"questionText": "Which of these is the most common trigger for AGEP?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1031096,
"choiceText": "Oral erosions",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031098,
"choiceText": "Leukopenia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031100,
"choiceText": "Fever",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031102,
"choiceText": "Neutropenia",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031104,
"choiceText": "Persistence of rash longer than a month after discontinuation of responsible drug",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "AGEP is a cutaneous eruption in which dozens to hundreds of sterile nonfollicular pustules on edematous and erythematous bases appear acutely on the skin. Dermatologic symptoms are almost always accompanied by fever and neutrophilic leukocytosis. Usually linked to drug intake, most reactions resolve rapidly and spontaneously after discontinuation of the responsible drug.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 326313,
"questionText": "Which is more commonly associated with AGEP?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 45-Year-Old Teacher With a Groin Rash That Is Spreading"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1031076,
"choiceText": "Acute generalized exanthematous pustulosis",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031078,
"choiceText": "Leukocytoclastic vasculitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031080,
"choiceText": "Pustular psoriasis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031082,
"choiceText": "Subcorneal pustular dermatosis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031084,
"choiceText": "Toxic epidermal necrolysis\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 326309,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1031086,
"choiceText": "Enterovirus",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031088,
"choiceText": "Mercury",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031090,
"choiceText": "Parvovirus B19",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031092,
"choiceText": "Penicillin V",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031094,
"choiceText": "Sulfasalazine\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Beta-lactams (eg, penicillin V) are the most common causes of AGEP. Enterovirus, mercury, and parvovirus B19 have all been implicated in some instances of AGEP but are not as common. Although sulfonamides (eg, sulfasalazine) are implicated in many cutaneous drug reactions, they are a very uncommon cause of AGEP.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 326311,
"questionText": "Which of these is the most common trigger for AGEP?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1031096,
"choiceText": "Oral erosions",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031098,
"choiceText": "Leukopenia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031100,
"choiceText": "Fever",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031102,
"choiceText": "Neutropenia",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1031104,
"choiceText": "Persistence of rash longer than a month after discontinuation of responsible drug",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "AGEP is a cutaneous eruption in which dozens to hundreds of sterile nonfollicular pustules on edematous and erythematous bases appear acutely on the skin. Dermatologic symptoms are almost always accompanied by fever and neutrophilic leukocytosis. Usually linked to drug intake, most reactions resolve rapidly and spontaneously after discontinuation of the responsible drug.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 326313,
"questionText": "Which is more commonly associated with AGEP?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
847975 | /viewarticle/847975 | [
{
"authors": "Carla R. Sterling, MD; Niccole Bart, MD",
"content": [
"Editor's Note:\n\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.",
"A 67-year-old man presents to the emergency department at the behest of his home health aide because she noticed he was wheezing. The aide is not sure when the wheezing started, but first noticed it while she was preparing his breakfast. She comes in the mornings, and another home health aide stays overnight. The overnight aide did not report any events to the morning aide.",
"The patient received two albuterol treatments and 10 mg of dexamethasone intramuscularly in the ambulance on the way to the hospital, with no improvement. The emergency medical service (EMS) performed an ECG that revealed no ST elevations.",
"His medical history includes hypertension; emphysema; myocardial infarction (two stents); and a cerebrovascular accident 5 years ago, with residual deficits involving left-sided hemiparesis, speech difficulty, and an inability to perform activities of daily living on his own. He takes enalapril, hydrochlorothiazide, aspirin, tiotropium bromide, quetiapine, and sertraline. He also uses continuous positive airway pressure ventilation at night.",
"The patient is nonverbal at baseline. His aide explains that she has been working with him for 8 months and thinks that today he has increased work of breathing. He has also been rubbing his chest."
],
"date": "October 19, 2022",
"figures": [],
"markdown": "# Emergency Med Case Challenge: Pain, Wheezing in a Nonverbal Man Who Keeps Rubbing His Chest\n\n **Authors:** Carla R. Sterling, MD; Niccole Bart, MD \n **Date:** October 19, 2022\n\n ## Content\n\n Editor's Note:\n\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.\nA 67-year-old man presents to the emergency department at the behest of his home health aide because she noticed he was wheezing. The aide is not sure when the wheezing started, but first noticed it while she was preparing his breakfast. She comes in the mornings, and another home health aide stays overnight. The overnight aide did not report any events to the morning aide.\nThe patient received two albuterol treatments and 10 mg of dexamethasone intramuscularly in the ambulance on the way to the hospital, with no improvement. The emergency medical service (EMS) performed an ECG that revealed no ST elevations.\nHis medical history includes hypertension; emphysema; myocardial infarction (two stents); and a cerebrovascular accident 5 years ago, with residual deficits involving left-sided hemiparesis, speech difficulty, and an inability to perform activities of daily living on his own. He takes enalapril, hydrochlorothiazide, aspirin, tiotropium bromide, quetiapine, and sertraline. He also uses continuous positive airway pressure ventilation at night.\nThe patient is nonverbal at baseline. His aide explains that she has been working with him for 8 months and thinks that today he has increased work of breathing. He has also been rubbing his chest.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Emergency Med Case Challenge: Pain, Wheezing in a Nonverbal Man Who Keeps Rubbing His Chest"
},
{
"authors": "Carla R. Sterling, MD; Niccole Bart, MD",
"content": [
"Upon initial assessment, the patient is an elderly, frail-appearing man with no acute respiratory distress. His vitals include a heart rate of 106 beats/min, blood pressure of 137/87 mm Hg, respiratory rate of 23 breaths/min, and oxygen saturation of 94% on a 2-L nasal cannula.",
"His ECG is unchanged from the ECG obtained by the EMS. Physical examination reveals S1 and S2 with crescendo/decrescendo systolic murmur, bilateral basilar crackles in his posterior lungs, and wheezing, with a slightly prolonged expiratory phase. He has bilateral and symmetrical pitting edema of the lower extremities to the mid-shin.",
"The patient's laboratory findings are unremarkable, including complete blood cell count, comprehensive medical panel, B-type natriuretic peptide, and cardiac enzymes. A shock panel shows an increased CO2 level and lactate level of 2.6 mg/dL (reference range, 4.5-19.8 mg/dL). Another round of albuterol and ipratropium is administered to treat a potential exacerbation of chronic obstructive pulmonary disease (COPD); however, no improvement in symptoms is noted.",
"At this point, the patient has received three doses of ipratropium and dexamethasone without improvement. His tachycardia resolves when he is resting comfortably, but any activity increases his heart rate. CT of the pulmonary vessels is considered, as is bedside echocardiography, bilevel positive airway pressure, and intubation.",
"Chest radiography reveals nonspecific atelectasis changes (Figures 1 and 2).",
"Figure 1.",
"Figure 1.",
"Figure 2.",
"Figure 2."
],
"date": "October 19, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/847/975/847975-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/847/975/847975-Thumb2.png"
}
],
"markdown": "# Emergency Med Case Challenge: Pain, Wheezing in a Nonverbal Man Who Keeps Rubbing His Chest\n\n **Authors:** Carla R. Sterling, MD; Niccole Bart, MD \n **Date:** October 19, 2022\n\n ## Content\n\n Upon initial assessment, the patient is an elderly, frail-appearing man with no acute respiratory distress. His vitals include a heart rate of 106 beats/min, blood pressure of 137/87 mm Hg, respiratory rate of 23 breaths/min, and oxygen saturation of 94% on a 2-L nasal cannula.\nHis ECG is unchanged from the ECG obtained by the EMS. Physical examination reveals S1 and S2 with crescendo/decrescendo systolic murmur, bilateral basilar crackles in his posterior lungs, and wheezing, with a slightly prolonged expiratory phase. He has bilateral and symmetrical pitting edema of the lower extremities to the mid-shin.\nThe patient's laboratory findings are unremarkable, including complete blood cell count, comprehensive medical panel, B-type natriuretic peptide, and cardiac enzymes. A shock panel shows an increased CO2 level and lactate level of 2.6 mg/dL (reference range, 4.5-19.8 mg/dL). Another round of albuterol and ipratropium is administered to treat a potential exacerbation of chronic obstructive pulmonary disease (COPD); however, no improvement in symptoms is noted.\nAt this point, the patient has received three doses of ipratropium and dexamethasone without improvement. His tachycardia resolves when he is resting comfortably, but any activity increases his heart rate. CT of the pulmonary vessels is considered, as is bedside echocardiography, bilevel positive airway pressure, and intubation.\nChest radiography reveals nonspecific atelectasis changes (Figures 1 and 2).\nFigure 1.\nFigure 1.\nFigure 2.\nFigure 2.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 869711,
"choiceText": "COPD exacerbation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869713,
"choiceText": "New-onset congestive heart failure",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869715,
"choiceText": "Foreign body aspiration",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869717,
"choiceText": "Pulmonary embolism",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 273657,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Emergency Med Case Challenge: Pain, Wheezing in a Nonverbal Man Who Keeps Rubbing His Chest"
},
{
"authors": "Carla R. Sterling, MD; Niccole Bart, MD",
"content": [
"The patient was admitted for presumed pneumonia, and antibiotic coverage for community-acquired pneumonia was started with ceftriaxone and azithromycin. While he was in the emergency department, he had a coughing fit and experienced an acute drop in consciousness and oxygen saturation, with not only cessation of wheezing but also loss of breath sounds. He was urgently intubated and transferred to the intensive care unit. A chest radiograph was obtained (Figure 3).",
"Figure 3.",
"Figure 3.",
"CT of the chest revealed an obstruction with collapse of the lobe. The critical care pulmonologist performed bronchoscopy and the obstruction was removed, with improvement in respiratory function and subsequent imaging studies revealing reexpansion of the lobe. Oxygenation improved, and the patient was extubated the following morning.",
"After 24 hours with stable respiratory function and vital signs, the patient was transferred to the medicine floor, where he was continued on pneumonia treatment and eventually discharged to his home at his baseline state. Aspirated foreign bodies are more common in children than adults. In general, 50% of all foreign body cases occur in children younger than 4 years.[1] Children are more likely to aspirate inorganic material, whereas adults are more likely to aspirate organic material, such as food. The most commonly aspirated foreign bodies are nuts and seeds.[2] Fish or chicken bones can also be commonly lodged in the oropharynx.",
"Certain adult populations are at higher risk for foreign body aspiration, including those with neurologic disorders; a history of alcoholism; any loss of consciousness, such as trauma or syncope; or any impaired swallowing mechanism. Adults older than 75 years and those who wear dentures also have high risk owing to loss of palatal sensation. The most common location of aspirated foreign bodies in adults is the right main stem bronchus.[3]",
"Aspiration of foreign bodies in adults can often result in chronic symptoms that may go undiagnosed. Multiple case series demonstrate chronic symptoms that are often masked as bronchitis.[4] Chronic cough or hoarseness secondary to bronchial irrigation can go undiagnosed for extended periods, with some case studies reporting that symptoms continue without diagnosis for months to years.",
"Consider foreign body in patients with respiratory symptoms that are not responding to typical therapy. Also imperative is clinical suspicion in patients who may be predisposed to aspiration; eliciting the history by asking the patient specific questions about possibility of aspiration may be helpful."
],
"date": "October 19, 2022",
"figures": [
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/847/975/847975-Thumb3.png"
}
],
"markdown": "# Emergency Med Case Challenge: Pain, Wheezing in a Nonverbal Man Who Keeps Rubbing His Chest\n\n **Authors:** Carla R. Sterling, MD; Niccole Bart, MD \n **Date:** October 19, 2022\n\n ## Content\n\n The patient was admitted for presumed pneumonia, and antibiotic coverage for community-acquired pneumonia was started with ceftriaxone and azithromycin. While he was in the emergency department, he had a coughing fit and experienced an acute drop in consciousness and oxygen saturation, with not only cessation of wheezing but also loss of breath sounds. He was urgently intubated and transferred to the intensive care unit. A chest radiograph was obtained (Figure 3).\nFigure 3.\nFigure 3.\nCT of the chest revealed an obstruction with collapse of the lobe. The critical care pulmonologist performed bronchoscopy and the obstruction was removed, with improvement in respiratory function and subsequent imaging studies revealing reexpansion of the lobe. Oxygenation improved, and the patient was extubated the following morning.\nAfter 24 hours with stable respiratory function and vital signs, the patient was transferred to the medicine floor, where he was continued on pneumonia treatment and eventually discharged to his home at his baseline state. Aspirated foreign bodies are more common in children than adults. In general, 50% of all foreign body cases occur in children younger than 4 years.[1] Children are more likely to aspirate inorganic material, whereas adults are more likely to aspirate organic material, such as food. The most commonly aspirated foreign bodies are nuts and seeds.[2] Fish or chicken bones can also be commonly lodged in the oropharynx.\nCertain adult populations are at higher risk for foreign body aspiration, including those with neurologic disorders; a history of alcoholism; any loss of consciousness, such as trauma or syncope; or any impaired swallowing mechanism. Adults older than 75 years and those who wear dentures also have high risk owing to loss of palatal sensation. The most common location of aspirated foreign bodies in adults is the right main stem bronchus.[3]\nAspiration of foreign bodies in adults can often result in chronic symptoms that may go undiagnosed. Multiple case series demonstrate chronic symptoms that are often masked as bronchitis.[4] Chronic cough or hoarseness secondary to bronchial irrigation can go undiagnosed for extended periods, with some case studies reporting that symptoms continue without diagnosis for months to years.\nConsider foreign body in patients with respiratory symptoms that are not responding to typical therapy. Also imperative is clinical suspicion in patients who may be predisposed to aspiration; eliciting the history by asking the patient specific questions about possibility of aspiration may be helpful.\n\n ## Figures\n\n **Figure 3.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 869711,
"choiceText": "COPD exacerbation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869713,
"choiceText": "New-onset congestive heart failure",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869715,
"choiceText": "Foreign body aspiration",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869717,
"choiceText": "Pulmonary embolism",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 273657,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Emergency Med Case Challenge: Pain, Wheezing in a Nonverbal Man Who Keeps Rubbing His Chest"
},
{
"authors": "Carla R. Sterling, MD; Niccole Bart, MD",
"content": [
"Airway obstruction with aspirated foreign bodies can be divided into three phases:",
"Acute choking episode (initial lack of air entry while the patient is still alert)",
"Lack of consciousness with intact pulses",
"Cardiopulmonary arrest",
"Acute choking presentations are more common in children but may occur in adults as well. Complete obstructions result in cardiopulmonary arrest if not reversed. Incomplete obstructions may cause more variations in symptoms. Unilateral diminished breath sounds have a low sensitivity of approximately 75%, with a similar but wider-ranging specificity.[5]",
"Initial symptoms and complications include the following:",
"Choking",
"Dysphagia",
"Odynophagia",
"Dysphonia",
"Stridor",
"Cyanosis",
"Partial or total lung collapse",
"Respiratory distress",
"Later symptoms and complications include the following:",
"Coughing",
"Stridor",
"Hoarseness",
"Chest pain",
"Foul-smelling sputum",
"Granulation tissue",
"Pneumonia",
"Empyema",
"Fistula",
"Pneumothorax",
"In the acute phase, patients should be encouraged to cough. In the second stage, cardiopulmonary resuscitative maneuvers, such as the Heimlich maneuver, should be initiated. Other airway maneuvers include jaw thrust to open the airway. More definitive management, such as intubation or cricothyrotomy, may be urgently indicated in complete airway obstruction. In the case of partial obstruction, the patient is typically stable for further imaging and can continue to attempt removal through such means as coughing. Partial obstructions can present as stable, but if the obstruction advances to complete obstruction abruptly, the patient can quickly become unstable, with progression to cardiopulmonary arrest within minutes.",
"Many foreign bodies are radiolucent and are not seen on radiography. Therefore, when the index of suspicion is high, bronchoscopy should be performed. Although flexible bronchoscopy has largely replaced rigid bronchoscopy, a rigid scope may be used in selected cases of larger, more proximal objects, given the larger luminal diameter.[6]"
],
"date": "October 19, 2022",
"figures": [],
"markdown": "# Emergency Med Case Challenge: Pain, Wheezing in a Nonverbal Man Who Keeps Rubbing His Chest\n\n **Authors:** Carla R. Sterling, MD; Niccole Bart, MD \n **Date:** October 19, 2022\n\n ## Content\n\n Airway obstruction with aspirated foreign bodies can be divided into three phases:\nAcute choking episode (initial lack of air entry while the patient is still alert)\nLack of consciousness with intact pulses\nCardiopulmonary arrest\nAcute choking presentations are more common in children but may occur in adults as well. Complete obstructions result in cardiopulmonary arrest if not reversed. Incomplete obstructions may cause more variations in symptoms. Unilateral diminished breath sounds have a low sensitivity of approximately 75%, with a similar but wider-ranging specificity.[5]\nInitial symptoms and complications include the following:\nChoking\nDysphagia\nOdynophagia\nDysphonia\nStridor\nCyanosis\nPartial or total lung collapse\nRespiratory distress\nLater symptoms and complications include the following:\nCoughing\nStridor\nHoarseness\nChest pain\nFoul-smelling sputum\nGranulation tissue\nPneumonia\nEmpyema\nFistula\nPneumothorax\nIn the acute phase, patients should be encouraged to cough. In the second stage, cardiopulmonary resuscitative maneuvers, such as the Heimlich maneuver, should be initiated. Other airway maneuvers include jaw thrust to open the airway. More definitive management, such as intubation or cricothyrotomy, may be urgently indicated in complete airway obstruction. In the case of partial obstruction, the patient is typically stable for further imaging and can continue to attempt removal through such means as coughing. Partial obstructions can present as stable, but if the obstruction advances to complete obstruction abruptly, the patient can quickly become unstable, with progression to cardiopulmonary arrest within minutes.\nMany foreign bodies are radiolucent and are not seen on radiography. Therefore, when the index of suspicion is high, bronchoscopy should be performed. Although flexible bronchoscopy has largely replaced rigid bronchoscopy, a rigid scope may be used in selected cases of larger, more proximal objects, given the larger luminal diameter.[6]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Emergency Med Case Challenge: Pain, Wheezing in a Nonverbal Man Who Keeps Rubbing His Chest"
},
{
"authors": "Carla R. Sterling, MD; Niccole Bart, MD",
"content": [
"Definitive treatment is removal of the foreign body, which requires consultation by an ear, nose, and throat specialist or pulmonologist. Specialist referral is essential unless the foreign body is easily visible and graspable.[7]",
"In addition, studies have shown that flexible bronchoscopy may be a less desirable approach because both the scope and object are removed together within a narrow suction canal; if the object is dropped during retraction, the airway may be at risk for complete obstruction. This research concluded that if flexible bronchoscopy is the first attempt, rigid bronchoscopy along with preparation for emergent tracheostomy should be available in the room during the procedure.[5] In a specific subset of patients who aspirate soft or thickening food, such as those who have had stroke, airway protection may require intubation, because the texture of the food makes it difficult to remove.",
"Caustic aspirations are significantly less frequent than caustic ingestions or foreign body aspirations, but these events can be fatal if not recognized and treated appropriately. Huang and colleagues[8] describe an alkali aspiration within the respiratory organs, causing chemical tracheobronchitis and corrosive necrosis of the lung parenchyma. These physiologic processes can result in rapid formation of tension pneumothorax and hemothorax, which ultimately requires surgical intervention of thoracotomy with lobectomy. Airway management is crucial; Huang and colleagues describe a specific technique involving bronchoscopic intubation with a large endotracheal tube and daily fiberoptic bronchoscopy to remove debris and clear the airway.[8] Airway fibrosis and mucociliary dysfunction are noted as the main complications after caustic injury. Cases have been reported of airway involvement in gastrointestinal ingestions of caustic agents involving both main bronchi.[9] The bottom line is early and aggressive airway management.",
"Aspiration of button batteries is cause for similar concerns to those of button battery ingestion. Metals immersed in potassium hydroxide can leak and cause liquefactive necrosis. The button battery itself can cause pressure necrosis and result in electrical injury if the positive and negative electrodes interact."
],
"date": "October 19, 2022",
"figures": [],
"markdown": "# Emergency Med Case Challenge: Pain, Wheezing in a Nonverbal Man Who Keeps Rubbing His Chest\n\n **Authors:** Carla R. Sterling, MD; Niccole Bart, MD \n **Date:** October 19, 2022\n\n ## Content\n\n Definitive treatment is removal of the foreign body, which requires consultation by an ear, nose, and throat specialist or pulmonologist. Specialist referral is essential unless the foreign body is easily visible and graspable.[7]\nIn addition, studies have shown that flexible bronchoscopy may be a less desirable approach because both the scope and object are removed together within a narrow suction canal; if the object is dropped during retraction, the airway may be at risk for complete obstruction. This research concluded that if flexible bronchoscopy is the first attempt, rigid bronchoscopy along with preparation for emergent tracheostomy should be available in the room during the procedure.[5] In a specific subset of patients who aspirate soft or thickening food, such as those who have had stroke, airway protection may require intubation, because the texture of the food makes it difficult to remove.\nCaustic aspirations are significantly less frequent than caustic ingestions or foreign body aspirations, but these events can be fatal if not recognized and treated appropriately. Huang and colleagues[8] describe an alkali aspiration within the respiratory organs, causing chemical tracheobronchitis and corrosive necrosis of the lung parenchyma. These physiologic processes can result in rapid formation of tension pneumothorax and hemothorax, which ultimately requires surgical intervention of thoracotomy with lobectomy. Airway management is crucial; Huang and colleagues describe a specific technique involving bronchoscopic intubation with a large endotracheal tube and daily fiberoptic bronchoscopy to remove debris and clear the airway.[8] Airway fibrosis and mucociliary dysfunction are noted as the main complications after caustic injury. Cases have been reported of airway involvement in gastrointestinal ingestions of caustic agents involving both main bronchi.[9] The bottom line is early and aggressive airway management.\nAspiration of button batteries is cause for similar concerns to those of button battery ingestion. Metals immersed in potassium hydroxide can leak and cause liquefactive necrosis. The button battery itself can cause pressure necrosis and result in electrical injury if the positive and negative electrodes interact.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 869719,
"choiceText": "Left inferior lobar bronchus",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869721,
"choiceText": "Right inferior lobar bronchus",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869723,
"choiceText": "Left main stem bronchus",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869725,
"choiceText": "Right main stem bronchus",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Certain adult populations are at higher risk for foreign body aspiration, including those with neurologic disorders; a history of alcoholism; any loss of consciousness, such as trauma or syncope; or any impaired swallowing mechanism. Adults older than 75 years and those who wear dentures also have high risk owing to loss of palatal sensation. The most common location of aspirated foreign bodies in adults is the right main stem bronchus.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 273659,
"questionText": "Which is the most common location of aspirated foreign bodies in adults?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 869727,
"choiceText": "Antibiotics are always prescribed after foreign body aspiration",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869729,
"choiceText": "Development of bronchitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869731,
"choiceText": "Development of bronchiectasis or pneumonia",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869733,
"choiceText": "Antibiotics are never indicated",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nForeign body in the airway can lead to such complications as atelectasis, pneumonia, lung abscess, and bronchiectasis. Cultures should be obtained during bronchoscopy and should guide antibiotic treatment; development of bronchiectasis should prompt antibiotic treatment. These complications are significantly more likely in cases where foreign body is retained for a prolonged period—for example, if the diagnosis is missed and treatment for other respiratory conditions is initiated. <br><br>\r\n\r\nBronchiectasis is an irreversible widening of the medium to small bronchi, characterized by chronic inflammation with destruction of bronchial walls. Although it can be caused by recurrent infectious or inflammatory processes, foreign body inhalation predisposes to bronchiectasis, and the resulting process can mimic chronic pulmonary conditions, such as COPD, with subsequent pulmonary hypertension, right-sided heart failure, and chronic progressive respiratory failure.<br><br>\r\n\r\nLong-term sequelae can also include chronic cough and sputum production, which can lead to life-threatening hemoptysis. Bronchiectasis can involve single lung lobes or entire lungs, or be diffuse and bilateral; however, in the case of an inhaled foreign body, it might be less likely to become bilateral. Prolonged use of antibiotics may reduce exacerbation rates and severity of symptoms, but the data are unclear on whether it reduces mortality or other significant outcome measures.<br><br>\r\n\r\nOther treatment modalities, such as inhaled corticosteroids and mucolytics, are not supported by the limited research data available. A bronchiectasis severity index was created to guide clinicians' treatment strategies, with higher indices indicating worsened mortality and higher rates of hospitalization leading to more aggressive and prolonged treatments. This should be used to escalate treatment in a similar manner to the asthma scale for treatment.\r\n\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 273661,
"questionText": "Which is the strongest indication for use of antibiotics after foreign body aspiration?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Emergency Med Case Challenge: Pain, Wheezing in a Nonverbal Man Who Keeps Rubbing His Chest"
},
{
"authors": "Carla R. Sterling, MD; Niccole Bart, MD",
"content": [],
"date": "October 19, 2022",
"figures": [],
"markdown": "# Emergency Med Case Challenge: Pain, Wheezing in a Nonverbal Man Who Keeps Rubbing His Chest\n\n **Authors:** Carla R. Sterling, MD; Niccole Bart, MD \n **Date:** October 19, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 869719,
"choiceText": "Left inferior lobar bronchus",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869721,
"choiceText": "Right inferior lobar bronchus",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869723,
"choiceText": "Left main stem bronchus",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869725,
"choiceText": "Right main stem bronchus",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Certain adult populations are at higher risk for foreign body aspiration, including those with neurologic disorders; a history of alcoholism; any loss of consciousness, such as trauma or syncope; or any impaired swallowing mechanism. Adults older than 75 years and those who wear dentures also have high risk owing to loss of palatal sensation. The most common location of aspirated foreign bodies in adults is the right main stem bronchus.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 273659,
"questionText": "Which is the most common location of aspirated foreign bodies in adults?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 869727,
"choiceText": "Antibiotics are always prescribed after foreign body aspiration",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869729,
"choiceText": "Development of bronchitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869731,
"choiceText": "Development of bronchiectasis or pneumonia",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869733,
"choiceText": "Antibiotics are never indicated",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nForeign body in the airway can lead to such complications as atelectasis, pneumonia, lung abscess, and bronchiectasis. Cultures should be obtained during bronchoscopy and should guide antibiotic treatment; development of bronchiectasis should prompt antibiotic treatment. These complications are significantly more likely in cases where foreign body is retained for a prolonged period—for example, if the diagnosis is missed and treatment for other respiratory conditions is initiated. <br><br>\r\n\r\nBronchiectasis is an irreversible widening of the medium to small bronchi, characterized by chronic inflammation with destruction of bronchial walls. Although it can be caused by recurrent infectious or inflammatory processes, foreign body inhalation predisposes to bronchiectasis, and the resulting process can mimic chronic pulmonary conditions, such as COPD, with subsequent pulmonary hypertension, right-sided heart failure, and chronic progressive respiratory failure.<br><br>\r\n\r\nLong-term sequelae can also include chronic cough and sputum production, which can lead to life-threatening hemoptysis. Bronchiectasis can involve single lung lobes or entire lungs, or be diffuse and bilateral; however, in the case of an inhaled foreign body, it might be less likely to become bilateral. Prolonged use of antibiotics may reduce exacerbation rates and severity of symptoms, but the data are unclear on whether it reduces mortality or other significant outcome measures.<br><br>\r\n\r\nOther treatment modalities, such as inhaled corticosteroids and mucolytics, are not supported by the limited research data available. A bronchiectasis severity index was created to guide clinicians' treatment strategies, with higher indices indicating worsened mortality and higher rates of hospitalization leading to more aggressive and prolonged treatments. This should be used to escalate treatment in a similar manner to the asthma scale for treatment.\r\n\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 273661,
"questionText": "Which is the strongest indication for use of antibiotics after foreign body aspiration?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Emergency Med Case Challenge: Pain, Wheezing in a Nonverbal Man Who Keeps Rubbing His Chest"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 869711,
"choiceText": "COPD exacerbation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869713,
"choiceText": "New-onset congestive heart failure",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869715,
"choiceText": "Foreign body aspiration",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869717,
"choiceText": "Pulmonary embolism",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 273657,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 869719,
"choiceText": "Left inferior lobar bronchus",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869721,
"choiceText": "Right inferior lobar bronchus",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869723,
"choiceText": "Left main stem bronchus",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869725,
"choiceText": "Right main stem bronchus",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Certain adult populations are at higher risk for foreign body aspiration, including those with neurologic disorders; a history of alcoholism; any loss of consciousness, such as trauma or syncope; or any impaired swallowing mechanism. Adults older than 75 years and those who wear dentures also have high risk owing to loss of palatal sensation. The most common location of aspirated foreign bodies in adults is the right main stem bronchus.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 273659,
"questionText": "Which is the most common location of aspirated foreign bodies in adults?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 869727,
"choiceText": "Antibiotics are always prescribed after foreign body aspiration",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869729,
"choiceText": "Development of bronchitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869731,
"choiceText": "Development of bronchiectasis or pneumonia",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 869733,
"choiceText": "Antibiotics are never indicated",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nForeign body in the airway can lead to such complications as atelectasis, pneumonia, lung abscess, and bronchiectasis. Cultures should be obtained during bronchoscopy and should guide antibiotic treatment; development of bronchiectasis should prompt antibiotic treatment. These complications are significantly more likely in cases where foreign body is retained for a prolonged period—for example, if the diagnosis is missed and treatment for other respiratory conditions is initiated. <br><br>\r\n\r\nBronchiectasis is an irreversible widening of the medium to small bronchi, characterized by chronic inflammation with destruction of bronchial walls. Although it can be caused by recurrent infectious or inflammatory processes, foreign body inhalation predisposes to bronchiectasis, and the resulting process can mimic chronic pulmonary conditions, such as COPD, with subsequent pulmonary hypertension, right-sided heart failure, and chronic progressive respiratory failure.<br><br>\r\n\r\nLong-term sequelae can also include chronic cough and sputum production, which can lead to life-threatening hemoptysis. Bronchiectasis can involve single lung lobes or entire lungs, or be diffuse and bilateral; however, in the case of an inhaled foreign body, it might be less likely to become bilateral. Prolonged use of antibiotics may reduce exacerbation rates and severity of symptoms, but the data are unclear on whether it reduces mortality or other significant outcome measures.<br><br>\r\n\r\nOther treatment modalities, such as inhaled corticosteroids and mucolytics, are not supported by the limited research data available. A bronchiectasis severity index was created to guide clinicians' treatment strategies, with higher indices indicating worsened mortality and higher rates of hospitalization leading to more aggressive and prolonged treatments. This should be used to escalate treatment in a similar manner to the asthma scale for treatment.\r\n\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 273661,
"questionText": "Which is the strongest indication for use of antibiotics after foreign body aspiration?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
981716 | /viewarticle/981716 | [
{
"authors": "Poornima Oruganti, MD, MPH; Jason Schairer, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 45-year-old African American woman presents with lesions on her legs. She has a history of hypertension, type 1 diabetes, and jejunal Crohn's disease, which was diagnosed 15 years ago. The patient injured her right leg 2 months earlier while riding her bicycle. The lesion was painful, weeping, and ulcerated but now appears to be healing. She also has a larger lesion on the left leg. She has not experienced nausea, vomiting, diarrhea, constipation, abdominal pain, melena, and hematochezia.",
"Her small-bowel Crohn's disease was diagnosed when she was 30 years old and was well-controlled for many years. She is currently taking azathioprine only. The patient was hospitalized for a flare of her Crohn's disease about 6 months ago and required intravenous corticosteroids along with a steroid taper.",
"The patient's mother has hypothyroidism. Her father has coronary artery disease and hypertension. She has no siblings. The patient quit smoking 5 years ago and does not drink alcohol."
],
"date": "October 10, 2022",
"figures": [],
"markdown": "# Dermatology Case Challenge: Painful Lesions, Open Wounds on a 45-Year-Old Woman\n\n **Authors:** Poornima Oruganti, MD, MPH; Jason Schairer, MD \n **Date:** October 10, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 45-year-old African American woman presents with lesions on her legs. She has a history of hypertension, type 1 diabetes, and jejunal Crohn's disease, which was diagnosed 15 years ago. The patient injured her right leg 2 months earlier while riding her bicycle. The lesion was painful, weeping, and ulcerated but now appears to be healing. She also has a larger lesion on the left leg. She has not experienced nausea, vomiting, diarrhea, constipation, abdominal pain, melena, and hematochezia.\nHer small-bowel Crohn's disease was diagnosed when she was 30 years old and was well-controlled for many years. She is currently taking azathioprine only. The patient was hospitalized for a flare of her Crohn's disease about 6 months ago and required intravenous corticosteroids along with a steroid taper.\nThe patient's mother has hypothyroidism. Her father has coronary artery disease and hypertension. She has no siblings. The patient quit smoking 5 years ago and does not drink alcohol.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Dermatology Case Challenge: Painful Lesions, Open Wounds on a 45-Year-Old Woman"
},
{
"authors": "Poornima Oruganti, MD, MPH; Jason Schairer, MD",
"content": [
"Upon examination, the patient's heart rate is 80 beats/min, her blood pressure is 128/70 mm Hg, and her temperature is 97.7 °F (36.5 °C). She is comfortable and is in no acute distress. The head and neck, cardiac, pulmonary, and abdominal examinations are all normal. The musculoskeletal examination reveals normal range of motion in all extremities.",
"A 2-cm slightly raised lesion with a hyperpigmented border and eschar is present on her right lower extremity (Figure 1). An open wound is noted on her left lower extremity on the medial aspect just above the ankle (Figure 2). It appears moist, ulcerated, and weeping. The patient provides a photograph of what the lesion on her right leg looked like 2 weeks ago, which shows blistering of the skin and ulceration (Figure 3). Upon presentation, the lesion is minimally tender to palpation.",
"Figure 1.",
"Figure 2.",
"Figure 3.",
"Results of laboratory studies include a normal complete blood cell count, normal liver function tests, and a normal basic metabolic panel. The erythrocyte sedimentation rate (ESR) as well as C-reactive protein (CRP) levels are both slightly elevated. Cultures of the skin were negative."
],
"date": "October 10, 2022",
"figures": [],
"markdown": "# Dermatology Case Challenge: Painful Lesions, Open Wounds on a 45-Year-Old Woman\n\n **Authors:** Poornima Oruganti, MD, MPH; Jason Schairer, MD \n **Date:** October 10, 2022\n\n ## Content\n\n Upon examination, the patient's heart rate is 80 beats/min, her blood pressure is 128/70 mm Hg, and her temperature is 97.7 °F (36.5 °C). She is comfortable and is in no acute distress. The head and neck, cardiac, pulmonary, and abdominal examinations are all normal. The musculoskeletal examination reveals normal range of motion in all extremities.\nA 2-cm slightly raised lesion with a hyperpigmented border and eschar is present on her right lower extremity (Figure 1). An open wound is noted on her left lower extremity on the medial aspect just above the ankle (Figure 2). It appears moist, ulcerated, and weeping. The patient provides a photograph of what the lesion on her right leg looked like 2 weeks ago, which shows blistering of the skin and ulceration (Figure 3). Upon presentation, the lesion is minimally tender to palpation.\nFigure 1.\nFigure 2.\nFigure 3.\nResults of laboratory studies include a normal complete blood cell count, normal liver function tests, and a normal basic metabolic panel. The erythrocyte sedimentation rate (ESR) as well as C-reactive protein (CRP) levels are both slightly elevated. Cultures of the skin were negative.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1727327,
"choiceText": "Healing injury from mechanical fall",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727328,
"choiceText": "Pyoderma gangrenosum",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727329,
"choiceText": "Erythema nodosum",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727330,
"choiceText": "Spider bite",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 557533,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Dermatology Case Challenge: Painful Lesions, Open Wounds on a 45-Year-Old Woman"
},
{
"authors": "Poornima Oruganti, MD, MPH; Jason Schairer, MD",
"content": [
"Pyoderma gangrenosum (PG) is a reactive noninfectious inflammatory dermatosis that falls under the spectrum of neutrophilic dermatoses, along with Sweet syndrome and Behçet syndrome.[1] PG is a known extraintestinal manifestation of inflammatory bowel disease (IBD). Its hallmark historical finding is pathergy, in which a small insult or injury can lead to a large, rapidly expanding wound. PG typically presents as an erythematous pustule that rapidly evolves into deep ulcers with irregular violaceous edges. A solitary lesion or multiple lesions may be present. Lesion size ranges from a few centimeters to covering an entire limb. Patients with severe IBD are more likely to develop PG. The pathophysiology of PG is unclear; however, neutrophils are thought to play a large role in the process.[1,2]",
"Patients who develop PG can experience a decline in their quality of life because the wounds may cause severe pain, limitations of activity, and sleep disturbances. In the setting of systemic disease, PG is also associated with depression. The prevalence of PG is similar among White and Black patients but is higher in women than in men.[3]",
"The hallmark examination findings are violaceous borders that have a deep, rapidly expanding edge.[1] Patients of African descent or who identify as Black or African American may have skin with that can alter the color of PG ulcers. The darker the skin tone, the more difficult appreciating pink, red, and purple hues can be. With residual scarring to the area, a patient may have hyperpigmentation with dark scars or hypopigmentation with light scars. It is important to learn to recognize common dermatologic lesions and the various subtle yet important differences that they can exhibit in patients with different skin tones. This allows physicians to recognize pathology and deliver appropriate care to patients of all races and ethnicities."
],
"date": "October 10, 2022",
"figures": [],
"markdown": "# Dermatology Case Challenge: Painful Lesions, Open Wounds on a 45-Year-Old Woman\n\n **Authors:** Poornima Oruganti, MD, MPH; Jason Schairer, MD \n **Date:** October 10, 2022\n\n ## Content\n\n Pyoderma gangrenosum (PG) is a reactive noninfectious inflammatory dermatosis that falls under the spectrum of neutrophilic dermatoses, along with Sweet syndrome and Behçet syndrome.[1] PG is a known extraintestinal manifestation of inflammatory bowel disease (IBD). Its hallmark historical finding is pathergy, in which a small insult or injury can lead to a large, rapidly expanding wound. PG typically presents as an erythematous pustule that rapidly evolves into deep ulcers with irregular violaceous edges. A solitary lesion or multiple lesions may be present. Lesion size ranges from a few centimeters to covering an entire limb. Patients with severe IBD are more likely to develop PG. The pathophysiology of PG is unclear; however, neutrophils are thought to play a large role in the process.[1,2]\nPatients who develop PG can experience a decline in their quality of life because the wounds may cause severe pain, limitations of activity, and sleep disturbances. In the setting of systemic disease, PG is also associated with depression. The prevalence of PG is similar among White and Black patients but is higher in women than in men.[3]\nThe hallmark examination findings are violaceous borders that have a deep, rapidly expanding edge.[1] Patients of African descent or who identify as Black or African American may have skin with that can alter the color of PG ulcers. The darker the skin tone, the more difficult appreciating pink, red, and purple hues can be. With residual scarring to the area, a patient may have hyperpigmentation with dark scars or hypopigmentation with light scars. It is important to learn to recognize common dermatologic lesions and the various subtle yet important differences that they can exhibit in patients with different skin tones. This allows physicians to recognize pathology and deliver appropriate care to patients of all races and ethnicities.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1727327,
"choiceText": "Healing injury from mechanical fall",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727328,
"choiceText": "Pyoderma gangrenosum",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727329,
"choiceText": "Erythema nodosum",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727330,
"choiceText": "Spider bite",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 557533,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Dermatology Case Challenge: Painful Lesions, Open Wounds on a 45-Year-Old Woman"
},
{
"authors": "Poornima Oruganti, MD, MPH; Jason Schairer, MD",
"content": [
"In this case, the left leg (Figure 2) shows a large, rapidly expanding ulcer. It is deeper in the middle and more superficial on the periphery. No violaceous border is present, although the top half of the lesion has a pink border, and the bottom half demonstrates hyperpigmentation.",
"Figure 2.",
"The lesion on the right leg (Figures 1 and 3) has healed at the time of presentation, and a distinct eschar with a hyperpigmented border is seen. Without seeing the previous ulceration, one could confuse this lesion with erythema nodosum. However, erythema nodosum presents with tender, red, raised lesions on the shins, typically in a symmetrical pattern on both legs, and is subcutaneous in depth without the overlying erosion of ulceration. Injury from a mechanical fall is also unlikely because the initial lesion demonstrates characteristic findings of PG, including a rapidly expanding ulcer, violaceous border, hyperpigmentation and hypopigmentation, and eschar.",
"Figure 1.",
"Figure 3.",
"Patients and physicians often blame spider bites for lesions on the skin. However, most spiders are not capable of piercing the skin, and very few species are capable of biting humans. Skin lesions should not be attributed to spider bites unless clear clinical evidence or visualization of a spider biting the skin is noted.[4] More commonly, PG can appear similar to a methicillin-resistant Staphylococcus aureus (MRSA) skin infection. However, a MRSA skin infection typically appears as a tender, swollen, erythematous area, usually with a pimple or pustule. In this patient's case and with her given history, the lesions on her legs show the hallmark findings of PG of pathergy, with an inflammatory border. She has a history of inflammatory bowel disease and has a negative culture. These findings make infection unlikely.",
"PG is difficult to diagnose and is often a diagnosis of exclusion. A Delphi consensus of experts states that a patient must have the major criterion of a biopsy of the ulcer edge that demonstrates neutrophilic infiltrate, as well as four of eight minor criteria to receive a diagnosis of PG.[5] The minor criteria include:",
"Exclusion of infection",
"Pathergy",
"History of IBD or inflammatory arthritis",
"History of a lesion that develops ulceration within 4 days of appearance",
"Peripheral erythema, an undermining border, and tenderness at the ulceration",
"Multiple ulcerations and at least one on the anterior lower leg",
"Cribriform scars at the healed ulcer sites",
"Decrease in size of the lesion within 1 month of immunosuppressive therapy",
"Another diagnostic tool asserts that a patient must have two major criteria (rapid progression of a painful cutaneous ulcer with an irregular, violaceous, and undermined border and exclusion of other causes of the ulcer) and two minor criteria (a history of pathergy or cribriform scarring, an associated systemic disease, classic findings on histopathology, and a response to treatment).[1] Although no validated or established diagnostic criteria exist, current data and practice suggest a role for biopsy to assist in the diagnosis of PG. However, some clinicians believe that a biopsy may worsen the ulcer and may not be necessary in the clinical context to diagnose PG.[6]",
"The management of PG involves a stepwise approach. Optimization of wound care, analgesia, and topical treatments such as topical corticosteroids or topical calcineurin inhibitors may be used first. Injection of intralesional steroids is also a potential treatment. If these therapies fail, patients may be candidates for systemic therapies such as oral or intravenous steroids as well as cyclosporin as a steroid-sparing agent. Ultimately, if topical or systemic therapies fail, consideration of biologic therapy is appropriate. Infliximab has a large body of evidence to support its use in the treatment of PG.[1,7]"
],
"date": "October 10, 2022",
"figures": [],
"markdown": "# Dermatology Case Challenge: Painful Lesions, Open Wounds on a 45-Year-Old Woman\n\n **Authors:** Poornima Oruganti, MD, MPH; Jason Schairer, MD \n **Date:** October 10, 2022\n\n ## Content\n\n In this case, the left leg (Figure 2) shows a large, rapidly expanding ulcer. It is deeper in the middle and more superficial on the periphery. No violaceous border is present, although the top half of the lesion has a pink border, and the bottom half demonstrates hyperpigmentation.\nFigure 2.\nThe lesion on the right leg (Figures 1 and 3) has healed at the time of presentation, and a distinct eschar with a hyperpigmented border is seen. Without seeing the previous ulceration, one could confuse this lesion with erythema nodosum. However, erythema nodosum presents with tender, red, raised lesions on the shins, typically in a symmetrical pattern on both legs, and is subcutaneous in depth without the overlying erosion of ulceration. Injury from a mechanical fall is also unlikely because the initial lesion demonstrates characteristic findings of PG, including a rapidly expanding ulcer, violaceous border, hyperpigmentation and hypopigmentation, and eschar.\nFigure 1.\nFigure 3.\nPatients and physicians often blame spider bites for lesions on the skin. However, most spiders are not capable of piercing the skin, and very few species are capable of biting humans. Skin lesions should not be attributed to spider bites unless clear clinical evidence or visualization of a spider biting the skin is noted.[4] More commonly, PG can appear similar to a methicillin-resistant Staphylococcus aureus (MRSA) skin infection. However, a MRSA skin infection typically appears as a tender, swollen, erythematous area, usually with a pimple or pustule. In this patient's case and with her given history, the lesions on her legs show the hallmark findings of PG of pathergy, with an inflammatory border. She has a history of inflammatory bowel disease and has a negative culture. These findings make infection unlikely.\nPG is difficult to diagnose and is often a diagnosis of exclusion. A Delphi consensus of experts states that a patient must have the major criterion of a biopsy of the ulcer edge that demonstrates neutrophilic infiltrate, as well as four of eight minor criteria to receive a diagnosis of PG.[5] The minor criteria include:\nExclusion of infection\nPathergy\nHistory of IBD or inflammatory arthritis\nHistory of a lesion that develops ulceration within 4 days of appearance\nPeripheral erythema, an undermining border, and tenderness at the ulceration\nMultiple ulcerations and at least one on the anterior lower leg\nCribriform scars at the healed ulcer sites\nDecrease in size of the lesion within 1 month of immunosuppressive therapy\nAnother diagnostic tool asserts that a patient must have two major criteria (rapid progression of a painful cutaneous ulcer with an irregular, violaceous, and undermined border and exclusion of other causes of the ulcer) and two minor criteria (a history of pathergy or cribriform scarring, an associated systemic disease, classic findings on histopathology, and a response to treatment).[1] Although no validated or established diagnostic criteria exist, current data and practice suggest a role for biopsy to assist in the diagnosis of PG. However, some clinicians believe that a biopsy may worsen the ulcer and may not be necessary in the clinical context to diagnose PG.[6]\nThe management of PG involves a stepwise approach. Optimization of wound care, analgesia, and topical treatments such as topical corticosteroids or topical calcineurin inhibitors may be used first. Injection of intralesional steroids is also a potential treatment. If these therapies fail, patients may be candidates for systemic therapies such as oral or intravenous steroids as well as cyclosporin as a steroid-sparing agent. Ultimately, if topical or systemic therapies fail, consideration of biologic therapy is appropriate. Infliximab has a large body of evidence to support its use in the treatment of PG.[1,7]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Dermatology Case Challenge: Painful Lesions, Open Wounds on a 45-Year-Old Woman"
},
{
"authors": "Poornima Oruganti, MD, MPH; Jason Schairer, MD",
"content": [
"PG is more commonly seen in active IBD, although it can also occur less frequently in inactive IBD. In addition, PG can be a clinical sign that indicates new active disease in patients with previously inactive disease. Therefore, investigating active PG with imaging or endoscopy is reasonable.[6,7] This patient has known jejunal disease; a colonoscopy would be unlikely to find active inflammation in her case. The patient's ESR and CRP levels may be elevated from active IBD, PG, or both; these findings cannot localize the source of the inflammation. A repeat biopsy of the lesion may help if confusion exists about the diagnosis; however, the clinical history, physical examination, negative culture, and histology all confirm the diagnosis of PG at this time. Therefore, concurrently with stepwise treatment of PG, it is reasonable to investigate active disease in this patient with magnetic resonance (MR) enterography.",
"She was treated with topical steroids, with improvement of her PG. Her gastroenterologist remained suspicious that her new diagnosis of PG, as well as her recent flare of Crohn's disease 6 months earlier, was indicative of a change in her disease process. The patient underwent MR enterography, which showed significant inflammation in the small bowel, including the terminal ileum. A regimen of infliximab infusions every 8 weeks was initiated. Four months after starting infliximab infusions, her Crohn's disease symptoms improved, she had no additional flares, and her PG completely healed, with no reoccurrence."
],
"date": "October 10, 2022",
"figures": [],
"markdown": "# Dermatology Case Challenge: Painful Lesions, Open Wounds on a 45-Year-Old Woman\n\n **Authors:** Poornima Oruganti, MD, MPH; Jason Schairer, MD \n **Date:** October 10, 2022\n\n ## Content\n\n PG is more commonly seen in active IBD, although it can also occur less frequently in inactive IBD. In addition, PG can be a clinical sign that indicates new active disease in patients with previously inactive disease. Therefore, investigating active PG with imaging or endoscopy is reasonable.[6,7] This patient has known jejunal disease; a colonoscopy would be unlikely to find active inflammation in her case. The patient's ESR and CRP levels may be elevated from active IBD, PG, or both; these findings cannot localize the source of the inflammation. A repeat biopsy of the lesion may help if confusion exists about the diagnosis; however, the clinical history, physical examination, negative culture, and histology all confirm the diagnosis of PG at this time. Therefore, concurrently with stepwise treatment of PG, it is reasonable to investigate active disease in this patient with magnetic resonance (MR) enterography.\nShe was treated with topical steroids, with improvement of her PG. Her gastroenterologist remained suspicious that her new diagnosis of PG, as well as her recent flare of Crohn's disease 6 months earlier, was indicative of a change in her disease process. The patient underwent MR enterography, which showed significant inflammation in the small bowel, including the terminal ileum. A regimen of infliximab infusions every 8 weeks was initiated. Four months after starting infliximab infusions, her Crohn's disease symptoms improved, she had no additional flares, and her PG completely healed, with no reoccurrence.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1727331,
"choiceText": "Biopsy after treatment is initiated",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727332,
"choiceText": "Biopsy after the lesions develop a scar\r\n",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727333,
"choiceText": "Biopsy now",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727334,
"choiceText": "No biopsy is needed",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "PG is often a diagnosis of exclusion. Various tools have criteria for the diagnosis of PG, including the major criterion of biopsy of an ulcer edge that demonstrates neutrophilic infiltrate.<sup>[5]</p> Therefore, biopsy of the lesion now is the correct approach.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 557534,
"questionText": "In a patient with a history and presentation similar to those of the patient in this case, what is the most appropriate course of action regarding biopsy?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1727335,
"choiceText": "Topical corticosteroids",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727336,
"choiceText": "Oral corticosteroids",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727337,
"choiceText": "Infliximab",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727338,
"choiceText": "Mycophenolate mofetil",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The treatment of PG involves a stepwise approach. First, optimization of wound care, analgesia, and topical medications, such as topical corticosteroids or calcineurin inhibitors, may be used. Another potential treatment is injection of intralesional steroids. If patients do not respond to these therapies, systemic therapies, such as oral or intravenous steroids, as well as cyclosporin as a steroid-sparing agent may be appropriate. If topical or systemic therapies fail, biologic agents may be considered. Infliximab has a large body of evidence to support its use in the treatment of PG.<sup>[1,7]</sup> In this case, because the patient has tried local wound care, the next step would be topical steroids.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 557535,
"questionText": "In addition to local wound care, what is the next step in the management of PG?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Dermatology Case Challenge: Painful Lesions, Open Wounds on a 45-Year-Old Woman"
},
{
"authors": "Poornima Oruganti, MD, MPH; Jason Schairer, MD",
"content": [
"Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult."
],
"date": "October 10, 2022",
"figures": [],
"markdown": "# Dermatology Case Challenge: Painful Lesions, Open Wounds on a 45-Year-Old Woman\n\n **Authors:** Poornima Oruganti, MD, MPH; Jason Schairer, MD \n **Date:** October 10, 2022\n\n ## Content\n\n Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult.\n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1727331,
"choiceText": "Biopsy after treatment is initiated",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727332,
"choiceText": "Biopsy after the lesions develop a scar\r\n",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727333,
"choiceText": "Biopsy now",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727334,
"choiceText": "No biopsy is needed",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "PG is often a diagnosis of exclusion. Various tools have criteria for the diagnosis of PG, including the major criterion of biopsy of an ulcer edge that demonstrates neutrophilic infiltrate.<sup>[5]</p> Therefore, biopsy of the lesion now is the correct approach.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 557534,
"questionText": "In a patient with a history and presentation similar to those of the patient in this case, what is the most appropriate course of action regarding biopsy?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1727335,
"choiceText": "Topical corticosteroids",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727336,
"choiceText": "Oral corticosteroids",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727337,
"choiceText": "Infliximab",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727338,
"choiceText": "Mycophenolate mofetil",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The treatment of PG involves a stepwise approach. First, optimization of wound care, analgesia, and topical medications, such as topical corticosteroids or calcineurin inhibitors, may be used. Another potential treatment is injection of intralesional steroids. If patients do not respond to these therapies, systemic therapies, such as oral or intravenous steroids, as well as cyclosporin as a steroid-sparing agent may be appropriate. If topical or systemic therapies fail, biologic agents may be considered. Infliximab has a large body of evidence to support its use in the treatment of PG.<sup>[1,7]</sup> In this case, because the patient has tried local wound care, the next step would be topical steroids.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 557535,
"questionText": "In addition to local wound care, what is the next step in the management of PG?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Dermatology Case Challenge: Painful Lesions, Open Wounds on a 45-Year-Old Woman"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1727327,
"choiceText": "Healing injury from mechanical fall",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727328,
"choiceText": "Pyoderma gangrenosum",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727329,
"choiceText": "Erythema nodosum",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727330,
"choiceText": "Spider bite",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 557533,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1727331,
"choiceText": "Biopsy after treatment is initiated",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727332,
"choiceText": "Biopsy after the lesions develop a scar\r\n",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727333,
"choiceText": "Biopsy now",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727334,
"choiceText": "No biopsy is needed",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "PG is often a diagnosis of exclusion. Various tools have criteria for the diagnosis of PG, including the major criterion of biopsy of an ulcer edge that demonstrates neutrophilic infiltrate.<sup>[5]</p> Therefore, biopsy of the lesion now is the correct approach.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 557534,
"questionText": "In a patient with a history and presentation similar to those of the patient in this case, what is the most appropriate course of action regarding biopsy?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1727335,
"choiceText": "Topical corticosteroids",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727336,
"choiceText": "Oral corticosteroids",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727337,
"choiceText": "Infliximab",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1727338,
"choiceText": "Mycophenolate mofetil",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The treatment of PG involves a stepwise approach. First, optimization of wound care, analgesia, and topical medications, such as topical corticosteroids or calcineurin inhibitors, may be used. Another potential treatment is injection of intralesional steroids. If patients do not respond to these therapies, systemic therapies, such as oral or intravenous steroids, as well as cyclosporin as a steroid-sparing agent may be appropriate. If topical or systemic therapies fail, biologic agents may be considered. Infliximab has a large body of evidence to support its use in the treatment of PG.<sup>[1,7]</sup> In this case, because the patient has tried local wound care, the next step would be topical steroids.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 557535,
"questionText": "In addition to local wound care, what is the next step in the management of PG?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
892848 | /viewarticle/892848 | [
{
"authors": "Dora Izaguirre-Anariba, MD, MPH, CHES; Hung-I Liao, MD; Jesus C. Lanza, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 43-year-old woman with obesity has a medical history that includes multiple respiratory infections, dyspepsia, hypertension, and breathing problems during childhood presents to her primary care physician. She reports dyspnea over the past several years, beginning prior to the COVID pandemic, that is exacerbated by changes in weather. Her dyspnea is accompanied by heart palpitations and chest tightness. She also complains of an intermittent productive cough with yellowish sputum that has responded to short courses of antibiotics in the past.",
"She has visited the emergency department on more than 10 occasions during the last 6 months, with an admission to the intensive care unit (ICU), where she was treated with noninvasive ventilatory support. She is currently negative for COVID-19.",
"She smoked as much as a pack of cigarettes per day before quitting 3 months ago. Although she has lived in the same neighborhood for the last 20 years, she recalls that a zookeeper has just moved into the apartment next door and keeps birds on his window. She acknowledges that she has not been compliant with her home medications, despite counseling given by her doctor. She also describes being embarrassed because her partner does not want to sleep in the same room due to her heavy snoring. Today, she feels more short of breath and anxious than on previous visits."
],
"date": "October 05, 2022",
"figures": [],
"markdown": "# Palpitations, Cough in a Woman Who Lives Next to a Zookeeper\n\n **Authors:** Dora Izaguirre-Anariba, MD, MPH, CHES; Hung-I Liao, MD; Jesus C. Lanza, MD \n **Date:** October 05, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 43-year-old woman with obesity has a medical history that includes multiple respiratory infections, dyspepsia, hypertension, and breathing problems during childhood presents to her primary care physician. She reports dyspnea over the past several years, beginning prior to the COVID pandemic, that is exacerbated by changes in weather. Her dyspnea is accompanied by heart palpitations and chest tightness. She also complains of an intermittent productive cough with yellowish sputum that has responded to short courses of antibiotics in the past.\nShe has visited the emergency department on more than 10 occasions during the last 6 months, with an admission to the intensive care unit (ICU), where she was treated with noninvasive ventilatory support. She is currently negative for COVID-19.\nShe smoked as much as a pack of cigarettes per day before quitting 3 months ago. Although she has lived in the same neighborhood for the last 20 years, she recalls that a zookeeper has just moved into the apartment next door and keeps birds on his window. She acknowledges that she has not been compliant with her home medications, despite counseling given by her doctor. She also describes being embarrassed because her partner does not want to sleep in the same room due to her heavy snoring. Today, she feels more short of breath and anxious than on previous visits.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Palpitations, Cough in a Woman Who Lives Next to a Zookeeper"
},
{
"authors": "Dora Izaguirre-Anariba, MD, MPH, CHES; Hung-I Liao, MD; Jesus C. Lanza, MD",
"content": [
"The physical examination reveals an alert and oriented woman with a regular pulse of 104 beats/min, a blood pressure of 134/89 mm Hg, a respiratory rate of 31 breaths/min, a temperature of 98.8°F, and oxygen saturation of 91% on room air. Her neck is short, supple, and without jugular venous distention or lymphadenopathy.",
"A cardiac examination reveals regular rhythm and normal S1 and S2 findings; no audible murmurs, rubs, or gallops are noted. A chest examination reveals bilateral decreased air entry with scattered wheezes; no rhonchi or rales are heard upon auscultation. Her abdomen is soft, nontender, and nondistended, with no evidence of visceromegaly. Her extremities show no edema, cyanosis, or clubbing. Her peripheral pulse is strong and palpable. A skin examination is remarkable for dryness in flexural foldings (Figure 1).",
"Figure 1.",
"Neurologic examination findings are normal. Laboratory workup, including a complete blood count, reveals blood eosinophils >10%. Polymerase chain reaction (PCR) tests for COVID are negative. Arterial blood gas findings are normal, except for mild hypoxemia with respiratory alkalosis. The cytoplasmic antineutrophil cytoplasmic antibody titer is negative, and serum levels of alpha-1 antitrypsin (AAT) are 14 µmol/L. The immunoglobulin E (IgE) level is 800 kU/L.",
"Pulmonary function testing reveals a forced expiratory volume in 1 second (FEV1) of 1.82 L (52% of predicted), with an FEV1/forced vital capacity (FVC) ratio of 68%. FEV1 improves with albuterol treatment (postbronchodilator increase in FEV1 of 14%). She is also found to have a reduced diffusing capacity for carbon monoxide of 17.72 mL/min/mm Hg (62% of predicted) and evidence of air trapping, with a residual volume of 3.26 L (127% of predicted).",
"A chest x-ray reveals hyperlucent areas on bilateral lower lobes (Figure 2). Chest CT scanning is also performed (Figure 3).",
"Figure 2.",
"Figure 3.",
"Echocardiography reveals an ejection fraction of 55%-60% with a pulmonary artery systolic pressure of 30 mm Hg."
],
"date": "October 05, 2022",
"figures": [],
"markdown": "# Palpitations, Cough in a Woman Who Lives Next to a Zookeeper\n\n **Authors:** Dora Izaguirre-Anariba, MD, MPH, CHES; Hung-I Liao, MD; Jesus C. Lanza, MD \n **Date:** October 05, 2022\n\n ## Content\n\n The physical examination reveals an alert and oriented woman with a regular pulse of 104 beats/min, a blood pressure of 134/89 mm Hg, a respiratory rate of 31 breaths/min, a temperature of 98.8°F, and oxygen saturation of 91% on room air. Her neck is short, supple, and without jugular venous distention or lymphadenopathy.\nA cardiac examination reveals regular rhythm and normal S1 and S2 findings; no audible murmurs, rubs, or gallops are noted. A chest examination reveals bilateral decreased air entry with scattered wheezes; no rhonchi or rales are heard upon auscultation. Her abdomen is soft, nontender, and nondistended, with no evidence of visceromegaly. Her extremities show no edema, cyanosis, or clubbing. Her peripheral pulse is strong and palpable. A skin examination is remarkable for dryness in flexural foldings (Figure 1).\nFigure 1.\nNeurologic examination findings are normal. Laboratory workup, including a complete blood count, reveals blood eosinophils >10%. Polymerase chain reaction (PCR) tests for COVID are negative. Arterial blood gas findings are normal, except for mild hypoxemia with respiratory alkalosis. The cytoplasmic antineutrophil cytoplasmic antibody titer is negative, and serum levels of alpha-1 antitrypsin (AAT) are 14 µmol/L. The immunoglobulin E (IgE) level is 800 kU/L.\nPulmonary function testing reveals a forced expiratory volume in 1 second (FEV1) of 1.82 L (52% of predicted), with an FEV1/forced vital capacity (FVC) ratio of 68%. FEV1 improves with albuterol treatment (postbronchodilator increase in FEV1 of 14%). She is also found to have a reduced diffusing capacity for carbon monoxide of 17.72 mL/min/mm Hg (62% of predicted) and evidence of air trapping, with a residual volume of 3.26 L (127% of predicted).\nA chest x-ray reveals hyperlucent areas on bilateral lower lobes (Figure 2). Chest CT scanning is also performed (Figure 3).\nFigure 2.\nFigure 3.\nEchocardiography reveals an ejection fraction of 55%-60% with a pulmonary artery systolic pressure of 30 mm Hg.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1190168,
"choiceText": "AAT deficiency (AATD)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190170,
"choiceText": "Chronic obstructive pulmonary disease (COPD)",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190172,
"choiceText": "Churg-Strauss syndrome (CSS)",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190174,
"choiceText": "Asthma",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190176,
"choiceText": "Allergic bronchopulmonary aspergillosis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190178,
"choiceText": "Congestive heart failure (CHF)\r\n",
"correct": false,
"displayOrder": 6,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 378337,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Palpitations, Cough in a Woman Who Lives Next to a Zookeeper"
},
{
"authors": "Dora Izaguirre-Anariba, MD, MPH, CHES; Hung-I Liao, MD; Jesus C. Lanza, MD",
"content": [
"Asthma should be suspected in any person who presents with shortness of breath, wheezing, and cough; however, differential diagnoses that may mimic asthma must be ruled out. This requires a detailed clinical history and physical examination. The pathophysiology is complex and involves airway inflammation, intermittent airflow obstruction, and bronchial hyperresponsiveness. Environmental exposure usually plays an important role in symptom exacerbations. Smoking has been found in as many as 40% of the patients diagnosed with asthma.",
"Spirometry with postbronchodilator response should be obtained as the primary test to establish airflow limitation consistent with asthma. Pulse oximetry measurement is desirable in all patients with acute asthma to determine hypoxemia. Chest radiography remains the initial imaging evaluation in most individuals with symptoms of asthma; however, in most patients with asthma, chest radiography findings are normal or may indicate hyperinflation. Exercise spirometry is the criterion standard method for assessing patients with exercise-induced bronchoconstriction. In addition, reversibility testing with steroid therapy should be performed, and any cardiac etiology should also be investigated.",
"AATD was ruled out because the patient's clinical history did not include an abnormal AAT level. AAT levels <11 µmol/L are consistent with AATD. However, low AAT levels alone have low sensitivity for the diagnosis of AATD. In addition, standard pulmonary tests play an important role in determining the severity of lung disease. Chest radiography in this patient revealed hyperlucent areas in bilateral lower lobes but failed to show evidence of emphysema and flattening of diaphragms commonly observed in AATD. Because the patient's clinical history did not include sputum production for at least 3 months per year for 2 consecutive years, and because the prompt resolution of symptoms with a trial of steroids is more commonly seen in patients with asthma, COPD was considered less likely. CSS was ruled out because, despite blood eosinophil levels above 10% and a history of respiratory problems in childhood, no migrating opacities or neuropathies were noted in serial chest radiography. Allergic bronchopulmonary aspergillosis was ruled out because CT scanning did not show central bronchiectasis or fleeting pulmonary opacities. The patient's IgE levels were elevated; however, they were not above 1000 kU/L, which is common in aspergillosis. IgG and IgE antibodies to Aspergillus, which confirm the diagnosis, were not present in this case. CHF was ruled out because the patient's physical examination lacked findings such as the S3 findings, jugular venous distention, orthopnea, and lower extremity edema. Approximately 30%-40% of patients with heart failure have normal systolic function but abnormal diastolic relaxation."
],
"date": "October 05, 2022",
"figures": [],
"markdown": "# Palpitations, Cough in a Woman Who Lives Next to a Zookeeper\n\n **Authors:** Dora Izaguirre-Anariba, MD, MPH, CHES; Hung-I Liao, MD; Jesus C. Lanza, MD \n **Date:** October 05, 2022\n\n ## Content\n\n Asthma should be suspected in any person who presents with shortness of breath, wheezing, and cough; however, differential diagnoses that may mimic asthma must be ruled out. This requires a detailed clinical history and physical examination. The pathophysiology is complex and involves airway inflammation, intermittent airflow obstruction, and bronchial hyperresponsiveness. Environmental exposure usually plays an important role in symptom exacerbations. Smoking has been found in as many as 40% of the patients diagnosed with asthma.\nSpirometry with postbronchodilator response should be obtained as the primary test to establish airflow limitation consistent with asthma. Pulse oximetry measurement is desirable in all patients with acute asthma to determine hypoxemia. Chest radiography remains the initial imaging evaluation in most individuals with symptoms of asthma; however, in most patients with asthma, chest radiography findings are normal or may indicate hyperinflation. Exercise spirometry is the criterion standard method for assessing patients with exercise-induced bronchoconstriction. In addition, reversibility testing with steroid therapy should be performed, and any cardiac etiology should also be investigated.\nAATD was ruled out because the patient's clinical history did not include an abnormal AAT level. AAT levels <11 µmol/L are consistent with AATD. However, low AAT levels alone have low sensitivity for the diagnosis of AATD. In addition, standard pulmonary tests play an important role in determining the severity of lung disease. Chest radiography in this patient revealed hyperlucent areas in bilateral lower lobes but failed to show evidence of emphysema and flattening of diaphragms commonly observed in AATD. Because the patient's clinical history did not include sputum production for at least 3 months per year for 2 consecutive years, and because the prompt resolution of symptoms with a trial of steroids is more commonly seen in patients with asthma, COPD was considered less likely. CSS was ruled out because, despite blood eosinophil levels above 10% and a history of respiratory problems in childhood, no migrating opacities or neuropathies were noted in serial chest radiography. Allergic bronchopulmonary aspergillosis was ruled out because CT scanning did not show central bronchiectasis or fleeting pulmonary opacities. The patient's IgE levels were elevated; however, they were not above 1000 kU/L, which is common in aspergillosis. IgG and IgE antibodies to Aspergillus, which confirm the diagnosis, were not present in this case. CHF was ruled out because the patient's physical examination lacked findings such as the S3 findings, jugular venous distention, orthopnea, and lower extremity edema. Approximately 30%-40% of patients with heart failure have normal systolic function but abnormal diastolic relaxation.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1190168,
"choiceText": "AAT deficiency (AATD)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190170,
"choiceText": "Chronic obstructive pulmonary disease (COPD)",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190172,
"choiceText": "Churg-Strauss syndrome (CSS)",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190174,
"choiceText": "Asthma",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190176,
"choiceText": "Allergic bronchopulmonary aspergillosis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190178,
"choiceText": "Congestive heart failure (CHF)\r\n",
"correct": false,
"displayOrder": 6,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 378337,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Palpitations, Cough in a Woman Who Lives Next to a Zookeeper"
},
{
"authors": "Dora Izaguirre-Anariba, MD, MPH, CHES; Hung-I Liao, MD; Jesus C. Lanza, MD",
"content": [
"According to the World Health Organization (WHO), approximately 262 million people currently have asthma, with most asthma-related deaths occurring in the low-income and lower-middle-income countries.[1] The WHO estimated that, in 2019, 455,000 deaths were attributed to asthma. No universal definition of severe asthma was recognized until the American Thoracic Society and European Respiratory Society were established in 2013; they define \"severe asthma\" as asthma that requires treatment with high-dose inhaled steroids plus a second controller (and/or systemic corticosteroids) to prevent asthma from becoming uncontrolled.[2] Of note, the WHO classification in 2010 divided asthma into three groups: untreated asthma, incorrectly treated asthma, and difficult-to-treat asthma.[3]",
"The Global Initiative for Asthma (GINA) now recognizes uncontrolled, difficult-to-treat, and severe asthma.[4] Difficult-to-treat asthma is defined as asthma that remains uncontrolled despite prescribing of medium or high dose inhaled corticosteroid/long-acting beta2-agonist (ICS-LABA) treatment or asthma requiring high-dose ICS-LABA treatment to maintain quality symptom control and reduce exacerbations. Severe asthma is defined as asthma that remains uncontrolled despite adherence with optimized high-dose ICS-LABA treatment, as well as management of contributory factors, or asthma that worsens if high-dose treatment is decreased.",
"The basic criteria for the diagnosis of asthma include a detailed clinical history, physical examination, and pulmonary function testing. The history should include the nature, duration, and triggers of episodes, as well as the circumstances of the initial onset of symptoms. Occupation, seasonality, and circadian variations are also important, as is the response to treatment. The history should also include questions about smoking, travel, family history, and exacerbations/hospitalizations over the last 12 months. Lung function testing with spirometry or whole-body plethysmography, followed by reversibility testing (if airway obstruction is present) or hyperreactivity testing (if no airway obstruction is present) aid in the diagnosis of asthma.[3] Additionally, allergy testing should always be performed; measurement of exhaled nitric oxide is optional. A differential blood count is also needed to identify eosinophilia.",
"Whenever severe asthma is suspected, differential diagnoses that mimic asthma should be ruled out. In smokers, the lack of reversibility with short-acting bronchodilators is consistent with COPD. For instance, the use of prednisone for 7-14 days improves airflow limitation in patients with asthma, making COPD less likely. The use of CT imaging along with bronchoscopy, echocardiography, and 24-hour pH measurement is recommended in patients for whom the asthma diagnosis is not clear.[2]",
"Other medical conditions that may contribute to the severity of asthma include the following:",
"Use of nonsteroidal anti-inflammatory drugs, beta-adrenergic blockers, or angiotensin converting enzyme inhibitors",
"Rhinosinusitis",
"Nasal polyps",
"Psychosocial factors (eg, anxiety, depression)",
"Smoking",
"Gastroesophageal disorders",
"Sleep-related disorders (eg, sleep apnea)",
"As mentioned above, the most common diseases that emulate severe asthma include allergic bronchopulmonary aspergillosis, CSS, COPD, CHF, pulmonary embolism, bronchiectasis, cystic fibrosis, dysfunctional breathlessness, vocal cord dysfunction, and hypereosinophilic syndromes.[5,6]"
],
"date": "October 05, 2022",
"figures": [],
"markdown": "# Palpitations, Cough in a Woman Who Lives Next to a Zookeeper\n\n **Authors:** Dora Izaguirre-Anariba, MD, MPH, CHES; Hung-I Liao, MD; Jesus C. Lanza, MD \n **Date:** October 05, 2022\n\n ## Content\n\n According to the World Health Organization (WHO), approximately 262 million people currently have asthma, with most asthma-related deaths occurring in the low-income and lower-middle-income countries.[1] The WHO estimated that, in 2019, 455,000 deaths were attributed to asthma. No universal definition of severe asthma was recognized until the American Thoracic Society and European Respiratory Society were established in 2013; they define \"severe asthma\" as asthma that requires treatment with high-dose inhaled steroids plus a second controller (and/or systemic corticosteroids) to prevent asthma from becoming uncontrolled.[2] Of note, the WHO classification in 2010 divided asthma into three groups: untreated asthma, incorrectly treated asthma, and difficult-to-treat asthma.[3]\nThe Global Initiative for Asthma (GINA) now recognizes uncontrolled, difficult-to-treat, and severe asthma.[4] Difficult-to-treat asthma is defined as asthma that remains uncontrolled despite prescribing of medium or high dose inhaled corticosteroid/long-acting beta2-agonist (ICS-LABA) treatment or asthma requiring high-dose ICS-LABA treatment to maintain quality symptom control and reduce exacerbations. Severe asthma is defined as asthma that remains uncontrolled despite adherence with optimized high-dose ICS-LABA treatment, as well as management of contributory factors, or asthma that worsens if high-dose treatment is decreased.\nThe basic criteria for the diagnosis of asthma include a detailed clinical history, physical examination, and pulmonary function testing. The history should include the nature, duration, and triggers of episodes, as well as the circumstances of the initial onset of symptoms. Occupation, seasonality, and circadian variations are also important, as is the response to treatment. The history should also include questions about smoking, travel, family history, and exacerbations/hospitalizations over the last 12 months. Lung function testing with spirometry or whole-body plethysmography, followed by reversibility testing (if airway obstruction is present) or hyperreactivity testing (if no airway obstruction is present) aid in the diagnosis of asthma.[3] Additionally, allergy testing should always be performed; measurement of exhaled nitric oxide is optional. A differential blood count is also needed to identify eosinophilia.\nWhenever severe asthma is suspected, differential diagnoses that mimic asthma should be ruled out. In smokers, the lack of reversibility with short-acting bronchodilators is consistent with COPD. For instance, the use of prednisone for 7-14 days improves airflow limitation in patients with asthma, making COPD less likely. The use of CT imaging along with bronchoscopy, echocardiography, and 24-hour pH measurement is recommended in patients for whom the asthma diagnosis is not clear.[2]\nOther medical conditions that may contribute to the severity of asthma include the following:\nUse of nonsteroidal anti-inflammatory drugs, beta-adrenergic blockers, or angiotensin converting enzyme inhibitors\nRhinosinusitis\nNasal polyps\nPsychosocial factors (eg, anxiety, depression)\nSmoking\nGastroesophageal disorders\nSleep-related disorders (eg, sleep apnea)\nAs mentioned above, the most common diseases that emulate severe asthma include allergic bronchopulmonary aspergillosis, CSS, COPD, CHF, pulmonary embolism, bronchiectasis, cystic fibrosis, dysfunctional breathlessness, vocal cord dysfunction, and hypereosinophilic syndromes.[5,6]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Palpitations, Cough in a Woman Who Lives Next to a Zookeeper"
},
{
"authors": "Dora Izaguirre-Anariba, MD, MPH, CHES; Hung-I Liao, MD; Jesus C. Lanza, MD",
"content": [
"General recommendations in patients with severe asthma include the following[7]:",
"Optimization of inhaled therapy, with re-education and retraining on the use of inhaled therapy",
"Elimination of persistent triggers, including occupational allergens",
"Therapy of comorbidities, including weight reduction, management of chronic rhinosinusitis, gastroesophageal reflux disease, depression, and anxiety disorders.",
"Rehabilitation therapy should be provided on an inpatient or outpatient basis. Inpatient pulmonary rehabilitation should be considered in patients with severe asthma in whom psychosocial or socioeconomic conditions can worsen asthma severity. Long-acting anticholinergic or long-acting muscarinic antagonists are useful because they act at parasympathetic nervous system receptors that control airway tone. Anti-IgE therapy is useful in cases of severe allergic asthma. Data have shown a decrease by half in the number of severe exacerbations and a reduction in the need for use of corticosteroids; however, this is an expensive choice and is required every 2-4 weeks.",
"Macrolides have been recommended due to their immunomodulating effect. A clinical trial showed that weekly use of azithromycin decreased the risk for exacerbation by almost half in patients with severe noneosinophilic asthma.[8] Potential side effects should be considered while using macrolides for severe asthma. The phosphodiesterase 4 inhibitors have also shown efficacy in management of patients. Bronchial thermoplasty and endobronchial radiofrequency remain under investigation. Antibodies that target interleukin 5 or its receptor are currently under investigation as well.",
"The patient in this case was confirmed to have asthma; she was started on high-dose inhaled corticosteroids with dual controller inhalers and had significant improvement of respiratory symptoms. Her spirometry demonstrated significant improvement in FEV1. She has had no significant recurrence for almost 2 years."
],
"date": "October 05, 2022",
"figures": [],
"markdown": "# Palpitations, Cough in a Woman Who Lives Next to a Zookeeper\n\n **Authors:** Dora Izaguirre-Anariba, MD, MPH, CHES; Hung-I Liao, MD; Jesus C. Lanza, MD \n **Date:** October 05, 2022\n\n ## Content\n\n General recommendations in patients with severe asthma include the following[7]:\nOptimization of inhaled therapy, with re-education and retraining on the use of inhaled therapy\nElimination of persistent triggers, including occupational allergens\nTherapy of comorbidities, including weight reduction, management of chronic rhinosinusitis, gastroesophageal reflux disease, depression, and anxiety disorders.\nRehabilitation therapy should be provided on an inpatient or outpatient basis. Inpatient pulmonary rehabilitation should be considered in patients with severe asthma in whom psychosocial or socioeconomic conditions can worsen asthma severity. Long-acting anticholinergic or long-acting muscarinic antagonists are useful because they act at parasympathetic nervous system receptors that control airway tone. Anti-IgE therapy is useful in cases of severe allergic asthma. Data have shown a decrease by half in the number of severe exacerbations and a reduction in the need for use of corticosteroids; however, this is an expensive choice and is required every 2-4 weeks.\nMacrolides have been recommended due to their immunomodulating effect. A clinical trial showed that weekly use of azithromycin decreased the risk for exacerbation by almost half in patients with severe noneosinophilic asthma.[8] Potential side effects should be considered while using macrolides for severe asthma. The phosphodiesterase 4 inhibitors have also shown efficacy in management of patients. Bronchial thermoplasty and endobronchial radiofrequency remain under investigation. Antibodies that target interleukin 5 or its receptor are currently under investigation as well.\nThe patient in this case was confirmed to have asthma; she was started on high-dose inhaled corticosteroids with dual controller inhalers and had significant improvement of respiratory symptoms. Her spirometry demonstrated significant improvement in FEV1. She has had no significant recurrence for almost 2 years.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1190180,
"choiceText": "Asthma that remains uncontrolled despite medium-dose ICS-LABA treatment",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190182,
"choiceText": "Asthma that worsens if high-dose treatment is decreased ",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190184,
"choiceText": "Asthma that requires high-dose ICS-LABA to maintain symptom control ",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190186,
"choiceText": "Asthma that requires high-dose ICS-LABA to reduce exacerbations",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The Global Initiative for Asthma (GINA) now recognizes uncontrolled, difficult-to-treat, and severe asthma. Difficult-to-treat asthma is defined as asthma that remains uncontrolled despite prescribing of medium or high dose inhaled corticosteroid/long-acting beta2-agonist (ICS-LABA) treatment or asthma requiring high-dose ICS-LABA treatment to maintain quality symptom control and reduce exacerbations. Severe asthma is defined as asthma that remains uncontrolled despite adherence with optimized high-dose ICS-LABA treatment, as well as management of contributory factors, or asthma that worsens if high-dose treatment is decreased.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 378339,
"questionText": "Which of the following criteria supports the diagnosis of severe asthma?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1190188,
"choiceText": "Immunotherapy",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190190,
"choiceText": "Vitamin D supplementation",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190192,
"choiceText": "Inhaled corticosteroids alone",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190194,
"choiceText": "Optimized high-dose ICS-LABA treatment",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190196,
"choiceText": "Inhaled corticosteroids plus an inhaled short-acting beta-agonist",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "General recommendations in patients with severe asthma include the following:<ul>\r\n<li>Optimization of ICS-LABA, with re-education and retraining on the use of inhaled therapy</li>\r\n<li>Elimination of persistent triggers, including occupational allergens</li>\r\n<li>Therapy of comorbidities, including weight reduction, management of chronic rhinosinusitis, gastroesophageal reflux disease, depression, and anxiety disorders. </li></ul>\r\nEvidence is insufficient to support the use of immunotherapy. Vitamin D supplementation in management of patients with severe asthma has been mentioned by some authors; however, research supporting this recommendation is also insufficient.\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 378341,
"questionText": "Which of the following interventions is indicated in the management of patients with severe asthma?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Palpitations, Cough in a Woman Who Lives Next to a Zookeeper"
},
{
"authors": "Dora Izaguirre-Anariba, MD, MPH, CHES; Hung-I Liao, MD; Jesus C. Lanza, MD",
"content": [],
"date": "October 05, 2022",
"figures": [],
"markdown": "# Palpitations, Cough in a Woman Who Lives Next to a Zookeeper\n\n **Authors:** Dora Izaguirre-Anariba, MD, MPH, CHES; Hung-I Liao, MD; Jesus C. Lanza, MD \n **Date:** October 05, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1190180,
"choiceText": "Asthma that remains uncontrolled despite medium-dose ICS-LABA treatment",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190182,
"choiceText": "Asthma that worsens if high-dose treatment is decreased ",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190184,
"choiceText": "Asthma that requires high-dose ICS-LABA to maintain symptom control ",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190186,
"choiceText": "Asthma that requires high-dose ICS-LABA to reduce exacerbations",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The Global Initiative for Asthma (GINA) now recognizes uncontrolled, difficult-to-treat, and severe asthma. Difficult-to-treat asthma is defined as asthma that remains uncontrolled despite prescribing of medium or high dose inhaled corticosteroid/long-acting beta2-agonist (ICS-LABA) treatment or asthma requiring high-dose ICS-LABA treatment to maintain quality symptom control and reduce exacerbations. Severe asthma is defined as asthma that remains uncontrolled despite adherence with optimized high-dose ICS-LABA treatment, as well as management of contributory factors, or asthma that worsens if high-dose treatment is decreased.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 378339,
"questionText": "Which of the following criteria supports the diagnosis of severe asthma?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1190188,
"choiceText": "Immunotherapy",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190190,
"choiceText": "Vitamin D supplementation",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190192,
"choiceText": "Inhaled corticosteroids alone",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190194,
"choiceText": "Optimized high-dose ICS-LABA treatment",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190196,
"choiceText": "Inhaled corticosteroids plus an inhaled short-acting beta-agonist",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "General recommendations in patients with severe asthma include the following:<ul>\r\n<li>Optimization of ICS-LABA, with re-education and retraining on the use of inhaled therapy</li>\r\n<li>Elimination of persistent triggers, including occupational allergens</li>\r\n<li>Therapy of comorbidities, including weight reduction, management of chronic rhinosinusitis, gastroesophageal reflux disease, depression, and anxiety disorders. </li></ul>\r\nEvidence is insufficient to support the use of immunotherapy. Vitamin D supplementation in management of patients with severe asthma has been mentioned by some authors; however, research supporting this recommendation is also insufficient.\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 378341,
"questionText": "Which of the following interventions is indicated in the management of patients with severe asthma?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Palpitations, Cough in a Woman Who Lives Next to a Zookeeper"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1190168,
"choiceText": "AAT deficiency (AATD)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190170,
"choiceText": "Chronic obstructive pulmonary disease (COPD)",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190172,
"choiceText": "Churg-Strauss syndrome (CSS)",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190174,
"choiceText": "Asthma",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190176,
"choiceText": "Allergic bronchopulmonary aspergillosis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190178,
"choiceText": "Congestive heart failure (CHF)\r\n",
"correct": false,
"displayOrder": 6,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 378337,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1190180,
"choiceText": "Asthma that remains uncontrolled despite medium-dose ICS-LABA treatment",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190182,
"choiceText": "Asthma that worsens if high-dose treatment is decreased ",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190184,
"choiceText": "Asthma that requires high-dose ICS-LABA to maintain symptom control ",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190186,
"choiceText": "Asthma that requires high-dose ICS-LABA to reduce exacerbations",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The Global Initiative for Asthma (GINA) now recognizes uncontrolled, difficult-to-treat, and severe asthma. Difficult-to-treat asthma is defined as asthma that remains uncontrolled despite prescribing of medium or high dose inhaled corticosteroid/long-acting beta2-agonist (ICS-LABA) treatment or asthma requiring high-dose ICS-LABA treatment to maintain quality symptom control and reduce exacerbations. Severe asthma is defined as asthma that remains uncontrolled despite adherence with optimized high-dose ICS-LABA treatment, as well as management of contributory factors, or asthma that worsens if high-dose treatment is decreased.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 378339,
"questionText": "Which of the following criteria supports the diagnosis of severe asthma?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1190188,
"choiceText": "Immunotherapy",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190190,
"choiceText": "Vitamin D supplementation",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190192,
"choiceText": "Inhaled corticosteroids alone",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190194,
"choiceText": "Optimized high-dose ICS-LABA treatment",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1190196,
"choiceText": "Inhaled corticosteroids plus an inhaled short-acting beta-agonist",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "General recommendations in patients with severe asthma include the following:<ul>\r\n<li>Optimization of ICS-LABA, with re-education and retraining on the use of inhaled therapy</li>\r\n<li>Elimination of persistent triggers, including occupational allergens</li>\r\n<li>Therapy of comorbidities, including weight reduction, management of chronic rhinosinusitis, gastroesophageal reflux disease, depression, and anxiety disorders. </li></ul>\r\nEvidence is insufficient to support the use of immunotherapy. Vitamin D supplementation in management of patients with severe asthma has been mentioned by some authors; however, research supporting this recommendation is also insufficient.\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 378341,
"questionText": "Which of the following interventions is indicated in the management of patients with severe asthma?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
888807 | /viewarticle/888807 | [
{
"authors": "Niranjan N. Singh, MBBS, MD, DM",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 35-year-old man presents to the neurology clinic due to abnormal movements over the past 6 years. The involuntary movements began in the right upper limb, followed sequentially by the left upper limb, left lower limb, and finally the head and neck. The movements occur during wakefulness and are absent in sleep. They are described as jerky and nonpurposeful. His gait has assumed a dancelike character. He also has had behavioral changes that include frequent outbursts of anger, aggressive behavior, depressive mood, and insomnia. His abnormal movements are aggravated during outbursts of anger and disturbances in mood.",
"He has no weakness in any limbs but is unable to perform regular household activities. Family members have also noted memory impairment. He has been unable to continue his work as a machine operator for the past 3 months.",
"He has no history of drug intake, including phenytoin, phenothiazines, haloperidol, L-dopa, lithium, isoniazid, amphetamines, tricyclic antidepressants, or any other relevant drugs. He reports no history of chest pain, breathlessness, or joint pain. His family history includes a paternal grandfather and father who had similar forms of abnormal movements and died at the age of 60 years and 55 years, respectively.",
"The patient has five siblings (two brothers, three sisters). His elder brother died by suicide at age 25 years, and his elder sister died at age 33 years. Both had abnormal movements and abnormal behaviors. One of his younger sisters (age 22 years) also has similar abnormal movements and depressed attitude. His younger brother (age 17 years) and other younger sister (age 14 years) are healthy and symptom-free. The patient's children, an 8-year-old son and a 10-year-old daughter, are symptom-free.",
"His past medical history is positive for hypertension, which is well controlled with lisinopril (20 mg daily). He has no surgical history. He does not smoke, drink, or use recreational drugs."
],
"date": "October 04, 2022",
"figures": [],
"markdown": "# Neuro Case Challenge: A 35-Year-Old With Angry, Aggressive Outbursts, Memory Loss, and Insomnia\n\n **Authors:** Niranjan N. Singh, MBBS, MD, DM \n **Date:** October 04, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 35-year-old man presents to the neurology clinic due to abnormal movements over the past 6 years. The involuntary movements began in the right upper limb, followed sequentially by the left upper limb, left lower limb, and finally the head and neck. The movements occur during wakefulness and are absent in sleep. They are described as jerky and nonpurposeful. His gait has assumed a dancelike character. He also has had behavioral changes that include frequent outbursts of anger, aggressive behavior, depressive mood, and insomnia. His abnormal movements are aggravated during outbursts of anger and disturbances in mood.\nHe has no weakness in any limbs but is unable to perform regular household activities. Family members have also noted memory impairment. He has been unable to continue his work as a machine operator for the past 3 months.\nHe has no history of drug intake, including phenytoin, phenothiazines, haloperidol, L-dopa, lithium, isoniazid, amphetamines, tricyclic antidepressants, or any other relevant drugs. He reports no history of chest pain, breathlessness, or joint pain. His family history includes a paternal grandfather and father who had similar forms of abnormal movements and died at the age of 60 years and 55 years, respectively.\nThe patient has five siblings (two brothers, three sisters). His elder brother died by suicide at age 25 years, and his elder sister died at age 33 years. Both had abnormal movements and abnormal behaviors. One of his younger sisters (age 22 years) also has similar abnormal movements and depressed attitude. His younger brother (age 17 years) and other younger sister (age 14 years) are healthy and symptom-free. The patient's children, an 8-year-old son and a 10-year-old daughter, are symptom-free.\nHis past medical history is positive for hypertension, which is well controlled with lisinopril (20 mg daily). He has no surgical history. He does not smoke, drink, or use recreational drugs.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Neuro Case Challenge: A 35-Year-Old With Angry, Aggressive Outbursts, Memory Loss, and Insomnia"
},
{
"authors": "Niranjan N. Singh, MBBS, MD, DM",
"content": [
"A general examination reveals a pleasant man who is well built and in no acute distress. His blood pressure is 140/80 mm Hg, his heart rate is 78 beats/min, his respiratory rate is 12 breaths/min, his SpO2 level is 98% on room air, and his body mass index (BMI) is 20. He is afebrile.",
"A cardiovascular examination reveals normal peripheral pulses and normal heart findings. A chest examination reveals normal auscultation and expansion. His abdomen is soft. Head, eyes, ears, nose, and throat (HEENT) examination findings are unremarkable. He does not have a skin rash. A visual examination reveals normal acuity, field, and fundi.",
"His affect is flat. A neurologic examination of the higher mental functions reveals that the patient is awake and alert, with normal orientation, attention, concentration, fund of knowledge, and language function. His memory is impaired, with recall one-third at 3 minutes. He has a normal past memory. His speech is normal. A cranial nerve examination reveals normal extraocular movements, increased blink rate, normal facial sensation, a symmetric face with abnormal fidgety movement, normal hearing, and normal palate movement. He has abnormal tongue movement and cannot protrude his tongue more than 20 seconds (darting tongue movement). He has normal shoulder shrug. No Kayser-Fleischer ring is noted during slit-lamp examination.",
"An examination of the motor system reveals decreased muscle tone, normal bulk, and 5/5 strength in both upper and lower extremities. No atrophy or fasciculation is noted. Deep tendon reflexes are normal (2+ with flexor planters). Sensory examination findings are normal. Finger-nose test findings are normal. An examination of the extrapyramidal system reveals reduced tone and involuntary choreoathetoid movements that affect both upper and lower extremities as well as his face. He has a dancing gait.",
"Diagnostic tests reveal normal complete blood cell count (CBC) and comprehensive metabolic panel findings. He has normal serum findings and urine copper levels. His erythrocyte sedimentation rate (ESR) is 22 mm/hr (reference range, 0-22 mm/hr). He has normal ECG findings, a normal thyroid-stimulating hormone (TSH) level, a normal transthoracic echo (with ejection fraction 65%), and normal chest radiography findings.",
"MRI of the brain reveals evidence of bilateral caudate atrophy, with increased intercaudate distance (Figure).",
"Figure.",
"Figure.",
"Cerebrospinal fluid (CSF) examination findings are normal."
],
"date": "October 04, 2022",
"figures": [
{
"caption": "Figure.",
"image_url": "https://img.medscapestatic.com/article/888/807/888807-Thumb1.png"
}
],
"markdown": "# Neuro Case Challenge: A 35-Year-Old With Angry, Aggressive Outbursts, Memory Loss, and Insomnia\n\n **Authors:** Niranjan N. Singh, MBBS, MD, DM \n **Date:** October 04, 2022\n\n ## Content\n\n A general examination reveals a pleasant man who is well built and in no acute distress. His blood pressure is 140/80 mm Hg, his heart rate is 78 beats/min, his respiratory rate is 12 breaths/min, his SpO2 level is 98% on room air, and his body mass index (BMI) is 20. He is afebrile.\nA cardiovascular examination reveals normal peripheral pulses and normal heart findings. A chest examination reveals normal auscultation and expansion. His abdomen is soft. Head, eyes, ears, nose, and throat (HEENT) examination findings are unremarkable. He does not have a skin rash. A visual examination reveals normal acuity, field, and fundi.\nHis affect is flat. A neurologic examination of the higher mental functions reveals that the patient is awake and alert, with normal orientation, attention, concentration, fund of knowledge, and language function. His memory is impaired, with recall one-third at 3 minutes. He has a normal past memory. His speech is normal. A cranial nerve examination reveals normal extraocular movements, increased blink rate, normal facial sensation, a symmetric face with abnormal fidgety movement, normal hearing, and normal palate movement. He has abnormal tongue movement and cannot protrude his tongue more than 20 seconds (darting tongue movement). He has normal shoulder shrug. No Kayser-Fleischer ring is noted during slit-lamp examination.\nAn examination of the motor system reveals decreased muscle tone, normal bulk, and 5/5 strength in both upper and lower extremities. No atrophy or fasciculation is noted. Deep tendon reflexes are normal (2+ with flexor planters). Sensory examination findings are normal. Finger-nose test findings are normal. An examination of the extrapyramidal system reveals reduced tone and involuntary choreoathetoid movements that affect both upper and lower extremities as well as his face. He has a dancing gait.\nDiagnostic tests reveal normal complete blood cell count (CBC) and comprehensive metabolic panel findings. He has normal serum findings and urine copper levels. His erythrocyte sedimentation rate (ESR) is 22 mm/hr (reference range, 0-22 mm/hr). He has normal ECG findings, a normal thyroid-stimulating hormone (TSH) level, a normal transthoracic echo (with ejection fraction 65%), and normal chest radiography findings.\nMRI of the brain reveals evidence of bilateral caudate atrophy, with increased intercaudate distance (Figure).\nFigure.\nFigure.\nCerebrospinal fluid (CSF) examination findings are normal.\n\n ## Figures\n\n **Figure.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1158164,
"choiceText": "Neuroacanthocytosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158166,
"choiceText": "Tardive dyskinesia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158168,
"choiceText": "Huntington disease",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158170,
"choiceText": "Sydenham chorea",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 367975,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Neuro Case Challenge: A 35-Year-Old With Angry, Aggressive Outbursts, Memory Loss, and Insomnia"
},
{
"authors": "Niranjan N. Singh, MBBS, MD, DM",
"content": [
"This 35-year-old man has Huntington disease. He has insidious-onset, slowly progressive movement disorder, and movements are absent during sleep. His movements are described as choreoathetoid. He has family history that suggests autosomal dominant transmission. Apart from the movement disorder, he also has neuropsychiatric manifestations, with early death in the family due to depression. A CT scan of the head revealed evidence of caudate nucleus atrophy. Brain MRI revealed evidence of caudate atrophy (Figure).",
"Figure.",
"Regarding the differential diagnoses, he has no history of antipsychotic medication use, which can lead to tardive dyskinesia. He has no history of infection or diagnostic evidence that suggested heart involvement. He had no ECG changes or abnormalities on transthoracic echocardiography, as is seen in patients with Sydenham chorea. His family history is negative for Sydenham chorea. No acanthocytes were noted.",
"Huntington disease is a rare neurodegenerative disorder of the central nervous system (CNS) characterized by choreiform movements, behavioral and psychiatric disturbances, and dementia.[1]Huntington disease is caused by an autosomal-dominantly inherited expansion of CAG trinucleotide repeats in the huntingtin (HTT) gene on chromosome 4; this leads to production of a mutant huntingtin (mHTT) protein, with an abnormally long polyglutamine repeat.[2]Individuals with more than 39 CAG repeats develop the disease, whereas reduced penetrance is seen in those with 36-39 CAG repeats. The disease can be anticipated when the gene is passed down the paternal line, as in this case; a father with a CAG repeat length in the intermediate range may have a child with an expanded pathogenic repeat length. This is because sperm from males shows greater repeat variability and larger repeat sizes than somatic tissues. Mutant huntingtin protein leads to death and neuronal dysfunction through various mechanisms. Postmortem studies reveal diffuse atrophy of the caudate and putamen.",
"Prevalence in the white population is estimated at 1 in 10,000 to 1 in 20,000. The mean age at symptom onset is 30-50 years. In some cases, symptoms begin before age 20 years, with behavior disturbances and learning difficulties at school; this is termed juvenile Huntington disease (Westphal disease).[3]The first description, by Waters, dates to 1842. However, after a description in 1872 by George Huntington, it became known as Huntington chorea. In 1983, a linkage on chromosome 4 was established, and in 1993 the gene for Huntington disease was found.[1]"
],
"date": "October 04, 2022",
"figures": [
{
"caption": "Figure.",
"image_url": "https://img.medscapestatic.com/article/888/807/888807-Thumb1.png"
}
],
"markdown": "# Neuro Case Challenge: A 35-Year-Old With Angry, Aggressive Outbursts, Memory Loss, and Insomnia\n\n **Authors:** Niranjan N. Singh, MBBS, MD, DM \n **Date:** October 04, 2022\n\n ## Content\n\n This 35-year-old man has Huntington disease. He has insidious-onset, slowly progressive movement disorder, and movements are absent during sleep. His movements are described as choreoathetoid. He has family history that suggests autosomal dominant transmission. Apart from the movement disorder, he also has neuropsychiatric manifestations, with early death in the family due to depression. A CT scan of the head revealed evidence of caudate nucleus atrophy. Brain MRI revealed evidence of caudate atrophy (Figure).\nFigure.\nRegarding the differential diagnoses, he has no history of antipsychotic medication use, which can lead to tardive dyskinesia. He has no history of infection or diagnostic evidence that suggested heart involvement. He had no ECG changes or abnormalities on transthoracic echocardiography, as is seen in patients with Sydenham chorea. His family history is negative for Sydenham chorea. No acanthocytes were noted.\nHuntington disease is a rare neurodegenerative disorder of the central nervous system (CNS) characterized by choreiform movements, behavioral and psychiatric disturbances, and dementia.[1]Huntington disease is caused by an autosomal-dominantly inherited expansion of CAG trinucleotide repeats in the huntingtin (HTT) gene on chromosome 4; this leads to production of a mutant huntingtin (mHTT) protein, with an abnormally long polyglutamine repeat.[2]Individuals with more than 39 CAG repeats develop the disease, whereas reduced penetrance is seen in those with 36-39 CAG repeats. The disease can be anticipated when the gene is passed down the paternal line, as in this case; a father with a CAG repeat length in the intermediate range may have a child with an expanded pathogenic repeat length. This is because sperm from males shows greater repeat variability and larger repeat sizes than somatic tissues. Mutant huntingtin protein leads to death and neuronal dysfunction through various mechanisms. Postmortem studies reveal diffuse atrophy of the caudate and putamen.\nPrevalence in the white population is estimated at 1 in 10,000 to 1 in 20,000. The mean age at symptom onset is 30-50 years. In some cases, symptoms begin before age 20 years, with behavior disturbances and learning difficulties at school; this is termed juvenile Huntington disease (Westphal disease).[3]The first description, by Waters, dates to 1842. However, after a description in 1872 by George Huntington, it became known as Huntington chorea. In 1983, a linkage on chromosome 4 was established, and in 1993 the gene for Huntington disease was found.[1]\n\n ## Figures\n\n **Figure.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1158164,
"choiceText": "Neuroacanthocytosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158166,
"choiceText": "Tardive dyskinesia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158168,
"choiceText": "Huntington disease",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158170,
"choiceText": "Sydenham chorea",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 367975,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Neuro Case Challenge: A 35-Year-Old With Angry, Aggressive Outbursts, Memory Loss, and Insomnia"
},
{
"authors": "Niranjan N. Singh, MBBS, MD, DM",
"content": [
"Diagnosis of Huntington disease is confirmed by demonstration of autosomal dominant transmission or gene testing in the presence of clinical features.[4]",
"The clinical features of Huntington disease consist of motor, cognitive, and neuropsychiatric manifestations. Huntington disease has a biphasic course of hyperkinetic phase with chorea in the early stages of disease that then plateaus into a hypokinetic phase, consisting of bradykinesia dystonia, balance issues, and gait disturbance. The younger-onset variant is associated with predominant bradykinesia.[5]Cognitive disturbance can be seen many years before other symptom onset and is characterized by impaired emotion recognition, processing speed, and executive function abnormality. Neuropsychiatric symptoms widely vary, including apathy, anxiety, irritability, depression, obsessive-compulsive behavior, and psychosis.",
"Numerous conditions can mimic Huntington disease, including a spinal cerebellar ataxia 17, spinocerebellar ataxia 1-3, and Friedreich ataxia, which involve neuropathy. If seizures are also present, dentatorubropallidoluysian atrophy should be considered. Acanthocytes are seen in patients with neuroacanthocytosis.[6,7,8] Isolated chorea can be seen in acquired conditions, including chorea gravidarum, systemic lupus erythematosus, antiphospholipid syndrome, thyrotoxicosis, postinfectious syndromes, polycythemia vera, and some drug use.",
"Genetic testing for the mHTT mutation can be either diagnostic or predictive.[5] A diagnostic test may be performed when a patient presents with typical motor features of Huntington disease. Prior to testing, the patient should be informed about Huntington disease and its hereditary nature, as a positive test result has implications for the patient and family. Predictive testing is performed in asymptomatic patients, mostly for reproductive reasons."
],
"date": "October 04, 2022",
"figures": [],
"markdown": "# Neuro Case Challenge: A 35-Year-Old With Angry, Aggressive Outbursts, Memory Loss, and Insomnia\n\n **Authors:** Niranjan N. Singh, MBBS, MD, DM \n **Date:** October 04, 2022\n\n ## Content\n\n Diagnosis of Huntington disease is confirmed by demonstration of autosomal dominant transmission or gene testing in the presence of clinical features.[4]\nThe clinical features of Huntington disease consist of motor, cognitive, and neuropsychiatric manifestations. Huntington disease has a biphasic course of hyperkinetic phase with chorea in the early stages of disease that then plateaus into a hypokinetic phase, consisting of bradykinesia dystonia, balance issues, and gait disturbance. The younger-onset variant is associated with predominant bradykinesia.[5]Cognitive disturbance can be seen many years before other symptom onset and is characterized by impaired emotion recognition, processing speed, and executive function abnormality. Neuropsychiatric symptoms widely vary, including apathy, anxiety, irritability, depression, obsessive-compulsive behavior, and psychosis.\nNumerous conditions can mimic Huntington disease, including a spinal cerebellar ataxia 17, spinocerebellar ataxia 1-3, and Friedreich ataxia, which involve neuropathy. If seizures are also present, dentatorubropallidoluysian atrophy should be considered. Acanthocytes are seen in patients with neuroacanthocytosis.[6,7,8] Isolated chorea can be seen in acquired conditions, including chorea gravidarum, systemic lupus erythematosus, antiphospholipid syndrome, thyrotoxicosis, postinfectious syndromes, polycythemia vera, and some drug use.\nGenetic testing for the mHTT mutation can be either diagnostic or predictive.[5] A diagnostic test may be performed when a patient presents with typical motor features of Huntington disease. Prior to testing, the patient should be informed about Huntington disease and its hereditary nature, as a positive test result has implications for the patient and family. Predictive testing is performed in asymptomatic patients, mostly for reproductive reasons.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Neuro Case Challenge: A 35-Year-Old With Angry, Aggressive Outbursts, Memory Loss, and Insomnia"
},
{
"authors": "Niranjan N. Singh, MBBS, MD, DM",
"content": [
"The optimal management of Huntington disease involves a multidisciplinary approach that includes neurology, nurses, physical therapy, speech-language pathology, and dietitians and other healthcare professionals. The goal is to optimize the quality of life based on the changing need of the patient. These consist of combined pharmacologic and lifestyle changes, including behavioral therapy. Tetrabenazine and the modified version, deutetrabenazine, can be used to treat choreiform movements. A sustained anti-choreic effect is seen at 50-75 mg/day.[9] Side effects include depression and anxiety. Sulpiride, olanzapine, risperidone, and quetiapine are also used to manage chorea; weight gain and sedation are important side effects.",
"Limited evidence is available regarding the treatment of psychiatric symptoms in Huntington disease. Depression, anxiety, obsessive-compulsive disorder, and irritability may be treated with nonpharmacologic interventions, such as cognitive-behavioral therapy or psychodynamic therapy. Pharmacologic interventions may involve selective serotonin reuptake inhibitors, including citalopram, fluoxetine, paroxetine, sertraline, mirtazapine, and venlafaxine. Neuroleptics can be used to treat psychosis. Methylphenidate, atomoxetine, modafinil, amantadine, bromocriptine, and bupropion have been used to treat apathy. Evidence does not support medications used to help cognitive symptoms. Coping strategies may be useful as an alternative.",
"Apart from symptomatic treatment, pharmacologic agents have failed to show benefit in clinical trials as disease-modifying agents. The most promising approaches in regard to disease modification are emerging therapies aimed at lowering levels of mHTT by targeting either the DNA or RNA of the mHTT gene.[10] RNA targeting can be achieved using antisense oligonucleotides (ASOs), RNA interference (RNAi), or small-molecule splicing inhibitors. ASOs are currently being tested in humans for the first time. They are delivered intrathecally and catalyze the degradation of HTT mRNA by RNAse H, thereby reducing the production of the mHTT protein. In animal models, this results in as much as an 80% sustained reduction in HTT mRNA levels. Targeting the DNA of mHTT can be achieved using two approaches: zinc finger proteins and the clustered interspaced short palindromic repeats (CRISPR)/Cas9 system. The method was successfully tested in a rodent model of Huntington disease.[11]",
"The patient in this case was diagnosed with Huntington disease with CAG repeat 78. He was started on tetrabenazine for abnormal movements and citalopram for depression. He opted to apply for federal disability. His children are asymptomatic, and the family decided not to investigate until symptoms develop or they are age 18 years."
],
"date": "October 04, 2022",
"figures": [],
"markdown": "# Neuro Case Challenge: A 35-Year-Old With Angry, Aggressive Outbursts, Memory Loss, and Insomnia\n\n **Authors:** Niranjan N. Singh, MBBS, MD, DM \n **Date:** October 04, 2022\n\n ## Content\n\n The optimal management of Huntington disease involves a multidisciplinary approach that includes neurology, nurses, physical therapy, speech-language pathology, and dietitians and other healthcare professionals. The goal is to optimize the quality of life based on the changing need of the patient. These consist of combined pharmacologic and lifestyle changes, including behavioral therapy. Tetrabenazine and the modified version, deutetrabenazine, can be used to treat choreiform movements. A sustained anti-choreic effect is seen at 50-75 mg/day.[9] Side effects include depression and anxiety. Sulpiride, olanzapine, risperidone, and quetiapine are also used to manage chorea; weight gain and sedation are important side effects.\nLimited evidence is available regarding the treatment of psychiatric symptoms in Huntington disease. Depression, anxiety, obsessive-compulsive disorder, and irritability may be treated with nonpharmacologic interventions, such as cognitive-behavioral therapy or psychodynamic therapy. Pharmacologic interventions may involve selective serotonin reuptake inhibitors, including citalopram, fluoxetine, paroxetine, sertraline, mirtazapine, and venlafaxine. Neuroleptics can be used to treat psychosis. Methylphenidate, atomoxetine, modafinil, amantadine, bromocriptine, and bupropion have been used to treat apathy. Evidence does not support medications used to help cognitive symptoms. Coping strategies may be useful as an alternative.\nApart from symptomatic treatment, pharmacologic agents have failed to show benefit in clinical trials as disease-modifying agents. The most promising approaches in regard to disease modification are emerging therapies aimed at lowering levels of mHTT by targeting either the DNA or RNA of the mHTT gene.[10] RNA targeting can be achieved using antisense oligonucleotides (ASOs), RNA interference (RNAi), or small-molecule splicing inhibitors. ASOs are currently being tested in humans for the first time. They are delivered intrathecally and catalyze the degradation of HTT mRNA by RNAse H, thereby reducing the production of the mHTT protein. In animal models, this results in as much as an 80% sustained reduction in HTT mRNA levels. Targeting the DNA of mHTT can be achieved using two approaches: zinc finger proteins and the clustered interspaced short palindromic repeats (CRISPR)/Cas9 system. The method was successfully tested in a rodent model of Huntington disease.[11]\nThe patient in this case was diagnosed with Huntington disease with CAG repeat 78. He was started on tetrabenazine for abnormal movements and citalopram for depression. He opted to apply for federal disability. His children are asymptomatic, and the family decided not to investigate until symptoms develop or they are age 18 years.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1158172,
"choiceText": "Peripheral neuropathy",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158174,
"choiceText": "Dysuria",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158176,
"choiceText": "Ophthalmoplegia",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158178,
"choiceText": " Neuropsychiatric manifestations",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Huntington disease is a disease of the CNS that predominantly affects the basal ganglia, including the caudate and putamen. The classic presentation involves a triad of chorea, neuropsychiatric manifestations, and dementia with autosomal dominant inheritance. Peripheral neuropathy, ophthalmoplegia, and dysuria are not commonly associated with Huntington disease.\r\n<br><br>\r\nOther conditions with chorea and neuropsychiatric manifestations, such as neuroacanthocytosis, spinocerebellar ataxia, and dentatorubropallidoluysian apathy, usually present with involvement of central and peripheral nervous systems and may have evidence of peripheral neuropathy.\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 367977,
"questionText": "Which is a clinical manifestation commonly associated with Huntington disease?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1158180,
"choiceText": "Tetrabenazine",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158182,
"choiceText": "Citalopram ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158184,
"choiceText": "Modafinil ",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158186,
"choiceText": "Atomoxetine",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Tetrabenazine is a synaptic vesicular amine transport inhibitor that provides a sustained anti-choreic effect at doses in the range of 50-75 mg/day. Side effects include sleep problems, depression, anxiety, and restlessness. Citalopram is a selective serotonin reuptake inhibitor used to manage depression. Modafinil and atomoxetine are stimulants used to manage apathy.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 367979,
"questionText": "Which medication is most commonly used to manage chorea in patients with Huntington disease?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Neuro Case Challenge: A 35-Year-Old With Angry, Aggressive Outbursts, Memory Loss, and Insomnia"
},
{
"authors": "Niranjan N. Singh, MBBS, MD, DM",
"content": [],
"date": "October 04, 2022",
"figures": [],
"markdown": "# Neuro Case Challenge: A 35-Year-Old With Angry, Aggressive Outbursts, Memory Loss, and Insomnia\n\n **Authors:** Niranjan N. Singh, MBBS, MD, DM \n **Date:** October 04, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1158172,
"choiceText": "Peripheral neuropathy",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158174,
"choiceText": "Dysuria",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158176,
"choiceText": "Ophthalmoplegia",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158178,
"choiceText": " Neuropsychiatric manifestations",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Huntington disease is a disease of the CNS that predominantly affects the basal ganglia, including the caudate and putamen. The classic presentation involves a triad of chorea, neuropsychiatric manifestations, and dementia with autosomal dominant inheritance. Peripheral neuropathy, ophthalmoplegia, and dysuria are not commonly associated with Huntington disease.\r\n<br><br>\r\nOther conditions with chorea and neuropsychiatric manifestations, such as neuroacanthocytosis, spinocerebellar ataxia, and dentatorubropallidoluysian apathy, usually present with involvement of central and peripheral nervous systems and may have evidence of peripheral neuropathy.\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 367977,
"questionText": "Which is a clinical manifestation commonly associated with Huntington disease?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1158180,
"choiceText": "Tetrabenazine",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158182,
"choiceText": "Citalopram ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158184,
"choiceText": "Modafinil ",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158186,
"choiceText": "Atomoxetine",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Tetrabenazine is a synaptic vesicular amine transport inhibitor that provides a sustained anti-choreic effect at doses in the range of 50-75 mg/day. Side effects include sleep problems, depression, anxiety, and restlessness. Citalopram is a selective serotonin reuptake inhibitor used to manage depression. Modafinil and atomoxetine are stimulants used to manage apathy.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 367979,
"questionText": "Which medication is most commonly used to manage chorea in patients with Huntington disease?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Neuro Case Challenge: A 35-Year-Old With Angry, Aggressive Outbursts, Memory Loss, and Insomnia"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1158164,
"choiceText": "Neuroacanthocytosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158166,
"choiceText": "Tardive dyskinesia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158168,
"choiceText": "Huntington disease",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158170,
"choiceText": "Sydenham chorea",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 367975,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1158172,
"choiceText": "Peripheral neuropathy",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158174,
"choiceText": "Dysuria",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158176,
"choiceText": "Ophthalmoplegia",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158178,
"choiceText": " Neuropsychiatric manifestations",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Huntington disease is a disease of the CNS that predominantly affects the basal ganglia, including the caudate and putamen. The classic presentation involves a triad of chorea, neuropsychiatric manifestations, and dementia with autosomal dominant inheritance. Peripheral neuropathy, ophthalmoplegia, and dysuria are not commonly associated with Huntington disease.\r\n<br><br>\r\nOther conditions with chorea and neuropsychiatric manifestations, such as neuroacanthocytosis, spinocerebellar ataxia, and dentatorubropallidoluysian apathy, usually present with involvement of central and peripheral nervous systems and may have evidence of peripheral neuropathy.\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 367977,
"questionText": "Which is a clinical manifestation commonly associated with Huntington disease?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1158180,
"choiceText": "Tetrabenazine",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158182,
"choiceText": "Citalopram ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158184,
"choiceText": "Modafinil ",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1158186,
"choiceText": "Atomoxetine",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Tetrabenazine is a synaptic vesicular amine transport inhibitor that provides a sustained anti-choreic effect at doses in the range of 50-75 mg/day. Side effects include sleep problems, depression, anxiety, and restlessness. Citalopram is a selective serotonin reuptake inhibitor used to manage depression. Modafinil and atomoxetine are stimulants used to manage apathy.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 367979,
"questionText": "Which medication is most commonly used to manage chorea in patients with Huntington disease?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
980966 | /viewarticle/980966 | [
{
"authors": "Bashar Sharma, MD; John W. Birk, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 48-year-old man presents to the emergency department with epigastric pain, nausea, nonbloody vomiting, and anorexia. He describes the pain as constant, with a sharp, stabbing nature. Lying in a fetal position alleviates the pain. He has no fever, chest pain, dyspnea, or recent weight loss. The pain started suddenly 2 days ago while he was at work. It progressively worsened, and he was unable to keep down oral intake. He had similar symptoms 2 months earlier; however, they were mild and resolved spontaneously.",
"The patient has a medical history of poorly controlled type 2 diabetes, obesity class 2 (body mass index, 35-40), hypertension, hypothyroidism, and obstructive sleep apnea treated with continuous positive airway pressure. He has not had any surgeries in the past.",
"His family history is significant for coronary artery disease in his father, diabetes in his mother, and alcoholic cirrhosis and chronic pancreatitis in a maternal uncle. He has no family history of gastrointestinal cancers or inflammatory bowel disease. He does not smoke cigarettes, and he drinks 1-2 glasses of wine on the weekend. He reports no illicit drug use.",
"He takes amlodipine (5 mg daily), levothyroxine (100 µg daily), and metformin (500 mg twice daily). He denies any new medications or changes to his current ones. He works as a paralegal and has not had any recent falls or trauma."
],
"date": "September 23, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: Pain, Vomiting in a 48-Year-Old on Levothyroxine, Metformin\n\n **Authors:** Bashar Sharma, MD; John W. Birk, MD \n **Date:** September 23, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 48-year-old man presents to the emergency department with epigastric pain, nausea, nonbloody vomiting, and anorexia. He describes the pain as constant, with a sharp, stabbing nature. Lying in a fetal position alleviates the pain. He has no fever, chest pain, dyspnea, or recent weight loss. The pain started suddenly 2 days ago while he was at work. It progressively worsened, and he was unable to keep down oral intake. He had similar symptoms 2 months earlier; however, they were mild and resolved spontaneously.\nThe patient has a medical history of poorly controlled type 2 diabetes, obesity class 2 (body mass index, 35-40), hypertension, hypothyroidism, and obstructive sleep apnea treated with continuous positive airway pressure. He has not had any surgeries in the past.\nHis family history is significant for coronary artery disease in his father, diabetes in his mother, and alcoholic cirrhosis and chronic pancreatitis in a maternal uncle. He has no family history of gastrointestinal cancers or inflammatory bowel disease. He does not smoke cigarettes, and he drinks 1-2 glasses of wine on the weekend. He reports no illicit drug use.\nHe takes amlodipine (5 mg daily), levothyroxine (100 µg daily), and metformin (500 mg twice daily). He denies any new medications or changes to his current ones. He works as a paralegal and has not had any recent falls or trauma.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Gastro Case Challenge: Pain, Vomiting in a 48-Year-Old on Levothyroxine, Metformin"
},
{
"authors": "Bashar Sharma, MD; John W. Birk, MD",
"content": [
"Upon examination, the patient is alert and oriented. He lies sideways in bed in mild distress due to the pain. He is afebrile, but his heart rate is tachycardic at 108 beats/min. His blood pressure is 88/59 mm Hg. His respiration rate is 24 breaths/min, and his oxygen saturation is 98% on room air. The results of cardiac and respiratory examinations are normal. The abdominal examination is significant for epigastric tenderness and decreased bowel sounds, but his abdomen is otherwise soft, without any guarding or rebound tenderness.",
"Laboratory investigations reveal these values:",
"Hemoglobin level: 15 g/dL (reference range, 13.2-17.1 g/dL)",
"Hematocrit: 47% (reference range, 40%-54%)",
"White blood cell count: 14,200 cells/µL (reference range, 5000-10,000 cells/µL)",
"Platelet count: 420,000 cells/µL (reference range, 135,000-337,000 cells/µL)",
"Creatinine: 1.5 mg/dL (reference range, 0.8-1.5 mg/dL)",
"Blood urea nitrogen: 34 mg/dL (reference range, 7-20 mg/dL)",
"Calcium: 9.9 mg/dL (reference range, 8-10 mg/dL)",
"Lactic acid: 3.7 mg/dL (reference range, 4.5-19.8 mg/dL)",
"Glucose: 466 mg/dL (reference range, 65-110 mg/dL)",
"Alanine aminotransferase: 54 U/L (reference range, 20-60 U/L)",
"Aspartate aminotransferase: 43 U/L (reference range, 6-34 U/L)",
"Alkaline phosphatase: 96 U/L (reference range, 44-147 U/L)",
"Bilirubin: 0.4 mg/dL (reference range, 0.1-1.2 mg/dL)",
"Lipase: 874 U/L (reference range, 8-51 U/L)",
"Amylase: 364 U/L (reference range, 25-125 U/L)",
"Antinuclear antibody: positive with 1:40 titer",
"Immunoglobulin G4 (IgG4): 187 mg/dL (reference range, 8-140 mg/dL)",
"Total cholesterol: 278 mg/dL (reference range, < 200 mg/dL)",
"Triglycerides: 921 mg/dL (reference range, < 150 mg/dL)",
"A CT of the abdomen and pelvis with intravenous (IV) contrast shows moderate peripancreatic edema, consistent with acute pancreatitis (Figure 1 and Figure 2). A 3 × 2 × 2.5 cm septated cyst is present in the tail of the pancreas. No pancreatic ductal dilatation is noted. The gallbladder is normal, without biliary ductal dilation.",
"Figure 1.",
"Figure 2."
],
"date": "September 23, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: Pain, Vomiting in a 48-Year-Old on Levothyroxine, Metformin\n\n **Authors:** Bashar Sharma, MD; John W. Birk, MD \n **Date:** September 23, 2022\n\n ## Content\n\n Upon examination, the patient is alert and oriented. He lies sideways in bed in mild distress due to the pain. He is afebrile, but his heart rate is tachycardic at 108 beats/min. His blood pressure is 88/59 mm Hg. His respiration rate is 24 breaths/min, and his oxygen saturation is 98% on room air. The results of cardiac and respiratory examinations are normal. The abdominal examination is significant for epigastric tenderness and decreased bowel sounds, but his abdomen is otherwise soft, without any guarding or rebound tenderness.\nLaboratory investigations reveal these values:\nHemoglobin level: 15 g/dL (reference range, 13.2-17.1 g/dL)\nHematocrit: 47% (reference range, 40%-54%)\nWhite blood cell count: 14,200 cells/µL (reference range, 5000-10,000 cells/µL)\nPlatelet count: 420,000 cells/µL (reference range, 135,000-337,000 cells/µL)\nCreatinine: 1.5 mg/dL (reference range, 0.8-1.5 mg/dL)\nBlood urea nitrogen: 34 mg/dL (reference range, 7-20 mg/dL)\nCalcium: 9.9 mg/dL (reference range, 8-10 mg/dL)\nLactic acid: 3.7 mg/dL (reference range, 4.5-19.8 mg/dL)\nGlucose: 466 mg/dL (reference range, 65-110 mg/dL)\nAlanine aminotransferase: 54 U/L (reference range, 20-60 U/L)\nAspartate aminotransferase: 43 U/L (reference range, 6-34 U/L)\nAlkaline phosphatase: 96 U/L (reference range, 44-147 U/L)\nBilirubin: 0.4 mg/dL (reference range, 0.1-1.2 mg/dL)\nLipase: 874 U/L (reference range, 8-51 U/L)\nAmylase: 364 U/L (reference range, 25-125 U/L)\nAntinuclear antibody: positive with 1:40 titer\nImmunoglobulin G4 (IgG4): 187 mg/dL (reference range, 8-140 mg/dL)\nTotal cholesterol: 278 mg/dL (reference range, < 200 mg/dL)\nTriglycerides: 921 mg/dL (reference range, < 150 mg/dL)\nA CT of the abdomen and pelvis with intravenous (IV) contrast shows moderate peripancreatic edema, consistent with acute pancreatitis (Figure 1 and Figure 2). A 3 × 2 × 2.5 cm septated cyst is present in the tail of the pancreas. No pancreatic ductal dilatation is noted. The gallbladder is normal, without biliary ductal dilation.\nFigure 1.\nFigure 2.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1719264,
"choiceText": "Autoimmune pancreatitis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719265,
"choiceText": "Drug-induced pancreatitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719266,
"choiceText": "Triglyceride-induced pancreatitis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719267,
"choiceText": "Alcoholic pancreatitis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719268,
"choiceText": "Hereditary pancreatitis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 554729,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: Pain, Vomiting in a 48-Year-Old on Levothyroxine, Metformin"
},
{
"authors": "Bashar Sharma, MD; John W. Birk, MD",
"content": [
"Autoimmune pancreatitis is an unusual cause of pancreatitis, in which the immune system attacks the pancreas, resulting in inflammation of the organ. It has two subtypes. Type 1, or lymphoplasmacytic sclerosing pancreatitis, which is the most common type, is characterized histologically by lymphocyte and plasma cell infiltration with fibrosis. It usually presents in older men with obstructive jaundice, with or without a pancreatic mass; diffuse pancreatic enlargement on imaging; and pancreatic ductal strictures. Abdominal pain occurs in less than 50% of cases.[1] It is associated with elevated serum IgG4 (more than two times the upper limit of normal) and can present as an isolated disease or as part of an IgG4-related systemic disorder with other organ involvement, such as the biliary system, lacrimal and salivary glands, kidneys, lymph nodes, and retroperitoneum.",
"Type 2 or idiopathic duct-centric pancreatitis is the less common type. Typically, patients present at a younger age, and 75% have abdominal pain. IgG4 is only mildly elevated. It is also the more frequent type in patients with inflammatory bowel disease. The diagnosis is made using the International Consensus Diagnostic Criteria, which include serology, imaging of pancreatic parenchyma and duct, pancreatic histology, other organ involvement, and response to corticosteroid therapy as an optional criterion.[2] The patient in this case is relatively young, with a serum IgG4 level less than twice the upper limit of normal, and he has a normal bilirubin level. He also has no other organ involvement besides the pancreas and no family history of inflammatory bowel disease. His imaging studies show no evidence of pancreatic masses or diffuse enlargement. Thus, autoimmune pancreatitis is less likely.",
"Drug-induced pancreatitis is unlikely because none of his medications are known to cause pancreatitis. In addition, his alcohol intake is not high enough to cause alcoholic pancreatitis; however, a skillful history of intake should be obtained. Hereditary pancreatitis is a genetic disorder in which acute recurrent pancreatitis develops in childhood or early adolescence and usually progresses to chronic pancreatitis by early adulthood. The most common type is secondary to a mutation in the trypsinogen gene (PRSS1), which is inherited in an autosomal dominant pattern.[3] The patient in this case had his first episode of pancreatitis in his fifth decade of life and does not have any family history of pancreatitis, except for his uncle, who probably has chronic pancreatitis due to alcohol abuse. Hereditary pancreatitis is thus unlikely."
],
"date": "September 23, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: Pain, Vomiting in a 48-Year-Old on Levothyroxine, Metformin\n\n **Authors:** Bashar Sharma, MD; John W. Birk, MD \n **Date:** September 23, 2022\n\n ## Content\n\n Autoimmune pancreatitis is an unusual cause of pancreatitis, in which the immune system attacks the pancreas, resulting in inflammation of the organ. It has two subtypes. Type 1, or lymphoplasmacytic sclerosing pancreatitis, which is the most common type, is characterized histologically by lymphocyte and plasma cell infiltration with fibrosis. It usually presents in older men with obstructive jaundice, with or without a pancreatic mass; diffuse pancreatic enlargement on imaging; and pancreatic ductal strictures. Abdominal pain occurs in less than 50% of cases.[1] It is associated with elevated serum IgG4 (more than two times the upper limit of normal) and can present as an isolated disease or as part of an IgG4-related systemic disorder with other organ involvement, such as the biliary system, lacrimal and salivary glands, kidneys, lymph nodes, and retroperitoneum.\nType 2 or idiopathic duct-centric pancreatitis is the less common type. Typically, patients present at a younger age, and 75% have abdominal pain. IgG4 is only mildly elevated. It is also the more frequent type in patients with inflammatory bowel disease. The diagnosis is made using the International Consensus Diagnostic Criteria, which include serology, imaging of pancreatic parenchyma and duct, pancreatic histology, other organ involvement, and response to corticosteroid therapy as an optional criterion.[2] The patient in this case is relatively young, with a serum IgG4 level less than twice the upper limit of normal, and he has a normal bilirubin level. He also has no other organ involvement besides the pancreas and no family history of inflammatory bowel disease. His imaging studies show no evidence of pancreatic masses or diffuse enlargement. Thus, autoimmune pancreatitis is less likely.\nDrug-induced pancreatitis is unlikely because none of his medications are known to cause pancreatitis. In addition, his alcohol intake is not high enough to cause alcoholic pancreatitis; however, a skillful history of intake should be obtained. Hereditary pancreatitis is a genetic disorder in which acute recurrent pancreatitis develops in childhood or early adolescence and usually progresses to chronic pancreatitis by early adulthood. The most common type is secondary to a mutation in the trypsinogen gene (PRSS1), which is inherited in an autosomal dominant pattern.[3] The patient in this case had his first episode of pancreatitis in his fifth decade of life and does not have any family history of pancreatitis, except for his uncle, who probably has chronic pancreatitis due to alcohol abuse. Hereditary pancreatitis is thus unlikely.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1719264,
"choiceText": "Autoimmune pancreatitis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719265,
"choiceText": "Drug-induced pancreatitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719266,
"choiceText": "Triglyceride-induced pancreatitis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719267,
"choiceText": "Alcoholic pancreatitis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719268,
"choiceText": "Hereditary pancreatitis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 554729,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: Pain, Vomiting in a 48-Year-Old on Levothyroxine, Metformin"
},
{
"authors": "Bashar Sharma, MD; John W. Birk, MD",
"content": [
"Triglyceride-induced pancreatitis accounts for 4% of all episodes of acute pancreatitis and as many as 56% of cases in pregnancy.[4] One study revealed that the risk for pancreatitis was 5% at triglyceride levels > 1000 mg/dL and 10%-20% at levels > 2000 mg/dL.[5] A triglyceride level > 1000 mg/dL has been used as a cutoff for the diagnosis; however, the risk for pancreatitis progressively increases with serum levels and can occur even at levels as low as 400 mg/dL. In addition, triglyceride levels can rapidly trend down soon after symptoms start because the decrease in oral intake and fasting will lower the triglyceride-rich chylomicrons in the serum. An elevation in serum triglycerides during acute pancreatitis has traditionally been associated with increased lipolysis, and thus the diagnosis is often discounted. However, a high index of suspicion is needed if the traditional causes seem unlikely and additional risk factors are present. Once the pancreatitis has resolved, serial triglyceride levels need to be obtained.",
"The exact mechanism of pancreatitis is not well understood, but it is believed to be secondary to free fatty acids generated from the breakdown of triglycerides by pancreatic lipase. These free fatty acids can cause pancreatic cell injury and ischemia, in addition to the inflammatory response caused by the pancreatitis itself that leads to tissue injury.[6]",
"The etiology of elevated triglycerides is divided into primary and secondary causes. Primary causes are genetic mutations in lipid metabolism that lead to severe hypertriglyceridemia and can predispose to pancreatitis. These include Fredrickson classification type I, IV, and V dyslipidemias, also known as familial hyperchylomicronemia, familial hypertriglyceridemia, and combined hypertriglyceridemia, respectively.[7] Types I and V typically present with hypertriglyceridemia early in life, whereas type IV presents later and is usually triggered by a secondary factor. Secondary causes of elevated triglycerides are environmental and include poorly controlled diabetes, obesity, hypothyroidism, and alcohol use disorder.[4] Moreover, some medications have been implicated in hypertriglyceridemia leading to pancreatitis, including estrogens, clomiphene, tamoxifen, propofol, beta-blockers, protease inhibitors, olanzapine, mirtazapine, valproic acid, and isotretinoin.[5]",
"The clinical presentation of triglyceride-induced pancreatitis is usually similar to that of pancreatitis from other causes, with epigastric abdominal pain that typically radiates to the back and is associated with nausea and vomiting. However, the course of the disease tends to be more complicated, and the incidence of pancreatic necrosis, abscess formation, sepsis, and organ failure is higher than in pancreatitis from other causes.[8] Physical examination can reveal lipemia retinalis, xanthelasmas, xanthomas over extensor surfaces of the extremities, and hepatomegaly from fatty infiltration of the liver. The serum amylase level can be falsely normal owing to the interference of triglycerides with the assay, and serial dilutions are required to correct it.[9]",
"Management of triglyceride-induced pancreatitis involves treatment of the acute pancreatitis and lowering the triglyceride levels to < 400 mg/dL. Medications that can contribute to hypertriglyceridemia should be discontinued. Risk stratification of acute pancreatitis should be done early on admission to assess the severity of pancreatitis, using established indexes such as Acute Physiology and Chronic Health Evaluation II (APACHE II), Systemic Inflammatory Response Syndrome (SIRS) criteria, and/or Modified Marshall Score.[6] Initial management of pancreatitis includes supportive measures, with aggressive IV hydration, analgesia, and bowel rest. If the patient has severe pancreatitis and prolonged fasting is expected, pancreatic rest with nasojejunal enteral feeding or total parenteral nutrition should be considered.[5] No guidelines exist to guide the management of acute triglyceride-induced pancreatitis; however, it has been suggested that in patients with severe pancreatitis, additional therapies should be considered on the basis of the current available data.",
"Insulin activates lipoprotein lipase, leading to enhanced chylomicron and very-low–density lipoprotein (VLDL) metabolism and lowering of serum triglyceride levels, usually by 50%-75% in 2-3 days.[10] Insulin has been used in patients with severe pancreatitis, especially in those with diabetes and concomitant hyperglycemia, although multiple reports have shown that it is also effective in patients who do not have diabetes.[6] Frequent blood glucose checks are required, and dextrose infusion is needed as well to maintain euglycemia. Insulin should be discontinued when the serum triglyceride level is < 500 mg/dL.",
"In the past, IV heparin was used in combination with insulin because it can cause an initial rise in lipoprotein lipase levels owing to the release of endothelial lipoprotein lipase. This rise is followed, however, by increased degradation by the liver, which leads to lower enzyme levels and chylomicron accumulation, with rebound hypertriglyceridemia.[11] For this reason, heparin should be avoided."
],
"date": "September 23, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: Pain, Vomiting in a 48-Year-Old on Levothyroxine, Metformin\n\n **Authors:** Bashar Sharma, MD; John W. Birk, MD \n **Date:** September 23, 2022\n\n ## Content\n\n Triglyceride-induced pancreatitis accounts for 4% of all episodes of acute pancreatitis and as many as 56% of cases in pregnancy.[4] One study revealed that the risk for pancreatitis was 5% at triglyceride levels > 1000 mg/dL and 10%-20% at levels > 2000 mg/dL.[5] A triglyceride level > 1000 mg/dL has been used as a cutoff for the diagnosis; however, the risk for pancreatitis progressively increases with serum levels and can occur even at levels as low as 400 mg/dL. In addition, triglyceride levels can rapidly trend down soon after symptoms start because the decrease in oral intake and fasting will lower the triglyceride-rich chylomicrons in the serum. An elevation in serum triglycerides during acute pancreatitis has traditionally been associated with increased lipolysis, and thus the diagnosis is often discounted. However, a high index of suspicion is needed if the traditional causes seem unlikely and additional risk factors are present. Once the pancreatitis has resolved, serial triglyceride levels need to be obtained.\nThe exact mechanism of pancreatitis is not well understood, but it is believed to be secondary to free fatty acids generated from the breakdown of triglycerides by pancreatic lipase. These free fatty acids can cause pancreatic cell injury and ischemia, in addition to the inflammatory response caused by the pancreatitis itself that leads to tissue injury.[6]\nThe etiology of elevated triglycerides is divided into primary and secondary causes. Primary causes are genetic mutations in lipid metabolism that lead to severe hypertriglyceridemia and can predispose to pancreatitis. These include Fredrickson classification type I, IV, and V dyslipidemias, also known as familial hyperchylomicronemia, familial hypertriglyceridemia, and combined hypertriglyceridemia, respectively.[7] Types I and V typically present with hypertriglyceridemia early in life, whereas type IV presents later and is usually triggered by a secondary factor. Secondary causes of elevated triglycerides are environmental and include poorly controlled diabetes, obesity, hypothyroidism, and alcohol use disorder.[4] Moreover, some medications have been implicated in hypertriglyceridemia leading to pancreatitis, including estrogens, clomiphene, tamoxifen, propofol, beta-blockers, protease inhibitors, olanzapine, mirtazapine, valproic acid, and isotretinoin.[5]\nThe clinical presentation of triglyceride-induced pancreatitis is usually similar to that of pancreatitis from other causes, with epigastric abdominal pain that typically radiates to the back and is associated with nausea and vomiting. However, the course of the disease tends to be more complicated, and the incidence of pancreatic necrosis, abscess formation, sepsis, and organ failure is higher than in pancreatitis from other causes.[8] Physical examination can reveal lipemia retinalis, xanthelasmas, xanthomas over extensor surfaces of the extremities, and hepatomegaly from fatty infiltration of the liver. The serum amylase level can be falsely normal owing to the interference of triglycerides with the assay, and serial dilutions are required to correct it.[9]\nManagement of triglyceride-induced pancreatitis involves treatment of the acute pancreatitis and lowering the triglyceride levels to < 400 mg/dL. Medications that can contribute to hypertriglyceridemia should be discontinued. Risk stratification of acute pancreatitis should be done early on admission to assess the severity of pancreatitis, using established indexes such as Acute Physiology and Chronic Health Evaluation II (APACHE II), Systemic Inflammatory Response Syndrome (SIRS) criteria, and/or Modified Marshall Score.[6] Initial management of pancreatitis includes supportive measures, with aggressive IV hydration, analgesia, and bowel rest. If the patient has severe pancreatitis and prolonged fasting is expected, pancreatic rest with nasojejunal enteral feeding or total parenteral nutrition should be considered.[5] No guidelines exist to guide the management of acute triglyceride-induced pancreatitis; however, it has been suggested that in patients with severe pancreatitis, additional therapies should be considered on the basis of the current available data.\nInsulin activates lipoprotein lipase, leading to enhanced chylomicron and very-low–density lipoprotein (VLDL) metabolism and lowering of serum triglyceride levels, usually by 50%-75% in 2-3 days.[10] Insulin has been used in patients with severe pancreatitis, especially in those with diabetes and concomitant hyperglycemia, although multiple reports have shown that it is also effective in patients who do not have diabetes.[6] Frequent blood glucose checks are required, and dextrose infusion is needed as well to maintain euglycemia. Insulin should be discontinued when the serum triglyceride level is < 500 mg/dL.\nIn the past, IV heparin was used in combination with insulin because it can cause an initial rise in lipoprotein lipase levels owing to the release of endothelial lipoprotein lipase. This rise is followed, however, by increased degradation by the liver, which leads to lower enzyme levels and chylomicron accumulation, with rebound hypertriglyceridemia.[11] For this reason, heparin should be avoided.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Gastro Case Challenge: Pain, Vomiting in a 48-Year-Old on Levothyroxine, Metformin"
},
{
"authors": "Bashar Sharma, MD; John W. Birk, MD",
"content": [
"Plasmapheresis has also been used in patients with severe triglyceride-induced pancreatitis because it can lead to a rapid decline in serum triglycerides by about 66% after one session and 83% after two sessions.[12] In addition, it has the potential benefit of removing proteases that can further damage the pancreas. However, studies have not shown improved outcomes or mortality benefit.[5] If plasmapheresis is used, it should be initiated early, and serum triglycerides should be measured after every session. It should be stopped when the serum triglyceride level is < 500 mg/dL.",
"Once the patient is able to tolerate oral intake, a fat-restricted diet is recommended. In addition, triglyceride-lowering agents should be started; fibrates are the most effective.[6] A reasonable second choice is high-dose omega-3 fatty acids. Niacin and statins can be added to the regimen; however, the risk for adverse events, including rhabdomyolysis and myopathy, is higher with combination therapy, especially fibrates and statins.[6] Long-term management should involve lifestyle modifications, including a low-fat diet, aerobic exercise, weight loss in patients with obesity, strict glycemic control in patients with diabetes, and alcohol cessation in patients with alcohol use disorder.",
"In the patient in this case, the SIRS criteria score was 2 and the Modified Marshall Score was 2. These scores indicate severe pancreatitis. He was admitted to the ICU, and IV fluids and analgesics were started. Given his hyperglycemia and severe pancreatitis with evidence of end-organ damage (hypotension, tachycardia, and leukocytosis), insulin infusions were initiated, with monitoring of his serum glucose. Dextrose infusion was also started once his glucose level was < 180 mg/dL. His serum triglyceride level was measured daily while he was receiving insulin.",
"After 48 hours, his triglyceride level dropped to < 500 mg/dL, and the insulin was discontinued. His symptoms also started to improve. He was transitioned to a clear-liquid diet, then to a low-fat diet, which he tolerated well. Fenofibrate was started, and the patient was discharged home in stable condition, with a short follow-up."
],
"date": "September 23, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: Pain, Vomiting in a 48-Year-Old on Levothyroxine, Metformin\n\n **Authors:** Bashar Sharma, MD; John W. Birk, MD \n **Date:** September 23, 2022\n\n ## Content\n\n Plasmapheresis has also been used in patients with severe triglyceride-induced pancreatitis because it can lead to a rapid decline in serum triglycerides by about 66% after one session and 83% after two sessions.[12] In addition, it has the potential benefit of removing proteases that can further damage the pancreas. However, studies have not shown improved outcomes or mortality benefit.[5] If plasmapheresis is used, it should be initiated early, and serum triglycerides should be measured after every session. It should be stopped when the serum triglyceride level is < 500 mg/dL.\nOnce the patient is able to tolerate oral intake, a fat-restricted diet is recommended. In addition, triglyceride-lowering agents should be started; fibrates are the most effective.[6] A reasonable second choice is high-dose omega-3 fatty acids. Niacin and statins can be added to the regimen; however, the risk for adverse events, including rhabdomyolysis and myopathy, is higher with combination therapy, especially fibrates and statins.[6] Long-term management should involve lifestyle modifications, including a low-fat diet, aerobic exercise, weight loss in patients with obesity, strict glycemic control in patients with diabetes, and alcohol cessation in patients with alcohol use disorder.\nIn the patient in this case, the SIRS criteria score was 2 and the Modified Marshall Score was 2. These scores indicate severe pancreatitis. He was admitted to the ICU, and IV fluids and analgesics were started. Given his hyperglycemia and severe pancreatitis with evidence of end-organ damage (hypotension, tachycardia, and leukocytosis), insulin infusions were initiated, with monitoring of his serum glucose. Dextrose infusion was also started once his glucose level was < 180 mg/dL. His serum triglyceride level was measured daily while he was receiving insulin.\nAfter 48 hours, his triglyceride level dropped to < 500 mg/dL, and the insulin was discontinued. His symptoms also started to improve. He was transitioned to a clear-liquid diet, then to a low-fat diet, which he tolerated well. Fenofibrate was started, and the patient was discharged home in stable condition, with a short follow-up.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1719269,
"choiceText": "Heparin",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719270,
"choiceText": "Insulin",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719271,
"choiceText": "Statin",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719272,
"choiceText": "Total parenteral nutrition",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "This patient has severe pancreatitis. Insulin has been used in patients with severe pancreatitis because it activates lipoprotein lipase, which leads to enhanced chylomicron and VLDL metabolism and lowering of serum triglycerides. In addition, it can help reduce hyperglycemia. <br><br>\r\nHeparin has shown benefit in lowering triglyceride levels initially by releasing endothelial lipoprotein lipase; however, it is associated with rebound hypertriglyceridemia and its use should be avoided. Oral lipid-lowering agents are usually started once the patient is able to tolerate oral intake. This patient has evidence of severe pancreatitis. She will need to be resuscitated first and managed with bowel rest until she is more stable and her triglyceride levels are trending down before starting nutrition, with oral or enteral feeding as the first choice.\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 554730,
"questionText": "A patient with a history of alcohol abuse presents with triglyceride-induced pancreatitis and evidence of severe disease based on the APACHE II score. Laboratory studies reveal hyperglycemia. She is admitted to the hospital, and IV fluids and analgesics are started. What is the most appropriate next treatment?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1719273,
"choiceText": "Statins",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719274,
"choiceText": "Niacin",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719275,
"choiceText": "Omega-3 fatty acids",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719276,
"choiceText": "Fibrates",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Fibrates are the most effective agents in lowering triglycerides and should be started in patients with triglyceride levels > 400 mg/dL. They have been shown to reduce triglyceride levels by 36.3% compared with 10%-18% for statins, 20% for niacin, and 25%-33.8% for omega-3 fatty acids.<sup>[6]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 554731,
"questionText": "Which of these is most effective in lowering hypertriglyceridemia?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: Pain, Vomiting in a 48-Year-Old on Levothyroxine, Metformin"
},
{
"authors": "Bashar Sharma, MD; John W. Birk, MD",
"content": [
"Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult."
],
"date": "September 23, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: Pain, Vomiting in a 48-Year-Old on Levothyroxine, Metformin\n\n **Authors:** Bashar Sharma, MD; John W. Birk, MD \n **Date:** September 23, 2022\n\n ## Content\n\n Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult.\n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1719269,
"choiceText": "Heparin",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719270,
"choiceText": "Insulin",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719271,
"choiceText": "Statin",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719272,
"choiceText": "Total parenteral nutrition",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "This patient has severe pancreatitis. Insulin has been used in patients with severe pancreatitis because it activates lipoprotein lipase, which leads to enhanced chylomicron and VLDL metabolism and lowering of serum triglycerides. In addition, it can help reduce hyperglycemia. <br><br>\r\nHeparin has shown benefit in lowering triglyceride levels initially by releasing endothelial lipoprotein lipase; however, it is associated with rebound hypertriglyceridemia and its use should be avoided. Oral lipid-lowering agents are usually started once the patient is able to tolerate oral intake. This patient has evidence of severe pancreatitis. She will need to be resuscitated first and managed with bowel rest until she is more stable and her triglyceride levels are trending down before starting nutrition, with oral or enteral feeding as the first choice.\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 554730,
"questionText": "A patient with a history of alcohol abuse presents with triglyceride-induced pancreatitis and evidence of severe disease based on the APACHE II score. Laboratory studies reveal hyperglycemia. She is admitted to the hospital, and IV fluids and analgesics are started. What is the most appropriate next treatment?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1719273,
"choiceText": "Statins",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719274,
"choiceText": "Niacin",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719275,
"choiceText": "Omega-3 fatty acids",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719276,
"choiceText": "Fibrates",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Fibrates are the most effective agents in lowering triglycerides and should be started in patients with triglyceride levels > 400 mg/dL. They have been shown to reduce triglyceride levels by 36.3% compared with 10%-18% for statins, 20% for niacin, and 25%-33.8% for omega-3 fatty acids.<sup>[6]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 554731,
"questionText": "Which of these is most effective in lowering hypertriglyceridemia?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: Pain, Vomiting in a 48-Year-Old on Levothyroxine, Metformin"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1719264,
"choiceText": "Autoimmune pancreatitis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719265,
"choiceText": "Drug-induced pancreatitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719266,
"choiceText": "Triglyceride-induced pancreatitis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719267,
"choiceText": "Alcoholic pancreatitis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719268,
"choiceText": "Hereditary pancreatitis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 554729,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1719269,
"choiceText": "Heparin",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719270,
"choiceText": "Insulin",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719271,
"choiceText": "Statin",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719272,
"choiceText": "Total parenteral nutrition",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "This patient has severe pancreatitis. Insulin has been used in patients with severe pancreatitis because it activates lipoprotein lipase, which leads to enhanced chylomicron and VLDL metabolism and lowering of serum triglycerides. In addition, it can help reduce hyperglycemia. <br><br>\r\nHeparin has shown benefit in lowering triglyceride levels initially by releasing endothelial lipoprotein lipase; however, it is associated with rebound hypertriglyceridemia and its use should be avoided. Oral lipid-lowering agents are usually started once the patient is able to tolerate oral intake. This patient has evidence of severe pancreatitis. She will need to be resuscitated first and managed with bowel rest until she is more stable and her triglyceride levels are trending down before starting nutrition, with oral or enteral feeding as the first choice.\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 554730,
"questionText": "A patient with a history of alcohol abuse presents with triglyceride-induced pancreatitis and evidence of severe disease based on the APACHE II score. Laboratory studies reveal hyperglycemia. She is admitted to the hospital, and IV fluids and analgesics are started. What is the most appropriate next treatment?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1719273,
"choiceText": "Statins",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719274,
"choiceText": "Niacin",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719275,
"choiceText": "Omega-3 fatty acids",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1719276,
"choiceText": "Fibrates",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Fibrates are the most effective agents in lowering triglycerides and should be started in patients with triglyceride levels > 400 mg/dL. They have been shown to reduce triglyceride levels by 36.3% compared with 10%-18% for statins, 20% for niacin, and 25%-33.8% for omega-3 fatty acids.<sup>[6]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 554731,
"questionText": "Which of these is most effective in lowering hypertriglyceridemia?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
926232 | /viewarticle/926232 | [
{
"authors": "Thomas S. Higgins, Jr, MD, MSPH",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 35-year-old man with a history of adult-onset asthma has had nasal obstruction and smelling loss for 4 months. He also reports postnasal drainage, cough, rhinorrhea, and facial pressure. He has no history of asthma or allergies as a child. He also has no history of previous nasal or paranasal sinus surgery. His symptoms worsen after drinking certain beers and also after using ibuprofen or aspirin.",
"Over the past 4 months, he has been given three courses of antibiotics, including amoxicillin, azithromycin, and amoxicillin-clavulanate with minimal effect on his symptoms. He has used nasal steroid spray one spray twice a day for 2 months, with partial improvement in symptoms of nasal congestion. He has had two courses of methylprednisolone, which had a significant effect on his symptoms; however, the effect was transient."
],
"date": "September 15, 2022",
"figures": [],
"markdown": "# Beer, Aspirin Worsen Nasal Issues in a 35-Year-Old With Asthma\n\n **Authors:** Thomas S. Higgins, Jr, MD, MSPH \n **Date:** September 15, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 35-year-old man with a history of adult-onset asthma has had nasal obstruction and smelling loss for 4 months. He also reports postnasal drainage, cough, rhinorrhea, and facial pressure. He has no history of asthma or allergies as a child. He also has no history of previous nasal or paranasal sinus surgery. His symptoms worsen after drinking certain beers and also after using ibuprofen or aspirin.\nOver the past 4 months, he has been given three courses of antibiotics, including amoxicillin, azithromycin, and amoxicillin-clavulanate with minimal effect on his symptoms. He has used nasal steroid spray one spray twice a day for 2 months, with partial improvement in symptoms of nasal congestion. He has had two courses of methylprednisolone, which had a significant effect on his symptoms; however, the effect was transient.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Beer, Aspirin Worsen Nasal Issues in a 35-Year-Old With Asthma"
},
{
"authors": "Thomas S. Higgins, Jr, MD, MSPH",
"content": [
"Upon physical examination, the patient is alert, oriented, and in no acute distress. Vital signs include an oral temperature of 97.9°F (36.6°C), a blood pressure of 115/83 mm Hg, a heart rate of 65 beats/min, and a respiratory rate of 14 breaths/min. Head, ear, throat, and neck examination findings are unremarkable. Nasal examination shows large nasal polyps that fill the nasal cavities bilaterally, large inferior turbinates, and clear mucoid secretions (Figure 1). No crusting or scarring is observed.",
"Figure 1.",
"Auscultation of the lungs demonstrates mild expiratory wheezing bilaterally. Allergy skin testing reveals no reactions. Spirometry revealed a forced expiratory volume in the first second of expiration (FEV1) of 75%. Chest radiography findings are normal.",
"CT scan of the paranasal sinuses reveals severe pansinusitis with complete to near-complete opacification of the paranasal sinus cavities and nasal cavities (Figure 2).",
"Figure 2.",
"Mild osteitis of the paranasal sinus bone is observed, with no dehiscence of the lamina papyracea or skull base. Surgical pathology of the lesion reveals findings similar to the image shown below (Figure 3).",
"Figure 3."
],
"date": "September 15, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/926/232/926232-fig1-thumb.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/926/232/926232-fig2-thumb.jpg"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/926/232/926232-fig3-thumb.jpg"
}
],
"markdown": "# Beer, Aspirin Worsen Nasal Issues in a 35-Year-Old With Asthma\n\n **Authors:** Thomas S. Higgins, Jr, MD, MSPH \n **Date:** September 15, 2022\n\n ## Content\n\n Upon physical examination, the patient is alert, oriented, and in no acute distress. Vital signs include an oral temperature of 97.9°F (36.6°C), a blood pressure of 115/83 mm Hg, a heart rate of 65 beats/min, and a respiratory rate of 14 breaths/min. Head, ear, throat, and neck examination findings are unremarkable. Nasal examination shows large nasal polyps that fill the nasal cavities bilaterally, large inferior turbinates, and clear mucoid secretions (Figure 1). No crusting or scarring is observed.\nFigure 1.\nAuscultation of the lungs demonstrates mild expiratory wheezing bilaterally. Allergy skin testing reveals no reactions. Spirometry revealed a forced expiratory volume in the first second of expiration (FEV1) of 75%. Chest radiography findings are normal.\nCT scan of the paranasal sinuses reveals severe pansinusitis with complete to near-complete opacification of the paranasal sinus cavities and nasal cavities (Figure 2).\nFigure 2.\nMild osteitis of the paranasal sinus bone is observed, with no dehiscence of the lamina papyracea or skull base. Surgical pathology of the lesion reveals findings similar to the image shown below (Figure 3).\nFigure 3.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1478705,
"choiceText": "Nasal polyposis related to allergic fungal rhinosinusitis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478706,
"choiceText": "Sinonasal inverted papilloma",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478707,
"choiceText": "Nasal polyposis related to granulomatosis with polyangiitis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478708,
"choiceText": "Sinonasal undifferentiated carcinoma",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478709,
"choiceText": "Nasal polyposis related to aspirin-exacerbated respiratory disease",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 473058,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Beer, Aspirin Worsen Nasal Issues in a 35-Year-Old With Asthma"
},
{
"authors": "Thomas S. Higgins, Jr, MD, MSPH",
"content": [
"Nasal polyps are benign inflammatory growths in the nasal cavities and paranasal sinuses. They usually have no potential for malignant degeneration. They may form related to type 1 inflammation (eg, cystic fibrosis [CF], infectious processes) or type 2 inflammation (eg, allergy, aspirin-exacerbated respiratory disease [AERD]). Nasal polyps are usually a component of a process involving the paranasal sinuses, thus the term chronic rhinosinusitis with nasal polyps (CRSwNP) is often used. The two hallmark symptoms of CRSwNP are smelling loss and nasal obstruction.[1]",
"CRSwNP is a ubiquitous condition with a few recognized disease processes. AERD includes the triad of nasal polyposis, eosinophilic asthma, and aspirin sensitivity.[1] In this case, after the initiation of inhaled fluticasone/salmeterol to control his asthma symptoms, the patient returned for an oral aspirin challenge. His FEV1 had improved to 90%. He was administered 40.5 mg of aspirin, followed by 81 mg. The patient reported significantly increased nasal congestion and cough 1 hour after administration of the 81-mg dosage. His FEV1 decreased to 85% of baseline during the trial.",
"Allergic fungal rhinosinusitis (AFRS) is characterized as nasal polyposis with a positive result on fungal stain, eosinophilic mucin, and heterogeneity in the paranasal sinus cavities on CT scanning.[2] This diagnosis was less likely in this patient due to the presence of bilateral disease, lack of heterogeneity on imaging, and the fact that aspirin or nonsteroidal anti-inflammatory drug (NSAID) sensitivity is not typically present in patients with AFRS. CF is an autosomal recessive genetic condition related to a defect in the chloride-ion channel cystic fibrosis transmembrane conductance regulator protein (CFTR), causing impaired mucociliary clearance. Nasal polyposis in CF is often identified in childhood.[3]",
"Granulomatosis with polyangiitis (GPA), formerly called Wegener granulomatosis, is a rare inflammatory condition of small- and medium-sized blood vessels (vasculitis) that primarily occurs in the respiratory tract and kidneys. Although sinonasal scarring and nasal septal perforation are often seen in patients with this condition, nasal polyposis is not common.[4] This diagnosis was excluded because patients with GPA typically have severe crusting and scarring with a lack of nasal polyposis. In addition, this patient's pathologic findings did not reveal granulomata.",
"Eosinophilic granulomatosis with polyangiitis (EGPA), also called Churg-Strauss syndrome, is a small- and medium-sized vasculitis characterized by tissue eosinophilia and granulomata. Patients with EGPA often have asthma and paranasal sinus disease, with nasal polyposis found in more than 50% of cases.[5] This diagnosis is much less common than AERD, and the pathologic findings of this patient did not reveal granulomata.",
"In addition, sinonasal papilloma and sinonasal undifferentiated carcinoma were ruled out based on pathologic findings. Red flags for neoplasms include unilateral disease, cranial neuropathies, and intraorbital or intracranial extension."
],
"date": "September 15, 2022",
"figures": [],
"markdown": "# Beer, Aspirin Worsen Nasal Issues in a 35-Year-Old With Asthma\n\n **Authors:** Thomas S. Higgins, Jr, MD, MSPH \n **Date:** September 15, 2022\n\n ## Content\n\n Nasal polyps are benign inflammatory growths in the nasal cavities and paranasal sinuses. They usually have no potential for malignant degeneration. They may form related to type 1 inflammation (eg, cystic fibrosis [CF], infectious processes) or type 2 inflammation (eg, allergy, aspirin-exacerbated respiratory disease [AERD]). Nasal polyps are usually a component of a process involving the paranasal sinuses, thus the term chronic rhinosinusitis with nasal polyps (CRSwNP) is often used. The two hallmark symptoms of CRSwNP are smelling loss and nasal obstruction.[1]\nCRSwNP is a ubiquitous condition with a few recognized disease processes. AERD includes the triad of nasal polyposis, eosinophilic asthma, and aspirin sensitivity.[1] In this case, after the initiation of inhaled fluticasone/salmeterol to control his asthma symptoms, the patient returned for an oral aspirin challenge. His FEV1 had improved to 90%. He was administered 40.5 mg of aspirin, followed by 81 mg. The patient reported significantly increased nasal congestion and cough 1 hour after administration of the 81-mg dosage. His FEV1 decreased to 85% of baseline during the trial.\nAllergic fungal rhinosinusitis (AFRS) is characterized as nasal polyposis with a positive result on fungal stain, eosinophilic mucin, and heterogeneity in the paranasal sinus cavities on CT scanning.[2] This diagnosis was less likely in this patient due to the presence of bilateral disease, lack of heterogeneity on imaging, and the fact that aspirin or nonsteroidal anti-inflammatory drug (NSAID) sensitivity is not typically present in patients with AFRS. CF is an autosomal recessive genetic condition related to a defect in the chloride-ion channel cystic fibrosis transmembrane conductance regulator protein (CFTR), causing impaired mucociliary clearance. Nasal polyposis in CF is often identified in childhood.[3]\nGranulomatosis with polyangiitis (GPA), formerly called Wegener granulomatosis, is a rare inflammatory condition of small- and medium-sized blood vessels (vasculitis) that primarily occurs in the respiratory tract and kidneys. Although sinonasal scarring and nasal septal perforation are often seen in patients with this condition, nasal polyposis is not common.[4] This diagnosis was excluded because patients with GPA typically have severe crusting and scarring with a lack of nasal polyposis. In addition, this patient's pathologic findings did not reveal granulomata.\nEosinophilic granulomatosis with polyangiitis (EGPA), also called Churg-Strauss syndrome, is a small- and medium-sized vasculitis characterized by tissue eosinophilia and granulomata. Patients with EGPA often have asthma and paranasal sinus disease, with nasal polyposis found in more than 50% of cases.[5] This diagnosis is much less common than AERD, and the pathologic findings of this patient did not reveal granulomata.\nIn addition, sinonasal papilloma and sinonasal undifferentiated carcinoma were ruled out based on pathologic findings. Red flags for neoplasms include unilateral disease, cranial neuropathies, and intraorbital or intracranial extension.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1478705,
"choiceText": "Nasal polyposis related to allergic fungal rhinosinusitis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478706,
"choiceText": "Sinonasal inverted papilloma",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478707,
"choiceText": "Nasal polyposis related to granulomatosis with polyangiitis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478708,
"choiceText": "Sinonasal undifferentiated carcinoma",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478709,
"choiceText": "Nasal polyposis related to aspirin-exacerbated respiratory disease",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 473058,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Beer, Aspirin Worsen Nasal Issues in a 35-Year-Old With Asthma"
},
{
"authors": "Thomas S. Higgins, Jr, MD, MSPH",
"content": [
"AERD, formerly known as Samter's triad, is an inflammatory condition of the respiratory tract that includes eosinophilic asthma, nasal polyposis, and aspirin hypersensitivity. It represents approximately 10% of cases of CRSwNP. The disease is characterized by hypersensitivity to compounds that inhibit the cyclooxygenase pathway, including aspirin, NSAIDs, and acetaminophen.[1] Widal and colleagues[6] first described AERD in 1922. Max Samter, MD, coined the term \"Samter's triad\" in 1967.[7] The hypersensitivity reaction causes type 2 inflammation, which affects both the lower and upper airways.[8]",
"Diagnosis of AERD should be considered in patients with concomitant asthma and opacified paranasal sinuses on imaging. AERD is highly likely in the population of patients who report respiratory symptoms within 90 minutes of exposure to aspirin or NSAIDs, complete anosmia associated with nasal polyps, rapid regrowth of nasal polyps after sinus surgery, or asthma attacks after ingestion of alcoholic beverages.[9] It should be noted that alcohol consumption has been reported to aggravate symptoms associated with nasal polyps, such as certain beers did for the patient in this case.[10] AERD is considered highly unlikely in patients who report asthma and nasal polyps in childhood. Oral aspirin challenge is considered the standard diagnostic confirmatory test for AERD and was used to confirm the diagnosis in this patient.[9]",
"The goal of AERD management is control of airway inflammation. Medical therapies include systemic glucocorticosteroids, antileukotriene inhibitors (ie, montelukast or zileuton), topical anti-inflammatory inhalers and nasal sprays, and sinonasal rinses. Aspirin desensitization is a therapy unique to AERD that has been shown to improve outcomes in many patients.[9] The process of desensitization is performed by slowly increasing dosages of aspirin over 1-3 days until the hypersensitivity reaction fails to occur. The patients then continue to receive an aspirin regimen, usually between 325 mg or 650 mg twice a day, as maintenance therapy. Two potential complications of this therapy include peptic ulcer disease and excessive bleeding.[9]",
"A few monoclonal antibody therapies (biologic agents) are also available for control of severe asthma and/or nasal polyposis related to AERD. These medications include benralizumab, dupilumab, mepolizumab, and omalizumab. Their mechanism of action is to reduce type 2 inflammation by inhibiting immunoglobulin E or the proliferation of eosinophils.[8]"
],
"date": "September 15, 2022",
"figures": [],
"markdown": "# Beer, Aspirin Worsen Nasal Issues in a 35-Year-Old With Asthma\n\n **Authors:** Thomas S. Higgins, Jr, MD, MSPH \n **Date:** September 15, 2022\n\n ## Content\n\n AERD, formerly known as Samter's triad, is an inflammatory condition of the respiratory tract that includes eosinophilic asthma, nasal polyposis, and aspirin hypersensitivity. It represents approximately 10% of cases of CRSwNP. The disease is characterized by hypersensitivity to compounds that inhibit the cyclooxygenase pathway, including aspirin, NSAIDs, and acetaminophen.[1] Widal and colleagues[6] first described AERD in 1922. Max Samter, MD, coined the term \"Samter's triad\" in 1967.[7] The hypersensitivity reaction causes type 2 inflammation, which affects both the lower and upper airways.[8]\nDiagnosis of AERD should be considered in patients with concomitant asthma and opacified paranasal sinuses on imaging. AERD is highly likely in the population of patients who report respiratory symptoms within 90 minutes of exposure to aspirin or NSAIDs, complete anosmia associated with nasal polyps, rapid regrowth of nasal polyps after sinus surgery, or asthma attacks after ingestion of alcoholic beverages.[9] It should be noted that alcohol consumption has been reported to aggravate symptoms associated with nasal polyps, such as certain beers did for the patient in this case.[10] AERD is considered highly unlikely in patients who report asthma and nasal polyps in childhood. Oral aspirin challenge is considered the standard diagnostic confirmatory test for AERD and was used to confirm the diagnosis in this patient.[9]\nThe goal of AERD management is control of airway inflammation. Medical therapies include systemic glucocorticosteroids, antileukotriene inhibitors (ie, montelukast or zileuton), topical anti-inflammatory inhalers and nasal sprays, and sinonasal rinses. Aspirin desensitization is a therapy unique to AERD that has been shown to improve outcomes in many patients.[9] The process of desensitization is performed by slowly increasing dosages of aspirin over 1-3 days until the hypersensitivity reaction fails to occur. The patients then continue to receive an aspirin regimen, usually between 325 mg or 650 mg twice a day, as maintenance therapy. Two potential complications of this therapy include peptic ulcer disease and excessive bleeding.[9]\nA few monoclonal antibody therapies (biologic agents) are also available for control of severe asthma and/or nasal polyposis related to AERD. These medications include benralizumab, dupilumab, mepolizumab, and omalizumab. Their mechanism of action is to reduce type 2 inflammation by inhibiting immunoglobulin E or the proliferation of eosinophils.[8]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Beer, Aspirin Worsen Nasal Issues in a 35-Year-Old With Asthma"
},
{
"authors": "Thomas S. Higgins, Jr, MD, MSPH",
"content": [
"Surgical intervention, including polypectomy and endoscopic sinus surgery, is often beneficial in reducing the nasal polyp disease burden, ventilating the paranasal sinus cavities, and allowing better access for topical therapies in patients with AERD. AERD is often associated with the need for repeat surgeries because of the aggressiveness of the inflammatory process. Therefore, continued medical treatment is important.[1]",
"This patient underwent endoscopic sinus surgery with a postoperative maintenance therapy of budesonide nasal steroid rinses and zileuton. He also underwent aspirin desensitization 6 weeks after surgery with a maintenance aspirin regimen of 625 mg of aspirin per day. He maintained minimal symptoms with no evidence of nasal polyposis regrowth at 3 years follow-up."
],
"date": "September 15, 2022",
"figures": [],
"markdown": "# Beer, Aspirin Worsen Nasal Issues in a 35-Year-Old With Asthma\n\n **Authors:** Thomas S. Higgins, Jr, MD, MSPH \n **Date:** September 15, 2022\n\n ## Content\n\n Surgical intervention, including polypectomy and endoscopic sinus surgery, is often beneficial in reducing the nasal polyp disease burden, ventilating the paranasal sinus cavities, and allowing better access for topical therapies in patients with AERD. AERD is often associated with the need for repeat surgeries because of the aggressiveness of the inflammatory process. Therefore, continued medical treatment is important.[1]\nThis patient underwent endoscopic sinus surgery with a postoperative maintenance therapy of budesonide nasal steroid rinses and zileuton. He also underwent aspirin desensitization 6 weeks after surgery with a maintenance aspirin regimen of 625 mg of aspirin per day. He maintained minimal symptoms with no evidence of nasal polyposis regrowth at 3 years follow-up.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1478710,
"choiceText": "Type 1 inflammation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478711,
"choiceText": "Type 2 inflammation",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478712,
"choiceText": "Type 3 inflammation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478713,
"choiceText": "Neutrophilic inflammation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "AERD causes type 2 immunologic inflammation, which is characterized by the release of interleukin (IL)-4, IL-5, and IL-13 cytokines and eosinophilia. Other causes of type 2 inflammation include helminth infections, allergy, and asthma.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 473059,
"questionText": "Which of the following types of immunologic inflammation is most prominently associated with AERD?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1478714,
"choiceText": "Nasal polyposis has a high risk of malignant degeneration",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478715,
"choiceText": "Nasal polyposis is most commonly related to aspirin sensitivity",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478716,
"choiceText": "Nasal polyps related to AERD are usually identified in childhood",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478717,
"choiceText": "Nasal obstruction and anosmia are associated with nasal polyposis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Nasal polyposis cause symptoms of rhinosinusitis, including anterior and posterior nasal drainage, nasal congestion/obstruction, facial pain/pressure, and olfactory dysfunction. Nasal obstruction and olfactory compromise are common symptoms in nasal polyposis.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 473060,
"questionText": "Which of the following is most accurate regarding nasal polyposis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Beer, Aspirin Worsen Nasal Issues in a 35-Year-Old With Asthma"
},
{
"authors": "Thomas S. Higgins, Jr, MD, MSPH",
"content": [],
"date": "September 15, 2022",
"figures": [],
"markdown": "# Beer, Aspirin Worsen Nasal Issues in a 35-Year-Old With Asthma\n\n **Authors:** Thomas S. Higgins, Jr, MD, MSPH \n **Date:** September 15, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1478710,
"choiceText": "Type 1 inflammation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478711,
"choiceText": "Type 2 inflammation",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478712,
"choiceText": "Type 3 inflammation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478713,
"choiceText": "Neutrophilic inflammation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "AERD causes type 2 immunologic inflammation, which is characterized by the release of interleukin (IL)-4, IL-5, and IL-13 cytokines and eosinophilia. Other causes of type 2 inflammation include helminth infections, allergy, and asthma.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 473059,
"questionText": "Which of the following types of immunologic inflammation is most prominently associated with AERD?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1478714,
"choiceText": "Nasal polyposis has a high risk of malignant degeneration",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478715,
"choiceText": "Nasal polyposis is most commonly related to aspirin sensitivity",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478716,
"choiceText": "Nasal polyps related to AERD are usually identified in childhood",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478717,
"choiceText": "Nasal obstruction and anosmia are associated with nasal polyposis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Nasal polyposis cause symptoms of rhinosinusitis, including anterior and posterior nasal drainage, nasal congestion/obstruction, facial pain/pressure, and olfactory dysfunction. Nasal obstruction and olfactory compromise are common symptoms in nasal polyposis.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 473060,
"questionText": "Which of the following is most accurate regarding nasal polyposis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Beer, Aspirin Worsen Nasal Issues in a 35-Year-Old With Asthma"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1478705,
"choiceText": "Nasal polyposis related to allergic fungal rhinosinusitis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478706,
"choiceText": "Sinonasal inverted papilloma",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478707,
"choiceText": "Nasal polyposis related to granulomatosis with polyangiitis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478708,
"choiceText": "Sinonasal undifferentiated carcinoma",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478709,
"choiceText": "Nasal polyposis related to aspirin-exacerbated respiratory disease",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 473058,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1478710,
"choiceText": "Type 1 inflammation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478711,
"choiceText": "Type 2 inflammation",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478712,
"choiceText": "Type 3 inflammation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478713,
"choiceText": "Neutrophilic inflammation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "AERD causes type 2 immunologic inflammation, which is characterized by the release of interleukin (IL)-4, IL-5, and IL-13 cytokines and eosinophilia. Other causes of type 2 inflammation include helminth infections, allergy, and asthma.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 473059,
"questionText": "Which of the following types of immunologic inflammation is most prominently associated with AERD?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1478714,
"choiceText": "Nasal polyposis has a high risk of malignant degeneration",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478715,
"choiceText": "Nasal polyposis is most commonly related to aspirin sensitivity",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478716,
"choiceText": "Nasal polyps related to AERD are usually identified in childhood",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1478717,
"choiceText": "Nasal obstruction and anosmia are associated with nasal polyposis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Nasal polyposis cause symptoms of rhinosinusitis, including anterior and posterior nasal drainage, nasal congestion/obstruction, facial pain/pressure, and olfactory dysfunction. Nasal obstruction and olfactory compromise are common symptoms in nasal polyposis.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 473060,
"questionText": "Which of the following is most accurate regarding nasal polyposis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
980564 | /viewarticle/980564 | [
{
"authors": "Benjamin Scott Harris, MD, MPH; Thomas Michael Price, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A healthy 38-year-old woman (gravida 0) presents for an infertility evaluation after 14 months of attempting to conceive without success. She reports new-onset amenorrhea 4 months before presentation, despite previously having regular menstrual cycles. She denies any physical symptoms but has noticed easy bruising and recently has had worsening emotional lability. During the past year, she has gained 30 lb (13.6 kg). She has no history of fertility treatment or evaluation.",
"The patient takes vitamin D, a multivitamin, folic acid, and vitamin B12 supplements. She has no past surgical history. Her Papanicolaou test is up to date, and she has no history of dysplasia. She has never smoked and consumes approximately three alcoholic beverages per month. Her family history is negative for breast, colon, and gynecologic cancer. Her brother has hypothyroidism, and her sister has thyroid disease. She has no history of birth defects, genetic diseases, venous thromboembolism, endometriosis, or fibroids.",
"Her partner is 35 years old and has a history of kidney stones. He takes no medications and smokes three or four cigarettes daily. He has no history of sexual dysfunction or family history of birth defects or genetic diseases. He has never had a semen analysis."
],
"date": "September 13, 2022",
"figures": [],
"markdown": "# Endo Case Challenge: Amenorrhea for Months, Mood Swings, Weight Gain in a 38-Year-Old Woman\n\n **Authors:** Benjamin Scott Harris, MD, MPH; Thomas Michael Price, MD \n **Date:** September 13, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA healthy 38-year-old woman (gravida 0) presents for an infertility evaluation after 14 months of attempting to conceive without success. She reports new-onset amenorrhea 4 months before presentation, despite previously having regular menstrual cycles. She denies any physical symptoms but has noticed easy bruising and recently has had worsening emotional lability. During the past year, she has gained 30 lb (13.6 kg). She has no history of fertility treatment or evaluation.\nThe patient takes vitamin D, a multivitamin, folic acid, and vitamin B12 supplements. She has no past surgical history. Her Papanicolaou test is up to date, and she has no history of dysplasia. She has never smoked and consumes approximately three alcoholic beverages per month. Her family history is negative for breast, colon, and gynecologic cancer. Her brother has hypothyroidism, and her sister has thyroid disease. She has no history of birth defects, genetic diseases, venous thromboembolism, endometriosis, or fibroids.\nHer partner is 35 years old and has a history of kidney stones. He takes no medications and smokes three or four cigarettes daily. He has no history of sexual dysfunction or family history of birth defects or genetic diseases. He has never had a semen analysis.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Endo Case Challenge: Amenorrhea for Months, Mood Swings, Weight Gain in a 38-Year-Old Woman"
},
{
"authors": "Benjamin Scott Harris, MD, MPH; Thomas Michael Price, MD",
"content": [
"Upon physical examination, the patient appears normally developed and well nourished. She is in no acute distress. Her heart rate is 92 beats/min, and her blood pressure is 142/98 mm Hg. She is afebrile. She has no evidence of lid lag, stare, or exophthalmos. Her thyroid is normal in size and texture. Her lungs are clear to auscultation. The heart examination reveals regular rate and rhythm, with normal S1 and S2. Her abdomen is soft and nontender and shows no striae. The pelvic examination is deferred.",
"Laboratory studies reveal these values:",
"Anti-müllerian hormone: 0.064 ng/mL (reference range, 1.0-3.0 ng/mL)",
"Day 3 follicle-stimulating hormone (FSH): 8.4 mIU/mL (reference range, 1.37-9.9 mIU/mL [follicular phase])",
"Day 3 estradiol: 48 pg/mL (reference range, 25-75 pg/mL)",
"Thyroid-stimulating hormone: 2.34 µIU/mL (reference range, 2-10 μU/mL)",
"Prolactin: 11.69 ng/mL (reference range, 3-27 ng/mL [adult female])",
"Total testosterone: < 7 ng/dL (reference range, 15-40 ng/dL [women])",
"Dehydroepiandrosterone sulfate (DHEA-S): 2 µg/dL (reference range, 45-270 µg/dL [women aged 30-39 years])",
"Owing to an abnormally low DHEA-S level, additional testing is performed, including:",
"Adrenocorticotropic hormone (ACTH): 3 pg/mL (reference range, 9-52 pg/mL)",
"Cortisol (PM): 12 µg/dL (reference range, 3-13 µg/dL)",
"Cortisol (AM): 12.1 µg/dL (reference range, 5-23 µg/dL)",
"24-hour free cortisol: 74 µg/24 h (reference range, 4-40 µg/24 h)",
"Aldosterone: 8.1 ng/dL (reference range, < 10 ng/dL)",
"Renin activity, plasma: 0.6 ng/mL/h (reference range, 0.6-4.3 ng/mL/h)",
"Metanephrines, plasma: < 10 pg/mL (reference range, 12-60 pg/mL)",
"Other laboratory values are:",
"White blood cell count: 8700 cells/µL, with 62% neutrophils (reference range, 4500-11,000 cells/µL, with 40%-70% neutrophils)",
"Hemoglobin: 13.8 g/dL (reference range, 12.1-15.1 g/dL)",
"Platelet count: 310,000 cells/µL (reference range, 150,000-450,000 cells/µL)",
"Sodium: 136 mmol/L (reference range, 134-145 mmol/L)",
"Potassium: 3.3 mmol/L (reference range, 3.5-5.1 mmol/L)",
"Chloride: 101 mmol/L (reference range, 96-106 mmol/L)",
"Blood urea nitrogen: 10 mg/dL (reference range, 7-20 mg/dL)",
"Creatinine: 0.7 mg/dL (reference range, 0.6-1.1 mg/dL)",
"Alkaline phosphatase: 42 U/L (reference range, 40-150 U/L)",
"Alanine aminotransferase: 15 U/L (reference range, 19-25 U/L)",
"Aspartate aminotransferase: 22 U/L (reference range, 9-32 U/L)",
"Total bilirubin: 0.7 mg/dL (reference range, 0.1-1.2 mg/dL)",
"CT of the abdomen and pelvis shows a large left adrenal mass measuring up to 4.9 × 2.9 cm, which is compatible with a lipid-rich adenoma."
],
"date": "September 13, 2022",
"figures": [],
"markdown": "# Endo Case Challenge: Amenorrhea for Months, Mood Swings, Weight Gain in a 38-Year-Old Woman\n\n **Authors:** Benjamin Scott Harris, MD, MPH; Thomas Michael Price, MD \n **Date:** September 13, 2022\n\n ## Content\n\n Upon physical examination, the patient appears normally developed and well nourished. She is in no acute distress. Her heart rate is 92 beats/min, and her blood pressure is 142/98 mm Hg. She is afebrile. She has no evidence of lid lag, stare, or exophthalmos. Her thyroid is normal in size and texture. Her lungs are clear to auscultation. The heart examination reveals regular rate and rhythm, with normal S1 and S2. Her abdomen is soft and nontender and shows no striae. The pelvic examination is deferred.\nLaboratory studies reveal these values:\nAnti-müllerian hormone: 0.064 ng/mL (reference range, 1.0-3.0 ng/mL)\nDay 3 follicle-stimulating hormone (FSH): 8.4 mIU/mL (reference range, 1.37-9.9 mIU/mL [follicular phase])\nDay 3 estradiol: 48 pg/mL (reference range, 25-75 pg/mL)\nThyroid-stimulating hormone: 2.34 µIU/mL (reference range, 2-10 μU/mL)\nProlactin: 11.69 ng/mL (reference range, 3-27 ng/mL [adult female])\nTotal testosterone: < 7 ng/dL (reference range, 15-40 ng/dL [women])\nDehydroepiandrosterone sulfate (DHEA-S): 2 µg/dL (reference range, 45-270 µg/dL [women aged 30-39 years])\nOwing to an abnormally low DHEA-S level, additional testing is performed, including:\nAdrenocorticotropic hormone (ACTH): 3 pg/mL (reference range, 9-52 pg/mL)\nCortisol (PM): 12 µg/dL (reference range, 3-13 µg/dL)\nCortisol (AM): 12.1 µg/dL (reference range, 5-23 µg/dL)\n24-hour free cortisol: 74 µg/24 h (reference range, 4-40 µg/24 h)\nAldosterone: 8.1 ng/dL (reference range, < 10 ng/dL)\nRenin activity, plasma: 0.6 ng/mL/h (reference range, 0.6-4.3 ng/mL/h)\nMetanephrines, plasma: < 10 pg/mL (reference range, 12-60 pg/mL)\nOther laboratory values are:\nWhite blood cell count: 8700 cells/µL, with 62% neutrophils (reference range, 4500-11,000 cells/µL, with 40%-70% neutrophils)\nHemoglobin: 13.8 g/dL (reference range, 12.1-15.1 g/dL)\nPlatelet count: 310,000 cells/µL (reference range, 150,000-450,000 cells/µL)\nSodium: 136 mmol/L (reference range, 134-145 mmol/L)\nPotassium: 3.3 mmol/L (reference range, 3.5-5.1 mmol/L)\nChloride: 101 mmol/L (reference range, 96-106 mmol/L)\nBlood urea nitrogen: 10 mg/dL (reference range, 7-20 mg/dL)\nCreatinine: 0.7 mg/dL (reference range, 0.6-1.1 mg/dL)\nAlkaline phosphatase: 42 U/L (reference range, 40-150 U/L)\nAlanine aminotransferase: 15 U/L (reference range, 19-25 U/L)\nAspartate aminotransferase: 22 U/L (reference range, 9-32 U/L)\nTotal bilirubin: 0.7 mg/dL (reference range, 0.1-1.2 mg/dL)\nCT of the abdomen and pelvis shows a large left adrenal mass measuring up to 4.9 × 2.9 cm, which is compatible with a lipid-rich adenoma.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1717130,
"choiceText": "Congenital adrenal hyperplasia",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717131,
"choiceText": "Ovarian insufficiency",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717132,
"choiceText": "Cushing syndrome",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717133,
"choiceText": "Adrenal insufficiency",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 553979,
"questionText": "On the basis of these findings only, which of these is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Endo Case Challenge: Amenorrhea for Months, Mood Swings, Weight Gain in a 38-Year-Old Woman"
},
{
"authors": "Benjamin Scott Harris, MD, MPH; Thomas Michael Price, MD",
"content": [
"Measurement of DHEA-S and testosterone is common in women with infertility, and evidence of ovulatory dysfunction is based on menstrual cycle irregularity. Testing is performed mainly to detect elevated androgen levels, which would suggest a diagnosis of polycystic ovary syndrome (PCOS), the most common cause of ovulatory dysfunction. Unexpectedly, this patient had a very low DHEA-S level, which suggests adrenal androgen suppression. Further testing showed this suppression to be due to a low ACTH level from hypercortisolism secondary to an adrenal tumor.",
"PCOS can be diagnosed using the Rotterdam criteria (two of three are required):",
"Oligoovulation/anovulation",
"Hyperandrogenism (clinical or laboratory evidence)",
"Polycystic ovaries",
"Although this patient had anovulation, she did not have evidence of hyperandrogenism. In fact, she had low adrenal androgen levels. Ultrasonography was not performed for evaluation of polycystic ovary morphology.",
"Ovarian insufficiency was unlikely in this patient. Although she had secondary amenorrhea, she did not yet meet the clinical criteria for menopause (absence of menses for 12 months). Moreover, she did not demonstrate additional symptoms of estrogen deficiency, such as hot flushes, night sweats, and atrophic symptoms, which further lowered this suspicion. Lastly, her FSH levels were < 10 mIU/mL in the presence of a normal estradiol level, which demonstrated normal ovarian function."
],
"date": "September 13, 2022",
"figures": [],
"markdown": "# Endo Case Challenge: Amenorrhea for Months, Mood Swings, Weight Gain in a 38-Year-Old Woman\n\n **Authors:** Benjamin Scott Harris, MD, MPH; Thomas Michael Price, MD \n **Date:** September 13, 2022\n\n ## Content\n\n Measurement of DHEA-S and testosterone is common in women with infertility, and evidence of ovulatory dysfunction is based on menstrual cycle irregularity. Testing is performed mainly to detect elevated androgen levels, which would suggest a diagnosis of polycystic ovary syndrome (PCOS), the most common cause of ovulatory dysfunction. Unexpectedly, this patient had a very low DHEA-S level, which suggests adrenal androgen suppression. Further testing showed this suppression to be due to a low ACTH level from hypercortisolism secondary to an adrenal tumor.\nPCOS can be diagnosed using the Rotterdam criteria (two of three are required):\nOligoovulation/anovulation\nHyperandrogenism (clinical or laboratory evidence)\nPolycystic ovaries\nAlthough this patient had anovulation, she did not have evidence of hyperandrogenism. In fact, she had low adrenal androgen levels. Ultrasonography was not performed for evaluation of polycystic ovary morphology.\nOvarian insufficiency was unlikely in this patient. Although she had secondary amenorrhea, she did not yet meet the clinical criteria for menopause (absence of menses for 12 months). Moreover, she did not demonstrate additional symptoms of estrogen deficiency, such as hot flushes, night sweats, and atrophic symptoms, which further lowered this suspicion. Lastly, her FSH levels were < 10 mIU/mL in the presence of a normal estradiol level, which demonstrated normal ovarian function.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1717130,
"choiceText": "Congenital adrenal hyperplasia",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717131,
"choiceText": "Ovarian insufficiency",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717132,
"choiceText": "Cushing syndrome",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717133,
"choiceText": "Adrenal insufficiency",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 553979,
"questionText": "On the basis of these findings only, which of these is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Endo Case Challenge: Amenorrhea for Months, Mood Swings, Weight Gain in a 38-Year-Old Woman"
},
{
"authors": "Benjamin Scott Harris, MD, MPH; Thomas Michael Price, MD",
"content": [
"Adrenal insufficiency was also unlikely in this patient. A morning cortisol level < 3 µg/dL is highly suggestive of adrenal insufficiency. Her morning cortisol levels were normal.",
"Cushing syndrome is rare, with an incidence of 6-8 per million per year.[1] Approximately 60%-70% of cases are due to an ACTH-producing pituitary adenoma (Cushing disease), 10%-15% to ectopic ACTH production, and 20% to adrenal tumors.[2] Symptomatology is nonspecific. The most common symptoms are decreased libido, obesity/weight gain, plethora, round facies, cycle irregularity, increased body hair, high blood pressure, ecchymoses, fatigue, depression, and glucose intolerance.",
"Adrenal adenomas are benign tumors of the adrenal cortex that are often found incidentally on imaging, particularly if they are hormonally inactive and are not causing symptoms. About 15% of adrenal adenomas are hormonally active and present with hypercortisolism (1%-29%), hyperaldosteronism (1.5%-3.3%), and/or adrenergic symptoms due to pheochromocytoma (1.5%-11%).[3,4]",
"Hypercortisolism that causes Cushing syndrome can be difficult to diagnose, given that it can present with a wide range of symptoms, including hypertension; hyperglycemia; obesity; muscle weakness and fatigue; depression; osteopenia; and dermatologic changes, such as striae and acne. Figure 1 shows an example of striae in Cushing syndrome.",
"Figure 1.",
"The prevalence of striae in patients with Cushing syndrome is less than 50%; however, when present, striae are specific for the syndrome.[5] Menstrual cycle changes, including oligomenorrhea and amenorrhea, are present in nearly 80% of women with Cushing syndrome, owing to low concentrations of luteinizing hormone and FSH resulting from gonadotropin-releasing hormone suppression by excess cortisol.[6,7]",
"CT is recommended if an adrenal tumor is suspected. Features that are more consistent with a benign adenoma than with cancer include[8]:",
"Round tumors that are < 4 cm and have sharp margins and homogenous density",
"Low attenuation (< 10 Hounsfield units) on unenhanced CT",
"If an adenoma is found, the Endocrine Society guidelines recommend testing patients for Cushing syndrome.[9] The diagnosis is confirmed when two different screening tests are abnormal. Discordant testing requires further evaluation. Recommended screening tests include measurement of 24-hour urinary free cortisol, late-night salivary cortisol (sample collected 11 PM to midnight), late-night serum cortisol (> 7.5 µg/dL is an abnormal result), and/or a low-dose dexamethasone suppression test (AM cortisol level >1.8 µg/dL is an abnormal result). When Cushing syndrome is suspected in patients with hyperandrogenism, the low-dose dexamethasone suppression test is an appropriate first step. It is performed by administering 1.0 mg of dexamethasone by mouth between 11 PM and midnight, followed by measurement of the serum cortisol at 8:00 AM the following morning.[10,11] Loss of diurnal variation in blood cortisol, as seen in this patient, is also commonly found in Cushing syndrome.[12]"
],
"date": "September 13, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/980/564/980564-Figure1-thumb.png"
}
],
"markdown": "# Endo Case Challenge: Amenorrhea for Months, Mood Swings, Weight Gain in a 38-Year-Old Woman\n\n **Authors:** Benjamin Scott Harris, MD, MPH; Thomas Michael Price, MD \n **Date:** September 13, 2022\n\n ## Content\n\n Adrenal insufficiency was also unlikely in this patient. A morning cortisol level < 3 µg/dL is highly suggestive of adrenal insufficiency. Her morning cortisol levels were normal.\nCushing syndrome is rare, with an incidence of 6-8 per million per year.[1] Approximately 60%-70% of cases are due to an ACTH-producing pituitary adenoma (Cushing disease), 10%-15% to ectopic ACTH production, and 20% to adrenal tumors.[2] Symptomatology is nonspecific. The most common symptoms are decreased libido, obesity/weight gain, plethora, round facies, cycle irregularity, increased body hair, high blood pressure, ecchymoses, fatigue, depression, and glucose intolerance.\nAdrenal adenomas are benign tumors of the adrenal cortex that are often found incidentally on imaging, particularly if they are hormonally inactive and are not causing symptoms. About 15% of adrenal adenomas are hormonally active and present with hypercortisolism (1%-29%), hyperaldosteronism (1.5%-3.3%), and/or adrenergic symptoms due to pheochromocytoma (1.5%-11%).[3,4]\nHypercortisolism that causes Cushing syndrome can be difficult to diagnose, given that it can present with a wide range of symptoms, including hypertension; hyperglycemia; obesity; muscle weakness and fatigue; depression; osteopenia; and dermatologic changes, such as striae and acne. Figure 1 shows an example of striae in Cushing syndrome.\nFigure 1.\nThe prevalence of striae in patients with Cushing syndrome is less than 50%; however, when present, striae are specific for the syndrome.[5] Menstrual cycle changes, including oligomenorrhea and amenorrhea, are present in nearly 80% of women with Cushing syndrome, owing to low concentrations of luteinizing hormone and FSH resulting from gonadotropin-releasing hormone suppression by excess cortisol.[6,7]\nCT is recommended if an adrenal tumor is suspected. Features that are more consistent with a benign adenoma than with cancer include[8]:\nRound tumors that are < 4 cm and have sharp margins and homogenous density\nLow attenuation (< 10 Hounsfield units) on unenhanced CT\nIf an adenoma is found, the Endocrine Society guidelines recommend testing patients for Cushing syndrome.[9] The diagnosis is confirmed when two different screening tests are abnormal. Discordant testing requires further evaluation. Recommended screening tests include measurement of 24-hour urinary free cortisol, late-night salivary cortisol (sample collected 11 PM to midnight), late-night serum cortisol (> 7.5 µg/dL is an abnormal result), and/or a low-dose dexamethasone suppression test (AM cortisol level >1.8 µg/dL is an abnormal result). When Cushing syndrome is suspected in patients with hyperandrogenism, the low-dose dexamethasone suppression test is an appropriate first step. It is performed by administering 1.0 mg of dexamethasone by mouth between 11 PM and midnight, followed by measurement of the serum cortisol at 8:00 AM the following morning.[10,11] Loss of diurnal variation in blood cortisol, as seen in this patient, is also commonly found in Cushing syndrome.[12]\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Endo Case Challenge: Amenorrhea for Months, Mood Swings, Weight Gain in a 38-Year-Old Woman"
},
{
"authors": "Benjamin Scott Harris, MD, MPH; Thomas Michael Price, MD",
"content": [
"Benign tumors that are hormonally active should be treated with adrenalectomy. Medical management may be indicated if surgery is contraindicated, but care should be taken to avoid overtreatment, which can lead to adrenal insufficiency.",
"This patient had an interesting case of Cushing syndrome, with an initial presentation for infertility evaluation, which made the diagnosis challenging. Her clinical presentation highlights the importance of a comprehensive history, physical examination, and endocrine laboratory evaluation for patients with irregular menstrual cycles. Extended evaluation was performed after identification of an abnormally low DHEA-S level. If the DHEA-S test had not been performed, an opportunity for treatment and cure would have been missed. She underwent a unilateral adrenalectomy and subsequently proceeded with fertility treatment."
],
"date": "September 13, 2022",
"figures": [],
"markdown": "# Endo Case Challenge: Amenorrhea for Months, Mood Swings, Weight Gain in a 38-Year-Old Woman\n\n **Authors:** Benjamin Scott Harris, MD, MPH; Thomas Michael Price, MD \n **Date:** September 13, 2022\n\n ## Content\n\n Benign tumors that are hormonally active should be treated with adrenalectomy. Medical management may be indicated if surgery is contraindicated, but care should be taken to avoid overtreatment, which can lead to adrenal insufficiency.\nThis patient had an interesting case of Cushing syndrome, with an initial presentation for infertility evaluation, which made the diagnosis challenging. Her clinical presentation highlights the importance of a comprehensive history, physical examination, and endocrine laboratory evaluation for patients with irregular menstrual cycles. Extended evaluation was performed after identification of an abnormally low DHEA-S level. If the DHEA-S test had not been performed, an opportunity for treatment and cure would have been missed. She underwent a unilateral adrenalectomy and subsequently proceeded with fertility treatment.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1717139,
"choiceText": "Significant blood cortisol elevation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717140,
"choiceText": "Lack of diurnal variation in blood cortisol levels",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717141,
"choiceText": "Low blood ACTH level",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717142,
"choiceText": "Low blood testosterone level",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "ACTH and cortisol levels normally have a 24-hour circadian pattern, with the maximum level in the morning correlating with the sleep-awake transition and the lowest level around midnight. The main external factors that regulate this variation include transitioning from sleeping to awake and food intake. This diurnal variation is interrupted by an abnormal persistent elevation in ACTH, seen with pituitary and ectopic sources, and an abnormal persistent elevation in cortisol from adrenal tumors.<sup>[13]</sup> The normal AM-to-PM cortisol ratio is ≥ 2.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 553984,
"questionText": "Which finding in the patient's initial blood testing most strongly suggested the possibility of Cushing syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1717148,
"choiceText": "Hirsutism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717149,
"choiceText": "Buffalo hump",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717150,
"choiceText": "Decreased libido",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717151,
"choiceText": "Weight gain",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The patient in this case had a significant weight gain of 30 lb (13.6 kg) within 1 year. Most presenting symptoms of Cushing syndrome are highly nonspecific and are also associated with more common disorders than Cushing syndrome. This leads to a significant delay in diagnosis, approximated at 34-50 months in one study.<sup>[14]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 553986,
"questionText": "Which is a common symptom of Cushing syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Endo Case Challenge: Amenorrhea for Months, Mood Swings, Weight Gain in a 38-Year-Old Woman"
},
{
"authors": "Benjamin Scott Harris, MD, MPH; Thomas Michael Price, MD",
"content": [
"Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult."
],
"date": "September 13, 2022",
"figures": [],
"markdown": "# Endo Case Challenge: Amenorrhea for Months, Mood Swings, Weight Gain in a 38-Year-Old Woman\n\n **Authors:** Benjamin Scott Harris, MD, MPH; Thomas Michael Price, MD \n **Date:** September 13, 2022\n\n ## Content\n\n Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult.\n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1717139,
"choiceText": "Significant blood cortisol elevation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717140,
"choiceText": "Lack of diurnal variation in blood cortisol levels",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717141,
"choiceText": "Low blood ACTH level",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717142,
"choiceText": "Low blood testosterone level",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "ACTH and cortisol levels normally have a 24-hour circadian pattern, with the maximum level in the morning correlating with the sleep-awake transition and the lowest level around midnight. The main external factors that regulate this variation include transitioning from sleeping to awake and food intake. This diurnal variation is interrupted by an abnormal persistent elevation in ACTH, seen with pituitary and ectopic sources, and an abnormal persistent elevation in cortisol from adrenal tumors.<sup>[13]</sup> The normal AM-to-PM cortisol ratio is ≥ 2.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 553984,
"questionText": "Which finding in the patient's initial blood testing most strongly suggested the possibility of Cushing syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1717148,
"choiceText": "Hirsutism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717149,
"choiceText": "Buffalo hump",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717150,
"choiceText": "Decreased libido",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717151,
"choiceText": "Weight gain",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The patient in this case had a significant weight gain of 30 lb (13.6 kg) within 1 year. Most presenting symptoms of Cushing syndrome are highly nonspecific and are also associated with more common disorders than Cushing syndrome. This leads to a significant delay in diagnosis, approximated at 34-50 months in one study.<sup>[14]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 553986,
"questionText": "Which is a common symptom of Cushing syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Endo Case Challenge: Amenorrhea for Months, Mood Swings, Weight Gain in a 38-Year-Old Woman"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1717130,
"choiceText": "Congenital adrenal hyperplasia",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717131,
"choiceText": "Ovarian insufficiency",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717132,
"choiceText": "Cushing syndrome",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717133,
"choiceText": "Adrenal insufficiency",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 553979,
"questionText": "On the basis of these findings only, which of these is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1717139,
"choiceText": "Significant blood cortisol elevation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717140,
"choiceText": "Lack of diurnal variation in blood cortisol levels",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717141,
"choiceText": "Low blood ACTH level",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717142,
"choiceText": "Low blood testosterone level",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "ACTH and cortisol levels normally have a 24-hour circadian pattern, with the maximum level in the morning correlating with the sleep-awake transition and the lowest level around midnight. The main external factors that regulate this variation include transitioning from sleeping to awake and food intake. This diurnal variation is interrupted by an abnormal persistent elevation in ACTH, seen with pituitary and ectopic sources, and an abnormal persistent elevation in cortisol from adrenal tumors.<sup>[13]</sup> The normal AM-to-PM cortisol ratio is ≥ 2.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 553984,
"questionText": "Which finding in the patient's initial blood testing most strongly suggested the possibility of Cushing syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1717148,
"choiceText": "Hirsutism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717149,
"choiceText": "Buffalo hump",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717150,
"choiceText": "Decreased libido",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1717151,
"choiceText": "Weight gain",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The patient in this case had a significant weight gain of 30 lb (13.6 kg) within 1 year. Most presenting symptoms of Cushing syndrome are highly nonspecific and are also associated with more common disorders than Cushing syndrome. This leads to a significant delay in diagnosis, approximated at 34-50 months in one study.<sup>[14]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 553986,
"questionText": "Which is a common symptom of Cushing syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
867089 | /viewarticle/867089 | [
{
"authors": "Juan Carlos Munoz, MD; Carmela Monteiro, MD; Ivan E. Rascon-Aguilar, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.",
"A 33-year-old man presents to the emergency department 2 hours after eating lunch describing food stuck in his esophagus. He is unable to swallow his own saliva, which he has been spitting up since the onset of his symptoms. He states that he has had problems with swallowing solid food since childhood, but no significant episodes have required him to seek medical evaluation.",
"For the past few months, the patient has been experiencing worsening dysphagia. The symptoms seem to be intermittent, and they are rectified by chewing carefully and drinking water after swallowing solids. He does report a remote history of esophageal reflux unresponsive to esomeprazole.",
"His past medical history is otherwise remarkable only for sinusitis and allergies, for which he is currently taking antihistamines. The patient does not have any chest pain, shortness of breath, a history of oral thrush, odynophagia, smoking, heavy alcohol use, or any illicit drug use. He does not have any weakness, numbness, diplopia, or other visual changes."
],
"date": "September 06, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: A 33-Year-Old Man Who Can’t Swallow His Own Saliva\n\n **Authors:** Juan Carlos Munoz, MD; Carmela Monteiro, MD; Ivan E. Rascon-Aguilar, MD \n **Date:** September 06, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.\nA 33-year-old man presents to the emergency department 2 hours after eating lunch describing food stuck in his esophagus. He is unable to swallow his own saliva, which he has been spitting up since the onset of his symptoms. He states that he has had problems with swallowing solid food since childhood, but no significant episodes have required him to seek medical evaluation.\nFor the past few months, the patient has been experiencing worsening dysphagia. The symptoms seem to be intermittent, and they are rectified by chewing carefully and drinking water after swallowing solids. He does report a remote history of esophageal reflux unresponsive to esomeprazole.\nHis past medical history is otherwise remarkable only for sinusitis and allergies, for which he is currently taking antihistamines. The patient does not have any chest pain, shortness of breath, a history of oral thrush, odynophagia, smoking, heavy alcohol use, or any illicit drug use. He does not have any weakness, numbness, diplopia, or other visual changes.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Gastro Case Challenge: A 33-Year-Old Man Who Can’t Swallow His Own Saliva"
},
{
"authors": "Juan Carlos Munoz, MD; Carmela Monteiro, MD; Ivan E. Rascon-Aguilar, MD",
"content": [
"Upon physical examination, his oral temperature is 98.6° F (37° C). His pulse is regular at a rate of 105 beats/min. His blood pressure is 120/70 mm Hg. His respiratory rate is 10 breaths/min. The patient is in no acute distress. Although he is noted to be spitting up saliva, he is not drooling, and no stridor, cyanosis, or pallor is detected.",
"The examination of his head and neck is normal, with no palpable masses or cervical lymphadenopathy. His lungs are clear to auscultation, and the patient has a normal respiratory effort. His heart evaluation demonstrates normal S1 and S2 heart sounds, without any murmurs. His abdomen is soft, nontender, and has normal bowel sounds. No skin is rash noted.",
"The laboratory findings, including a complete blood cell (CBC) count and a basic metabolic panel, are normal. Plain chest radiographs are unremarkable, with no radiolucent objects or extravasations of air seen. The patient is diagnosed with an esophageal foreign-body obstruction and treated in the emergency department with intravenous fluids and glucagon (Figures 1 and 2). Two hours after this initial treatment, his symptoms persist; a gastroenterologist is brought in for consultation for endoscopy and food bolus extraction.",
"Figure 1.",
"Figure 2."
],
"date": "September 06, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/867/089/867089-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/867/089/867089-Thumb2.png"
}
],
"markdown": "# Gastro Case Challenge: A 33-Year-Old Man Who Can’t Swallow His Own Saliva\n\n **Authors:** Juan Carlos Munoz, MD; Carmela Monteiro, MD; Ivan E. Rascon-Aguilar, MD \n **Date:** September 06, 2022\n\n ## Content\n\n Upon physical examination, his oral temperature is 98.6° F (37° C). His pulse is regular at a rate of 105 beats/min. His blood pressure is 120/70 mm Hg. His respiratory rate is 10 breaths/min. The patient is in no acute distress. Although he is noted to be spitting up saliva, he is not drooling, and no stridor, cyanosis, or pallor is detected.\nThe examination of his head and neck is normal, with no palpable masses or cervical lymphadenopathy. His lungs are clear to auscultation, and the patient has a normal respiratory effort. His heart evaluation demonstrates normal S1 and S2 heart sounds, without any murmurs. His abdomen is soft, nontender, and has normal bowel sounds. No skin is rash noted.\nThe laboratory findings, including a complete blood cell (CBC) count and a basic metabolic panel, are normal. Plain chest radiographs are unremarkable, with no radiolucent objects or extravasations of air seen. The patient is diagnosed with an esophageal foreign-body obstruction and treated in the emergency department with intravenous fluids and glucagon (Figures 1 and 2). Two hours after this initial treatment, his symptoms persist; a gastroenterologist is brought in for consultation for endoscopy and food bolus extraction.\nFigure 1.\nFigure 2.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 996039,
"choiceText": "Incidental esophageal food impaction",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996041,
"choiceText": "Eosinophilic esophagitis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996043,
"choiceText": "Gastroesophageal reflux disease",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996045,
"choiceText": "Chemical esophagitis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 315367,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: A 33-Year-Old Man Who Can’t Swallow His Own Saliva"
},
{
"authors": "Juan Carlos Munoz, MD; Carmela Monteiro, MD; Ivan E. Rascon-Aguilar, MD",
"content": [
"Eosinophilic esophagitis is an inflammatory condition of the esophagus characterized by eosinophilic infiltration. It was first reported in 1978,[1] and its incidence appears to be increasing. It is a condition that mainly affects children; the adult form has only recently gained recognition as a distinct entity. It is characterized clinically by dysphagia. Often, the patient's history of dysphagia dates to childhood or adolescence.",
"In a study by Desai and colleagues,[2] the authors reported that eosinophilic esophagitis may have an identical appearance to a Schatzki ring, as seen in this case. In some patients, eosinophilic esophagitis may occur in association with eosinophilic gastroenteritis.[2]",
"The cause of eosinophilic esophagitis is poorly understood. Most studies have mentioned a high prevalence of allergies in family members. It is not clear whether eosinophilic esophagitis has a purely genetic base or whether this condition occurs in genetically predisposed individuals with an environmental trigger. In many cases, the disease manifestations are intermittent in nature.",
"Most adult patients with eosinophilic esophagitis are men (the male-to-female ratio is 3:1). Most commonly, patients present in the third or fourth decade of life. The presenting symptoms include dysphagia (93%), food impaction (62%), and heartburn (24%). More unusual manifestations of eosinophilic esophagitis include odynophagia, atypical chest pain, and vomiting.",
"Most adult patients with eosinophilic esophagitis do not respond to antisecretory therapy and may have objective evidence of reflux on a 24-hour pH study. About 50% of patients give a history of allergies (food, atopic dermatitis, allergic rhinitis) and 31% have peripheral blood eosinophilia. Serum immunoglobulin E (IgE) levels are increased in about 55% of patients."
],
"date": "September 06, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: A 33-Year-Old Man Who Can’t Swallow His Own Saliva\n\n **Authors:** Juan Carlos Munoz, MD; Carmela Monteiro, MD; Ivan E. Rascon-Aguilar, MD \n **Date:** September 06, 2022\n\n ## Content\n\n Eosinophilic esophagitis is an inflammatory condition of the esophagus characterized by eosinophilic infiltration. It was first reported in 1978,[1] and its incidence appears to be increasing. It is a condition that mainly affects children; the adult form has only recently gained recognition as a distinct entity. It is characterized clinically by dysphagia. Often, the patient's history of dysphagia dates to childhood or adolescence.\nIn a study by Desai and colleagues,[2] the authors reported that eosinophilic esophagitis may have an identical appearance to a Schatzki ring, as seen in this case. In some patients, eosinophilic esophagitis may occur in association with eosinophilic gastroenteritis.[2]\nThe cause of eosinophilic esophagitis is poorly understood. Most studies have mentioned a high prevalence of allergies in family members. It is not clear whether eosinophilic esophagitis has a purely genetic base or whether this condition occurs in genetically predisposed individuals with an environmental trigger. In many cases, the disease manifestations are intermittent in nature.\nMost adult patients with eosinophilic esophagitis are men (the male-to-female ratio is 3:1). Most commonly, patients present in the third or fourth decade of life. The presenting symptoms include dysphagia (93%), food impaction (62%), and heartburn (24%). More unusual manifestations of eosinophilic esophagitis include odynophagia, atypical chest pain, and vomiting.\nMost adult patients with eosinophilic esophagitis do not respond to antisecretory therapy and may have objective evidence of reflux on a 24-hour pH study. About 50% of patients give a history of allergies (food, atopic dermatitis, allergic rhinitis) and 31% have peripheral blood eosinophilia. Serum immunoglobulin E (IgE) levels are increased in about 55% of patients.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 996039,
"choiceText": "Incidental esophageal food impaction",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996041,
"choiceText": "Eosinophilic esophagitis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996043,
"choiceText": "Gastroesophageal reflux disease",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996045,
"choiceText": "Chemical esophagitis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 315367,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: A 33-Year-Old Man Who Can’t Swallow His Own Saliva"
},
{
"authors": "Juan Carlos Munoz, MD; Carmela Monteiro, MD; Ivan E. Rascon-Aguilar, MD",
"content": [
"Barium esophagography may be performed as the initial diagnostic test for eosinophilic esophagitis, but upper endoscopy is the preferred diagnostic test. Endoscopic findings include strictures, rings, and a narrowed lumen of the esophagus. Subtle but prevalent findings of eosinophilic esophagitis that are seen with endoscopy (mucosal furrowing, white spikes, the easy tearing of the mucosa) may not be seen on barium studies. Esophageal manometry studies are typically normal in patients with eosinophilic esophagitis. About 40% of cases may have uncoordinated contractions of the esophagus, which suggests involvement of the muscular layers. Monitoring with an esophageal 24-hour pH study is normal in 90% of affected patients. About 10% of patients are found to have gastroesophageal reflux disease (GERD).",
"An endoscopy (with biopsies taken from the upper and lower esophagus) is the test of choice for definitive diagnosis. Most patients have abnormal endoscopic findings. The most common structural alterations seen in adult patients with eosinophilic esophagitis may occur in combination or as the primary characteristics (eg, mucosal fragility, uniform small-caliber esophagus, single or multiple corrugations or rings, proximal or distal esophageal stenosis, or 1-2 mm whitish vesicles scattered over the mucosal surface, and, in rare cases, a Schatzki ring [Figure 2]).",
"Figure 2.",
"Histology is critical to the diagnosis of eosinophilic esophagitis. Extreme care must be taken when interpreting the biopsies; the histopathologic diagnostic criteria for eosinophilic esophagitis widely varies. Most studies suggest that > 20 eosinophils per high-power field (HPF) in a single field or > 15 eosinophils per HPF in two fields are findings that are diagnostic of eosinophilic esophagitis. Esophageal reflux may produce an eosinophilic infiltration (< 10 eosinophils per HPF) that is usually limited to the distal esophagus.",
"Treatment for eosinophilic esophagitis focuses on different aspects of the disease, including:",
"Identification and elimination of the underlying allergens that may be causing the disease (especially in pediatric and adolescent patients)",
"The use of steroids and proton pump inhibitors (PPIs)",
"Endoscopic treatment for stricture complications"
],
"date": "September 06, 2022",
"figures": [
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/867/089/867089-Thumb2.png"
}
],
"markdown": "# Gastro Case Challenge: A 33-Year-Old Man Who Can’t Swallow His Own Saliva\n\n **Authors:** Juan Carlos Munoz, MD; Carmela Monteiro, MD; Ivan E. Rascon-Aguilar, MD \n **Date:** September 06, 2022\n\n ## Content\n\n Barium esophagography may be performed as the initial diagnostic test for eosinophilic esophagitis, but upper endoscopy is the preferred diagnostic test. Endoscopic findings include strictures, rings, and a narrowed lumen of the esophagus. Subtle but prevalent findings of eosinophilic esophagitis that are seen with endoscopy (mucosal furrowing, white spikes, the easy tearing of the mucosa) may not be seen on barium studies. Esophageal manometry studies are typically normal in patients with eosinophilic esophagitis. About 40% of cases may have uncoordinated contractions of the esophagus, which suggests involvement of the muscular layers. Monitoring with an esophageal 24-hour pH study is normal in 90% of affected patients. About 10% of patients are found to have gastroesophageal reflux disease (GERD).\nAn endoscopy (with biopsies taken from the upper and lower esophagus) is the test of choice for definitive diagnosis. Most patients have abnormal endoscopic findings. The most common structural alterations seen in adult patients with eosinophilic esophagitis may occur in combination or as the primary characteristics (eg, mucosal fragility, uniform small-caliber esophagus, single or multiple corrugations or rings, proximal or distal esophageal stenosis, or 1-2 mm whitish vesicles scattered over the mucosal surface, and, in rare cases, a Schatzki ring [Figure 2]).\nFigure 2.\nHistology is critical to the diagnosis of eosinophilic esophagitis. Extreme care must be taken when interpreting the biopsies; the histopathologic diagnostic criteria for eosinophilic esophagitis widely varies. Most studies suggest that > 20 eosinophils per high-power field (HPF) in a single field or > 15 eosinophils per HPF in two fields are findings that are diagnostic of eosinophilic esophagitis. Esophageal reflux may produce an eosinophilic infiltration (< 10 eosinophils per HPF) that is usually limited to the distal esophagus.\nTreatment for eosinophilic esophagitis focuses on different aspects of the disease, including:\nIdentification and elimination of the underlying allergens that may be causing the disease (especially in pediatric and adolescent patients)\nThe use of steroids and proton pump inhibitors (PPIs)\nEndoscopic treatment for stricture complications\n\n ## Figures\n\n **Figure 2.** \n \n\n\n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Gastro Case Challenge: A 33-Year-Old Man Who Can’t Swallow His Own Saliva"
},
{
"authors": "Juan Carlos Munoz, MD; Carmela Monteiro, MD; Ivan E. Rascon-Aguilar, MD",
"content": [
"After specific food allergies are identified, pediatric or adolescent patients can be started on a targeted elimination diet, an elemental diet, or a six-food elimination diet for 6 weeks. Data in adults also suggest that a six-food elimination diet can improve symptoms, improve esophageal eosinophilia, and help to identify causative foods.",
"Steroids and PPIs are considered to be first-line treatment for eosinophilic esophagitis, alongside diet therapy and esophageal dilation.[3]",
"In this patient, a large piece of pork was seen in the lower esophagus on endoscopy (Figure 1), which was removed during endoscopy with a commercially available retrieval net device. A lesion with the appearance of a Schatzki ring was identified during the endoscopic evaluation (Figure 2).",
"Figure 1.",
"Figure 2.",
"In addition to a mucosal tear, subtle concentric esophageal rings were seen. Biopsies were taken from the lower and upper esophagus. The biopsy of the lower esophagus revealed a squamous mucosa with reactive changes and marked eosinophilia (> 20 per HPF). A biopsy of the upper esophagus also revealed a squamous mucosa with reactive changes and marked eosinophilia. The prominent eosinophilic infiltrate seen in both biopsies is highly suggestive of eosinophilic esophagitis. The patient was subsequently referred to an allergist for skin prick and/or patch testing for food and other environmental allergens. He was then started on a course of oral fluticasone (as described above). The patient was doing well 6 weeks after the diagnosis, with minimal dysphagia."
],
"date": "September 06, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/867/089/867089-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/867/089/867089-Thumb2.png"
}
],
"markdown": "# Gastro Case Challenge: A 33-Year-Old Man Who Can’t Swallow His Own Saliva\n\n **Authors:** Juan Carlos Munoz, MD; Carmela Monteiro, MD; Ivan E. Rascon-Aguilar, MD \n **Date:** September 06, 2022\n\n ## Content\n\n After specific food allergies are identified, pediatric or adolescent patients can be started on a targeted elimination diet, an elemental diet, or a six-food elimination diet for 6 weeks. Data in adults also suggest that a six-food elimination diet can improve symptoms, improve esophageal eosinophilia, and help to identify causative foods.\nSteroids and PPIs are considered to be first-line treatment for eosinophilic esophagitis, alongside diet therapy and esophageal dilation.[3]\nIn this patient, a large piece of pork was seen in the lower esophagus on endoscopy (Figure 1), which was removed during endoscopy with a commercially available retrieval net device. A lesion with the appearance of a Schatzki ring was identified during the endoscopic evaluation (Figure 2).\nFigure 1.\nFigure 2.\nIn addition to a mucosal tear, subtle concentric esophageal rings were seen. Biopsies were taken from the lower and upper esophagus. The biopsy of the lower esophagus revealed a squamous mucosa with reactive changes and marked eosinophilia (> 20 per HPF). A biopsy of the upper esophagus also revealed a squamous mucosa with reactive changes and marked eosinophilia. The prominent eosinophilic infiltrate seen in both biopsies is highly suggestive of eosinophilic esophagitis. The patient was subsequently referred to an allergist for skin prick and/or patch testing for food and other environmental allergens. He was then started on a course of oral fluticasone (as described above). The patient was doing well 6 weeks after the diagnosis, with minimal dysphagia.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 996047,
"choiceText": "Patients most commonly present with eosinophilic esophagitis in the second decade of life",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996049,
"choiceText": "Most patients affected with eosinophilic esophagitis are women",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996051,
"choiceText": "Results of monitoring with a 24-hour pH study are normal in a third of patients",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996053,
"choiceText": "A history of allergy is rare",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996521,
"choiceText": "Dysphagia is the most common presenting symptom ",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Eosinophilic esophagitis is clinically characterized by dysphagia. Most commonly, patients present in the third or fourth decade of life. About 50% of patients give a history of allergies (food, atopic dermatitis, allergic rhinitis) Most adult patients with eosinophilic esophagitis are men (the male-to-female ratio is 3:1). Monitoring with an esophageal 24-hour pH study is normal in 90% of affected patients.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 315369,
"questionText": "Which statement about eosinophilic esophagitis is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 996055,
"choiceText": "Strictures",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996057,
"choiceText": "Narrowed lumen of the esophagus",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996059,
"choiceText": "Mucosal furrowing\r\n",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996061,
"choiceText": "Esophageal rings",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996063,
"choiceText": "Multiple esophageal ulcerations",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The most common endoscopic finding in patients with eosinophilic esophagitis is a ringed esophagus.<sup type=\"ref\">[4]</sup> Other endoscopic findings include strictures and a narrowed lumen of the esophagus. Subtle but prevalent findings of eosinophilic esophagitis that are seen with endoscopy (mucosal furrowing, white spikes, the easy tearing of the mucosa) may not be seen on barium studies.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 315371,
"questionText": "Which of these is the most common endoscopic abnormality associated with eosinophilic esophagitis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: A 33-Year-Old Man Who Can’t Swallow His Own Saliva"
},
{
"authors": "Juan Carlos Munoz, MD; Carmela Monteiro, MD; Ivan E. Rascon-Aguilar, MD",
"content": [],
"date": "September 06, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: A 33-Year-Old Man Who Can’t Swallow His Own Saliva\n\n **Authors:** Juan Carlos Munoz, MD; Carmela Monteiro, MD; Ivan E. Rascon-Aguilar, MD \n **Date:** September 06, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 996047,
"choiceText": "Patients most commonly present with eosinophilic esophagitis in the second decade of life",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996049,
"choiceText": "Most patients affected with eosinophilic esophagitis are women",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996051,
"choiceText": "Results of monitoring with a 24-hour pH study are normal in a third of patients",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996053,
"choiceText": "A history of allergy is rare",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996521,
"choiceText": "Dysphagia is the most common presenting symptom ",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Eosinophilic esophagitis is clinically characterized by dysphagia. Most commonly, patients present in the third or fourth decade of life. About 50% of patients give a history of allergies (food, atopic dermatitis, allergic rhinitis) Most adult patients with eosinophilic esophagitis are men (the male-to-female ratio is 3:1). Monitoring with an esophageal 24-hour pH study is normal in 90% of affected patients.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 315369,
"questionText": "Which statement about eosinophilic esophagitis is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 996055,
"choiceText": "Strictures",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996057,
"choiceText": "Narrowed lumen of the esophagus",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996059,
"choiceText": "Mucosal furrowing\r\n",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996061,
"choiceText": "Esophageal rings",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996063,
"choiceText": "Multiple esophageal ulcerations",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The most common endoscopic finding in patients with eosinophilic esophagitis is a ringed esophagus.<sup type=\"ref\">[4]</sup> Other endoscopic findings include strictures and a narrowed lumen of the esophagus. Subtle but prevalent findings of eosinophilic esophagitis that are seen with endoscopy (mucosal furrowing, white spikes, the easy tearing of the mucosa) may not be seen on barium studies.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 315371,
"questionText": "Which of these is the most common endoscopic abnormality associated with eosinophilic esophagitis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: A 33-Year-Old Man Who Can’t Swallow His Own Saliva"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 996039,
"choiceText": "Incidental esophageal food impaction",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996041,
"choiceText": "Eosinophilic esophagitis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996043,
"choiceText": "Gastroesophageal reflux disease",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996045,
"choiceText": "Chemical esophagitis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 315367,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 996047,
"choiceText": "Patients most commonly present with eosinophilic esophagitis in the second decade of life",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996049,
"choiceText": "Most patients affected with eosinophilic esophagitis are women",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996051,
"choiceText": "Results of monitoring with a 24-hour pH study are normal in a third of patients",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996053,
"choiceText": "A history of allergy is rare",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996521,
"choiceText": "Dysphagia is the most common presenting symptom ",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Eosinophilic esophagitis is clinically characterized by dysphagia. Most commonly, patients present in the third or fourth decade of life. About 50% of patients give a history of allergies (food, atopic dermatitis, allergic rhinitis) Most adult patients with eosinophilic esophagitis are men (the male-to-female ratio is 3:1). Monitoring with an esophageal 24-hour pH study is normal in 90% of affected patients.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 315369,
"questionText": "Which statement about eosinophilic esophagitis is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 996055,
"choiceText": "Strictures",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996057,
"choiceText": "Narrowed lumen of the esophagus",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996059,
"choiceText": "Mucosal furrowing\r\n",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996061,
"choiceText": "Esophageal rings",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 996063,
"choiceText": "Multiple esophageal ulcerations",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The most common endoscopic finding in patients with eosinophilic esophagitis is a ringed esophagus.<sup type=\"ref\">[4]</sup> Other endoscopic findings include strictures and a narrowed lumen of the esophagus. Subtle but prevalent findings of eosinophilic esophagitis that are seen with endoscopy (mucosal furrowing, white spikes, the easy tearing of the mucosa) may not be seen on barium studies.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 315371,
"questionText": "Which of these is the most common endoscopic abnormality associated with eosinophilic esophagitis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
827431 | /viewarticle/827431 | [
{
"authors": "George T. Griffing, MD",
"content": [
"Editorial Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 27-year-old woman presents because of hot flashes and cessation of menses since stopping her oral contraceptives six months ago. The hot flashes occur several times a day without perspiration or other symptoms and disturb her sleep. The patient had normal developmental milestones and menarche at age 12 years. She started taking oral contraceptives five years later for irregular menses and contraception. She stopped them recently because she got married and desired fertility. Since then, her only other symptoms have been fatigue and a swelling sensation in her neck that sometimes \"chokes\" her at night when she sleeps on her back.",
"The patient is taking no medications. No contributory factors are found in her previous or family medical history or in the review of systems. She works in the insurance field, has a normal diet, and engages in normal physical activity."
],
"date": "September 02, 2022",
"figures": [],
"markdown": "# A Recently Married 27-Year-Old With Hot Flashes, Amenorrhea\n\n **Authors:** George T. Griffing, MD \n **Date:** September 02, 2022\n\n ## Content\n\n Editorial Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 27-year-old woman presents because of hot flashes and cessation of menses since stopping her oral contraceptives six months ago. The hot flashes occur several times a day without perspiration or other symptoms and disturb her sleep. The patient had normal developmental milestones and menarche at age 12 years. She started taking oral contraceptives five years later for irregular menses and contraception. She stopped them recently because she got married and desired fertility. Since then, her only other symptoms have been fatigue and a swelling sensation in her neck that sometimes \"chokes\" her at night when she sleeps on her back.\nThe patient is taking no medications. No contributory factors are found in her previous or family medical history or in the review of systems. She works in the insurance field, has a normal diet, and engages in normal physical activity.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A Recently Married 27-Year-Old With Hot Flashes, Amenorrhea"
},
{
"authors": "George T. Griffing, MD",
"content": [
"Upon examination, she appears normal with no dysmorphic features. Vital signs are normal except for mild, symptomatic orthostasis; blood pressure and heart rate are 90/60 mm Hg and 72 beats/min (lying), respectively, and > 70/50 mm Hg and 90 beats/min (standing), respectively. Body weight, height, and proportions are normal. She has Tanner stage 5 breast and pubic hair development, no excessive body hair, and no galactorrhea. Her uterus is normal to palpation. The patient is found to have a diffuse and nontender thyroid swelling.",
"General laboratory studies, including a comprehensive metabolic panel, urinalysis, and complete blood count (CBC), are remarkable only for a slightly elevated serum potassium level of 5.1 mEq/L (reference range, 3.5-5 mEq/L) and absolute eosinophil count of 0.61 x 109/L (reference range, 0.05-0.50 x 109/L). Specialized laboratory tests show an elevated thyroid-stimulating hormone (TSH) level of 8.2 mIU/L (reference range, 0.3-5 mIU/L), an antithyroid peroxidase (anti-TPO) antibody level of over 1000 IU/mL (reference range, <9 IU/mL), and a follicle-stimulating hormone (FSH) level of 68 IU/L (follicular phase reference range, 3.9-8.8 IU/L). Prolactin, testosterone and free thyroxin levels are normal. Pregnancy test result is negative."
],
"date": "September 02, 2022",
"figures": [],
"markdown": "# A Recently Married 27-Year-Old With Hot Flashes, Amenorrhea\n\n **Authors:** George T. Griffing, MD \n **Date:** September 02, 2022\n\n ## Content\n\n Upon examination, she appears normal with no dysmorphic features. Vital signs are normal except for mild, symptomatic orthostasis; blood pressure and heart rate are 90/60 mm Hg and 72 beats/min (lying), respectively, and > 70/50 mm Hg and 90 beats/min (standing), respectively. Body weight, height, and proportions are normal. She has Tanner stage 5 breast and pubic hair development, no excessive body hair, and no galactorrhea. Her uterus is normal to palpation. The patient is found to have a diffuse and nontender thyroid swelling.\nGeneral laboratory studies, including a comprehensive metabolic panel, urinalysis, and complete blood count (CBC), are remarkable only for a slightly elevated serum potassium level of 5.1 mEq/L (reference range, 3.5-5 mEq/L) and absolute eosinophil count of 0.61 x 109/L (reference range, 0.05-0.50 x 109/L). Specialized laboratory tests show an elevated thyroid-stimulating hormone (TSH) level of 8.2 mIU/L (reference range, 0.3-5 mIU/L), an antithyroid peroxidase (anti-TPO) antibody level of over 1000 IU/mL (reference range, <9 IU/mL), and a follicle-stimulating hormone (FSH) level of 68 IU/L (follicular phase reference range, 3.9-8.8 IU/L). Prolactin, testosterone and free thyroxin levels are normal. Pregnancy test result is negative.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 742825,
"choiceText": "Primary amenorrhea",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742827,
"choiceText": "Hypothalamic amenorrhea",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742829,
"choiceText": "Primary ovarian insufficiency from Turner syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742831,
"choiceText": "Outflow tract obstruction",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742833,
"choiceText": "Autoimmune oophoritis",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 232361,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Recently Married 27-Year-Old With Hot Flashes, Amenorrhea"
},
{
"authors": "George T. Griffing, MD",
"content": [
"The patient's elevated FSH level indicated the presence of premature ovarian failure (POF; also known as primary ovarian insufficiency), in which the ovaries stop functioning before age 40 years.[1,2,3] Increased FSH results from loss of feedback inhibition from ovarian estrogen and inhibin production (see Figure 1).",
"Figure 1.",
"The two major causes of POF are sex chromosome abnormalities (eg, Turner syndrome) and autoimmune oophoritis.[4,5] Although sex chromosome abnormalities usually present with primary amenorrhea (PA) and complete gonadal failure, an incomplete phenotype, sometimes from genetic mosaicism, manifests after a variable period of relatively normal menstrual function. In this case, additional karyotype testing showed 46,XX, thus ruling out classic Turner syndrome.[5]",
"Loss of menses is normal during pregnancy and during menopause (occurring at about age 50 y). Amenorrhea is the absence of menarche by age 16 years (PA) or the abnormal cessation of established menses (secondary amenorrhea). Although PA is rare, secondary amenorrhea (SA) occurs in 3%-4% of the US female population.",
"The distinction between PA and SA with regard to uterine bleeding can sometimes be blurred by the possibility of a short history of perimenarchal uterine bleeding with PA or by menarchal onset of SA. PA was unlikely in this patient, because her menses were relatively normal for almost five years postmenarche and because the presence of normal female breasts and a normal uterus excluded several diagnostic possibilities for PA. See the following table:",
"Table 1. Primary Amenorrhea: Clinical Diagnostic Differentiation",
"Etiology",
"Breast*",
"Uterus*",
"Additional Testing",
"Delayed puberty",
"no",
"yes",
"FSH ↓",
"Turner 45,X",
"no",
"yes",
"FSH ↑",
"Genital tract agenesis",
"yes",
"no",
"Ultrasonography",
"Androgen insensitivity",
"yes",
"no",
"Karyotype",
"Outflow tract obstruction",
"yes",
"yes",
"Estrogen/progesterone withdrawal test",
"* Normal female development",
"After exclusion of pregnancy and natural menopause, all women with three months of SA should have a diagnostic evaluation. Although the differential diagnosis of SA is extensive, five major etiologies account for the vast majority of cases: hypothalamic amenorrhea, polycystic ovary syndrome (PCOS), hyperprolactinemia; POF, and uterine adhesions. SA can also result from pituitary causes (Sheehan syndrome, empty sella syndrome), hypothyroidism, and fragile-X premutations (FMR1 gene expansions). See Table 2.",
"Table 2. Secondary Amenorrhea (Major Causes): Clinical Diagnostic Differentiation",
"Etiology",
"Body Weight",
"Androgenic",
"Galactorrhea & High Prolactin",
"High FSH",
"History of D&C",
"Hypothalamic amenorrhea",
"↓",
"-",
"-",
"-",
"-",
"Polycystic ovary syndrome",
"↑",
"+",
"-",
"-",
"-",
"Hyperprolactinemia",
"-",
"-",
"+",
"-",
"-",
"Premature ovarian failure",
"-",
"-",
"-",
"+",
"-",
"Uterine adhesions",
"-",
"-",
"-",
"-",
"+"
],
"date": "September 02, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/827/431/827431-thumb-1.jpg"
}
],
"markdown": "# A Recently Married 27-Year-Old With Hot Flashes, Amenorrhea\n\n **Authors:** George T. Griffing, MD \n **Date:** September 02, 2022\n\n ## Content\n\n The patient's elevated FSH level indicated the presence of premature ovarian failure (POF; also known as primary ovarian insufficiency), in which the ovaries stop functioning before age 40 years.[1,2,3] Increased FSH results from loss of feedback inhibition from ovarian estrogen and inhibin production (see Figure 1).\nFigure 1.\nThe two major causes of POF are sex chromosome abnormalities (eg, Turner syndrome) and autoimmune oophoritis.[4,5] Although sex chromosome abnormalities usually present with primary amenorrhea (PA) and complete gonadal failure, an incomplete phenotype, sometimes from genetic mosaicism, manifests after a variable period of relatively normal menstrual function. In this case, additional karyotype testing showed 46,XX, thus ruling out classic Turner syndrome.[5]\nLoss of menses is normal during pregnancy and during menopause (occurring at about age 50 y). Amenorrhea is the absence of menarche by age 16 years (PA) or the abnormal cessation of established menses (secondary amenorrhea). Although PA is rare, secondary amenorrhea (SA) occurs in 3%-4% of the US female population.\nThe distinction between PA and SA with regard to uterine bleeding can sometimes be blurred by the possibility of a short history of perimenarchal uterine bleeding with PA or by menarchal onset of SA. PA was unlikely in this patient, because her menses were relatively normal for almost five years postmenarche and because the presence of normal female breasts and a normal uterus excluded several diagnostic possibilities for PA. See the following table:\nTable 1. Primary Amenorrhea: Clinical Diagnostic Differentiation\nEtiology\nBreast*\nUterus*\nAdditional Testing\nDelayed puberty\nno\nyes\nFSH ↓\nTurner 45,X\nno\nyes\nFSH ↑\nGenital tract agenesis\nyes\nno\nUltrasonography\nAndrogen insensitivity\nyes\nno\nKaryotype\nOutflow tract obstruction\nyes\nyes\nEstrogen/progesterone withdrawal test\n* Normal female development\nAfter exclusion of pregnancy and natural menopause, all women with three months of SA should have a diagnostic evaluation. Although the differential diagnosis of SA is extensive, five major etiologies account for the vast majority of cases: hypothalamic amenorrhea, polycystic ovary syndrome (PCOS), hyperprolactinemia; POF, and uterine adhesions. SA can also result from pituitary causes (Sheehan syndrome, empty sella syndrome), hypothyroidism, and fragile-X premutations (FMR1 gene expansions). See Table 2.\nTable 2. Secondary Amenorrhea (Major Causes): Clinical Diagnostic Differentiation\nEtiology\nBody Weight\nAndrogenic\nGalactorrhea & High Prolactin\nHigh FSH\nHistory of D&C\nHypothalamic amenorrhea\n↓\n-\n-\n-\n-\nPolycystic ovary syndrome\n↑\n+\n-\n-\n-\nHyperprolactinemia\n-\n-\n+\n-\n-\nPremature ovarian failure\n-\n-\n-\n+\n-\nUterine adhesions\n-\n-\n-\n-\n+\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 742825,
"choiceText": "Primary amenorrhea",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742827,
"choiceText": "Hypothalamic amenorrhea",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742829,
"choiceText": "Primary ovarian insufficiency from Turner syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742831,
"choiceText": "Outflow tract obstruction",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742833,
"choiceText": "Autoimmune oophoritis",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 232361,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Recently Married 27-Year-Old With Hot Flashes, Amenorrhea"
},
{
"authors": "George T. Griffing, MD",
"content": [
"This patient's body weight was normal. An excessively low body weight, seen with bulimia or anorexia nervosa, can be associated with hypothalamic amenorrhea. The physiologic stress of being underweight may inhibit normal reproductive function and, therefore, pregnancy; other causes of stress are also believed to inhibit reproductive function at the hypothalamic level.",
"An excessively high body weight, on the other hand, is frequently associated with PCOS, which is characterized by the triad of hyperandrogenism, oligo-ovulation or anovulation, and polycystic ovaries (figures 2-4), with the presence of two of these criteria being necessary for diagnosis. The manifestations of the PCOS triad can vary, and most women have irregular menses rather than amenorrhea.[4,5]",
"Figure 2.",
"Figure 3.",
"Figure 4.",
"Although the etiology of PCOS is uncertain, it is probably a multifactorial process in which insulin resistance leads to hyperinsulinism, which in turn leads to ovarian hyperandrogenesis, which results in hyperaromatization (conversion of androgens to estrogens) in adipose tissue; this causes hyperestrogenemic tonic inhibition of the ovulatory gonadotropin surge, leading to ovulatory dysfunction and polycystic ovaries. PCOS therapies have targeted various points in this process through treatments such as weight loss, insulin sensitizers, antiandrogens, aromatase inhibitors, and ovulation inducers, albeit with varying degrees of success.",
"Because this patient did not manifest galactorrhea or an elevated prolactin level, hyperprolactinemia, another cause of SA, was ruled out. Generally, the prolactin levels would be relatively high, usually five- to ten-fold greater than normal, in this diagnosis This increase often occurs as a result of a prolactin-secreting pituitary tumor. The occurrence of galactorrhea requires prolactin and sufficient estrogen to promote lactogenesis. In extreme cases, however, the lack of estrogen may not support galactorrhea, so its absence cannot rule out hyperprolactinemia.",
"Asherman syndrome was also unlikely in this case. In Asherman syndrome, uterine adhesions (most often resulting from uterine surgery) can block the outflow tract. Almost all patients in which this occurs have a history of dilatation and curettage (D&C), which was not elicited in this patient's history. Many such cases also manifest uterine pain resulting from distention of retained menstrual blood.",
"Almost one-half of patients with POF may have an autoimmune etiology, which is sometimes associated with other endocrinopathies. This patient had clinical and biochemical evidence of autoimmune thyroiditis with her goiter, elevated TSH, and anti-TPO antibodies. Primary adrenal insufficiency was also suggested and was later confirmed; the patient was fatigued, with postural hypotension, mild hyperkalemia, and eosinophilia. Upon closer scrutiny, her skin was hyperpigmented in nonsuntanned areas of the body, and she had an elevated adrenocorticotropic hormone (ACTH) level, as well as an inadequate adrenal cortisol response to exogenous ACTH. Further confirmation of an autoimmune adrenal etiology is possible with measurement of adrenal 21-hydroxylase antibodies, but the test was not performed in this case.",
"Direct confirmation of autoimmune oophoritis with ovarian antibodies is not yet possible, but lymphocytic infiltration, which has been found in patients' ovaries, suggests this etiology.",
"Based on this patient's workup, evidence for the failure of three endocrine glands—ovary, thyroid, and adrenal—were found. The presence of multiple autoimmune endocrine diseases in the same patient suggested the existence of an autoimmune polyglandular syndrome (APS; also referred to as polyglandular autoimmune syndrome), either APS-I, APS-II, or APS-III.[8,9]",
"APS-I is characterized by the classic triad of hypoparathyroidism, chronic mucocutaneous candidiasis, and adrenal dysfunction, with diagnosis requiring the presence of at least two of these conditions. The disease, an autosomal-recessive disorder that begins in infancy, is associated with an autoimmune regulatory (AIRE) gene mutation that alters thymus-mediated cellular immunity.",
"In APS-II, the manifestations include adrenal insufficiency, type 1 diabetes mellitus, gonadal failure, celiac disease, and autoimmune hyperthyroidism or autoimmune hypothyroidism. It has a variable inheritance but is predominantly found in females, with peak onset being between the ages of 20 and 60 years.[8] APS-III is characterized by autoimmune thyroiditis occurring in association with another organ-specific autoimmune disease, such as pernicious anemia, type 1 diabetes mellitus, or vitiligo and/or alopecia. This patient's combination of conditions suggested APS-II with gonadal, thyroid, and adrenal involvement.",
"The mechanistic explanation for the three APS syndromes is unknown, but assignment of a patient to one of them should raise awareness of the possibility of, and perhaps lead to screening for, other associated glandular disorders. For example, assignment of this patient to APS-II prompted testing for celiac disease and/or type 1 diabetes mellitus. The results for her celiac and diabetes autoantibody panels were negative."
],
"date": "September 02, 2022",
"figures": [
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/827/431/827431-thumb-2.jpg"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/827/431/827431-thumb-3.jpg"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/827/431/827431-thumb-4.jpg"
}
],
"markdown": "# A Recently Married 27-Year-Old With Hot Flashes, Amenorrhea\n\n **Authors:** George T. Griffing, MD \n **Date:** September 02, 2022\n\n ## Content\n\n This patient's body weight was normal. An excessively low body weight, seen with bulimia or anorexia nervosa, can be associated with hypothalamic amenorrhea. The physiologic stress of being underweight may inhibit normal reproductive function and, therefore, pregnancy; other causes of stress are also believed to inhibit reproductive function at the hypothalamic level.\nAn excessively high body weight, on the other hand, is frequently associated with PCOS, which is characterized by the triad of hyperandrogenism, oligo-ovulation or anovulation, and polycystic ovaries (figures 2-4), with the presence of two of these criteria being necessary for diagnosis. The manifestations of the PCOS triad can vary, and most women have irregular menses rather than amenorrhea.[4,5]\nFigure 2.\nFigure 3.\nFigure 4.\nAlthough the etiology of PCOS is uncertain, it is probably a multifactorial process in which insulin resistance leads to hyperinsulinism, which in turn leads to ovarian hyperandrogenesis, which results in hyperaromatization (conversion of androgens to estrogens) in adipose tissue; this causes hyperestrogenemic tonic inhibition of the ovulatory gonadotropin surge, leading to ovulatory dysfunction and polycystic ovaries. PCOS therapies have targeted various points in this process through treatments such as weight loss, insulin sensitizers, antiandrogens, aromatase inhibitors, and ovulation inducers, albeit with varying degrees of success.\nBecause this patient did not manifest galactorrhea or an elevated prolactin level, hyperprolactinemia, another cause of SA, was ruled out. Generally, the prolactin levels would be relatively high, usually five- to ten-fold greater than normal, in this diagnosis This increase often occurs as a result of a prolactin-secreting pituitary tumor. The occurrence of galactorrhea requires prolactin and sufficient estrogen to promote lactogenesis. In extreme cases, however, the lack of estrogen may not support galactorrhea, so its absence cannot rule out hyperprolactinemia.\nAsherman syndrome was also unlikely in this case. In Asherman syndrome, uterine adhesions (most often resulting from uterine surgery) can block the outflow tract. Almost all patients in which this occurs have a history of dilatation and curettage (D&C), which was not elicited in this patient's history. Many such cases also manifest uterine pain resulting from distention of retained menstrual blood.\nAlmost one-half of patients with POF may have an autoimmune etiology, which is sometimes associated with other endocrinopathies. This patient had clinical and biochemical evidence of autoimmune thyroiditis with her goiter, elevated TSH, and anti-TPO antibodies. Primary adrenal insufficiency was also suggested and was later confirmed; the patient was fatigued, with postural hypotension, mild hyperkalemia, and eosinophilia. Upon closer scrutiny, her skin was hyperpigmented in nonsuntanned areas of the body, and she had an elevated adrenocorticotropic hormone (ACTH) level, as well as an inadequate adrenal cortisol response to exogenous ACTH. Further confirmation of an autoimmune adrenal etiology is possible with measurement of adrenal 21-hydroxylase antibodies, but the test was not performed in this case.\nDirect confirmation of autoimmune oophoritis with ovarian antibodies is not yet possible, but lymphocytic infiltration, which has been found in patients' ovaries, suggests this etiology.\nBased on this patient's workup, evidence for the failure of three endocrine glands—ovary, thyroid, and adrenal—were found. The presence of multiple autoimmune endocrine diseases in the same patient suggested the existence of an autoimmune polyglandular syndrome (APS; also referred to as polyglandular autoimmune syndrome), either APS-I, APS-II, or APS-III.[8,9]\nAPS-I is characterized by the classic triad of hypoparathyroidism, chronic mucocutaneous candidiasis, and adrenal dysfunction, with diagnosis requiring the presence of at least two of these conditions. The disease, an autosomal-recessive disorder that begins in infancy, is associated with an autoimmune regulatory (AIRE) gene mutation that alters thymus-mediated cellular immunity.\nIn APS-II, the manifestations include adrenal insufficiency, type 1 diabetes mellitus, gonadal failure, celiac disease, and autoimmune hyperthyroidism or autoimmune hypothyroidism. It has a variable inheritance but is predominantly found in females, with peak onset being between the ages of 20 and 60 years.[8] APS-III is characterized by autoimmune thyroiditis occurring in association with another organ-specific autoimmune disease, such as pernicious anemia, type 1 diabetes mellitus, or vitiligo and/or alopecia. This patient's combination of conditions suggested APS-II with gonadal, thyroid, and adrenal involvement.\nThe mechanistic explanation for the three APS syndromes is unknown, but assignment of a patient to one of them should raise awareness of the possibility of, and perhaps lead to screening for, other associated glandular disorders. For example, assignment of this patient to APS-II prompted testing for celiac disease and/or type 1 diabetes mellitus. The results for her celiac and diabetes autoantibody panels were negative.\n\n ## Figures\n\n **Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4.** \n \n\n\n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A Recently Married 27-Year-Old With Hot Flashes, Amenorrhea"
},
{
"authors": "George T. Griffing, MD",
"content": [
"In follow-up, the patient was diagnosed with APS-II manifesting as primary adrenal insufficiency, autoimmune thyroiditis with subclinical hypothyroidism, and POF caused by autoimmune oophoritis. Treatment included adrenal gland replacement therapy with glucocorticoids, thyroid hormone replacement with L-thyroxin, and gonadal replacement therapy with estrogen and progesterone.",
"The patient was given a medi-alert bracelet and sick-day instructions for adrenal replacement. Following institution of hormonal replacement, her fatigue, orthostasis, and hot flashes resolved. In addition, her goiter shrank, and she had cyclic menses on gonadal replacement. Understanding that her chances of fertility were greatly reduced, she initiated adoption procedures.",
"However, 10% of patients with POF presenting as SA spontaneously conceive. Moreover, for women with POF who wish to conceive, donor oocytes and donor embryos can increase the chance of pregnancy.[8] Women with POF who do not wish to conceive should be advised to use barrier methods of contraception or surgical sterilization, because their high baseline FSH level makes hormonal contraception ineffective."
],
"date": "September 02, 2022",
"figures": [],
"markdown": "# A Recently Married 27-Year-Old With Hot Flashes, Amenorrhea\n\n **Authors:** George T. Griffing, MD \n **Date:** September 02, 2022\n\n ## Content\n\n In follow-up, the patient was diagnosed with APS-II manifesting as primary adrenal insufficiency, autoimmune thyroiditis with subclinical hypothyroidism, and POF caused by autoimmune oophoritis. Treatment included adrenal gland replacement therapy with glucocorticoids, thyroid hormone replacement with L-thyroxin, and gonadal replacement therapy with estrogen and progesterone.\nThe patient was given a medi-alert bracelet and sick-day instructions for adrenal replacement. Following institution of hormonal replacement, her fatigue, orthostasis, and hot flashes resolved. In addition, her goiter shrank, and she had cyclic menses on gonadal replacement. Understanding that her chances of fertility were greatly reduced, she initiated adoption procedures.\nHowever, 10% of patients with POF presenting as SA spontaneously conceive. Moreover, for women with POF who wish to conceive, donor oocytes and donor embryos can increase the chance of pregnancy.[8] Women with POF who do not wish to conceive should be advised to use barrier methods of contraception or surgical sterilization, because their high baseline FSH level makes hormonal contraception ineffective.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 742837,
"choiceText": "Estrogen/progesterone withdrawal test",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742839,
"choiceText": "Karyotype",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742841,
"choiceText": "Pelvic ultrasonography",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742843,
"choiceText": "FSH level",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "In a woman with an intact uterus, estrogen/progesterone stimulation should produce uterine bleeding. If it does not, an outflow tract obstruction is the only explanation. Other studies would not be as definitive. The karyotype should be normal, based on the presence of normal breasts, uterus, and FSH level. Pelvic ultrasonography should show the uterus detected on exam. The FSH level, whether high or low, would not interfere with the estrogen/progesterone withdrawal test.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 232363,
"questionText": "If this patient had presented with PA with normal female breasts and uterus, which would have been the most revealing diagnostic test?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 742845,
"choiceText": "Normal 46,XX karyotype",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742847,
"choiceText": "Other autoimmune glandular disorders",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742849,
"choiceText": "Elevated TSH",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742851,
"choiceText": "Hot flashes",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Although no tests can definitively prove autoimmune oophoritis, the etiology is inferred by the finding of other autoimmune glandular diseases, in this case of the adrenal and thyroid glands. This patient’s pattern of association has been described for APS-II. Normal karyotype testing does not rule out mosaicism, which may affect only the ovary and cause incomplete penetrance, explaining a presentation of SA rather than PA. The elevated TSH can occur with etiologies other than autoimmune disorders, and the mild degree of hypothyroidism is insufficient to affect menses. Finally, hot flashes are indicative of estrogen deficiency and are not helpful in the etiology other than to exclude non-hypoestrogenemic causes, such as Asherman syndrome.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 232365,
"questionText": "In the patient in this case, with SA and high FSH, what additional finding was most helpful?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Recently Married 27-Year-Old With Hot Flashes, Amenorrhea"
},
{
"authors": "George T. Griffing, MD",
"content": [],
"date": "September 02, 2022",
"figures": [],
"markdown": "# A Recently Married 27-Year-Old With Hot Flashes, Amenorrhea\n\n **Authors:** George T. Griffing, MD \n **Date:** September 02, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 742837,
"choiceText": "Estrogen/progesterone withdrawal test",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742839,
"choiceText": "Karyotype",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742841,
"choiceText": "Pelvic ultrasonography",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742843,
"choiceText": "FSH level",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "In a woman with an intact uterus, estrogen/progesterone stimulation should produce uterine bleeding. If it does not, an outflow tract obstruction is the only explanation. Other studies would not be as definitive. The karyotype should be normal, based on the presence of normal breasts, uterus, and FSH level. Pelvic ultrasonography should show the uterus detected on exam. The FSH level, whether high or low, would not interfere with the estrogen/progesterone withdrawal test.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 232363,
"questionText": "If this patient had presented with PA with normal female breasts and uterus, which would have been the most revealing diagnostic test?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 742845,
"choiceText": "Normal 46,XX karyotype",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742847,
"choiceText": "Other autoimmune glandular disorders",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742849,
"choiceText": "Elevated TSH",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742851,
"choiceText": "Hot flashes",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Although no tests can definitively prove autoimmune oophoritis, the etiology is inferred by the finding of other autoimmune glandular diseases, in this case of the adrenal and thyroid glands. This patient’s pattern of association has been described for APS-II. Normal karyotype testing does not rule out mosaicism, which may affect only the ovary and cause incomplete penetrance, explaining a presentation of SA rather than PA. The elevated TSH can occur with etiologies other than autoimmune disorders, and the mild degree of hypothyroidism is insufficient to affect menses. Finally, hot flashes are indicative of estrogen deficiency and are not helpful in the etiology other than to exclude non-hypoestrogenemic causes, such as Asherman syndrome.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 232365,
"questionText": "In the patient in this case, with SA and high FSH, what additional finding was most helpful?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Recently Married 27-Year-Old With Hot Flashes, Amenorrhea"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 742825,
"choiceText": "Primary amenorrhea",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742827,
"choiceText": "Hypothalamic amenorrhea",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742829,
"choiceText": "Primary ovarian insufficiency from Turner syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742831,
"choiceText": "Outflow tract obstruction",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742833,
"choiceText": "Autoimmune oophoritis",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 232361,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 742837,
"choiceText": "Estrogen/progesterone withdrawal test",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742839,
"choiceText": "Karyotype",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742841,
"choiceText": "Pelvic ultrasonography",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742843,
"choiceText": "FSH level",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "In a woman with an intact uterus, estrogen/progesterone stimulation should produce uterine bleeding. If it does not, an outflow tract obstruction is the only explanation. Other studies would not be as definitive. The karyotype should be normal, based on the presence of normal breasts, uterus, and FSH level. Pelvic ultrasonography should show the uterus detected on exam. The FSH level, whether high or low, would not interfere with the estrogen/progesterone withdrawal test.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 232363,
"questionText": "If this patient had presented with PA with normal female breasts and uterus, which would have been the most revealing diagnostic test?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 742845,
"choiceText": "Normal 46,XX karyotype",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742847,
"choiceText": "Other autoimmune glandular disorders",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742849,
"choiceText": "Elevated TSH",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 742851,
"choiceText": "Hot flashes",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Although no tests can definitively prove autoimmune oophoritis, the etiology is inferred by the finding of other autoimmune glandular diseases, in this case of the adrenal and thyroid glands. This patient’s pattern of association has been described for APS-II. Normal karyotype testing does not rule out mosaicism, which may affect only the ovary and cause incomplete penetrance, explaining a presentation of SA rather than PA. The elevated TSH can occur with etiologies other than autoimmune disorders, and the mild degree of hypothyroidism is insufficient to affect menses. Finally, hot flashes are indicative of estrogen deficiency and are not helpful in the etiology other than to exclude non-hypoestrogenemic causes, such as Asherman syndrome.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 232365,
"questionText": "In the patient in this case, with SA and high FSH, what additional finding was most helpful?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
979595 | /viewarticle/979595 | [
{
"authors": "Ryan J. Cole, MD; Christopher P. Holstege, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 45-year-old man with a history of bipolar disorder, hypertension, hyperlipidemia, and asthma is transported to the emergency department after his sister found him crawling on the floor of his home, confused and incontinent. She reports that she talked with him 3 days earlier on the phone and that he sounded slightly confused at the time. She called again today, and when he failed to answer, she stopped at his home and found him delirious and unable to walk, which prompted her to call emergency services.",
"His medications include lithium carbonate (1200 mg/d), amlodipine (10 mg/d), atorvastatin (10 mg/d), and an albuterol rescue inhaler as needed. He is a former smoker who quit 20 years ago. He drinks alcohol socially and does not use illicit drugs."
],
"date": "September 01, 2022",
"figures": [],
"markdown": "# Delirious, Incontinent 45-Year-Old Found Crawling on the Floor\n\n **Authors:** Ryan J. Cole, MD; Christopher P. Holstege, MD \n **Date:** September 01, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 45-year-old man with a history of bipolar disorder, hypertension, hyperlipidemia, and asthma is transported to the emergency department after his sister found him crawling on the floor of his home, confused and incontinent. She reports that she talked with him 3 days earlier on the phone and that he sounded slightly confused at the time. She called again today, and when he failed to answer, she stopped at his home and found him delirious and unable to walk, which prompted her to call emergency services.\nHis medications include lithium carbonate (1200 mg/d), amlodipine (10 mg/d), atorvastatin (10 mg/d), and an albuterol rescue inhaler as needed. He is a former smoker who quit 20 years ago. He drinks alcohol socially and does not use illicit drugs.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Delirious, Incontinent 45-Year-Old Found Crawling on the Floor"
},
{
"authors": "Ryan J. Cole, MD; Christopher P. Holstege, MD",
"content": [
"Upon presentation, the patient is disheveled, smells of urine, has slurred speech, and is unable to provide coherent additional history. He is alert but oriented to person only. His initial vital signs include a blood pressure of 93/34 mm Hg, a heart rate of 124 beats/min, a respiration rate of 22 breaths/min, a transcutaneous oxygen saturation of 98%, and a rectal temperature of 100.6 °F (38.1 °C).",
"The examination is significant for: dry mucous membranes, tachycardia, lateral gaze nystagmus, resting tremor of his extremities that worsens with activity, inability to perform finger-to-nose testing, truncal ataxia with inability to walk, hyperreflexia, and six beats of bilateral ankle clonus.",
"Initial laboratory studies reveal these values:",
"White blood cell count: 17,000 cells/mm3 (reference range, 4500-11,000 cells/mm3)",
"Potassium level: 3.8 mEq/L (reference range, 3.5-5.0 mEq/L)",
"Sodium level: 124 mEq/L (reference range, 135-145 mEq/L)",
"Chloride level: 111 mEq/L (reference range, 98-106 mEq/L)",
"Serum bicarbonate level: 14 mEq/L (reference range, 21-28 mEq/L)",
"Creatinine level: 2.88 mg/dL (reference range, 0.8-1.5 mg/dL)",
"Blood urea nitrogen (BUN) level: 52 mg/dL (reference range, 9-20 mg/dL)",
"Glucose level: 155 mg/dL (reference range [fasting], 74-106 mg/dL)",
"Calcium level: 8.8 mg/dL (reference range, 8-10 mg/dL)",
"Lactate level: 3.2 mg/dL (reference range, 0.5-1 mg/dL)",
"Thyroid-stimulating hormone (TSH) level: 1.41 mIU/L (reference range, 0.4-4.0 mIU/L)",
"Lithium level: 2.4 mEq/L (reference range, 0.6-1.2 mEq/L)",
"A urine drug screen is negative, and his urine specific gravity is < 1.010, with ketones detected. A head CT is normal. The only significant finding on the ECG is sinus tachycardia. The patient is admitted to a monitored bed. His urine output is 6.5 L during the first 24 hours of admission despite fluid restrictions."
],
"date": "September 01, 2022",
"figures": [],
"markdown": "# Delirious, Incontinent 45-Year-Old Found Crawling on the Floor\n\n **Authors:** Ryan J. Cole, MD; Christopher P. Holstege, MD \n **Date:** September 01, 2022\n\n ## Content\n\n Upon presentation, the patient is disheveled, smells of urine, has slurred speech, and is unable to provide coherent additional history. He is alert but oriented to person only. His initial vital signs include a blood pressure of 93/34 mm Hg, a heart rate of 124 beats/min, a respiration rate of 22 breaths/min, a transcutaneous oxygen saturation of 98%, and a rectal temperature of 100.6 °F (38.1 °C).\nThe examination is significant for: dry mucous membranes, tachycardia, lateral gaze nystagmus, resting tremor of his extremities that worsens with activity, inability to perform finger-to-nose testing, truncal ataxia with inability to walk, hyperreflexia, and six beats of bilateral ankle clonus.\nInitial laboratory studies reveal these values:\nWhite blood cell count: 17,000 cells/mm3 (reference range, 4500-11,000 cells/mm3)\nPotassium level: 3.8 mEq/L (reference range, 3.5-5.0 mEq/L)\nSodium level: 124 mEq/L (reference range, 135-145 mEq/L)\nChloride level: 111 mEq/L (reference range, 98-106 mEq/L)\nSerum bicarbonate level: 14 mEq/L (reference range, 21-28 mEq/L)\nCreatinine level: 2.88 mg/dL (reference range, 0.8-1.5 mg/dL)\nBlood urea nitrogen (BUN) level: 52 mg/dL (reference range, 9-20 mg/dL)\nGlucose level: 155 mg/dL (reference range [fasting], 74-106 mg/dL)\nCalcium level: 8.8 mg/dL (reference range, 8-10 mg/dL)\nLactate level: 3.2 mg/dL (reference range, 0.5-1 mg/dL)\nThyroid-stimulating hormone (TSH) level: 1.41 mIU/L (reference range, 0.4-4.0 mIU/L)\nLithium level: 2.4 mEq/L (reference range, 0.6-1.2 mEq/L)\nA urine drug screen is negative, and his urine specific gravity is < 1.010, with ketones detected. A head CT is normal. The only significant finding on the ECG is sinus tachycardia. The patient is admitted to a monitored bed. His urine output is 6.5 L during the first 24 hours of admission despite fluid restrictions.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1713453,
"choiceText": "Lithium-induced hyperthyroidism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713454,
"choiceText": "Lithium-induced hypothyroidism",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713455,
"choiceText": "Lithium-induced nephrogenic diabetes insipidus",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713456,
"choiceText": "Lithium-induced hyperparathyroidism",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 552510,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Delirious, Incontinent 45-Year-Old Found Crawling on the Floor"
},
{
"authors": "Ryan J. Cole, MD; Christopher P. Holstege, MD",
"content": [
"The patient in this case had chronic lithium toxicity, which was precipitated by the development of nephrogenic diabetes insipidus (DI) during long-term lithium therapy for bipolar disorder. He developed confusion, slurred speech, nystagmus, and ataxia, all of which are manifestations of lithium toxicity. His lithium level was elevated at 2.4 mEq/L (reference range, 0.6-1.2 mEq/L). This elevation was due to nephrogenic DI, which interferes with lithium excretion through polyuria and leads to excessive fluid losses. Clues in this case that point toward nephrogenic DI include incontinence of urine, elevation of creatinine, low urine specific gravity, and a large urine output despite fluid restriction. Hypothyroidism, hyperthyroidism, and hyperparathyroidism are also in the differential diagnosis; however, this patient's TSH and calcium levels are within normal limits, making these conditions less likely.",
"Lithium is a metal that has been used in psychiatry since the mid-19th century for the treatment of mania and bipolar disorder and for the prophylaxis of depression.[1] The exact mechanism responsible for its clinical effectiveness in treating these conditions is still not known, although many complex mechanisms have been proposed.[2] Lithium is available in both immediate-release and sustained-release formulations. Owing to its narrow therapeutic index (0.6-1.2 mEq/L), serum levels must be monitored to avoid toxicity.[3] In 2020, there were 6276 cases of lithium toxicity reported to US poison centers.[4] The mortality rate for lithium toxicity has been reported at 0.8%, with deaths occurring only in cases of chronic toxicity.[5]",
"Although lithium toxicity can affect multiple organ systems in overdose, the central nervous system (CNS) is the primary site of toxicity. How the CNS is affected depends on the pattern of toxicity, which is divided into three categories[2,6]:",
"Acute (acute ingestion of lithium in a patient who is not taking lithium)",
"Acute-on-chronic (acute ingestion of lithium beyond the prescribed dose in a patient who is taking lithium)",
"Chronic (patient on lithium who shows signs of toxicity without an acute ingestion, usually occurring over weeks)",
"The risk for neurotoxicity is lowest with acute toxicity and highest in chronic cases.[2]",
"An irreversible syndrome of neurotoxicity has been described with lithium use, which is known as the syndrome of irreversible lithium-effectuated neurotoxicity (SILENT). SILENT typically presents with persistent symptoms of cerebellar dysfunction, extrapyramidal symptoms, brainstem dysfunction, and dementia. It is diagnosed by the causation of symptoms by lithium in the absence of prior neurologic illness, with the persistence of neurologic findings for 2 months after the cessation of lithium. Symptoms may resolve spontaneously; however, most last for long periods and are irreversible.[7]"
],
"date": "September 01, 2022",
"figures": [],
"markdown": "# Delirious, Incontinent 45-Year-Old Found Crawling on the Floor\n\n **Authors:** Ryan J. Cole, MD; Christopher P. Holstege, MD \n **Date:** September 01, 2022\n\n ## Content\n\n The patient in this case had chronic lithium toxicity, which was precipitated by the development of nephrogenic diabetes insipidus (DI) during long-term lithium therapy for bipolar disorder. He developed confusion, slurred speech, nystagmus, and ataxia, all of which are manifestations of lithium toxicity. His lithium level was elevated at 2.4 mEq/L (reference range, 0.6-1.2 mEq/L). This elevation was due to nephrogenic DI, which interferes with lithium excretion through polyuria and leads to excessive fluid losses. Clues in this case that point toward nephrogenic DI include incontinence of urine, elevation of creatinine, low urine specific gravity, and a large urine output despite fluid restriction. Hypothyroidism, hyperthyroidism, and hyperparathyroidism are also in the differential diagnosis; however, this patient's TSH and calcium levels are within normal limits, making these conditions less likely.\nLithium is a metal that has been used in psychiatry since the mid-19th century for the treatment of mania and bipolar disorder and for the prophylaxis of depression.[1] The exact mechanism responsible for its clinical effectiveness in treating these conditions is still not known, although many complex mechanisms have been proposed.[2] Lithium is available in both immediate-release and sustained-release formulations. Owing to its narrow therapeutic index (0.6-1.2 mEq/L), serum levels must be monitored to avoid toxicity.[3] In 2020, there were 6276 cases of lithium toxicity reported to US poison centers.[4] The mortality rate for lithium toxicity has been reported at 0.8%, with deaths occurring only in cases of chronic toxicity.[5]\nAlthough lithium toxicity can affect multiple organ systems in overdose, the central nervous system (CNS) is the primary site of toxicity. How the CNS is affected depends on the pattern of toxicity, which is divided into three categories[2,6]:\nAcute (acute ingestion of lithium in a patient who is not taking lithium)\nAcute-on-chronic (acute ingestion of lithium beyond the prescribed dose in a patient who is taking lithium)\nChronic (patient on lithium who shows signs of toxicity without an acute ingestion, usually occurring over weeks)\nThe risk for neurotoxicity is lowest with acute toxicity and highest in chronic cases.[2]\nAn irreversible syndrome of neurotoxicity has been described with lithium use, which is known as the syndrome of irreversible lithium-effectuated neurotoxicity (SILENT). SILENT typically presents with persistent symptoms of cerebellar dysfunction, extrapyramidal symptoms, brainstem dysfunction, and dementia. It is diagnosed by the causation of symptoms by lithium in the absence of prior neurologic illness, with the persistence of neurologic findings for 2 months after the cessation of lithium. Symptoms may resolve spontaneously; however, most last for long periods and are irreversible.[7]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1713453,
"choiceText": "Lithium-induced hyperthyroidism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713454,
"choiceText": "Lithium-induced hypothyroidism",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713455,
"choiceText": "Lithium-induced nephrogenic diabetes insipidus",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713456,
"choiceText": "Lithium-induced hyperparathyroidism",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 552510,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Delirious, Incontinent 45-Year-Old Found Crawling on the Floor"
},
{
"authors": "Ryan J. Cole, MD; Christopher P. Holstege, MD",
"content": [
"Chronic toxicity can be triggered by a variety of factors that lead to decreased renal function, which in turn impairs the elimination of lithium from the body. Lithium is a monovalent cation and alkali earth metal; its mechanics of reabsorption are very similar to those of sodium, with reabsorption occurring in the proximal tubule, distal tubule, and collecting duct. Conditions that lead to greater sodium reabsorption also increase reabsorption of lithium.[8] Illness that results in hypovolemia from fluid loss can cause an acute kidney injury and thereby decrease elimination. Drugs that lower the glomerular filtration rate (GFR), such as nonsteroidal anti-inflammatory drugs (NSAIDs) and angiotensin-converting enzyme (ACE) inhibitors, also reduce elimination. Medications that promote renal absorption, such as thiazide diuretics and spironolactone, cause reabsorption of both sodium and lithium via the same mechanisms.[2] Other known risk factors include the presence of nephrogenic DI, age older than 50 years, and the presence of thyroid dysfunction.[6]",
"Long-term use of lithium is associated with renal impairment.[9] Nephrogenic DI is the most common adverse effect observed in patients who are receiving long-term lithium therapy.[10,11] Lithium interferes with the kidney's ability to concentrate urine, owing to a loss of responsiveness to vasopressin.[12,13] Polyuria leads to volume contraction and subsequent hypernatremia, hyperchloremic metabolic acidosis, and distal renal tubular acidosis.[6,13] These fluid losses trigger increased reabsorption of sodium and also lithium, reducing both the GFR and lithium excretion.",
"The mechanisms by which lithium affects the kidney's ability to concentrate urine can help shed light on the treatment of lithium-induced nephrogenic DI. Lithium enters the principal cells of the collecting duct via the epithelial sodium channel (ENaC), which is more permeable to lithium than to sodium.[8,10,12,13] Although sodium is removed from the cell by sodium/potassium adenosine triphosphatase (Na/K ATPase), lithium is not, causing intracellular levels of lithium to rise.[8] This interferes with the cell's responsiveness to aldosterone and vasopressin, which, in turn, limits insertion of aquaporin-2 and leads to decreased water reabsorption.[8] Amiloride, which blocks the ENaC, has a theoretical benefit by blocking lithium entry and thereby restoring urine concentrating ability.[8] However, its onset of action is slow (weeks), and it does not significantly enhance lithium elimination, limiting its use in current practice.[2,14] Thiazide diuretics, which are useful in treating other forms of nephrogenic DI, should be avoided because they reduce lithium excretion, resulting in further toxicity.[11]",
"Lithium also induces cyclooxygenase-2 (COX-2) expression in the kidney medulla.[8] Increased COX-2 leads to the production of prostaglandin E2 (PGE2), which interferes with the ability of the collecting duct to concentrate urine by modulating the expression of aquaporin-2 (Figures 1 and 2).[12] Treatment with indomethacin, which blocks PGE2, has been shown to enable the kidney to concentrate urine.[14 ]",
"Figure 1. Normal transport of sodium and water in the collecting duct. Sodium enters the cell via the ENaC and is transported out of the cell via Na/K ATPase on the basolateral surface in exchange for potassium. Vasopressin binds V2 receptors, which are coupled to G proteins. Activation of this receptor increases cAMP by activating AC. Downstream effects lead to phosphorylation, causing movement of intracellular AQP-2 to the apical surface of the cell. Water flows through AQP-2 and finally through AQP-3 or AQP-4 to the basal surface of the cell. AC = adenylate cyclase; AQP = aquaporin; cAMP = cyclic adenosine monophosphate; ENaC = epithelial sodium channel; Na/K ATPase = sodium/potassium adenosine triphosphatase",
"Figure 2. Impaired function by lithium. Lithium enters the cell via the ENaC, which has a higher affinity for lithium than sodium. The Na/K ATPase at the basal surface cannot pump lithium out of the cell, causing lithium to build up intracellularly. Amiloride, which blocks the ENaC, has a theoretical benefit by blocking entry of lithium into the cell. Intracellular lithium interferes with the cell's ability to insert AQP-2 into the membrane, decreasing water reabsorption. Lithium stimulates production of PGE2, which interferes with the effect of vasopressin on the cell. This, in addition to the intracellular interference, reduces AQP-2 insertion and water reabsorption. Indomethacin, a PGE2 inhibitor, helps restore concentrating ability.",
"AQP = aquaporin; ENaC = epithelial sodium channel; Na/K ATPase = sodium/potassium adenosine triphosphatase; PGE2 = prostaglandin E2",
"Lithium has several endocrine effects. Hypothyroidism commonly occurs because of lithium's inhibitory effects on thyroid hormone production and secretion. Hypothyroidism can lower the GFR and thereby decrease lithium excretion. Although not directly caused by lithium, hyperthyroidism increases lithium reuptake, which can result in toxicity. Lithium also interferes with calcium sensing, which can lead to hyperparathyroidism.[15]Hypercalcemia can cause osmotic diuresis, resulting in volume depletion.[2]",
"The manifestations of lithium toxicity range from a lack of symptoms to profound neurotoxicity.[2] Common symptoms include gastrointestinal (GI) distress (nausea, vomiting), muscle weakness, slurred speech, tremor, nystagmus, and ataxia. More severe intoxication can cause seizures, hyperthermia, delirium, and coma.",
"The workup includes obtaining and trending lithium levels and evaluation of electrolyte levels, kidney function, and thyroid function. Lithium levels should not be drawn in tubes containing lithium heparin because this can falsely elevate the level.[16] Acetaminophen, salicylate, and ethanol levels should also be obtained in case of possible co-ingestion. An ECG may reveal nonspecific T-wave abnormalities, QTc prolongation, or bradycardia. Hypotension can occur in severe cases.[3]",
"Treatment of lithium toxicity is aimed at preventing absorption and promoting elimination to lower serum levels and improve clinical symptoms. The first step in preventing absorption is to hold the patient's lithium and discontinue medications that can lead to increased lithium levels through impairment of kidney function. Although activated charcoal is useful in many types of overdoses, it has no role in lithium toxicity owing to its limited ability to bind metals.[17] In cases of severe toxicity or toxicity from sustained-release formulations, whole-bowel irrigation with polyethylene glycol electrolyte solution (PEG-ES) can be considered to speed transit through the GI tract in an effort to limit absorption.[18] The recommended regimen is 1-2 L/h of PEG-ES via nasogastric tube until the rectal effluent is clear.[2]"
],
"date": "September 01, 2022",
"figures": [],
"markdown": "# Delirious, Incontinent 45-Year-Old Found Crawling on the Floor\n\n **Authors:** Ryan J. Cole, MD; Christopher P. Holstege, MD \n **Date:** September 01, 2022\n\n ## Content\n\n Chronic toxicity can be triggered by a variety of factors that lead to decreased renal function, which in turn impairs the elimination of lithium from the body. Lithium is a monovalent cation and alkali earth metal; its mechanics of reabsorption are very similar to those of sodium, with reabsorption occurring in the proximal tubule, distal tubule, and collecting duct. Conditions that lead to greater sodium reabsorption also increase reabsorption of lithium.[8] Illness that results in hypovolemia from fluid loss can cause an acute kidney injury and thereby decrease elimination. Drugs that lower the glomerular filtration rate (GFR), such as nonsteroidal anti-inflammatory drugs (NSAIDs) and angiotensin-converting enzyme (ACE) inhibitors, also reduce elimination. Medications that promote renal absorption, such as thiazide diuretics and spironolactone, cause reabsorption of both sodium and lithium via the same mechanisms.[2] Other known risk factors include the presence of nephrogenic DI, age older than 50 years, and the presence of thyroid dysfunction.[6]\nLong-term use of lithium is associated with renal impairment.[9] Nephrogenic DI is the most common adverse effect observed in patients who are receiving long-term lithium therapy.[10,11] Lithium interferes with the kidney's ability to concentrate urine, owing to a loss of responsiveness to vasopressin.[12,13] Polyuria leads to volume contraction and subsequent hypernatremia, hyperchloremic metabolic acidosis, and distal renal tubular acidosis.[6,13] These fluid losses trigger increased reabsorption of sodium and also lithium, reducing both the GFR and lithium excretion.\nThe mechanisms by which lithium affects the kidney's ability to concentrate urine can help shed light on the treatment of lithium-induced nephrogenic DI. Lithium enters the principal cells of the collecting duct via the epithelial sodium channel (ENaC), which is more permeable to lithium than to sodium.[8,10,12,13] Although sodium is removed from the cell by sodium/potassium adenosine triphosphatase (Na/K ATPase), lithium is not, causing intracellular levels of lithium to rise.[8] This interferes with the cell's responsiveness to aldosterone and vasopressin, which, in turn, limits insertion of aquaporin-2 and leads to decreased water reabsorption.[8] Amiloride, which blocks the ENaC, has a theoretical benefit by blocking lithium entry and thereby restoring urine concentrating ability.[8] However, its onset of action is slow (weeks), and it does not significantly enhance lithium elimination, limiting its use in current practice.[2,14] Thiazide diuretics, which are useful in treating other forms of nephrogenic DI, should be avoided because they reduce lithium excretion, resulting in further toxicity.[11]\nLithium also induces cyclooxygenase-2 (COX-2) expression in the kidney medulla.[8] Increased COX-2 leads to the production of prostaglandin E2 (PGE2), which interferes with the ability of the collecting duct to concentrate urine by modulating the expression of aquaporin-2 (Figures 1 and 2).[12] Treatment with indomethacin, which blocks PGE2, has been shown to enable the kidney to concentrate urine.[14 ]\nFigure 1. Normal transport of sodium and water in the collecting duct. Sodium enters the cell via the ENaC and is transported out of the cell via Na/K ATPase on the basolateral surface in exchange for potassium. Vasopressin binds V2 receptors, which are coupled to G proteins. Activation of this receptor increases cAMP by activating AC. Downstream effects lead to phosphorylation, causing movement of intracellular AQP-2 to the apical surface of the cell. Water flows through AQP-2 and finally through AQP-3 or AQP-4 to the basal surface of the cell. AC = adenylate cyclase; AQP = aquaporin; cAMP = cyclic adenosine monophosphate; ENaC = epithelial sodium channel; Na/K ATPase = sodium/potassium adenosine triphosphatase\nFigure 2. Impaired function by lithium. Lithium enters the cell via the ENaC, which has a higher affinity for lithium than sodium. The Na/K ATPase at the basal surface cannot pump lithium out of the cell, causing lithium to build up intracellularly. Amiloride, which blocks the ENaC, has a theoretical benefit by blocking entry of lithium into the cell. Intracellular lithium interferes with the cell's ability to insert AQP-2 into the membrane, decreasing water reabsorption. Lithium stimulates production of PGE2, which interferes with the effect of vasopressin on the cell. This, in addition to the intracellular interference, reduces AQP-2 insertion and water reabsorption. Indomethacin, a PGE2 inhibitor, helps restore concentrating ability.\nAQP = aquaporin; ENaC = epithelial sodium channel; Na/K ATPase = sodium/potassium adenosine triphosphatase; PGE2 = prostaglandin E2\nLithium has several endocrine effects. Hypothyroidism commonly occurs because of lithium's inhibitory effects on thyroid hormone production and secretion. Hypothyroidism can lower the GFR and thereby decrease lithium excretion. Although not directly caused by lithium, hyperthyroidism increases lithium reuptake, which can result in toxicity. Lithium also interferes with calcium sensing, which can lead to hyperparathyroidism.[15]Hypercalcemia can cause osmotic diuresis, resulting in volume depletion.[2]\nThe manifestations of lithium toxicity range from a lack of symptoms to profound neurotoxicity.[2] Common symptoms include gastrointestinal (GI) distress (nausea, vomiting), muscle weakness, slurred speech, tremor, nystagmus, and ataxia. More severe intoxication can cause seizures, hyperthermia, delirium, and coma.\nThe workup includes obtaining and trending lithium levels and evaluation of electrolyte levels, kidney function, and thyroid function. Lithium levels should not be drawn in tubes containing lithium heparin because this can falsely elevate the level.[16] Acetaminophen, salicylate, and ethanol levels should also be obtained in case of possible co-ingestion. An ECG may reveal nonspecific T-wave abnormalities, QTc prolongation, or bradycardia. Hypotension can occur in severe cases.[3]\nTreatment of lithium toxicity is aimed at preventing absorption and promoting elimination to lower serum levels and improve clinical symptoms. The first step in preventing absorption is to hold the patient's lithium and discontinue medications that can lead to increased lithium levels through impairment of kidney function. Although activated charcoal is useful in many types of overdoses, it has no role in lithium toxicity owing to its limited ability to bind metals.[17] In cases of severe toxicity or toxicity from sustained-release formulations, whole-bowel irrigation with polyethylene glycol electrolyte solution (PEG-ES) can be considered to speed transit through the GI tract in an effort to limit absorption.[18] The recommended regimen is 1-2 L/h of PEG-ES via nasogastric tube until the rectal effluent is clear.[2]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Delirious, Incontinent 45-Year-Old Found Crawling on the Floor"
},
{
"authors": "Ryan J. Cole, MD; Christopher P. Holstege, MD",
"content": [
"Once efforts to limit absorption have been undertaken, the focus shifts to enhancing elimination. The exclusive elimination of lithium via the kidneys forms the cornerstone of treatment. Most patients can be managed conservatively with intravenous (IV) normal saline, which provides a sodium load in addition to hydration. If hyponatremia is present, the body retains sodium, resulting in lithium reabsorption. Maintaining sodium at the upper limit of normal is essential to ensure adequate elimination. Kidney function and urine output should be monitored, along with lithium levels, to confirm a continued downtrend.",
"In cases of severe toxicity, hemodialysis may be required for lithium removal. Properties of lithium that make it amenable to dialysis include low molecular weight, low volume of distribution, and low protein binding. Hemodialysis can increase the clearance of lithium four- to tenfold.[19] Expert consensus guidelines from the Extracorporeal Treatments in Poisoning (EXTRIP) Workgroup recommend dialysis when kidney function is impaired and the lithium level is > 4 mEq/L or when mental status changes, seizures, or life-threatening arrhythmias are present, regardless of the lithium level. Other considerations include a lithium level > 5 mEq/L, the presence of significant confusion, or if the time expected to reduce the lithium level to < 1 mEq/L is more than 36 hours.",
"Dialysis should continue until the lithium level is < 1 mEq/L or clinical improvement is noted. Intermittent hemodialysis is the preferred method for removal.[20] If hemodialysis is unavailable, continuous renal replacement therapy is an alternative, but it is approximately three times less efficient than hemodialysis.[20,21,22] After dialysis, a rebound effect may occur, either from continued GI absorption or from redistribution of lithium out of the tissues into the blood compartment. Symptoms may return during rebound, and redistribution into the tissues will occur if lithium is not removed.[20]",
"The patient in this case was given indomethacin 50 mg orally every 8 hours. This resulted in an increase in urine osmolality within hours of administration. Hydration was continued with IV normal saline, and the sodium level was kept within the higher range of normal to facilitate lithium excretion. Over the next 3 days, lithium levels trended down into the therapeutic range, and the patient's mental status, tremor, and ataxia gradually improved. In discussions with the psychiatry service, it was decided that the benefits of maintaining the patient on lithium for mood stabilization outweighed the risks for future episodes of chronic toxicity."
],
"date": "September 01, 2022",
"figures": [],
"markdown": "# Delirious, Incontinent 45-Year-Old Found Crawling on the Floor\n\n **Authors:** Ryan J. Cole, MD; Christopher P. Holstege, MD \n **Date:** September 01, 2022\n\n ## Content\n\n Once efforts to limit absorption have been undertaken, the focus shifts to enhancing elimination. The exclusive elimination of lithium via the kidneys forms the cornerstone of treatment. Most patients can be managed conservatively with intravenous (IV) normal saline, which provides a sodium load in addition to hydration. If hyponatremia is present, the body retains sodium, resulting in lithium reabsorption. Maintaining sodium at the upper limit of normal is essential to ensure adequate elimination. Kidney function and urine output should be monitored, along with lithium levels, to confirm a continued downtrend.\nIn cases of severe toxicity, hemodialysis may be required for lithium removal. Properties of lithium that make it amenable to dialysis include low molecular weight, low volume of distribution, and low protein binding. Hemodialysis can increase the clearance of lithium four- to tenfold.[19] Expert consensus guidelines from the Extracorporeal Treatments in Poisoning (EXTRIP) Workgroup recommend dialysis when kidney function is impaired and the lithium level is > 4 mEq/L or when mental status changes, seizures, or life-threatening arrhythmias are present, regardless of the lithium level. Other considerations include a lithium level > 5 mEq/L, the presence of significant confusion, or if the time expected to reduce the lithium level to < 1 mEq/L is more than 36 hours.\nDialysis should continue until the lithium level is < 1 mEq/L or clinical improvement is noted. Intermittent hemodialysis is the preferred method for removal.[20] If hemodialysis is unavailable, continuous renal replacement therapy is an alternative, but it is approximately three times less efficient than hemodialysis.[20,21,22] After dialysis, a rebound effect may occur, either from continued GI absorption or from redistribution of lithium out of the tissues into the blood compartment. Symptoms may return during rebound, and redistribution into the tissues will occur if lithium is not removed.[20]\nThe patient in this case was given indomethacin 50 mg orally every 8 hours. This resulted in an increase in urine osmolality within hours of administration. Hydration was continued with IV normal saline, and the sodium level was kept within the higher range of normal to facilitate lithium excretion. Over the next 3 days, lithium levels trended down into the therapeutic range, and the patient's mental status, tremor, and ataxia gradually improved. In discussions with the psychiatry service, it was decided that the benefits of maintaining the patient on lithium for mood stabilization outweighed the risks for future episodes of chronic toxicity.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1713461,
"choiceText": "Strict intake and output documentation",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713462,
"choiceText": "Activated charcoal",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713463,
"choiceText": "Furosemide diuresis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713464,
"choiceText": "Sodium bicarbonate infusion",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713465,
"choiceText": "Deferoxamine chelation",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Nephrogenic DI is the most common adverse effect observed in patients who are receiving long-term lithium therapy.<sup>[10,11] </sup>Lithium interferes with the kidney's ability to concentrate urine owing to a loss of responsiveness to vasopressin. When a patient presents with lithium toxicity, it is imperative that the care team follow strict intake and output documentation so that nephrogenic DI is not missed.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 552512,
"questionText": "When a patient presents with lithium intoxication, which is most imperative to order?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1713478,
"choiceText": "Miosis, respiratory depression, and CNS depression",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713479,
"choiceText": "Salivation, lacrimation, vomiting, diarrhea, diaphoresis, and miosis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713480,
"choiceText": "Cerebellar dysfunction, extrapyramidal symptoms, brainstem dysfunction, and dementia",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713481,
"choiceText": "Tachycardia, agitation, lack of sweat, mydriasis, and urinary retention",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "SILENT typically presents with persistent symptoms of cerebellar dysfunction, extrapyramidal symptoms, brainstem dysfunction, and dementia. The diagnosis is made by the causation of symptoms by lithium in the absence of prior neurologic illness and the persistence of neurologic findings for 2 months after lithium therapy is discontinued. Although symptoms may resolve spontaneously, most last for long periods and are irreversible.<sup>[7]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 552516,
"questionText": "SILENT is an irreversible syndrome of neurotoxicity that has been described with lithium use. It typically presents with which symptoms?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Delirious, Incontinent 45-Year-Old Found Crawling on the Floor"
},
{
"authors": "Ryan J. Cole, MD; Christopher P. Holstege, MD",
"content": [
"Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult."
],
"date": "September 01, 2022",
"figures": [],
"markdown": "# Delirious, Incontinent 45-Year-Old Found Crawling on the Floor\n\n **Authors:** Ryan J. Cole, MD; Christopher P. Holstege, MD \n **Date:** September 01, 2022\n\n ## Content\n\n Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult.\n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1713461,
"choiceText": "Strict intake and output documentation",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713462,
"choiceText": "Activated charcoal",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713463,
"choiceText": "Furosemide diuresis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713464,
"choiceText": "Sodium bicarbonate infusion",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713465,
"choiceText": "Deferoxamine chelation",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Nephrogenic DI is the most common adverse effect observed in patients who are receiving long-term lithium therapy.<sup>[10,11] </sup>Lithium interferes with the kidney's ability to concentrate urine owing to a loss of responsiveness to vasopressin. When a patient presents with lithium toxicity, it is imperative that the care team follow strict intake and output documentation so that nephrogenic DI is not missed.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 552512,
"questionText": "When a patient presents with lithium intoxication, which is most imperative to order?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1713478,
"choiceText": "Miosis, respiratory depression, and CNS depression",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713479,
"choiceText": "Salivation, lacrimation, vomiting, diarrhea, diaphoresis, and miosis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713480,
"choiceText": "Cerebellar dysfunction, extrapyramidal symptoms, brainstem dysfunction, and dementia",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713481,
"choiceText": "Tachycardia, agitation, lack of sweat, mydriasis, and urinary retention",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "SILENT typically presents with persistent symptoms of cerebellar dysfunction, extrapyramidal symptoms, brainstem dysfunction, and dementia. The diagnosis is made by the causation of symptoms by lithium in the absence of prior neurologic illness and the persistence of neurologic findings for 2 months after lithium therapy is discontinued. Although symptoms may resolve spontaneously, most last for long periods and are irreversible.<sup>[7]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 552516,
"questionText": "SILENT is an irreversible syndrome of neurotoxicity that has been described with lithium use. It typically presents with which symptoms?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Delirious, Incontinent 45-Year-Old Found Crawling on the Floor"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1713453,
"choiceText": "Lithium-induced hyperthyroidism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713454,
"choiceText": "Lithium-induced hypothyroidism",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713455,
"choiceText": "Lithium-induced nephrogenic diabetes insipidus",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713456,
"choiceText": "Lithium-induced hyperparathyroidism",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 552510,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1713461,
"choiceText": "Strict intake and output documentation",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713462,
"choiceText": "Activated charcoal",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713463,
"choiceText": "Furosemide diuresis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713464,
"choiceText": "Sodium bicarbonate infusion",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713465,
"choiceText": "Deferoxamine chelation",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Nephrogenic DI is the most common adverse effect observed in patients who are receiving long-term lithium therapy.<sup>[10,11] </sup>Lithium interferes with the kidney's ability to concentrate urine owing to a loss of responsiveness to vasopressin. When a patient presents with lithium toxicity, it is imperative that the care team follow strict intake and output documentation so that nephrogenic DI is not missed.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 552512,
"questionText": "When a patient presents with lithium intoxication, which is most imperative to order?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1713478,
"choiceText": "Miosis, respiratory depression, and CNS depression",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713479,
"choiceText": "Salivation, lacrimation, vomiting, diarrhea, diaphoresis, and miosis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713480,
"choiceText": "Cerebellar dysfunction, extrapyramidal symptoms, brainstem dysfunction, and dementia",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1713481,
"choiceText": "Tachycardia, agitation, lack of sweat, mydriasis, and urinary retention",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "SILENT typically presents with persistent symptoms of cerebellar dysfunction, extrapyramidal symptoms, brainstem dysfunction, and dementia. The diagnosis is made by the causation of symptoms by lithium in the absence of prior neurologic illness and the persistence of neurologic findings for 2 months after lithium therapy is discontinued. Although symptoms may resolve spontaneously, most last for long periods and are irreversible.<sup>[7]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 552516,
"questionText": "SILENT is an irreversible syndrome of neurotoxicity that has been described with lithium use. It typically presents with which symptoms?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
889050 | /viewarticle/889050 | [
{
"authors": "Francesco Brigo, MD; Giampaolo Tomelleri, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 57-year-old man presents to the emergency department with left-sided facial, arm, and leg weakness along with slurred speech after suffering violent and repetitive bouts of coughing. His wife also suggests that his right eye is smaller than the left. The patient complains of pain over his right eye.",
"His medical history is notable for hypertension and smoking one pack of cigarettes per day for 10 years. He denies any illicit drug use. He does not consume alcohol. He is employed, does not exercise, and has a sedentary lifestyle. He has no history of previous head or neck injury."
],
"date": "August 23, 2022",
"figures": [],
"markdown": "# Violent Cough, Slurred Speech, and Ptosis in a Middle-Aged Man\n\n **Authors:** Francesco Brigo, MD; Giampaolo Tomelleri, MD \n **Date:** August 23, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 57-year-old man presents to the emergency department with left-sided facial, arm, and leg weakness along with slurred speech after suffering violent and repetitive bouts of coughing. His wife also suggests that his right eye is smaller than the left. The patient complains of pain over his right eye.\nHis medical history is notable for hypertension and smoking one pack of cigarettes per day for 10 years. He denies any illicit drug use. He does not consume alcohol. He is employed, does not exercise, and has a sedentary lifestyle. He has no history of previous head or neck injury.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Violent Cough, Slurred Speech, and Ptosis in a Middle-Aged Man"
},
{
"authors": "Francesco Brigo, MD; Giampaolo Tomelleri, MD",
"content": [
"Upon physical examination, his oral temperature is 97.3°F (36.3°C). His pulse is regular with a rate of 94 beats/min. His blood pressure is 195/105 mm Hg. Head and neck findings are normal. His lungs are clear to auscultation and have normal respiratory effort. No cardiac murmurs are detected. His abdomen is soft and nontender, with normal bowel sounds on auscultation.",
"Upon neurologic examination, the patient is alert and oriented to time and place. His speech is slurred and dysarthric. Upon cranial nerve examination, the right pupil constricts from 2 mm to 1.5 mm in response to light, whereas the left pupil constricts from 3 mm to 2 mm. The right eyelid has 3 mm of ptosis compared with the left eye, and the right eye appears to be smaller than the left. Pupillary asymmetry is more apparent when lights in the room are dimmed. Funduscopic examination reveals normal fundi. Visual acuity is normal bilaterally. The extraocular movements are intact.",
"Facial sensation is decreased to light touch and pinprick on the left side. The patient has a decreased left nasolabial fold. He has weak movements of the left side of the face, without forehead involvement. The gag reflex is present, and normal palate elevation is observed. After pinching the left side of the neck, the left pupil dilates normally (ciliospinal reflex). After pinching the right side of the neck, the right pupil does not dilate. He is unable to stand and walk. Muscular tone is flaccid on the left side but normal on the right. He has marked left hemiparesis.",
"The patient's reflexes are normal throughout, except for an upgoing plantar response on the left side, compared with a downgoing one on the right. The patient reports decreased sensation to light touch, temperature, pinprick, joint position, and vibration on the left half of the body. His National Institute of Health Stroke Scale (NIHSS) score is 11.",
"Routine laboratory analyses are performed, and results are normal. Chest x-ray findings are normal. ECG shows left ventricular hypertrophy. A noncontrast CT scan of the head reveals a hyperdense right middle cerebral artery (Figure 1).",
"Figure 1.",
"Conventional angiography reveals stenosis at the origin of the right internal carotid artery, with an abrupt narrowing of its lumen (\"rattail-filling defect\"; Figure 2).",
"Figure 2."
],
"date": "August 23, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/889/050/889050-Thumb1.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/889/050/889050-Thumb2.jpg"
}
],
"markdown": "# Violent Cough, Slurred Speech, and Ptosis in a Middle-Aged Man\n\n **Authors:** Francesco Brigo, MD; Giampaolo Tomelleri, MD \n **Date:** August 23, 2022\n\n ## Content\n\n Upon physical examination, his oral temperature is 97.3°F (36.3°C). His pulse is regular with a rate of 94 beats/min. His blood pressure is 195/105 mm Hg. Head and neck findings are normal. His lungs are clear to auscultation and have normal respiratory effort. No cardiac murmurs are detected. His abdomen is soft and nontender, with normal bowel sounds on auscultation.\nUpon neurologic examination, the patient is alert and oriented to time and place. His speech is slurred and dysarthric. Upon cranial nerve examination, the right pupil constricts from 2 mm to 1.5 mm in response to light, whereas the left pupil constricts from 3 mm to 2 mm. The right eyelid has 3 mm of ptosis compared with the left eye, and the right eye appears to be smaller than the left. Pupillary asymmetry is more apparent when lights in the room are dimmed. Funduscopic examination reveals normal fundi. Visual acuity is normal bilaterally. The extraocular movements are intact.\nFacial sensation is decreased to light touch and pinprick on the left side. The patient has a decreased left nasolabial fold. He has weak movements of the left side of the face, without forehead involvement. The gag reflex is present, and normal palate elevation is observed. After pinching the left side of the neck, the left pupil dilates normally (ciliospinal reflex). After pinching the right side of the neck, the right pupil does not dilate. He is unable to stand and walk. Muscular tone is flaccid on the left side but normal on the right. He has marked left hemiparesis.\nThe patient's reflexes are normal throughout, except for an upgoing plantar response on the left side, compared with a downgoing one on the right. The patient reports decreased sensation to light touch, temperature, pinprick, joint position, and vibration on the left half of the body. His National Institute of Health Stroke Scale (NIHSS) score is 11.\nRoutine laboratory analyses are performed, and results are normal. Chest x-ray findings are normal. ECG shows left ventricular hypertrophy. A noncontrast CT scan of the head reveals a hyperdense right middle cerebral artery (Figure 1).\nFigure 1.\nConventional angiography reveals stenosis at the origin of the right internal carotid artery, with an abrupt narrowing of its lumen (\"rattail-filling defect\"; Figure 2).\nFigure 2.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1160278,
"choiceText": "Right internal carotid artery dissection",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160280,
"choiceText": "Complete occlusion of right internal carotid artery due to atherosclerosis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160282,
"choiceText": "Embolic stroke",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160284,
"choiceText": "Traumatic injury to the sympathetic chain in the right neck",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 368681,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Violent Cough, Slurred Speech, and Ptosis in a Middle-Aged Man"
},
{
"authors": "Francesco Brigo, MD; Giampaolo Tomelleri, MD",
"content": [
"The patient in this case presented with a pattern of sensory loss and weakness on the left side of his body consistent with a lesion involving the right corticospinal and corticobulbar fibers and the primary somatosensory cortex. The most likely diagnosis was an ischemic stroke.",
"Neurologic examination also revealed ptosis of the right eye with narrowing of the palpebral aperture, miosis in the right eye with a pupil that was reactive to light, and reduced ciliospinal reflex on pinching the right side of the neck. These signs are consistent with a partial Horner syndrome resulting from injury to sympathetic fibers traveling with the internal carotid artery. The sudden onset of neurologic deficits after violent coughing and the presence of pain over the patient's right eye are highly suggestive of a right internal carotid artery dissection.",
"Conventional angiography was performed because the clinical findings were highly suspicious for an internal carotid artery dissection; this confirmed the diagnosis by showing an abrupt narrowing of the vessel's lumen (\"rattail-filling defect\"). The hyperdense middle cerebral artery revealed by noncontrast CT scan of the head suggested an occlusion of this artery. Laboratory analysis performed during hospitalization revealed the presence of mild hyperlipidemia. Screening analyses for hypercoagulability and rheumatologic disorders were normal. Transthoracic echocardiography was normal; however, duplex ultrasonographic imaging showed a stenosis in the right internal carotid artery.",
"Dissection of the internal carotid artery is an important cause of cerebrovascular disease in young adults. One study out of Rochester, Minnesota, showed an annual incidence of 2.6 patients out of 100,000 population. The actual incidence is difficult to evaluate, however, and may be higher because this condition, which may be asymptomatic or have various clinical presentations, may go unrecognized.[1] The incidence appears to have increased since the 1980s, but that is likely due to the availability of better imaging studies.[1]"
],
"date": "August 23, 2022",
"figures": [],
"markdown": "# Violent Cough, Slurred Speech, and Ptosis in a Middle-Aged Man\n\n **Authors:** Francesco Brigo, MD; Giampaolo Tomelleri, MD \n **Date:** August 23, 2022\n\n ## Content\n\n The patient in this case presented with a pattern of sensory loss and weakness on the left side of his body consistent with a lesion involving the right corticospinal and corticobulbar fibers and the primary somatosensory cortex. The most likely diagnosis was an ischemic stroke.\nNeurologic examination also revealed ptosis of the right eye with narrowing of the palpebral aperture, miosis in the right eye with a pupil that was reactive to light, and reduced ciliospinal reflex on pinching the right side of the neck. These signs are consistent with a partial Horner syndrome resulting from injury to sympathetic fibers traveling with the internal carotid artery. The sudden onset of neurologic deficits after violent coughing and the presence of pain over the patient's right eye are highly suggestive of a right internal carotid artery dissection.\nConventional angiography was performed because the clinical findings were highly suspicious for an internal carotid artery dissection; this confirmed the diagnosis by showing an abrupt narrowing of the vessel's lumen (\"rattail-filling defect\"). The hyperdense middle cerebral artery revealed by noncontrast CT scan of the head suggested an occlusion of this artery. Laboratory analysis performed during hospitalization revealed the presence of mild hyperlipidemia. Screening analyses for hypercoagulability and rheumatologic disorders were normal. Transthoracic echocardiography was normal; however, duplex ultrasonographic imaging showed a stenosis in the right internal carotid artery.\nDissection of the internal carotid artery is an important cause of cerebrovascular disease in young adults. One study out of Rochester, Minnesota, showed an annual incidence of 2.6 patients out of 100,000 population. The actual incidence is difficult to evaluate, however, and may be higher because this condition, which may be asymptomatic or have various clinical presentations, may go unrecognized.[1] The incidence appears to have increased since the 1980s, but that is likely due to the availability of better imaging studies.[1]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1160278,
"choiceText": "Right internal carotid artery dissection",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160280,
"choiceText": "Complete occlusion of right internal carotid artery due to atherosclerosis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160282,
"choiceText": "Embolic stroke",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160284,
"choiceText": "Traumatic injury to the sympathetic chain in the right neck",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 368681,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Violent Cough, Slurred Speech, and Ptosis in a Middle-Aged Man"
},
{
"authors": "Francesco Brigo, MD; Giampaolo Tomelleri, MD",
"content": [
"Dissection normally occurs in the extracranial segment of the epiaortic vessels. The internal carotid artery is affected more often than the vertebral artery.[2] Dissections can be classified as traumatic or spontaneous. Traumatic dissections are linked to direct neck trauma or injury, whereas spontaneous dissections may be secondary to predisposing factors, such as fibromuscular dysplasia, Ehlers-Danlos syndrome, cystic medial necrosis, or Marfan syndrome. These conditions cause an abnormal, weakened arterial wall, thus predisposing patients to arterial dissection.[3]",
"Internal carotid artery dissection develops as a consequence of a tear in the intimal layer of the vessel, which allows blood to enter the wall of the artery and to split its layers; this is termed a subintimal hematoma. This means that the hematoma is located between the intimal and medial layers of the artery. Alternatively, a rupture of the vasa vasorum causes a subadventitial hematoma (ie, a hematoma between the media and the adventitial layers). Internal carotid artery dissection can lead to thrombus formation and the risk for distal embolization, whereas arterial narrowing with stroke due to inadequate blood flow is a less common mechanism of ischemia.[4] Hematoma formation and a localized inflammatory response result in compression of nearby structures, such as the sympathetic fibers of the superior cervical ganglion, which lies in the posterior wall of the carotid sheath. This can cause a postganglionic oculosympathetic palsy. Anhidrosis is not present because sweat fibers run with the uninvolved external carotid artery.",
"A highly suggestive constellation of signs and symptoms frequently seen with internal carotid artery dissection is Horner syndrome. Oculosympathetic palsy in the form of Horner syndrome has long been recognized as a typical manifestation of internal carotid artery dissection, although it is found in fewer than half of patients. The classic signs of Horner syndrome include ptosis of the upper lid, slight elevation of the lower lid (upside-down ptosis), and miosis reactive to light. The narrow palpebral aperture secondary to upper-lid ptosis and elevation of the lower lid give the illusion that the affected eye is smaller than the contralateral eye (illusory enophthalmos).",
"Horner syndrome is an expression of a disruption of oculosympathetic pathways. Ptosis (ie, upper eyelid droop) is caused by a loss of innervation to Müller smooth muscle in the upper lid. This small muscle is innervated by sympathetic fibers and is responsible for eye opening, together with the superior and levator palpebrae: striated skeletal muscle innervated by the third cranial nerve. Similarly, miosis (ie, decreased pupillary size) is caused by a loss of sympathetic innervation to the iris pupillodilator muscle. As a consequence, the pupil cannot dilate. This impaired dilation of the pupil may also be observed in a test of the ciliospinal reflex. Normally, pinching the neck causes a pupillary dilation secondary to the activation of the sympathetic pathway. In an eye with Horner syndrome, this dilation does not occur.",
"The most typical signs and symptoms of internal carotid artery dissection are neck pain and/or a partial Horner syndrome. This may be followed by an ischemic event ipsilateral to the ocular signs, with somatosensory and/or motor deficits contralateral to ocular signs as a consequence of distal embolization to the intracerebral arteries.",
"Currently, the most commonly available imaging modalities are carotid ultrasonography and CT angiography (CTA) of the head and neck. However, the best method to diagnose an internal carotid artery dissection is a combination of CTA and magnetic resonance angiography (MRA) with fat-suppressed T1 images.[1,5,6] CTA and MRA are replacing conventional angiography in the diagnosis of internal carotid and vertebral artery dissection because the resolution and accuracy of CTA and MRA are similar to that of angiography.[7,8,9] Moreover, MRI may show the intramural hematoma itself.",
"A review comparing MRI/MRA with CTA showed the performance characteristics to be very similar for the diagnosis of carotid artery dissection.[10] As an alternative, conventional angiography with digital subtraction may be used, although these tests are more expensive and invasive than MRI/MRA. Additionally, MRI/MRA is superior to conventional angiography in diagnosing dissections without associated luminal abnormalities.[1] Conventional angiography may reveal an abrupt narrowing of the internal carotid artery lumen (rattail-filling defect or the \"string sign\"). Carotid duplex ultrasonographic imaging may also be useful, especially in the younger population with less chance of severe atherosclerotic disease, which can interfere in the diagnosis.[11] Direct observation of a luminal intimal flap is diagnostic but rare; the most frequent finding is a stenosed or occluded vessel in the absence of atheromatous lesions.[12]"
],
"date": "August 23, 2022",
"figures": [],
"markdown": "# Violent Cough, Slurred Speech, and Ptosis in a Middle-Aged Man\n\n **Authors:** Francesco Brigo, MD; Giampaolo Tomelleri, MD \n **Date:** August 23, 2022\n\n ## Content\n\n Dissection normally occurs in the extracranial segment of the epiaortic vessels. The internal carotid artery is affected more often than the vertebral artery.[2] Dissections can be classified as traumatic or spontaneous. Traumatic dissections are linked to direct neck trauma or injury, whereas spontaneous dissections may be secondary to predisposing factors, such as fibromuscular dysplasia, Ehlers-Danlos syndrome, cystic medial necrosis, or Marfan syndrome. These conditions cause an abnormal, weakened arterial wall, thus predisposing patients to arterial dissection.[3]\nInternal carotid artery dissection develops as a consequence of a tear in the intimal layer of the vessel, which allows blood to enter the wall of the artery and to split its layers; this is termed a subintimal hematoma. This means that the hematoma is located between the intimal and medial layers of the artery. Alternatively, a rupture of the vasa vasorum causes a subadventitial hematoma (ie, a hematoma between the media and the adventitial layers). Internal carotid artery dissection can lead to thrombus formation and the risk for distal embolization, whereas arterial narrowing with stroke due to inadequate blood flow is a less common mechanism of ischemia.[4] Hematoma formation and a localized inflammatory response result in compression of nearby structures, such as the sympathetic fibers of the superior cervical ganglion, which lies in the posterior wall of the carotid sheath. This can cause a postganglionic oculosympathetic palsy. Anhidrosis is not present because sweat fibers run with the uninvolved external carotid artery.\nA highly suggestive constellation of signs and symptoms frequently seen with internal carotid artery dissection is Horner syndrome. Oculosympathetic palsy in the form of Horner syndrome has long been recognized as a typical manifestation of internal carotid artery dissection, although it is found in fewer than half of patients. The classic signs of Horner syndrome include ptosis of the upper lid, slight elevation of the lower lid (upside-down ptosis), and miosis reactive to light. The narrow palpebral aperture secondary to upper-lid ptosis and elevation of the lower lid give the illusion that the affected eye is smaller than the contralateral eye (illusory enophthalmos).\nHorner syndrome is an expression of a disruption of oculosympathetic pathways. Ptosis (ie, upper eyelid droop) is caused by a loss of innervation to Müller smooth muscle in the upper lid. This small muscle is innervated by sympathetic fibers and is responsible for eye opening, together with the superior and levator palpebrae: striated skeletal muscle innervated by the third cranial nerve. Similarly, miosis (ie, decreased pupillary size) is caused by a loss of sympathetic innervation to the iris pupillodilator muscle. As a consequence, the pupil cannot dilate. This impaired dilation of the pupil may also be observed in a test of the ciliospinal reflex. Normally, pinching the neck causes a pupillary dilation secondary to the activation of the sympathetic pathway. In an eye with Horner syndrome, this dilation does not occur.\nThe most typical signs and symptoms of internal carotid artery dissection are neck pain and/or a partial Horner syndrome. This may be followed by an ischemic event ipsilateral to the ocular signs, with somatosensory and/or motor deficits contralateral to ocular signs as a consequence of distal embolization to the intracerebral arteries.\nCurrently, the most commonly available imaging modalities are carotid ultrasonography and CT angiography (CTA) of the head and neck. However, the best method to diagnose an internal carotid artery dissection is a combination of CTA and magnetic resonance angiography (MRA) with fat-suppressed T1 images.[1,5,6] CTA and MRA are replacing conventional angiography in the diagnosis of internal carotid and vertebral artery dissection because the resolution and accuracy of CTA and MRA are similar to that of angiography.[7,8,9] Moreover, MRI may show the intramural hematoma itself.\nA review comparing MRI/MRA with CTA showed the performance characteristics to be very similar for the diagnosis of carotid artery dissection.[10] As an alternative, conventional angiography with digital subtraction may be used, although these tests are more expensive and invasive than MRI/MRA. Additionally, MRI/MRA is superior to conventional angiography in diagnosing dissections without associated luminal abnormalities.[1] Conventional angiography may reveal an abrupt narrowing of the internal carotid artery lumen (rattail-filling defect or the \"string sign\"). Carotid duplex ultrasonographic imaging may also be useful, especially in the younger population with less chance of severe atherosclerotic disease, which can interfere in the diagnosis.[11] Direct observation of a luminal intimal flap is diagnostic but rare; the most frequent finding is a stenosed or occluded vessel in the absence of atheromatous lesions.[12]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Violent Cough, Slurred Speech, and Ptosis in a Middle-Aged Man"
},
{
"authors": "Francesco Brigo, MD; Giampaolo Tomelleri, MD",
"content": [
"The treatment of internal carotid artery dissection consists of anticoagulation with intravenous heparin followed by oral anticoagulation for 3-6 months.[13] However, no randomized controlled trials support such a therapeutic approach, and the validity of such treatment has never been definitively proven. A Cochrane review also reported that no randomized controlled trials have been conducted that directly compare the efficacy of anticoagulants and antiplatelet drugs; nonrandomized trials have shown no evidence of a significant difference between the two.[14]",
"Intravenous thrombolysis with recombinant tissue plasminogen activator has become a standard therapy for ischemic stroke; however, its use in patients with ischemic stroke due to internal carotid artery dissection may potentially worsen intramural hematoma. Nevertheless, studies indicate that the risks for intracranial bleeding and recurrent stroke after thrombolysis in patients with carotid artery dissection appear to be similar to those in patients without carotid artery dissection.[15,16]",
"Endovascular stenting is another emerging treatment for carotid artery dissection. In a systematic review of the literature, the technical success rate for stenting was 99%, and the procedural complication rate was 2%. Over a mean angiographic follow-up period of 12.8 months, 2% of patients had stent stenosis or occlusion; over a mean clinical follow-up period of 17.7 months, 1.4% of patients had a neurologic event.[17] Randomized, prospective clinical trials are needed to further elucidate the role of endovascular stenting and other strategies in the management of internal carotid artery dissection.[18,19,20,21]",
"The patient in this case was first treated with intravenous heparin followed by oral anticoagulation in order to prevent distal embolization. He continued anticoagulant therapy for 3 months. The patient's Horner syndrome completely resolved after 3 days, but the left-sided sensorimotor deficits persisted at discharge."
],
"date": "August 23, 2022",
"figures": [],
"markdown": "# Violent Cough, Slurred Speech, and Ptosis in a Middle-Aged Man\n\n **Authors:** Francesco Brigo, MD; Giampaolo Tomelleri, MD \n **Date:** August 23, 2022\n\n ## Content\n\n The treatment of internal carotid artery dissection consists of anticoagulation with intravenous heparin followed by oral anticoagulation for 3-6 months.[13] However, no randomized controlled trials support such a therapeutic approach, and the validity of such treatment has never been definitively proven. A Cochrane review also reported that no randomized controlled trials have been conducted that directly compare the efficacy of anticoagulants and antiplatelet drugs; nonrandomized trials have shown no evidence of a significant difference between the two.[14]\nIntravenous thrombolysis with recombinant tissue plasminogen activator has become a standard therapy for ischemic stroke; however, its use in patients with ischemic stroke due to internal carotid artery dissection may potentially worsen intramural hematoma. Nevertheless, studies indicate that the risks for intracranial bleeding and recurrent stroke after thrombolysis in patients with carotid artery dissection appear to be similar to those in patients without carotid artery dissection.[15,16]\nEndovascular stenting is another emerging treatment for carotid artery dissection. In a systematic review of the literature, the technical success rate for stenting was 99%, and the procedural complication rate was 2%. Over a mean angiographic follow-up period of 12.8 months, 2% of patients had stent stenosis or occlusion; over a mean clinical follow-up period of 17.7 months, 1.4% of patients had a neurologic event.[17] Randomized, prospective clinical trials are needed to further elucidate the role of endovascular stenting and other strategies in the management of internal carotid artery dissection.[18,19,20,21]\nThe patient in this case was first treated with intravenous heparin followed by oral anticoagulation in order to prevent distal embolization. He continued anticoagulant therapy for 3 months. The patient's Horner syndrome completely resolved after 3 days, but the left-sided sensorimotor deficits persisted at discharge.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1160286,
"choiceText": "MRI/MRA with fat-suppressed T1 images",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160288,
"choiceText": "Noncontrast CT scan of the head",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160290,
"choiceText": "Electroencephalogram",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160292,
"choiceText": "Skull x-ray",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160294,
"choiceText": "Standard angiography",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The clinical suspicion should be that of a left internal carotid artery dissection due to neck trauma secondary to chiropractic manipulation. The ideal imaging study is MRI/MRA with fat-suppressed T1 images, which is considered the standard tool in diagnosing an epiaortic vessel dissection. This method may also reveal early cerebral ischemic lesions through diffusion-weighted imaging. CTA of the neck is also an acceptable option. A noncontrast CT scan of the head can't reveal a vessel dissection. CTA or standard angiography may also be carried out when a vessel dissection is suspected. Compared with CTA or MRI/MRA, direct angiography is expensive, invasive, and a potentially harmful diagnostic tool.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 368683,
"questionText": "A 60-year-old man presents with Horner syndrome on the left side and pain over his left eye. A few days before presentation, he underwent a chiropractic neck manipulation. Which of the following imaging studies is indicated in order to confirm a carotid artery dissection?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1160296,
"choiceText": "Observation (“watchful waiting”)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160298,
"choiceText": "Lifelong oral anticoagulation therapy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160300,
"choiceText": "Statin therapy",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160302,
"choiceText": "Intravenous heparin followed by oral anticoagulation for 3-6 months with periodic MRI/MRA",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "No clear recommendations for the treatment of carotid artery dissection have been established, as stenting, antithrombotic therapy, and anticoagulation studies are under continued investigation. Anticoagulation with intravenous heparin followed by oral anticoagulation for 3-6 months based on MRI/MRA findings is one reasonable approach. After 3-6 months, anticoagulation is typically discontinued, and antiplatelet therapy is initiated. Statins are useful for atherosclerotic plaques and have pleiotropic effects but are not used in treating vessel dissection. An observation approach is unacceptable because internal carotid artery dissections may lead to severe neurologic deficits.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 368685,
"questionText": "If an internal carotid artery dissection is confirmed, which of these therapies is most reasonable?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Violent Cough, Slurred Speech, and Ptosis in a Middle-Aged Man"
},
{
"authors": "Francesco Brigo, MD; Giampaolo Tomelleri, MD",
"content": [],
"date": "August 23, 2022",
"figures": [],
"markdown": "# Violent Cough, Slurred Speech, and Ptosis in a Middle-Aged Man\n\n **Authors:** Francesco Brigo, MD; Giampaolo Tomelleri, MD \n **Date:** August 23, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1160286,
"choiceText": "MRI/MRA with fat-suppressed T1 images",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160288,
"choiceText": "Noncontrast CT scan of the head",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160290,
"choiceText": "Electroencephalogram",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160292,
"choiceText": "Skull x-ray",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160294,
"choiceText": "Standard angiography",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The clinical suspicion should be that of a left internal carotid artery dissection due to neck trauma secondary to chiropractic manipulation. The ideal imaging study is MRI/MRA with fat-suppressed T1 images, which is considered the standard tool in diagnosing an epiaortic vessel dissection. This method may also reveal early cerebral ischemic lesions through diffusion-weighted imaging. CTA of the neck is also an acceptable option. A noncontrast CT scan of the head can't reveal a vessel dissection. CTA or standard angiography may also be carried out when a vessel dissection is suspected. Compared with CTA or MRI/MRA, direct angiography is expensive, invasive, and a potentially harmful diagnostic tool.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 368683,
"questionText": "A 60-year-old man presents with Horner syndrome on the left side and pain over his left eye. A few days before presentation, he underwent a chiropractic neck manipulation. Which of the following imaging studies is indicated in order to confirm a carotid artery dissection?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1160296,
"choiceText": "Observation (“watchful waiting”)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160298,
"choiceText": "Lifelong oral anticoagulation therapy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160300,
"choiceText": "Statin therapy",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160302,
"choiceText": "Intravenous heparin followed by oral anticoagulation for 3-6 months with periodic MRI/MRA",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "No clear recommendations for the treatment of carotid artery dissection have been established, as stenting, antithrombotic therapy, and anticoagulation studies are under continued investigation. Anticoagulation with intravenous heparin followed by oral anticoagulation for 3-6 months based on MRI/MRA findings is one reasonable approach. After 3-6 months, anticoagulation is typically discontinued, and antiplatelet therapy is initiated. Statins are useful for atherosclerotic plaques and have pleiotropic effects but are not used in treating vessel dissection. An observation approach is unacceptable because internal carotid artery dissections may lead to severe neurologic deficits.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 368685,
"questionText": "If an internal carotid artery dissection is confirmed, which of these therapies is most reasonable?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Violent Cough, Slurred Speech, and Ptosis in a Middle-Aged Man"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1160278,
"choiceText": "Right internal carotid artery dissection",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160280,
"choiceText": "Complete occlusion of right internal carotid artery due to atherosclerosis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160282,
"choiceText": "Embolic stroke",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160284,
"choiceText": "Traumatic injury to the sympathetic chain in the right neck",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 368681,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1160286,
"choiceText": "MRI/MRA with fat-suppressed T1 images",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160288,
"choiceText": "Noncontrast CT scan of the head",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160290,
"choiceText": "Electroencephalogram",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160292,
"choiceText": "Skull x-ray",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160294,
"choiceText": "Standard angiography",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The clinical suspicion should be that of a left internal carotid artery dissection due to neck trauma secondary to chiropractic manipulation. The ideal imaging study is MRI/MRA with fat-suppressed T1 images, which is considered the standard tool in diagnosing an epiaortic vessel dissection. This method may also reveal early cerebral ischemic lesions through diffusion-weighted imaging. CTA of the neck is also an acceptable option. A noncontrast CT scan of the head can't reveal a vessel dissection. CTA or standard angiography may also be carried out when a vessel dissection is suspected. Compared with CTA or MRI/MRA, direct angiography is expensive, invasive, and a potentially harmful diagnostic tool.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 368683,
"questionText": "A 60-year-old man presents with Horner syndrome on the left side and pain over his left eye. A few days before presentation, he underwent a chiropractic neck manipulation. Which of the following imaging studies is indicated in order to confirm a carotid artery dissection?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1160296,
"choiceText": "Observation (“watchful waiting”)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160298,
"choiceText": "Lifelong oral anticoagulation therapy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160300,
"choiceText": "Statin therapy",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1160302,
"choiceText": "Intravenous heparin followed by oral anticoagulation for 3-6 months with periodic MRI/MRA",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "No clear recommendations for the treatment of carotid artery dissection have been established, as stenting, antithrombotic therapy, and anticoagulation studies are under continued investigation. Anticoagulation with intravenous heparin followed by oral anticoagulation for 3-6 months based on MRI/MRA findings is one reasonable approach. After 3-6 months, anticoagulation is typically discontinued, and antiplatelet therapy is initiated. Statins are useful for atherosclerotic plaques and have pleiotropic effects but are not used in treating vessel dissection. An observation approach is unacceptable because internal carotid artery dissections may lead to severe neurologic deficits.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 368685,
"questionText": "If an internal carotid artery dissection is confirmed, which of these therapies is most reasonable?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
979164 | /viewarticle/979164 | [
{
"authors": "Amber M. Bokhari, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians, but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please email us at [email protected] with the subject line \"Case Challenge Suggestion.\" We look forward to hearing from you.",
"A 50-year-old man presents with a 1-month history of oral thrush, skin rash, significant weight loss, diarrhea, and severe weakness. He has been febrile, with malaise, shortness of breath, and a dry cough for 5 days. He also has intermittent dull headaches and neck stiffness without any focal signs.",
"The patient is unhoused and has not sought medical care for decades. He has not been diagnosed with HIV infection, hepatitis, or any other condition. His clothes are soiled and in poor condition. During the past year, he has lost a significant amount of weight and appears cachectic. He has multiple sex partners and does not use any protection during sexual intercourse. He reports using crack cocaine but does not report intravenous (IV) drug use. When he is able to obtain cigarettes, he smokes about one pack a day."
],
"date": "May 06, 2024",
"figures": [],
"markdown": "# Severe Weakness After Unprotected Sex\n\n **Authors:** Amber M. Bokhari, MD \n **Date:** May 06, 2024\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians, but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please email us at [email protected] with the subject line \"Case Challenge Suggestion.\" We look forward to hearing from you.\nA 50-year-old man presents with a 1-month history of oral thrush, skin rash, significant weight loss, diarrhea, and severe weakness. He has been febrile, with malaise, shortness of breath, and a dry cough for 5 days. He also has intermittent dull headaches and neck stiffness without any focal signs.\nThe patient is unhoused and has not sought medical care for decades. He has not been diagnosed with HIV infection, hepatitis, or any other condition. His clothes are soiled and in poor condition. During the past year, he has lost a significant amount of weight and appears cachectic. He has multiple sex partners and does not use any protection during sexual intercourse. He reports using crack cocaine but does not report intravenous (IV) drug use. When he is able to obtain cigarettes, he smokes about one pack a day.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Severe Weakness After Unprotected Sex"
},
{
"authors": "Amber M. Bokhari, MD",
"content": [
"Upon examination, the patient is febrile, with a temperature of 101.6 °F (38.7 °C). He has a blood pressure of 120/80 mm Hg, a heart rate of 100 beats/min, a respiration rate of 23 breaths/min, and an oxygen saturation of 85%.",
"He is cachectic and has a rash on his body that consists of widespread small papules, some of which are umbilicated. Lesions are noted on the face, abdomen, thighs, arms, and back. Some of the papules coalesce to form plaques. He also has oral thrush, with a white-coated tongue that bleeds on scraping. The head and neck examination reveals some nuchal rigidity and cervical lymphadenopathy. Bilateral crackles and coarse rhonchi are noted on lung auscultation. The remainder of the physical examination results are unremarkable.",
"A complete blood cell (CBC) count reveals a white blood cell (WBC) count of 11,000 cells/µL (reference range, 4000-11,000 cells/µL), with predominantly elevated lymphocytes. The urinalysis results are normal. The results of a comprehensive metabolic panel are within normal limits.",
"A rapid plasma reagin test and hepatitis B and C tests are negative. An HIV antigen/antibody test is positive for HIV-1, and the results of a polymerase chain reaction (PCR) test are pending. The results of urine Neisseria gonorrhoeae/Chlamydia trachomatis nucleic acid amplification tests and a cytomegalovirus quantitative PCR test are negative. A 1,3-beta-D-glucan test is positive, at 450 pg/mL. The results of urine and serum cryptococcal antigen tests, a urine Histoplasma test, an Aspergillus galactomannan test, a Quantiferon-TB Gold test, a Mycobacterium tuberculosis (MTB) probe, and Toxoplasma serology and PCR tests are pending. Blood, sputum, stool, and urine cultures have been ordered and are in progress.",
"A lumbar puncture (LP) is performed, with an opening pressure of 200-cm H2O. Cerebrospinal fluid (CSF) cytology shows a glucose level of 70 mg/dL (reference range, 50-80 mg/dL), a protein level of 30 mg/dL (reference range, 20-40 mg/dL), and a lymphocyte count of 200 cells/µL (reference range, < 5 cells/µL). The results of CSF cultures, Venereal Disease Research Laboratory (VDRL) test, and cryptococcal antigen test are pending. A biopsy sample of a skin lesion is obtained. Bronchoscopy is performed, and bronchoalveolar lavage (BAL) fluid is sent for an MTB probe; Pneumocystis jirovecii (Pneumocystis carinii) pneumonia (PCP), fungal, acid-fast bacilli (AFB), and other bacterial staining and cultures; and silver staining. The PCP test is negative, and the other stains and cultures are in progress. Silver staining is negative. The serum cryptococcal antigen test is negative. Empiric treatment of toxoplasmosis is started with pyrimethamine and sulfadiazine.",
"A chest radiograph shows lymphadenopathy, bilateral interstitial infiltrates, multiple pulmonary nodules, and small pleural effusions. An MRI of the brain with contrast reveals lesions in the left frontal lobe. Figure 1 demonstrates lesions similar to those in this case."
],
"date": "May 06, 2024",
"figures": [],
"markdown": "# Severe Weakness After Unprotected Sex\n\n **Authors:** Amber M. Bokhari, MD \n **Date:** May 06, 2024\n\n ## Content\n\n Upon examination, the patient is febrile, with a temperature of 101.6 °F (38.7 °C). He has a blood pressure of 120/80 mm Hg, a heart rate of 100 beats/min, a respiration rate of 23 breaths/min, and an oxygen saturation of 85%.\nHe is cachectic and has a rash on his body that consists of widespread small papules, some of which are umbilicated. Lesions are noted on the face, abdomen, thighs, arms, and back. Some of the papules coalesce to form plaques. He also has oral thrush, with a white-coated tongue that bleeds on scraping. The head and neck examination reveals some nuchal rigidity and cervical lymphadenopathy. Bilateral crackles and coarse rhonchi are noted on lung auscultation. The remainder of the physical examination results are unremarkable.\nA complete blood cell (CBC) count reveals a white blood cell (WBC) count of 11,000 cells/µL (reference range, 4000-11,000 cells/µL), with predominantly elevated lymphocytes. The urinalysis results are normal. The results of a comprehensive metabolic panel are within normal limits.\nA rapid plasma reagin test and hepatitis B and C tests are negative. An HIV antigen/antibody test is positive for HIV-1, and the results of a polymerase chain reaction (PCR) test are pending. The results of urine Neisseria gonorrhoeae/Chlamydia trachomatis nucleic acid amplification tests and a cytomegalovirus quantitative PCR test are negative. A 1,3-beta-D-glucan test is positive, at 450 pg/mL. The results of urine and serum cryptococcal antigen tests, a urine Histoplasma test, an Aspergillus galactomannan test, a Quantiferon-TB Gold test, a Mycobacterium tuberculosis (MTB) probe, and Toxoplasma serology and PCR tests are pending. Blood, sputum, stool, and urine cultures have been ordered and are in progress.\nA lumbar puncture (LP) is performed, with an opening pressure of 200-cm H2O. Cerebrospinal fluid (CSF) cytology shows a glucose level of 70 mg/dL (reference range, 50-80 mg/dL), a protein level of 30 mg/dL (reference range, 20-40 mg/dL), and a lymphocyte count of 200 cells/µL (reference range, < 5 cells/µL). The results of CSF cultures, Venereal Disease Research Laboratory (VDRL) test, and cryptococcal antigen test are pending. A biopsy sample of a skin lesion is obtained. Bronchoscopy is performed, and bronchoalveolar lavage (BAL) fluid is sent for an MTB probe; Pneumocystis jirovecii (Pneumocystis carinii) pneumonia (PCP), fungal, acid-fast bacilli (AFB), and other bacterial staining and cultures; and silver staining. The PCP test is negative, and the other stains and cultures are in progress. Silver staining is negative. The serum cryptococcal antigen test is negative. Empiric treatment of toxoplasmosis is started with pyrimethamine and sulfadiazine.\nA chest radiograph shows lymphadenopathy, bilateral interstitial infiltrates, multiple pulmonary nodules, and small pleural effusions. An MRI of the brain with contrast reveals lesions in the left frontal lobe. Figure 1 demonstrates lesions similar to those in this case.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1711237,
"choiceText": "Toxoplasmosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711238,
"choiceText": "Disseminated Cryptococcus infection",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711239,
"choiceText": "Acute HIV infection",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711240,
"choiceText": "Molluscum contagiosum",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 551743,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Severe Weakness After Unprotected Sex"
},
{
"authors": "Amber M. Bokhari, MD",
"content": [
"The differential diagnosis for the patient in this case included toxoplasmosis, Cryptococcus infection, acute HIV infection, and molluscum contagiosum. Toxoplasmosis of the central nervous system (CNS) was excluded because of the absence of ring enhancement on the patient's MRI scan. In addition, no clinical improvement occurred during empiric treatment, which was discontinued after a negative Toxoplasma immunoglobulin G (IgG) assay. Toxoplasma IgG is found in 95% of patients with preexisting latent infection.",
"Acute HIV infection was ruled out owing to this patient's positive HIV antibody tests, which are negative in acute retroviral syndrome. This syndrome presents as acute mononucleosis because of very high viral loads, with fever, lymphadenopathy, rash, and sore throat; however, a mononucleosis spot test would be negative.",
"Other umbilicated lesions in patients with HIV infection include molluscum contagiosum or penicilliosis, which are confirmed on skin biopsy and by clinical appearance. Molluscum contagiosum is caused by a poxvirus, and histology will reveal eosinophilic cytoplasmic inclusion bodies. Treatment consists of local removal with cryotherapy, podophyllin application, or curettage. Molluscum contagiosum improves after highly active antiretroviral therapy (HAART) is initiated. The disseminated CNS, lung, and skin lesions in the patient in this case made molluscum contagiosum less likely, and the histopathology results ruled it out.",
"Cryptococcosis is caused by an endemic fungus, Cryptococcus neoformans or Cryptococcus gattii. Primary infection is in the lungs, but if the host immune system is weakened, it can result in fungemia and dissemination to the CNS and other extrapulmonary sites, including the skin, bones, joints, and prostate.",
"Immunocompromised hosts have more severe and disseminated disease, with pulmonary as well as extrapulmonary symptoms, most commonly due to reactivation of latent infection. This occurs in patients who have advanced HIV/AIDS, cancer treated with chemotherapy, hematopoietic stem cell transplant, solid organ transplant, chronic obstructive pulmonary disease, end-stage renal disease, diabetes, or who are receiving long-term glucocorticoid or immunosuppressive medications, including immune modulators such as tumor necrosis factor–alpha antagonists.[1]",
"Clinical manifestations include severe pulmonary cryptococcosis in patients who are HIV-positive with CD4 T-cell counts < 100 cells/µL. Patients present with fever, cough, shortness of breath, and headache. Disseminated CNS infection is very common in this patient population. It is important to rule out concurrent P jirovecii , Mycobacterium avium complex (MAC), M tuberculosis, cytomegalovirus, and Histoplasma capsulatum infections, which are also common in this patient population.[2]"
],
"date": "May 06, 2024",
"figures": [],
"markdown": "# Severe Weakness After Unprotected Sex\n\n **Authors:** Amber M. Bokhari, MD \n **Date:** May 06, 2024\n\n ## Content\n\n The differential diagnosis for the patient in this case included toxoplasmosis, Cryptococcus infection, acute HIV infection, and molluscum contagiosum. Toxoplasmosis of the central nervous system (CNS) was excluded because of the absence of ring enhancement on the patient's MRI scan. In addition, no clinical improvement occurred during empiric treatment, which was discontinued after a negative Toxoplasma immunoglobulin G (IgG) assay. Toxoplasma IgG is found in 95% of patients with preexisting latent infection.\nAcute HIV infection was ruled out owing to this patient's positive HIV antibody tests, which are negative in acute retroviral syndrome. This syndrome presents as acute mononucleosis because of very high viral loads, with fever, lymphadenopathy, rash, and sore throat; however, a mononucleosis spot test would be negative.\nOther umbilicated lesions in patients with HIV infection include molluscum contagiosum or penicilliosis, which are confirmed on skin biopsy and by clinical appearance. Molluscum contagiosum is caused by a poxvirus, and histology will reveal eosinophilic cytoplasmic inclusion bodies. Treatment consists of local removal with cryotherapy, podophyllin application, or curettage. Molluscum contagiosum improves after highly active antiretroviral therapy (HAART) is initiated. The disseminated CNS, lung, and skin lesions in the patient in this case made molluscum contagiosum less likely, and the histopathology results ruled it out.\nCryptococcosis is caused by an endemic fungus, Cryptococcus neoformans or Cryptococcus gattii. Primary infection is in the lungs, but if the host immune system is weakened, it can result in fungemia and dissemination to the CNS and other extrapulmonary sites, including the skin, bones, joints, and prostate.\nImmunocompromised hosts have more severe and disseminated disease, with pulmonary as well as extrapulmonary symptoms, most commonly due to reactivation of latent infection. This occurs in patients who have advanced HIV/AIDS, cancer treated with chemotherapy, hematopoietic stem cell transplant, solid organ transplant, chronic obstructive pulmonary disease, end-stage renal disease, diabetes, or who are receiving long-term glucocorticoid or immunosuppressive medications, including immune modulators such as tumor necrosis factor–alpha antagonists.[1]\nClinical manifestations include severe pulmonary cryptococcosis in patients who are HIV-positive with CD4 T-cell counts < 100 cells/µL. Patients present with fever, cough, shortness of breath, and headache. Disseminated CNS infection is very common in this patient population. It is important to rule out concurrent P jirovecii , Mycobacterium avium complex (MAC), M tuberculosis, cytomegalovirus, and Histoplasma capsulatum infections, which are also common in this patient population.[2]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1711237,
"choiceText": "Toxoplasmosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711238,
"choiceText": "Disseminated Cryptococcus infection",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711239,
"choiceText": "Acute HIV infection",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711240,
"choiceText": "Molluscum contagiosum",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 551743,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Severe Weakness After Unprotected Sex"
},
{
"authors": "Amber M. Bokhari, MD",
"content": [
"Diagnostic confirmation of pulmonary cryptococcal infection includes histopathologic examination of suspected lesions, fungal stains and culture, serum and BAL fluid cryptococcal antigen tests, and radiography. Figure 2 shows cryptococcosis in a human lung. If the results of diagnostic tests are positive and the patient is immunocompromised, they must be evaluated for disseminated infection. Dissemination to the CNS is most likely; thus, blood and CSF cultures and cryptococcal antigen testing should be ordered, as in this patient.",
"The serum cryptococcal antigen test is an excellent screening modality in immunocompromised hosts owing to a high sensitivity of over 70%. False-positive tests can occur with fungal infection with Trichosporon spp or bacterial infection with Stomatococcus or Capnocytophaga. False-negative tests are associated with the prozone effect owing to high antigenemia detected with an agglutination assay without prior treatment with pronase.",
"Sputum culture is often positive in immunocompromised patients, including those who have a solid organ transplant or HIV infection or who are receiving immune therapy. Performing a bronchoscopy is important in patients with advanced HIV infection to rule out other opportunistic infections, such as PCP, M tuberculosis infection, or MAC infection. A biopsy should be obtained for histopathologic confirmation of the diagnosis as well as to rule out cancer.",
"In immunocompromised hosts, including patients with advanced HIV/AIDS, chest radiography and other imaging modalities may show abnormalities such as bilateral alveolar lymphadenopathy, mass lesions, alveolar infiltrates, and pleural effusions. It is not unusual to see other opportunistic infections as well.",
"In patients with disseminated disease, neurologic symptoms, or a compromised immune system, as in the man in this case, LP is required to evaluate for possible cryptococcal meningoencephalitis. If the opening pressure is > 250-cm H2O, serial therapeutic LPs may be necessary to lower the intracranial pressure to < 200-cm H2O. If the intracranial pressure remains elevated, an LP shunt may be placed. Figure 3 shows cryptococcal disease in a human brain at light magnification.",
"Patients with mild to moderate pulmonary disease with few infiltrates can be treated effectively with oral fluconazole 400 mg or 6 mg/kg for a total duration of 6-12 months. Other azoles such as itraconazole, voriconazole, or posaconazole may be used if fluconazole is contraindicated or unavailable. However, severe pulmonary disease, disseminated cryptococcal infection, or a serum cryptococcal antigen titer ≥ 1:512 can be treated depending on the severity of the infection with IV induction vs an oral regimen.",
"Meningoencephalitis should be treated with a 2-week induction phase of liposomal amphotericin B 3-4 mg/kg IV every 24 hours plus oral flucytosine 25 mg/kg four times a day. This phase can be prolonged if cultures are not sterilized or the patient's condition fails to improve. The induction is followed by a 10-week consolidation phase with oral fluconazole 400 mg once daily. This phase is followed by maintenance or secondary prophylaxis with oral fluconazole 200 mg once daily until the immune system recovers with HAART in patients with HIV infection or with cessation of immunosuppressive therapy in patients with a solid organ transplant.[3]",
"Patients with HIV should continue chronic suppressive therapy with fluconazole 200 mg per day. HAART can be deferred until after 5 weeks of treatment to avoid clinical worsening due to immune reconstitution inflammatory syndrome. In patients with HIV infection who are receiving antiretroviral therapy and have a CD4 T-cell count > 100 cells/µL, with a suppressed viral load and a declining cryptococcal antigen titer, maintenance fluconazole can be discontinued after 1 year of treatment. However, no role has been established for monitoring serum cryptococcal antigen titers to determine the duration of therapy, and serial testing is not done.",
"Localized cryptococcal infections of the lung that are resistant to medical therapy or cryptococcomas in the brain parenchyma that cause mass effects may be surgically removed if necessary. Similarly, skin or joint lesions may be removed if they cause symptoms."
],
"date": "May 06, 2024",
"figures": [],
"markdown": "# Severe Weakness After Unprotected Sex\n\n **Authors:** Amber M. Bokhari, MD \n **Date:** May 06, 2024\n\n ## Content\n\n Diagnostic confirmation of pulmonary cryptococcal infection includes histopathologic examination of suspected lesions, fungal stains and culture, serum and BAL fluid cryptococcal antigen tests, and radiography. Figure 2 shows cryptococcosis in a human lung. If the results of diagnostic tests are positive and the patient is immunocompromised, they must be evaluated for disseminated infection. Dissemination to the CNS is most likely; thus, blood and CSF cultures and cryptococcal antigen testing should be ordered, as in this patient.\nThe serum cryptococcal antigen test is an excellent screening modality in immunocompromised hosts owing to a high sensitivity of over 70%. False-positive tests can occur with fungal infection with Trichosporon spp or bacterial infection with Stomatococcus or Capnocytophaga. False-negative tests are associated with the prozone effect owing to high antigenemia detected with an agglutination assay without prior treatment with pronase.\nSputum culture is often positive in immunocompromised patients, including those who have a solid organ transplant or HIV infection or who are receiving immune therapy. Performing a bronchoscopy is important in patients with advanced HIV infection to rule out other opportunistic infections, such as PCP, M tuberculosis infection, or MAC infection. A biopsy should be obtained for histopathologic confirmation of the diagnosis as well as to rule out cancer.\nIn immunocompromised hosts, including patients with advanced HIV/AIDS, chest radiography and other imaging modalities may show abnormalities such as bilateral alveolar lymphadenopathy, mass lesions, alveolar infiltrates, and pleural effusions. It is not unusual to see other opportunistic infections as well.\nIn patients with disseminated disease, neurologic symptoms, or a compromised immune system, as in the man in this case, LP is required to evaluate for possible cryptococcal meningoencephalitis. If the opening pressure is > 250-cm H2O, serial therapeutic LPs may be necessary to lower the intracranial pressure to < 200-cm H2O. If the intracranial pressure remains elevated, an LP shunt may be placed. Figure 3 shows cryptococcal disease in a human brain at light magnification.\nPatients with mild to moderate pulmonary disease with few infiltrates can be treated effectively with oral fluconazole 400 mg or 6 mg/kg for a total duration of 6-12 months. Other azoles such as itraconazole, voriconazole, or posaconazole may be used if fluconazole is contraindicated or unavailable. However, severe pulmonary disease, disseminated cryptococcal infection, or a serum cryptococcal antigen titer ≥ 1:512 can be treated depending on the severity of the infection with IV induction vs an oral regimen.\nMeningoencephalitis should be treated with a 2-week induction phase of liposomal amphotericin B 3-4 mg/kg IV every 24 hours plus oral flucytosine 25 mg/kg four times a day. This phase can be prolonged if cultures are not sterilized or the patient's condition fails to improve. The induction is followed by a 10-week consolidation phase with oral fluconazole 400 mg once daily. This phase is followed by maintenance or secondary prophylaxis with oral fluconazole 200 mg once daily until the immune system recovers with HAART in patients with HIV infection or with cessation of immunosuppressive therapy in patients with a solid organ transplant.[3]\nPatients with HIV should continue chronic suppressive therapy with fluconazole 200 mg per day. HAART can be deferred until after 5 weeks of treatment to avoid clinical worsening due to immune reconstitution inflammatory syndrome. In patients with HIV infection who are receiving antiretroviral therapy and have a CD4 T-cell count > 100 cells/µL, with a suppressed viral load and a declining cryptococcal antigen titer, maintenance fluconazole can be discontinued after 1 year of treatment. However, no role has been established for monitoring serum cryptococcal antigen titers to determine the duration of therapy, and serial testing is not done.\nLocalized cryptococcal infections of the lung that are resistant to medical therapy or cryptococcomas in the brain parenchyma that cause mass effects may be surgically removed if necessary. Similarly, skin or joint lesions may be removed if they cause symptoms.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Severe Weakness After Unprotected Sex"
},
{
"authors": "Amber M. Bokhari, MD",
"content": [
"The patient in this case had newly diagnosed HIV/AIDS, with a CD4 T-cell count of 32 cells/µL and an HIV viral load of 459,000 copies/mL. His serum cryptococcal antigen test was initially negative, but when the laboratory repeated the test with latex agglutination and pretreated with pronase, the serum cryptococcal antigen titer was ≥ 1:512. This in itself was a poor prognostic factor.",
"The urine Histoplasma antigen test, Aspergillus galactomannan test, Quantiferon-TB Gold test, MTB probe, and Toxoplasma serology and PCR tests were negative. Blood and sputum cultures grew C neoformans. Stool and urine cultures showed no growth.",
"The CSF cultures were positive for C neoformans, and the CSF cryptococcal antigen titer was > 1:512. Biopsy of the skin lesion revealed encapsulated yeast forms identified as C neoformans. The CSF VDRL test was negative. The BAL fluid MTB probe and PCP test were negative, and AFB and other bacterial staining and cultures showed no growth. The BAL fungal cultures grew C neoformans.",
"Because this patient had evidence of severe disseminated Cryptococcus infection, he was treated with an induction phase of 2 weeks with liposomal amphotericin B 3-4 mg/kg IV every 24 hours plus oral flucytosine 25 mg/kg four times a day. The induction phase was prolonged for another 2 weeks because he showed slow clinical improvement with gradual resolution of his headaches. The induction phase was followed by a 10-week consolidation phase with oral fluconazole 400 mg once daily. During the sixth week of therapy, a bictegravir-based one-pill regimen was started, as his HIV-1 was pansensitive on GenoSure PRIme.",
"After 10 weeks, the patient was switched to maintenance therapy with oral fluconazole 200 mg once daily for 1 year. His CD4 counts remained > 200 cells/µL, and his viral load was undetectable during this phase. Repeat cryptococcal antigen titers remained < 100.[45]"
],
"date": "May 06, 2024",
"figures": [],
"markdown": "# Severe Weakness After Unprotected Sex\n\n **Authors:** Amber M. Bokhari, MD \n **Date:** May 06, 2024\n\n ## Content\n\n The patient in this case had newly diagnosed HIV/AIDS, with a CD4 T-cell count of 32 cells/µL and an HIV viral load of 459,000 copies/mL. His serum cryptococcal antigen test was initially negative, but when the laboratory repeated the test with latex agglutination and pretreated with pronase, the serum cryptococcal antigen titer was ≥ 1:512. This in itself was a poor prognostic factor.\nThe urine Histoplasma antigen test, Aspergillus galactomannan test, Quantiferon-TB Gold test, MTB probe, and Toxoplasma serology and PCR tests were negative. Blood and sputum cultures grew C neoformans. Stool and urine cultures showed no growth.\nThe CSF cultures were positive for C neoformans, and the CSF cryptococcal antigen titer was > 1:512. Biopsy of the skin lesion revealed encapsulated yeast forms identified as C neoformans. The CSF VDRL test was negative. The BAL fluid MTB probe and PCP test were negative, and AFB and other bacterial staining and cultures showed no growth. The BAL fungal cultures grew C neoformans.\nBecause this patient had evidence of severe disseminated Cryptococcus infection, he was treated with an induction phase of 2 weeks with liposomal amphotericin B 3-4 mg/kg IV every 24 hours plus oral flucytosine 25 mg/kg four times a day. The induction phase was prolonged for another 2 weeks because he showed slow clinical improvement with gradual resolution of his headaches. The induction phase was followed by a 10-week consolidation phase with oral fluconazole 400 mg once daily. During the sixth week of therapy, a bictegravir-based one-pill regimen was started, as his HIV-1 was pansensitive on GenoSure PRIme.\nAfter 10 weeks, the patient was switched to maintenance therapy with oral fluconazole 200 mg once daily for 1 year. His CD4 counts remained > 200 cells/µL, and his viral load was undetectable during this phase. Repeat cryptococcal antigen titers remained < 100.[45]\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1711241,
"choiceText": "Advanced HIV infection",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711242,
"choiceText": "Concurrent infection with Capnocytophaga",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711243,
"choiceText": "Prozone effect",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711244,
"choiceText": "CNS toxoplasmosis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "A false-negative cryptococcal antigen test can occur when a very large amount of antigen is present, and the laboratory uses a latex agglutination assay without pretreatment with pronase. This is known as the prozone effect. Advanced HIV infection and CNS toxoplasmosis do not affect the results of a cryptococcal antigen test. Concurrent infection with Capnocytophaga or Trichosporon species can cause a false-positive cryptococcal antigen test.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 551744,
"questionText": "Which of these may produce a false-negative cryptococcal antigen test?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1711245,
"choiceText": "Serial cryptococcal antigen titers",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711246,
"choiceText": "Serial 1,3-beta-D-glucan levels",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711247,
"choiceText": "Repeat imaging",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711248,
"choiceText": "Clinical improvement after therapy",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The best indicator of response to therapy for disseminated Cryptococcus infection is clinical improvement after therapy, with a rise in CD4 T-cell count and an undetectable viral load after HAART. There is no role for serial cryptococcal antigen titers, serial 1,3-beta-D-glucan levels, or repeat imaging.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 551745,
"questionText": "What is the best indicator of a response to therapy for disseminated Cryptococcus infection?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Severe Weakness After Unprotected Sex"
},
{
"authors": "Amber M. Bokhari, MD",
"content": [
"Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult."
],
"date": "May 06, 2024",
"figures": [],
"markdown": "# Severe Weakness After Unprotected Sex\n\n **Authors:** Amber M. Bokhari, MD \n **Date:** May 06, 2024\n\n ## Content\n\n Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult.\n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1711241,
"choiceText": "Advanced HIV infection",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711242,
"choiceText": "Concurrent infection with Capnocytophaga",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711243,
"choiceText": "Prozone effect",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711244,
"choiceText": "CNS toxoplasmosis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "A false-negative cryptococcal antigen test can occur when a very large amount of antigen is present, and the laboratory uses a latex agglutination assay without pretreatment with pronase. This is known as the prozone effect. Advanced HIV infection and CNS toxoplasmosis do not affect the results of a cryptococcal antigen test. Concurrent infection with Capnocytophaga or Trichosporon species can cause a false-positive cryptococcal antigen test.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 551744,
"questionText": "Which of these may produce a false-negative cryptococcal antigen test?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1711245,
"choiceText": "Serial cryptococcal antigen titers",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711246,
"choiceText": "Serial 1,3-beta-D-glucan levels",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711247,
"choiceText": "Repeat imaging",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711248,
"choiceText": "Clinical improvement after therapy",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The best indicator of response to therapy for disseminated Cryptococcus infection is clinical improvement after therapy, with a rise in CD4 T-cell count and an undetectable viral load after HAART. There is no role for serial cryptococcal antigen titers, serial 1,3-beta-D-glucan levels, or repeat imaging.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 551745,
"questionText": "What is the best indicator of a response to therapy for disseminated Cryptococcus infection?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Severe Weakness After Unprotected Sex"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1711237,
"choiceText": "Toxoplasmosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711238,
"choiceText": "Disseminated Cryptococcus infection",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711239,
"choiceText": "Acute HIV infection",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711240,
"choiceText": "Molluscum contagiosum",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 551743,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1711241,
"choiceText": "Advanced HIV infection",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711242,
"choiceText": "Concurrent infection with Capnocytophaga",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711243,
"choiceText": "Prozone effect",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711244,
"choiceText": "CNS toxoplasmosis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "A false-negative cryptococcal antigen test can occur when a very large amount of antigen is present, and the laboratory uses a latex agglutination assay without pretreatment with pronase. This is known as the prozone effect. Advanced HIV infection and CNS toxoplasmosis do not affect the results of a cryptococcal antigen test. Concurrent infection with Capnocytophaga or Trichosporon species can cause a false-positive cryptococcal antigen test.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 551744,
"questionText": "Which of these may produce a false-negative cryptococcal antigen test?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1711245,
"choiceText": "Serial cryptococcal antigen titers",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711246,
"choiceText": "Serial 1,3-beta-D-glucan levels",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711247,
"choiceText": "Repeat imaging",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1711248,
"choiceText": "Clinical improvement after therapy",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The best indicator of response to therapy for disseminated Cryptococcus infection is clinical improvement after therapy, with a rise in CD4 T-cell count and an undetectable viral load after HAART. There is no role for serial cryptococcal antigen titers, serial 1,3-beta-D-glucan levels, or repeat imaging.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 551745,
"questionText": "What is the best indicator of a response to therapy for disseminated Cryptococcus infection?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
881807 | /viewarticle/881807 | [
{
"authors": "Unnikrishnan Pillai, MD; Jameel Muzaffar, MD; Santosh G. John, MD; Pascale Salem, MD; Philip B. Vaidyan, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 46-year-old Black woman is admitted to the intensive care unit with a diagnosis of congestive heart failure after presenting to the emergency department with a 4-day history of progressive generalized weakness, increasing shortness of breath, and leg swelling. She denies having any recent chest pain, cough, or fever.",
"The patient reports that approximately 7 months ago, she had been admitted to another hospital for chest pain and shortness of breath. She states that at that time, she had elevated cardiac enzyme levels, and a cardiologist performed angiography that revealed normal coronary arteries. Three months ago, she was admitted to a different hospital with shortness of breath and leg swelling and was diagnosed with congestive heart failure.",
"In addition to the leg swelling and trouble breathing that had prompted her to call 911 in this instance, she is also complaining of mild dysphagia, gastroesophageal reflux, and difficulty getting up from a sitting position (which has been getting progressively worse for about 4 weeks). She mentions that she has lately been using a cane to help her walk. In addition, for the past 4 months, she has noticed swelling of her tongue, with loss of taste sensation; hair loss; bruising of her eyes; and a nontender, nonpruritic, ecchymotic rash on her abdomen and chest."
],
"date": "August 10, 2022",
"figures": [],
"markdown": "# Loss of Taste, Rash, and Dyspnea in a 46-Year-Old With GERD\n\n **Authors:** Unnikrishnan Pillai, MD; Jameel Muzaffar, MD; Santosh G. John, MD; Pascale Salem, MD; Philip B. Vaidyan, MD \n **Date:** August 10, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 46-year-old Black woman is admitted to the intensive care unit with a diagnosis of congestive heart failure after presenting to the emergency department with a 4-day history of progressive generalized weakness, increasing shortness of breath, and leg swelling. She denies having any recent chest pain, cough, or fever.\nThe patient reports that approximately 7 months ago, she had been admitted to another hospital for chest pain and shortness of breath. She states that at that time, she had elevated cardiac enzyme levels, and a cardiologist performed angiography that revealed normal coronary arteries. Three months ago, she was admitted to a different hospital with shortness of breath and leg swelling and was diagnosed with congestive heart failure.\nIn addition to the leg swelling and trouble breathing that had prompted her to call 911 in this instance, she is also complaining of mild dysphagia, gastroesophageal reflux, and difficulty getting up from a sitting position (which has been getting progressively worse for about 4 weeks). She mentions that she has lately been using a cane to help her walk. In addition, for the past 4 months, she has noticed swelling of her tongue, with loss of taste sensation; hair loss; bruising of her eyes; and a nontender, nonpruritic, ecchymotic rash on her abdomen and chest.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Loss of Taste, Rash, and Dyspnea in a 46-Year-Old With GERD"
},
{
"authors": "Unnikrishnan Pillai, MD; Jameel Muzaffar, MD; Santosh G. John, MD; Pascale Salem, MD; Philip B. Vaidyan, MD",
"content": [
"Upon physical examination, the patient's heart rate is 88 beats/min, blood pressure is 88/54 mm Hg, and respiratory rate is 22 breaths/min. She has an oxygen saturation of 99% while breathing room air.",
"Pertinent findings on clinical examination include bilateral subconjunctival hemorrhaging; periorbital ecchymoses; multiple ecchymotic lesions around the anterior neck, chest, and abdomen (Figure 1); and bilateral pitting pretibial and pedal edema. Localized swelling with imprinted tooth marks (Figure 2) are noted on the lateral aspect of the tongue.",
"Figure 1.",
"Figure 2.",
"Jugular venous distention of 12 cm with normal first and second heart sounds, decreased air entry with mild rales at both lung bases, and bilateral proximal leg weakness are also found.",
"Other relevant findings include a B-type natriuretic peptide level of 1026 pg/mL (reference range, < 100 pg/mL), mildly elevated cardiac enzyme levels, and a chest radiograph showing cardiomegaly along with bilateral basal air space opacities. CT of the thorax shows bilateral pleural effusion (which is greater on the right than the left) and a small pericardial effusion. A urine analysis reveals mild proteinuria, but no red blood cells, white blood cells, or casts are detected. A 24-hour urine protein collection reveals proteinuria of 135 mg. ECG demonstrates low-voltage complexes with poor R-wave progression. A serum ferritin level and a panel of autoimmune tests are all normal. Transthoracic echocardiography is performed (Figure 3).",
"Figure 3."
],
"date": "August 10, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/881/807/881807-Thumb1.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/881/807/881807-Thumb2.jpg"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/881/807/881807-Thumb3.jpg"
}
],
"markdown": "# Loss of Taste, Rash, and Dyspnea in a 46-Year-Old With GERD\n\n **Authors:** Unnikrishnan Pillai, MD; Jameel Muzaffar, MD; Santosh G. John, MD; Pascale Salem, MD; Philip B. Vaidyan, MD \n **Date:** August 10, 2022\n\n ## Content\n\n Upon physical examination, the patient's heart rate is 88 beats/min, blood pressure is 88/54 mm Hg, and respiratory rate is 22 breaths/min. She has an oxygen saturation of 99% while breathing room air.\nPertinent findings on clinical examination include bilateral subconjunctival hemorrhaging; periorbital ecchymoses; multiple ecchymotic lesions around the anterior neck, chest, and abdomen (Figure 1); and bilateral pitting pretibial and pedal edema. Localized swelling with imprinted tooth marks (Figure 2) are noted on the lateral aspect of the tongue.\nFigure 1.\nFigure 2.\nJugular venous distention of 12 cm with normal first and second heart sounds, decreased air entry with mild rales at both lung bases, and bilateral proximal leg weakness are also found.\nOther relevant findings include a B-type natriuretic peptide level of 1026 pg/mL (reference range, < 100 pg/mL), mildly elevated cardiac enzyme levels, and a chest radiograph showing cardiomegaly along with bilateral basal air space opacities. CT of the thorax shows bilateral pleural effusion (which is greater on the right than the left) and a small pericardial effusion. A urine analysis reveals mild proteinuria, but no red blood cells, white blood cells, or casts are detected. A 24-hour urine protein collection reveals proteinuria of 135 mg. ECG demonstrates low-voltage complexes with poor R-wave progression. A serum ferritin level and a panel of autoimmune tests are all normal. Transthoracic echocardiography is performed (Figure 3).\nFigure 3.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1114140,
"choiceText": "Hypertrophic cardiomyopathy",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114142,
"choiceText": "Cardiac amyloidosis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114144,
"choiceText": "Hemochromatosis\r\n",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114146,
"choiceText": "Systemic lupus erythematosus ",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353111,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Loss of Taste, Rash, and Dyspnea in a 46-Year-Old With GERD"
},
{
"authors": "Unnikrishnan Pillai, MD; Jameel Muzaffar, MD; Santosh G. John, MD; Pascale Salem, MD; Philip B. Vaidyan, MD",
"content": [
"The clinical findings of multiple ecchymotic lesions, enlarged tongue, features of congestive heart failure, low-voltage complexes on ECG, and an echocardiographic pattern showing a \"ground-glass\" appearance in the myocardium were consistent with cardiac amyloidosis.",
"Other echocardiographic findings in this patient included a left ventricle with mildly reduced systolic function (ejection fraction of 45%; normal range, 55%-70%); a moderately dilated left atrium, at 5.5 cm; moderately increased ventricular wall thickness, with an interventricular septal thickness of 2 cm (normal range, 0.7-1.1 cm) and a similarly increased thickness in the posterior wall; moderate diastolic dysfunction; and a small pericardial effusion. An abdominal fat pad biopsy to confirm amyloidosis was negative; however, biopsy of the swollen tongue showed homogenous extracellular fibrils positive for Congo red staining and positive for green birefringence (Figures 4 and 5). This result was diagnostic of systemic amyloidosis.",
"Figure 4.",
"Figure 5.",
"Serum protein electrophoresis was negative for monoclonal bands, but immunofixation electrophoresis revealed evidence of a monoclonal population of lambda light chains. A serum free light chain (FLC) assay revealed an elevated lambda free light chain level of 270 mg/L (reference range, 5.7-26.3 mg/L) and a kappa-to-lambda ratio of 0.03 (reference range, 0.26-1.65). Bone marrow aspiration and biopsy revealed hypocellular marrow, with trilineage maturation and mature plasma cells. Congo red staining demonstrated microfocal green birefringence within the vessel walls. Flow cytometry of the bone marrow revealed plasma cell dyscrasia of the monoclonal lambda type. A skeletal survey revealed no lytic lesions. On the basis of the above information, systemic amyloidosis was diagnosed.",
"A characteristic feature of amyloidosis is the extracellular deposition of pathogenic insoluble fibrillar proteins.[1] The age-adjusted incidence of amyloidosis is estimated to be 5-12 cases per 1 million persons per year.[2] The causative protein is an immunoglobulin light chain or a fragment of light chain produced by monoclonal proliferation of plasma cells.[3,4] Amyloidosis is a plasma cell dyscrasia that has a low plasma cell burden of only 5%-10% in the bone marrow. This is in contrast to multiple myeloma, which has 10%-15% plasma cells that express a lambda-type light chain.",
"The clinical features of amyloidosis depend on the organs involved. The three most common internal organs affected are the kidneys, the heart, and the peripheral nerves. Amyloid cardiomyopathy is the second most common presentation. It can lead to rapidly progressive heart failure, with predominant features of right-sided heart failure. Increased ventricular wall thickness resulting from amyloid deposition leads to diastolic dysfunction. Systolic dysfunction is a late feature caused by myocyte necrosis and local interstitial fibrosis. Atrial arrhythmias (in particular, atrial fibrillation) are common in patients with cardiac amyloidosis.",
"Many patients with amyloidosis report easy bruising, resulting from amyloid deposits in the capillaries and deficiency of clotting factor X. Cutaneous ecchymoses may also develop. The lesions seen on this patient's abdomen may have been caused by the above-mentioned factors."
],
"date": "August 10, 2022",
"figures": [
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/881/807/881807-Thumb4.jpg"
},
{
"caption": "Figure 5.",
"image_url": "https://img.medscapestatic.com/article/881/807/881807-Thumb5.jpg"
}
],
"markdown": "# Loss of Taste, Rash, and Dyspnea in a 46-Year-Old With GERD\n\n **Authors:** Unnikrishnan Pillai, MD; Jameel Muzaffar, MD; Santosh G. John, MD; Pascale Salem, MD; Philip B. Vaidyan, MD \n **Date:** August 10, 2022\n\n ## Content\n\n The clinical findings of multiple ecchymotic lesions, enlarged tongue, features of congestive heart failure, low-voltage complexes on ECG, and an echocardiographic pattern showing a \"ground-glass\" appearance in the myocardium were consistent with cardiac amyloidosis.\nOther echocardiographic findings in this patient included a left ventricle with mildly reduced systolic function (ejection fraction of 45%; normal range, 55%-70%); a moderately dilated left atrium, at 5.5 cm; moderately increased ventricular wall thickness, with an interventricular septal thickness of 2 cm (normal range, 0.7-1.1 cm) and a similarly increased thickness in the posterior wall; moderate diastolic dysfunction; and a small pericardial effusion. An abdominal fat pad biopsy to confirm amyloidosis was negative; however, biopsy of the swollen tongue showed homogenous extracellular fibrils positive for Congo red staining and positive for green birefringence (Figures 4 and 5). This result was diagnostic of systemic amyloidosis.\nFigure 4.\nFigure 5.\nSerum protein electrophoresis was negative for monoclonal bands, but immunofixation electrophoresis revealed evidence of a monoclonal population of lambda light chains. A serum free light chain (FLC) assay revealed an elevated lambda free light chain level of 270 mg/L (reference range, 5.7-26.3 mg/L) and a kappa-to-lambda ratio of 0.03 (reference range, 0.26-1.65). Bone marrow aspiration and biopsy revealed hypocellular marrow, with trilineage maturation and mature plasma cells. Congo red staining demonstrated microfocal green birefringence within the vessel walls. Flow cytometry of the bone marrow revealed plasma cell dyscrasia of the monoclonal lambda type. A skeletal survey revealed no lytic lesions. On the basis of the above information, systemic amyloidosis was diagnosed.\nA characteristic feature of amyloidosis is the extracellular deposition of pathogenic insoluble fibrillar proteins.[1] The age-adjusted incidence of amyloidosis is estimated to be 5-12 cases per 1 million persons per year.[2] The causative protein is an immunoglobulin light chain or a fragment of light chain produced by monoclonal proliferation of plasma cells.[3,4] Amyloidosis is a plasma cell dyscrasia that has a low plasma cell burden of only 5%-10% in the bone marrow. This is in contrast to multiple myeloma, which has 10%-15% plasma cells that express a lambda-type light chain.\nThe clinical features of amyloidosis depend on the organs involved. The three most common internal organs affected are the kidneys, the heart, and the peripheral nerves. Amyloid cardiomyopathy is the second most common presentation. It can lead to rapidly progressive heart failure, with predominant features of right-sided heart failure. Increased ventricular wall thickness resulting from amyloid deposition leads to diastolic dysfunction. Systolic dysfunction is a late feature caused by myocyte necrosis and local interstitial fibrosis. Atrial arrhythmias (in particular, atrial fibrillation) are common in patients with cardiac amyloidosis.\nMany patients with amyloidosis report easy bruising, resulting from amyloid deposits in the capillaries and deficiency of clotting factor X. Cutaneous ecchymoses may also develop. The lesions seen on this patient's abdomen may have been caused by the above-mentioned factors.\n\n ## Figures\n\n **Figure 4.** \n \n\n**Figure 5.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1114140,
"choiceText": "Hypertrophic cardiomyopathy",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114142,
"choiceText": "Cardiac amyloidosis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114144,
"choiceText": "Hemochromatosis\r\n",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114146,
"choiceText": "Systemic lupus erythematosus ",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353111,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Loss of Taste, Rash, and Dyspnea in a 46-Year-Old With GERD"
},
{
"authors": "Unnikrishnan Pillai, MD; Jameel Muzaffar, MD; Santosh G. John, MD; Pascale Salem, MD; Philip B. Vaidyan, MD",
"content": [
"ECG findings in cardiac amyloidosis include low voltage in as many as 70% of cases and a pseudoinfarct pattern in as many as 75% of cases.[5,6] Binding of amyloid fibrils to His-Purkinje cells can lead to sudden cardiac death secondary to atrioventricular block and ventricular dysrhythmias. Echocardiography typically reveals thickening of the ventricular septal and free walls, normal or reduced ventricular cavity size, dilated atria, and a normal or slightly reduced ejection fraction; however, cardiac output is significantly reduced.[5]",
"Atrial septal thickening with granular, sparkling myocardium is highly specific for differentiating cardiac amyloidosis from other causes of left ventricular hypertrophy.[7] Of note, sarcoidosis and hemochromatosis can also present similarly, with normal or low-voltage ECG findings and thickened ventricle walls. Coronary angiography findings are usually normal; amyloid deposition involving the epicardial vessels may be rarely seen.[8]",
"The definitive diagnosis of amyloidosis usually requires tissue biopsy. Fine-needle aspiration of abdominal fat is a simple procedure that is positive in > 70% of patients with amyloidosis.[9,10] Biopsies can also be obtained from the minor salivary glands, gingiva, rectum, and skin. Rarely, obtaining tissue from an affected organ may be necessary. In some cases of isolated cardiac involvement, percutaneous endomyocardial biopsy of the right ventricle or interventricular septum may be required.",
"Other methods of diagnosis include bone marrow biopsy to look for a monoclonal population of plasma cells (either kappa or lambda) or immunofixation electrophoresis to look for monoclonal light chain in the urine or serum (which is more sensitive than conventional electrophoresis). Another, more sensitive method is FLC assay, which detects circulating FLCs of both the kappa and lambda types. This assay can also be used for following the progression of the disease and the response to treatment. A combination of an abnormal kappa-to-lambda ratio and a positive serum immunofixation can identify 99% of patients with amyloidosis.[11]",
"The median survival in systemic amyloidosis is only 1-2 years; patients with symptomatic heart involvement have a median survival of only 6 months. An elevated N-terminal pro-brain natriuretic peptide level, an elevated cardiac troponin level, a high circulating level of free light chains, and increasing wall thickness all portend a poor prognosis.[12] The thickness of the ventricular septum in diastole is a predictor of survival, with survival ranging from 2.4 years in patients with normal wall thickness to 0.4 year in those with increased wall thickness.[13]"
],
"date": "August 10, 2022",
"figures": [],
"markdown": "# Loss of Taste, Rash, and Dyspnea in a 46-Year-Old With GERD\n\n **Authors:** Unnikrishnan Pillai, MD; Jameel Muzaffar, MD; Santosh G. John, MD; Pascale Salem, MD; Philip B. Vaidyan, MD \n **Date:** August 10, 2022\n\n ## Content\n\n ECG findings in cardiac amyloidosis include low voltage in as many as 70% of cases and a pseudoinfarct pattern in as many as 75% of cases.[5,6] Binding of amyloid fibrils to His-Purkinje cells can lead to sudden cardiac death secondary to atrioventricular block and ventricular dysrhythmias. Echocardiography typically reveals thickening of the ventricular septal and free walls, normal or reduced ventricular cavity size, dilated atria, and a normal or slightly reduced ejection fraction; however, cardiac output is significantly reduced.[5]\nAtrial septal thickening with granular, sparkling myocardium is highly specific for differentiating cardiac amyloidosis from other causes of left ventricular hypertrophy.[7] Of note, sarcoidosis and hemochromatosis can also present similarly, with normal or low-voltage ECG findings and thickened ventricle walls. Coronary angiography findings are usually normal; amyloid deposition involving the epicardial vessels may be rarely seen.[8]\nThe definitive diagnosis of amyloidosis usually requires tissue biopsy. Fine-needle aspiration of abdominal fat is a simple procedure that is positive in > 70% of patients with amyloidosis.[9,10] Biopsies can also be obtained from the minor salivary glands, gingiva, rectum, and skin. Rarely, obtaining tissue from an affected organ may be necessary. In some cases of isolated cardiac involvement, percutaneous endomyocardial biopsy of the right ventricle or interventricular septum may be required.\nOther methods of diagnosis include bone marrow biopsy to look for a monoclonal population of plasma cells (either kappa or lambda) or immunofixation electrophoresis to look for monoclonal light chain in the urine or serum (which is more sensitive than conventional electrophoresis). Another, more sensitive method is FLC assay, which detects circulating FLCs of both the kappa and lambda types. This assay can also be used for following the progression of the disease and the response to treatment. A combination of an abnormal kappa-to-lambda ratio and a positive serum immunofixation can identify 99% of patients with amyloidosis.[11]\nThe median survival in systemic amyloidosis is only 1-2 years; patients with symptomatic heart involvement have a median survival of only 6 months. An elevated N-terminal pro-brain natriuretic peptide level, an elevated cardiac troponin level, a high circulating level of free light chains, and increasing wall thickness all portend a poor prognosis.[12] The thickness of the ventricular septum in diastole is a predictor of survival, with survival ranging from 2.4 years in patients with normal wall thickness to 0.4 year in those with increased wall thickness.[13]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Loss of Taste, Rash, and Dyspnea in a 46-Year-Old With GERD"
},
{
"authors": "Unnikrishnan Pillai, MD; Jameel Muzaffar, MD; Santosh G. John, MD; Pascale Salem, MD; Philip B. Vaidyan, MD",
"content": [
"The treatment of cardiac amyloidosis includes oral chemotherapy (melphalan and prednisone) or high-dose melphalan with autologous peripheral blood stem cell transplantation (HDM/SCT). The conventional approach is low-dose oral melphalan with prednisone administered in a cyclical manner; however, the impact of this regimen is modest and rarely results in a complete hematologic response or reversal of organ dysfunction.[13]",
"Studies have demonstrated a 25%-75% complete response with HDM/SCT. A \"complete response\" is defined as the absence of monoclonal protein in serum and urine on immunofixation electrophoresis, a normal serum free light chain ratio, and a bone marrow biopsy with < 5% plasma cells and no clonal predominance. In a study by Skinner and colleagues[14] involving 277 patients, HDM/SCT had a 40% complete hematologic response, with 47% survival at 5 years. The major limitation of HDM/SCT is the high rate of treatment-related mortality.",
"The Boston University amyloid program has put forward the following patient eligibility criteria for HDM/SCT treatment[13]:",
"Confirmed tissue diagnosis",
"Evidence of plasma cell dyscrasia",
"Age > 18 years",
"Left ventricular ejection fraction > 40%",
"Supine systolic blood pressure > 90 mm Hg",
"Room air oxygen saturation > 95%",
"Performance status score of 0-2",
"Heart failure caused by amyloidosis is treated with careful diuresis, daily monitoring of fluid and salt intake, careful use of angiotensin-converting enzyme inhibitors, anticoagulation, and tetramer stabilizer therapy. Calcium-channel blockers and digoxin should be avoided. Heart transplantation followed by adjuvant chemotherapy is an option in people with end-stage heart failure.[15,16] Although survival in this group of patients has been statistically lower than that of other cardiac transplantation patients, those with end-stage heart failure still had a 5-year survival of up to 50%.[15]",
"Amyloidosis is a rare cause of rapidly progressing heart failure. An important clue to the diagnosis of cardiac amyloidosis is the paradoxical finding of low-voltage complexes on ECG but concentric ventricular hypertrophy on echocardiography. As seen in the patient in this case, coronary angiography findings are usually normal because the epicardial vessels are not involved. This patient was started on furosemide and lisinopril and was referred to a transplant hematologist for stem cell transplantation and high-dose melphalan. Unfortunately, within 1 month, her condition deteriorated, and she died of multiorgan failure.",
"This case also highlights the importance of obtaining a biopsy from an affected organ if the clinical suspicion is high, particularly in cases where the initial fat pad biopsy is inconclusive. Timely referral to a specialized center is key to treating these patients because of the high mortality and rapid rate of progression of the disease."
],
"date": "August 10, 2022",
"figures": [],
"markdown": "# Loss of Taste, Rash, and Dyspnea in a 46-Year-Old With GERD\n\n **Authors:** Unnikrishnan Pillai, MD; Jameel Muzaffar, MD; Santosh G. John, MD; Pascale Salem, MD; Philip B. Vaidyan, MD \n **Date:** August 10, 2022\n\n ## Content\n\n The treatment of cardiac amyloidosis includes oral chemotherapy (melphalan and prednisone) or high-dose melphalan with autologous peripheral blood stem cell transplantation (HDM/SCT). The conventional approach is low-dose oral melphalan with prednisone administered in a cyclical manner; however, the impact of this regimen is modest and rarely results in a complete hematologic response or reversal of organ dysfunction.[13]\nStudies have demonstrated a 25%-75% complete response with HDM/SCT. A \"complete response\" is defined as the absence of monoclonal protein in serum and urine on immunofixation electrophoresis, a normal serum free light chain ratio, and a bone marrow biopsy with < 5% plasma cells and no clonal predominance. In a study by Skinner and colleagues[14] involving 277 patients, HDM/SCT had a 40% complete hematologic response, with 47% survival at 5 years. The major limitation of HDM/SCT is the high rate of treatment-related mortality.\nThe Boston University amyloid program has put forward the following patient eligibility criteria for HDM/SCT treatment[13]:\nConfirmed tissue diagnosis\nEvidence of plasma cell dyscrasia\nAge > 18 years\nLeft ventricular ejection fraction > 40%\nSupine systolic blood pressure > 90 mm Hg\nRoom air oxygen saturation > 95%\nPerformance status score of 0-2\nHeart failure caused by amyloidosis is treated with careful diuresis, daily monitoring of fluid and salt intake, careful use of angiotensin-converting enzyme inhibitors, anticoagulation, and tetramer stabilizer therapy. Calcium-channel blockers and digoxin should be avoided. Heart transplantation followed by adjuvant chemotherapy is an option in people with end-stage heart failure.[15,16] Although survival in this group of patients has been statistically lower than that of other cardiac transplantation patients, those with end-stage heart failure still had a 5-year survival of up to 50%.[15]\nAmyloidosis is a rare cause of rapidly progressing heart failure. An important clue to the diagnosis of cardiac amyloidosis is the paradoxical finding of low-voltage complexes on ECG but concentric ventricular hypertrophy on echocardiography. As seen in the patient in this case, coronary angiography findings are usually normal because the epicardial vessels are not involved. This patient was started on furosemide and lisinopril and was referred to a transplant hematologist for stem cell transplantation and high-dose melphalan. Unfortunately, within 1 month, her condition deteriorated, and she died of multiorgan failure.\nThis case also highlights the importance of obtaining a biopsy from an affected organ if the clinical suspicion is high, particularly in cases where the initial fat pad biopsy is inconclusive. Timely referral to a specialized center is key to treating these patients because of the high mortality and rapid rate of progression of the disease.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1114148,
"choiceText": "Calcium-channel blockers",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114150,
"choiceText": "Digoxin",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114152,
"choiceText": "Implanted cardio-defibrillator",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114154,
"choiceText": "Angiotensin-converting enzyme inhibitors",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Heart failure caused by amyloidosis is treated with careful diuresis, daily monitoring of fluid and salt intake, careful use of angiotensin-converting enzyme inhibitors, anticoagulation, and tetramer stabilizer therapy. Calcium-channel blockers and digoxin should be avoided. Heart transplantation followed by adjuvant chemotherapy is an option in people with end-stage heart failure.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353113,
"questionText": "Of these, which is the most appropriate treatment option for patients with heart failure caused by amyloidosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1114168,
"choiceText": "CT scan",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114170,
"choiceText": "Serum protein electrophoresis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114172,
"choiceText": "Tissue biopsy",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114174,
"choiceText": "Urine analysis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The definitive diagnosis of amyloidosis usually requires a tissue biopsy. Fine-needle aspiration of abdominal fat is a simple procedure that is positive in > 70% of patients with amyloidosis. Biopsies can also be obtained from the minor salivary glands, gingiva, rectum, and skin. Rarely, obtaining tissue from an affected organ may be necessary.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353117,
"questionText": "Which is the definitive examination for diagnosing amyloidosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Loss of Taste, Rash, and Dyspnea in a 46-Year-Old With GERD"
},
{
"authors": "Unnikrishnan Pillai, MD; Jameel Muzaffar, MD; Santosh G. John, MD; Pascale Salem, MD; Philip B. Vaidyan, MD",
"content": [],
"date": "August 10, 2022",
"figures": [],
"markdown": "# Loss of Taste, Rash, and Dyspnea in a 46-Year-Old With GERD\n\n **Authors:** Unnikrishnan Pillai, MD; Jameel Muzaffar, MD; Santosh G. John, MD; Pascale Salem, MD; Philip B. Vaidyan, MD \n **Date:** August 10, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1114148,
"choiceText": "Calcium-channel blockers",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114150,
"choiceText": "Digoxin",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114152,
"choiceText": "Implanted cardio-defibrillator",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114154,
"choiceText": "Angiotensin-converting enzyme inhibitors",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Heart failure caused by amyloidosis is treated with careful diuresis, daily monitoring of fluid and salt intake, careful use of angiotensin-converting enzyme inhibitors, anticoagulation, and tetramer stabilizer therapy. Calcium-channel blockers and digoxin should be avoided. Heart transplantation followed by adjuvant chemotherapy is an option in people with end-stage heart failure.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353113,
"questionText": "Of these, which is the most appropriate treatment option for patients with heart failure caused by amyloidosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1114168,
"choiceText": "CT scan",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114170,
"choiceText": "Serum protein electrophoresis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114172,
"choiceText": "Tissue biopsy",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114174,
"choiceText": "Urine analysis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The definitive diagnosis of amyloidosis usually requires a tissue biopsy. Fine-needle aspiration of abdominal fat is a simple procedure that is positive in > 70% of patients with amyloidosis. Biopsies can also be obtained from the minor salivary glands, gingiva, rectum, and skin. Rarely, obtaining tissue from an affected organ may be necessary.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353117,
"questionText": "Which is the definitive examination for diagnosing amyloidosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Loss of Taste, Rash, and Dyspnea in a 46-Year-Old With GERD"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1114140,
"choiceText": "Hypertrophic cardiomyopathy",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114142,
"choiceText": "Cardiac amyloidosis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114144,
"choiceText": "Hemochromatosis\r\n",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114146,
"choiceText": "Systemic lupus erythematosus ",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353111,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1114148,
"choiceText": "Calcium-channel blockers",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114150,
"choiceText": "Digoxin",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114152,
"choiceText": "Implanted cardio-defibrillator",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114154,
"choiceText": "Angiotensin-converting enzyme inhibitors",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Heart failure caused by amyloidosis is treated with careful diuresis, daily monitoring of fluid and salt intake, careful use of angiotensin-converting enzyme inhibitors, anticoagulation, and tetramer stabilizer therapy. Calcium-channel blockers and digoxin should be avoided. Heart transplantation followed by adjuvant chemotherapy is an option in people with end-stage heart failure.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353113,
"questionText": "Of these, which is the most appropriate treatment option for patients with heart failure caused by amyloidosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1114168,
"choiceText": "CT scan",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114170,
"choiceText": "Serum protein electrophoresis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114172,
"choiceText": "Tissue biopsy",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1114174,
"choiceText": "Urine analysis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The definitive diagnosis of amyloidosis usually requires a tissue biopsy. Fine-needle aspiration of abdominal fat is a simple procedure that is positive in > 70% of patients with amyloidosis. Biopsies can also be obtained from the minor salivary glands, gingiva, rectum, and skin. Rarely, obtaining tissue from an affected organ may be necessary.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353117,
"questionText": "Which is the definitive examination for diagnosing amyloidosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
752121 | /viewarticle/752121 | [
{
"authors": "Arun Gupta, MD, DNB",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 42-year-old woman presents to the emergency department with a 2-day history of bleeding from her gums. For the past month, the patient has also experienced progressive weakness and occasional bruising over the buttocks, thighs, and shoulders without significant trauma. For the past year the patient has been intermittently using oral analgesics for low back pain.",
"She has no history of hematemesis, melena, hemoptysis, epistaxis, fever, or rash. The patient does not smoke or use illicit drugs; however she does consume 1-2 cans of beer daily. She denies using any regular medications, including oral contraceptives. She has no history of any gastrointestinal or genitourinary illnesses. She is unmarried, lives alone, and works as a clerk in an office."
],
"date": "July 28, 2022",
"figures": [],
"markdown": "# Oncology Case Challenge: A Daily Beer Drinker With Bruises, Back Pain, and Bleeding\n\n **Authors:** Arun Gupta, MD, DNB \n **Date:** July 28, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 42-year-old woman presents to the emergency department with a 2-day history of bleeding from her gums. For the past month, the patient has also experienced progressive weakness and occasional bruising over the buttocks, thighs, and shoulders without significant trauma. For the past year the patient has been intermittently using oral analgesics for low back pain.\nShe has no history of hematemesis, melena, hemoptysis, epistaxis, fever, or rash. The patient does not smoke or use illicit drugs; however she does consume 1-2 cans of beer daily. She denies using any regular medications, including oral contraceptives. She has no history of any gastrointestinal or genitourinary illnesses. She is unmarried, lives alone, and works as a clerk in an office.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Oncology Case Challenge: A Daily Beer Drinker With Bruises, Back Pain, and Bleeding"
},
{
"authors": "Arun Gupta, MD, DNB",
"content": [
"Upon physical examination, the patient is an alert, middle-aged woman in no apparent distress. She has an oral temperature of 98°F (36.7°C), pulse rate of 92 beats/min, blood pressure of 110/68 mm Hg, respiratory rate of 12 breaths/min, and an oxygen saturation of 97% on room air. Examination of the head and neck reveals pale sclerae but no evidence of jaundice. Chest examination demonstrates lungs clear to auscultation with normal S1 and S2 heart sounds. The abdomen is soft and nontender with no palpable organomegaly. No evidence suggests cervical, axillary, or inguinal lymphadenopathy. Rectal examination shows normal sphincter tone with no evidence of blood. Examination of the skin over the buttocks, thighs, and shoulders shows a few ecchymotic patches ranging from 2 to 4 cm in diameter. A few tiny petechial spots are also visible on the skin in the scapular and abdominal regions.",
"Laboratory investigations reveal moderate normocytic normochromic anemia, with a hemoglobin level of 6.7 g/dL (reference range, 12.1-15.1 g/dL), and thrombocytopenia, with a platelet count of 22 × 109/L (reference range, 150-400 × 109/L). The white blood cell count is within the normal range. A blood film examination demonstrates a leukoerythroblastic picture with many band neutrophils, occasional metamyelocytes, and nucleated red blood cells. A few plasmacytoid lymphocytes can also be appreciated. The erythrocyte sedimentation rate (ESR) is 42 mm/hr (reference range, < 20 mm/hr). Her coagulation profile is normal. Direct antiglobulin test results are negative, and a 24-hour urine sample is negative for protein. Her serum chemistry panel demonstrates normal kidney function and electrolyte levels. The liver function tests are normal, except for her lactate dehydrogenase (LDH), which is elevated at 1341 IU/L (reference range, 105-333 IU/L), and a mildly raised alkaline phosphatase level at 161 IU/L (reference range, 20-140 IU/L).",
"The patient's serum beta-2 microglobulin level is elevated at 3.5 µg/mL (reference range, 0.7-1.80 µg/mL). Serum iron, transferrin saturation, ferritin, B12, folic acid, and red cell folate levels are all normal. Serum haptoglobin levels are also within normal limits. Serum immunoglobulin levels are normal, and serum protein electrophoresis does not demonstrate an M-protein spike. A skeletal survey with a radiograph of the skull is ordered (Figure).",
"Figure 1."
],
"date": "July 28, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/749/980/749980-thumb1.png"
}
],
"markdown": "# Oncology Case Challenge: A Daily Beer Drinker With Bruises, Back Pain, and Bleeding\n\n **Authors:** Arun Gupta, MD, DNB \n **Date:** July 28, 2022\n\n ## Content\n\n Upon physical examination, the patient is an alert, middle-aged woman in no apparent distress. She has an oral temperature of 98°F (36.7°C), pulse rate of 92 beats/min, blood pressure of 110/68 mm Hg, respiratory rate of 12 breaths/min, and an oxygen saturation of 97% on room air. Examination of the head and neck reveals pale sclerae but no evidence of jaundice. Chest examination demonstrates lungs clear to auscultation with normal S1 and S2 heart sounds. The abdomen is soft and nontender with no palpable organomegaly. No evidence suggests cervical, axillary, or inguinal lymphadenopathy. Rectal examination shows normal sphincter tone with no evidence of blood. Examination of the skin over the buttocks, thighs, and shoulders shows a few ecchymotic patches ranging from 2 to 4 cm in diameter. A few tiny petechial spots are also visible on the skin in the scapular and abdominal regions.\nLaboratory investigations reveal moderate normocytic normochromic anemia, with a hemoglobin level of 6.7 g/dL (reference range, 12.1-15.1 g/dL), and thrombocytopenia, with a platelet count of 22 × 109/L (reference range, 150-400 × 109/L). The white blood cell count is within the normal range. A blood film examination demonstrates a leukoerythroblastic picture with many band neutrophils, occasional metamyelocytes, and nucleated red blood cells. A few plasmacytoid lymphocytes can also be appreciated. The erythrocyte sedimentation rate (ESR) is 42 mm/hr (reference range, < 20 mm/hr). Her coagulation profile is normal. Direct antiglobulin test results are negative, and a 24-hour urine sample is negative for protein. Her serum chemistry panel demonstrates normal kidney function and electrolyte levels. The liver function tests are normal, except for her lactate dehydrogenase (LDH), which is elevated at 1341 IU/L (reference range, 105-333 IU/L), and a mildly raised alkaline phosphatase level at 161 IU/L (reference range, 20-140 IU/L).\nThe patient's serum beta-2 microglobulin level is elevated at 3.5 µg/mL (reference range, 0.7-1.80 µg/mL). Serum iron, transferrin saturation, ferritin, B12, folic acid, and red cell folate levels are all normal. Serum haptoglobin levels are also within normal limits. Serum immunoglobulin levels are normal, and serum protein electrophoresis does not demonstrate an M-protein spike. A skeletal survey with a radiograph of the skull is ordered (Figure).\nFigure 1.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 438907,
"choiceText": "Acute myeloid leukemia",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438908,
"choiceText": "Metastatic carcinoma",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438909,
"choiceText": "Nonsecretory myeloma",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438910,
"choiceText": "Paget disease",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438911,
"choiceText": "Primary amyloidosis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 130189,
"questionText": "Based on only these findings, which is the most likely diagnosis?<br/><br/>\r\n<i>Hint: Note the radiographic findings.</i>",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Oncology Case Challenge: A Daily Beer Drinker With Bruises, Back Pain, and Bleeding"
},
{
"authors": "Arun Gupta, MD, DNB",
"content": [
"The patient's skull radiograph shows multiple punched-out osteolytic lesions, which are considered a characteristic feature of myeloma. Similar osteolytic lesions were noted on radiographs of the patient's lumbar spine, pelvic bones, and scapula. A bone marrow biopsy revealed sheets of plasmacytoid cells in various stages of development, with marked replacement of normal hematopoietic tissue. More than 90% of these cells were morphologically plasmablasts, whereas the rest were mature plasma cells. These cells were negative for antibodies to leukocyte common antigen, CD117, cytokeratin, carcinoembryonic antigen, and anaplastic lymphoma kinase; however, they were positive for antibodies to CD38, CD138, CD56, and lambda-light chain, thereby confirming the plasmablastic nature and monoclonal origin of these cells. This established the diagnosis of myeloma. The patient did not have hypergammaglobulinemia, a monoclonal spike on serum protein electrophoresis, or Bence-Jones proteins in the urine, indicating the nonsecretory nature of these cells.",
"Multiple myeloma is a B-cell lymphoid malignancy characterized by malignant clonal proliferation and accumulation of plasma cells in the bone marrow that synthesize abnormal immunoglobulins. It is the most common primary malignant tumor of the bone, accounting for approximately 1% of all bone malignancies and 10% of all hematologic malignancies. The median age at diagnosis is 60-65 years; however, in less than 2% of people it occurs before age 40 years. No risk factors have been established for myeloma, although lifestyle, dietary habits, occupational and environmental agents, chronic immune stimulation, obesity, and lower socioeconomic status have been implicated.[1]",
"The clinical presentation of myeloma varies, ranging from indolent to a highly aggressive disease. The symptoms are related to tumor mass effects, bone destruction, protein deposition in various organs, and immunosuppression.[2] Among the varied presentations, 10%-40% of patients are asymptomatic. The most common symptoms observed are spine pain (reported in approximately 70% of patients), pathologic fractures, symptoms related to anemia, bleeding tendency, and/or peripheral neuropathy.[3] The patient may also have a history of repeated infections due to hypogammaglobulinemia. The diagnosis of multiple myeloma is based on major and minor criteria, including the presence and number of plasma cells in the bone marrow, quantitation of monoclonal immunoglobulins in serum by protein immunoelectrophoresis, immunofixation, and lytic bone lesions. MRI is useful for detecting thoracic and lumbar spine lesions, paraspinal involvement, and early cord compression; it can detect as many as 40% of spinal abnormalities in patients with asymptomatic gammopathies in whom radiographic studies are normal.[4] Numerous structural and numerical aberrations in chromosomes have been reported, the most common of which is translocation (11;14). The presence of a chromosome 11q13 translocation has been associated with an unfavorable prognosis.[5,6]",
"Measurement of circulating monoclonal immunoglobulins has been the standard for diagnosis and management of patients with myeloma. However, in about 1%-5% of cases, no protein can be detected in the serum or urine. This variant is known as nonsecretory multiple myeloma (NSMM) and results from either a lack of synthesis by tumor cells or rapid degradation of these proteins in circulation. [7]",
"Based on the inability of malignant plasma cells to synthesize immunoglobulin or the failure of such components to be exported from the cells, these have been classified into 2 types: the nonproducer type (15%), wherein immunoglobulins are not found in plasma cells, and the producer type (85%), in which the immunoglobulins are demonstrable in plasma cells but not in the blood. In such cases, bone marrow immunostaining positivity for CD38, CD138, and CD56 markers and anti-kappa- or anti-lambda-light chain antibodies are helpful in confirming a diagnosis of nonsecretory myeloma. The introduction of assays to quantitate circulating free kappa and free lambda-light chains has made it possible to reclassify approximately one half to two thirds of patients previously thought to have nonsecretory myeloma.[8]"
],
"date": "July 28, 2022",
"figures": [],
"markdown": "# Oncology Case Challenge: A Daily Beer Drinker With Bruises, Back Pain, and Bleeding\n\n **Authors:** Arun Gupta, MD, DNB \n **Date:** July 28, 2022\n\n ## Content\n\n The patient's skull radiograph shows multiple punched-out osteolytic lesions, which are considered a characteristic feature of myeloma. Similar osteolytic lesions were noted on radiographs of the patient's lumbar spine, pelvic bones, and scapula. A bone marrow biopsy revealed sheets of plasmacytoid cells in various stages of development, with marked replacement of normal hematopoietic tissue. More than 90% of these cells were morphologically plasmablasts, whereas the rest were mature plasma cells. These cells were negative for antibodies to leukocyte common antigen, CD117, cytokeratin, carcinoembryonic antigen, and anaplastic lymphoma kinase; however, they were positive for antibodies to CD38, CD138, CD56, and lambda-light chain, thereby confirming the plasmablastic nature and monoclonal origin of these cells. This established the diagnosis of myeloma. The patient did not have hypergammaglobulinemia, a monoclonal spike on serum protein electrophoresis, or Bence-Jones proteins in the urine, indicating the nonsecretory nature of these cells.\nMultiple myeloma is a B-cell lymphoid malignancy characterized by malignant clonal proliferation and accumulation of plasma cells in the bone marrow that synthesize abnormal immunoglobulins. It is the most common primary malignant tumor of the bone, accounting for approximately 1% of all bone malignancies and 10% of all hematologic malignancies. The median age at diagnosis is 60-65 years; however, in less than 2% of people it occurs before age 40 years. No risk factors have been established for myeloma, although lifestyle, dietary habits, occupational and environmental agents, chronic immune stimulation, obesity, and lower socioeconomic status have been implicated.[1]\nThe clinical presentation of myeloma varies, ranging from indolent to a highly aggressive disease. The symptoms are related to tumor mass effects, bone destruction, protein deposition in various organs, and immunosuppression.[2] Among the varied presentations, 10%-40% of patients are asymptomatic. The most common symptoms observed are spine pain (reported in approximately 70% of patients), pathologic fractures, symptoms related to anemia, bleeding tendency, and/or peripheral neuropathy.[3] The patient may also have a history of repeated infections due to hypogammaglobulinemia. The diagnosis of multiple myeloma is based on major and minor criteria, including the presence and number of plasma cells in the bone marrow, quantitation of monoclonal immunoglobulins in serum by protein immunoelectrophoresis, immunofixation, and lytic bone lesions. MRI is useful for detecting thoracic and lumbar spine lesions, paraspinal involvement, and early cord compression; it can detect as many as 40% of spinal abnormalities in patients with asymptomatic gammopathies in whom radiographic studies are normal.[4] Numerous structural and numerical aberrations in chromosomes have been reported, the most common of which is translocation (11;14). The presence of a chromosome 11q13 translocation has been associated with an unfavorable prognosis.[5,6]\nMeasurement of circulating monoclonal immunoglobulins has been the standard for diagnosis and management of patients with myeloma. However, in about 1%-5% of cases, no protein can be detected in the serum or urine. This variant is known as nonsecretory multiple myeloma (NSMM) and results from either a lack of synthesis by tumor cells or rapid degradation of these proteins in circulation. [7]\nBased on the inability of malignant plasma cells to synthesize immunoglobulin or the failure of such components to be exported from the cells, these have been classified into 2 types: the nonproducer type (15%), wherein immunoglobulins are not found in plasma cells, and the producer type (85%), in which the immunoglobulins are demonstrable in plasma cells but not in the blood. In such cases, bone marrow immunostaining positivity for CD38, CD138, and CD56 markers and anti-kappa- or anti-lambda-light chain antibodies are helpful in confirming a diagnosis of nonsecretory myeloma. The introduction of assays to quantitate circulating free kappa and free lambda-light chains has made it possible to reclassify approximately one half to two thirds of patients previously thought to have nonsecretory myeloma.[8]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 438907,
"choiceText": "Acute myeloid leukemia",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438908,
"choiceText": "Metastatic carcinoma",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438909,
"choiceText": "Nonsecretory myeloma",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438910,
"choiceText": "Paget disease",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438911,
"choiceText": "Primary amyloidosis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 130189,
"questionText": "Based on only these findings, which is the most likely diagnosis?<br/><br/>\r\n<i>Hint: Note the radiographic findings.</i>",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Oncology Case Challenge: A Daily Beer Drinker With Bruises, Back Pain, and Bleeding"
},
{
"authors": "Arun Gupta, MD, DNB",
"content": [
"Due to the absence of high serum immunoglobulin levels in NSMM, the rouleaux formation and high ESR may not be observed. An elevated level of alkaline phosphatase and LDH enzymes may be found, the latter being predictive of an aggressive clinical course. Beta-2 microglobulin levels may also be elevated and tend to directly correlate with tumor burden. Bone marrow biopsy shows infiltration by plasma cells in the range of 20%-90%.",
"Once diagnosed, disease staging is accomplished with the traditional Durie-Salmon staging system or the now more commonly used International Staging System (ISS). ISS defines factors that influence a patient's survival and has 3 stages that are based on the levels of serum albumin and beta-2 microglobulin. The overall median survival is 62 months for stage I, 44 months for stage II, and 29 months for stage III disease. Other factors that influence the prognosis and survival are the status of a patient's renal function, plasma cell morphology, plasma cell labeling index (PCLI), and chromosomal changes.[9,10,11]",
"The PCLI may be helpful in establishing a diagnosis of myeloma and can provide information about the prognosis. The PLCI provides a measure of the proliferative rate of the malignant bone marrow plasma cells.[12] A PCLI of ≥ 1% is a strong indicator of active disease and indicates a worse prognosis.",
"Serum free light chain (sFLC) testing is another potential tool to determine multiple myeloma disease progression and treatment response. Khoriaty et al evaluated the use of sFLC in assessing patients with nonsecretory multiple myeloma, as proposed by the International Myeloma Working Group (IMWG) response and progression criteria.[13] Although the investigators corroborated the prognostic reliability of sFLC testing, this assay was limited by the fact that half of the patients' disease was not evaluable (as defined by sFLC <100 mg/L). Thus, the sFLC assay can be used to monitor the course of multiple myeloma and the effect of therapy only in patients whose sFLC is measurable (100 mg/L or greater).[13] Further investigation is needed.",
"The main goal when treating myeloma is to control the disease and to provide comfort for patients. Different treatment modalities are available including chemotherapy, radiation therapy, immunomodulation, and bone marrow transplantation. Multiple myeloma is very sensitive to chemotherapy, which is the primary treatment method. The choice of chemotherapy depends on several factors, such as a patient's age, likelihood of receiving autologous stem cell transplantation, performance status, and renal function. Patients are divided into 3 main categories: (1) young, potential transplant recipients; (2) high-risk patients with advanced disease who are potential transplant recipients; and (3) elderly patients not suitable for transplantation. In general, the first decision made in the management of patients with myeloma who require systemic therapy is whether stem cell transplantation is part of the strategy.",
"For the first category of patients, the most commonly used medication combination is lenalidomide and dexamethasone or bortezomib-based treatment with dexamethasone. Lenalidomide, an analogue of thalidomide, provides a better response rate when combined with high-dose dexamethasone than high-dose dexamethasone used alone.[14] In 2003, the US Food and Drug Administration (FDA) approved a proteasome inhibitor, bortezomib, for patients with relapsed myeloma. A randomized trial found bortezomib plus dexamethasone more effective than VAD (vincristine/doxorubicin [Adriamycin]//dexamethasone) for induction. A superior response rate has also been demonstrated when a combination of bortezomib, thalidomide, and dexamethasone was compared with thalidomide plus dexamethasone. Bortezomib also demonstrates a special benefit in patients with plasma cell leukemia and renal failure.[15]",
"The second category is that of high-risk patients with advanced-stage disease. These patients represent approximately 25% of those with newly diagnosed multiple myeloma, and these patients tend to have a shorter overall survival. They respond to traditional therapies for induction but tend to relapse rapidly. The use of thalidomide, lenalidomide, and bortezomib has improved outcomes for this high-risk group.",
"One typical regimen is bortezomib/lenalidomide/dexamethasone; bortezomib is administered with intravenous push at 1.3 mg/m2 IVP on days 1, 4, 8, and 11, plus lenalidomide orally administered at 25 mg daily on days 1-14, plus dexamethasone administered orally at 20 mg daily on days 1, 2, 4, 5, 8, 9, 11, and 12 or 40 mg orally daily on days 1, 8, and 15. This is on a 21-day cycle for 3 or 4 cycles.",
"Once a response has been achieved, these patients can be considered for autologous stem cell transplantation.",
"In 2012, carfilzomib (Kyprolis), a proteasome inhibitor, was approved in United States for the treatment of patients with multiple myeloma who have received at least two prior therapies including bortezomib and an immunomodulatory agent and have demonstrated disease progression on or within 60 days of therapy completion. The approval was based on a phase 2b, single-arm, multicenter clinical study of 266 patients with relapsed multiple myeloma with other therapies. The study assessed for overall response rate, which was 22.9% over a median duration of 7.8 months.[19]",
"Pomalidomide (Pomalyst), a thalidomide analogue, is also approved for multiple myeloma in patients who have disease progression despite two prior therapies (including lenalidomide and bortezomib). For additional information, see Multiple Myeloma Treatment Protocols.",
"The third category, which is made up of elderly patients (> 70 years) not qualifying for stem cell transplantation, are usually given combination therapy with one of the commonly used regimens -- depending on a patient's clinical condition and risk stratification. Patients who have a relapse after the initial disease is controlled may be treated with any agent not already used. If the disease relapses 6 months after initial therapy, then the initial regimen can be used again. Patients with refractory myeloma are treated with conventional chemotherapy or autologous stem cell transplantation. The use of combinations and targeted therapies has improved responses in these patients.[16]"
],
"date": "July 28, 2022",
"figures": [],
"markdown": "# Oncology Case Challenge: A Daily Beer Drinker With Bruises, Back Pain, and Bleeding\n\n **Authors:** Arun Gupta, MD, DNB \n **Date:** July 28, 2022\n\n ## Content\n\n Due to the absence of high serum immunoglobulin levels in NSMM, the rouleaux formation and high ESR may not be observed. An elevated level of alkaline phosphatase and LDH enzymes may be found, the latter being predictive of an aggressive clinical course. Beta-2 microglobulin levels may also be elevated and tend to directly correlate with tumor burden. Bone marrow biopsy shows infiltration by plasma cells in the range of 20%-90%.\nOnce diagnosed, disease staging is accomplished with the traditional Durie-Salmon staging system or the now more commonly used International Staging System (ISS). ISS defines factors that influence a patient's survival and has 3 stages that are based on the levels of serum albumin and beta-2 microglobulin. The overall median survival is 62 months for stage I, 44 months for stage II, and 29 months for stage III disease. Other factors that influence the prognosis and survival are the status of a patient's renal function, plasma cell morphology, plasma cell labeling index (PCLI), and chromosomal changes.[9,10,11]\nThe PCLI may be helpful in establishing a diagnosis of myeloma and can provide information about the prognosis. The PLCI provides a measure of the proliferative rate of the malignant bone marrow plasma cells.[12] A PCLI of ≥ 1% is a strong indicator of active disease and indicates a worse prognosis.\nSerum free light chain (sFLC) testing is another potential tool to determine multiple myeloma disease progression and treatment response. Khoriaty et al evaluated the use of sFLC in assessing patients with nonsecretory multiple myeloma, as proposed by the International Myeloma Working Group (IMWG) response and progression criteria.[13] Although the investigators corroborated the prognostic reliability of sFLC testing, this assay was limited by the fact that half of the patients' disease was not evaluable (as defined by sFLC <100 mg/L). Thus, the sFLC assay can be used to monitor the course of multiple myeloma and the effect of therapy only in patients whose sFLC is measurable (100 mg/L or greater).[13] Further investigation is needed.\nThe main goal when treating myeloma is to control the disease and to provide comfort for patients. Different treatment modalities are available including chemotherapy, radiation therapy, immunomodulation, and bone marrow transplantation. Multiple myeloma is very sensitive to chemotherapy, which is the primary treatment method. The choice of chemotherapy depends on several factors, such as a patient's age, likelihood of receiving autologous stem cell transplantation, performance status, and renal function. Patients are divided into 3 main categories: (1) young, potential transplant recipients; (2) high-risk patients with advanced disease who are potential transplant recipients; and (3) elderly patients not suitable for transplantation. In general, the first decision made in the management of patients with myeloma who require systemic therapy is whether stem cell transplantation is part of the strategy.\nFor the first category of patients, the most commonly used medication combination is lenalidomide and dexamethasone or bortezomib-based treatment with dexamethasone. Lenalidomide, an analogue of thalidomide, provides a better response rate when combined with high-dose dexamethasone than high-dose dexamethasone used alone.[14] In 2003, the US Food and Drug Administration (FDA) approved a proteasome inhibitor, bortezomib, for patients with relapsed myeloma. A randomized trial found bortezomib plus dexamethasone more effective than VAD (vincristine/doxorubicin [Adriamycin]//dexamethasone) for induction. A superior response rate has also been demonstrated when a combination of bortezomib, thalidomide, and dexamethasone was compared with thalidomide plus dexamethasone. Bortezomib also demonstrates a special benefit in patients with plasma cell leukemia and renal failure.[15]\nThe second category is that of high-risk patients with advanced-stage disease. These patients represent approximately 25% of those with newly diagnosed multiple myeloma, and these patients tend to have a shorter overall survival. They respond to traditional therapies for induction but tend to relapse rapidly. The use of thalidomide, lenalidomide, and bortezomib has improved outcomes for this high-risk group.\nOne typical regimen is bortezomib/lenalidomide/dexamethasone; bortezomib is administered with intravenous push at 1.3 mg/m2 IVP on days 1, 4, 8, and 11, plus lenalidomide orally administered at 25 mg daily on days 1-14, plus dexamethasone administered orally at 20 mg daily on days 1, 2, 4, 5, 8, 9, 11, and 12 or 40 mg orally daily on days 1, 8, and 15. This is on a 21-day cycle for 3 or 4 cycles.\nOnce a response has been achieved, these patients can be considered for autologous stem cell transplantation.\nIn 2012, carfilzomib (Kyprolis), a proteasome inhibitor, was approved in United States for the treatment of patients with multiple myeloma who have received at least two prior therapies including bortezomib and an immunomodulatory agent and have demonstrated disease progression on or within 60 days of therapy completion. The approval was based on a phase 2b, single-arm, multicenter clinical study of 266 patients with relapsed multiple myeloma with other therapies. The study assessed for overall response rate, which was 22.9% over a median duration of 7.8 months.[19]\nPomalidomide (Pomalyst), a thalidomide analogue, is also approved for multiple myeloma in patients who have disease progression despite two prior therapies (including lenalidomide and bortezomib). For additional information, see Multiple Myeloma Treatment Protocols.\nThe third category, which is made up of elderly patients (> 70 years) not qualifying for stem cell transplantation, are usually given combination therapy with one of the commonly used regimens -- depending on a patient's clinical condition and risk stratification. Patients who have a relapse after the initial disease is controlled may be treated with any agent not already used. If the disease relapses 6 months after initial therapy, then the initial regimen can be used again. Patients with refractory myeloma are treated with conventional chemotherapy or autologous stem cell transplantation. The use of combinations and targeted therapies has improved responses in these patients.[16]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Oncology Case Challenge: A Daily Beer Drinker With Bruises, Back Pain, and Bleeding"
},
{
"authors": "Arun Gupta, MD, DNB",
"content": [
"Numerous studies have demonstrated that autologous stem cell transplantation is superior to combination chemotherapy for patients with myeloma who are younger than 65 years. Patients usually receive 4-6 courses of initial chemotherapy, and their stem cells are mobilized with a growth-promoting factor specific for early marrow cells. Some patients (approximately 10%) relapse even after autologous stem cell transplantation, with the average time to relapse being 4 years. At relapse, select patients may benefit from a repeat stem cell transplant, particularly if an adequate number of previously harvested stem cells are still available. The major problems are transplant-related mortality and a late relapse, with patients relapsing as long as 10 years after allogeneic stem cell transplantation.[17] Bisphosphonates are used for the prevention of bony complications, and their use results in an improvement of pain and an overall better quality of life. Radiation therapy is employed to treat areas where there is localized bone damage or pain, or to prevent or treat a fracture. It may be used in combination with chemotherapy.[18]",
"Patients with nonsecretory myeloma are treated in the same fashion as classic multiple myeloma. The diagnosis and monitoring of patients with nonsecretory myeloma depends on an excess of monoclonal plasma cells in the bone marrow and lytic lesions of the bone. Most published reports suggest that there is no significant difference in survival between NSMM and multiple myeloma. Patients with NSMM usually have more advanced disease than those with classic myeloma, and the overall survival ranges from 6 months to 12 years. In this case, examination of the bone marrow aspiration smears showed 65% plasmacytoid cells that were positive for CD38 and CD138 on flow cytometric analysis. Conventional cytogenetic evaluation did not reveal any chromosomal abnormalities.",
"The patient in this case belongs to the producer subtype of NSMM and is currently on induction therapy with cyclophosphamide, dexamethasone, and thalidomide. She is clinically stable, and her biochemical parameters have started improving. During her most recent visit, her hemoglobin level was 10.5 g/dL, platelet count was 95 × 109/L, alkaline phosphatase was 150 U/L, LDH was 610 IU/L, and beta-2 microglobulin was 2.1 µg/mL. Radiographs of the skull showed significant resolution of the lytic lesions. She is scheduled for bone marrow transplantation."
],
"date": "July 28, 2022",
"figures": [],
"markdown": "# Oncology Case Challenge: A Daily Beer Drinker With Bruises, Back Pain, and Bleeding\n\n **Authors:** Arun Gupta, MD, DNB \n **Date:** July 28, 2022\n\n ## Content\n\n Numerous studies have demonstrated that autologous stem cell transplantation is superior to combination chemotherapy for patients with myeloma who are younger than 65 years. Patients usually receive 4-6 courses of initial chemotherapy, and their stem cells are mobilized with a growth-promoting factor specific for early marrow cells. Some patients (approximately 10%) relapse even after autologous stem cell transplantation, with the average time to relapse being 4 years. At relapse, select patients may benefit from a repeat stem cell transplant, particularly if an adequate number of previously harvested stem cells are still available. The major problems are transplant-related mortality and a late relapse, with patients relapsing as long as 10 years after allogeneic stem cell transplantation.[17] Bisphosphonates are used for the prevention of bony complications, and their use results in an improvement of pain and an overall better quality of life. Radiation therapy is employed to treat areas where there is localized bone damage or pain, or to prevent or treat a fracture. It may be used in combination with chemotherapy.[18]\nPatients with nonsecretory myeloma are treated in the same fashion as classic multiple myeloma. The diagnosis and monitoring of patients with nonsecretory myeloma depends on an excess of monoclonal plasma cells in the bone marrow and lytic lesions of the bone. Most published reports suggest that there is no significant difference in survival between NSMM and multiple myeloma. Patients with NSMM usually have more advanced disease than those with classic myeloma, and the overall survival ranges from 6 months to 12 years. In this case, examination of the bone marrow aspiration smears showed 65% plasmacytoid cells that were positive for CD38 and CD138 on flow cytometric analysis. Conventional cytogenetic evaluation did not reveal any chromosomal abnormalities.\nThe patient in this case belongs to the producer subtype of NSMM and is currently on induction therapy with cyclophosphamide, dexamethasone, and thalidomide. She is clinically stable, and her biochemical parameters have started improving. During her most recent visit, her hemoglobin level was 10.5 g/dL, platelet count was 95 × 109/L, alkaline phosphatase was 150 U/L, LDH was 610 IU/L, and beta-2 microglobulin was 2.1 µg/mL. Radiographs of the skull showed significant resolution of the lytic lesions. She is scheduled for bone marrow transplantation.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 438912,
"choiceText": "Low beta-2 microglobulin levels",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438913,
"choiceText": "Low serum lactate dehydrogenase levels",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438914,
"choiceText": "A high plasma cell labeling index",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438915,
"choiceText": "Bone marrow biopsy showing mostly mature plasma cells",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438916,
"choiceText": "Absence of a chromosome 11q13 translocation",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The PCLI is a powerful and independent predictor of survival in patients with newly diagnosed multiple myeloma because it provides a measure of the proliferative rate of the malignant bone marrow plasma cells.<sup>[12]</sup> A PCLI of ≥ 1% is a strong indicator of active disease, and patients have a 3-fold decrease in survival vs patients with a PCLI < 1%. In a classic case of myeloma, the prognostic risk profile of a patient is determined with clinical and laboratory data. Raised levels of serum calcium, beta-2 microglobulin, and LDH indicate high tumor burden and are included in the Durie-Salmon staging system. The prognosis is worse if the bone marrow biopsy shows a majority of blast cells. With the mature plasmacytic type, the median survival is approximately 39.7 months; the mixed cellular type has a survival of 16.1 months; and in the plasmablastic type, survival is 9.8 months. The presence of a chromosome 11q13 translocation indicates a worse prognosis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 130190,
"questionText": "Which condition indicates a worse prognosis in a patient newly diagnosed with multiple myeloma?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 438917,
"choiceText": "Treatment options are similar to classic multiple myeloma",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438918,
"choiceText": "Protein can be detected in the urine but not in the serum",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438919,
"choiceText": "The rouleaux formation of red blood cells is commonly seen",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438920,
"choiceText": "A high erythrocyte sedimentation rate is seen",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438921,
"choiceText": "Nonsecretory multiple myeloma is divided into 2 subtypes based on serum calcium levels",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The treatment of NSMM is on same lines as classic multiple myeloma; therefore, chemotherapy remains the primary treatment modality with other techniques such as radiation therapy and bone marrow transplantation having specific indications. In NSMM, protein cannot be detected in either patients' serum or urine due to either the nonsecretory nature of the plasma cells or rapid degradation of the immunoglobulin proteins in circulation. This lack of circulating immunoglobulins also prevents the red blood cell rouleaux formation as well as a significant rise in ESR. NSMM is divided into 2 subtypes on the basis of whether immunoglobulins are present in the plasma cells but not the blood (producer type) or neither (nonproducer type).",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 130191,
"questionText": "Which statement about nonsecretory multiple myeloma is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Oncology Case Challenge: A Daily Beer Drinker With Bruises, Back Pain, and Bleeding"
},
{
"authors": "Arun Gupta, MD, DNB",
"content": [],
"date": "July 28, 2022",
"figures": [],
"markdown": "# Oncology Case Challenge: A Daily Beer Drinker With Bruises, Back Pain, and Bleeding\n\n **Authors:** Arun Gupta, MD, DNB \n **Date:** July 28, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 438912,
"choiceText": "Low beta-2 microglobulin levels",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438913,
"choiceText": "Low serum lactate dehydrogenase levels",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438914,
"choiceText": "A high plasma cell labeling index",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438915,
"choiceText": "Bone marrow biopsy showing mostly mature plasma cells",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438916,
"choiceText": "Absence of a chromosome 11q13 translocation",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The PCLI is a powerful and independent predictor of survival in patients with newly diagnosed multiple myeloma because it provides a measure of the proliferative rate of the malignant bone marrow plasma cells.<sup>[12]</sup> A PCLI of ≥ 1% is a strong indicator of active disease, and patients have a 3-fold decrease in survival vs patients with a PCLI < 1%. In a classic case of myeloma, the prognostic risk profile of a patient is determined with clinical and laboratory data. Raised levels of serum calcium, beta-2 microglobulin, and LDH indicate high tumor burden and are included in the Durie-Salmon staging system. The prognosis is worse if the bone marrow biopsy shows a majority of blast cells. With the mature plasmacytic type, the median survival is approximately 39.7 months; the mixed cellular type has a survival of 16.1 months; and in the plasmablastic type, survival is 9.8 months. The presence of a chromosome 11q13 translocation indicates a worse prognosis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 130190,
"questionText": "Which condition indicates a worse prognosis in a patient newly diagnosed with multiple myeloma?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 438917,
"choiceText": "Treatment options are similar to classic multiple myeloma",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438918,
"choiceText": "Protein can be detected in the urine but not in the serum",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438919,
"choiceText": "The rouleaux formation of red blood cells is commonly seen",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438920,
"choiceText": "A high erythrocyte sedimentation rate is seen",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438921,
"choiceText": "Nonsecretory multiple myeloma is divided into 2 subtypes based on serum calcium levels",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The treatment of NSMM is on same lines as classic multiple myeloma; therefore, chemotherapy remains the primary treatment modality with other techniques such as radiation therapy and bone marrow transplantation having specific indications. In NSMM, protein cannot be detected in either patients' serum or urine due to either the nonsecretory nature of the plasma cells or rapid degradation of the immunoglobulin proteins in circulation. This lack of circulating immunoglobulins also prevents the red blood cell rouleaux formation as well as a significant rise in ESR. NSMM is divided into 2 subtypes on the basis of whether immunoglobulins are present in the plasma cells but not the blood (producer type) or neither (nonproducer type).",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 130191,
"questionText": "Which statement about nonsecretory multiple myeloma is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Oncology Case Challenge: A Daily Beer Drinker With Bruises, Back Pain, and Bleeding"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 438907,
"choiceText": "Acute myeloid leukemia",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438908,
"choiceText": "Metastatic carcinoma",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438909,
"choiceText": "Nonsecretory myeloma",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438910,
"choiceText": "Paget disease",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438911,
"choiceText": "Primary amyloidosis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 130189,
"questionText": "Based on only these findings, which is the most likely diagnosis?<br/><br/>\r\n<i>Hint: Note the radiographic findings.</i>",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 438912,
"choiceText": "Low beta-2 microglobulin levels",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438913,
"choiceText": "Low serum lactate dehydrogenase levels",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438914,
"choiceText": "A high plasma cell labeling index",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438915,
"choiceText": "Bone marrow biopsy showing mostly mature plasma cells",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438916,
"choiceText": "Absence of a chromosome 11q13 translocation",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The PCLI is a powerful and independent predictor of survival in patients with newly diagnosed multiple myeloma because it provides a measure of the proliferative rate of the malignant bone marrow plasma cells.<sup>[12]</sup> A PCLI of ≥ 1% is a strong indicator of active disease, and patients have a 3-fold decrease in survival vs patients with a PCLI < 1%. In a classic case of myeloma, the prognostic risk profile of a patient is determined with clinical and laboratory data. Raised levels of serum calcium, beta-2 microglobulin, and LDH indicate high tumor burden and are included in the Durie-Salmon staging system. The prognosis is worse if the bone marrow biopsy shows a majority of blast cells. With the mature plasmacytic type, the median survival is approximately 39.7 months; the mixed cellular type has a survival of 16.1 months; and in the plasmablastic type, survival is 9.8 months. The presence of a chromosome 11q13 translocation indicates a worse prognosis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 130190,
"questionText": "Which condition indicates a worse prognosis in a patient newly diagnosed with multiple myeloma?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 438917,
"choiceText": "Treatment options are similar to classic multiple myeloma",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438918,
"choiceText": "Protein can be detected in the urine but not in the serum",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438919,
"choiceText": "The rouleaux formation of red blood cells is commonly seen",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438920,
"choiceText": "A high erythrocyte sedimentation rate is seen",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 438921,
"choiceText": "Nonsecretory multiple myeloma is divided into 2 subtypes based on serum calcium levels",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The treatment of NSMM is on same lines as classic multiple myeloma; therefore, chemotherapy remains the primary treatment modality with other techniques such as radiation therapy and bone marrow transplantation having specific indications. In NSMM, protein cannot be detected in either patients' serum or urine due to either the nonsecretory nature of the plasma cells or rapid degradation of the immunoglobulin proteins in circulation. This lack of circulating immunoglobulins also prevents the red blood cell rouleaux formation as well as a significant rise in ESR. NSMM is divided into 2 subtypes on the basis of whether immunoglobulins are present in the plasma cells but not the blood (producer type) or neither (nonproducer type).",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 130191,
"questionText": "Which statement about nonsecretory multiple myeloma is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
877044 | /viewarticle/877044 | [
{
"authors": "Ramy Saleh, DO; Robert Bassett, DO; Alan Lucerna, DO; Wayne Tamaska, DO; James Espinosa, MD; Kumail Kazim; Frederick Barnum IV; Emeka Ezidiegwu",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 28-year-old man presents to the emergency department with his mother after a suicide attempt via pill ingestion. He stated that he took about 60 tablets 1 hour ago.",
"He was recently diagnosed with systemic lupus erythematosus but has no other medical history, surgical history, or hospitalizations. With the exception of medication for systemic lupus erythematosus, he does not take any prescription or over-the-counter medications. He does not have any allergies to medications or any significant history of tobacco, alcohol, or recreational drug use. His maternal and paternal family history is noncontributory.",
"The patient states that he has been feeling depressed, but he does not have any documented psychiatric history. He reports some nausea and vague abdominal pain. He denies having any other symptoms."
],
"date": "July 28, 2022",
"figures": [],
"markdown": "# Intentional Overdose in a Suicidal 28-Year-Old With Lupus\n\n **Authors:** Ramy Saleh, DO; Robert Bassett, DO; Alan Lucerna, DO; Wayne Tamaska, DO; James Espinosa, MD; Kumail Kazim; Frederick Barnum IV; Emeka Ezidiegwu \n **Date:** July 28, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 28-year-old man presents to the emergency department with his mother after a suicide attempt via pill ingestion. He stated that he took about 60 tablets 1 hour ago.\nHe was recently diagnosed with systemic lupus erythematosus but has no other medical history, surgical history, or hospitalizations. With the exception of medication for systemic lupus erythematosus, he does not take any prescription or over-the-counter medications. He does not have any allergies to medications or any significant history of tobacco, alcohol, or recreational drug use. His maternal and paternal family history is noncontributory.\nThe patient states that he has been feeling depressed, but he does not have any documented psychiatric history. He reports some nausea and vague abdominal pain. He denies having any other symptoms.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Intentional Overdose in a Suicidal 28-Year-Old With Lupus"
},
{
"authors": "Ramy Saleh, DO; Robert Bassett, DO; Alan Lucerna, DO; Wayne Tamaska, DO; James Espinosa, MD; Kumail Kazim; Frederick Barnum IV; Emeka Ezidiegwu",
"content": [
"The patient's Glasgow Coma Scale score on presentation was 15/15, and his vital signs were as follows:",
"Temperature: 100.4°F (38°C)",
"Blood pressure: 93/52 mm Hg",
"Pulse: 127 beats/min",
"Respiratory rate: 18 breaths/min",
"Oxygen saturation: 95% on room air",
"ECG revealed a prolonged QTc of 507 msec (reference range in men, < 440 msec). His serum potassium level was 3.1 mmol/L (reference range, 3.5-5.1 mmol/L).",
"Physical examination findings included a soft, nondistended abdomen with unspecified diffuse abdominal tenderness to palpation and positive bowel sounds in all four quadrants. The findings were otherwise unremarkable.",
"A toxicology consult was immediately obtained. Recommendations included placement of a nasogastric tube, 1 g/kg of activated charcoal, and whole-bowel irrigation with polyethylene glycol solution at 1.5-2 L/hr via nasogastric tube until rectal effluent was clear. Potassium supplementation was initiated, targeting a serum level of 3.5-4 mmol/L. During this time, serial ECGs were performed to monitor the QRS and QTc intervals in particular.",
"Two hours after arrival, the patient exhibited approximately 15 seconds of generalized seizure activity, followed by polymorphic ventricular tachycardia (Figure 1).",
"Figure 1",
"The patient's cardiac rhythm spontaneously converted back to normal sinus rhythm just before receiving 2 g of magnesium sulfate and 10 mg of diazepam. However, the patient's potassium level dropped to 2.5 mmol/L, and the rate of potassium repletion was increased."
],
"date": "July 28, 2022",
"figures": [
{
"caption": "Figure 1",
"image_url": "https://img.medscapestatic.com/article/877/044/877044-Thumb-2.png"
}
],
"markdown": "# Intentional Overdose in a Suicidal 28-Year-Old With Lupus\n\n **Authors:** Ramy Saleh, DO; Robert Bassett, DO; Alan Lucerna, DO; Wayne Tamaska, DO; James Espinosa, MD; Kumail Kazim; Frederick Barnum IV; Emeka Ezidiegwu \n **Date:** July 28, 2022\n\n ## Content\n\n The patient's Glasgow Coma Scale score on presentation was 15/15, and his vital signs were as follows:\nTemperature: 100.4°F (38°C)\nBlood pressure: 93/52 mm Hg\nPulse: 127 beats/min\nRespiratory rate: 18 breaths/min\nOxygen saturation: 95% on room air\nECG revealed a prolonged QTc of 507 msec (reference range in men, < 440 msec). His serum potassium level was 3.1 mmol/L (reference range, 3.5-5.1 mmol/L).\nPhysical examination findings included a soft, nondistended abdomen with unspecified diffuse abdominal tenderness to palpation and positive bowel sounds in all four quadrants. The findings were otherwise unremarkable.\nA toxicology consult was immediately obtained. Recommendations included placement of a nasogastric tube, 1 g/kg of activated charcoal, and whole-bowel irrigation with polyethylene glycol solution at 1.5-2 L/hr via nasogastric tube until rectal effluent was clear. Potassium supplementation was initiated, targeting a serum level of 3.5-4 mmol/L. During this time, serial ECGs were performed to monitor the QRS and QTc intervals in particular.\nTwo hours after arrival, the patient exhibited approximately 15 seconds of generalized seizure activity, followed by polymorphic ventricular tachycardia (Figure 1).\nFigure 1\nThe patient's cardiac rhythm spontaneously converted back to normal sinus rhythm just before receiving 2 g of magnesium sulfate and 10 mg of diazepam. However, the patient's potassium level dropped to 2.5 mmol/L, and the rate of potassium repletion was increased.\n\n ## Figures\n\n **Figure 1** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1073644,
"choiceText": "Amitriptyline overdose",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073646,
"choiceText": "Sotalol overdose",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073648,
"choiceText": "Celecoxib overdose",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073650,
"choiceText": "Hydroxychloroquine overdose",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073652,
"choiceText": "Methotrexate overdose",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 339971,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Intentional Overdose in a Suicidal 28-Year-Old With Lupus"
},
{
"authors": "Ramy Saleh, DO; Robert Bassett, DO; Alan Lucerna, DO; Wayne Tamaska, DO; James Espinosa, MD; Kumail Kazim; Frederick Barnum IV; Emeka Ezidiegwu",
"content": [
"This case illustrates a potentially fatal toxicity. Hydroxychloroquine (Figure 2) is synthesized by adding a hydroxyl group to chloroquine; this results in a slight decrease of the toxicity level of this substance compared with other quinines.[1]",
"Figure 2",
"The exact pathophysiology of hydroxychloroquine toxicity is not completely understood. Furthermore, because animal and human data are limited, the optimal treatment strategy remains unclear. This case illustrates the many complexities in caring for patients with hydroxychloroquine overdose.",
"Acute toxicity can result in altered mental status, seizures, hypotension, malignant dysrhythmias, rapid cardiovascular collapse, and death.[2] Chronic toxicity has been shown to cause retinopathy, the mechanism of which is poorly understood.[3,4]",
"The deadliest side effects of hydroxychloroquine are due to cardiotoxicity. The cardiotoxicity associated with any chloroquine-type medication can be attributed to the quinidine-like actions, which result in a negative ionotropic effect on the heart, slower conduction rate, inhibition of spontaneous diastolic depolarization, decreased cardiac excitability by raising electrical thresholds, and overall decreased contractility.[1]"
],
"date": "July 28, 2022",
"figures": [
{
"caption": "Figure 2",
"image_url": "https://img.medscapestatic.com/article/877/044/877044-Thumb-1.png"
}
],
"markdown": "# Intentional Overdose in a Suicidal 28-Year-Old With Lupus\n\n **Authors:** Ramy Saleh, DO; Robert Bassett, DO; Alan Lucerna, DO; Wayne Tamaska, DO; James Espinosa, MD; Kumail Kazim; Frederick Barnum IV; Emeka Ezidiegwu \n **Date:** July 28, 2022\n\n ## Content\n\n This case illustrates a potentially fatal toxicity. Hydroxychloroquine (Figure 2) is synthesized by adding a hydroxyl group to chloroquine; this results in a slight decrease of the toxicity level of this substance compared with other quinines.[1]\nFigure 2\nThe exact pathophysiology of hydroxychloroquine toxicity is not completely understood. Furthermore, because animal and human data are limited, the optimal treatment strategy remains unclear. This case illustrates the many complexities in caring for patients with hydroxychloroquine overdose.\nAcute toxicity can result in altered mental status, seizures, hypotension, malignant dysrhythmias, rapid cardiovascular collapse, and death.[2] Chronic toxicity has been shown to cause retinopathy, the mechanism of which is poorly understood.[3,4]\nThe deadliest side effects of hydroxychloroquine are due to cardiotoxicity. The cardiotoxicity associated with any chloroquine-type medication can be attributed to the quinidine-like actions, which result in a negative ionotropic effect on the heart, slower conduction rate, inhibition of spontaneous diastolic depolarization, decreased cardiac excitability by raising electrical thresholds, and overall decreased contractility.[1]\n\n ## Figures\n\n **Figure 2** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1073644,
"choiceText": "Amitriptyline overdose",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073646,
"choiceText": "Sotalol overdose",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073648,
"choiceText": "Celecoxib overdose",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073650,
"choiceText": "Hydroxychloroquine overdose",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073652,
"choiceText": "Methotrexate overdose",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 339971,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Intentional Overdose in a Suicidal 28-Year-Old With Lupus"
},
{
"authors": "Ramy Saleh, DO; Robert Bassett, DO; Alan Lucerna, DO; Wayne Tamaska, DO; James Espinosa, MD; Kumail Kazim; Frederick Barnum IV; Emeka Ezidiegwu",
"content": [
"Because of its structural similarity to quinine, the proposed mechanism of toxicity for hydroxychloroquine includes sodium and potassium channel blockade.[5,6] Therefore, continuous telemetry monitoring with close observation for QRS widening and QT interval prolongation is imperative. Unlike for quinine, patients with significant exposures to chloroquine derivatives (including hydroxychloroquine) routinely demonstrate hypokalemia. Severe hypokalemia is commonly associated with cardiac manifestations, such that it is considered a useful prognostic tool in predicting the severity of the exposure.[5,7,8] Of note, this appears to be due to an intracellular shift rather than systemic depletion.[2,9,10]",
"The potential for hyperkalemia as the toxicity and cellular shifting resolve underscores the complexity of potassium derangements. Thus, monitoring potassium levels and careful repletions are important because overzealous repletion can result in hyperkalemia during the evolution and resolution of the poisoning.[11,12] Although aggressive potassium supplementation seems intuitive, evidence on the optimal potassium level is conflicting, with some reports suggesting that mild hypokalemia may have a protective benefit.[2,7]",
"This phenomenon also complicates the routine use of sodium bicarbonate (NaHCO3) to overcome sodium channel inhibition. The injudicious use of NaHCO3 in a patient with uncorrected hypokalemia could result in lowering potassium levels to the point of cardiac collapse. Consultation with a medical toxicologist regarding the role of NaHCO3 and potassium along with treatment endpoints should be considered."
],
"date": "July 28, 2022",
"figures": [],
"markdown": "# Intentional Overdose in a Suicidal 28-Year-Old With Lupus\n\n **Authors:** Ramy Saleh, DO; Robert Bassett, DO; Alan Lucerna, DO; Wayne Tamaska, DO; James Espinosa, MD; Kumail Kazim; Frederick Barnum IV; Emeka Ezidiegwu \n **Date:** July 28, 2022\n\n ## Content\n\n Because of its structural similarity to quinine, the proposed mechanism of toxicity for hydroxychloroquine includes sodium and potassium channel blockade.[5,6] Therefore, continuous telemetry monitoring with close observation for QRS widening and QT interval prolongation is imperative. Unlike for quinine, patients with significant exposures to chloroquine derivatives (including hydroxychloroquine) routinely demonstrate hypokalemia. Severe hypokalemia is commonly associated with cardiac manifestations, such that it is considered a useful prognostic tool in predicting the severity of the exposure.[5,7,8] Of note, this appears to be due to an intracellular shift rather than systemic depletion.[2,9,10]\nThe potential for hyperkalemia as the toxicity and cellular shifting resolve underscores the complexity of potassium derangements. Thus, monitoring potassium levels and careful repletions are important because overzealous repletion can result in hyperkalemia during the evolution and resolution of the poisoning.[11,12] Although aggressive potassium supplementation seems intuitive, evidence on the optimal potassium level is conflicting, with some reports suggesting that mild hypokalemia may have a protective benefit.[2,7]\nThis phenomenon also complicates the routine use of sodium bicarbonate (NaHCO3) to overcome sodium channel inhibition. The injudicious use of NaHCO3 in a patient with uncorrected hypokalemia could result in lowering potassium levels to the point of cardiac collapse. Consultation with a medical toxicologist regarding the role of NaHCO3 and potassium along with treatment endpoints should be considered.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Intentional Overdose in a Suicidal 28-Year-Old With Lupus"
},
{
"authors": "Ramy Saleh, DO; Robert Bassett, DO; Alan Lucerna, DO; Wayne Tamaska, DO; James Espinosa, MD; Kumail Kazim; Frederick Barnum IV; Emeka Ezidiegwu",
"content": [
"Hydroxychloroquine poisoning can result in significant morbidity and mortality. Treatment options include early airway protection, gastrointestinal (GI) decontamination, cautious electrolyte supplementation with serial ECG monitoring, epinephrine, and high-dose diazepam infusion for refractory hypotension.[1] If these methods fail to provide improvement, consideration of extracorporeal membrane oxygenation (ECMO) in selected patients is warranted.[13]",
"The mainstay of early treatment includes consideration of GI decontamination. A full review of the potential risks and benefits of activated charcoal and whole-bowel irrigation are beyond the scope of this article. If a patient is encountered early after a potentially life-threatening exposure in which the presence of unabsorbed drug in the GI tract is a concern, then GI decontamination should be considered. Early airway protection is essential and yet still may not eliminate the risk for aspiration, as was the case in the patient described here.[1,2]",
"In the most recalcitrant cases that fail to respond to standard medical therapy, an intra-aortic balloon pump or ECMO may be used to bridge therapy during the period of cardiovascular collapse while awaiting resolution of the hydroxychloroquine toxicity.[13]",
"In patients who experience persistent shock after an overdose of chloroquine-related medications, certain adjunctive medicines may be useful in restoring cellular perfusion. Although any direct acting vasopressor may confer benefit, epinephrine is the most studied and routinely recommended.[14,15] Owing to the potential for profound shock, a reasonable starting dose is 0.25 mcg/kg/min, with upward titration to maintain adequate perfusion.[5]",
"High-dose diazepam can also be beneficial in severe hydroxychloroquine toxicity. The exact mechanism of action is not well understood, but a review of the postulated theories described in Goldfrank's Toxicologic Emergencies include \"(1) a central antagonistic effect, (2) anticonvulsant effect, (3) antidysrhythmic effect by an electrophysiologic action inverse to chloroquine, (4) pharmacokinetic interaction between diazepam and chloroquine, and (5) decrease in chloroquine-induced vasodilation.\" Discussion with a medical toxicologist may help clinicians allay any reticence over the extraordinarily high, but recommended, starting dose of 2 mg/kg over 30 minutes followed by 1-2 mg/kg/d for 2-4 days.",
"Despite early airway protection with a standard cuffed endotracheal tube, the course of the patient in this case was complicated by aspiration pneumonia that required further antibiotics and mechanical ventilation. The patient remained in the intensive care unit, where he also had episodes of upper GI bleeding; however, he improved with medical management and was eventually discharged in stable condition."
],
"date": "July 28, 2022",
"figures": [],
"markdown": "# Intentional Overdose in a Suicidal 28-Year-Old With Lupus\n\n **Authors:** Ramy Saleh, DO; Robert Bassett, DO; Alan Lucerna, DO; Wayne Tamaska, DO; James Espinosa, MD; Kumail Kazim; Frederick Barnum IV; Emeka Ezidiegwu \n **Date:** July 28, 2022\n\n ## Content\n\n Hydroxychloroquine poisoning can result in significant morbidity and mortality. Treatment options include early airway protection, gastrointestinal (GI) decontamination, cautious electrolyte supplementation with serial ECG monitoring, epinephrine, and high-dose diazepam infusion for refractory hypotension.[1] If these methods fail to provide improvement, consideration of extracorporeal membrane oxygenation (ECMO) in selected patients is warranted.[13]\nThe mainstay of early treatment includes consideration of GI decontamination. A full review of the potential risks and benefits of activated charcoal and whole-bowel irrigation are beyond the scope of this article. If a patient is encountered early after a potentially life-threatening exposure in which the presence of unabsorbed drug in the GI tract is a concern, then GI decontamination should be considered. Early airway protection is essential and yet still may not eliminate the risk for aspiration, as was the case in the patient described here.[1,2]\nIn the most recalcitrant cases that fail to respond to standard medical therapy, an intra-aortic balloon pump or ECMO may be used to bridge therapy during the period of cardiovascular collapse while awaiting resolution of the hydroxychloroquine toxicity.[13]\nIn patients who experience persistent shock after an overdose of chloroquine-related medications, certain adjunctive medicines may be useful in restoring cellular perfusion. Although any direct acting vasopressor may confer benefit, epinephrine is the most studied and routinely recommended.[14,15] Owing to the potential for profound shock, a reasonable starting dose is 0.25 mcg/kg/min, with upward titration to maintain adequate perfusion.[5]\nHigh-dose diazepam can also be beneficial in severe hydroxychloroquine toxicity. The exact mechanism of action is not well understood, but a review of the postulated theories described in Goldfrank's Toxicologic Emergencies include \"(1) a central antagonistic effect, (2) anticonvulsant effect, (3) antidysrhythmic effect by an electrophysiologic action inverse to chloroquine, (4) pharmacokinetic interaction between diazepam and chloroquine, and (5) decrease in chloroquine-induced vasodilation.\" Discussion with a medical toxicologist may help clinicians allay any reticence over the extraordinarily high, but recommended, starting dose of 2 mg/kg over 30 minutes followed by 1-2 mg/kg/d for 2-4 days.\nDespite early airway protection with a standard cuffed endotracheal tube, the course of the patient in this case was complicated by aspiration pneumonia that required further antibiotics and mechanical ventilation. The patient remained in the intensive care unit, where he also had episodes of upper GI bleeding; however, he improved with medical management and was eventually discharged in stable condition.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1073654,
"choiceText": "Increased serum potassium levels are a known side effect of hydroxychloroquine",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073656,
"choiceText": "As the intracellular shift corrects, the patient's serum potassium levels rise",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073658,
"choiceText": "Hyperkalemia is uncommon in patients with this presentation ",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073660,
"choiceText": "Hydroxychloroquine reduces potassium excretion by the kidneys",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Hypokalemia due to hydroxychloroquine appears to be a result of an intracellular shift rather than systemic depletion of potassium. Therefore, as the effects of hydroxychloroquine wear off, the potassium levels rise. For this reason, potassium repletion in patients of a hydroxychloroquine overdose should be done judiciously, with frequent checks of the potassium level. The potassium level should initially be corrected to a state of mild hypokalemia.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 339973,
"questionText": "Which mechanism may result in hyperkalemia in patients such as the one described above?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1073662,
"choiceText": "Eplerenone",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073664,
"choiceText": "Ramipril",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073666,
"choiceText": "Calcium gluconate",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073668,
"choiceText": "Kayexalate",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Eplerenone is a potassium-sparing diuretic, which increases serum potassium.<br/><br/>\r\nRamipril is an angiotensin-converting enzyme inhibitor, which works by inhibiting the conversion of angiotensin I to angiotensin II, ultimately inhibiting the production of aldosterone to reduce sodium and water retention. As sodium is lost through the Na-K channels, potassium is retained in the serum.<br/><br/>\r\nKayexalate is a potassium binder, which helps to remove potassium from the body. However, its onset of action is approximately 2-24 hours, which is not appropriate in an emergent setting. <br/><br/>\r\nCalcium gluconate has a rapid onset of approximately 5 minutes and is used to protect the myocardium in a hyperkalemic state. For this reason, calcium gluconate is the most appropriate choice.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 339975,
"questionText": "If a patient who experienced hydroxychloroquine overdose has potassium levels that are too aggressively corrected and experiences hyperkalemia, which agent may be indicated?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Intentional Overdose in a Suicidal 28-Year-Old With Lupus"
},
{
"authors": "Ramy Saleh, DO; Robert Bassett, DO; Alan Lucerna, DO; Wayne Tamaska, DO; James Espinosa, MD; Kumail Kazim; Frederick Barnum IV; Emeka Ezidiegwu",
"content": [],
"date": "July 28, 2022",
"figures": [],
"markdown": "# Intentional Overdose in a Suicidal 28-Year-Old With Lupus\n\n **Authors:** Ramy Saleh, DO; Robert Bassett, DO; Alan Lucerna, DO; Wayne Tamaska, DO; James Espinosa, MD; Kumail Kazim; Frederick Barnum IV; Emeka Ezidiegwu \n **Date:** July 28, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1073654,
"choiceText": "Increased serum potassium levels are a known side effect of hydroxychloroquine",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073656,
"choiceText": "As the intracellular shift corrects, the patient's serum potassium levels rise",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073658,
"choiceText": "Hyperkalemia is uncommon in patients with this presentation ",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073660,
"choiceText": "Hydroxychloroquine reduces potassium excretion by the kidneys",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Hypokalemia due to hydroxychloroquine appears to be a result of an intracellular shift rather than systemic depletion of potassium. Therefore, as the effects of hydroxychloroquine wear off, the potassium levels rise. For this reason, potassium repletion in patients of a hydroxychloroquine overdose should be done judiciously, with frequent checks of the potassium level. The potassium level should initially be corrected to a state of mild hypokalemia.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 339973,
"questionText": "Which mechanism may result in hyperkalemia in patients such as the one described above?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1073662,
"choiceText": "Eplerenone",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073664,
"choiceText": "Ramipril",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073666,
"choiceText": "Calcium gluconate",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073668,
"choiceText": "Kayexalate",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Eplerenone is a potassium-sparing diuretic, which increases serum potassium.<br/><br/>\r\nRamipril is an angiotensin-converting enzyme inhibitor, which works by inhibiting the conversion of angiotensin I to angiotensin II, ultimately inhibiting the production of aldosterone to reduce sodium and water retention. As sodium is lost through the Na-K channels, potassium is retained in the serum.<br/><br/>\r\nKayexalate is a potassium binder, which helps to remove potassium from the body. However, its onset of action is approximately 2-24 hours, which is not appropriate in an emergent setting. <br/><br/>\r\nCalcium gluconate has a rapid onset of approximately 5 minutes and is used to protect the myocardium in a hyperkalemic state. For this reason, calcium gluconate is the most appropriate choice.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 339975,
"questionText": "If a patient who experienced hydroxychloroquine overdose has potassium levels that are too aggressively corrected and experiences hyperkalemia, which agent may be indicated?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Intentional Overdose in a Suicidal 28-Year-Old With Lupus"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1073644,
"choiceText": "Amitriptyline overdose",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073646,
"choiceText": "Sotalol overdose",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073648,
"choiceText": "Celecoxib overdose",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073650,
"choiceText": "Hydroxychloroquine overdose",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073652,
"choiceText": "Methotrexate overdose",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 339971,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1073654,
"choiceText": "Increased serum potassium levels are a known side effect of hydroxychloroquine",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073656,
"choiceText": "As the intracellular shift corrects, the patient's serum potassium levels rise",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073658,
"choiceText": "Hyperkalemia is uncommon in patients with this presentation ",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073660,
"choiceText": "Hydroxychloroquine reduces potassium excretion by the kidneys",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Hypokalemia due to hydroxychloroquine appears to be a result of an intracellular shift rather than systemic depletion of potassium. Therefore, as the effects of hydroxychloroquine wear off, the potassium levels rise. For this reason, potassium repletion in patients of a hydroxychloroquine overdose should be done judiciously, with frequent checks of the potassium level. The potassium level should initially be corrected to a state of mild hypokalemia.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 339973,
"questionText": "Which mechanism may result in hyperkalemia in patients such as the one described above?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1073662,
"choiceText": "Eplerenone",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073664,
"choiceText": "Ramipril",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073666,
"choiceText": "Calcium gluconate",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073668,
"choiceText": "Kayexalate",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Eplerenone is a potassium-sparing diuretic, which increases serum potassium.<br/><br/>\r\nRamipril is an angiotensin-converting enzyme inhibitor, which works by inhibiting the conversion of angiotensin I to angiotensin II, ultimately inhibiting the production of aldosterone to reduce sodium and water retention. As sodium is lost through the Na-K channels, potassium is retained in the serum.<br/><br/>\r\nKayexalate is a potassium binder, which helps to remove potassium from the body. However, its onset of action is approximately 2-24 hours, which is not appropriate in an emergent setting. <br/><br/>\r\nCalcium gluconate has a rapid onset of approximately 5 minutes and is used to protect the myocardium in a hyperkalemic state. For this reason, calcium gluconate is the most appropriate choice.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 339975,
"questionText": "If a patient who experienced hydroxychloroquine overdose has potassium levels that are too aggressively corrected and experiences hyperkalemia, which agent may be indicated?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
976833 | /viewarticle/976833 | [
{
"authors": "Minh Chung; Eric Warren, DO; Darshan Rola; Brian Zacharias; Jennifer Broyles, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 59-year-old man with a past history of hypertension, hypokalemia, type 2 diabetes, hyperlipidemia, asthma, sleep apnea, and gastroesophageal reflux disease (GERD) presents for follow-up of his chronic conditions. During the two previous visits, his systolic blood pressure ranged between the 150s and the 170s, when measured in a sitting position. The patient reports that his blood pressure has always been elevated, and that the systolic pressure was in the high 130s at home.",
"He currently takes lisinopril 20 mg twice a day, hydrochlorothiazide 25 mg every morning, and extended-release nifedipine 90 mg once a day for uncontrolled hypertension. He takes extended-release potassium chloride 20 mEq twice a day for hypokalemia and metformin 500 mg twice a day for type 2 diabetes. Despite taking three antihypertensives from three different classes (an angiotensin-converting enzyme [ACE] inhibitor, a thiazide diuretic, and a calcium channel blocker), he continues to be hypertensive and to have hypokalemia, which requires potassium supplementation.",
"The patient does not report any associated symptoms of chest pain, shortness of breath, fatigue, palpitations, headaches, muscle weakness, or changes in vision. His family history is not significant for cardiovascular disease (CVD), hyperlipidemia, or diabetes. He has no history of tobacco use, illicit drug use, or alcohol consumption."
],
"date": "July 20, 2022",
"figures": [],
"markdown": "# A Man With Hypokalemia, Sleep Apnea, and Resistant Hypertension\n\n **Authors:** Minh Chung; Eric Warren, DO; Darshan Rola; Brian Zacharias; Jennifer Broyles, MD \n **Date:** July 20, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 59-year-old man with a past history of hypertension, hypokalemia, type 2 diabetes, hyperlipidemia, asthma, sleep apnea, and gastroesophageal reflux disease (GERD) presents for follow-up of his chronic conditions. During the two previous visits, his systolic blood pressure ranged between the 150s and the 170s, when measured in a sitting position. The patient reports that his blood pressure has always been elevated, and that the systolic pressure was in the high 130s at home.\nHe currently takes lisinopril 20 mg twice a day, hydrochlorothiazide 25 mg every morning, and extended-release nifedipine 90 mg once a day for uncontrolled hypertension. He takes extended-release potassium chloride 20 mEq twice a day for hypokalemia and metformin 500 mg twice a day for type 2 diabetes. Despite taking three antihypertensives from three different classes (an angiotensin-converting enzyme [ACE] inhibitor, a thiazide diuretic, and a calcium channel blocker), he continues to be hypertensive and to have hypokalemia, which requires potassium supplementation.\nThe patient does not report any associated symptoms of chest pain, shortness of breath, fatigue, palpitations, headaches, muscle weakness, or changes in vision. His family history is not significant for cardiovascular disease (CVD), hyperlipidemia, or diabetes. He has no history of tobacco use, illicit drug use, or alcohol consumption.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A Man With Hypokalemia, Sleep Apnea, and Resistant Hypertension"
},
{
"authors": "Minh Chung; Eric Warren, DO; Darshan Rola; Brian Zacharias; Jennifer Broyles, MD",
"content": [
"The patient's vital signs on his initial visit showed a blood pressure of 170/88 mm Hg and a repeat blood pressure of 162/80 mm Hg, a temperature of 98.8°F (37.1°C), a heart rate of 77 beats/min, a respiration rate of 18 breaths/min, and an oxygen saturation of 99% on room air. His height was 65 in (165.1 cm), his weight was 176 lb (79.8 kg), and his body mass index was 29.5 kg/m2.",
"Upon physical examination, the patient is well developed, well nourished, and in no acute distress. His head shows no trauma; his conjunctiva are clear. The skin is warm, with no rashes. His neck is supple, and the trachea is in midline. The lungs are clear to auscultation bilaterally. Heart rate and rhythm are regular, with no audible murmurs. Bowel sounds are normal, and no abdominal distention is noted. No focal neurologic deficits are detected. The patient does not have a shuffling or wide-based gait. His affect is normal, and he is oriented to person, place, and time.",
"A routine comprehensive metabolic panel (CMP), complete blood cell (CBC) count, albumin level, random urine sample with creatinine measurement, and lipid panel are ordered. The patient's CBC count is within the normal range. The CMP reveals the following values:",
"Calcium: 9.6 mg/dL (reference range, 8.5-10.5 mg/dL)",
"Glucose: 93 mg/dL (reference range, 65-110 mg/dL)",
"Blood urea nitrogen (BUN): 13 mg/dL (reference range, 8-24 mg/dL)",
"Total protein: 7.4 g/dL (reference range, 6-8.3 g/dL)",
"Albumin: 4.7 g/dL (reference range, 3.4 to 5.4 g/dL)",
"Total bilirubin: 0.3 mg/dL (reference range, 0.1-1.2 mg/dL)",
"Alkaline phosphatase: 76 IU/L (reference range, 44-147 IU/L)",
"Aspartate aminotransferase: 19 IU/L (reference range, 6-34 IU/L)",
"Alanine aminotransferase: 17 IU/L (reference range, 20-60 IU/L)",
"Potassium: 3.4 mmol/L (reference range, 3.5-5.5 mmol/L)",
"Sodium: 140 mmol/L (reference range, 135-147 mmol/L",
"Chloride: 99 mmol/L (reference range, 96-106 mmol/L)",
"Creatinine: 0.79 mg/dL (reference range, 0.9-1.3 mg/dL)",
"Total carbon dioxide: 27 mmol/L (reference range, 23-29 mmol/L)",
"BUN/creatinine ratio: 16 (reference range, 10-20)",
"Total globulin: 2.7 g/dL (reference range, 2.0-3.9 g/dL)",
"Albumin/globulin ratio: 1.7 (reference range, 1.1-2.5)",
"Estimated glomerular filtration rate (non–African American): 98 mL/min/1.73 m2 (reference range, > 90 mL/min/1.73 m2)",
"The patient's potassium level (3.4 mmol/L) is low despite potassium chloride supplementation. The urine albumin/creatinine ratio is elevated at 47 mg/g (reference range, < 30 mg/g). The lipid panel shows an elevated total cholesterol level of 203 mg/dL (reference range, < 200 mg/dL), a high triglyceride level of 183 mg/dL (reference range, < 150 mg/dL), and a high low-density lipoprotein cholesterol level of 126 mg/dL (reference range, < 100 mg/dL). The aldosterone-to-renin ratio is elevated at 75.5 (reference range, 0-30), as is the aldosterone level at 13.9 ng/dL (reference range, 2-9 ng/dL)."
],
"date": "July 20, 2022",
"figures": [],
"markdown": "# A Man With Hypokalemia, Sleep Apnea, and Resistant Hypertension\n\n **Authors:** Minh Chung; Eric Warren, DO; Darshan Rola; Brian Zacharias; Jennifer Broyles, MD \n **Date:** July 20, 2022\n\n ## Content\n\n The patient's vital signs on his initial visit showed a blood pressure of 170/88 mm Hg and a repeat blood pressure of 162/80 mm Hg, a temperature of 98.8°F (37.1°C), a heart rate of 77 beats/min, a respiration rate of 18 breaths/min, and an oxygen saturation of 99% on room air. His height was 65 in (165.1 cm), his weight was 176 lb (79.8 kg), and his body mass index was 29.5 kg/m2.\nUpon physical examination, the patient is well developed, well nourished, and in no acute distress. His head shows no trauma; his conjunctiva are clear. The skin is warm, with no rashes. His neck is supple, and the trachea is in midline. The lungs are clear to auscultation bilaterally. Heart rate and rhythm are regular, with no audible murmurs. Bowel sounds are normal, and no abdominal distention is noted. No focal neurologic deficits are detected. The patient does not have a shuffling or wide-based gait. His affect is normal, and he is oriented to person, place, and time.\nA routine comprehensive metabolic panel (CMP), complete blood cell (CBC) count, albumin level, random urine sample with creatinine measurement, and lipid panel are ordered. The patient's CBC count is within the normal range. The CMP reveals the following values:\nCalcium: 9.6 mg/dL (reference range, 8.5-10.5 mg/dL)\nGlucose: 93 mg/dL (reference range, 65-110 mg/dL)\nBlood urea nitrogen (BUN): 13 mg/dL (reference range, 8-24 mg/dL)\nTotal protein: 7.4 g/dL (reference range, 6-8.3 g/dL)\nAlbumin: 4.7 g/dL (reference range, 3.4 to 5.4 g/dL)\nTotal bilirubin: 0.3 mg/dL (reference range, 0.1-1.2 mg/dL)\nAlkaline phosphatase: 76 IU/L (reference range, 44-147 IU/L)\nAspartate aminotransferase: 19 IU/L (reference range, 6-34 IU/L)\nAlanine aminotransferase: 17 IU/L (reference range, 20-60 IU/L)\nPotassium: 3.4 mmol/L (reference range, 3.5-5.5 mmol/L)\nSodium: 140 mmol/L (reference range, 135-147 mmol/L\nChloride: 99 mmol/L (reference range, 96-106 mmol/L)\nCreatinine: 0.79 mg/dL (reference range, 0.9-1.3 mg/dL)\nTotal carbon dioxide: 27 mmol/L (reference range, 23-29 mmol/L)\nBUN/creatinine ratio: 16 (reference range, 10-20)\nTotal globulin: 2.7 g/dL (reference range, 2.0-3.9 g/dL)\nAlbumin/globulin ratio: 1.7 (reference range, 1.1-2.5)\nEstimated glomerular filtration rate (non–African American): 98 mL/min/1.73 m2 (reference range, > 90 mL/min/1.73 m2)\nThe patient's potassium level (3.4 mmol/L) is low despite potassium chloride supplementation. The urine albumin/creatinine ratio is elevated at 47 mg/g (reference range, < 30 mg/g). The lipid panel shows an elevated total cholesterol level of 203 mg/dL (reference range, < 200 mg/dL), a high triglyceride level of 183 mg/dL (reference range, < 150 mg/dL), and a high low-density lipoprotein cholesterol level of 126 mg/dL (reference range, < 100 mg/dL). The aldosterone-to-renin ratio is elevated at 75.5 (reference range, 0-30), as is the aldosterone level at 13.9 ng/dL (reference range, 2-9 ng/dL).\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1704463,
"choiceText": "Renal artery stenosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704464,
"choiceText": "Primary hyperaldosteronism",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704465,
"choiceText": "Cushing syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704466,
"choiceText": "Pheochromocytoma",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 549507,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Man With Hypokalemia, Sleep Apnea, and Resistant Hypertension"
},
{
"authors": "Minh Chung; Eric Warren, DO; Darshan Rola; Brian Zacharias; Jennifer Broyles, MD",
"content": [
"Hypertension is a worldwide pandemic. In 2010, 31.1% of adults had a systolic pressure ≥ 140 mm Hg and/or a diastolic pressure ≥ 90 mm Hg.[1] The prevalence continues to rise, along with the burden on patients and the healthcare system to prevent the complications of long-standing, uncontrolled disease.",
"Perhaps the most feared complication of hypertension is the associated cardiovascular morbidity and mortality. CVD continues to be the leading cause of mortality worldwide, and approximately half of CVD events are ascribed to hypertension.[2] This is an important public health issue because the evidence suggests that the risks and complications are largely preventable. When hypertension is treated and well controlled, the risk of all-cause and CVD-specific mortality is not significantly (or at all) increased. Therefore, hypertension must be promptly identified and managed in patients to prevent negative outcomes.",
"Hypertension is categorized as primary or secondary, based on whether the cause of the elevated blood pressure is identifiable. Primary hypertension, which accounts for about 90% of adult patients with high blood pressure, has an idiopathic etiology.[3] It is managed with nonpharmacologic and pharmacologic interventions, such as weight loss, increased physical activity, reduction in salt intake and, if necessary, antihypertensive agents, such as dihydropyridine calcium channel blockers, thiazide diuretics, ACE inhibitors, and angiotensin II receptor blockers.[4]",
"Although secondary causes should routinely be considered in patients with a new diagnosis of hypertension, certain clinical scenarios warrant further investigation. Some of these circumstances include resistant hypertension (defined as a blood pressure ≥ 140/90 mm Hg despite concurrent use of three antihypertensive medications from different classes, including a diuretic), onset at an age younger than 30 years, and acute worsening of blood pressure control.[3]",
"Secondary hypertension encompasses all potential causes of chronically elevated blood pressure, including renal artery stenosis, medications, renal parenchymal disease, obstructive sleep apnea, primary hyperaldosteronism, coarctation of the aorta, pheochromocytoma, Cushing syndrome, hypothyroidism, and hyperthyroidism.[3] Primary hyperaldosteronism is the most common cause of secondary hypertension, accounting for about 20% of all cases of resistant hypertension.[5]",
"Renal artery stenosis was considered as part of the differential diagnosis for this patient. Primary hyperaldosteronism and renal artery stenosis have many similarities, but key differences in the workup can distinguish the two conditions. Both involve hypertension that is usually refractory to typical blood pressure management, as well as hypokalemia and metabolic alkalosis. The key difference arises when the plasma aldosterone-to-renin ratio is measured. In renal artery stenosis, the renin-angiotensin-aldosterone system becomes activated secondary to the decreased afferent arteriole flow. In turn, the juxtaglomerular cells activate the renin cascade, leading to high levels of renin and aldosterone. This causes a low plasma aldosterone-to-renin ratio. In primary hyperaldosteronism, the ratio is high owing to the direct production of aldosterone, which provides negative feedback and reduces the levels of renin. A CT angiogram would reveal the stenosed renal artery, which could produce an audible bruit. A CT in a patient with primary hyperaldosteronism would show an adrenal adenoma rather than impairment of the renal artery. Moreover, an audible bruit would not be present.",
"Cushing syndrome was also considered in the differential diagnosis for this patient. Cushing syndrome can cause hypertension secondary to an increase in cortisol, which leads to suppression of the vasodilatory systems as well as some minor mineralocorticoid activity. Patients with this syndrome typically have distinct physical features, which were not present in this patient. Cushing syndrome can cause weight gain as well as fatty deposits in areas such as the face and interscapular area, leading to the typical moon facies and buffalo hump appearance. Striae would be present on the flanks, arms, and thighs as well. Thin, fragile skin that bruises easily is also present in some cases. Patients may experience muscle weakness and severe fatigue. To make a definitive diagnosis, a 24-hour urine cortisol sample or a late-night saliva cortisol sample can be obtained. Follow-up with a low-dose dexamethasone suppression test can help confirm the diagnosis if needed.",
"Pheochromocytomas are tumors that consist of chromaffin tissue and secrete catecholamines. These tumors can occur in the adrenal medulla or other extra-adrenal sites, such as the organ of Zuckerkandl. The symptoms that result from the excess of catecholamines are typically episodic. Patients can experience episodes of tachycardia, palpitations, chest pain, diaphoresis, hypertension, headache, tremor, and anxiety. The patient in this case was not experiencing episodic hypertension; instead, his hypertension was constant. Furthermore, he reported no chest pain, palpitations, or headache, which helped exclude this diagnosis. To confirm the diagnosis of pheochromocytoma, 24-hour urine levels of metanephrines and catecholamines or plasma-fractionated metanephrines levels can be measured. Elevated levels, in conjunction with the typical episodic physical symptoms, can help to make the final diagnosis."
],
"date": "July 20, 2022",
"figures": [],
"markdown": "# A Man With Hypokalemia, Sleep Apnea, and Resistant Hypertension\n\n **Authors:** Minh Chung; Eric Warren, DO; Darshan Rola; Brian Zacharias; Jennifer Broyles, MD \n **Date:** July 20, 2022\n\n ## Content\n\n Hypertension is a worldwide pandemic. In 2010, 31.1% of adults had a systolic pressure ≥ 140 mm Hg and/or a diastolic pressure ≥ 90 mm Hg.[1] The prevalence continues to rise, along with the burden on patients and the healthcare system to prevent the complications of long-standing, uncontrolled disease.\nPerhaps the most feared complication of hypertension is the associated cardiovascular morbidity and mortality. CVD continues to be the leading cause of mortality worldwide, and approximately half of CVD events are ascribed to hypertension.[2] This is an important public health issue because the evidence suggests that the risks and complications are largely preventable. When hypertension is treated and well controlled, the risk of all-cause and CVD-specific mortality is not significantly (or at all) increased. Therefore, hypertension must be promptly identified and managed in patients to prevent negative outcomes.\nHypertension is categorized as primary or secondary, based on whether the cause of the elevated blood pressure is identifiable. Primary hypertension, which accounts for about 90% of adult patients with high blood pressure, has an idiopathic etiology.[3] It is managed with nonpharmacologic and pharmacologic interventions, such as weight loss, increased physical activity, reduction in salt intake and, if necessary, antihypertensive agents, such as dihydropyridine calcium channel blockers, thiazide diuretics, ACE inhibitors, and angiotensin II receptor blockers.[4]\nAlthough secondary causes should routinely be considered in patients with a new diagnosis of hypertension, certain clinical scenarios warrant further investigation. Some of these circumstances include resistant hypertension (defined as a blood pressure ≥ 140/90 mm Hg despite concurrent use of three antihypertensive medications from different classes, including a diuretic), onset at an age younger than 30 years, and acute worsening of blood pressure control.[3]\nSecondary hypertension encompasses all potential causes of chronically elevated blood pressure, including renal artery stenosis, medications, renal parenchymal disease, obstructive sleep apnea, primary hyperaldosteronism, coarctation of the aorta, pheochromocytoma, Cushing syndrome, hypothyroidism, and hyperthyroidism.[3] Primary hyperaldosteronism is the most common cause of secondary hypertension, accounting for about 20% of all cases of resistant hypertension.[5]\nRenal artery stenosis was considered as part of the differential diagnosis for this patient. Primary hyperaldosteronism and renal artery stenosis have many similarities, but key differences in the workup can distinguish the two conditions. Both involve hypertension that is usually refractory to typical blood pressure management, as well as hypokalemia and metabolic alkalosis. The key difference arises when the plasma aldosterone-to-renin ratio is measured. In renal artery stenosis, the renin-angiotensin-aldosterone system becomes activated secondary to the decreased afferent arteriole flow. In turn, the juxtaglomerular cells activate the renin cascade, leading to high levels of renin and aldosterone. This causes a low plasma aldosterone-to-renin ratio. In primary hyperaldosteronism, the ratio is high owing to the direct production of aldosterone, which provides negative feedback and reduces the levels of renin. A CT angiogram would reveal the stenosed renal artery, which could produce an audible bruit. A CT in a patient with primary hyperaldosteronism would show an adrenal adenoma rather than impairment of the renal artery. Moreover, an audible bruit would not be present.\nCushing syndrome was also considered in the differential diagnosis for this patient. Cushing syndrome can cause hypertension secondary to an increase in cortisol, which leads to suppression of the vasodilatory systems as well as some minor mineralocorticoid activity. Patients with this syndrome typically have distinct physical features, which were not present in this patient. Cushing syndrome can cause weight gain as well as fatty deposits in areas such as the face and interscapular area, leading to the typical moon facies and buffalo hump appearance. Striae would be present on the flanks, arms, and thighs as well. Thin, fragile skin that bruises easily is also present in some cases. Patients may experience muscle weakness and severe fatigue. To make a definitive diagnosis, a 24-hour urine cortisol sample or a late-night saliva cortisol sample can be obtained. Follow-up with a low-dose dexamethasone suppression test can help confirm the diagnosis if needed.\nPheochromocytomas are tumors that consist of chromaffin tissue and secrete catecholamines. These tumors can occur in the adrenal medulla or other extra-adrenal sites, such as the organ of Zuckerkandl. The symptoms that result from the excess of catecholamines are typically episodic. Patients can experience episodes of tachycardia, palpitations, chest pain, diaphoresis, hypertension, headache, tremor, and anxiety. The patient in this case was not experiencing episodic hypertension; instead, his hypertension was constant. Furthermore, he reported no chest pain, palpitations, or headache, which helped exclude this diagnosis. To confirm the diagnosis of pheochromocytoma, 24-hour urine levels of metanephrines and catecholamines or plasma-fractionated metanephrines levels can be measured. Elevated levels, in conjunction with the typical episodic physical symptoms, can help to make the final diagnosis.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1704463,
"choiceText": "Renal artery stenosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704464,
"choiceText": "Primary hyperaldosteronism",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704465,
"choiceText": "Cushing syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704466,
"choiceText": "Pheochromocytoma",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 549507,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Man With Hypokalemia, Sleep Apnea, and Resistant Hypertension"
},
{
"authors": "Minh Chung; Eric Warren, DO; Darshan Rola; Brian Zacharias; Jennifer Broyles, MD",
"content": [
"Primary hyperaldosteronism is defined as an inappropriately elevated aldosterone level despite a low plasma renin level.[5] The excess aldosterone is produced through one of two main mechanisms: an aldosterone-producing adenoma of the right or left adrenal gland or bilateral hyperaldosteronism.[5]",
"Aldosterone, a product of the renin-angiotensin-aldosterone system in normal physiology, activates mineralocorticoid receptors expressed in various sites throughout the body, including endothelial cells, the hypothalamus, cardiomyocytes, and the kidneys.[5] The renal effect of mineralocorticoid receptor activation by aldosterone is the primary mechanism by which a hyperaldosterone state will lead to hypertension. Aldosterone acts at the distal tubule and cortical collecting duct to reabsorb sodium and water, which expands intravascular volume. This mechanism also drives the urinary secretion of potassium. In addition, aldosterone acts at the H+-ATPase of the alpha-intercalated cell at the cortical collecting duct, which stimulates the renal loss of hydrogen ions.[5]",
"Screening for primary hyperaldosteronism should be performed in high-risk patients, which includes those with resistant hypertension, hypertension and a family history of early-onset hypertension or a cerebrovascular accident at age younger than 40 years, hypertension and hypokalemia, and/or hypertension with an adrenal mass, according to the 2017 American College of Cardiology (ACC)/American Heart Association (AHA) hypertension guidelines.[6] Screening is widely performed with a serum aldosterone-to-renin ratio. A ratio > 20 is commonly accepted as a positive screening result.[5]",
"A positive screen warrants referral to an endocrinologist or other hypertension specialist to confirm the diagnosis of primary hyperaldosteronism and, if necessary, to identify the subtype. Confirmatory assessment is performed with the saline infusion test, which expands the intravascular volume. In a patient with normal physiology, volume expansion suppresses endogenous aldosterone production, whereas in a patient with primary hyperaldosteronism, the aldosterone level remains elevated.[5]"
],
"date": "July 20, 2022",
"figures": [],
"markdown": "# A Man With Hypokalemia, Sleep Apnea, and Resistant Hypertension\n\n **Authors:** Minh Chung; Eric Warren, DO; Darshan Rola; Brian Zacharias; Jennifer Broyles, MD \n **Date:** July 20, 2022\n\n ## Content\n\n Primary hyperaldosteronism is defined as an inappropriately elevated aldosterone level despite a low plasma renin level.[5] The excess aldosterone is produced through one of two main mechanisms: an aldosterone-producing adenoma of the right or left adrenal gland or bilateral hyperaldosteronism.[5]\nAldosterone, a product of the renin-angiotensin-aldosterone system in normal physiology, activates mineralocorticoid receptors expressed in various sites throughout the body, including endothelial cells, the hypothalamus, cardiomyocytes, and the kidneys.[5] The renal effect of mineralocorticoid receptor activation by aldosterone is the primary mechanism by which a hyperaldosterone state will lead to hypertension. Aldosterone acts at the distal tubule and cortical collecting duct to reabsorb sodium and water, which expands intravascular volume. This mechanism also drives the urinary secretion of potassium. In addition, aldosterone acts at the H+-ATPase of the alpha-intercalated cell at the cortical collecting duct, which stimulates the renal loss of hydrogen ions.[5]\nScreening for primary hyperaldosteronism should be performed in high-risk patients, which includes those with resistant hypertension, hypertension and a family history of early-onset hypertension or a cerebrovascular accident at age younger than 40 years, hypertension and hypokalemia, and/or hypertension with an adrenal mass, according to the 2017 American College of Cardiology (ACC)/American Heart Association (AHA) hypertension guidelines.[6] Screening is widely performed with a serum aldosterone-to-renin ratio. A ratio > 20 is commonly accepted as a positive screening result.[5]\nA positive screen warrants referral to an endocrinologist or other hypertension specialist to confirm the diagnosis of primary hyperaldosteronism and, if necessary, to identify the subtype. Confirmatory assessment is performed with the saline infusion test, which expands the intravascular volume. In a patient with normal physiology, volume expansion suppresses endogenous aldosterone production, whereas in a patient with primary hyperaldosteronism, the aldosterone level remains elevated.[5]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A Man With Hypokalemia, Sleep Apnea, and Resistant Hypertension"
},
{
"authors": "Minh Chung; Eric Warren, DO; Darshan Rola; Brian Zacharias; Jennifer Broyles, MD",
"content": [
"Primary hyperaldosteronism is often amenable to surgical intervention, which is usually the treatment of choice. Laparoscopic unilateral adrenalectomy for an aldosterone-producing adenoma of the right or left adrenal gland results in complete biochemical resolution of the disease state in about 94% of patients and partial or complete clinical success in approximately 85% of patients.[5] Bilateral hyperaldosteronism is significantly less amenable to unilateral adrenalectomy; the procedure is about half as successful in this setting compared with unilateral disease.",
"For patients who are unable or unwilling to undergo surgical intervention and for those with bilateral disease, medical therapy with a mineralocorticoid receptor antagonist can be initiated. Spironolactone can be used as a first-line agent. The long-term outcomes of patients with primary hyperaldosteronism who are treated with mineralocorticoid receptor antagonists are not clear, and some evidence suggests that they have a worse prognosis than do patients who are treated surgically.[5]",
"The patient in this case was referred to an endocrinologist for further workup and management. An MRI revealed a unilateral adrenal adenoma, which makes surgical removal the best option for this patient. Figure 1 shows an example of a section through an adrenal adenoma. If he is not fit for surgery or declines to have the operation, spironolactone can be used for medical management. Both methods will achieve adequate control of the patient's blood pressure. The overall prognosis is good, with minimal complications once the hypertension is well controlled with medical or surgical management.",
"Figure 1."
],
"date": "July 20, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/thumbnail_library/ps_220511_adrenal_gland_adenoma_282x180.jpg"
}
],
"markdown": "# A Man With Hypokalemia, Sleep Apnea, and Resistant Hypertension\n\n **Authors:** Minh Chung; Eric Warren, DO; Darshan Rola; Brian Zacharias; Jennifer Broyles, MD \n **Date:** July 20, 2022\n\n ## Content\n\n Primary hyperaldosteronism is often amenable to surgical intervention, which is usually the treatment of choice. Laparoscopic unilateral adrenalectomy for an aldosterone-producing adenoma of the right or left adrenal gland results in complete biochemical resolution of the disease state in about 94% of patients and partial or complete clinical success in approximately 85% of patients.[5] Bilateral hyperaldosteronism is significantly less amenable to unilateral adrenalectomy; the procedure is about half as successful in this setting compared with unilateral disease.\nFor patients who are unable or unwilling to undergo surgical intervention and for those with bilateral disease, medical therapy with a mineralocorticoid receptor antagonist can be initiated. Spironolactone can be used as a first-line agent. The long-term outcomes of patients with primary hyperaldosteronism who are treated with mineralocorticoid receptor antagonists are not clear, and some evidence suggests that they have a worse prognosis than do patients who are treated surgically.[5]\nThe patient in this case was referred to an endocrinologist for further workup and management. An MRI revealed a unilateral adrenal adenoma, which makes surgical removal the best option for this patient. Figure 1 shows an example of a section through an adrenal adenoma. If he is not fit for surgery or declines to have the operation, spironolactone can be used for medical management. Both methods will achieve adequate control of the patient's blood pressure. The overall prognosis is good, with minimal complications once the hypertension is well controlled with medical or surgical management.\nFigure 1.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1704467,
"choiceText": "CT of the pituitary",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704468,
"choiceText": "MRI of the abdomen",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704469,
"choiceText": "Urine metanephrine levels",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704470,
"choiceText": "Saline infusion test",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704471,
"choiceText": "Oral glucose suppression test",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "<p>The saline infusion test is a confirmatory test, unlike the aldosterone-to-renin ratio, which is a screening test for primary hyperaldosteronism. The saline infusion test verifies that aldosterone production is nonsuppressible and not regulated by the renin-angiotensin-aldosterone system. The saline infusion test is performed by first drawing blood for baseline laboratory studies (plasma renin ratio, plasma aldosterone concentration). Normal saline is then infused over 4 hours, and a repeat blood draw is done. Primary hyperaldosteronism is very probable in a patient with aldosterone levels that are > 10 ng/dL. Another confirmatory test such as an oral sodium-loading test can be done to test for primary hyperaldosteronism. Oral sodium loading involves a high-sodium diet for 3 days, which can cause severe hypertension.</p>\r\n\r\n<p>The aldosterone-to-renin ratio test is used to screen for primary hyperaldosteronism and to differentiate it from other causes of elevated aldosterone, such as secondary hyperaldosteronism. An imaging test, such as an adrenal CT or MRI, is performed once hyperaldosteronism is confirmed to help determine the underlying cause and to select treatment.</p>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 549508,
"questionText": "A 50-year-old man with uncontrolled hypertension presents with a 2-month history of progressive headaches and fatigue. He has had headaches for the past 3 years, and they have increased in intensity. He does not smoke or drink and has no other significant medical history. Serum studies show a morning renin level of 0.100 ng/mL/hr (reference range, 0.167-5.380 ng/mL/hr) and an aldosterone-to-renin ratio of 90 (reference range, 0-30). His potassium concentration is 3 mmol/L (reference range, 3.5-5.5 mmol/L). What test would confirm the suspected diagnosis of primary hyperaldosteronism?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1704472,
"choiceText": "Spironolactone",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704473,
"choiceText": "Surgery",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704474,
"choiceText": "Radiation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704475,
"choiceText": "Adding another antihypertensive",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704476,
"choiceText": "Eplerenone",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "<p>Spironolactone is an aldosterone receptor antagonist that is the first line of treatment for bilateral hyperaldosteronism. Because spironolactone is an aldosterone antagonist, it can cause hyperkalemia; thus, it will help treat the patient's hypokalemia. Adverse effects may include gynecomastia and decreased libido. Eplerenone is another medication used for medical management, but it is only half as potent as spironolactone in blocking the mineralocorticoid receptor and is less effective at lowering blood pressure.</p>\r\n\r\n<p>Adrenalectomy is indicated in unilateral adrenal hyperaldosteronism because the unaffected gland can compensate for the loss of hormones. In a bilateral adrenalectomy, both adrenal glands are removed, leaving an uncompensated hormone deficit. Bilateral adrenalectomy would require lifelong glucocorticoid and mineralocorticoid replacement.</p>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 549509,
"questionText": "The patient described in Question 1 is confirmed to have primary hyperaldosteronism, and an adrenal CT shows large (5-cm) masses bilaterally. What is the first-line treatment for this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Man With Hypokalemia, Sleep Apnea, and Resistant Hypertension"
},
{
"authors": "Minh Chung; Eric Warren, DO; Darshan Rola; Brian Zacharias; Jennifer Broyles, MD",
"content": [
"Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult."
],
"date": "July 20, 2022",
"figures": [],
"markdown": "# A Man With Hypokalemia, Sleep Apnea, and Resistant Hypertension\n\n **Authors:** Minh Chung; Eric Warren, DO; Darshan Rola; Brian Zacharias; Jennifer Broyles, MD \n **Date:** July 20, 2022\n\n ## Content\n\n Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult.\n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1704467,
"choiceText": "CT of the pituitary",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704468,
"choiceText": "MRI of the abdomen",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704469,
"choiceText": "Urine metanephrine levels",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704470,
"choiceText": "Saline infusion test",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704471,
"choiceText": "Oral glucose suppression test",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "<p>The saline infusion test is a confirmatory test, unlike the aldosterone-to-renin ratio, which is a screening test for primary hyperaldosteronism. The saline infusion test verifies that aldosterone production is nonsuppressible and not regulated by the renin-angiotensin-aldosterone system. The saline infusion test is performed by first drawing blood for baseline laboratory studies (plasma renin ratio, plasma aldosterone concentration). Normal saline is then infused over 4 hours, and a repeat blood draw is done. Primary hyperaldosteronism is very probable in a patient with aldosterone levels that are > 10 ng/dL. Another confirmatory test such as an oral sodium-loading test can be done to test for primary hyperaldosteronism. Oral sodium loading involves a high-sodium diet for 3 days, which can cause severe hypertension.</p>\r\n\r\n<p>The aldosterone-to-renin ratio test is used to screen for primary hyperaldosteronism and to differentiate it from other causes of elevated aldosterone, such as secondary hyperaldosteronism. An imaging test, such as an adrenal CT or MRI, is performed once hyperaldosteronism is confirmed to help determine the underlying cause and to select treatment.</p>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 549508,
"questionText": "A 50-year-old man with uncontrolled hypertension presents with a 2-month history of progressive headaches and fatigue. He has had headaches for the past 3 years, and they have increased in intensity. He does not smoke or drink and has no other significant medical history. Serum studies show a morning renin level of 0.100 ng/mL/hr (reference range, 0.167-5.380 ng/mL/hr) and an aldosterone-to-renin ratio of 90 (reference range, 0-30). His potassium concentration is 3 mmol/L (reference range, 3.5-5.5 mmol/L). What test would confirm the suspected diagnosis of primary hyperaldosteronism?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1704472,
"choiceText": "Spironolactone",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704473,
"choiceText": "Surgery",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704474,
"choiceText": "Radiation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704475,
"choiceText": "Adding another antihypertensive",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704476,
"choiceText": "Eplerenone",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "<p>Spironolactone is an aldosterone receptor antagonist that is the first line of treatment for bilateral hyperaldosteronism. Because spironolactone is an aldosterone antagonist, it can cause hyperkalemia; thus, it will help treat the patient's hypokalemia. Adverse effects may include gynecomastia and decreased libido. Eplerenone is another medication used for medical management, but it is only half as potent as spironolactone in blocking the mineralocorticoid receptor and is less effective at lowering blood pressure.</p>\r\n\r\n<p>Adrenalectomy is indicated in unilateral adrenal hyperaldosteronism because the unaffected gland can compensate for the loss of hormones. In a bilateral adrenalectomy, both adrenal glands are removed, leaving an uncompensated hormone deficit. Bilateral adrenalectomy would require lifelong glucocorticoid and mineralocorticoid replacement.</p>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 549509,
"questionText": "The patient described in Question 1 is confirmed to have primary hyperaldosteronism, and an adrenal CT shows large (5-cm) masses bilaterally. What is the first-line treatment for this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Man With Hypokalemia, Sleep Apnea, and Resistant Hypertension"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1704463,
"choiceText": "Renal artery stenosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704464,
"choiceText": "Primary hyperaldosteronism",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704465,
"choiceText": "Cushing syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704466,
"choiceText": "Pheochromocytoma",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 549507,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1704467,
"choiceText": "CT of the pituitary",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704468,
"choiceText": "MRI of the abdomen",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704469,
"choiceText": "Urine metanephrine levels",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704470,
"choiceText": "Saline infusion test",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704471,
"choiceText": "Oral glucose suppression test",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "<p>The saline infusion test is a confirmatory test, unlike the aldosterone-to-renin ratio, which is a screening test for primary hyperaldosteronism. The saline infusion test verifies that aldosterone production is nonsuppressible and not regulated by the renin-angiotensin-aldosterone system. The saline infusion test is performed by first drawing blood for baseline laboratory studies (plasma renin ratio, plasma aldosterone concentration). Normal saline is then infused over 4 hours, and a repeat blood draw is done. Primary hyperaldosteronism is very probable in a patient with aldosterone levels that are > 10 ng/dL. Another confirmatory test such as an oral sodium-loading test can be done to test for primary hyperaldosteronism. Oral sodium loading involves a high-sodium diet for 3 days, which can cause severe hypertension.</p>\r\n\r\n<p>The aldosterone-to-renin ratio test is used to screen for primary hyperaldosteronism and to differentiate it from other causes of elevated aldosterone, such as secondary hyperaldosteronism. An imaging test, such as an adrenal CT or MRI, is performed once hyperaldosteronism is confirmed to help determine the underlying cause and to select treatment.</p>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 549508,
"questionText": "A 50-year-old man with uncontrolled hypertension presents with a 2-month history of progressive headaches and fatigue. He has had headaches for the past 3 years, and they have increased in intensity. He does not smoke or drink and has no other significant medical history. Serum studies show a morning renin level of 0.100 ng/mL/hr (reference range, 0.167-5.380 ng/mL/hr) and an aldosterone-to-renin ratio of 90 (reference range, 0-30). His potassium concentration is 3 mmol/L (reference range, 3.5-5.5 mmol/L). What test would confirm the suspected diagnosis of primary hyperaldosteronism?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1704472,
"choiceText": "Spironolactone",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704473,
"choiceText": "Surgery",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704474,
"choiceText": "Radiation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704475,
"choiceText": "Adding another antihypertensive",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1704476,
"choiceText": "Eplerenone",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "<p>Spironolactone is an aldosterone receptor antagonist that is the first line of treatment for bilateral hyperaldosteronism. Because spironolactone is an aldosterone antagonist, it can cause hyperkalemia; thus, it will help treat the patient's hypokalemia. Adverse effects may include gynecomastia and decreased libido. Eplerenone is another medication used for medical management, but it is only half as potent as spironolactone in blocking the mineralocorticoid receptor and is less effective at lowering blood pressure.</p>\r\n\r\n<p>Adrenalectomy is indicated in unilateral adrenal hyperaldosteronism because the unaffected gland can compensate for the loss of hormones. In a bilateral adrenalectomy, both adrenal glands are removed, leaving an uncompensated hormone deficit. Bilateral adrenalectomy would require lifelong glucocorticoid and mineralocorticoid replacement.</p>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 549509,
"questionText": "The patient described in Question 1 is confirmed to have primary hyperaldosteronism, and an adrenal CT shows large (5-cm) masses bilaterally. What is the first-line treatment for this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
858606 | /viewarticle/858606 | [
{
"authors": "Alexander B. Norinsky, DO; Andrew Caravello, DO; James Espinosa, MD",
"content": [
"Editor's Note:\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 43-year-old man who is nontoxic but somewhat uncomfortable presents to the emergency department (ED) with dyspnea secondary to swelling in his left neck region. He also has progressive difficulty tolerating his secretions and swallowing. He initially noted the swelling earlier that night while trying to eat dinner when he was unable to swallow. He also describes his voice becoming progressively muffled over the past few days and foul-smelling breath.",
"He does not have fever, chills, sore throat, congestion, rhinorrhea, pain elsewhere, or any other symptoms. He has no recent history of tooth extractions or dental procedures. He has never experienced anything similar and, prior to this event, reports being in his normal state of health, without any illnesses or known sick contacts or exposures.",
"He has no significant medical history; however, he has not seen a primary care physician in more than 10 years. The patient has had no surgeries. His family history is unavailable because he was adopted and is unaware of the health status of his biological parents. Social history is significant for smoking one pack of cigarettes daily for about 15 years, without any illicit drug or alcohol abuse. He has no known drug allergies and does not routinely take any medications."
],
"date": "July 14, 2022",
"figures": [],
"markdown": "# An Adopted 43-Year-Old With Bad Breath, Dyspnea, Dysphagia\n\n **Authors:** Alexander B. Norinsky, DO; Andrew Caravello, DO; James Espinosa, MD \n **Date:** July 14, 2022\n\n ## Content\n\n Editor's Note:\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 43-year-old man who is nontoxic but somewhat uncomfortable presents to the emergency department (ED) with dyspnea secondary to swelling in his left neck region. He also has progressive difficulty tolerating his secretions and swallowing. He initially noted the swelling earlier that night while trying to eat dinner when he was unable to swallow. He also describes his voice becoming progressively muffled over the past few days and foul-smelling breath.\nHe does not have fever, chills, sore throat, congestion, rhinorrhea, pain elsewhere, or any other symptoms. He has no recent history of tooth extractions or dental procedures. He has never experienced anything similar and, prior to this event, reports being in his normal state of health, without any illnesses or known sick contacts or exposures.\nHe has no significant medical history; however, he has not seen a primary care physician in more than 10 years. The patient has had no surgeries. His family history is unavailable because he was adopted and is unaware of the health status of his biological parents. Social history is significant for smoking one pack of cigarettes daily for about 15 years, without any illicit drug or alcohol abuse. He has no known drug allergies and does not routinely take any medications.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "An Adopted 43-Year-Old With Bad Breath, Dyspnea, Dysphagia"
},
{
"authors": "Alexander B. Norinsky, DO; Andrew Caravello, DO; James Espinosa, MD",
"content": [
"The patient is a well-nourished male sitting upright in the stretcher. Upon initial triage and evaluation, he is in no obvious distress but appears somewhat uncomfortable and is cooperative with the examination. His blood pressure is 156/95 mm Hg, his pulse is 112 beats/min with a regular rhythm, his respiratory rate is 18 breaths/min, and his temperature (measured orally) is 98.5°F (36.9°C).",
"Physical examination findings are significant for an erythematous posterior pharynx without exudates. No trismus or stridor is present, and the patient is not in the tripod position, preferring to remain erect. He has poor dentition, with a foul-smelling odor. A hoarse voice is noted. No visible or palpable intraoral abscesses are observed; however, examination is somewhat limited secondary to poor patient compliance.",
"The uvula is midline and nonedematous. No tongue or sublingual elevation is noted, nor is any brawny edema observed on examination of neck. Several anterior cervical lymph nodes are identified bilaterally, as well as tenderness to palpation, with swelling around the left side of the upper neck and mandibular angle. Thyromegaly is not observed. The patient exhibits full range of motion of the neck; his cardiopulmonary and abdominal examination, along with the other systems, is unremarkable.",
"Flexible fiberoptic nasolaryngoscopy is immediately performed at bedside, revealing an injected oropharynx with a fair amount of parapharyngeal and retropharyngeal swelling with airway deviation. Given his relative comfort level after administration of intravenous fluids, dexamethasone, and morphine, as well as several sets of stable vital signs and concerning but stable nasolaryngoscopic examination findings, the decision is made to fully image the airway and surrounding structures with a CT scan of the neck and soft tissues with intravenous contrast (Figures 1-4).",
"Figure 1.",
"Figure 1.",
"Figure 2.",
"Figure 2.",
"Figure 3.",
"Figure 3.",
"Figure 4",
"Figure 4",
"Bloodwork is significant for mild leukocytosis (white blood cell count, 11,800/µL; reference range, 3700-10,500/µL) with neutrophilic predominance (9900/µL; reference range, 2100-6700/µL). Outside of that finding, the complete blood count, basic metabolic panel, coagulation profile, and lactate findings are within normal limits. Throat and blood cultures are obtained as well."
],
"date": "July 14, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/858/606/858606-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/858/606/858606-Thumb2.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/858/606/858606-Thumb3.png"
},
{
"caption": "Figure 4",
"image_url": "https://img.medscapestatic.com/article/858/606/858606-Thumb4.png"
}
],
"markdown": "# An Adopted 43-Year-Old With Bad Breath, Dyspnea, Dysphagia\n\n **Authors:** Alexander B. Norinsky, DO; Andrew Caravello, DO; James Espinosa, MD \n **Date:** July 14, 2022\n\n ## Content\n\n The patient is a well-nourished male sitting upright in the stretcher. Upon initial triage and evaluation, he is in no obvious distress but appears somewhat uncomfortable and is cooperative with the examination. His blood pressure is 156/95 mm Hg, his pulse is 112 beats/min with a regular rhythm, his respiratory rate is 18 breaths/min, and his temperature (measured orally) is 98.5°F (36.9°C).\nPhysical examination findings are significant for an erythematous posterior pharynx without exudates. No trismus or stridor is present, and the patient is not in the tripod position, preferring to remain erect. He has poor dentition, with a foul-smelling odor. A hoarse voice is noted. No visible or palpable intraoral abscesses are observed; however, examination is somewhat limited secondary to poor patient compliance.\nThe uvula is midline and nonedematous. No tongue or sublingual elevation is noted, nor is any brawny edema observed on examination of neck. Several anterior cervical lymph nodes are identified bilaterally, as well as tenderness to palpation, with swelling around the left side of the upper neck and mandibular angle. Thyromegaly is not observed. The patient exhibits full range of motion of the neck; his cardiopulmonary and abdominal examination, along with the other systems, is unremarkable.\nFlexible fiberoptic nasolaryngoscopy is immediately performed at bedside, revealing an injected oropharynx with a fair amount of parapharyngeal and retropharyngeal swelling with airway deviation. Given his relative comfort level after administration of intravenous fluids, dexamethasone, and morphine, as well as several sets of stable vital signs and concerning but stable nasolaryngoscopic examination findings, the decision is made to fully image the airway and surrounding structures with a CT scan of the neck and soft tissues with intravenous contrast (Figures 1-4).\nFigure 1.\nFigure 1.\nFigure 2.\nFigure 2.\nFigure 3.\nFigure 3.\nFigure 4\nFigure 4\nBloodwork is significant for mild leukocytosis (white blood cell count, 11,800/µL; reference range, 3700-10,500/µL) with neutrophilic predominance (9900/µL; reference range, 2100-6700/µL). Outside of that finding, the complete blood count, basic metabolic panel, coagulation profile, and lactate findings are within normal limits. Throat and blood cultures are obtained as well.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 942123,
"choiceText": "Lemierre syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942125,
"choiceText": "Parapharyngeal/retropharyngeal cellulitis and abscess formation",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942127,
"choiceText": "Ludwig angina",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942129,
"choiceText": "Epiglottitis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942131,
"choiceText": "Bacterial tracheitis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 298079,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "An Adopted 43-Year-Old With Bad Breath, Dyspnea, Dysphagia"
},
{
"authors": "Alexander B. Norinsky, DO; Andrew Caravello, DO; James Espinosa, MD",
"content": [
"The patient's airway was compromised secondary to parapharyngeal abscess and cellulitis due to Haemophilus influenzae infection.",
"Lemierre syndrome is a rare clinical entity wherein bacterial infection (specifically Fusobacterium necrophorum) spreads from the peritonsillar spaces to involve the internal jugular vein, causing a purulent thrombophlebitis with potential for embolization. A contrast-enhanced CT scan of the neck exhibits distended jugular veins, with wall enhancement and intraluminal filling defects. Ultrasonography may be considered as well, with diagnosis confirmed by exhibiting the bacteria on blood cultures. Management includes antibiotics, abscess drainage, and internal jugular vein ligation or excision.",
"Ludwig angina is a gangrenous cellulitis of the soft tissues of the mouth's floor and neck, classically characterized following a dental procedure. Specifically, infection extends directly from the second or third molar via the submandibular, sublingual, submaxillary, and retropharyngeal spaces. It is very aggressive, and management principles are similar to retropharyngeal abscesses: airway stabilization and early empiric antibiotic coverage. Implicated bacteria, as in retropharyngeal infections, are polymicrobial (eg, \nStaphylococcus\n, \nStreptococcus\n, \nBacteroides\n). Although often seen in the healthy population, the immunocompromised demographic (eg, those with diabetes, alcoholism, or autoimmune conditions) is particularly susceptible. Historically, mortality was found to be as high as 50%; that statistic has decreased to less than 10%.",
"Epiglottitis is rapidly progressive inflammation of the supraglottic structures (epiglottis, arytenoids, and aryepiglottic folds). As with retropharyngeal infections, H influenzae used to be the most commonly cited bacteria; however, the H influenzae type b (Hib) vaccine has significantly limited the incidence and severity of epiglottitis nowadays. As opposed to retropharyngeal space infections, direct visualization via nasopharyngoscopy of the inflamed epiglottis and periepiglottic structures remains the preferred modality for diagnosis and trending progress/management. The classic finding on lateral neck radiographs is the \"thumb sign\" (swollen epiglottis) as well as thickened aryepiglottic folds and loss of the vallecular space. One study found excellent sensitivity and specificity parameters when using 7 mm thickness of the epiglottis and 4.5 mm of the aryepiglottic folds as cutoffs.[1]",
"Bacterial tracheitis is also a relatively infrequent clinical entity, with the most commonly encountered clinical vignette involving a pediatric patient with classic croup-like symptoms that do not respond to croup interventions. The length of the oropharynx may be affected; the cricoid cartilage is the most critically important site because it is the narrowest point of the pediatric trachea. The most commonly cited pathogens include Staphylococcus aureus, Streptococcus species, \nKlebsiella\n, Peptostreptococcus, Bacteroides, and anaerobes; the leading cause is \nMoraxella catarrhalis\n.",
"To diagnose parapharyngeal abscess with cellulitis, the practitioner must maintain a high index of suspicion. Physical examination findings are notoriously unreliable; one series found as few as 37% of case reports reviewed noting visible swelling of the posterior pharynx.[2] Negative examination findings with high suspicion mandate further investigation. This case is similar; the most important and concerning physical examination finding in this patient was preference for erect positioning despite discomfort. Other less specific but relevant findings included the erythematous posterior pharynx, poor dentition, foul-smelling odor, and hoarse voice."
],
"date": "July 14, 2022",
"figures": [],
"markdown": "# An Adopted 43-Year-Old With Bad Breath, Dyspnea, Dysphagia\n\n **Authors:** Alexander B. Norinsky, DO; Andrew Caravello, DO; James Espinosa, MD \n **Date:** July 14, 2022\n\n ## Content\n\n The patient's airway was compromised secondary to parapharyngeal abscess and cellulitis due to Haemophilus influenzae infection.\nLemierre syndrome is a rare clinical entity wherein bacterial infection (specifically Fusobacterium necrophorum) spreads from the peritonsillar spaces to involve the internal jugular vein, causing a purulent thrombophlebitis with potential for embolization. A contrast-enhanced CT scan of the neck exhibits distended jugular veins, with wall enhancement and intraluminal filling defects. Ultrasonography may be considered as well, with diagnosis confirmed by exhibiting the bacteria on blood cultures. Management includes antibiotics, abscess drainage, and internal jugular vein ligation or excision.\nLudwig angina is a gangrenous cellulitis of the soft tissues of the mouth's floor and neck, classically characterized following a dental procedure. Specifically, infection extends directly from the second or third molar via the submandibular, sublingual, submaxillary, and retropharyngeal spaces. It is very aggressive, and management principles are similar to retropharyngeal abscesses: airway stabilization and early empiric antibiotic coverage. Implicated bacteria, as in retropharyngeal infections, are polymicrobial (eg, \nStaphylococcus\n, \nStreptococcus\n, \nBacteroides\n). Although often seen in the healthy population, the immunocompromised demographic (eg, those with diabetes, alcoholism, or autoimmune conditions) is particularly susceptible. Historically, mortality was found to be as high as 50%; that statistic has decreased to less than 10%.\nEpiglottitis is rapidly progressive inflammation of the supraglottic structures (epiglottis, arytenoids, and aryepiglottic folds). As with retropharyngeal infections, H influenzae used to be the most commonly cited bacteria; however, the H influenzae type b (Hib) vaccine has significantly limited the incidence and severity of epiglottitis nowadays. As opposed to retropharyngeal space infections, direct visualization via nasopharyngoscopy of the inflamed epiglottis and periepiglottic structures remains the preferred modality for diagnosis and trending progress/management. The classic finding on lateral neck radiographs is the \"thumb sign\" (swollen epiglottis) as well as thickened aryepiglottic folds and loss of the vallecular space. One study found excellent sensitivity and specificity parameters when using 7 mm thickness of the epiglottis and 4.5 mm of the aryepiglottic folds as cutoffs.[1]\nBacterial tracheitis is also a relatively infrequent clinical entity, with the most commonly encountered clinical vignette involving a pediatric patient with classic croup-like symptoms that do not respond to croup interventions. The length of the oropharynx may be affected; the cricoid cartilage is the most critically important site because it is the narrowest point of the pediatric trachea. The most commonly cited pathogens include Staphylococcus aureus, Streptococcus species, \nKlebsiella\n, Peptostreptococcus, Bacteroides, and anaerobes; the leading cause is \nMoraxella catarrhalis\n.\nTo diagnose parapharyngeal abscess with cellulitis, the practitioner must maintain a high index of suspicion. Physical examination findings are notoriously unreliable; one series found as few as 37% of case reports reviewed noting visible swelling of the posterior pharynx.[2] Negative examination findings with high suspicion mandate further investigation. This case is similar; the most important and concerning physical examination finding in this patient was preference for erect positioning despite discomfort. Other less specific but relevant findings included the erythematous posterior pharynx, poor dentition, foul-smelling odor, and hoarse voice.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 942123,
"choiceText": "Lemierre syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942125,
"choiceText": "Parapharyngeal/retropharyngeal cellulitis and abscess formation",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942127,
"choiceText": "Ludwig angina",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942129,
"choiceText": "Epiglottitis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942131,
"choiceText": "Bacterial tracheitis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 298079,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "An Adopted 43-Year-Old With Bad Breath, Dyspnea, Dysphagia"
},
{
"authors": "Alexander B. Norinsky, DO; Andrew Caravello, DO; James Espinosa, MD",
"content": [
"Retropharyngeal cellulitis and abscesses are often secondary to polymicrobial infection; the most commonly encountered species are Streptococcus (beta-hemolytic and pyogenes), S aureus, H influenza, and Klebsiella pneumoniae, along with several others (eg, Neisseria, Peptococcus, Bacteroides, and Fusobacterium).",
"Despite its name, H influenzae is not a virus but a Gram-negative bacillus commonly found to be the cause of pneumonia, meningitis, and skin-soft tissue infections, especially in the pediatric population.[3] Prior to routine vaccination of Hib in 1985, as many as 1 in 200 children developed this disease before age 5 years; it has since diminished considerably.[4,5,6] Most cases in adults are nontypable species seen in the context of an immunocompromised state (eg, diabetes, alcoholism, neoplasm) and/or longstanding lung disease (eg, chronic obstructive pulmonary disease, smoking).",
"Imaging modalities (plain radiography and CT scanning) help confirm the diagnosis, exclude other diagnoses and/or confounding factors, and trend progress of treatment. When imaging these patients, one must be familiar with the potential spaces lying behind the oropharynx as that helps to localize the infection and predict the potential spread if not adequately treated. Immediately behind the visceral fascia, as one goes beyond the posterior pharynx, lies the retropharyngeal space, specifically between the middle layers of the deep cervical fascia. That is followed by the alar fascia of the prevertebral fascia. The retropharyngeal space extends from the base of the skull inferiorly to C7 or T1, with the carotid sheath running laterally. The space contains lymph nodes that regress after childhood (usually after age 4 years). This might explain the low incidence of retropharyngeal abscess development in adults. Beyond this space, one encounters the prevertebral fascia and space, followed by the vertebral bodies.",
"In one study, lateral neck radiographs were abnormal in as many as 86% of presentations.[7] Findings include swelling in the retropharyngeal space; the most commonly quoted figures are >7 mm at the level of C2 and 22 mm at the level of C6, regardless of age. Of note, the advancement of CT technology and resolution capabilities has made it a very useful modality, helping to differentiate cellulitis in the retropharyngeal space from abscess formation and visualize the extent of the disease. It is also a helpful planning tool for the surgeon. Contrast enhancement has excellent sensitivity (more than 90%); however, several reviews found a significantly poor specificity (as low as 60%), with difficulty differentiating lymphadenopathy from abscess formation or cellulitis.[8] Findings on CT include cavitary ring enhancement, air-fluid levels, and development of subcutaneous air.",
"Laboratory findings (ie, inflammatory markers such as leukocytosis and an elevated C-reactive protein) generally don't mirror the extent or severity of disease in minor-to-moderate cases and should generally be reserved for severe cases. Local cultures are useful for narrowing antibiotic coverage once speciation becomes available. Morbidity and mortality are usually secondary to complications from the predicted course of extension of infection via the fascial planes: epidural abscesses, cranial nerve dysfunction, cavernous venous sinus thrombosis, mediastinitis, and spread into the vasculature (carotid artery or jugular vein), as well as inflicting mass effect on the airway (as seen in this case)."
],
"date": "July 14, 2022",
"figures": [],
"markdown": "# An Adopted 43-Year-Old With Bad Breath, Dyspnea, Dysphagia\n\n **Authors:** Alexander B. Norinsky, DO; Andrew Caravello, DO; James Espinosa, MD \n **Date:** July 14, 2022\n\n ## Content\n\n Retropharyngeal cellulitis and abscesses are often secondary to polymicrobial infection; the most commonly encountered species are Streptococcus (beta-hemolytic and pyogenes), S aureus, H influenza, and Klebsiella pneumoniae, along with several others (eg, Neisseria, Peptococcus, Bacteroides, and Fusobacterium).\nDespite its name, H influenzae is not a virus but a Gram-negative bacillus commonly found to be the cause of pneumonia, meningitis, and skin-soft tissue infections, especially in the pediatric population.[3] Prior to routine vaccination of Hib in 1985, as many as 1 in 200 children developed this disease before age 5 years; it has since diminished considerably.[4,5,6] Most cases in adults are nontypable species seen in the context of an immunocompromised state (eg, diabetes, alcoholism, neoplasm) and/or longstanding lung disease (eg, chronic obstructive pulmonary disease, smoking).\nImaging modalities (plain radiography and CT scanning) help confirm the diagnosis, exclude other diagnoses and/or confounding factors, and trend progress of treatment. When imaging these patients, one must be familiar with the potential spaces lying behind the oropharynx as that helps to localize the infection and predict the potential spread if not adequately treated. Immediately behind the visceral fascia, as one goes beyond the posterior pharynx, lies the retropharyngeal space, specifically between the middle layers of the deep cervical fascia. That is followed by the alar fascia of the prevertebral fascia. The retropharyngeal space extends from the base of the skull inferiorly to C7 or T1, with the carotid sheath running laterally. The space contains lymph nodes that regress after childhood (usually after age 4 years). This might explain the low incidence of retropharyngeal abscess development in adults. Beyond this space, one encounters the prevertebral fascia and space, followed by the vertebral bodies.\nIn one study, lateral neck radiographs were abnormal in as many as 86% of presentations.[7] Findings include swelling in the retropharyngeal space; the most commonly quoted figures are >7 mm at the level of C2 and 22 mm at the level of C6, regardless of age. Of note, the advancement of CT technology and resolution capabilities has made it a very useful modality, helping to differentiate cellulitis in the retropharyngeal space from abscess formation and visualize the extent of the disease. It is also a helpful planning tool for the surgeon. Contrast enhancement has excellent sensitivity (more than 90%); however, several reviews found a significantly poor specificity (as low as 60%), with difficulty differentiating lymphadenopathy from abscess formation or cellulitis.[8] Findings on CT include cavitary ring enhancement, air-fluid levels, and development of subcutaneous air.\nLaboratory findings (ie, inflammatory markers such as leukocytosis and an elevated C-reactive protein) generally don't mirror the extent or severity of disease in minor-to-moderate cases and should generally be reserved for severe cases. Local cultures are useful for narrowing antibiotic coverage once speciation becomes available. Morbidity and mortality are usually secondary to complications from the predicted course of extension of infection via the fascial planes: epidural abscesses, cranial nerve dysfunction, cavernous venous sinus thrombosis, mediastinitis, and spread into the vasculature (carotid artery or jugular vein), as well as inflicting mass effect on the airway (as seen in this case).\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "An Adopted 43-Year-Old With Bad Breath, Dyspnea, Dysphagia"
},
{
"authors": "Alexander B. Norinsky, DO; Andrew Caravello, DO; James Espinosa, MD",
"content": [
"Intraoral infections, including retropharyngeal and parapharyngeal abscesses, pose a potentially life-threatening difficult airway situation. The immediate proximity to the upper airways and potential for rapid progression (even with minor edema or deviation) may result in near-total or complete obstruction, demanding immediate intervention measures and airway stabilization.",
"In the ideal scenario, an endotracheal or nasotracheal airway should be established in the operating theater under the auspices of the anesthesiology services, with involvement of the otolaryngology or surgical services readily available should the need for a surgical airway become necessary. If these services aren't immediately available, awake intubation should be attempted to optimize success. Furthermore, given the tenuous nature of the patient's stability, and given the potential for rapid progression (as seen in this case), practitioners should be keen on securing the airway sooner than later; if possible, they should discuss with the patient the risk/benefit ratio for an early urgent intubation vs the potential of a later emergent procedure should he or she decompensate.",
"Numerous pharmacologic agents are available to maximize successful airway control, be it endotracheal, nasotracheal, or otherwise. First-pass success is always the goal; the best environment to maximize these conditions is an adequate degree of patient sedation while still maintaining their respiratory effort and hemodynamics. The best approach should include a combination of dissociative sedatives, anesthetics, and adjunctive agents. Ketamine and etomidate allow for an adequate degree of sedation/dissociation while maintaining respiratory and cardiopulmonary parameters. Benzodiazepines, fentanyl, and dexmedetomidine may be used as well to allow appropriate relaxation on the part of the patient, but with caution, as they affect the respiratory drive and may augment blood pressure and heart rate.",
"Anesthetics are an important and often underused class of medications that can help maximize first-pass success as well. Several routes of administration are available, including the following:",
"Topical (in the posterior oropharynx and/or nares);",
"Nebulized/atomized form; and",
"Local nerve blocks (eg, glossopharyngeal, superior laryngeal, recurrent laryngeal nerves).",
"Used alone or in combination, these can offer the patient a great degree of comfort and tolerance during the procedure and maintenance of the tube. Finally, one may consider using adjunctive agents to facilitate intubation; antisialagogues (eg, glycopyrrolate or atropine) help combat excessive secretions and offer good visualization, and steroids (eg, dexamethasone) can help reduce airway edema.",
"Of note, paralytics may be used very judiciously in these cases, as an edematous incompetent airway that collapses may be disastrous. As with all medications, the practitioner needs to be aware of appropriate dosing regimens, depending on the degree of sedation required, as well as any potential interactions with other agents and the patient's diagnosis and underlying medical conditions.",
"Numerous approaches are available: direct laryngoscopy, fiber-optics, and intubating bronchoscopes, to mention just a few. The practitioner may choose what they are most comfortable with and be aware of local availability in their facility. A surgical approach must be readily available, should the need for an emergent surgical airway become necessary in the context of a patient who decompensates into the dangerous \"can't oxygenate, can't ventilate, can't intubate\" scenario.",
"In this patient, after discussing the case with the otolaryngology and anesthesia services, the decision was made for awake intubation in the ED by anesthesia via endotracheal fiberoptic laryngoscopy, with a combination of racemized epinephrine, dexamethasone and lidocaine, topical lidocaine to the posterior oropharynx, and small aliquots of midazolam with fentanyl for sedation.",
"After the airway is secured, empiric antibiotics must be initiated immediately. Available antibiotics include beta-lactams, fluoroquinolones, macrolides, tetracyclines, and aminoglycosides. Several beta lactam-resistant strains have recently emerged; multiple alternative agents are readily available.[9] In the patients who are more significantly ill (as in this case), the intravenous route is obviously preferred.",
"H influenzae is particularly susceptible to third-generation cephalosporins. In extreme situations, such as secondary to multiple allergies or unavailability of other the antibiotics mentioned, chloramphenicol may be considered. Extra caution is important given chloramphenicol's considerable adverse effects. Steroids may also be given; although they may augment the body's inflammatory response, they have been shown to be beneficial and improve morbidity and mortality. In the presence of abscess formation, standard of care remains incision and drainage. In this case, the otolaryngologist attempted intraoperative drainage of the fluid collection with minimal output."
],
"date": "July 14, 2022",
"figures": [],
"markdown": "# An Adopted 43-Year-Old With Bad Breath, Dyspnea, Dysphagia\n\n **Authors:** Alexander B. Norinsky, DO; Andrew Caravello, DO; James Espinosa, MD \n **Date:** July 14, 2022\n\n ## Content\n\n Intraoral infections, including retropharyngeal and parapharyngeal abscesses, pose a potentially life-threatening difficult airway situation. The immediate proximity to the upper airways and potential for rapid progression (even with minor edema or deviation) may result in near-total or complete obstruction, demanding immediate intervention measures and airway stabilization.\nIn the ideal scenario, an endotracheal or nasotracheal airway should be established in the operating theater under the auspices of the anesthesiology services, with involvement of the otolaryngology or surgical services readily available should the need for a surgical airway become necessary. If these services aren't immediately available, awake intubation should be attempted to optimize success. Furthermore, given the tenuous nature of the patient's stability, and given the potential for rapid progression (as seen in this case), practitioners should be keen on securing the airway sooner than later; if possible, they should discuss with the patient the risk/benefit ratio for an early urgent intubation vs the potential of a later emergent procedure should he or she decompensate.\nNumerous pharmacologic agents are available to maximize successful airway control, be it endotracheal, nasotracheal, or otherwise. First-pass success is always the goal; the best environment to maximize these conditions is an adequate degree of patient sedation while still maintaining their respiratory effort and hemodynamics. The best approach should include a combination of dissociative sedatives, anesthetics, and adjunctive agents. Ketamine and etomidate allow for an adequate degree of sedation/dissociation while maintaining respiratory and cardiopulmonary parameters. Benzodiazepines, fentanyl, and dexmedetomidine may be used as well to allow appropriate relaxation on the part of the patient, but with caution, as they affect the respiratory drive and may augment blood pressure and heart rate.\nAnesthetics are an important and often underused class of medications that can help maximize first-pass success as well. Several routes of administration are available, including the following:\nTopical (in the posterior oropharynx and/or nares);\nNebulized/atomized form; and\nLocal nerve blocks (eg, glossopharyngeal, superior laryngeal, recurrent laryngeal nerves).\nUsed alone or in combination, these can offer the patient a great degree of comfort and tolerance during the procedure and maintenance of the tube. Finally, one may consider using adjunctive agents to facilitate intubation; antisialagogues (eg, glycopyrrolate or atropine) help combat excessive secretions and offer good visualization, and steroids (eg, dexamethasone) can help reduce airway edema.\nOf note, paralytics may be used very judiciously in these cases, as an edematous incompetent airway that collapses may be disastrous. As with all medications, the practitioner needs to be aware of appropriate dosing regimens, depending on the degree of sedation required, as well as any potential interactions with other agents and the patient's diagnosis and underlying medical conditions.\nNumerous approaches are available: direct laryngoscopy, fiber-optics, and intubating bronchoscopes, to mention just a few. The practitioner may choose what they are most comfortable with and be aware of local availability in their facility. A surgical approach must be readily available, should the need for an emergent surgical airway become necessary in the context of a patient who decompensates into the dangerous \"can't oxygenate, can't ventilate, can't intubate\" scenario.\nIn this patient, after discussing the case with the otolaryngology and anesthesia services, the decision was made for awake intubation in the ED by anesthesia via endotracheal fiberoptic laryngoscopy, with a combination of racemized epinephrine, dexamethasone and lidocaine, topical lidocaine to the posterior oropharynx, and small aliquots of midazolam with fentanyl for sedation.\nAfter the airway is secured, empiric antibiotics must be initiated immediately. Available antibiotics include beta-lactams, fluoroquinolones, macrolides, tetracyclines, and aminoglycosides. Several beta lactam-resistant strains have recently emerged; multiple alternative agents are readily available.[9] In the patients who are more significantly ill (as in this case), the intravenous route is obviously preferred.\nH influenzae is particularly susceptible to third-generation cephalosporins. In extreme situations, such as secondary to multiple allergies or unavailability of other the antibiotics mentioned, chloramphenicol may be considered. Extra caution is important given chloramphenicol's considerable adverse effects. Steroids may also be given; although they may augment the body's inflammatory response, they have been shown to be beneficial and improve morbidity and mortality. In the presence of abscess formation, standard of care remains incision and drainage. In this case, the otolaryngologist attempted intraoperative drainage of the fluid collection with minimal output.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 942143,
"choiceText": "Ketamine and a benzodiazepine",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942145,
"choiceText": "Etomidate alone",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942147,
"choiceText": "Fentanyl alone",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942149,
"choiceText": "Paralytics",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942151,
"choiceText": "A combination of dissociatives-sedatives, anesthetics, and adjunctive agents",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "In order to maximize first-pass success while maintaining optimal hemodynamic parameters, respiratory effort, and patient participation and comfort, a multifaceted approach should be used with dissociatives and/or sedatives, local/nebulized/topical anesthetics, and adjunctive agents (such as antisialagogues and steroids). However, whenever possible, the patient should be transported to the operating theater because it lends to a multidisciplinary approach, better lighting conditions, and more resources, should the need for a surgical airway become necessary.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 298083,
"questionText": "Which is the preferred pharmacologic approach to awake intubation in this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 942133,
"choiceText": "Tetracycline",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942135,
"choiceText": "Fluoroquinolones",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942137,
"choiceText": "Third-generation cephalosporins",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942139,
"choiceText": "Chloramphenicol",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942141,
"choiceText": "Macrolides\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "In the case of moderate-to-severe <i>H influenzae</i> infection, third-generation cephalosporins are considered first-line therapy.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 298081,
"questionText": "Which is a first-line agent for severe <em>H influenzae</em> disease?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "An Adopted 43-Year-Old With Bad Breath, Dyspnea, Dysphagia"
},
{
"authors": "Alexander B. Norinsky, DO; Andrew Caravello, DO; James Espinosa, MD",
"content": [],
"date": "July 14, 2022",
"figures": [],
"markdown": "# An Adopted 43-Year-Old With Bad Breath, Dyspnea, Dysphagia\n\n **Authors:** Alexander B. Norinsky, DO; Andrew Caravello, DO; James Espinosa, MD \n **Date:** July 14, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 942143,
"choiceText": "Ketamine and a benzodiazepine",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942145,
"choiceText": "Etomidate alone",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942147,
"choiceText": "Fentanyl alone",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942149,
"choiceText": "Paralytics",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942151,
"choiceText": "A combination of dissociatives-sedatives, anesthetics, and adjunctive agents",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "In order to maximize first-pass success while maintaining optimal hemodynamic parameters, respiratory effort, and patient participation and comfort, a multifaceted approach should be used with dissociatives and/or sedatives, local/nebulized/topical anesthetics, and adjunctive agents (such as antisialagogues and steroids). However, whenever possible, the patient should be transported to the operating theater because it lends to a multidisciplinary approach, better lighting conditions, and more resources, should the need for a surgical airway become necessary.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 298083,
"questionText": "Which is the preferred pharmacologic approach to awake intubation in this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 942133,
"choiceText": "Tetracycline",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942135,
"choiceText": "Fluoroquinolones",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942137,
"choiceText": "Third-generation cephalosporins",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942139,
"choiceText": "Chloramphenicol",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942141,
"choiceText": "Macrolides\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "In the case of moderate-to-severe <i>H influenzae</i> infection, third-generation cephalosporins are considered first-line therapy.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 298081,
"questionText": "Which is a first-line agent for severe <em>H influenzae</em> disease?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "An Adopted 43-Year-Old With Bad Breath, Dyspnea, Dysphagia"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 942123,
"choiceText": "Lemierre syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942125,
"choiceText": "Parapharyngeal/retropharyngeal cellulitis and abscess formation",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942127,
"choiceText": "Ludwig angina",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942129,
"choiceText": "Epiglottitis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942131,
"choiceText": "Bacterial tracheitis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 298079,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 942143,
"choiceText": "Ketamine and a benzodiazepine",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942145,
"choiceText": "Etomidate alone",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942147,
"choiceText": "Fentanyl alone",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942149,
"choiceText": "Paralytics",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942151,
"choiceText": "A combination of dissociatives-sedatives, anesthetics, and adjunctive agents",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "In order to maximize first-pass success while maintaining optimal hemodynamic parameters, respiratory effort, and patient participation and comfort, a multifaceted approach should be used with dissociatives and/or sedatives, local/nebulized/topical anesthetics, and adjunctive agents (such as antisialagogues and steroids). However, whenever possible, the patient should be transported to the operating theater because it lends to a multidisciplinary approach, better lighting conditions, and more resources, should the need for a surgical airway become necessary.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 298083,
"questionText": "Which is the preferred pharmacologic approach to awake intubation in this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 942133,
"choiceText": "Tetracycline",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942135,
"choiceText": "Fluoroquinolones",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942137,
"choiceText": "Third-generation cephalosporins",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942139,
"choiceText": "Chloramphenicol",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 942141,
"choiceText": "Macrolides\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "In the case of moderate-to-severe <i>H influenzae</i> infection, third-generation cephalosporins are considered first-line therapy.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 298081,
"questionText": "Which is a first-line agent for severe <em>H influenzae</em> disease?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
885142 | /viewarticle/885142 | [
{
"authors": "Saad A. Shebrain, MD; Hailey Chang, MD",
"content": [
"Editor's Note:",
"The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"Background",
"A 24-year-old man presents with generalized weakness, progressive weight loss, intractable nausea, vomiting, and abdominal pain over the past few years. He describes his abdominal pain as intermittent episodes of sharp, intense pain localized to the epigastric region. In the past 2 days, he has had over 10 episodes in which his symptoms are exacerbated by food. He does not have fevers, chills, shortness of breath, chest pain, hemoptysis, hematemesis, diarrhea, constipation, hematochezia, and melena.",
"His medical history is significant for asthma, gastroesophageal reflux disease, and a hiatal hernia for which he underwent repair a few years ago. He smokes cigarettes daily, with a 1.8–pack-year smoking history; he drinks alcohol occasionally and uses cannabis daily for chronic pain relief."
],
"date": "July 11, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: A Daily Cannabis User With Sharp, Intense Epigastric Pain\n\n **Authors:** Saad A. Shebrain, MD; Hailey Chang, MD \n **Date:** July 11, 2022\n\n ## Content\n\n Editor's Note:\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nBackground\nA 24-year-old man presents with generalized weakness, progressive weight loss, intractable nausea, vomiting, and abdominal pain over the past few years. He describes his abdominal pain as intermittent episodes of sharp, intense pain localized to the epigastric region. In the past 2 days, he has had over 10 episodes in which his symptoms are exacerbated by food. He does not have fevers, chills, shortness of breath, chest pain, hemoptysis, hematemesis, diarrhea, constipation, hematochezia, and melena.\nHis medical history is significant for asthma, gastroesophageal reflux disease, and a hiatal hernia for which he underwent repair a few years ago. He smokes cigarettes daily, with a 1.8–pack-year smoking history; he drinks alcohol occasionally and uses cannabis daily for chronic pain relief.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Gastro Case Challenge: A Daily Cannabis User With Sharp, Intense Epigastric Pain"
},
{
"authors": "Saad A. Shebrain, MD; Hailey Chang, MD",
"content": [
"Physical Examination and Workup",
"Upon physical examination, the patient is well-developed, malnourished, and in mild distress. His temperature is 98.1°F (36.7°C), his heart rate is 75 beats/min, his respiratory rate is 20 breaths/min, and his blood pressure is 117/63 mm Hg. His height is 5'7\" (1.7 m), his body weight is 135 lb (61.2 kg), and his body mass index is 21.1 kg/m2.",
"The patient's head is normocephalic and atraumatic, his extraocular movements are intact, and no scleral icterus is observed. His mucous membranes are slightly dry, and his neck is supple, with normal range of motion. Auscultation of the lungs reveal equal and symmetrical breath sounds that are clear bilaterally, with no increased work of breathing.",
"Cardiovascular examination reveals a regular rate and rhythm with normal heart sounds, absence of murmurs, and intact distal pulses. Abdominal examination reveals a soft, scaphoid, nondistended abdomen, with no tenderness to palpation and normal bowel sounds. Musculoskeletal survey reveals normal range of motion, and skin examination reveals skin that is warm, relatively well-perfused, and without any lesions. Neuropsychiatric examination reveals normal mood and affect, and the patient is neurologically intact.",
"The patient is admitted to the hospital and started on fluid resuscitation and given multiple doses of ondansetron and morphine for nausea and pain control. His symptoms persist, so promethazine is given, with minimal relief. A work-up is initiated. Basic laboratory test results, including complete metabolic profiles and complete blood count, are within normal limits.",
"CT of the abdomen and pelvis are obtained to evaluate the abdominal pain (Figure 1). Upper gastrointestinal endoscopy is also performed (Figures 2 and 3).",
"Figure 1.",
"Figure 2.",
"Figure 3."
],
"date": "July 11, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/885/142/Figure-1_thumb.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/885/142/Figure-2_thumb.jpg"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/885/142/Figure-3_thumb.jpg"
}
],
"markdown": "# Gastro Case Challenge: A Daily Cannabis User With Sharp, Intense Epigastric Pain\n\n **Authors:** Saad A. Shebrain, MD; Hailey Chang, MD \n **Date:** July 11, 2022\n\n ## Content\n\n Physical Examination and Workup\nUpon physical examination, the patient is well-developed, malnourished, and in mild distress. His temperature is 98.1°F (36.7°C), his heart rate is 75 beats/min, his respiratory rate is 20 breaths/min, and his blood pressure is 117/63 mm Hg. His height is 5'7\" (1.7 m), his body weight is 135 lb (61.2 kg), and his body mass index is 21.1 kg/m2.\nThe patient's head is normocephalic and atraumatic, his extraocular movements are intact, and no scleral icterus is observed. His mucous membranes are slightly dry, and his neck is supple, with normal range of motion. Auscultation of the lungs reveal equal and symmetrical breath sounds that are clear bilaterally, with no increased work of breathing.\nCardiovascular examination reveals a regular rate and rhythm with normal heart sounds, absence of murmurs, and intact distal pulses. Abdominal examination reveals a soft, scaphoid, nondistended abdomen, with no tenderness to palpation and normal bowel sounds. Musculoskeletal survey reveals normal range of motion, and skin examination reveals skin that is warm, relatively well-perfused, and without any lesions. Neuropsychiatric examination reveals normal mood and affect, and the patient is neurologically intact.\nThe patient is admitted to the hospital and started on fluid resuscitation and given multiple doses of ondansetron and morphine for nausea and pain control. His symptoms persist, so promethazine is given, with minimal relief. A work-up is initiated. Basic laboratory test results, including complete metabolic profiles and complete blood count, are within normal limits.\nCT of the abdomen and pelvis are obtained to evaluate the abdominal pain (Figure 1). Upper gastrointestinal endoscopy is also performed (Figures 2 and 3).\nFigure 1.\nFigure 2.\nFigure 3.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1135880,
"choiceText": "Acute gastritis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135882,
"choiceText": "Cannabinoid hyperemesis syndrome",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135884,
"choiceText": "Superior mesenteric artery syndrome",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135886,
"choiceText": "Peptic ulcer disease",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135888,
"choiceText": "Cholecystitis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360407,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: A Daily Cannabis User With Sharp, Intense Epigastric Pain"
},
{
"authors": "Saad A. Shebrain, MD; Hailey Chang, MD",
"content": [
"Discussion",
"Superior mesenteric artery (SMA) syndrome is an uncommon cause of intestinal obstruction due to vascular compression of the third portion of the duodenum (D3) between the aorta and the SMA. It was first described in an anatomy text by Austrian professor Carl von Rokitansky in 1861.[1] Wilkie[2] subsequently published the first comprehensive series of 75 patients in 1927, and his name became an eponym for the syndrome.",
"The SMA originates from the anterior surface of the abdominal aorta just inferior to the origin of the celiac trunk at the level of the first lumbar vertebra. It then courses anteroinferiorly behind the neck of the pancreas to create the aortomesenteric angle, embedded with retroperitoneal fat tissue and lymphatics. The third portion of duodenum is suspended within this angle by the suspensory ligament of Treitz and crosses the vertebral column at the level of the third lumbar vertebrae.",
"Under normal conditions, the mass of fat and lymphatic tissue surrounding the SMA origin forms a physiologic \"fat pad\" that surrounds and protects the duodenum against vascular compression. Loss of this buffer results in narrowing of the vascular angle and the development of SMA syndrome (SMAS).[3] The normal angle between the aorta and the SMA ranges from 38°-65°, and the normal aortomesenteric distance ranges from 10-28 mm. In SMAS, the angle is decreased to 6°-25°, and the aortomesenteric distance is decreased to 2-8 mm.[4]",
"SMAS has an estimated prevalence of 0.013%-0.3% in the general population.[5,6] Females are more commonly affected than males, and most cases are diagnosed between age 10 and 39 years, with a median age of 28 years.[4,7] Individuals with conditions causing catabolic states or severe weight loss are at particular risk. owing to depletion of the mesenteric and retroperitoneal fat surrounding the SMA. This leads to reduction of the aortomesenteric angle and subsequent duodenal obstruction.[5,7]",
"Both acute and chronic forms of SMAS have been described. The most common comorbidities are mental and behavioral disorders (eg, anorexia nervosa, drug abuse), infectious diseases, and diseases of the nervous system (eg, cerebral palsy, paraplegia, juvenile rheumatoid arthritis, brain injury).[4] Numerous predisposing conditions have been identified, including chronic wasting diseases (eg, cancer, cardiac cachexia, malabsorption, hyperthyroidism), trauma (eg, severe burn injury, polytrauma), postoperative states (eg, bariatric surgery, Nissen fundoplication, posterior spinal fusion or scoliosis surgery, body cast, proctocolectomy, ileoanal pouch anastomosis), anatomical and congenital anomalies (eg, intestinal malrotation, high insertion of the ligament of Treitz, low origin of the SMA, increased lumbar lordosis), and local pathology (eg, neoplastic growth in the mesenteric root, dissecting aortic aneurysm).[3,7,8]"
],
"date": "July 11, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: A Daily Cannabis User With Sharp, Intense Epigastric Pain\n\n **Authors:** Saad A. Shebrain, MD; Hailey Chang, MD \n **Date:** July 11, 2022\n\n ## Content\n\n Discussion\nSuperior mesenteric artery (SMA) syndrome is an uncommon cause of intestinal obstruction due to vascular compression of the third portion of the duodenum (D3) between the aorta and the SMA. It was first described in an anatomy text by Austrian professor Carl von Rokitansky in 1861.[1] Wilkie[2] subsequently published the first comprehensive series of 75 patients in 1927, and his name became an eponym for the syndrome.\nThe SMA originates from the anterior surface of the abdominal aorta just inferior to the origin of the celiac trunk at the level of the first lumbar vertebra. It then courses anteroinferiorly behind the neck of the pancreas to create the aortomesenteric angle, embedded with retroperitoneal fat tissue and lymphatics. The third portion of duodenum is suspended within this angle by the suspensory ligament of Treitz and crosses the vertebral column at the level of the third lumbar vertebrae.\nUnder normal conditions, the mass of fat and lymphatic tissue surrounding the SMA origin forms a physiologic \"fat pad\" that surrounds and protects the duodenum against vascular compression. Loss of this buffer results in narrowing of the vascular angle and the development of SMA syndrome (SMAS).[3] The normal angle between the aorta and the SMA ranges from 38°-65°, and the normal aortomesenteric distance ranges from 10-28 mm. In SMAS, the angle is decreased to 6°-25°, and the aortomesenteric distance is decreased to 2-8 mm.[4]\nSMAS has an estimated prevalence of 0.013%-0.3% in the general population.[5,6] Females are more commonly affected than males, and most cases are diagnosed between age 10 and 39 years, with a median age of 28 years.[4,7] Individuals with conditions causing catabolic states or severe weight loss are at particular risk. owing to depletion of the mesenteric and retroperitoneal fat surrounding the SMA. This leads to reduction of the aortomesenteric angle and subsequent duodenal obstruction.[5,7]\nBoth acute and chronic forms of SMAS have been described. The most common comorbidities are mental and behavioral disorders (eg, anorexia nervosa, drug abuse), infectious diseases, and diseases of the nervous system (eg, cerebral palsy, paraplegia, juvenile rheumatoid arthritis, brain injury).[4] Numerous predisposing conditions have been identified, including chronic wasting diseases (eg, cancer, cardiac cachexia, malabsorption, hyperthyroidism), trauma (eg, severe burn injury, polytrauma), postoperative states (eg, bariatric surgery, Nissen fundoplication, posterior spinal fusion or scoliosis surgery, body cast, proctocolectomy, ileoanal pouch anastomosis), anatomical and congenital anomalies (eg, intestinal malrotation, high insertion of the ligament of Treitz, low origin of the SMA, increased lumbar lordosis), and local pathology (eg, neoplastic growth in the mesenteric root, dissecting aortic aneurysm).[3,7,8]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1135880,
"choiceText": "Acute gastritis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135882,
"choiceText": "Cannabinoid hyperemesis syndrome",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135884,
"choiceText": "Superior mesenteric artery syndrome",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135886,
"choiceText": "Peptic ulcer disease",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135888,
"choiceText": "Cholecystitis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360407,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: A Daily Cannabis User With Sharp, Intense Epigastric Pain"
},
{
"authors": "Saad A. Shebrain, MD; Hailey Chang, MD",
"content": [
"The typical symptoms of SMAS mimic those of partial duodenal obstruction and include nausea, vomiting, abdominal pain, early satiety, and anorexia that results in weight loss.[6,7,9] Most individuals experience more than one symptom, with the triad of abdominal pain, vomiting, and nausea being the most common. Although weight loss is frequently associated with SMA syndrome SMAS, a low body mass index is not necessarily a prerequisite.[5]",
"The pain associated with SMA syndrome is classically described as postprandial epigastric pain that is relieved by lying in the prone, knee-chest, or left lateral decubitus position. These all reduce tension of the small-bowel mesentery at the aortomesenteric angle, leading to alleviation of symptoms.[3,7,9]",
"Duodenal obstruction may also lead to proximal duodenal dilatation (with or without gastric dilatation) along with duodenal stasis and gastric reflux leading to bilious emesis and associated peptic ulcer disease.[7] Case reports of the prevalence of SMAS after scoliosis surgery range from 0.5% to 2.4%.[10] Patients typically experience symptoms within the first postoperative week, and symptoms typically resolve. In contrast, reports of SMAS developing after severe burn injury describe mean burn areas of 48.5% of total body surface area, with a range of 32%-64.5%, indicative of an extreme catabolic state. These patients typically develop symptoms of SMAS after 2 weeks. Once established, the SMAS becomes self-perpetuating, with cyclical vomiting, further weight loss, and exacerbation of symptoms.[7,9]",
"The differential diagnosis for SMAS includes a wide variety of other causes of abdominal pain. In particular, SMA syndrome should be differentiated from SMA-like syndrome, in which symptoms are caused by generalized duodenal dilatation rather than secondary duodenal compression. The most common causes of SMA-like syndrome are mixed connective tissue disorders (eg, systemic sclerosis, scleroderma) that result in duodenal muscular atrophy, reduced duodenal peristalsis, and development of megaduodenum. Other causes of reduced duodenal peristalsis include diabetes, pancreatitis, dermatomyositis, systemic lupus erythematosus, myxedema, amyloidosis, myotonic dystrophy, and chronic idiopathic intestinal pseudo-obstruction.[3] The differential diagnosis can be further expanded to include irritable bowel syndrome, peptic ulcer disease, gastritis, duodenitis, hiatal hernia, cholelithiasis, obstruction (adhesive, neoplastic), visceral neuropathy, porphyria, and abdominal vessel aneurysm.[6,11] In children, SMA-like syndrome is associated with annular pancreas, duodenal web or stenosis, preduodenal portal vein, duodenal duplication, malrotation, and history of duodenal surgery. Ultimately, diagnosis of SMAS requires high clinical suspicion and is often a diagnosis of exclusion.[9]",
"Patients who present with signs and symptoms suggestive of SMAS should undergo further workup with radiographic studies. The diagnostic criteria for SMAS include the following[7,9,12]:",
"Evidence of D3 obstruction with dilatation of D1 and D2, with or without gastric dilatation",
"Reverse peristalsis in the duodenum proximal to the obstruction",
"Delayed gastroduodenal transit of 4-6 hours",
"Position-dependent relief of obstruction (prone, knee-chest, or left lateral decubitus)",
"Reduced aortosuperior mesenteric artery angle",
"Reduced aortomesenteric space",
"Duodenal obstruction can be demonstrated with barium upper gastrointestinal studies.[9] Findings consistent with SMAS include delayed gastroduodenal transit of 4-6 hours, barium retention, proximal duodenal dilatation (> 3 cm), reverse peristalsis in the proximal duodenum, and a characteristic vertical linear extrinsic compression at D3.[3,7,9,13,14] These radiologic features may disappear in the knee-chest or left lateral decubitus position or through the Hayes maneuver, in which direct manual pressure is applied infraumbilical and dorsocephalad in order to elevate the root of the small-bowel mesentery and provide temporary relief of the obstruction.[3,11]",
"Contrast-enhanced CT or MRI angiography can be performed to evaluate the aortomesenteric anatomy. Patients with SMAS have a mean aortomesenteric angle of 13.5° with a range of 6°-25°, and a mean aortomesenteric distance of 4.4 mm with a range of 2-8 mm. This contrasts with the normal angle and distance of 25°-65° and 10-28 mm, respectively. In general, an angle < 22° and distance < 8 mm is suggestive of SMAS. This is further supported by radiologic evidence of duodenal obstruction with gastric and proximal duodenal dilatation, followed by an abrupt transition point at the level of the SMA.",
"In some cases, this may cause displacement of the gastric antrum anterosuperiorly into the porta hepatis. Other ancillary findings include left renal vein compression that results in left-sided venous collaterals, isolated left renal vein thrombosis, or left gonadal vein enlargement.[15]",
"The combination of barium upper gastrointestinal studies and angiography are regarded as definitive diagnostic modalities for SMAS.[4] However, other imaging studies may aid in diagnosis. Plain abdominal radiography may reveal gastric dilatation suggestive of SMAS.[3] Endoscopic examination is nonspecific but may demonstrate signs of stasis and chronic obstruction, with findings of reflux esophagitis and gastritis. The main use of endoscopy is to rule out more common intraluminal pathologies.[9,14,16] Ultrasonography with Doppler imaging may also be used to evaluate the aortomesenteric angle and distance but does not allow three-dimensional angiographic reconstruction.[6,13] Conventional angiography was historically considered the criterion standard but is less commonly performed today, owing to its invasive nature and associated risks and the advent of CT vascular imaging.[7]",
"The CT scan of this patient showed fluid and contrast distention of the stomach and duodenum to the level of the aorta, and an SMA that suggested SMA compression. The aortomesenteric angle was reduced, at about 15°-19° (normal, 25°-60°), and the distance was reduced to ≤ 4 mm. These findings are suggestive of SMA syndrome (Figure 4).",
"Figure 4."
],
"date": "July 11, 2022",
"figures": [
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/885/142/Figure-4_thumb.jpg"
}
],
"markdown": "# Gastro Case Challenge: A Daily Cannabis User With Sharp, Intense Epigastric Pain\n\n **Authors:** Saad A. Shebrain, MD; Hailey Chang, MD \n **Date:** July 11, 2022\n\n ## Content\n\n The typical symptoms of SMAS mimic those of partial duodenal obstruction and include nausea, vomiting, abdominal pain, early satiety, and anorexia that results in weight loss.[6,7,9] Most individuals experience more than one symptom, with the triad of abdominal pain, vomiting, and nausea being the most common. Although weight loss is frequently associated with SMA syndrome SMAS, a low body mass index is not necessarily a prerequisite.[5]\nThe pain associated with SMA syndrome is classically described as postprandial epigastric pain that is relieved by lying in the prone, knee-chest, or left lateral decubitus position. These all reduce tension of the small-bowel mesentery at the aortomesenteric angle, leading to alleviation of symptoms.[3,7,9]\nDuodenal obstruction may also lead to proximal duodenal dilatation (with or without gastric dilatation) along with duodenal stasis and gastric reflux leading to bilious emesis and associated peptic ulcer disease.[7] Case reports of the prevalence of SMAS after scoliosis surgery range from 0.5% to 2.4%.[10] Patients typically experience symptoms within the first postoperative week, and symptoms typically resolve. In contrast, reports of SMAS developing after severe burn injury describe mean burn areas of 48.5% of total body surface area, with a range of 32%-64.5%, indicative of an extreme catabolic state. These patients typically develop symptoms of SMAS after 2 weeks. Once established, the SMAS becomes self-perpetuating, with cyclical vomiting, further weight loss, and exacerbation of symptoms.[7,9]\nThe differential diagnosis for SMAS includes a wide variety of other causes of abdominal pain. In particular, SMA syndrome should be differentiated from SMA-like syndrome, in which symptoms are caused by generalized duodenal dilatation rather than secondary duodenal compression. The most common causes of SMA-like syndrome are mixed connective tissue disorders (eg, systemic sclerosis, scleroderma) that result in duodenal muscular atrophy, reduced duodenal peristalsis, and development of megaduodenum. Other causes of reduced duodenal peristalsis include diabetes, pancreatitis, dermatomyositis, systemic lupus erythematosus, myxedema, amyloidosis, myotonic dystrophy, and chronic idiopathic intestinal pseudo-obstruction.[3] The differential diagnosis can be further expanded to include irritable bowel syndrome, peptic ulcer disease, gastritis, duodenitis, hiatal hernia, cholelithiasis, obstruction (adhesive, neoplastic), visceral neuropathy, porphyria, and abdominal vessel aneurysm.[6,11] In children, SMA-like syndrome is associated with annular pancreas, duodenal web or stenosis, preduodenal portal vein, duodenal duplication, malrotation, and history of duodenal surgery. Ultimately, diagnosis of SMAS requires high clinical suspicion and is often a diagnosis of exclusion.[9]\nPatients who present with signs and symptoms suggestive of SMAS should undergo further workup with radiographic studies. The diagnostic criteria for SMAS include the following[7,9,12]:\nEvidence of D3 obstruction with dilatation of D1 and D2, with or without gastric dilatation\nReverse peristalsis in the duodenum proximal to the obstruction\nDelayed gastroduodenal transit of 4-6 hours\nPosition-dependent relief of obstruction (prone, knee-chest, or left lateral decubitus)\nReduced aortosuperior mesenteric artery angle\nReduced aortomesenteric space\nDuodenal obstruction can be demonstrated with barium upper gastrointestinal studies.[9] Findings consistent with SMAS include delayed gastroduodenal transit of 4-6 hours, barium retention, proximal duodenal dilatation (> 3 cm), reverse peristalsis in the proximal duodenum, and a characteristic vertical linear extrinsic compression at D3.[3,7,9,13,14] These radiologic features may disappear in the knee-chest or left lateral decubitus position or through the Hayes maneuver, in which direct manual pressure is applied infraumbilical and dorsocephalad in order to elevate the root of the small-bowel mesentery and provide temporary relief of the obstruction.[3,11]\nContrast-enhanced CT or MRI angiography can be performed to evaluate the aortomesenteric anatomy. Patients with SMAS have a mean aortomesenteric angle of 13.5° with a range of 6°-25°, and a mean aortomesenteric distance of 4.4 mm with a range of 2-8 mm. This contrasts with the normal angle and distance of 25°-65° and 10-28 mm, respectively. In general, an angle < 22° and distance < 8 mm is suggestive of SMAS. This is further supported by radiologic evidence of duodenal obstruction with gastric and proximal duodenal dilatation, followed by an abrupt transition point at the level of the SMA.\nIn some cases, this may cause displacement of the gastric antrum anterosuperiorly into the porta hepatis. Other ancillary findings include left renal vein compression that results in left-sided venous collaterals, isolated left renal vein thrombosis, or left gonadal vein enlargement.[15]\nThe combination of barium upper gastrointestinal studies and angiography are regarded as definitive diagnostic modalities for SMAS.[4] However, other imaging studies may aid in diagnosis. Plain abdominal radiography may reveal gastric dilatation suggestive of SMAS.[3] Endoscopic examination is nonspecific but may demonstrate signs of stasis and chronic obstruction, with findings of reflux esophagitis and gastritis. The main use of endoscopy is to rule out more common intraluminal pathologies.[9,14,16] Ultrasonography with Doppler imaging may also be used to evaluate the aortomesenteric angle and distance but does not allow three-dimensional angiographic reconstruction.[6,13] Conventional angiography was historically considered the criterion standard but is less commonly performed today, owing to its invasive nature and associated risks and the advent of CT vascular imaging.[7]\nThe CT scan of this patient showed fluid and contrast distention of the stomach and duodenum to the level of the aorta, and an SMA that suggested SMA compression. The aortomesenteric angle was reduced, at about 15°-19° (normal, 25°-60°), and the distance was reduced to ≤ 4 mm. These findings are suggestive of SMA syndrome (Figure 4).\nFigure 4.\n\n ## Figures\n\n **Figure 4.** \n \n\n\n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Gastro Case Challenge: A Daily Cannabis User With Sharp, Intense Epigastric Pain"
},
{
"authors": "Saad A. Shebrain, MD; Hailey Chang, MD",
"content": [
"Initial management of SMAS is conservative, with gastric decompression, posture adjustment (prone, left lateral decubitus position), and correction of fluid/electrolyte imbalances. When SMAS is associated with cast syndrome, the body cast must be removed. This is promptly followed by aggressive nutritional support, with the goal of increasing body weight to increase retroperitoneal fat tissue and reexpand the aortomesenteric distance, thereby relieving duodenal obstruction. The preferred method is enteral feeding of small, frequent high-calorie meals. If symptoms persist or if the patient is unable to tolerate oral feedings, enteral feedings through a nasojejunal tube past the point of obstruction may be required. Alternatively, total parenteral nutrition or a combination of enteral and parenteral feedings may be used.[3,11,17]",
"Advances in nutritional treatments have dramatically improved the success rate of medical management.[4,7] However, surgery is indicated for symptomatic patients who do not respond to medical management. The optimal duration of medical management has not yet been established, but in general, a trial of 4-6 weeks of medical management and nutritional support is used before pursuing surgical treatment.[14,17]",
"Numerous surgical procedures have been described to treat SMAS. The Strong procedure involves mobilization of the duodenum by dividing the ligament of Treitz. It can be done laparoscopically, is less invasive, allows maintenance of bowel integrity, and is associated with earlier postoperative recovery; however, it has a high failure rate (25%), probably owing to short branches of the inferior pancreaticoduodenal artery that prevent the duodenum from falling caudally and away from the aorta.[9,18] Gastrojejunostomy allows gastric decompression but may result in dumping syndromes and failure to adequately relieve duodenal obstruction. This leads to recurrent symptoms that may necessitate a second operation. Persistent unrelieved obstruction may also result in blind loop syndrome and gastric reflux with peptic ulceration.[7,9,18,19]",
"Duodenojejunostomy is regarded as the procedure of choice for SMAS. It was first described by Stavely in 1908, can now be performed laparoscopically, and has a success rate of up to 90%.[18,20] The advent of laparoscopic surgery has allowed faster recovery, decreased postoperative pain, and decreased length of operation, all while providing the same favorable results as open surgery.[14,21,22]",
"In this procedure, the third portion of duodenum is mobilized to the right of the superior mesenteric vessels (artery and vein), and a side-to-side duodenojejunostomy is created between the third part of duodenum and jejunum distal to ligament of Treitz, to bypass the area of compression created by SMA. Development of blind loop syndrome can be further diminished with a Roux-en-Y duodenojejunal bypass, allowing free drainage of duodenum both proximal and distal to the SMA compression site.[23]",
"The patient in this case underwent laparoscopic duodenojejunostomy and had an uneventful postoperative recovery. Oral nutrition was reinstated on postoperative day 2, with clear liquids and advancement to soft diet by day 5. No complications, such as wound infection or anastomotic leak, occurred. The length of his hospital stay was 5 days. His nausea and vomiting disappeared. Follow-up at 18 months showed significant improvement of symptoms and better quality of life."
],
"date": "July 11, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: A Daily Cannabis User With Sharp, Intense Epigastric Pain\n\n **Authors:** Saad A. Shebrain, MD; Hailey Chang, MD \n **Date:** July 11, 2022\n\n ## Content\n\n Initial management of SMAS is conservative, with gastric decompression, posture adjustment (prone, left lateral decubitus position), and correction of fluid/electrolyte imbalances. When SMAS is associated with cast syndrome, the body cast must be removed. This is promptly followed by aggressive nutritional support, with the goal of increasing body weight to increase retroperitoneal fat tissue and reexpand the aortomesenteric distance, thereby relieving duodenal obstruction. The preferred method is enteral feeding of small, frequent high-calorie meals. If symptoms persist or if the patient is unable to tolerate oral feedings, enteral feedings through a nasojejunal tube past the point of obstruction may be required. Alternatively, total parenteral nutrition or a combination of enteral and parenteral feedings may be used.[3,11,17]\nAdvances in nutritional treatments have dramatically improved the success rate of medical management.[4,7] However, surgery is indicated for symptomatic patients who do not respond to medical management. The optimal duration of medical management has not yet been established, but in general, a trial of 4-6 weeks of medical management and nutritional support is used before pursuing surgical treatment.[14,17]\nNumerous surgical procedures have been described to treat SMAS. The Strong procedure involves mobilization of the duodenum by dividing the ligament of Treitz. It can be done laparoscopically, is less invasive, allows maintenance of bowel integrity, and is associated with earlier postoperative recovery; however, it has a high failure rate (25%), probably owing to short branches of the inferior pancreaticoduodenal artery that prevent the duodenum from falling caudally and away from the aorta.[9,18] Gastrojejunostomy allows gastric decompression but may result in dumping syndromes and failure to adequately relieve duodenal obstruction. This leads to recurrent symptoms that may necessitate a second operation. Persistent unrelieved obstruction may also result in blind loop syndrome and gastric reflux with peptic ulceration.[7,9,18,19]\nDuodenojejunostomy is regarded as the procedure of choice for SMAS. It was first described by Stavely in 1908, can now be performed laparoscopically, and has a success rate of up to 90%.[18,20] The advent of laparoscopic surgery has allowed faster recovery, decreased postoperative pain, and decreased length of operation, all while providing the same favorable results as open surgery.[14,21,22]\nIn this procedure, the third portion of duodenum is mobilized to the right of the superior mesenteric vessels (artery and vein), and a side-to-side duodenojejunostomy is created between the third part of duodenum and jejunum distal to ligament of Treitz, to bypass the area of compression created by SMA. Development of blind loop syndrome can be further diminished with a Roux-en-Y duodenojejunal bypass, allowing free drainage of duodenum both proximal and distal to the SMA compression site.[23]\nThe patient in this case underwent laparoscopic duodenojejunostomy and had an uneventful postoperative recovery. Oral nutrition was reinstated on postoperative day 2, with clear liquids and advancement to soft diet by day 5. No complications, such as wound infection or anastomotic leak, occurred. The length of his hospital stay was 5 days. His nausea and vomiting disappeared. Follow-up at 18 months showed significant improvement of symptoms and better quality of life.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1135890,
"choiceText": "Surgery",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135892,
"choiceText": "Weight loss",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135894,
"choiceText": "Pharmaceutical intervention",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135896,
"choiceText": "Gastric decompression",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "<p>Initial management of SMA syndrome is conservative, with gastric decompression, posture adjustment (prone, left lateral decubitus position), and correction of fluid/electrolyte imbalances. This is promptly followed by aggressive nutritional support with the goal of increasing body weight to increase retroperitoneal fat tissue and reexpand the aortomesenteric distance, thereby relieving duodenal obstruction. Surgery is indicated only for symptomatic patients who do not respond to medical management.</p>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360409,
"questionText": "Which is included in the initial management of SMAS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1135898,
"choiceText": "The Strong procedure",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135900,
"choiceText": "Gastrojejunostomy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135902,
"choiceText": "Open duodenojejunostomy",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135904,
"choiceText": "Laparoscopic duodenojejunostomy",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "<p>Duodenojejunostomy is generally regarded as the procedure of choice for SMA syndrome. It was first described by Stavely in 1908 and has a success rate of up to 90%. The advent of laparoscopic surgery has allowed faster recovery, decreased postoperative pain, and decreased length of operation, all while providing the same results as open surgery, with favorable results.</p>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360411,
"questionText": "Which is the surgical procedure of choice for treatment of SMAS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: A Daily Cannabis User With Sharp, Intense Epigastric Pain"
},
{
"authors": "Saad A. Shebrain, MD; Hailey Chang, MD",
"content": [],
"date": "July 11, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: A Daily Cannabis User With Sharp, Intense Epigastric Pain\n\n **Authors:** Saad A. Shebrain, MD; Hailey Chang, MD \n **Date:** July 11, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1135890,
"choiceText": "Surgery",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135892,
"choiceText": "Weight loss",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135894,
"choiceText": "Pharmaceutical intervention",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135896,
"choiceText": "Gastric decompression",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "<p>Initial management of SMA syndrome is conservative, with gastric decompression, posture adjustment (prone, left lateral decubitus position), and correction of fluid/electrolyte imbalances. This is promptly followed by aggressive nutritional support with the goal of increasing body weight to increase retroperitoneal fat tissue and reexpand the aortomesenteric distance, thereby relieving duodenal obstruction. Surgery is indicated only for symptomatic patients who do not respond to medical management.</p>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360409,
"questionText": "Which is included in the initial management of SMAS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1135898,
"choiceText": "The Strong procedure",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135900,
"choiceText": "Gastrojejunostomy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135902,
"choiceText": "Open duodenojejunostomy",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135904,
"choiceText": "Laparoscopic duodenojejunostomy",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "<p>Duodenojejunostomy is generally regarded as the procedure of choice for SMA syndrome. It was first described by Stavely in 1908 and has a success rate of up to 90%. The advent of laparoscopic surgery has allowed faster recovery, decreased postoperative pain, and decreased length of operation, all while providing the same results as open surgery, with favorable results.</p>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360411,
"questionText": "Which is the surgical procedure of choice for treatment of SMAS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: A Daily Cannabis User With Sharp, Intense Epigastric Pain"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1135880,
"choiceText": "Acute gastritis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135882,
"choiceText": "Cannabinoid hyperemesis syndrome",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135884,
"choiceText": "Superior mesenteric artery syndrome",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135886,
"choiceText": "Peptic ulcer disease",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135888,
"choiceText": "Cholecystitis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360407,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1135890,
"choiceText": "Surgery",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135892,
"choiceText": "Weight loss",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135894,
"choiceText": "Pharmaceutical intervention",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135896,
"choiceText": "Gastric decompression",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "<p>Initial management of SMA syndrome is conservative, with gastric decompression, posture adjustment (prone, left lateral decubitus position), and correction of fluid/electrolyte imbalances. This is promptly followed by aggressive nutritional support with the goal of increasing body weight to increase retroperitoneal fat tissue and reexpand the aortomesenteric distance, thereby relieving duodenal obstruction. Surgery is indicated only for symptomatic patients who do not respond to medical management.</p>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360409,
"questionText": "Which is included in the initial management of SMAS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1135898,
"choiceText": "The Strong procedure",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135900,
"choiceText": "Gastrojejunostomy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135902,
"choiceText": "Open duodenojejunostomy",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1135904,
"choiceText": "Laparoscopic duodenojejunostomy",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "<p>Duodenojejunostomy is generally regarded as the procedure of choice for SMA syndrome. It was first described by Stavely in 1908 and has a success rate of up to 90%. The advent of laparoscopic surgery has allowed faster recovery, decreased postoperative pain, and decreased length of operation, all while providing the same results as open surgery, with favorable results.</p>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360411,
"questionText": "Which is the surgical procedure of choice for treatment of SMAS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
823046 | /viewarticle/823046 | [
{
"authors": "Sumaira Nabi, MBBS; Mazhar Badshah, MBBS, MD, FCPS",
"content": [
"Editor's Note:\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to recognize accurately. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 16-year-old boy presents to the emergency department with a 1-week history of weakness in both lower extremities, which progressed to involve both arms over the course of 1 day. He also complains of dysesthesia. No sphincteric dysfunction is noted.",
"Two weeks before presentation, he had been treated for an upper respiratory tract infection. He has no history of diarrhea, vomiting, or abdominal pain. He is a nonsmoker and is not taking any medications on regular basis. His family history is unremarkable."
],
"date": "June 29, 2022",
"figures": [],
"markdown": "# Neuro Case Challenge: A 16-Year-Old With Quadriparesis After Respiratory Infection\n\n **Authors:** Sumaira Nabi, MBBS; Mazhar Badshah, MBBS, MD, FCPS \n **Date:** June 29, 2022\n\n ## Content\n\n Editor's Note:\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to recognize accurately. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 16-year-old boy presents to the emergency department with a 1-week history of weakness in both lower extremities, which progressed to involve both arms over the course of 1 day. He also complains of dysesthesia. No sphincteric dysfunction is noted.\nTwo weeks before presentation, he had been treated for an upper respiratory tract infection. He has no history of diarrhea, vomiting, or abdominal pain. He is a nonsmoker and is not taking any medications on regular basis. His family history is unremarkable.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Neuro Case Challenge: A 16-Year-Old With Quadriparesis After Respiratory Infection"
},
{
"authors": "Sumaira Nabi, MBBS; Mazhar Badshah, MBBS, MD, FCPS",
"content": [
"His vital signs include an oral temperature of 98.6°F (37°C), regular pulse of 70 beats/min, blood pressure of 120/70 mm Hg. His Glasgow Coma Scale score is 15/15, and he is completely alert and oriented to person, place, and time. He has flaccid quadriparesis with hyporeflexia and bilateral mute planter response. Sensations are intact.",
"Cranial nerve examination findings are unremarkable. Signs of meningeal irritation are absent. His abdomen is soft and nontender. No clinical evidence suggests organomegaly or ascites. His bowel sounds are audible and normal. The patient’s precordial examination reveals normal heart sounds without murmurs. His lungs are clear upon auscultation, with a normal respiratory rate and effort.",
"Laboratory analysis reveals a normal complete blood cell count and erythrocyte sedimentation rate. Aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, and creatinine concentrations are normal; electrocardiography, anteroposterior chest radiography, and abdominal ultrasonography findings also are unremarkable. Nerve conduction studies show abnormalities consistent with demyelination. MRI of the cervical spine with contrast is normal.",
"On day 2 of admission, the patient becomes drowsy and subsequently has multiple generalized tonic-clonic seizures. His Glasgow Coma Scale score drops to 5/15, and he is moved to the intensive care unit for endotracheal intubation and assisted ventilation. He is started on empiric acyclovir and ceftriaxone along with sodium valproate, and his workup is further extended.",
"MRI of the brain (Figures 1-4) reveals bilateral, asymmetric areas of high signal intensity in the subcortical and deep white matter on T2-weighted/fluid-attenuated inversion recovery (FLAIR) sequences.",
"Figure 1.",
"Figure 1.",
"Figure 2.",
"Figure 2.",
"Figure 3.",
"Figure 3.",
"Figure 4.",
"Figure 4.",
"Lumbar puncture for cerebrospinal fluid (CSF) analysis shows an elevated CSF protein of 0.77g/L, a lymphocytic pleocytosis (280 white blood cells/cmm, with 95% lymphocytes), and a normal glucose concentration. Polymerase chain reaction of CSF for herpes simplex virus is negative.",
"Electroencephalography findings are consistent with diffuse encephalopathy (Figure 5).",
"Figure 5.",
"Figure 5."
],
"date": "June 29, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/823/046/823046-thumb-1.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/823/046/823046-thumb-2.jpg"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/823/046/823046-thumb-3.jpg"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/823/046/823046-thumb-4.jpg"
},
{
"caption": "Figure 5.",
"image_url": "https://img.medscapestatic.com/article/823/046/823046-thumb-5.jpg"
}
],
"markdown": "# Neuro Case Challenge: A 16-Year-Old With Quadriparesis After Respiratory Infection\n\n **Authors:** Sumaira Nabi, MBBS; Mazhar Badshah, MBBS, MD, FCPS \n **Date:** June 29, 2022\n\n ## Content\n\n His vital signs include an oral temperature of 98.6°F (37°C), regular pulse of 70 beats/min, blood pressure of 120/70 mm Hg. His Glasgow Coma Scale score is 15/15, and he is completely alert and oriented to person, place, and time. He has flaccid quadriparesis with hyporeflexia and bilateral mute planter response. Sensations are intact.\nCranial nerve examination findings are unremarkable. Signs of meningeal irritation are absent. His abdomen is soft and nontender. No clinical evidence suggests organomegaly or ascites. His bowel sounds are audible and normal. The patient’s precordial examination reveals normal heart sounds without murmurs. His lungs are clear upon auscultation, with a normal respiratory rate and effort.\nLaboratory analysis reveals a normal complete blood cell count and erythrocyte sedimentation rate. Aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, and creatinine concentrations are normal; electrocardiography, anteroposterior chest radiography, and abdominal ultrasonography findings also are unremarkable. Nerve conduction studies show abnormalities consistent with demyelination. MRI of the cervical spine with contrast is normal.\nOn day 2 of admission, the patient becomes drowsy and subsequently has multiple generalized tonic-clonic seizures. His Glasgow Coma Scale score drops to 5/15, and he is moved to the intensive care unit for endotracheal intubation and assisted ventilation. He is started on empiric acyclovir and ceftriaxone along with sodium valproate, and his workup is further extended.\nMRI of the brain (Figures 1-4) reveals bilateral, asymmetric areas of high signal intensity in the subcortical and deep white matter on T2-weighted/fluid-attenuated inversion recovery (FLAIR) sequences.\nFigure 1.\nFigure 1.\nFigure 2.\nFigure 2.\nFigure 3.\nFigure 3.\nFigure 4.\nFigure 4.\nLumbar puncture for cerebrospinal fluid (CSF) analysis shows an elevated CSF protein of 0.77g/L, a lymphocytic pleocytosis (280 white blood cells/cmm, with 95% lymphocytes), and a normal glucose concentration. Polymerase chain reaction of CSF for herpes simplex virus is negative.\nElectroencephalography findings are consistent with diffuse encephalopathy (Figure 5).\nFigure 5.\nFigure 5.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4.** \n \n\n**Figure 5.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 717869,
"choiceText": "Viral encephalitis with Guillain-Barré syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717871,
"choiceText": "Bickerstaff encephalitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717873,
"choiceText": "Acute disseminated encephalomyelitis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717875,
"choiceText": "Spinal cord compression",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 224055,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Neuro Case Challenge: A 16-Year-Old With Quadriparesis After Respiratory Infection"
},
{
"authors": "Sumaira Nabi, MBBS; Mazhar Badshah, MBBS, MD, FCPS",
"content": [
"Acute disseminated encephalomyelitis (ADEM) is an inflammatory demyelinating disease of the nervous system.[1] It is typically a monophasic disease that occurs in prepubescent children; more than 80% of cases are reported in children younger than 10 years.[2,3] The onset of ADEM usually occurs in the wake of a clearly identifiable febrile prodromal illness, especially in the form of a nonspecific upper respiratory tract infection or immunization. Most cases of ADEM are thought to occur as a result of an inflammatory response provoked by infection with a virus, viral vaccine, or other infectious agent. ADEM is more common during the winter and spring months.[4,5,6]",
"A wide array of viral and bacterial pathogens have been associated with ADEM, including viruses such as measles, coronavirus, coxsackieviruses, cytomegalovirus, Epstein-Barr virus, herpes simplex virus, hepatitis A, human immunodeficiency virus, influenza, rubella, varicella zoster, and West Nile virus and bacteria such as Mycoplasma, Leptospira, Borrelia, Chlamydia, Rickettsia, and beta-hemolytic streptococci.[7,8,9] Less than 5% of ADEM cases occur after immunization. ADEM after vaccination has been associated with immunization for measles, rabies, hepatitis B, influenza, mumps, Japanese encephalitis, rubella, polio, varicella, diphtheria/pertussis/tetanus, pneumococcus, and smallpox. ADEM has rarely been reported after the administration of drugs such as sulfonamides, para-aminosalicylic acid, and streptomycin.",
"The neuropathogenesis of ADEM has not been fully elucidated.[1,2,3] The concepts of immune dysregulation and molecular mimicry have been implicated. T-helper cells sensitized to myelin autoantigens, such as myelin basic protein, proteolipid protein, and myelin oligodendrocyte proteins, may produce cytokines and chemokines, leading to further activation of T-cell and B-cell lines as well as phagocytes. The outcome is acute inflammatory demyelination, most often in the central neurons and rarely in the peripheral neurons. For more pathological details, see the study by Young et al.[22]",
"ADEM is typically monophasic, but the disease can be recurrent, relapsing, and multiphasic as well. It is mostly associated with constitutional symptoms such as fever, malaise, and lethargy. The hallmark clinical feature is encephalopathy, which ranges from simple lethargy to frank coma and seizures.[1,2,3] Encephalopathy is the first sign of ADEM in more than 94% of cases. Convulsive seizures occur around the onset of ADEM in as many as 25% of cases. Other initial features include focal and multifocal signs manifesting as isolated features or in various combinations.[4,5,6,7] These reflect cerebral, brainstem, and spinal cord dysfunction and include acute hemiparesis, aphasia, cerebellar ataxia, paraparesis and quadriparesis, cranial neuropathies, and, rarely, peripheral neuropathies.[10,11] Cranial nerve palsies are seen in 35% to 40% of ADEM cases. The optic nerve is most commonly involved."
],
"date": "June 29, 2022",
"figures": [],
"markdown": "# Neuro Case Challenge: A 16-Year-Old With Quadriparesis After Respiratory Infection\n\n **Authors:** Sumaira Nabi, MBBS; Mazhar Badshah, MBBS, MD, FCPS \n **Date:** June 29, 2022\n\n ## Content\n\n Acute disseminated encephalomyelitis (ADEM) is an inflammatory demyelinating disease of the nervous system.[1] It is typically a monophasic disease that occurs in prepubescent children; more than 80% of cases are reported in children younger than 10 years.[2,3] The onset of ADEM usually occurs in the wake of a clearly identifiable febrile prodromal illness, especially in the form of a nonspecific upper respiratory tract infection or immunization. Most cases of ADEM are thought to occur as a result of an inflammatory response provoked by infection with a virus, viral vaccine, or other infectious agent. ADEM is more common during the winter and spring months.[4,5,6]\nA wide array of viral and bacterial pathogens have been associated with ADEM, including viruses such as measles, coronavirus, coxsackieviruses, cytomegalovirus, Epstein-Barr virus, herpes simplex virus, hepatitis A, human immunodeficiency virus, influenza, rubella, varicella zoster, and West Nile virus and bacteria such as Mycoplasma, Leptospira, Borrelia, Chlamydia, Rickettsia, and beta-hemolytic streptococci.[7,8,9] Less than 5% of ADEM cases occur after immunization. ADEM after vaccination has been associated with immunization for measles, rabies, hepatitis B, influenza, mumps, Japanese encephalitis, rubella, polio, varicella, diphtheria/pertussis/tetanus, pneumococcus, and smallpox. ADEM has rarely been reported after the administration of drugs such as sulfonamides, para-aminosalicylic acid, and streptomycin.\nThe neuropathogenesis of ADEM has not been fully elucidated.[1,2,3] The concepts of immune dysregulation and molecular mimicry have been implicated. T-helper cells sensitized to myelin autoantigens, such as myelin basic protein, proteolipid protein, and myelin oligodendrocyte proteins, may produce cytokines and chemokines, leading to further activation of T-cell and B-cell lines as well as phagocytes. The outcome is acute inflammatory demyelination, most often in the central neurons and rarely in the peripheral neurons. For more pathological details, see the study by Young et al.[22]\nADEM is typically monophasic, but the disease can be recurrent, relapsing, and multiphasic as well. It is mostly associated with constitutional symptoms such as fever, malaise, and lethargy. The hallmark clinical feature is encephalopathy, which ranges from simple lethargy to frank coma and seizures.[1,2,3] Encephalopathy is the first sign of ADEM in more than 94% of cases. Convulsive seizures occur around the onset of ADEM in as many as 25% of cases. Other initial features include focal and multifocal signs manifesting as isolated features or in various combinations.[4,5,6,7] These reflect cerebral, brainstem, and spinal cord dysfunction and include acute hemiparesis, aphasia, cerebellar ataxia, paraparesis and quadriparesis, cranial neuropathies, and, rarely, peripheral neuropathies.[10,11] Cranial nerve palsies are seen in 35% to 40% of ADEM cases. The optic nerve is most commonly involved.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 717869,
"choiceText": "Viral encephalitis with Guillain-Barré syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717871,
"choiceText": "Bickerstaff encephalitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717873,
"choiceText": "Acute disseminated encephalomyelitis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717875,
"choiceText": "Spinal cord compression",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 224055,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Neuro Case Challenge: A 16-Year-Old With Quadriparesis After Respiratory Infection"
},
{
"authors": "Sumaira Nabi, MBBS; Mazhar Badshah, MBBS, MD, FCPS",
"content": [
"Most ADEM presentations can be categorized into 7 clinical syndromes: mild encephalopathy, severe encephalopathy, predominantly brainstem presentation, hemiparesis/long tract signs, predominantly ataxic, transverse myelitis, and encephalomyeloradiculoneuropathy, which is a syndrome that combines upper and lower motor neuron signs.[1] The patient in this case had both upper and lower motor neuron involvement and was categorized as having encephalomyeloradiculoneuropathy.",
"Differentiating ADEM from multiple sclerosis (MS) is important.[22] History of a preceding infectious illness or immunization, association with constitutional symptoms such as fever, and prominence of cortical signs such as mental status changes and seizures all favor ADEM. Cerebellar abnormalities that are common in MS are rare in ADEM. The age of onset is younger than 11 or 12 years in ADEM and older than 11 or 12 years in MS.[12]",
"Early recognition is important so that appropriate therapy can be started. Laboratory studies of most patients with ADEM evidence nonspecific inflammation in the form of lymphocytosis or an increased erythrocyte sedimentation rate or C-reactive protein, although these findings can be very nonspecific. Lumbar puncture and CSF examination usually reveal a normal opening pressure with mild pleocytosis and/or a modest increase in protein concentration consistent with ongoing inflammation, as was seen in this case. In some patients, the CSF may be normal. Some patients with ADEM may have oligoclonal bands. CSF myelin basic protein levels may be increased, indicating demyelination.[1,6,7]",
"Electroencephalography is not diagnostic for ADEM. It may reveal increased background slow wave activity that is typical of an encephalopathy, but epileptic activity is rarely seen.[11,13] In patients with optic neuritis, visual evoked potentials may be prolonged. Nerve conduction studies are indicated in patients with lower motor neuron signs, as in this case. Patients may have a demyelinating neuropathy with prolonged F waves, slower conduction velocities, and prolonged distal latencies. Conduction blocks are usually not observed. Features consistent with an axonal neuropathy may be seen in rare cases.[10,11]",
"Imaging studies of the central nervous system are important in establishing the diagnosis of ADEM. MRI of the brain with contrast is the imaging modality of choice. CT scanning of the brain is less sensitive and is often normal. MRI abnormalities are best defined by T2-weighted images and FLAIR sequences. The lesions are typically bilateral and asymmetric and tend to be poorly marginated, located in the deep and subcortical white matter, and have relative periventricular sparing.[1,2,6,7] Acute lesions are sometimes enhanced by contrast. In patients with features suggestive of spinal cord dysfunction, an MRI of the spine may be helpful. It may show swelling of the cord, especially on T2-weighted sequences in cases of myelitis. Demyelinating plaques may be seen, and contrast enhancement with gadolinium may be noted."
],
"date": "June 29, 2022",
"figures": [],
"markdown": "# Neuro Case Challenge: A 16-Year-Old With Quadriparesis After Respiratory Infection\n\n **Authors:** Sumaira Nabi, MBBS; Mazhar Badshah, MBBS, MD, FCPS \n **Date:** June 29, 2022\n\n ## Content\n\n Most ADEM presentations can be categorized into 7 clinical syndromes: mild encephalopathy, severe encephalopathy, predominantly brainstem presentation, hemiparesis/long tract signs, predominantly ataxic, transverse myelitis, and encephalomyeloradiculoneuropathy, which is a syndrome that combines upper and lower motor neuron signs.[1] The patient in this case had both upper and lower motor neuron involvement and was categorized as having encephalomyeloradiculoneuropathy.\nDifferentiating ADEM from multiple sclerosis (MS) is important.[22] History of a preceding infectious illness or immunization, association with constitutional symptoms such as fever, and prominence of cortical signs such as mental status changes and seizures all favor ADEM. Cerebellar abnormalities that are common in MS are rare in ADEM. The age of onset is younger than 11 or 12 years in ADEM and older than 11 or 12 years in MS.[12]\nEarly recognition is important so that appropriate therapy can be started. Laboratory studies of most patients with ADEM evidence nonspecific inflammation in the form of lymphocytosis or an increased erythrocyte sedimentation rate or C-reactive protein, although these findings can be very nonspecific. Lumbar puncture and CSF examination usually reveal a normal opening pressure with mild pleocytosis and/or a modest increase in protein concentration consistent with ongoing inflammation, as was seen in this case. In some patients, the CSF may be normal. Some patients with ADEM may have oligoclonal bands. CSF myelin basic protein levels may be increased, indicating demyelination.[1,6,7]\nElectroencephalography is not diagnostic for ADEM. It may reveal increased background slow wave activity that is typical of an encephalopathy, but epileptic activity is rarely seen.[11,13] In patients with optic neuritis, visual evoked potentials may be prolonged. Nerve conduction studies are indicated in patients with lower motor neuron signs, as in this case. Patients may have a demyelinating neuropathy with prolonged F waves, slower conduction velocities, and prolonged distal latencies. Conduction blocks are usually not observed. Features consistent with an axonal neuropathy may be seen in rare cases.[10,11]\nImaging studies of the central nervous system are important in establishing the diagnosis of ADEM. MRI of the brain with contrast is the imaging modality of choice. CT scanning of the brain is less sensitive and is often normal. MRI abnormalities are best defined by T2-weighted images and FLAIR sequences. The lesions are typically bilateral and asymmetric and tend to be poorly marginated, located in the deep and subcortical white matter, and have relative periventricular sparing.[1,2,6,7] Acute lesions are sometimes enhanced by contrast. In patients with features suggestive of spinal cord dysfunction, an MRI of the spine may be helpful. It may show swelling of the cord, especially on T2-weighted sequences in cases of myelitis. Demyelinating plaques may be seen, and contrast enhancement with gadolinium may be noted.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Neuro Case Challenge: A 16-Year-Old With Quadriparesis After Respiratory Infection"
},
{
"authors": "Sumaira Nabi, MBBS; Mazhar Badshah, MBBS, MD, FCPS",
"content": [
"Treatment with broad-spectrum antibiotics and acyclovir is recommended until an infectious cause is excluded. Once the diagnosis of ADEM is established, steroids remain the mainstay of treatment. High-dose intravenous (IV) corticosteroids are recommended.[1,2,6,7] Methylprednisolone should be administered at a dose of 10-30 mg/kg/day for 3-5 days. Oral steroid taper is recommended only in patients who continue to show clinical symptoms after completion of the high-dose IV glucocorticoid treatment. The chief alternative treatment option is IV immunoglobulin, given at a dose of 2 g/kg/day for 2-3 days[14,15,16,17]; this is especially preferred in cases where meningoencephalitis cannot be excluded or there is an insufficient response to corticosteroids. Plasma exchange should be considered for patients who fail to respond to treatment with glucocorticoids and IV immunoglobulin.[18,19,20] It may be of particular benefit in patients with ADEM-associated myelopathy. The preferred regimen is a total of 6 exchanges, one every other day, with each exchange consisting of 1-1.5 plasma volumes."
],
"date": "June 29, 2022",
"figures": [],
"markdown": "# Neuro Case Challenge: A 16-Year-Old With Quadriparesis After Respiratory Infection\n\n **Authors:** Sumaira Nabi, MBBS; Mazhar Badshah, MBBS, MD, FCPS \n **Date:** June 29, 2022\n\n ## Content\n\n Treatment with broad-spectrum antibiotics and acyclovir is recommended until an infectious cause is excluded. Once the diagnosis of ADEM is established, steroids remain the mainstay of treatment. High-dose intravenous (IV) corticosteroids are recommended.[1,2,6,7] Methylprednisolone should be administered at a dose of 10-30 mg/kg/day for 3-5 days. Oral steroid taper is recommended only in patients who continue to show clinical symptoms after completion of the high-dose IV glucocorticoid treatment. The chief alternative treatment option is IV immunoglobulin, given at a dose of 2 g/kg/day for 2-3 days[14,15,16,17]; this is especially preferred in cases where meningoencephalitis cannot be excluded or there is an insufficient response to corticosteroids. Plasma exchange should be considered for patients who fail to respond to treatment with glucocorticoids and IV immunoglobulin.[18,19,20] It may be of particular benefit in patients with ADEM-associated myelopathy. The preferred regimen is a total of 6 exchanges, one every other day, with each exchange consisting of 1-1.5 plasma volumes.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 717877,
"choiceText": "IV immunoglobulin",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717879,
"choiceText": "Plasmapheresis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717881,
"choiceText": "High-dose IV corticosteroids",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717883,
"choiceText": "IV immunoglobulin + corticosteroids",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717885,
"choiceText": "IV acyclovir",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Treatment with broad-spectrum antibiotics and acyclovir is recommended until an infectious cause is excluded. Once the diagnosis of ADEM is established, steroids remain the mainstay of treatment. Methylprednisolone should be administered at a dose of 10-30 mg/kg/day for 3-5 days. Oral steroid taper is recommended only in patients who continue to show clinical symptoms after completion of the high-dose IV glucocorticoid treatment. IV immunoglobulin is especially preferred in cases where meningoencephalitis cannot be excluded or there is an insufficient response to corticosteroids. Plasmapheresis may be considered for patients who fail to respond to treatment with glucocorticoids and IV immunoglobulin.\r\n<br><br>\r\nRecovery from ADEM begins within days. The patient in this case was treated with pulse steroid therapy for 5 days. At discharge, he was conscious, free of seizures, and mobile with support after a 3-week stay in the hospital. Physiotherapy and a repeat MRI of the brain after 6 weeks were advised.\r\n<br><br>Most patients make a full recovery, usually slowly over 4-6 weeks. Relapses are rare. If they do occur, particularly after cessation of steroids, the administration of antibodies to myelin oligodendrocyte glycoprotein should be considered. At follow-up, approximately 60% to 90% of patients have minimal or no neurological deficits.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 224057,
"questionText": "Which is the best treatment option for the patient described in this case?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 717887,
"choiceText": "Central nervous system infection",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717889,
"choiceText": "Malignancy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717891,
"choiceText": "Vasculitis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717893,
"choiceText": "Demyelination",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717895,
"choiceText": "Paraneoplastic syndrome",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "ADEM has not been fully elucidated. The concepts of immune dysregulation and molecular mimicry, however, are implicated. T-helper cells sensitized to myelin autoantigens, such as myelin basic protein, proteolipid protein, and myelin oligodendrocyte proteins, may produce cytokines and chemokines, leading to further activation of T-cell and B-cell lines as well as phagocytes. The outcome is acute inflammatory demyelination, most often in the central neurons and rarely in the peripheral neurons.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 224059,
"questionText": "Which is the most likely neuropathogenesis of ADEM?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Neuro Case Challenge: A 16-Year-Old With Quadriparesis After Respiratory Infection"
},
{
"authors": "Sumaira Nabi, MBBS; Mazhar Badshah, MBBS, MD, FCPS",
"content": [],
"date": "June 29, 2022",
"figures": [],
"markdown": "# Neuro Case Challenge: A 16-Year-Old With Quadriparesis After Respiratory Infection\n\n **Authors:** Sumaira Nabi, MBBS; Mazhar Badshah, MBBS, MD, FCPS \n **Date:** June 29, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 717877,
"choiceText": "IV immunoglobulin",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717879,
"choiceText": "Plasmapheresis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717881,
"choiceText": "High-dose IV corticosteroids",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717883,
"choiceText": "IV immunoglobulin + corticosteroids",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717885,
"choiceText": "IV acyclovir",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Treatment with broad-spectrum antibiotics and acyclovir is recommended until an infectious cause is excluded. Once the diagnosis of ADEM is established, steroids remain the mainstay of treatment. Methylprednisolone should be administered at a dose of 10-30 mg/kg/day for 3-5 days. Oral steroid taper is recommended only in patients who continue to show clinical symptoms after completion of the high-dose IV glucocorticoid treatment. IV immunoglobulin is especially preferred in cases where meningoencephalitis cannot be excluded or there is an insufficient response to corticosteroids. Plasmapheresis may be considered for patients who fail to respond to treatment with glucocorticoids and IV immunoglobulin.\r\n<br><br>\r\nRecovery from ADEM begins within days. The patient in this case was treated with pulse steroid therapy for 5 days. At discharge, he was conscious, free of seizures, and mobile with support after a 3-week stay in the hospital. Physiotherapy and a repeat MRI of the brain after 6 weeks were advised.\r\n<br><br>Most patients make a full recovery, usually slowly over 4-6 weeks. Relapses are rare. If they do occur, particularly after cessation of steroids, the administration of antibodies to myelin oligodendrocyte glycoprotein should be considered. At follow-up, approximately 60% to 90% of patients have minimal or no neurological deficits.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 224057,
"questionText": "Which is the best treatment option for the patient described in this case?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 717887,
"choiceText": "Central nervous system infection",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717889,
"choiceText": "Malignancy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717891,
"choiceText": "Vasculitis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717893,
"choiceText": "Demyelination",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717895,
"choiceText": "Paraneoplastic syndrome",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "ADEM has not been fully elucidated. The concepts of immune dysregulation and molecular mimicry, however, are implicated. T-helper cells sensitized to myelin autoantigens, such as myelin basic protein, proteolipid protein, and myelin oligodendrocyte proteins, may produce cytokines and chemokines, leading to further activation of T-cell and B-cell lines as well as phagocytes. The outcome is acute inflammatory demyelination, most often in the central neurons and rarely in the peripheral neurons.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 224059,
"questionText": "Which is the most likely neuropathogenesis of ADEM?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Neuro Case Challenge: A 16-Year-Old With Quadriparesis After Respiratory Infection"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 717869,
"choiceText": "Viral encephalitis with Guillain-Barré syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717871,
"choiceText": "Bickerstaff encephalitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717873,
"choiceText": "Acute disseminated encephalomyelitis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717875,
"choiceText": "Spinal cord compression",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 224055,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 717877,
"choiceText": "IV immunoglobulin",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717879,
"choiceText": "Plasmapheresis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717881,
"choiceText": "High-dose IV corticosteroids",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717883,
"choiceText": "IV immunoglobulin + corticosteroids",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717885,
"choiceText": "IV acyclovir",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Treatment with broad-spectrum antibiotics and acyclovir is recommended until an infectious cause is excluded. Once the diagnosis of ADEM is established, steroids remain the mainstay of treatment. Methylprednisolone should be administered at a dose of 10-30 mg/kg/day for 3-5 days. Oral steroid taper is recommended only in patients who continue to show clinical symptoms after completion of the high-dose IV glucocorticoid treatment. IV immunoglobulin is especially preferred in cases where meningoencephalitis cannot be excluded or there is an insufficient response to corticosteroids. Plasmapheresis may be considered for patients who fail to respond to treatment with glucocorticoids and IV immunoglobulin.\r\n<br><br>\r\nRecovery from ADEM begins within days. The patient in this case was treated with pulse steroid therapy for 5 days. At discharge, he was conscious, free of seizures, and mobile with support after a 3-week stay in the hospital. Physiotherapy and a repeat MRI of the brain after 6 weeks were advised.\r\n<br><br>Most patients make a full recovery, usually slowly over 4-6 weeks. Relapses are rare. If they do occur, particularly after cessation of steroids, the administration of antibodies to myelin oligodendrocyte glycoprotein should be considered. At follow-up, approximately 60% to 90% of patients have minimal or no neurological deficits.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 224057,
"questionText": "Which is the best treatment option for the patient described in this case?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 717887,
"choiceText": "Central nervous system infection",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717889,
"choiceText": "Malignancy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717891,
"choiceText": "Vasculitis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717893,
"choiceText": "Demyelination",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 717895,
"choiceText": "Paraneoplastic syndrome",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "ADEM has not been fully elucidated. The concepts of immune dysregulation and molecular mimicry, however, are implicated. T-helper cells sensitized to myelin autoantigens, such as myelin basic protein, proteolipid protein, and myelin oligodendrocyte proteins, may produce cytokines and chemokines, leading to further activation of T-cell and B-cell lines as well as phagocytes. The outcome is acute inflammatory demyelination, most often in the central neurons and rarely in the peripheral neurons.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 224059,
"questionText": "Which is the most likely neuropathogenesis of ADEM?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
868041 | /viewarticle/868041 | [
{
"authors": "Derik L. Davis, MD; Ogechukwu R. Menkiti, MD; Brighita Weinberg, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 7-year-old boy presents to the emergency department (ED) complaining of left hip and knee pain and refuses to bear weight on his left leg. His mother reports that the child fell in the street 2 days ago. The pain is described as mild to moderate in intensity. The patient denies any numbness or tingling in the distal left lower extremity.",
"No skin laceration or bruising is reported by the family. Upon further questioning, the mother admits to having witnessed evolving symptoms over the past 2 months. She describes a worsening limp, decreasing mobility, and increasing left hip and knee pain, without any identified inciting trauma.",
"The patient was brought to the ED 10 months before this presentation for a similar episode of left knee pain after a vague history of a fall. At that visit, radiography of the affected knee demonstrated changes consistent with a mild form of unilateral left-sided juvenile Blount disease. The patient was given a prescription for a nonsteroidal anti-inflammatory medication as needed for pain control, and he was discharged without hospital admission. The symptoms resolved after only 3 days, and the child was asymptomatic for the following 8 months.",
"The past medical history is remarkable for the use of an albuterol inhaler to treat intermittent episodes of asthma. The patient is also markedly obese. He has no previous history of surgery and no known drug allergies. The patient is up-to-date on his immunizations. The patient's mother denies any exposure of the child to cigarette smoke. The family history is noncontributory."
],
"date": "June 15, 2022",
"figures": [],
"markdown": "# Pediatric Case Challenge: A 7-Year-Old Boy With a Limp and Obesity Who Fell in the Street\n\n **Authors:** Derik L. Davis, MD; Ogechukwu R. Menkiti, MD; Brighita Weinberg, MD \n **Date:** June 15, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 7-year-old boy presents to the emergency department (ED) complaining of left hip and knee pain and refuses to bear weight on his left leg. His mother reports that the child fell in the street 2 days ago. The pain is described as mild to moderate in intensity. The patient denies any numbness or tingling in the distal left lower extremity.\nNo skin laceration or bruising is reported by the family. Upon further questioning, the mother admits to having witnessed evolving symptoms over the past 2 months. She describes a worsening limp, decreasing mobility, and increasing left hip and knee pain, without any identified inciting trauma.\nThe patient was brought to the ED 10 months before this presentation for a similar episode of left knee pain after a vague history of a fall. At that visit, radiography of the affected knee demonstrated changes consistent with a mild form of unilateral left-sided juvenile Blount disease. The patient was given a prescription for a nonsteroidal anti-inflammatory medication as needed for pain control, and he was discharged without hospital admission. The symptoms resolved after only 3 days, and the child was asymptomatic for the following 8 months.\nThe past medical history is remarkable for the use of an albuterol inhaler to treat intermittent episodes of asthma. The patient is also markedly obese. He has no previous history of surgery and no known drug allergies. The patient is up-to-date on his immunizations. The patient's mother denies any exposure of the child to cigarette smoke. The family history is noncontributory.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Pediatric Case Challenge: A 7-Year-Old Boy With a Limp and Obesity Who Fell in the Street"
},
{
"authors": "Derik L. Davis, MD; Ogechukwu R. Menkiti, MD; Brighita Weinberg, MD",
"content": [
"Upon physical examination, the patient has a temperature of 98.2° F (36.8° C). He has a pulse of 82 beats/min and a blood pressure of 138/74 mm Hg. The patient's respiratory rate is 19 breaths/min, and his oxygen saturation is 99% while he is breathing room air. The patient is obese in appearance. His weight is 181 lb (82 kg), well above the 95th percentile for boys of the same age. He is alert, oriented x 3, and in no acute distress.",
"The neurovascular examination reveals normal pulses, capillary refill, sensation, and motor function. The right and left upper extremities are unremarkable. The right lower extremity is normal. The left hip has a decreased range of motion, with pain elicited on passive internal rotation while the patient is lying in the supine position, and positive tenderness to palpation at the left groin. The left knee is tender to palpation and has a decreased range of motion, with no swelling, laxity, or effusion. The left ankle and foot examinations are unremarkable. The patient refuses to bear weight on the left lower extremity and demonstrates an antalgic gait. The skin has no abrasions, ecchymosis, or lacerations.",
"A frontal radiograph of the knees shows abnormal medial metaphyseal beaking of the left proximal tibia and mild flattening of the epiphysis medially. The right knee is normal. When compared with the previous radiographs of the knees obtained 10 months earlier, no significant change is noted for the patient's mild form of unilateral left-sided juvenile Blount disease. A review of the frontal and lateral radiographs of the hips obtained 10 months ago demonstrates that the left hip showed only slight physial widening compared with the right hip but was otherwise unremarkable. Films of the hips at the present visit (Figures 1 and 2) show an interval change.",
"Figure 1",
"Figure 2"
],
"date": "June 15, 2022",
"figures": [
{
"caption": "Figure 1",
"image_url": "https://img.medscapestatic.com/article/868/041/868041-Thumb1.png"
},
{
"caption": "Figure 2",
"image_url": "https://img.medscapestatic.com/article/868/041/868041-Thumb2.png"
}
],
"markdown": "# Pediatric Case Challenge: A 7-Year-Old Boy With a Limp and Obesity Who Fell in the Street\n\n **Authors:** Derik L. Davis, MD; Ogechukwu R. Menkiti, MD; Brighita Weinberg, MD \n **Date:** June 15, 2022\n\n ## Content\n\n Upon physical examination, the patient has a temperature of 98.2° F (36.8° C). He has a pulse of 82 beats/min and a blood pressure of 138/74 mm Hg. The patient's respiratory rate is 19 breaths/min, and his oxygen saturation is 99% while he is breathing room air. The patient is obese in appearance. His weight is 181 lb (82 kg), well above the 95th percentile for boys of the same age. He is alert, oriented x 3, and in no acute distress.\nThe neurovascular examination reveals normal pulses, capillary refill, sensation, and motor function. The right and left upper extremities are unremarkable. The right lower extremity is normal. The left hip has a decreased range of motion, with pain elicited on passive internal rotation while the patient is lying in the supine position, and positive tenderness to palpation at the left groin. The left knee is tender to palpation and has a decreased range of motion, with no swelling, laxity, or effusion. The left ankle and foot examinations are unremarkable. The patient refuses to bear weight on the left lower extremity and demonstrates an antalgic gait. The skin has no abrasions, ecchymosis, or lacerations.\nA frontal radiograph of the knees shows abnormal medial metaphyseal beaking of the left proximal tibia and mild flattening of the epiphysis medially. The right knee is normal. When compared with the previous radiographs of the knees obtained 10 months earlier, no significant change is noted for the patient's mild form of unilateral left-sided juvenile Blount disease. A review of the frontal and lateral radiographs of the hips obtained 10 months ago demonstrates that the left hip showed only slight physial widening compared with the right hip but was otherwise unremarkable. Films of the hips at the present visit (Figures 1 and 2) show an interval change.\nFigure 1\nFigure 2\n\n ## Figures\n\n **Figure 1** \n \n\n**Figure 2** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1007343,
"choiceText": "Septic arthritis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007345,
"choiceText": "Transient synovitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007347,
"choiceText": "Legg-Calvé-Perthes disease",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007349,
"choiceText": "Slipped capital femoral epiphysis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 318781,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Pediatric Case Challenge: A 7-Year-Old Boy With a Limp and Obesity Who Fell in the Street"
},
{
"authors": "Derik L. Davis, MD; Ogechukwu R. Menkiti, MD; Brighita Weinberg, MD",
"content": [
"The frontal radiograph of the hips (Figure 1) shows loss of the normal spherical shape of the left capital femoral epiphysis in comparison with the contralateral lower extremity. The contour is flattened; the flattening is most severe along the lateral aspect. The left femoral ossification center is sclerotic, small in size, and presents with slight subluxation laterally. Radiolucent fissures are present superiorly. A large irregular cystic lucency occupies the left proximal femoral metaphysis. The frog-leg radiograph of the hips (Figure 2) demonstrates prominent widening of the physis on the left.",
"Figure 1",
"Figure 2",
"Legg-Calvé-Perthes disease is a pediatric disorder that affects children aged 3-12 years. The peak incidence for this condition occurs between the ages of 4 and 8 years. Males are affected more frequently than females, by about a 5:1 ratio. Legg-Calvé-Perthes disease occurs most often in white children.[1,2,3,4] About 90% of cases are unilateral in presentation. The remaining 10% of cases often present with apparent unilateral symptoms, only to develop disease of the contralateral hip at a later date. Involvement of both hips at the same time is uncommon, and this sequence of bilateral hip findings can help differentiate Legg-Calvé-Perthes disease from other disorders.[1,2,4]",
"Osteonecrosis of the capital femoral epiphysis is the eventual outcome of this disease process. A vascular insult to the blood supply of the epiphysis leads to infarction of the trabecular bone, flattening, and structural collapse of the proximal femur, with associated overgrowth of the articular cartilage. The cause of the ensuing vascular compromise is not well understood.[1,3,4] Hip osteoarthritis rarely develops before age 50 years. The risk of osteoarthrosis depends chiefly on the final degree of joint abnormality.",
"Several hypotheses relating to the etiology of Legg-Calvé-Perthes disease have been postulated, including exposure to passive smoking, low socioeconomic status, trauma, genetic factors, and dietary deficiencies. However, despite extensive research, no proven cause has been described, and the disease remains idiopathic in nature.[5]",
"Generally, Legg-Calvé-Perthes disease progresses in three successive phases: a period of destruction, followed by a stable phase, and finally a healing phase. Each phase may occur over a period of months to years. The chondral surface of the hip joint is not usually directly involved, but it may be secondarily affected at later stages by joint incongruity. The magnitude of the abnormal structural changes to the proximal femur varies and depends on the extent of osteonecrosis and the amount of mechanical pressure exerted on the joint.[1,2,4] Dead bone is reabsorbed, and revascularization and restoration of the epiphysis occur. The shape of the femoral head reflects the severity of the original vascular insult and the influence of treatment. The femoral head can be restored to a normal appearance similar to that of the unaffected contralateral hip, or it can become flattened (coxa plana) and widened (coxa magna), with the development of coxa vara. As a result of these changes, leg-length discrepancy and degenerative joint disease can develop."
],
"date": "June 15, 2022",
"figures": [
{
"caption": "Figure 1",
"image_url": "https://img.medscapestatic.com/article/868/041/868041-Thumb1.png"
},
{
"caption": "Figure 2",
"image_url": "https://img.medscapestatic.com/article/868/041/868041-Thumb2.png"
}
],
"markdown": "# Pediatric Case Challenge: A 7-Year-Old Boy With a Limp and Obesity Who Fell in the Street\n\n **Authors:** Derik L. Davis, MD; Ogechukwu R. Menkiti, MD; Brighita Weinberg, MD \n **Date:** June 15, 2022\n\n ## Content\n\n The frontal radiograph of the hips (Figure 1) shows loss of the normal spherical shape of the left capital femoral epiphysis in comparison with the contralateral lower extremity. The contour is flattened; the flattening is most severe along the lateral aspect. The left femoral ossification center is sclerotic, small in size, and presents with slight subluxation laterally. Radiolucent fissures are present superiorly. A large irregular cystic lucency occupies the left proximal femoral metaphysis. The frog-leg radiograph of the hips (Figure 2) demonstrates prominent widening of the physis on the left.\nFigure 1\nFigure 2\nLegg-Calvé-Perthes disease is a pediatric disorder that affects children aged 3-12 years. The peak incidence for this condition occurs between the ages of 4 and 8 years. Males are affected more frequently than females, by about a 5:1 ratio. Legg-Calvé-Perthes disease occurs most often in white children.[1,2,3,4] About 90% of cases are unilateral in presentation. The remaining 10% of cases often present with apparent unilateral symptoms, only to develop disease of the contralateral hip at a later date. Involvement of both hips at the same time is uncommon, and this sequence of bilateral hip findings can help differentiate Legg-Calvé-Perthes disease from other disorders.[1,2,4]\nOsteonecrosis of the capital femoral epiphysis is the eventual outcome of this disease process. A vascular insult to the blood supply of the epiphysis leads to infarction of the trabecular bone, flattening, and structural collapse of the proximal femur, with associated overgrowth of the articular cartilage. The cause of the ensuing vascular compromise is not well understood.[1,3,4] Hip osteoarthritis rarely develops before age 50 years. The risk of osteoarthrosis depends chiefly on the final degree of joint abnormality.\nSeveral hypotheses relating to the etiology of Legg-Calvé-Perthes disease have been postulated, including exposure to passive smoking, low socioeconomic status, trauma, genetic factors, and dietary deficiencies. However, despite extensive research, no proven cause has been described, and the disease remains idiopathic in nature.[5]\nGenerally, Legg-Calvé-Perthes disease progresses in three successive phases: a period of destruction, followed by a stable phase, and finally a healing phase. Each phase may occur over a period of months to years. The chondral surface of the hip joint is not usually directly involved, but it may be secondarily affected at later stages by joint incongruity. The magnitude of the abnormal structural changes to the proximal femur varies and depends on the extent of osteonecrosis and the amount of mechanical pressure exerted on the joint.[1,2,4] Dead bone is reabsorbed, and revascularization and restoration of the epiphysis occur. The shape of the femoral head reflects the severity of the original vascular insult and the influence of treatment. The femoral head can be restored to a normal appearance similar to that of the unaffected contralateral hip, or it can become flattened (coxa plana) and widened (coxa magna), with the development of coxa vara. As a result of these changes, leg-length discrepancy and degenerative joint disease can develop.\n\n ## Figures\n\n **Figure 1** \n \n\n**Figure 2** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1007343,
"choiceText": "Septic arthritis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007345,
"choiceText": "Transient synovitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007347,
"choiceText": "Legg-Calvé-Perthes disease",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007349,
"choiceText": "Slipped capital femoral epiphysis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 318781,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Pediatric Case Challenge: A 7-Year-Old Boy With a Limp and Obesity Who Fell in the Street"
},
{
"authors": "Derik L. Davis, MD; Ogechukwu R. Menkiti, MD; Brighita Weinberg, MD",
"content": [
"Imaging plays an important role in establishing the diagnosis of Legg-Calvé-Perthes disease, grading the disease severity, and guiding clinical treatment. Early radiographic signs are nonspecific and related to synovitis. Capsular bulging is noted, with displacement of the fat pads around the capsule. More characteristic features include the appearance of a subchondral peripheral fracture of the femoral epiphysis (crescent sign). This fracture is best seen when the patient is in the frog-leg position.",
"Later stages show a decrease in size, sclerosis, flattening, fragmentation, and fissuring of the epiphysis. These findings represent a combination of processes, including compaction and infarction of bone trabeculae, new bone formation, calcification of saponified fat in the marrow, and relative density to the adjacent osteopenia. The epiphysis may also become displaced laterally, producing the appearance of medial joint space widening. A lucent and cystic metaphysis is an accompanying sign. Widening of the femoral head and neck (coxa magna) can occur. The greater trochanter appears larger when compared with the shortened femoral neck. Coxa plana and coxa vara may be radiographic findings seen in chronic disease.",
"MRI is useful for early diagnosis when radiographs are normal or when the diagnosis is in doubt. MRI can demonstrate areas of low signal intensity within the capital femoral epiphysis on T1- and T2-weighted images, which is consistent with early osteonecrosis. Revascularization is demonstrated as a bright signal, similar to fat on T1-weighted images. The asterisk sign (low signal intensity on T1-weighted images and bright signal intensity on T2-weighted images in the epiphyseal marrow) and the double-line sign (a low signal intensity line representing the line between the necrotic and viable bone and a bright signal intensity line representing the granulation tissue) are seen in 80% of cases. Articular cartilage irregularities and joint effusion have bright signal intensity on T2-weighted images. MRI also provides excellent prognostic information by revealing the extent of infarction, growth plate abnormality, and loss of femoral containment within the acetabulum. Bone scintigraphy, arthrography, and ultrasonography can serve as adjunctive modalities in some cases.[1,2,3,4]",
"The differential diagnosis for Legg-Calvé-Perthes disease includes focal and systemic disorders that can cause osteonecrosis of the hip. Systemic diseases that can lead to osteonecrosis of the hip include sickle cell anemia and other hemoglobinopathies, Gaucher disease, steroid arthropathy, Cushing syndrome, and hypothyroidism; focal processes that do so include posttraumatic osteonecrosis, posttreatment osteonecrosis in congenital hip dislocation, slipped capital femoral epiphysis, and inflammatory arthropathies. Inflammatory diseases can induce osteonecrosis of the hip as well; these include toxic synovitis, septic arthritis, osteomyelitis, synovitis secondary to osteoid osteoma, and juvenile chronic arthritis. Other hip dysplasias include multiple epiphyseal dysplasia and, in children younger than age 5 years, Meyer dysplasia (which is localized to the epiphysis only).[2,3,4]",
"Children with Legg-Calvé-Perthes disease most commonly present with a limp as well as hip and/or knee pain. The family often denies an incident of associated trauma, although an inciting injury may be reported. Some children without pain are unexpectedly diagnosed with the disease. Upon physical examination, an antalgic gait, thigh atrophy, and decreased range of motion to internal rotation and abduction of the hip are found. Pain is also elicited on palpation of the groin.",
"Children between aged 3-5 years generally have the best prognosis, whereas those older than 8 years typically have the worst prognosis.[1,2,3,6,7] Several classification schemes have been devised to grade the severity of disease based on radiographic findings, with no consensus as to the best classification system. The Catterall criteria are one example of a well-established and commonly used grading system. Group I involves less than one fourth of the epiphysis, affecting only the anterior portion. No crescent sign, collapse, sequestration, or metaphyseal involvement is seen. Group II shows more advanced changes affecting the anterior portion, but not more than one half of the epiphysis is affected. Osseous structural abnormalities, the crescent sign, and collapse are seen, with possible focal abnormalities within the metaphysis. Group III encompasses nearly the entire epiphysis, with diffuse metaphyseal abnormalities. Group IV represents the complete involvement of the epiphysis. Children in Groups III and IV have the worst prognoses; however, those patients in Groups I and II may develop more advanced disease at follow-up. Additional Catterall risk factors for potential increased morbidity include a V-shaped radiolucency in the lateral aspect of the epiphysis (Gage sign), lateral subluxation of the epiphysis, calcification lateral to the epiphysis, and a horizontal appearance of the physis.[2,3,4]"
],
"date": "June 15, 2022",
"figures": [],
"markdown": "# Pediatric Case Challenge: A 7-Year-Old Boy With a Limp and Obesity Who Fell in the Street\n\n **Authors:** Derik L. Davis, MD; Ogechukwu R. Menkiti, MD; Brighita Weinberg, MD \n **Date:** June 15, 2022\n\n ## Content\n\n Imaging plays an important role in establishing the diagnosis of Legg-Calvé-Perthes disease, grading the disease severity, and guiding clinical treatment. Early radiographic signs are nonspecific and related to synovitis. Capsular bulging is noted, with displacement of the fat pads around the capsule. More characteristic features include the appearance of a subchondral peripheral fracture of the femoral epiphysis (crescent sign). This fracture is best seen when the patient is in the frog-leg position.\nLater stages show a decrease in size, sclerosis, flattening, fragmentation, and fissuring of the epiphysis. These findings represent a combination of processes, including compaction and infarction of bone trabeculae, new bone formation, calcification of saponified fat in the marrow, and relative density to the adjacent osteopenia. The epiphysis may also become displaced laterally, producing the appearance of medial joint space widening. A lucent and cystic metaphysis is an accompanying sign. Widening of the femoral head and neck (coxa magna) can occur. The greater trochanter appears larger when compared with the shortened femoral neck. Coxa plana and coxa vara may be radiographic findings seen in chronic disease.\nMRI is useful for early diagnosis when radiographs are normal or when the diagnosis is in doubt. MRI can demonstrate areas of low signal intensity within the capital femoral epiphysis on T1- and T2-weighted images, which is consistent with early osteonecrosis. Revascularization is demonstrated as a bright signal, similar to fat on T1-weighted images. The asterisk sign (low signal intensity on T1-weighted images and bright signal intensity on T2-weighted images in the epiphyseal marrow) and the double-line sign (a low signal intensity line representing the line between the necrotic and viable bone and a bright signal intensity line representing the granulation tissue) are seen in 80% of cases. Articular cartilage irregularities and joint effusion have bright signal intensity on T2-weighted images. MRI also provides excellent prognostic information by revealing the extent of infarction, growth plate abnormality, and loss of femoral containment within the acetabulum. Bone scintigraphy, arthrography, and ultrasonography can serve as adjunctive modalities in some cases.[1,2,3,4]\nThe differential diagnosis for Legg-Calvé-Perthes disease includes focal and systemic disorders that can cause osteonecrosis of the hip. Systemic diseases that can lead to osteonecrosis of the hip include sickle cell anemia and other hemoglobinopathies, Gaucher disease, steroid arthropathy, Cushing syndrome, and hypothyroidism; focal processes that do so include posttraumatic osteonecrosis, posttreatment osteonecrosis in congenital hip dislocation, slipped capital femoral epiphysis, and inflammatory arthropathies. Inflammatory diseases can induce osteonecrosis of the hip as well; these include toxic synovitis, septic arthritis, osteomyelitis, synovitis secondary to osteoid osteoma, and juvenile chronic arthritis. Other hip dysplasias include multiple epiphyseal dysplasia and, in children younger than age 5 years, Meyer dysplasia (which is localized to the epiphysis only).[2,3,4]\nChildren with Legg-Calvé-Perthes disease most commonly present with a limp as well as hip and/or knee pain. The family often denies an incident of associated trauma, although an inciting injury may be reported. Some children without pain are unexpectedly diagnosed with the disease. Upon physical examination, an antalgic gait, thigh atrophy, and decreased range of motion to internal rotation and abduction of the hip are found. Pain is also elicited on palpation of the groin.\nChildren between aged 3-5 years generally have the best prognosis, whereas those older than 8 years typically have the worst prognosis.[1,2,3,6,7] Several classification schemes have been devised to grade the severity of disease based on radiographic findings, with no consensus as to the best classification system. The Catterall criteria are one example of a well-established and commonly used grading system. Group I involves less than one fourth of the epiphysis, affecting only the anterior portion. No crescent sign, collapse, sequestration, or metaphyseal involvement is seen. Group II shows more advanced changes affecting the anterior portion, but not more than one half of the epiphysis is affected. Osseous structural abnormalities, the crescent sign, and collapse are seen, with possible focal abnormalities within the metaphysis. Group III encompasses nearly the entire epiphysis, with diffuse metaphyseal abnormalities. Group IV represents the complete involvement of the epiphysis. Children in Groups III and IV have the worst prognoses; however, those patients in Groups I and II may develop more advanced disease at follow-up. Additional Catterall risk factors for potential increased morbidity include a V-shaped radiolucency in the lateral aspect of the epiphysis (Gage sign), lateral subluxation of the epiphysis, calcification lateral to the epiphysis, and a horizontal appearance of the physis.[2,3,4]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Pediatric Case Challenge: A 7-Year-Old Boy With a Limp and Obesity Who Fell in the Street"
},
{
"authors": "Derik L. Davis, MD; Ogechukwu R. Menkiti, MD; Brighita Weinberg, MD",
"content": [
"Important priorities in the treatment of Legg-Calvé-Perthes disease include maintaining the spherical shape of the femoral head and containing its presence within the acetabulum. Alleviation of symptoms and restoration of range of motion of the lower extremity are desired clinical outcomes. Various therapeutic strategies are used for patient management, but there is still controversy over which methods of intervention are optimal for each patient and how best to grade the severity of disease. The general philosophy of the surgeon on these matters typically dictates the treatment plan. Management is directed by the patient's symptoms and the severity of the disease, as determined by imaging studies.",
"The bone age of the child is another important consideration for treatment.[4,6,7] Patients younger than 6 years or older children whose condition is classified in Catterall Group I may require only conservative management, without surgery. These children may receive range-of-motion exercises, traction, avoidance of weight bearing, and/or bracing as the only therapy. In certain children, only bedrest and anti-inflammatory medications may be indicated. In older children or in those with advanced disease (Catterall Groups III and IV), surgical intervention may be necessary. Because the outcome in adulthood is usually good, surgery is now performed less often than in the past, as it is effective only in patients with lateral pillar group B or B/C disease with onset after age 8 years.[8] Age at onset and the lateral pillar classification are the two main outcome predictors and serve to guide the surgical indications.",
"Various procedures are used, depending on the clinical situation and surgeon's preference, to avoid long-term disability. Femoral varus osteotomy and Salter's innominate osteotomy provide good outcomes. In severe forms, combining these two techniques or performing a triple pelvic osteotomy appears preferable. For less severe anatomic alterations, surgical intervention is not recommended. Because risk factors cannot be altered, preventive strategies are not available.",
"The patient in this case was placed on crutches and given instructions not to bear weight on the left lower extremity. Following discharge from the ED, he received follow-up evaluation by the pediatric orthopedics service of an affiliated institution, and he subsequently received surgical management 4 months later."
],
"date": "June 15, 2022",
"figures": [],
"markdown": "# Pediatric Case Challenge: A 7-Year-Old Boy With a Limp and Obesity Who Fell in the Street\n\n **Authors:** Derik L. Davis, MD; Ogechukwu R. Menkiti, MD; Brighita Weinberg, MD \n **Date:** June 15, 2022\n\n ## Content\n\n Important priorities in the treatment of Legg-Calvé-Perthes disease include maintaining the spherical shape of the femoral head and containing its presence within the acetabulum. Alleviation of symptoms and restoration of range of motion of the lower extremity are desired clinical outcomes. Various therapeutic strategies are used for patient management, but there is still controversy over which methods of intervention are optimal for each patient and how best to grade the severity of disease. The general philosophy of the surgeon on these matters typically dictates the treatment plan. Management is directed by the patient's symptoms and the severity of the disease, as determined by imaging studies.\nThe bone age of the child is another important consideration for treatment.[4,6,7] Patients younger than 6 years or older children whose condition is classified in Catterall Group I may require only conservative management, without surgery. These children may receive range-of-motion exercises, traction, avoidance of weight bearing, and/or bracing as the only therapy. In certain children, only bedrest and anti-inflammatory medications may be indicated. In older children or in those with advanced disease (Catterall Groups III and IV), surgical intervention may be necessary. Because the outcome in adulthood is usually good, surgery is now performed less often than in the past, as it is effective only in patients with lateral pillar group B or B/C disease with onset after age 8 years.[8] Age at onset and the lateral pillar classification are the two main outcome predictors and serve to guide the surgical indications.\nVarious procedures are used, depending on the clinical situation and surgeon's preference, to avoid long-term disability. Femoral varus osteotomy and Salter's innominate osteotomy provide good outcomes. In severe forms, combining these two techniques or performing a triple pelvic osteotomy appears preferable. For less severe anatomic alterations, surgical intervention is not recommended. Because risk factors cannot be altered, preventive strategies are not available.\nThe patient in this case was placed on crutches and given instructions not to bear weight on the left lower extremity. Following discharge from the ED, he received follow-up evaluation by the pediatric orthopedics service of an affiliated institution, and he subsequently received surgical management 4 months later.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1007351,
"choiceText": "The only option for definitive treatment is surgery",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007353,
"choiceText": "Children may present with knee pain",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007355,
"choiceText": "Most cases are bilateral in presentation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007357,
"choiceText": "Girls are affected more often than boys",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007359,
"choiceText": "Exposure to passive smoking is an accepted cause",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Children with Legg-Calvé-Perthes disease most commonly present with a limp as well as hip and/or knee pain. The family often denies an incident of associated trauma, although an inciting injury may be reported in a minority of cases.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 318783,
"questionText": "Which statement about Legg-Calvé Perthes disease is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1007409,
"choiceText": "Systemic lupus erythematosus",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007411,
"choiceText": "Freiberg infarction",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007413,
"choiceText": "Ankylosing spondylitis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007415,
"choiceText": "Fibromyalgia",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007417,
"choiceText": "Sickle cell anemia ",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The differential diagnosis for Legg-Calvé-Perthes disease includes focal and systemic disorders that can cause osteonecrosis of the hip. Systemic diseases that can lead to osteonecrosis of the hip include sickle cell anemia and other hemoglobinopathies, Gaucher disease, steroid arthropathy, Cushing syndrome, and hypothyroidism; focal processes that do so include posttraumatic osteonecrosis, posttreatment osteonecrosis in congenital hip dislocation, slipped capital femoral epiphysis, and inflammatory arthropathies. Inflammatory diseases can induce osteonecrosis of the hip as well; these include toxic synovitis, septic arthritis, osteomyelitis, synovitis secondary to osteoid osteoma, and juvenile chronic arthritis. Other hip dysplasias include multiple epiphyseal dysplasia and, in children younger than age 5 years, Meyer dysplasia (which is localized to the epiphysis only).\r\n\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 318803,
"questionText": "Which is best established as a differential diagnosis of Legg-Calvé-Perthes disease?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Pediatric Case Challenge: A 7-Year-Old Boy With a Limp and Obesity Who Fell in the Street"
},
{
"authors": "Derik L. Davis, MD; Ogechukwu R. Menkiti, MD; Brighita Weinberg, MD",
"content": [],
"date": "June 15, 2022",
"figures": [],
"markdown": "# Pediatric Case Challenge: A 7-Year-Old Boy With a Limp and Obesity Who Fell in the Street\n\n **Authors:** Derik L. Davis, MD; Ogechukwu R. Menkiti, MD; Brighita Weinberg, MD \n **Date:** June 15, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1007351,
"choiceText": "The only option for definitive treatment is surgery",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007353,
"choiceText": "Children may present with knee pain",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007355,
"choiceText": "Most cases are bilateral in presentation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007357,
"choiceText": "Girls are affected more often than boys",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007359,
"choiceText": "Exposure to passive smoking is an accepted cause",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Children with Legg-Calvé-Perthes disease most commonly present with a limp as well as hip and/or knee pain. The family often denies an incident of associated trauma, although an inciting injury may be reported in a minority of cases.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 318783,
"questionText": "Which statement about Legg-Calvé Perthes disease is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1007409,
"choiceText": "Systemic lupus erythematosus",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007411,
"choiceText": "Freiberg infarction",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007413,
"choiceText": "Ankylosing spondylitis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007415,
"choiceText": "Fibromyalgia",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007417,
"choiceText": "Sickle cell anemia ",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The differential diagnosis for Legg-Calvé-Perthes disease includes focal and systemic disorders that can cause osteonecrosis of the hip. Systemic diseases that can lead to osteonecrosis of the hip include sickle cell anemia and other hemoglobinopathies, Gaucher disease, steroid arthropathy, Cushing syndrome, and hypothyroidism; focal processes that do so include posttraumatic osteonecrosis, posttreatment osteonecrosis in congenital hip dislocation, slipped capital femoral epiphysis, and inflammatory arthropathies. Inflammatory diseases can induce osteonecrosis of the hip as well; these include toxic synovitis, septic arthritis, osteomyelitis, synovitis secondary to osteoid osteoma, and juvenile chronic arthritis. Other hip dysplasias include multiple epiphyseal dysplasia and, in children younger than age 5 years, Meyer dysplasia (which is localized to the epiphysis only).\r\n\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 318803,
"questionText": "Which is best established as a differential diagnosis of Legg-Calvé-Perthes disease?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Pediatric Case Challenge: A 7-Year-Old Boy With a Limp and Obesity Who Fell in the Street"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1007343,
"choiceText": "Septic arthritis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007345,
"choiceText": "Transient synovitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007347,
"choiceText": "Legg-Calvé-Perthes disease",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007349,
"choiceText": "Slipped capital femoral epiphysis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 318781,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1007351,
"choiceText": "The only option for definitive treatment is surgery",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007353,
"choiceText": "Children may present with knee pain",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007355,
"choiceText": "Most cases are bilateral in presentation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007357,
"choiceText": "Girls are affected more often than boys",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007359,
"choiceText": "Exposure to passive smoking is an accepted cause",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Children with Legg-Calvé-Perthes disease most commonly present with a limp as well as hip and/or knee pain. The family often denies an incident of associated trauma, although an inciting injury may be reported in a minority of cases.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 318783,
"questionText": "Which statement about Legg-Calvé Perthes disease is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1007409,
"choiceText": "Systemic lupus erythematosus",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007411,
"choiceText": "Freiberg infarction",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007413,
"choiceText": "Ankylosing spondylitis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007415,
"choiceText": "Fibromyalgia",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1007417,
"choiceText": "Sickle cell anemia ",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The differential diagnosis for Legg-Calvé-Perthes disease includes focal and systemic disorders that can cause osteonecrosis of the hip. Systemic diseases that can lead to osteonecrosis of the hip include sickle cell anemia and other hemoglobinopathies, Gaucher disease, steroid arthropathy, Cushing syndrome, and hypothyroidism; focal processes that do so include posttraumatic osteonecrosis, posttreatment osteonecrosis in congenital hip dislocation, slipped capital femoral epiphysis, and inflammatory arthropathies. Inflammatory diseases can induce osteonecrosis of the hip as well; these include toxic synovitis, septic arthritis, osteomyelitis, synovitis secondary to osteoid osteoma, and juvenile chronic arthritis. Other hip dysplasias include multiple epiphyseal dysplasia and, in children younger than age 5 years, Meyer dysplasia (which is localized to the epiphysis only).\r\n\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 318803,
"questionText": "Which is best established as a differential diagnosis of Legg-Calvé-Perthes disease?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
975148 | /viewarticle/975148 | [
{
"authors": "Marwa Saleem, MD; Ahmad Al Maradni, MD; Mahmoud Alsayed, MD; Ricardo Correa, MD, EdD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 32-year-old man with no significant past medical history presents to the hospital after a syncopal episode at work, which was associated with excessive sweating. His initial workup in the emergency department shows a random fingerstick glucose level of 44 mg/dL (reference range, 80-140 mg/dL). His last meal was 6 hours before his presentation. The patient reports remote episodes of being unwell and having low blood glucose levels (50-55 mg/dL) during fasting and after high-carbohydrate meals.",
"He uses cannabis regularly and consumes alcohol on the weekends. His family history is unremarkable for any endocrinopathies. No use of over-the-counter medications, herbal supplements, or antihyperglycemic agents is documented."
],
"date": "June 13, 2022",
"figures": [],
"markdown": "# Endo Case Challenge: A Cannabis User With Excessive Sweating and Syncope at Work\n\n **Authors:** Marwa Saleem, MD; Ahmad Al Maradni, MD; Mahmoud Alsayed, MD; Ricardo Correa, MD, EdD \n **Date:** June 13, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 32-year-old man with no significant past medical history presents to the hospital after a syncopal episode at work, which was associated with excessive sweating. His initial workup in the emergency department shows a random fingerstick glucose level of 44 mg/dL (reference range, 80-140 mg/dL). His last meal was 6 hours before his presentation. The patient reports remote episodes of being unwell and having low blood glucose levels (50-55 mg/dL) during fasting and after high-carbohydrate meals.\nHe uses cannabis regularly and consumes alcohol on the weekends. His family history is unremarkable for any endocrinopathies. No use of over-the-counter medications, herbal supplements, or antihyperglycemic agents is documented.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Endo Case Challenge: A Cannabis User With Excessive Sweating and Syncope at Work"
},
{
"authors": "Marwa Saleem, MD; Ahmad Al Maradni, MD; Mahmoud Alsayed, MD; Ricardo Correa, MD, EdD",
"content": [
"The physical examination is unremarkable except for tachycardia (heart rate, 105 beats/min), elevated blood pressure (142/87 mm Hg), excessive sweating, and mild anxiety. The patient receives intravenous dextrose in the emergency department and is subsequently admitted to the hospital. The results of an initial biochemical workup, including measurement of serum morning cortisol, insulin-like growth factor 1, and metanephrines and a thyroid function test, are within normal limits.",
"Multiple attempts to wean the patient off intravenous dextrose are unsuccessful and are accompanied by a drop in his plasma glucose level to the mid-30s and then 40 mg/dL within a few hours. He is transferred to the intensive care unit for close blood glucose monitoring. Intravenous dextrose is stopped, and a 72-hour fasting protocol is initiated. After 28 hours of fasting, his fingerstick blood glucose level is 54 mg/dL (reference range, 70-100 mg/dL). A subsequent plasma glucose level is 47 mg/dL. Additional laboratory investigations show values of:",
"C-peptide level: 1.0 ng/mL (reference range, 0.5-2.0 ng/mL)",
"Insulin level: 3 µIU/mL (reference range [fasting], 5-15 µIU/mL)",
"Proinsulin level: 5 pmol/L (reference range, 3.6-22 pmol/L)",
"Insulin-like growth factor 2 (IGF-2) level: 400 ng/mL (reference range, 267-616 ng/mL)",
"Beta-hydroxybutyrate level: 4.7 mg/dL (reference range, 0.21-2.81 mg/dL)",
"The patient is given orange juice and a high-protein, low-carbohydrate meal."
],
"date": "June 13, 2022",
"figures": [],
"markdown": "# Endo Case Challenge: A Cannabis User With Excessive Sweating and Syncope at Work\n\n **Authors:** Marwa Saleem, MD; Ahmad Al Maradni, MD; Mahmoud Alsayed, MD; Ricardo Correa, MD, EdD \n **Date:** June 13, 2022\n\n ## Content\n\n The physical examination is unremarkable except for tachycardia (heart rate, 105 beats/min), elevated blood pressure (142/87 mm Hg), excessive sweating, and mild anxiety. The patient receives intravenous dextrose in the emergency department and is subsequently admitted to the hospital. The results of an initial biochemical workup, including measurement of serum morning cortisol, insulin-like growth factor 1, and metanephrines and a thyroid function test, are within normal limits.\nMultiple attempts to wean the patient off intravenous dextrose are unsuccessful and are accompanied by a drop in his plasma glucose level to the mid-30s and then 40 mg/dL within a few hours. He is transferred to the intensive care unit for close blood glucose monitoring. Intravenous dextrose is stopped, and a 72-hour fasting protocol is initiated. After 28 hours of fasting, his fingerstick blood glucose level is 54 mg/dL (reference range, 70-100 mg/dL). A subsequent plasma glucose level is 47 mg/dL. Additional laboratory investigations show values of:\nC-peptide level: 1.0 ng/mL (reference range, 0.5-2.0 ng/mL)\nInsulin level: 3 µIU/mL (reference range [fasting], 5-15 µIU/mL)\nProinsulin level: 5 pmol/L (reference range, 3.6-22 pmol/L)\nInsulin-like growth factor 2 (IGF-2) level: 400 ng/mL (reference range, 267-616 ng/mL)\nBeta-hydroxybutyrate level: 4.7 mg/dL (reference range, 0.21-2.81 mg/dL)\nThe patient is given orange juice and a high-protein, low-carbohydrate meal.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1693881,
"choiceText": "Non–islet cell insulin-producing neuroendocrine tumor",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693882,
"choiceText": "Insulinoma",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693883,
"choiceText": "Factitious hypoglycemia due to insulin administration",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693884,
"choiceText": "Factitious hypoglycemia due to sulfonylurea consumption",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 545882,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Endo Case Challenge: A Cannabis User With Excessive Sweating and Syncope at Work"
},
{
"authors": "Marwa Saleem, MD; Ahmad Al Maradni, MD; Mahmoud Alsayed, MD; Ricardo Correa, MD, EdD",
"content": [
"Endogenous insulin is synthesized as a precursor — a proinsulin — which undergoes enzymatic cleavage to produce insulin and C-peptide in equimolar amounts. Therefore, factitious hypoglycemia produced by exogenous insulin administration results in suppressed C-peptide. Factitious hypoglycemia produced by sulfonylurea consumption often produces high levels of C-peptide and insulin.",
"An insulinoma and a non–islet cell insulin-producing neuroendocrine tumor have a similar biochemical picture; however, the latter usually causes postprandial hypoglycemia. Fasting hypoglycemia, which is a characteristic feature of an insulinoma, is rare in this disorder. Moreover, a non–islet cell insulin-producing neuroendocrine tumor is typically associated with abnormally high IGF-2 levels.",
"An insulinoma is a type of functional neuroendocrine tumor that manifests with hypoglycemia caused by inappropriately high secretion of insulin. The incidence is approximately one to four patients per million per year.[1,2] Insulinomas typically occur in persons aged between 40 and 60 years but are not uncommon in older patients.[2] Usually, an insulinoma is a single benign tumor; it is malignant in only 5.8% of patients.",
"Insulinomas generally have a variable and nonspecific clinical picture that could be attributable to the episodic insulin secretion from the tumor. Patients may develop vague symptoms early in the disease course or they may present with life-threatening symptoms, such as syncope, arrhythmia, and hypoglycemic coma. The median duration of symptoms varies and can range from months to even years from the onset of the symptoms until diagnosis. Owing to the wide range of symptoms and varying severity, insulinomas can remain undiagnosed and carry significant mortality and morbidity.",
"The pathogenesis of insulinomas remains unclear. In patients with insulinomas, insulin secretion continues despite a low glucose level for a substantial period. Minn and colleagues identified an insulin splice variant in isolated human pancreatic islets of nondiabetic donors that retains 26 bp of intron 1 and thereby changes the 5' untranslated region. The splice variant has increased translational activities compared with native insulin mRNA.[3] The mammalian target of rapamycin (mTOR) functions downstream of phosphatidylinositol 3–kinase and AKT (also known as protein kinase B) and could be abnormally activated in several cancers, including insulinomas. Inhibitors of the mTOR could stabilize blood glucose in patients with insulinomas.[3]",
"Insulinomas can occur sporadically or in conjunction with multiple endocrine neoplasia type 1 (MEN1) syndrome, which is an autosomal dominant disorder associated with mutations in the MEN1 gene mapped to chromosome 11q13.[4] MEN1 syndrome is characterized by parathyroid hyperplasia, anterior pituitary adenomas, and tumors of the endocrine pancreas and duodenum. In addition, a variety of sporadic endocrine tumors, such as parathyroid adenomas, pancreatic insulinomas, and pituitary prolactinomas, have expressed somatic mutations and loss of heterozygosity of the MEN1 alleles. Thus, the MEN1 gene may play the same role in nonhereditary endocrine tumors.[5,6]"
],
"date": "June 13, 2022",
"figures": [],
"markdown": "# Endo Case Challenge: A Cannabis User With Excessive Sweating and Syncope at Work\n\n **Authors:** Marwa Saleem, MD; Ahmad Al Maradni, MD; Mahmoud Alsayed, MD; Ricardo Correa, MD, EdD \n **Date:** June 13, 2022\n\n ## Content\n\n Endogenous insulin is synthesized as a precursor — a proinsulin — which undergoes enzymatic cleavage to produce insulin and C-peptide in equimolar amounts. Therefore, factitious hypoglycemia produced by exogenous insulin administration results in suppressed C-peptide. Factitious hypoglycemia produced by sulfonylurea consumption often produces high levels of C-peptide and insulin.\nAn insulinoma and a non–islet cell insulin-producing neuroendocrine tumor have a similar biochemical picture; however, the latter usually causes postprandial hypoglycemia. Fasting hypoglycemia, which is a characteristic feature of an insulinoma, is rare in this disorder. Moreover, a non–islet cell insulin-producing neuroendocrine tumor is typically associated with abnormally high IGF-2 levels.\nAn insulinoma is a type of functional neuroendocrine tumor that manifests with hypoglycemia caused by inappropriately high secretion of insulin. The incidence is approximately one to four patients per million per year.[1,2] Insulinomas typically occur in persons aged between 40 and 60 years but are not uncommon in older patients.[2] Usually, an insulinoma is a single benign tumor; it is malignant in only 5.8% of patients.\nInsulinomas generally have a variable and nonspecific clinical picture that could be attributable to the episodic insulin secretion from the tumor. Patients may develop vague symptoms early in the disease course or they may present with life-threatening symptoms, such as syncope, arrhythmia, and hypoglycemic coma. The median duration of symptoms varies and can range from months to even years from the onset of the symptoms until diagnosis. Owing to the wide range of symptoms and varying severity, insulinomas can remain undiagnosed and carry significant mortality and morbidity.\nThe pathogenesis of insulinomas remains unclear. In patients with insulinomas, insulin secretion continues despite a low glucose level for a substantial period. Minn and colleagues identified an insulin splice variant in isolated human pancreatic islets of nondiabetic donors that retains 26 bp of intron 1 and thereby changes the 5' untranslated region. The splice variant has increased translational activities compared with native insulin mRNA.[3] The mammalian target of rapamycin (mTOR) functions downstream of phosphatidylinositol 3–kinase and AKT (also known as protein kinase B) and could be abnormally activated in several cancers, including insulinomas. Inhibitors of the mTOR could stabilize blood glucose in patients with insulinomas.[3]\nInsulinomas can occur sporadically or in conjunction with multiple endocrine neoplasia type 1 (MEN1) syndrome, which is an autosomal dominant disorder associated with mutations in the MEN1 gene mapped to chromosome 11q13.[4] MEN1 syndrome is characterized by parathyroid hyperplasia, anterior pituitary adenomas, and tumors of the endocrine pancreas and duodenum. In addition, a variety of sporadic endocrine tumors, such as parathyroid adenomas, pancreatic insulinomas, and pituitary prolactinomas, have expressed somatic mutations and loss of heterozygosity of the MEN1 alleles. Thus, the MEN1 gene may play the same role in nonhereditary endocrine tumors.[5,6]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1693881,
"choiceText": "Non–islet cell insulin-producing neuroendocrine tumor",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693882,
"choiceText": "Insulinoma",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693883,
"choiceText": "Factitious hypoglycemia due to insulin administration",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693884,
"choiceText": "Factitious hypoglycemia due to sulfonylurea consumption",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 545882,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Endo Case Challenge: A Cannabis User With Excessive Sweating and Syncope at Work"
},
{
"authors": "Marwa Saleem, MD; Ahmad Al Maradni, MD; Mahmoud Alsayed, MD; Ricardo Correa, MD, EdD",
"content": [
"The supervised 72-hour fast is the diagnostic test of choice for an insulinoma. The protocol consists of measuring plasma glucose, insulin, C-peptide, and proinsulin levels every 6 hours until the plasma glucose level is ≤ 60 mg/dL, which is when the interval is reduced to every 1-2 hours.[2,7] The fast should be terminated when the plasma glucose level is ≤ 45 mg/dL and the patient has signs and symptoms of hypoglycemia. The diagnostic criteria from the Endocrine Society for endogenous hyperinsulinism are an insulin level ≥ 3 µIU/mL and a proinsulin level > 5 pmol/L when the plasma glucose level is < 55 mg/dL and the patient has signs and symptoms.[8] Common diagnostic criteria for an insulinoma are:",
"Documentation of a blood glucose level of < 55 mg/dL with hypoglycemic symptoms",
"Relief of symptoms after eating",
"Increased plasma insulin level (≥ 3 μIU/mL)",
"Increased C-peptide level (≥ 0.2 nmol/L)",
"Increased proinsulin level (≥ 5 pmol/L)",
"Absence of plasma sulfonylurea",
"In this patient, the cause of his hypoglycemia was suggestive owing to endogenous insulin production because his insulin level was 3 µIU/mL, proinsulin was 5 pmol, and C-peptide was 1 ng/mL.",
"CT of the abdomen was obtained. No pancreatic lesions or concerning findings were initially reported. A meticulous review of the initial CT by two radiologists suggested a possible missed 1.8 × 1.7–cm mass at the tail of the pancreas. A multiphase CT confirmed a 1.8 × 1.7 × 1.3–cm enhancing pancreatic tail lesion (Figure 1), which raised concern for a neuroendocrine tumor, given the patient's clinical history. A gallium 68 dotatate (68Ga-DOTA) test showed uptake in the distal pancreatic mass and splenic hilum (Figure 2).",
"Figure 1.",
"Figure 2.",
"Various imaging modalities may be used to localize the tumor and to exclude or confirm metastatic disease. Three-phase CT is the preferred initial option, followed by endoscopic ultrasonography (EUS) or MRI. Glucagon-like peptide 1 receptor (GLP-1R) PET/CT is a promising new localization technique.[9,10] The GLP-1R is mainly expressed on the pancreatic beta-cells and is therefore an interesting target for imaging of previously occult insulinomas. However, in contrast to benign insulinomas, malignant insulinomas frequently lack the GLP-1R. Malignant insulinomas often do express the somatostatin receptor subtype (SSTR) 2, which can be targeted with PET/CT or PET/MRI using 68Ga-DOTA–labeled somatostatin analogs (SSAs) or with somatostatin receptor scintigraphy and single-photon emission CT (SPECT). If all localization and regionalization techniques fail to localize a tumor, intraoperative palpation of the pancreas and ultrasonography might prove to be successful.[11,12]",
"Treatment includes initial stabilization of the patient with intravenous dextrose, diazoxide, and octreotide if needed. For solitary tumors, surgical excision is the treatment of choice.[2] In patients with malignant tumors, debulking of the pancreatic neuroendocrine tumors, including locoregional lymph nodes, can be considered. If hyperinsulinemia and hypoglycemia persist, diazoxide (150-200 mg in two or three divided doses per day, which can be titrated to a maximum dose of 400 mg/d) with a thiazide diuretic can be used for hypoglycemic relief.[9] Octreotide is another medical option that lowers plasma insulin levels and alleviates symptoms in about 50% of patients.[13,14] Octreotide has a half-life of approximately 100 minutes and is typically administered in doses of 50 or 100 μg every 12 hours.",
"Liver metastases can be resected or treated by embolization, radioembolization (selective internal radiation therapy), radiofrequency ablation, microwave and cryoablation, high-intensity focused ultrasound, laser therapy, brachytherapy, and irreversible electroporation, depending on local availability.[7,15,16,17] In patients with unresectable, low-grade, metastatic malignant insulinomas, the long-acting somatostatin analog lanreotide autogel is the approved first-line therapy for control of tumor growth. In addition, control of hypoglycemia is sometimes achieved with this drug. If indicated, peptide receptor radiotherapy with radiolabeled SSAs or everolimus can be used for tumor, symptom, and biochemical control.[18] Malignant neuroendocrine tumors, particularly those with a high tumor grade, can also be treated with cytotoxic chemotherapy regimens.[1,19]",
"The patient in this case underwent distal pancreatectomy with splenectomy. Pathology reports showed a low-grade pancreatic neuroendocrine tumor in the pancreatic tail, with a negative tumor margin and no lymphadenopathy. The specimen was stained positive for insulin (Figure 3). The patient's hypoglycemia resolved postoperatively, and plasma glucose level remains normal on subsequent follow-up.",
"Figure 3."
],
"date": "June 13, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/975/148/975148-Figure1-thumb.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/975/148/975148-Figure2-thumb.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/975/148/975148-Figure3-thumb.png"
}
],
"markdown": "# Endo Case Challenge: A Cannabis User With Excessive Sweating and Syncope at Work\n\n **Authors:** Marwa Saleem, MD; Ahmad Al Maradni, MD; Mahmoud Alsayed, MD; Ricardo Correa, MD, EdD \n **Date:** June 13, 2022\n\n ## Content\n\n The supervised 72-hour fast is the diagnostic test of choice for an insulinoma. The protocol consists of measuring plasma glucose, insulin, C-peptide, and proinsulin levels every 6 hours until the plasma glucose level is ≤ 60 mg/dL, which is when the interval is reduced to every 1-2 hours.[2,7] The fast should be terminated when the plasma glucose level is ≤ 45 mg/dL and the patient has signs and symptoms of hypoglycemia. The diagnostic criteria from the Endocrine Society for endogenous hyperinsulinism are an insulin level ≥ 3 µIU/mL and a proinsulin level > 5 pmol/L when the plasma glucose level is < 55 mg/dL and the patient has signs and symptoms.[8] Common diagnostic criteria for an insulinoma are:\nDocumentation of a blood glucose level of < 55 mg/dL with hypoglycemic symptoms\nRelief of symptoms after eating\nIncreased plasma insulin level (≥ 3 μIU/mL)\nIncreased C-peptide level (≥ 0.2 nmol/L)\nIncreased proinsulin level (≥ 5 pmol/L)\nAbsence of plasma sulfonylurea\nIn this patient, the cause of his hypoglycemia was suggestive owing to endogenous insulin production because his insulin level was 3 µIU/mL, proinsulin was 5 pmol, and C-peptide was 1 ng/mL.\nCT of the abdomen was obtained. No pancreatic lesions or concerning findings were initially reported. A meticulous review of the initial CT by two radiologists suggested a possible missed 1.8 × 1.7–cm mass at the tail of the pancreas. A multiphase CT confirmed a 1.8 × 1.7 × 1.3–cm enhancing pancreatic tail lesion (Figure 1), which raised concern for a neuroendocrine tumor, given the patient's clinical history. A gallium 68 dotatate (68Ga-DOTA) test showed uptake in the distal pancreatic mass and splenic hilum (Figure 2).\nFigure 1.\nFigure 2.\nVarious imaging modalities may be used to localize the tumor and to exclude or confirm metastatic disease. Three-phase CT is the preferred initial option, followed by endoscopic ultrasonography (EUS) or MRI. Glucagon-like peptide 1 receptor (GLP-1R) PET/CT is a promising new localization technique.[9,10] The GLP-1R is mainly expressed on the pancreatic beta-cells and is therefore an interesting target for imaging of previously occult insulinomas. However, in contrast to benign insulinomas, malignant insulinomas frequently lack the GLP-1R. Malignant insulinomas often do express the somatostatin receptor subtype (SSTR) 2, which can be targeted with PET/CT or PET/MRI using 68Ga-DOTA–labeled somatostatin analogs (SSAs) or with somatostatin receptor scintigraphy and single-photon emission CT (SPECT). If all localization and regionalization techniques fail to localize a tumor, intraoperative palpation of the pancreas and ultrasonography might prove to be successful.[11,12]\nTreatment includes initial stabilization of the patient with intravenous dextrose, diazoxide, and octreotide if needed. For solitary tumors, surgical excision is the treatment of choice.[2] In patients with malignant tumors, debulking of the pancreatic neuroendocrine tumors, including locoregional lymph nodes, can be considered. If hyperinsulinemia and hypoglycemia persist, diazoxide (150-200 mg in two or three divided doses per day, which can be titrated to a maximum dose of 400 mg/d) with a thiazide diuretic can be used for hypoglycemic relief.[9] Octreotide is another medical option that lowers plasma insulin levels and alleviates symptoms in about 50% of patients.[13,14] Octreotide has a half-life of approximately 100 minutes and is typically administered in doses of 50 or 100 μg every 12 hours.\nLiver metastases can be resected or treated by embolization, radioembolization (selective internal radiation therapy), radiofrequency ablation, microwave and cryoablation, high-intensity focused ultrasound, laser therapy, brachytherapy, and irreversible electroporation, depending on local availability.[7,15,16,17] In patients with unresectable, low-grade, metastatic malignant insulinomas, the long-acting somatostatin analog lanreotide autogel is the approved first-line therapy for control of tumor growth. In addition, control of hypoglycemia is sometimes achieved with this drug. If indicated, peptide receptor radiotherapy with radiolabeled SSAs or everolimus can be used for tumor, symptom, and biochemical control.[18] Malignant neuroendocrine tumors, particularly those with a high tumor grade, can also be treated with cytotoxic chemotherapy regimens.[1,19]\nThe patient in this case underwent distal pancreatectomy with splenectomy. Pathology reports showed a low-grade pancreatic neuroendocrine tumor in the pancreatic tail, with a negative tumor margin and no lymphadenopathy. The specimen was stained positive for insulin (Figure 3). The patient's hypoglycemia resolved postoperatively, and plasma glucose level remains normal on subsequent follow-up.\nFigure 3.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n\n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Endo Case Challenge: A Cannabis User With Excessive Sweating and Syncope at Work"
},
{
"authors": "Marwa Saleem, MD; Ahmad Al Maradni, MD; Mahmoud Alsayed, MD; Ricardo Correa, MD, EdD",
"content": [
"This case underscores the need to remain vigilant when evaluating a hypoglycemic patient who has unusual imaging characteristics. With the presence of unsuppressed insulin levels accompanying a plasma glucose level of 47 mg/dL, the biochemical picture did suggest endogenous insulin production, according to the guideline criteria. The initial report of a CT of the abdomen described a normal pancreas. However, owing to high suspicion, a multiphase abdominal CT was ordered, which showed a lesion in the pancreatic tail that measured up to 1.8 cm, with extension to the splenic hilum. A 68Ga-DOTA uptake test confirmed the findings.",
"Ruling out metastatic disease before planning surgical treatment is prudent, especially when surgery is intended to be curative. EUS with biopsy might confirm the presence of a pancreatic mass and a subsequent neuroendocrine tumor but could miss distant metastases. An MRI of the abdomen may not provide any more information than would a CT. A 68Ga-DOTA uptake is comparable to GLP-1R PET/CT and has a high affinity for SSTR2 and SSTR5; thus, it can detect most insulinomas, including metastatic lesions.[9,10]",
"The follow-up for patients with an insulinoma who do not have MEN1 syndrome should include biochemical testing and imaging studies at 3-6 months after resection.[2] If cured, patients can be followed up as needed if their symptoms recur. Patients with persistent symptoms after surgery might have multiple tumors or MEN1 syndrome, and they should undergo repeat imaging studies.[20] Those with multiple insulinomas or MEN1 should be followed up yearly, even if they continue to be cured after resection.[2]"
],
"date": "June 13, 2022",
"figures": [],
"markdown": "# Endo Case Challenge: A Cannabis User With Excessive Sweating and Syncope at Work\n\n **Authors:** Marwa Saleem, MD; Ahmad Al Maradni, MD; Mahmoud Alsayed, MD; Ricardo Correa, MD, EdD \n **Date:** June 13, 2022\n\n ## Content\n\n This case underscores the need to remain vigilant when evaluating a hypoglycemic patient who has unusual imaging characteristics. With the presence of unsuppressed insulin levels accompanying a plasma glucose level of 47 mg/dL, the biochemical picture did suggest endogenous insulin production, according to the guideline criteria. The initial report of a CT of the abdomen described a normal pancreas. However, owing to high suspicion, a multiphase abdominal CT was ordered, which showed a lesion in the pancreatic tail that measured up to 1.8 cm, with extension to the splenic hilum. A 68Ga-DOTA uptake test confirmed the findings.\nRuling out metastatic disease before planning surgical treatment is prudent, especially when surgery is intended to be curative. EUS with biopsy might confirm the presence of a pancreatic mass and a subsequent neuroendocrine tumor but could miss distant metastases. An MRI of the abdomen may not provide any more information than would a CT. A 68Ga-DOTA uptake is comparable to GLP-1R PET/CT and has a high affinity for SSTR2 and SSTR5; thus, it can detect most insulinomas, including metastatic lesions.[9,10]\nThe follow-up for patients with an insulinoma who do not have MEN1 syndrome should include biochemical testing and imaging studies at 3-6 months after resection.[2] If cured, patients can be followed up as needed if their symptoms recur. Patients with persistent symptoms after surgery might have multiple tumors or MEN1 syndrome, and they should undergo repeat imaging studies.[20] Those with multiple insulinomas or MEN1 should be followed up yearly, even if they continue to be cured after resection.[2]\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1693885,
"choiceText": "Surgical resection of the pancreatic lesion",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693886,
"choiceText": "MRI of the abdomen ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693887,
"choiceText": "<sup>68</sup>Ga-DOTA uptake test",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693888,
"choiceText": "GLP1R PET/CT",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nMalignant insulinomas often lack the GLP-1R but do express SSTR2, which can be targeted with PET/CT or PET/MRI using <sup>68</sup>Ga-DOTA–labeled SSAs or with somatostatin receptor scintigraphy and SPECT. Surgical resection is indicated in metastatic insulinoma after staging the disease and determining all the areas of metastasis. An MRI of the abdomen will not give additional information beyond that provided by the abdominal CT the patient already received.\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 545883,
"questionText": "If a patient's biochemical findings confirm endogenous insulin production and an abdominal CT shows a pancreatic lesion and a suspicious liver lesion, which is the best next step?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1693889,
"choiceText": "3-6 months",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693890,
"choiceText": "1 year",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693891,
"choiceText": "2 weeks",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693892,
"choiceText": "5 years",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Follow-up for insulinoma in patients without MEN1 should include biochemical testing and imaging studies at 3-6 months after resection. Two weeks is too soon to demonstrate complete resolution. One-year follow-up and 5-year follow-up are both too long for patients who have metastatic insulinoma.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 545884,
"questionText": "A patient has confirmed multiple insulinomas in the pancreas and liver and underwent successive resections of both. When should the patient be seen for postoperative follow-up?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Endo Case Challenge: A Cannabis User With Excessive Sweating and Syncope at Work"
},
{
"authors": "Marwa Saleem, MD; Ahmad Al Maradni, MD; Mahmoud Alsayed, MD; Ricardo Correa, MD, EdD",
"content": [
"Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult."
],
"date": "June 13, 2022",
"figures": [],
"markdown": "# Endo Case Challenge: A Cannabis User With Excessive Sweating and Syncope at Work\n\n **Authors:** Marwa Saleem, MD; Ahmad Al Maradni, MD; Mahmoud Alsayed, MD; Ricardo Correa, MD, EdD \n **Date:** June 13, 2022\n\n ## Content\n\n Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult.\n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1693885,
"choiceText": "Surgical resection of the pancreatic lesion",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693886,
"choiceText": "MRI of the abdomen ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693887,
"choiceText": "<sup>68</sup>Ga-DOTA uptake test",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693888,
"choiceText": "GLP1R PET/CT",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nMalignant insulinomas often lack the GLP-1R but do express SSTR2, which can be targeted with PET/CT or PET/MRI using <sup>68</sup>Ga-DOTA–labeled SSAs or with somatostatin receptor scintigraphy and SPECT. Surgical resection is indicated in metastatic insulinoma after staging the disease and determining all the areas of metastasis. An MRI of the abdomen will not give additional information beyond that provided by the abdominal CT the patient already received.\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 545883,
"questionText": "If a patient's biochemical findings confirm endogenous insulin production and an abdominal CT shows a pancreatic lesion and a suspicious liver lesion, which is the best next step?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1693889,
"choiceText": "3-6 months",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693890,
"choiceText": "1 year",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693891,
"choiceText": "2 weeks",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693892,
"choiceText": "5 years",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Follow-up for insulinoma in patients without MEN1 should include biochemical testing and imaging studies at 3-6 months after resection. Two weeks is too soon to demonstrate complete resolution. One-year follow-up and 5-year follow-up are both too long for patients who have metastatic insulinoma.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 545884,
"questionText": "A patient has confirmed multiple insulinomas in the pancreas and liver and underwent successive resections of both. When should the patient be seen for postoperative follow-up?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Endo Case Challenge: A Cannabis User With Excessive Sweating and Syncope at Work"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1693881,
"choiceText": "Non–islet cell insulin-producing neuroendocrine tumor",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693882,
"choiceText": "Insulinoma",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693883,
"choiceText": "Factitious hypoglycemia due to insulin administration",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693884,
"choiceText": "Factitious hypoglycemia due to sulfonylurea consumption",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 545882,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1693885,
"choiceText": "Surgical resection of the pancreatic lesion",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693886,
"choiceText": "MRI of the abdomen ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693887,
"choiceText": "<sup>68</sup>Ga-DOTA uptake test",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693888,
"choiceText": "GLP1R PET/CT",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nMalignant insulinomas often lack the GLP-1R but do express SSTR2, which can be targeted with PET/CT or PET/MRI using <sup>68</sup>Ga-DOTA–labeled SSAs or with somatostatin receptor scintigraphy and SPECT. Surgical resection is indicated in metastatic insulinoma after staging the disease and determining all the areas of metastasis. An MRI of the abdomen will not give additional information beyond that provided by the abdominal CT the patient already received.\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 545883,
"questionText": "If a patient's biochemical findings confirm endogenous insulin production and an abdominal CT shows a pancreatic lesion and a suspicious liver lesion, which is the best next step?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1693889,
"choiceText": "3-6 months",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693890,
"choiceText": "1 year",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693891,
"choiceText": "2 weeks",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1693892,
"choiceText": "5 years",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Follow-up for insulinoma in patients without MEN1 should include biochemical testing and imaging studies at 3-6 months after resection. Two weeks is too soon to demonstrate complete resolution. One-year follow-up and 5-year follow-up are both too long for patients who have metastatic insulinoma.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 545884,
"questionText": "A patient has confirmed multiple insulinomas in the pancreas and liver and underwent successive resections of both. When should the patient be seen for postoperative follow-up?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
849308 | /viewarticle/849308 | [
{
"authors": "Inas H. Thomas, MD",
"content": [
"Editor's Note:\n\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.",
"A 14-year-old athletic boy with type 1 diabetes and Hashimoto thyroiditis has had four fractures over the past 2 years. He had two sternum fractures from playing basketball (Figure 1) and two separate falls that led to a thumb (Figure 2) and radius (Figure 3) fracture. He also has had a scaphoid injury (Figure 4).",
"Figure 1.",
"Figure 1.",
"Figure 2.",
"Figure 2.",
"Figure 3.",
"Figure 3.",
"Figure 4.",
"Figure 4.",
"The injuries all had trauma associated with them; however, his mother points out that the injuries were more common in her son than among his teammates, who also have similar activity levels. The mother also has a question about an outside radiology report that states \"osteopenia is noted.\" He does not have a history of previous injuries or fractures and does not easily bruise.",
"His type 1 diabetes, which was diagnosed at age 10 years, is poorly controlled, with A1c in the 9%-10% range. He has positive thyroid peroxidase antibodies but has not developed acquired hypothyroidism yet. Medications include insulin via insulin pump, antacids at 750 mg daily, and vitamin D at 1000 international units (IU) daily (started 3 years prior due to a vitamin D level of 23 ng/mL [reference range, 25-100 ng/mL]). His vision is checked as part of his annual examinations for diabetes and is unremarkable.",
"His family history includes a mother with Hashimoto thyroiditis and a grandmother with osteoporosis diagnosed in her 60s. No family history of genetic disorders or other autoimmune diseases is noted.",
"A review of systems is negative for hearing abnormalities, diarrhea, or developmental delay. He denies increased joint flexibility or skin laxity."
],
"date": "June 06, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/849/308/849308Thumb-1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/849/308/849308Thumb-2.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/849/308/849308Thumb-3.png"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/849/308/849308Thumb-4.png"
}
],
"markdown": "# An Athletic Teen Suddenly Prone to Falls and Fractures\n\n **Authors:** Inas H. Thomas, MD \n **Date:** June 06, 2022\n\n ## Content\n\n Editor's Note:\n\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.\nA 14-year-old athletic boy with type 1 diabetes and Hashimoto thyroiditis has had four fractures over the past 2 years. He had two sternum fractures from playing basketball (Figure 1) and two separate falls that led to a thumb (Figure 2) and radius (Figure 3) fracture. He also has had a scaphoid injury (Figure 4).\nFigure 1.\nFigure 1.\nFigure 2.\nFigure 2.\nFigure 3.\nFigure 3.\nFigure 4.\nFigure 4.\nThe injuries all had trauma associated with them; however, his mother points out that the injuries were more common in her son than among his teammates, who also have similar activity levels. The mother also has a question about an outside radiology report that states \"osteopenia is noted.\" He does not have a history of previous injuries or fractures and does not easily bruise.\nHis type 1 diabetes, which was diagnosed at age 10 years, is poorly controlled, with A1c in the 9%-10% range. He has positive thyroid peroxidase antibodies but has not developed acquired hypothyroidism yet. Medications include insulin via insulin pump, antacids at 750 mg daily, and vitamin D at 1000 international units (IU) daily (started 3 years prior due to a vitamin D level of 23 ng/mL [reference range, 25-100 ng/mL]). His vision is checked as part of his annual examinations for diabetes and is unremarkable.\nHis family history includes a mother with Hashimoto thyroiditis and a grandmother with osteoporosis diagnosed in her 60s. No family history of genetic disorders or other autoimmune diseases is noted.\nA review of systems is negative for hearing abnormalities, diarrhea, or developmental delay. He denies increased joint flexibility or skin laxity.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4.** \n \n\n\n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "An Athletic Teen Suddenly Prone to Falls and Fractures"
},
{
"authors": "Inas H. Thomas, MD",
"content": [
"His weight is 109 lb 9.1 oz (49.7 kg), which places him in the 34th percentile based on the Centers for Disease Control and Prevention (CDC) weight-for-age data. His height is 5 ft 3.7 in (1.618 m), which places him in the 26th percentile, based on CDC data. His body mass index (BMI) is 18.98 kg/m2, which places him in the 42nd percentile, based on CDC data.",
"He is a thin, average-height male with an unremarkable examination. His sclera is white. His dentition is normal without caries. He is in Tanner stage 3 for puberty. No scoliosis is present. His extremities are thin but with appropriate muscle tone. He has no bowing and no birthmarks.",
"His laboratory results are as follows:",
"Intact parathyroid hormone (PTH) level: 65 pg/mL (reference range, 10-65 pg/mL)",
"Calcium PTH level: 7 mg/dL (reference range, 8.6-10.3 mg/dL)",
"Phosphorus level: 3 mg/dL (reference range, 2.7-4.6 mg/dL)",
"Alkaline phosphatase level: 370 IU/L (reference range, 90-420 IU/L)",
"Thyroid-stimulating hormone (TSH) level: 2.43 mIU/L (reference range, 0.3-5.5 mIU/L)",
"25-hydroxy vitamin D level: 20 ng/mL (reference range, 25-100 ng/mL)",
"Dual-energy x-ray absorptiometry (DEXA) scanning (Hologic Discovery A) reveals a left femoral neck Z-score of -0.8, a left hip Z-score of -1, and a lumbar spine Z-score of -1.8."
],
"date": "June 06, 2022",
"figures": [],
"markdown": "# An Athletic Teen Suddenly Prone to Falls and Fractures\n\n **Authors:** Inas H. Thomas, MD \n **Date:** June 06, 2022\n\n ## Content\n\n His weight is 109 lb 9.1 oz (49.7 kg), which places him in the 34th percentile based on the Centers for Disease Control and Prevention (CDC) weight-for-age data. His height is 5 ft 3.7 in (1.618 m), which places him in the 26th percentile, based on CDC data. His body mass index (BMI) is 18.98 kg/m2, which places him in the 42nd percentile, based on CDC data.\nHe is a thin, average-height male with an unremarkable examination. His sclera is white. His dentition is normal without caries. He is in Tanner stage 3 for puberty. No scoliosis is present. His extremities are thin but with appropriate muscle tone. He has no bowing and no birthmarks.\nHis laboratory results are as follows:\nIntact parathyroid hormone (PTH) level: 65 pg/mL (reference range, 10-65 pg/mL)\nCalcium PTH level: 7 mg/dL (reference range, 8.6-10.3 mg/dL)\nPhosphorus level: 3 mg/dL (reference range, 2.7-4.6 mg/dL)\nAlkaline phosphatase level: 370 IU/L (reference range, 90-420 IU/L)\nThyroid-stimulating hormone (TSH) level: 2.43 mIU/L (reference range, 0.3-5.5 mIU/L)\n25-hydroxy vitamin D level: 20 ng/mL (reference range, 25-100 ng/mL)\nDual-energy x-ray absorptiometry (DEXA) scanning (Hologic Discovery A) reveals a left femoral neck Z-score of -0.8, a left hip Z-score of -1, and a lumbar spine Z-score of -1.8.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 877193,
"choiceText": "Paget disease",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877195,
"choiceText": "Vitamin D deficiency",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877197,
"choiceText": "Osteogenesis imperfecta",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877199,
"choiceText": "Hypophosphatemic rickets\r\n\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 276123,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "An Athletic Teen Suddenly Prone to Falls and Fractures"
},
{
"authors": "Inas H. Thomas, MD",
"content": [
"This patient, who has uncontrolled type 1 diabetes, has had multiple fractures in the setting of vitamin D deficiency. DEXA scanning did not demonstrate low bone mineral density; his Z-scores were all above -2.[1] Of note, the spine and total body less head (TBLH) measurements are the most reliable sites for measuring bone density in growing children. The hip can have wide variability as the child grows, and comparing the images may be difficult.[1] Although he could have a complication of an autoimmune disorder, his 25-hydroxy vitamin D levels are lower than the reference range and must be corrected before any further evaluation is undertaken.",
"Diabetic osteopathy can alter the structure of the bone over time, leading to weaker bones that may easily fracture.[2] However, this patient has only had diabetes for the past 4 years and is not be expected to have frank diabetic complications yet.",
"The patient does not have many of the physical findings associated with osteogenesis imperfecta. Individuals affected with type 1 osteogenesis imperfecta are usually of normal height and have few bone deformities. This disorder usually becomes evident around the time children start to walk and improves after puberty. However, they usually have blue sclera, and about 50% of individuals experience hearing loss. Other types of osteogenesis imperfecta are more severe, with frequent fractures occurring perinatally to immediately postnatally. Short stature is usually associated along with many bone deformities. Varying degrees of dentinogenesis imperfecta and hearing loss can be present.[3]",
"This patient also did not demonstrate the phenotype of a child with hypophosphatemic rickets. Not only does he not have the bowing of legs, short stature, or abnormal dentition, his serum phosphorus level is high-normal and not low.[4] He is also not a likely candidate for Paget disease, as his alkaline phosphatase level was within the reference range and not elevated, as is typically the case in Paget disease."
],
"date": "June 06, 2022",
"figures": [],
"markdown": "# An Athletic Teen Suddenly Prone to Falls and Fractures\n\n **Authors:** Inas H. Thomas, MD \n **Date:** June 06, 2022\n\n ## Content\n\n This patient, who has uncontrolled type 1 diabetes, has had multiple fractures in the setting of vitamin D deficiency. DEXA scanning did not demonstrate low bone mineral density; his Z-scores were all above -2.[1] Of note, the spine and total body less head (TBLH) measurements are the most reliable sites for measuring bone density in growing children. The hip can have wide variability as the child grows, and comparing the images may be difficult.[1] Although he could have a complication of an autoimmune disorder, his 25-hydroxy vitamin D levels are lower than the reference range and must be corrected before any further evaluation is undertaken.\nDiabetic osteopathy can alter the structure of the bone over time, leading to weaker bones that may easily fracture.[2] However, this patient has only had diabetes for the past 4 years and is not be expected to have frank diabetic complications yet.\nThe patient does not have many of the physical findings associated with osteogenesis imperfecta. Individuals affected with type 1 osteogenesis imperfecta are usually of normal height and have few bone deformities. This disorder usually becomes evident around the time children start to walk and improves after puberty. However, they usually have blue sclera, and about 50% of individuals experience hearing loss. Other types of osteogenesis imperfecta are more severe, with frequent fractures occurring perinatally to immediately postnatally. Short stature is usually associated along with many bone deformities. Varying degrees of dentinogenesis imperfecta and hearing loss can be present.[3]\nThis patient also did not demonstrate the phenotype of a child with hypophosphatemic rickets. Not only does he not have the bowing of legs, short stature, or abnormal dentition, his serum phosphorus level is high-normal and not low.[4] He is also not a likely candidate for Paget disease, as his alkaline phosphatase level was within the reference range and not elevated, as is typically the case in Paget disease.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 877193,
"choiceText": "Paget disease",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877195,
"choiceText": "Vitamin D deficiency",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877197,
"choiceText": "Osteogenesis imperfecta",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877199,
"choiceText": "Hypophosphatemic rickets\r\n\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 276123,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "An Athletic Teen Suddenly Prone to Falls and Fractures"
},
{
"authors": "Inas H. Thomas, MD",
"content": [
"This patient's type 1 diabetes may contribute to low bone mineral density, which can increase his risk for fractures and also affect his ability to absorb vitamin D from his diet. However, his low vitamin D level needed to be addressed first. In the United States, vitamin D deficiency is prevalent, with different studies citing between 40% and 50% of teens as having vitamin D deficiency or insufficiency.[5] Many factors lead to vitamin D deficiency, including a change in diet (consuming less vitamin D-fortified milk), reduced time outdoors, and sun protection.[5] Medications such as antiseizure drugs and glucocorticoids can affect the metabolism of vitamin D, leading to increased requirements. Other disorders that can affect absorption of vitamin D, such as cystic fibrosis and Crohn disease, can also result in rickets due to vitamin D deficiency.[6]",
"The exact value that determines whether a patient is vitamin D sufficient is highly debated; most experts believe that a 25-hydroxy vitamin D level greater than 30-32 ng/mL excludes clinically significant deficiency.[6,7] PTH levels rise when 25-hydroxy vitamin D levels are below 20 ng/mL and stabilize when the level is more than 30 ng/mL.[8] Secondary hyperparathyroidism contributes to decreased bone mineral density by releasing calcium from the skeleton in order to maintain normal serum calcium levels. Phosphorus is also released and excreted in the urine, which may result in low or low-normal serum phosphorus levels. With the change in the calcium-phosphorus balance, mineralization is affected, which changes the architecture of the bones. This eventually may lead to small areas in the skeleton that are more fragile and at risk for fractures.[5]",
"Not only is vitamin D critical for maintaining adequate calcium and phosphorus levels and bone health, but it also may have other subtle roles. Vitamin D is known to affect the T lymphocytes and B lymphocytes in the immune system.[9] With that knowledge, studies are underway to assess how vitamin D affects certain autoimmune diseases such as type 1 diabetes and multiple sclerosis. Topical vitamin D medications are used to treat psoriasis because keratinocytes have vitamin D receptors. Additional studies are investigating the interaction of vitamin D on various cancers, mental health, and development.[9]"
],
"date": "June 06, 2022",
"figures": [],
"markdown": "# An Athletic Teen Suddenly Prone to Falls and Fractures\n\n **Authors:** Inas H. Thomas, MD \n **Date:** June 06, 2022\n\n ## Content\n\n This patient's type 1 diabetes may contribute to low bone mineral density, which can increase his risk for fractures and also affect his ability to absorb vitamin D from his diet. However, his low vitamin D level needed to be addressed first. In the United States, vitamin D deficiency is prevalent, with different studies citing between 40% and 50% of teens as having vitamin D deficiency or insufficiency.[5] Many factors lead to vitamin D deficiency, including a change in diet (consuming less vitamin D-fortified milk), reduced time outdoors, and sun protection.[5] Medications such as antiseizure drugs and glucocorticoids can affect the metabolism of vitamin D, leading to increased requirements. Other disorders that can affect absorption of vitamin D, such as cystic fibrosis and Crohn disease, can also result in rickets due to vitamin D deficiency.[6]\nThe exact value that determines whether a patient is vitamin D sufficient is highly debated; most experts believe that a 25-hydroxy vitamin D level greater than 30-32 ng/mL excludes clinically significant deficiency.[6,7] PTH levels rise when 25-hydroxy vitamin D levels are below 20 ng/mL and stabilize when the level is more than 30 ng/mL.[8] Secondary hyperparathyroidism contributes to decreased bone mineral density by releasing calcium from the skeleton in order to maintain normal serum calcium levels. Phosphorus is also released and excreted in the urine, which may result in low or low-normal serum phosphorus levels. With the change in the calcium-phosphorus balance, mineralization is affected, which changes the architecture of the bones. This eventually may lead to small areas in the skeleton that are more fragile and at risk for fractures.[5]\nNot only is vitamin D critical for maintaining adequate calcium and phosphorus levels and bone health, but it also may have other subtle roles. Vitamin D is known to affect the T lymphocytes and B lymphocytes in the immune system.[9] With that knowledge, studies are underway to assess how vitamin D affects certain autoimmune diseases such as type 1 diabetes and multiple sclerosis. Topical vitamin D medications are used to treat psoriasis because keratinocytes have vitamin D receptors. Additional studies are investigating the interaction of vitamin D on various cancers, mental health, and development.[9]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "An Athletic Teen Suddenly Prone to Falls and Fractures"
},
{
"authors": "Inas H. Thomas, MD",
"content": [
"The Endocrine Society Clinical Practice Guidelines for evaluation, treatment, and prevention of vitamin D deficiency released in 2011 gave recommendations for the amount of vitamin D per age group.[5] Infants (0-1 year) should receive 400 IU/day, and children aged 1-18 years should receive 600 IU/day; however, although those amounts should be sufficient, the guidelines acknowledged that 1000 IU/day may be needed if trying to maintain a serum 25-hydroxy vitamin D level above 30 ng/mL in those at risk for vitamin D deficiency. In adults aged 19-50 years, 600 IU/day should be adequate for daily activities; however, 1500-2000 IU/day may be necessary in those at risk.",
"Guidelines for Vitamin D Intake[5]",
"Age (years)",
"Recommendations",
"For Those at Risk for Vitamin D Deficiency",
"Upper Limit Recommended",
"0-1",
"400 IU",
"...",
"1000 IU",
"1-18",
"600 IU",
"600-1000 IU",
"4,000-10,000 IU",
"19-50",
"600 IU",
"1500-2000 IU",
"10,000 IU",
"Upper limits for the amount of vitamin D were also given by age to reduce the chance of achieving vitamin D intoxication, which is characterized by a 25-hydroxy vitamin D level of > 150 ng/mL, which may lead to hypercalcemia and hyperphosphatemia.[10]",
"Vitamin D levels should be checked in those at risk for vitamin D deficiency. Individuals who should be screened include[6,8]:",
"Children on chronic glucocorticoids, antiepileptic drugs, and antifungal medications",
"Those with chronic diseases that lead to malabsorption",
"Darker-skinned infants who live in higher-latitude areas with a lack of sunshine",
"Those with signs/symptoms of poor growth or irritability that could be due to an electrolyte abnormality",
"Those with frequent fractures",
"Women who are pregnant/lactating",
"Those with elevated alkaline phosphatase level for age",
"The vitamin D levels for the patient in this case were corrected. PTH and calcium levels within the reference range were observed 3 months after starting vitamin D. He continues to follow up with his primary care physician and consulting endocrinologist to control his type 1 diabetes and Hashimoto thyroiditis."
],
"date": "June 06, 2022",
"figures": [],
"markdown": "# An Athletic Teen Suddenly Prone to Falls and Fractures\n\n **Authors:** Inas H. Thomas, MD \n **Date:** June 06, 2022\n\n ## Content\n\n The Endocrine Society Clinical Practice Guidelines for evaluation, treatment, and prevention of vitamin D deficiency released in 2011 gave recommendations for the amount of vitamin D per age group.[5] Infants (0-1 year) should receive 400 IU/day, and children aged 1-18 years should receive 600 IU/day; however, although those amounts should be sufficient, the guidelines acknowledged that 1000 IU/day may be needed if trying to maintain a serum 25-hydroxy vitamin D level above 30 ng/mL in those at risk for vitamin D deficiency. In adults aged 19-50 years, 600 IU/day should be adequate for daily activities; however, 1500-2000 IU/day may be necessary in those at risk.\nGuidelines for Vitamin D Intake[5]\nAge (years)\nRecommendations\nFor Those at Risk for Vitamin D Deficiency\nUpper Limit Recommended\n0-1\n400 IU\n...\n1000 IU\n1-18\n600 IU\n600-1000 IU\n4,000-10,000 IU\n19-50\n600 IU\n1500-2000 IU\n10,000 IU\nUpper limits for the amount of vitamin D were also given by age to reduce the chance of achieving vitamin D intoxication, which is characterized by a 25-hydroxy vitamin D level of > 150 ng/mL, which may lead to hypercalcemia and hyperphosphatemia.[10]\nVitamin D levels should be checked in those at risk for vitamin D deficiency. Individuals who should be screened include[6,8]:\nChildren on chronic glucocorticoids, antiepileptic drugs, and antifungal medications\nThose with chronic diseases that lead to malabsorption\nDarker-skinned infants who live in higher-latitude areas with a lack of sunshine\nThose with signs/symptoms of poor growth or irritability that could be due to an electrolyte abnormality\nThose with frequent fractures\nWomen who are pregnant/lactating\nThose with elevated alkaline phosphatase level for age\nThe vitamin D levels for the patient in this case were corrected. PTH and calcium levels within the reference range were observed 3 months after starting vitamin D. He continues to follow up with his primary care physician and consulting endocrinologist to control his type 1 diabetes and Hashimoto thyroiditis.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 877201,
"choiceText": "Vitamin D at 1000 IU daily",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877203,
"choiceText": "Vitamin D at 50,000 IU weekly for 6 weeks",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877205,
"choiceText": "Calcium at 3000 mg daily",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877207,
"choiceText": "Increased sun exposure only",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The Endocrine Society Clinical Practice Guidelines recommend that individuals aged 1-18 years start with 2000 IU daily for at least 6 weeks or 50,000 IU weekly for at least 6 weeks. Once the goal 25-hydroxy vitamin D level is greater than 30 ng/mL, the individual can then be continued on 600-1000 IU daily as maintenance. In those with malabsorption, with obesity, or who are taking medications that interfere with vitamin D absorption, higher doses may be needed to accomplish this goal to replete and maintain the 25-hydroxy vitamin D level above 30 ng/mL. Calcium levels may increase with the improvement in vitamin D levels. Sun exposure alone is not enough to maintain appropriate vitamin D levels in teenaged individuals.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 276125,
"questionText": "An appropriate starting treatment plan for a patient like the one described in this case includes which of these?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 877209,
"choiceText": "Tissue transglutaminase immunoglobulin (Ig)A level with a concurrent IgA level",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877211,
"choiceText": "A1c",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877213,
"choiceText": "<em>COL1A1</em> gene",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877215,
"choiceText": "1,25-dihydroxy vitamin D",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "If vitamin D levels do not improve, the patient should be screened for <a href=\"http://emedicine.medscape.com/article/171805-overview\">celiac disease</a>, which is another autoimmune disorder associated with type 1 diabetes. Recommended screening for celiac disease varies; a reasonable approach would be to start with a tissue transglutaminase IgA level. A concurrent IgA level needs to be checked and documented as normal because this is an IgA antibody test and is not valid in those who have selective IgA deficiency. Upon a diagnosis of celiac disease, many children have decreased bone mineral density as determined by DEXA scan.<sup type=\"ref\">[11]</sup> This may be due to malabsorption of the fat-soluble vitamins that occur due to the inflammation of the intestine. With a gluten-free diet, bone mass density has been noted to improve within 1 year on DEXA scan, although it may not fully normalize.\r\n<br/><br/>\r\nA1c would not give additional information about fractures if the patient has diabetes that is now well controlled. Obtaining genetic testing of the <em>COL1A1</em> gene would only be warranted if it is suspected that the patient has osteogenesis imperfecta. While the 25-hydroxy vitamin D level is the amount of vitamin D stored, the 1,25-dihydroxy vitamin D is the active form. The half-life is much shorter than 25-hydroxy vitamin D (4-6 hours for 1,25-dihydroxy vitamin D compared with 2-3 weeks for 25-hydroxy vitamin D). This value also increases as the 25-hydroxy vitamin D level decreases and as the PTH increases 1,25-dihydroxy vitamin D to increase calcium absorption.\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 276127,
"questionText": "If, after treatment in a patient like the one described in this case, vitamin D levels do not improve, which study should be obtained?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "An Athletic Teen Suddenly Prone to Falls and Fractures"
},
{
"authors": "Inas H. Thomas, MD",
"content": [],
"date": "June 06, 2022",
"figures": [],
"markdown": "# An Athletic Teen Suddenly Prone to Falls and Fractures\n\n **Authors:** Inas H. Thomas, MD \n **Date:** June 06, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 877201,
"choiceText": "Vitamin D at 1000 IU daily",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877203,
"choiceText": "Vitamin D at 50,000 IU weekly for 6 weeks",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877205,
"choiceText": "Calcium at 3000 mg daily",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877207,
"choiceText": "Increased sun exposure only",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The Endocrine Society Clinical Practice Guidelines recommend that individuals aged 1-18 years start with 2000 IU daily for at least 6 weeks or 50,000 IU weekly for at least 6 weeks. Once the goal 25-hydroxy vitamin D level is greater than 30 ng/mL, the individual can then be continued on 600-1000 IU daily as maintenance. In those with malabsorption, with obesity, or who are taking medications that interfere with vitamin D absorption, higher doses may be needed to accomplish this goal to replete and maintain the 25-hydroxy vitamin D level above 30 ng/mL. Calcium levels may increase with the improvement in vitamin D levels. Sun exposure alone is not enough to maintain appropriate vitamin D levels in teenaged individuals.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 276125,
"questionText": "An appropriate starting treatment plan for a patient like the one described in this case includes which of these?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 877209,
"choiceText": "Tissue transglutaminase immunoglobulin (Ig)A level with a concurrent IgA level",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877211,
"choiceText": "A1c",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877213,
"choiceText": "<em>COL1A1</em> gene",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877215,
"choiceText": "1,25-dihydroxy vitamin D",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "If vitamin D levels do not improve, the patient should be screened for <a href=\"http://emedicine.medscape.com/article/171805-overview\">celiac disease</a>, which is another autoimmune disorder associated with type 1 diabetes. Recommended screening for celiac disease varies; a reasonable approach would be to start with a tissue transglutaminase IgA level. A concurrent IgA level needs to be checked and documented as normal because this is an IgA antibody test and is not valid in those who have selective IgA deficiency. Upon a diagnosis of celiac disease, many children have decreased bone mineral density as determined by DEXA scan.<sup type=\"ref\">[11]</sup> This may be due to malabsorption of the fat-soluble vitamins that occur due to the inflammation of the intestine. With a gluten-free diet, bone mass density has been noted to improve within 1 year on DEXA scan, although it may not fully normalize.\r\n<br/><br/>\r\nA1c would not give additional information about fractures if the patient has diabetes that is now well controlled. Obtaining genetic testing of the <em>COL1A1</em> gene would only be warranted if it is suspected that the patient has osteogenesis imperfecta. While the 25-hydroxy vitamin D level is the amount of vitamin D stored, the 1,25-dihydroxy vitamin D is the active form. The half-life is much shorter than 25-hydroxy vitamin D (4-6 hours for 1,25-dihydroxy vitamin D compared with 2-3 weeks for 25-hydroxy vitamin D). This value also increases as the 25-hydroxy vitamin D level decreases and as the PTH increases 1,25-dihydroxy vitamin D to increase calcium absorption.\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 276127,
"questionText": "If, after treatment in a patient like the one described in this case, vitamin D levels do not improve, which study should be obtained?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "An Athletic Teen Suddenly Prone to Falls and Fractures"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 877193,
"choiceText": "Paget disease",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877195,
"choiceText": "Vitamin D deficiency",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877197,
"choiceText": "Osteogenesis imperfecta",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877199,
"choiceText": "Hypophosphatemic rickets\r\n\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 276123,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 877201,
"choiceText": "Vitamin D at 1000 IU daily",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877203,
"choiceText": "Vitamin D at 50,000 IU weekly for 6 weeks",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877205,
"choiceText": "Calcium at 3000 mg daily",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877207,
"choiceText": "Increased sun exposure only",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The Endocrine Society Clinical Practice Guidelines recommend that individuals aged 1-18 years start with 2000 IU daily for at least 6 weeks or 50,000 IU weekly for at least 6 weeks. Once the goal 25-hydroxy vitamin D level is greater than 30 ng/mL, the individual can then be continued on 600-1000 IU daily as maintenance. In those with malabsorption, with obesity, or who are taking medications that interfere with vitamin D absorption, higher doses may be needed to accomplish this goal to replete and maintain the 25-hydroxy vitamin D level above 30 ng/mL. Calcium levels may increase with the improvement in vitamin D levels. Sun exposure alone is not enough to maintain appropriate vitamin D levels in teenaged individuals.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 276125,
"questionText": "An appropriate starting treatment plan for a patient like the one described in this case includes which of these?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 877209,
"choiceText": "Tissue transglutaminase immunoglobulin (Ig)A level with a concurrent IgA level",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877211,
"choiceText": "A1c",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877213,
"choiceText": "<em>COL1A1</em> gene",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 877215,
"choiceText": "1,25-dihydroxy vitamin D",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "If vitamin D levels do not improve, the patient should be screened for <a href=\"http://emedicine.medscape.com/article/171805-overview\">celiac disease</a>, which is another autoimmune disorder associated with type 1 diabetes. Recommended screening for celiac disease varies; a reasonable approach would be to start with a tissue transglutaminase IgA level. A concurrent IgA level needs to be checked and documented as normal because this is an IgA antibody test and is not valid in those who have selective IgA deficiency. Upon a diagnosis of celiac disease, many children have decreased bone mineral density as determined by DEXA scan.<sup type=\"ref\">[11]</sup> This may be due to malabsorption of the fat-soluble vitamins that occur due to the inflammation of the intestine. With a gluten-free diet, bone mass density has been noted to improve within 1 year on DEXA scan, although it may not fully normalize.\r\n<br/><br/>\r\nA1c would not give additional information about fractures if the patient has diabetes that is now well controlled. Obtaining genetic testing of the <em>COL1A1</em> gene would only be warranted if it is suspected that the patient has osteogenesis imperfecta. While the 25-hydroxy vitamin D level is the amount of vitamin D stored, the 1,25-dihydroxy vitamin D is the active form. The half-life is much shorter than 25-hydroxy vitamin D (4-6 hours for 1,25-dihydroxy vitamin D compared with 2-3 weeks for 25-hydroxy vitamin D). This value also increases as the 25-hydroxy vitamin D level decreases and as the PTH increases 1,25-dihydroxy vitamin D to increase calcium absorption.\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 276127,
"questionText": "If, after treatment in a patient like the one described in this case, vitamin D levels do not improve, which study should be obtained?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
885533 | /viewarticle/885533 | [
{
"authors": "Sunny B. Patel, MD; Richa Dhawan, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 60-year-old woman presents with nausea, vomiting, diarrhea, abdominal pain, and chest pain. She reports eating wings at a local restaurant 3 days prior, after which she developed nausea and subsequently had multiple episodes of nonbloody, nonbilious emesis and diarrhea. She reports that the emesis and diarrhea improved after 2 days; however, the substernal chest pain and epigastric abdominal pain, with radiation to her back, worsened, prompting her to seek medical attention. She denies any fevers, chills, sick contacts, diaphoresis, dizziness, shortness of breath, or palpitations.",
"She has a known past medical history of systemic lupus erythematosus (SLE); breast cancer, which was treated with lumpectomy, chemotherapy, and radiation and is now in remission; hypertension; diabetes mellitus; asthma; and osteoarthritis. About 2 months prior, her dose of prednisone was increased to 60 mg daily due to a lower-extremity rash thought to be secondary to lupus (Figure 1).",
"Figure 1.",
"Despite multiple medical comorbidities, she is still independently performing activities of daily living and doing well, without any recent hospitalizations."
],
"date": "May 31, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/885/533/885533-thumb2.jpg"
}
],
"markdown": "# A Woman With Back, Chest Pain After Eating Wings at a Restaurant\n\n **Authors:** Sunny B. Patel, MD; Richa Dhawan, MD \n **Date:** May 31, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 60-year-old woman presents with nausea, vomiting, diarrhea, abdominal pain, and chest pain. She reports eating wings at a local restaurant 3 days prior, after which she developed nausea and subsequently had multiple episodes of nonbloody, nonbilious emesis and diarrhea. She reports that the emesis and diarrhea improved after 2 days; however, the substernal chest pain and epigastric abdominal pain, with radiation to her back, worsened, prompting her to seek medical attention. She denies any fevers, chills, sick contacts, diaphoresis, dizziness, shortness of breath, or palpitations.\nShe has a known past medical history of systemic lupus erythematosus (SLE); breast cancer, which was treated with lumpectomy, chemotherapy, and radiation and is now in remission; hypertension; diabetes mellitus; asthma; and osteoarthritis. About 2 months prior, her dose of prednisone was increased to 60 mg daily due to a lower-extremity rash thought to be secondary to lupus (Figure 1).\nFigure 1.\nDespite multiple medical comorbidities, she is still independently performing activities of daily living and doing well, without any recent hospitalizations.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A Woman With Back, Chest Pain After Eating Wings at a Restaurant"
},
{
"authors": "Sunny B. Patel, MD; Richa Dhawan, MD",
"content": [
"Upon physical examination, the patient is afebrile with a heart rate of 95 beats/min, a respiratory rate of 16 breaths/min, and blood pressure of 165/86 mm Hg. She has a normal mood and affect, good hygiene, and is in mild distress due to pain. Her pupils are round and reactive to light, and her extraocular movements are intact bilaterally. Oral mucous membranes are moist. Lungs are clear to auscultation bilaterally.",
"Her heart rhythm is regular, and no murmurs, rubs, or gallops are observed. The abdomen is soft with positive bowel sounds, although mild tenderness is noted upon palpation of epigastric region. Well-healing discoid lupus lesions are noted on lower extremities. She is alert and oriented without any neurologic deficits.",
"Her laboratory test findings are as follows:",
"Hemoglobin level: 9.3 g/dL (reference range, 11.6-15 g/dL)",
"Platelet count: 9000 (reference range, 150,000-450,000)",
"Creatinine level: 2.2 mg/dL (reference range, 0.59-1.04 mg/dL)",
"Alanine aminotransferase (ALT) level: 109 U/L (reference range, 7 to 56 U/L)",
"Aspartate aminotransferase (AST) level: 234 U/L (reference range, 9-32 U/L)",
"Total bilirubin level: 4.3 mg/dL (reference range, 0.1-1.2 mg/dL)",
"Troponin level: 0.32 ng/mL (reference range, 0-0.04 ng/mL)",
"Lactate dehydrogenase (LDH) level: 1948 U/L (reference range, 105-333 U/L)",
"Haptoglobin level: < 8 mg/dL (reference range, 41-165 mg/dL)",
"Two months prior, her hemoglobin level, platelet count, and creatinine level were within the reference range. Antinuclear antibody test findings are positive, with titer of 1:320. Anti-Sjögren's-syndrome-related antigen (SSA) findings are positive. C3, C4, and anti-dsDNA findings are normal. Her prothrombin time (PT), partial thromboplastin time (PTT), fibrinogen level, and antithrombin III function are normal. She also has proteinuria and microscopic hematuria.",
"Her hepatitis panel is positive for hepatitis C virus infection, with confirmatory testing showing genotype 1a. This is a new finding, as her prior acute hepatitis panel 1 year ago was negative. A peripheral blood smear reveals schistocytes (Figure 2).",
"Figure 2.",
"Stool studies for Escherichia coli, Salmonella, Shigella, Campylobacter, Clostridium difficile, ova, and parasites are negative. Blood and urine culture findings are negative. Coombs test results are negative, and antiplatelet antibody findings are negative. An antiphospholipid syndrome panel finding is negative. ADAMTS13 inhibitor findings are negative, ADAMTS13 activity is 61% (reference range, > 67%), and ADAMTS13 antibody level is 71 (reference range, < 18).",
"Ultrasonography of the abdomen and CT of the abdomen and pelvis reveals perinephric fat stranding around the bilateral kidneys without evidence of obstruction; it is otherwise unremarkable, with normal liver and spleen findings. Echocardiography reveals normal left and right ventricular function."
],
"date": "May 31, 2022",
"figures": [
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/885/533/885533-thumb1.jpg"
}
],
"markdown": "# A Woman With Back, Chest Pain After Eating Wings at a Restaurant\n\n **Authors:** Sunny B. Patel, MD; Richa Dhawan, MD \n **Date:** May 31, 2022\n\n ## Content\n\n Upon physical examination, the patient is afebrile with a heart rate of 95 beats/min, a respiratory rate of 16 breaths/min, and blood pressure of 165/86 mm Hg. She has a normal mood and affect, good hygiene, and is in mild distress due to pain. Her pupils are round and reactive to light, and her extraocular movements are intact bilaterally. Oral mucous membranes are moist. Lungs are clear to auscultation bilaterally.\nHer heart rhythm is regular, and no murmurs, rubs, or gallops are observed. The abdomen is soft with positive bowel sounds, although mild tenderness is noted upon palpation of epigastric region. Well-healing discoid lupus lesions are noted on lower extremities. She is alert and oriented without any neurologic deficits.\nHer laboratory test findings are as follows:\nHemoglobin level: 9.3 g/dL (reference range, 11.6-15 g/dL)\nPlatelet count: 9000 (reference range, 150,000-450,000)\nCreatinine level: 2.2 mg/dL (reference range, 0.59-1.04 mg/dL)\nAlanine aminotransferase (ALT) level: 109 U/L (reference range, 7 to 56 U/L)\nAspartate aminotransferase (AST) level: 234 U/L (reference range, 9-32 U/L)\nTotal bilirubin level: 4.3 mg/dL (reference range, 0.1-1.2 mg/dL)\nTroponin level: 0.32 ng/mL (reference range, 0-0.04 ng/mL)\nLactate dehydrogenase (LDH) level: 1948 U/L (reference range, 105-333 U/L)\nHaptoglobin level: < 8 mg/dL (reference range, 41-165 mg/dL)\nTwo months prior, her hemoglobin level, platelet count, and creatinine level were within the reference range. Antinuclear antibody test findings are positive, with titer of 1:320. Anti-Sjögren's-syndrome-related antigen (SSA) findings are positive. C3, C4, and anti-dsDNA findings are normal. Her prothrombin time (PT), partial thromboplastin time (PTT), fibrinogen level, and antithrombin III function are normal. She also has proteinuria and microscopic hematuria.\nHer hepatitis panel is positive for hepatitis C virus infection, with confirmatory testing showing genotype 1a. This is a new finding, as her prior acute hepatitis panel 1 year ago was negative. A peripheral blood smear reveals schistocytes (Figure 2).\nFigure 2.\nStool studies for Escherichia coli, Salmonella, Shigella, Campylobacter, Clostridium difficile, ova, and parasites are negative. Blood and urine culture findings are negative. Coombs test results are negative, and antiplatelet antibody findings are negative. An antiphospholipid syndrome panel finding is negative. ADAMTS13 inhibitor findings are negative, ADAMTS13 activity is 61% (reference range, > 67%), and ADAMTS13 antibody level is 71 (reference range, < 18).\nUltrasonography of the abdomen and CT of the abdomen and pelvis reveals perinephric fat stranding around the bilateral kidneys without evidence of obstruction; it is otherwise unremarkable, with normal liver and spleen findings. Echocardiography reveals normal left and right ventricular function.\n\n ## Figures\n\n **Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136356,
"choiceText": "Antiphospholipid syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136358,
"choiceText": "Lupus-associated thrombotic thrombocytopenic purpura",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136360,
"choiceText": "Sepsis-induced thrombocytopenia",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136362,
"choiceText": "Idiopathic thrombocytopenic purpura",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136364,
"choiceText": "Disseminated intravascular coagulation",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360563,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Woman With Back, Chest Pain After Eating Wings at a Restaurant"
},
{
"authors": "Sunny B. Patel, MD; Richa Dhawan, MD",
"content": [
"The patient in this case presented in stable condition without major abnormal physical findings. Although her chest pain prompted presentation to the ED, this was found to be noncardiac and of lesser concern. Her workup revealed severe thrombocytopenia, which prompted further investigation, given that such low platelet counts can lead to hemorrhage, cerebrovascular events, and death. Even after determining a thrombotic microangiopathic process was occurring, the etiology was complicated by her known SLE, recent gastroenteritis, and newly diagnosed viral hepatitis C infection. The suspected gastroenteritis resolved, and stool study findings were negative, with no documented fever, leukocytosis, or other signs of sepsis. Viral hepatitis C may contribute to thrombocytopenia, but it does not account for an acute drop in both hemoglobin level and platelet count, as well as other abnormalities on laboratory findings.",
"Disseminated intravascular coagulation and antiphospholipid syndrome, two other etiologies for thrombocytopenia in patients with connective tissue disease, were unlikely, owing to the normal coagulation study findings and negative antiphospholipid panel results. Thus, an exacerbation of the patient's SLE most likely resulted in her presenting condition. In the past, her cutaneous manifestations of lupus were difficult to control, and she had been on multiple immunosuppressive agents, including prednisone, hydroxychloroquine, methotrexate, mycophenolate, and belimumab.",
"Cytopenias, including anemia, leukopenia or lymphopenia, and thrombocytopenia, are common manifestations of SLE; they may or may not be immune mediated. Almost 50% of patients with SLE have anemia; the most common etiologies are anemia of chronic disease and iron-deficiency anemia. Autoimmune hemolytic anemia is also observed, although Coombs test findings are positive in only 10% of patients with significant hemolysis."
],
"date": "May 31, 2022",
"figures": [],
"markdown": "# A Woman With Back, Chest Pain After Eating Wings at a Restaurant\n\n **Authors:** Sunny B. Patel, MD; Richa Dhawan, MD \n **Date:** May 31, 2022\n\n ## Content\n\n The patient in this case presented in stable condition without major abnormal physical findings. Although her chest pain prompted presentation to the ED, this was found to be noncardiac and of lesser concern. Her workup revealed severe thrombocytopenia, which prompted further investigation, given that such low platelet counts can lead to hemorrhage, cerebrovascular events, and death. Even after determining a thrombotic microangiopathic process was occurring, the etiology was complicated by her known SLE, recent gastroenteritis, and newly diagnosed viral hepatitis C infection. The suspected gastroenteritis resolved, and stool study findings were negative, with no documented fever, leukocytosis, or other signs of sepsis. Viral hepatitis C may contribute to thrombocytopenia, but it does not account for an acute drop in both hemoglobin level and platelet count, as well as other abnormalities on laboratory findings.\nDisseminated intravascular coagulation and antiphospholipid syndrome, two other etiologies for thrombocytopenia in patients with connective tissue disease, were unlikely, owing to the normal coagulation study findings and negative antiphospholipid panel results. Thus, an exacerbation of the patient's SLE most likely resulted in her presenting condition. In the past, her cutaneous manifestations of lupus were difficult to control, and she had been on multiple immunosuppressive agents, including prednisone, hydroxychloroquine, methotrexate, mycophenolate, and belimumab.\nCytopenias, including anemia, leukopenia or lymphopenia, and thrombocytopenia, are common manifestations of SLE; they may or may not be immune mediated. Almost 50% of patients with SLE have anemia; the most common etiologies are anemia of chronic disease and iron-deficiency anemia. Autoimmune hemolytic anemia is also observed, although Coombs test findings are positive in only 10% of patients with significant hemolysis.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136356,
"choiceText": "Antiphospholipid syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136358,
"choiceText": "Lupus-associated thrombotic thrombocytopenic purpura",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136360,
"choiceText": "Sepsis-induced thrombocytopenia",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136362,
"choiceText": "Idiopathic thrombocytopenic purpura",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136364,
"choiceText": "Disseminated intravascular coagulation",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360563,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Woman With Back, Chest Pain After Eating Wings at a Restaurant"
},
{
"authors": "Sunny B. Patel, MD; Richa Dhawan, MD",
"content": [
"Other causes of hemolytic anemia including medications, microangiopathic hemolytic anemia (MAHA), and infections (commonly malaria, babesiosis, nontyphoidal salmonella, E coli, HIV) should be ruled out.[1] This patient had a low likelihood of drug-induced hemolysis and no signs of protozoal or bacterial infection. MAHA is a rare but known hematologic manifestation of SLE that has been documented in case reports throughout the world; it was in the differential diagnosis for the patient in this case. This type of anemia is characterized by intravascular hemolysis, and laboratory findings include normocytic anemia, thrombocytopenia, low haptoglobin level, increased LDH level, and increased indirect bilirubin level.",
"Thrombotic thrombocytopenic purpura (TTP) is one of the primary thrombotic microangiopathy syndromes that cause MAHA. TTP is diagnosed based on clinical judgement and can affect multiple organ systems, including the neurologic, gastrointestinal, and renal systems. The entire classic pentad of thrombocytopenia, MAHA, neurologic abnormalities, renal dysfunction, and fever is rarely seen. In fact, this pentad was seen in only 5% of patients in data collected from the Oklahoma TTP-hemolytic-uremic syndrome (HUS) registry.[2] Out of 65 patients with a first episode of TTP, the most common initial presenting feature was gastrointestinal symptoms (pain, nausea, vomiting, diarrhea) followed by neurologic abnormalities (seizure, stroke, coma, confusion, headache).[2]",
"TTP is typically defined by a deficiency of ADAMTS13, a metalloprotease enzyme that cleaves von Willebrand factor. This could be hereditary through a genetic mutation or acquired through an autoantibody. However, measurements of ADAMTS13 are not required for diagnosis or for critical initial management decisions in TTP.",
"SLE and TTP are both rare diseases; thus, one can understand why SLE-associated TTP is an even rarer disease entity. One study identified only 56 such cases from 1968 to 2002.[3] The many overlapping clinical and laboratory features also make diagnosing TTP in patients with SLE difficult. Patients may be diagnosed with TTP following an established SLE diagnosis, but patients may also develop SLE following recovery from an episode of TTP. One case series found that TTP in association with SLE appears to be underdiagnosed and that a positive Coombs test finding does not rule out diagnosis of TTP in this setting.[4]",
"Another study from Toronto followed the course of 35 children with TTP and found that nine (26%) met the criteria for SLE, with an additional eight having features consistent with an incomplete lupus phenotype.[5] Some case reports of patients with TTP-associated SLE had normal or near-normal ADAMTS13 activity, suggesting a possible different pathogenetic mechanism than what occurs in TTP. Nonetheless, identifying and initiating treatment with plasma exchange for TTP early in patients with suspected exacerbation of SLE can be life-saving.",
"Recently, caplacizumab, a monoclonal antibody directed against von Willebrand factor, was introduced as a treatment for TTP.[6] When added to standard treatment with plasma exchange and high dose corticosteroids, caplacizumab reduces thrombotic events and improves outcomes.[7] This drug was not available at the time the patient in the case was treated."
],
"date": "May 31, 2022",
"figures": [],
"markdown": "# A Woman With Back, Chest Pain After Eating Wings at a Restaurant\n\n **Authors:** Sunny B. Patel, MD; Richa Dhawan, MD \n **Date:** May 31, 2022\n\n ## Content\n\n Other causes of hemolytic anemia including medications, microangiopathic hemolytic anemia (MAHA), and infections (commonly malaria, babesiosis, nontyphoidal salmonella, E coli, HIV) should be ruled out.[1] This patient had a low likelihood of drug-induced hemolysis and no signs of protozoal or bacterial infection. MAHA is a rare but known hematologic manifestation of SLE that has been documented in case reports throughout the world; it was in the differential diagnosis for the patient in this case. This type of anemia is characterized by intravascular hemolysis, and laboratory findings include normocytic anemia, thrombocytopenia, low haptoglobin level, increased LDH level, and increased indirect bilirubin level.\nThrombotic thrombocytopenic purpura (TTP) is one of the primary thrombotic microangiopathy syndromes that cause MAHA. TTP is diagnosed based on clinical judgement and can affect multiple organ systems, including the neurologic, gastrointestinal, and renal systems. The entire classic pentad of thrombocytopenia, MAHA, neurologic abnormalities, renal dysfunction, and fever is rarely seen. In fact, this pentad was seen in only 5% of patients in data collected from the Oklahoma TTP-hemolytic-uremic syndrome (HUS) registry.[2] Out of 65 patients with a first episode of TTP, the most common initial presenting feature was gastrointestinal symptoms (pain, nausea, vomiting, diarrhea) followed by neurologic abnormalities (seizure, stroke, coma, confusion, headache).[2]\nTTP is typically defined by a deficiency of ADAMTS13, a metalloprotease enzyme that cleaves von Willebrand factor. This could be hereditary through a genetic mutation or acquired through an autoantibody. However, measurements of ADAMTS13 are not required for diagnosis or for critical initial management decisions in TTP.\nSLE and TTP are both rare diseases; thus, one can understand why SLE-associated TTP is an even rarer disease entity. One study identified only 56 such cases from 1968 to 2002.[3] The many overlapping clinical and laboratory features also make diagnosing TTP in patients with SLE difficult. Patients may be diagnosed with TTP following an established SLE diagnosis, but patients may also develop SLE following recovery from an episode of TTP. One case series found that TTP in association with SLE appears to be underdiagnosed and that a positive Coombs test finding does not rule out diagnosis of TTP in this setting.[4]\nAnother study from Toronto followed the course of 35 children with TTP and found that nine (26%) met the criteria for SLE, with an additional eight having features consistent with an incomplete lupus phenotype.[5] Some case reports of patients with TTP-associated SLE had normal or near-normal ADAMTS13 activity, suggesting a possible different pathogenetic mechanism than what occurs in TTP. Nonetheless, identifying and initiating treatment with plasma exchange for TTP early in patients with suspected exacerbation of SLE can be life-saving.\nRecently, caplacizumab, a monoclonal antibody directed against von Willebrand factor, was introduced as a treatment for TTP.[6] When added to standard treatment with plasma exchange and high dose corticosteroids, caplacizumab reduces thrombotic events and improves outcomes.[7] This drug was not available at the time the patient in the case was treated.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A Woman With Back, Chest Pain After Eating Wings at a Restaurant"
},
{
"authors": "Sunny B. Patel, MD; Richa Dhawan, MD",
"content": [
"The patient in this case had hemolytic anemia, thrombocytopenia, hyperbilirubinemia, low C3, proteinuria, and recent discoid lupus rash. Her ADAMTS13 findings did come back slightly low, with elevated anti-ADAMTS13 autoantibody results; however, these studies often take longer than 1 week for results. The schistocytes noted on the peripheral blood smear were of greater concern. This prompted immediate initiation of daily plasma exchange. Plasma exchange is the combination of plasmapheresis, which may remove unusually large multimers of von Willebrand factor and autoantibodies against ADAMTS13, and infusion of fresh-frozen plasma or cryosupernatant, which contains additional metalloprotease. Plasma exchange has significantly improved survival rates of TTP, which was previously around 10%. Approximately 80% of patients now survive without permanent organ damage.[6]",
"The patient was also started on high-dose intravenous (IV) steroids (methylprednisolone, 1 g daily for 3 days) as part of treatment for TTP and exacerbation of SLE. Liver and kidney biopsies were deferred because the risks outweighed the benefits of performing each procedure. The management of this patient was discussed with an infectious disease specialist, given the newly diagnosed viral hepatitis C infection. Acute therapy for hepatitis C was postponed until after successful treatment of TTP due to the potential for worsening the condition.",
"This patient initially did well, with a platelet count nearing normal after 7 days of plasma exchange and IV steroids; however, she then had an exacerbation without any inciting factors, during which laboratory results again demonstrated thrombocytopenia, hemolytic anemia, a positive Coombs test result, and severe ADAMTS13 deficiency (activity level, 16%), as well as hypocomplementemia. Some data support the idea that higher titers of anti-ADAMTS13 autoantibodies (as in this patient) place patients at greater risk for complications and multiple exacerbations. Given the severity of illness and inadequate response, the patient was then given rituximab as adjuvant therapy.",
"The patient had a complicated hospitalization, with development of neurologic abnormalities, including confusion, headache, and left foot drop. She also developed renal failure that required hemodialysis, and multiple infections, including methicillin-sensitive Staphylococcus aureus and methicillin-resistant S aureus (MRSA) bacteremia, E coli pneumonia, and urinary tract infection (UTI) secondary to Klebsiella pneumoniae . Patients with TTP requiring ICU stay have a high mortality rate; this patient survived, however, and plasma exchange was subsequently tapered off after 32 sessions. Hemodialysis was no longer required and steroids were tapered. Given persistent the nonnephrotic range proteinuria and mild renal dysfunction, this patient will probably require a renal biopsy to help further guide long-term management, particularly if lupus nephritis or membranous proliferative glomerulonephritis is found. The patient was physically deconditioned, as is expected after a prolonged hospitalization, but her confusion and headache resolved and her hemoglobin level and platelet counts have remained stable, near baseline."
],
"date": "May 31, 2022",
"figures": [],
"markdown": "# A Woman With Back, Chest Pain After Eating Wings at a Restaurant\n\n **Authors:** Sunny B. Patel, MD; Richa Dhawan, MD \n **Date:** May 31, 2022\n\n ## Content\n\n The patient in this case had hemolytic anemia, thrombocytopenia, hyperbilirubinemia, low C3, proteinuria, and recent discoid lupus rash. Her ADAMTS13 findings did come back slightly low, with elevated anti-ADAMTS13 autoantibody results; however, these studies often take longer than 1 week for results. The schistocytes noted on the peripheral blood smear were of greater concern. This prompted immediate initiation of daily plasma exchange. Plasma exchange is the combination of plasmapheresis, which may remove unusually large multimers of von Willebrand factor and autoantibodies against ADAMTS13, and infusion of fresh-frozen plasma or cryosupernatant, which contains additional metalloprotease. Plasma exchange has significantly improved survival rates of TTP, which was previously around 10%. Approximately 80% of patients now survive without permanent organ damage.[6]\nThe patient was also started on high-dose intravenous (IV) steroids (methylprednisolone, 1 g daily for 3 days) as part of treatment for TTP and exacerbation of SLE. Liver and kidney biopsies were deferred because the risks outweighed the benefits of performing each procedure. The management of this patient was discussed with an infectious disease specialist, given the newly diagnosed viral hepatitis C infection. Acute therapy for hepatitis C was postponed until after successful treatment of TTP due to the potential for worsening the condition.\nThis patient initially did well, with a platelet count nearing normal after 7 days of plasma exchange and IV steroids; however, she then had an exacerbation without any inciting factors, during which laboratory results again demonstrated thrombocytopenia, hemolytic anemia, a positive Coombs test result, and severe ADAMTS13 deficiency (activity level, 16%), as well as hypocomplementemia. Some data support the idea that higher titers of anti-ADAMTS13 autoantibodies (as in this patient) place patients at greater risk for complications and multiple exacerbations. Given the severity of illness and inadequate response, the patient was then given rituximab as adjuvant therapy.\nThe patient had a complicated hospitalization, with development of neurologic abnormalities, including confusion, headache, and left foot drop. She also developed renal failure that required hemodialysis, and multiple infections, including methicillin-sensitive Staphylococcus aureus and methicillin-resistant S aureus (MRSA) bacteremia, E coli pneumonia, and urinary tract infection (UTI) secondary to Klebsiella pneumoniae . Patients with TTP requiring ICU stay have a high mortality rate; this patient survived, however, and plasma exchange was subsequently tapered off after 32 sessions. Hemodialysis was no longer required and steroids were tapered. Given persistent the nonnephrotic range proteinuria and mild renal dysfunction, this patient will probably require a renal biopsy to help further guide long-term management, particularly if lupus nephritis or membranous proliferative glomerulonephritis is found. The patient was physically deconditioned, as is expected after a prolonged hospitalization, but her confusion and headache resolved and her hemoglobin level and platelet counts have remained stable, near baseline.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136374,
"choiceText": "Low indirect bilirubin level",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136376,
"choiceText": "Thrombocytosis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136378,
"choiceText": "Elevated haptoglobin level",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136380,
"choiceText": "Normocytic anemia",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136382,
"choiceText": "Decreased LDH level",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "This type of anemia is characterized by intravascular hemolysis, and laboratory findings include normocytic anemia, thrombocytopenia, low haptoglobin level, increased LDH level, and increased indirect bilirubin level.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360567,
"questionText": "Which is most commonly associated with MAHA?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136410,
"choiceText": "Broad-spectrum antibiotics",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136412,
"choiceText": "Low-dose steroids",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136414,
"choiceText": "Plasma exchange and high-dose steroids",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136416,
"choiceText": "Hemodialysis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136418,
"choiceText": "Cyclosporine",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Plasma exchange is the combination of plasmapheresis, which may remove unusually large multimers of von Willebrand factor and autoantibodies against ADAMTS13, and infusion of fresh-frozen plasma or cryosupernatant, which contains additional metalloprotease. Plasma exchange has significantly improved survival rates of TTP, which was previously around 10%. Approximately 80% of patients now survive without permanent organ damage. Patients also receive high-dose intravenous steroids as part of treatment for TTP and exacerbation of SLE. Recently, caplacizumab, a monoclonal antibody directed against von Willebrand factor, was introduced as a treatment for TTP.<sup>[6]</sup> When added to standard treatment with plasma exchange and high dose corticosteroids, caplacizumab reduces thrombotic events and improves outcomes.<sup>[7]</sup> ",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360575,
"questionText": "You are treating a patient with SLE who is found to have hemolytic anemia, severe thrombocytopenia, neurological abnormalities, schistocytes on peripheral smear, and anti-ADAMTS13 autoantibodies. You suspect TTP-like syndrome. Which treatment option is initially indicated?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Woman With Back, Chest Pain After Eating Wings at a Restaurant"
},
{
"authors": "Sunny B. Patel, MD; Richa Dhawan, MD",
"content": [],
"date": "May 31, 2022",
"figures": [],
"markdown": "# A Woman With Back, Chest Pain After Eating Wings at a Restaurant\n\n **Authors:** Sunny B. Patel, MD; Richa Dhawan, MD \n **Date:** May 31, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136374,
"choiceText": "Low indirect bilirubin level",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136376,
"choiceText": "Thrombocytosis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136378,
"choiceText": "Elevated haptoglobin level",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136380,
"choiceText": "Normocytic anemia",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136382,
"choiceText": "Decreased LDH level",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "This type of anemia is characterized by intravascular hemolysis, and laboratory findings include normocytic anemia, thrombocytopenia, low haptoglobin level, increased LDH level, and increased indirect bilirubin level.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360567,
"questionText": "Which is most commonly associated with MAHA?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136410,
"choiceText": "Broad-spectrum antibiotics",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136412,
"choiceText": "Low-dose steroids",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136414,
"choiceText": "Plasma exchange and high-dose steroids",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136416,
"choiceText": "Hemodialysis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136418,
"choiceText": "Cyclosporine",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Plasma exchange is the combination of plasmapheresis, which may remove unusually large multimers of von Willebrand factor and autoantibodies against ADAMTS13, and infusion of fresh-frozen plasma or cryosupernatant, which contains additional metalloprotease. Plasma exchange has significantly improved survival rates of TTP, which was previously around 10%. Approximately 80% of patients now survive without permanent organ damage. Patients also receive high-dose intravenous steroids as part of treatment for TTP and exacerbation of SLE. Recently, caplacizumab, a monoclonal antibody directed against von Willebrand factor, was introduced as a treatment for TTP.<sup>[6]</sup> When added to standard treatment with plasma exchange and high dose corticosteroids, caplacizumab reduces thrombotic events and improves outcomes.<sup>[7]</sup> ",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360575,
"questionText": "You are treating a patient with SLE who is found to have hemolytic anemia, severe thrombocytopenia, neurological abnormalities, schistocytes on peripheral smear, and anti-ADAMTS13 autoantibodies. You suspect TTP-like syndrome. Which treatment option is initially indicated?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Woman With Back, Chest Pain After Eating Wings at a Restaurant"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136356,
"choiceText": "Antiphospholipid syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136358,
"choiceText": "Lupus-associated thrombotic thrombocytopenic purpura",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136360,
"choiceText": "Sepsis-induced thrombocytopenia",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136362,
"choiceText": "Idiopathic thrombocytopenic purpura",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136364,
"choiceText": "Disseminated intravascular coagulation",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360563,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136374,
"choiceText": "Low indirect bilirubin level",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136376,
"choiceText": "Thrombocytosis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136378,
"choiceText": "Elevated haptoglobin level",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136380,
"choiceText": "Normocytic anemia",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136382,
"choiceText": "Decreased LDH level",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "This type of anemia is characterized by intravascular hemolysis, and laboratory findings include normocytic anemia, thrombocytopenia, low haptoglobin level, increased LDH level, and increased indirect bilirubin level.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360567,
"questionText": "Which is most commonly associated with MAHA?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136410,
"choiceText": "Broad-spectrum antibiotics",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136412,
"choiceText": "Low-dose steroids",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136414,
"choiceText": "Plasma exchange and high-dose steroids",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136416,
"choiceText": "Hemodialysis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136418,
"choiceText": "Cyclosporine",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Plasma exchange is the combination of plasmapheresis, which may remove unusually large multimers of von Willebrand factor and autoantibodies against ADAMTS13, and infusion of fresh-frozen plasma or cryosupernatant, which contains additional metalloprotease. Plasma exchange has significantly improved survival rates of TTP, which was previously around 10%. Approximately 80% of patients now survive without permanent organ damage. Patients also receive high-dose intravenous steroids as part of treatment for TTP and exacerbation of SLE. Recently, caplacizumab, a monoclonal antibody directed against von Willebrand factor, was introduced as a treatment for TTP.<sup>[6]</sup> When added to standard treatment with plasma exchange and high dose corticosteroids, caplacizumab reduces thrombotic events and improves outcomes.<sup>[7]</sup> ",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360575,
"questionText": "You are treating a patient with SLE who is found to have hemolytic anemia, severe thrombocytopenia, neurological abnormalities, schistocytes on peripheral smear, and anti-ADAMTS13 autoantibodies. You suspect TTP-like syndrome. Which treatment option is initially indicated?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
845962 | /viewarticle/845962 | [
{
"authors": "Ziad R. Hubayter, MD, MPH",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.",
"A 33-year-old woman, gravida 0, presents owing to sudden onset of shortness of breath 1 week after in vitro fertilization (IVF). Her shortness of breath began acutely earlier in the day, but she states that for the past few days, she has had generalized abdominal pain associated with distention, nausea, and occasional nonbloody, nonbilious vomiting. Her pain became worse overnight, and she states that it now hurts in her abdomen when she takes a deep breath. She also cannot lie flat because it exacerbates both the pain and the difficulty with breathing.",
"She has a known history of polycystic ovary syndrome (PCOS) and has failed to conceive for several years. Three weeks before presentation, controlled ovarian stimulation was performed with gonadotropins. A total of 25 oocytes were retrieved. The peak estradiol during ovarian stimulation was 4638 pg/mL. She then underwent transvaginal ultrasonography-guided oocyte retrieval, followed by embryo transfer 1 week before presentation.",
"The patient's medical history is otherwise unremarkable. Other than the recent hormonal therapy, her only medication has been a daily multivitamin, and she has no known drug allergies. She does not smoke or use illicit drugs or alcohol."
],
"date": "May 19, 2022",
"figures": [],
"markdown": "# Ob/Gyn Case Challenge: A 33-Year-Old Woman Trying to Conceive Has Dyspnea, Pain\n\n **Authors:** Ziad R. Hubayter, MD, MPH \n **Date:** May 19, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.\nA 33-year-old woman, gravida 0, presents owing to sudden onset of shortness of breath 1 week after in vitro fertilization (IVF). Her shortness of breath began acutely earlier in the day, but she states that for the past few days, she has had generalized abdominal pain associated with distention, nausea, and occasional nonbloody, nonbilious vomiting. Her pain became worse overnight, and she states that it now hurts in her abdomen when she takes a deep breath. She also cannot lie flat because it exacerbates both the pain and the difficulty with breathing.\nShe has a known history of polycystic ovary syndrome (PCOS) and has failed to conceive for several years. Three weeks before presentation, controlled ovarian stimulation was performed with gonadotropins. A total of 25 oocytes were retrieved. The peak estradiol during ovarian stimulation was 4638 pg/mL. She then underwent transvaginal ultrasonography-guided oocyte retrieval, followed by embryo transfer 1 week before presentation.\nThe patient's medical history is otherwise unremarkable. Other than the recent hormonal therapy, her only medication has been a daily multivitamin, and she has no known drug allergies. She does not smoke or use illicit drugs or alcohol.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Ob/Gyn Case Challenge: A 33-Year-Old Woman Trying to Conceive Has Dyspnea, Pain"
},
{
"authors": "Ziad R. Hubayter, MD, MPH",
"content": [
"Upon physical examination, the patient is awake, alert, and oriented. She appears to be in moderate distress. Her pulse is 108 beats/min, and her blood pressure is 110/60 mm Hg. She has rapid, shallow breathing, with a respiratory rate of 26 breaths/min. The pulse oximetry reading is 95% while she is breathing room air, but it rises to 98% on 2 L/min oxygen supplementation.",
"The patient weighs 200 lbs (90.7 kg). Head and neck examination findings are unremarkable, without jugular venous distention. Her pulmonary examination reveals egophony, bilaterally decreased breath sounds, and a loss of tactile fremitus. The heart is regular, tachycardic, and without murmurs. The abdomen is distended, but normal bowel sounds are noted. No palpable mass or organomegaly is noted, but she exhibits moderate tenderness to palpation throughout the abdomen, with a positive fluid wave. A pelvic speculum examination reveals no vaginal bleeding or discharge. The bimanual examination is deferred.",
"Serum blood testing performed in the emergency department reveals a white blood cell count of 12.2 × 109/L (reference range, 4.5 to 11.0 × 109/L), hemoglobin level of 16.2 g/dL (reference range, 11.6-15 g/dL), hematocrit of 48.7% (reference range, 35.5% to 44.9%), sodium level of 130 mEq (reference range, 135-145 mEq), potassium level of 5.2 mEq/L (reference range, 3.5-5 mEq/L), blood urea nitrogen level of 10 mg/dL (reference range, 6-24 mg/dL), and creatinine concentration of 1 mg/dL (reference range, 0.59 to 1.04 mg/dL). Liver function tests and the remaining chemistry profile are normal.",
"An abdomen-shielded chest radiograph is obtained that reveals bilateral pleural effusions (not shown). Transvaginal ultrasonography is also obtained (Figures 1 and 2).",
"Figure 1.",
"Figure 1.",
"Figure 2.",
"Figure 2."
],
"date": "May 19, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/845/962/845962-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/845/962/845962-Thumb2.png"
}
],
"markdown": "# Ob/Gyn Case Challenge: A 33-Year-Old Woman Trying to Conceive Has Dyspnea, Pain\n\n **Authors:** Ziad R. Hubayter, MD, MPH \n **Date:** May 19, 2022\n\n ## Content\n\n Upon physical examination, the patient is awake, alert, and oriented. She appears to be in moderate distress. Her pulse is 108 beats/min, and her blood pressure is 110/60 mm Hg. She has rapid, shallow breathing, with a respiratory rate of 26 breaths/min. The pulse oximetry reading is 95% while she is breathing room air, but it rises to 98% on 2 L/min oxygen supplementation.\nThe patient weighs 200 lbs (90.7 kg). Head and neck examination findings are unremarkable, without jugular venous distention. Her pulmonary examination reveals egophony, bilaterally decreased breath sounds, and a loss of tactile fremitus. The heart is regular, tachycardic, and without murmurs. The abdomen is distended, but normal bowel sounds are noted. No palpable mass or organomegaly is noted, but she exhibits moderate tenderness to palpation throughout the abdomen, with a positive fluid wave. A pelvic speculum examination reveals no vaginal bleeding or discharge. The bimanual examination is deferred.\nSerum blood testing performed in the emergency department reveals a white blood cell count of 12.2 × 109/L (reference range, 4.5 to 11.0 × 109/L), hemoglobin level of 16.2 g/dL (reference range, 11.6-15 g/dL), hematocrit of 48.7% (reference range, 35.5% to 44.9%), sodium level of 130 mEq (reference range, 135-145 mEq), potassium level of 5.2 mEq/L (reference range, 3.5-5 mEq/L), blood urea nitrogen level of 10 mg/dL (reference range, 6-24 mg/dL), and creatinine concentration of 1 mg/dL (reference range, 0.59 to 1.04 mg/dL). Liver function tests and the remaining chemistry profile are normal.\nAn abdomen-shielded chest radiograph is obtained that reveals bilateral pleural effusions (not shown). Transvaginal ultrasonography is also obtained (Figures 1 and 2).\nFigure 1.\nFigure 1.\nFigure 2.\nFigure 2.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 852575,
"choiceText": "Heterotopic pregnancy",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 852577,
"choiceText": "Ovarian torsion",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 852579,
"choiceText": "Ovarian hyperstimulation syndrome",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 852581,
"choiceText": "Pulmonary embolism",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 267919,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Ob/Gyn Case Challenge: A 33-Year-Old Woman Trying to Conceive Has Dyspnea, Pain"
},
{
"authors": "Ziad R. Hubayter, MD, MPH",
"content": [
"The clinical presentation of this patient was strongly suggestive of ovarian hyperstimulation syndrome (OHSS), a known complication of IVF. In this case, the severity of the symptoms, including the respiratory status, marked ascites (Figure 1), hyponatremia, and the large ovarian volume (Figure 2) indicated that this patient had severe OHSS.",
"Figure 1.",
"Figure 1.",
"Figure 2.",
"Figure 2.",
"Because 1 of every 6 couples face infertility issues and the demand for IVF may be on the rise owing to delayed childbearing (resulting from later age at marriage, divorce and remarriage, professional careers, and economic hardship), healthcare providers need to be familiar with this condition.",
"During a cycle of IVF, a woman receives gonadotropin stimulation for around 2 weeks until several follicles achieve a diameter larger than 18 mm. Once appropriately sized follicles develop, a dose of human chorionic gonadotropin (hCG) is administered to cause maturation of the oocytes before transvaginal oocyte retrieval. The hCG leads to luteinization of the large number of follicles.",
"In OHSS, the enlarged and luteinized ovaries produce a large amount of vascular endothelial growth factor (VEGF). VEGF is a vasoactive substance that may cause leaky capillary membranes. Subsequently, fluid shifts out of the intravascular space and into the lungs and peritoneum, causing pleural effusions, pulmonary edema, or ascites.[1,2]",
"The clinical symptoms of OHSS include bloating, nausea, vomiting, fatigue, shortness of breath, rapid weight gain, and decreased urine output. Third spacing may cause fluid to accumulate in the pleural and peritoneal spaces. The resulting decreased intravascular volume may cause hypotension, tachycardia, hemoconcentration, and decreased renal blood flow, resulting in renal failure, hyponatremia, and hyperkalemia.",
"Pelvic ultrasonography usually demonstrates ascites and bilaterally enlarged ovaries with multiple cysts. Ovarian torsion or rupture with internal bleeding may also occur. Other severe complications include hypovolemic shock, thromboembolic episode, acute respiratory distress syndrome, and, very rarely, death.[1,3]",
"Risk factors for OHSS include young age, low body weight, high serum estradiol concentrations, polycystic ovaries, higher doses of gonadotropins during ovarian stimulation, and a greater number of oocytes retrieved. The disease is self-limited and usually resolves within 1 week; however, if a patient becomes pregnant in the future, the endogenous production of hCG may lead to a recurrence of OHSS, which is then typically more severe than the previous incidence.[1,4]"
],
"date": "May 19, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/845/962/845962-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/845/962/845962-Thumb2.png"
}
],
"markdown": "# Ob/Gyn Case Challenge: A 33-Year-Old Woman Trying to Conceive Has Dyspnea, Pain\n\n **Authors:** Ziad R. Hubayter, MD, MPH \n **Date:** May 19, 2022\n\n ## Content\n\n The clinical presentation of this patient was strongly suggestive of ovarian hyperstimulation syndrome (OHSS), a known complication of IVF. In this case, the severity of the symptoms, including the respiratory status, marked ascites (Figure 1), hyponatremia, and the large ovarian volume (Figure 2) indicated that this patient had severe OHSS.\nFigure 1.\nFigure 1.\nFigure 2.\nFigure 2.\nBecause 1 of every 6 couples face infertility issues and the demand for IVF may be on the rise owing to delayed childbearing (resulting from later age at marriage, divorce and remarriage, professional careers, and economic hardship), healthcare providers need to be familiar with this condition.\nDuring a cycle of IVF, a woman receives gonadotropin stimulation for around 2 weeks until several follicles achieve a diameter larger than 18 mm. Once appropriately sized follicles develop, a dose of human chorionic gonadotropin (hCG) is administered to cause maturation of the oocytes before transvaginal oocyte retrieval. The hCG leads to luteinization of the large number of follicles.\nIn OHSS, the enlarged and luteinized ovaries produce a large amount of vascular endothelial growth factor (VEGF). VEGF is a vasoactive substance that may cause leaky capillary membranes. Subsequently, fluid shifts out of the intravascular space and into the lungs and peritoneum, causing pleural effusions, pulmonary edema, or ascites.[1,2]\nThe clinical symptoms of OHSS include bloating, nausea, vomiting, fatigue, shortness of breath, rapid weight gain, and decreased urine output. Third spacing may cause fluid to accumulate in the pleural and peritoneal spaces. The resulting decreased intravascular volume may cause hypotension, tachycardia, hemoconcentration, and decreased renal blood flow, resulting in renal failure, hyponatremia, and hyperkalemia.\nPelvic ultrasonography usually demonstrates ascites and bilaterally enlarged ovaries with multiple cysts. Ovarian torsion or rupture with internal bleeding may also occur. Other severe complications include hypovolemic shock, thromboembolic episode, acute respiratory distress syndrome, and, very rarely, death.[1,3]\nRisk factors for OHSS include young age, low body weight, high serum estradiol concentrations, polycystic ovaries, higher doses of gonadotropins during ovarian stimulation, and a greater number of oocytes retrieved. The disease is self-limited and usually resolves within 1 week; however, if a patient becomes pregnant in the future, the endogenous production of hCG may lead to a recurrence of OHSS, which is then typically more severe than the previous incidence.[1,4]\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 852575,
"choiceText": "Heterotopic pregnancy",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 852577,
"choiceText": "Ovarian torsion",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 852579,
"choiceText": "Ovarian hyperstimulation syndrome",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 852581,
"choiceText": "Pulmonary embolism",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 267919,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Ob/Gyn Case Challenge: A 33-Year-Old Woman Trying to Conceive Has Dyspnea, Pain"
},
{
"authors": "Ziad R. Hubayter, MD, MPH",
"content": [
"The treatment of OHSS is primarily supportive and includes rehydration with intravenous normal saline, treatment of electrolyte abnormalities, and discontinuation of fertility agents. It is important to remember that a bimanual pelvic examination should not be performed because it may rupture the enlarged, friable ovaries that could result from IVF and transvaginal oocyte retrieval.",
"The goal of giving intravenous fluids is to achieve a urine output of around 25-30 mL/hr. Overly aggressive fluid resuscitation may worsen the condition because of third spacing. The fluid of choice is normal saline because it maintains fluid within the intravascular volume better than other solutions, such as lactated Ringer solution or half-normal saline.",
"Once the desired urine output is achieved, the patient is monitored for symptomatic improvement. If ascites is severe, paracentesis may improve both the pain and ventilation. Unfortunately, ascites typically recur within 24-48 hours after paracentesis.[1,3,4]",
"Pulmonary complications associated with the diagnosis, treatment, and prevention of OHSS deserve special mention. Patients with OHSS almost always have some degree of pleural effusion, most commonly on the right side. Because of the increased permeability of capillary membranes, the patient is at risk for pulmonary edema. This condition reinforces the need for judicious use of intravenous fluids. The most serious pulmonary complication is pulmonary embolism.",
"Patients with OHSS have an increased risk for thromboembolism caused by supraphysiologic estradiol levels and hyperviscosity from hemoconcentration. Of note, 25% of these thrombotic events are arterial. Moreover, at least one half of the primary sites of these events occur above the level of the umbilicus (eg, internal jugular, subclavian, axillary, and mesenteric vessels).",
"Upper-extremity deep vein thromboses are observed in 0.11% of women undergoing assisted reproductive techniques. Therefore, administration of prophylactic heparin is recommended once the hematocrit reaches a concentration higher than 48%.[1,3,4]",
"Although patients with mild cases of OHSS may be discharged home with close follow-up, admission is recommended for patients who demonstrate any of the following markers of severity[3]:",
"Severe abdominal pain or peritoneal signs",
"Severe nausea or vomiting",
"Oliguria (<50 mL/hr)",
"Tense ascites",
"Dyspnea",
"Tachypnea",
"Hypotension",
"Electrolyte imbalance",
"Hemoconcentration",
"Abnormal liver function test findings"
],
"date": "May 19, 2022",
"figures": [],
"markdown": "# Ob/Gyn Case Challenge: A 33-Year-Old Woman Trying to Conceive Has Dyspnea, Pain\n\n **Authors:** Ziad R. Hubayter, MD, MPH \n **Date:** May 19, 2022\n\n ## Content\n\n The treatment of OHSS is primarily supportive and includes rehydration with intravenous normal saline, treatment of electrolyte abnormalities, and discontinuation of fertility agents. It is important to remember that a bimanual pelvic examination should not be performed because it may rupture the enlarged, friable ovaries that could result from IVF and transvaginal oocyte retrieval.\nThe goal of giving intravenous fluids is to achieve a urine output of around 25-30 mL/hr. Overly aggressive fluid resuscitation may worsen the condition because of third spacing. The fluid of choice is normal saline because it maintains fluid within the intravascular volume better than other solutions, such as lactated Ringer solution or half-normal saline.\nOnce the desired urine output is achieved, the patient is monitored for symptomatic improvement. If ascites is severe, paracentesis may improve both the pain and ventilation. Unfortunately, ascites typically recur within 24-48 hours after paracentesis.[1,3,4]\nPulmonary complications associated with the diagnosis, treatment, and prevention of OHSS deserve special mention. Patients with OHSS almost always have some degree of pleural effusion, most commonly on the right side. Because of the increased permeability of capillary membranes, the patient is at risk for pulmonary edema. This condition reinforces the need for judicious use of intravenous fluids. The most serious pulmonary complication is pulmonary embolism.\nPatients with OHSS have an increased risk for thromboembolism caused by supraphysiologic estradiol levels and hyperviscosity from hemoconcentration. Of note, 25% of these thrombotic events are arterial. Moreover, at least one half of the primary sites of these events occur above the level of the umbilicus (eg, internal jugular, subclavian, axillary, and mesenteric vessels).\nUpper-extremity deep vein thromboses are observed in 0.11% of women undergoing assisted reproductive techniques. Therefore, administration of prophylactic heparin is recommended once the hematocrit reaches a concentration higher than 48%.[1,3,4]\nAlthough patients with mild cases of OHSS may be discharged home with close follow-up, admission is recommended for patients who demonstrate any of the following markers of severity[3]:\nSevere abdominal pain or peritoneal signs\nSevere nausea or vomiting\nOliguria (<50 mL/hr)\nTense ascites\nDyspnea\nTachypnea\nHypotension\nElectrolyte imbalance\nHemoconcentration\nAbnormal liver function test findings\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Ob/Gyn Case Challenge: A 33-Year-Old Woman Trying to Conceive Has Dyspnea, Pain"
},
{
"authors": "Ziad R. Hubayter, MD, MPH",
"content": [
"Interventions to prevent OHSS include the following:[5,6]",
"Decreased hormone dosage and aborting cycles if estrogen levels are too high or too many follicles are present",
"Less-risky ovarian protocols using gonadotropin-releasing hormone (GnRH) or luteinizing hormone-releasing hormone antagonists for ovarian suppression",
"GnRH agonists triggering versus hCG for oocyte maturation",
"Dopamine agonists that reduce VEGF production",
"Metformin use for patients with PCOS",
"Although rates and severity have decreased with use of these techniques, the problem remains, and efforts to further reduce risk must continue.[7]",
"The patient in this case was hospitalized and was given enough intravenous normal saline to maintain adequate urine output. The repletion of intravascular volume also corrected the hyponatremia and the hyperkalemia. Upon gentle diuresis, the ascites and the pleural effusion improved.",
"Because the patient was experiencing shortness of breath and had an elevated hematocrit, arterial blood gas analysis was obtained, despite the normal pulse oximetry results. The arterial blood gas was normal. Heparin was started for thromboembolic prophylaxis, and the patient was eventually discharged in stable condition.",
"Two weeks later, the patient's symptoms returned, and she had a similar course of events. With similar management and paracentesis, the symptoms ultimately subsided. The recurrence coincided with a positive pregnancy test. Endogenous hormonal production during pregnancy is known to reactivate OHSS. After a brief hospitalization, she was again discharged to home, where her pregnancy has progressed without further complication."
],
"date": "May 19, 2022",
"figures": [],
"markdown": "# Ob/Gyn Case Challenge: A 33-Year-Old Woman Trying to Conceive Has Dyspnea, Pain\n\n **Authors:** Ziad R. Hubayter, MD, MPH \n **Date:** May 19, 2022\n\n ## Content\n\n Interventions to prevent OHSS include the following:[5,6]\nDecreased hormone dosage and aborting cycles if estrogen levels are too high or too many follicles are present\nLess-risky ovarian protocols using gonadotropin-releasing hormone (GnRH) or luteinizing hormone-releasing hormone antagonists for ovarian suppression\nGnRH agonists triggering versus hCG for oocyte maturation\nDopamine agonists that reduce VEGF production\nMetformin use for patients with PCOS\nAlthough rates and severity have decreased with use of these techniques, the problem remains, and efforts to further reduce risk must continue.[7]\nThe patient in this case was hospitalized and was given enough intravenous normal saline to maintain adequate urine output. The repletion of intravascular volume also corrected the hyponatremia and the hyperkalemia. Upon gentle diuresis, the ascites and the pleural effusion improved.\nBecause the patient was experiencing shortness of breath and had an elevated hematocrit, arterial blood gas analysis was obtained, despite the normal pulse oximetry results. The arterial blood gas was normal. Heparin was started for thromboembolic prophylaxis, and the patient was eventually discharged in stable condition.\nTwo weeks later, the patient's symptoms returned, and she had a similar course of events. With similar management and paracentesis, the symptoms ultimately subsided. The recurrence coincided with a positive pregnancy test. Endogenous hormonal production during pregnancy is known to reactivate OHSS. After a brief hospitalization, she was again discharged to home, where her pregnancy has progressed without further complication.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 852583,
"choiceText": "Pulmonary embolism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 852585,
"choiceText": "Pleural effusion",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 852587,
"choiceText": "Cardiac tamponade",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 852589,
"choiceText": "Tense ascites",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 852591,
"choiceText": "Pulmonary edema resulting from capillary leak",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Fluid shifting out of the intravascular space and into the lungs and peritoneum can cause pleural effusion, pulmonary edema, or ascites. The most serious pulmonary complication is pulmonary embolism. Patients with OHSS have an increased risk for thromboembolism caused by supraphysiologic estradiol levels and hyperviscosity from hemoconcentration.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 267921,
"questionText": "You are examining a patient with suspected OHSS. Among other symptoms, you note that the patient has dyspnea. Which of the following findings is <i>least</i> likely to occur in association with the patient's dyspnea and OHSS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 855283,
"choiceText": "Paracentesis",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 855285,
"choiceText": "Bimanual pelvic examination",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 855287,
"choiceText": "Transvaginal ultrasonography",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 855289,
"choiceText": "Intravenous fluid administration",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "A bimanual pelvic examination should not be performed because it may rupture the enlarged, friable ovaries that could result from IVF and transvaginal oocyte retrieval.",
"displayOrder": 4,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 268761,
"questionText": "Which of the following examinations or interventions may exacerbate the above patient's suspected OHSS and should be avoided during your investigation?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Ob/Gyn Case Challenge: A 33-Year-Old Woman Trying to Conceive Has Dyspnea, Pain"
},
{
"authors": "Ziad R. Hubayter, MD, MPH",
"content": [],
"date": "May 19, 2022",
"figures": [],
"markdown": "# Ob/Gyn Case Challenge: A 33-Year-Old Woman Trying to Conceive Has Dyspnea, Pain\n\n **Authors:** Ziad R. Hubayter, MD, MPH \n **Date:** May 19, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 852583,
"choiceText": "Pulmonary embolism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 852585,
"choiceText": "Pleural effusion",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 852587,
"choiceText": "Cardiac tamponade",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 852589,
"choiceText": "Tense ascites",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 852591,
"choiceText": "Pulmonary edema resulting from capillary leak",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Fluid shifting out of the intravascular space and into the lungs and peritoneum can cause pleural effusion, pulmonary edema, or ascites. The most serious pulmonary complication is pulmonary embolism. Patients with OHSS have an increased risk for thromboembolism caused by supraphysiologic estradiol levels and hyperviscosity from hemoconcentration.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 267921,
"questionText": "You are examining a patient with suspected OHSS. Among other symptoms, you note that the patient has dyspnea. Which of the following findings is <i>least</i> likely to occur in association with the patient's dyspnea and OHSS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 855283,
"choiceText": "Paracentesis",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 855285,
"choiceText": "Bimanual pelvic examination",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 855287,
"choiceText": "Transvaginal ultrasonography",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 855289,
"choiceText": "Intravenous fluid administration",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "A bimanual pelvic examination should not be performed because it may rupture the enlarged, friable ovaries that could result from IVF and transvaginal oocyte retrieval.",
"displayOrder": 4,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 268761,
"questionText": "Which of the following examinations or interventions may exacerbate the above patient's suspected OHSS and should be avoided during your investigation?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Ob/Gyn Case Challenge: A 33-Year-Old Woman Trying to Conceive Has Dyspnea, Pain"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 852575,
"choiceText": "Heterotopic pregnancy",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 852577,
"choiceText": "Ovarian torsion",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 852579,
"choiceText": "Ovarian hyperstimulation syndrome",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 852581,
"choiceText": "Pulmonary embolism",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 267919,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 852583,
"choiceText": "Pulmonary embolism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 852585,
"choiceText": "Pleural effusion",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 852587,
"choiceText": "Cardiac tamponade",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 852589,
"choiceText": "Tense ascites",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 852591,
"choiceText": "Pulmonary edema resulting from capillary leak",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Fluid shifting out of the intravascular space and into the lungs and peritoneum can cause pleural effusion, pulmonary edema, or ascites. The most serious pulmonary complication is pulmonary embolism. Patients with OHSS have an increased risk for thromboembolism caused by supraphysiologic estradiol levels and hyperviscosity from hemoconcentration.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 267921,
"questionText": "You are examining a patient with suspected OHSS. Among other symptoms, you note that the patient has dyspnea. Which of the following findings is <i>least</i> likely to occur in association with the patient's dyspnea and OHSS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 855283,
"choiceText": "Paracentesis",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 855285,
"choiceText": "Bimanual pelvic examination",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 855287,
"choiceText": "Transvaginal ultrasonography",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 855289,
"choiceText": "Intravenous fluid administration",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "A bimanual pelvic examination should not be performed because it may rupture the enlarged, friable ovaries that could result from IVF and transvaginal oocyte retrieval.",
"displayOrder": 4,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 268761,
"questionText": "Which of the following examinations or interventions may exacerbate the above patient's suspected OHSS and should be avoided during your investigation?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
973953 | /viewarticle/973953 | [
{
"authors": "Catherine Divingian, MD, PhD; Valerie Gironda, MD; Francisco Torano, MD; Jeffrey Jordan, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 59-year-old man is rushed to the emergency department (ED) after he experienced intense, sudden-onset pain, particularly on the right side of his flank and lumbar region. Initially, the patient had presented to his primary care physician with orthopnea, dyspnea on exertion, and an increase in peripheral edema over the past few weeks. Laboratory test results were within normal limits, with the exception of these elevated values:",
"Fasting glucose level: 127 mg/dL (reference range, 70-99 mg/dL)",
"Leukocyte count: 11,520 cells/µL (reference range, 4000-11,000 cells/µL)",
"Low-density lipoprotein cholesterol level: 126 mg/dL (reference range, < 100 mg/dL)",
"Triglyceride level: 162 mg/dL (reference range, < 150 mg/dL)",
"He was referred to a cardiologist and had just completed an echocardiogram that morning as part of the workup before he collapsed in the hallway.",
"The patient has a past medical history of coronary artery disease, hypertension, and hyperlipidemia. He underwent emergent coronary angiography 5 years earlier and had two stents placed in the diagonal arteries. His current medications include metoprolol tartrate, atorvastatin, aspirin, and amlodipine. He states that he takes his medications and regularly follows up with his primary care physician.",
"The patient smoked cigarettes for more than 35 years, starting at age 18 years, but quit nearly 7 years ago. He does not drink alcohol or use illicit drugs."
],
"date": "May 19, 2022",
"figures": [],
"markdown": "# A Patient Who Collapsed in Agony After Echocardiography\n\n **Authors:** Catherine Divingian, MD, PhD; Valerie Gironda, MD; Francisco Torano, MD; Jeffrey Jordan, MD \n **Date:** May 19, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 59-year-old man is rushed to the emergency department (ED) after he experienced intense, sudden-onset pain, particularly on the right side of his flank and lumbar region. Initially, the patient had presented to his primary care physician with orthopnea, dyspnea on exertion, and an increase in peripheral edema over the past few weeks. Laboratory test results were within normal limits, with the exception of these elevated values:\nFasting glucose level: 127 mg/dL (reference range, 70-99 mg/dL)\nLeukocyte count: 11,520 cells/µL (reference range, 4000-11,000 cells/µL)\nLow-density lipoprotein cholesterol level: 126 mg/dL (reference range, < 100 mg/dL)\nTriglyceride level: 162 mg/dL (reference range, < 150 mg/dL)\nHe was referred to a cardiologist and had just completed an echocardiogram that morning as part of the workup before he collapsed in the hallway.\nThe patient has a past medical history of coronary artery disease, hypertension, and hyperlipidemia. He underwent emergent coronary angiography 5 years earlier and had two stents placed in the diagonal arteries. His current medications include metoprolol tartrate, atorvastatin, aspirin, and amlodipine. He states that he takes his medications and regularly follows up with his primary care physician.\nThe patient smoked cigarettes for more than 35 years, starting at age 18 years, but quit nearly 7 years ago. He does not drink alcohol or use illicit drugs.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A Patient Who Collapsed in Agony After Echocardiography"
},
{
"authors": "Catherine Divingian, MD, PhD; Valerie Gironda, MD; Francisco Torano, MD; Jeffrey Jordan, MD",
"content": [
"Upon initial presentation in the ED, the patient's heart rate is 56 beats/min, his blood pressure is 149/81 mm Hg, his respiration rate is 18 breaths/min, and his temperature is 98.5 °F (36.9 °C). His height is 67 in (170.2 cm), and his weight is 212 lb (96.2 kg). He is alert and oriented. His pupils are equal, round, and reactive to light. No erythema is noted in his mouth, and the mucous membranes appear moist. The patient can move all four extremities spontaneously. No rashes are visible; however, he appears pale and diaphoretic.",
"Lung fields are clear; no wheezing, rales, or rhonchi are audible. During auscultation of the heart, no murmurs, rubs, or gallops are noted. Radial pulses are equal and palpable. The patient has mild nonpitting bilateral lower extremity edema. His abdomen is soft and nontender to palpation. Bowel sounds are audible in all four quadrants. Costovertebral angle tenderness is noted on examination. The patient reports no tenderness on palpation of the lumbar region.",
"A stat one-view portable radiograph and an ECG are ordered. The only abnormal radiographic findings are slightly flattened diaphragmatic domes and large lung volumes. No cardiomegaly and no effusions or other signs of fluid overload are present.",
"The ECG demonstrates normal sinus rhythm at 62 beats/min. All intervals are within normal limits. No ischemic ST-segment changes are observed. Poor R-wave progression is noted; this finding suggests a previous anterior myocardial infarction. Evidence of left ventricular hypertrophy is present.",
"The results of repeated laboratory studies are within normal limits and reveal no elevations in troponin levels. His brain natriuretic peptide (BNP) level is 46 pg/mL (reference range, < 450 pg/mL). His leukocyte count is 10,105 cells/µL (reference range, 4000-11,000 cells/µL). His blood glucose level is 156 mg/dL (reference range, < 200 mg/dL [random measurement]), as he had not fasted.",
"The patient reports the complete resolution of his symptoms prior to the administration of diphenhydramine. He is given the medication and is observed in the ED for several hours before being sent home with strict follow-up instructions."
],
"date": "May 19, 2022",
"figures": [],
"markdown": "# A Patient Who Collapsed in Agony After Echocardiography\n\n **Authors:** Catherine Divingian, MD, PhD; Valerie Gironda, MD; Francisco Torano, MD; Jeffrey Jordan, MD \n **Date:** May 19, 2022\n\n ## Content\n\n Upon initial presentation in the ED, the patient's heart rate is 56 beats/min, his blood pressure is 149/81 mm Hg, his respiration rate is 18 breaths/min, and his temperature is 98.5 °F (36.9 °C). His height is 67 in (170.2 cm), and his weight is 212 lb (96.2 kg). He is alert and oriented. His pupils are equal, round, and reactive to light. No erythema is noted in his mouth, and the mucous membranes appear moist. The patient can move all four extremities spontaneously. No rashes are visible; however, he appears pale and diaphoretic.\nLung fields are clear; no wheezing, rales, or rhonchi are audible. During auscultation of the heart, no murmurs, rubs, or gallops are noted. Radial pulses are equal and palpable. The patient has mild nonpitting bilateral lower extremity edema. His abdomen is soft and nontender to palpation. Bowel sounds are audible in all four quadrants. Costovertebral angle tenderness is noted on examination. The patient reports no tenderness on palpation of the lumbar region.\nA stat one-view portable radiograph and an ECG are ordered. The only abnormal radiographic findings are slightly flattened diaphragmatic domes and large lung volumes. No cardiomegaly and no effusions or other signs of fluid overload are present.\nThe ECG demonstrates normal sinus rhythm at 62 beats/min. All intervals are within normal limits. No ischemic ST-segment changes are observed. Poor R-wave progression is noted; this finding suggests a previous anterior myocardial infarction. Evidence of left ventricular hypertrophy is present.\nThe results of repeated laboratory studies are within normal limits and reveal no elevations in troponin levels. His brain natriuretic peptide (BNP) level is 46 pg/mL (reference range, < 450 pg/mL). His leukocyte count is 10,105 cells/µL (reference range, 4000-11,000 cells/µL). His blood glucose level is 156 mg/dL (reference range, < 200 mg/dL [random measurement]), as he had not fasted.\nThe patient reports the complete resolution of his symptoms prior to the administration of diphenhydramine. He is given the medication and is observed in the ED for several hours before being sent home with strict follow-up instructions.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1688258,
"choiceText": "Chronic obstructive pulmonary disease exacerbation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688259,
"choiceText": "Diastolic heart failure exacerbation",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688260,
"choiceText": "Severe mitral valve regurgitation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688261,
"choiceText": "Pseudoallergic reaction",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688262,
"choiceText": "Sepsis secondary to upper respiratory tract infection",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 543957,
"questionText": "On the basis of these findings only, what is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Patient Who Collapsed in Agony After Echocardiography"
},
{
"authors": "Catherine Divingian, MD, PhD; Valerie Gironda, MD; Francisco Torano, MD; Jeffrey Jordan, MD",
"content": [
"The patient in this case did not exhibit the symptoms indicative of chronic obstructive pulmonary disease, such as an increase in shortness of breath, sputum production, and cough. Thus, this diagnosis is unlikely. Although his ECG shows evidence of left ventricular hypertrophy and he has a history of anterior myocardial infarction, the low BNP level and the lack of volume-overload status make heart failure less likely. Severe mitral valve regurgitation is unlikely, as auscultation revealed no murmurs. The patient's laboratory results and vital signs are not indicative of sepsis.",
"This patient is probably experiencing an acute pseudoallergic reaction to ultrasound contrast agent (UCA). Unlike \"true\" allergic reactions, immunoglobulin E is not involved; also, the pathophysiology of the response is different, requiring slightly different treatment. Pseudoallergic reactions can be brief and transient or longer lasting. Recognizing this response in a patient who presents with symptoms that may initially appear puzzling is important, as it is rare and may be unexpected.[1]",
"Echocardiographic technology has been improving over the past few decades. However, as many as 30% of all ultrasound studies are considered \"technically difficult,\" often because of obesity, lung disease, increased anterior-posterior dimensions, and the rapid heart rate associated with stress echocardiography or tachycardias. UCAs were developed to help overcome these limitations.[2,3]",
"This patient received a microsphere contrast agent, with a lipid coating around perflutren. Other UCAs may be composed of protein microspheres around perflutren. Perflutren is an octafluoropropane gas that vibrates when it encounters ultrasound waves and returns a resonant wave that improves the signal-to-noise ratio. Earlier forms of UCAs started with a sulfur hexafluoride core, which was chosen for its inert properties, surrounded by a phospholipid bubble.[1,2,3,4,5]",
"Since the 1980s, UCAs have been used to enhance imaging not only by providing a first set of harmonics in resonant waves, but also by adding a second set of harmonics. Local tissues do not resonate with the ultrasound waves, which assists with the visualization of structures. UCA microspheres are typically half the diameter of red blood cells (ranging from 1 to 7 microns in diameter) and can make an initial pass through the circulation with minimal degradation. This enables the microspheres to travel from peripheral injection sites to the heart intact, without signal diminution as they traverse the pulmonary vasculature."
],
"date": "May 19, 2022",
"figures": [],
"markdown": "# A Patient Who Collapsed in Agony After Echocardiography\n\n **Authors:** Catherine Divingian, MD, PhD; Valerie Gironda, MD; Francisco Torano, MD; Jeffrey Jordan, MD \n **Date:** May 19, 2022\n\n ## Content\n\n The patient in this case did not exhibit the symptoms indicative of chronic obstructive pulmonary disease, such as an increase in shortness of breath, sputum production, and cough. Thus, this diagnosis is unlikely. Although his ECG shows evidence of left ventricular hypertrophy and he has a history of anterior myocardial infarction, the low BNP level and the lack of volume-overload status make heart failure less likely. Severe mitral valve regurgitation is unlikely, as auscultation revealed no murmurs. The patient's laboratory results and vital signs are not indicative of sepsis.\nThis patient is probably experiencing an acute pseudoallergic reaction to ultrasound contrast agent (UCA). Unlike \"true\" allergic reactions, immunoglobulin E is not involved; also, the pathophysiology of the response is different, requiring slightly different treatment. Pseudoallergic reactions can be brief and transient or longer lasting. Recognizing this response in a patient who presents with symptoms that may initially appear puzzling is important, as it is rare and may be unexpected.[1]\nEchocardiographic technology has been improving over the past few decades. However, as many as 30% of all ultrasound studies are considered \"technically difficult,\" often because of obesity, lung disease, increased anterior-posterior dimensions, and the rapid heart rate associated with stress echocardiography or tachycardias. UCAs were developed to help overcome these limitations.[2,3]\nThis patient received a microsphere contrast agent, with a lipid coating around perflutren. Other UCAs may be composed of protein microspheres around perflutren. Perflutren is an octafluoropropane gas that vibrates when it encounters ultrasound waves and returns a resonant wave that improves the signal-to-noise ratio. Earlier forms of UCAs started with a sulfur hexafluoride core, which was chosen for its inert properties, surrounded by a phospholipid bubble.[1,2,3,4,5]\nSince the 1980s, UCAs have been used to enhance imaging not only by providing a first set of harmonics in resonant waves, but also by adding a second set of harmonics. Local tissues do not resonate with the ultrasound waves, which assists with the visualization of structures. UCA microspheres are typically half the diameter of red blood cells (ranging from 1 to 7 microns in diameter) and can make an initial pass through the circulation with minimal degradation. This enables the microspheres to travel from peripheral injection sites to the heart intact, without signal diminution as they traverse the pulmonary vasculature.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1688258,
"choiceText": "Chronic obstructive pulmonary disease exacerbation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688259,
"choiceText": "Diastolic heart failure exacerbation",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688260,
"choiceText": "Severe mitral valve regurgitation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688261,
"choiceText": "Pseudoallergic reaction",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688262,
"choiceText": "Sepsis secondary to upper respiratory tract infection",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 543957,
"questionText": "On the basis of these findings only, what is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Patient Who Collapsed in Agony After Echocardiography"
},
{
"authors": "Catherine Divingian, MD, PhD; Valerie Gironda, MD; Francisco Torano, MD; Jeffrey Jordan, MD",
"content": [
"UCAs enhance imaging in patients with poor echocardiographic studies, particularly if the left ventricles and apex need to be viewed. These agents are useful for visualization of the endocardium and measurement of the ejection fraction. Additionally, the small size of the microbubbles permits better image resolution compared with saline bubbles. For this reason, UCAs are often the preferred agents, particularly for delineating cardiac wall structures and detecting masses and thrombi, patent foramen ovale, and endocarditis. Visualization of abnormal wall motion is also improved.[1,3,4]",
"Off-label uses of UCAs have been noted. The gastrointestinal tract, liver, kidneys, spleen, urinary tract, and carotids have been visualized with these agents. Studies of endovascular repair describe the use of UCAs to detect leaks. Documentation has been developed to help clinicians best utilize these agents for alternative applications.[1,5]",
"In 2007, the risk for adverse cardiac, pulmonary, and allergic reactions to UCAs was first recognized. Most formulations are contraindicated in patients with bidirectional or right-to-left intracardiac shunts, as central nervous system or microvascular occlusions may occur, although they are rare. UCAs should be avoided in patients with acute respiratory distress syndrome or severe pulmonary hypertension. They are also not recommended for patients with hypertensive emergency or urgency. Additional contraindications include New York Heart Association class III or IV heart failure, acute endocarditis, prosthetic valves, and uncontrolled systolic blood pressure.[1,2,3,5]",
"Hypersensitivity reactions have also been reported; they typically result from a complement activation–related pseudoallergy (CARPA). Allergy and anaphylactoid events are rare but significant. Symptoms can include pruritus, urticaria, shortness of breath, wheezing, angioedema, headaches, nausea, hypotension, and ST-segment elevations secondary to myocardial infarction or coronary artery vasospasm.[1,2,5] These responses are thought to be mediated by mast cells and basophils, which release inflammatory markers; histamines and cytokines are most commonly cited in the literature.[3,5] The patient does not need to be presensitized to the agent to develop these reactions.[3] Additionally, allergies to polyethylene glycol can predispose patients to allergic reactions to some UCAs and are a contraindication to their use.[6]",
"Deaths have also occurred after the administration of UCAs; however, they were not directly ascribed to the use of contrast agents. Deaths attributed to UCAs remain much lower (4 per 10,000 patients) than those associated with coronary angiography (1 per 100 patients).[5] The US Food and Drug Administration required hazard warnings on the labels of UCAs, which have subsequently been revised as further research has been conducted.[1,2,3]",
"The safety of UCAs has not been studied in children. Similarly, data on pregnant women are sparse. For these reasons, contrast agents should generally be avoided in these populations whenever possible.[2,5]",
"The speed of administration may make a difference in the development of some reactions. Bolus administration has been found to result in worse pathophysiologic responses compared with slow infusion of solution, particularly if it has been diluted with water.[2]"
],
"date": "May 19, 2022",
"figures": [],
"markdown": "# A Patient Who Collapsed in Agony After Echocardiography\n\n **Authors:** Catherine Divingian, MD, PhD; Valerie Gironda, MD; Francisco Torano, MD; Jeffrey Jordan, MD \n **Date:** May 19, 2022\n\n ## Content\n\n UCAs enhance imaging in patients with poor echocardiographic studies, particularly if the left ventricles and apex need to be viewed. These agents are useful for visualization of the endocardium and measurement of the ejection fraction. Additionally, the small size of the microbubbles permits better image resolution compared with saline bubbles. For this reason, UCAs are often the preferred agents, particularly for delineating cardiac wall structures and detecting masses and thrombi, patent foramen ovale, and endocarditis. Visualization of abnormal wall motion is also improved.[1,3,4]\nOff-label uses of UCAs have been noted. The gastrointestinal tract, liver, kidneys, spleen, urinary tract, and carotids have been visualized with these agents. Studies of endovascular repair describe the use of UCAs to detect leaks. Documentation has been developed to help clinicians best utilize these agents for alternative applications.[1,5]\nIn 2007, the risk for adverse cardiac, pulmonary, and allergic reactions to UCAs was first recognized. Most formulations are contraindicated in patients with bidirectional or right-to-left intracardiac shunts, as central nervous system or microvascular occlusions may occur, although they are rare. UCAs should be avoided in patients with acute respiratory distress syndrome or severe pulmonary hypertension. They are also not recommended for patients with hypertensive emergency or urgency. Additional contraindications include New York Heart Association class III or IV heart failure, acute endocarditis, prosthetic valves, and uncontrolled systolic blood pressure.[1,2,3,5]\nHypersensitivity reactions have also been reported; they typically result from a complement activation–related pseudoallergy (CARPA). Allergy and anaphylactoid events are rare but significant. Symptoms can include pruritus, urticaria, shortness of breath, wheezing, angioedema, headaches, nausea, hypotension, and ST-segment elevations secondary to myocardial infarction or coronary artery vasospasm.[1,2,5] These responses are thought to be mediated by mast cells and basophils, which release inflammatory markers; histamines and cytokines are most commonly cited in the literature.[3,5] The patient does not need to be presensitized to the agent to develop these reactions.[3] Additionally, allergies to polyethylene glycol can predispose patients to allergic reactions to some UCAs and are a contraindication to their use.[6]\nDeaths have also occurred after the administration of UCAs; however, they were not directly ascribed to the use of contrast agents. Deaths attributed to UCAs remain much lower (4 per 10,000 patients) than those associated with coronary angiography (1 per 100 patients).[5] The US Food and Drug Administration required hazard warnings on the labels of UCAs, which have subsequently been revised as further research has been conducted.[1,2,3]\nThe safety of UCAs has not been studied in children. Similarly, data on pregnant women are sparse. For these reasons, contrast agents should generally be avoided in these populations whenever possible.[2,5]\nThe speed of administration may make a difference in the development of some reactions. Bolus administration has been found to result in worse pathophysiologic responses compared with slow infusion of solution, particularly if it has been diluted with water.[2]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A Patient Who Collapsed in Agony After Echocardiography"
},
{
"authors": "Catherine Divingian, MD, PhD; Valerie Gironda, MD; Francisco Torano, MD; Jeffrey Jordan, MD",
"content": [
"The patient in this case received a UCA for his echocardiographic study and exhibited an allergic reaction. The pain in the right flank and back has been described in the literature, particularly with agents that use the same microsphere and perflutren core as in this case. The flank pain, in particular, is possibly secondary to trapping of the microspheres in the kidneys due to complement adhesion.[2]",
"As in this case, many adverse reactions to UCAs are transient.[1,2] This patient was given diphenhydramine, but the symptoms had started to resolve prior to the administration of the medication. For those who experience more serious allergic or anaphylactoid responses, epinephrine may be required as part of the emergency treatment protocol. It is injected into the anterior thigh. Beta2 blockers have been used to control symptoms as well.[3] Monitoring the patient for up to 30 minutes after the administration of a UCA is also recommended as a safety precaution.[5]",
"Although pathophysiologic responses do occur with UCAs, the risks of missing a diagnosis by not using contrast for ultrasound studies should be considered, as should the benefits of finding a structural abnormality. Nevertheless, the risk for a reaction must be kept in mind depending on the history and presenting symptoms. In emergency situations, the risk of a possible adverse response may be worth taking, given the statistical improbability. However, the probability of a poor outcome is significantly increased in larger facilities that perform more of these specialized studies.[1,2] Patients need to be informed of the possible complications when their consent is obtained, and shared decision-making is critical."
],
"date": "May 19, 2022",
"figures": [],
"markdown": "# A Patient Who Collapsed in Agony After Echocardiography\n\n **Authors:** Catherine Divingian, MD, PhD; Valerie Gironda, MD; Francisco Torano, MD; Jeffrey Jordan, MD \n **Date:** May 19, 2022\n\n ## Content\n\n The patient in this case received a UCA for his echocardiographic study and exhibited an allergic reaction. The pain in the right flank and back has been described in the literature, particularly with agents that use the same microsphere and perflutren core as in this case. The flank pain, in particular, is possibly secondary to trapping of the microspheres in the kidneys due to complement adhesion.[2]\nAs in this case, many adverse reactions to UCAs are transient.[1,2] This patient was given diphenhydramine, but the symptoms had started to resolve prior to the administration of the medication. For those who experience more serious allergic or anaphylactoid responses, epinephrine may be required as part of the emergency treatment protocol. It is injected into the anterior thigh. Beta2 blockers have been used to control symptoms as well.[3] Monitoring the patient for up to 30 minutes after the administration of a UCA is also recommended as a safety precaution.[5]\nAlthough pathophysiologic responses do occur with UCAs, the risks of missing a diagnosis by not using contrast for ultrasound studies should be considered, as should the benefits of finding a structural abnormality. Nevertheless, the risk for a reaction must be kept in mind depending on the history and presenting symptoms. In emergency situations, the risk of a possible adverse response may be worth taking, given the statistical improbability. However, the probability of a poor outcome is significantly increased in larger facilities that perform more of these specialized studies.[1,2] Patients need to be informed of the possible complications when their consent is obtained, and shared decision-making is critical.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1688263,
"choiceText": "A 28-year-old patient who is pregnant and presents with preeclampsia in the 32nd week of gestation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688264,
"choiceText": "A 42-year-old man with a suspected new-onset right-to-left ventricular shunt as a complication of a myocardial infarction",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688265,
"choiceText": "A 64-year-old woman who presents with bilateral pedal edema, bilateral pleural effusions, and elevated jugular venous distention pressure and whose initial echocardiogram was of poor quality",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688266,
"choiceText": "A 16-year-old boy with a family history of hypertrophic cardiomyopathy who had a syncopal episode on the basketball court",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "UCAs are not recommended for pregnant women, as safety data are lacking. Patients with bidirectional or right-to-left ventricular shunts should not receive these agents because of the possible occurrence of occlusions. Pediatric patients should not be given UCAs as they have not been studied in this population.<br><br>\r\nFor the woman with a poorly visualized echocardiogram, a better view of the left ventricle is required because she probably has cardiomyopathy. Moreover, she does not have any contraindications to the use of UCAs.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 543958,
"questionText": "For which of these patients is the use of UCAs best indicated?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1688267,
"choiceText": "A beta<sub>2</sub> blocker",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688268,
"choiceText": "Epinephrine 1:1000",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688269,
"choiceText": "Diphenhydramine",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688270,
"choiceText": "All of the above",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Research has shown that beta2 blockers, epinephrine 1:1000, and diphenhydramine are appropriate treatments for anaphylactoid reactions to UCAs. Epinephrine, in particular, is best used in a patient who has a serious anaphylactoid reaction.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 543959,
"questionText": "What treatment that can be provided in the ED is recommended for anaphylactoid reactions to UCAs?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Patient Who Collapsed in Agony After Echocardiography"
},
{
"authors": "Catherine Divingian, MD, PhD; Valerie Gironda, MD; Francisco Torano, MD; Jeffrey Jordan, MD",
"content": [
"Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult."
],
"date": "May 19, 2022",
"figures": [],
"markdown": "# A Patient Who Collapsed in Agony After Echocardiography\n\n **Authors:** Catherine Divingian, MD, PhD; Valerie Gironda, MD; Francisco Torano, MD; Jeffrey Jordan, MD \n **Date:** May 19, 2022\n\n ## Content\n\n Interested in following real cases from colleagues around the world? Have a challenging case you'd like to discuss with peers? Check out Medscape Consult.\n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1688263,
"choiceText": "A 28-year-old patient who is pregnant and presents with preeclampsia in the 32nd week of gestation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688264,
"choiceText": "A 42-year-old man with a suspected new-onset right-to-left ventricular shunt as a complication of a myocardial infarction",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688265,
"choiceText": "A 64-year-old woman who presents with bilateral pedal edema, bilateral pleural effusions, and elevated jugular venous distention pressure and whose initial echocardiogram was of poor quality",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688266,
"choiceText": "A 16-year-old boy with a family history of hypertrophic cardiomyopathy who had a syncopal episode on the basketball court",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "UCAs are not recommended for pregnant women, as safety data are lacking. Patients with bidirectional or right-to-left ventricular shunts should not receive these agents because of the possible occurrence of occlusions. Pediatric patients should not be given UCAs as they have not been studied in this population.<br><br>\r\nFor the woman with a poorly visualized echocardiogram, a better view of the left ventricle is required because she probably has cardiomyopathy. Moreover, she does not have any contraindications to the use of UCAs.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 543958,
"questionText": "For which of these patients is the use of UCAs best indicated?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1688267,
"choiceText": "A beta<sub>2</sub> blocker",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688268,
"choiceText": "Epinephrine 1:1000",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688269,
"choiceText": "Diphenhydramine",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688270,
"choiceText": "All of the above",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Research has shown that beta2 blockers, epinephrine 1:1000, and diphenhydramine are appropriate treatments for anaphylactoid reactions to UCAs. Epinephrine, in particular, is best used in a patient who has a serious anaphylactoid reaction.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 543959,
"questionText": "What treatment that can be provided in the ED is recommended for anaphylactoid reactions to UCAs?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Patient Who Collapsed in Agony After Echocardiography"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1688258,
"choiceText": "Chronic obstructive pulmonary disease exacerbation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688259,
"choiceText": "Diastolic heart failure exacerbation",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688260,
"choiceText": "Severe mitral valve regurgitation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688261,
"choiceText": "Pseudoallergic reaction",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688262,
"choiceText": "Sepsis secondary to upper respiratory tract infection",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 543957,
"questionText": "On the basis of these findings only, what is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1688263,
"choiceText": "A 28-year-old patient who is pregnant and presents with preeclampsia in the 32nd week of gestation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688264,
"choiceText": "A 42-year-old man with a suspected new-onset right-to-left ventricular shunt as a complication of a myocardial infarction",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688265,
"choiceText": "A 64-year-old woman who presents with bilateral pedal edema, bilateral pleural effusions, and elevated jugular venous distention pressure and whose initial echocardiogram was of poor quality",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688266,
"choiceText": "A 16-year-old boy with a family history of hypertrophic cardiomyopathy who had a syncopal episode on the basketball court",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "UCAs are not recommended for pregnant women, as safety data are lacking. Patients with bidirectional or right-to-left ventricular shunts should not receive these agents because of the possible occurrence of occlusions. Pediatric patients should not be given UCAs as they have not been studied in this population.<br><br>\r\nFor the woman with a poorly visualized echocardiogram, a better view of the left ventricle is required because she probably has cardiomyopathy. Moreover, she does not have any contraindications to the use of UCAs.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 543958,
"questionText": "For which of these patients is the use of UCAs best indicated?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1688267,
"choiceText": "A beta<sub>2</sub> blocker",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688268,
"choiceText": "Epinephrine 1:1000",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688269,
"choiceText": "Diphenhydramine",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1688270,
"choiceText": "All of the above",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Research has shown that beta2 blockers, epinephrine 1:1000, and diphenhydramine are appropriate treatments for anaphylactoid reactions to UCAs. Epinephrine, in particular, is best used in a patient who has a serious anaphylactoid reaction.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 543959,
"questionText": "What treatment that can be provided in the ED is recommended for anaphylactoid reactions to UCAs?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
720150 | /viewarticle/720150 | [
{
"authors": "Vanya Grover, DO; Solmaz Amirnazmi, MD; Robert Graham, MD, MPH",
"content": [
"Editor's Note:\n\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.",
"A 61-year-old woman with a medical history of insulin-dependent diabetes mellitus for 7 years, hypertension, hyperlipidemia, and one previous episode of idiopathic pancreatitis presents with worsening abdominal pain that has lasted for the past month. The pain is intermittent and localized to the epigastric region. It is nonradiating and not associated with food intake.",
"No nausea, vomiting, diarrhea, constipation, vaginal discharge or bleeding, fever, coughing, or urinary symptoms are reported. She denies having any chest pain or shortness of breath. She is not a smoker. She states that has abstained from any alcohol use for as long as she can remember. She cannot identify any exacerbating or relieving factors for her pain.",
"Her previous medical history includes a total abdominal hysterectomy with bilateral salpingo-oophorectomy performed 30 years ago. The family history is significant for pancreatic cancer in her mother, the details of which are unknown to the patient. Her medications include insulin, lisinopril, and simvastatin. Her diabetes control has been poor, and a recent hemoglobin A1c value was 10%."
],
"date": "May 05, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: A Woman Who Abstains from Alcohol Has Worsening Abdominal Pain\n\n **Authors:** Vanya Grover, DO; Solmaz Amirnazmi, MD; Robert Graham, MD, MPH \n **Date:** May 05, 2022\n\n ## Content\n\n Editor's Note:\n\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.\nA 61-year-old woman with a medical history of insulin-dependent diabetes mellitus for 7 years, hypertension, hyperlipidemia, and one previous episode of idiopathic pancreatitis presents with worsening abdominal pain that has lasted for the past month. The pain is intermittent and localized to the epigastric region. It is nonradiating and not associated with food intake.\nNo nausea, vomiting, diarrhea, constipation, vaginal discharge or bleeding, fever, coughing, or urinary symptoms are reported. She denies having any chest pain or shortness of breath. She is not a smoker. She states that has abstained from any alcohol use for as long as she can remember. She cannot identify any exacerbating or relieving factors for her pain.\nHer previous medical history includes a total abdominal hysterectomy with bilateral salpingo-oophorectomy performed 30 years ago. The family history is significant for pancreatic cancer in her mother, the details of which are unknown to the patient. Her medications include insulin, lisinopril, and simvastatin. Her diabetes control has been poor, and a recent hemoglobin A1c value was 10%.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Gastro Case Challenge: A Woman Who Abstains from Alcohol Has Worsening Abdominal Pain"
},
{
"authors": "Vanya Grover, DO; Solmaz Amirnazmi, MD; Robert Graham, MD, MPH",
"content": [
"Upon presentation, she has a pulse of 77 beats/min, blood pressure of 159/78 mm Hg, and temperature of 97.9° F (36.6° C). The physical examination reveals a comfortable-appearing woman in no acute distress. The head and neck examination findings are normal, and no scleral icterus is noted. She does not appear dehydrated.",
"Her lung sounds are clear bilaterally. The S1 and S2 heart sounds are normal, with no audible murmurs, rubs, or gallops. The patient has a soft abdomen, with bowel sounds heard in all 4 quadrants. Tenderness to deep palpation of the epigastrium is observed. The patient does not demonstrate guarding, and no Murphy sign or McBurney point tenderness is noted. A rectal examination reveals brown, guaiac-negative stool. No neurologic deficits are noted.",
"Laboratory studies include normal findings for serum amylase, lipase, alkaline phosphatase, aspartate transaminase (AST), alanine transaminase (ALT), bilirubin, albumin, serum chemistries, and renal function tests, as well as a normal complete blood count (CBC). Radiography of the chest is performed and is unremarkable. She has a normal electrocardiogram (ECG) that does not show evidence of ischemic disease.",
"CT scanning of the abdomen and pelvis with oral and intravenous contrast is performed. Magnetic resonance cholangiopancreatography (MRCP) is performed (see Figures 1-4).",
"Figure 1.",
"Figure 1.",
"Figure 2.",
"Figure 2.",
"Figure 3.",
"Figure 3.",
"Figure 4.",
"Figure 4."
],
"date": "May 05, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/720/150/720150-thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/720/150/720150-thumb2.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/720/150/720150-thumb3.png"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/720/150/720150-thumb4.png"
}
],
"markdown": "# Gastro Case Challenge: A Woman Who Abstains from Alcohol Has Worsening Abdominal Pain\n\n **Authors:** Vanya Grover, DO; Solmaz Amirnazmi, MD; Robert Graham, MD, MPH \n **Date:** May 05, 2022\n\n ## Content\n\n Upon presentation, she has a pulse of 77 beats/min, blood pressure of 159/78 mm Hg, and temperature of 97.9° F (36.6° C). The physical examination reveals a comfortable-appearing woman in no acute distress. The head and neck examination findings are normal, and no scleral icterus is noted. She does not appear dehydrated.\nHer lung sounds are clear bilaterally. The S1 and S2 heart sounds are normal, with no audible murmurs, rubs, or gallops. The patient has a soft abdomen, with bowel sounds heard in all 4 quadrants. Tenderness to deep palpation of the epigastrium is observed. The patient does not demonstrate guarding, and no Murphy sign or McBurney point tenderness is noted. A rectal examination reveals brown, guaiac-negative stool. No neurologic deficits are noted.\nLaboratory studies include normal findings for serum amylase, lipase, alkaline phosphatase, aspartate transaminase (AST), alanine transaminase (ALT), bilirubin, albumin, serum chemistries, and renal function tests, as well as a normal complete blood count (CBC). Radiography of the chest is performed and is unremarkable. She has a normal electrocardiogram (ECG) that does not show evidence of ischemic disease.\nCT scanning of the abdomen and pelvis with oral and intravenous contrast is performed. Magnetic resonance cholangiopancreatography (MRCP) is performed (see Figures 1-4).\nFigure 1.\nFigure 1.\nFigure 2.\nFigure 2.\nFigure 3.\nFigure 3.\nFigure 4.\nFigure 4.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 337574,
"choiceText": "Fatty infiltration of the pancreas",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337575,
"choiceText": "Dorsal agenesis of the pancreas",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337576,
"choiceText": "Pancreas divisum",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337577,
"choiceText": " Autogenesis of the pancreas",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 94894,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: A Woman Who Abstains from Alcohol Has Worsening Abdominal Pain"
},
{
"authors": "Vanya Grover, DO; Solmaz Amirnazmi, MD; Robert Graham, MD, MPH",
"content": [
"The diagnosis of dorsal agenesis of the pancreas was made based on the imaging studies performed to evaluate the patient's abdominal pain. CT scanning demonstrated the pancreatic head, with absence of the pancreatic neck, body, and tail ventral to the splenic vein (see Figures 1 and 2). These results were followed up with MRCP, which confirmed the absence of the body and tail of the pancreas as well as the dorsal ductal system, accessory duct, and minor papilla (see Figures 3 and 4).",
"Figure 1.",
"Figure 1.",
"Figure 2.",
"Figure 2.",
"Figure 3.",
"Figure 3.",
"Figure 4.",
"Figure 4.",
"The human pancreas forms from the foregut endoderm as dorsal and ventral buds during embryogenesis. Failure of the dorsal pancreatic bud to develop can potentially result in agenesis of the dorsal pancreas, an extremely rare congenital anomaly.[1] The dorsal bud forms the upper part of the head, body, and tail of the pancreas. These drain through the duct of Santorini into the minor papilla. The ventral bud forms the major part of the head and uncinate process that drains through the duct of Wirsung into the major papilla.[1] The main pancreatic duct drains through both the major and minor papilla (see Figure 5). Agenesis of the dorsal pancreatic duct can result in a complete or partial anomaly.",
"Figure 5.",
"Figure 5.",
"Complete agenesis of the dorsal pancreas has rarely been described in the medical literature. The diagnosis is usually made when a patient with abdominal pain undergoes diagnostic radiologic testing. Dorsal agenesis of the pancreas is suggested when the body and tail of the pancreas are not visualized ventral to the splenic vein. This may be seen on abdominal ultrasonography or CT scanning.[1] The diagnosis should be confirmed by MRCP or endoscopic retrograde cholangiopancreatography (ERCP) to demonstrate absence of the pancreatic dorsal duct system.[2] During either MRCP or ERCP, the diagnostic triad is required to confirm the diagnosis. This triad includes absence of the dorsal ductal system, the accessory duct or duct of Santorini, and the minor papilla.[2,3]",
"MRCP or CT scanning best demonstrate the absence of the body and tail of the pancreas.[3] ERCP is a more operator-dependent procedure and it may be difficult to visualize the pancreatic and biliary trees, especially with cannulation of the minor papilla.[2] In contrast, with MRCP one can clearly see the pancreaticobiliary system and make the diagnosis without need for an invasive procedure or the risks of radiation.[4] The limitations of MRCP include the inability to perform an intervention if necessary."
],
"date": "May 05, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/720/150/720150-thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/720/150/720150-thumb2.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/720/150/720150-thumb3.png"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/720/150/720150-thumb4.png"
},
{
"caption": "Figure 5.",
"image_url": "https://img.medscapestatic.com/article/720/150/720150-thumb5.png"
}
],
"markdown": "# Gastro Case Challenge: A Woman Who Abstains from Alcohol Has Worsening Abdominal Pain\n\n **Authors:** Vanya Grover, DO; Solmaz Amirnazmi, MD; Robert Graham, MD, MPH \n **Date:** May 05, 2022\n\n ## Content\n\n The diagnosis of dorsal agenesis of the pancreas was made based on the imaging studies performed to evaluate the patient's abdominal pain. CT scanning demonstrated the pancreatic head, with absence of the pancreatic neck, body, and tail ventral to the splenic vein (see Figures 1 and 2). These results were followed up with MRCP, which confirmed the absence of the body and tail of the pancreas as well as the dorsal ductal system, accessory duct, and minor papilla (see Figures 3 and 4).\nFigure 1.\nFigure 1.\nFigure 2.\nFigure 2.\nFigure 3.\nFigure 3.\nFigure 4.\nFigure 4.\nThe human pancreas forms from the foregut endoderm as dorsal and ventral buds during embryogenesis. Failure of the dorsal pancreatic bud to develop can potentially result in agenesis of the dorsal pancreas, an extremely rare congenital anomaly.[1] The dorsal bud forms the upper part of the head, body, and tail of the pancreas. These drain through the duct of Santorini into the minor papilla. The ventral bud forms the major part of the head and uncinate process that drains through the duct of Wirsung into the major papilla.[1] The main pancreatic duct drains through both the major and minor papilla (see Figure 5). Agenesis of the dorsal pancreatic duct can result in a complete or partial anomaly.\nFigure 5.\nFigure 5.\nComplete agenesis of the dorsal pancreas has rarely been described in the medical literature. The diagnosis is usually made when a patient with abdominal pain undergoes diagnostic radiologic testing. Dorsal agenesis of the pancreas is suggested when the body and tail of the pancreas are not visualized ventral to the splenic vein. This may be seen on abdominal ultrasonography or CT scanning.[1] The diagnosis should be confirmed by MRCP or endoscopic retrograde cholangiopancreatography (ERCP) to demonstrate absence of the pancreatic dorsal duct system.[2] During either MRCP or ERCP, the diagnostic triad is required to confirm the diagnosis. This triad includes absence of the dorsal ductal system, the accessory duct or duct of Santorini, and the minor papilla.[2,3]\nMRCP or CT scanning best demonstrate the absence of the body and tail of the pancreas.[3] ERCP is a more operator-dependent procedure and it may be difficult to visualize the pancreatic and biliary trees, especially with cannulation of the minor papilla.[2] In contrast, with MRCP one can clearly see the pancreaticobiliary system and make the diagnosis without need for an invasive procedure or the risks of radiation.[4] The limitations of MRCP include the inability to perform an intervention if necessary.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4.** \n \n\n**Figure 5.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 337574,
"choiceText": "Fatty infiltration of the pancreas",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337575,
"choiceText": "Dorsal agenesis of the pancreas",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337576,
"choiceText": "Pancreas divisum",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337577,
"choiceText": " Autogenesis of the pancreas",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 94894,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: A Woman Who Abstains from Alcohol Has Worsening Abdominal Pain"
},
{
"authors": "Vanya Grover, DO; Solmaz Amirnazmi, MD; Robert Graham, MD, MPH",
"content": [
"Clinically, these patients can present with recurrent pancreatitis, jaundice, and/or a medical history of diabetes mellitus. However, most patients remain asymptomatic.[1] Diabetes mellitus presents because most of the B cells of the islets of Langerhans are located in the pancreatic body and tail. The association of dorsal agenesis of the pancreas and pancreatitis is less well-defined.",
"A few theories behind the etiology of this process have been proposed. Sphincter of Oddi dysfunction may play a role. Alternatively, compensatory hypersecretion results in hypertrophy of the remnant ventral gland and higher intrapancreatic duct pressure.[5] Carcinoma risk does not appear to be elevated in these patients. The most common cancers associated with this condition appear to be solid intraductal mucinous papillary and solid pseudopapillary tumors, as well as adenocarcinomas.[5] Laboratory findings, such as amylase or lipase in the serum, tend to be within normal limits. Abdominal pain associated with this condition is generally attributed to pancreatitis, duodenal obstruction, sphincter of Oddi dysfunction, or autonomic neuropathy.[5]",
"The diagnostic differential of dorsal agenesis of the pancreas includes fat replacement of the pancreas, pancreatic divisum, atrophy of the pancreas secondary to chronic pancreatitis, congenital short pancreas, or partial agenesis.[2,4] All of these conditions must be ruled out before making the diagnosis of dorsal agenesis of the pancreas.",
"Pancreatic divisum occurs due to failure of the ventral and dorsal ducts to fuse during embryogenesis; therefore, the pancreatic body and tail continue to drain into the minor papilla and the head into the major papilla instead of one joint pancreatic duct. These patients tend to be asymptomatic but may have recurrences of pancreatitis, likely secondary to a narrow minor papilla.[2] In patients who have fat replacement, the pancreatic ducts are still present and the entire gland is visible on imaging studies. These patients may ultimately have decreased pancreatic function. The causes of fat replacement of the pancreas include obesity, diabetes mellitus, chronic pancreatitis, hepatic disease, dietary deficiency, viral infection, steroid therapy, obstruction of the pancreatic duct, and fibrocystic disease.[6]",
"Generally, CT scanning has been the most useful method in diagnosing this condition. Fat replacement of the pancreas can be reversible in cases secondary to obesity.[6] Patients with atrophy of the body and tail of the pancreas can present similarly to patients with dorsal agenesis of the pancreas; such cases are referred to as pseudoagenesis.[2] Therefore, the ductal system must be visualized. These patients often present with a history of recurrent pancreatitis. Neoplasm must also always be considered and ruled out."
],
"date": "May 05, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: A Woman Who Abstains from Alcohol Has Worsening Abdominal Pain\n\n **Authors:** Vanya Grover, DO; Solmaz Amirnazmi, MD; Robert Graham, MD, MPH \n **Date:** May 05, 2022\n\n ## Content\n\n Clinically, these patients can present with recurrent pancreatitis, jaundice, and/or a medical history of diabetes mellitus. However, most patients remain asymptomatic.[1] Diabetes mellitus presents because most of the B cells of the islets of Langerhans are located in the pancreatic body and tail. The association of dorsal agenesis of the pancreas and pancreatitis is less well-defined.\nA few theories behind the etiology of this process have been proposed. Sphincter of Oddi dysfunction may play a role. Alternatively, compensatory hypersecretion results in hypertrophy of the remnant ventral gland and higher intrapancreatic duct pressure.[5] Carcinoma risk does not appear to be elevated in these patients. The most common cancers associated with this condition appear to be solid intraductal mucinous papillary and solid pseudopapillary tumors, as well as adenocarcinomas.[5] Laboratory findings, such as amylase or lipase in the serum, tend to be within normal limits. Abdominal pain associated with this condition is generally attributed to pancreatitis, duodenal obstruction, sphincter of Oddi dysfunction, or autonomic neuropathy.[5]\nThe diagnostic differential of dorsal agenesis of the pancreas includes fat replacement of the pancreas, pancreatic divisum, atrophy of the pancreas secondary to chronic pancreatitis, congenital short pancreas, or partial agenesis.[2,4] All of these conditions must be ruled out before making the diagnosis of dorsal agenesis of the pancreas.\nPancreatic divisum occurs due to failure of the ventral and dorsal ducts to fuse during embryogenesis; therefore, the pancreatic body and tail continue to drain into the minor papilla and the head into the major papilla instead of one joint pancreatic duct. These patients tend to be asymptomatic but may have recurrences of pancreatitis, likely secondary to a narrow minor papilla.[2] In patients who have fat replacement, the pancreatic ducts are still present and the entire gland is visible on imaging studies. These patients may ultimately have decreased pancreatic function. The causes of fat replacement of the pancreas include obesity, diabetes mellitus, chronic pancreatitis, hepatic disease, dietary deficiency, viral infection, steroid therapy, obstruction of the pancreatic duct, and fibrocystic disease.[6]\nGenerally, CT scanning has been the most useful method in diagnosing this condition. Fat replacement of the pancreas can be reversible in cases secondary to obesity.[6] Patients with atrophy of the body and tail of the pancreas can present similarly to patients with dorsal agenesis of the pancreas; such cases are referred to as pseudoagenesis.[2] Therefore, the ductal system must be visualized. These patients often present with a history of recurrent pancreatitis. Neoplasm must also always be considered and ruled out.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Gastro Case Challenge: A Woman Who Abstains from Alcohol Has Worsening Abdominal Pain"
},
{
"authors": "Vanya Grover, DO; Solmaz Amirnazmi, MD; Robert Graham, MD, MPH",
"content": [
"The treatment of patients diagnosed with dorsal agenesis of the pancreas may include insulin administration or exogenous replacement with pancreatic enzymes. The abdominal pain is often attributed to pancreatitis, duodenal obstruction, sphincter of Oddi dysfunction, or autonomic neuropathy. Although a rare diagnosis in adults, dorsal agenesis of the pancreas should be included in the differential diagnosis of diabetic patients with pancreatitis or abdominal pain, or when the body and tail of the pancreas are not visualized on imaging.",
"The patient in this case was admitted to the hospital to rule out pancreatitis. She was hospitalized for 2 days, during which she received intravenous hydration and morphine for abdominal pain, as well as her regular medications. The patient's abdominal pain subsided the following day, and she was discharged with a diagnosis of autonomic neuropathy pain related to her poorly controlled diabetes. She was discharged with outpatient follow-up."
],
"date": "May 05, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: A Woman Who Abstains from Alcohol Has Worsening Abdominal Pain\n\n **Authors:** Vanya Grover, DO; Solmaz Amirnazmi, MD; Robert Graham, MD, MPH \n **Date:** May 05, 2022\n\n ## Content\n\n The treatment of patients diagnosed with dorsal agenesis of the pancreas may include insulin administration or exogenous replacement with pancreatic enzymes. The abdominal pain is often attributed to pancreatitis, duodenal obstruction, sphincter of Oddi dysfunction, or autonomic neuropathy. Although a rare diagnosis in adults, dorsal agenesis of the pancreas should be included in the differential diagnosis of diabetic patients with pancreatitis or abdominal pain, or when the body and tail of the pancreas are not visualized on imaging.\nThe patient in this case was admitted to the hospital to rule out pancreatitis. She was hospitalized for 2 days, during which she received intravenous hydration and morphine for abdominal pain, as well as her regular medications. The patient's abdominal pain subsided the following day, and she was discharged with a diagnosis of autonomic neuropathy pain related to her poorly controlled diabetes. She was discharged with outpatient follow-up.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 337590,
"choiceText": "Abdominal ultrasonography",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337591,
"choiceText": "MRCP or ERCP",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337592,
"choiceText": "Abdominal radiography",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337593,
"choiceText": "Colonoscopy",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "In the setting of abdominal pain, the best modality for evaluating pancreatic disease is CT scanning or MRI of the abdomen. When the pancreatic anatomy is altered, the next best imaging modality for evaluation is an ERCP or MRCP to visualize the pancreatic tree. MRCP has certain advantages over ERCP; primarily it is a noninvasive means of evaluating the biliary and pancreatic systems in their natural state. In addition, it is an imaging modality that is not operator-dependent; however, it does not allow for therapeutic intervention if such intervention is necessary.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 94898,
"questionText": "A patient with abdominal pain undergoes a CT scan. Her pancreas does not have a body or tail. Which imaging modalities or interventions is indicated?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 337594,
"choiceText": "Exogenous replacement of pancreatic enzymes",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337595,
"choiceText": "Pancreas transplant",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337596,
"choiceText": "Hemodialysis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337597,
"choiceText": "Surgical consultation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Treatment of dorsal agenesis of the pancreas is generally supportive and may include insulin administration or exogenous replacement with pancreatic enzymes. The abdominal pain is often attributed to pancreatitis, duodenal obstruction, sphincter of Oddi dysfunction, or autonomic neuropathy. Although a rare diagnosis in adults, dorsal agenesis of the pancreas should be included in the differential diagnosis of diabetic patients with pancreatitis or abdominal pain, or when body and tail of the pancreas are not visualized on imaging.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 94899,
"questionText": "Which is indicated for a patient with vague abdominal pain with dorsal agenesis of the pancreas?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: A Woman Who Abstains from Alcohol Has Worsening Abdominal Pain"
},
{
"authors": "Vanya Grover, DO; Solmaz Amirnazmi, MD; Robert Graham, MD, MPH",
"content": [],
"date": "May 05, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: A Woman Who Abstains from Alcohol Has Worsening Abdominal Pain\n\n **Authors:** Vanya Grover, DO; Solmaz Amirnazmi, MD; Robert Graham, MD, MPH \n **Date:** May 05, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 337590,
"choiceText": "Abdominal ultrasonography",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337591,
"choiceText": "MRCP or ERCP",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337592,
"choiceText": "Abdominal radiography",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337593,
"choiceText": "Colonoscopy",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "In the setting of abdominal pain, the best modality for evaluating pancreatic disease is CT scanning or MRI of the abdomen. When the pancreatic anatomy is altered, the next best imaging modality for evaluation is an ERCP or MRCP to visualize the pancreatic tree. MRCP has certain advantages over ERCP; primarily it is a noninvasive means of evaluating the biliary and pancreatic systems in their natural state. In addition, it is an imaging modality that is not operator-dependent; however, it does not allow for therapeutic intervention if such intervention is necessary.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 94898,
"questionText": "A patient with abdominal pain undergoes a CT scan. Her pancreas does not have a body or tail. Which imaging modalities or interventions is indicated?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 337594,
"choiceText": "Exogenous replacement of pancreatic enzymes",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337595,
"choiceText": "Pancreas transplant",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337596,
"choiceText": "Hemodialysis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337597,
"choiceText": "Surgical consultation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Treatment of dorsal agenesis of the pancreas is generally supportive and may include insulin administration or exogenous replacement with pancreatic enzymes. The abdominal pain is often attributed to pancreatitis, duodenal obstruction, sphincter of Oddi dysfunction, or autonomic neuropathy. Although a rare diagnosis in adults, dorsal agenesis of the pancreas should be included in the differential diagnosis of diabetic patients with pancreatitis or abdominal pain, or when body and tail of the pancreas are not visualized on imaging.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 94899,
"questionText": "Which is indicated for a patient with vague abdominal pain with dorsal agenesis of the pancreas?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: A Woman Who Abstains from Alcohol Has Worsening Abdominal Pain"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 337574,
"choiceText": "Fatty infiltration of the pancreas",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337575,
"choiceText": "Dorsal agenesis of the pancreas",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337576,
"choiceText": "Pancreas divisum",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337577,
"choiceText": " Autogenesis of the pancreas",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 94894,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 337590,
"choiceText": "Abdominal ultrasonography",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337591,
"choiceText": "MRCP or ERCP",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337592,
"choiceText": "Abdominal radiography",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337593,
"choiceText": "Colonoscopy",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "In the setting of abdominal pain, the best modality for evaluating pancreatic disease is CT scanning or MRI of the abdomen. When the pancreatic anatomy is altered, the next best imaging modality for evaluation is an ERCP or MRCP to visualize the pancreatic tree. MRCP has certain advantages over ERCP; primarily it is a noninvasive means of evaluating the biliary and pancreatic systems in their natural state. In addition, it is an imaging modality that is not operator-dependent; however, it does not allow for therapeutic intervention if such intervention is necessary.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 94898,
"questionText": "A patient with abdominal pain undergoes a CT scan. Her pancreas does not have a body or tail. Which imaging modalities or interventions is indicated?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 337594,
"choiceText": "Exogenous replacement of pancreatic enzymes",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337595,
"choiceText": "Pancreas transplant",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337596,
"choiceText": "Hemodialysis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 337597,
"choiceText": "Surgical consultation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Treatment of dorsal agenesis of the pancreas is generally supportive and may include insulin administration or exogenous replacement with pancreatic enzymes. The abdominal pain is often attributed to pancreatitis, duodenal obstruction, sphincter of Oddi dysfunction, or autonomic neuropathy. Although a rare diagnosis in adults, dorsal agenesis of the pancreas should be included in the differential diagnosis of diabetic patients with pancreatitis or abdominal pain, or when body and tail of the pancreas are not visualized on imaging.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 94899,
"questionText": "Which is indicated for a patient with vague abdominal pain with dorsal agenesis of the pancreas?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
842254 | /viewarticle/842254 | [
{
"authors": "Lemi Luu, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 40-year-old man presents to the emergency department with palpitations and shortness of breath that started a few minutes before his arrival.",
"The patient states that he was closing his shop when his heart began to beat rapidly and he had difficulty catching his breath. His symptoms started suddenly and continued when paramedics arrived minutes later. They observed a rapid heart rate on the cardiac monitor and associated rhythm strips (Figures 1 and 2). He was subsequently given adenosine 0.6 mg en route to the hospital. The patient had a momentary period of asystole, but his rapid heart rate returned.",
"Figure 1.",
"Figure 2.",
"On his arrival to the emergency department, the patient continued to have the sensation that his heart was racing. He denies having any chest pain, nausea, vomiting, diaphoresis, light-headedness, or recent illness. He felt well before this episode. He denies having any symptoms of infection, such as fever, cough, vomiting, diarrhea, anorexia, or dysuria. He reports increased stress at work and is drinking at least 4 cups of coffee a day. He reports no notable history of medical conditions except for a similar episode of a rapid heart rate about 4 years ago; for this, he was treated with a drug he does not remember for 2 years.",
"His family history is significant for a father who died of a myocardial infarction at age 45 years. The patient takes 1 baby aspirin daily. He denies using any over-the-counter or illicit drugs; however, he smokes 3 packs of cigarettes per week."
],
"date": "April 28, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/842/254/842254-thumb-1.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/842/254/842254-thumb-2.jpg"
}
],
"markdown": "# A Coffee Drinker With Sudden-Onset Dyspnea, Tachycardia\n\n **Authors:** Lemi Luu, MD \n **Date:** April 28, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 40-year-old man presents to the emergency department with palpitations and shortness of breath that started a few minutes before his arrival.\nThe patient states that he was closing his shop when his heart began to beat rapidly and he had difficulty catching his breath. His symptoms started suddenly and continued when paramedics arrived minutes later. They observed a rapid heart rate on the cardiac monitor and associated rhythm strips (Figures 1 and 2). He was subsequently given adenosine 0.6 mg en route to the hospital. The patient had a momentary period of asystole, but his rapid heart rate returned.\nFigure 1.\nFigure 2.\nOn his arrival to the emergency department, the patient continued to have the sensation that his heart was racing. He denies having any chest pain, nausea, vomiting, diaphoresis, light-headedness, or recent illness. He felt well before this episode. He denies having any symptoms of infection, such as fever, cough, vomiting, diarrhea, anorexia, or dysuria. He reports increased stress at work and is drinking at least 4 cups of coffee a day. He reports no notable history of medical conditions except for a similar episode of a rapid heart rate about 4 years ago; for this, he was treated with a drug he does not remember for 2 years.\nHis family history is significant for a father who died of a myocardial infarction at age 45 years. The patient takes 1 baby aspirin daily. He denies using any over-the-counter or illicit drugs; however, he smokes 3 packs of cigarettes per week.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A Coffee Drinker With Sudden-Onset Dyspnea, Tachycardia"
},
{
"authors": "Lemi Luu, MD",
"content": [
"Upon physical examination, the patient is afebrile and has a heart rate of 165 beats/min and a blood pressure of 138/79 mm Hg. He appears well and is in no acute distress.",
"Findings on head and neck examination are unremarkable. The patient has no jugular venous distention. His heart rate is rapid and irregular, with an audible S1 and S2 and no gallops, rubs, or murmurs. His lungs are clear bilaterally. His abdomen is soft and nontender, and without masses. He has no peripheral edema. Results of his laboratory work-up, including a complete blood count (CBC), serum electrolyte and cardiac enzyme measurements, and a coagulation panel, are all normal. His chest radiograph findings are also normal.",
"An ECG is obtained (Figure 3).",
"Figure 3."
],
"date": "April 28, 2022",
"figures": [
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/842/254/842254-thumb-3.jpg"
}
],
"markdown": "# A Coffee Drinker With Sudden-Onset Dyspnea, Tachycardia\n\n **Authors:** Lemi Luu, MD \n **Date:** April 28, 2022\n\n ## Content\n\n Upon physical examination, the patient is afebrile and has a heart rate of 165 beats/min and a blood pressure of 138/79 mm Hg. He appears well and is in no acute distress.\nFindings on head and neck examination are unremarkable. The patient has no jugular venous distention. His heart rate is rapid and irregular, with an audible S1 and S2 and no gallops, rubs, or murmurs. His lungs are clear bilaterally. His abdomen is soft and nontender, and without masses. He has no peripheral edema. Results of his laboratory work-up, including a complete blood count (CBC), serum electrolyte and cardiac enzyme measurements, and a coagulation panel, are all normal. His chest radiograph findings are also normal.\nAn ECG is obtained (Figure 3).\nFigure 3.\n\n ## Figures\n\n **Figure 3.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 831329,
"choiceText": "Ventricular fibrillation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831331,
"choiceText": "Atrial fibrillation",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831333,
"choiceText": "Torsade de pointes",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831335,
"choiceText": "Sinus tachycardia ",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 261405,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Coffee Drinker With Sudden-Onset Dyspnea, Tachycardia"
},
{
"authors": "Lemi Luu, MD",
"content": [
"The ECG shows an irregularly irregular heart rhythm with no discernible P waves. Rapid atrial fibrillation (AF) may be hard to differentiate from a narrow supraventricular tachycardia (SVT) without close examination of an ECG. The two conditions can result in similar symptoms of heart palpitations and shortness of breath. Patients with rapid AF are not uncommonly given adenosine to treat presumed SVT, as in this case. Although this treatment is typically unsuccessful, the underlying atrial rhythm may be accurately determined when the heart rate briefly slows.",
"The conversion from a normal sinus rhythm to AF may be due to numerous conditions, including hyperthyroidism, anemia, infection, ischemic heart disease, valvular disease, drug intoxication, or use of stimulants. Increased stress, overconsumption of coffee, and smoking are possible instigating factors in this patient.",
"AF is a common arrhythmia characterized by chaotic atrial depolarizations without effective mechanical atrial contractions. This rhythm is often seen with increasing age, with a male predominance. This arrhythmia can result in decreased cardiac output and the formation of atrial thrombi. Many patients with AF are asymptomatic, and most have recurrent episodes without knowledge of them.",
"The American College of Cardiology established a classification system for AF that is based on its duration and etiology. The categories are paroxysmal AF, persistent AF, permanent AF, and lone AF.",
"In paroxysmal AF, the episodes last less than 1 week. If they recur, the condition is considered recurrent paroxysmal AF.",
"In persistent AF, the episodes last longer than 1 week. In long-standing persistent AF, the episode lasts longer than 1 year. In permanent AF, the episode is long-standing, and no further efforts are made to restore sinus rhythm.",
"Finally, in lone AF, no underlying structural cardiac or pulmonary disease is found. Patients with lone AF have a low risk for death and thromboembolism and may have paroxysmal, persistent, or permanent AF."
],
"date": "April 28, 2022",
"figures": [],
"markdown": "# A Coffee Drinker With Sudden-Onset Dyspnea, Tachycardia\n\n **Authors:** Lemi Luu, MD \n **Date:** April 28, 2022\n\n ## Content\n\n The ECG shows an irregularly irregular heart rhythm with no discernible P waves. Rapid atrial fibrillation (AF) may be hard to differentiate from a narrow supraventricular tachycardia (SVT) without close examination of an ECG. The two conditions can result in similar symptoms of heart palpitations and shortness of breath. Patients with rapid AF are not uncommonly given adenosine to treat presumed SVT, as in this case. Although this treatment is typically unsuccessful, the underlying atrial rhythm may be accurately determined when the heart rate briefly slows.\nThe conversion from a normal sinus rhythm to AF may be due to numerous conditions, including hyperthyroidism, anemia, infection, ischemic heart disease, valvular disease, drug intoxication, or use of stimulants. Increased stress, overconsumption of coffee, and smoking are possible instigating factors in this patient.\nAF is a common arrhythmia characterized by chaotic atrial depolarizations without effective mechanical atrial contractions. This rhythm is often seen with increasing age, with a male predominance. This arrhythmia can result in decreased cardiac output and the formation of atrial thrombi. Many patients with AF are asymptomatic, and most have recurrent episodes without knowledge of them.\nThe American College of Cardiology established a classification system for AF that is based on its duration and etiology. The categories are paroxysmal AF, persistent AF, permanent AF, and lone AF.\nIn paroxysmal AF, the episodes last less than 1 week. If they recur, the condition is considered recurrent paroxysmal AF.\nIn persistent AF, the episodes last longer than 1 week. In long-standing persistent AF, the episode lasts longer than 1 year. In permanent AF, the episode is long-standing, and no further efforts are made to restore sinus rhythm.\nFinally, in lone AF, no underlying structural cardiac or pulmonary disease is found. Patients with lone AF have a low risk for death and thromboembolism and may have paroxysmal, persistent, or permanent AF.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 831329,
"choiceText": "Ventricular fibrillation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831331,
"choiceText": "Atrial fibrillation",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831333,
"choiceText": "Torsade de pointes",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831335,
"choiceText": "Sinus tachycardia ",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 261405,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Coffee Drinker With Sudden-Onset Dyspnea, Tachycardia"
},
{
"authors": "Lemi Luu, MD",
"content": [
"The work-up for AF involves careful history taking and physical examination, laboratory studies (including a CBC, serum electrolyte tests, toxicology screening, and thyroid function tests), ECG, chest radiography, and echocardiography. The patient's history should include the time of onset, the frequency of episodes, any associated symptoms, and any history of treatment for AF. Laboratory studies may be useful in determining possible etiologies of AF. The WBC count may help in finding an underlying infection, and the hemoglobin concentration may demonstrate anemia. Electrolyte levels, such as magnesium and potassium, may be abnormal, and an elevated creatinine value may indicate renal insufficiency.",
"Certain illicit drugs can cause a rapid heart rate; therefore, a toxicology screening may be useful when indicated.",
"Hyperthyroidism can predispose patients to AF. For this reason, an evaluation of thyroid function with measurement of the patient's thyroid-stimulating hormone level is warranted.",
"AF can be diagnosed when the ECG shows an irregular rhythm with the absence of P waves. In addition, examine the patient for any signs of left ventricular hypertrophy, bundle branch blocks, and atrioventricular nodal blocks, as well as for evidence of cardiac ischemia or previous myocardial infarction. Chest radiographs may be useful in evaluating the cardiac silhouette for cardiomegaly and the lung fields and vasculature for evidence of airspace disease or pulmonary edema.",
"A transthoracic echocardiogram should be obtained to identify the size and motion of the atria, ventricles, and cardiac valves, and it can reveal pericardial disease. Transesophageal echocardiography is more sensitive than transthoracic echocardiography for diagnosing left atrial thrombus or left atrial appendage thrombus.",
"Rate control is important in patients who present with rapid AF of more than 72 hours' duration, and beta-blockers (metoprolol) or calcium-channel blockers (diltiazem) are recommended in patients who do not have an accessory pathway. Digoxin and amiodarone are the drugs of choice for controlling rapid AF in patients with left ventricular failure and no accessory pathway; however, digoxin should be loaded over 24 hours.",
"Anticoagulation treatment is also recommended for most patients with AF to help reduce the risk for stroke. The CHADS2 and CHA2DS2-VASc scores can help determine risk and help make decisions about anticoagulation treatment. These scores use such components as age; sex; and associated conditions, including hypertension, congestive heart failure, diabetes, vascular disease, or a prior stroke.",
"Anticoagulation is typically achieved with warfarin (dosed to maintain an international normalized ratio of 2-3) or one of the new novel oral anticoagulants (NOAC), such as dabigatran, rivaroxaban, or apixaban. In patients considered to be at low risk for thromboembolism or in patients who have a contraindication to the use of warfarin or NOACs, aspirin can be administered.",
"Conversion to sinus rhythm may be achieved with pharmacologic agents or with synchronized external electrical cardioversion. Conversion should be done only when the risk for thromboembolism is limited, as in patients with an onset of symptoms less than 72 hours before presentation, in those who received anticoagulation for 4 weeks, or in those in whom transesophageal echocardiography rules out a left atrial or left atrial appendage thrombus. For patients with chronic symptomatic AF, catheter-based ablation (via pulmonary vein isolation) is used to decrease the burden."
],
"date": "April 28, 2022",
"figures": [],
"markdown": "# A Coffee Drinker With Sudden-Onset Dyspnea, Tachycardia\n\n **Authors:** Lemi Luu, MD \n **Date:** April 28, 2022\n\n ## Content\n\n The work-up for AF involves careful history taking and physical examination, laboratory studies (including a CBC, serum electrolyte tests, toxicology screening, and thyroid function tests), ECG, chest radiography, and echocardiography. The patient's history should include the time of onset, the frequency of episodes, any associated symptoms, and any history of treatment for AF. Laboratory studies may be useful in determining possible etiologies of AF. The WBC count may help in finding an underlying infection, and the hemoglobin concentration may demonstrate anemia. Electrolyte levels, such as magnesium and potassium, may be abnormal, and an elevated creatinine value may indicate renal insufficiency.\nCertain illicit drugs can cause a rapid heart rate; therefore, a toxicology screening may be useful when indicated.\nHyperthyroidism can predispose patients to AF. For this reason, an evaluation of thyroid function with measurement of the patient's thyroid-stimulating hormone level is warranted.\nAF can be diagnosed when the ECG shows an irregular rhythm with the absence of P waves. In addition, examine the patient for any signs of left ventricular hypertrophy, bundle branch blocks, and atrioventricular nodal blocks, as well as for evidence of cardiac ischemia or previous myocardial infarction. Chest radiographs may be useful in evaluating the cardiac silhouette for cardiomegaly and the lung fields and vasculature for evidence of airspace disease or pulmonary edema.\nA transthoracic echocardiogram should be obtained to identify the size and motion of the atria, ventricles, and cardiac valves, and it can reveal pericardial disease. Transesophageal echocardiography is more sensitive than transthoracic echocardiography for diagnosing left atrial thrombus or left atrial appendage thrombus.\nRate control is important in patients who present with rapid AF of more than 72 hours' duration, and beta-blockers (metoprolol) or calcium-channel blockers (diltiazem) are recommended in patients who do not have an accessory pathway. Digoxin and amiodarone are the drugs of choice for controlling rapid AF in patients with left ventricular failure and no accessory pathway; however, digoxin should be loaded over 24 hours.\nAnticoagulation treatment is also recommended for most patients with AF to help reduce the risk for stroke. The CHADS2 and CHA2DS2-VASc scores can help determine risk and help make decisions about anticoagulation treatment. These scores use such components as age; sex; and associated conditions, including hypertension, congestive heart failure, diabetes, vascular disease, or a prior stroke.\nAnticoagulation is typically achieved with warfarin (dosed to maintain an international normalized ratio of 2-3) or one of the new novel oral anticoagulants (NOAC), such as dabigatran, rivaroxaban, or apixaban. In patients considered to be at low risk for thromboembolism or in patients who have a contraindication to the use of warfarin or NOACs, aspirin can be administered.\nConversion to sinus rhythm may be achieved with pharmacologic agents or with synchronized external electrical cardioversion. Conversion should be done only when the risk for thromboembolism is limited, as in patients with an onset of symptoms less than 72 hours before presentation, in those who received anticoagulation for 4 weeks, or in those in whom transesophageal echocardiography rules out a left atrial or left atrial appendage thrombus. For patients with chronic symptomatic AF, catheter-based ablation (via pulmonary vein isolation) is used to decrease the burden.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A Coffee Drinker With Sudden-Onset Dyspnea, Tachycardia"
},
{
"authors": "Lemi Luu, MD",
"content": [
"After successful cardioversion, anticoagulation therapy should continue for at least 1 month to decrease the risk for thromboembolism, which may occur from the formation of a mural thrombus. After cardioversion is done and the patient's AF reverts to a sinus rhythm, use of daily outpatient antiarrhythmic drugs is not typically recommended, as these drugs have associated risks; therefore, they should be taken only when patients have persistent or frequently recurring symptoms.",
"Antiarrhythmic drugs that can be used to convert AF to a normal sinus rhythm include ibutilide, flecainide, procainamide, and amiodarone. Each has different risks, success rates, and indications, based on the duration of AF. As a group, antiarrhythmic drugs can convert 30%-60% of cases of AF to a normal sinus rhythm. Electrical cardioversion has a higher success rate, converting 75%-95% of AF cases to normal sinus rhythm.",
"Electrical cardioversion may be done in a nonemergency setting after 4 weeks of anticoagulation treatment to decrease the risk for thromboembolism, or it can be done after transesophageal echocardiography has ruled out a left atrial or appendage thrombus. It may be required on an emergency basis in a hemodynamically unstable patient. In this situation, AF often has an acute onset, and the benefits of cardioversion outweigh the risks for thromboembolism.",
"The role of cardioversion to manage AF in the emergency department is an emerging one. Patients who are at low risk, are clinically stable, and present to the emergency department with new-onset AF can be treated with chemical or electrical cardioversion and safely discharged home, with close follow-up by a primary physician or cardiologist."
],
"date": "April 28, 2022",
"figures": [],
"markdown": "# A Coffee Drinker With Sudden-Onset Dyspnea, Tachycardia\n\n **Authors:** Lemi Luu, MD \n **Date:** April 28, 2022\n\n ## Content\n\n After successful cardioversion, anticoagulation therapy should continue for at least 1 month to decrease the risk for thromboembolism, which may occur from the formation of a mural thrombus. After cardioversion is done and the patient's AF reverts to a sinus rhythm, use of daily outpatient antiarrhythmic drugs is not typically recommended, as these drugs have associated risks; therefore, they should be taken only when patients have persistent or frequently recurring symptoms.\nAntiarrhythmic drugs that can be used to convert AF to a normal sinus rhythm include ibutilide, flecainide, procainamide, and amiodarone. Each has different risks, success rates, and indications, based on the duration of AF. As a group, antiarrhythmic drugs can convert 30%-60% of cases of AF to a normal sinus rhythm. Electrical cardioversion has a higher success rate, converting 75%-95% of AF cases to normal sinus rhythm.\nElectrical cardioversion may be done in a nonemergency setting after 4 weeks of anticoagulation treatment to decrease the risk for thromboembolism, or it can be done after transesophageal echocardiography has ruled out a left atrial or appendage thrombus. It may be required on an emergency basis in a hemodynamically unstable patient. In this situation, AF often has an acute onset, and the benefits of cardioversion outweigh the risks for thromboembolism.\nThe role of cardioversion to manage AF in the emergency department is an emerging one. Patients who are at low risk, are clinically stable, and present to the emergency department with new-onset AF can be treated with chemical or electrical cardioversion and safely discharged home, with close follow-up by a primary physician or cardiologist.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 831337,
"choiceText": "Nephrotic syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831339,
"choiceText": "Moderate caffeine consumption",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831341,
"choiceText": "Hyperlipidemia",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831343,
"choiceText": "Infection",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831345,
"choiceText": "Hypothyroidism",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "An underlying infection, such as a urinary tract infection or pneumonia, can lead to the development of AF. Electrolyte levels, such as magnesium and potassium levels, may be abnormal, and an elevated creatinine value may indicate a renal insufficiency. Certain illicit drugs, such as amphetamines and cocaine, can cause a rapid heart rate, including AF; therefore, toxicology screening may be useful when indicated. Moderate caffeine consumption does not appear to increase the risk for AF. Hyperthyroidism can also predispose patients to AF, whereas the evidence on hypothyroidism is not as clear. Nephrotic syndrome and hyperlipidemia have not been conclusively linked to AF development.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 261407,
"questionText": "Of these, which is best supported as a cause of AF?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 831347,
"choiceText": "Hydrochlorothiazide",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831349,
"choiceText": "Metolazone",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831351,
"choiceText": "Ethacrynic acid",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831353,
"choiceText": "Triamterene",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831355,
"choiceText": "Metoprolol",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Rate control is important in patients who present with rapid AF of more than 72 hours' duration, and beta-blockers (metoprolol) or calcium-channel blockers (diltiazem) are recommended in patients who do not have an accessory pathway. Digoxin and amiodarone are the drugs of choice for controlling rapid AF in patients with left ventricular failure and no accessory pathway; however, digoxin should be loaded over 24 hours. Therefore, it is unlikely to have a notable effect in the acute setting. Hydrochlorothiazide, metolazone, ethacrynic acid, and triamterene are all diuretics and therefore not rate-control agents.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 261409,
"questionText": "What medication is an acceptable rate control agent in AF?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Coffee Drinker With Sudden-Onset Dyspnea, Tachycardia"
},
{
"authors": "Lemi Luu, MD",
"content": [],
"date": "April 28, 2022",
"figures": [],
"markdown": "# A Coffee Drinker With Sudden-Onset Dyspnea, Tachycardia\n\n **Authors:** Lemi Luu, MD \n **Date:** April 28, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 831337,
"choiceText": "Nephrotic syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831339,
"choiceText": "Moderate caffeine consumption",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831341,
"choiceText": "Hyperlipidemia",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831343,
"choiceText": "Infection",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831345,
"choiceText": "Hypothyroidism",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "An underlying infection, such as a urinary tract infection or pneumonia, can lead to the development of AF. Electrolyte levels, such as magnesium and potassium levels, may be abnormal, and an elevated creatinine value may indicate a renal insufficiency. Certain illicit drugs, such as amphetamines and cocaine, can cause a rapid heart rate, including AF; therefore, toxicology screening may be useful when indicated. Moderate caffeine consumption does not appear to increase the risk for AF. Hyperthyroidism can also predispose patients to AF, whereas the evidence on hypothyroidism is not as clear. Nephrotic syndrome and hyperlipidemia have not been conclusively linked to AF development.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 261407,
"questionText": "Of these, which is best supported as a cause of AF?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 831347,
"choiceText": "Hydrochlorothiazide",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831349,
"choiceText": "Metolazone",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831351,
"choiceText": "Ethacrynic acid",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831353,
"choiceText": "Triamterene",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831355,
"choiceText": "Metoprolol",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Rate control is important in patients who present with rapid AF of more than 72 hours' duration, and beta-blockers (metoprolol) or calcium-channel blockers (diltiazem) are recommended in patients who do not have an accessory pathway. Digoxin and amiodarone are the drugs of choice for controlling rapid AF in patients with left ventricular failure and no accessory pathway; however, digoxin should be loaded over 24 hours. Therefore, it is unlikely to have a notable effect in the acute setting. Hydrochlorothiazide, metolazone, ethacrynic acid, and triamterene are all diuretics and therefore not rate-control agents.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 261409,
"questionText": "What medication is an acceptable rate control agent in AF?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Coffee Drinker With Sudden-Onset Dyspnea, Tachycardia"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 831329,
"choiceText": "Ventricular fibrillation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831331,
"choiceText": "Atrial fibrillation",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831333,
"choiceText": "Torsade de pointes",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831335,
"choiceText": "Sinus tachycardia ",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 261405,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 831337,
"choiceText": "Nephrotic syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831339,
"choiceText": "Moderate caffeine consumption",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831341,
"choiceText": "Hyperlipidemia",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831343,
"choiceText": "Infection",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831345,
"choiceText": "Hypothyroidism",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "An underlying infection, such as a urinary tract infection or pneumonia, can lead to the development of AF. Electrolyte levels, such as magnesium and potassium levels, may be abnormal, and an elevated creatinine value may indicate a renal insufficiency. Certain illicit drugs, such as amphetamines and cocaine, can cause a rapid heart rate, including AF; therefore, toxicology screening may be useful when indicated. Moderate caffeine consumption does not appear to increase the risk for AF. Hyperthyroidism can also predispose patients to AF, whereas the evidence on hypothyroidism is not as clear. Nephrotic syndrome and hyperlipidemia have not been conclusively linked to AF development.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 261407,
"questionText": "Of these, which is best supported as a cause of AF?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 831347,
"choiceText": "Hydrochlorothiazide",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831349,
"choiceText": "Metolazone",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831351,
"choiceText": "Ethacrynic acid",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831353,
"choiceText": "Triamterene",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831355,
"choiceText": "Metoprolol",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Rate control is important in patients who present with rapid AF of more than 72 hours' duration, and beta-blockers (metoprolol) or calcium-channel blockers (diltiazem) are recommended in patients who do not have an accessory pathway. Digoxin and amiodarone are the drugs of choice for controlling rapid AF in patients with left ventricular failure and no accessory pathway; however, digoxin should be loaded over 24 hours. Therefore, it is unlikely to have a notable effect in the acute setting. Hydrochlorothiazide, metolazone, ethacrynic acid, and triamterene are all diuretics and therefore not rate-control agents.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 261409,
"questionText": "What medication is an acceptable rate control agent in AF?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
847158 | /viewarticle/847158 | [
{
"authors": "Lars Grimm, MD",
"content": [
"Editor's Note:\n\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 57-year-old man with a history of type 2 diabetes mellitus and hypertension presents with a 2-week history of vesiculobullous lesions on his feet and hands. The lesions first appeared on both of his feet and have been increasing in size and number; over the past several days, they have begun to develop on both of his palms and on the sides of the fingers. The patient was seen at a different clinic approximately 1 week ago and was given an ointment to treat the lesions; this has not resulted in any improvement. The lesions are extremely pruritic.",
"The patient has not had any recent travel history, and he lives alone, without any pets, in a regularly cleaned apartment. He has had no discernible new exposures and has not experienced any fevers or constitutional symptoms. The patient is on insulin, labetalol, and a combination pill of lisinopril/hydrochlorothiazide plus omeprazole; he has been on these medications for a long time and has had no prior complications. The patient has no known allergies."
],
"date": "April 20, 2022",
"figures": [],
"markdown": "# PCP Case Challenge: Lesions on the Hands, Palms, and Feet of a 57-Year-Old Man\n\n **Authors:** Lars Grimm, MD \n **Date:** April 20, 2022\n\n ## Content\n\n Editor's Note:\n\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 57-year-old man with a history of type 2 diabetes mellitus and hypertension presents with a 2-week history of vesiculobullous lesions on his feet and hands. The lesions first appeared on both of his feet and have been increasing in size and number; over the past several days, they have begun to develop on both of his palms and on the sides of the fingers. The patient was seen at a different clinic approximately 1 week ago and was given an ointment to treat the lesions; this has not resulted in any improvement. The lesions are extremely pruritic.\nThe patient has not had any recent travel history, and he lives alone, without any pets, in a regularly cleaned apartment. He has had no discernible new exposures and has not experienced any fevers or constitutional symptoms. The patient is on insulin, labetalol, and a combination pill of lisinopril/hydrochlorothiazide plus omeprazole; he has been on these medications for a long time and has had no prior complications. The patient has no known allergies.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "PCP Case Challenge: Lesions on the Hands, Palms, and Feet of a 57-Year-Old Man"
},
{
"authors": "Lars Grimm, MD",
"content": [
"Upon physical examination, the patient is well-appearing at rest, without any signs of undue anxiety or discomfort. His vital signs show a temperature of 98.7ºF (37.1ºC), blood pressure of 130/85 mm Hg, heart rate of 70 beats/min, respiratory rate of 18 breaths/min, and oxygen saturation of 98% while breathing room air.",
"Fluid-filled vesicles ranging in size from 1 mm to 3 cm are present on the instep and plantar aspects of his feet (Figures 1 and 2). The vesicles are present on the palms of his hands and the sides of the fingers as well. The lesions are all skin-colored, without any surrounding erythema.",
"Figure 1.",
"Figure 1.",
"Figure 2.",
"Figure 2.",
"No other lesions are found anywhere else on the patient's body. The lesions are nontender to palpation; additionally, his legs exhibit nonpitting edema up to the knees and reduced sensation to light touch, both long-standing conditions. The oropharynx is clear of any lesions, and the rest of the physical examination is unremarkable."
],
"date": "April 20, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/847/158/847158-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/847/158/847158-Thumb2.png"
}
],
"markdown": "# PCP Case Challenge: Lesions on the Hands, Palms, and Feet of a 57-Year-Old Man\n\n **Authors:** Lars Grimm, MD \n **Date:** April 20, 2022\n\n ## Content\n\n Upon physical examination, the patient is well-appearing at rest, without any signs of undue anxiety or discomfort. His vital signs show a temperature of 98.7ºF (37.1ºC), blood pressure of 130/85 mm Hg, heart rate of 70 beats/min, respiratory rate of 18 breaths/min, and oxygen saturation of 98% while breathing room air.\nFluid-filled vesicles ranging in size from 1 mm to 3 cm are present on the instep and plantar aspects of his feet (Figures 1 and 2). The vesicles are present on the palms of his hands and the sides of the fingers as well. The lesions are all skin-colored, without any surrounding erythema.\nFigure 1.\nFigure 1.\nFigure 2.\nFigure 2.\nNo other lesions are found anywhere else on the patient's body. The lesions are nontender to palpation; additionally, his legs exhibit nonpitting edema up to the knees and reduced sensation to light touch, both long-standing conditions. The oropharynx is clear of any lesions, and the rest of the physical examination is unremarkable.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 867285,
"choiceText": "Allergic contact dermatitis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867287,
"choiceText": "Herpes simplex",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867289,
"choiceText": "Impetigo",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867291,
"choiceText": "Dyshidrotic eczema",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 272843,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "PCP Case Challenge: Lesions on the Hands, Palms, and Feet of a 57-Year-Old Man"
},
{
"authors": "Lars Grimm, MD",
"content": [
"The diagnosis of dyshidrotic eczema, also known as pompholyx (Greek for \"bubble\"), was made on the basis of the patient's history and the results of the physical examination. Additional testing (described below) ruled out any alternative diagnoses. The pruritic lesions were progressive in number and size, but they were restricted to the hands and feet. The blisters were classically vesiculobullous in nature, without any surrounding erythema. Lesions in multiple stages of development, from emerging vesicles to ruptured bullae, were concurrently present.",
"The history did not reveal any etiologic factors, such as recent exposures to allergens, new medications, or animal-borne vectors. The patient did not have any systemic symptoms and was afebrile. No evidence of concurrent cellulitis or lymphangitis was apparent.",
"Dyshidrotic eczema is estimated to be present in 0.5%-1% of the population and is twice as common in women than in men. Most cases present before the patients reach age 40 years, and no racial predominance is noted. It is more commonly found in warmer, more humid climates, especially during the spring and summer. Recurrences may occur throughout a patient's lifetime, with or without treatment.",
"The pathophysiology of dyshidrotic eczema has not been definitively established,[1] but several hypotheses have been proposed. The term \"dyshidrosis\" is a misnomer that refers to the original hypothesis of sweat gland dysfunction, which has fallen out of favor. In addition, patients are not typically noted to experience hyperhidrosis. The association of the condition with atopy is interesting,[2] as approximately 20% of patients experience concomitant hand eczema, and approximately 50% of patients have a general disposition to an atopic diathesis (eg, asthma, hay fever, and sinusitis).[3]",
"Other exogenous factors that have been implicated and may trigger episodes include contact dermatitis to heavy metals (such as with exposure to costume jewelry, nickel,[1,3] cobalt,[1] or chromates); sensitivity to ingested metals[1]; exposure to other contact allergens such as balsam,[1] paraphenylenediamine, and sesquiterpene lactones; and infection by dermatophytes or bacteria. Emotional stress (many patients report recurrences during stressful periods of their life) and environmental factors (eg, seasonal changes, hot or cold temperatures, and humidity) are also reported to exacerbate dyshidrosis.[1,3]",
"Dyshidrotic eczema has also been reported in patients recently treated with intravenous immunoglobulin (IVIg) therapy; in HIV-positive patients with an immune reconstitution inflammatory syndrome shortly after starting active antiretroviral therapy[1]; with the use of aspirin or oral contraceptives; and with cigarette smoking. In most cases, the condition remains idiopathic."
],
"date": "April 20, 2022",
"figures": [],
"markdown": "# PCP Case Challenge: Lesions on the Hands, Palms, and Feet of a 57-Year-Old Man\n\n **Authors:** Lars Grimm, MD \n **Date:** April 20, 2022\n\n ## Content\n\n The diagnosis of dyshidrotic eczema, also known as pompholyx (Greek for \"bubble\"), was made on the basis of the patient's history and the results of the physical examination. Additional testing (described below) ruled out any alternative diagnoses. The pruritic lesions were progressive in number and size, but they were restricted to the hands and feet. The blisters were classically vesiculobullous in nature, without any surrounding erythema. Lesions in multiple stages of development, from emerging vesicles to ruptured bullae, were concurrently present.\nThe history did not reveal any etiologic factors, such as recent exposures to allergens, new medications, or animal-borne vectors. The patient did not have any systemic symptoms and was afebrile. No evidence of concurrent cellulitis or lymphangitis was apparent.\nDyshidrotic eczema is estimated to be present in 0.5%-1% of the population and is twice as common in women than in men. Most cases present before the patients reach age 40 years, and no racial predominance is noted. It is more commonly found in warmer, more humid climates, especially during the spring and summer. Recurrences may occur throughout a patient's lifetime, with or without treatment.\nThe pathophysiology of dyshidrotic eczema has not been definitively established,[1] but several hypotheses have been proposed. The term \"dyshidrosis\" is a misnomer that refers to the original hypothesis of sweat gland dysfunction, which has fallen out of favor. In addition, patients are not typically noted to experience hyperhidrosis. The association of the condition with atopy is interesting,[2] as approximately 20% of patients experience concomitant hand eczema, and approximately 50% of patients have a general disposition to an atopic diathesis (eg, asthma, hay fever, and sinusitis).[3]\nOther exogenous factors that have been implicated and may trigger episodes include contact dermatitis to heavy metals (such as with exposure to costume jewelry, nickel,[1,3] cobalt,[1] or chromates); sensitivity to ingested metals[1]; exposure to other contact allergens such as balsam,[1] paraphenylenediamine, and sesquiterpene lactones; and infection by dermatophytes or bacteria. Emotional stress (many patients report recurrences during stressful periods of their life) and environmental factors (eg, seasonal changes, hot or cold temperatures, and humidity) are also reported to exacerbate dyshidrosis.[1,3]\nDyshidrotic eczema has also been reported in patients recently treated with intravenous immunoglobulin (IVIg) therapy; in HIV-positive patients with an immune reconstitution inflammatory syndrome shortly after starting active antiretroviral therapy[1]; with the use of aspirin or oral contraceptives; and with cigarette smoking. In most cases, the condition remains idiopathic.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 867285,
"choiceText": "Allergic contact dermatitis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867287,
"choiceText": "Herpes simplex",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867289,
"choiceText": "Impetigo",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867291,
"choiceText": "Dyshidrotic eczema",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 272843,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "PCP Case Challenge: Lesions on the Hands, Palms, and Feet of a 57-Year-Old Man"
},
{
"authors": "Lars Grimm, MD",
"content": [
"Dyshidrotic eczema is a recurrent or chronic, relapsing form of vesicular dermatitis. The classic presentation is of crops of vesicles or bullae that erupt bilaterally on the palms and the lateral aspects of the fingers. The vesicles may coalesce over time to form multiloculated bullae. Most cases involve the hands alone (cheiropompholyx), but roughly 10% of patients have lesions on both the hands and feet, and another 10% have lesions on just the feet (podopompholyx).",
"The lesions may be intensely pruritic, leading to secondary desquamation and erosions and ulcerations from scratching. Dyshidrotic eczema developing near the tips of the fingers or toes may lead to dystrophic changes of the nails. Cellulitis, lymphangitis, or infection of the lesions themselves may all develop with the long-standing presence of lesions and/or poor hygiene. The vesicular crops usually resolve spontaneously after 3-4 weeks, leaving behind collarettes of scale. Although self-limited, outbreaks frequently alternate with disease-free intervals of weeks to months and, if severe, may be extremely disabling.[1]",
"The differential diagnosis includes immunobullous disorders, such as bullous pemphigoid and pemphigus vulgaris, or other dermatoses, such as contact dermatitis, herpes simplex virus infection, bullous tinea pedis, and pustular psoriasis. The diagnosis is usually made on the basis of the clinical history, the physical examination, and the exclusion of alternative diagnoses. Bacterial culture and sensitivities may be evaluated for secondary infections.",
"Additionally, potassium hydroxide wet mount preparations may be useful for excluding dermatophyte infections. A skin biopsy may also be useful for confirming the clinical impression in unresponsive cases and for excluding alternative diagnoses. It can be difficult to differentiate dyshidrotic eczema from an id reaction (autoeczematization), which is a cutaneous eruption that develops in response to various infectious and inflammatory stimuli at a distant site from the primary dermatosis.[1]"
],
"date": "April 20, 2022",
"figures": [],
"markdown": "# PCP Case Challenge: Lesions on the Hands, Palms, and Feet of a 57-Year-Old Man\n\n **Authors:** Lars Grimm, MD \n **Date:** April 20, 2022\n\n ## Content\n\n Dyshidrotic eczema is a recurrent or chronic, relapsing form of vesicular dermatitis. The classic presentation is of crops of vesicles or bullae that erupt bilaterally on the palms and the lateral aspects of the fingers. The vesicles may coalesce over time to form multiloculated bullae. Most cases involve the hands alone (cheiropompholyx), but roughly 10% of patients have lesions on both the hands and feet, and another 10% have lesions on just the feet (podopompholyx).\nThe lesions may be intensely pruritic, leading to secondary desquamation and erosions and ulcerations from scratching. Dyshidrotic eczema developing near the tips of the fingers or toes may lead to dystrophic changes of the nails. Cellulitis, lymphangitis, or infection of the lesions themselves may all develop with the long-standing presence of lesions and/or poor hygiene. The vesicular crops usually resolve spontaneously after 3-4 weeks, leaving behind collarettes of scale. Although self-limited, outbreaks frequently alternate with disease-free intervals of weeks to months and, if severe, may be extremely disabling.[1]\nThe differential diagnosis includes immunobullous disorders, such as bullous pemphigoid and pemphigus vulgaris, or other dermatoses, such as contact dermatitis, herpes simplex virus infection, bullous tinea pedis, and pustular psoriasis. The diagnosis is usually made on the basis of the clinical history, the physical examination, and the exclusion of alternative diagnoses. Bacterial culture and sensitivities may be evaluated for secondary infections.\nAdditionally, potassium hydroxide wet mount preparations may be useful for excluding dermatophyte infections. A skin biopsy may also be useful for confirming the clinical impression in unresponsive cases and for excluding alternative diagnoses. It can be difficult to differentiate dyshidrotic eczema from an id reaction (autoeczematization), which is a cutaneous eruption that develops in response to various infectious and inflammatory stimuli at a distant site from the primary dermatosis.[1]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "PCP Case Challenge: Lesions on the Hands, Palms, and Feet of a 57-Year-Old Man"
},
{
"authors": "Lars Grimm, MD",
"content": [
"Treatment for dyshidrotic eczema begins with topical corticosteroid therapy; topical class I steroids are the first-line treatment regimen, with oral steroids reserved for more severe cases. Large lesions should be drained, but not unroofed, to prevent subsequent infection. The patient should make appropriate modifications to daily activities and should avoid scratching to limit unwarranted skin irritation, exacerbation, and subsequent infection.",
"In addition, numerous adjuvant therapies are available, such as ultraviolet light, botulinum toxin occlusive dressings, and immunosuppressive agents, which may be helpful on a case-by-case basis for refractory patients. Unfortunately, no preventive therapy is available other than avoidance in patients with well-established triggers. Untreated dyshidrotic eczema can lead to concomitant infections; therefore, prompt detection and treatment are essential.",
"In this case, one of the bullae, measuring approximately 3 cm x 1.5 cm, was percutaneously drained with a 10-cc syringe. Approximately 3 mL of a clear fluid was aspirated. The roof of the vesicle was left intact. To confirm the diagnosis and exclude alternative diagnoses, a punch biopsy of the skin was performed from the foot (Figures 1-3).",
"Figure 1.",
"Figure 1.",
"Figure 2.",
"Figure 2.",
"Figure 3.",
"Figure 3.",
"Histologically, spongiotic dermatitis and an intraepidermal vesicle were present, which were consistent with the diagnosis of dyshidrotic eczema. A periodic acid-Schiff stain performed on this specimen did not reveal any fungal elements; scrapings of skin from the feet were negative for fungal infection as well.",
"The patient was instructed to begin a regimen of topical steroids and moisturizing emollient as well as wet compresses. An over-the-counter moisturizer was recommended, and prescriptions for Burrow's solution (10% aluminum acetate) and clobetasol propionate were written. At a follow-up visit, the patient underwent patch testing, but a causative contact allergen was not identified."
],
"date": "April 20, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/847/158/847158-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/847/158/847158-Thumb2.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/847/158/847158-Thumb3.png"
}
],
"markdown": "# PCP Case Challenge: Lesions on the Hands, Palms, and Feet of a 57-Year-Old Man\n\n **Authors:** Lars Grimm, MD \n **Date:** April 20, 2022\n\n ## Content\n\n Treatment for dyshidrotic eczema begins with topical corticosteroid therapy; topical class I steroids are the first-line treatment regimen, with oral steroids reserved for more severe cases. Large lesions should be drained, but not unroofed, to prevent subsequent infection. The patient should make appropriate modifications to daily activities and should avoid scratching to limit unwarranted skin irritation, exacerbation, and subsequent infection.\nIn addition, numerous adjuvant therapies are available, such as ultraviolet light, botulinum toxin occlusive dressings, and immunosuppressive agents, which may be helpful on a case-by-case basis for refractory patients. Unfortunately, no preventive therapy is available other than avoidance in patients with well-established triggers. Untreated dyshidrotic eczema can lead to concomitant infections; therefore, prompt detection and treatment are essential.\nIn this case, one of the bullae, measuring approximately 3 cm x 1.5 cm, was percutaneously drained with a 10-cc syringe. Approximately 3 mL of a clear fluid was aspirated. The roof of the vesicle was left intact. To confirm the diagnosis and exclude alternative diagnoses, a punch biopsy of the skin was performed from the foot (Figures 1-3).\nFigure 1.\nFigure 1.\nFigure 2.\nFigure 2.\nFigure 3.\nFigure 3.\nHistologically, spongiotic dermatitis and an intraepidermal vesicle were present, which were consistent with the diagnosis of dyshidrotic eczema. A periodic acid-Schiff stain performed on this specimen did not reveal any fungal elements; scrapings of skin from the feet were negative for fungal infection as well.\nThe patient was instructed to begin a regimen of topical steroids and moisturizing emollient as well as wet compresses. An over-the-counter moisturizer was recommended, and prescriptions for Burrow's solution (10% aluminum acetate) and clobetasol propionate were written. At a follow-up visit, the patient underwent patch testing, but a causative contact allergen was not identified.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n\n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 867293,
"choiceText": "Nickel allergy",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867295,
"choiceText": "IVIg therapy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867297,
"choiceText": "Emotional stress",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867299,
"choiceText": "Tinea pedis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867301,
"choiceText": "Person-to-person contact",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The exact etiology of dyshidrotic eczema is not completely understood; however, studies have elucidated associations with contact allergens (notably nickel), IVIg therapy, emotional stress, and concomitant tinea pedis infection. Unfortunately, in many cases, the causative agent is not discovered. No evidence suggests person-to-person transmission.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 272845,
"questionText": "Dyshidrotic eczema is frequently idiopathic. Which is <i>not</i> well-supported as a cause of dyshidrotic eczema?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 867303,
"choiceText": "Mouth",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867305,
"choiceText": "Hands",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867307,
"choiceText": "Feet",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867309,
"choiceText": "Hands and feet",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867311,
"choiceText": "Trunk",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Approximately 80% of cases of dyshidrotic eczema are localized to the hands only; 10% of cases are limited to the feet only; and 10% include both the hands and the feet, as in the patient in this case. Vesicles are rarely found elsewhere on the body.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 272847,
"questionText": "Which is the most common anatomic location for the presentation of dyshidrotic eczema?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "PCP Case Challenge: Lesions on the Hands, Palms, and Feet of a 57-Year-Old Man"
},
{
"authors": "Lars Grimm, MD",
"content": [],
"date": "April 20, 2022",
"figures": [],
"markdown": "# PCP Case Challenge: Lesions on the Hands, Palms, and Feet of a 57-Year-Old Man\n\n **Authors:** Lars Grimm, MD \n **Date:** April 20, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 867293,
"choiceText": "Nickel allergy",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867295,
"choiceText": "IVIg therapy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867297,
"choiceText": "Emotional stress",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867299,
"choiceText": "Tinea pedis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867301,
"choiceText": "Person-to-person contact",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The exact etiology of dyshidrotic eczema is not completely understood; however, studies have elucidated associations with contact allergens (notably nickel), IVIg therapy, emotional stress, and concomitant tinea pedis infection. Unfortunately, in many cases, the causative agent is not discovered. No evidence suggests person-to-person transmission.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 272845,
"questionText": "Dyshidrotic eczema is frequently idiopathic. Which is <i>not</i> well-supported as a cause of dyshidrotic eczema?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 867303,
"choiceText": "Mouth",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867305,
"choiceText": "Hands",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867307,
"choiceText": "Feet",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867309,
"choiceText": "Hands and feet",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867311,
"choiceText": "Trunk",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Approximately 80% of cases of dyshidrotic eczema are localized to the hands only; 10% of cases are limited to the feet only; and 10% include both the hands and the feet, as in the patient in this case. Vesicles are rarely found elsewhere on the body.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 272847,
"questionText": "Which is the most common anatomic location for the presentation of dyshidrotic eczema?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "PCP Case Challenge: Lesions on the Hands, Palms, and Feet of a 57-Year-Old Man"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 867285,
"choiceText": "Allergic contact dermatitis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867287,
"choiceText": "Herpes simplex",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867289,
"choiceText": "Impetigo",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867291,
"choiceText": "Dyshidrotic eczema",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 272843,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 867293,
"choiceText": "Nickel allergy",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867295,
"choiceText": "IVIg therapy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867297,
"choiceText": "Emotional stress",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867299,
"choiceText": "Tinea pedis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867301,
"choiceText": "Person-to-person contact",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The exact etiology of dyshidrotic eczema is not completely understood; however, studies have elucidated associations with contact allergens (notably nickel), IVIg therapy, emotional stress, and concomitant tinea pedis infection. Unfortunately, in many cases, the causative agent is not discovered. No evidence suggests person-to-person transmission.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 272845,
"questionText": "Dyshidrotic eczema is frequently idiopathic. Which is <i>not</i> well-supported as a cause of dyshidrotic eczema?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 867303,
"choiceText": "Mouth",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867305,
"choiceText": "Hands",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867307,
"choiceText": "Feet",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867309,
"choiceText": "Hands and feet",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 867311,
"choiceText": "Trunk",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Approximately 80% of cases of dyshidrotic eczema are localized to the hands only; 10% of cases are limited to the feet only; and 10% include both the hands and the feet, as in the patient in this case. Vesicles are rarely found elsewhere on the body.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 272847,
"questionText": "Which is the most common anatomic location for the presentation of dyshidrotic eczema?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
972301 | /viewarticle/972301 | [
{
"authors": "Jennifer Wachala, DO; Dushyant Singh Dahiya, MD; Farah Wani, MD; Asim Kichloo, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 54-year-old woman presents to the emergency department (ED) with a 5-day history of worsening diarrhea and weakness. Her past medical history includes well-controlled type 2 diabetes, gastroesophageal reflux disease (GERD), lymphoma, anxiety, and depression.",
"The patient describes the diarrhea as three or four loose, watery bowel movements per day. She has no abdominal pain, nausea, vomiting, hematemesis, hematochezia, or stool incontinence. She also reports no recent changes in diet or appetite, changes in weight, changes in medication, recent illness, or travel. She has been taking a psyllium fiber supplement (Metamucil) for 5 days without improvement in her symptoms.",
"In addition, she reports generalized weakness, which started at about the same time as the diarrhea. She is usually able to take her dogs on a 2-mile walk after work. During the past week, however, she has struggled to walk even half a mile. She has not had any recent falls.",
"She also reports palpitations that last a few seconds, which she attributes to her anxiety. She has an occasional productive cough with clear phlegm, which she attributes to chronic postnasal drip. She reports no fever, chills, night sweats, lightheadedness, dizziness, changes in vision, nasal congestion, rhinorrhea, sore throat, chest discomfort, shortness of breath, tremors, or urinary symptoms.",
"The patient works as a nurse in an elementary school. She reports sick contacts, without significant exposure. However, about a week ago, three students and one staff member tested positive for SARS-CoV-2 at the school. The patient underwent a COVID-19 rapid antigen test immediately after the students and staff member tested positive, and her result was negative. She was vaccinated with two doses of the COVID-19 vaccine in 2021 but has not yet received her booster dose.",
"She lives in a private home with her husband and two dogs. She does not use tobacco products or illicit drugs. She drinks alcohol on occasion.",
"She reports no recent hospitalizations. Her surgical history is positive for an appendectomy and an open reduction and internal fixation of the right ankle after a traumatic fracture. She has no significant family history. She is highly adherent to metformin therapy, and her A1c level was 5.8% about 4 months ago. Her childhood lymphoma has been in remission for the past 40 years. She takes omeprazole for GERD and attends monthly counseling sessions for her anxiety and depression. She follows up with her primary care provider every 6 months and is up to date on all routine health screening tests for her age, including colonoscopy at age 50 years, which was normal."
],
"date": "April 19, 2022",
"figures": [],
"markdown": "# A School Nurse With Anxiety, Diarrhea, Palpitations, and Cough\n\n **Authors:** Jennifer Wachala, DO; Dushyant Singh Dahiya, MD; Farah Wani, MD; Asim Kichloo, MD \n **Date:** April 19, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 54-year-old woman presents to the emergency department (ED) with a 5-day history of worsening diarrhea and weakness. Her past medical history includes well-controlled type 2 diabetes, gastroesophageal reflux disease (GERD), lymphoma, anxiety, and depression.\nThe patient describes the diarrhea as three or four loose, watery bowel movements per day. She has no abdominal pain, nausea, vomiting, hematemesis, hematochezia, or stool incontinence. She also reports no recent changes in diet or appetite, changes in weight, changes in medication, recent illness, or travel. She has been taking a psyllium fiber supplement (Metamucil) for 5 days without improvement in her symptoms.\nIn addition, she reports generalized weakness, which started at about the same time as the diarrhea. She is usually able to take her dogs on a 2-mile walk after work. During the past week, however, she has struggled to walk even half a mile. She has not had any recent falls.\nShe also reports palpitations that last a few seconds, which she attributes to her anxiety. She has an occasional productive cough with clear phlegm, which she attributes to chronic postnasal drip. She reports no fever, chills, night sweats, lightheadedness, dizziness, changes in vision, nasal congestion, rhinorrhea, sore throat, chest discomfort, shortness of breath, tremors, or urinary symptoms.\nThe patient works as a nurse in an elementary school. She reports sick contacts, without significant exposure. However, about a week ago, three students and one staff member tested positive for SARS-CoV-2 at the school. The patient underwent a COVID-19 rapid antigen test immediately after the students and staff member tested positive, and her result was negative. She was vaccinated with two doses of the COVID-19 vaccine in 2021 but has not yet received her booster dose.\nShe lives in a private home with her husband and two dogs. She does not use tobacco products or illicit drugs. She drinks alcohol on occasion.\nShe reports no recent hospitalizations. Her surgical history is positive for an appendectomy and an open reduction and internal fixation of the right ankle after a traumatic fracture. She has no significant family history. She is highly adherent to metformin therapy, and her A1c level was 5.8% about 4 months ago. Her childhood lymphoma has been in remission for the past 40 years. She takes omeprazole for GERD and attends monthly counseling sessions for her anxiety and depression. She follows up with her primary care provider every 6 months and is up to date on all routine health screening tests for her age, including colonoscopy at age 50 years, which was normal.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A School Nurse With Anxiety, Diarrhea, Palpitations, and Cough"
},
{
"authors": "Jennifer Wachala, DO; Dushyant Singh Dahiya, MD; Farah Wani, MD; Asim Kichloo, MD",
"content": [
"Upon examination, the patient appears comfortable and is in no acute distress. Her mucous membranes and skin are dry. She has a temperature of 99.8 °F (37.7 °C), a heart rate of 118 beats/min, a blood pressure of 139/82 mm Hg, and a respiration rate of 20 breaths/min, with an oxygen saturation of 95% on room air. Her body mass index is 29.",
"Her neck is supple, and no thyromegaly or lymphadenopathy is noted. The cardiac examination reveals a regular rate, tachycardia, and normal S1 and S2 heart sounds, without murmurs, rubs, or gallops. The lungs are clear to auscultation bilaterally, and no wheezing, rales, or rhonchi are detected. The abdominal examination reveals moderate tenderness with deep palpation in the right and left lower quadrants and diffuse hyperactive bowel sounds. No masses or hernia, abdominal distention, or hepatosplenomegaly is noted. The neurologic examination reveals 5/5 strength in all extremities, intact sensations, and no deficits in cranial nerves III-XII.",
"Laboratory investigations show the following values:",
"Hemoglobin level: 12 g/dL (reference range, 12-16 g/dL)",
"Hematocrit: 40% (reference range, 36%-46%)",
"Platelet count: 352 × 103 cells/µL (reference range, 150-400 × 103 cells/µL)",
"White blood cell count: 4000 cells/µL (reference range, 4000-11,000 cells/µL) with 74% neutrophils (reference range, 55%-70%)",
"Results of a basic metabolic panel are as follows:",
"Sodium level: 133 mmol/L (reference range, 135-147 mmol/L)",
"Potassium level: 3.4 mmol/L (reference range, 3.5-5.0 mmol/L)",
"Chloride level: 92 mmol/L (reference range, 98-106 mmol/L)",
"Bicarbonate level: 38 mmol/L (reference range, 22-30 mmol/L)",
"Blood urea nitrogen level: 38 mg/dL (reference range, 8-21 mg/dL)",
"Creatinine level: 0.87 mg/dL (reference range, 0.5-1.1 mg/dL)",
"Fasting glucose level: 112 mg/dL (reference range, 70-100 mg/dL)",
"Magnesium level: 1.7 mmol/L (reference range, 0.65-1.05 mmol/L)",
"Liver function test results are within normal limits. The D-dimer level is 260 ng/mL (reference range, < 250 ng/mL); the ferritin level is 500 µg/L (reference range, 11-307 µg/L); and the C-reactive protein level is 1.20 mg/L (reference range, 0-10 mg/L). An ECG demonstrates sinus rhythm, with a heart rate of 120 beats/min and a QTc of 359 msec. A chest radiograph is obtained. The findings are similar to those shown in the Figure. CT of the abdomen and pelvis is also performed, and the results are pending.",
"Figure 1."
],
"date": "April 19, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/972/301/972301-Thumb1.png"
}
],
"markdown": "# A School Nurse With Anxiety, Diarrhea, Palpitations, and Cough\n\n **Authors:** Jennifer Wachala, DO; Dushyant Singh Dahiya, MD; Farah Wani, MD; Asim Kichloo, MD \n **Date:** April 19, 2022\n\n ## Content\n\n Upon examination, the patient appears comfortable and is in no acute distress. Her mucous membranes and skin are dry. She has a temperature of 99.8 °F (37.7 °C), a heart rate of 118 beats/min, a blood pressure of 139/82 mm Hg, and a respiration rate of 20 breaths/min, with an oxygen saturation of 95% on room air. Her body mass index is 29.\nHer neck is supple, and no thyromegaly or lymphadenopathy is noted. The cardiac examination reveals a regular rate, tachycardia, and normal S1 and S2 heart sounds, without murmurs, rubs, or gallops. The lungs are clear to auscultation bilaterally, and no wheezing, rales, or rhonchi are detected. The abdominal examination reveals moderate tenderness with deep palpation in the right and left lower quadrants and diffuse hyperactive bowel sounds. No masses or hernia, abdominal distention, or hepatosplenomegaly is noted. The neurologic examination reveals 5/5 strength in all extremities, intact sensations, and no deficits in cranial nerves III-XII.\nLaboratory investigations show the following values:\nHemoglobin level: 12 g/dL (reference range, 12-16 g/dL)\nHematocrit: 40% (reference range, 36%-46%)\nPlatelet count: 352 × 103 cells/µL (reference range, 150-400 × 103 cells/µL)\nWhite blood cell count: 4000 cells/µL (reference range, 4000-11,000 cells/µL) with 74% neutrophils (reference range, 55%-70%)\nResults of a basic metabolic panel are as follows:\nSodium level: 133 mmol/L (reference range, 135-147 mmol/L)\nPotassium level: 3.4 mmol/L (reference range, 3.5-5.0 mmol/L)\nChloride level: 92 mmol/L (reference range, 98-106 mmol/L)\nBicarbonate level: 38 mmol/L (reference range, 22-30 mmol/L)\nBlood urea nitrogen level: 38 mg/dL (reference range, 8-21 mg/dL)\nCreatinine level: 0.87 mg/dL (reference range, 0.5-1.1 mg/dL)\nFasting glucose level: 112 mg/dL (reference range, 70-100 mg/dL)\nMagnesium level: 1.7 mmol/L (reference range, 0.65-1.05 mmol/L)\nLiver function test results are within normal limits. The D-dimer level is 260 ng/mL (reference range, < 250 ng/mL); the ferritin level is 500 µg/L (reference range, 11-307 µg/L); and the C-reactive protein level is 1.20 mg/L (reference range, 0-10 mg/L). An ECG demonstrates sinus rhythm, with a heart rate of 120 beats/min and a QTc of 359 msec. A chest radiograph is obtained. The findings are similar to those shown in the Figure. CT of the abdomen and pelvis is also performed, and the results are pending.\nFigure 1.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1680826,
"choiceText": "<i>Clostridioides difficile</i> colitis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680827,
"choiceText": "Hyperthyroidism",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680828,
"choiceText": "Reactivation of lymphoma",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680829,
"choiceText": "Colon adenocarcinoma",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680830,
"choiceText": "SARS-CoV-2 infection",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 541511,
"questionText": "On the basis of these findings only, what is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A School Nurse With Anxiety, Diarrhea, Palpitations, and Cough"
},
{
"authors": "Jennifer Wachala, DO; Dushyant Singh Dahiya, MD; Farah Wani, MD; Asim Kichloo, MD",
"content": [
"The patient's clinical presentation of acute diarrhea, generalized weakness, tachycardia, mildly elevated D-dimer level, and recent exposure to sick contacts with SARS-CoV-2 infection raises suspicion of COVID-19. Her chest radiograph shows no lymphadenopathy, masses, opacities, or consolidations. She is most likely exhibiting gastrointestinal manifestations of infection with the Omicron variant of SARS-CoV-2.",
"Upon further questioning, the patient confirms that she has had no increase in appetite or unintentional weight changes and reports no skin changes, including diaphoresis, or heat intolerance. Results of thyroid function tests are within normal limits. In addition, despite a change in the quality and frequency of bowel movements, the patient reports no change in odor. She denies recent antibiotic use, recent hospitalization, or a prior history of C difficile colitis. The CT scan of the abdomen and pelvis did not show lymphadenopathy, colonic wall thickening, fat stranding, or other acute pathology.",
"For patients who present with diarrhea, a review of their medical history to assess susceptibility to other diseases is essential. The patient in this case is immunocompromised and is receiving long-term proton pump inhibitor therapy. These factors, in addition to her history of three or more bowel movements per day for more than 2 consecutive days, raise suspicion of C difficile colitis. However, she did not complain of additional abdominal symptoms, such as pain; stool testing for C difficile was negative; and the imaging studies showed no structural changes associated with C difficile colitis.",
"The patient's palpitations and tachycardia, coupled with new-onset diarrhea, raise concern for hyperthyroidism. This diagnosis is less likely given the chronicity of her symptoms, absence of change from baseline, and negative history and examination findings. In addition, she was not found to have depressed thyroid-stimulating hormone, elevated triiodothyronine, or elevated thyroxine levels.",
"She had a recent colonoscopy at age 50 years and has not had unintentional weight loss or hematochezia; thus, suspicion for colon adenocarcinoma is low. Finally, owing to the absence of lymphadenopathy and hepatosplenomegaly on both examination and imaging, and the lack of early satiety, fever, or night sweats, lymphoma reactivation seems unlikely. In this case, the patient's presentation is best explained by gastrointestinal complications of COVID-19 caused by the Omicron variant."
],
"date": "April 19, 2022",
"figures": [],
"markdown": "# A School Nurse With Anxiety, Diarrhea, Palpitations, and Cough\n\n **Authors:** Jennifer Wachala, DO; Dushyant Singh Dahiya, MD; Farah Wani, MD; Asim Kichloo, MD \n **Date:** April 19, 2022\n\n ## Content\n\n The patient's clinical presentation of acute diarrhea, generalized weakness, tachycardia, mildly elevated D-dimer level, and recent exposure to sick contacts with SARS-CoV-2 infection raises suspicion of COVID-19. Her chest radiograph shows no lymphadenopathy, masses, opacities, or consolidations. She is most likely exhibiting gastrointestinal manifestations of infection with the Omicron variant of SARS-CoV-2.\nUpon further questioning, the patient confirms that she has had no increase in appetite or unintentional weight changes and reports no skin changes, including diaphoresis, or heat intolerance. Results of thyroid function tests are within normal limits. In addition, despite a change in the quality and frequency of bowel movements, the patient reports no change in odor. She denies recent antibiotic use, recent hospitalization, or a prior history of C difficile colitis. The CT scan of the abdomen and pelvis did not show lymphadenopathy, colonic wall thickening, fat stranding, or other acute pathology.\nFor patients who present with diarrhea, a review of their medical history to assess susceptibility to other diseases is essential. The patient in this case is immunocompromised and is receiving long-term proton pump inhibitor therapy. These factors, in addition to her history of three or more bowel movements per day for more than 2 consecutive days, raise suspicion of C difficile colitis. However, she did not complain of additional abdominal symptoms, such as pain; stool testing for C difficile was negative; and the imaging studies showed no structural changes associated with C difficile colitis.\nThe patient's palpitations and tachycardia, coupled with new-onset diarrhea, raise concern for hyperthyroidism. This diagnosis is less likely given the chronicity of her symptoms, absence of change from baseline, and negative history and examination findings. In addition, she was not found to have depressed thyroid-stimulating hormone, elevated triiodothyronine, or elevated thyroxine levels.\nShe had a recent colonoscopy at age 50 years and has not had unintentional weight loss or hematochezia; thus, suspicion for colon adenocarcinoma is low. Finally, owing to the absence of lymphadenopathy and hepatosplenomegaly on both examination and imaging, and the lack of early satiety, fever, or night sweats, lymphoma reactivation seems unlikely. In this case, the patient's presentation is best explained by gastrointestinal complications of COVID-19 caused by the Omicron variant.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1680826,
"choiceText": "<i>Clostridioides difficile</i> colitis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680827,
"choiceText": "Hyperthyroidism",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680828,
"choiceText": "Reactivation of lymphoma",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680829,
"choiceText": "Colon adenocarcinoma",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680830,
"choiceText": "SARS-CoV-2 infection",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 541511,
"questionText": "On the basis of these findings only, what is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A School Nurse With Anxiety, Diarrhea, Palpitations, and Cough"
},
{
"authors": "Jennifer Wachala, DO; Dushyant Singh Dahiya, MD; Farah Wani, MD; Asim Kichloo, MD",
"content": [
"COVID-19 was first recognized in 2019. Since then, it has undergone numerous gene mutations resulting in variants of concern, including Omicron, which was first reported in the United States in December 2021. Omicron has greater transmissibility and immune evasion than previous variants and the ancestral strain, regardless of an individual's vaccination status.[1] Further observation is needed to fully determine hospitalization and mortality rates; however, despite its apparent lower risk for severe disease and fatality, the overall risk for infection remains high.",
"Patients with COVID-19 caused by the Omicron variant may present with fever, chills, fatigue, headache, anosmia, nasal congestion or rhinorrhea, pharyngitis, cough, dyspnea, or myalgia. Occasionally, patients have gastrointestinal involvement, including dysgeusia, diarrhea, nausea, vomiting, abdominal pain, and diminished appetite.[2] Although some COVID-19 variants are associated with prolonged viral shedding in the gastrointestinal tract and the virus is detectable in waste water, whether fecal-oral transmission is a significant mode of transmission remains unclear.[2]",
"Symptom severity varies, ranging from asymptomatic to mild, moderate, severe, or critical illness.[3] Patients with increased viral load or underlying comorbidities, such as diabetes, cardiovascular disease, obesity, or immunosuppression, are at increased risk for worse disease or delayed recovery.[2] COVID-19 is also linked to leukopenia or leukocytosis with lymphopenia, as well as elevation of inflammatory markers, such as ferritin, lactate dehydrogenase, and C-reactive protein.[2] Furthermore, owing to liver involvement, liver enzyme levels may also be elevated.[2]",
"In patients with suspected COVID-19, rapid antigen detection tests (RADTs) and real-time reverse-transcriptase polymerase chain reaction (rRT-PCR) are the most common diagnostic tests. According to the Centers for Disease Control and Prevention guidelines, suspicion of COVID-19 is low in persons without close contact exposure within the past 14 days, who have full vaccination status, or who have had COVID-19 within the past 3 months. Suspicion of COVID-19 is high in persons with known close contact exposure within the past 14 days, an incomplete vaccination series, and an absence of COVID-19 infection within the past 3 months. [4] The initial COVID-19 test for both asymptomatic and symptomatic patients in the community setting is RADT, with rRT-PCR recommended as a follow-up confirmatory test if suspicion of COVID-19 remains high.[4]",
"COVID-19 RADT is the most common and commercially available test and is typically performed with nasal, nasopharyngeal, or saliva specimens in point-of-care settings. It can detect viral antigens in high viral loads of active COVID-19 and can allow for faster diagnosis, isolation, and therapy initiation.[4,5]",
"COVID-19 rRT-PCR is the criterion standard test for COVID-19 diagnosis and is typically performed with nasal and nasopharyngeal specimens. It uses nucleic acid amplification testing to detect and measure viral RNA despite viral load and can complete whole-genome sequencing to determine variant lineage.[5,6]",
"The diagnostic accuracy of RADTs for the detection of COVID-19 variants is concerning, given the emergence of gene-sequencing mutations. Most notably, false-negative results and decreased sensitivity for the detection of vaccine-breakthrough Omicron variant have been investigated.[5] In fully vaccinated, COVID-19–naive patients with new-onset symptoms, the specificity (100%) and sensitivity (81.8%) of RADTs are dependent on a greater viral load and specimen collection within 0-1 days of symptom onset.[5,6] Furthermore, evidence suggests that RADTs have a significant increase in sensitivity with increasing viral loads.[5]Oral cheek (9% sensitivity) and tonsillar (46.9% sensitivity) specimens have been reported to be less reliable than nasal swab (85.7% sensitivity) specimens.[4] Of note, RADTs manufactured by different companies have different sensitivities and results. Therefore, further studies are needed to compare diagnostic accuracy among these tests.",
"rRT-PCR consistently produces better viral load measurements and is more sensitive than RADT, despite the time of specimen collection.[6] Nasopharyngeal swab remains the ideal specimen collection site for COVID-19 detection. In the patient in this case, who had gastrointestinal manifestations of COVID-19, rRT-PCR is the recommended test; it may detect viral particles in feces despite a negative result in a nasopharyngeal specimen from the respiratory tract.[2]"
],
"date": "April 19, 2022",
"figures": [],
"markdown": "# A School Nurse With Anxiety, Diarrhea, Palpitations, and Cough\n\n **Authors:** Jennifer Wachala, DO; Dushyant Singh Dahiya, MD; Farah Wani, MD; Asim Kichloo, MD \n **Date:** April 19, 2022\n\n ## Content\n\n COVID-19 was first recognized in 2019. Since then, it has undergone numerous gene mutations resulting in variants of concern, including Omicron, which was first reported in the United States in December 2021. Omicron has greater transmissibility and immune evasion than previous variants and the ancestral strain, regardless of an individual's vaccination status.[1] Further observation is needed to fully determine hospitalization and mortality rates; however, despite its apparent lower risk for severe disease and fatality, the overall risk for infection remains high.\nPatients with COVID-19 caused by the Omicron variant may present with fever, chills, fatigue, headache, anosmia, nasal congestion or rhinorrhea, pharyngitis, cough, dyspnea, or myalgia. Occasionally, patients have gastrointestinal involvement, including dysgeusia, diarrhea, nausea, vomiting, abdominal pain, and diminished appetite.[2] Although some COVID-19 variants are associated with prolonged viral shedding in the gastrointestinal tract and the virus is detectable in waste water, whether fecal-oral transmission is a significant mode of transmission remains unclear.[2]\nSymptom severity varies, ranging from asymptomatic to mild, moderate, severe, or critical illness.[3] Patients with increased viral load or underlying comorbidities, such as diabetes, cardiovascular disease, obesity, or immunosuppression, are at increased risk for worse disease or delayed recovery.[2] COVID-19 is also linked to leukopenia or leukocytosis with lymphopenia, as well as elevation of inflammatory markers, such as ferritin, lactate dehydrogenase, and C-reactive protein.[2] Furthermore, owing to liver involvement, liver enzyme levels may also be elevated.[2]\nIn patients with suspected COVID-19, rapid antigen detection tests (RADTs) and real-time reverse-transcriptase polymerase chain reaction (rRT-PCR) are the most common diagnostic tests. According to the Centers for Disease Control and Prevention guidelines, suspicion of COVID-19 is low in persons without close contact exposure within the past 14 days, who have full vaccination status, or who have had COVID-19 within the past 3 months. Suspicion of COVID-19 is high in persons with known close contact exposure within the past 14 days, an incomplete vaccination series, and an absence of COVID-19 infection within the past 3 months. [4] The initial COVID-19 test for both asymptomatic and symptomatic patients in the community setting is RADT, with rRT-PCR recommended as a follow-up confirmatory test if suspicion of COVID-19 remains high.[4]\nCOVID-19 RADT is the most common and commercially available test and is typically performed with nasal, nasopharyngeal, or saliva specimens in point-of-care settings. It can detect viral antigens in high viral loads of active COVID-19 and can allow for faster diagnosis, isolation, and therapy initiation.[4,5]\nCOVID-19 rRT-PCR is the criterion standard test for COVID-19 diagnosis and is typically performed with nasal and nasopharyngeal specimens. It uses nucleic acid amplification testing to detect and measure viral RNA despite viral load and can complete whole-genome sequencing to determine variant lineage.[5,6]\nThe diagnostic accuracy of RADTs for the detection of COVID-19 variants is concerning, given the emergence of gene-sequencing mutations. Most notably, false-negative results and decreased sensitivity for the detection of vaccine-breakthrough Omicron variant have been investigated.[5] In fully vaccinated, COVID-19–naive patients with new-onset symptoms, the specificity (100%) and sensitivity (81.8%) of RADTs are dependent on a greater viral load and specimen collection within 0-1 days of symptom onset.[5,6] Furthermore, evidence suggests that RADTs have a significant increase in sensitivity with increasing viral loads.[5]Oral cheek (9% sensitivity) and tonsillar (46.9% sensitivity) specimens have been reported to be less reliable than nasal swab (85.7% sensitivity) specimens.[4] Of note, RADTs manufactured by different companies have different sensitivities and results. Therefore, further studies are needed to compare diagnostic accuracy among these tests.\nrRT-PCR consistently produces better viral load measurements and is more sensitive than RADT, despite the time of specimen collection.[6] Nasopharyngeal swab remains the ideal specimen collection site for COVID-19 detection. In the patient in this case, who had gastrointestinal manifestations of COVID-19, rRT-PCR is the recommended test; it may detect viral particles in feces despite a negative result in a nasopharyngeal specimen from the respiratory tract.[2]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A School Nurse With Anxiety, Diarrhea, Palpitations, and Cough"
},
{
"authors": "Jennifer Wachala, DO; Dushyant Singh Dahiya, MD; Farah Wani, MD; Asim Kichloo, MD",
"content": [
"The management of COVID-19 is dynamic and changes as new variants emerge. Thus far, Omicron has the greatest number of gene mutations. It is unaffected by most therapeutic antibodies and effectively evades humoral immunity gained from prior infection or vaccination.[7] Thus, new therapies and adjusted protocols have been adopted.[7,8,9]",
"Sotrovimab is a monoclonal antibody administered as a 1-hour outpatient intravenous infusion within 10 days of mild or moderate symptom onset in patients at high risk for severe COVID-19 progression. A 1-hour observation period after the infusion is required to ensure good tolerance. The US Food and Drug Administration has updated the emergency use authorization for sotrovimab, which is no longer authorized to treat COVID-19 in any US region owing to the Omicron BA.2 subvariant.[10]",
"Remdesivir is a broad-spectrum antiviral that requires intravenous infusion for 3-5 consecutive days within 7 days of mild or moderate symptom onset in patients at high risk for severe COVID-19 progression. It can be administered in an outpatient or inpatient setting, depending on symptom severity and patient feasibility. In an inpatient setting, remdesivir and dexamethasone are recommended for those who require supplemental oxygen.",
"Baricitinib and dexamethasone can be administered, in addition to remdesivir, to patients with rapidly worsening hypoxia and systemic inflammation. This inpatient Janus kinase (JAK1/JAK2) inhibitor and corticosteroid combination therapy is discontinued at discharge.",
"Tocilizumab and dexamethasone can be administered, in addition to remdesivir, within 24 hours of admission to an intensive care unit (ICU) for COVID-19 complications. This inpatient monoclonal antibody and corticosteroid combination therapy is discontinued at discharge.",
"In patients who require oxygen supplementation, dexamethasone should be stopped after 10 days to prevent adverse events from prolonged corticosteroid use.[8,9] Baricitinib is administered orally and may be continued for up to 14 days with renal dosing adjustments.[8,9] Tocilizumab inhibits interleukin-6 and is a single-dose intravenous infusion; a second dose may be given 8 hours later if there is no appreciable clinical improvement.[8,9] In addition, supportive care and prevention of further transmission with a 5-day isolation followed by wearing a mask for the next 5 days are recommended for all symptomatic patients found to be positive for the COVID-19 Omicron variant.",
"The patient in this case was admitted for correction of her electrolyte abnormalities and fluid resuscitation. She was also found to be positive for COVID-19 by rRT-PCR and received remdesivir. She was placed on isolation precautions. The hematology/oncology service was consulted regarding the patient's history of lymphoma and current lymphopenia, and no further intervention was recommended because her abnormal white blood cell count was attributed to COVID-19. Throughout her hospitalization, she received a consistent carbohydrate diet and sliding-scale insulin for diabetes management. Upon discharge, she was scheduled for outpatient follow-up with her primary care provider.",
"Editor's Note: The discussion in this Case Challenge applies to COVID-19 diagnosis and treatment recommendations as of April 19, 2022. This scenario will not be regularly updated, and users are encouraged to find the latest information in Medscape's COVID-19 Resource Center."
],
"date": "April 19, 2022",
"figures": [],
"markdown": "# A School Nurse With Anxiety, Diarrhea, Palpitations, and Cough\n\n **Authors:** Jennifer Wachala, DO; Dushyant Singh Dahiya, MD; Farah Wani, MD; Asim Kichloo, MD \n **Date:** April 19, 2022\n\n ## Content\n\n The management of COVID-19 is dynamic and changes as new variants emerge. Thus far, Omicron has the greatest number of gene mutations. It is unaffected by most therapeutic antibodies and effectively evades humoral immunity gained from prior infection or vaccination.[7] Thus, new therapies and adjusted protocols have been adopted.[7,8,9]\nSotrovimab is a monoclonal antibody administered as a 1-hour outpatient intravenous infusion within 10 days of mild or moderate symptom onset in patients at high risk for severe COVID-19 progression. A 1-hour observation period after the infusion is required to ensure good tolerance. The US Food and Drug Administration has updated the emergency use authorization for sotrovimab, which is no longer authorized to treat COVID-19 in any US region owing to the Omicron BA.2 subvariant.[10]\nRemdesivir is a broad-spectrum antiviral that requires intravenous infusion for 3-5 consecutive days within 7 days of mild or moderate symptom onset in patients at high risk for severe COVID-19 progression. It can be administered in an outpatient or inpatient setting, depending on symptom severity and patient feasibility. In an inpatient setting, remdesivir and dexamethasone are recommended for those who require supplemental oxygen.\nBaricitinib and dexamethasone can be administered, in addition to remdesivir, to patients with rapidly worsening hypoxia and systemic inflammation. This inpatient Janus kinase (JAK1/JAK2) inhibitor and corticosteroid combination therapy is discontinued at discharge.\nTocilizumab and dexamethasone can be administered, in addition to remdesivir, within 24 hours of admission to an intensive care unit (ICU) for COVID-19 complications. This inpatient monoclonal antibody and corticosteroid combination therapy is discontinued at discharge.\nIn patients who require oxygen supplementation, dexamethasone should be stopped after 10 days to prevent adverse events from prolonged corticosteroid use.[8,9] Baricitinib is administered orally and may be continued for up to 14 days with renal dosing adjustments.[8,9] Tocilizumab inhibits interleukin-6 and is a single-dose intravenous infusion; a second dose may be given 8 hours later if there is no appreciable clinical improvement.[8,9] In addition, supportive care and prevention of further transmission with a 5-day isolation followed by wearing a mask for the next 5 days are recommended for all symptomatic patients found to be positive for the COVID-19 Omicron variant.\nThe patient in this case was admitted for correction of her electrolyte abnormalities and fluid resuscitation. She was also found to be positive for COVID-19 by rRT-PCR and received remdesivir. She was placed on isolation precautions. The hematology/oncology service was consulted regarding the patient's history of lymphoma and current lymphopenia, and no further intervention was recommended because her abnormal white blood cell count was attributed to COVID-19. Throughout her hospitalization, she received a consistent carbohydrate diet and sliding-scale insulin for diabetes management. Upon discharge, she was scheduled for outpatient follow-up with her primary care provider.\nEditor's Note: The discussion in this Case Challenge applies to COVID-19 diagnosis and treatment recommendations as of April 19, 2022. This scenario will not be regularly updated, and users are encouraged to find the latest information in Medscape's COVID-19 Resource Center.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1680831,
"choiceText": "Start sotrovimab, baricitinib, and dexamethasone",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680832,
"choiceText": "Start baricitinib, dexamethasone, and remdesivir",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680833,
"choiceText": "Start tocilizumab, dexamethasone, and baricitinib",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680834,
"choiceText": "Supportive care for 24 hours, followed by baricitinib and dexamethasone",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Acute hypoxia secondary to COVID-19 warrants initiation of supplemental oxygen in addition to remdesivir and dexamethasone in an inpatient setting.<sup>[8,9]</sup> Dexamethasone is not recommended for outpatient management of mild to moderate symptoms of COVID-19. Patients who have rapidly worsening hypoxia or who require high-flow oxygen or noninvasive ventilation may also be started on baricitinib; on further decompensation and ICU admission, they should receive a single dose of tocilizumab in place of baricitinib.<sup>[8,9]</sup> Baricitinib must not be used in combination with tocilizumab because of the aggressive immunosuppression caused by each medication and the potential heightened risk for infection if used simultaneously.<sup>[8,9]</sup> Supportive care should be continued throughout hospitalization but should not delay appropriate medical therapy.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 541512,
"questionText": "What is the current recommendation for a patient with worsening acute hypoxia secondary to COVID-19 who will be admitted to the hospital in a non-ICU setting?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1680835,
"choiceText": "5 days",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680836,
"choiceText": "7 days",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680837,
"choiceText": "10 days",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680838,
"choiceText": "14 days",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Baricitinib should be administered for 14 days for worsening hypoxia and is not to be continued in an outpatient setting after the hospitalization owing to lack of information regarding safety and efficacy.<sup>[8,9]</sup> To prevent adverse events such as hyperglycemia, acquisition of a secondary infection due to immunosuppression, and psychiatric disturbances, dexamethasone administration should not exceed 10 days.<sup>[8,9]</sup> In the inpatient setting with supplemental oxygen requirements, remdesivir should be given for 5 consecutive days and is recommended in combination with baricitinib and dexamethasone.<sup>[8,9]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 541513,
"questionText": "What is the recommended duration of treatment for baricitinib for worsening hypoxia in hospitalized patients with COVID-19? ",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A School Nurse With Anxiety, Diarrhea, Palpitations, and Cough"
},
{
"authors": "Jennifer Wachala, DO; Dushyant Singh Dahiya, MD; Farah Wani, MD; Asim Kichloo, MD",
"content": [],
"date": "April 19, 2022",
"figures": [],
"markdown": "# A School Nurse With Anxiety, Diarrhea, Palpitations, and Cough\n\n **Authors:** Jennifer Wachala, DO; Dushyant Singh Dahiya, MD; Farah Wani, MD; Asim Kichloo, MD \n **Date:** April 19, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1680831,
"choiceText": "Start sotrovimab, baricitinib, and dexamethasone",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680832,
"choiceText": "Start baricitinib, dexamethasone, and remdesivir",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680833,
"choiceText": "Start tocilizumab, dexamethasone, and baricitinib",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680834,
"choiceText": "Supportive care for 24 hours, followed by baricitinib and dexamethasone",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Acute hypoxia secondary to COVID-19 warrants initiation of supplemental oxygen in addition to remdesivir and dexamethasone in an inpatient setting.<sup>[8,9]</sup> Dexamethasone is not recommended for outpatient management of mild to moderate symptoms of COVID-19. Patients who have rapidly worsening hypoxia or who require high-flow oxygen or noninvasive ventilation may also be started on baricitinib; on further decompensation and ICU admission, they should receive a single dose of tocilizumab in place of baricitinib.<sup>[8,9]</sup> Baricitinib must not be used in combination with tocilizumab because of the aggressive immunosuppression caused by each medication and the potential heightened risk for infection if used simultaneously.<sup>[8,9]</sup> Supportive care should be continued throughout hospitalization but should not delay appropriate medical therapy.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 541512,
"questionText": "What is the current recommendation for a patient with worsening acute hypoxia secondary to COVID-19 who will be admitted to the hospital in a non-ICU setting?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1680835,
"choiceText": "5 days",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680836,
"choiceText": "7 days",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680837,
"choiceText": "10 days",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680838,
"choiceText": "14 days",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Baricitinib should be administered for 14 days for worsening hypoxia and is not to be continued in an outpatient setting after the hospitalization owing to lack of information regarding safety and efficacy.<sup>[8,9]</sup> To prevent adverse events such as hyperglycemia, acquisition of a secondary infection due to immunosuppression, and psychiatric disturbances, dexamethasone administration should not exceed 10 days.<sup>[8,9]</sup> In the inpatient setting with supplemental oxygen requirements, remdesivir should be given for 5 consecutive days and is recommended in combination with baricitinib and dexamethasone.<sup>[8,9]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 541513,
"questionText": "What is the recommended duration of treatment for baricitinib for worsening hypoxia in hospitalized patients with COVID-19? ",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A School Nurse With Anxiety, Diarrhea, Palpitations, and Cough"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1680826,
"choiceText": "<i>Clostridioides difficile</i> colitis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680827,
"choiceText": "Hyperthyroidism",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680828,
"choiceText": "Reactivation of lymphoma",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680829,
"choiceText": "Colon adenocarcinoma",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680830,
"choiceText": "SARS-CoV-2 infection",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 541511,
"questionText": "On the basis of these findings only, what is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1680831,
"choiceText": "Start sotrovimab, baricitinib, and dexamethasone",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680832,
"choiceText": "Start baricitinib, dexamethasone, and remdesivir",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680833,
"choiceText": "Start tocilizumab, dexamethasone, and baricitinib",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680834,
"choiceText": "Supportive care for 24 hours, followed by baricitinib and dexamethasone",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Acute hypoxia secondary to COVID-19 warrants initiation of supplemental oxygen in addition to remdesivir and dexamethasone in an inpatient setting.<sup>[8,9]</sup> Dexamethasone is not recommended for outpatient management of mild to moderate symptoms of COVID-19. Patients who have rapidly worsening hypoxia or who require high-flow oxygen or noninvasive ventilation may also be started on baricitinib; on further decompensation and ICU admission, they should receive a single dose of tocilizumab in place of baricitinib.<sup>[8,9]</sup> Baricitinib must not be used in combination with tocilizumab because of the aggressive immunosuppression caused by each medication and the potential heightened risk for infection if used simultaneously.<sup>[8,9]</sup> Supportive care should be continued throughout hospitalization but should not delay appropriate medical therapy.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 541512,
"questionText": "What is the current recommendation for a patient with worsening acute hypoxia secondary to COVID-19 who will be admitted to the hospital in a non-ICU setting?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1680835,
"choiceText": "5 days",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680836,
"choiceText": "7 days",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680837,
"choiceText": "10 days",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1680838,
"choiceText": "14 days",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Baricitinib should be administered for 14 days for worsening hypoxia and is not to be continued in an outpatient setting after the hospitalization owing to lack of information regarding safety and efficacy.<sup>[8,9]</sup> To prevent adverse events such as hyperglycemia, acquisition of a secondary infection due to immunosuppression, and psychiatric disturbances, dexamethasone administration should not exceed 10 days.<sup>[8,9]</sup> In the inpatient setting with supplemental oxygen requirements, remdesivir should be given for 5 consecutive days and is recommended in combination with baricitinib and dexamethasone.<sup>[8,9]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 541513,
"questionText": "What is the recommended duration of treatment for baricitinib for worsening hypoxia in hospitalized patients with COVID-19? ",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
893850 | /viewarticle/893850 | [
{
"authors": "Alexander Potashinsky, MD; John W. Birk, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 36-year-old woman with a medical history that includes hypertension and Hashimoto thyroiditis presents with recurrent diarrhea. For the past 2 years, she has experienced diffuse abdominal cramping and discomfort after eating. This has been associated with bloating and increased flatulence. She describes having three soft stools almost daily.",
"Other than her loose stools, her most troublesome symptom is a \"foggy brain,\" which she has about 4 days a week. This is described as a feeling of reduced memory, delayed thinking/focus, and difficulty staying awake. She has also noticed intermittent muscle and joint aches.",
"The patient denies fever, significant change in weight, temperature sensitivity, blood in her stool, or any rashes. She has no family history of any gastrointestinal issues, including gastrointestinal (GI) cancer, inflammatory bowel disease or celiac disease. She has never had endoscopy or colonoscopy but has had normal \"routine\" blood work in the past.",
"She has tried changing her diet, including cutting out dairy and gas-producing foods, with limited success. Over the past 3 months, she has tried cutting out bread and other gluten-containing products. After stopping gluten-containing foods, she felt her symptoms quickly improve. Her primary care doctor performed serology for celiac disease, but results were negative. She restarted eating gluten-containing food and had a gradual return of her diarrhea and \"foggy brain.\""
],
"date": "April 19, 2022",
"figures": [],
"markdown": "# A 36-Year-Old Woman With Flatulence and Memory Problems\n\n **Authors:** Alexander Potashinsky, MD; John W. Birk, MD \n **Date:** April 19, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 36-year-old woman with a medical history that includes hypertension and Hashimoto thyroiditis presents with recurrent diarrhea. For the past 2 years, she has experienced diffuse abdominal cramping and discomfort after eating. This has been associated with bloating and increased flatulence. She describes having three soft stools almost daily.\nOther than her loose stools, her most troublesome symptom is a \"foggy brain,\" which she has about 4 days a week. This is described as a feeling of reduced memory, delayed thinking/focus, and difficulty staying awake. She has also noticed intermittent muscle and joint aches.\nThe patient denies fever, significant change in weight, temperature sensitivity, blood in her stool, or any rashes. She has no family history of any gastrointestinal issues, including gastrointestinal (GI) cancer, inflammatory bowel disease or celiac disease. She has never had endoscopy or colonoscopy but has had normal \"routine\" blood work in the past.\nShe has tried changing her diet, including cutting out dairy and gas-producing foods, with limited success. Over the past 3 months, she has tried cutting out bread and other gluten-containing products. After stopping gluten-containing foods, she felt her symptoms quickly improve. Her primary care doctor performed serology for celiac disease, but results were negative. She restarted eating gluten-containing food and had a gradual return of her diarrhea and \"foggy brain.\"\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A 36-Year-Old Woman With Flatulence and Memory Problems"
},
{
"authors": "Alexander Potashinsky, MD; John W. Birk, MD",
"content": [
"Upon physical examination, the patient is a healthy-appearing woman who is mildly anxious but is otherwise in no acute distress. Her blood pressure is 128/74 mm Hg, with a heart rate of 78 beats/min. Her respiratory rate is 12 breaths/min, with saturation of 99% on room air. She is afebrile, with a temperature of 98.4°F (36.9°C). Her body weight is 188 lb (85.3 kg), and her height is 5' 6\" (1.7 m); her resulting body mass index is 30 kg/m2.",
"The patient's eyes show no scleral icterus, with pupils equally reactive to light and intact extraocular muscle movements. The mucous membranes are moist, with no neck or supraclavicular adenopathy. Auscultation of the lungs reveals normal work of breathing, with clear, symmetrical breath sounds. Cardiovascular auscultation reveals a regular rate and rhythm, with normal heart sounds and absence of murmurs. Abdominal examination reveals an obese, soft, nondistended abdomen, with no tenderness to palpation and normal bowel sounds. Musculoskeletal examination reveals normal joint range of motion, with no swelling or tenderness. Skin examination reveals warm skin and no jaundice. Rectal examination shows normal sphincter tone and soft, brown stool, which is negative for occult blood.",
"Laboratory testing reveals a normal complete blood count, liver panel findings, and metabolic profile. Serology testing reveals normal thyroid-stimulating hormone (TSH) levels, A1c levels, and serum immunoglobulin (Ig)A tissue transglutaminase levels. Upper esophagogastroduodenoscopy (EGD) reveals a normal esophagus, stomach, and duodenum (Figure 1).",
"Figure 1.",
"Six random biopsy samples are obtained from the duodenal bulb and distal duodenum. Pathologic examination reveals normal duodenal histology, except for mildly increased intraepithelial lymphocytes. No crypt hyperplasia or villous atrophy is present (Figure 2).",
"Figure 2."
],
"date": "April 19, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/893/850/893850-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/893/850/893850-Thumb2.png"
}
],
"markdown": "# A 36-Year-Old Woman With Flatulence and Memory Problems\n\n **Authors:** Alexander Potashinsky, MD; John W. Birk, MD \n **Date:** April 19, 2022\n\n ## Content\n\n Upon physical examination, the patient is a healthy-appearing woman who is mildly anxious but is otherwise in no acute distress. Her blood pressure is 128/74 mm Hg, with a heart rate of 78 beats/min. Her respiratory rate is 12 breaths/min, with saturation of 99% on room air. She is afebrile, with a temperature of 98.4°F (36.9°C). Her body weight is 188 lb (85.3 kg), and her height is 5' 6\" (1.7 m); her resulting body mass index is 30 kg/m2.\nThe patient's eyes show no scleral icterus, with pupils equally reactive to light and intact extraocular muscle movements. The mucous membranes are moist, with no neck or supraclavicular adenopathy. Auscultation of the lungs reveals normal work of breathing, with clear, symmetrical breath sounds. Cardiovascular auscultation reveals a regular rate and rhythm, with normal heart sounds and absence of murmurs. Abdominal examination reveals an obese, soft, nondistended abdomen, with no tenderness to palpation and normal bowel sounds. Musculoskeletal examination reveals normal joint range of motion, with no swelling or tenderness. Skin examination reveals warm skin and no jaundice. Rectal examination shows normal sphincter tone and soft, brown stool, which is negative for occult blood.\nLaboratory testing reveals a normal complete blood count, liver panel findings, and metabolic profile. Serology testing reveals normal thyroid-stimulating hormone (TSH) levels, A1c levels, and serum immunoglobulin (Ig)A tissue transglutaminase levels. Upper esophagogastroduodenoscopy (EGD) reveals a normal esophagus, stomach, and duodenum (Figure 1).\nFigure 1.\nSix random biopsy samples are obtained from the duodenal bulb and distal duodenum. Pathologic examination reveals normal duodenal histology, except for mildly increased intraepithelial lymphocytes. No crypt hyperplasia or villous atrophy is present (Figure 2).\nFigure 2.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1196708,
"choiceText": "Infectious agent causing gastroenteritis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196710,
"choiceText": "Irritable bowel syndrome",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196712,
"choiceText": "Celiac disease",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196714,
"choiceText": "Nonceliac gluten sensitivity",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196716,
"choiceText": "Hyperthyroidism",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 380413,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 36-Year-Old Woman With Flatulence and Memory Problems"
},
{
"authors": "Alexander Potashinsky, MD; John W. Birk, MD",
"content": [
"This patient with a medical history of autoimmune thyroid disease presented with chronic diarrhea and \"foggy brain\" that responded to a gluten-free diet. When she reintroduced gluten into her diet, her symptoms returned. Her blood work was unrevealing, including a normal TSH level and absence of anemia. Her celiac serology testing was normal, and she had unremarkable EGD findings, with biopsies showing only mildly increased intraepithelial lymphocytes. This is a typical presentation of nonceliac gluten sensitivity (NCGS).",
"Gluten is a primary structural protein of wheat and other grains, such as rye and barley. Over the past 50 years, large-scale farming and use of gluten in food additives and thickeners has led to a fourfold increase in the consumption of gluten.[1] These grains comprise a large proportion of the Western diet, with an average adult in the United States consuming at least 10-15 g/day.[2] Besides gluten, wheat also contains many other proteins, including proinflammatory alpha amylase and trypsin inhibitors (AITs). The exposure of partially digested gluten and AITs to the intestinal mucosa leads to the cascades of both celiac disease and NCGS.[1]",
"Celiac disease is a well-described autoimmune disease that triggers a body-wide reaction to gluten. First termed \"Gee disease,\" it was first described in 1887 by the British physician Samuel Gee as a childhood condition related to diet. It was then linked to wheat ingestion by Dutch physician William Dicke, who noticed an increase in and abatement of symptoms during wheat shortages during World War II.[3]",
"Today, celiac disease is a hot topic of public discussion and a major contributor to various food fads. Despite a prevalence of only 1%-3%, the US food market has seen an explosion of gluten-free foods. A survey estimated that about one third of the US population is trying to cut down gluten in their diet.[4] The gluten-free food market is estimated to be over $12 billion dollars, and is growing at over 10% per year. NCGS has been increasingly recognized over the past decade as a medical condition. The prevalence of NCGS is much more difficult to pinpoint, with certain studies reporting a prevalence as high as 13%.[2]"
],
"date": "April 19, 2022",
"figures": [],
"markdown": "# A 36-Year-Old Woman With Flatulence and Memory Problems\n\n **Authors:** Alexander Potashinsky, MD; John W. Birk, MD \n **Date:** April 19, 2022\n\n ## Content\n\n This patient with a medical history of autoimmune thyroid disease presented with chronic diarrhea and \"foggy brain\" that responded to a gluten-free diet. When she reintroduced gluten into her diet, her symptoms returned. Her blood work was unrevealing, including a normal TSH level and absence of anemia. Her celiac serology testing was normal, and she had unremarkable EGD findings, with biopsies showing only mildly increased intraepithelial lymphocytes. This is a typical presentation of nonceliac gluten sensitivity (NCGS).\nGluten is a primary structural protein of wheat and other grains, such as rye and barley. Over the past 50 years, large-scale farming and use of gluten in food additives and thickeners has led to a fourfold increase in the consumption of gluten.[1] These grains comprise a large proportion of the Western diet, with an average adult in the United States consuming at least 10-15 g/day.[2] Besides gluten, wheat also contains many other proteins, including proinflammatory alpha amylase and trypsin inhibitors (AITs). The exposure of partially digested gluten and AITs to the intestinal mucosa leads to the cascades of both celiac disease and NCGS.[1]\nCeliac disease is a well-described autoimmune disease that triggers a body-wide reaction to gluten. First termed \"Gee disease,\" it was first described in 1887 by the British physician Samuel Gee as a childhood condition related to diet. It was then linked to wheat ingestion by Dutch physician William Dicke, who noticed an increase in and abatement of symptoms during wheat shortages during World War II.[3]\nToday, celiac disease is a hot topic of public discussion and a major contributor to various food fads. Despite a prevalence of only 1%-3%, the US food market has seen an explosion of gluten-free foods. A survey estimated that about one third of the US population is trying to cut down gluten in their diet.[4] The gluten-free food market is estimated to be over $12 billion dollars, and is growing at over 10% per year. NCGS has been increasingly recognized over the past decade as a medical condition. The prevalence of NCGS is much more difficult to pinpoint, with certain studies reporting a prevalence as high as 13%.[2]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1196708,
"choiceText": "Infectious agent causing gastroenteritis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196710,
"choiceText": "Irritable bowel syndrome",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196712,
"choiceText": "Celiac disease",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196714,
"choiceText": "Nonceliac gluten sensitivity",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196716,
"choiceText": "Hyperthyroidism",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 380413,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 36-Year-Old Woman With Flatulence and Memory Problems"
},
{
"authors": "Alexander Potashinsky, MD; John W. Birk, MD",
"content": [
"NCGS is a condition in which consumption of gluten leads to symptoms similar to those of celiac disease. It is nonallergic and nonautoimmune in nature. It is termed \"sensitivity\" because symptoms are relieved by gluten withdrawal and reappear with reintroduction of gluten to the diet, which triggers a constellation of GI and extraintestinal symptoms.[5]",
"Typical GI symptoms of NCGS include postprandial abdominal pain, bloating, diarrhea, and/or constipation. Extraintestinal symptoms can be diverse and include peripheral neuropathy, eczema, joint and muscle aches, anxiety, and headaches. A prominent feature is the feeling of a \"foggy brain,\" which manifests as slowed thinking and memory issues. These extraintestinal features are in major contrast with irritable bowel syndrome (IBS) symptoms, which are primarily GI symptoms.",
"Unlike in celiac disease, other systemic features are absent, including iron deficiency anemia, weight loss, and dermatitis herpetiformis rash. Because NCGS does not cause malabsorption, no nutrient deficiencies (eg, folic acid, fat-soluble vitamins) are noted. Whereas in celiac disease, symptoms may take weeks to manifest and subside, the associated symptoms in NCGS generally increase and diminish within hours to days of gluten exposure. As in the patient in this case, many patients often notice the association of gluten-containing foods with their symptoms.[1,2,3]",
"The pathophysiology of NCGS is still under investigation. The main antigen present in gluten is a protein called \"gliadin.\" When gluten is partially digested, gliadin binds to gut wall receptors, leading to increased intestinal permeability. This allows gluten to be mistakenly recognized as a pathogen by the immune system. In celiac disease, the adaptive immune response leads to gluten molecules being cross-linked by tissue transglutaminase. This then binds to human leukocyte antigen (HLA) DQ2 or DQ8 on antigen-presenting cells. This interacts with CD+ T cells in the lamina propria and activates a proinflammatory cascade, which leads to the systemic response to gluten and secretory diarrhea due to increased gut permeability.[3,5]",
"In NCGS, unlike in celiac disease, the innate immune response is thought to play a larger role, with local cytokine release leading to recruitment of intraepithelial lymphocytes.[4] The reaction is expressed by decreased gut permeability and an increased epithelial barrier, causing osmotic diarrhea. Although a systemic effect is observed, it is much less robust compared with the adaptive immune system cascade.",
"In addition to celiac disease and NCGS, wheat allergy is another important acute reaction. This is a true food allergy, with an immunoglobulin E (IgE)-mediated response that activates basophils and mast cells. The cascade releases histamine and causes rapid onset of symptoms, including flushing, diarrhea, and potentially anaphylaxis. Unlike celiac disease and NCGS, the onset of symptoms occurs within minutes to hours of ingestion of the wheat-containing food. Testing for wheat allergy is performed via skin prick testing or with a food challenge. Patients with wheat allergy must carry epinephrine pens in case of accidental exposure.[2]",
"The testing algorithms for celiac disease have been well described. The initial test of a patient consuming a gluten-rich diet is checking serology with tissue transglutaminase antibodies. If positive, this is validated by EGD duodenal biopsies that reveal villous blunting, crypt hyperplasia, and intraepithelial lymphocytes.[6] Unfortunately, NCGS is much more difficult to pinpoint because no serologic or histologic markers have been validated. Diagnosis is based on clinical symptoms after celiac disease and other potential causes have been ruled out and with resolution of symptoms when a gluten/wheat-free diet is adhered to for at least 3 weeks.[3,7]",
"In 2015, a group of experts met in Salerno, Italy, to describe a standard way of testing for NCGS. Their consensus statement describes a double-blind, placebo-controlled gluten challenge. The first step is to rule out celiac disease while a patient is consuming a gluten-rich diet. The patient is given a questionnaire to assess their baseline symptoms while consuming gluten.",
"The patient is then placed on a 6-week gluten-free diet, and the questionnaire is repeated. If symptoms improvement is less than 30%, NCGS is ruled out. If a larger improvement is noted, the patient is then moved to phase 2, where they are introduced to either a placebo or gluten-containing pill. The gluten dose is standardized to 8 g, which is equivalent to about two pieces of bread. This is given over the course of a week, followed by a 1-week washout period with a gluten-free diet. The other pill is then given for another week. Symptoms are reassessed at each step.",
"The goal is to determine whether gluten is associated with at least a 30% change in symptoms.[8] In clinical practice, where standardized gluten and placebo pills may be hard to come by, this can be done with gluten-containing or gluten-free bread."
],
"date": "April 19, 2022",
"figures": [],
"markdown": "# A 36-Year-Old Woman With Flatulence and Memory Problems\n\n **Authors:** Alexander Potashinsky, MD; John W. Birk, MD \n **Date:** April 19, 2022\n\n ## Content\n\n NCGS is a condition in which consumption of gluten leads to symptoms similar to those of celiac disease. It is nonallergic and nonautoimmune in nature. It is termed \"sensitivity\" because symptoms are relieved by gluten withdrawal and reappear with reintroduction of gluten to the diet, which triggers a constellation of GI and extraintestinal symptoms.[5]\nTypical GI symptoms of NCGS include postprandial abdominal pain, bloating, diarrhea, and/or constipation. Extraintestinal symptoms can be diverse and include peripheral neuropathy, eczema, joint and muscle aches, anxiety, and headaches. A prominent feature is the feeling of a \"foggy brain,\" which manifests as slowed thinking and memory issues. These extraintestinal features are in major contrast with irritable bowel syndrome (IBS) symptoms, which are primarily GI symptoms.\nUnlike in celiac disease, other systemic features are absent, including iron deficiency anemia, weight loss, and dermatitis herpetiformis rash. Because NCGS does not cause malabsorption, no nutrient deficiencies (eg, folic acid, fat-soluble vitamins) are noted. Whereas in celiac disease, symptoms may take weeks to manifest and subside, the associated symptoms in NCGS generally increase and diminish within hours to days of gluten exposure. As in the patient in this case, many patients often notice the association of gluten-containing foods with their symptoms.[1,2,3]\nThe pathophysiology of NCGS is still under investigation. The main antigen present in gluten is a protein called \"gliadin.\" When gluten is partially digested, gliadin binds to gut wall receptors, leading to increased intestinal permeability. This allows gluten to be mistakenly recognized as a pathogen by the immune system. In celiac disease, the adaptive immune response leads to gluten molecules being cross-linked by tissue transglutaminase. This then binds to human leukocyte antigen (HLA) DQ2 or DQ8 on antigen-presenting cells. This interacts with CD+ T cells in the lamina propria and activates a proinflammatory cascade, which leads to the systemic response to gluten and secretory diarrhea due to increased gut permeability.[3,5]\nIn NCGS, unlike in celiac disease, the innate immune response is thought to play a larger role, with local cytokine release leading to recruitment of intraepithelial lymphocytes.[4] The reaction is expressed by decreased gut permeability and an increased epithelial barrier, causing osmotic diarrhea. Although a systemic effect is observed, it is much less robust compared with the adaptive immune system cascade.\nIn addition to celiac disease and NCGS, wheat allergy is another important acute reaction. This is a true food allergy, with an immunoglobulin E (IgE)-mediated response that activates basophils and mast cells. The cascade releases histamine and causes rapid onset of symptoms, including flushing, diarrhea, and potentially anaphylaxis. Unlike celiac disease and NCGS, the onset of symptoms occurs within minutes to hours of ingestion of the wheat-containing food. Testing for wheat allergy is performed via skin prick testing or with a food challenge. Patients with wheat allergy must carry epinephrine pens in case of accidental exposure.[2]\nThe testing algorithms for celiac disease have been well described. The initial test of a patient consuming a gluten-rich diet is checking serology with tissue transglutaminase antibodies. If positive, this is validated by EGD duodenal biopsies that reveal villous blunting, crypt hyperplasia, and intraepithelial lymphocytes.[6] Unfortunately, NCGS is much more difficult to pinpoint because no serologic or histologic markers have been validated. Diagnosis is based on clinical symptoms after celiac disease and other potential causes have been ruled out and with resolution of symptoms when a gluten/wheat-free diet is adhered to for at least 3 weeks.[3,7]\nIn 2015, a group of experts met in Salerno, Italy, to describe a standard way of testing for NCGS. Their consensus statement describes a double-blind, placebo-controlled gluten challenge. The first step is to rule out celiac disease while a patient is consuming a gluten-rich diet. The patient is given a questionnaire to assess their baseline symptoms while consuming gluten.\nThe patient is then placed on a 6-week gluten-free diet, and the questionnaire is repeated. If symptoms improvement is less than 30%, NCGS is ruled out. If a larger improvement is noted, the patient is then moved to phase 2, where they are introduced to either a placebo or gluten-containing pill. The gluten dose is standardized to 8 g, which is equivalent to about two pieces of bread. This is given over the course of a week, followed by a 1-week washout period with a gluten-free diet. The other pill is then given for another week. Symptoms are reassessed at each step.\nThe goal is to determine whether gluten is associated with at least a 30% change in symptoms.[8] In clinical practice, where standardized gluten and placebo pills may be hard to come by, this can be done with gluten-containing or gluten-free bread.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A 36-Year-Old Woman With Flatulence and Memory Problems"
},
{
"authors": "Alexander Potashinsky, MD; John W. Birk, MD",
"content": [
"In the age of food fads and needless gluten avoidance, clinicians still need to recognize NCGS. A high degree of suspicion should be present in patients who are believed to have IBS but who demonstrate extraintestinal symptoms, as well as patients who have features of celiac disease but negative serologic testing results. Active research is being done to determine the exact pathophysiology of NCGS and to determine markers of disease that would enable more definitive testing.",
"Besides a gluten-free diet, further treatment options for NCGS are currently under investigation. These include use of probiotics for alleviation of NCGS-related symptoms while maintaining a gluten-free diet and reintroduction of gluten in a controlled environment. This is intended to resolve gut dysbiosis by reintroducing gut flora, reducing both gut and systemic inflammation.[5] The enzyme Aspergillus niger prolyl endoprotease (AN-PEP) has been reported to significantly enhance gluten digestion in the stomach of healthy individuals. Thus, it could be considered another treatment option for these patients by means of degrading gluten before it affects the human gut, allowing individuals to enjoy food without dietary restrictions, worrisome symptoms, or soaring food costs.[5]",
"The patient in this case had already initiated her own treatment by starting a gluten-free diet. After other common causes of her symptoms, such as uncontrolled thyroid disease and celiac disease, were ruled out, she was evaluated with a simplified food challenge for NCGS. She was asked to use gluten-containing bread, which led to a relapse of symptoms, and then gluten-free bread, which led to resolution of symptoms. Given this high degree of correlation, she was diagnosed with NCGS and was relieved to find out the cause of her problems. One year after starting a strict gluten-free diet, she remains mostly symptom-free."
],
"date": "April 19, 2022",
"figures": [],
"markdown": "# A 36-Year-Old Woman With Flatulence and Memory Problems\n\n **Authors:** Alexander Potashinsky, MD; John W. Birk, MD \n **Date:** April 19, 2022\n\n ## Content\n\n In the age of food fads and needless gluten avoidance, clinicians still need to recognize NCGS. A high degree of suspicion should be present in patients who are believed to have IBS but who demonstrate extraintestinal symptoms, as well as patients who have features of celiac disease but negative serologic testing results. Active research is being done to determine the exact pathophysiology of NCGS and to determine markers of disease that would enable more definitive testing.\nBesides a gluten-free diet, further treatment options for NCGS are currently under investigation. These include use of probiotics for alleviation of NCGS-related symptoms while maintaining a gluten-free diet and reintroduction of gluten in a controlled environment. This is intended to resolve gut dysbiosis by reintroducing gut flora, reducing both gut and systemic inflammation.[5] The enzyme Aspergillus niger prolyl endoprotease (AN-PEP) has been reported to significantly enhance gluten digestion in the stomach of healthy individuals. Thus, it could be considered another treatment option for these patients by means of degrading gluten before it affects the human gut, allowing individuals to enjoy food without dietary restrictions, worrisome symptoms, or soaring food costs.[5]\nThe patient in this case had already initiated her own treatment by starting a gluten-free diet. After other common causes of her symptoms, such as uncontrolled thyroid disease and celiac disease, were ruled out, she was evaluated with a simplified food challenge for NCGS. She was asked to use gluten-containing bread, which led to a relapse of symptoms, and then gluten-free bread, which led to resolution of symptoms. Given this high degree of correlation, she was diagnosed with NCGS and was relieved to find out the cause of her problems. One year after starting a strict gluten-free diet, she remains mostly symptom-free.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1196718,
"choiceText": "Anxiety",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196720,
"choiceText": "Dermatitis herpetiformis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196722,
"choiceText": "Iron-deficiency anemia",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196724,
"choiceText": "Gastroesophageal reflux",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196726,
"choiceText": "Weight loss",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The typical GI symptoms of NCGS include postprandial abdominal pain, bloating, diarrhea, and/or constipation. The extraintestinal symptoms can be diverse and include peripheral neuropathy, eczema, joint and muscle aches, anxiety, and headaches. A prominent feature is feelings of a \"foggy brain,\" which manifests as slowed thinking and memory issues. <br><br>\r\n\r\nThese extraintestinal features are in major contrast to those of IBS, which primarily consists of GI symptoms. In patients with celiac disease, systemic features include iron deficiency anemia, weight loss, and dermatitis herpetiformis rash.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 380415,
"questionText": "Which is a well-established feature of NCGS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1196738,
"choiceText": "IgE-mediated histamine release",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196740,
"choiceText": "Osmotic effect of gluten",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196742,
"choiceText": "Innate immune response",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196744,
"choiceText": "Adaptive immune response",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196746,
"choiceText": "Formation of serum antibodies",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The pathophysiology of NCGS is still under investigation. The main antigen present in gluten is the protein gliadin. When gluten is partially digested, gliadin binds receptors in the gut wall and leads to increased intestinal permeability. This allows gluten to be mistakenly recognized as a pathogen by the immune system. In celiac disease, the adaptive immune response leads to gluten molecules being cross-linked by tissue transglutaminase. This then binds HLA DQ2 or DQ8 on antigen-presenting cells. This interacts with CD+ T cells in the lamina propria and activates a proinflammatory cascade, which leads to the systemic response to gluten.<br><br>\r\n\r\nIn NCGS, the innate immune response is thought to play larger role, with local cytokine release leading to recruitment of intraepithelial lymphocytes. Although a systemic effect is observed, it is much less robust than the adaptive immune system cascade.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 380419,
"questionText": "Which is thought to be the underlying pathophysiology of NCGS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 36-Year-Old Woman With Flatulence and Memory Problems"
},
{
"authors": "Alexander Potashinsky, MD; John W. Birk, MD",
"content": [],
"date": "April 19, 2022",
"figures": [],
"markdown": "# A 36-Year-Old Woman With Flatulence and Memory Problems\n\n **Authors:** Alexander Potashinsky, MD; John W. Birk, MD \n **Date:** April 19, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1196718,
"choiceText": "Anxiety",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196720,
"choiceText": "Dermatitis herpetiformis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196722,
"choiceText": "Iron-deficiency anemia",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196724,
"choiceText": "Gastroesophageal reflux",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196726,
"choiceText": "Weight loss",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The typical GI symptoms of NCGS include postprandial abdominal pain, bloating, diarrhea, and/or constipation. The extraintestinal symptoms can be diverse and include peripheral neuropathy, eczema, joint and muscle aches, anxiety, and headaches. A prominent feature is feelings of a \"foggy brain,\" which manifests as slowed thinking and memory issues. <br><br>\r\n\r\nThese extraintestinal features are in major contrast to those of IBS, which primarily consists of GI symptoms. In patients with celiac disease, systemic features include iron deficiency anemia, weight loss, and dermatitis herpetiformis rash.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 380415,
"questionText": "Which is a well-established feature of NCGS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1196738,
"choiceText": "IgE-mediated histamine release",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196740,
"choiceText": "Osmotic effect of gluten",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196742,
"choiceText": "Innate immune response",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196744,
"choiceText": "Adaptive immune response",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196746,
"choiceText": "Formation of serum antibodies",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The pathophysiology of NCGS is still under investigation. The main antigen present in gluten is the protein gliadin. When gluten is partially digested, gliadin binds receptors in the gut wall and leads to increased intestinal permeability. This allows gluten to be mistakenly recognized as a pathogen by the immune system. In celiac disease, the adaptive immune response leads to gluten molecules being cross-linked by tissue transglutaminase. This then binds HLA DQ2 or DQ8 on antigen-presenting cells. This interacts with CD+ T cells in the lamina propria and activates a proinflammatory cascade, which leads to the systemic response to gluten.<br><br>\r\n\r\nIn NCGS, the innate immune response is thought to play larger role, with local cytokine release leading to recruitment of intraepithelial lymphocytes. Although a systemic effect is observed, it is much less robust than the adaptive immune system cascade.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 380419,
"questionText": "Which is thought to be the underlying pathophysiology of NCGS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 36-Year-Old Woman With Flatulence and Memory Problems"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1196708,
"choiceText": "Infectious agent causing gastroenteritis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196710,
"choiceText": "Irritable bowel syndrome",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196712,
"choiceText": "Celiac disease",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196714,
"choiceText": "Nonceliac gluten sensitivity",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196716,
"choiceText": "Hyperthyroidism",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 380413,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1196718,
"choiceText": "Anxiety",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196720,
"choiceText": "Dermatitis herpetiformis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196722,
"choiceText": "Iron-deficiency anemia",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196724,
"choiceText": "Gastroesophageal reflux",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196726,
"choiceText": "Weight loss",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The typical GI symptoms of NCGS include postprandial abdominal pain, bloating, diarrhea, and/or constipation. The extraintestinal symptoms can be diverse and include peripheral neuropathy, eczema, joint and muscle aches, anxiety, and headaches. A prominent feature is feelings of a \"foggy brain,\" which manifests as slowed thinking and memory issues. <br><br>\r\n\r\nThese extraintestinal features are in major contrast to those of IBS, which primarily consists of GI symptoms. In patients with celiac disease, systemic features include iron deficiency anemia, weight loss, and dermatitis herpetiformis rash.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 380415,
"questionText": "Which is a well-established feature of NCGS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1196738,
"choiceText": "IgE-mediated histamine release",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196740,
"choiceText": "Osmotic effect of gluten",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196742,
"choiceText": "Innate immune response",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196744,
"choiceText": "Adaptive immune response",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1196746,
"choiceText": "Formation of serum antibodies",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The pathophysiology of NCGS is still under investigation. The main antigen present in gluten is the protein gliadin. When gluten is partially digested, gliadin binds receptors in the gut wall and leads to increased intestinal permeability. This allows gluten to be mistakenly recognized as a pathogen by the immune system. In celiac disease, the adaptive immune response leads to gluten molecules being cross-linked by tissue transglutaminase. This then binds HLA DQ2 or DQ8 on antigen-presenting cells. This interacts with CD+ T cells in the lamina propria and activates a proinflammatory cascade, which leads to the systemic response to gluten.<br><br>\r\n\r\nIn NCGS, the innate immune response is thought to play larger role, with local cytokine release leading to recruitment of intraepithelial lymphocytes. Although a systemic effect is observed, it is much less robust than the adaptive immune system cascade.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 380419,
"questionText": "Which is thought to be the underlying pathophysiology of NCGS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
745798 | /viewarticle/745798 | [
{
"authors": "Maria Cristina Bravi, MD, PhD",
"content": [
"Editorial Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 53-year-old woman with a history of hypertension, hyperlipidemia, active tobacco use, and obesity presents to the emergency department (ED) with a 1-week history of chest pain and dyspnea. She notes associated symptoms of weakness, dizziness, and syncope. The symptoms have been gradually progressive over the course of the week. On the day of presentation, she had an episode of chest pain at rest during the early morning hours, which prompted her to seek medical attention.",
"She has not taken any medications for her symptoms outside of her chronic angiotensin-converting enzyme (ACE) inhibitor and statin therapy. The patient does not report any significant family history of arrhythmias, cardiomyopathy, or sudden cardiac death. She does note use any illicit drugs."
],
"date": "April 18, 2022",
"figures": [],
"markdown": "# Cardio Case Challenge: Syncope in a 53-Year-Old Woman With Dyspnea and Morning Chest Pain\n\n **Authors:** Maria Cristina Bravi, MD, PhD \n **Date:** April 18, 2022\n\n ## Content\n\n Editorial Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 53-year-old woman with a history of hypertension, hyperlipidemia, active tobacco use, and obesity presents to the emergency department (ED) with a 1-week history of chest pain and dyspnea. She notes associated symptoms of weakness, dizziness, and syncope. The symptoms have been gradually progressive over the course of the week. On the day of presentation, she had an episode of chest pain at rest during the early morning hours, which prompted her to seek medical attention.\nShe has not taken any medications for her symptoms outside of her chronic angiotensin-converting enzyme (ACE) inhibitor and statin therapy. The patient does not report any significant family history of arrhythmias, cardiomyopathy, or sudden cardiac death. She does note use any illicit drugs.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Cardio Case Challenge: Syncope in a 53-Year-Old Woman With Dyspnea and Morning Chest Pain"
},
{
"authors": "Maria Cristina Bravi, MD, PhD",
"content": [
"The physical examination reveals a normal heart rate and regular rhythm, normal oxygenation, an elevated blood pressure (170/90 mm Hg) and obesity (body mass index of 35; central obesity with an abdominal circumference of 110 cm is noted). Jugular venous distention is estimated at 6-8 cm; however, this is difficult to assess because of the patient's obesity.",
"Carotid artery bruits are absent. Her lungs are clear to auscultation bilaterally, with normal respiratory effort and good air movement throughout the lung fields. The cardiac examination demonstrates a regular rate and rhythm, with a normal S1 and a physiologically split S2 without murmurs, rubs, or gallops. The abdomen is soft and nontender. Her peripheral pulses are 2+ and symmetric in all 4 extremities. The lower extremities are warm, well perfused, and without edema. The neurologic examination shows the patient to be alert and oriented to person, place, and time, without any focal deficits.",
"The rest of her examination is unremarkable. Chest radiography reveals a dilated aortic arch.",
"Laboratory investigations reveal a normal complete blood cell count. Serial measurements of her cardiac biomarkers remain normal. Liver function tests are performed, including: aspartate aminotransferase (AST), 112 IU/L (reference range 3-45 IU/L); alanine aminotransferase (ALT), 87 IU/L (reference range 5-35 IU/L); alkaline phosphatase, 384 IU/L (reference range 10-95 IU/L); and gamma-glutamyl transferase, 227 IU/L (reference value < 45 IU/L). Despite physician recommendations for admission and further evaluation, the patient signs out of the ED against medical advice and returns home with her husband.",
"Three days later, the patient suffers cardiac arrest while at a shopping mall. EMS arrives at the scene and, a few minutes later, they obtain a rhythm strip that demonstrates ventricular fibrillation. Cardiopulmonary resuscitation (CPR) is initiated and the patient is electrically shocked into a sinus rhythm. She slowly regains consciousness after cardioversion. Upon arrival to the ED, the patient is placed on a cardiac monitor. A 12-lead ECG reveals a normal rhythm and normal ST segments and T waves.",
"No evidence suggests a prolonged QTc or hypertrophy. A bedside echocardiogram demonstrates no wall motion abnormalities and a preserved ejection fraction with mild left ventricular hypertrophy. A cardiology service consultation is obtained and the patient is admitted to the cardiac care unit in anticipation of coronary angiography and left ventriculography. Early in the morning 2 days later, while on cardiac monitoring, the patient experiences another short episode of chest pain that evolves into a cardiac arrest. She spontaneously regains circulation after 2 minutes of CPR."
],
"date": "April 18, 2022",
"figures": [],
"markdown": "# Cardio Case Challenge: Syncope in a 53-Year-Old Woman With Dyspnea and Morning Chest Pain\n\n **Authors:** Maria Cristina Bravi, MD, PhD \n **Date:** April 18, 2022\n\n ## Content\n\n The physical examination reveals a normal heart rate and regular rhythm, normal oxygenation, an elevated blood pressure (170/90 mm Hg) and obesity (body mass index of 35; central obesity with an abdominal circumference of 110 cm is noted). Jugular venous distention is estimated at 6-8 cm; however, this is difficult to assess because of the patient's obesity.\nCarotid artery bruits are absent. Her lungs are clear to auscultation bilaterally, with normal respiratory effort and good air movement throughout the lung fields. The cardiac examination demonstrates a regular rate and rhythm, with a normal S1 and a physiologically split S2 without murmurs, rubs, or gallops. The abdomen is soft and nontender. Her peripheral pulses are 2+ and symmetric in all 4 extremities. The lower extremities are warm, well perfused, and without edema. The neurologic examination shows the patient to be alert and oriented to person, place, and time, without any focal deficits.\nThe rest of her examination is unremarkable. Chest radiography reveals a dilated aortic arch.\nLaboratory investigations reveal a normal complete blood cell count. Serial measurements of her cardiac biomarkers remain normal. Liver function tests are performed, including: aspartate aminotransferase (AST), 112 IU/L (reference range 3-45 IU/L); alanine aminotransferase (ALT), 87 IU/L (reference range 5-35 IU/L); alkaline phosphatase, 384 IU/L (reference range 10-95 IU/L); and gamma-glutamyl transferase, 227 IU/L (reference value < 45 IU/L). Despite physician recommendations for admission and further evaluation, the patient signs out of the ED against medical advice and returns home with her husband.\nThree days later, the patient suffers cardiac arrest while at a shopping mall. EMS arrives at the scene and, a few minutes later, they obtain a rhythm strip that demonstrates ventricular fibrillation. Cardiopulmonary resuscitation (CPR) is initiated and the patient is electrically shocked into a sinus rhythm. She slowly regains consciousness after cardioversion. Upon arrival to the ED, the patient is placed on a cardiac monitor. A 12-lead ECG reveals a normal rhythm and normal ST segments and T waves.\nNo evidence suggests a prolonged QTc or hypertrophy. A bedside echocardiogram demonstrates no wall motion abnormalities and a preserved ejection fraction with mild left ventricular hypertrophy. A cardiology service consultation is obtained and the patient is admitted to the cardiac care unit in anticipation of coronary angiography and left ventriculography. Early in the morning 2 days later, while on cardiac monitoring, the patient experiences another short episode of chest pain that evolves into a cardiac arrest. She spontaneously regains circulation after 2 minutes of CPR.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 415589,
"choiceText": "Myocardial infarction",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415590,
"choiceText": "Torsade de pointes secondary to long-QT syndrome",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415591,
"choiceText": "Hypertrophic cardiomyopathy",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415592,
"choiceText": "Prinzmetal angina or variant angina",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 122184,
"questionText": "What is the likely diagnosis of these repeated episodes of cardiac arrest with no identified ST segment or T-wave changes?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Cardio Case Challenge: Syncope in a 53-Year-Old Woman With Dyspnea and Morning Chest Pain"
},
{
"authors": "Maria Cristina Bravi, MD, PhD",
"content": [
"Analysis of the patient's cardiac monitoring during her cardiac arrest was diagnostic. During the episode of chest pain, which began at 7:37 am, the tracing revealed hyperacute T waves in the inferior leads, II, III, and aVF (Figure 1).",
"Figure 1.",
"Diffuse T-wave inversions in the precordial leads were also seen. The patient described an unpleasant sensation like \"a brick\" on her chest, with associated dyspnea. She appeared pale and diaphoretic. Twenty minutes later, at 7:57 am, the monitoring demonstrated ST-segment elevation of 2-3 mm in the inferior leads with reciprocal depressions in the anterioseptal leads (Figure 2). The ST-segment elevations increased to between 8 and 10 mm (Figure 3), and subsequently degenerated into polymorphic ventricular tachycardia (Figure 4).",
"Figure 2.",
"Figure 3.",
"Figure 4.",
"A few minutes later (at 8:01 am), she spontaneously converted to a supraventricular tachycardia with frequent premature ventricular contractions, and then to a sinus rhythm. During the ventricular arrhythmia, the patient experienced cardiac arrest but recovered spontaneous circulation and regained consciousness after 2 minutes of CPR with concomitant spontaneous cardioversion. Immediately following the event, the patient underwent coronary angiography; no evidence of coronary artery disease was noted. During angiography, vasospasm of the right coronary artery was witnessed and successfully treated with intracoronary injection of nitroglycerin. Angiographic findings lead to the diagnosis of coronary artery spasm (CAS) or Prinzmetal angina.",
"In 1959, Prinzmetal and colleagues described a syndrome characterized by nonexertional chest pain and ST-segment elevation.[1] The episodes of chest pain occurred in a cyclic manner, especially in the early morning hours. This syndrome was named Prinzmetal angina or variant angina. Coronary artery vasospasm without atherosclerotic lesions is hypothesized to be the pathophysiologic mechanism responsible for the associated chest pain and ST-segment elevation. Vagal withdrawal or changes in sympathetic activity may play a role in CAS.[2] Endothelial dysfunction with reduced nitric oxide synthase is a contributory factor in CAS even though it has been demonstrated that basal nitric oxide levels do not appear to be decreased during coronary spasm.[3] Another possible mechanism for CAS may be the effects of p122 protein on phospholipase C-δ1activity.[4] In a small study, investigators determined that not only does the p122 protein appear to be upregulated in patients with coronary spasm, thus enhancing vasomotility, but it also increases intracellular calcium to acetylcholine."
],
"date": "April 18, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/745/000/745000-thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/745/000/745000-thumb2.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/745/000/745000-thumb3.png"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/745/000/745000-thumb4.png"
}
],
"markdown": "# Cardio Case Challenge: Syncope in a 53-Year-Old Woman With Dyspnea and Morning Chest Pain\n\n **Authors:** Maria Cristina Bravi, MD, PhD \n **Date:** April 18, 2022\n\n ## Content\n\n Analysis of the patient's cardiac monitoring during her cardiac arrest was diagnostic. During the episode of chest pain, which began at 7:37 am, the tracing revealed hyperacute T waves in the inferior leads, II, III, and aVF (Figure 1).\nFigure 1.\nDiffuse T-wave inversions in the precordial leads were also seen. The patient described an unpleasant sensation like \"a brick\" on her chest, with associated dyspnea. She appeared pale and diaphoretic. Twenty minutes later, at 7:57 am, the monitoring demonstrated ST-segment elevation of 2-3 mm in the inferior leads with reciprocal depressions in the anterioseptal leads (Figure 2). The ST-segment elevations increased to between 8 and 10 mm (Figure 3), and subsequently degenerated into polymorphic ventricular tachycardia (Figure 4).\nFigure 2.\nFigure 3.\nFigure 4.\nA few minutes later (at 8:01 am), she spontaneously converted to a supraventricular tachycardia with frequent premature ventricular contractions, and then to a sinus rhythm. During the ventricular arrhythmia, the patient experienced cardiac arrest but recovered spontaneous circulation and regained consciousness after 2 minutes of CPR with concomitant spontaneous cardioversion. Immediately following the event, the patient underwent coronary angiography; no evidence of coronary artery disease was noted. During angiography, vasospasm of the right coronary artery was witnessed and successfully treated with intracoronary injection of nitroglycerin. Angiographic findings lead to the diagnosis of coronary artery spasm (CAS) or Prinzmetal angina.\nIn 1959, Prinzmetal and colleagues described a syndrome characterized by nonexertional chest pain and ST-segment elevation.[1] The episodes of chest pain occurred in a cyclic manner, especially in the early morning hours. This syndrome was named Prinzmetal angina or variant angina. Coronary artery vasospasm without atherosclerotic lesions is hypothesized to be the pathophysiologic mechanism responsible for the associated chest pain and ST-segment elevation. Vagal withdrawal or changes in sympathetic activity may play a role in CAS.[2] Endothelial dysfunction with reduced nitric oxide synthase is a contributory factor in CAS even though it has been demonstrated that basal nitric oxide levels do not appear to be decreased during coronary spasm.[3] Another possible mechanism for CAS may be the effects of p122 protein on phospholipase C-δ1activity.[4] In a small study, investigators determined that not only does the p122 protein appear to be upregulated in patients with coronary spasm, thus enhancing vasomotility, but it also increases intracellular calcium to acetylcholine.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 415589,
"choiceText": "Myocardial infarction",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415590,
"choiceText": "Torsade de pointes secondary to long-QT syndrome",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415591,
"choiceText": "Hypertrophic cardiomyopathy",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415592,
"choiceText": "Prinzmetal angina or variant angina",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 122184,
"questionText": "What is the likely diagnosis of these repeated episodes of cardiac arrest with no identified ST segment or T-wave changes?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Cardio Case Challenge: Syncope in a 53-Year-Old Woman With Dyspnea and Morning Chest Pain"
},
{
"authors": "Maria Cristina Bravi, MD, PhD",
"content": [
"Chronic low-grade inflammation as demonstrated by increased monocyte count and elevation of serum high-sensitive C-reactive protein levels is associated with CAS. However, other than smoking, classic atherosclerotic risk factors were poorly associated with CAS in a study of Japanese patients.[5] CAS is reported to occur in 1%-5% of coronary angiography cases.[6] Ethnic differences in the frequency of CAS are noted, with CAS being more frequent in Japanese patients (a 3-fold greater incidence of spasm) than Caucasian patients. Traditionally, female patients are felt to be much more likely to develop coronary spasm, although recent observations suggest a male preponderance.",
"Patients with CAS typically describe classic angina symptoms, such as chest pain with radiation to the arm, shoulder, neck, and jaw. Transient ST-segment elevation during episodes of chest pain that resolves completely within minutes is a pathognomonic finding in patients with variant angina. Some episodes of CAS are brief and may be asymptomatic. Severe vasospastic angina may result in potentially fatal ventricular arrhythmias with hemodynamic deterioration and syncope.[7] Other causes of cardiac arrest, such as myocardial infarction, long-QT syndrome, and hypertrophic obstructive cardiomyopathy, must be excluded by assessment of cardiac biomarkers, electrocardiography, and echocardiography. Cocaine and certain other drug use, which can also cause coronary vasospasm, must be ruled out.[8]",
"Patients with CAS presenting with symptoms or signs of acute myocardial ischemia require admission. A 12-lead ECG and continuous telemetry monitoring are critical in the initial evaluation of patients presenting with chest pain concerning for acute coronary syndromes. Serial measurements of cardiac enzymes and troponin levels should be performed to assess for evidence of ischemia. Other laboratory tests should include a complete blood count, serum chemistry, and lipid profile. Urine toxicology to assess for recent cocaine use can be helpful, but it does not absolutely rule out cocaine-induced vasospasm because spasm can continue to occur even weeks after usage, at which time the urine screening may be negative.",
"Transthoracic echocardiography can rule out structural heart disease as well as other causes of symptoms, including pericarditis, valvular disease, or abnormalities of the aorta. Stress testing with myocardial perfusion imaging or coronary angiography is essential to assess coexisting or contributory atherosclerotic coronary disease. Because transient ST-segment elevation during episodes of chest pain that resolves completely within minutes is a characteristic finding in patients with variant angina, a 12-lead ECG is essential to diagnose CAS. Holter monitoring may facilitate the diagnosis of silent CAS as well as the detection of life-threatening arrhythmias (ventricular fibrillation, ventricular tachycardia, and complete atrioventricular block).",
"Coronary angiography with provocative testing (using acetylcholine, ergonovine, or methylergonovine) is the criterion standard for diagnosis. Angiography may reveal minimal or no angiographic evidence of coronary artery disease.[9] Variant angina is the most likely diagnosis in relatively young patients without angiographic evidence of coronary artery disease."
],
"date": "April 18, 2022",
"figures": [],
"markdown": "# Cardio Case Challenge: Syncope in a 53-Year-Old Woman With Dyspnea and Morning Chest Pain\n\n **Authors:** Maria Cristina Bravi, MD, PhD \n **Date:** April 18, 2022\n\n ## Content\n\n Chronic low-grade inflammation as demonstrated by increased monocyte count and elevation of serum high-sensitive C-reactive protein levels is associated with CAS. However, other than smoking, classic atherosclerotic risk factors were poorly associated with CAS in a study of Japanese patients.[5] CAS is reported to occur in 1%-5% of coronary angiography cases.[6] Ethnic differences in the frequency of CAS are noted, with CAS being more frequent in Japanese patients (a 3-fold greater incidence of spasm) than Caucasian patients. Traditionally, female patients are felt to be much more likely to develop coronary spasm, although recent observations suggest a male preponderance.\nPatients with CAS typically describe classic angina symptoms, such as chest pain with radiation to the arm, shoulder, neck, and jaw. Transient ST-segment elevation during episodes of chest pain that resolves completely within minutes is a pathognomonic finding in patients with variant angina. Some episodes of CAS are brief and may be asymptomatic. Severe vasospastic angina may result in potentially fatal ventricular arrhythmias with hemodynamic deterioration and syncope.[7] Other causes of cardiac arrest, such as myocardial infarction, long-QT syndrome, and hypertrophic obstructive cardiomyopathy, must be excluded by assessment of cardiac biomarkers, electrocardiography, and echocardiography. Cocaine and certain other drug use, which can also cause coronary vasospasm, must be ruled out.[8]\nPatients with CAS presenting with symptoms or signs of acute myocardial ischemia require admission. A 12-lead ECG and continuous telemetry monitoring are critical in the initial evaluation of patients presenting with chest pain concerning for acute coronary syndromes. Serial measurements of cardiac enzymes and troponin levels should be performed to assess for evidence of ischemia. Other laboratory tests should include a complete blood count, serum chemistry, and lipid profile. Urine toxicology to assess for recent cocaine use can be helpful, but it does not absolutely rule out cocaine-induced vasospasm because spasm can continue to occur even weeks after usage, at which time the urine screening may be negative.\nTransthoracic echocardiography can rule out structural heart disease as well as other causes of symptoms, including pericarditis, valvular disease, or abnormalities of the aorta. Stress testing with myocardial perfusion imaging or coronary angiography is essential to assess coexisting or contributory atherosclerotic coronary disease. Because transient ST-segment elevation during episodes of chest pain that resolves completely within minutes is a characteristic finding in patients with variant angina, a 12-lead ECG is essential to diagnose CAS. Holter monitoring may facilitate the diagnosis of silent CAS as well as the detection of life-threatening arrhythmias (ventricular fibrillation, ventricular tachycardia, and complete atrioventricular block).\nCoronary angiography with provocative testing (using acetylcholine, ergonovine, or methylergonovine) is the criterion standard for diagnosis. Angiography may reveal minimal or no angiographic evidence of coronary artery disease.[9] Variant angina is the most likely diagnosis in relatively young patients without angiographic evidence of coronary artery disease.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Cardio Case Challenge: Syncope in a 53-Year-Old Woman With Dyspnea and Morning Chest Pain"
},
{
"authors": "Maria Cristina Bravi, MD, PhD",
"content": [
"Intravenous or sublingual nitrate therapy is the initial medical treatment, whereas long-acting nitrates and calcium channel blockers are used to reduce the frequency of recurrent episodes of chest pain.[10] The amino acid L-arginine, which is converted by the body into the vasodilator nitric oxide, may also be prescribed for chest pain. Magnesium deficiency may contribute to CAS; therefore, oral supplementation of magnesium should be considered.[11] Statins in combination with calcium channel antagonists have beneficial effects on endothelial function. Yasue and colleagues demonstrated that the addition of a statin (fluvastatin) to conventional calcium channel blocker therapy is able to suppress acetylcholine-induced CAS.[12]",
"Beta-blockers can be beneficial in patients with atherosclerotic coronary lesions, and when used in conjunction with calcium channel blockers and nitrates, they can aid in symptom control in Prinzmetal angina. Nevertheless, because of their effect on beta-2 receptors, which physiologically mediate vasodilatation, nonselective beta-blockers may induce coronary spasm, worsening vasospastic angina. Beta blockade may also place the patient at risk for unopposed alpha activity in the setting of cocaine-induced vasospasm.[10] Cardioselective beta blockers have a stronger affinity for beta-1 than for beta-2 receptors, but at higher dosages they lose their selectivity and so can also induce CAS. Therefore, many clinicians avoid using even cardioselective beta-blockers in patients with Prinzmetal angina.",
"Very high dosages of aspirin (325 mg tablets taken 4-8 times daily) should also be avoided in Prinzmetal angina, since, by inhibiting the function of cyclo-oxygenase (COX), they suppress prostaglandin synthesis, aggravating CAS.[13]",
"Myocardial infarction is a potential complication of CAS, and its incidence and prognosis depend on the extent and severity of underlying atherosclerotic coronary stenosis. Even if patients with CAS are considered to be \"at high cardiovascular risk,\" overall mortality is low.",
"A poorer prognosis is related to intolerance of calcium channel antagonists, concurrent coronary atherosclerosis, and smoking. The risk for sudden death is about 2%. If life-threatening arrhythmias are documented, defibrillator implantation may be considered.[14] Patients with CAS should receive appropriate medical and lifestyle interventions to prevent atherosclerotic lesions, as atherosclerosis is common in patients with vasospastic angina.",
"The patient in this case was discharged from the hospital several days after her angiography with recommendations to quit smoking, pursue a moderate daily exercise program, and follow a low-calorie and low-fat diet. She was discharged with prescriptions for a calcium channel blocker and long-acting nitrate therapy in addition to her home ACE inhibitor and statin regimen. The patient was offered an implantable cardioverter-defibrillator (ICD) for secondary prevention of sudden cardiac death, but she refused. For the first month after discharge, the patient was monitored by outpatient telemetry for rhythm disturbances and episodes of myocardial ischemia. She remained symptom-free without recurrence of dysrhythmia or cardiac syncope during the first year of monitoring following her cardiac arrest. At the time of this report, the patient is in good health and is followed regularly by her cardiologist."
],
"date": "April 18, 2022",
"figures": [],
"markdown": "# Cardio Case Challenge: Syncope in a 53-Year-Old Woman With Dyspnea and Morning Chest Pain\n\n **Authors:** Maria Cristina Bravi, MD, PhD \n **Date:** April 18, 2022\n\n ## Content\n\n Intravenous or sublingual nitrate therapy is the initial medical treatment, whereas long-acting nitrates and calcium channel blockers are used to reduce the frequency of recurrent episodes of chest pain.[10] The amino acid L-arginine, which is converted by the body into the vasodilator nitric oxide, may also be prescribed for chest pain. Magnesium deficiency may contribute to CAS; therefore, oral supplementation of magnesium should be considered.[11] Statins in combination with calcium channel antagonists have beneficial effects on endothelial function. Yasue and colleagues demonstrated that the addition of a statin (fluvastatin) to conventional calcium channel blocker therapy is able to suppress acetylcholine-induced CAS.[12]\nBeta-blockers can be beneficial in patients with atherosclerotic coronary lesions, and when used in conjunction with calcium channel blockers and nitrates, they can aid in symptom control in Prinzmetal angina. Nevertheless, because of their effect on beta-2 receptors, which physiologically mediate vasodilatation, nonselective beta-blockers may induce coronary spasm, worsening vasospastic angina. Beta blockade may also place the patient at risk for unopposed alpha activity in the setting of cocaine-induced vasospasm.[10] Cardioselective beta blockers have a stronger affinity for beta-1 than for beta-2 receptors, but at higher dosages they lose their selectivity and so can also induce CAS. Therefore, many clinicians avoid using even cardioselective beta-blockers in patients with Prinzmetal angina.\nVery high dosages of aspirin (325 mg tablets taken 4-8 times daily) should also be avoided in Prinzmetal angina, since, by inhibiting the function of cyclo-oxygenase (COX), they suppress prostaglandin synthesis, aggravating CAS.[13]\nMyocardial infarction is a potential complication of CAS, and its incidence and prognosis depend on the extent and severity of underlying atherosclerotic coronary stenosis. Even if patients with CAS are considered to be \"at high cardiovascular risk,\" overall mortality is low.\nA poorer prognosis is related to intolerance of calcium channel antagonists, concurrent coronary atherosclerosis, and smoking. The risk for sudden death is about 2%. If life-threatening arrhythmias are documented, defibrillator implantation may be considered.[14] Patients with CAS should receive appropriate medical and lifestyle interventions to prevent atherosclerotic lesions, as atherosclerosis is common in patients with vasospastic angina.\nThe patient in this case was discharged from the hospital several days after her angiography with recommendations to quit smoking, pursue a moderate daily exercise program, and follow a low-calorie and low-fat diet. She was discharged with prescriptions for a calcium channel blocker and long-acting nitrate therapy in addition to her home ACE inhibitor and statin regimen. The patient was offered an implantable cardioverter-defibrillator (ICD) for secondary prevention of sudden cardiac death, but she refused. For the first month after discharge, the patient was monitored by outpatient telemetry for rhythm disturbances and episodes of myocardial ischemia. She remained symptom-free without recurrence of dysrhythmia or cardiac syncope during the first year of monitoring following her cardiac arrest. At the time of this report, the patient is in good health and is followed regularly by her cardiologist.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 415593,
"choiceText": "Nitrates",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415594,
"choiceText": "Nonselective beta-blockers",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415595,
"choiceText": "Calcium channel blockers",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415596,
"choiceText": "Statins",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415597,
"choiceText": "Magnesium supplementation",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Beta-blockers are beneficial in patients with atherosclerotic coronary lesions and, when used in conjunction with other drugs (calcium channel blockers and nitrates), they can help to control symptoms of Prinzmetal angina. Nevertheless, nonselective beta-blockers can potentially have detrimental effects in some patients with CAS due to their effect on beta-2 receptors, which physiologically mediate vasodilatation. Thus, when used in patients with CAS, beta-blockers may induce coronary spasm, worsening vasospastic angina. Beta blockade may also place the patient at risk for unopposed alpha activity in the setting of cocaine-induced vasospasm.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 122185,
"questionText": "Which drug can potentially be harmful in the treatment of CAS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 415598,
"choiceText": "ICD",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415599,
"choiceText": "Coronary angioplasty",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415600,
"choiceText": "Coronary artery bypass graft surgery",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415601,
"choiceText": "Pacemaker device",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415602,
"choiceText": "Nothing, as these cannot be prevented",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "If life-threatening arrhythmias are documented, defibrillator implantation may be considered, because the risk for sudden cardiac death is about 2%. Coronary angioplasty may be indicated in rare cases of medically intractable CAS. Stent implantation may successfully serve as a scaffold to maintain patency in spastic areas that are refractory to medical therapy. The efficacy of coronary bypass is greater in patients with associated coronary atherosclerotic lesions.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 122186,
"questionText": "The patient you are examining with CAS is not responding to pharmaceutical therapy and continues to have documented ventricular arrhythmias. Which is the most appropriate invasive approach to prevent mortality from these life-threatening arrhythmias?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Cardio Case Challenge: Syncope in a 53-Year-Old Woman With Dyspnea and Morning Chest Pain"
},
{
"authors": "Maria Cristina Bravi, MD, PhD",
"content": [],
"date": "April 18, 2022",
"figures": [],
"markdown": "# Cardio Case Challenge: Syncope in a 53-Year-Old Woman With Dyspnea and Morning Chest Pain\n\n **Authors:** Maria Cristina Bravi, MD, PhD \n **Date:** April 18, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 415593,
"choiceText": "Nitrates",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415594,
"choiceText": "Nonselective beta-blockers",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415595,
"choiceText": "Calcium channel blockers",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415596,
"choiceText": "Statins",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415597,
"choiceText": "Magnesium supplementation",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Beta-blockers are beneficial in patients with atherosclerotic coronary lesions and, when used in conjunction with other drugs (calcium channel blockers and nitrates), they can help to control symptoms of Prinzmetal angina. Nevertheless, nonselective beta-blockers can potentially have detrimental effects in some patients with CAS due to their effect on beta-2 receptors, which physiologically mediate vasodilatation. Thus, when used in patients with CAS, beta-blockers may induce coronary spasm, worsening vasospastic angina. Beta blockade may also place the patient at risk for unopposed alpha activity in the setting of cocaine-induced vasospasm.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 122185,
"questionText": "Which drug can potentially be harmful in the treatment of CAS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 415598,
"choiceText": "ICD",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415599,
"choiceText": "Coronary angioplasty",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415600,
"choiceText": "Coronary artery bypass graft surgery",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415601,
"choiceText": "Pacemaker device",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415602,
"choiceText": "Nothing, as these cannot be prevented",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "If life-threatening arrhythmias are documented, defibrillator implantation may be considered, because the risk for sudden cardiac death is about 2%. Coronary angioplasty may be indicated in rare cases of medically intractable CAS. Stent implantation may successfully serve as a scaffold to maintain patency in spastic areas that are refractory to medical therapy. The efficacy of coronary bypass is greater in patients with associated coronary atherosclerotic lesions.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 122186,
"questionText": "The patient you are examining with CAS is not responding to pharmaceutical therapy and continues to have documented ventricular arrhythmias. Which is the most appropriate invasive approach to prevent mortality from these life-threatening arrhythmias?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Cardio Case Challenge: Syncope in a 53-Year-Old Woman With Dyspnea and Morning Chest Pain"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 415589,
"choiceText": "Myocardial infarction",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415590,
"choiceText": "Torsade de pointes secondary to long-QT syndrome",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415591,
"choiceText": "Hypertrophic cardiomyopathy",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415592,
"choiceText": "Prinzmetal angina or variant angina",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 122184,
"questionText": "What is the likely diagnosis of these repeated episodes of cardiac arrest with no identified ST segment or T-wave changes?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 415593,
"choiceText": "Nitrates",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415594,
"choiceText": "Nonselective beta-blockers",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415595,
"choiceText": "Calcium channel blockers",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415596,
"choiceText": "Statins",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415597,
"choiceText": "Magnesium supplementation",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Beta-blockers are beneficial in patients with atherosclerotic coronary lesions and, when used in conjunction with other drugs (calcium channel blockers and nitrates), they can help to control symptoms of Prinzmetal angina. Nevertheless, nonselective beta-blockers can potentially have detrimental effects in some patients with CAS due to their effect on beta-2 receptors, which physiologically mediate vasodilatation. Thus, when used in patients with CAS, beta-blockers may induce coronary spasm, worsening vasospastic angina. Beta blockade may also place the patient at risk for unopposed alpha activity in the setting of cocaine-induced vasospasm.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 122185,
"questionText": "Which drug can potentially be harmful in the treatment of CAS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 415598,
"choiceText": "ICD",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415599,
"choiceText": "Coronary angioplasty",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415600,
"choiceText": "Coronary artery bypass graft surgery",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415601,
"choiceText": "Pacemaker device",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 415602,
"choiceText": "Nothing, as these cannot be prevented",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "If life-threatening arrhythmias are documented, defibrillator implantation may be considered, because the risk for sudden cardiac death is about 2%. Coronary angioplasty may be indicated in rare cases of medically intractable CAS. Stent implantation may successfully serve as a scaffold to maintain patency in spastic areas that are refractory to medical therapy. The efficacy of coronary bypass is greater in patients with associated coronary atherosclerotic lesions.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 122186,
"questionText": "The patient you are examining with CAS is not responding to pharmaceutical therapy and continues to have documented ventricular arrhythmias. Which is the most appropriate invasive approach to prevent mortality from these life-threatening arrhythmias?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
971990 | /viewarticle/971990 | [
{
"authors": "Liana Meffert; Daniel Miller, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 12-year-old boy presents to the emergency department with bilateral arm pain and notable weakness and numbness that he describes as feeling \"fuzzy.\" The patient reports that approximately 2 weeks ago, he fell off his bicycle and landed on his right arm. He had no head trauma or loss of consciousness as a result of the accident. Since his accident, he has experienced worsening right arm pain, which now extends to his back and left arm and does not radiate.",
"An initial radiograph of the right arm showed no fractures. When left arm pain later developed, cervical and lumbar spine radiographs were ordered, which were negative for spine fracture but raised concern for acromioclavicular joint injury, with an elevation of the distal clavicle relative to the acromion.",
"Last night, the patient was awakened by the pain; this morning, he was unable to grasp objects. His mother brought him to the emergency department. On a review of systems, he notes that yesterday, he began having trouble emptying his bladder. He does not report any recent confusion, dizziness, headaches, nausea, or emesis. His mother has been treating him at home with ibuprofen and acetaminophen, without much relief."
],
"date": "April 18, 2022",
"figures": [],
"markdown": "# A 12-Year-Old With Urinary Retention Who Can't Grasp Objects\n\n **Authors:** Liana Meffert; Daniel Miller, MD \n **Date:** April 18, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 12-year-old boy presents to the emergency department with bilateral arm pain and notable weakness and numbness that he describes as feeling \"fuzzy.\" The patient reports that approximately 2 weeks ago, he fell off his bicycle and landed on his right arm. He had no head trauma or loss of consciousness as a result of the accident. Since his accident, he has experienced worsening right arm pain, which now extends to his back and left arm and does not radiate.\nAn initial radiograph of the right arm showed no fractures. When left arm pain later developed, cervical and lumbar spine radiographs were ordered, which were negative for spine fracture but raised concern for acromioclavicular joint injury, with an elevation of the distal clavicle relative to the acromion.\nLast night, the patient was awakened by the pain; this morning, he was unable to grasp objects. His mother brought him to the emergency department. On a review of systems, he notes that yesterday, he began having trouble emptying his bladder. He does not report any recent confusion, dizziness, headaches, nausea, or emesis. His mother has been treating him at home with ibuprofen and acetaminophen, without much relief.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A 12-Year-Old With Urinary Retention Who Can't Grasp Objects"
},
{
"authors": "Liana Meffert; Daniel Miller, MD",
"content": [
"Upon physical examination, the patient appears anxious and in distress. He holds his neck in a partially flexed position. His heart rate is 76 beats/min, his blood pressure is 143/102 mm Hg, his respiration rate is 15 breaths/min, and his temperature is 97.5 °F (36.4 °C).",
"The patient exhibits tenderness through T2-T10 and can shrug his shoulders but is unable to abduct his arms. He exhibits no tenderness over the acromioclavicular joint or any palpable step-off deformity on examination. Decreased upper-extremity strength is evident bilaterally. Deltoid strength is 0/5 on the right and 2/5 on the left; biceps strength is 0/5 on the right and 3/5 on the left; and triceps strength is 0/5 on the right and 3/5 on the left. Grip strength is 2/5 for the right upper extremity. He has no loss of temperature or other sensation in the upper extremities. The patient has normal reflexes and strength in both lower extremities. He is able to walk without assistance but has difficulty in raising himself from a lying to a standing position.",
"He has a postvoid residual bladder volume of 1 L. The results of a complete blood cell count and a basic metabolic panel are within normal limits.",
"An MRI of the cervical and thoracic spine with and without contrast is ordered."
],
"date": "April 18, 2022",
"figures": [],
"markdown": "# A 12-Year-Old With Urinary Retention Who Can't Grasp Objects\n\n **Authors:** Liana Meffert; Daniel Miller, MD \n **Date:** April 18, 2022\n\n ## Content\n\n Upon physical examination, the patient appears anxious and in distress. He holds his neck in a partially flexed position. His heart rate is 76 beats/min, his blood pressure is 143/102 mm Hg, his respiration rate is 15 breaths/min, and his temperature is 97.5 °F (36.4 °C).\nThe patient exhibits tenderness through T2-T10 and can shrug his shoulders but is unable to abduct his arms. He exhibits no tenderness over the acromioclavicular joint or any palpable step-off deformity on examination. Decreased upper-extremity strength is evident bilaterally. Deltoid strength is 0/5 on the right and 2/5 on the left; biceps strength is 0/5 on the right and 3/5 on the left; and triceps strength is 0/5 on the right and 3/5 on the left. Grip strength is 2/5 for the right upper extremity. He has no loss of temperature or other sensation in the upper extremities. The patient has normal reflexes and strength in both lower extremities. He is able to walk without assistance but has difficulty in raising himself from a lying to a standing position.\nHe has a postvoid residual bladder volume of 1 L. The results of a complete blood cell count and a basic metabolic panel are within normal limits.\nAn MRI of the cervical and thoracic spine with and without contrast is ordered.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1679360,
"choiceText": "Central cord syndrome",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679361,
"choiceText": "Thoracic spine fracture",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679362,
"choiceText": "Acromioclavicular joint dislocation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679363,
"choiceText": "Brachial plexus injury",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 541032,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 12-Year-Old With Urinary Retention Who Can't Grasp Objects"
},
{
"authors": "Liana Meffert; Daniel Miller, MD",
"content": [
"The MRI of the cervical and thoracic spine with and without contrast showed an epidural, possibly subdural, lesion from C7-T5 (Figure 1), with high intrinsic cord signal change at C2-C6 (Figure 2). These findings raised concern for a hematoma compressing the spinal nerve tracts. MRI also revealed a conglomerated lymph node in the left neck at level III/IV and a supraclavicular lymph node measuring 1 cm (Figure 3).",
"Figure 1.",
"Figure 2.",
"Figure 3.",
"Neurosurgery was consulted, and the patient underwent immediate spinal decompression and laminectomy. The operation revealed an intradural extramedullary mass that raised suspicion of a malignant neoplasm. The results of histopathologic examination of the mass pointed to a diagnosis of anaplastic large cell lymphoma (ALCL).",
"ALCL is a form of peripheral T-cell lymphoma that typically has a bimodal distribution, in which the incidence peaks during adolescence and again at about 60 years of age. The classic presentation of ALCL is similar to that of other lymphomas: rapidly progressive adenopathy with the B symptoms of fevers, night sweats, and weight loss. Approximately two thirds of patients present at later stages, with extranodal involvement.",
"The main predictors of prognosis are the presence or absence of an anaplastic lymphoma kinase (ALK) gene mutation, the presence of which is associated with a better outcome, and the International Prognostic Index (IPI), which incorporates the patient's age, serum lactate dehydrogenase level, Eastern Cooperative Oncology Group (ECOG) performance status, Ann Arbor clinical stage, and the number of involved extranodal sites.[1]",
"This patient ultimately received a diagnosis of ALK-positive ALCL. For advanced-stage pediatric non-Hodgkin lymphomas, chemotherapy is the recommended initial treatment. After this patient received chemotherapy, a follow-up MRI of the cervical and thoracic spine showed complete resolution of the extensive neoplastic dural involvement. The enlarged lymph nodes that were noted previously on imaging had also resolved. In addition, his upper-extremity strength had returned to baseline, with minimal residual tingling in his fingertips. Although the data are limited, this patient's ALK-positive status and his initial response to treatment suggest that his prognosis is good."
],
"date": "April 18, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/971/990/971990-Figure1-thumb.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/971/990/971990-Figure2-thumb.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/971/990/971990-Figure3-thumb.png"
}
],
"markdown": "# A 12-Year-Old With Urinary Retention Who Can't Grasp Objects\n\n **Authors:** Liana Meffert; Daniel Miller, MD \n **Date:** April 18, 2022\n\n ## Content\n\n The MRI of the cervical and thoracic spine with and without contrast showed an epidural, possibly subdural, lesion from C7-T5 (Figure 1), with high intrinsic cord signal change at C2-C6 (Figure 2). These findings raised concern for a hematoma compressing the spinal nerve tracts. MRI also revealed a conglomerated lymph node in the left neck at level III/IV and a supraclavicular lymph node measuring 1 cm (Figure 3).\nFigure 1.\nFigure 2.\nFigure 3.\nNeurosurgery was consulted, and the patient underwent immediate spinal decompression and laminectomy. The operation revealed an intradural extramedullary mass that raised suspicion of a malignant neoplasm. The results of histopathologic examination of the mass pointed to a diagnosis of anaplastic large cell lymphoma (ALCL).\nALCL is a form of peripheral T-cell lymphoma that typically has a bimodal distribution, in which the incidence peaks during adolescence and again at about 60 years of age. The classic presentation of ALCL is similar to that of other lymphomas: rapidly progressive adenopathy with the B symptoms of fevers, night sweats, and weight loss. Approximately two thirds of patients present at later stages, with extranodal involvement.\nThe main predictors of prognosis are the presence or absence of an anaplastic lymphoma kinase (ALK) gene mutation, the presence of which is associated with a better outcome, and the International Prognostic Index (IPI), which incorporates the patient's age, serum lactate dehydrogenase level, Eastern Cooperative Oncology Group (ECOG) performance status, Ann Arbor clinical stage, and the number of involved extranodal sites.[1]\nThis patient ultimately received a diagnosis of ALK-positive ALCL. For advanced-stage pediatric non-Hodgkin lymphomas, chemotherapy is the recommended initial treatment. After this patient received chemotherapy, a follow-up MRI of the cervical and thoracic spine showed complete resolution of the extensive neoplastic dural involvement. The enlarged lymph nodes that were noted previously on imaging had also resolved. In addition, his upper-extremity strength had returned to baseline, with minimal residual tingling in his fingertips. Although the data are limited, this patient's ALK-positive status and his initial response to treatment suggest that his prognosis is good.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1679360,
"choiceText": "Central cord syndrome",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679361,
"choiceText": "Thoracic spine fracture",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679362,
"choiceText": "Acromioclavicular joint dislocation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679363,
"choiceText": "Brachial plexus injury",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 541032,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 12-Year-Old With Urinary Retention Who Can't Grasp Objects"
},
{
"authors": "Liana Meffert; Daniel Miller, MD",
"content": [
"Central cord syndrome (CCS) is most frequently associated with traumatic hyperextension of the cervical spinal cord in patients with chronic cervical spondylosis; however, it can also be caused by slow-growing intramedullary tumors, as seen in this patient. CCS is defined as a symptomatic central cord lesion involving either the corticospinal tract (CST) or the anterior horn. As in this patient's presentation, weakness is more evident in the upper extremities than in the lower ones. CCS usually presents without bladder symptoms, although urinary retention can occur. Classically, pain and temperature sensation are impaired, whereas vibration and proprioception are typically uninvolved.",
"The potential differential diagnoses for myelopathy include classic spinal cord syndromes. Brown-Séquard syndrome (BSS), also known as lateral hemisection syndrome, results in ipsilateral weakness via disruption of the CST. Of note, both upper motor neuron (UMN) and lower motor neuron (LMN) lesion signs are evident, with LMN signs at the level of the lesion and UMN signs below the level of the lesion. UMN-positive features include hyperreflexia and spasticity, whereas LMN syndrome is typified by weakness, hyporeflexia, fasciculations, and atrophy.[2]",
"BSS also presents with the loss of proprioception and the contralateral loss of pain, temperature, and fine touch sensation. Proprioception and vibration loss are due to interruption of the posterior dorsal columns (consisting of the fasciculus gracilis, which is responsible for the lower half of the body, and the fasciculus cuneatus, which is responsible for the upper half). Contralateral loss of pain, temperature, and fine touch sensation several levels below the lesion results from interruption of the spinothalamic tract. This finding occurs because the spinothalamic tract crosses to the contralateral side several levels below the lesion.[3]",
"The most common cause of BSS is a traumatic injury, such as a knife or bullet wound, a motor vehicle accident, or blunt trauma. Nontraumatic causes include multiple sclerosis, radiation, and vertebral disc herniation.[4]",
"Dorsal, or posterior, cord syndrome results from the loss of the posterior columns and the lateral CST, as well as the descending central autonomic tracts involved in bladder function. Dorsal column interruption typically causes gait ataxia, whereas CST interruption produces muscle weakness and ultimately hyperreflexia and hypertonia when chronic. Although many possible etiologies exist, some of the better-known ones include multiple sclerosis, tabes dorsalis (secondary to tertiary neurosyphilis), and Friedreich ataxia, a hereditary trinucleotide repeat expansion.",
"In contrast, anterior cord syndrome typically spares the dorsal columns and affects only the anterior two thirds of the spinal cord, which includes the CST and spinothalamic tracts as well as the autonomic tracts involved in bladder control. The most common causes of anterior cord syndrome are spinal cord infarction (of the anterior spinal artery), intervertebral disc herniation, and radiation myelopathy (a complication of radiation therapy).",
"The conus medullaris typically terminates around the L1 vertebra[5]; thus, lesions near L1 can result in conus medullaris syndrome, which presents with distinct sphincter dysfunction, urinary and/or anal incontinence or constipation, impotence, and the oft-cited saddle sensory loss.[6] In contrast to cauda equina syndrome, the deficits are usually symmetric, and lower-extremity weakness may not be present. Typical causes include disc herniation, spinal fracture and, less commonly, tumors that compress the spinal cord.[6]",
"Another possible initial presentation for patients with neurologic symptoms induced by neoplasms is neoplastic epidural spinal cord compression (ESCC), which is the first sign of cancer in approximately 20% of patients.[7] In children, the tumors that are most commonly responsible for ESCC include sarcomas, neuroblastomas, germ cell neoplasms, and Hodgkin lymphoma.[8] ESCC usually occurs in the thoracic spine (60%-70%) and presents with pain that is often worse at night and predates neurologic dysfunction by an average of 7 weeks.[9] Motor findings indicate more advanced stages of ESCC, whereas the degree of weakness coincides with the degree of severity.[10] Urinary retention is considered the most common autonomic dysfunction finding yet is rarely the only presenting symptom in ESCC.[11]",
"MRI is considered the criterion standard for the diagnosis of ESCC. A retrospective study evaluating the diagnostic accuracy of MRI in the detection of neoplastic spinal cord compression and cauda equina syndrome in patients presenting with myelopathy found a high sensitivity of 93% and specificity of 97%.[12] CT is considered a second-line option when MRI is contraindicated."
],
"date": "April 18, 2022",
"figures": [],
"markdown": "# A 12-Year-Old With Urinary Retention Who Can't Grasp Objects\n\n **Authors:** Liana Meffert; Daniel Miller, MD \n **Date:** April 18, 2022\n\n ## Content\n\n Central cord syndrome (CCS) is most frequently associated with traumatic hyperextension of the cervical spinal cord in patients with chronic cervical spondylosis; however, it can also be caused by slow-growing intramedullary tumors, as seen in this patient. CCS is defined as a symptomatic central cord lesion involving either the corticospinal tract (CST) or the anterior horn. As in this patient's presentation, weakness is more evident in the upper extremities than in the lower ones. CCS usually presents without bladder symptoms, although urinary retention can occur. Classically, pain and temperature sensation are impaired, whereas vibration and proprioception are typically uninvolved.\nThe potential differential diagnoses for myelopathy include classic spinal cord syndromes. Brown-Séquard syndrome (BSS), also known as lateral hemisection syndrome, results in ipsilateral weakness via disruption of the CST. Of note, both upper motor neuron (UMN) and lower motor neuron (LMN) lesion signs are evident, with LMN signs at the level of the lesion and UMN signs below the level of the lesion. UMN-positive features include hyperreflexia and spasticity, whereas LMN syndrome is typified by weakness, hyporeflexia, fasciculations, and atrophy.[2]\nBSS also presents with the loss of proprioception and the contralateral loss of pain, temperature, and fine touch sensation. Proprioception and vibration loss are due to interruption of the posterior dorsal columns (consisting of the fasciculus gracilis, which is responsible for the lower half of the body, and the fasciculus cuneatus, which is responsible for the upper half). Contralateral loss of pain, temperature, and fine touch sensation several levels below the lesion results from interruption of the spinothalamic tract. This finding occurs because the spinothalamic tract crosses to the contralateral side several levels below the lesion.[3]\nThe most common cause of BSS is a traumatic injury, such as a knife or bullet wound, a motor vehicle accident, or blunt trauma. Nontraumatic causes include multiple sclerosis, radiation, and vertebral disc herniation.[4]\nDorsal, or posterior, cord syndrome results from the loss of the posterior columns and the lateral CST, as well as the descending central autonomic tracts involved in bladder function. Dorsal column interruption typically causes gait ataxia, whereas CST interruption produces muscle weakness and ultimately hyperreflexia and hypertonia when chronic. Although many possible etiologies exist, some of the better-known ones include multiple sclerosis, tabes dorsalis (secondary to tertiary neurosyphilis), and Friedreich ataxia, a hereditary trinucleotide repeat expansion.\nIn contrast, anterior cord syndrome typically spares the dorsal columns and affects only the anterior two thirds of the spinal cord, which includes the CST and spinothalamic tracts as well as the autonomic tracts involved in bladder control. The most common causes of anterior cord syndrome are spinal cord infarction (of the anterior spinal artery), intervertebral disc herniation, and radiation myelopathy (a complication of radiation therapy).\nThe conus medullaris typically terminates around the L1 vertebra[5]; thus, lesions near L1 can result in conus medullaris syndrome, which presents with distinct sphincter dysfunction, urinary and/or anal incontinence or constipation, impotence, and the oft-cited saddle sensory loss.[6] In contrast to cauda equina syndrome, the deficits are usually symmetric, and lower-extremity weakness may not be present. Typical causes include disc herniation, spinal fracture and, less commonly, tumors that compress the spinal cord.[6]\nAnother possible initial presentation for patients with neurologic symptoms induced by neoplasms is neoplastic epidural spinal cord compression (ESCC), which is the first sign of cancer in approximately 20% of patients.[7] In children, the tumors that are most commonly responsible for ESCC include sarcomas, neuroblastomas, germ cell neoplasms, and Hodgkin lymphoma.[8] ESCC usually occurs in the thoracic spine (60%-70%) and presents with pain that is often worse at night and predates neurologic dysfunction by an average of 7 weeks.[9] Motor findings indicate more advanced stages of ESCC, whereas the degree of weakness coincides with the degree of severity.[10] Urinary retention is considered the most common autonomic dysfunction finding yet is rarely the only presenting symptom in ESCC.[11]\nMRI is considered the criterion standard for the diagnosis of ESCC. A retrospective study evaluating the diagnostic accuracy of MRI in the detection of neoplastic spinal cord compression and cauda equina syndrome in patients presenting with myelopathy found a high sensitivity of 93% and specificity of 97%.[12] CT is considered a second-line option when MRI is contraindicated.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A 12-Year-Old With Urinary Retention Who Can't Grasp Objects"
},
{
"authors": "Liana Meffert; Daniel Miller, MD",
"content": [
"In less than 1% of patients who present to primary care with a chief complaint of back pain, the cause is a malignant neoplasm (primary or metastatic), spinal cord compression, cauda equina syndrome, or infection.[13] To decide which patients require further evaluation with advanced imaging, look for \"red flag\" signs and symptoms in conjunction with risk factors and select the imaging modality that is best suited to the specific clinical concern.",
"Pain that begins abruptly and is associated with point tenderness is suggestive of spinal fracture, and plain radiography (less radiation but less sensitive) or CT (more radiation but also more sensitive) should be considered to evaluate for bone abnormalities. Weakness that correlates with a spinal sensory level raises concern for spinal cord injury. Bladder or bowel incontinence or retention suggests spinal cord compression. The spinal cord is best imaged with MRI; thus, this modality is preferred for evaluating pathology of the spinal cord.",
"A history of cancer raises suspicion for metastatic disease, which can cause vertebral compression, fractures, and/or spinal cord compression. A history of intravenous drug use places a patient at risk for vertebral osteomyelitis or an epidural abscess. If vertebral fractures are suspected, CT is adequate in most cases. If cord compression from metastatic disease or an abscess is suspected, MRI is generally preferred.",
"The patient in this case had urinary retention and signs of cord compression (arm weakness) on physical examination. Although vertebral injury was suspected, the most urgent concern was for cord compression. In addition, avoiding ionizing radiation when feasible is desirable in children because they have more active cell division than adults do and are thus at higher risk for the mutagenic effects of ionizing radiation (as involved in CT). For all these reasons, MRI was used in this case.",
"Last, this case is an interesting example of spinal cord injury without radiographic abnormality (SCIWORA), defined as objective signs of neurologic deficits or reported paresthesia, numbness, or paralysis, without findings on plain radiographs or CT. With the advent of MRI, a reported two thirds of cases that were historically considered to be SCIWORA exhibited evident pathology on MRI.[14] This case reinforces the importance of considering the possibility of spinal cord injury in the presence of new or progressing neurologic findings and the absence of initial radiographic evidence."
],
"date": "April 18, 2022",
"figures": [],
"markdown": "# A 12-Year-Old With Urinary Retention Who Can't Grasp Objects\n\n **Authors:** Liana Meffert; Daniel Miller, MD \n **Date:** April 18, 2022\n\n ## Content\n\n In less than 1% of patients who present to primary care with a chief complaint of back pain, the cause is a malignant neoplasm (primary or metastatic), spinal cord compression, cauda equina syndrome, or infection.[13] To decide which patients require further evaluation with advanced imaging, look for \"red flag\" signs and symptoms in conjunction with risk factors and select the imaging modality that is best suited to the specific clinical concern.\nPain that begins abruptly and is associated with point tenderness is suggestive of spinal fracture, and plain radiography (less radiation but less sensitive) or CT (more radiation but also more sensitive) should be considered to evaluate for bone abnormalities. Weakness that correlates with a spinal sensory level raises concern for spinal cord injury. Bladder or bowel incontinence or retention suggests spinal cord compression. The spinal cord is best imaged with MRI; thus, this modality is preferred for evaluating pathology of the spinal cord.\nA history of cancer raises suspicion for metastatic disease, which can cause vertebral compression, fractures, and/or spinal cord compression. A history of intravenous drug use places a patient at risk for vertebral osteomyelitis or an epidural abscess. If vertebral fractures are suspected, CT is adequate in most cases. If cord compression from metastatic disease or an abscess is suspected, MRI is generally preferred.\nThe patient in this case had urinary retention and signs of cord compression (arm weakness) on physical examination. Although vertebral injury was suspected, the most urgent concern was for cord compression. In addition, avoiding ionizing radiation when feasible is desirable in children because they have more active cell division than adults do and are thus at higher risk for the mutagenic effects of ionizing radiation (as involved in CT). For all these reasons, MRI was used in this case.\nLast, this case is an interesting example of spinal cord injury without radiographic abnormality (SCIWORA), defined as objective signs of neurologic deficits or reported paresthesia, numbness, or paralysis, without findings on plain radiographs or CT. With the advent of MRI, a reported two thirds of cases that were historically considered to be SCIWORA exhibited evident pathology on MRI.[14] This case reinforces the importance of considering the possibility of spinal cord injury in the presence of new or progressing neurologic findings and the absence of initial radiographic evidence.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1679364,
"choiceText": "Two-week history of back pain that radiates to the right leg",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679365,
"choiceText": "New-onset urinary retention in a patient with 4 days of back pain",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679366,
"choiceText": "Low back pain that occurred after heavy lifting",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679367,
"choiceText": "Chronic urinary retention in a patient with 1 week of back pain",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Although back pain that lasts 4 days is not immediately concerning, the new-onset urinary retention exemplifies a \"red flag\" symptom and suggests spinal cord compression. In the absence of red flags, back pain that lasts less than 4 weeks generally does not require consideration of imaging.<sup>[13]</sup>\r\nNumerous studies have established the inefficacy and potential for harm with the overuse of imaging. Back pain is very common, and unnecessary imaging increases healthcare costs without improving patient outcomes. In some cases, gratuitous imaging leads to further workup and nonbeneficial intervention and, in the instance of CT, exposes the patient to ionizing radiation. In the absence of progressive and severe neurologic deficits or signs and symptoms that suggest an etiology causing spinal cord compression (eg, neurologic findings on examination), routine diagnostic imaging for patients who present with low back pain does not lead to better outcomes. <sup>[15,16]</sup>\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 541033,
"questionText": "Which associated symptom warrants emergent imaging in a patient who presents with back pain?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1679368,
"choiceText": "Loss of fine touch, vibration, and pressure sensation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679369,
"choiceText": "Ipsilateral loss of motor function",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679370,
"choiceText": "Motor paresis that is greater in the upper extremities than in the lower extremities",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679371,
"choiceText": "Ipsilateral loss of motor, pain, and temperature sensation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Owing to the anatomical organization of the spinal cord, CCS is characterized by bilateral paresis that is greater in the upper extremities than in the lower extremities, bladder dysfunction, and sensory loss below the level of the injury. Loss of fine touch, vibration, and pressure sensation would be caused by damage to the posterior columns of the spinal cord, which are usually uninvolved in CCS. In addition, ipsilateral loss of motor function, with contralateral pain and temperature sensation loss, is classically associated with BSS. This finding is present on opposing sides of the body because the spinothalamic tract crosses contralaterally in the ventral commissure before ascending.<sup>[17]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 541034,
"questionText": "Which is a common presentation of CCS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 12-Year-Old With Urinary Retention Who Can't Grasp Objects"
},
{
"authors": "Liana Meffert; Daniel Miller, MD",
"content": [],
"date": "April 18, 2022",
"figures": [],
"markdown": "# A 12-Year-Old With Urinary Retention Who Can't Grasp Objects\n\n **Authors:** Liana Meffert; Daniel Miller, MD \n **Date:** April 18, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1679364,
"choiceText": "Two-week history of back pain that radiates to the right leg",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679365,
"choiceText": "New-onset urinary retention in a patient with 4 days of back pain",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679366,
"choiceText": "Low back pain that occurred after heavy lifting",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679367,
"choiceText": "Chronic urinary retention in a patient with 1 week of back pain",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Although back pain that lasts 4 days is not immediately concerning, the new-onset urinary retention exemplifies a \"red flag\" symptom and suggests spinal cord compression. In the absence of red flags, back pain that lasts less than 4 weeks generally does not require consideration of imaging.<sup>[13]</sup>\r\nNumerous studies have established the inefficacy and potential for harm with the overuse of imaging. Back pain is very common, and unnecessary imaging increases healthcare costs without improving patient outcomes. In some cases, gratuitous imaging leads to further workup and nonbeneficial intervention and, in the instance of CT, exposes the patient to ionizing radiation. In the absence of progressive and severe neurologic deficits or signs and symptoms that suggest an etiology causing spinal cord compression (eg, neurologic findings on examination), routine diagnostic imaging for patients who present with low back pain does not lead to better outcomes. <sup>[15,16]</sup>\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 541033,
"questionText": "Which associated symptom warrants emergent imaging in a patient who presents with back pain?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1679368,
"choiceText": "Loss of fine touch, vibration, and pressure sensation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679369,
"choiceText": "Ipsilateral loss of motor function",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679370,
"choiceText": "Motor paresis that is greater in the upper extremities than in the lower extremities",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679371,
"choiceText": "Ipsilateral loss of motor, pain, and temperature sensation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Owing to the anatomical organization of the spinal cord, CCS is characterized by bilateral paresis that is greater in the upper extremities than in the lower extremities, bladder dysfunction, and sensory loss below the level of the injury. Loss of fine touch, vibration, and pressure sensation would be caused by damage to the posterior columns of the spinal cord, which are usually uninvolved in CCS. In addition, ipsilateral loss of motor function, with contralateral pain and temperature sensation loss, is classically associated with BSS. This finding is present on opposing sides of the body because the spinothalamic tract crosses contralaterally in the ventral commissure before ascending.<sup>[17]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 541034,
"questionText": "Which is a common presentation of CCS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 12-Year-Old With Urinary Retention Who Can't Grasp Objects"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1679360,
"choiceText": "Central cord syndrome",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679361,
"choiceText": "Thoracic spine fracture",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679362,
"choiceText": "Acromioclavicular joint dislocation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679363,
"choiceText": "Brachial plexus injury",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 541032,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1679364,
"choiceText": "Two-week history of back pain that radiates to the right leg",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679365,
"choiceText": "New-onset urinary retention in a patient with 4 days of back pain",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679366,
"choiceText": "Low back pain that occurred after heavy lifting",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679367,
"choiceText": "Chronic urinary retention in a patient with 1 week of back pain",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Although back pain that lasts 4 days is not immediately concerning, the new-onset urinary retention exemplifies a \"red flag\" symptom and suggests spinal cord compression. In the absence of red flags, back pain that lasts less than 4 weeks generally does not require consideration of imaging.<sup>[13]</sup>\r\nNumerous studies have established the inefficacy and potential for harm with the overuse of imaging. Back pain is very common, and unnecessary imaging increases healthcare costs without improving patient outcomes. In some cases, gratuitous imaging leads to further workup and nonbeneficial intervention and, in the instance of CT, exposes the patient to ionizing radiation. In the absence of progressive and severe neurologic deficits or signs and symptoms that suggest an etiology causing spinal cord compression (eg, neurologic findings on examination), routine diagnostic imaging for patients who present with low back pain does not lead to better outcomes. <sup>[15,16]</sup>\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 541033,
"questionText": "Which associated symptom warrants emergent imaging in a patient who presents with back pain?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1679368,
"choiceText": "Loss of fine touch, vibration, and pressure sensation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679369,
"choiceText": "Ipsilateral loss of motor function",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679370,
"choiceText": "Motor paresis that is greater in the upper extremities than in the lower extremities",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1679371,
"choiceText": "Ipsilateral loss of motor, pain, and temperature sensation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Owing to the anatomical organization of the spinal cord, CCS is characterized by bilateral paresis that is greater in the upper extremities than in the lower extremities, bladder dysfunction, and sensory loss below the level of the injury. Loss of fine touch, vibration, and pressure sensation would be caused by damage to the posterior columns of the spinal cord, which are usually uninvolved in CCS. In addition, ipsilateral loss of motor function, with contralateral pain and temperature sensation loss, is classically associated with BSS. This finding is present on opposing sides of the body because the spinothalamic tract crosses contralaterally in the ventral commissure before ascending.<sup>[17]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 541034,
"questionText": "Which is a common presentation of CCS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
971546 | /viewarticle/971546 | [
{
"authors": "Mounika Gangireddy, MD, MBBS",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"An otherwise healthy 46-year-old woman presents with diffuse abdominal pain that awakens her from sleep. She describes the pain as sharp, 10/10 in intensity, and constant in nature. The pain worsens with movement. She reports no fevers or chills, rectal bleeding, melena, hematemesis, vomiting, or change in bowel habits.",
"Polycystic ovarian syndrome was previously diagnosed in this patient and is managed with lifestyle changes. She had iron deficiency anemia from menorrhagia and took iron supplements for a brief period. She has a remote history of deep venous thrombosis and pulmonary embolism and was treated with warfarin for 6 months. Her surgical history includes a gastric bypass procedure and a myomectomy. She has never smoked and does not consume alcohol but does use cannabis occasionally. She lives with her children. She takes over-the-counter vitamin supplements. Her family history is not significant for cancers or clotting disorders."
],
"date": "April 13, 2022",
"figures": [],
"markdown": "# Oncology Case Challenge: A 46-Year-Old Mother With Severe, Constant Abdominal Pain\n\n **Authors:** Mounika Gangireddy, MD, MBBS \n **Date:** April 13, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nAn otherwise healthy 46-year-old woman presents with diffuse abdominal pain that awakens her from sleep. She describes the pain as sharp, 10/10 in intensity, and constant in nature. The pain worsens with movement. She reports no fevers or chills, rectal bleeding, melena, hematemesis, vomiting, or change in bowel habits.\nPolycystic ovarian syndrome was previously diagnosed in this patient and is managed with lifestyle changes. She had iron deficiency anemia from menorrhagia and took iron supplements for a brief period. She has a remote history of deep venous thrombosis and pulmonary embolism and was treated with warfarin for 6 months. Her surgical history includes a gastric bypass procedure and a myomectomy. She has never smoked and does not consume alcohol but does use cannabis occasionally. She lives with her children. She takes over-the-counter vitamin supplements. Her family history is not significant for cancers or clotting disorders.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Oncology Case Challenge: A 46-Year-Old Mother With Severe, Constant Abdominal Pain"
},
{
"authors": "Mounika Gangireddy, MD, MBBS",
"content": [
"Upon physical examination, the patient appears to be in moderate distress. Her heart rate is 110 beats/min, her respiration rate is 20 breaths/min, and her oxygen saturation level is 95% on room air. She is afebrile. Her head appears normal and shows no trauma. Her abdomen is soft and diffusely tender to palpation in all four quadrants. No lymphadenopathy or hepatosplenomegaly is noted. Her lungs are clear to auscultation, and S1 and S2 heart sounds are audible.",
"Laboratory studies reveal these values:",
"White blood cell (WBC) count: 7800 cells/µL, with 61% neutrophils, 8% basophils (reference range, 3800-10,500 cells/µL, with 55%-70% neutrophils, 0.5%-1% basophils)",
"Hemoglobin level: 9.6 g/dL (reference range, 11.8-15.7 g/dL)",
"Platelet count: 3,056,000 cells/µL (reference range, 150,000-369,000 cells/µL)",
"International normalized ratio: 0.97 (reference range, < 1.1)",
"Partial thromboplastin time: 24.3 sec (reference range, 60-70 sec)",
"Lactate dehydrogenase level: 235 U/L (reference range, 140-280 U/L)",
"Iron saturation and ferritin level: 8% (reference range, 15%-45%) and 8 ng/mL (reference range, 11-250 ng/mL), respectively",
"Folate level: 15.4 ng/mL (reference range, > 5.8 ng/mL)",
"Vitamin B12 level: 352 pg/mL (reference range, 180-914 pg/mL)",
"Sodium level: 138 mmol/L (reference range, 135-145 mmol/L)",
"Potassium level: 4.5 mmol/L (reference range, 3.6-5.2 mmol/L)",
"Chloride level: 107 mmol/L (reference range, 96-106 mmol/L)",
"Blood urea nitrogen level: 10 mg/dL (reference range, 6-24 mg/dL)",
"Creatinine level: 1.1 mg/dL (reference range, 0.6-1.2 mg/dL)",
"Alkaline phosphatase level: 65 IU/L (reference range, 44-147 IU/L)",
"Alanine aminotransferase level: 19 IU/L (reference range, 4-36 IU/L)",
"Aspartate aminotransferase level: 32 U/L (reference range, 8-33 U/L)",
"Total bilirubin level: 0.8 mg/dL (reference range, 0.1-1.2 mg/dL)",
"Flow cytometry reveals no evidence of immunophenotypically abnormal T or B cells.",
"A CT of the abdomen and pelvis shows hemorrhagic products in the left pelvic region, likely secondary to a ruptured ovarian cyst. No active extravasation of dye is noted.",
"The peripheral blood smear reveals thrombocytosis and polychromatophilic red cells with circulating blasts (Figures 1 and 2). Examination of the bone marrow shows hypercellular marrow with increased megakaryocytes (Figures 3 and 4).",
"Figure 1.",
"Figure 2.",
"Figure 3.",
"Figure 4.",
"The results of bone marrow cytogenetic analysis are positive for t(9;22). A review of outside records shows that the patient had an elevated platelet count of approximately 900,000 cells/µL several years prior to the current presentation. The elevation was thought to be reactive from her known iron deficiency. She was lost to follow-up."
],
"date": "April 13, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/971/546/971546-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/971/546/971546-Thumb2.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/971/546/971546-Thumb3.png"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/971/546/971546-Thumb4.png"
}
],
"markdown": "# Oncology Case Challenge: A 46-Year-Old Mother With Severe, Constant Abdominal Pain\n\n **Authors:** Mounika Gangireddy, MD, MBBS \n **Date:** April 13, 2022\n\n ## Content\n\n Upon physical examination, the patient appears to be in moderate distress. Her heart rate is 110 beats/min, her respiration rate is 20 breaths/min, and her oxygen saturation level is 95% on room air. She is afebrile. Her head appears normal and shows no trauma. Her abdomen is soft and diffusely tender to palpation in all four quadrants. No lymphadenopathy or hepatosplenomegaly is noted. Her lungs are clear to auscultation, and S1 and S2 heart sounds are audible.\nLaboratory studies reveal these values:\nWhite blood cell (WBC) count: 7800 cells/µL, with 61% neutrophils, 8% basophils (reference range, 3800-10,500 cells/µL, with 55%-70% neutrophils, 0.5%-1% basophils)\nHemoglobin level: 9.6 g/dL (reference range, 11.8-15.7 g/dL)\nPlatelet count: 3,056,000 cells/µL (reference range, 150,000-369,000 cells/µL)\nInternational normalized ratio: 0.97 (reference range, < 1.1)\nPartial thromboplastin time: 24.3 sec (reference range, 60-70 sec)\nLactate dehydrogenase level: 235 U/L (reference range, 140-280 U/L)\nIron saturation and ferritin level: 8% (reference range, 15%-45%) and 8 ng/mL (reference range, 11-250 ng/mL), respectively\nFolate level: 15.4 ng/mL (reference range, > 5.8 ng/mL)\nVitamin B12 level: 352 pg/mL (reference range, 180-914 pg/mL)\nSodium level: 138 mmol/L (reference range, 135-145 mmol/L)\nPotassium level: 4.5 mmol/L (reference range, 3.6-5.2 mmol/L)\nChloride level: 107 mmol/L (reference range, 96-106 mmol/L)\nBlood urea nitrogen level: 10 mg/dL (reference range, 6-24 mg/dL)\nCreatinine level: 1.1 mg/dL (reference range, 0.6-1.2 mg/dL)\nAlkaline phosphatase level: 65 IU/L (reference range, 44-147 IU/L)\nAlanine aminotransferase level: 19 IU/L (reference range, 4-36 IU/L)\nAspartate aminotransferase level: 32 U/L (reference range, 8-33 U/L)\nTotal bilirubin level: 0.8 mg/dL (reference range, 0.1-1.2 mg/dL)\nFlow cytometry reveals no evidence of immunophenotypically abnormal T or B cells.\nA CT of the abdomen and pelvis shows hemorrhagic products in the left pelvic region, likely secondary to a ruptured ovarian cyst. No active extravasation of dye is noted.\nThe peripheral blood smear reveals thrombocytosis and polychromatophilic red cells with circulating blasts (Figures 1 and 2). Examination of the bone marrow shows hypercellular marrow with increased megakaryocytes (Figures 3 and 4).\nFigure 1.\nFigure 2.\nFigure 3.\nFigure 4.\nThe results of bone marrow cytogenetic analysis are positive for t(9;22). A review of outside records shows that the patient had an elevated platelet count of approximately 900,000 cells/µL several years prior to the current presentation. The elevation was thought to be reactive from her known iron deficiency. She was lost to follow-up.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1677609,
"choiceText": "Essential thrombocytosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677610,
"choiceText": "Severe iron deficiency anemia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677611,
"choiceText": "Chronic myeloid leukemia",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677612,
"choiceText": "Chronic lymphocytic leukemia\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 540372,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Oncology Case Challenge: A 46-Year-Old Mother With Severe, Constant Abdominal Pain"
},
{
"authors": "Mounika Gangireddy, MD, MBBS",
"content": [
"Thrombocytosis (> 600,000 cells/µL) occurs in about 15%-30% of patients with chronic myeloid leukemia (CML). Approximately 20% of patients present with bleeding complications due to dysfunctional platelets, as in this case. This patient had an atypical presentation of CML with marked thrombocytosis without leukocytosis, which made the diagnosis challenging.",
"The differential diagnosis of CML includes leukemoid reaction, myeloproliferative disorders, essential thrombocythemia, and polycythemia vera with iron deficiency. Leukemoid reaction presents with an elevated WBC count (< 50 × 109/L), toxic vacuolation, Döhle bodies, and an absence of basophilia.",
"It is difficult to differentiate myeloproliferative or myelodysplastic syndrome from CML owing to the presence of thrombocytosis, neutrophilia, and splenomegaly in both diseases. Bone marrow biopsy and mutational analysis are helpful in such instances. Patients who have polycythemia vera with severe iron deficiency can exhibit leukocytosis and thrombocytosis. Such patients have normal or increased leukocyte alkaline phosphatase scores with a WBC count < 25 × 109/L and no Philadelphia (Ph) abnormality.",
"In the patient in this case, other causes of thrombocytosis were excluded by JAK-2V617, exon 12, MPL exon 10, CALR exon 9, and CSF3R exon 14/17 mutation analyses. The results were all negative, thus ruling out myeloproliferative disorders. Chronic lymphocytic leukemia (CLL) is less likely given the left-shifted marrow and normal flow cytometry results. Severe iron deficiency can result in thrombocytosis. However, it does not solely explain the platelet count of over 3 million cells/µL with the presence of Ph chromosome. Quantitative polymerase chain reaction (PCR) testing for percentage of BCR-ABL1/Abl1 was elevated at 66%, with detection of p210 BCR-ABL transcript along with the presence of t(9;22) on the bone marrow sample. These findings confirmed the diagnosis of CML.",
"CML is a clonal myeloproliferative disorder of pluripotent stem cells. It accounts for about 10%-15% of adult leukemias. The incidence is 1-2 per 100,000, and the prevalence is 5 per 100,000 adults.[1] The 10-year overall survival rates have increased from 20% to 90% with the introduction of tyrosine kinase inhibitors (TKIs).[2]"
],
"date": "April 13, 2022",
"figures": [],
"markdown": "# Oncology Case Challenge: A 46-Year-Old Mother With Severe, Constant Abdominal Pain\n\n **Authors:** Mounika Gangireddy, MD, MBBS \n **Date:** April 13, 2022\n\n ## Content\n\n Thrombocytosis (> 600,000 cells/µL) occurs in about 15%-30% of patients with chronic myeloid leukemia (CML). Approximately 20% of patients present with bleeding complications due to dysfunctional platelets, as in this case. This patient had an atypical presentation of CML with marked thrombocytosis without leukocytosis, which made the diagnosis challenging.\nThe differential diagnosis of CML includes leukemoid reaction, myeloproliferative disorders, essential thrombocythemia, and polycythemia vera with iron deficiency. Leukemoid reaction presents with an elevated WBC count (< 50 × 109/L), toxic vacuolation, Döhle bodies, and an absence of basophilia.\nIt is difficult to differentiate myeloproliferative or myelodysplastic syndrome from CML owing to the presence of thrombocytosis, neutrophilia, and splenomegaly in both diseases. Bone marrow biopsy and mutational analysis are helpful in such instances. Patients who have polycythemia vera with severe iron deficiency can exhibit leukocytosis and thrombocytosis. Such patients have normal or increased leukocyte alkaline phosphatase scores with a WBC count < 25 × 109/L and no Philadelphia (Ph) abnormality.\nIn the patient in this case, other causes of thrombocytosis were excluded by JAK-2V617, exon 12, MPL exon 10, CALR exon 9, and CSF3R exon 14/17 mutation analyses. The results were all negative, thus ruling out myeloproliferative disorders. Chronic lymphocytic leukemia (CLL) is less likely given the left-shifted marrow and normal flow cytometry results. Severe iron deficiency can result in thrombocytosis. However, it does not solely explain the platelet count of over 3 million cells/µL with the presence of Ph chromosome. Quantitative polymerase chain reaction (PCR) testing for percentage of BCR-ABL1/Abl1 was elevated at 66%, with detection of p210 BCR-ABL transcript along with the presence of t(9;22) on the bone marrow sample. These findings confirmed the diagnosis of CML.\nCML is a clonal myeloproliferative disorder of pluripotent stem cells. It accounts for about 10%-15% of adult leukemias. The incidence is 1-2 per 100,000, and the prevalence is 5 per 100,000 adults.[1] The 10-year overall survival rates have increased from 20% to 90% with the introduction of tyrosine kinase inhibitors (TKIs).[2]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1677609,
"choiceText": "Essential thrombocytosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677610,
"choiceText": "Severe iron deficiency anemia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677611,
"choiceText": "Chronic myeloid leukemia",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677612,
"choiceText": "Chronic lymphocytic leukemia\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 540372,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Oncology Case Challenge: A 46-Year-Old Mother With Severe, Constant Abdominal Pain"
},
{
"authors": "Mounika Gangireddy, MD, MBBS",
"content": [
"The pathogenesis of CML is fusion of the ABL1 gene on chromosome 9 with the BCR gene on chromosome 22, resulting in overexpression of the oncoprotein BCR-ABL1.[3] This translocation, t(9;22), is known as the Ph chromosome. Ninety percent of patients with CML harbor Ph chromosome, whereas 5% have Ph variants; the other 5% are Ph-negative by cytogenetic analysis but are positive for BCR-ABL by fluorescence in situ hybridization (FISH) and PCR. BCR-ABL1 is a tyrosine kinase that promotes growth and replication by increasing signaling pathways such as STAT, RAS, RAF, JUN kinase, and MYC.[4]",
"About 50% of patients with CML are asymptomatic, and the disease is diagnosed during routine blood tests. The clinical presentation consists of leukocytosis, splenomegaly, thrombocytosis, and anemia. Symptoms vary and include early satiety, left upper quadrant pain, fatigue, malaise, weight loss, thrombosis, and bleeding episodes.",
"The diagnosis of typical CML is based on persistent leukocytosis along with detection of the Ph chromosome abnormality and t(9;22) (q34; q11) or Ph-related molecular BCR-ABL1 abnormalities by FISH or molecular studies. Baseline chromosome banding analysis is required to evaluate for clonal evolution, i(17) (q10)-7/del7q, and 3q26.2 rearrangements.[5] These findings are associated with a relatively poor prognosis. The most common BCR-ABL transcript is p210, and p190 is rare in CML but often seen in Ph-positive acute lymphoblastic leukemia.",
"Because of this patient's initial presentation with thrombocytosis and bleeding, CML was always in the differential diagnosis. The peripheral blood smear that showed neutrophilia, basophilia, and eosinophilia prompted BCR-ABL PCR testing, which confirmed the diagnosis.",
"CML is divided into three phases: chronic, accelerated, and blast. The blast phase (BP) is defined as the presence ≥ 30% blasts. The accelerated phase (AP) is defined as peripheral blood or bone marrow blasts of 10%-19%, peripheral blood basophils ≥ 20%, or the presence of cytogenetic evolution.",
"To determine the phase of CML, this patient underwent bone marrow biopsy. The biopsy revealed hypercellular marrow (90%) with normal myeloid to erythroid ratio, granulopoiesis with left shift, and increased blasts (15% of marrow cellularity). The results of cytogenetic analysis were positive for t(9;22). Her CML was classified as CML-AP owing to the presence of 15% blasts in the marrow.",
"There are several prognostic scores for CML, such as Sokal, Euro/Hasford, EUTOS (EUropean Treatment Outcome Study), and ELTS (EUTOS long-term survival).[6,7,8] The Sokal score is a widely used prognostic index that includes age, size of the spleen, platelets, and blasts. On the basis of this score, patients are classified into low- (0.8), intermediate- (0.8-1.2), and high- (> 1.2) risk. With a score of 4.5, this patient is considered high-risk, with a 2-year overall survival of 65% and a median overall survival of 2.5-5 years.",
"While the results of diagnostic studies are pending, hydroxyurea can be used for cytoreduction. The recommended dosage of hydroxyurea is 20-40 mg/kg/d in divided doses until a diagnosis is obtained. Hydroxyurea, 40 mg/kg/d, was started in this patient for cytoreduction.",
"TKIs are the mainstay of treatment. TKIs are designed to block interaction between the BCR-ABL1 protein and adenosine triphosphate, halting the proliferation of leukemic cells. Available treatment options include:",
"First-generation TKI: imatinib",
"Second-generation TKIs: dasatinib, nilotinib, and bosutinib",
"Third-generation TKI: ponatinib",
"Omacetaxine",
"Imatinib was the first TKI approved by the US Food and Drug Administration for chronic-phase CML (CML-CP) on the basis of the results of the International Randomized Study of Interferon and STI571 (IRIS) trial.[9,10] It improved event-free survival (80%) and 10-year overall survival (83%).",
"The DASISION trial compared the second-generation TKI dasatinib with imatinib. Dasatinib provided deeper and faster responses when compared with imatinib, but there was no improvement in overall survival or event-free survival.[11,12,13] The ENESTnd study and the BFORE study compared nilotinib and bosutinib with imatinib, respectively, and again revealed deeper responses without an improvement in overall survival.[14,15] Based on the results of these trials, second-generation TKIs are the first-line choice to treat CML.",
"Ponatinib is approved by the FDA as a second-line agent in patients who have a T315I mutation.[16,17] Omacetaxine is approved for patients who have disease progression on more than two TKIs.[18]",
"The doses of TKIs used in chronic and advanced phases of CML are listed in the Table.",
"Table. Doses of TKIs in Chronic and Advanced Phases of CML",
"Phase",
"Imatinib",
"Dasatinib",
"Bosutinib",
"Nilotinib",
"Ponatinib",
"Chronic",
"400 mg/d",
"100 mg/d",
"400 mg/d",
"300 mg twice daily",
"45 mg/d",
"Advanced",
"600 mg/d",
"140 mg/d",
"500 mg/d",
"400 mg twice daily",
"45 mg/d"
],
"date": "April 13, 2022",
"figures": [],
"markdown": "# Oncology Case Challenge: A 46-Year-Old Mother With Severe, Constant Abdominal Pain\n\n **Authors:** Mounika Gangireddy, MD, MBBS \n **Date:** April 13, 2022\n\n ## Content\n\n The pathogenesis of CML is fusion of the ABL1 gene on chromosome 9 with the BCR gene on chromosome 22, resulting in overexpression of the oncoprotein BCR-ABL1.[3] This translocation, t(9;22), is known as the Ph chromosome. Ninety percent of patients with CML harbor Ph chromosome, whereas 5% have Ph variants; the other 5% are Ph-negative by cytogenetic analysis but are positive for BCR-ABL by fluorescence in situ hybridization (FISH) and PCR. BCR-ABL1 is a tyrosine kinase that promotes growth and replication by increasing signaling pathways such as STAT, RAS, RAF, JUN kinase, and MYC.[4]\nAbout 50% of patients with CML are asymptomatic, and the disease is diagnosed during routine blood tests. The clinical presentation consists of leukocytosis, splenomegaly, thrombocytosis, and anemia. Symptoms vary and include early satiety, left upper quadrant pain, fatigue, malaise, weight loss, thrombosis, and bleeding episodes.\nThe diagnosis of typical CML is based on persistent leukocytosis along with detection of the Ph chromosome abnormality and t(9;22) (q34; q11) or Ph-related molecular BCR-ABL1 abnormalities by FISH or molecular studies. Baseline chromosome banding analysis is required to evaluate for clonal evolution, i(17) (q10)-7/del7q, and 3q26.2 rearrangements.[5] These findings are associated with a relatively poor prognosis. The most common BCR-ABL transcript is p210, and p190 is rare in CML but often seen in Ph-positive acute lymphoblastic leukemia.\nBecause of this patient's initial presentation with thrombocytosis and bleeding, CML was always in the differential diagnosis. The peripheral blood smear that showed neutrophilia, basophilia, and eosinophilia prompted BCR-ABL PCR testing, which confirmed the diagnosis.\nCML is divided into three phases: chronic, accelerated, and blast. The blast phase (BP) is defined as the presence ≥ 30% blasts. The accelerated phase (AP) is defined as peripheral blood or bone marrow blasts of 10%-19%, peripheral blood basophils ≥ 20%, or the presence of cytogenetic evolution.\nTo determine the phase of CML, this patient underwent bone marrow biopsy. The biopsy revealed hypercellular marrow (90%) with normal myeloid to erythroid ratio, granulopoiesis with left shift, and increased blasts (15% of marrow cellularity). The results of cytogenetic analysis were positive for t(9;22). Her CML was classified as CML-AP owing to the presence of 15% blasts in the marrow.\nThere are several prognostic scores for CML, such as Sokal, Euro/Hasford, EUTOS (EUropean Treatment Outcome Study), and ELTS (EUTOS long-term survival).[6,7,8] The Sokal score is a widely used prognostic index that includes age, size of the spleen, platelets, and blasts. On the basis of this score, patients are classified into low- (0.8), intermediate- (0.8-1.2), and high- (> 1.2) risk. With a score of 4.5, this patient is considered high-risk, with a 2-year overall survival of 65% and a median overall survival of 2.5-5 years.\nWhile the results of diagnostic studies are pending, hydroxyurea can be used for cytoreduction. The recommended dosage of hydroxyurea is 20-40 mg/kg/d in divided doses until a diagnosis is obtained. Hydroxyurea, 40 mg/kg/d, was started in this patient for cytoreduction.\nTKIs are the mainstay of treatment. TKIs are designed to block interaction between the BCR-ABL1 protein and adenosine triphosphate, halting the proliferation of leukemic cells. Available treatment options include:\nFirst-generation TKI: imatinib\nSecond-generation TKIs: dasatinib, nilotinib, and bosutinib\nThird-generation TKI: ponatinib\nOmacetaxine\nImatinib was the first TKI approved by the US Food and Drug Administration for chronic-phase CML (CML-CP) on the basis of the results of the International Randomized Study of Interferon and STI571 (IRIS) trial.[9,10] It improved event-free survival (80%) and 10-year overall survival (83%).\nThe DASISION trial compared the second-generation TKI dasatinib with imatinib. Dasatinib provided deeper and faster responses when compared with imatinib, but there was no improvement in overall survival or event-free survival.[11,12,13] The ENESTnd study and the BFORE study compared nilotinib and bosutinib with imatinib, respectively, and again revealed deeper responses without an improvement in overall survival.[14,15] Based on the results of these trials, second-generation TKIs are the first-line choice to treat CML.\nPonatinib is approved by the FDA as a second-line agent in patients who have a T315I mutation.[16,17] Omacetaxine is approved for patients who have disease progression on more than two TKIs.[18]\nThe doses of TKIs used in chronic and advanced phases of CML are listed in the Table.\nTable. Doses of TKIs in Chronic and Advanced Phases of CML\nPhase\nImatinib\nDasatinib\nBosutinib\nNilotinib\nPonatinib\nChronic\n400 mg/d\n100 mg/d\n400 mg/d\n300 mg twice daily\n45 mg/d\nAdvanced\n600 mg/d\n140 mg/d\n500 mg/d\n400 mg twice daily\n45 mg/d\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Oncology Case Challenge: A 46-Year-Old Mother With Severe, Constant Abdominal Pain"
},
{
"authors": "Mounika Gangireddy, MD, MBBS",
"content": [
"The toxicity profiles of all the TKIs are similar. The most common toxicities are hepatotoxicity, cardiotoxicity, pleural effusion, myelosuppression, and QT prolongation.",
"Allogeneic stem cell transplant is used for salvage in patients with CML-CP whose disease has progressed on more than two TKIs. The cure rates with allogeneic stem cell transplant are about 15%-40% for CML-AP and 10%-20% for CML-BP.[19]",
"The response to treatment can be monitored with chromosome analysis, FISH, and PCR. PCR is the most sensitive and evaluable test and predicts relapse.[20,21,22,23]",
"A complete hematologic response is defined as a WBC count < 10 × 109/L, a platelet count < 450 × 109/L, no blasts, basophils < 20%, and no extramedullary involvement.",
"A cytogenetic response is determined by analyzing all 20 chromosomes. A complete cytogenetic response is defined as none of the metaphases having the Ph chromosome, a partial cytogenetic response indicates that 1%-35% of the metaphases harbor the Ph chromosome, and a minor cytogenetic response indicates that 36%-95% of the metaphases have the Ph chromosome.",
"A molecular response is determined by BCR-ABL reverse transcription–PCR analysis. A major molecular response (MMR) is classified into MR3, MR4, MR4.5, and undetectable based on the log findings on PCR. These are defined as < 0.1, < 0.01, < 0.0032, and 0 respectively.",
"The European LeukemiaNet guidelines and the National Comprehensive Cancer Network Clinical Practice Guidelines recommend performing chromosome analysis, FISH (in Ph-CML), and PCR at diagnosis followed by every 3 months.[8,10] Continue PCR every 3 months until 2 years after the BCR-ABL is < 1% (international scale) and then every 3-6 months. Repeat PCR in 1-3 months if there is a 1-log increase in a patient with an MMR.[24]",
"This patient started the second-generation TKI dasatinib at a dosage of 140 mg/d. At 3 months, she is in complete hematologic response, with a BCR-ABL < 0.1% (MMR)."
],
"date": "April 13, 2022",
"figures": [],
"markdown": "# Oncology Case Challenge: A 46-Year-Old Mother With Severe, Constant Abdominal Pain\n\n **Authors:** Mounika Gangireddy, MD, MBBS \n **Date:** April 13, 2022\n\n ## Content\n\n The toxicity profiles of all the TKIs are similar. The most common toxicities are hepatotoxicity, cardiotoxicity, pleural effusion, myelosuppression, and QT prolongation.\nAllogeneic stem cell transplant is used for salvage in patients with CML-CP whose disease has progressed on more than two TKIs. The cure rates with allogeneic stem cell transplant are about 15%-40% for CML-AP and 10%-20% for CML-BP.[19]\nThe response to treatment can be monitored with chromosome analysis, FISH, and PCR. PCR is the most sensitive and evaluable test and predicts relapse.[20,21,22,23]\nA complete hematologic response is defined as a WBC count < 10 × 109/L, a platelet count < 450 × 109/L, no blasts, basophils < 20%, and no extramedullary involvement.\nA cytogenetic response is determined by analyzing all 20 chromosomes. A complete cytogenetic response is defined as none of the metaphases having the Ph chromosome, a partial cytogenetic response indicates that 1%-35% of the metaphases harbor the Ph chromosome, and a minor cytogenetic response indicates that 36%-95% of the metaphases have the Ph chromosome.\nA molecular response is determined by BCR-ABL reverse transcription–PCR analysis. A major molecular response (MMR) is classified into MR3, MR4, MR4.5, and undetectable based on the log findings on PCR. These are defined as < 0.1, < 0.01, < 0.0032, and 0 respectively.\nThe European LeukemiaNet guidelines and the National Comprehensive Cancer Network Clinical Practice Guidelines recommend performing chromosome analysis, FISH (in Ph-CML), and PCR at diagnosis followed by every 3 months.[8,10] Continue PCR every 3 months until 2 years after the BCR-ABL is < 1% (international scale) and then every 3-6 months. Repeat PCR in 1-3 months if there is a 1-log increase in a patient with an MMR.[24]\nThis patient started the second-generation TKI dasatinib at a dosage of 140 mg/d. At 3 months, she is in complete hematologic response, with a BCR-ABL < 0.1% (MMR).\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1677613,
"choiceText": "Discontinue the TKI",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677614,
"choiceText": "Assess for compliance and drug interactions",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677615,
"choiceText": "Switch to omacetaxine",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677616,
"choiceText": "Consider bone marrow transplant",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The goal percentage of BCR-ABLwhen checked at 3 months should be < 10%. When it is above 10%, always assess first for compliance and drug interactions, which could result in failure to achieve the goal.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 540373,
"questionText": "A 40-year-old woman is diagnosed with CML-CP. She starts dasatinib at 100 mg/d. The BCR-ABL PCR at 3 months is 11%. What is the next step?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1677617,
"choiceText": "Imatinib",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677618,
"choiceText": "Dasatinib",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677619,
"choiceText": "Bosutinib",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677620,
"choiceText": "Ponatinib",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Ponatinib is a third-generation TKI that is approved by the FDA for patients with CML who have a T315I mutation. The most common adverse effects of ponatinib are thrombocytopenia and abdominal pain.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 540374,
"questionText": "Which is the drug of choice in patients with CML who have a T315I mutation?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Oncology Case Challenge: A 46-Year-Old Mother With Severe, Constant Abdominal Pain"
},
{
"authors": "Mounika Gangireddy, MD, MBBS",
"content": [],
"date": "April 13, 2022",
"figures": [],
"markdown": "# Oncology Case Challenge: A 46-Year-Old Mother With Severe, Constant Abdominal Pain\n\n **Authors:** Mounika Gangireddy, MD, MBBS \n **Date:** April 13, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1677613,
"choiceText": "Discontinue the TKI",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677614,
"choiceText": "Assess for compliance and drug interactions",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677615,
"choiceText": "Switch to omacetaxine",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677616,
"choiceText": "Consider bone marrow transplant",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The goal percentage of BCR-ABLwhen checked at 3 months should be < 10%. When it is above 10%, always assess first for compliance and drug interactions, which could result in failure to achieve the goal.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 540373,
"questionText": "A 40-year-old woman is diagnosed with CML-CP. She starts dasatinib at 100 mg/d. The BCR-ABL PCR at 3 months is 11%. What is the next step?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1677617,
"choiceText": "Imatinib",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677618,
"choiceText": "Dasatinib",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677619,
"choiceText": "Bosutinib",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677620,
"choiceText": "Ponatinib",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Ponatinib is a third-generation TKI that is approved by the FDA for patients with CML who have a T315I mutation. The most common adverse effects of ponatinib are thrombocytopenia and abdominal pain.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 540374,
"questionText": "Which is the drug of choice in patients with CML who have a T315I mutation?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Oncology Case Challenge: A 46-Year-Old Mother With Severe, Constant Abdominal Pain"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1677609,
"choiceText": "Essential thrombocytosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677610,
"choiceText": "Severe iron deficiency anemia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677611,
"choiceText": "Chronic myeloid leukemia",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677612,
"choiceText": "Chronic lymphocytic leukemia\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 540372,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1677613,
"choiceText": "Discontinue the TKI",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677614,
"choiceText": "Assess for compliance and drug interactions",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677615,
"choiceText": "Switch to omacetaxine",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677616,
"choiceText": "Consider bone marrow transplant",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The goal percentage of BCR-ABLwhen checked at 3 months should be < 10%. When it is above 10%, always assess first for compliance and drug interactions, which could result in failure to achieve the goal.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 540373,
"questionText": "A 40-year-old woman is diagnosed with CML-CP. She starts dasatinib at 100 mg/d. The BCR-ABL PCR at 3 months is 11%. What is the next step?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1677617,
"choiceText": "Imatinib",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677618,
"choiceText": "Dasatinib",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677619,
"choiceText": "Bosutinib",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1677620,
"choiceText": "Ponatinib",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Ponatinib is a third-generation TKI that is approved by the FDA for patients with CML who have a T315I mutation. The most common adverse effects of ponatinib are thrombocytopenia and abdominal pain.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 540374,
"questionText": "Which is the drug of choice in patients with CML who have a T315I mutation?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
727941 | /viewarticle/727941 | [
{
"authors": "Kennedy O. Omonuwa, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 42-year-old man with no significant past medical history presents to the emergency department (ED) with a long-standing history of dyspnea that has been persistently worsening for the past 2 years. The dyspnea is worse upon exertion and is associated with decreased exercise tolerance. No associated chest pains, palpitations, dizziness, or syncope are noted. The patient denies any associated cough, hemoptysis, fever, or weight loss.",
"Upon initial presentation to his primary care physician (PCP) at the time of symptom onset, a cardiac stress test and pulmonary function testing were within normal limits; however, his symptoms have persisted. He has been prescribed zolpidem, as needed, by his PCP, who labeled his condition anxiety-related. The shortness of breath has progressively gotten worse. The patient can no longer exercise, or even walk, without becoming short of breath. The patient is an active tennis player and has no family history of heart disease. He does not take any medications or herbal supplements, and he has no known drug or food allergies. The patient has no history of smoking, alcohol abuse, or illicit drug use."
],
"date": "April 08, 2022",
"figures": [],
"markdown": "# A 42-Year-Old Tennis Player With Dyspnea Blamed on Anxiety\n\n **Authors:** Kennedy O. Omonuwa, MD \n **Date:** April 08, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 42-year-old man with no significant past medical history presents to the emergency department (ED) with a long-standing history of dyspnea that has been persistently worsening for the past 2 years. The dyspnea is worse upon exertion and is associated with decreased exercise tolerance. No associated chest pains, palpitations, dizziness, or syncope are noted. The patient denies any associated cough, hemoptysis, fever, or weight loss.\nUpon initial presentation to his primary care physician (PCP) at the time of symptom onset, a cardiac stress test and pulmonary function testing were within normal limits; however, his symptoms have persisted. He has been prescribed zolpidem, as needed, by his PCP, who labeled his condition anxiety-related. The shortness of breath has progressively gotten worse. The patient can no longer exercise, or even walk, without becoming short of breath. The patient is an active tennis player and has no family history of heart disease. He does not take any medications or herbal supplements, and he has no known drug or food allergies. The patient has no history of smoking, alcohol abuse, or illicit drug use.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A 42-Year-Old Tennis Player With Dyspnea Blamed on Anxiety"
},
{
"authors": "Kennedy O. Omonuwa, MD",
"content": [
"Physical examination reveals an alert and oriented male with a regular pulse of 92 beats/min, blood pressure of 135/85 mm Hg, respiratory rate of 20 breaths/min, a temperature of 98.6°F (37°C), and an O2 saturation of 92% on room air. The neck is supple and without any jugular venous distention, lymphadenopathy, tracheal deviation, or thyroid nodules.",
"Cardiac examination reveals a normal S1, fixed split S2, and a prominent P2, but no audible murmurs, rubs, or gallops are noted. The chest examination shows bilateral equal air entry, without any wheezes, rhonchi, or rales. The abdomen is soft, nontender and nondistended, without any evidence of organomegaly. No lower extremity edema, cyanosis, or clubbing is seen. The peripheral arterial pulses are palpable. The neurologic examination is normal.",
"Laboratory investigations, including a complete blood count, comprehensive metabolic panel, B-type natriuretic peptide (BNP), and troponin are within normal limits.",
"Stool guaiac test findings are negative. Arterial blood gas on room air shows a pH of 7.48, a partial carbon dioxide pressure (pCO2) of 31 mm Hg, and a partial oxygen pressure (pO2) of 70 mm Hg. Chest radiography shows clear lung fields with prominent central pulmonary arteries. A 12-lead electrocardiogram (ECG) shows tall R waves in V1, inverted T waves in leads V1 to V4, II, II, and aVF. A CT angiogram of the chest is obtained (Figure 1).",
"Figure 1."
],
"date": "April 08, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/727/941/727941-Thumb1.png"
}
],
"markdown": "# A 42-Year-Old Tennis Player With Dyspnea Blamed on Anxiety\n\n **Authors:** Kennedy O. Omonuwa, MD \n **Date:** April 08, 2022\n\n ## Content\n\n Physical examination reveals an alert and oriented male with a regular pulse of 92 beats/min, blood pressure of 135/85 mm Hg, respiratory rate of 20 breaths/min, a temperature of 98.6°F (37°C), and an O2 saturation of 92% on room air. The neck is supple and without any jugular venous distention, lymphadenopathy, tracheal deviation, or thyroid nodules.\nCardiac examination reveals a normal S1, fixed split S2, and a prominent P2, but no audible murmurs, rubs, or gallops are noted. The chest examination shows bilateral equal air entry, without any wheezes, rhonchi, or rales. The abdomen is soft, nontender and nondistended, without any evidence of organomegaly. No lower extremity edema, cyanosis, or clubbing is seen. The peripheral arterial pulses are palpable. The neurologic examination is normal.\nLaboratory investigations, including a complete blood count, comprehensive metabolic panel, B-type natriuretic peptide (BNP), and troponin are within normal limits.\nStool guaiac test findings are negative. Arterial blood gas on room air shows a pH of 7.48, a partial carbon dioxide pressure (pCO2) of 31 mm Hg, and a partial oxygen pressure (pO2) of 70 mm Hg. Chest radiography shows clear lung fields with prominent central pulmonary arteries. A 12-lead electrocardiogram (ECG) shows tall R waves in V1, inverted T waves in leads V1 to V4, II, II, and aVF. A CT angiogram of the chest is obtained (Figure 1).\nFigure 1.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 363778,
"choiceText": "Chronic aortic dissection",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363779,
"choiceText": "Ischemic cardiomyopathy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363780,
"choiceText": "Chronic obstructive pulmonary disease",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363781,
"choiceText": "Chronic thromboembolic pulmonary hypertension",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 104039,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 42-Year-Old Tennis Player With Dyspnea Blamed on Anxiety"
},
{
"authors": "Kennedy O. Omonuwa, MD",
"content": [
"The axial image of the chest CT angiogram demonstrated a constellation of findings suggestive of chronic thromboembolic pulmonary hypertension (CTEPH); the flattened eccentric thrombus in the right pulmonary artery caused the contour of the intimal surface to become irregular, and the abrupt vessel narrowing resulted from recanalization of the organized thrombus. These findings are direct signs of chronic thromboembolic disease. The CT image also showed an enlarged pulmonary trunk and a ratio of the diameter of the main pulmonary artery to the diameter of the aorta that was greater than 1. This finding, together with the fixed, split S2 and prominent P2 on cardiac examination and the ECG changes (suggestive of right ventricular hypertrophy [RVH] and right heart strain) pointed toward a diagnosis of chronic pulmonary hypertension. The combination of the CT signs of chronic thromboembolic disease and clinical signs of chronic pulmonary hypertension made CTEPH the most likely diagnosis.",
"Further testing in this patient included a duplex ultrasound scan of the lower extremities, which revealed a bilateral calf deep vein thrombosis; a ventilation/perfusion scan, which showed several mismatched perfusion defects of the posterior segment of the right and anterior segments of the left upper lobes (read as high probability for pulmonary embolism); and an elevated factor VIII assay. Echocardiography showed a high pulmonary systolic pressure of 82 mm Hg, right ventricular hypertrophy, and reduced right ventricular function. A subsequent right heart catheterization confirmed the diagnosis of pulmonary hypertension, with an elevated mean pulmonary artery pressure of 52 mm Hg and pulmonary vascular resistance of 12.3 Wood units.",
"CTEPH is the result of obstruction of the pulmonary arteries by acute and recurrent PE, with subsequent organization of the thrombi.[1] In most patients with acute PE, the thrombus resolves with minimal or no residua. The incidence of CTEPH is unclear. In a study that enrolled 223 patients with PE, the cumulative incidence of symptomatic CTEPH was 1% of cases that occurred 6 months after acute episodes of PE, 3.1% at 1 year, and 3.8% at 2 years.[2] Elevated factor VIII and antiphospholipid antibodies have been seen in patients with CTEPH.[3] Other factors that have been shown to place patients at greater risk for CTEPH include a younger age at presentation, larger perfusion defects at diagnosis, idiopathic pulmonary embolic disease, pulmonary artery systolic pressures > 50 mm Hg at presentation, and the size of the initial thrombus burden.[2,4] Additionally, certain medical conditions, such as prior splenectomy, the presence of a ventriculoatrial shunt to treat hydrocephalus, and chronic inflammatory disorders (such as osteomyelitis and inflammatory bowel disease), have all been associated with an increased risk for CTEPH.[5]",
"A patient may provide a history that is consistent with acute PE, but nearly two thirds of patients with CTEPH may not have a history of acute PE, which may result in diagnostic delays.[6] Patients who have CTEPH usually complain of exertional dyspnea and a gradual decrease in exercise tolerance over months to years. Other symptoms that may be reported include a nonproductive cough, hemoptysis, pleuritic chest pain, and presyncope/syncope. Findings on physical examination in patients with CTEPH reflect the degree of pulmonary vascular disease on presentation. Physical signs attributable to CTEPH may be subtle or absent in the absence of right-sided heart failure. Signs of pulmonary hypertension include right parasternal heave, fixed splitting of S2 with accentuated pulmonic component (P2), right ventricular fourth heart sound gallop, tricuspid regurgitation, and/or pulmonary insufficiency murmur. As the disease progresses and if left untreated, right ventricular dysfunction and right heart failure occur; significant findings at this time include pedal edema, elevated jugular venous pressure, and hepatomegaly."
],
"date": "April 08, 2022",
"figures": [],
"markdown": "# A 42-Year-Old Tennis Player With Dyspnea Blamed on Anxiety\n\n **Authors:** Kennedy O. Omonuwa, MD \n **Date:** April 08, 2022\n\n ## Content\n\n The axial image of the chest CT angiogram demonstrated a constellation of findings suggestive of chronic thromboembolic pulmonary hypertension (CTEPH); the flattened eccentric thrombus in the right pulmonary artery caused the contour of the intimal surface to become irregular, and the abrupt vessel narrowing resulted from recanalization of the organized thrombus. These findings are direct signs of chronic thromboembolic disease. The CT image also showed an enlarged pulmonary trunk and a ratio of the diameter of the main pulmonary artery to the diameter of the aorta that was greater than 1. This finding, together with the fixed, split S2 and prominent P2 on cardiac examination and the ECG changes (suggestive of right ventricular hypertrophy [RVH] and right heart strain) pointed toward a diagnosis of chronic pulmonary hypertension. The combination of the CT signs of chronic thromboembolic disease and clinical signs of chronic pulmonary hypertension made CTEPH the most likely diagnosis.\nFurther testing in this patient included a duplex ultrasound scan of the lower extremities, which revealed a bilateral calf deep vein thrombosis; a ventilation/perfusion scan, which showed several mismatched perfusion defects of the posterior segment of the right and anterior segments of the left upper lobes (read as high probability for pulmonary embolism); and an elevated factor VIII assay. Echocardiography showed a high pulmonary systolic pressure of 82 mm Hg, right ventricular hypertrophy, and reduced right ventricular function. A subsequent right heart catheterization confirmed the diagnosis of pulmonary hypertension, with an elevated mean pulmonary artery pressure of 52 mm Hg and pulmonary vascular resistance of 12.3 Wood units.\nCTEPH is the result of obstruction of the pulmonary arteries by acute and recurrent PE, with subsequent organization of the thrombi.[1] In most patients with acute PE, the thrombus resolves with minimal or no residua. The incidence of CTEPH is unclear. In a study that enrolled 223 patients with PE, the cumulative incidence of symptomatic CTEPH was 1% of cases that occurred 6 months after acute episodes of PE, 3.1% at 1 year, and 3.8% at 2 years.[2] Elevated factor VIII and antiphospholipid antibodies have been seen in patients with CTEPH.[3] Other factors that have been shown to place patients at greater risk for CTEPH include a younger age at presentation, larger perfusion defects at diagnosis, idiopathic pulmonary embolic disease, pulmonary artery systolic pressures > 50 mm Hg at presentation, and the size of the initial thrombus burden.[2,4] Additionally, certain medical conditions, such as prior splenectomy, the presence of a ventriculoatrial shunt to treat hydrocephalus, and chronic inflammatory disorders (such as osteomyelitis and inflammatory bowel disease), have all been associated with an increased risk for CTEPH.[5]\nA patient may provide a history that is consistent with acute PE, but nearly two thirds of patients with CTEPH may not have a history of acute PE, which may result in diagnostic delays.[6] Patients who have CTEPH usually complain of exertional dyspnea and a gradual decrease in exercise tolerance over months to years. Other symptoms that may be reported include a nonproductive cough, hemoptysis, pleuritic chest pain, and presyncope/syncope. Findings on physical examination in patients with CTEPH reflect the degree of pulmonary vascular disease on presentation. Physical signs attributable to CTEPH may be subtle or absent in the absence of right-sided heart failure. Signs of pulmonary hypertension include right parasternal heave, fixed splitting of S2 with accentuated pulmonic component (P2), right ventricular fourth heart sound gallop, tricuspid regurgitation, and/or pulmonary insufficiency murmur. As the disease progresses and if left untreated, right ventricular dysfunction and right heart failure occur; significant findings at this time include pedal edema, elevated jugular venous pressure, and hepatomegaly.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 363778,
"choiceText": "Chronic aortic dissection",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363779,
"choiceText": "Ischemic cardiomyopathy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363780,
"choiceText": "Chronic obstructive pulmonary disease",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363781,
"choiceText": "Chronic thromboembolic pulmonary hypertension",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 104039,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 42-Year-Old Tennis Player With Dyspnea Blamed on Anxiety"
},
{
"authors": "Kennedy O. Omonuwa, MD",
"content": [
"Dyspnea is a common presenting symptom with many potential causes. Most cases of dyspnea are caused by cardiac or pulmonary disease. CTEPH has been misdiagnosed as being more common causes of dyspnea, such as coronary artery disease, chronic obstructive pulmonary disease, or interstitial lung disease. Some patients have been further improperly labeled with psychogenic dyspnea or physical deconditioning when the dyspnea persists. All clinicians evaluating patients with unexplained dyspnea must have a high index of suspicion for abnormalities of the pulmonary vascular system and should rule out pulmonary vascular etiologies such as PE and pulmonary hypertension.",
"The diagnosis of CTEPH requires a high index of suspicion because the presenting symptoms and signs are nonspecific. Chest radiography findings may be normal in early stages. It can also reveal dilatation of the central pulmonary arteries (suggestive of pulmonary hypertension) and oligemic lung fields or parenchymal opacities from prior infarcts. Electrocardiography may reveal changes of right heart disease (eg, right ventricular hypertrophy, right atrial enlargement, or strain with T-wave inversions in anterior, precordial, and inferior limb leads), depending on the severity of CTEPH; however, these are not specific to this disease. Transthoracic Doppler echocardiography is a useful screening test for suspected pulmonary hypertension.",
"Echocardiography can help estimate the level of systolic pulmonary arterial pressure (PAP) and assess the presence of associated abnormalities, such as right atrial enlargement, right ventricular dilation or hypertrophy, right or left ventricular dysfunction, valvular heart disease, interventricular septal motion abnormalities, and pericardial effusion. A diagnosis of CTEPH is supported by an echocardiographic finding of a mean PAP exceeding 40 mm Hg in a patient with a history of PE.[6] Pulmonary function testing identifies coexisting parenchymal disease and exclude other causes of pulmonary hypertension, such as interstitial lung disease. Patients with CTEPH may show a mild-to-moderate restrictive ventilatory defect secondary to parenchymal scarring from prior parenchymal infarcts.",
"Any patient with unexplained dyspnea should have the pulmonary vascular system evaluated. Chest CT angiography can provide pertinent clues to both the presence of thromboembolic disease and pulmonary hypertension in patients with CTEPH.[7] Direct CT signs of chronic thromboembolic disease include the presence of organized thrombus lining the pulmonary vessels in a concentric or eccentric pattern that may cause pouch defects, intimal irregularities, bands/webs, or abrupt vessel narrowing. These signs differ from the intraluminal filling defect and complete vessel cutoff of acute thromboembolism.",
"Indirect signs of chronic thromboembolic disease on CT scanning include poststenotic dilatation, tortuous vessels, asymmetric dilatation of the central pulmonary arteries, enlargement of the bronchial arteries and/or presence of collaterals and parenchymal abnormalities of mosaic attenuation (from irregular perfusion), and peripheral densities (scars from prior pulmonary infarct). A CT sign of pulmonary hypertension is enlargement of the main pulmonary artery, with a ratio between the CT diameter of the main pulmonary artery to the diameter of the aorta greater than 1:1.",
"Other CT signs of pulmonary hypertension, resulting from right heart disease secondary to the pulmonary hypertension, include right ventricular dilatation, leftward septal bowing, thickening of the free right ventricular wall, and right atrial dilatation. Findings on CT angiography of the chest may appear normal in the presence of CTEPH, and it should not be considered the diagnostic study of choice to rule out this disorder.",
"Ventilation/perfusion (V/Q) scanning is another imaging technique that is important in the diagnosis of CTEPH. Normal V/Q scan findings rule out the diagnosis of CTEPH. In patients with chronic thromboembolic disease, the V/Q invariably shows multiple segmental or larger perfusion defects in lung regions with normal ventilation. In contrast, patients with primary pulmonary hypertension show normal or subsegmental mottled perfusion patterns. Because V/Q mismatch defects are not specific to CTEPH, further imaging studies should be done to define the vascular abnormality with a view to establishing the diagnosis.",
"Pulmonary angiography is the criterion standard test to diagnose chronic thromboembolic disease. The 5 angiographic patterns seen in CTEPH include pouch defects, intimal irregularities, pulmonary artery webs or band like narrowings, abrupt and often angular narrowing of major pulmonary arteries, and proximal obstruction of the pulmonary vessels.[7] Right heart catheterization, which can be performed at the time of pulmonary angiography, defines the severity of pulmonary hypertension and degree of cardiac dysfunction; it measures mean pulmonary artery pressure, pulmonary vascular resistance, right atrial pressure, cardiac output, and cardiac index.",
"The definitive treatment of patients with CTEPH is pulmonary thromboendarterectomy (PTE).[8] Survival without surgical treatment is based on the degree of pulmonary hypertension. With mean pulmonary artery pressures of 30-50 mm Hg, 5-year survival is 30%, whereas among patients with mean pulmonary artery pressures of greater than 50 mm Hg, 5-year survival is only 10%. However, survival remains approximately 90-95% (5-10% mortality rate) after PTE.",
"The decision to opt for surgery is based on the patient's symptom severity and comorbidities. The criteria for surgical selection in patients with CTEPH include accessibility of the thrombi (more proximal thrombi are more amendable to surgery than distal ones), hemodynamic/ventilatory compromise, and the patient's comorbid conditions and associated risks of the procedure.",
"Moser and colleagues pointed out 3 major areas to consider when evaluating a patient for thromboendarterectomy: hemodynamic, alveolo-respiratory, and prophylactic considerations.[11] The hemodynamic goal is to prevent or ameliorate right ventricular compromise caused by pulmonary hypertension. The respiratory objective is to improve respiratory function by the removal of a large ventilated but nonperfused physiologic dead space, regardless of the severity of pulmonary hypertension. The prophylactic goal is to prevent progressive right ventricular dysfunction or retrograde extension of the obstruction, which may result in further cardiorespiratory deterioration or death."
],
"date": "April 08, 2022",
"figures": [],
"markdown": "# A 42-Year-Old Tennis Player With Dyspnea Blamed on Anxiety\n\n **Authors:** Kennedy O. Omonuwa, MD \n **Date:** April 08, 2022\n\n ## Content\n\n Dyspnea is a common presenting symptom with many potential causes. Most cases of dyspnea are caused by cardiac or pulmonary disease. CTEPH has been misdiagnosed as being more common causes of dyspnea, such as coronary artery disease, chronic obstructive pulmonary disease, or interstitial lung disease. Some patients have been further improperly labeled with psychogenic dyspnea or physical deconditioning when the dyspnea persists. All clinicians evaluating patients with unexplained dyspnea must have a high index of suspicion for abnormalities of the pulmonary vascular system and should rule out pulmonary vascular etiologies such as PE and pulmonary hypertension.\nThe diagnosis of CTEPH requires a high index of suspicion because the presenting symptoms and signs are nonspecific. Chest radiography findings may be normal in early stages. It can also reveal dilatation of the central pulmonary arteries (suggestive of pulmonary hypertension) and oligemic lung fields or parenchymal opacities from prior infarcts. Electrocardiography may reveal changes of right heart disease (eg, right ventricular hypertrophy, right atrial enlargement, or strain with T-wave inversions in anterior, precordial, and inferior limb leads), depending on the severity of CTEPH; however, these are not specific to this disease. Transthoracic Doppler echocardiography is a useful screening test for suspected pulmonary hypertension.\nEchocardiography can help estimate the level of systolic pulmonary arterial pressure (PAP) and assess the presence of associated abnormalities, such as right atrial enlargement, right ventricular dilation or hypertrophy, right or left ventricular dysfunction, valvular heart disease, interventricular septal motion abnormalities, and pericardial effusion. A diagnosis of CTEPH is supported by an echocardiographic finding of a mean PAP exceeding 40 mm Hg in a patient with a history of PE.[6] Pulmonary function testing identifies coexisting parenchymal disease and exclude other causes of pulmonary hypertension, such as interstitial lung disease. Patients with CTEPH may show a mild-to-moderate restrictive ventilatory defect secondary to parenchymal scarring from prior parenchymal infarcts.\nAny patient with unexplained dyspnea should have the pulmonary vascular system evaluated. Chest CT angiography can provide pertinent clues to both the presence of thromboembolic disease and pulmonary hypertension in patients with CTEPH.[7] Direct CT signs of chronic thromboembolic disease include the presence of organized thrombus lining the pulmonary vessels in a concentric or eccentric pattern that may cause pouch defects, intimal irregularities, bands/webs, or abrupt vessel narrowing. These signs differ from the intraluminal filling defect and complete vessel cutoff of acute thromboembolism.\nIndirect signs of chronic thromboembolic disease on CT scanning include poststenotic dilatation, tortuous vessels, asymmetric dilatation of the central pulmonary arteries, enlargement of the bronchial arteries and/or presence of collaterals and parenchymal abnormalities of mosaic attenuation (from irregular perfusion), and peripheral densities (scars from prior pulmonary infarct). A CT sign of pulmonary hypertension is enlargement of the main pulmonary artery, with a ratio between the CT diameter of the main pulmonary artery to the diameter of the aorta greater than 1:1.\nOther CT signs of pulmonary hypertension, resulting from right heart disease secondary to the pulmonary hypertension, include right ventricular dilatation, leftward septal bowing, thickening of the free right ventricular wall, and right atrial dilatation. Findings on CT angiography of the chest may appear normal in the presence of CTEPH, and it should not be considered the diagnostic study of choice to rule out this disorder.\nVentilation/perfusion (V/Q) scanning is another imaging technique that is important in the diagnosis of CTEPH. Normal V/Q scan findings rule out the diagnosis of CTEPH. In patients with chronic thromboembolic disease, the V/Q invariably shows multiple segmental or larger perfusion defects in lung regions with normal ventilation. In contrast, patients with primary pulmonary hypertension show normal or subsegmental mottled perfusion patterns. Because V/Q mismatch defects are not specific to CTEPH, further imaging studies should be done to define the vascular abnormality with a view to establishing the diagnosis.\nPulmonary angiography is the criterion standard test to diagnose chronic thromboembolic disease. The 5 angiographic patterns seen in CTEPH include pouch defects, intimal irregularities, pulmonary artery webs or band like narrowings, abrupt and often angular narrowing of major pulmonary arteries, and proximal obstruction of the pulmonary vessels.[7] Right heart catheterization, which can be performed at the time of pulmonary angiography, defines the severity of pulmonary hypertension and degree of cardiac dysfunction; it measures mean pulmonary artery pressure, pulmonary vascular resistance, right atrial pressure, cardiac output, and cardiac index.\nThe definitive treatment of patients with CTEPH is pulmonary thromboendarterectomy (PTE).[8] Survival without surgical treatment is based on the degree of pulmonary hypertension. With mean pulmonary artery pressures of 30-50 mm Hg, 5-year survival is 30%, whereas among patients with mean pulmonary artery pressures of greater than 50 mm Hg, 5-year survival is only 10%. However, survival remains approximately 90-95% (5-10% mortality rate) after PTE.\nThe decision to opt for surgery is based on the patient's symptom severity and comorbidities. The criteria for surgical selection in patients with CTEPH include accessibility of the thrombi (more proximal thrombi are more amendable to surgery than distal ones), hemodynamic/ventilatory compromise, and the patient's comorbid conditions and associated risks of the procedure.\nMoser and colleagues pointed out 3 major areas to consider when evaluating a patient for thromboendarterectomy: hemodynamic, alveolo-respiratory, and prophylactic considerations.[11] The hemodynamic goal is to prevent or ameliorate right ventricular compromise caused by pulmonary hypertension. The respiratory objective is to improve respiratory function by the removal of a large ventilated but nonperfused physiologic dead space, regardless of the severity of pulmonary hypertension. The prophylactic goal is to prevent progressive right ventricular dysfunction or retrograde extension of the obstruction, which may result in further cardiorespiratory deterioration or death.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A 42-Year-Old Tennis Player With Dyspnea Blamed on Anxiety"
},
{
"authors": "Kennedy O. Omonuwa, MD",
"content": [
"Surgical treatment and endarterectomy must be bilateral because this is a bilateral disease in the vast majority of patients. The procedure is conducted with the aid of cardiopulmonary bypass, and the patient is cooled to allow for hypothermic circulatory arrest. Meticulous postoperative management is essential to the success of this surgical procedure.[9]",
"All patients are mechanically ventilated for at least 24 hours, and all patients are subjected to maintained diuresis. Patients are subject to all complications associated with open-heart and major lung surgery (eg, arrhythmias, atelectasis, wound infection, pneumonia, renal failure, stroke, mediastinal bleeding) but may also develop complications specific to this operation. These include persistent pulmonary hypertension, reperfusion injuries, and neurologic disorders related to hypothermic arrest and deep hypothermia. Reduction in pulmonary pressures, resistance to normal levels, and corresponding improvements in pulmonary blood flow and cardiac output are generally immediate and sustained. In general, these changes can be assumed to be permanent.",
"Prior to surgery, more than 95% of the patients are in New York Heart Association (NYHA) functional class III or IV. After surgery, 95% of patients remain in NYHA functional class I or II after 1 year. After successful surgery, reduction in pulmonary vascular resistance exceeding 50% is usually seen and translates into improved functional status of the patient, with 6-year postsurgery survival of 75%. After surgery, 93% were in NYHA class I or II, compared with about 95% who were NYHA class II or IV preoperatively.",
"Medical therapy for patients with CTEPH should be considered in patients in whom PTE is contraindicated because of significant comorbidities or unresectable (distal) chronic thrombus, and in patients who elect not to undergo PTE by personal choice. Also, medical therapy is beneficial as a “stabilizing bridge” to surgery to reduce the postoperative mortality risk in patients who have severe pulmonary hypertension and/or right heart failure, and in patients who have residual pulmonary hypertension after surgery. Pulmonary vasodilator therapies used in idiopathic pulmonary arterial hypertension (IPAH) have been evaluated in patients with CTEPH, including prostacyclin analogs, endothelin receptor antagonists, and phosphodiesterase-5 inhibitors.[10] Soluble guanylate cyclase (sGC) stimulators have been approved by US Food and Drug Administration (FDA) for the treatment of IPAH and CTEPH. Lifelong anticoagulation therapy is recommended for all patients with CTEPH, but it does not generally affect the underlying disease process of CTEPH. Lung transplantation can be considered for patients who do not respond to medical therapy or in those whose disease is not amenable to correction by PTE.",
"CTEPH is one of the leading treatable causes of pulmonary hypertension. This case emphasizes the need for clinicians to be aware of CTEPH because its diagnosis is commonly delayed or missed because of the nonspecific nature of its presentation and, sometimes, because of a lack of prior history of acute symptomatic PE or deep vein thrombosis. All clinicians should have a high index of suspicion and consider pulmonary vascular disease (thromboembolic disease/ pulmonary hypertension) in the differential diagnosis of any patient complaining of unexplained persistent dyspnea.",
"The patient in this case was admitted and started on anticoagulation (heparin and warfarin) and an inferior vena cava filter was placed. He was evaluated by a thoracic surgeon with expertise in CTEPH and offered PTE, but he refused. He was also evaluated by a pulmonary hypertension specialist who started him on intravenous epoprostenol and bosentan for his elevated pulmonary pressures. After achieving a therapeutic international normalized ratio, the patient was discharged to follow-up with the pulmonary hypertension clinic. After 2 months of medical therapy, the patient's dyspnea moderately improved."
],
"date": "April 08, 2022",
"figures": [],
"markdown": "# A 42-Year-Old Tennis Player With Dyspnea Blamed on Anxiety\n\n **Authors:** Kennedy O. Omonuwa, MD \n **Date:** April 08, 2022\n\n ## Content\n\n Surgical treatment and endarterectomy must be bilateral because this is a bilateral disease in the vast majority of patients. The procedure is conducted with the aid of cardiopulmonary bypass, and the patient is cooled to allow for hypothermic circulatory arrest. Meticulous postoperative management is essential to the success of this surgical procedure.[9]\nAll patients are mechanically ventilated for at least 24 hours, and all patients are subjected to maintained diuresis. Patients are subject to all complications associated with open-heart and major lung surgery (eg, arrhythmias, atelectasis, wound infection, pneumonia, renal failure, stroke, mediastinal bleeding) but may also develop complications specific to this operation. These include persistent pulmonary hypertension, reperfusion injuries, and neurologic disorders related to hypothermic arrest and deep hypothermia. Reduction in pulmonary pressures, resistance to normal levels, and corresponding improvements in pulmonary blood flow and cardiac output are generally immediate and sustained. In general, these changes can be assumed to be permanent.\nPrior to surgery, more than 95% of the patients are in New York Heart Association (NYHA) functional class III or IV. After surgery, 95% of patients remain in NYHA functional class I or II after 1 year. After successful surgery, reduction in pulmonary vascular resistance exceeding 50% is usually seen and translates into improved functional status of the patient, with 6-year postsurgery survival of 75%. After surgery, 93% were in NYHA class I or II, compared with about 95% who were NYHA class II or IV preoperatively.\nMedical therapy for patients with CTEPH should be considered in patients in whom PTE is contraindicated because of significant comorbidities or unresectable (distal) chronic thrombus, and in patients who elect not to undergo PTE by personal choice. Also, medical therapy is beneficial as a “stabilizing bridge” to surgery to reduce the postoperative mortality risk in patients who have severe pulmonary hypertension and/or right heart failure, and in patients who have residual pulmonary hypertension after surgery. Pulmonary vasodilator therapies used in idiopathic pulmonary arterial hypertension (IPAH) have been evaluated in patients with CTEPH, including prostacyclin analogs, endothelin receptor antagonists, and phosphodiesterase-5 inhibitors.[10] Soluble guanylate cyclase (sGC) stimulators have been approved by US Food and Drug Administration (FDA) for the treatment of IPAH and CTEPH. Lifelong anticoagulation therapy is recommended for all patients with CTEPH, but it does not generally affect the underlying disease process of CTEPH. Lung transplantation can be considered for patients who do not respond to medical therapy or in those whose disease is not amenable to correction by PTE.\nCTEPH is one of the leading treatable causes of pulmonary hypertension. This case emphasizes the need for clinicians to be aware of CTEPH because its diagnosis is commonly delayed or missed because of the nonspecific nature of its presentation and, sometimes, because of a lack of prior history of acute symptomatic PE or deep vein thrombosis. All clinicians should have a high index of suspicion and consider pulmonary vascular disease (thromboembolic disease/ pulmonary hypertension) in the differential diagnosis of any patient complaining of unexplained persistent dyspnea.\nThe patient in this case was admitted and started on anticoagulation (heparin and warfarin) and an inferior vena cava filter was placed. He was evaluated by a thoracic surgeon with expertise in CTEPH and offered PTE, but he refused. He was also evaluated by a pulmonary hypertension specialist who started him on intravenous epoprostenol and bosentan for his elevated pulmonary pressures. After achieving a therapeutic international normalized ratio, the patient was discharged to follow-up with the pulmonary hypertension clinic. After 2 months of medical therapy, the patient's dyspnea moderately improved.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 363782,
"choiceText": "V/Q scan",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363783,
"choiceText": "Pulmonary function test",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363784,
"choiceText": "Chest radiography",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363785,
"choiceText": "Pulmonary angiography",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "In a patient with chronic thromboembolic disease, the V/Q scan shows multiple segmental or larger perfusion defects in lung areas with normal ventilation. Because V/Q mismatch defects are not specific to CTEPH, further imaging should be done to define vascular abnormalities with a view to establishing the diagnosis. A patient with CTEPH may show a restrictive ventilatory defect secondary to scarring from prior parenchymal infarcts. Chest radiography, which may be normal in early stages, may reveal dilatation of the central pulmonary arteries suggestive of pulmonary hypertension and oligemic lung fields or parenchymal opacities from prior infarcts. Pulmonary angiography is the criterion standard for diagnosing chronic thromboembolic disease. The 5 angiographic patterns seen include pouch defects, intimal irregularities, pulmonary arterial webs or band like narrowings, abrupt and often angular narrowing of major pulmonary arteries, and proximal obstruction of pulmonary vessels.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 104040,
"questionText": "Which diagnostic test is the criterion standard for diagnosing chronic thromboembolic disease?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 363786,
"choiceText": "Lifelong anticoagulation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363787,
"choiceText": "Endothelin receptor antagonists",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363788,
"choiceText": "Pulmonary thromboendarterectomy",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363789,
"choiceText": "Lung transplantation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The definitive treatment is PTE. Medical therapy should be considered when PTE is contraindicated because of comorbidities or unresectable (distal) chronic thrombus, and in patients who refuse. Adjunct medical therapy is beneficial for reducing postoperative mortality risk in patients who have severe pulmonary hypertension and/or right heart failure, and in patients who have residual pulmonary hypertension after surgery. Pulmonary vasodilator therapies used in idiopathic pulmonary arterial hypertension have been evaluated in patients with CTEPH, and these include prostacyclin analogs, endothelin receptor antagonists, and phosphodiesterase-5 inhibitors. Lifelong anticoagulation therapy is recommended for all patients with CTEPH, but this does not generally affect the underlying disease process. Lung transplantation can be considered for patients who do not respond to medical therapy and are not thromboendarterectomy candidates due to thrombus location.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 104041,
"questionText": "Which is the definitive treatment for a patient with a diagnosis of CTEPH who is experiencing chronic dyspnea upon exertion and who has ECG findings suggestive of right ventricular strain and a CT angiogram finding of thromboembolic phenomena?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 42-Year-Old Tennis Player With Dyspnea Blamed on Anxiety"
},
{
"authors": "Kennedy O. Omonuwa, MD",
"content": [],
"date": "April 08, 2022",
"figures": [],
"markdown": "# A 42-Year-Old Tennis Player With Dyspnea Blamed on Anxiety\n\n **Authors:** Kennedy O. Omonuwa, MD \n **Date:** April 08, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 363782,
"choiceText": "V/Q scan",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363783,
"choiceText": "Pulmonary function test",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363784,
"choiceText": "Chest radiography",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363785,
"choiceText": "Pulmonary angiography",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "In a patient with chronic thromboembolic disease, the V/Q scan shows multiple segmental or larger perfusion defects in lung areas with normal ventilation. Because V/Q mismatch defects are not specific to CTEPH, further imaging should be done to define vascular abnormalities with a view to establishing the diagnosis. A patient with CTEPH may show a restrictive ventilatory defect secondary to scarring from prior parenchymal infarcts. Chest radiography, which may be normal in early stages, may reveal dilatation of the central pulmonary arteries suggestive of pulmonary hypertension and oligemic lung fields or parenchymal opacities from prior infarcts. Pulmonary angiography is the criterion standard for diagnosing chronic thromboembolic disease. The 5 angiographic patterns seen include pouch defects, intimal irregularities, pulmonary arterial webs or band like narrowings, abrupt and often angular narrowing of major pulmonary arteries, and proximal obstruction of pulmonary vessels.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 104040,
"questionText": "Which diagnostic test is the criterion standard for diagnosing chronic thromboembolic disease?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 363786,
"choiceText": "Lifelong anticoagulation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363787,
"choiceText": "Endothelin receptor antagonists",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363788,
"choiceText": "Pulmonary thromboendarterectomy",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363789,
"choiceText": "Lung transplantation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The definitive treatment is PTE. Medical therapy should be considered when PTE is contraindicated because of comorbidities or unresectable (distal) chronic thrombus, and in patients who refuse. Adjunct medical therapy is beneficial for reducing postoperative mortality risk in patients who have severe pulmonary hypertension and/or right heart failure, and in patients who have residual pulmonary hypertension after surgery. Pulmonary vasodilator therapies used in idiopathic pulmonary arterial hypertension have been evaluated in patients with CTEPH, and these include prostacyclin analogs, endothelin receptor antagonists, and phosphodiesterase-5 inhibitors. Lifelong anticoagulation therapy is recommended for all patients with CTEPH, but this does not generally affect the underlying disease process. Lung transplantation can be considered for patients who do not respond to medical therapy and are not thromboendarterectomy candidates due to thrombus location.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 104041,
"questionText": "Which is the definitive treatment for a patient with a diagnosis of CTEPH who is experiencing chronic dyspnea upon exertion and who has ECG findings suggestive of right ventricular strain and a CT angiogram finding of thromboembolic phenomena?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 42-Year-Old Tennis Player With Dyspnea Blamed on Anxiety"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 363778,
"choiceText": "Chronic aortic dissection",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363779,
"choiceText": "Ischemic cardiomyopathy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363780,
"choiceText": "Chronic obstructive pulmonary disease",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363781,
"choiceText": "Chronic thromboembolic pulmonary hypertension",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 104039,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 363782,
"choiceText": "V/Q scan",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363783,
"choiceText": "Pulmonary function test",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363784,
"choiceText": "Chest radiography",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363785,
"choiceText": "Pulmonary angiography",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "In a patient with chronic thromboembolic disease, the V/Q scan shows multiple segmental or larger perfusion defects in lung areas with normal ventilation. Because V/Q mismatch defects are not specific to CTEPH, further imaging should be done to define vascular abnormalities with a view to establishing the diagnosis. A patient with CTEPH may show a restrictive ventilatory defect secondary to scarring from prior parenchymal infarcts. Chest radiography, which may be normal in early stages, may reveal dilatation of the central pulmonary arteries suggestive of pulmonary hypertension and oligemic lung fields or parenchymal opacities from prior infarcts. Pulmonary angiography is the criterion standard for diagnosing chronic thromboembolic disease. The 5 angiographic patterns seen include pouch defects, intimal irregularities, pulmonary arterial webs or band like narrowings, abrupt and often angular narrowing of major pulmonary arteries, and proximal obstruction of pulmonary vessels.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 104040,
"questionText": "Which diagnostic test is the criterion standard for diagnosing chronic thromboembolic disease?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 363786,
"choiceText": "Lifelong anticoagulation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363787,
"choiceText": "Endothelin receptor antagonists",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363788,
"choiceText": "Pulmonary thromboendarterectomy",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 363789,
"choiceText": "Lung transplantation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The definitive treatment is PTE. Medical therapy should be considered when PTE is contraindicated because of comorbidities or unresectable (distal) chronic thrombus, and in patients who refuse. Adjunct medical therapy is beneficial for reducing postoperative mortality risk in patients who have severe pulmonary hypertension and/or right heart failure, and in patients who have residual pulmonary hypertension after surgery. Pulmonary vasodilator therapies used in idiopathic pulmonary arterial hypertension have been evaluated in patients with CTEPH, and these include prostacyclin analogs, endothelin receptor antagonists, and phosphodiesterase-5 inhibitors. Lifelong anticoagulation therapy is recommended for all patients with CTEPH, but this does not generally affect the underlying disease process. Lung transplantation can be considered for patients who do not respond to medical therapy and are not thromboendarterectomy candidates due to thrombus location.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 104041,
"questionText": "Which is the definitive treatment for a patient with a diagnosis of CTEPH who is experiencing chronic dyspnea upon exertion and who has ECG findings suggestive of right ventricular strain and a CT angiogram finding of thromboembolic phenomena?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
843818 | /viewarticle/843818 | [
{
"authors": "Elena Cecilia Rosca, MD, PhD; Cristina Dijmarescu, MD; Mihaela Simu, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 78-year-old man is brought to the emergency department by his family owing to sudden onset of an inability to speak or swallow. Three years earlier, he had a left frontal ischemic stroke with right hemiparesis and motor aphasia, from which he had completely recovered.",
"His history also includes a left cerebellar infarct, asymptomatic lacunar infarcts, stage 3 hypertension, atrial fibrillation, ischemic cardiomyopathy, and dyslipidemia. Current medications include aspirin, ramipril, indapamide, isosorbide dinitrate, digoxin, and rosuvastatin. He does not smoke, drink alcohol, or use illicit drugs."
],
"date": "April 04, 2022",
"figures": [],
"markdown": "# Neurology Case Challenge: Drooling and Dysphagia in a Man Who Can’t Speak\n\n **Authors:** Elena Cecilia Rosca, MD, PhD; Cristina Dijmarescu, MD; Mihaela Simu, MD \n **Date:** April 04, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 78-year-old man is brought to the emergency department by his family owing to sudden onset of an inability to speak or swallow. Three years earlier, he had a left frontal ischemic stroke with right hemiparesis and motor aphasia, from which he had completely recovered.\nHis history also includes a left cerebellar infarct, asymptomatic lacunar infarcts, stage 3 hypertension, atrial fibrillation, ischemic cardiomyopathy, and dyslipidemia. Current medications include aspirin, ramipril, indapamide, isosorbide dinitrate, digoxin, and rosuvastatin. He does not smoke, drink alcohol, or use illicit drugs.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Neurology Case Challenge: Drooling and Dysphagia in a Man Who Can’t Speak"
},
{
"authors": "Elena Cecilia Rosca, MD, PhD; Cristina Dijmarescu, MD; Mihaela Simu, MD",
"content": [
"Upon physical examination, the patient appears well and has a temperature of 98.1°F (36.7°C). His blood pressure is 170/87 mm Hg. He has an irregular pulse of 92 beats/min. The respiratory and abdominal examination findings are normal.",
"Neurologic examination reveals a wide-based gait with small steps, mild ataxia of the left limbs, brisk tendon reflexes on the right side, and a right Babinski sign. Sensation is unremarkable. On cranial nerve assessment, he has bilateral loss of voluntary movement of muscles supplied by cranial nerves V, VII, IX, X, and XII.",
"The patient is anarthric, unable to volitionally open his mouth or smile; he can minimally move his tongue in the mouth but cannot protrude it. The mouth is slightly open. The patient is drooling and has severe dysphagia. The jaw jerk is increased, and the gag reflex is absent. The automatic movements of the face are preserved. The patient can open his mouth and retract his tongue with yawning. Cranial nerves I-IV and VI are normal. Taste, corneal reflex, trapezius, and sternocleidomastoid muscles are unremarkable.",
"The patient communicates by writing, with intact grammar, and he understands spoken and written language. He is emotionally appropriate, without involuntary laughter or crying.",
"Laboratory analysis findings, including complete blood cell count; erythrocyte sedimentation rate; and liver, renal, thyroid, and lipid panel are normal.",
"Electrocardiography reveals atrial fibrillation, with a heart rate of 96 beats/min and chronic ischemic cardiomyopathy changes. MRI of the brain shows multiple infarcts, bilaterally in the frontal, parietal, and occipital lobes, and cerebellar and cortical atrophy (Figures 1-3).",
"Figure 1.",
"Figure 2.",
"Figure 3."
],
"date": "April 04, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/843/818/843818-thumb1.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/843/818/843818-thumb2.jpg"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/843/818/843818-thumb3.jpg"
}
],
"markdown": "# Neurology Case Challenge: Drooling and Dysphagia in a Man Who Can’t Speak\n\n **Authors:** Elena Cecilia Rosca, MD, PhD; Cristina Dijmarescu, MD; Mihaela Simu, MD \n **Date:** April 04, 2022\n\n ## Content\n\n Upon physical examination, the patient appears well and has a temperature of 98.1°F (36.7°C). His blood pressure is 170/87 mm Hg. He has an irregular pulse of 92 beats/min. The respiratory and abdominal examination findings are normal.\nNeurologic examination reveals a wide-based gait with small steps, mild ataxia of the left limbs, brisk tendon reflexes on the right side, and a right Babinski sign. Sensation is unremarkable. On cranial nerve assessment, he has bilateral loss of voluntary movement of muscles supplied by cranial nerves V, VII, IX, X, and XII.\nThe patient is anarthric, unable to volitionally open his mouth or smile; he can minimally move his tongue in the mouth but cannot protrude it. The mouth is slightly open. The patient is drooling and has severe dysphagia. The jaw jerk is increased, and the gag reflex is absent. The automatic movements of the face are preserved. The patient can open his mouth and retract his tongue with yawning. Cranial nerves I-IV and VI are normal. Taste, corneal reflex, trapezius, and sternocleidomastoid muscles are unremarkable.\nThe patient communicates by writing, with intact grammar, and he understands spoken and written language. He is emotionally appropriate, without involuntary laughter or crying.\nLaboratory analysis findings, including complete blood cell count; erythrocyte sedimentation rate; and liver, renal, thyroid, and lipid panel are normal.\nElectrocardiography reveals atrial fibrillation, with a heart rate of 96 beats/min and chronic ischemic cardiomyopathy changes. MRI of the brain shows multiple infarcts, bilaterally in the frontal, parietal, and occipital lobes, and cerebellar and cortical atrophy (Figures 1-3).\nFigure 1.\nFigure 2.\nFigure 3.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 837663,
"choiceText": "Brainstem stroke",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837665,
"choiceText": "Foix-Chavany-Marie syndrome",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837667,
"choiceText": "Myasthenia gravis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837669,
"choiceText": "Botulism",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837671,
"choiceText": "Amyotrophic lateral sclerosis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 263421,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Neurology Case Challenge: Drooling and Dysphagia in a Man Who Can’t Speak"
},
{
"authors": "Elena Cecilia Rosca, MD, PhD; Cristina Dijmarescu, MD; Mihaela Simu, MD",
"content": [
"Pseudobulbar paralysis caused by bilateral opercular lesions, or Foix-Chavany-Marie syndrome (FCMS), was diagnosed on the basis of the patient's neurologic signs and neuroimaging findings. The clinical manifestations indicating paralysis of volitional facial, masticatory, pharyngeal, and lingual muscle movements, with preserved movement of these muscles with autonomic functions and emotion, are the defining features of FCMS.",
"The cortical form of pseudobulbar palsy is distinguished from a noncortical pseudobulbar palsy by the absence of emotional lability or pathological laughter and crying and the absence of bladder and bowel incontinence. Furthermore, brain MRI confirmed the presence of ischemic lesions in both anterior opercula.",
"FCMS is a rare form of pseudobulbar paralysis caused by bilateral lesions of the anterior opercular cortex. Although it was first described in 1837 by Magnus,[1] FCMS was named after the French authors who investigated it more extensively in 1926.[2,3] A congenital form of the syndrome was reported in 1953 by Worster-Drought.[4]",
"On the basis of etiology, five forms of FCMS have been proposed[5]:",
"Classical acute form: This is most often related to vascular causes. Most cases are due to bilateral sequential, rarely simultaneous,[6] lesions of the anterior operculum. Some cases can be due to a unilateral opercular lesion. Rarely, an opercular lesion associated with a contralateral subcortical lesion can lead to FCMS.[5,7,8] The most common cause of the acute form is cerebral infarct. Less frequently, it has been described in multiple sclerosis,[9]acute disseminated encephalomyelitis,[10]vasculitis,[11]moyamoya disease,[12] and head trauma.[13]",
"Subacute form: This is due to central nervous system infections, such as herpes simplex encephalitis,[14,15]HIV infection,[16]toxoplasmosis,[17] and tuberculous meningitis.[18]",
"Developmental form: This is mostly due to neuronal migration disorders, such as dysgenesis of the opercular cortex.[5,19] The most common radiologic and pathologic findings have included polymicrogyria, incomplete opercular formation, associated absence of septum pellucidum,[20,21] and bilateral perisylvian ulegyria.[22]",
"Reversible form: This is found in patients with epilepsy. Most cases are in children with benign rolandic epilepsy or hemispheric malformations, who develop a reversible FCMS-like condition in status epilepticus.[5,19,23] However, it has also been reported in some adult patients.[24,25]",
"Chronic, slowly progressive FCMS: This is present in neurodegenerative disorders, such as primary progressive aphasia.[26,27]",
"The present case is a classical acute form of FCMS due to a cerebral infarction. The main differential diagnosis of pseudobulbar syndrome is bulbar paralysis. In FCMS, contrary to bulbar palsy due to lower motor neuron lesions, the brainstem reflexes (eg, jaw jerk) are preserved or hyperactive and no fasciculations or muscle atrophies are noted. However, the gag reflex is absent, and it is not by itself a discriminating sign. Furthermore, the voluntary-automatic dissociation of bulbar muscle is another cardinal sign of pseudobulbar palsy."
],
"date": "April 04, 2022",
"figures": [],
"markdown": "# Neurology Case Challenge: Drooling and Dysphagia in a Man Who Can’t Speak\n\n **Authors:** Elena Cecilia Rosca, MD, PhD; Cristina Dijmarescu, MD; Mihaela Simu, MD \n **Date:** April 04, 2022\n\n ## Content\n\n Pseudobulbar paralysis caused by bilateral opercular lesions, or Foix-Chavany-Marie syndrome (FCMS), was diagnosed on the basis of the patient's neurologic signs and neuroimaging findings. The clinical manifestations indicating paralysis of volitional facial, masticatory, pharyngeal, and lingual muscle movements, with preserved movement of these muscles with autonomic functions and emotion, are the defining features of FCMS.\nThe cortical form of pseudobulbar palsy is distinguished from a noncortical pseudobulbar palsy by the absence of emotional lability or pathological laughter and crying and the absence of bladder and bowel incontinence. Furthermore, brain MRI confirmed the presence of ischemic lesions in both anterior opercula.\nFCMS is a rare form of pseudobulbar paralysis caused by bilateral lesions of the anterior opercular cortex. Although it was first described in 1837 by Magnus,[1] FCMS was named after the French authors who investigated it more extensively in 1926.[2,3] A congenital form of the syndrome was reported in 1953 by Worster-Drought.[4]\nOn the basis of etiology, five forms of FCMS have been proposed[5]:\nClassical acute form: This is most often related to vascular causes. Most cases are due to bilateral sequential, rarely simultaneous,[6] lesions of the anterior operculum. Some cases can be due to a unilateral opercular lesion. Rarely, an opercular lesion associated with a contralateral subcortical lesion can lead to FCMS.[5,7,8] The most common cause of the acute form is cerebral infarct. Less frequently, it has been described in multiple sclerosis,[9]acute disseminated encephalomyelitis,[10]vasculitis,[11]moyamoya disease,[12] and head trauma.[13]\nSubacute form: This is due to central nervous system infections, such as herpes simplex encephalitis,[14,15]HIV infection,[16]toxoplasmosis,[17] and tuberculous meningitis.[18]\nDevelopmental form: This is mostly due to neuronal migration disorders, such as dysgenesis of the opercular cortex.[5,19] The most common radiologic and pathologic findings have included polymicrogyria, incomplete opercular formation, associated absence of septum pellucidum,[20,21] and bilateral perisylvian ulegyria.[22]\nReversible form: This is found in patients with epilepsy. Most cases are in children with benign rolandic epilepsy or hemispheric malformations, who develop a reversible FCMS-like condition in status epilepticus.[5,19,23] However, it has also been reported in some adult patients.[24,25]\nChronic, slowly progressive FCMS: This is present in neurodegenerative disorders, such as primary progressive aphasia.[26,27]\nThe present case is a classical acute form of FCMS due to a cerebral infarction. The main differential diagnosis of pseudobulbar syndrome is bulbar paralysis. In FCMS, contrary to bulbar palsy due to lower motor neuron lesions, the brainstem reflexes (eg, jaw jerk) are preserved or hyperactive and no fasciculations or muscle atrophies are noted. However, the gag reflex is absent, and it is not by itself a discriminating sign. Furthermore, the voluntary-automatic dissociation of bulbar muscle is another cardinal sign of pseudobulbar palsy.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 837663,
"choiceText": "Brainstem stroke",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837665,
"choiceText": "Foix-Chavany-Marie syndrome",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837667,
"choiceText": "Myasthenia gravis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837669,
"choiceText": "Botulism",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837671,
"choiceText": "Amyotrophic lateral sclerosis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 263421,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Neurology Case Challenge: Drooling and Dysphagia in a Man Who Can’t Speak"
},
{
"authors": "Elena Cecilia Rosca, MD, PhD; Cristina Dijmarescu, MD; Mihaela Simu, MD",
"content": [
"The acute onset of dysphagia and anarthria should be differentiated from a lateral medullary syndrome (Wallenberg syndrome) due to vertebral artery occlusion or to posterior inferior cerebellar artery occlusion. The ipsilateral signs of a lateral medullary lesion include the following:",
"Dysarthria and dysphagia",
"Loss of taste from the posterior third of the tongue (due to lesions of cranial nerves IX, X, XI, and XII)",
"Ataxia (caused by damage to the inferior cerebellar peduncle and cerebellum)",
"Reduced corneal reflex temperature loss and facial pain (due to cranial nerve V damage)",
"Nystagmus",
"Hypoacousia (due to a cranial nerve VIII lesion)",
"Horner syndrome (caused by a lesion of the descending sympathetic fibers)",
"Contralateral findings include loss of pain and temperature sensation, indicating a lesion of the anterior spinothalamic tract. Other clinical signs of Wallenberg syndrome include tachycardia and dyspnea caused by cranial nerve X dysfunction.",
"Other causes of acute bulbar muscle dysfunction must also be considered. Botulism is an acute neurologic disease that causes severe paralysis due to a neurotoxin produced by Clostridium botulinum. In adults, botulism can be caused by the introduction of toxin-producing spores into wounds from injury involving contaminated soil; intravenous use of contaminated drugs; or ingestion of preformed neurotoxins in high-risk foods, including home-canned or home-processed fruits and vegetables, fish and fish products, condiments such as relish, and chili peppers. Most patients present with three to five of the following signs:",
"Dysphagia",
"Diplopia",
"Fixed mydriasis",
"Nausea",
"Vomiting",
"Dry mouth unrelieved by drinking fluids",
"Cranial nerve symptoms consist of dysarthria; dysphagia; suppressed gag reflex; extraocular muscle weakness; diplopia; and fixed, dilated pupils. Patients also present with descending paralysis of the motor and autonomic nerves. The patient in this case had only one of the major botulism symptoms, no oculomotor nerve involvement, and no lower motor neuron signs.",
"Another entity in the differential diagnosis is myasthenia gravis, an autoimmune disorder that involves the neuromuscular junction. The initial symptom is usually extraocular muscle weakness, tending to spread to the facial and bulbar muscles. Bulbar muscle involvement is common and is accompanied by weakness of head extension and flexion. As the disease progresses, truncal and limb muscles can be also affected. However, the weakness is fatigable, increased by sustained activity and alleviated by rest. The disease typically progresses over weeks or months, with exacerbations and remissions. Myasthenia gravis is diagnosed using clinical, laboratory (anti-acetylcholine receptor antibodies or autoantibodies to muscle-specific kinase), and electrophysiologic investigations.",
"In the present case, the bulbar muscle weakness was isolated, with no extraocular, neck, or trunk muscle involvement. Furthermore, the onset was acute and without fluctuations in the deficit."
],
"date": "April 04, 2022",
"figures": [],
"markdown": "# Neurology Case Challenge: Drooling and Dysphagia in a Man Who Can’t Speak\n\n **Authors:** Elena Cecilia Rosca, MD, PhD; Cristina Dijmarescu, MD; Mihaela Simu, MD \n **Date:** April 04, 2022\n\n ## Content\n\n The acute onset of dysphagia and anarthria should be differentiated from a lateral medullary syndrome (Wallenberg syndrome) due to vertebral artery occlusion or to posterior inferior cerebellar artery occlusion. The ipsilateral signs of a lateral medullary lesion include the following:\nDysarthria and dysphagia\nLoss of taste from the posterior third of the tongue (due to lesions of cranial nerves IX, X, XI, and XII)\nAtaxia (caused by damage to the inferior cerebellar peduncle and cerebellum)\nReduced corneal reflex temperature loss and facial pain (due to cranial nerve V damage)\nNystagmus\nHypoacousia (due to a cranial nerve VIII lesion)\nHorner syndrome (caused by a lesion of the descending sympathetic fibers)\nContralateral findings include loss of pain and temperature sensation, indicating a lesion of the anterior spinothalamic tract. Other clinical signs of Wallenberg syndrome include tachycardia and dyspnea caused by cranial nerve X dysfunction.\nOther causes of acute bulbar muscle dysfunction must also be considered. Botulism is an acute neurologic disease that causes severe paralysis due to a neurotoxin produced by Clostridium botulinum. In adults, botulism can be caused by the introduction of toxin-producing spores into wounds from injury involving contaminated soil; intravenous use of contaminated drugs; or ingestion of preformed neurotoxins in high-risk foods, including home-canned or home-processed fruits and vegetables, fish and fish products, condiments such as relish, and chili peppers. Most patients present with three to five of the following signs:\nDysphagia\nDiplopia\nFixed mydriasis\nNausea\nVomiting\nDry mouth unrelieved by drinking fluids\nCranial nerve symptoms consist of dysarthria; dysphagia; suppressed gag reflex; extraocular muscle weakness; diplopia; and fixed, dilated pupils. Patients also present with descending paralysis of the motor and autonomic nerves. The patient in this case had only one of the major botulism symptoms, no oculomotor nerve involvement, and no lower motor neuron signs.\nAnother entity in the differential diagnosis is myasthenia gravis, an autoimmune disorder that involves the neuromuscular junction. The initial symptom is usually extraocular muscle weakness, tending to spread to the facial and bulbar muscles. Bulbar muscle involvement is common and is accompanied by weakness of head extension and flexion. As the disease progresses, truncal and limb muscles can be also affected. However, the weakness is fatigable, increased by sustained activity and alleviated by rest. The disease typically progresses over weeks or months, with exacerbations and remissions. Myasthenia gravis is diagnosed using clinical, laboratory (anti-acetylcholine receptor antibodies or autoantibodies to muscle-specific kinase), and electrophysiologic investigations.\nIn the present case, the bulbar muscle weakness was isolated, with no extraocular, neck, or trunk muscle involvement. Furthermore, the onset was acute and without fluctuations in the deficit.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Neurology Case Challenge: Drooling and Dysphagia in a Man Who Can’t Speak"
},
{
"authors": "Elena Cecilia Rosca, MD, PhD; Cristina Dijmarescu, MD; Mihaela Simu, MD",
"content": [
"Amyotrophic lateral sclerosis (ALS) with bulbar onset is another diagnosis that could be considered. Initial symptoms are dysarthria and dysphagia, but the onset is subacute. The diagnosis of ALS may not be obvious early in the disease course; observation of progression of symptoms is necessary. Clinically definite ALS is diagnosed when the patient has upper motor neuron and lower motor neuron signs in at least three body segments.",
"Management of FCMS depends on the etiology and clinical type. In this case, treatment was focused on preventing further progression of the underlying cerebrovascular disease; the patient received anticoagulant therapy (a new oral anticoagulant), antiarrhythmic agents (digoxin, metoprolol), a statin (rosuvastatin), an angiotensin-converting enzyme inhibitor (perindopril), and antidiabetics. Because of the severe swallowing problems and in order to prevent aspiration pneumonia, a nasogastric feeding tube was placed. For communication, the patient used writing as an alternative to speech output, and he underwent speech therapy.",
"After 1 month of hospitalization, the patient was discharged with mildly improved status. He was able to open and close his mouth, to make some movements of the tongue in the mouth, and to articulate some monosyllabic words (\"yes,\" \"no\"). At the end of the 4 weeks, he was tube-dependent, but with some oral diet of a semi-liquid consistency."
],
"date": "April 04, 2022",
"figures": [],
"markdown": "# Neurology Case Challenge: Drooling and Dysphagia in a Man Who Can’t Speak\n\n **Authors:** Elena Cecilia Rosca, MD, PhD; Cristina Dijmarescu, MD; Mihaela Simu, MD \n **Date:** April 04, 2022\n\n ## Content\n\n Amyotrophic lateral sclerosis (ALS) with bulbar onset is another diagnosis that could be considered. Initial symptoms are dysarthria and dysphagia, but the onset is subacute. The diagnosis of ALS may not be obvious early in the disease course; observation of progression of symptoms is necessary. Clinically definite ALS is diagnosed when the patient has upper motor neuron and lower motor neuron signs in at least three body segments.\nManagement of FCMS depends on the etiology and clinical type. In this case, treatment was focused on preventing further progression of the underlying cerebrovascular disease; the patient received anticoagulant therapy (a new oral anticoagulant), antiarrhythmic agents (digoxin, metoprolol), a statin (rosuvastatin), an angiotensin-converting enzyme inhibitor (perindopril), and antidiabetics. Because of the severe swallowing problems and in order to prevent aspiration pneumonia, a nasogastric feeding tube was placed. For communication, the patient used writing as an alternative to speech output, and he underwent speech therapy.\nAfter 1 month of hospitalization, the patient was discharged with mildly improved status. He was able to open and close his mouth, to make some movements of the tongue in the mouth, and to articulate some monosyllabic words (\"yes,\" \"no\"). At the end of the 4 weeks, he was tube-dependent, but with some oral diet of a semi-liquid consistency.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 837673,
"choiceText": "Absence of gag reflex",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837675,
"choiceText": "Presence of bowel and bladder incontinence",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837677,
"choiceText": "Dissociation of automatic and voluntary movements of the bulbar muscles",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837679,
"choiceText": "Presence of pathological laughter and crying",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Voluntary control of the masticatory, facial, pharyngeal, and lingual muscles is provided by primary motor cortex and their projections to the nuclei of the cranial nerves V, VII, IX, X, and XII. The emotional, automatic control of these muscles is provided by alternative pathways from amygdala and lateral hypothalamus that go to the brainstem via the medial forebrain bundle and dorsal longitudinal fasciculus.<sup>8,28,29</sup><br>\r\n<br>\r\nAlthough pseudobulbar cortical palsy due to anterior opercular lesions shares some clinical features with subcortical pseudobulbar paralysis, subtle differences help the diagnosis. In the cortical form, the dissociation between automatic and voluntary movements of the bulbar muscles, the absence of emotional lability, and the absence of bowel and bladder incontinence are the main distinctive features. Although frontal release signs are rarely reported in FCMS, pathological laughter or crying suggests that the lesions extend beyond the opercular cortex.<sup>5</sup><br>\r\n<br>\r\nThe gag reflex is variably absent or diminished in FCMS. In subcortical lesions, the gag reflex is usually exaggerated.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 263423,
"questionText": "Which is a core feature that distinguishes FCMS from noncortical pseudobulbar lesions?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 837681,
"choiceText": "Good, with almost complete recovery of dysphagia and dysarthria",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837683,
"choiceText": "Good, with rapid return to oral feeding",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837685,
"choiceText": "Slow, but complete recovery of swallowing and speech functions",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837687,
"choiceText": "Poor, with need for percutaneous endoscopic gastrostomy (PEG) tube feeding",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "In general, patients with FCMS have a poor prognosis for recovery of speech and swallowing. Most cases involve severe impairment of the voluntary phase of swallowing; PEG tube placement can prevent the adverse effects of nasogastric tube feeding.<br>\r\n<br>\r\nSpeech therapy that emphasizes alternative communication strategies can be useful. In patients who have had a stroke, logopedic dysphagia training combined with neuromuscular electrical stimulation was reported to improve swallowing problems; however, no universally accepted protocol for these methods is recognized.<sup>30,31</sup> Rare cases with unilateral lesions of the rolandic operculum have been associated with a better prognosis.<sup>8,32</sup> Some patients with FCMS of epileptic cause have reversible symptoms.<sup>33</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 263425,
"questionText": "FCMS is associated with which prognosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Neurology Case Challenge: Drooling and Dysphagia in a Man Who Can’t Speak"
},
{
"authors": "Elena Cecilia Rosca, MD, PhD; Cristina Dijmarescu, MD; Mihaela Simu, MD",
"content": [],
"date": "April 04, 2022",
"figures": [],
"markdown": "# Neurology Case Challenge: Drooling and Dysphagia in a Man Who Can’t Speak\n\n **Authors:** Elena Cecilia Rosca, MD, PhD; Cristina Dijmarescu, MD; Mihaela Simu, MD \n **Date:** April 04, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 837673,
"choiceText": "Absence of gag reflex",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837675,
"choiceText": "Presence of bowel and bladder incontinence",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837677,
"choiceText": "Dissociation of automatic and voluntary movements of the bulbar muscles",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837679,
"choiceText": "Presence of pathological laughter and crying",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Voluntary control of the masticatory, facial, pharyngeal, and lingual muscles is provided by primary motor cortex and their projections to the nuclei of the cranial nerves V, VII, IX, X, and XII. The emotional, automatic control of these muscles is provided by alternative pathways from amygdala and lateral hypothalamus that go to the brainstem via the medial forebrain bundle and dorsal longitudinal fasciculus.<sup>8,28,29</sup><br>\r\n<br>\r\nAlthough pseudobulbar cortical palsy due to anterior opercular lesions shares some clinical features with subcortical pseudobulbar paralysis, subtle differences help the diagnosis. In the cortical form, the dissociation between automatic and voluntary movements of the bulbar muscles, the absence of emotional lability, and the absence of bowel and bladder incontinence are the main distinctive features. Although frontal release signs are rarely reported in FCMS, pathological laughter or crying suggests that the lesions extend beyond the opercular cortex.<sup>5</sup><br>\r\n<br>\r\nThe gag reflex is variably absent or diminished in FCMS. In subcortical lesions, the gag reflex is usually exaggerated.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 263423,
"questionText": "Which is a core feature that distinguishes FCMS from noncortical pseudobulbar lesions?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 837681,
"choiceText": "Good, with almost complete recovery of dysphagia and dysarthria",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837683,
"choiceText": "Good, with rapid return to oral feeding",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837685,
"choiceText": "Slow, but complete recovery of swallowing and speech functions",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837687,
"choiceText": "Poor, with need for percutaneous endoscopic gastrostomy (PEG) tube feeding",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "In general, patients with FCMS have a poor prognosis for recovery of speech and swallowing. Most cases involve severe impairment of the voluntary phase of swallowing; PEG tube placement can prevent the adverse effects of nasogastric tube feeding.<br>\r\n<br>\r\nSpeech therapy that emphasizes alternative communication strategies can be useful. In patients who have had a stroke, logopedic dysphagia training combined with neuromuscular electrical stimulation was reported to improve swallowing problems; however, no universally accepted protocol for these methods is recognized.<sup>30,31</sup> Rare cases with unilateral lesions of the rolandic operculum have been associated with a better prognosis.<sup>8,32</sup> Some patients with FCMS of epileptic cause have reversible symptoms.<sup>33</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 263425,
"questionText": "FCMS is associated with which prognosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Neurology Case Challenge: Drooling and Dysphagia in a Man Who Can’t Speak"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 837663,
"choiceText": "Brainstem stroke",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837665,
"choiceText": "Foix-Chavany-Marie syndrome",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837667,
"choiceText": "Myasthenia gravis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837669,
"choiceText": "Botulism",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837671,
"choiceText": "Amyotrophic lateral sclerosis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 263421,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 837673,
"choiceText": "Absence of gag reflex",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837675,
"choiceText": "Presence of bowel and bladder incontinence",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837677,
"choiceText": "Dissociation of automatic and voluntary movements of the bulbar muscles",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837679,
"choiceText": "Presence of pathological laughter and crying",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Voluntary control of the masticatory, facial, pharyngeal, and lingual muscles is provided by primary motor cortex and their projections to the nuclei of the cranial nerves V, VII, IX, X, and XII. The emotional, automatic control of these muscles is provided by alternative pathways from amygdala and lateral hypothalamus that go to the brainstem via the medial forebrain bundle and dorsal longitudinal fasciculus.<sup>8,28,29</sup><br>\r\n<br>\r\nAlthough pseudobulbar cortical palsy due to anterior opercular lesions shares some clinical features with subcortical pseudobulbar paralysis, subtle differences help the diagnosis. In the cortical form, the dissociation between automatic and voluntary movements of the bulbar muscles, the absence of emotional lability, and the absence of bowel and bladder incontinence are the main distinctive features. Although frontal release signs are rarely reported in FCMS, pathological laughter or crying suggests that the lesions extend beyond the opercular cortex.<sup>5</sup><br>\r\n<br>\r\nThe gag reflex is variably absent or diminished in FCMS. In subcortical lesions, the gag reflex is usually exaggerated.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 263423,
"questionText": "Which is a core feature that distinguishes FCMS from noncortical pseudobulbar lesions?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 837681,
"choiceText": "Good, with almost complete recovery of dysphagia and dysarthria",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837683,
"choiceText": "Good, with rapid return to oral feeding",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837685,
"choiceText": "Slow, but complete recovery of swallowing and speech functions",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 837687,
"choiceText": "Poor, with need for percutaneous endoscopic gastrostomy (PEG) tube feeding",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "In general, patients with FCMS have a poor prognosis for recovery of speech and swallowing. Most cases involve severe impairment of the voluntary phase of swallowing; PEG tube placement can prevent the adverse effects of nasogastric tube feeding.<br>\r\n<br>\r\nSpeech therapy that emphasizes alternative communication strategies can be useful. In patients who have had a stroke, logopedic dysphagia training combined with neuromuscular electrical stimulation was reported to improve swallowing problems; however, no universally accepted protocol for these methods is recognized.<sup>30,31</sup> Rare cases with unilateral lesions of the rolandic operculum have been associated with a better prognosis.<sup>8,32</sup> Some patients with FCMS of epileptic cause have reversible symptoms.<sup>33</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 263425,
"questionText": "FCMS is associated with which prognosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
833128 | /viewarticle/833128 | [
{
"authors": "Romesh Khardori, MD, PhD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 36-year-old man presents with fatigue, increased thirst, and leg cramps for the past several months. He reports feeling warm and having cough with expectoration for the past 10 days.",
"He was recently informed that he has diabetes and hypertension (blood pressure, 140/90 mm Hg) and was advised to watch his diet, lose weight, and check weekly fasting blood glucose levels. He was placed on metformin (500 mg twice daily). His fasting blood glucose level has steadily increased; 4 months prior, his glycated hemoglobin level was 8.3%. Insulin glargine (30 U at bedtime) was added to his treatment protocol.",
"He does not report any other medical problems and is a nonsmoker. He also states that he is not able to lose weight, despite his efforts."
],
"date": "March 31, 2022",
"figures": [],
"markdown": "# Endo Case Challenge: A 36-Year-Old Has Cramping, Lung Issues and Can’t Lose Weight\n\n **Authors:** Romesh Khardori, MD, PhD \n **Date:** March 31, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 36-year-old man presents with fatigue, increased thirst, and leg cramps for the past several months. He reports feeling warm and having cough with expectoration for the past 10 days.\nHe was recently informed that he has diabetes and hypertension (blood pressure, 140/90 mm Hg) and was advised to watch his diet, lose weight, and check weekly fasting blood glucose levels. He was placed on metformin (500 mg twice daily). His fasting blood glucose level has steadily increased; 4 months prior, his glycated hemoglobin level was 8.3%. Insulin glargine (30 U at bedtime) was added to his treatment protocol.\nHe does not report any other medical problems and is a nonsmoker. He also states that he is not able to lose weight, despite his efforts.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Endo Case Challenge: A 36-Year-Old Has Cramping, Lung Issues and Can’t Lose Weight"
},
{
"authors": "Romesh Khardori, MD, PhD",
"content": [
"The patient is alert and in no distress. His face appears plethoric, and his eyes are mildly congested. He is 5 ft, 7 in tall and weighs 187 lb (84.8 kg). His blood pressure is 180/100 mm Hg. His heart rate and respirations are normal. He has 1+ pedal edema.",
"A pulmonary examination was remarkable for dullness over the left lower lung posteriorly and diminished air entry. He has no visceromegaly. In the past 4 months, he has gained 20 lb. Lung radiography is obtained and reveals loss of volume at the left base, elevation of the diaphragm on the left side, and opacity behind the heart (Figure 1).",
"Figure 1.",
"His CBC count is unremarkable. His BUN level is 28 mg/dL (reference range, 6-24 mg/dL), and his creatinine level is 0.9 mg/dL (reference range, 0.7-1.3 mg/dL). Serum electrolyte levels were all within reference ranges, except for a low potassium level (3.2 mmol/L). His serum glucose level is 234 mg/dL, and his glycated hemoglobin level is 9.2%.",
"He has type 2 diabetes mellitus and is diagnosed with recovering pneumonia in the setting of left lower lobe atelectasis. Weight gain, hypertension, facial flushing, and hypokalemia are also present. He is scheduled for bronchoscopy to evaluate his lung mass and referred to an endocrinologist for further evaluation. Given the lung mass and facial flushing, further testing was performed.",
"His fasting plasma cortisol is 27 µg/dL (reference range, 5-25 µg/dL), and his adrenocorticotropic hormone (ACTH) level is 127 pg/mL (reference range, 10-60 pg/mL). The patient fails a high-dose (8 mg) overnight dexamethasone suppression test (morning plasma cortisol, 26 µg/dL; ACTH level is 132 pg/mL)."
],
"date": "March 31, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/833/128/833128-thumb-1.jpg"
}
],
"markdown": "# Endo Case Challenge: A 36-Year-Old Has Cramping, Lung Issues and Can’t Lose Weight\n\n **Authors:** Romesh Khardori, MD, PhD \n **Date:** March 31, 2022\n\n ## Content\n\n The patient is alert and in no distress. His face appears plethoric, and his eyes are mildly congested. He is 5 ft, 7 in tall and weighs 187 lb (84.8 kg). His blood pressure is 180/100 mm Hg. His heart rate and respirations are normal. He has 1+ pedal edema.\nA pulmonary examination was remarkable for dullness over the left lower lung posteriorly and diminished air entry. He has no visceromegaly. In the past 4 months, he has gained 20 lb. Lung radiography is obtained and reveals loss of volume at the left base, elevation of the diaphragm on the left side, and opacity behind the heart (Figure 1).\nFigure 1.\nHis CBC count is unremarkable. His BUN level is 28 mg/dL (reference range, 6-24 mg/dL), and his creatinine level is 0.9 mg/dL (reference range, 0.7-1.3 mg/dL). Serum electrolyte levels were all within reference ranges, except for a low potassium level (3.2 mmol/L). His serum glucose level is 234 mg/dL, and his glycated hemoglobin level is 9.2%.\nHe has type 2 diabetes mellitus and is diagnosed with recovering pneumonia in the setting of left lower lobe atelectasis. Weight gain, hypertension, facial flushing, and hypokalemia are also present. He is scheduled for bronchoscopy to evaluate his lung mass and referred to an endocrinologist for further evaluation. Given the lung mass and facial flushing, further testing was performed.\nHis fasting plasma cortisol is 27 µg/dL (reference range, 5-25 µg/dL), and his adrenocorticotropic hormone (ACTH) level is 127 pg/mL (reference range, 10-60 pg/mL). The patient fails a high-dose (8 mg) overnight dexamethasone suppression test (morning plasma cortisol, 26 µg/dL; ACTH level is 132 pg/mL).\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 777529,
"choiceText": "Dietary indiscretion/stress hyperphagia",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777531,
"choiceText": "Acquired hypothyroidism",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777533,
"choiceText": "Stress hypercortisolemia and hyperphagia",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777535,
"choiceText": "Cushing syndrome/endobronchial carcinoid with ectopic ACTH secretion",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 243583,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Endo Case Challenge: A 36-Year-Old Has Cramping, Lung Issues and Can’t Lose Weight"
},
{
"authors": "Romesh Khardori, MD, PhD",
"content": [
"The endocrinologist obtained an additional history of verified \"stretch marks\" as striae often seen in Cushing syndrome. He also noticed prominent supraclavicular fat pads. A combination of hypercortisolemia, elevated ACTH levels, hypokalemia, fatigue, and persistent left lower lung atelectasis persuaded the endocrinologist to strongly consider ectopic ACTH syndrome. The facial flushing and lack of a tobacco smoking history favored an endobronchial carcinoid, as opposed to small cell lung cancer. Bronchoscopy was performed, and histoimmunopathology confirmed the diagnosis of an ACTH-secreting carcinoid. An example of similar immunohistopathology is shown in Figure 2.",
"Figure 2.",
"Although other causes of type 2 diabetes mellitus and hypertension are possible, this combination of findings with unprovoked hypokalemia strongly suggests Cushing syndrome.",
"Dietary indiscretion and consumption of excess calories can cause weight gain; however, in a patient with worsening glycemic control, the presence of glycosuria generally negates excessive weight gain. Hypothyroidism makes it difficult to lose weight and may lead to increase in blood pressure or worsening of hypertension. However, neither causes unprovoked hypokalemia.",
"Stress hyperphagia is often noticed in people operating under pressure. People report frequent snacking, and stress leads to worsening of glycemia. Catecholamine surge associated with physical injury is accompanied by catecholamine-mediated hypokalemia. Hypokalemia is not persistent and abates when the stress level recedes. Weight gain is not a feature of catecholamine-driven hypertension or hypokalemia (eg, pheochromocytoma)."
],
"date": "March 31, 2022",
"figures": [
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/833/128/833128-thumb-2.jpg"
}
],
"markdown": "# Endo Case Challenge: A 36-Year-Old Has Cramping, Lung Issues and Can’t Lose Weight\n\n **Authors:** Romesh Khardori, MD, PhD \n **Date:** March 31, 2022\n\n ## Content\n\n The endocrinologist obtained an additional history of verified \"stretch marks\" as striae often seen in Cushing syndrome. He also noticed prominent supraclavicular fat pads. A combination of hypercortisolemia, elevated ACTH levels, hypokalemia, fatigue, and persistent left lower lung atelectasis persuaded the endocrinologist to strongly consider ectopic ACTH syndrome. The facial flushing and lack of a tobacco smoking history favored an endobronchial carcinoid, as opposed to small cell lung cancer. Bronchoscopy was performed, and histoimmunopathology confirmed the diagnosis of an ACTH-secreting carcinoid. An example of similar immunohistopathology is shown in Figure 2.\nFigure 2.\nAlthough other causes of type 2 diabetes mellitus and hypertension are possible, this combination of findings with unprovoked hypokalemia strongly suggests Cushing syndrome.\nDietary indiscretion and consumption of excess calories can cause weight gain; however, in a patient with worsening glycemic control, the presence of glycosuria generally negates excessive weight gain. Hypothyroidism makes it difficult to lose weight and may lead to increase in blood pressure or worsening of hypertension. However, neither causes unprovoked hypokalemia.\nStress hyperphagia is often noticed in people operating under pressure. People report frequent snacking, and stress leads to worsening of glycemia. Catecholamine surge associated with physical injury is accompanied by catecholamine-mediated hypokalemia. Hypokalemia is not persistent and abates when the stress level recedes. Weight gain is not a feature of catecholamine-driven hypertension or hypokalemia (eg, pheochromocytoma).\n\n ## Figures\n\n **Figure 2.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 777529,
"choiceText": "Dietary indiscretion/stress hyperphagia",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777531,
"choiceText": "Acquired hypothyroidism",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777533,
"choiceText": "Stress hypercortisolemia and hyperphagia",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777535,
"choiceText": "Cushing syndrome/endobronchial carcinoid with ectopic ACTH secretion",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 243583,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Endo Case Challenge: A 36-Year-Old Has Cramping, Lung Issues and Can’t Lose Weight"
},
{
"authors": "Romesh Khardori, MD, PhD",
"content": [
"The constellation of worsening glycemic control, hypertension, hypokalemia, and weight gain strongly supports the diagnosis of Cushing syndrome. In this case, the elevated ACTH level did not indicate a cortisol-producing adrenal tumor, which would suppress ACTH. The patient had normal head MRI findings, which does not exclude pituitary Cushing syndrome because these tumors are often small. The nonsuppressible high-dose dexamethasone suppression test results rule out pituitary Cushing syndrome, which would suppress with high doses of dexamethasone but not with low doses. Some bronchial carcinoids produce corticotropin-releasing hormone (CRH) instead of ACTH and otherwise mimic pituitary Cushing syndrome. Even inferior petrosal sinus sampling (IPSS) for ACTH suggests pituitary Cushing syndrome in these cases, and bronchoscopic evaluation may be required.",
"A low-risk procedure such as bronchoscopy or biopsy is available in most centers and should be performed first if the index of suspicion is high for a bronchial carcinoid.",
"In this patient, the surgical excision of carcinoid tumor was accompanied by rapid normalization of blood pressure and hypokalemia. Plasma ACTH and cortisol levels rapidly decreased over the next few days. He was sent home on prednisone, which was tapered over 12 weeks to 5 mg/day and completely stopped at 6 months, when the hypothalamic-pituitary-adrenal axis became fully operational. By then, he had lost 30 lb. His fasting blood glucose level was 112 mg/dL, and insulin was stopped. His glycated hemoglobin was 7.3%.",
"Association between nonpituitary or adrenal neoplasm and Cushing syndrome dates back to 1928 when Brown first described a case with small cell lung cancer with features resembling Cushing syndrome.[1] ACTH was later shown to be produced by these neoplasms.[2] The spectrum of ACTH-secreting neoplasms now extends to carcinoid tumors, pheochromocytomas, medullary thyroid carcinoma, and islet cell tumors. Other rare ectopic locations have been described as well. Occasionally the driver may be ectopic CRH.",
"Ectopic ACTH/CRH secretion accounts for 10% to 15% of Cushing syndrome cases. Bronchial carcinoid tumors represent 1% to 5% of all lung tumors; approximately 1% to 5% of them are associated with ectopic ACTH secretion. Bronchopulmonary tumors are considered to be l-w grade, although some can metastasize. They have epithelial and neuroendocrine differentiation. Resolution of hormonal abnormalities is quite rapid. Somatostatin scintigraphy and selective pulmonary artery sampling for ACTH have been used to localize carcinoid tumors."
],
"date": "March 31, 2022",
"figures": [],
"markdown": "# Endo Case Challenge: A 36-Year-Old Has Cramping, Lung Issues and Can’t Lose Weight\n\n **Authors:** Romesh Khardori, MD, PhD \n **Date:** March 31, 2022\n\n ## Content\n\n The constellation of worsening glycemic control, hypertension, hypokalemia, and weight gain strongly supports the diagnosis of Cushing syndrome. In this case, the elevated ACTH level did not indicate a cortisol-producing adrenal tumor, which would suppress ACTH. The patient had normal head MRI findings, which does not exclude pituitary Cushing syndrome because these tumors are often small. The nonsuppressible high-dose dexamethasone suppression test results rule out pituitary Cushing syndrome, which would suppress with high doses of dexamethasone but not with low doses. Some bronchial carcinoids produce corticotropin-releasing hormone (CRH) instead of ACTH and otherwise mimic pituitary Cushing syndrome. Even inferior petrosal sinus sampling (IPSS) for ACTH suggests pituitary Cushing syndrome in these cases, and bronchoscopic evaluation may be required.\nA low-risk procedure such as bronchoscopy or biopsy is available in most centers and should be performed first if the index of suspicion is high for a bronchial carcinoid.\nIn this patient, the surgical excision of carcinoid tumor was accompanied by rapid normalization of blood pressure and hypokalemia. Plasma ACTH and cortisol levels rapidly decreased over the next few days. He was sent home on prednisone, which was tapered over 12 weeks to 5 mg/day and completely stopped at 6 months, when the hypothalamic-pituitary-adrenal axis became fully operational. By then, he had lost 30 lb. His fasting blood glucose level was 112 mg/dL, and insulin was stopped. His glycated hemoglobin was 7.3%.\nAssociation between nonpituitary or adrenal neoplasm and Cushing syndrome dates back to 1928 when Brown first described a case with small cell lung cancer with features resembling Cushing syndrome.[1] ACTH was later shown to be produced by these neoplasms.[2] The spectrum of ACTH-secreting neoplasms now extends to carcinoid tumors, pheochromocytomas, medullary thyroid carcinoma, and islet cell tumors. Other rare ectopic locations have been described as well. Occasionally the driver may be ectopic CRH.\nEctopic ACTH/CRH secretion accounts for 10% to 15% of Cushing syndrome cases. Bronchial carcinoid tumors represent 1% to 5% of all lung tumors; approximately 1% to 5% of them are associated with ectopic ACTH secretion. Bronchopulmonary tumors are considered to be l-w grade, although some can metastasize. They have epithelial and neuroendocrine differentiation. Resolution of hormonal abnormalities is quite rapid. Somatostatin scintigraphy and selective pulmonary artery sampling for ACTH have been used to localize carcinoid tumors.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Endo Case Challenge: A 36-Year-Old Has Cramping, Lung Issues and Can’t Lose Weight"
},
{
"authors": "Romesh Khardori, MD, PhD",
"content": [
"In this patient, gain from surgical excision extended to better achievement of glycemic control and near resolution of hypertension. He was normotensive on 10 mg daily of ramipril. Previously, he required four agents and his blood pressure control was suboptimal. At higher concentrations of cortisol, activity spills over to mineralocorticoid receptor, thus mimicking a primary mineralocorticoid excess state.",
"Failure to lose weight and worsening of glycemic control should prompt search for precipitating factors beyond consideration of dietary indiscretion or noncompliance with therapy. When worsening of hypertension and emergence/persistence of hypokalemia is noticed, consider glucocorticoid/mineralocorticoid and catecholamine excess states. Although hyperthyroidism causes worsening of glycemic control, weight gain is less common.",
"Glucocorticoid excess state (more so in hyperglycemic patients with diabetes) is a perfect setup for superadded bacterial or fungal infections, often with fatal outcome.[3] Early diagnosis and treatment is life-saving.",
"A single-institution review of ACTH-secreting bronchial carcinoid tumor reinforced early detection and aggressive management to reduce consequences of chronic hypercortisolism and reduce risk for metastases.[4] Mifepristone, a glucocorticoid/progesterone receptor antagonist, was approved for the management of hyperglycemia in patients with Cushing syndrome. However, it may worsen hypertension and hypokalemia."
],
"date": "March 31, 2022",
"figures": [],
"markdown": "# Endo Case Challenge: A 36-Year-Old Has Cramping, Lung Issues and Can’t Lose Weight\n\n **Authors:** Romesh Khardori, MD, PhD \n **Date:** March 31, 2022\n\n ## Content\n\n In this patient, gain from surgical excision extended to better achievement of glycemic control and near resolution of hypertension. He was normotensive on 10 mg daily of ramipril. Previously, he required four agents and his blood pressure control was suboptimal. At higher concentrations of cortisol, activity spills over to mineralocorticoid receptor, thus mimicking a primary mineralocorticoid excess state.\nFailure to lose weight and worsening of glycemic control should prompt search for precipitating factors beyond consideration of dietary indiscretion or noncompliance with therapy. When worsening of hypertension and emergence/persistence of hypokalemia is noticed, consider glucocorticoid/mineralocorticoid and catecholamine excess states. Although hyperthyroidism causes worsening of glycemic control, weight gain is less common.\nGlucocorticoid excess state (more so in hyperglycemic patients with diabetes) is a perfect setup for superadded bacterial or fungal infections, often with fatal outcome.[3] Early diagnosis and treatment is life-saving.\nA single-institution review of ACTH-secreting bronchial carcinoid tumor reinforced early detection and aggressive management to reduce consequences of chronic hypercortisolism and reduce risk for metastases.[4] Mifepristone, a glucocorticoid/progesterone receptor antagonist, was approved for the management of hyperglycemia in patients with Cushing syndrome. However, it may worsen hypertension and hypokalemia.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 777537,
"choiceText": "Increasing glucagon secretion ",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777539,
"choiceText": "Decreasing hepatic gluconeogenesis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777541,
"choiceText": "Increasing peripheral glucose uptake",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777543,
"choiceText": "Increasing pancreatic insulin secretion",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777561,
"choiceText": "Increasing hepatic glucose output",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Glucocorticoids do not cause increased glucagon concentration. Glucocorticoids lead to hyperglycemia by inducing insulin resistance in the periphery and impairing insulin release from the beta cell of pancreas.<sup>[5]</sup> Osteocalcin reduction induced by glucocorticoids may be involved in the impairment of function of pancreatic beta cell.<sup>[6]</sup>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 243585,
"questionText": "Which of these mechanisms worsen glycemic control in patients with type 2 diabetes who are administered glucocorticoids?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 777545,
"choiceText": "Impaired renal function",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777547,
"choiceText": "Clinical syndrome of adrenal insufficiency",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777549,
"choiceText": "Diarrhea",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777551,
"choiceText": "Liver impairment",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Mifepristone is a glucocorticoid and progesterone receptor antagonist. Although it is approved for management of hyperglycemia associated with Cushing syndrome, patients must be carefully monitored for worsening of hypertension and hypokalemia. This has to do with mineralocorticoid receptor's exposure to higher circulating concentrations of plasma cortisol. This results in a clinical situation that mimics a mineralocorticoid excess state, worsening hypertension and hypokalemia. Furthermore, it also increases the risk for clinical syndrome of adrenal insufficiency.<sup>[7]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 243587,
"questionText": "Which is a potential risk factor in patients with Cushing syndrome and diabetes mellitus?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Endo Case Challenge: A 36-Year-Old Has Cramping, Lung Issues and Can’t Lose Weight"
},
{
"authors": "Romesh Khardori, MD, PhD",
"content": [],
"date": "March 31, 2022",
"figures": [],
"markdown": "# Endo Case Challenge: A 36-Year-Old Has Cramping, Lung Issues and Can’t Lose Weight\n\n **Authors:** Romesh Khardori, MD, PhD \n **Date:** March 31, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 777537,
"choiceText": "Increasing glucagon secretion ",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777539,
"choiceText": "Decreasing hepatic gluconeogenesis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777541,
"choiceText": "Increasing peripheral glucose uptake",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777543,
"choiceText": "Increasing pancreatic insulin secretion",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777561,
"choiceText": "Increasing hepatic glucose output",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Glucocorticoids do not cause increased glucagon concentration. Glucocorticoids lead to hyperglycemia by inducing insulin resistance in the periphery and impairing insulin release from the beta cell of pancreas.<sup>[5]</sup> Osteocalcin reduction induced by glucocorticoids may be involved in the impairment of function of pancreatic beta cell.<sup>[6]</sup>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 243585,
"questionText": "Which of these mechanisms worsen glycemic control in patients with type 2 diabetes who are administered glucocorticoids?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 777545,
"choiceText": "Impaired renal function",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777547,
"choiceText": "Clinical syndrome of adrenal insufficiency",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777549,
"choiceText": "Diarrhea",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777551,
"choiceText": "Liver impairment",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Mifepristone is a glucocorticoid and progesterone receptor antagonist. Although it is approved for management of hyperglycemia associated with Cushing syndrome, patients must be carefully monitored for worsening of hypertension and hypokalemia. This has to do with mineralocorticoid receptor's exposure to higher circulating concentrations of plasma cortisol. This results in a clinical situation that mimics a mineralocorticoid excess state, worsening hypertension and hypokalemia. Furthermore, it also increases the risk for clinical syndrome of adrenal insufficiency.<sup>[7]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 243587,
"questionText": "Which is a potential risk factor in patients with Cushing syndrome and diabetes mellitus?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Endo Case Challenge: A 36-Year-Old Has Cramping, Lung Issues and Can’t Lose Weight"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 777529,
"choiceText": "Dietary indiscretion/stress hyperphagia",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777531,
"choiceText": "Acquired hypothyroidism",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777533,
"choiceText": "Stress hypercortisolemia and hyperphagia",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777535,
"choiceText": "Cushing syndrome/endobronchial carcinoid with ectopic ACTH secretion",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 243583,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 777537,
"choiceText": "Increasing glucagon secretion ",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777539,
"choiceText": "Decreasing hepatic gluconeogenesis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777541,
"choiceText": "Increasing peripheral glucose uptake",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777543,
"choiceText": "Increasing pancreatic insulin secretion",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777561,
"choiceText": "Increasing hepatic glucose output",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Glucocorticoids do not cause increased glucagon concentration. Glucocorticoids lead to hyperglycemia by inducing insulin resistance in the periphery and impairing insulin release from the beta cell of pancreas.<sup>[5]</sup> Osteocalcin reduction induced by glucocorticoids may be involved in the impairment of function of pancreatic beta cell.<sup>[6]</sup>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 243585,
"questionText": "Which of these mechanisms worsen glycemic control in patients with type 2 diabetes who are administered glucocorticoids?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 777545,
"choiceText": "Impaired renal function",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777547,
"choiceText": "Clinical syndrome of adrenal insufficiency",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777549,
"choiceText": "Diarrhea",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 777551,
"choiceText": "Liver impairment",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Mifepristone is a glucocorticoid and progesterone receptor antagonist. Although it is approved for management of hyperglycemia associated with Cushing syndrome, patients must be carefully monitored for worsening of hypertension and hypokalemia. This has to do with mineralocorticoid receptor's exposure to higher circulating concentrations of plasma cortisol. This results in a clinical situation that mimics a mineralocorticoid excess state, worsening hypertension and hypokalemia. Furthermore, it also increases the risk for clinical syndrome of adrenal insufficiency.<sup>[7]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 243587,
"questionText": "Which is a potential risk factor in patients with Cushing syndrome and diabetes mellitus?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
753945 | /viewarticle/753945 | [
{
"authors": "Payman Vahedi, MD; Zahra Mohajernezhad, MD; Mohammad Faraji-Rad, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 16-year-old girl presents to the emergency department with an acute-onset severe headache as well as nausea, vomiting, and intermittent diplopia. She feels dizzy while walking and cannot walk independently. She also complains of blurred vision. This is her first physician's visit for the headaches, which have been episodic during the past 2 weeks. The headaches involve her entire head. They are not throbbing, are not associated with an aura, and do not occur at a certain time of the day. The severity increases while coughing or straining. She has photophobia and photophobia during these episodes. The headaches previously responded to over-the-counter analgesics, but now she has intolerable pain unrelieved by medications.",
"She has no significant medical history except for minor head trauma while cycling 1 month ago. Her only medication is an oral contraceptive that she has taken for 2 years. She does not use illicit drugs. The family history is positive for atypical migraine headaches; her mother has been treated with medications for this condition for years."
],
"date": "March 25, 2022",
"figures": [],
"markdown": "# Seizure After Sudden Headache in a 16-Year-Old Cyclist\n\n **Authors:** Payman Vahedi, MD; Zahra Mohajernezhad, MD; Mohammad Faraji-Rad, MD \n **Date:** March 25, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 16-year-old girl presents to the emergency department with an acute-onset severe headache as well as nausea, vomiting, and intermittent diplopia. She feels dizzy while walking and cannot walk independently. She also complains of blurred vision. This is her first physician's visit for the headaches, which have been episodic during the past 2 weeks. The headaches involve her entire head. They are not throbbing, are not associated with an aura, and do not occur at a certain time of the day. The severity increases while coughing or straining. She has photophobia and photophobia during these episodes. The headaches previously responded to over-the-counter analgesics, but now she has intolerable pain unrelieved by medications.\nShe has no significant medical history except for minor head trauma while cycling 1 month ago. Her only medication is an oral contraceptive that she has taken for 2 years. She does not use illicit drugs. The family history is positive for atypical migraine headaches; her mother has been treated with medications for this condition for years.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Seizure After Sudden Headache in a 16-Year-Old Cyclist"
},
{
"authors": "Payman Vahedi, MD; Zahra Mohajernezhad, MD; Mohammad Faraji-Rad, MD",
"content": [
"Upon physical examination, the patient is a normal-appearing teenager, but she is agitated due to her headache. She has a regular heart rate of 65 beats/min, her blood pressure is 165/95 mm Hg, and her oral temperature is normal at 98.6°F (37°C). The general physical examination reveals no abnormalities in the head, neck, chest, abdomen, or extremities.",
"A thorough neurologic examination is performed, which reveals decreased visual acuity in each eye to 6/10 (or about 20/30 US Standard). Ophthalmoscopy reveals papilledema, venous engorgement, and a diminished venous pulse. Bilateral sixth cranial nerve palsy is evident. Other neurologic examinations, including sensory and motor examinations, deep tendon reflexes, and cerebellar tests, are all within normal range.",
"During the initial assessment of the patient in the emergency department, she develops a generalized tonic-clonic seizure, which is immediately controlled with intravenous diazepam. Her blood pressure rises to 175/100 mm Hg, and her heart rate is 60 beats/min after the convulsion. A repeat neurologic examination reveals bilateral extensor plantar reflexes and midsized pupils with slight reaction to light. After initiating a loading dose of intravenous phenytoin, an urgent CT scan of the head is performed (Figure 1).",
"Figure 1."
],
"date": "March 25, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/733/328/733328-thumb1.jpg"
}
],
"markdown": "# Seizure After Sudden Headache in a 16-Year-Old Cyclist\n\n **Authors:** Payman Vahedi, MD; Zahra Mohajernezhad, MD; Mohammad Faraji-Rad, MD \n **Date:** March 25, 2022\n\n ## Content\n\n Upon physical examination, the patient is a normal-appearing teenager, but she is agitated due to her headache. She has a regular heart rate of 65 beats/min, her blood pressure is 165/95 mm Hg, and her oral temperature is normal at 98.6°F (37°C). The general physical examination reveals no abnormalities in the head, neck, chest, abdomen, or extremities.\nA thorough neurologic examination is performed, which reveals decreased visual acuity in each eye to 6/10 (or about 20/30 US Standard). Ophthalmoscopy reveals papilledema, venous engorgement, and a diminished venous pulse. Bilateral sixth cranial nerve palsy is evident. Other neurologic examinations, including sensory and motor examinations, deep tendon reflexes, and cerebellar tests, are all within normal range.\nDuring the initial assessment of the patient in the emergency department, she develops a generalized tonic-clonic seizure, which is immediately controlled with intravenous diazepam. Her blood pressure rises to 175/100 mm Hg, and her heart rate is 60 beats/min after the convulsion. A repeat neurologic examination reveals bilateral extensor plantar reflexes and midsized pupils with slight reaction to light. After initiating a loading dose of intravenous phenytoin, an urgent CT scan of the head is performed (Figure 1).\nFigure 1.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1184000,
"choiceText": "Brain tumor",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184002,
"choiceText": "Brain abscess",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184004,
"choiceText": "Acute intraparenchymal bleed",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184006,
"choiceText": "Colloid cyst",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184008,
"choiceText": "No acute abnormality",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 376437,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Seizure After Sudden Headache in a 16-Year-Old Cyclist"
},
{
"authors": "Payman Vahedi, MD; Zahra Mohajernezhad, MD; Mohammad Faraji-Rad, MD",
"content": [
"The new onset of headache with nausea, vomiting, blurred vision, and diplopia were strongly suggestive of increased intracranial pressure in this patient. The presence of bilateral sixth nerve palsy and bilateral papilledema on neurologic examination confirmed this suspicion. Laboratory tests revealed normal electrolytes, renal function, and complete blood cell count findings. The CT scan of the brain revealed acute lateral ventricular hydrocephalus, with periventricular edema and a hyperdense round mass within the third ventricle causing obstruction of the foramen of Monro. The most likely diagnosis was colloid cyst of the third ventricle.",
"Colloid cysts of the third ventricle account for 10%-15% of intraventricular tumors. They are the most common masses of the third ventricle found in adults. Controversy exists over whether these cysts can be classified as brain neoplasms. The cysts are considered to be congenital in origin, and familial occurrence of the disease has been reported[1,2]; however, no specific gene has been identified. Autosomal dominant inheritance is the proposed mechanism in such cases.[2] Some believe that the cysts originate from the neuroepithelium, but other sources, such as endoderm or ectopic respiratory tissue, have also been hypothesized. The cysts are thin-walled benign masses with a gelatinous content.[3] They are located in the anterior third ventricular area and are connected to the rostral aspect of its roof, projecting inferiorly close to the foramina of Monro.",
"The inner epithelium with simple cuboidal and columnar cells secretes a mucinous content, which accumulates under pressure. Most cysts are asymptomatic and rarely are a cause of headache. In symptomatic cysts, headache is the most common presentation. Persistent or intermittent obstruction of the foramina of Monro is believed to be the cause of headache.[4] Symptomatic cysts typically present in mid-adulthood with headache, signs of increased intracranial pressure, and acute lateral ventricular hydrocephalus, although atypical presentations (eg hemorrhagic cysts) have been described during childhood as well.[3]",
"Other symptoms may include altered mental status, nausea and vomiting, seizure, vertigo, and sudden attacks of leg weakness.[2] The latter might be rarely associated with other brain tumors and may be due to stretching of corticospinal nerve fibers to the legs after acute hydrocephalus. Cortical blindness due to bilateral occipital lobe infarction from posterior cerebral artery compression has been reported. The most severe presentation is sudden death. The cause of this rare phenomenon is debatable, but it may be secondary to reflex cardiac effects due to the cyst compressing of the hypothalamus.[2] Acute blockage of cerebrospinal fluid with instant herniation or decompensation in chronic hydrocephalus has also been postulated.[5]",
"The differential diagnosis of colloid cyst includes a wide range of tumors of the anterior third ventricle. These lesions usually originate outside the third ventricle and deform the ventricle by encroachment of the surrounding parenchyma; however, intraventricular tumors may also be the source of cerebrospinal fluid pathway blockage. Choroid plexus papillomas usually present during the first 2 decades of life. Although 10%-30% are found within the third ventricle, mobile tumors may slip from lateral ventricles into the foramina of Monro and become trapped in the third ventricle, thereby causing hydrocephalus.[6] Neurocytomas are intraventricular tumors that are seen in young adults and may be found in the lateral and third ventricular regions. These tumors are frequently misdiagnosed as oligodendroglioma or ependymoma under light microscopy, and the true incidence of this condition may be more than expected."
],
"date": "March 25, 2022",
"figures": [],
"markdown": "# Seizure After Sudden Headache in a 16-Year-Old Cyclist\n\n **Authors:** Payman Vahedi, MD; Zahra Mohajernezhad, MD; Mohammad Faraji-Rad, MD \n **Date:** March 25, 2022\n\n ## Content\n\n The new onset of headache with nausea, vomiting, blurred vision, and diplopia were strongly suggestive of increased intracranial pressure in this patient. The presence of bilateral sixth nerve palsy and bilateral papilledema on neurologic examination confirmed this suspicion. Laboratory tests revealed normal electrolytes, renal function, and complete blood cell count findings. The CT scan of the brain revealed acute lateral ventricular hydrocephalus, with periventricular edema and a hyperdense round mass within the third ventricle causing obstruction of the foramen of Monro. The most likely diagnosis was colloid cyst of the third ventricle.\nColloid cysts of the third ventricle account for 10%-15% of intraventricular tumors. They are the most common masses of the third ventricle found in adults. Controversy exists over whether these cysts can be classified as brain neoplasms. The cysts are considered to be congenital in origin, and familial occurrence of the disease has been reported[1,2]; however, no specific gene has been identified. Autosomal dominant inheritance is the proposed mechanism in such cases.[2] Some believe that the cysts originate from the neuroepithelium, but other sources, such as endoderm or ectopic respiratory tissue, have also been hypothesized. The cysts are thin-walled benign masses with a gelatinous content.[3] They are located in the anterior third ventricular area and are connected to the rostral aspect of its roof, projecting inferiorly close to the foramina of Monro.\nThe inner epithelium with simple cuboidal and columnar cells secretes a mucinous content, which accumulates under pressure. Most cysts are asymptomatic and rarely are a cause of headache. In symptomatic cysts, headache is the most common presentation. Persistent or intermittent obstruction of the foramina of Monro is believed to be the cause of headache.[4] Symptomatic cysts typically present in mid-adulthood with headache, signs of increased intracranial pressure, and acute lateral ventricular hydrocephalus, although atypical presentations (eg hemorrhagic cysts) have been described during childhood as well.[3]\nOther symptoms may include altered mental status, nausea and vomiting, seizure, vertigo, and sudden attacks of leg weakness.[2] The latter might be rarely associated with other brain tumors and may be due to stretching of corticospinal nerve fibers to the legs after acute hydrocephalus. Cortical blindness due to bilateral occipital lobe infarction from posterior cerebral artery compression has been reported. The most severe presentation is sudden death. The cause of this rare phenomenon is debatable, but it may be secondary to reflex cardiac effects due to the cyst compressing of the hypothalamus.[2] Acute blockage of cerebrospinal fluid with instant herniation or decompensation in chronic hydrocephalus has also been postulated.[5]\nThe differential diagnosis of colloid cyst includes a wide range of tumors of the anterior third ventricle. These lesions usually originate outside the third ventricle and deform the ventricle by encroachment of the surrounding parenchyma; however, intraventricular tumors may also be the source of cerebrospinal fluid pathway blockage. Choroid plexus papillomas usually present during the first 2 decades of life. Although 10%-30% are found within the third ventricle, mobile tumors may slip from lateral ventricles into the foramina of Monro and become trapped in the third ventricle, thereby causing hydrocephalus.[6] Neurocytomas are intraventricular tumors that are seen in young adults and may be found in the lateral and third ventricular regions. These tumors are frequently misdiagnosed as oligodendroglioma or ependymoma under light microscopy, and the true incidence of this condition may be more than expected.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1184000,
"choiceText": "Brain tumor",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184002,
"choiceText": "Brain abscess",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184004,
"choiceText": "Acute intraparenchymal bleed",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184006,
"choiceText": "Colloid cyst",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184008,
"choiceText": "No acute abnormality",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 376437,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Seizure After Sudden Headache in a 16-Year-Old Cyclist"
},
{
"authors": "Payman Vahedi, MD; Zahra Mohajernezhad, MD; Mohammad Faraji-Rad, MD",
"content": [
"Intraventricular meningiomas account for 15%-17% of meningiomas in pediatric patients, but only 1.6% of meningiomas in adults.[6] Only 50 reported cases of third ventricle meningioma exist in the literature, and most lesions are found within lateral ventricles.[6] They commonly present as basal tumors with extension up into the floor of the third ventricle.",
"Most other lesions encroach on the third ventricle from the surrounding parenchyma. These are mostly glial tumors, including juvenile pilocytic astrocytoma, fibrillary astrocytoma, protoplasmic astrocytoma, subependymal giant cell astrocytoma, glioblastoma multiforme, and ependymoma. Metastatic neoplasms may involve the third ventricle via its roof, floor, lateral wall, or choroid plexus. Metastases from the lungs, colon, kidneys, and breasts are most common. In these cases, the prognosis is poor, and death is often due to progressive systemic disease. Suprasellar germinomas and craniopharyngiomas can invade the floor of the third ventricle from below. Suprasellar extension of pituitary macroadenomas may also involve the third ventricle. Decreased visual acuity or visual field, endocrinopathy, and headache are the main symptoms in these cases.",
"Other cystic lesions in the anterior third ventricular area include epidermoid cyst, dermoid cyst, and neurocysticercosis. Epidermoid and dermoid cysts are rarely found in the third ventricle, and neurocysticercosis is endemic to Mexico, Eastern Europe, Asia, Central and South America, and Africa. Fenestration into the third ventricle has occurred in 15%-25% of cases with ensuing hydrocephalus.[7] Inflammatory lesions, such as pyogenic abscesses, and granulomatous diseases, such as tuberculosis or fungal infection, may rarely impinge on the third ventricle. Other lesions, such as sarcoidosis and histiocytosis, may involve the third ventricle via its floor and hypothalamus. Finally, vascular lesions, such as cavernous malformations and arteriovenous malformations, should be added to the differential diagnosis of third ventricular mass lesions.",
"The contents of the colloid cyst determine its appearance on imaging studies. The cyst may be found incidentally on CT scanning or when the patient presents with symptoms and signs of increased intracerebral pressure suggestive of acute obstructive hydrocephalus. It is generally a round homogeneous hyperdense mass within the third ventricle at the level of the foramina of Monro.[5] Acute lateral hydrocephalus with periventricular edema might be seen due to the blockage of the cerebrospinal fluid pathway into the third ventricle. On T2-weighted MRI, the cyst might be either hypo- or hyperintense, and fluid-attenuated inversion recovery (FLAIR) shows periventricular edema in the acute stage of hydrocephalus as hyperintensity surrounding the lateral ventricle."
],
"date": "March 25, 2022",
"figures": [],
"markdown": "# Seizure After Sudden Headache in a 16-Year-Old Cyclist\n\n **Authors:** Payman Vahedi, MD; Zahra Mohajernezhad, MD; Mohammad Faraji-Rad, MD \n **Date:** March 25, 2022\n\n ## Content\n\n Intraventricular meningiomas account for 15%-17% of meningiomas in pediatric patients, but only 1.6% of meningiomas in adults.[6] Only 50 reported cases of third ventricle meningioma exist in the literature, and most lesions are found within lateral ventricles.[6] They commonly present as basal tumors with extension up into the floor of the third ventricle.\nMost other lesions encroach on the third ventricle from the surrounding parenchyma. These are mostly glial tumors, including juvenile pilocytic astrocytoma, fibrillary astrocytoma, protoplasmic astrocytoma, subependymal giant cell astrocytoma, glioblastoma multiforme, and ependymoma. Metastatic neoplasms may involve the third ventricle via its roof, floor, lateral wall, or choroid plexus. Metastases from the lungs, colon, kidneys, and breasts are most common. In these cases, the prognosis is poor, and death is often due to progressive systemic disease. Suprasellar germinomas and craniopharyngiomas can invade the floor of the third ventricle from below. Suprasellar extension of pituitary macroadenomas may also involve the third ventricle. Decreased visual acuity or visual field, endocrinopathy, and headache are the main symptoms in these cases.\nOther cystic lesions in the anterior third ventricular area include epidermoid cyst, dermoid cyst, and neurocysticercosis. Epidermoid and dermoid cysts are rarely found in the third ventricle, and neurocysticercosis is endemic to Mexico, Eastern Europe, Asia, Central and South America, and Africa. Fenestration into the third ventricle has occurred in 15%-25% of cases with ensuing hydrocephalus.[7] Inflammatory lesions, such as pyogenic abscesses, and granulomatous diseases, such as tuberculosis or fungal infection, may rarely impinge on the third ventricle. Other lesions, such as sarcoidosis and histiocytosis, may involve the third ventricle via its floor and hypothalamus. Finally, vascular lesions, such as cavernous malformations and arteriovenous malformations, should be added to the differential diagnosis of third ventricular mass lesions.\nThe contents of the colloid cyst determine its appearance on imaging studies. The cyst may be found incidentally on CT scanning or when the patient presents with symptoms and signs of increased intracerebral pressure suggestive of acute obstructive hydrocephalus. It is generally a round homogeneous hyperdense mass within the third ventricle at the level of the foramina of Monro.[5] Acute lateral hydrocephalus with periventricular edema might be seen due to the blockage of the cerebrospinal fluid pathway into the third ventricle. On T2-weighted MRI, the cyst might be either hypo- or hyperintense, and fluid-attenuated inversion recovery (FLAIR) shows periventricular edema in the acute stage of hydrocephalus as hyperintensity surrounding the lateral ventricle.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Seizure After Sudden Headache in a 16-Year-Old Cyclist"
},
{
"authors": "Payman Vahedi, MD; Zahra Mohajernezhad, MD; Mohammad Faraji-Rad, MD",
"content": [
"Surgical intervention is indicated after considering certain factors, such as the patient's age, symptoms, and cyst size. Because of the threat of sudden death, surgery is recommended for cysts exceeding 1.5 cm in diameter in young patients, even in asymptomatic cases.[8] Symptomatic patients should always receive treatment.[9] Options for treatment include endoscopic removal of the cyst[10] and open surgery with different approaches, such as transcortical or interhemispheric transcallosal approaches.[4,9]",
"A study by Denby et al concluded that patients who have removal of a colloid cyst frequently experience atrophy of the mammillary bodies, and attribute this partially to a loss of temporal lobe projections in the fornix. The authors suggest that mammillary body atrophy is correlated with day-to-day memory loss experienced by patients following treatment for a colloid cyst. Denby et al used stereologic volume-estimation techniques to measure the atrophy of the mammillary bodies in 38 patients after surgical removal of colloid cysts and 20 control subjects.[11]",
"In this case, MRI revealed a round mass with high signal intensity on T1-weighted imaging, low signal intensity on T2-weighted imaging, and high signal intensity on FLAIR images. The patient was taken to the operating room. Bilateral external ventricular drainage was inserted in the frontal horns of the lateral ventricles. Bilateral drainage was performed because unilateral ventricular drainage may fail to reduce intracranial pressure when a third ventricular mass simultaneously obstructs both foramina of Monro. Unilateral drainage may also result in selective enlargement (or \"trapping\") of the contralateral lateral ventricle.",
"The tumor was totally resected via an interhemispheric transcallosal approach under a surgical microscope. The macroscopic appearance of the tumor was a creamy soft cyst suggestive of colloid cyst. Histopathology revealed a fibrous wall lined by inner ciliated columnar epithelium and colloid and cell ghosts, confirming the diagnosis. On the first postoperative day, the patient's diplopia and headache resolved. The patient had an uneventful postoperative course and was discharged from the hospital 6 days after surgery. She was on phenobarbital for 6 months, which was tapered and discontinued after a normal EEG. Gradual improvement in visual acuity was observed, and she regained her full vision 5 months later."
],
"date": "March 25, 2022",
"figures": [],
"markdown": "# Seizure After Sudden Headache in a 16-Year-Old Cyclist\n\n **Authors:** Payman Vahedi, MD; Zahra Mohajernezhad, MD; Mohammad Faraji-Rad, MD \n **Date:** March 25, 2022\n\n ## Content\n\n Surgical intervention is indicated after considering certain factors, such as the patient's age, symptoms, and cyst size. Because of the threat of sudden death, surgery is recommended for cysts exceeding 1.5 cm in diameter in young patients, even in asymptomatic cases.[8] Symptomatic patients should always receive treatment.[9] Options for treatment include endoscopic removal of the cyst[10] and open surgery with different approaches, such as transcortical or interhemispheric transcallosal approaches.[4,9]\nA study by Denby et al concluded that patients who have removal of a colloid cyst frequently experience atrophy of the mammillary bodies, and attribute this partially to a loss of temporal lobe projections in the fornix. The authors suggest that mammillary body atrophy is correlated with day-to-day memory loss experienced by patients following treatment for a colloid cyst. Denby et al used stereologic volume-estimation techniques to measure the atrophy of the mammillary bodies in 38 patients after surgical removal of colloid cysts and 20 control subjects.[11]\nIn this case, MRI revealed a round mass with high signal intensity on T1-weighted imaging, low signal intensity on T2-weighted imaging, and high signal intensity on FLAIR images. The patient was taken to the operating room. Bilateral external ventricular drainage was inserted in the frontal horns of the lateral ventricles. Bilateral drainage was performed because unilateral ventricular drainage may fail to reduce intracranial pressure when a third ventricular mass simultaneously obstructs both foramina of Monro. Unilateral drainage may also result in selective enlargement (or \"trapping\") of the contralateral lateral ventricle.\nThe tumor was totally resected via an interhemispheric transcallosal approach under a surgical microscope. The macroscopic appearance of the tumor was a creamy soft cyst suggestive of colloid cyst. Histopathology revealed a fibrous wall lined by inner ciliated columnar epithelium and colloid and cell ghosts, confirming the diagnosis. On the first postoperative day, the patient's diplopia and headache resolved. The patient had an uneventful postoperative course and was discharged from the hospital 6 days after surgery. She was on phenobarbital for 6 months, which was tapered and discontinued after a normal EEG. Gradual improvement in visual acuity was observed, and she regained her full vision 5 months later.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1184010,
"choiceText": "It is seen in up to 5% of all intraventricular tumors",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184012,
"choiceText": "The pathogenesis is definitely acquired",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184014,
"choiceText": "It is the most common third ventricular mass in adult patients",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184016,
"choiceText": "It is usually symptomatic",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The cyst is seen in 10%-15% of intraventricular tumors, and it is the most common third ventricular mass in adult patients. It is considered congenital in origin, and familial occurrence has been reported. Most cysts are asymptomatic and rarely cause headaches.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 376439,
"questionText": "Which is most accurate about colloid cyst of the third ventricle?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1184018,
"choiceText": "Symptomatic cyst",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184020,
"choiceText": "Cyst causing acute hydrocephalus",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184022,
"choiceText": "Incidental cyst of 2 cm in an asymptomatic young adult",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184024,
"choiceText": "All of the above",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Surgical intervention is indicated after considering certain factors, such as the patient's age, symptoms, and cyst size. Because of the threat of sudden death, surgery is recommended for cysts exceeding 1.5 cm in diameter in young patients, even in asymptomatic patients. Symptomatic patients should always receive treatment.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 376441,
"questionText": "Which is considered an indication for surgical resection of colloid cyst in the third ventricle?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Seizure After Sudden Headache in a 16-Year-Old Cyclist"
},
{
"authors": "Payman Vahedi, MD; Zahra Mohajernezhad, MD; Mohammad Faraji-Rad, MD",
"content": [],
"date": "March 25, 2022",
"figures": [],
"markdown": "# Seizure After Sudden Headache in a 16-Year-Old Cyclist\n\n **Authors:** Payman Vahedi, MD; Zahra Mohajernezhad, MD; Mohammad Faraji-Rad, MD \n **Date:** March 25, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1184010,
"choiceText": "It is seen in up to 5% of all intraventricular tumors",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184012,
"choiceText": "The pathogenesis is definitely acquired",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184014,
"choiceText": "It is the most common third ventricular mass in adult patients",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184016,
"choiceText": "It is usually symptomatic",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The cyst is seen in 10%-15% of intraventricular tumors, and it is the most common third ventricular mass in adult patients. It is considered congenital in origin, and familial occurrence has been reported. Most cysts are asymptomatic and rarely cause headaches.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 376439,
"questionText": "Which is most accurate about colloid cyst of the third ventricle?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1184018,
"choiceText": "Symptomatic cyst",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184020,
"choiceText": "Cyst causing acute hydrocephalus",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184022,
"choiceText": "Incidental cyst of 2 cm in an asymptomatic young adult",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184024,
"choiceText": "All of the above",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Surgical intervention is indicated after considering certain factors, such as the patient's age, symptoms, and cyst size. Because of the threat of sudden death, surgery is recommended for cysts exceeding 1.5 cm in diameter in young patients, even in asymptomatic patients. Symptomatic patients should always receive treatment.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 376441,
"questionText": "Which is considered an indication for surgical resection of colloid cyst in the third ventricle?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Seizure After Sudden Headache in a 16-Year-Old Cyclist"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1184000,
"choiceText": "Brain tumor",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184002,
"choiceText": "Brain abscess",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184004,
"choiceText": "Acute intraparenchymal bleed",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184006,
"choiceText": "Colloid cyst",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184008,
"choiceText": "No acute abnormality",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 376437,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1184010,
"choiceText": "It is seen in up to 5% of all intraventricular tumors",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184012,
"choiceText": "The pathogenesis is definitely acquired",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184014,
"choiceText": "It is the most common third ventricular mass in adult patients",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184016,
"choiceText": "It is usually symptomatic",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The cyst is seen in 10%-15% of intraventricular tumors, and it is the most common third ventricular mass in adult patients. It is considered congenital in origin, and familial occurrence has been reported. Most cysts are asymptomatic and rarely cause headaches.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 376439,
"questionText": "Which is most accurate about colloid cyst of the third ventricle?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1184018,
"choiceText": "Symptomatic cyst",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184020,
"choiceText": "Cyst causing acute hydrocephalus",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184022,
"choiceText": "Incidental cyst of 2 cm in an asymptomatic young adult",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1184024,
"choiceText": "All of the above",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Surgical intervention is indicated after considering certain factors, such as the patient's age, symptoms, and cyst size. Because of the threat of sudden death, surgery is recommended for cysts exceeding 1.5 cm in diameter in young patients, even in asymptomatic patients. Symptomatic patients should always receive treatment.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 376441,
"questionText": "Which is considered an indication for surgical resection of colloid cyst in the third ventricle?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
885563 | /viewarticle/885563 | [
{
"authors": "Abhimanyu Beri, MD; Fadi Abu-Yasin, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 60-year-old man with a history of diabetes mellitus and hypertension presents with a 1-day history of retrosternal chest pain. The chest pain began while he had been resting and continued to worsen over the next few hours. He describes it as a sharp pain that is moderate in intensity, with radiation to his right shoulder and neck. The pain worsens when he is lying down and with deep breathing, but it is relieved by bending forward. He denies having shortness of breath or palpitations.",
"The patient has a medical history of hypertension, diabetes, hypercholesterolemia, and adenocarcinoma of the prostate. In addition, the day before the symptoms occurred, he was diagnosed with costochondritis during a visit to his family doctor.",
"Review of his systems is significant only for a recent respiratory infection that had improved approximately 2 weeks before presentation. His medications include enalapril, hydrochlorothiazide, metformin, and a statin. He has smoked one pack of cigarettes a day for the past 20 years. The patient's family history is significant for premature coronary artery disease in two of his brothers."
],
"date": "March 24, 2022",
"figures": [],
"markdown": "# Cardiology Case Challenge: Worsening Chest Pain After a Respiratory Infection in a Man With Hypertension\n\n **Authors:** Abhimanyu Beri, MD; Fadi Abu-Yasin, MD \n **Date:** March 24, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 60-year-old man with a history of diabetes mellitus and hypertension presents with a 1-day history of retrosternal chest pain. The chest pain began while he had been resting and continued to worsen over the next few hours. He describes it as a sharp pain that is moderate in intensity, with radiation to his right shoulder and neck. The pain worsens when he is lying down and with deep breathing, but it is relieved by bending forward. He denies having shortness of breath or palpitations.\nThe patient has a medical history of hypertension, diabetes, hypercholesterolemia, and adenocarcinoma of the prostate. In addition, the day before the symptoms occurred, he was diagnosed with costochondritis during a visit to his family doctor.\nReview of his systems is significant only for a recent respiratory infection that had improved approximately 2 weeks before presentation. His medications include enalapril, hydrochlorothiazide, metformin, and a statin. He has smoked one pack of cigarettes a day for the past 20 years. The patient's family history is significant for premature coronary artery disease in two of his brothers.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Cardiology Case Challenge: Worsening Chest Pain After a Respiratory Infection in a Man With Hypertension"
},
{
"authors": "Abhimanyu Beri, MD; Fadi Abu-Yasin, MD",
"content": [
"Upon physical examination, the patient's pulse is regular, with a rate of 80 beats/min and good volume. His blood pressure is recorded at 130/80 mm Hg in the right arm and 134/77 mm Hg in the left arm. His oral temperature is 98.6°F (37°C).",
"Examination of the head, ears, eyes, nose, and throat is unremarkable, and no evidence of xanthelasma is noted. Neck examination shows the absence of jugular venous distention. Cardiovascular examination reveals normal S1 and S2 heart sounds, and no murmurs, gallops, or rubs are found. The chest examination shows good respiratory effort, with normal breath sounds and no splinting. The chest is not tender to palpation. The patient's abdomen is nontender and without palpable pulsatile masses. No indication of edema or erythema is seen in the patient's legs. The Homan sign is negative, and no venous cords are noted. The peripheral pulses are strong and symmetrical in all four extremities.",
"The laboratory evaluation shows a normal complete blood cell count and a normal basic metabolic panel. The creatine kinase level is slightly elevated, at 289 U/L (reference range, 0-200 U/L), with a creatine kinase-MB fraction of 3.9 ng/mL (reference range, 0-7.0 ng/mL) and an undetectable troponin I level (< 0.02 ng/mL). ECG is obtained (Figure 1).",
"Figure 1.",
"The initial management includes administration of aspirin, nasal oxygen, sublingual nitroglycerine, and morphine for pain control. Given his cardiac risk factors and presentation, the patient is admitted for observation to rule out an acute coronary syndrome. Serial cardiac enzyme measurements continue to be negative."
],
"date": "March 24, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/885/563/885563-thumb1.jpg"
}
],
"markdown": "# Cardiology Case Challenge: Worsening Chest Pain After a Respiratory Infection in a Man With Hypertension\n\n **Authors:** Abhimanyu Beri, MD; Fadi Abu-Yasin, MD \n **Date:** March 24, 2022\n\n ## Content\n\n Upon physical examination, the patient's pulse is regular, with a rate of 80 beats/min and good volume. His blood pressure is recorded at 130/80 mm Hg in the right arm and 134/77 mm Hg in the left arm. His oral temperature is 98.6°F (37°C).\nExamination of the head, ears, eyes, nose, and throat is unremarkable, and no evidence of xanthelasma is noted. Neck examination shows the absence of jugular venous distention. Cardiovascular examination reveals normal S1 and S2 heart sounds, and no murmurs, gallops, or rubs are found. The chest examination shows good respiratory effort, with normal breath sounds and no splinting. The chest is not tender to palpation. The patient's abdomen is nontender and without palpable pulsatile masses. No indication of edema or erythema is seen in the patient's legs. The Homan sign is negative, and no venous cords are noted. The peripheral pulses are strong and symmetrical in all four extremities.\nThe laboratory evaluation shows a normal complete blood cell count and a normal basic metabolic panel. The creatine kinase level is slightly elevated, at 289 U/L (reference range, 0-200 U/L), with a creatine kinase-MB fraction of 3.9 ng/mL (reference range, 0-7.0 ng/mL) and an undetectable troponin I level (< 0.02 ng/mL). ECG is obtained (Figure 1).\nFigure 1.\nThe initial management includes administration of aspirin, nasal oxygen, sublingual nitroglycerine, and morphine for pain control. Given his cardiac risk factors and presentation, the patient is admitted for observation to rule out an acute coronary syndrome. Serial cardiac enzyme measurements continue to be negative.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136552,
"choiceText": "Acute pericarditis",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136554,
"choiceText": "Acute inferior ST-segment myocardial infarction",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136556,
"choiceText": "Aortic dissection",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136558,
"choiceText": "Pulmonary embolus",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360607,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Cardiology Case Challenge: Worsening Chest Pain After a Respiratory Infection in a Man With Hypertension"
},
{
"authors": "Abhimanyu Beri, MD; Fadi Abu-Yasin, MD",
"content": [
"This patient presented with retrosternal chest pain, which began while he was at rest and radiated to the right shoulder and neck. The pain worsened on deep inspiration and while lying down, but it improved when he bent forward. In addition, a friction rub was detected on repeat examination. The initial ECG showed mild ST-segment elevation in the inferior and anterior leads that became much more pronounced over the following 12 hours, as well as PR-segment elevation in lead aVR. These findings prompted the diagnosis of acute pericarditis.",
"Acute pericarditis may occur as an isolated entity or as the result of systemic disease. The incidence is estimated to be about 5% of emergency department patients with chest pain but without myocardial infarction. Most cases are idiopathic; however, the clinician must also consider infectious, neoplastic, autoimmune, uremic, radiation-induced, postischemic, postvaccine, and traumatic etiologies. Important conditions that may cause chest pain similar to that of pericarditis include myocardial infarction, pulmonary embolism, aortic dissection, pleural effusion, and pneumomediastinum.[1,2,3]",
"The typical history for a patient with acute pericarditis consists of chest pain that is sudden in onset and pleuritic in nature. It is usually more intense when the patient is supine and improves when he or she sits upright and leans forward. The pain often radiates to the neck, upper arm, or shoulder as referred pain from the phrenic nerve's course over the pericardium.",
"The physical examination may reveal a high-pitched scratchy or squeaky friction rub that is best heard at the left sternal border at end expiration when the patient is leaning forward. Because pericardial friction rubs often vary in intensity from minute to minute, patients who have suspected pericarditis should have cardiac auscultation repeated multiple times. The friction rub is classically described as having three components, which correspond to atrial systole, ventricular systole, and rapid ventricular filling during early diastole; however, all phases may not be discernible in all patients. A pericardial friction rub can be distinguished from a pleural rub by the fact that it can be heard even when respirations are suspended.[1,2,3]"
],
"date": "March 24, 2022",
"figures": [],
"markdown": "# Cardiology Case Challenge: Worsening Chest Pain After a Respiratory Infection in a Man With Hypertension\n\n **Authors:** Abhimanyu Beri, MD; Fadi Abu-Yasin, MD \n **Date:** March 24, 2022\n\n ## Content\n\n This patient presented with retrosternal chest pain, which began while he was at rest and radiated to the right shoulder and neck. The pain worsened on deep inspiration and while lying down, but it improved when he bent forward. In addition, a friction rub was detected on repeat examination. The initial ECG showed mild ST-segment elevation in the inferior and anterior leads that became much more pronounced over the following 12 hours, as well as PR-segment elevation in lead aVR. These findings prompted the diagnosis of acute pericarditis.\nAcute pericarditis may occur as an isolated entity or as the result of systemic disease. The incidence is estimated to be about 5% of emergency department patients with chest pain but without myocardial infarction. Most cases are idiopathic; however, the clinician must also consider infectious, neoplastic, autoimmune, uremic, radiation-induced, postischemic, postvaccine, and traumatic etiologies. Important conditions that may cause chest pain similar to that of pericarditis include myocardial infarction, pulmonary embolism, aortic dissection, pleural effusion, and pneumomediastinum.[1,2,3]\nThe typical history for a patient with acute pericarditis consists of chest pain that is sudden in onset and pleuritic in nature. It is usually more intense when the patient is supine and improves when he or she sits upright and leans forward. The pain often radiates to the neck, upper arm, or shoulder as referred pain from the phrenic nerve's course over the pericardium.\nThe physical examination may reveal a high-pitched scratchy or squeaky friction rub that is best heard at the left sternal border at end expiration when the patient is leaning forward. Because pericardial friction rubs often vary in intensity from minute to minute, patients who have suspected pericarditis should have cardiac auscultation repeated multiple times. The friction rub is classically described as having three components, which correspond to atrial systole, ventricular systole, and rapid ventricular filling during early diastole; however, all phases may not be discernible in all patients. A pericardial friction rub can be distinguished from a pleural rub by the fact that it can be heard even when respirations are suspended.[1,2,3]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136552,
"choiceText": "Acute pericarditis",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136554,
"choiceText": "Acute inferior ST-segment myocardial infarction",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136556,
"choiceText": "Aortic dissection",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136558,
"choiceText": "Pulmonary embolus",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360607,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Cardiology Case Challenge: Worsening Chest Pain After a Respiratory Infection in a Man With Hypertension"
},
{
"authors": "Abhimanyu Beri, MD; Fadi Abu-Yasin, MD",
"content": [
"Pericardial effusions are common sequelae of acute pericarditis. The presence of systemic arterial hypotension, tachycardia, elevated jugular venous pressure, and/or pulsus paradoxus (a decrease in systolic arterial pressure of more than 10 mm Hg with inspiration) suggests the development of a pericardial effusion and cardiac tamponade. In cardiac tamponade, the accumulation of pericardial fluid increases the intrapericardial pressure and leads to impaired diastolic cardiac filling, which results in collapse of the right atrium and ventricle during their diastolic periods and diminished cardiac output.",
"Any of the examination findings above that do not have an alternate explanation should prompt immediate echocardiographic evaluation, including pulsed-wave Doppler analysis. A body temperature > 100.4°F (38°C) is uncommon and may indicate purulent pericarditis; this finding should also prompt echocardiography and, possibly, pericardiocentesis.[1]",
"Diagnostic testing in patients with suspected pericarditis should include ECG, chest radiography, and echocardiography. The 12-lead ECG in patients with acute pericarditis classically shows widespread, concave-upward ST-segment elevation associated with PR-segment depression and PR-segment elevation in lead aVR.",
"The ECG abnormalities may evolve through four phases:",
"Stage I: diffuse ST-segment elevation and PR-segment depression",
"Stage II: normalization of the ST and PR segments, with flattening of the T wave",
"Stage III: widespread T-wave inversions",
"Stage IV: normalization of the T waves",
"Prompt institution of therapy may prevent the appearance of all four stages. Nonetheless, the changes in stage I are observed in 60%-80% of patients with pericarditis.",
"ST-segment elevation may occur with many other diseases, most notably myocardial infarction; however, several echocardiographic features may help to distinguish these two entities. In myocardial infarction, the ST-segment elevations are often convex (dome-shaped) rather than concave, and they are often associated with Q-wave formation and the loss of R-wave voltage. PR-segment depression is uncommon, and atrioventricular block or ventricular arrhythmia is usually seen.",
"The most reliable distinguishing feature may be the ratio of ST-segment elevation (in mm) to T-wave amplitude (height in mm) in lead V6. When this ratio exceeds 0.24, acute pericarditis is almost always present.[4]",
"The findings on chest radiography are usually normal, but they may reveal cardiomegaly when there is a large pericardial effusion. Most important, radiography may help to provide diagnostic information regarding the likelihood of other conditions, such as pneumothorax, pneumomediastinum, pneumonia, or aortic dissection.[3]",
"The white blood cell count, erythrocyte sedimentation rate (ESR), and serum C-reactive protein (CRP) concentration are usually all elevated in patients with acute pericarditis; however, they are of little use in determining the etiology of the disease. Antinuclear and rheumatoid factor antibodies are seen in 10%-15% of cases. Viral cultures and antibody titers are not clinically useful. Plasma troponin concentrations are elevated in 35%-50% of patients with pericarditis; this finding is thought to be caused by epicardial inflammation rather than myocyte necrosis, although the long-term risk for troponin elevation in acute pericarditis is not clear. The concentration usually returns to normal within 1-2 weeks after the diagnosis. Serum creatine kinase and MB fractions are less often elevated than is the troponin value.[3]",
"Transthoracic echocardiography is recommended in all patients with suspected pericarditis because the presence of an effusion helps to confirm the diagnosis, and clinical or echocardiographic evidence of tamponade indicates the need for therapeutic pericardiocentesis. Pericardiocentesis is indicated in patients with pericardial tamponade and in those with known or suspected purulent or neoplastic pericarditis. When pericardiocentesis is performed, the fluid should be analyzed for red and white blood cell counts, cytologic evidence of cancer, and triglycerides (which are elevated in patients with chylous effusion). The fluid should be cultured as well as examined microscopically.[3]"
],
"date": "March 24, 2022",
"figures": [],
"markdown": "# Cardiology Case Challenge: Worsening Chest Pain After a Respiratory Infection in a Man With Hypertension\n\n **Authors:** Abhimanyu Beri, MD; Fadi Abu-Yasin, MD \n **Date:** March 24, 2022\n\n ## Content\n\n Pericardial effusions are common sequelae of acute pericarditis. The presence of systemic arterial hypotension, tachycardia, elevated jugular venous pressure, and/or pulsus paradoxus (a decrease in systolic arterial pressure of more than 10 mm Hg with inspiration) suggests the development of a pericardial effusion and cardiac tamponade. In cardiac tamponade, the accumulation of pericardial fluid increases the intrapericardial pressure and leads to impaired diastolic cardiac filling, which results in collapse of the right atrium and ventricle during their diastolic periods and diminished cardiac output.\nAny of the examination findings above that do not have an alternate explanation should prompt immediate echocardiographic evaluation, including pulsed-wave Doppler analysis. A body temperature > 100.4°F (38°C) is uncommon and may indicate purulent pericarditis; this finding should also prompt echocardiography and, possibly, pericardiocentesis.[1]\nDiagnostic testing in patients with suspected pericarditis should include ECG, chest radiography, and echocardiography. The 12-lead ECG in patients with acute pericarditis classically shows widespread, concave-upward ST-segment elevation associated with PR-segment depression and PR-segment elevation in lead aVR.\nThe ECG abnormalities may evolve through four phases:\nStage I: diffuse ST-segment elevation and PR-segment depression\nStage II: normalization of the ST and PR segments, with flattening of the T wave\nStage III: widespread T-wave inversions\nStage IV: normalization of the T waves\nPrompt institution of therapy may prevent the appearance of all four stages. Nonetheless, the changes in stage I are observed in 60%-80% of patients with pericarditis.\nST-segment elevation may occur with many other diseases, most notably myocardial infarction; however, several echocardiographic features may help to distinguish these two entities. In myocardial infarction, the ST-segment elevations are often convex (dome-shaped) rather than concave, and they are often associated with Q-wave formation and the loss of R-wave voltage. PR-segment depression is uncommon, and atrioventricular block or ventricular arrhythmia is usually seen.\nThe most reliable distinguishing feature may be the ratio of ST-segment elevation (in mm) to T-wave amplitude (height in mm) in lead V6. When this ratio exceeds 0.24, acute pericarditis is almost always present.[4]\nThe findings on chest radiography are usually normal, but they may reveal cardiomegaly when there is a large pericardial effusion. Most important, radiography may help to provide diagnostic information regarding the likelihood of other conditions, such as pneumothorax, pneumomediastinum, pneumonia, or aortic dissection.[3]\nThe white blood cell count, erythrocyte sedimentation rate (ESR), and serum C-reactive protein (CRP) concentration are usually all elevated in patients with acute pericarditis; however, they are of little use in determining the etiology of the disease. Antinuclear and rheumatoid factor antibodies are seen in 10%-15% of cases. Viral cultures and antibody titers are not clinically useful. Plasma troponin concentrations are elevated in 35%-50% of patients with pericarditis; this finding is thought to be caused by epicardial inflammation rather than myocyte necrosis, although the long-term risk for troponin elevation in acute pericarditis is not clear. The concentration usually returns to normal within 1-2 weeks after the diagnosis. Serum creatine kinase and MB fractions are less often elevated than is the troponin value.[3]\nTransthoracic echocardiography is recommended in all patients with suspected pericarditis because the presence of an effusion helps to confirm the diagnosis, and clinical or echocardiographic evidence of tamponade indicates the need for therapeutic pericardiocentesis. Pericardiocentesis is indicated in patients with pericardial tamponade and in those with known or suspected purulent or neoplastic pericarditis. When pericardiocentesis is performed, the fluid should be analyzed for red and white blood cell counts, cytologic evidence of cancer, and triglycerides (which are elevated in patients with chylous effusion). The fluid should be cultured as well as examined microscopically.[3]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Cardiology Case Challenge: Worsening Chest Pain After a Respiratory Infection in a Man With Hypertension"
},
{
"authors": "Abhimanyu Beri, MD; Fadi Abu-Yasin, MD",
"content": [
"The treatment of acute pericarditis not complicated by cardiac tamponade depends on whether a primary cause is identified or highly suspected. Therapy for patients with idiopathic pericarditis is aimed at the relief of chest pain and inflammation. Treatment has not been shown to prevent tamponade or long-term complications, such as constrictive pericarditis or recurrent pericarditis.",
"Although nonsteroidal anti-inflammatory drugs are the traditional mainstay of therapy, data suggest that colchicine, administered at a dosage of 0.6 mg twice daily for 90 days, is more likely to prevent recurrent idiopathic pericarditis. However, aspirin (2-4 g/day), indomethacin (75-225 mg/day), or ibuprofen (1600-3200 mg/day) are still often prescribed. Colchicine is also preferred for patients who have recurrent pericarditis.",
"Typically, symptoms improve within days of initiation of anti-inflammatory therapy. If chest pain persists after 2 weeks of treatment, a different agent or combination therapy should be considered.",
"If a patient continues to have chest pain despite combination therapy, glucocorticoids should be considered. Some data suggest that the use of steroids is associated with a higher risk for later recurrence. Patients with a relapse of pericarditis after a short-term course of low-dose glucocorticoid therapy often obtain symptomatic relief when higher-dose prednisone therapy (1-1.5 mg/kg of body weight daily) is administered for 4 weeks.[2,3,5]",
"Therapy for secondary pericarditis is targeted at the primary cause. In cases of HIV-associated pericarditis, appropriate antibiotics or antivirals for targeting the infection should be used. For patients with autoimmune conditions, steroids or other immunomodulators are usually appropriate in consultation with the primary care clinician.",
"A diagnosis of acute pericarditis should be reserved for patients with an audible pericardial friction rub or chest pain with typical ECG findings, most notably widespread ST-segment elevation. Indicators of a poor prognosis include a temperature > 100.4°F (38°C), a subacute onset (ie, symptoms developing over several weeks), an immunosuppressed state, pericarditis associated with trauma, a history of oral anticoagulation therapy, myopericarditis (pericarditis with clinical or serologic evidence of myocardial involvement), a large pericardial effusion (an echo-free space > 20 mm in width) or cardiac tamponade.[2]",
"The patient in this case had multiple coronary artery disease risk factors but presented with a history that is typical of acute pericarditis. Although the initial physical examination was normal, reexamination several hours later revealed the presence of a friction rub. His initial ECG was ambiguous; however, the next morning, a repeat ECG showed more pronounced changes (Figure 2).",
"Figure 2.",
"His creatine kinase level gradually came down, and his troponin remained normal. Given these findings, a two-dimensional echocardiogram was ordered and his ESR and CRP were checked, both of which had normal results. His rheumatoid factor and antinuclear antibody examinations were normal as well.",
"The patient was started on colchicine at 2 mg on day 1, which was then reduced to 0.5 mg twice daily for 90 days. His symptoms resolved within 24 hours. He was discharged from the hospital. On an outpatient cardiac stress test, no evidence of ischemia was noted."
],
"date": "March 24, 2022",
"figures": [
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/885/563/885563-thumb2.jpg"
}
],
"markdown": "# Cardiology Case Challenge: Worsening Chest Pain After a Respiratory Infection in a Man With Hypertension\n\n **Authors:** Abhimanyu Beri, MD; Fadi Abu-Yasin, MD \n **Date:** March 24, 2022\n\n ## Content\n\n The treatment of acute pericarditis not complicated by cardiac tamponade depends on whether a primary cause is identified or highly suspected. Therapy for patients with idiopathic pericarditis is aimed at the relief of chest pain and inflammation. Treatment has not been shown to prevent tamponade or long-term complications, such as constrictive pericarditis or recurrent pericarditis.\nAlthough nonsteroidal anti-inflammatory drugs are the traditional mainstay of therapy, data suggest that colchicine, administered at a dosage of 0.6 mg twice daily for 90 days, is more likely to prevent recurrent idiopathic pericarditis. However, aspirin (2-4 g/day), indomethacin (75-225 mg/day), or ibuprofen (1600-3200 mg/day) are still often prescribed. Colchicine is also preferred for patients who have recurrent pericarditis.\nTypically, symptoms improve within days of initiation of anti-inflammatory therapy. If chest pain persists after 2 weeks of treatment, a different agent or combination therapy should be considered.\nIf a patient continues to have chest pain despite combination therapy, glucocorticoids should be considered. Some data suggest that the use of steroids is associated with a higher risk for later recurrence. Patients with a relapse of pericarditis after a short-term course of low-dose glucocorticoid therapy often obtain symptomatic relief when higher-dose prednisone therapy (1-1.5 mg/kg of body weight daily) is administered for 4 weeks.[2,3,5]\nTherapy for secondary pericarditis is targeted at the primary cause. In cases of HIV-associated pericarditis, appropriate antibiotics or antivirals for targeting the infection should be used. For patients with autoimmune conditions, steroids or other immunomodulators are usually appropriate in consultation with the primary care clinician.\nA diagnosis of acute pericarditis should be reserved for patients with an audible pericardial friction rub or chest pain with typical ECG findings, most notably widespread ST-segment elevation. Indicators of a poor prognosis include a temperature > 100.4°F (38°C), a subacute onset (ie, symptoms developing over several weeks), an immunosuppressed state, pericarditis associated with trauma, a history of oral anticoagulation therapy, myopericarditis (pericarditis with clinical or serologic evidence of myocardial involvement), a large pericardial effusion (an echo-free space > 20 mm in width) or cardiac tamponade.[2]\nThe patient in this case had multiple coronary artery disease risk factors but presented with a history that is typical of acute pericarditis. Although the initial physical examination was normal, reexamination several hours later revealed the presence of a friction rub. His initial ECG was ambiguous; however, the next morning, a repeat ECG showed more pronounced changes (Figure 2).\nFigure 2.\nHis creatine kinase level gradually came down, and his troponin remained normal. Given these findings, a two-dimensional echocardiogram was ordered and his ESR and CRP were checked, both of which had normal results. His rheumatoid factor and antinuclear antibody examinations were normal as well.\nThe patient was started on colchicine at 2 mg on day 1, which was then reduced to 0.5 mg twice daily for 90 days. His symptoms resolved within 24 hours. He was discharged from the hospital. On an outpatient cardiac stress test, no evidence of ischemia was noted.\n\n ## Figures\n\n **Figure 2.** \n \n\n\n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136560,
"choiceText": "Evolution of the Q waves",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136562,
"choiceText": "Diffuse ST-segment depression",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136564,
"choiceText": "PR depression in lead aVR",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136566,
"choiceText": "PR elevation in lead aVR",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136568,
"choiceText": "T-wave inversion after segment normalization",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The 12-lead ECG in patients with acute pericarditis classically shows widespread, concave-upward ST-segment elevation associated with PR-segment depression and PR-segment elevation in lead aVR. The ECG abnormalities may evolve through four phases:<br>\r\n\r\n<ul>\r\n <li>Stage I: diffuse ST-segment elevation and PR-segment depression</li>\r\n\r\n <li>Stage II: normalization of the ST and PR segments, with flattening of the T wave</li>\r\n\r\n <li>Stage III: widespread T-wave inversions</li>\r\n\r\n <li>Stage IV: normalization of the T waves</li>\r\n</ul>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360609,
"questionText": "Which of the following ECG abnormalities is more likely to be associated with acute pericarditis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136570,
"choiceText": "Neoplasm",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136572,
"choiceText": "Uremia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136574,
"choiceText": "Viral/idiopathic etiology",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136576,
"choiceText": "Radiation exposure",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1139010,
"choiceText": "Complication of myocardial infarction",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Most cases are idiopathic in origin; however, the clinician must also consider infectious, neoplastic, autoimmune, uremic, radiation-induced, postischemic, postvaccine, and traumatic etiologies.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360611,
"questionText": "Which is the most common cause of acute pericarditis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Cardiology Case Challenge: Worsening Chest Pain After a Respiratory Infection in a Man With Hypertension"
},
{
"authors": "Abhimanyu Beri, MD; Fadi Abu-Yasin, MD",
"content": [],
"date": "March 24, 2022",
"figures": [],
"markdown": "# Cardiology Case Challenge: Worsening Chest Pain After a Respiratory Infection in a Man With Hypertension\n\n **Authors:** Abhimanyu Beri, MD; Fadi Abu-Yasin, MD \n **Date:** March 24, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136560,
"choiceText": "Evolution of the Q waves",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136562,
"choiceText": "Diffuse ST-segment depression",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136564,
"choiceText": "PR depression in lead aVR",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136566,
"choiceText": "PR elevation in lead aVR",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136568,
"choiceText": "T-wave inversion after segment normalization",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The 12-lead ECG in patients with acute pericarditis classically shows widespread, concave-upward ST-segment elevation associated with PR-segment depression and PR-segment elevation in lead aVR. The ECG abnormalities may evolve through four phases:<br>\r\n\r\n<ul>\r\n <li>Stage I: diffuse ST-segment elevation and PR-segment depression</li>\r\n\r\n <li>Stage II: normalization of the ST and PR segments, with flattening of the T wave</li>\r\n\r\n <li>Stage III: widespread T-wave inversions</li>\r\n\r\n <li>Stage IV: normalization of the T waves</li>\r\n</ul>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360609,
"questionText": "Which of the following ECG abnormalities is more likely to be associated with acute pericarditis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136570,
"choiceText": "Neoplasm",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136572,
"choiceText": "Uremia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136574,
"choiceText": "Viral/idiopathic etiology",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136576,
"choiceText": "Radiation exposure",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1139010,
"choiceText": "Complication of myocardial infarction",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Most cases are idiopathic in origin; however, the clinician must also consider infectious, neoplastic, autoimmune, uremic, radiation-induced, postischemic, postvaccine, and traumatic etiologies.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360611,
"questionText": "Which is the most common cause of acute pericarditis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Cardiology Case Challenge: Worsening Chest Pain After a Respiratory Infection in a Man With Hypertension"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136552,
"choiceText": "Acute pericarditis",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136554,
"choiceText": "Acute inferior ST-segment myocardial infarction",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136556,
"choiceText": "Aortic dissection",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136558,
"choiceText": "Pulmonary embolus",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360607,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136560,
"choiceText": "Evolution of the Q waves",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136562,
"choiceText": "Diffuse ST-segment depression",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136564,
"choiceText": "PR depression in lead aVR",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136566,
"choiceText": "PR elevation in lead aVR",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136568,
"choiceText": "T-wave inversion after segment normalization",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The 12-lead ECG in patients with acute pericarditis classically shows widespread, concave-upward ST-segment elevation associated with PR-segment depression and PR-segment elevation in lead aVR. The ECG abnormalities may evolve through four phases:<br>\r\n\r\n<ul>\r\n <li>Stage I: diffuse ST-segment elevation and PR-segment depression</li>\r\n\r\n <li>Stage II: normalization of the ST and PR segments, with flattening of the T wave</li>\r\n\r\n <li>Stage III: widespread T-wave inversions</li>\r\n\r\n <li>Stage IV: normalization of the T waves</li>\r\n</ul>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360609,
"questionText": "Which of the following ECG abnormalities is more likely to be associated with acute pericarditis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1136570,
"choiceText": "Neoplasm",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136572,
"choiceText": "Uremia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136574,
"choiceText": "Viral/idiopathic etiology",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1136576,
"choiceText": "Radiation exposure",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1139010,
"choiceText": "Complication of myocardial infarction",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Most cases are idiopathic in origin; however, the clinician must also consider infectious, neoplastic, autoimmune, uremic, radiation-induced, postischemic, postvaccine, and traumatic etiologies.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 360611,
"questionText": "Which is the most common cause of acute pericarditis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
970288 | /viewarticle/970288 | [
{
"authors": "Avan Armaghani, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 53-year-old postmenopausal woman has had worsening low back pain for the past 2 months. The pain is in the mid to lower back region and does not radiate. She describes it as a constant dull ache that worsens when she stands for long periods. Over-the-counter analgesics initially relieved the pain; however, over the past 2 months, these medications have become ineffective in alleviating her symptoms.",
"She has no loss of bladder or bowel function, and she reports no numbness or tingling sensation in her legs. She is able to ambulate without difficulty, but she experiences the back pain when she walks. The patient has never had back pain before. She has not sustained any recent injury. She does not recall experiencing fever, chills, dizziness, changes in vision, nausea, vomiting, diarrhea, constipation, or chest pain. She has an occasional dry cough that has been ongoing for about 6 months. The cough does not produce any sputum or blood.",
"The patient's past medical history is significant for hypertension, for which she takes a beta-blocker once daily. She also has hyperlipidemia, for which she takes a statin once daily.",
"The patient had a mammogram 2 years earlier, which did not reveal any abnormalities. Her most recent Pap test was 2 years ago, and the results were normal. She has never had a colonoscopy.",
"The patient is a current smoker; she has smoked one pack per day for the past 31 years. She drinks one glass of wine a week and does not use any illicit drugs. She currently works full-time as a server at a local restaurant.",
"Her family history is significant for the death of her father from lung cancer at the age of 62 years. Her mother was diagnosed with colon cancer at the age of 52 years; she received treatment and is still living. The patient has a younger sister, aged 50 years, who is healthy."
],
"date": "March 22, 2022",
"figures": [],
"markdown": "# A 53-Year-Old Waitress With a Cough and Constant Back Pain\n\n **Authors:** Avan Armaghani, MD \n **Date:** March 22, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 53-year-old postmenopausal woman has had worsening low back pain for the past 2 months. The pain is in the mid to lower back region and does not radiate. She describes it as a constant dull ache that worsens when she stands for long periods. Over-the-counter analgesics initially relieved the pain; however, over the past 2 months, these medications have become ineffective in alleviating her symptoms.\nShe has no loss of bladder or bowel function, and she reports no numbness or tingling sensation in her legs. She is able to ambulate without difficulty, but she experiences the back pain when she walks. The patient has never had back pain before. She has not sustained any recent injury. She does not recall experiencing fever, chills, dizziness, changes in vision, nausea, vomiting, diarrhea, constipation, or chest pain. She has an occasional dry cough that has been ongoing for about 6 months. The cough does not produce any sputum or blood.\nThe patient's past medical history is significant for hypertension, for which she takes a beta-blocker once daily. She also has hyperlipidemia, for which she takes a statin once daily.\nThe patient had a mammogram 2 years earlier, which did not reveal any abnormalities. Her most recent Pap test was 2 years ago, and the results were normal. She has never had a colonoscopy.\nThe patient is a current smoker; she has smoked one pack per day for the past 31 years. She drinks one glass of wine a week and does not use any illicit drugs. She currently works full-time as a server at a local restaurant.\nHer family history is significant for the death of her father from lung cancer at the age of 62 years. Her mother was diagnosed with colon cancer at the age of 52 years; she received treatment and is still living. The patient has a younger sister, aged 50 years, who is healthy.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A 53-Year-Old Waitress With a Cough and Constant Back Pain"
},
{
"authors": "Avan Armaghani, MD",
"content": [
"The patient's temperature is 98.1 °F (36.7 °C), blood pressure is 132/91 mm Hg, heart rate is 88 beats/min, respiration rate is 18 breaths/min, and oxygen saturation level is 98% on room air.",
"She is alert and oriented to person, place, and time. She appears to be comfortable sitting on the examination table and is in no acute distress. Pupils are equal and reactive to light, extraocular motions are intact, and conjunctiva are normal. She has no palpable lymphadenopathy in the cervical, submandibular, or supraclavicular regions. Her throat is normal, without erythema.",
"The lungs are clear to auscultation, no wheezing is audible, and breath sounds are equal bilaterally. The heart rhythm is regular, with no murmurs, rubs, or gallops. The abdomen is soft, nontender, and nondistended. No splenomegaly or hepatomegaly is detected. No rashes are noted. Cranial nerves two through twelve are intact. The patient has equal patellar reflexes bilaterally. She has normal strength and sensation in the bilateral upper and lower extremities. Her gait is normal.",
"A breast examination reveals no palpable lumps or nodules in either breast. No nipple inversion or overlying rashes or nodules are noted. There is no palpable axillary adenopathy bilaterally.",
"A complete blood cell count and a comprehensive metabolic panel reveal the following values:",
"Hemoglobin level: 12.9 g/dL (reference range, 12-16 g/dL)",
"Hematocrit: 36.9% (reference range, 36-46%)",
"Platelet count: 226,000 cells/µL (reference range, 150,000-400,000 cells/µL)",
"Sodium level: 140 mmol/L (reference range, 135-147 mmol/L)",
"Potassium level: 3.9 mmol/L (reference range, 3.5-5.0 mmol/L)",
"Creatinine level: 0.8 mg/dL (reference range, 0.9-1.3 mg/dL)",
"Total bilirubin level: 0.4 mg/dL (reference range, 0.1-1.2 mg/dL)",
"Aspartate aminotransferase level: 32 U/L (reference range, 8-40 U/L)",
"Alanine aminotransferase level: 24 U/L (reference range, 4-36 U/L)",
"Alkaline phosphatase level: 355 U/L (reference range, 35-105 U/L).",
"A chest radiograph shows hyperinflated lungs, with flattening of the diaphragm bilaterally (see example shown in the figure below). No nodules or other abnormalities are identified.",
"Figure 1.",
"A radiograph of the spine reveals multiple lucent lesions in the vertebral bodies at levels T8, T9, L1, and L3. MRI of the thoracic and lumbar spine shows destructive lesions at vertebral body levels T8, T9, L1, and L3; the spinal cord is not involved. Similar lesions are evident on an MRI of the spine in another patient (Figure 2).",
"Figure 2."
],
"date": "March 22, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/970/288/970288-Thumb.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/970/288/970288-Thumb2.png"
}
],
"markdown": "# A 53-Year-Old Waitress With a Cough and Constant Back Pain\n\n **Authors:** Avan Armaghani, MD \n **Date:** March 22, 2022\n\n ## Content\n\n The patient's temperature is 98.1 °F (36.7 °C), blood pressure is 132/91 mm Hg, heart rate is 88 beats/min, respiration rate is 18 breaths/min, and oxygen saturation level is 98% on room air.\nShe is alert and oriented to person, place, and time. She appears to be comfortable sitting on the examination table and is in no acute distress. Pupils are equal and reactive to light, extraocular motions are intact, and conjunctiva are normal. She has no palpable lymphadenopathy in the cervical, submandibular, or supraclavicular regions. Her throat is normal, without erythema.\nThe lungs are clear to auscultation, no wheezing is audible, and breath sounds are equal bilaterally. The heart rhythm is regular, with no murmurs, rubs, or gallops. The abdomen is soft, nontender, and nondistended. No splenomegaly or hepatomegaly is detected. No rashes are noted. Cranial nerves two through twelve are intact. The patient has equal patellar reflexes bilaterally. She has normal strength and sensation in the bilateral upper and lower extremities. Her gait is normal.\nA breast examination reveals no palpable lumps or nodules in either breast. No nipple inversion or overlying rashes or nodules are noted. There is no palpable axillary adenopathy bilaterally.\nA complete blood cell count and a comprehensive metabolic panel reveal the following values:\nHemoglobin level: 12.9 g/dL (reference range, 12-16 g/dL)\nHematocrit: 36.9% (reference range, 36-46%)\nPlatelet count: 226,000 cells/µL (reference range, 150,000-400,000 cells/µL)\nSodium level: 140 mmol/L (reference range, 135-147 mmol/L)\nPotassium level: 3.9 mmol/L (reference range, 3.5-5.0 mmol/L)\nCreatinine level: 0.8 mg/dL (reference range, 0.9-1.3 mg/dL)\nTotal bilirubin level: 0.4 mg/dL (reference range, 0.1-1.2 mg/dL)\nAspartate aminotransferase level: 32 U/L (reference range, 8-40 U/L)\nAlanine aminotransferase level: 24 U/L (reference range, 4-36 U/L)\nAlkaline phosphatase level: 355 U/L (reference range, 35-105 U/L).\nA chest radiograph shows hyperinflated lungs, with flattening of the diaphragm bilaterally (see example shown in the figure below). No nodules or other abnormalities are identified.\nFigure 1.\nA radiograph of the spine reveals multiple lucent lesions in the vertebral bodies at levels T8, T9, L1, and L3. MRI of the thoracic and lumbar spine shows destructive lesions at vertebral body levels T8, T9, L1, and L3; the spinal cord is not involved. Similar lesions are evident on an MRI of the spine in another patient (Figure 2).\nFigure 2.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1670349,
"choiceText": "Work-related injury",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670350,
"choiceText": "Sciatica",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670351,
"choiceText": "Osteoporosis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670352,
"choiceText": "Metastatic cancer",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 538008,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 53-Year-Old Waitress With a Cough and Constant Back Pain"
},
{
"authors": "Avan Armaghani, MD",
"content": [
"The patient underwent a biopsy of the T9 vertebral body lesion. The results were consistent with metastatic adenocarcinoma. Immunohistochemical staining of the biopsy specimen was positive for CK7 and GATA-3 and negative for TTF-1 and CK20.",
"A PET was performed for further evaluation. Fluorodeoxyglucose (FDG) avidity was noted in the previously identified areas at T8, T9, L1, and L3. In addition, FDG avidity was present in the sternum, pelvis, and left femur. These findings were consistent with metastatic disease.",
"A mammogram revealed heterogeneously dense breasts. No architectural distortion or suspicious masses or calcifications were noted in either breast.",
"An MRI showed no suspicious masses or patterns of no mass enhancement in the left or right breast. The left and right chest wall and nipple-areolar complex appeared normal. No suspicious left or right axillary lymph nodes or left or right internal mammary lymph nodes were identified.",
"On the basis of the bone biopsy results, a diagnosis of occult primary breast cancer (OPBC) was made. With respect to other possible diagnoses, the patient did not recall any previous trauma or injury that may have caused her back pain, and no clinical evidence was suggestive of this. Although sciatica typically presents with low back pain, it also is commonly associated with pain that radiates down the leg. This patient reported low back pain but no radiation of the pain. Osteoporosis usually does not present with low back pain.",
"OPBC is a rare entity and accounts for 0.1%-0.7% of all breast cancers. Patients typically present with axillary lymphadenopathy and/or distant disease, without clinical or radiographic evidence of a primary breast mass. OPBC was first described in 1907 by Halsted[1] and since then has been reported in case series.[2,3,4]"
],
"date": "March 22, 2022",
"figures": [],
"markdown": "# A 53-Year-Old Waitress With a Cough and Constant Back Pain\n\n **Authors:** Avan Armaghani, MD \n **Date:** March 22, 2022\n\n ## Content\n\n The patient underwent a biopsy of the T9 vertebral body lesion. The results were consistent with metastatic adenocarcinoma. Immunohistochemical staining of the biopsy specimen was positive for CK7 and GATA-3 and negative for TTF-1 and CK20.\nA PET was performed for further evaluation. Fluorodeoxyglucose (FDG) avidity was noted in the previously identified areas at T8, T9, L1, and L3. In addition, FDG avidity was present in the sternum, pelvis, and left femur. These findings were consistent with metastatic disease.\nA mammogram revealed heterogeneously dense breasts. No architectural distortion or suspicious masses or calcifications were noted in either breast.\nAn MRI showed no suspicious masses or patterns of no mass enhancement in the left or right breast. The left and right chest wall and nipple-areolar complex appeared normal. No suspicious left or right axillary lymph nodes or left or right internal mammary lymph nodes were identified.\nOn the basis of the bone biopsy results, a diagnosis of occult primary breast cancer (OPBC) was made. With respect to other possible diagnoses, the patient did not recall any previous trauma or injury that may have caused her back pain, and no clinical evidence was suggestive of this. Although sciatica typically presents with low back pain, it also is commonly associated with pain that radiates down the leg. This patient reported low back pain but no radiation of the pain. Osteoporosis usually does not present with low back pain.\nOPBC is a rare entity and accounts for 0.1%-0.7% of all breast cancers. Patients typically present with axillary lymphadenopathy and/or distant disease, without clinical or radiographic evidence of a primary breast mass. OPBC was first described in 1907 by Halsted[1] and since then has been reported in case series.[2,3,4]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1670349,
"choiceText": "Work-related injury",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670350,
"choiceText": "Sciatica",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670351,
"choiceText": "Osteoporosis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670352,
"choiceText": "Metastatic cancer",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 538008,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 53-Year-Old Waitress With a Cough and Constant Back Pain"
},
{
"authors": "Avan Armaghani, MD",
"content": [
"Initially, this patient presented with low back pain, and radiographic and MRI studies showed lesions in the thoracic and lumbar vertebral bodies. PET revealed additional bone lesions and no evidence of disease in other organs (ie, liver and lungs). Further imaging to consider in a woman with carcinoma of unknown primary site includes mammography, ultrasonography, and breast MRI. Following the recommendations for colonoscopy screening and gynecologic examination is important in such patients.",
"Immunohistochemical staining of a biopsy specimen is helpful in determining the originating site of the cancer. Breast cancer is typically positive for CK7 and GATA-3 and negative for CK20.[5]",
"Additional testing showed that this patient's bone biopsy specimen was estrogen and progesterone receptor–positive and HER2-negative. The rarity of this form of breast cancer has made it difficult to establish standard guidelines for treatment. Therefore, management is based on guidelines set out by the National Comprehensive Cancer Network (NCCN).[6,7,8]",
"Aromatase inhibitors (AIs) include anastrozole, letrozole, and exemestane. Although AI monotherapy is not the preferred first-line therapy in patients with hormone receptor–positive, HER2-negative (HR+/HER2-) metastatic breast cancer, it can be used in selected patients who may not be able to tolerate other combination treatment regimens. A meta-analysis showed that AI monotherapy had a statistically significant survival benefit compared with tamoxifen and other endocrine therapies.[9]",
"Targeted therapies, including CDK 4/6 inhibitors and mammalian target of rapamycin (mTOR) inhibitors, are also used in the treatment of HR+/HER2- metastatic breast cancer. Palbociclib, ribociclib, and abemaciclib are the three CDK 4/6 inhibitors that are currently approved by the US Food and Drug Administration. Palbociclib in combination with an AI as first-line treatment of estrogen receptor–positive (ER+)/HER2- metastatic breast cancer has demonstrated a significant improvement in progression-free survival (PFS).[10] Similar findings have been reported with ribociclib and abemaciclib.[11,12]",
"CDK 4/6 inhibitors in combination with AIs are the preferred first-line treatment in ER+/HER2- metastatic breast cancer. Fulvestrant is an alternative to first-line treatment for HR+/HER2- metastatic breast cancer.[13] This selective estrogen receptor degrader (SERD) has shown to be effective as monotherapy and in combination therapy in the treatment of metastatic breast cancer.[13] Fulvestrant in combination with ribociclib has demonstrated improved PFS in patients with HR+/HER2- metastatic breast cancer who have not received any prior treatment or as much as one line of prior endocrine therapy.[14] The mTOR inhibitor everolimus, in combination with exemestane, has shown to improve PFS in patients with HR+/HER2- metastatic breast cancer who were previously treated with nonsteroidal AI therapy.[15]",
"Subsequent lines of therapy in HR+/HER2- metastatic breast cancer include abemaciclib, which has been shown to be effective monotherapy in patients whose disease progressed on or after prior endocrine therapy and who had one or two chemotherapy regimens.[16] Abemaciclib has also shown to have overall survival benefit in combination with fulvestrant for women with disease progression after endocrine therapy.[17]",
"Chemotherapy remains an acceptable option. However, with the advent of effective nonchemotherapy modalities that are associated with fewer adverse effects, chemotherapy is generally used in much later lines of treatment.",
"The treatment of breast cancer continues to evolve, and therapies are becoming more personalized. For example, oral poly(adenosine diphosphate-ribose) polymerase inhibitors (PARP-Is) are approved by the FDA for the treatment of HER2- metastatic breast cancer in women who harbor a germline BRCA mutation and have received prior lines of therapy. Both olaparib and talazoparib are PARP-Is that have been approved in this setting.[18,19] Patients who harbor a germline mutation of PIK3CA and who have previously received endocrine therapy but not chemotherapy are eligible to receive a novel therapy: Alpelisib in combination with fulvestrant.[20]"
],
"date": "March 22, 2022",
"figures": [],
"markdown": "# A 53-Year-Old Waitress With a Cough and Constant Back Pain\n\n **Authors:** Avan Armaghani, MD \n **Date:** March 22, 2022\n\n ## Content\n\n Initially, this patient presented with low back pain, and radiographic and MRI studies showed lesions in the thoracic and lumbar vertebral bodies. PET revealed additional bone lesions and no evidence of disease in other organs (ie, liver and lungs). Further imaging to consider in a woman with carcinoma of unknown primary site includes mammography, ultrasonography, and breast MRI. Following the recommendations for colonoscopy screening and gynecologic examination is important in such patients.\nImmunohistochemical staining of a biopsy specimen is helpful in determining the originating site of the cancer. Breast cancer is typically positive for CK7 and GATA-3 and negative for CK20.[5]\nAdditional testing showed that this patient's bone biopsy specimen was estrogen and progesterone receptor–positive and HER2-negative. The rarity of this form of breast cancer has made it difficult to establish standard guidelines for treatment. Therefore, management is based on guidelines set out by the National Comprehensive Cancer Network (NCCN).[6,7,8]\nAromatase inhibitors (AIs) include anastrozole, letrozole, and exemestane. Although AI monotherapy is not the preferred first-line therapy in patients with hormone receptor–positive, HER2-negative (HR+/HER2-) metastatic breast cancer, it can be used in selected patients who may not be able to tolerate other combination treatment regimens. A meta-analysis showed that AI monotherapy had a statistically significant survival benefit compared with tamoxifen and other endocrine therapies.[9]\nTargeted therapies, including CDK 4/6 inhibitors and mammalian target of rapamycin (mTOR) inhibitors, are also used in the treatment of HR+/HER2- metastatic breast cancer. Palbociclib, ribociclib, and abemaciclib are the three CDK 4/6 inhibitors that are currently approved by the US Food and Drug Administration. Palbociclib in combination with an AI as first-line treatment of estrogen receptor–positive (ER+)/HER2- metastatic breast cancer has demonstrated a significant improvement in progression-free survival (PFS).[10] Similar findings have been reported with ribociclib and abemaciclib.[11,12]\nCDK 4/6 inhibitors in combination with AIs are the preferred first-line treatment in ER+/HER2- metastatic breast cancer. Fulvestrant is an alternative to first-line treatment for HR+/HER2- metastatic breast cancer.[13] This selective estrogen receptor degrader (SERD) has shown to be effective as monotherapy and in combination therapy in the treatment of metastatic breast cancer.[13] Fulvestrant in combination with ribociclib has demonstrated improved PFS in patients with HR+/HER2- metastatic breast cancer who have not received any prior treatment or as much as one line of prior endocrine therapy.[14] The mTOR inhibitor everolimus, in combination with exemestane, has shown to improve PFS in patients with HR+/HER2- metastatic breast cancer who were previously treated with nonsteroidal AI therapy.[15]\nSubsequent lines of therapy in HR+/HER2- metastatic breast cancer include abemaciclib, which has been shown to be effective monotherapy in patients whose disease progressed on or after prior endocrine therapy and who had one or two chemotherapy regimens.[16] Abemaciclib has also shown to have overall survival benefit in combination with fulvestrant for women with disease progression after endocrine therapy.[17]\nChemotherapy remains an acceptable option. However, with the advent of effective nonchemotherapy modalities that are associated with fewer adverse effects, chemotherapy is generally used in much later lines of treatment.\nThe treatment of breast cancer continues to evolve, and therapies are becoming more personalized. For example, oral poly(adenosine diphosphate-ribose) polymerase inhibitors (PARP-Is) are approved by the FDA for the treatment of HER2- metastatic breast cancer in women who harbor a germline BRCA mutation and have received prior lines of therapy. Both olaparib and talazoparib are PARP-Is that have been approved in this setting.[18,19] Patients who harbor a germline mutation of PIK3CA and who have previously received endocrine therapy but not chemotherapy are eligible to receive a novel therapy: Alpelisib in combination with fulvestrant.[20]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A 53-Year-Old Waitress With a Cough and Constant Back Pain"
},
{
"authors": "Avan Armaghani, MD",
"content": [
"Oral SERDs are currently under investigation as a new therapy for ER+/HER2- metastatic breast cancer. A phase 1 study recently evaluated the safety and antitumor activity of the oral SERD elacestrant in heavily pretreated women with ER+/HER2- metastatic breast cancer. The median number of prior therapies was three. The objective response rate was 19.4% and the clinical benefit rate was 42.6% in the overall population. The most common adverse events were nausea, increased blood triglyceride levels, and decreased serum phosphorous levels.[21] These data show promise for the future use of oral SERDs in the treatment of ER+/HER2- metastatic breast cancer.",
"Current NCCN guideline category 1 recommendations for the treatment of HR+/HER2- metastatic breast cancer include an AI plus a CDK 4/6 inhibitor, fulvestrant with or without an AI, and fulvestrant plus a CDK 4/6 inhibitor.[22] Category 1 recommendations for second and subsequent lines of therapy include fulvestrant plus a CDK 4/6 inhibitor if a CKD 4/6 inhibitor has not previously been used. Other considerations for second and subsequent lines of therapy include single-agent fulvestrant, AIs, targeted agents, and chemotherapy.",
"The patient in this case was referred to a medical oncologist, and systemic treatment was subsequently started. She was also referred to a radiation oncologist and received palliative radiation to the lower back for the alleviation of pain."
],
"date": "March 22, 2022",
"figures": [],
"markdown": "# A 53-Year-Old Waitress With a Cough and Constant Back Pain\n\n **Authors:** Avan Armaghani, MD \n **Date:** March 22, 2022\n\n ## Content\n\n Oral SERDs are currently under investigation as a new therapy for ER+/HER2- metastatic breast cancer. A phase 1 study recently evaluated the safety and antitumor activity of the oral SERD elacestrant in heavily pretreated women with ER+/HER2- metastatic breast cancer. The median number of prior therapies was three. The objective response rate was 19.4% and the clinical benefit rate was 42.6% in the overall population. The most common adverse events were nausea, increased blood triglyceride levels, and decreased serum phosphorous levels.[21] These data show promise for the future use of oral SERDs in the treatment of ER+/HER2- metastatic breast cancer.\nCurrent NCCN guideline category 1 recommendations for the treatment of HR+/HER2- metastatic breast cancer include an AI plus a CDK 4/6 inhibitor, fulvestrant with or without an AI, and fulvestrant plus a CDK 4/6 inhibitor.[22] Category 1 recommendations for second and subsequent lines of therapy include fulvestrant plus a CDK 4/6 inhibitor if a CKD 4/6 inhibitor has not previously been used. Other considerations for second and subsequent lines of therapy include single-agent fulvestrant, AIs, targeted agents, and chemotherapy.\nThe patient in this case was referred to a medical oncologist, and systemic treatment was subsequently started. She was also referred to a radiation oncologist and received palliative radiation to the lower back for the alleviation of pain.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1670359,
"choiceText": "Bilateral breast MRI ",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670360,
"choiceText": "PET ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670361,
"choiceText": "Breast ultrasound ",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670362,
"choiceText": "No further workup",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nMammography fails to detect 15% of breast cancers, which are termed mammographically occult.<sup>[2,3,4]</sup> If suspicion remains high for breast cancer and the mammogram is negative, an MRI of the breast is recommended owing to the high sensitivity of MRI for detecting breast cancers.\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 538010,
"questionText": "For a patient with suspected breast cancer who has negative mammography findings, which is the most appropriate next step?\r\n",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1670363,
"choiceText": "Olaparib",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670364,
"choiceText": "Everolimus",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670365,
"choiceText": "Alpelisib",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670366,
"choiceText": "Pembrolizumab",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Alpelisib is approved by the FDA in combination with fulvestrant for the treatment of ER+/HER2- metastatic breast cancer that harbors a <i>PIK3CA</i> mutation. Next-generation sequencing is performed on the tumor to identify potentially targetable mutations. Olaparib is approved for the treatment of patients with a <i>BRCA1</i> or <i>BRCA2</i> mutation. Everolimus is approved for the treatment of patients with ER+/HER2- metastatic breast cancer in combination with exemestane and is not dependent on any mutation. Immunotherapy with pembrolizumab is currently used only in the treatment of triple-negative breast cancer.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 538011,
"questionText": "The patient in this case underwent a next-generation sequencing test of her tumor. The results showed a <i>PIK3CA</i> mutation. Which therapy is she eligible to receive?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 53-Year-Old Waitress With a Cough and Constant Back Pain"
},
{
"authors": "Avan Armaghani, MD",
"content": [],
"date": "March 22, 2022",
"figures": [],
"markdown": "# A 53-Year-Old Waitress With a Cough and Constant Back Pain\n\n **Authors:** Avan Armaghani, MD \n **Date:** March 22, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1670359,
"choiceText": "Bilateral breast MRI ",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670360,
"choiceText": "PET ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670361,
"choiceText": "Breast ultrasound ",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670362,
"choiceText": "No further workup",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nMammography fails to detect 15% of breast cancers, which are termed mammographically occult.<sup>[2,3,4]</sup> If suspicion remains high for breast cancer and the mammogram is negative, an MRI of the breast is recommended owing to the high sensitivity of MRI for detecting breast cancers.\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 538010,
"questionText": "For a patient with suspected breast cancer who has negative mammography findings, which is the most appropriate next step?\r\n",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1670363,
"choiceText": "Olaparib",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670364,
"choiceText": "Everolimus",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670365,
"choiceText": "Alpelisib",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670366,
"choiceText": "Pembrolizumab",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Alpelisib is approved by the FDA in combination with fulvestrant for the treatment of ER+/HER2- metastatic breast cancer that harbors a <i>PIK3CA</i> mutation. Next-generation sequencing is performed on the tumor to identify potentially targetable mutations. Olaparib is approved for the treatment of patients with a <i>BRCA1</i> or <i>BRCA2</i> mutation. Everolimus is approved for the treatment of patients with ER+/HER2- metastatic breast cancer in combination with exemestane and is not dependent on any mutation. Immunotherapy with pembrolizumab is currently used only in the treatment of triple-negative breast cancer.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 538011,
"questionText": "The patient in this case underwent a next-generation sequencing test of her tumor. The results showed a <i>PIK3CA</i> mutation. Which therapy is she eligible to receive?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 53-Year-Old Waitress With a Cough and Constant Back Pain"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1670349,
"choiceText": "Work-related injury",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670350,
"choiceText": "Sciatica",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670351,
"choiceText": "Osteoporosis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670352,
"choiceText": "Metastatic cancer",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 538008,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1670359,
"choiceText": "Bilateral breast MRI ",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670360,
"choiceText": "PET ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670361,
"choiceText": "Breast ultrasound ",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670362,
"choiceText": "No further workup",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nMammography fails to detect 15% of breast cancers, which are termed mammographically occult.<sup>[2,3,4]</sup> If suspicion remains high for breast cancer and the mammogram is negative, an MRI of the breast is recommended owing to the high sensitivity of MRI for detecting breast cancers.\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 538010,
"questionText": "For a patient with suspected breast cancer who has negative mammography findings, which is the most appropriate next step?\r\n",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1670363,
"choiceText": "Olaparib",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670364,
"choiceText": "Everolimus",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670365,
"choiceText": "Alpelisib",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1670366,
"choiceText": "Pembrolizumab",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Alpelisib is approved by the FDA in combination with fulvestrant for the treatment of ER+/HER2- metastatic breast cancer that harbors a <i>PIK3CA</i> mutation. Next-generation sequencing is performed on the tumor to identify potentially targetable mutations. Olaparib is approved for the treatment of patients with a <i>BRCA1</i> or <i>BRCA2</i> mutation. Everolimus is approved for the treatment of patients with ER+/HER2- metastatic breast cancer in combination with exemestane and is not dependent on any mutation. Immunotherapy with pembrolizumab is currently used only in the treatment of triple-negative breast cancer.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 538011,
"questionText": "The patient in this case underwent a next-generation sequencing test of her tumor. The results showed a <i>PIK3CA</i> mutation. Which therapy is she eligible to receive?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
876163 | /viewarticle/876163 | [
{
"authors": "Nicola E. Burch, MBChB, MRCP; Victoria M. Gordon, MBBS, MRCP",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 24-year-old Caribbean man who is currently incarcerated presents with symptomatic anemia. He is primarily complaining of exertional dyspnea, generalized fatigue, and some mild chronic nausea. He has no known history of hematemesis, melena, rectal bleeding, or hemoptysis.",
"His family history is significant for sickle cell anemia in both his grandmother and sister. His medical history is limited to asthma that is controlled with salbutamol and beclomethasone inhalers and to previous admissions for symptomatic idiopathic anemia, for which he has been maintained on iron supplementation.",
"The patient is a nonsmoker and does not drink alcohol. He has no history of nonsteroidal anti-inflammatory drug or aspirin use. His diet is varied and nonvegetarian."
],
"date": "March 18, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: An Incarcerated 24-Year-Old With Dyspnea, Fatigue, and Chronic Nausea\n\n **Authors:** Nicola E. Burch, MBChB, MRCP; Victoria M. Gordon, MBBS, MRCP \n **Date:** March 18, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 24-year-old Caribbean man who is currently incarcerated presents with symptomatic anemia. He is primarily complaining of exertional dyspnea, generalized fatigue, and some mild chronic nausea. He has no known history of hematemesis, melena, rectal bleeding, or hemoptysis.\nHis family history is significant for sickle cell anemia in both his grandmother and sister. His medical history is limited to asthma that is controlled with salbutamol and beclomethasone inhalers and to previous admissions for symptomatic idiopathic anemia, for which he has been maintained on iron supplementation.\nThe patient is a nonsmoker and does not drink alcohol. He has no history of nonsteroidal anti-inflammatory drug or aspirin use. His diet is varied and nonvegetarian.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Gastro Case Challenge: An Incarcerated 24-Year-Old With Dyspnea, Fatigue, and Chronic Nausea"
},
{
"authors": "Nicola E. Burch, MBChB, MRCP; Victoria M. Gordon, MBBS, MRCP",
"content": [
"Upon physical examination, the patient appears to be well, although he does exhibit significant conjunctival pallor. His pulse is regular, at 88 beats/min, and his blood pressure is 110/64 mm Hg. No lymphadenopathy, jaundice, clubbing, or edema is noted. A soft, pansystolic murmur is detected over the tricuspid and aortic valves, without any stigmata of endocarditis.",
"The respiratory examination is unremarkable. No masses, tenderness, or hepatosplenomegaly are noted on the abdominal examination. A rectal examination reveals no masses, gross blood, or melena. The stool is brown and heme-negative.",
"The patient has had multiple admissions in the past 5 years for symptomatic anemia, all with similar presentations. Each time, he was noted to have iron deficiency anemia, with a hemoglobin level between 6 g/dL and 7 g/dL, as well as low mean corpuscular volume and low serum ferritin. He has never had documented episodes of gastrointestinal (GI) or extra-GI blood loss. He has complained intermittently of nausea but has not had any vomiting.",
"Numerous investigative procedures were completed during these previous admissions; the findings of these procedures included normal endoscopic findings (however, no D2 biopsies were done) and negative tissue transglutaminase, with normal levels of immunoglobulin A. Autoantibody findings (antinuclear antibody, antineutrophil cytoplasmic autoantibodies, double-stranded DNA, and small nuclear ribonucleoprotein Sm) were all negative. A direct Coombs test result was also negative. In addition, hemoglobin electrophoresis was normal, eliminating the possibility of sickle cell anemia.",
"During the current admission, another series of tests is performed. The results are as follows:",
"Hemoglobin level: 6.5 g/dL (reference range, 13.5-17.5 g/dL)",
"Mean corpuscular volume: 64.5 μm3 (reference range, 76-100 μm3)",
"White blood cell count: 4.2 × 103 cells/μL (reference range, 4.5-11 x 103 cells/μL)",
"Platelet count: 405 × 103 cells/μL (reference range, 150-450 x 103 cells/μL)",
"Neutrophil count: 1.6 × 109 cells/L (reference range, 1.5-8 × 109 cells/L)",
"Lymphocyte count: 2.1 × 109 cells/L (reference range, 1-4.8 × 109 cells/L)",
"Eosinophil count: 1 × 109 cells/L (reference range, 0-0.45 cells x 109/L)",
"Ferritin level: 9 ng/mL (reference range, 12-300 ng/mL)",
"C-reactive protein level: <5 mg/L (reference range, <3 mg/L)",
"Tests for autoantibodies (immunoglobulin), celiac serology, liver function, hemoglobin electrophoresis, vitamin B12, and folate all return normal results.",
"Colonoscopy is performed and is normal to the terminal ileum, with no underlying cause of anemia established. The patient undergoes a repeat endoscopy (having already had a normal endoscopy 1 year earlier). The appearance of the esophagus and duodenum is unremarkable. Patches of the gastric mucosa however, have an odd, nodular appearance (Figure 1). The area is biopsied; the histology is shown here (Figure 2).",
"Figure 1.",
"Figure 2."
],
"date": "March 18, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/876/163/876163-Thumb1.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/876/163/876163-Thumb2.jpg"
}
],
"markdown": "# Gastro Case Challenge: An Incarcerated 24-Year-Old With Dyspnea, Fatigue, and Chronic Nausea\n\n **Authors:** Nicola E. Burch, MBChB, MRCP; Victoria M. Gordon, MBBS, MRCP \n **Date:** March 18, 2022\n\n ## Content\n\n Upon physical examination, the patient appears to be well, although he does exhibit significant conjunctival pallor. His pulse is regular, at 88 beats/min, and his blood pressure is 110/64 mm Hg. No lymphadenopathy, jaundice, clubbing, or edema is noted. A soft, pansystolic murmur is detected over the tricuspid and aortic valves, without any stigmata of endocarditis.\nThe respiratory examination is unremarkable. No masses, tenderness, or hepatosplenomegaly are noted on the abdominal examination. A rectal examination reveals no masses, gross blood, or melena. The stool is brown and heme-negative.\nThe patient has had multiple admissions in the past 5 years for symptomatic anemia, all with similar presentations. Each time, he was noted to have iron deficiency anemia, with a hemoglobin level between 6 g/dL and 7 g/dL, as well as low mean corpuscular volume and low serum ferritin. He has never had documented episodes of gastrointestinal (GI) or extra-GI blood loss. He has complained intermittently of nausea but has not had any vomiting.\nNumerous investigative procedures were completed during these previous admissions; the findings of these procedures included normal endoscopic findings (however, no D2 biopsies were done) and negative tissue transglutaminase, with normal levels of immunoglobulin A. Autoantibody findings (antinuclear antibody, antineutrophil cytoplasmic autoantibodies, double-stranded DNA, and small nuclear ribonucleoprotein Sm) were all negative. A direct Coombs test result was also negative. In addition, hemoglobin electrophoresis was normal, eliminating the possibility of sickle cell anemia.\nDuring the current admission, another series of tests is performed. The results are as follows:\nHemoglobin level: 6.5 g/dL (reference range, 13.5-17.5 g/dL)\nMean corpuscular volume: 64.5 μm3 (reference range, 76-100 μm3)\nWhite blood cell count: 4.2 × 103 cells/μL (reference range, 4.5-11 x 103 cells/μL)\nPlatelet count: 405 × 103 cells/μL (reference range, 150-450 x 103 cells/μL)\nNeutrophil count: 1.6 × 109 cells/L (reference range, 1.5-8 × 109 cells/L)\nLymphocyte count: 2.1 × 109 cells/L (reference range, 1-4.8 × 109 cells/L)\nEosinophil count: 1 × 109 cells/L (reference range, 0-0.45 cells x 109/L)\nFerritin level: 9 ng/mL (reference range, 12-300 ng/mL)\nC-reactive protein level: <5 mg/L (reference range, <3 mg/L)\nTests for autoantibodies (immunoglobulin), celiac serology, liver function, hemoglobin electrophoresis, vitamin B12, and folate all return normal results.\nColonoscopy is performed and is normal to the terminal ileum, with no underlying cause of anemia established. The patient undergoes a repeat endoscopy (having already had a normal endoscopy 1 year earlier). The appearance of the esophagus and duodenum is unremarkable. Patches of the gastric mucosa however, have an odd, nodular appearance (Figure 1). The area is biopsied; the histology is shown here (Figure 2).\nFigure 1.\nFigure 2.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1070070,
"choiceText": "Celiac sprue",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070072,
"choiceText": "Idiopathic eosinophilic gastroenteritis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070074,
"choiceText": "Eosinophilic granuloma (histiocytosis X)",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070076,
"choiceText": "Crohn disease\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 338825,
"questionText": "Based on only these findings, which is the most likely underlying etiology of the patient's anemia?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: An Incarcerated 24-Year-Old With Dyspnea, Fatigue, and Chronic Nausea"
},
{
"authors": "Nicola E. Burch, MBChB, MRCP; Victoria M. Gordon, MBBS, MRCP",
"content": [
"The patient was diagnosed with idiopathic eosinophilic gastroenteritis on the basis of the diffuse eosinophilic infiltrate seen on the histologic samples taken from the nodular area of his gastric antrum (Figure 2).",
"Figure 2.",
"Eosinophilic gastroenteritis is a rare inflammatory disorder characterized by eosinophilic infiltration of the GI tract, without any known cause of eosinophilia. The gastric antrum and duodenum are primarily involved, but it can also affect the esophagus and colon. It was first described by Kaijser in 1937.[1] Although more than 300 cases have been reported worldwide, the true incidence is unclear. A confounding factor in its characterization is the lack of diagnostic precision.[2]",
"This condition is an uncommon GI disease that affects adults and children. It usually presents between the third and fifth decades of life; however, it may present in patients of any age. It appears to be slightly more common in white males. A coexistent history of atopy (in approximately 50% of cases), such as asthma (as seen in this case), hay fever, eczema, or food intolerances, is common.",
"Although the precise underlying pathophysiologic mechanism remains unknown, the most widely accepted theory involves mast cell activation by possible allergenic insult, leading to histamine and cytokine release, which causes eosinophil activation. Allergens (eg, food, virus, immunoglobulin) initially enter the GI tract via the compromised integrity of the gut mucosa. The subsequent activation of eosinophils by the allergen leads to the release of platelet-activating factor, histamines, toxic proteins, and leukotrienes, which results in mucosal damage and inflammation. Few reports have described death resulting from this condition; however, malnutrition and intestinal perforation may be seen.[2,3,4,5,6,7]",
"The time between the initial presentation and the diagnosis may be months or years, as a result of the broad spectrum of presenting symptoms. The fact that the presenting features may overlap with those of other, more common underlying GI diseases (such as inflammatory bowel disease) can lead to misdiagnosis and unnecessary therapy.[2,4]"
],
"date": "March 18, 2022",
"figures": [
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/876/163/876163-Thumb2.jpg"
}
],
"markdown": "# Gastro Case Challenge: An Incarcerated 24-Year-Old With Dyspnea, Fatigue, and Chronic Nausea\n\n **Authors:** Nicola E. Burch, MBChB, MRCP; Victoria M. Gordon, MBBS, MRCP \n **Date:** March 18, 2022\n\n ## Content\n\n The patient was diagnosed with idiopathic eosinophilic gastroenteritis on the basis of the diffuse eosinophilic infiltrate seen on the histologic samples taken from the nodular area of his gastric antrum (Figure 2).\nFigure 2.\nEosinophilic gastroenteritis is a rare inflammatory disorder characterized by eosinophilic infiltration of the GI tract, without any known cause of eosinophilia. The gastric antrum and duodenum are primarily involved, but it can also affect the esophagus and colon. It was first described by Kaijser in 1937.[1] Although more than 300 cases have been reported worldwide, the true incidence is unclear. A confounding factor in its characterization is the lack of diagnostic precision.[2]\nThis condition is an uncommon GI disease that affects adults and children. It usually presents between the third and fifth decades of life; however, it may present in patients of any age. It appears to be slightly more common in white males. A coexistent history of atopy (in approximately 50% of cases), such as asthma (as seen in this case), hay fever, eczema, or food intolerances, is common.\nAlthough the precise underlying pathophysiologic mechanism remains unknown, the most widely accepted theory involves mast cell activation by possible allergenic insult, leading to histamine and cytokine release, which causes eosinophil activation. Allergens (eg, food, virus, immunoglobulin) initially enter the GI tract via the compromised integrity of the gut mucosa. The subsequent activation of eosinophils by the allergen leads to the release of platelet-activating factor, histamines, toxic proteins, and leukotrienes, which results in mucosal damage and inflammation. Few reports have described death resulting from this condition; however, malnutrition and intestinal perforation may be seen.[2,3,4,5,6,7]\nThe time between the initial presentation and the diagnosis may be months or years, as a result of the broad spectrum of presenting symptoms. The fact that the presenting features may overlap with those of other, more common underlying GI diseases (such as inflammatory bowel disease) can lead to misdiagnosis and unnecessary therapy.[2,4]\n\n ## Figures\n\n **Figure 2.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1070070,
"choiceText": "Celiac sprue",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070072,
"choiceText": "Idiopathic eosinophilic gastroenteritis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070074,
"choiceText": "Eosinophilic granuloma (histiocytosis X)",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070076,
"choiceText": "Crohn disease\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 338825,
"questionText": "Based on only these findings, which is the most likely underlying etiology of the patient's anemia?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: An Incarcerated 24-Year-Old With Dyspnea, Fatigue, and Chronic Nausea"
},
{
"authors": "Nicola E. Burch, MBChB, MRCP; Victoria M. Gordon, MBBS, MRCP",
"content": [
"For a definitive diagnosis of eosinophilic gastroenteritis, the following four criteria must be met[2,6]:",
"Presence of GI symptoms",
"Demonstration of eosinophilic infiltration (>20 eosinophils per high-power field) in one or more areas of the GI tract",
"Absence of alternative causes of eosinophilia",
"No involvement outside of the GI tract (ie, no systemic eosinophilic pathology)",
"Histologic subclassification of eosinophilic gastroenteritis is determined according to the layer of the GI tract involved (mucosa, muscularis, or serosa). The clinical manifestations are also dependent on the affected area. Patients presenting with vomiting, abdominal pain, diarrhea, bloody stools, failure to thrive, and iron deficiency anemia often have mucosal infiltration. Patients with obstructive symptoms or dysphagia tend to have muscular involvement. Serosal involvement presents with eosinophilic ascites, which has been well described in the literature.[2,4]",
"The differential diagnosis includes all conditions with presenting features similar to those described above (ie, inflammatory bowel disease), as well as those that produce eosinophilia. Eosinophilic infections include parasitic infections (Ancylostoma caninum, giardiasis, strongyloidosis, and other zoonoses), connective tissue diseases (scleroderma, dermatomyositis, polymyositis), vasculitis (Churg-Strauss syndrome, polyarteritis nodosa), drug reactions (sulfonamides, penicillin, cephalosporin, carbamazepine, azathioprine, L-tryptophan, gold salts), celiac disease, and lymphoma.[2]",
"Investigations must center on confirmation of peripheral eosinophilia, evidence of increased eosinophil counts in GI tissue (defined variably as 10-50 eosinophils per high-power field), and the exclusion of alternative diagnoses. Imaging may help demonstrate the extent of bowel involvement, but it cannot distinguish this condition from alternative, more common diagnoses (eg, Crohn disease, ulcerative colitis).",
"Radiographic findings may be nonspecific or totally absent. Thickened intestinal walls and lymphadenopathy may be seen on ultrasonography and CT. Endoscopic findings are nonspecific and varied, but histologic demonstration of eosinophils in tissue samples is the criterion standard. If serosal involvement with ascites is noted, an ascitic tap that is rich in eosinophils is diagnostic.[2,3,4]"
],
"date": "March 18, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: An Incarcerated 24-Year-Old With Dyspnea, Fatigue, and Chronic Nausea\n\n **Authors:** Nicola E. Burch, MBChB, MRCP; Victoria M. Gordon, MBBS, MRCP \n **Date:** March 18, 2022\n\n ## Content\n\n For a definitive diagnosis of eosinophilic gastroenteritis, the following four criteria must be met[2,6]:\nPresence of GI symptoms\nDemonstration of eosinophilic infiltration (>20 eosinophils per high-power field) in one or more areas of the GI tract\nAbsence of alternative causes of eosinophilia\nNo involvement outside of the GI tract (ie, no systemic eosinophilic pathology)\nHistologic subclassification of eosinophilic gastroenteritis is determined according to the layer of the GI tract involved (mucosa, muscularis, or serosa). The clinical manifestations are also dependent on the affected area. Patients presenting with vomiting, abdominal pain, diarrhea, bloody stools, failure to thrive, and iron deficiency anemia often have mucosal infiltration. Patients with obstructive symptoms or dysphagia tend to have muscular involvement. Serosal involvement presents with eosinophilic ascites, which has been well described in the literature.[2,4]\nThe differential diagnosis includes all conditions with presenting features similar to those described above (ie, inflammatory bowel disease), as well as those that produce eosinophilia. Eosinophilic infections include parasitic infections (Ancylostoma caninum, giardiasis, strongyloidosis, and other zoonoses), connective tissue diseases (scleroderma, dermatomyositis, polymyositis), vasculitis (Churg-Strauss syndrome, polyarteritis nodosa), drug reactions (sulfonamides, penicillin, cephalosporin, carbamazepine, azathioprine, L-tryptophan, gold salts), celiac disease, and lymphoma.[2]\nInvestigations must center on confirmation of peripheral eosinophilia, evidence of increased eosinophil counts in GI tissue (defined variably as 10-50 eosinophils per high-power field), and the exclusion of alternative diagnoses. Imaging may help demonstrate the extent of bowel involvement, but it cannot distinguish this condition from alternative, more common diagnoses (eg, Crohn disease, ulcerative colitis).\nRadiographic findings may be nonspecific or totally absent. Thickened intestinal walls and lymphadenopathy may be seen on ultrasonography and CT. Endoscopic findings are nonspecific and varied, but histologic demonstration of eosinophils in tissue samples is the criterion standard. If serosal involvement with ascites is noted, an ascitic tap that is rich in eosinophils is diagnostic.[2,3,4]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Gastro Case Challenge: An Incarcerated 24-Year-Old With Dyspnea, Fatigue, and Chronic Nausea"
},
{
"authors": "Nicola E. Burch, MBChB, MRCP; Victoria M. Gordon, MBBS, MRCP",
"content": [
"Once the diagnosis of idiopathic eosinophilic gastroenteritis has been confirmed, the mainstay of treatment is primarily oral glucocorticoids, such as prednisone, to halt the inflammatory process and control symptoms. Budesonide has also been used successfully as an alternative.",
"Some researchers have investigated the elimination of possible allergenic foci (eg, dietary components, including milk, eggs, wheat and/or gluten, soy, and beef), as well as the use of skin testing to identify allergens; however, the effectiveness of this has yet to be proven.[2,7] In addition, mast cell stabilizers and other immunosuppressants (eg, montelukast, ketotifen, suplatast tosilate, mycophenolate mofetil) have been used in some cases; however, the success of these therapies has varied. Herbal therapies and Chinese medicine have also been evaluated, but no definite benefit has been shown to date. Surgery may be necessary in treatment-resistant cases, but this is generally considered a last resort, unless it is necessary to relieve persistent pyloric or small-bowel obstruction.[2,3,7]",
"The aim of early diagnosis and treatment is to prevent long-term complications, such as refractory ascites, bowel obstruction, perforation, recurrent iron deficiency anemia, and (rarely) premature death.[2]",
"In view of the histologic findings, the patient in this case was prescribed budesonide (9 mg daily). After the first month, the dose was reduced to 6 mg, and then to 3 mg for the third and final month. After budesonide was initiated, the eosinophilia apparently dropped.",
"After completion of a course of reduced-dose budesonide over 3 months, the patient remained well, and on laboratory examination had an eosinophil count at the higher end of the normal range. He did not require any further admissions for management of his symptomatic anemia and did not experience any other known complications. He was followed on a quarterly basis. A plan for the reinstatement of budesonide treatment should the patient develop additional complications was established.",
"This case highlights the diagnostic challenge of a condition that presents with common symptoms and apparently normal investigations. These findings should motivate and encourage the clinician to consider rarer diagnoses and pay special attention to seemingly unimportant clues, no matter how small, that may have been present all along. In this case, the patient had low-grade eosinophilia at the very first presentation, which was confirmed on review of previous examinations."
],
"date": "March 18, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: An Incarcerated 24-Year-Old With Dyspnea, Fatigue, and Chronic Nausea\n\n **Authors:** Nicola E. Burch, MBChB, MRCP; Victoria M. Gordon, MBBS, MRCP \n **Date:** March 18, 2022\n\n ## Content\n\n Once the diagnosis of idiopathic eosinophilic gastroenteritis has been confirmed, the mainstay of treatment is primarily oral glucocorticoids, such as prednisone, to halt the inflammatory process and control symptoms. Budesonide has also been used successfully as an alternative.\nSome researchers have investigated the elimination of possible allergenic foci (eg, dietary components, including milk, eggs, wheat and/or gluten, soy, and beef), as well as the use of skin testing to identify allergens; however, the effectiveness of this has yet to be proven.[2,7] In addition, mast cell stabilizers and other immunosuppressants (eg, montelukast, ketotifen, suplatast tosilate, mycophenolate mofetil) have been used in some cases; however, the success of these therapies has varied. Herbal therapies and Chinese medicine have also been evaluated, but no definite benefit has been shown to date. Surgery may be necessary in treatment-resistant cases, but this is generally considered a last resort, unless it is necessary to relieve persistent pyloric or small-bowel obstruction.[2,3,7]\nThe aim of early diagnosis and treatment is to prevent long-term complications, such as refractory ascites, bowel obstruction, perforation, recurrent iron deficiency anemia, and (rarely) premature death.[2]\nIn view of the histologic findings, the patient in this case was prescribed budesonide (9 mg daily). After the first month, the dose was reduced to 6 mg, and then to 3 mg for the third and final month. After budesonide was initiated, the eosinophilia apparently dropped.\nAfter completion of a course of reduced-dose budesonide over 3 months, the patient remained well, and on laboratory examination had an eosinophil count at the higher end of the normal range. He did not require any further admissions for management of his symptomatic anemia and did not experience any other known complications. He was followed on a quarterly basis. A plan for the reinstatement of budesonide treatment should the patient develop additional complications was established.\nThis case highlights the diagnostic challenge of a condition that presents with common symptoms and apparently normal investigations. These findings should motivate and encourage the clinician to consider rarer diagnoses and pay special attention to seemingly unimportant clues, no matter how small, that may have been present all along. In this case, the patient had low-grade eosinophilia at the very first presentation, which was confirmed on review of previous examinations.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1070078,
"choiceText": "Extra-GI involvement",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070080,
"choiceText": "History of atopy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070082,
"choiceText": "Demonstration of eosinophilic infiltration in the GI tract ",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070084,
"choiceText": "Systemic symptoms",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070086,
"choiceText": "Confirmatory radiographic findings",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "For a definitive diagnosis of eosinophilic gastroenteritis, the following four criteria must be met:<br><ul>\r\n<li>Presence of GI symptoms</li>\r\n<li>Demonstration of eosinophilic infiltration (>20 eosinophils per high-power field) in one or more areas of the GI tract</li>\r\n<li>Absence of alternative causes of eosinophilia</li>\r\n<li>No involvement outside of the GI tract (ie, no systemic eosinophilic pathology)</li>\r\n</ul>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 338827,
"questionText": "Which of the following is required for the diagnosis of idiopathic eosinophilic gastroenteritis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1070088,
"choiceText": "Surgery",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070090,
"choiceText": "Corticosteroids",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070092,
"choiceText": "Herbal medicine",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070094,
"choiceText": "Elimination diets",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070096,
"choiceText": "Infliximab",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Prednisone is the mainstay treatment for induction of remission of eosinophilic gastroenteritis. Mast cell stabilizers and other immunosuppressants (eg, montelukast, ketotifen, suplatast tosilate, mycophenolate mofetil) have also been used to treat eosinophilic gastroenteritis. <br><br>Surgery is only indicated for patients with severe disease complicated by perforation, intussusception, or intestinal occlusion. <br><br>Some researchers have investigated the elimination of possible allergenic agents (eg, dietary components, including milk, eggs, wheat and/or gluten, soy, and beef), as well as the use of skin testing to identify allergens; however, the effectiveness of this has yet to be proven. Herbal therapies and Chinese medicines have also been evaluated, but no definite benefit has been shown to date.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 338829,
"questionText": "Which of the following is most strongly supported to induce remission in patients with eosinophilic gastroenteritis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: An Incarcerated 24-Year-Old With Dyspnea, Fatigue, and Chronic Nausea"
},
{
"authors": "Nicola E. Burch, MBChB, MRCP; Victoria M. Gordon, MBBS, MRCP",
"content": [],
"date": "March 18, 2022",
"figures": [],
"markdown": "# Gastro Case Challenge: An Incarcerated 24-Year-Old With Dyspnea, Fatigue, and Chronic Nausea\n\n **Authors:** Nicola E. Burch, MBChB, MRCP; Victoria M. Gordon, MBBS, MRCP \n **Date:** March 18, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1070078,
"choiceText": "Extra-GI involvement",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070080,
"choiceText": "History of atopy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070082,
"choiceText": "Demonstration of eosinophilic infiltration in the GI tract ",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070084,
"choiceText": "Systemic symptoms",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070086,
"choiceText": "Confirmatory radiographic findings",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "For a definitive diagnosis of eosinophilic gastroenteritis, the following four criteria must be met:<br><ul>\r\n<li>Presence of GI symptoms</li>\r\n<li>Demonstration of eosinophilic infiltration (>20 eosinophils per high-power field) in one or more areas of the GI tract</li>\r\n<li>Absence of alternative causes of eosinophilia</li>\r\n<li>No involvement outside of the GI tract (ie, no systemic eosinophilic pathology)</li>\r\n</ul>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 338827,
"questionText": "Which of the following is required for the diagnosis of idiopathic eosinophilic gastroenteritis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1070088,
"choiceText": "Surgery",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070090,
"choiceText": "Corticosteroids",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070092,
"choiceText": "Herbal medicine",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070094,
"choiceText": "Elimination diets",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070096,
"choiceText": "Infliximab",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Prednisone is the mainstay treatment for induction of remission of eosinophilic gastroenteritis. Mast cell stabilizers and other immunosuppressants (eg, montelukast, ketotifen, suplatast tosilate, mycophenolate mofetil) have also been used to treat eosinophilic gastroenteritis. <br><br>Surgery is only indicated for patients with severe disease complicated by perforation, intussusception, or intestinal occlusion. <br><br>Some researchers have investigated the elimination of possible allergenic agents (eg, dietary components, including milk, eggs, wheat and/or gluten, soy, and beef), as well as the use of skin testing to identify allergens; however, the effectiveness of this has yet to be proven. Herbal therapies and Chinese medicines have also been evaluated, but no definite benefit has been shown to date.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 338829,
"questionText": "Which of the following is most strongly supported to induce remission in patients with eosinophilic gastroenteritis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Gastro Case Challenge: An Incarcerated 24-Year-Old With Dyspnea, Fatigue, and Chronic Nausea"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1070070,
"choiceText": "Celiac sprue",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070072,
"choiceText": "Idiopathic eosinophilic gastroenteritis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070074,
"choiceText": "Eosinophilic granuloma (histiocytosis X)",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070076,
"choiceText": "Crohn disease\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 338825,
"questionText": "Based on only these findings, which is the most likely underlying etiology of the patient's anemia?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1070078,
"choiceText": "Extra-GI involvement",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070080,
"choiceText": "History of atopy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070082,
"choiceText": "Demonstration of eosinophilic infiltration in the GI tract ",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070084,
"choiceText": "Systemic symptoms",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070086,
"choiceText": "Confirmatory radiographic findings",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "For a definitive diagnosis of eosinophilic gastroenteritis, the following four criteria must be met:<br><ul>\r\n<li>Presence of GI symptoms</li>\r\n<li>Demonstration of eosinophilic infiltration (>20 eosinophils per high-power field) in one or more areas of the GI tract</li>\r\n<li>Absence of alternative causes of eosinophilia</li>\r\n<li>No involvement outside of the GI tract (ie, no systemic eosinophilic pathology)</li>\r\n</ul>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 338827,
"questionText": "Which of the following is required for the diagnosis of idiopathic eosinophilic gastroenteritis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1070088,
"choiceText": "Surgery",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070090,
"choiceText": "Corticosteroids",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070092,
"choiceText": "Herbal medicine",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070094,
"choiceText": "Elimination diets",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070096,
"choiceText": "Infliximab",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Prednisone is the mainstay treatment for induction of remission of eosinophilic gastroenteritis. Mast cell stabilizers and other immunosuppressants (eg, montelukast, ketotifen, suplatast tosilate, mycophenolate mofetil) have also been used to treat eosinophilic gastroenteritis. <br><br>Surgery is only indicated for patients with severe disease complicated by perforation, intussusception, or intestinal occlusion. <br><br>Some researchers have investigated the elimination of possible allergenic agents (eg, dietary components, including milk, eggs, wheat and/or gluten, soy, and beef), as well as the use of skin testing to identify allergens; however, the effectiveness of this has yet to be proven. Herbal therapies and Chinese medicines have also been evaluated, but no definite benefit has been shown to date.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 338829,
"questionText": "Which of the following is most strongly supported to induce remission in patients with eosinophilic gastroenteritis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
746588 | /viewarticle/746588 | [
{
"authors": "Syeda Sabahat Mansur, MB BS; Fardidullah Shah, MB BS",
"content": [
"Editorial Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 17-year-old girl presents to the outpatient department with chronic, recurrent oral fungal infections, chronic diarrhea, recurrent abdominal pain, and vomiting since childhood. She has also been experiencing dizziness (especially on erect posture), darkening of the skin and oral cavity, and a low-grade fever for the last 6-8 months.",
"The oral thrush and ulcers have been recurrent since childhood; these are not associated with any antibiotic intake or trauma. Diarrhea has also occurred on and off since childhood, with 4-7 watery-to-semisolid bowel movements per day associated with crampy abdominal pain but not blood or mucus. The bowel movements are not associated with intake of wheat or wheat products; however, they do occur more frequently with the ingestion of meat and meat products.",
"The recurrent abdominal pain is more prominent in the central abdomen, is colicky without radiation, and is not associated with distention. Vomiting has occurred with a variable frequency of approximately 3-5 episodes a day. When she vomits, it is watery, usually associated with meals, and occasionally contains food particles; there have been no instances of blood in the vomitus. She complains of dizziness, especially on standing up from a supine or a sitting position.",
"According to the patient, darkening of the oral mucosa and the skin on her palms (especially in the palm creases), digits, and joints has been progressing for the last 1-2 years, with no history of prolonged exposure to sunlight.",
"Her intermittent fevers over the last 6-8 months have tended to be low-grade, occur at night, and be associated with sweating but not rigors or chills. She also has a history of lethargy, easy fatigability, and palpitations on exertion without chest pain; however, she has no history of loss of consciousness. Her appetite has decreased. The patient has lost about 11 lb (5 kg) over a period of 6 months.",
"She has experienced some hair loss, but no vitiligo has been noted. She also reports a history of nasal obstruction, sneezing, and postnasal drip, but she has not had hemoptysis. She has no history of joint swelling or pain. Additionally, she has not had any eye pain or decreased vision, but she has had difficulty in performing her routine activities such as going to the bathroom because of dizziness and weakness. She generally remains in bed.",
"The patient also reports dysmenorrhea. She has a history of polymenorrhagia but has had amenorrhea for the last year. She remains anxious and depressed. She has no known allergies, does not smoke, drink alcohol, or use illicit drugs, and she is not currently on any regular medication. She is unmarried, has no sexual contacts, and belongs to a middle-class family. She has no history of blood transfusion. The family history is significant for 2 siblings with similar presentations from early childhood. Her parents are alive and healthy."
],
"date": "March 15, 2022",
"figures": [],
"markdown": "# 17-Year-Old With Hair Loss, Dysmenorrhea, Thrush, and Diarrhea\n\n **Authors:** Syeda Sabahat Mansur, MB BS; Fardidullah Shah, MB BS \n **Date:** March 15, 2022\n\n ## Content\n\n Editorial Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 17-year-old girl presents to the outpatient department with chronic, recurrent oral fungal infections, chronic diarrhea, recurrent abdominal pain, and vomiting since childhood. She has also been experiencing dizziness (especially on erect posture), darkening of the skin and oral cavity, and a low-grade fever for the last 6-8 months.\nThe oral thrush and ulcers have been recurrent since childhood; these are not associated with any antibiotic intake or trauma. Diarrhea has also occurred on and off since childhood, with 4-7 watery-to-semisolid bowel movements per day associated with crampy abdominal pain but not blood or mucus. The bowel movements are not associated with intake of wheat or wheat products; however, they do occur more frequently with the ingestion of meat and meat products.\nThe recurrent abdominal pain is more prominent in the central abdomen, is colicky without radiation, and is not associated with distention. Vomiting has occurred with a variable frequency of approximately 3-5 episodes a day. When she vomits, it is watery, usually associated with meals, and occasionally contains food particles; there have been no instances of blood in the vomitus. She complains of dizziness, especially on standing up from a supine or a sitting position.\nAccording to the patient, darkening of the oral mucosa and the skin on her palms (especially in the palm creases), digits, and joints has been progressing for the last 1-2 years, with no history of prolonged exposure to sunlight.\nHer intermittent fevers over the last 6-8 months have tended to be low-grade, occur at night, and be associated with sweating but not rigors or chills. She also has a history of lethargy, easy fatigability, and palpitations on exertion without chest pain; however, she has no history of loss of consciousness. Her appetite has decreased. The patient has lost about 11 lb (5 kg) over a period of 6 months.\nShe has experienced some hair loss, but no vitiligo has been noted. She also reports a history of nasal obstruction, sneezing, and postnasal drip, but she has not had hemoptysis. She has no history of joint swelling or pain. Additionally, she has not had any eye pain or decreased vision, but she has had difficulty in performing her routine activities such as going to the bathroom because of dizziness and weakness. She generally remains in bed.\nThe patient also reports dysmenorrhea. She has a history of polymenorrhagia but has had amenorrhea for the last year. She remains anxious and depressed. She has no known allergies, does not smoke, drink alcohol, or use illicit drugs, and she is not currently on any regular medication. She is unmarried, has no sexual contacts, and belongs to a middle-class family. She has no history of blood transfusion. The family history is significant for 2 siblings with similar presentations from early childhood. Her parents are alive and healthy.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "17-Year-Old With Hair Loss, Dysmenorrhea, Thrush, and Diarrhea"
},
{
"authors": "Syeda Sabahat Mansur, MB BS; Fardidullah Shah, MB BS",
"content": [
"Upon physical examination, she is an alert, thin, pale, dehydrated female. She has a regular pulse of 96 beats/min, a respiratory rate of 14 breaths/min, a temperature of 98.2oF (36.7oC) and a blood pressure of 75/40 mm Hg while supine (she does exhibit a 45 mm Hg systolic pressure with nil diastolic pressure on standing). The patient weighs 87.6 lb (37 kg).",
"No jaundice is noted. Hyperpigmentation of the skin is seen, most prominently in the palmar creases, digits of both upper and lower limbs, lips, and oral mucosa (see Figure 1).",
"Figure 1.",
"Angular stomatitis is apparent on inspection of the oral cavity, with a smooth, glossy tongue. White patches consistent with thrush are also seen (see Figure 2).",
"Figure 2.",
"Her neck is supple and without lymphadenopathy, her trachea is midline, and she has a normal jugular venous pulse. No bruises, petechiae, or evidence of bleeding, cutaneous nodules, or abnormal movements of the limbs are noted. Peripheral edema is absent. The heart examination reveals normal S1 and S2 sounds without murmur. Her chest auscultation is normal. Upon abdominal examination, no tenderness or visceromegaly are detected, and her bowel sounds are normal.",
"Laboratory investigations reveal a serum hemoglobin level of 8.7 g/dL, with a mean corpuscular volume of 68 fL, a platelet count of 348,000/μL (reference range, 150,000-450,000/μL) and a white blood cell count of 3980/μL (reference range, 4,500-10,000/μL). Her eosinophil levels are at 3% (within the normal range). Peripheral blood films show evidence of hypochromic microcytic anemia. The patient also has multifactorial iron-deficiency anemia (nutritional, gastritis, menorrhagia).",
"The erythrocyte sedimentation rate is 30 mm/hr. Her serum iron is measured at 20 µg/dL (reference range, 26-170 µg/dL), serum ferritin levels are 10 ng/mL (reference range, 12-160 ng/mL), and total iron binding capacity is 580 µg/dL (reference range, 262-474 µg/dL). Vitamin B12 levels are normal, serum glucose is measured at 65 mg/dL, and renal function and liver function test results are normal. Her sodium level is 140 mEq/L, potassium level is 5.6 mEq/L (high), serum urea level is 60 mg/dL (high), and serum creatinine level is 1 mg/dL. An ECG reveals no abnormalities.",
"Although urinalysis shows 2+ leukocytes, culture and sensitivities are normal. Blood cultures and sensitivity testing remain negative. The arterial blood gas is normal. The anti-transglutaminase antibody (anti-TTG) test shows an immunoglobulin A (IgA) level of 6.1 μ/mL (reference range, < 7 μ/mL) and an immunoglobulin G (IgG) level of 6.2 μ/mL (reference range,< 15 μ/mL; borderline, 15-17 μ/mL; elevated, > 17 μ/mL).",
"Serum cortisol measured in the evening is 0.11 μg/dL (reference range, 1.7-16.6 μg/dL) and again in the morning is 4.2 μg/dL (reference range, 6-23 μg/dL). In addition, her adrenocorticotropin (ACTH) level is 75.8 pg/mL (reference range,< 46 pg/mL), her thyroid-stimulating hormone level (TSH) is 3.5 mIU/L (reference range, 0.5-4.70 mIU/L), triiodothyronine (T3) level is 4.4 pmol/L (reference range, 3.5-6.5 pmol/L), thyroxine (T4) level is 18.7 pmol/L (reference range, 10-23 pmol/L), luteinizing hormone level is 1.17 mIU/mL (reference range, 0.5-9.0 mIU/mL), follicle-stimulating hormone (FSH) level is 4.72 mIU/mL (reference range, 3-10 mIU/mL), and parathyroid hormone (PTH) level is 58 pg/mL (reference range, 16-87 pg/mL).",
"A swab taken from the oral mucosa reveals Candida albicans. Chest radiography, abdominal and pelvic ultrasonography, and barium follow-through findings are all normal."
],
"date": "March 15, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/746/588/746588-thumb2.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/746/588/746588-thumb1.png"
}
],
"markdown": "# 17-Year-Old With Hair Loss, Dysmenorrhea, Thrush, and Diarrhea\n\n **Authors:** Syeda Sabahat Mansur, MB BS; Fardidullah Shah, MB BS \n **Date:** March 15, 2022\n\n ## Content\n\n Upon physical examination, she is an alert, thin, pale, dehydrated female. She has a regular pulse of 96 beats/min, a respiratory rate of 14 breaths/min, a temperature of 98.2oF (36.7oC) and a blood pressure of 75/40 mm Hg while supine (she does exhibit a 45 mm Hg systolic pressure with nil diastolic pressure on standing). The patient weighs 87.6 lb (37 kg).\nNo jaundice is noted. Hyperpigmentation of the skin is seen, most prominently in the palmar creases, digits of both upper and lower limbs, lips, and oral mucosa (see Figure 1).\nFigure 1.\nAngular stomatitis is apparent on inspection of the oral cavity, with a smooth, glossy tongue. White patches consistent with thrush are also seen (see Figure 2).\nFigure 2.\nHer neck is supple and without lymphadenopathy, her trachea is midline, and she has a normal jugular venous pulse. No bruises, petechiae, or evidence of bleeding, cutaneous nodules, or abnormal movements of the limbs are noted. Peripheral edema is absent. The heart examination reveals normal S1 and S2 sounds without murmur. Her chest auscultation is normal. Upon abdominal examination, no tenderness or visceromegaly are detected, and her bowel sounds are normal.\nLaboratory investigations reveal a serum hemoglobin level of 8.7 g/dL, with a mean corpuscular volume of 68 fL, a platelet count of 348,000/μL (reference range, 150,000-450,000/μL) and a white blood cell count of 3980/μL (reference range, 4,500-10,000/μL). Her eosinophil levels are at 3% (within the normal range). Peripheral blood films show evidence of hypochromic microcytic anemia. The patient also has multifactorial iron-deficiency anemia (nutritional, gastritis, menorrhagia).\nThe erythrocyte sedimentation rate is 30 mm/hr. Her serum iron is measured at 20 µg/dL (reference range, 26-170 µg/dL), serum ferritin levels are 10 ng/mL (reference range, 12-160 ng/mL), and total iron binding capacity is 580 µg/dL (reference range, 262-474 µg/dL). Vitamin B12 levels are normal, serum glucose is measured at 65 mg/dL, and renal function and liver function test results are normal. Her sodium level is 140 mEq/L, potassium level is 5.6 mEq/L (high), serum urea level is 60 mg/dL (high), and serum creatinine level is 1 mg/dL. An ECG reveals no abnormalities.\nAlthough urinalysis shows 2+ leukocytes, culture and sensitivities are normal. Blood cultures and sensitivity testing remain negative. The arterial blood gas is normal. The anti-transglutaminase antibody (anti-TTG) test shows an immunoglobulin A (IgA) level of 6.1 μ/mL (reference range, < 7 μ/mL) and an immunoglobulin G (IgG) level of 6.2 μ/mL (reference range,< 15 μ/mL; borderline, 15-17 μ/mL; elevated, > 17 μ/mL).\nSerum cortisol measured in the evening is 0.11 μg/dL (reference range, 1.7-16.6 μg/dL) and again in the morning is 4.2 μg/dL (reference range, 6-23 μg/dL). In addition, her adrenocorticotropin (ACTH) level is 75.8 pg/mL (reference range,< 46 pg/mL), her thyroid-stimulating hormone level (TSH) is 3.5 mIU/L (reference range, 0.5-4.70 mIU/L), triiodothyronine (T3) level is 4.4 pmol/L (reference range, 3.5-6.5 pmol/L), thyroxine (T4) level is 18.7 pmol/L (reference range, 10-23 pmol/L), luteinizing hormone level is 1.17 mIU/mL (reference range, 0.5-9.0 mIU/mL), follicle-stimulating hormone (FSH) level is 4.72 mIU/mL (reference range, 3-10 mIU/mL), and parathyroid hormone (PTH) level is 58 pg/mL (reference range, 16-87 pg/mL).\nA swab taken from the oral mucosa reveals Candida albicans. Chest radiography, abdominal and pelvic ultrasonography, and barium follow-through findings are all normal.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 417751,
"choiceText": "Anorexia nervosa",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417752,
"choiceText": "Abdominal tuberculosis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417753,
"choiceText": "Addison disease (AD)",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417754,
"choiceText": "Polyglandular failure (type I)",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417755,
"choiceText": "Polyglandular failure (type II)",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 122956,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "17-Year-Old With Hair Loss, Dysmenorrhea, Thrush, and Diarrhea"
},
{
"authors": "Syeda Sabahat Mansur, MB BS; Fardidullah Shah, MB BS",
"content": [
"This patient's diagnosis of polyglandular failure type I was made on the basis of her peculiar clinical presentation (her history of oral ulcers, hyperpigmentation, postural drop in blood pressure, and significant family history) and the pertinent laboratory findings of decreased cortisol levels, elevated adrenocorticotropin level, and evidence of candidiasis on oral mucosal swab.",
"Polyglandular autoimmune syndromes (PGA) are rare immune endocrinopathies characterized by the coexistence of at least 2 endocrine gland insufficiencies that are based on autoimmune mechanisms. Associations with nonendocrine immune diseases also occur.[1] PGA can be classified as type I (PGA-I) and type II (PGA-II), which is more common and is also known as Schmidt syndrome. A third type (type III) occurs in adults and does not affect the adrenal cortex, but does include 2 of the following: thyroid deficiency, pernicious anemia, type 1A diabetes mellitus, vitiligo, and alopecia.[2]",
"PGA-I is also known by the terms autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy (APECED), Whitaker syndrome,[2] and autoimmune polyendocrine syndrome. It is a rare autosomal-recessive disorder that first manifests in early childhood and results in tissue-specific multiorgan autoimmunity, leading to decreased functioning of multiple glands. Endocrine organs such as the adrenal cortex, ovaries, and parathyroid glands are typically affected, which results in various clinical presentations, including hypocortisolism, hypoaldosteronism, delayed puberty, premature ovarian failure, and hypoparathyroidism with life-threatening hypocalcemia. PGA-I is clinically defined as the presence of at least 2 components of the classic triad of hypoparathyroidism, adrenal insufficiency, and mucocutaneous candidiasis.[3,4] HIV infection should also be considered in patients with oral candidiasis and adrenal insufficiency.",
"Chronic mucocutaneous candidiasis (CMC) generally occurs earlier than the other presentations of this syndrome and is the most frequently encountered of the 3 main diseases of PGA-I. It can appear as early as the first month of life or at any time up to 21 years of age, with the incidence peaking during early childhood. CMC is present in 73%-100% of those with PGA-I. Chronic hypoparathyroidism is the first endocrine disease to occur during the course of the disease, usually after CMC and before AD, and it usually occurs when the patient is less than 10 years of age.[2] AD is usually the third condition to manifest, usually between 6 months and 41 years of age, with a peak around the age of 13 years. AD occurs in 60%-100% of cases of autoimmune polyglandular syndrome-1.[5]"
],
"date": "March 15, 2022",
"figures": [],
"markdown": "# 17-Year-Old With Hair Loss, Dysmenorrhea, Thrush, and Diarrhea\n\n **Authors:** Syeda Sabahat Mansur, MB BS; Fardidullah Shah, MB BS \n **Date:** March 15, 2022\n\n ## Content\n\n This patient's diagnosis of polyglandular failure type I was made on the basis of her peculiar clinical presentation (her history of oral ulcers, hyperpigmentation, postural drop in blood pressure, and significant family history) and the pertinent laboratory findings of decreased cortisol levels, elevated adrenocorticotropin level, and evidence of candidiasis on oral mucosal swab.\nPolyglandular autoimmune syndromes (PGA) are rare immune endocrinopathies characterized by the coexistence of at least 2 endocrine gland insufficiencies that are based on autoimmune mechanisms. Associations with nonendocrine immune diseases also occur.[1] PGA can be classified as type I (PGA-I) and type II (PGA-II), which is more common and is also known as Schmidt syndrome. A third type (type III) occurs in adults and does not affect the adrenal cortex, but does include 2 of the following: thyroid deficiency, pernicious anemia, type 1A diabetes mellitus, vitiligo, and alopecia.[2]\nPGA-I is also known by the terms autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy (APECED), Whitaker syndrome,[2] and autoimmune polyendocrine syndrome. It is a rare autosomal-recessive disorder that first manifests in early childhood and results in tissue-specific multiorgan autoimmunity, leading to decreased functioning of multiple glands. Endocrine organs such as the adrenal cortex, ovaries, and parathyroid glands are typically affected, which results in various clinical presentations, including hypocortisolism, hypoaldosteronism, delayed puberty, premature ovarian failure, and hypoparathyroidism with life-threatening hypocalcemia. PGA-I is clinically defined as the presence of at least 2 components of the classic triad of hypoparathyroidism, adrenal insufficiency, and mucocutaneous candidiasis.[3,4] HIV infection should also be considered in patients with oral candidiasis and adrenal insufficiency.\nChronic mucocutaneous candidiasis (CMC) generally occurs earlier than the other presentations of this syndrome and is the most frequently encountered of the 3 main diseases of PGA-I. It can appear as early as the first month of life or at any time up to 21 years of age, with the incidence peaking during early childhood. CMC is present in 73%-100% of those with PGA-I. Chronic hypoparathyroidism is the first endocrine disease to occur during the course of the disease, usually after CMC and before AD, and it usually occurs when the patient is less than 10 years of age.[2] AD is usually the third condition to manifest, usually between 6 months and 41 years of age, with a peak around the age of 13 years. AD occurs in 60%-100% of cases of autoimmune polyglandular syndrome-1.[5]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 417751,
"choiceText": "Anorexia nervosa",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417752,
"choiceText": "Abdominal tuberculosis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417753,
"choiceText": "Addison disease (AD)",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417754,
"choiceText": "Polyglandular failure (type I)",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417755,
"choiceText": "Polyglandular failure (type II)",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 122956,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "17-Year-Old With Hair Loss, Dysmenorrhea, Thrush, and Diarrhea"
},
{
"authors": "Syeda Sabahat Mansur, MB BS; Fardidullah Shah, MB BS",
"content": [
"Patients with PGA-I often have gastrointestinal manifestations such as autoimmune gastritis, autoimmune hepatitis, and malabsorption. Hyposplenism and asplenia are also common unexplained features.[6] In many cases, dental enamel hypoplasia, keratoconjunctivitis, vitiligo, alopecia, nail pitting, and/or tympanic membrane calcifications are also present. Most patients will exhibit 3-7 different manifestations early in the course of the disease, but other components may appear throughout life.[7,8]",
"PGA-I is a very rare disorder. In Finland, where the highest number of cases of PGA-I have been reported, the estimated prevalence is about 1 in 25,000 inhabitants. In the majority of cases, the syndrome occurs in childhood. The female-to-male ratio varies in different reports from 0.8-1.5. In Italy, only a few case reports have been described to date.[5]",
"Patients with PGA-I have loss-of-function mutations in the autoimmune regulator gene, located on chromosome 21q22.3.[9,10] Patients with PGA-I have demonstrable circulating antibodies directed against a wide range of self-antigens, most with a restricted tissue distribution corresponding to the affected organs. The majority of patients have antibodies against enzymes involved in the steroid biosynthesis and hepatic metabolism of xenobiotics.[4] Because a large variation in phenotype and presentation has been recognized (even in siblings), the traditional clinical definition does not identify all patients.[11] Mutational analysis of the AIRE gene (eg, R257X mutation) may help in identifying such patients with atypical presentations.[12]",
"The clinical presentation of PGA component diseases is often preceded by an asymptomatic latent period of months or years characterized by the presence of circulating disease-associated antibodies. Autoantibodies are useful markers for predicting the development of PGA. The absence of these antibodies does not exclude the disease because not all patients show positive antibodies. The present long-term follow-up data emphasize that the detection of these antibodies facilitates early diagnosis of autoimmune endocrine disorders. In view of the possible long time interval between manifestation of the first autoimmune endocrinopathies and subsequent manifestations, regular and long-term observation of patients with autoimmune endocrine disorders seems necessary.",
"For patients with monoglandular autoimmune endocrinopathy, functional screening for PGA is recommended once every 3 years until age 75 years. If pathologic findings of a second autoimmune endocrine disease are noted, measurement of organ-specific autoantibodies should be added. Furthermore, functional screening for autoimmune endocrine diseases of first-degree relatives of patients with newly diagnosed PGA may also be done. Serologic testing for the presence of diabetes-associated antibodies should especially be considered in the offspring of patients with type 1 diabetes. According to the literature, genetic screening may only be useful in PGA-I.[1]"
],
"date": "March 15, 2022",
"figures": [],
"markdown": "# 17-Year-Old With Hair Loss, Dysmenorrhea, Thrush, and Diarrhea\n\n **Authors:** Syeda Sabahat Mansur, MB BS; Fardidullah Shah, MB BS \n **Date:** March 15, 2022\n\n ## Content\n\n Patients with PGA-I often have gastrointestinal manifestations such as autoimmune gastritis, autoimmune hepatitis, and malabsorption. Hyposplenism and asplenia are also common unexplained features.[6] In many cases, dental enamel hypoplasia, keratoconjunctivitis, vitiligo, alopecia, nail pitting, and/or tympanic membrane calcifications are also present. Most patients will exhibit 3-7 different manifestations early in the course of the disease, but other components may appear throughout life.[7,8]\nPGA-I is a very rare disorder. In Finland, where the highest number of cases of PGA-I have been reported, the estimated prevalence is about 1 in 25,000 inhabitants. In the majority of cases, the syndrome occurs in childhood. The female-to-male ratio varies in different reports from 0.8-1.5. In Italy, only a few case reports have been described to date.[5]\nPatients with PGA-I have loss-of-function mutations in the autoimmune regulator gene, located on chromosome 21q22.3.[9,10] Patients with PGA-I have demonstrable circulating antibodies directed against a wide range of self-antigens, most with a restricted tissue distribution corresponding to the affected organs. The majority of patients have antibodies against enzymes involved in the steroid biosynthesis and hepatic metabolism of xenobiotics.[4] Because a large variation in phenotype and presentation has been recognized (even in siblings), the traditional clinical definition does not identify all patients.[11] Mutational analysis of the AIRE gene (eg, R257X mutation) may help in identifying such patients with atypical presentations.[12]\nThe clinical presentation of PGA component diseases is often preceded by an asymptomatic latent period of months or years characterized by the presence of circulating disease-associated antibodies. Autoantibodies are useful markers for predicting the development of PGA. The absence of these antibodies does not exclude the disease because not all patients show positive antibodies. The present long-term follow-up data emphasize that the detection of these antibodies facilitates early diagnosis of autoimmune endocrine disorders. In view of the possible long time interval between manifestation of the first autoimmune endocrinopathies and subsequent manifestations, regular and long-term observation of patients with autoimmune endocrine disorders seems necessary.\nFor patients with monoglandular autoimmune endocrinopathy, functional screening for PGA is recommended once every 3 years until age 75 years. If pathologic findings of a second autoimmune endocrine disease are noted, measurement of organ-specific autoantibodies should be added. Furthermore, functional screening for autoimmune endocrine diseases of first-degree relatives of patients with newly diagnosed PGA may also be done. Serologic testing for the presence of diabetes-associated antibodies should especially be considered in the offspring of patients with type 1 diabetes. According to the literature, genetic screening may only be useful in PGA-I.[1]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "17-Year-Old With Hair Loss, Dysmenorrhea, Thrush, and Diarrhea"
},
{
"authors": "Syeda Sabahat Mansur, MB BS; Fardidullah Shah, MB BS",
"content": [
"After diagnosis, patients with PGA-1 require close monitoring. Monitoring can help prevent illness associated with the delayed diagnosis of additional autoimmune diseases (eg, AD and hypoparathyroidism, which can develop during adulthood), as well as oral cancer (which may develop if candidiasis is not treated aggressively) and infection caused by asplenism, which is present in a subgroup of patients.[13]",
"At present, the treatment of polyendocrine autoimmune syndromes is dictated by the treatment of the individual disorders and usually includes lifelong hormone replacement therapy for affected organs as well as close monitoring of the rest of the endocrine organs because they can also become affected. Knowledge of the syndromes allows early therapy of component disorders.[13]",
"Thyroxine treatment for hypothyroidism increases the basal metabolic rate and therefore the body's requirement for cortisol; treating such cases of hypothyroidism can precipitate an episode of Addisonian crisis in a patient with undiagnosed adrenal insufficiency in the setting of PGA. CMC usually requires lifelong antifungal therapy, usually a topical one. It can also respond to systemic therapy, such as fluconazole or ketoconazole.[2] Reports from several Hungarian studies have shown a good response to therapy with cyclosporin.[14,15,16]",
"The patient in this case was hospitalized and adequate hydration was given. A local antifungal was provided for the thrush, and iron was multivitamins were given. She was placed on oral steroids after initially receiving intravenous steroids. The patient and her parents were educated and counseled about the disease, its treatment, follow-up, and the side effects of treatment.",
"At her first follow-up visit 10 days after being discharged from the hospital, the patient had greatly improved both subjectively and objectively. The patient's vital signs were within normal limits, with a regular pulse of 86 beats/min and blood pressure of 110-120/70-80 mm Hg. She had marked improvement in her dizziness and no longer complained of abdominal pain or vomiting. Her thrush had disappeared, and she had gained 1.1- 2.2 lb (0.5 -1 kg) over the span of 10 days. Her hemoglobin level improved to 11.70 gm/dL."
],
"date": "March 15, 2022",
"figures": [],
"markdown": "# 17-Year-Old With Hair Loss, Dysmenorrhea, Thrush, and Diarrhea\n\n **Authors:** Syeda Sabahat Mansur, MB BS; Fardidullah Shah, MB BS \n **Date:** March 15, 2022\n\n ## Content\n\n After diagnosis, patients with PGA-1 require close monitoring. Monitoring can help prevent illness associated with the delayed diagnosis of additional autoimmune diseases (eg, AD and hypoparathyroidism, which can develop during adulthood), as well as oral cancer (which may develop if candidiasis is not treated aggressively) and infection caused by asplenism, which is present in a subgroup of patients.[13]\nAt present, the treatment of polyendocrine autoimmune syndromes is dictated by the treatment of the individual disorders and usually includes lifelong hormone replacement therapy for affected organs as well as close monitoring of the rest of the endocrine organs because they can also become affected. Knowledge of the syndromes allows early therapy of component disorders.[13]\nThyroxine treatment for hypothyroidism increases the basal metabolic rate and therefore the body's requirement for cortisol; treating such cases of hypothyroidism can precipitate an episode of Addisonian crisis in a patient with undiagnosed adrenal insufficiency in the setting of PGA. CMC usually requires lifelong antifungal therapy, usually a topical one. It can also respond to systemic therapy, such as fluconazole or ketoconazole.[2] Reports from several Hungarian studies have shown a good response to therapy with cyclosporin.[14,15,16]\nThe patient in this case was hospitalized and adequate hydration was given. A local antifungal was provided for the thrush, and iron was multivitamins were given. She was placed on oral steroids after initially receiving intravenous steroids. The patient and her parents were educated and counseled about the disease, its treatment, follow-up, and the side effects of treatment.\nAt her first follow-up visit 10 days after being discharged from the hospital, the patient had greatly improved both subjectively and objectively. The patient's vital signs were within normal limits, with a regular pulse of 86 beats/min and blood pressure of 110-120/70-80 mm Hg. She had marked improvement in her dizziness and no longer complained of abdominal pain or vomiting. Her thrush had disappeared, and she had gained 1.1- 2.2 lb (0.5 -1 kg) over the span of 10 days. Her hemoglobin level improved to 11.70 gm/dL.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 417756,
"choiceText": "For the diagnosis of PGA-I, the patient should have AD, hypoparathyroidism, and evidence of mucocutaneous candidiasis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417757,
"choiceText": "For the diagnosis of PGA-I, the patient should have at least 2 components of the typical triad of AD, hypoparathyroidism, and evidence of mucocutaneous candidiasis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417758,
"choiceText": "A finding of organ-specific antibodies in the presence of 2 components of the typical triad is essential for the diagnosis of PGA-I",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417759,
"choiceText": "Organ-specific antibodies are essential for the diagnosis of PGA-I",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417760,
"choiceText": "The presence of hypoparathyroidism is required for the diagnosis of PGA-I",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The diagnosis of PGA-I is made on the basis of the clinical findings. The classic triad for this condition includes AD, hypoparathyroidism, and mucocutaneous candidiasis. At least 2 of these 3 disorders must be present to establish the diagnosis. ",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 122957,
"questionText": "Which statement about PGA-I is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 417761,
"choiceText": "If you treat the mucosal fungal infection adequately, patients do not require further management",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417762,
"choiceText": "Treatment of PGA-I only requires short-term antifungal medications and rehydration therapy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417763,
"choiceText": "PGA-I requires lifelong treatment of the manifestations of the disorders",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417764,
"choiceText": "Treatment with thyroxine is good for the AD component of PGA-I ",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "After diagnosis, patients with PGA type I require close monitoring for life as well as treatment for each of the component disorders. They usually require lifelong antifungal therapy for the thrush, which if untreated, can lead to oral carcinoma. Moreover, they often need lifelong hormone replacement therapy to compensate for the organ deficiencies of the disorder. Thyroxine, in fact, can precipitate an Addison crisis because it increases the need for cortisol, for which the deficient adrenal glands cannot compensate.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 122958,
"questionText": "Which of the following statements concerning the management of PGA-I is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "17-Year-Old With Hair Loss, Dysmenorrhea, Thrush, and Diarrhea"
},
{
"authors": "Syeda Sabahat Mansur, MB BS; Fardidullah Shah, MB BS",
"content": [],
"date": "March 15, 2022",
"figures": [],
"markdown": "# 17-Year-Old With Hair Loss, Dysmenorrhea, Thrush, and Diarrhea\n\n **Authors:** Syeda Sabahat Mansur, MB BS; Fardidullah Shah, MB BS \n **Date:** March 15, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 417756,
"choiceText": "For the diagnosis of PGA-I, the patient should have AD, hypoparathyroidism, and evidence of mucocutaneous candidiasis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417757,
"choiceText": "For the diagnosis of PGA-I, the patient should have at least 2 components of the typical triad of AD, hypoparathyroidism, and evidence of mucocutaneous candidiasis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417758,
"choiceText": "A finding of organ-specific antibodies in the presence of 2 components of the typical triad is essential for the diagnosis of PGA-I",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417759,
"choiceText": "Organ-specific antibodies are essential for the diagnosis of PGA-I",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417760,
"choiceText": "The presence of hypoparathyroidism is required for the diagnosis of PGA-I",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The diagnosis of PGA-I is made on the basis of the clinical findings. The classic triad for this condition includes AD, hypoparathyroidism, and mucocutaneous candidiasis. At least 2 of these 3 disorders must be present to establish the diagnosis. ",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 122957,
"questionText": "Which statement about PGA-I is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 417761,
"choiceText": "If you treat the mucosal fungal infection adequately, patients do not require further management",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417762,
"choiceText": "Treatment of PGA-I only requires short-term antifungal medications and rehydration therapy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417763,
"choiceText": "PGA-I requires lifelong treatment of the manifestations of the disorders",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417764,
"choiceText": "Treatment with thyroxine is good for the AD component of PGA-I ",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "After diagnosis, patients with PGA type I require close monitoring for life as well as treatment for each of the component disorders. They usually require lifelong antifungal therapy for the thrush, which if untreated, can lead to oral carcinoma. Moreover, they often need lifelong hormone replacement therapy to compensate for the organ deficiencies of the disorder. Thyroxine, in fact, can precipitate an Addison crisis because it increases the need for cortisol, for which the deficient adrenal glands cannot compensate.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 122958,
"questionText": "Which of the following statements concerning the management of PGA-I is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "17-Year-Old With Hair Loss, Dysmenorrhea, Thrush, and Diarrhea"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 417751,
"choiceText": "Anorexia nervosa",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417752,
"choiceText": "Abdominal tuberculosis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417753,
"choiceText": "Addison disease (AD)",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417754,
"choiceText": "Polyglandular failure (type I)",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417755,
"choiceText": "Polyglandular failure (type II)",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 122956,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 417756,
"choiceText": "For the diagnosis of PGA-I, the patient should have AD, hypoparathyroidism, and evidence of mucocutaneous candidiasis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417757,
"choiceText": "For the diagnosis of PGA-I, the patient should have at least 2 components of the typical triad of AD, hypoparathyroidism, and evidence of mucocutaneous candidiasis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417758,
"choiceText": "A finding of organ-specific antibodies in the presence of 2 components of the typical triad is essential for the diagnosis of PGA-I",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417759,
"choiceText": "Organ-specific antibodies are essential for the diagnosis of PGA-I",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417760,
"choiceText": "The presence of hypoparathyroidism is required for the diagnosis of PGA-I",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The diagnosis of PGA-I is made on the basis of the clinical findings. The classic triad for this condition includes AD, hypoparathyroidism, and mucocutaneous candidiasis. At least 2 of these 3 disorders must be present to establish the diagnosis. ",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 122957,
"questionText": "Which statement about PGA-I is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 417761,
"choiceText": "If you treat the mucosal fungal infection adequately, patients do not require further management",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417762,
"choiceText": "Treatment of PGA-I only requires short-term antifungal medications and rehydration therapy",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417763,
"choiceText": "PGA-I requires lifelong treatment of the manifestations of the disorders",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 417764,
"choiceText": "Treatment with thyroxine is good for the AD component of PGA-I ",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "After diagnosis, patients with PGA type I require close monitoring for life as well as treatment for each of the component disorders. They usually require lifelong antifungal therapy for the thrush, which if untreated, can lead to oral carcinoma. Moreover, they often need lifelong hormone replacement therapy to compensate for the organ deficiencies of the disorder. Thyroxine, in fact, can precipitate an Addison crisis because it increases the need for cortisol, for which the deficient adrenal glands cannot compensate.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 122958,
"questionText": "Which of the following statements concerning the management of PGA-I is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
968988 | /viewarticle/968988 | [
{
"authors": "Guillaume Davido, MD",
"content": [
"A 35-year-old man found by firefighters has had a cardiac arrest. He presented with a Glasgow Coma Scale (GCS) score of 6 and symmetrical miosis in both eyes. Naloxone 4 mg is administered, which causes him to wake up. Paramedics then bring him to the emergency department for monitoring. It's difficult to get information from the patient because he is agitated, insulting healthcare staff, and demanding to be discharged against medical advice. Skin examination reveals track marks on his forearms.",
"His companion explains that she found him sprawled across his bed, unconscious. According to her, the only things in his medical history are alcohol dependence, from which he has been weaned, and an anxiety–depressive disorder, which has been successfully treated.",
"The patient is afebrile, and the clinical exam is normal except for bradypnea (6 breaths/minute). ECG showed no abnormalities."
],
"date": "March 09, 2022",
"figures": [],
"markdown": "# Case Report: Cardiac Arrest in a Man Who Has Overdosed\n\n **Authors:** Guillaume Davido, MD \n **Date:** March 09, 2022\n\n ## Content\n\n A 35-year-old man found by firefighters has had a cardiac arrest. He presented with a Glasgow Coma Scale (GCS) score of 6 and symmetrical miosis in both eyes. Naloxone 4 mg is administered, which causes him to wake up. Paramedics then bring him to the emergency department for monitoring. It's difficult to get information from the patient because he is agitated, insulting healthcare staff, and demanding to be discharged against medical advice. Skin examination reveals track marks on his forearms.\nHis companion explains that she found him sprawled across his bed, unconscious. According to her, the only things in his medical history are alcohol dependence, from which he has been weaned, and an anxiety–depressive disorder, which has been successfully treated.\nThe patient is afebrile, and the clinical exam is normal except for bradypnea (6 breaths/minute). ECG showed no abnormalities.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1665647,
"choiceText": "Tricyclic antidepressant poisoning",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1665648,
"choiceText": "Alcohol poisoning",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1665649,
"choiceText": "Opioid poisoning",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1665650,
"choiceText": "Cocaine intoxication",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1665651,
"choiceText": "Digitalis poisoning",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 4,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 536372,
"questionText": "What do you think explains the cardiac arrest?",
"questionTypeId": 1,
"required": true,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Case Report: Cardiac Arrest in a Man Who Has Overdosed"
},
{
"authors": "Guillaume Davido, MD",
"content": [
"The patient's medical history and condition point to opioid poisoning. This young man, who has psychiatric and addictive comorbidities, experienced cardiac arrest, responded to an opioid antagonist medication (naloxone), and had symmetrical miosis in both eyes. In addition, the patient has track marks (suggesting IV injections of substances such as methadone or heroin). Waking up agitated after the administration of naloxone is an antagonizing effect that can be explained by the presence of opioids in the patient's system.",
"Because the ECG is normal, we can rule out other types of poisoning, such as that caused by tricyclic antidepressants (which elevates the risk for a membrane stabilizing effect on the ECG), digitalis (which elevates the risk for arrhythmia and conduction disturbances on the ECG), or cocaine (which elevates the risk for acute coronary syndrome).",
"Finally, there's not much to suggest acute alcohol poisoning (for example, there is no smell of alcohol on the patient's breath, and he is currently withdrawing from alcohol dependence).",
"When the patient fully regains consciousness — his GCS score is 15/15 — his diagnosis is confirmed. He tells you that he doesn't understand what happened to him, because — he admits — he's been opioid-dependent for a long time and hasn't made any recent changes to his opioid use. However, he informs you that he was just discharged from the hospital — where he had been for several weeks after experiencing a fracture — and that he stopped all substance use during that period."
],
"date": "March 09, 2022",
"figures": [],
"markdown": "# Case Report: Cardiac Arrest in a Man Who Has Overdosed\n\n **Authors:** Guillaume Davido, MD \n **Date:** March 09, 2022\n\n ## Content\n\n The patient's medical history and condition point to opioid poisoning. This young man, who has psychiatric and addictive comorbidities, experienced cardiac arrest, responded to an opioid antagonist medication (naloxone), and had symmetrical miosis in both eyes. In addition, the patient has track marks (suggesting IV injections of substances such as methadone or heroin). Waking up agitated after the administration of naloxone is an antagonizing effect that can be explained by the presence of opioids in the patient's system.\nBecause the ECG is normal, we can rule out other types of poisoning, such as that caused by tricyclic antidepressants (which elevates the risk for a membrane stabilizing effect on the ECG), digitalis (which elevates the risk for arrhythmia and conduction disturbances on the ECG), or cocaine (which elevates the risk for acute coronary syndrome).\nFinally, there's not much to suggest acute alcohol poisoning (for example, there is no smell of alcohol on the patient's breath, and he is currently withdrawing from alcohol dependence).\nWhen the patient fully regains consciousness — his GCS score is 15/15 — his diagnosis is confirmed. He tells you that he doesn't understand what happened to him, because — he admits — he's been opioid-dependent for a long time and hasn't made any recent changes to his opioid use. However, he informs you that he was just discharged from the hospital — where he had been for several weeks after experiencing a fracture — and that he stopped all substance use during that period.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1665647,
"choiceText": "Tricyclic antidepressant poisoning",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1665648,
"choiceText": "Alcohol poisoning",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1665649,
"choiceText": "Opioid poisoning",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1665650,
"choiceText": "Cocaine intoxication",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1665651,
"choiceText": "Digitalis poisoning",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 4,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 536372,
"questionText": "What do you think explains the cardiac arrest?",
"questionTypeId": 1,
"required": true,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Case Report: Cardiac Arrest in a Man Who Has Overdosed"
},
{
"authors": "Guillaume Davido, MD",
"content": [
"Keeping the patient on naloxone depends on whether there was opioid poisoning. If a long-acting opioid is involved, such as a high dose of methadone or heroin, it's better to institute several hours of monitoring with a continuous IV infusion of naloxone to prevent remorphinization.",
"There is nothing to indicate that the patient should be intubated, given that naloxone brought the patient back to full consciousness in an emergency setting.",
"Because track marks indicate that the patient has used IV substances, an infectious disease panel is recommended. Although the clinical exam doesn't point to any infection, it's common for one to precipitate the risk for overdose, even if patients control their intake of substances. However, what probably precipitated this overdose is the fact that the patient had abstained for several weeks before he abruptly resumed using.",
"A psychiatric evaluation is not indicated. This was a case of accidental, unintentional poisoning, and the patient's companion said that she hadn't seen any deterioration in terms of his mental health.",
"Finally, there is nothing to suggest that emergency opioid substitution therapy should be initiated, particularly as a way to prevent the recurrence of intoxication. That treatment, which reduces risk in opioid-dependent patients, should be prescribed only after a sufficient amount of time has passed since the patient's last opioid dose, and after the patient has given consent. It does not stabilize patients suffering from acute opioid poisoning.",
"The patient is discharged and you don't seen him for 6 months. Then one day, you find him back in the emergency department with flu-like symptoms. He's afraid that he has COVID because, for a few hours, he's been shivering and feeling asthenic (to the point of yawning), and experiencing severe rhinorrhea associated with profuse sweating, lacrimation, myalgia, and severe diarrhea. He has a slight fever (37.8 °C), his blood pressure is 140/90 mm Hg, and his heart rate indicates tachycardia (100 beats/minute). He tells you that he's trying to stay clean, he's just found a job, and he's proud of himself because he hasn't used in a little over 3 days."
],
"date": "March 09, 2022",
"figures": [],
"markdown": "# Case Report: Cardiac Arrest in a Man Who Has Overdosed\n\n **Authors:** Guillaume Davido, MD \n **Date:** March 09, 2022\n\n ## Content\n\n Keeping the patient on naloxone depends on whether there was opioid poisoning. If a long-acting opioid is involved, such as a high dose of methadone or heroin, it's better to institute several hours of monitoring with a continuous IV infusion of naloxone to prevent remorphinization.\nThere is nothing to indicate that the patient should be intubated, given that naloxone brought the patient back to full consciousness in an emergency setting.\nBecause track marks indicate that the patient has used IV substances, an infectious disease panel is recommended. Although the clinical exam doesn't point to any infection, it's common for one to precipitate the risk for overdose, even if patients control their intake of substances. However, what probably precipitated this overdose is the fact that the patient had abstained for several weeks before he abruptly resumed using.\nA psychiatric evaluation is not indicated. This was a case of accidental, unintentional poisoning, and the patient's companion said that she hadn't seen any deterioration in terms of his mental health.\nFinally, there is nothing to suggest that emergency opioid substitution therapy should be initiated, particularly as a way to prevent the recurrence of intoxication. That treatment, which reduces risk in opioid-dependent patients, should be prescribed only after a sufficient amount of time has passed since the patient's last opioid dose, and after the patient has given consent. It does not stabilize patients suffering from acute opioid poisoning.\nThe patient is discharged and you don't seen him for 6 months. Then one day, you find him back in the emergency department with flu-like symptoms. He's afraid that he has COVID because, for a few hours, he's been shivering and feeling asthenic (to the point of yawning), and experiencing severe rhinorrhea associated with profuse sweating, lacrimation, myalgia, and severe diarrhea. He has a slight fever (37.8 °C), his blood pressure is 140/90 mm Hg, and his heart rate indicates tachycardia (100 beats/minute). He tells you that he's trying to stay clean, he's just found a job, and he's proud of himself because he hasn't used in a little over 3 days.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1664786,
"choiceText": "Keep the patient on a continuous IV infusion of naloxone in case he's been poisoned with a long-acting opioid like methadone",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664787,
"choiceText": "Perform orotracheal intubation to prevent further respiratory distress",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664788,
"choiceText": "Suggest that the patient undergo serology testing for HIV, HBV, and HCV",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664789,
"choiceText": "Recommend emergency psychiatric evaluation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664790,
"choiceText": "Start opioid substitution therapy to prevent further respiratory distress",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 2,
"displayType": 2,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 536108,
"questionText": "How do you treat this patient? <i>(You can select more than one answer.)</i>",
"questionTypeId": 1,
"required": true,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Case Report: Cardiac Arrest in a Man Who Has Overdosed"
},
{
"authors": "Guillaume Davido, MD",
"content": [
"Of course, we can't exclude any of these diagnoses, but considering the context, the most likely diagnosis is opioid withdrawal.",
"All of the usual symptoms of opioid withdrawal are present (which include mydriasis, tremors, nausea, and \"psychiatric\" signs, such as anxiety, depressive disorder, insomnia, irritability, and panic attacks). Lab tests sometimes show hemoconcentration with hyperleukocytosis and hyperglycemia. The symptoms of opioid withdrawal can start within hours of the last dose and generally last a week."
],
"date": "March 09, 2022",
"figures": [],
"markdown": "# Case Report: Cardiac Arrest in a Man Who Has Overdosed\n\n **Authors:** Guillaume Davido, MD \n **Date:** March 09, 2022\n\n ## Content\n\n Of course, we can't exclude any of these diagnoses, but considering the context, the most likely diagnosis is opioid withdrawal.\nAll of the usual symptoms of opioid withdrawal are present (which include mydriasis, tremors, nausea, and \"psychiatric\" signs, such as anxiety, depressive disorder, insomnia, irritability, and panic attacks). Lab tests sometimes show hemoconcentration with hyperleukocytosis and hyperglycemia. The symptoms of opioid withdrawal can start within hours of the last dose and generally last a week.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1665652,
"choiceText": "Bacterial infection at the injection site",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1665653,
"choiceText": "COVID-19",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1665654,
"choiceText": "Viral gastroenteritis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1665655,
"choiceText": "Depressive disorder",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1665656,
"choiceText": "Opioid withdrawal",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 6,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 536373,
"questionText": "Which is the most likely diagnosis?",
"questionTypeId": 1,
"required": true,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Case Report: Cardiac Arrest in a Man Who Has Overdosed"
},
{
"authors": "Guillaume Davido, MD",
"content": [
"All of the answers are correct. There's a bidirectional relationship between addictions and psychiatric disorders. For example, depressive disorders can be secondary to substance use, or they can be primary, just like addictive disorders; often, alcohol helps a person stay in control as they're \"coming down\" after taking opioids, and opioids make it possible to cope with the depression that can set in after the consumption of alcohol.",
"Infectious complications are commonly related to IV injections (such as cellulitis, lymphangitis, abscess, hepatic viral infections, HIV, bacterial endocarditis, and candida infections of the eyes or joints). ENT complications can arise when a person snorts drugs, because inhaling cocaine or any other substance through the nose increases the risk for sinusitis or nasal septum perforation."
],
"date": "March 09, 2022",
"figures": [],
"markdown": "# Case Report: Cardiac Arrest in a Man Who Has Overdosed\n\n **Authors:** Guillaume Davido, MD \n **Date:** March 09, 2022\n\n ## Content\n\n All of the answers are correct. There's a bidirectional relationship between addictions and psychiatric disorders. For example, depressive disorders can be secondary to substance use, or they can be primary, just like addictive disorders; often, alcohol helps a person stay in control as they're \"coming down\" after taking opioids, and opioids make it possible to cope with the depression that can set in after the consumption of alcohol.\nInfectious complications are commonly related to IV injections (such as cellulitis, lymphangitis, abscess, hepatic viral infections, HIV, bacterial endocarditis, and candida infections of the eyes or joints). ENT complications can arise when a person snorts drugs, because inhaling cocaine or any other substance through the nose increases the risk for sinusitis or nasal septum perforation.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1664841,
"choiceText": "Antisocial personality disorder",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664842,
"choiceText": "Co-occurring alcohol addiction",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664843,
"choiceText": "Infectious complications",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664844,
"choiceText": "ENT complications",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664845,
"choiceText": "Depressive disorder",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 4,
"displayType": 2,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 536133,
"questionText": "What are the main comorbidities and complications in opioid-dependent patients? <i>(You can select more than one answer.)</i>",
"questionTypeId": 1,
"required": true,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Case Report: Cardiac Arrest in a Man Who Has Overdosed"
},
{
"authors": "Guillaume Davido, MD",
"content": [
"All of the answers are correct. In the case of opioid withdrawal, we're mostly treating the symptoms. Opioid or anxiolytic analgesics (benzodiazepines) are contraindicated in these patients because of the risk for polysubstance dependence.",
"Opioid substitution therapy could be helpful, but it's not essential. The patient must be showing signs of withdrawal, or a sufficient amount of time must have passed since the last opioid dose (at least 10 hours for methadone and 4 hours for buprenorphine). Such therapy can reduce the possibility of harm related to opioids bought on the black market, used syringes, medicalized addiction, and split dispensing. In addition, buprenorphine can reduce the likelihood of an overdose and buprenorphine/naloxone (Suboxone) does not require IV administration. Ideally, the patient should be given opioid substitution therapy in an addiction treatment, support, and prevention center.",
"This article originally appeared in the French edition of Medscape.",
"Follow Medscape on Facebook, Twitter, Instagram, and YouTube"
],
"date": "March 09, 2022",
"figures": [],
"markdown": "# Case Report: Cardiac Arrest in a Man Who Has Overdosed\n\n **Authors:** Guillaume Davido, MD \n **Date:** March 09, 2022\n\n ## Content\n\n All of the answers are correct. In the case of opioid withdrawal, we're mostly treating the symptoms. Opioid or anxiolytic analgesics (benzodiazepines) are contraindicated in these patients because of the risk for polysubstance dependence.\nOpioid substitution therapy could be helpful, but it's not essential. The patient must be showing signs of withdrawal, or a sufficient amount of time must have passed since the last opioid dose (at least 10 hours for methadone and 4 hours for buprenorphine). Such therapy can reduce the possibility of harm related to opioids bought on the black market, used syringes, medicalized addiction, and split dispensing. In addition, buprenorphine can reduce the likelihood of an overdose and buprenorphine/naloxone (Suboxone) does not require IV administration. Ideally, the patient should be given opioid substitution therapy in an addiction treatment, support, and prevention center.\nThis article originally appeared in the French edition of Medscape.\nFollow Medscape on Facebook, Twitter, Instagram, and YouTube\n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1664965,
"choiceText": "Antispasmodics/antidiarrheals",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664966,
"choiceText": "Antihistamines or antipsychotics that have an anxiolytic effect",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664967,
"choiceText": "Analgesics (acetaminophen)",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664968,
"choiceText": "Opioid substitution therapy",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664969,
"choiceText": "Specialized care in an addiction treatment, support, and prevention center",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 5,
"displayType": 2,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 536160,
"questionText": "What treatment do you recommend for this patient? <i>(You can select more than one answer.) </i>",
"questionTypeId": 1,
"required": true,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Case Report: Cardiac Arrest in a Man Who Has Overdosed"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1665647,
"choiceText": "Tricyclic antidepressant poisoning",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1665648,
"choiceText": "Alcohol poisoning",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1665649,
"choiceText": "Opioid poisoning",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1665650,
"choiceText": "Cocaine intoxication",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1665651,
"choiceText": "Digitalis poisoning",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 4,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 536372,
"questionText": "What do you think explains the cardiac arrest?",
"questionTypeId": 1,
"required": true,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1664786,
"choiceText": "Keep the patient on a continuous IV infusion of naloxone in case he's been poisoned with a long-acting opioid like methadone",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664787,
"choiceText": "Perform orotracheal intubation to prevent further respiratory distress",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664788,
"choiceText": "Suggest that the patient undergo serology testing for HIV, HBV, and HCV",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664789,
"choiceText": "Recommend emergency psychiatric evaluation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664790,
"choiceText": "Start opioid substitution therapy to prevent further respiratory distress",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 2,
"displayType": 2,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 536108,
"questionText": "How do you treat this patient? <i>(You can select more than one answer.)</i>",
"questionTypeId": 1,
"required": true,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1665652,
"choiceText": "Bacterial infection at the injection site",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1665653,
"choiceText": "COVID-19",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1665654,
"choiceText": "Viral gastroenteritis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1665655,
"choiceText": "Depressive disorder",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1665656,
"choiceText": "Opioid withdrawal",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 6,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 536373,
"questionText": "Which is the most likely diagnosis?",
"questionTypeId": 1,
"required": true,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1664841,
"choiceText": "Antisocial personality disorder",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664842,
"choiceText": "Co-occurring alcohol addiction",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664843,
"choiceText": "Infectious complications",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664844,
"choiceText": "ENT complications",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664845,
"choiceText": "Depressive disorder",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 4,
"displayType": 2,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 536133,
"questionText": "What are the main comorbidities and complications in opioid-dependent patients? <i>(You can select more than one answer.)</i>",
"questionTypeId": 1,
"required": true,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1664965,
"choiceText": "Antispasmodics/antidiarrheals",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664966,
"choiceText": "Antihistamines or antipsychotics that have an anxiolytic effect",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664967,
"choiceText": "Analgesics (acetaminophen)",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664968,
"choiceText": "Opioid substitution therapy",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664969,
"choiceText": "Specialized care in an addiction treatment, support, and prevention center",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 5,
"displayType": 2,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 536160,
"questionText": "What treatment do you recommend for this patient? <i>(You can select more than one answer.) </i>",
"questionTypeId": 1,
"required": true,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
869215 | /viewarticle/869215 | [
{
"authors": "Djamil Fertikh, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 66-year-old man presents to his primary care physician complaining of bilateral, palpable, nontender neck masses. The patient states that the lesions first appeared about 2 months ago and have been progressing. He reports no recent viral infection, fever, chills, or any other associated systemic symptoms.",
"The patient's medical and surgical history is only remarkable for type 2 diabetes. He has not had any illicit drug use. The patient works as an accountant and lives in an apartment with his mother and two younger sisters. No pets live in the home."
],
"date": "March 02, 2022",
"figures": [],
"markdown": "# Primary Care Case Challenge: An Accountant With Bilateral Neck Masses\n\n **Authors:** Djamil Fertikh, MD \n **Date:** March 02, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 66-year-old man presents to his primary care physician complaining of bilateral, palpable, nontender neck masses. The patient states that the lesions first appeared about 2 months ago and have been progressing. He reports no recent viral infection, fever, chills, or any other associated systemic symptoms.\nThe patient's medical and surgical history is only remarkable for type 2 diabetes. He has not had any illicit drug use. The patient works as an accountant and lives in an apartment with his mother and two younger sisters. No pets live in the home.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Primary Care Case Challenge: An Accountant With Bilateral Neck Masses"
},
{
"authors": "Djamil Fertikh, MD",
"content": [
"Upon physical examination, the patient is not in any apparent discomfort. His oral temperature is 95.6°F (35.3°C). His pulse has a regular sinus rhythm and a rate of 89 beats/min. His blood pressure is 150/78 mm Hg. No skin color changes or cutaneous drainage are noted. Close examination of the patient's head and neck reveals bilateral, palpable, nontender neck masses with no evidence of fixation to the adjacent soft tissues.",
"Examination of the oral cavity shows poor dental hygiene; multiple dental caries are observed. Auscultation of the neck, including over the lesions, reveals no bruits. Examination of the patient's axillary and inguinal regions is unremarkable. His lungs are clear upon bilateral auscultation, and normal respiratory effort is noted. His abdomen is soft and not tender to deep palpation in the epigastric region. No organomegaly is detected. Rectal examination reveals normal muscle tone and guaiac-negative stool. Peripheral arterial pulses in the lower extremities are palpable and symmetric.",
"His laboratory workup, including a complete blood cell (CBC) count, shows a normal white blood cell (WBC) count; however, a hypochromic, microcytic anemia is noted. The patient's erythrocyte sedimentation rate (ESR) is mildly elevated. A basic metabolic panel is within normal limits. A contrast-enhanced CT scan of the neck is performed (Figures 1 and 2).",
"Figure 1.",
"Figure 2."
],
"date": "March 02, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/869/215/869215-thumb-1.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/869/215/869215-thumb-2.jpg"
}
],
"markdown": "# Primary Care Case Challenge: An Accountant With Bilateral Neck Masses\n\n **Authors:** Djamil Fertikh, MD \n **Date:** March 02, 2022\n\n ## Content\n\n Upon physical examination, the patient is not in any apparent discomfort. His oral temperature is 95.6°F (35.3°C). His pulse has a regular sinus rhythm and a rate of 89 beats/min. His blood pressure is 150/78 mm Hg. No skin color changes or cutaneous drainage are noted. Close examination of the patient's head and neck reveals bilateral, palpable, nontender neck masses with no evidence of fixation to the adjacent soft tissues.\nExamination of the oral cavity shows poor dental hygiene; multiple dental caries are observed. Auscultation of the neck, including over the lesions, reveals no bruits. Examination of the patient's axillary and inguinal regions is unremarkable. His lungs are clear upon bilateral auscultation, and normal respiratory effort is noted. His abdomen is soft and not tender to deep palpation in the epigastric region. No organomegaly is detected. Rectal examination reveals normal muscle tone and guaiac-negative stool. Peripheral arterial pulses in the lower extremities are palpable and symmetric.\nHis laboratory workup, including a complete blood cell (CBC) count, shows a normal white blood cell (WBC) count; however, a hypochromic, microcytic anemia is noted. The patient's erythrocyte sedimentation rate (ESR) is mildly elevated. A basic metabolic panel is within normal limits. A contrast-enhanced CT scan of the neck is performed (Figures 1 and 2).\nFigure 1.\nFigure 2.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1018882,
"choiceText": "Thyroid cancer",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018884,
"choiceText": "Scrofula",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018886,
"choiceText": "Cervicofacial lymphangioma",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018888,
"choiceText": "Cat scratch disease",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 322465,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Primary Care Case Challenge: An Accountant With Bilateral Neck Masses"
},
{
"authors": "Djamil Fertikh, MD",
"content": [
"In this case, a contrast-enhanced CT scan showed multiple bilateral, rim-enhancing, irregular lesions with hypodense centers, which is consistent with necrotic lymph nodes (Figures 1 and 2). A hypodense right thyroid gland lesion was incidentally noted. The differential diagnosis for necrotic lymph nodes includes metastatic squamous cell carcinoma, metastatic thyroid carcinoma, mycobacterial infection, and treated lymphoma.",
"Figure 1.",
"Figure 2.",
"Because the patient had a thyroid nodule, metastatic thyroid neoplasm was the initial working diagnosis, so ultrasonography-guided fine-needle aspiration of one of the nodes was performed. The initial results showed no evidence of malignant cells; however, they were positive for acid-fast bacilli. A screening CT scan of the chest revealed multiple bilateral nodules, with enlarged bilateral hilar nodes; this finding is consistent with tuberculosis (TB). A subsequent right cervical node aspirate was positive for pansensitive Mycobacterium tuberculosis.",
"M tuberculosis is an obligate, aerobic, nonspore-forming rod. Humans act as its sole reservoir, and it continues to be a major health problem worldwide. Nearly one-third of the global population (ie, 2 billion people) is infected with M tuberculosis and is at risk of developing the disease. An estimated 10 million people develop active TB every year; of those, about 1.5 million die. The vast majority of global TB cases and deaths occur in the developing world.",
"Patient-to-patient transmission typically occurs through the inhalation of small aerosols and, in most cases, the disease is confined to the respiratory system. It can, however, affect any organ system, particularly in immunocompromised individuals, where it can involve multiple extrapulmonary sites, including the skeleton, gastrointestinal tract, genitourinary tract, and central nervous system. After a period of replication within the lungs, dissemination occurs—through the lymphatic and circulatory systems—to extrapulmonary sites, including the cervical lymph nodes.",
"In the adult population, most nodal diseases are caused by M tuberculosis; the remaining cases are caused by atypical Mycobacterium or nontuberculous Mycobacterium (NTM). In the United States, most cases affecting children are caused by NTM, and most of those are the result of Mycobacterium avium complex, which is typically considered a surgical disease. Since the 1940s, when antituberculosis antibiotics were first developed, the general prevalence of TB has declined. However, since the mid-1980s, there has been a resurgence in TB, which is related to the AIDS epidemic, to the increase in immigration from developing countries, and to the increase in the number of drug-resistant strains of M tuberculosis.[1,2,3,4,5,6,7]"
],
"date": "March 02, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/869/215/869215-thumb-1.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/869/215/869215-thumb-2.jpg"
}
],
"markdown": "# Primary Care Case Challenge: An Accountant With Bilateral Neck Masses\n\n **Authors:** Djamil Fertikh, MD \n **Date:** March 02, 2022\n\n ## Content\n\n In this case, a contrast-enhanced CT scan showed multiple bilateral, rim-enhancing, irregular lesions with hypodense centers, which is consistent with necrotic lymph nodes (Figures 1 and 2). A hypodense right thyroid gland lesion was incidentally noted. The differential diagnosis for necrotic lymph nodes includes metastatic squamous cell carcinoma, metastatic thyroid carcinoma, mycobacterial infection, and treated lymphoma.\nFigure 1.\nFigure 2.\nBecause the patient had a thyroid nodule, metastatic thyroid neoplasm was the initial working diagnosis, so ultrasonography-guided fine-needle aspiration of one of the nodes was performed. The initial results showed no evidence of malignant cells; however, they were positive for acid-fast bacilli. A screening CT scan of the chest revealed multiple bilateral nodules, with enlarged bilateral hilar nodes; this finding is consistent with tuberculosis (TB). A subsequent right cervical node aspirate was positive for pansensitive Mycobacterium tuberculosis.\nM tuberculosis is an obligate, aerobic, nonspore-forming rod. Humans act as its sole reservoir, and it continues to be a major health problem worldwide. Nearly one-third of the global population (ie, 2 billion people) is infected with M tuberculosis and is at risk of developing the disease. An estimated 10 million people develop active TB every year; of those, about 1.5 million die. The vast majority of global TB cases and deaths occur in the developing world.\nPatient-to-patient transmission typically occurs through the inhalation of small aerosols and, in most cases, the disease is confined to the respiratory system. It can, however, affect any organ system, particularly in immunocompromised individuals, where it can involve multiple extrapulmonary sites, including the skeleton, gastrointestinal tract, genitourinary tract, and central nervous system. After a period of replication within the lungs, dissemination occurs—through the lymphatic and circulatory systems—to extrapulmonary sites, including the cervical lymph nodes.\nIn the adult population, most nodal diseases are caused by M tuberculosis; the remaining cases are caused by atypical Mycobacterium or nontuberculous Mycobacterium (NTM). In the United States, most cases affecting children are caused by NTM, and most of those are the result of Mycobacterium avium complex, which is typically considered a surgical disease. Since the 1940s, when antituberculosis antibiotics were first developed, the general prevalence of TB has declined. However, since the mid-1980s, there has been a resurgence in TB, which is related to the AIDS epidemic, to the increase in immigration from developing countries, and to the increase in the number of drug-resistant strains of M tuberculosis.[1,2,3,4,5,6,7]\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1018882,
"choiceText": "Thyroid cancer",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018884,
"choiceText": "Scrofula",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018886,
"choiceText": "Cervicofacial lymphangioma",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018888,
"choiceText": "Cat scratch disease",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 322465,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Primary Care Case Challenge: An Accountant With Bilateral Neck Masses"
},
{
"authors": "Djamil Fertikh, MD",
"content": [
"Evidence suggests that M tuberculosis has been present since antiquity. The mummy of Nesperhan, a priest of the Egyptian god Amun, revealed ventral destruction of the lower thoracic spine that led to the gibbus formation typical of spinal TB. \"Scrofula\" is an old term, initially used to describe chronic lesions of the head and neck that today are believed to have likely been related TB infection. In 1882, Robert Koch discovered a staining technique that enabled him to isolate the tubercle bacillus and establish TB as an infectious disease.",
"Head and neck TB is often difficult to diagnose clinically, and it is seldom suspected by clinicians. It is frequently confused for a neoplastic process (as it was in this case), which results in a treatment delay. About 15% of cases of extrapulmonary TB manifest in the head and neck, as do about 1.5% of all new cases of TB. Tuberculous lymphadenitis causes rubbery, painless enlargement of the cervical lymph nodes, usually bilateral; most commonly, the posterior cervical chain is also involved. Lung involvement is encountered most often, with lower nodal involvement. If left untreated, the nodes can ulcerate, producing draining sores. Fever, chills, sweats, and weight loss have been reported in about 20% of individuals. Complications of head and neck disease include scar formation in a draining fistula of the neck, especially after biopsy.[3,8,9]",
"A chest radiograph reveals associated active or healed TB in around 40% to 70% of cases. CT scanning and MRI are the most common imaging studies used to identify head and neck pathology. On both MRI and CT scans, during the initial stage of the disease, the involved nodes are homogeneous before and after the administration of intravenous contrast medium. The nodes then undergo central necrosis, which is represented histologically by caseating material. This translates into central low density on CT scans, which corresponds to a central hypointense signal on T1-weighted images and a hyperintense signal on T2-weighted MRI scans. Uniform or nodular peripheral rim enhancement, reflecting granulation tissue with inflammatory hypervascularity, is almost always encountered with both modes of imaging. The enhancing rim might show signal hypointensity on T2-weighted images. The main differential includes metastatic disease from head and neck squamous cell carcinoma, treated lymphoma, and non-nodal lesions (such as an infected branchial cleft cyst). The affected nodes can become calcified later in the course of the disease.[1,6]",
"Mantoux skin testing using purified protein derivative (PPD) is generally the first line of investigation, and approximately 85% of patients develop a skin induration larger than 10 mm (a positive test). Typically, 5 units of PPD are injected into the skin, and if a raised bump larger than 5 mm (0.2 in) appears at the site 48 hours later, the test could be positive, depending on specific criteria. A positive Mantoux skin test indicates infection with M tuberculosis, but it does not indicate the activity of the infection. Anergy to the test can occur with immunosuppressed patients.[1,3] Two interferon-gamma release assays (IGRAs) are also approved by the US Food and Drug Administration (FDA) to aid in diagnosing M tuberculosis infection. Both QuantiFERON-TB Gold In-Tube test (QFT-GIT) and T-SPOT do not help differentiate latent TB infection from TB disease but can be used to measure a patient’s immune reactivity to M tuberculosis.[10,11,12,13]",
"Fine-needle aspiration—with CT guidance or, most often, ultrasonographic guidance—is usually the first diagnostic investigation performed; it has a reported sensitivity of 77% and specificity of 93%. Biopsies are not usually recommended, because they can spread the disease and result in sinus formation. The most reliable diagnostic criteria are the presence of stainable acid-fast bacilli and cultured organisms. Caseating granulomas are considered highly suggestive but not definitive, and cultures can take 4 to 6 weeks to grow.[3,4,5]"
],
"date": "March 02, 2022",
"figures": [],
"markdown": "# Primary Care Case Challenge: An Accountant With Bilateral Neck Masses\n\n **Authors:** Djamil Fertikh, MD \n **Date:** March 02, 2022\n\n ## Content\n\n Evidence suggests that M tuberculosis has been present since antiquity. The mummy of Nesperhan, a priest of the Egyptian god Amun, revealed ventral destruction of the lower thoracic spine that led to the gibbus formation typical of spinal TB. \"Scrofula\" is an old term, initially used to describe chronic lesions of the head and neck that today are believed to have likely been related TB infection. In 1882, Robert Koch discovered a staining technique that enabled him to isolate the tubercle bacillus and establish TB as an infectious disease.\nHead and neck TB is often difficult to diagnose clinically, and it is seldom suspected by clinicians. It is frequently confused for a neoplastic process (as it was in this case), which results in a treatment delay. About 15% of cases of extrapulmonary TB manifest in the head and neck, as do about 1.5% of all new cases of TB. Tuberculous lymphadenitis causes rubbery, painless enlargement of the cervical lymph nodes, usually bilateral; most commonly, the posterior cervical chain is also involved. Lung involvement is encountered most often, with lower nodal involvement. If left untreated, the nodes can ulcerate, producing draining sores. Fever, chills, sweats, and weight loss have been reported in about 20% of individuals. Complications of head and neck disease include scar formation in a draining fistula of the neck, especially after biopsy.[3,8,9]\nA chest radiograph reveals associated active or healed TB in around 40% to 70% of cases. CT scanning and MRI are the most common imaging studies used to identify head and neck pathology. On both MRI and CT scans, during the initial stage of the disease, the involved nodes are homogeneous before and after the administration of intravenous contrast medium. The nodes then undergo central necrosis, which is represented histologically by caseating material. This translates into central low density on CT scans, which corresponds to a central hypointense signal on T1-weighted images and a hyperintense signal on T2-weighted MRI scans. Uniform or nodular peripheral rim enhancement, reflecting granulation tissue with inflammatory hypervascularity, is almost always encountered with both modes of imaging. The enhancing rim might show signal hypointensity on T2-weighted images. The main differential includes metastatic disease from head and neck squamous cell carcinoma, treated lymphoma, and non-nodal lesions (such as an infected branchial cleft cyst). The affected nodes can become calcified later in the course of the disease.[1,6]\nMantoux skin testing using purified protein derivative (PPD) is generally the first line of investigation, and approximately 85% of patients develop a skin induration larger than 10 mm (a positive test). Typically, 5 units of PPD are injected into the skin, and if a raised bump larger than 5 mm (0.2 in) appears at the site 48 hours later, the test could be positive, depending on specific criteria. A positive Mantoux skin test indicates infection with M tuberculosis, but it does not indicate the activity of the infection. Anergy to the test can occur with immunosuppressed patients.[1,3] Two interferon-gamma release assays (IGRAs) are also approved by the US Food and Drug Administration (FDA) to aid in diagnosing M tuberculosis infection. Both QuantiFERON-TB Gold In-Tube test (QFT-GIT) and T-SPOT do not help differentiate latent TB infection from TB disease but can be used to measure a patient’s immune reactivity to M tuberculosis.[10,11,12,13]\nFine-needle aspiration—with CT guidance or, most often, ultrasonographic guidance—is usually the first diagnostic investigation performed; it has a reported sensitivity of 77% and specificity of 93%. Biopsies are not usually recommended, because they can spread the disease and result in sinus formation. The most reliable diagnostic criteria are the presence of stainable acid-fast bacilli and cultured organisms. Caseating granulomas are considered highly suggestive but not definitive, and cultures can take 4 to 6 weeks to grow.[3,4,5]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Primary Care Case Challenge: An Accountant With Bilateral Neck Masses"
},
{
"authors": "Djamil Fertikh, MD",
"content": [
"With proper treatment, recovery is usually complete. Antibiotic regimens for the treatment of pulmonary infection can be used for TB lymphadenitis. The disease is slow to develop and slow to respond to medical therapy. Antibiotics must be taken for at least 6 months, and longer courses can be required. If the treatment is prematurely discontinued, recurrence of the disease is usually the result.",
"Different treatment regimens are available, but the most common involves of an initial empiric four-drug combination that typically consists of isoniazid, rifampin, pyrazinamide, and ethambutol. After sensitivities return, two drugs are continued for 6 months. According to the World Health Organization, the first 2 months of TB therapy should be directly observed by an independent observer (usually, a healthcare worker who watches patients swallow their medications). When short-course directly observed therapy (DOT) is properly implemented, the success rate is over 95%, which prevents the emergence of new multidrug-resistant strains of TB. Depending on the drugs used, complications associated with treatment include thrombocytopenia, neuropathy, vertigo, fever, hepatitis, itching, and rash.[7]",
"Surgical treatment is typically reserved for cases in which medical treatment fails. About 25% of household contacts acquire the infection, so the close friends and family of patients may need to undergo skin testing and/or chest radiography.[5]",
"Initial treatment for the 66-year-old man described in this case consisted of 2 months of DOT with isoniazid 300 mg, rifampin 600 mg, pyrazinamide 1500 mg, and pyridoxine 50 mg. The patient reported a mild tingling sensation in his fingers during this phase, but it eventually subsided. After 2 months, he reported feeling significantly better overall, and his weight rose from 151 lb to 164 lb. His contacts underwent Mantoux skin testing, and all were negative. The continuation phase of his DOT treatment consisted of isoniazid 900 mg, rifampin 600 mg, and pyridoxine 50 mg administered twice weekly for 36 weeks. At follow-up, the patient's sputum cultures were negative."
],
"date": "March 02, 2022",
"figures": [],
"markdown": "# Primary Care Case Challenge: An Accountant With Bilateral Neck Masses\n\n **Authors:** Djamil Fertikh, MD \n **Date:** March 02, 2022\n\n ## Content\n\n With proper treatment, recovery is usually complete. Antibiotic regimens for the treatment of pulmonary infection can be used for TB lymphadenitis. The disease is slow to develop and slow to respond to medical therapy. Antibiotics must be taken for at least 6 months, and longer courses can be required. If the treatment is prematurely discontinued, recurrence of the disease is usually the result.\nDifferent treatment regimens are available, but the most common involves of an initial empiric four-drug combination that typically consists of isoniazid, rifampin, pyrazinamide, and ethambutol. After sensitivities return, two drugs are continued for 6 months. According to the World Health Organization, the first 2 months of TB therapy should be directly observed by an independent observer (usually, a healthcare worker who watches patients swallow their medications). When short-course directly observed therapy (DOT) is properly implemented, the success rate is over 95%, which prevents the emergence of new multidrug-resistant strains of TB. Depending on the drugs used, complications associated with treatment include thrombocytopenia, neuropathy, vertigo, fever, hepatitis, itching, and rash.[7]\nSurgical treatment is typically reserved for cases in which medical treatment fails. About 25% of household contacts acquire the infection, so the close friends and family of patients may need to undergo skin testing and/or chest radiography.[5]\nInitial treatment for the 66-year-old man described in this case consisted of 2 months of DOT with isoniazid 300 mg, rifampin 600 mg, pyrazinamide 1500 mg, and pyridoxine 50 mg. The patient reported a mild tingling sensation in his fingers during this phase, but it eventually subsided. After 2 months, he reported feeling significantly better overall, and his weight rose from 151 lb to 164 lb. His contacts underwent Mantoux skin testing, and all were negative. The continuation phase of his DOT treatment consisted of isoniazid 900 mg, rifampin 600 mg, and pyridoxine 50 mg administered twice weekly for 36 weeks. At follow-up, the patient's sputum cultures were negative.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1018890,
"choiceText": "5%",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018892,
"choiceText": "15%",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018894,
"choiceText": "25%",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018896,
"choiceText": "50%",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "About 15% of cases of extrapulmonary TB manifest in the head and neck, as do about 1.5% of all new cases of TB.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 322467,
"questionText": "What percentage of cases of extrapulmonary tuberculosis occur in the head and neck?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1018898,
"choiceText": "PPD results always indicate active disease",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018900,
"choiceText": "PPD can indicate an exposure to <i>M tuberculosis</i>",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018902,
"choiceText": "A raised bump > 3 mm after PPD administration indicates a positive result",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018904,
"choiceText": "Mantoux skin testing using PPD is only indicated for confirmatory testing, as opposed to first-line investigation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Mantoux skin testing using PPD is generally the first line of investigation and can indicate exposure to <em>M tuberculosis.</em> Approximately 85% of patients develop a skin induration larger than 10 mm (a positive test). Typically, 5 units of PPD are injected into the skin. If a raised bump larger than 5 mm (0.2 in) appears at the site 48 hours later, the test may be positive, depending on specific criteria. A positive Mantoux skin test indicates infection with <em>M tuberculosis,</em> but it does not indicate the activity of the infection. In addition, anergy to the test can occur with immunosuppressed patients.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 322469,
"questionText": "Which of the following statements about positive PPD testing is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Primary Care Case Challenge: An Accountant With Bilateral Neck Masses"
},
{
"authors": "Djamil Fertikh, MD",
"content": [],
"date": "March 02, 2022",
"figures": [],
"markdown": "# Primary Care Case Challenge: An Accountant With Bilateral Neck Masses\n\n **Authors:** Djamil Fertikh, MD \n **Date:** March 02, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1018890,
"choiceText": "5%",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018892,
"choiceText": "15%",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018894,
"choiceText": "25%",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018896,
"choiceText": "50%",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "About 15% of cases of extrapulmonary TB manifest in the head and neck, as do about 1.5% of all new cases of TB.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 322467,
"questionText": "What percentage of cases of extrapulmonary tuberculosis occur in the head and neck?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1018898,
"choiceText": "PPD results always indicate active disease",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018900,
"choiceText": "PPD can indicate an exposure to <i>M tuberculosis</i>",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018902,
"choiceText": "A raised bump > 3 mm after PPD administration indicates a positive result",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018904,
"choiceText": "Mantoux skin testing using PPD is only indicated for confirmatory testing, as opposed to first-line investigation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Mantoux skin testing using PPD is generally the first line of investigation and can indicate exposure to <em>M tuberculosis.</em> Approximately 85% of patients develop a skin induration larger than 10 mm (a positive test). Typically, 5 units of PPD are injected into the skin. If a raised bump larger than 5 mm (0.2 in) appears at the site 48 hours later, the test may be positive, depending on specific criteria. A positive Mantoux skin test indicates infection with <em>M tuberculosis,</em> but it does not indicate the activity of the infection. In addition, anergy to the test can occur with immunosuppressed patients.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 322469,
"questionText": "Which of the following statements about positive PPD testing is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Primary Care Case Challenge: An Accountant With Bilateral Neck Masses"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1018882,
"choiceText": "Thyroid cancer",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018884,
"choiceText": "Scrofula",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018886,
"choiceText": "Cervicofacial lymphangioma",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018888,
"choiceText": "Cat scratch disease",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 322465,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1018890,
"choiceText": "5%",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018892,
"choiceText": "15%",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018894,
"choiceText": "25%",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018896,
"choiceText": "50%",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "About 15% of cases of extrapulmonary TB manifest in the head and neck, as do about 1.5% of all new cases of TB.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 322467,
"questionText": "What percentage of cases of extrapulmonary tuberculosis occur in the head and neck?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1018898,
"choiceText": "PPD results always indicate active disease",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018900,
"choiceText": "PPD can indicate an exposure to <i>M tuberculosis</i>",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018902,
"choiceText": "A raised bump > 3 mm after PPD administration indicates a positive result",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1018904,
"choiceText": "Mantoux skin testing using PPD is only indicated for confirmatory testing, as opposed to first-line investigation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Mantoux skin testing using PPD is generally the first line of investigation and can indicate exposure to <em>M tuberculosis.</em> Approximately 85% of patients develop a skin induration larger than 10 mm (a positive test). Typically, 5 units of PPD are injected into the skin. If a raised bump larger than 5 mm (0.2 in) appears at the site 48 hours later, the test may be positive, depending on specific criteria. A positive Mantoux skin test indicates infection with <em>M tuberculosis,</em> but it does not indicate the activity of the infection. In addition, anergy to the test can occur with immunosuppressed patients.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 322469,
"questionText": "Which of the following statements about positive PPD testing is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
968993 | /viewarticle/968993 | [
{
"authors": "Kanchan Kaur, MBBS, MS(Surg), MRCS(Edin)",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 37-year-old woman presented to a breast clinic with a 5-year history of multiple lumps in her breasts. She had no comorbidities.",
"The patient had undergone surgical excision of benign lumps in both breasts on two occasions during the past 5 years. She had no family history of breast cancer or ovarian cancer. She had two full-term pregnancies.",
"The results of a general physical examination and routine blood tests were unremarkable; however, spotty pigmentation of the skin was noted. A local breast examination revealed very nodular, tender breasts. The largest lumps in both breasts were approximately 40 mm. Scars from previous surgery were visible on the breasts.",
"An ultrasound examination of both breasts showed numerous well-defined isoechoic nodules studded in the breasts. The larger nodules measured up to 4-4.5 cm (Breast Imaging Reporting and Data System [BI-RADS] 4A).",
"Because of the extensive nature of the florid benign breast changes, it was challenging to characterize the multiple lumps on ultrasound examination alone. Hence, a breast contrast-enhanced MRI (CEMRI) was ordered; it showed extensive bilateral BI-RADS 3 lumps, which were suggestive of fibroadenomas (Figure 1).",
"Figure 1.",
"Tru-Cut biopsy of the largest lumps in both breasts was performed, and the diagnosis of fibroadenoma was confirmed. The patient was advised to remain under close follow-up for clinical checkups and serial ultrasounds."
],
"date": "March 01, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/968/993a/968993-Thumb1.png"
}
],
"markdown": "# Oncology Case Challenge: A 37-Year-Old Woman With Multiple Fibroadenomas\n\n **Authors:** Kanchan Kaur, MBBS, MS(Surg), MRCS(Edin) \n **Date:** March 01, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 37-year-old woman presented to a breast clinic with a 5-year history of multiple lumps in her breasts. She had no comorbidities.\nThe patient had undergone surgical excision of benign lumps in both breasts on two occasions during the past 5 years. She had no family history of breast cancer or ovarian cancer. She had two full-term pregnancies.\nThe results of a general physical examination and routine blood tests were unremarkable; however, spotty pigmentation of the skin was noted. A local breast examination revealed very nodular, tender breasts. The largest lumps in both breasts were approximately 40 mm. Scars from previous surgery were visible on the breasts.\nAn ultrasound examination of both breasts showed numerous well-defined isoechoic nodules studded in the breasts. The larger nodules measured up to 4-4.5 cm (Breast Imaging Reporting and Data System [BI-RADS] 4A).\nBecause of the extensive nature of the florid benign breast changes, it was challenging to characterize the multiple lumps on ultrasound examination alone. Hence, a breast contrast-enhanced MRI (CEMRI) was ordered; it showed extensive bilateral BI-RADS 3 lumps, which were suggestive of fibroadenomas (Figure 1).\nFigure 1.\nTru-Cut biopsy of the largest lumps in both breasts was performed, and the diagnosis of fibroadenoma was confirmed. The patient was advised to remain under close follow-up for clinical checkups and serial ultrasounds.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Oncology Case Challenge: A 37-Year-Old Woman With Multiple Fibroadenomas"
},
{
"authors": "Kanchan Kaur, MBBS, MS(Surg), MRCS(Edin)",
"content": [
"After 9 months, the patient returned to the breast clinic and reports the recent onset of inversion of the right nipple. There was no history of nipple discharge, and she was not aware of any change in the size of the palpable bilateral breast lumps.",
"Upon examination, nipple retraction was noted on the right side, with peau d'orange in the surrounding skin of the breast. The skin was not erythematous. Small, mobile lymph nodes were palpable in the right axilla.",
"The patient was advised to undergo mammography, ultrasonography, and breast CEMRI. The mammogram showed marked skin thickening and multiple masses with prominent right axillary nodes (Figures 2-5).",
"Figure 2.",
"Figure 3.",
"Figure 4.",
"Figure 5.",
"Ultrasonography of the right breast revealed numerous well-defined isoechoic to low echogenic nodules; the larger ones measured up to 4-4.5 cm. The nodules were unchanged compared with those seen in both breasts on the previous ultrasound. However, marked internal vascularity is noted, along with marked thickening of the nipple-areola complex (BI-RADS 4B).",
"A breast CEMRI showed innumerable enhancing mass lesions of varying sizes that were scattered throughout both breasts; some of these were conglomerated to form larger masses (Figure 6). As on the patient's previous CEMRI scan, the larger nodule in the right breast upper inner quadrant measured 3.6 × 3.3 cm and the one in the left breast upper inner quadrant measured 3.9 × 2.8 cm. A few nonenhancing cystic lesions were noted in the left breast, which are consistent with simple cysts. Marked skin thickening and edematous changes were visible in the right breast, with nipple retraction. These findings were new as compared with the CEMRI that was performed 9 months earlier.",
"Figure 6."
],
"date": "March 01, 2022",
"figures": [
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/968/993a/968993-Thumb2.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/968/993a/968993-Thumb3.png"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/968/993a/968993-Thumb4.png"
},
{
"caption": "Figure 5.",
"image_url": "https://img.medscapestatic.com/article/968/993a/968993-Thumb5.png"
},
{
"caption": "Figure 6.",
"image_url": "https://img.medscapestatic.com/article/968/993a/968993-Thumb6.png"
}
],
"markdown": "# Oncology Case Challenge: A 37-Year-Old Woman With Multiple Fibroadenomas\n\n **Authors:** Kanchan Kaur, MBBS, MS(Surg), MRCS(Edin) \n **Date:** March 01, 2022\n\n ## Content\n\n After 9 months, the patient returned to the breast clinic and reports the recent onset of inversion of the right nipple. There was no history of nipple discharge, and she was not aware of any change in the size of the palpable bilateral breast lumps.\nUpon examination, nipple retraction was noted on the right side, with peau d'orange in the surrounding skin of the breast. The skin was not erythematous. Small, mobile lymph nodes were palpable in the right axilla.\nThe patient was advised to undergo mammography, ultrasonography, and breast CEMRI. The mammogram showed marked skin thickening and multiple masses with prominent right axillary nodes (Figures 2-5).\nFigure 2.\nFigure 3.\nFigure 4.\nFigure 5.\nUltrasonography of the right breast revealed numerous well-defined isoechoic to low echogenic nodules; the larger ones measured up to 4-4.5 cm. The nodules were unchanged compared with those seen in both breasts on the previous ultrasound. However, marked internal vascularity is noted, along with marked thickening of the nipple-areola complex (BI-RADS 4B).\nA breast CEMRI showed innumerable enhancing mass lesions of varying sizes that were scattered throughout both breasts; some of these were conglomerated to form larger masses (Figure 6). As on the patient's previous CEMRI scan, the larger nodule in the right breast upper inner quadrant measured 3.6 × 3.3 cm and the one in the left breast upper inner quadrant measured 3.9 × 2.8 cm. A few nonenhancing cystic lesions were noted in the left breast, which are consistent with simple cysts. Marked skin thickening and edematous changes were visible in the right breast, with nipple retraction. These findings were new as compared with the CEMRI that was performed 9 months earlier.\nFigure 6.\n\n ## Figures\n\n **Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4.** \n \n\n**Figure 5.** \n \n\n**Figure 6.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1664970,
"choiceText": "Inflammatory breast cancer",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664971,
"choiceText": "Primary breast cancer",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664972,
"choiceText": "Metastasis from another primary site",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664973,
"choiceText": "Malignant phyllodes",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664974,
"choiceText": "Breast lymphoma",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 536161,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Oncology Case Challenge: A 37-Year-Old Woman With Multiple Fibroadenomas"
},
{
"authors": "Kanchan Kaur, MBBS, MS(Surg), MRCS(Edin)",
"content": [
"Multiple bilateral breast lumps are usually fibroadenomas or breast cysts. Both are benign. The incidence of fibroadenomas peaks in the second decade, whereas cysts commonly occur during the fourth and fifth decades in perimenopausal women.",
"Phyllodes tumors are a rare type of breast lump with clinical and imaging features that are very similar to those of fibroadenomas. Histopathologic examination helps differentiate the two conditions. Other less common benign multiple breast lumps include hamartomas, papillomas, adenomas, galactoceles, pseudoangiomatous stromal hyperplasia (PASH), and lipomas.",
"Primary breast cancer may also present as multiple breast lumps, especially lobular carcinoma, which is commonly multifocal. Bilateral multifocal breast cancer is rare and is more likely to occur in patients with lobular carcinoma.",
"Fibroadenomas are by far the most common breast lumps and account for almost half of all breast biopsies. They are present in about 25% of asymptomatic women and are multiple in 20% of cases. Fibroadenomas are innocuous lumps that require active intervention only if they are large or rapidly increase in size. Most can be safely monitored. Most women with simple fibroadenomas do not have a significantly increased risk of developing breast cancer (relative risk [RR] < 2).[1,2]",
"The risk for breast cancer, however, increases in patients who have complex fibroadenomas. These lesions contain other changes, such as sclerosing adenosis, duct epithelial hyperplasia, epithelial calcification, or papillary apocrine changes. Multicentric proliferative changes in the surrounding tissue and fibroadenomas associated with surrounding stromal hyperplasia or atypia pose a higher risk for malignant changes (RR = 4.24). Patients with fibroadenomas who have a strong family history of breast cancer are also at higher risk for malignancy.[1,2]",
"In rare instances, breast cancer develops within a fibroadenoma. The reported incidence ranges from 0.125% to 0.02%.[3,4]",
"When fibroadenomas occur in pubertal girls, they are termed juvenile fibroadenomas. Giant fibroadenomas are larger than 5 cm and are usually encountered in pregnant or lactating women. These fibroadenomas have a tendency to grow rapidly, leading to distortion of the breast with associated skin changes. Although they exhibit an aggressive growth pattern, they are not associated with an increased risk for breast cancer.",
"The exact etiology of fibroadenomas is not clear. They are assumed to be aberrations of normal breast development and are the result of hyperplastic processes, involving glandular and stromal components.",
"Current evidence supports that at least some fibroadenomas are a result of clonal neoplasms linked to recurrent stromal MED12 mutations and RARA mutations.[5] Some mutations may be associated with familial syndromes."
],
"date": "March 01, 2022",
"figures": [],
"markdown": "# Oncology Case Challenge: A 37-Year-Old Woman With Multiple Fibroadenomas\n\n **Authors:** Kanchan Kaur, MBBS, MS(Surg), MRCS(Edin) \n **Date:** March 01, 2022\n\n ## Content\n\n Multiple bilateral breast lumps are usually fibroadenomas or breast cysts. Both are benign. The incidence of fibroadenomas peaks in the second decade, whereas cysts commonly occur during the fourth and fifth decades in perimenopausal women.\nPhyllodes tumors are a rare type of breast lump with clinical and imaging features that are very similar to those of fibroadenomas. Histopathologic examination helps differentiate the two conditions. Other less common benign multiple breast lumps include hamartomas, papillomas, adenomas, galactoceles, pseudoangiomatous stromal hyperplasia (PASH), and lipomas.\nPrimary breast cancer may also present as multiple breast lumps, especially lobular carcinoma, which is commonly multifocal. Bilateral multifocal breast cancer is rare and is more likely to occur in patients with lobular carcinoma.\nFibroadenomas are by far the most common breast lumps and account for almost half of all breast biopsies. They are present in about 25% of asymptomatic women and are multiple in 20% of cases. Fibroadenomas are innocuous lumps that require active intervention only if they are large or rapidly increase in size. Most can be safely monitored. Most women with simple fibroadenomas do not have a significantly increased risk of developing breast cancer (relative risk [RR] < 2).[1,2]\nThe risk for breast cancer, however, increases in patients who have complex fibroadenomas. These lesions contain other changes, such as sclerosing adenosis, duct epithelial hyperplasia, epithelial calcification, or papillary apocrine changes. Multicentric proliferative changes in the surrounding tissue and fibroadenomas associated with surrounding stromal hyperplasia or atypia pose a higher risk for malignant changes (RR = 4.24). Patients with fibroadenomas who have a strong family history of breast cancer are also at higher risk for malignancy.[1,2]\nIn rare instances, breast cancer develops within a fibroadenoma. The reported incidence ranges from 0.125% to 0.02%.[3,4]\nWhen fibroadenomas occur in pubertal girls, they are termed juvenile fibroadenomas. Giant fibroadenomas are larger than 5 cm and are usually encountered in pregnant or lactating women. These fibroadenomas have a tendency to grow rapidly, leading to distortion of the breast with associated skin changes. Although they exhibit an aggressive growth pattern, they are not associated with an increased risk for breast cancer.\nThe exact etiology of fibroadenomas is not clear. They are assumed to be aberrations of normal breast development and are the result of hyperplastic processes, involving glandular and stromal components.\nCurrent evidence supports that at least some fibroadenomas are a result of clonal neoplasms linked to recurrent stromal MED12 mutations and RARA mutations.[5] Some mutations may be associated with familial syndromes.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1664970,
"choiceText": "Inflammatory breast cancer",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664971,
"choiceText": "Primary breast cancer",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664972,
"choiceText": "Metastasis from another primary site",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664973,
"choiceText": "Malignant phyllodes",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664974,
"choiceText": "Breast lymphoma",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 536161,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Oncology Case Challenge: A 37-Year-Old Woman With Multiple Fibroadenomas"
},
{
"authors": "Kanchan Kaur, MBBS, MS(Surg), MRCS(Edin)",
"content": [
"The PTEN mutation leads to increased cell proliferation with decreased apoptosis. PTEN hamartoma tumor syndrome is a family of clinical syndromes characterized by germline mutations in the PTEN gene. This family includes conditions such as Cowden syndrome, which is associated with an increased lifetime cumulative risk of developing cancer in the breast (67%-85%), thyroid (35%), kidney (33%), and endometrium (28%). Benign breast disease, especially multiple fibroadenomas, is common in Cowden syndrome.[6] Li-Fraumeni syndrome, Carney complex, Peutz-Jeghers syndrome, and Beckwith-Wiedemann syndrome are other familial conditions that may be associated with multiple benign or malignant breast lumps as part of a syndrome complex involving multiple other organs.[7,8]",
"Differentiating fibroadenoma from a phyllodes tumor is important. Phyllodes tumors of the breast are rare; fibroepithelial lesions account for less than 1% of all breast tumors. They have a high potential to recur and also carry a 10% risk for malignancy. They can exhibit rapid and tremendous growth, and in neglected cases, skin ulceration can occur owing to the pressure of the growing lump.[9]",
"Phyllodes tumors are subclassified histologically as benign, borderline, or malignant according to features such as stromal overgrowth, tumor necrosis, cellular atypia, and number of mitoses per high-power field. Most phyllodes tumors (35%-64%) are benign.[9]",
"Bilateral multiple phyllodes tumors are very rare. Surgical excision is always indicated for phyllodes tumors even if the biopsy results are benign. In contrast to fibroadenomas, which can be \"scooped out\" during surgery, it is advisable to take a margin of normal breast tissue with phyllodes tumors. The likelihood of recurrence is generally very high, and patients must be counseled accordingly and maintained on close follow-up.",
"Inflammatory breast cancer is a rare form of locally advanced breast cancer (classified as T4d according to tumor, node, metastasis staging). It is a separate clinicopathologic entity in which the classic presentation is that of erythema and edema occupying at least one third of the breast. Patients present with a short history of rapidly increasing inflammation, heaviness, and swelling in the breast, which is often mistaken for infection. An underlying breast lump may not always be palpable. Many patients have lymph node metastasis at presentation. The diffuse tissue edema and parenchymal architectural distortion make the identification of a primary breast lesion more challenging on mammography and ultrasonography. MRI has greater diagnostic value in such patients.",
"Multiple small, confluent, heterogeneously enhancing masses and global skin thickening are key MRI features in such cases. In addition to aiding diagnosis, serial MRI can help monitor the response to chemotherapy.",
"In the absence of an identifiable mass in the breast on imaging, a punch biopsy of the involved skin and a biopsy of the lymph nodes help establish the diagnosis. The classic histologic finding in inflammatory breast cancer on biopsy of the affected skin is dermal lymphatic invasion by tumor cells.",
"Lymphoma of the breast is another rare cause of multiple breast lumps. Malignant lymphoma can originate as a primary breast tumor or may metastasize to the breast from another primary site. Primary malignant lymphomas of the breast comprise 0.05%-0.53% of malignant breast tumors. The median age of patients with diagnosed primary breast lymphomas ranges from 60 to 65 years. Approximately 5%-11% of patients have bilateral breast involvement.[10]",
"For a diagnosis of primary breast lymphoma, the disease process should be limited to the breast and axilla. If disease is present elsewhere in the body, the breast is considered to be a metastatic site. Clinically, breast lymphoma can occasionally present as a diffuse rapid breast enlargement in younger age groups, or as breast skin thickening due to lymphatic blockage by lymphoma resulting in retrograde edema.[6,10]",
"Melanoma is also a rare source of metastasis to the breast.",
"Evaluation of all breast lumps must be done through a formal triple assessment that includes clinical examination, appropriate imaging, and tissue diagnosis. Breast cysts and lumps such as lipomas and hamartomas can be diagnosed with certainty on ultrasound alone and need not be subjected to needle biopsy.",
"The criterion standard of tissue diagnosis for breast lumps is image-guided Tru-Cut biopsy. Fine-needle aspiration cytology is not recommended, as its diagnostic accuracy is lower than that of Tru-Cut biopsy.[11] Vacuum-assisted biopsy is recommended in certain settings to increase the diagnostic yield.",
"In patients who present with multiple lumps, imaging may not be able to detect subtle malignant transformation. For such patients, extensive tissue sampling and close imaging follow-up are required.",
"The patient in this case presented a diagnostic challenge because none of the visible lumps on the most recent ultrasound were suspicious. In addition, the lumps were unchanged when compared with the ultrasound and MRI that were performed 9 months earlier. Breast cancer was suspected purely as a diagnosis of exclusion. Inflammatory breast cancer and lymphoma were at the top of the list of differential diagnoses."
],
"date": "March 01, 2022",
"figures": [],
"markdown": "# Oncology Case Challenge: A 37-Year-Old Woman With Multiple Fibroadenomas\n\n **Authors:** Kanchan Kaur, MBBS, MS(Surg), MRCS(Edin) \n **Date:** March 01, 2022\n\n ## Content\n\n The PTEN mutation leads to increased cell proliferation with decreased apoptosis. PTEN hamartoma tumor syndrome is a family of clinical syndromes characterized by germline mutations in the PTEN gene. This family includes conditions such as Cowden syndrome, which is associated with an increased lifetime cumulative risk of developing cancer in the breast (67%-85%), thyroid (35%), kidney (33%), and endometrium (28%). Benign breast disease, especially multiple fibroadenomas, is common in Cowden syndrome.[6] Li-Fraumeni syndrome, Carney complex, Peutz-Jeghers syndrome, and Beckwith-Wiedemann syndrome are other familial conditions that may be associated with multiple benign or malignant breast lumps as part of a syndrome complex involving multiple other organs.[7,8]\nDifferentiating fibroadenoma from a phyllodes tumor is important. Phyllodes tumors of the breast are rare; fibroepithelial lesions account for less than 1% of all breast tumors. They have a high potential to recur and also carry a 10% risk for malignancy. They can exhibit rapid and tremendous growth, and in neglected cases, skin ulceration can occur owing to the pressure of the growing lump.[9]\nPhyllodes tumors are subclassified histologically as benign, borderline, or malignant according to features such as stromal overgrowth, tumor necrosis, cellular atypia, and number of mitoses per high-power field. Most phyllodes tumors (35%-64%) are benign.[9]\nBilateral multiple phyllodes tumors are very rare. Surgical excision is always indicated for phyllodes tumors even if the biopsy results are benign. In contrast to fibroadenomas, which can be \"scooped out\" during surgery, it is advisable to take a margin of normal breast tissue with phyllodes tumors. The likelihood of recurrence is generally very high, and patients must be counseled accordingly and maintained on close follow-up.\nInflammatory breast cancer is a rare form of locally advanced breast cancer (classified as T4d according to tumor, node, metastasis staging). It is a separate clinicopathologic entity in which the classic presentation is that of erythema and edema occupying at least one third of the breast. Patients present with a short history of rapidly increasing inflammation, heaviness, and swelling in the breast, which is often mistaken for infection. An underlying breast lump may not always be palpable. Many patients have lymph node metastasis at presentation. The diffuse tissue edema and parenchymal architectural distortion make the identification of a primary breast lesion more challenging on mammography and ultrasonography. MRI has greater diagnostic value in such patients.\nMultiple small, confluent, heterogeneously enhancing masses and global skin thickening are key MRI features in such cases. In addition to aiding diagnosis, serial MRI can help monitor the response to chemotherapy.\nIn the absence of an identifiable mass in the breast on imaging, a punch biopsy of the involved skin and a biopsy of the lymph nodes help establish the diagnosis. The classic histologic finding in inflammatory breast cancer on biopsy of the affected skin is dermal lymphatic invasion by tumor cells.\nLymphoma of the breast is another rare cause of multiple breast lumps. Malignant lymphoma can originate as a primary breast tumor or may metastasize to the breast from another primary site. Primary malignant lymphomas of the breast comprise 0.05%-0.53% of malignant breast tumors. The median age of patients with diagnosed primary breast lymphomas ranges from 60 to 65 years. Approximately 5%-11% of patients have bilateral breast involvement.[10]\nFor a diagnosis of primary breast lymphoma, the disease process should be limited to the breast and axilla. If disease is present elsewhere in the body, the breast is considered to be a metastatic site. Clinically, breast lymphoma can occasionally present as a diffuse rapid breast enlargement in younger age groups, or as breast skin thickening due to lymphatic blockage by lymphoma resulting in retrograde edema.[6,10]\nMelanoma is also a rare source of metastasis to the breast.\nEvaluation of all breast lumps must be done through a formal triple assessment that includes clinical examination, appropriate imaging, and tissue diagnosis. Breast cysts and lumps such as lipomas and hamartomas can be diagnosed with certainty on ultrasound alone and need not be subjected to needle biopsy.\nThe criterion standard of tissue diagnosis for breast lumps is image-guided Tru-Cut biopsy. Fine-needle aspiration cytology is not recommended, as its diagnostic accuracy is lower than that of Tru-Cut biopsy.[11] Vacuum-assisted biopsy is recommended in certain settings to increase the diagnostic yield.\nIn patients who present with multiple lumps, imaging may not be able to detect subtle malignant transformation. For such patients, extensive tissue sampling and close imaging follow-up are required.\nThe patient in this case presented a diagnostic challenge because none of the visible lumps on the most recent ultrasound were suspicious. In addition, the lumps were unchanged when compared with the ultrasound and MRI that were performed 9 months earlier. Breast cancer was suspected purely as a diagnosis of exclusion. Inflammatory breast cancer and lymphoma were at the top of the list of differential diagnoses.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Oncology Case Challenge: A 37-Year-Old Woman With Multiple Fibroadenomas"
},
{
"authors": "Kanchan Kaur, MBBS, MS(Surg), MRCS(Edin)",
"content": [
"This patient had been monitored for many years and was known to have multiple fibroadenomas. Lymphomas generally occur in older women. Primary breast lymphoma often presents as a solitary lump. Secondary lymphoma presents as multiple bilateral lumps and is associated with skin changes, such as skin tethering, peau d'orange, and erythema. Patients often exhibit systemic features, such as fever, weight loss, and night sweats (B symptoms of lymphoma). Blood counts in patients with lymphoma are mostly deranged. This patient had only local symptoms of swelling of the breast, and the results of her blood tests were normal.",
"Although she presented with a short history of changes in the breast, particularly skin changes (peau d'orange), no erythema of the skin was noted, which made the diagnosis of inflammatory breast cancer less likely. A malignant phyllodes tumor can present with a short history of rapid growth and associated skin changes; however, the lumps in her breast were unchanged in size and appearance on repeated ultrasound and MRI scans. Metastasis to the breast from another site was a possibility, although it is extremely rare, and she had no evident symptoms of any other coexistent pathology.",
"Histopathologic examination showed benign breast changes comprising adenosis and columnar cell change/hyperplasia. In addition, many tumor emboli were scattered amidst the breast tissue (Figures 7, 8).",
"Figure 7.",
"Figure 8.",
"The results of the immunohistochemistry (IHC) report on the tumor emboli were:",
"ER(SP1)-negative(3/8); Allred's score",
"PgR(1E2)-negative(0/8); Allred's score",
"HER2neu(4B5)-negative(1+)",
"Tru-Cut biopsy of the lymph node revealed metastatic breast cancer.",
"A PET-CT was recommended for this patient prior to instituting treatment to help stage the disease and to scan the whole body for evidence of coexistent pathology. In addition, because routine breast imaging had failed to identify a discrete breast primary site, a PET-CT could possibly delineate areas of increased 18F-fluorodeoxyglucose (FDG) avidity in the breast.",
"In this case, there was diffuse FDG uptake in the breast and overlying skin, along with FDG-avid ipsilateral lymph nodes. Coexistent atrial myxoma and non–FDG-avid thyroid nodules were noted."
],
"date": "March 01, 2022",
"figures": [
{
"caption": "Figure 7.",
"image_url": "https://img.medscapestatic.com/article/968/993a/968993-Thumb7.png"
},
{
"caption": "Figure 8.",
"image_url": "https://img.medscapestatic.com/article/968/993a/968993-Thumb8.png"
}
],
"markdown": "# Oncology Case Challenge: A 37-Year-Old Woman With Multiple Fibroadenomas\n\n **Authors:** Kanchan Kaur, MBBS, MS(Surg), MRCS(Edin) \n **Date:** March 01, 2022\n\n ## Content\n\n This patient had been monitored for many years and was known to have multiple fibroadenomas. Lymphomas generally occur in older women. Primary breast lymphoma often presents as a solitary lump. Secondary lymphoma presents as multiple bilateral lumps and is associated with skin changes, such as skin tethering, peau d'orange, and erythema. Patients often exhibit systemic features, such as fever, weight loss, and night sweats (B symptoms of lymphoma). Blood counts in patients with lymphoma are mostly deranged. This patient had only local symptoms of swelling of the breast, and the results of her blood tests were normal.\nAlthough she presented with a short history of changes in the breast, particularly skin changes (peau d'orange), no erythema of the skin was noted, which made the diagnosis of inflammatory breast cancer less likely. A malignant phyllodes tumor can present with a short history of rapid growth and associated skin changes; however, the lumps in her breast were unchanged in size and appearance on repeated ultrasound and MRI scans. Metastasis to the breast from another site was a possibility, although it is extremely rare, and she had no evident symptoms of any other coexistent pathology.\nHistopathologic examination showed benign breast changes comprising adenosis and columnar cell change/hyperplasia. In addition, many tumor emboli were scattered amidst the breast tissue (Figures 7, 8).\nFigure 7.\nFigure 8.\nThe results of the immunohistochemistry (IHC) report on the tumor emboli were:\nER(SP1)-negative(3/8); Allred's score\nPgR(1E2)-negative(0/8); Allred's score\nHER2neu(4B5)-negative(1+)\nTru-Cut biopsy of the lymph node revealed metastatic breast cancer.\nA PET-CT was recommended for this patient prior to instituting treatment to help stage the disease and to scan the whole body for evidence of coexistent pathology. In addition, because routine breast imaging had failed to identify a discrete breast primary site, a PET-CT could possibly delineate areas of increased 18F-fluorodeoxyglucose (FDG) avidity in the breast.\nIn this case, there was diffuse FDG uptake in the breast and overlying skin, along with FDG-avid ipsilateral lymph nodes. Coexistent atrial myxoma and non–FDG-avid thyroid nodules were noted.\n\n ## Figures\n\n **Figure 7.** \n \n\n**Figure 8.** \n \n\n\n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1664975,
"choiceText": "Incisional wedge biopsy of the periareolar skin",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664976,
"choiceText": "Multiple biopsies of the most suspicious breast lumps",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664977,
"choiceText": "Tru-Cut biopsy of the retroareolar region and the lymph node",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664978,
"choiceText": "Fine-needle aspiration cytology of the axillary node",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "No obvious suspicious breast lump was noted on either ultrasound or CEMRI. The tumor board decision was to perform random Tru-Cut biopsies of the tissue under the nipple-areola complex because increased abnormal echogenicity of the breast parenchyma was noted in this region. Skin biopsy was not performed because no clinical evidence of metastatic skin involvement was found and the changes consisted of skin edema only. If the random Tru-Cut biopsies of the breast did not reveal a diagnosis, an incisional wedge biopsy of the periareolar region would be performed. Furthermore, if none of these measures provided sufficient tissue for diagnosis, the patient's treatment would be based on the histopathologic examination results and the IHC profile obtained on the metastatic lymph node.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 536162,
"questionText": "How should a tissue diagnosis be obtained in this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1664979,
"choiceText": "Multiple bilateral breast lumps",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664980,
"choiceText": "Spotty skin pigmentation",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664981,
"choiceText": "Atrial myxoma seen on PET-CT",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664982,
"choiceText": "Multiple thyroid nodules",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664983,
"choiceText": "All of the above",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "This patient's clinical presentation and imaging findings suggested the presence of a family cancer syndrome. She received genetic counseling, and testing revealed a germline mutation in the <i>PRKAR1A</i> gene, confirming the diagnosis of Carney syndrome.<sup>[7,8]</sup><br><br>\r\n\r\nWhen multiple bilateral fibroadenomas are present, this \"innocuous\" lump may turn out to be malignant instead. This case highlights the importance of genetic testing in patients with unusual presentations of early-onset, bilateral, and multiple fibroadenomas.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 536163,
"questionText": "Which features in the history and workup suggest a cancer syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Oncology Case Challenge: A 37-Year-Old Woman With Multiple Fibroadenomas"
},
{
"authors": "Kanchan Kaur, MBBS, MS(Surg), MRCS(Edin)",
"content": [
"Follow Medscape on Facebook, Twitter, Instagram, and YouTube"
],
"date": "March 01, 2022",
"figures": [],
"markdown": "# Oncology Case Challenge: A 37-Year-Old Woman With Multiple Fibroadenomas\n\n **Authors:** Kanchan Kaur, MBBS, MS(Surg), MRCS(Edin) \n **Date:** March 01, 2022\n\n ## Content\n\n Follow Medscape on Facebook, Twitter, Instagram, and YouTube\n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1664975,
"choiceText": "Incisional wedge biopsy of the periareolar skin",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664976,
"choiceText": "Multiple biopsies of the most suspicious breast lumps",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664977,
"choiceText": "Tru-Cut biopsy of the retroareolar region and the lymph node",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664978,
"choiceText": "Fine-needle aspiration cytology of the axillary node",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "No obvious suspicious breast lump was noted on either ultrasound or CEMRI. The tumor board decision was to perform random Tru-Cut biopsies of the tissue under the nipple-areola complex because increased abnormal echogenicity of the breast parenchyma was noted in this region. Skin biopsy was not performed because no clinical evidence of metastatic skin involvement was found and the changes consisted of skin edema only. If the random Tru-Cut biopsies of the breast did not reveal a diagnosis, an incisional wedge biopsy of the periareolar region would be performed. Furthermore, if none of these measures provided sufficient tissue for diagnosis, the patient's treatment would be based on the histopathologic examination results and the IHC profile obtained on the metastatic lymph node.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 536162,
"questionText": "How should a tissue diagnosis be obtained in this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1664979,
"choiceText": "Multiple bilateral breast lumps",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664980,
"choiceText": "Spotty skin pigmentation",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664981,
"choiceText": "Atrial myxoma seen on PET-CT",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664982,
"choiceText": "Multiple thyroid nodules",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664983,
"choiceText": "All of the above",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "This patient's clinical presentation and imaging findings suggested the presence of a family cancer syndrome. She received genetic counseling, and testing revealed a germline mutation in the <i>PRKAR1A</i> gene, confirming the diagnosis of Carney syndrome.<sup>[7,8]</sup><br><br>\r\n\r\nWhen multiple bilateral fibroadenomas are present, this \"innocuous\" lump may turn out to be malignant instead. This case highlights the importance of genetic testing in patients with unusual presentations of early-onset, bilateral, and multiple fibroadenomas.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 536163,
"questionText": "Which features in the history and workup suggest a cancer syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Oncology Case Challenge: A 37-Year-Old Woman With Multiple Fibroadenomas"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1664970,
"choiceText": "Inflammatory breast cancer",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664971,
"choiceText": "Primary breast cancer",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664972,
"choiceText": "Metastasis from another primary site",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664973,
"choiceText": "Malignant phyllodes",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664974,
"choiceText": "Breast lymphoma",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 536161,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1664975,
"choiceText": "Incisional wedge biopsy of the periareolar skin",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664976,
"choiceText": "Multiple biopsies of the most suspicious breast lumps",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664977,
"choiceText": "Tru-Cut biopsy of the retroareolar region and the lymph node",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664978,
"choiceText": "Fine-needle aspiration cytology of the axillary node",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "No obvious suspicious breast lump was noted on either ultrasound or CEMRI. The tumor board decision was to perform random Tru-Cut biopsies of the tissue under the nipple-areola complex because increased abnormal echogenicity of the breast parenchyma was noted in this region. Skin biopsy was not performed because no clinical evidence of metastatic skin involvement was found and the changes consisted of skin edema only. If the random Tru-Cut biopsies of the breast did not reveal a diagnosis, an incisional wedge biopsy of the periareolar region would be performed. Furthermore, if none of these measures provided sufficient tissue for diagnosis, the patient's treatment would be based on the histopathologic examination results and the IHC profile obtained on the metastatic lymph node.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 536162,
"questionText": "How should a tissue diagnosis be obtained in this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1664979,
"choiceText": "Multiple bilateral breast lumps",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664980,
"choiceText": "Spotty skin pigmentation",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664981,
"choiceText": "Atrial myxoma seen on PET-CT",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664982,
"choiceText": "Multiple thyroid nodules",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1664983,
"choiceText": "All of the above",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "This patient's clinical presentation and imaging findings suggested the presence of a family cancer syndrome. She received genetic counseling, and testing revealed a germline mutation in the <i>PRKAR1A</i> gene, confirming the diagnosis of Carney syndrome.<sup>[7,8]</sup><br><br>\r\n\r\nWhen multiple bilateral fibroadenomas are present, this \"innocuous\" lump may turn out to be malignant instead. This case highlights the importance of genetic testing in patients with unusual presentations of early-onset, bilateral, and multiple fibroadenomas.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 536163,
"questionText": "Which features in the history and workup suggest a cancer syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
889891 | /viewarticle/889891 | [
{
"authors": "Daniel Beardmore, DO; Sonika Loona, MD; Mia Mallon, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 13-year-old athletic boy with no significant past medical history is transferred from a nearby suburban emergency department (ED) to an urban children's hospital for inpatient management of pneumomediastinum. On the day before transfer, he was physically active, participating in a track meet and then soccer practice immediately afterward. After the track meet finished, he began to have some mild chest pain, which increased during his soccer practice. During this second activity, he did not have to stop because of the pain but noted progressively worsening pain during \"deep breathing.\" The night before presentation, he had increasing pain in his chest, making sleep difficult.",
"He describes the pain as dull, located in the substernal region, extending into his neck, aggravated by deep breaths, and alleviated with rest. He does not have any dyspnea, wheezing, palpitations, dizziness, headache, sweating, or abdominal pain. He describes a mild, intermittent dry cough, which has mostly dissipated since resolution of an upper respiratory infection about 3 weeks ago.",
"The patient lives at home with his immediate family in a suburban area. His social history includes no smoke exposure or significant travel history, and his immunizations, including an annual influenza vaccination and COVID-19 vaccination with booster, are up to date. Family medical history is noncontributory and includes no history of asthma, heart disease, blood clots, or sudden/early death."
],
"date": "March 01, 2022",
"figures": [],
"markdown": "# A 13-Year-Old Athlete With Chest Pain, Cough After Practice\n\n **Authors:** Daniel Beardmore, DO; Sonika Loona, MD; Mia Mallon, MD \n **Date:** March 01, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 13-year-old athletic boy with no significant past medical history is transferred from a nearby suburban emergency department (ED) to an urban children's hospital for inpatient management of pneumomediastinum. On the day before transfer, he was physically active, participating in a track meet and then soccer practice immediately afterward. After the track meet finished, he began to have some mild chest pain, which increased during his soccer practice. During this second activity, he did not have to stop because of the pain but noted progressively worsening pain during \"deep breathing.\" The night before presentation, he had increasing pain in his chest, making sleep difficult.\nHe describes the pain as dull, located in the substernal region, extending into his neck, aggravated by deep breaths, and alleviated with rest. He does not have any dyspnea, wheezing, palpitations, dizziness, headache, sweating, or abdominal pain. He describes a mild, intermittent dry cough, which has mostly dissipated since resolution of an upper respiratory infection about 3 weeks ago.\nThe patient lives at home with his immediate family in a suburban area. His social history includes no smoke exposure or significant travel history, and his immunizations, including an annual influenza vaccination and COVID-19 vaccination with booster, are up to date. Family medical history is noncontributory and includes no history of asthma, heart disease, blood clots, or sudden/early death.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A 13-Year-Old Athlete With Chest Pain, Cough After Practice"
},
{
"authors": "Daniel Beardmore, DO; Sonika Loona, MD; Mia Mallon, MD",
"content": [
"Upon initial physical examination at the ED, the patient was reported to be well-appearing and in no acute distress, with normal vital signs. The transport team brings with them his initial ED complete blood count and complete metabolic panel, which are both within normal limits, and an EKG that reveals a normal sinus rhythm. The ED information also includes a chest radiograph (Figure 1), which identifies extensive pneumomediastinum with subcutaneous emphysema, and air extending into his neck.",
"Figure 1.",
"CT reveals extensive pneumomediastinum (Figure 2) with associated pneumopericardium (Figure 3); air in the pleural space and subcutaneous emphysema (Figure 4); and an additional finding (Figures 5 and 6), which is the primary reason for his transfer to a children's hospital for further management.",
"Figure 2.",
"Figure 3.",
"Figure 4.",
"Figure 5.",
"Figure 6.",
"Upon arrival, the boy is in stable condition. His vital signs are still normal, and he is in no respiratory distress. His physical examination includes palpable crepitus surrounding the proximal neck base and the thoracic inlet. No tenderness is noted in response to palpation of the chest wall, sternum, or rib cage. Cardiac auscultation demonstrates regular rate and rhythm, with no murmur. Lung auscultation is completely clear, and the remainder of his examination, including full neurologic examination, is likewise unremarkable. Test results are negative for COVID-19."
],
"date": "March 01, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/889/891/889891-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/889/891/889891-Thumb2.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/889/891/889891-Thumb3.png"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/889/891/889891-Thumb4.png"
},
{
"caption": "Figure 5.",
"image_url": "https://img.medscapestatic.com/article/889/891/889891-Thumb5.png"
},
{
"caption": "Figure 6.",
"image_url": "https://img.medscapestatic.com/article/889/891/889891-Thumb6.png"
}
],
"markdown": "# A 13-Year-Old Athlete With Chest Pain, Cough After Practice\n\n **Authors:** Daniel Beardmore, DO; Sonika Loona, MD; Mia Mallon, MD \n **Date:** March 01, 2022\n\n ## Content\n\n Upon initial physical examination at the ED, the patient was reported to be well-appearing and in no acute distress, with normal vital signs. The transport team brings with them his initial ED complete blood count and complete metabolic panel, which are both within normal limits, and an EKG that reveals a normal sinus rhythm. The ED information also includes a chest radiograph (Figure 1), which identifies extensive pneumomediastinum with subcutaneous emphysema, and air extending into his neck.\nFigure 1.\nCT reveals extensive pneumomediastinum (Figure 2) with associated pneumopericardium (Figure 3); air in the pleural space and subcutaneous emphysema (Figure 4); and an additional finding (Figures 5 and 6), which is the primary reason for his transfer to a children's hospital for further management.\nFigure 2.\nFigure 3.\nFigure 4.\nFigure 5.\nFigure 6.\nUpon arrival, the boy is in stable condition. His vital signs are still normal, and he is in no respiratory distress. His physical examination includes palpable crepitus surrounding the proximal neck base and the thoracic inlet. No tenderness is noted in response to palpation of the chest wall, sternum, or rib cage. Cardiac auscultation demonstrates regular rate and rhythm, with no murmur. Lung auscultation is completely clear, and the remainder of his examination, including full neurologic examination, is likewise unremarkable. Test results are negative for COVID-19.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4.** \n \n\n**Figure 5.** \n \n\n**Figure 6.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1170260,
"choiceText": "Ruptured main bronchus",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170262,
"choiceText": "Spinal fracture",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170264,
"choiceText": "Cardiac tamponade",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170266,
"choiceText": "Pneumorrhachis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170268,
"choiceText": "Mallory-Weiss tear",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 372053,
"questionText": "Based on only these findings, which is the likely diagnosis that prompted transport to the children's hospital?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 13-Year-Old Athlete With Chest Pain, Cough After Practice"
},
{
"authors": "Daniel Beardmore, DO; Sonika Loona, MD; Mia Mallon, MD",
"content": [
"The patient described in this case presented with the unique finding of pneumomediastinum after prolonged physical activity, with the \"exceptional radiographic finding\" of pneumorrhachis—the presence of intraspinal air, as described and defined in a 2006 European Spine Journal review.[1]",
"Spontaneous pneumomediastinum is an uncommon finding in healthy pediatric patients, although the exact incidence is unknown.[2] The three main causes of spontaneous pneumomediastinum are alveolar rupture; perforation or rupture of the esophagus, trachea, or main bronchi; and dissection of air from the neck or abdomen. Most patients who develop pneumomediastinum do so owing to a significant prolonged or strong cough, which is a common symptom of many conditions, or through bronchospasm related to respiratory tract infection; both of these can lead to alveolar rupture. The usual course of recovery depends on the ability of the alveoli to heal, which is only possible if the cough can be suppressed or if the underlying condition improves.",
"Pneumomediastinum is discovered either by crepitus on examination or by identification of air outside the lungs on imaging. The imaging modality initially used determines whether further imaging is necessary for diagnosis; for example, in this case, the patient's pneumomediastinum was diagnosed on anteroposterior chest radiography, which prompted CT of the neck and chest. This revealed pneumopericardium, air in the pleural space, subcutaneous emphysema, and pneumorrhachis. Further workup depends on the circumstance of the individual case but may include complete blood count with differential and blood and/or sputum culture if respiratory tract infection is a concern."
],
"date": "March 01, 2022",
"figures": [],
"markdown": "# A 13-Year-Old Athlete With Chest Pain, Cough After Practice\n\n **Authors:** Daniel Beardmore, DO; Sonika Loona, MD; Mia Mallon, MD \n **Date:** March 01, 2022\n\n ## Content\n\n The patient described in this case presented with the unique finding of pneumomediastinum after prolonged physical activity, with the \"exceptional radiographic finding\" of pneumorrhachis—the presence of intraspinal air, as described and defined in a 2006 European Spine Journal review.[1]\nSpontaneous pneumomediastinum is an uncommon finding in healthy pediatric patients, although the exact incidence is unknown.[2] The three main causes of spontaneous pneumomediastinum are alveolar rupture; perforation or rupture of the esophagus, trachea, or main bronchi; and dissection of air from the neck or abdomen. Most patients who develop pneumomediastinum do so owing to a significant prolonged or strong cough, which is a common symptom of many conditions, or through bronchospasm related to respiratory tract infection; both of these can lead to alveolar rupture. The usual course of recovery depends on the ability of the alveoli to heal, which is only possible if the cough can be suppressed or if the underlying condition improves.\nPneumomediastinum is discovered either by crepitus on examination or by identification of air outside the lungs on imaging. The imaging modality initially used determines whether further imaging is necessary for diagnosis; for example, in this case, the patient's pneumomediastinum was diagnosed on anteroposterior chest radiography, which prompted CT of the neck and chest. This revealed pneumopericardium, air in the pleural space, subcutaneous emphysema, and pneumorrhachis. Further workup depends on the circumstance of the individual case but may include complete blood count with differential and blood and/or sputum culture if respiratory tract infection is a concern.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1170260,
"choiceText": "Ruptured main bronchus",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170262,
"choiceText": "Spinal fracture",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170264,
"choiceText": "Cardiac tamponade",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170266,
"choiceText": "Pneumorrhachis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170268,
"choiceText": "Mallory-Weiss tear",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 372053,
"questionText": "Based on only these findings, which is the likely diagnosis that prompted transport to the children's hospital?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 13-Year-Old Athlete With Chest Pain, Cough After Practice"
},
{
"authors": "Daniel Beardmore, DO; Sonika Loona, MD; Mia Mallon, MD",
"content": [
"The patient in this case was unique because he did not have a history of the known risk factor, asthma. The case was also unusual because the patient's pneumomediastinum developed as a result of excessive physical exertion during sports activity, another recognized but less common cause of pneumomediastinum. This activity probably resulted in an alveolar rupture and air tracking back to the chest and beyond.",
"The patient's presentation was clinically similar to that of most pneumomediastinum cases, in that he improved quickly after being admitted; this is the usual scenario when the initial insult has ceased. Again, his case was unusual because the insult that resolved was exertion and not bronchospasm or cough, as is most common.",
"Suspicion for this condition should be high when the presentation is preceded by the Valsalva maneuver, forceful coughing or vomiting, hyperpnea, bronchial asthma, inhalation of drugs, foreign body aspiration, childbirth, or intense physical exertion. His hospitalization was average compared with other patients with a similar condition, in that he spent 1 day in the hospital.[2]",
"Furthermore, this case was unusual owing to the finding of pneumorrhachis, which is quite rare. In the author's review of the literature, a study from the Journal of Trauma identified only 50 cases of pneumorrhachis in 42 total studies.[3] This finding further demonstrates that pneumorrhachis is a rare phenomenon that is specifically seen after spontaneous pneumothorax. These rare nontraumatic case reports of pneumorrhachis typically include histories of significant cough.[4] The patient in this case reported only a lingering, nearly resolved, and mild intermittent cough that was not worsened during his prolonged physical activity. In addition, no cough was observed during his hospital stay. Although some case reports in the literature describe pneumorrhachis with significant signs and symptoms, including cervical myelopathy, paraplegia, and mild headache, these findings were in adults.[5,6] The patient in this case had none of those signs or symptoms."
],
"date": "March 01, 2022",
"figures": [],
"markdown": "# A 13-Year-Old Athlete With Chest Pain, Cough After Practice\n\n **Authors:** Daniel Beardmore, DO; Sonika Loona, MD; Mia Mallon, MD \n **Date:** March 01, 2022\n\n ## Content\n\n The patient in this case was unique because he did not have a history of the known risk factor, asthma. The case was also unusual because the patient's pneumomediastinum developed as a result of excessive physical exertion during sports activity, another recognized but less common cause of pneumomediastinum. This activity probably resulted in an alveolar rupture and air tracking back to the chest and beyond.\nThe patient's presentation was clinically similar to that of most pneumomediastinum cases, in that he improved quickly after being admitted; this is the usual scenario when the initial insult has ceased. Again, his case was unusual because the insult that resolved was exertion and not bronchospasm or cough, as is most common.\nSuspicion for this condition should be high when the presentation is preceded by the Valsalva maneuver, forceful coughing or vomiting, hyperpnea, bronchial asthma, inhalation of drugs, foreign body aspiration, childbirth, or intense physical exertion. His hospitalization was average compared with other patients with a similar condition, in that he spent 1 day in the hospital.[2]\nFurthermore, this case was unusual owing to the finding of pneumorrhachis, which is quite rare. In the author's review of the literature, a study from the Journal of Trauma identified only 50 cases of pneumorrhachis in 42 total studies.[3] This finding further demonstrates that pneumorrhachis is a rare phenomenon that is specifically seen after spontaneous pneumothorax. These rare nontraumatic case reports of pneumorrhachis typically include histories of significant cough.[4] The patient in this case reported only a lingering, nearly resolved, and mild intermittent cough that was not worsened during his prolonged physical activity. In addition, no cough was observed during his hospital stay. Although some case reports in the literature describe pneumorrhachis with significant signs and symptoms, including cervical myelopathy, paraplegia, and mild headache, these findings were in adults.[5,6] The patient in this case had none of those signs or symptoms.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A 13-Year-Old Athlete With Chest Pain, Cough After Practice"
},
{
"authors": "Daniel Beardmore, DO; Sonika Loona, MD; Mia Mallon, MD",
"content": [
"Treatment for pneumomediastinum and any further spread of air throughout the chest and neck, including pneumorrhachis, is symptomatic and for comfort, and includes analgesics for pain. Although these patients may have respiratory signs and symptoms, positive pressure (eg, continuous positive airway pressure, nonrebreather mask) should be avoided because high airway pressures can worsen the air leak. Nasal cannula with FiO2 greater than room air may be given for hypoxia because it is low pressure. Oxygen therapy to reduce blood nitrogen partial pressure and encourage resorption of gas, so-called \"nitrogen washout,\" may also be considered for either pneumomediastinum or pneumorrhachis. Calming an agitated or anxious patient can be very beneficial in preventing hyperventilation as well.",
"Surgical intervention may also be needed when persistent or intense cerebrospinal fluid leakage is present, as well as thoracic/arachnoid fistulas and lung injuries. CT-guided air aspiration through a spinal needle inserted in the neural foramen has been described. Prophylactic antibiotics are not recommended unless signs of meningitis are present.",
"The patient in this case was admitted to the general medical floor for conservative management. General surgery and neurosurgery were consulted, and both recommended observation until resolution of clinical symptoms. Follow-up imaging was not recommended. The patient was discharged on hospital day 2 in stable condition; he was breathing comfortably, and no further pain was elicited in his chest or neck, even with deep breathing. His thoracic inlet and neck crepitus was noted to have resolved at the time of discharge. He was recommended to refrain from sports, gym class, or other strenuous physical activity until clearance at an outpatient follow-up, scheduled within the week."
],
"date": "March 01, 2022",
"figures": [],
"markdown": "# A 13-Year-Old Athlete With Chest Pain, Cough After Practice\n\n **Authors:** Daniel Beardmore, DO; Sonika Loona, MD; Mia Mallon, MD \n **Date:** March 01, 2022\n\n ## Content\n\n Treatment for pneumomediastinum and any further spread of air throughout the chest and neck, including pneumorrhachis, is symptomatic and for comfort, and includes analgesics for pain. Although these patients may have respiratory signs and symptoms, positive pressure (eg, continuous positive airway pressure, nonrebreather mask) should be avoided because high airway pressures can worsen the air leak. Nasal cannula with FiO2 greater than room air may be given for hypoxia because it is low pressure. Oxygen therapy to reduce blood nitrogen partial pressure and encourage resorption of gas, so-called \"nitrogen washout,\" may also be considered for either pneumomediastinum or pneumorrhachis. Calming an agitated or anxious patient can be very beneficial in preventing hyperventilation as well.\nSurgical intervention may also be needed when persistent or intense cerebrospinal fluid leakage is present, as well as thoracic/arachnoid fistulas and lung injuries. CT-guided air aspiration through a spinal needle inserted in the neural foramen has been described. Prophylactic antibiotics are not recommended unless signs of meningitis are present.\nThe patient in this case was admitted to the general medical floor for conservative management. General surgery and neurosurgery were consulted, and both recommended observation until resolution of clinical symptoms. Follow-up imaging was not recommended. The patient was discharged on hospital day 2 in stable condition; he was breathing comfortably, and no further pain was elicited in his chest or neck, even with deep breathing. His thoracic inlet and neck crepitus was noted to have resolved at the time of discharge. He was recommended to refrain from sports, gym class, or other strenuous physical activity until clearance at an outpatient follow-up, scheduled within the week.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1170270,
"choiceText": "1-2 days",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170272,
"choiceText": "3-4 days",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170274,
"choiceText": "5-7 days",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170276,
"choiceText": "1-2 weeks",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "A retrospective cohort study on the management and outcomes of spontaneous pneumomediastinum in children found a median hospital stay of 27 hours.<sup>[7]</sup> If the condition was caused by external trauma that resulted in dissection of air from the neck or abdomen, or from perforation or rupture of the esophagus, trachea, or main bronchi, surgical care is required and a much longer recovery course is expected.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 372055,
"questionText": "What is the expected length of hospital stay for pediatric patients with spontaneous pneumomediastinum?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1170278,
"choiceText": "Disc herniation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170280,
"choiceText": "Tachycardia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170282,
"choiceText": "Impaired bowel control",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170284,
"choiceText": "Spinal cord compression",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170286,
"choiceText": "Hypotension",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Although rare, pockets of intraspinal air can result in spinal cord compression and resulting signs or symptoms, such as myelopathy, paraplegia, and headache.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 372057,
"questionText": "Which is recognized as a complication of nontraumatic pneumorrhachis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 13-Year-Old Athlete With Chest Pain, Cough After Practice"
},
{
"authors": "Daniel Beardmore, DO; Sonika Loona, MD; Mia Mallon, MD",
"content": [],
"date": "March 01, 2022",
"figures": [],
"markdown": "# A 13-Year-Old Athlete With Chest Pain, Cough After Practice\n\n **Authors:** Daniel Beardmore, DO; Sonika Loona, MD; Mia Mallon, MD \n **Date:** March 01, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1170270,
"choiceText": "1-2 days",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170272,
"choiceText": "3-4 days",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170274,
"choiceText": "5-7 days",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170276,
"choiceText": "1-2 weeks",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "A retrospective cohort study on the management and outcomes of spontaneous pneumomediastinum in children found a median hospital stay of 27 hours.<sup>[7]</sup> If the condition was caused by external trauma that resulted in dissection of air from the neck or abdomen, or from perforation or rupture of the esophagus, trachea, or main bronchi, surgical care is required and a much longer recovery course is expected.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 372055,
"questionText": "What is the expected length of hospital stay for pediatric patients with spontaneous pneumomediastinum?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1170278,
"choiceText": "Disc herniation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170280,
"choiceText": "Tachycardia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170282,
"choiceText": "Impaired bowel control",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170284,
"choiceText": "Spinal cord compression",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170286,
"choiceText": "Hypotension",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Although rare, pockets of intraspinal air can result in spinal cord compression and resulting signs or symptoms, such as myelopathy, paraplegia, and headache.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 372057,
"questionText": "Which is recognized as a complication of nontraumatic pneumorrhachis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 13-Year-Old Athlete With Chest Pain, Cough After Practice"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1170260,
"choiceText": "Ruptured main bronchus",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170262,
"choiceText": "Spinal fracture",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170264,
"choiceText": "Cardiac tamponade",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170266,
"choiceText": "Pneumorrhachis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170268,
"choiceText": "Mallory-Weiss tear",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 372053,
"questionText": "Based on only these findings, which is the likely diagnosis that prompted transport to the children's hospital?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1170270,
"choiceText": "1-2 days",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170272,
"choiceText": "3-4 days",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170274,
"choiceText": "5-7 days",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170276,
"choiceText": "1-2 weeks",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "A retrospective cohort study on the management and outcomes of spontaneous pneumomediastinum in children found a median hospital stay of 27 hours.<sup>[7]</sup> If the condition was caused by external trauma that resulted in dissection of air from the neck or abdomen, or from perforation or rupture of the esophagus, trachea, or main bronchi, surgical care is required and a much longer recovery course is expected.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 372055,
"questionText": "What is the expected length of hospital stay for pediatric patients with spontaneous pneumomediastinum?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1170278,
"choiceText": "Disc herniation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170280,
"choiceText": "Tachycardia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170282,
"choiceText": "Impaired bowel control",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170284,
"choiceText": "Spinal cord compression",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1170286,
"choiceText": "Hypotension",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Although rare, pockets of intraspinal air can result in spinal cord compression and resulting signs or symptoms, such as myelopathy, paraplegia, and headache.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 372057,
"questionText": "Which is recognized as a complication of nontraumatic pneumorrhachis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
727294 | /viewarticle/727294 | [
{
"authors": "Prasenjit Das, MD, MB BS",
"content": [
"Editorial Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 42-year-old woman is referred to the neurosurgery outpatient department with a gradual-onset headache that is constant and located in the right half of her head. She has also had frequent, repetitive, nonprojectile vomiting not related to meal intake for 3-4 months. In addition, the patient has had cognitive defects for the last 3-4 months, especially a reduction of what she describes as \"thinking power.\"",
"She underwent enucleation of her left eye in a different hospital 8 years ago, the details of which the patient could not recall. No other significant medical history is known. The first-degree family members also report no significant medical or surgical history."
],
"date": "February 11, 2022",
"figures": [],
"markdown": "# A 42-Year-Old With Declining Cognition and Frequent Vomiting\n\n **Authors:** Prasenjit Das, MD, MB BS \n **Date:** February 11, 2022\n\n ## Content\n\n Editorial Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 42-year-old woman is referred to the neurosurgery outpatient department with a gradual-onset headache that is constant and located in the right half of her head. She has also had frequent, repetitive, nonprojectile vomiting not related to meal intake for 3-4 months. In addition, the patient has had cognitive defects for the last 3-4 months, especially a reduction of what she describes as \"thinking power.\"\nShe underwent enucleation of her left eye in a different hospital 8 years ago, the details of which the patient could not recall. No other significant medical history is known. The first-degree family members also report no significant medical or surgical history.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A 42-Year-Old With Declining Cognition and Frequent Vomiting"
},
{
"authors": "Prasenjit Das, MD, MB BS",
"content": [
"Upon examination, the right pupil is reactive to light. No localized lesions are found in the enucleated left orbital fossa.",
"The hematologic parameters of the patient are as follows:",
"Hemoglobin level, 9.8 g/dL (reference range, 12-15.5 g/dL)",
"Total leukocyte count, 15,000/μL (reference range, 4,500-11,000/μL)",
"Platelet count, 190 x 103/μL (reference range, 150-400 x 103/μL)",
"Erythrocyte sedimentation rate (ESR), 36 mm/hr (reference range, 1-20 mm/hr)",
"The peripheral blood smears show no abnormal morphology. Her biochemical parameters are also within normal physiological limits.",
"The patient's vital signs include a pulse rate of 90 beats/min, blood pressure of 138/86 mm Hg, and a respiratory rate of 18 breaths/min, and she is afebrile. Her abdominal organs are not palpable. Radiography of the chest does not reveal any acute findings.",
"Sagittal T1-weighted MRI of the brain reveals a hyperintense lesion in the superficial cortex of the posterior frontal region, with surrounding edema (Figure 1).",
"Figure 1.",
"A sagittal T2-weighted MRI scan of the brain reveals a hypointense lesion in the posterior frontal region, with surrounding edema that appears hyperintense (Figure 2).",
"Figure 2.",
"The lesion is excised; a postoperative noncontrast CT scan of the head shows no evidence of residual tumor, with mild cerebral edema (Figure 3).",
"Figure 3.",
"Upon histopathologic examination, a tumor is noted in the cerebral cortex infiltrating into the Virchow-Robbins spaces. Subpial spread of the cells is seen, as well as marked nuclear pleomorphism and prominent nucleoli. Frequent mitotic activity is detected (Figure 4).",
"Figure 4."
],
"date": "February 11, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/726/851/726851-thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/726/851/726851-thumb2.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/726/851/726851-thumb3.png"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/726/851/726851-thumb4.png"
}
],
"markdown": "# A 42-Year-Old With Declining Cognition and Frequent Vomiting\n\n **Authors:** Prasenjit Das, MD, MB BS \n **Date:** February 11, 2022\n\n ## Content\n\n Upon examination, the right pupil is reactive to light. No localized lesions are found in the enucleated left orbital fossa.\nThe hematologic parameters of the patient are as follows:\nHemoglobin level, 9.8 g/dL (reference range, 12-15.5 g/dL)\nTotal leukocyte count, 15,000/μL (reference range, 4,500-11,000/μL)\nPlatelet count, 190 x 103/μL (reference range, 150-400 x 103/μL)\nErythrocyte sedimentation rate (ESR), 36 mm/hr (reference range, 1-20 mm/hr)\nThe peripheral blood smears show no abnormal morphology. Her biochemical parameters are also within normal physiological limits.\nThe patient's vital signs include a pulse rate of 90 beats/min, blood pressure of 138/86 mm Hg, and a respiratory rate of 18 breaths/min, and she is afebrile. Her abdominal organs are not palpable. Radiography of the chest does not reveal any acute findings.\nSagittal T1-weighted MRI of the brain reveals a hyperintense lesion in the superficial cortex of the posterior frontal region, with surrounding edema (Figure 1).\nFigure 1.\nA sagittal T2-weighted MRI scan of the brain reveals a hypointense lesion in the posterior frontal region, with surrounding edema that appears hyperintense (Figure 2).\nFigure 2.\nThe lesion is excised; a postoperative noncontrast CT scan of the head shows no evidence of residual tumor, with mild cerebral edema (Figure 3).\nFigure 3.\nUpon histopathologic examination, a tumor is noted in the cerebral cortex infiltrating into the Virchow-Robbins spaces. Subpial spread of the cells is seen, as well as marked nuclear pleomorphism and prominent nucleoli. Frequent mitotic activity is detected (Figure 4).\nFigure 4.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 361933,
"choiceText": "Glioblastoma",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361934,
"choiceText": "Choroid plexus papilloma",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361935,
"choiceText": "Retinoblastoma",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361936,
"choiceText": "Metastatic melanoma",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 103389,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 42-Year-Old With Declining Cognition and Frequent Vomiting"
},
{
"authors": "Prasenjit Das, MD, MB BS",
"content": [
"The patient's imaging findings coupled with the history of left orbital enucleation were the most important clues to the presumptive metastatic melanoma diagnosis. The melanoma likely stemmed from a previous ocular melanoma. This could not be verified, however, because the patient had lost all previous medical records.",
"The characteristic histopathology of sheets of spindled-to-polygonal cells with frequent mitotic activity and dense cytoplasmic collection of brownish-black melanin pigment confirmed the clinical suspicion (Figure 4).",
"Figure 4.",
"The tumor cells were immunopositive for S-100 protein, HMB-45, and Melan-A. An MIB-1 labeling index of 38% was detected in the highest proliferating areas, where the immunohistochemical stains were performed after bleaching the melanin pigment on slides with KMnO4 solution. This combination of radiologic and histologic features is diagnostic. The characteristic T1- and T2-weighted MRI images with marked perilesional edema suggested a metastatic mitotic lesion.",
"Melanoma is a lethal cutaneous malignancy that usually arises from the neural crest cells. Intracranial melanomas are seen in 10%-40% of cases of either cutaneous or visceral melanomas, whereas cerebral metastases are found in 50%-75% of melanoma patients at autopsy.[1,2] These tumors can be either primary de novo or secondary from the adjacent pigment-containing structures.",
"Primary malignant melanomas arise from meningeal melanocytes.[1] These melanocytes are commonly seen in the pons, cerebellum, cerebral peduncles, medulla, interpeduncular fossa, and inferior surfaces of the frontal, temporal, and occipital lobes; therefore, intracranial malignant melanomas are seen to cluster around these sites.[3] These primary melanomas are commonly associated with neurocutaneous melanosis syndrome or they may arise from malignant transformation of premalignant pigment-containing lesions, such as in meningeal melanosis.",
"Secondary melanomas are extensions of ocular melanomas or are caused by hematogenous spread from cutaneous or other visceral melanomas.[1]",
"Primary de novo malignant melanomas are usually situated closer to the meninges, as they arise from the meningeal melanocytes, whereas secondary metastatic melanomas are situated deep in the gray-white matter junction.[3] These metastatic tumors are either solitary, relatively well-delineated lesions or (most often) they are multifocal and have a unique tendency to hemorrhage."
],
"date": "February 11, 2022",
"figures": [
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/726/851/726851-thumb4.png"
}
],
"markdown": "# A 42-Year-Old With Declining Cognition and Frequent Vomiting\n\n **Authors:** Prasenjit Das, MD, MB BS \n **Date:** February 11, 2022\n\n ## Content\n\n The patient's imaging findings coupled with the history of left orbital enucleation were the most important clues to the presumptive metastatic melanoma diagnosis. The melanoma likely stemmed from a previous ocular melanoma. This could not be verified, however, because the patient had lost all previous medical records.\nThe characteristic histopathology of sheets of spindled-to-polygonal cells with frequent mitotic activity and dense cytoplasmic collection of brownish-black melanin pigment confirmed the clinical suspicion (Figure 4).\nFigure 4.\nThe tumor cells were immunopositive for S-100 protein, HMB-45, and Melan-A. An MIB-1 labeling index of 38% was detected in the highest proliferating areas, where the immunohistochemical stains were performed after bleaching the melanin pigment on slides with KMnO4 solution. This combination of radiologic and histologic features is diagnostic. The characteristic T1- and T2-weighted MRI images with marked perilesional edema suggested a metastatic mitotic lesion.\nMelanoma is a lethal cutaneous malignancy that usually arises from the neural crest cells. Intracranial melanomas are seen in 10%-40% of cases of either cutaneous or visceral melanomas, whereas cerebral metastases are found in 50%-75% of melanoma patients at autopsy.[1,2] These tumors can be either primary de novo or secondary from the adjacent pigment-containing structures.\nPrimary malignant melanomas arise from meningeal melanocytes.[1] These melanocytes are commonly seen in the pons, cerebellum, cerebral peduncles, medulla, interpeduncular fossa, and inferior surfaces of the frontal, temporal, and occipital lobes; therefore, intracranial malignant melanomas are seen to cluster around these sites.[3] These primary melanomas are commonly associated with neurocutaneous melanosis syndrome or they may arise from malignant transformation of premalignant pigment-containing lesions, such as in meningeal melanosis.\nSecondary melanomas are extensions of ocular melanomas or are caused by hematogenous spread from cutaneous or other visceral melanomas.[1]\nPrimary de novo malignant melanomas are usually situated closer to the meninges, as they arise from the meningeal melanocytes, whereas secondary metastatic melanomas are situated deep in the gray-white matter junction.[3] These metastatic tumors are either solitary, relatively well-delineated lesions or (most often) they are multifocal and have a unique tendency to hemorrhage.\n\n ## Figures\n\n **Figure 4.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 361933,
"choiceText": "Glioblastoma",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361934,
"choiceText": "Choroid plexus papilloma",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361935,
"choiceText": "Retinoblastoma",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361936,
"choiceText": "Metastatic melanoma",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 103389,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 42-Year-Old With Declining Cognition and Frequent Vomiting"
},
{
"authors": "Prasenjit Das, MD, MB BS",
"content": [
"When examining a patient with a suspected intracranial melanoma, a careful clinical history with physical examination is required, as a systemic primary lesion may be missed and later detected during postmortem examination. Approximately 10%-20% of patients with an unknown primary melanoma have had a pigmented lesion removed in the past or have noted a pigmented cutaneous lesion that has involuted.",
"No specific indications prompt screening laboratory studies of patients with suspected melanomas; however, radiologic studies are imperative. Metastatic lesions are usually multiple, and they show a characteristic perilesional edema. A contrast-enhanced MRI scan is more informative than contrast-enhanced CT scans in these cases. On MRI, melanoma may appear hyperintense on T1-weighted scans and hypointense on T2-weighted scans due to the melanin content of the tumor.[1] When a metastatic melanoma is suspected, chest radiography followed by abdominal CT scanning, radionuclide bone scanning, and positron emission tomography (PET) scans are highly sensitive techniques to determine systemic metastatic malignancy.",
"While assessing any extra- or intra-axial, mitotically active lesions in the central nervous system (CNS), the possibility of a melanoma should be kept as a differential diagnosis, even in an apparent absence of pigmentation. Cytologic atypia, prominent nucleoli, and atypical mitotic figures are indicative of this lesion in the absence of melanin pigment. When such a lesion is detected, a diligent search for the melanin on histopathologic sections is necessary. Sometimes, the melanocytic nature of the lesions can only be established by immunohistochemical stains for S-100 proteins, Melan-A or HMB-45 stains, or by ultrastructural studies.",
"The relative positioning and number of the lesions in the CNS sometimes help to differentiate the primary from the metastatic lesions. The metastatic lesions are usually intraparenchymal and multiple, but they can also be solitary.[1] In this context, the importance of a detailed clinical history and physical examination should again be stressed.",
"The differential diagnosis includes meningeal melanocytomas, pigmented meningioma, schwannoma, medulloblastoma, choroid plexus papilloma, astrocytoma, and pituitary tumors. Although sometimes difficult to distinguish with imaging, melanocytomas have less cytological atypia and mitotic activity, and the presence of a complete basal lamina around the tumor cells.[3] Ocular or uveal melanoma is a malignant tumor of the eye involving the iris, ciliary body, or choroid (collectively referred to as the uvea).[4] It is regarded as a malignant tumor with a high recurrence rate, as > 50% of primary ocular melanomas recur within 15 years of primary treatment.",
"The prognosis for these tumors depends on several factors, such as tumor size, involvement of ciliary body, and age of the patient. Histologic factors, such as epithelioid morphology, high extracellular matrix production, or tumor-infiltrating lymphocytes, also play a role. Multiple studies, including the Collaborative Ocular Melanoma Study (COMS), have specified tumor size as the strongest indicator of metastasis and, therefore, survival. The gene expression profile of these tumors is crucial in the prognosis of ocular melanomas. A gain on chromosome 6 or 8 and monosomy 3 are especially poor prognostic indicators. Metastasis to the liver has been documented, with a survival of only 8-10 months following the identification of metastasis. Although metastases within the cortical parenchyma have been reported, these are relatively rare."
],
"date": "February 11, 2022",
"figures": [],
"markdown": "# A 42-Year-Old With Declining Cognition and Frequent Vomiting\n\n **Authors:** Prasenjit Das, MD, MB BS \n **Date:** February 11, 2022\n\n ## Content\n\n When examining a patient with a suspected intracranial melanoma, a careful clinical history with physical examination is required, as a systemic primary lesion may be missed and later detected during postmortem examination. Approximately 10%-20% of patients with an unknown primary melanoma have had a pigmented lesion removed in the past or have noted a pigmented cutaneous lesion that has involuted.\nNo specific indications prompt screening laboratory studies of patients with suspected melanomas; however, radiologic studies are imperative. Metastatic lesions are usually multiple, and they show a characteristic perilesional edema. A contrast-enhanced MRI scan is more informative than contrast-enhanced CT scans in these cases. On MRI, melanoma may appear hyperintense on T1-weighted scans and hypointense on T2-weighted scans due to the melanin content of the tumor.[1] When a metastatic melanoma is suspected, chest radiography followed by abdominal CT scanning, radionuclide bone scanning, and positron emission tomography (PET) scans are highly sensitive techniques to determine systemic metastatic malignancy.\nWhile assessing any extra- or intra-axial, mitotically active lesions in the central nervous system (CNS), the possibility of a melanoma should be kept as a differential diagnosis, even in an apparent absence of pigmentation. Cytologic atypia, prominent nucleoli, and atypical mitotic figures are indicative of this lesion in the absence of melanin pigment. When such a lesion is detected, a diligent search for the melanin on histopathologic sections is necessary. Sometimes, the melanocytic nature of the lesions can only be established by immunohistochemical stains for S-100 proteins, Melan-A or HMB-45 stains, or by ultrastructural studies.\nThe relative positioning and number of the lesions in the CNS sometimes help to differentiate the primary from the metastatic lesions. The metastatic lesions are usually intraparenchymal and multiple, but they can also be solitary.[1] In this context, the importance of a detailed clinical history and physical examination should again be stressed.\nThe differential diagnosis includes meningeal melanocytomas, pigmented meningioma, schwannoma, medulloblastoma, choroid plexus papilloma, astrocytoma, and pituitary tumors. Although sometimes difficult to distinguish with imaging, melanocytomas have less cytological atypia and mitotic activity, and the presence of a complete basal lamina around the tumor cells.[3] Ocular or uveal melanoma is a malignant tumor of the eye involving the iris, ciliary body, or choroid (collectively referred to as the uvea).[4] It is regarded as a malignant tumor with a high recurrence rate, as > 50% of primary ocular melanomas recur within 15 years of primary treatment.\nThe prognosis for these tumors depends on several factors, such as tumor size, involvement of ciliary body, and age of the patient. Histologic factors, such as epithelioid morphology, high extracellular matrix production, or tumor-infiltrating lymphocytes, also play a role. Multiple studies, including the Collaborative Ocular Melanoma Study (COMS), have specified tumor size as the strongest indicator of metastasis and, therefore, survival. The gene expression profile of these tumors is crucial in the prognosis of ocular melanomas. A gain on chromosome 6 or 8 and monosomy 3 are especially poor prognostic indicators. Metastasis to the liver has been documented, with a survival of only 8-10 months following the identification of metastasis. Although metastases within the cortical parenchyma have been reported, these are relatively rare.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A 42-Year-Old With Declining Cognition and Frequent Vomiting"
},
{
"authors": "Prasenjit Das, MD, MB BS",
"content": [
"Metastatic melanoma in the CNS is almost incurable. Treatment is symptomatic and involves surgical tumor debulking and symptomatic relief. The use of steroids for perilesional edema is indicated for the reduction of intracranial pressure.",
"Previous reports have found that patients with solitary primary intracranial melanoma have overall mean survival of less than 2 years, whereas patients with diffuse leptomeningeal spread have a survival of only around 6 months.[5] Rare reports describe metastasis from primary intracranial melanoma to the lungs, spleen, pancreas, and kidneys.[5]",
"The treatment options should be individualized for each patient based on the number of lesions and access to them, as well as the possibility of extracranial metastases. Radiation therapy, stereotactic radiosurgery, surgical resection, or immunologic are options.",
"Whole-brain radiation treatment for either solitary or multiple brain metastases can improve neurologic deficits, as well as the patient's survival, if associated with tumor excision. Response rates vary from 37% to 100%, and the mean survival following irradiation ranges from 2 months to 7.6 months (average 3.8 months).[6] Similarly, stereotactic radiosurgery can be performed on the solitary or multiple metastatic lesions in the brain, which has the advantage of remarkably less radiotoxicity in the peritumoral brain tissue. This treatment has been shown to achieve local tumor control as well as improve the medial survival by 4-7 months.[6] Local tumor excision can improve the neurologic deficits to a great extent; however, better tumor control has been achieved when this is combined with postoperative radiation therapy.[1]",
"In order for any targeted therapy to be effective, the treatment should cross the blood-brain barrier (BBB). P-glycoprotein, a multidrug resistance protein (MRP), has been identified in the vascular endothelium, resulting in the prevention of cytotoxic drugs from entering the brain. Some agents, such as neuroattenuated herpes simplex virus 1 (HSV-1), can ease the crossing of the BBB for intracranial therapy of brain metastases. Neuroattenuated HSV-1, with a deletion in the RL1 gene, has been shown to prolong survival in mice bearing various tumors. Due to the mutation of the HSV-1 RL1 gene, this virus cannot replicate in the central nervous system; however, it does ignite the immunologic response, which, in turn, kills the tumor cells.[2] P-glycoprotein inhibitors, such as PSC-833, have been tried along with paclitaxel or vinblastin in mice, and have been shown to improve BBB penetration of these chemotherapeutic agents.",
"Advancements to ease this drug delivery include the use of nanoparticle-coated doxorubicin and liposome-containing drugs tagged with an antibody that recognizes receptors along the endothelium; other proteins, peptides, and siRNAs are also being used. Methylating agents, which impair the ability of cancer cells to divide (including dacarbazine, temozolomide [TMZ], and procarbazine) are effective in treating metastatic melanoma. Temozolomide and nitrosoureas, such as carmustine and lomustine, are known to effectively cross the BBB. Taxanes, such as docetaxel and paclitaxel, also show a low-level activity against melanoma. Corticosteroids have been used to reduce the swelling caused by brain metastases.",
"Apart from this, a wide array of targeted monoclonal antibodies have been tried in intracranial melanomas, including 131I, 90Y, 211At, 212Bi, 67Cu, 186Re, 188Re, 212Pb and ME1-14 F (ab2). However, these targeted therapies have been shown to increase the survival by only 1-3 months and are therefore not popular owing to the high cost-benefit ratio.[6]",
"Many therapeutic options for ocular melanoma are available, including plaque radiation therapy (iodine-125, ruthenium-106, and palladium-103), brachytherapy, the use of proton- or helium-charged particles, transscleral resection, the use of a microwave heat delivery system or laser heat coagulation to accentuate the effect of radiation therapy, xenon arc photocoagulation or diode laser transpupillary thermotherapy, gamma-knife stereotactic radiosurgery, or a combination of these different modalities.[4]",
"Among the drugs available for the treatment of metastatic melanoma are ipilimumab, an immunotherapeutic agent that was approved by the US Food and Drug Administration (FDA) in 2011 for the treatment of late-stage disease.[7] Vemurafenib, also approved by the FDA in 2011, is another drug that has been found to be effective in advanced metastatic melanoma; it is indicated for patients with a V600E mutation in the BRAF gene.[8] The combination of vemurafenib and cobimetinib has been shown to improve progression-free survival compared with vemurafenib alone. Other drugs for metastatic melanoma include dabrafenib (approved 2013), for patients with the BRAF V600E mutation, and trametinib (also approved 2013), for patients with the BRAF V600E or V600K mutation.In this case, the lesion was completely excised and postoperative external beam radiation therapy of 60 Gray in 30 fractions was administered over 6 weeks using a 3-dimensional conformal technique with right and left lateral and vertex fields on linear accelerator. All the patient's neurologic symptoms were relieved with treatment and, at more than 1 year of follow-up, no recurrent neurologic problems have occurred."
],
"date": "February 11, 2022",
"figures": [],
"markdown": "# A 42-Year-Old With Declining Cognition and Frequent Vomiting\n\n **Authors:** Prasenjit Das, MD, MB BS \n **Date:** February 11, 2022\n\n ## Content\n\n Metastatic melanoma in the CNS is almost incurable. Treatment is symptomatic and involves surgical tumor debulking and symptomatic relief. The use of steroids for perilesional edema is indicated for the reduction of intracranial pressure.\nPrevious reports have found that patients with solitary primary intracranial melanoma have overall mean survival of less than 2 years, whereas patients with diffuse leptomeningeal spread have a survival of only around 6 months.[5] Rare reports describe metastasis from primary intracranial melanoma to the lungs, spleen, pancreas, and kidneys.[5]\nThe treatment options should be individualized for each patient based on the number of lesions and access to them, as well as the possibility of extracranial metastases. Radiation therapy, stereotactic radiosurgery, surgical resection, or immunologic are options.\nWhole-brain radiation treatment for either solitary or multiple brain metastases can improve neurologic deficits, as well as the patient's survival, if associated with tumor excision. Response rates vary from 37% to 100%, and the mean survival following irradiation ranges from 2 months to 7.6 months (average 3.8 months).[6] Similarly, stereotactic radiosurgery can be performed on the solitary or multiple metastatic lesions in the brain, which has the advantage of remarkably less radiotoxicity in the peritumoral brain tissue. This treatment has been shown to achieve local tumor control as well as improve the medial survival by 4-7 months.[6] Local tumor excision can improve the neurologic deficits to a great extent; however, better tumor control has been achieved when this is combined with postoperative radiation therapy.[1]\nIn order for any targeted therapy to be effective, the treatment should cross the blood-brain barrier (BBB). P-glycoprotein, a multidrug resistance protein (MRP), has been identified in the vascular endothelium, resulting in the prevention of cytotoxic drugs from entering the brain. Some agents, such as neuroattenuated herpes simplex virus 1 (HSV-1), can ease the crossing of the BBB for intracranial therapy of brain metastases. Neuroattenuated HSV-1, with a deletion in the RL1 gene, has been shown to prolong survival in mice bearing various tumors. Due to the mutation of the HSV-1 RL1 gene, this virus cannot replicate in the central nervous system; however, it does ignite the immunologic response, which, in turn, kills the tumor cells.[2] P-glycoprotein inhibitors, such as PSC-833, have been tried along with paclitaxel or vinblastin in mice, and have been shown to improve BBB penetration of these chemotherapeutic agents.\nAdvancements to ease this drug delivery include the use of nanoparticle-coated doxorubicin and liposome-containing drugs tagged with an antibody that recognizes receptors along the endothelium; other proteins, peptides, and siRNAs are also being used. Methylating agents, which impair the ability of cancer cells to divide (including dacarbazine, temozolomide [TMZ], and procarbazine) are effective in treating metastatic melanoma. Temozolomide and nitrosoureas, such as carmustine and lomustine, are known to effectively cross the BBB. Taxanes, such as docetaxel and paclitaxel, also show a low-level activity against melanoma. Corticosteroids have been used to reduce the swelling caused by brain metastases.\nApart from this, a wide array of targeted monoclonal antibodies have been tried in intracranial melanomas, including 131I, 90Y, 211At, 212Bi, 67Cu, 186Re, 188Re, 212Pb and ME1-14 F (ab2). However, these targeted therapies have been shown to increase the survival by only 1-3 months and are therefore not popular owing to the high cost-benefit ratio.[6]\nMany therapeutic options for ocular melanoma are available, including plaque radiation therapy (iodine-125, ruthenium-106, and palladium-103), brachytherapy, the use of proton- or helium-charged particles, transscleral resection, the use of a microwave heat delivery system or laser heat coagulation to accentuate the effect of radiation therapy, xenon arc photocoagulation or diode laser transpupillary thermotherapy, gamma-knife stereotactic radiosurgery, or a combination of these different modalities.[4]\nAmong the drugs available for the treatment of metastatic melanoma are ipilimumab, an immunotherapeutic agent that was approved by the US Food and Drug Administration (FDA) in 2011 for the treatment of late-stage disease.[7] Vemurafenib, also approved by the FDA in 2011, is another drug that has been found to be effective in advanced metastatic melanoma; it is indicated for patients with a V600E mutation in the BRAF gene.[8] The combination of vemurafenib and cobimetinib has been shown to improve progression-free survival compared with vemurafenib alone. Other drugs for metastatic melanoma include dabrafenib (approved 2013), for patients with the BRAF V600E mutation, and trametinib (also approved 2013), for patients with the BRAF V600E or V600K mutation.In this case, the lesion was completely excised and postoperative external beam radiation therapy of 60 Gray in 30 fractions was administered over 6 weeks using a 3-dimensional conformal technique with right and left lateral and vertex fields on linear accelerator. All the patient's neurologic symptoms were relieved with treatment and, at more than 1 year of follow-up, no recurrent neurologic problems have occurred.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 361937,
"choiceText": "They are rarely situated at the gray-white matter junction",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361938,
"choiceText": "The metastases are always multifocal lesions",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361939,
"choiceText": "A diligent clinical history is important for identifying an extracranial primary source ",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361940,
"choiceText": "This diagnosis has a generally good prognosis and survivability",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Metastatic melanoma lesions can be solitary, relatively well-delineated tumors or (most often) they can be multifocal. The role of careful history is very important to rule out a false diagnosis of primary malignant melanoma in the brain. Although metastatic lesions can be seen in any anatomic site, the most common site is the gray-white junction. Metastatic melanoma in the CNS is almost incurable. Patients with solitary primary intracranial melanomas have an overall mean survival of less than 2 years, whereas patients with diffuse leptomeningeal spread have a survival of only around 6 months.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 103390,
"questionText": "You are treating a 41-year-old patient with headaches, vomiting, and a prior history of cutaneous melanoma. You are concerned she may have metastatic melanoma lesions in her brain. Which of statement regarding CNS melanoma metastases is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 361941,
"choiceText": "Contrast-enhanced MRI",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361942,
"choiceText": "Contrast-enhanced CT scanning",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361943,
"choiceText": "Serum tumor markers",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361944,
"choiceText": "PET scanning",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "No specific indications for screening laboratory studies of patients with suspected melanomas have been clearly established; however, radiologic studies are imperative. A contrast-enhanced MRI scan is more informative than contrast-enhanced CT scans in these cases. When a metastatic melanoma is suspected based on cerebral imaging, chest radiography followed by abdominal CT scanning, radionuclide bone scanning, and PET scans are highly sensitive techniques to determine systemic metastatic malignancy.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 103391,
"questionText": "Which of the following is the most appropriate staging study to evaluate metastatic melanoma in this patient's brain?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 42-Year-Old With Declining Cognition and Frequent Vomiting"
},
{
"authors": "Prasenjit Das, MD, MB BS",
"content": [],
"date": "February 11, 2022",
"figures": [],
"markdown": "# A 42-Year-Old With Declining Cognition and Frequent Vomiting\n\n **Authors:** Prasenjit Das, MD, MB BS \n **Date:** February 11, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 361937,
"choiceText": "They are rarely situated at the gray-white matter junction",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361938,
"choiceText": "The metastases are always multifocal lesions",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361939,
"choiceText": "A diligent clinical history is important for identifying an extracranial primary source ",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361940,
"choiceText": "This diagnosis has a generally good prognosis and survivability",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Metastatic melanoma lesions can be solitary, relatively well-delineated tumors or (most often) they can be multifocal. The role of careful history is very important to rule out a false diagnosis of primary malignant melanoma in the brain. Although metastatic lesions can be seen in any anatomic site, the most common site is the gray-white junction. Metastatic melanoma in the CNS is almost incurable. Patients with solitary primary intracranial melanomas have an overall mean survival of less than 2 years, whereas patients with diffuse leptomeningeal spread have a survival of only around 6 months.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 103390,
"questionText": "You are treating a 41-year-old patient with headaches, vomiting, and a prior history of cutaneous melanoma. You are concerned she may have metastatic melanoma lesions in her brain. Which of statement regarding CNS melanoma metastases is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 361941,
"choiceText": "Contrast-enhanced MRI",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361942,
"choiceText": "Contrast-enhanced CT scanning",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361943,
"choiceText": "Serum tumor markers",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361944,
"choiceText": "PET scanning",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "No specific indications for screening laboratory studies of patients with suspected melanomas have been clearly established; however, radiologic studies are imperative. A contrast-enhanced MRI scan is more informative than contrast-enhanced CT scans in these cases. When a metastatic melanoma is suspected based on cerebral imaging, chest radiography followed by abdominal CT scanning, radionuclide bone scanning, and PET scans are highly sensitive techniques to determine systemic metastatic malignancy.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 103391,
"questionText": "Which of the following is the most appropriate staging study to evaluate metastatic melanoma in this patient's brain?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 42-Year-Old With Declining Cognition and Frequent Vomiting"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 361933,
"choiceText": "Glioblastoma",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361934,
"choiceText": "Choroid plexus papilloma",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361935,
"choiceText": "Retinoblastoma",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361936,
"choiceText": "Metastatic melanoma",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 103389,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 361937,
"choiceText": "They are rarely situated at the gray-white matter junction",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361938,
"choiceText": "The metastases are always multifocal lesions",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361939,
"choiceText": "A diligent clinical history is important for identifying an extracranial primary source ",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361940,
"choiceText": "This diagnosis has a generally good prognosis and survivability",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Metastatic melanoma lesions can be solitary, relatively well-delineated tumors or (most often) they can be multifocal. The role of careful history is very important to rule out a false diagnosis of primary malignant melanoma in the brain. Although metastatic lesions can be seen in any anatomic site, the most common site is the gray-white junction. Metastatic melanoma in the CNS is almost incurable. Patients with solitary primary intracranial melanomas have an overall mean survival of less than 2 years, whereas patients with diffuse leptomeningeal spread have a survival of only around 6 months.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 103390,
"questionText": "You are treating a 41-year-old patient with headaches, vomiting, and a prior history of cutaneous melanoma. You are concerned she may have metastatic melanoma lesions in her brain. Which of statement regarding CNS melanoma metastases is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 361941,
"choiceText": "Contrast-enhanced MRI",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361942,
"choiceText": "Contrast-enhanced CT scanning",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361943,
"choiceText": "Serum tumor markers",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 361944,
"choiceText": "PET scanning",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "No specific indications for screening laboratory studies of patients with suspected melanomas have been clearly established; however, radiologic studies are imperative. A contrast-enhanced MRI scan is more informative than contrast-enhanced CT scans in these cases. When a metastatic melanoma is suspected based on cerebral imaging, chest radiography followed by abdominal CT scanning, radionuclide bone scanning, and PET scans are highly sensitive techniques to determine systemic metastatic malignancy.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 103391,
"questionText": "Which of the following is the most appropriate staging study to evaluate metastatic melanoma in this patient's brain?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
729365 | /viewarticle/729365 | [
{
"authors": "Mehtap Cakir, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 55-year-old man presents with a 2-day history of nausea and vomiting. He has been seen a few times in the gastroenterology clinic during the past 6 months for similar symptoms. Multivitamins, antacids, and proton-pump inhibitors had been prescribed but failed to control his symptoms. He has no history of trauma, weight loss, fever, dyspnea, abdominal pain, hematemesis, diarrhea, constipation, or peripheral edema.",
"Six years ago, he was diagnosed with type 2 diabetes and was prescribed an oral agent and a long-acting insulin. Although he was nonadherent to his recommended diet, he used his medications as prescribed. Four years ago, the patient began experiencing hypoglycemic episodes even though his daily activity and diet had not changed and his weight had remained stable. From that point on, he gradually tapered his insulin use and eventually stopped both insulin and his oral medication. Following that, occasional fingerstick glucose measurements were reportedly normal. He does not smoke tobacco, drink alcohol, or use illicit drugs. When further queried about his medical history and review of systems, he reports having a decreased libido and impotence for 3 years."
],
"date": "February 08, 2022",
"figures": [],
"markdown": "# Endocrinology Case Challenge: A 55-Year-Old With Impotence, Decreased Libido, and Hyponatremia\n\n **Authors:** Mehtap Cakir, MD \n **Date:** February 08, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 55-year-old man presents with a 2-day history of nausea and vomiting. He has been seen a few times in the gastroenterology clinic during the past 6 months for similar symptoms. Multivitamins, antacids, and proton-pump inhibitors had been prescribed but failed to control his symptoms. He has no history of trauma, weight loss, fever, dyspnea, abdominal pain, hematemesis, diarrhea, constipation, or peripheral edema.\nSix years ago, he was diagnosed with type 2 diabetes and was prescribed an oral agent and a long-acting insulin. Although he was nonadherent to his recommended diet, he used his medications as prescribed. Four years ago, the patient began experiencing hypoglycemic episodes even though his daily activity and diet had not changed and his weight had remained stable. From that point on, he gradually tapered his insulin use and eventually stopped both insulin and his oral medication. Following that, occasional fingerstick glucose measurements were reportedly normal. He does not smoke tobacco, drink alcohol, or use illicit drugs. When further queried about his medical history and review of systems, he reports having a decreased libido and impotence for 3 years.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Endocrinology Case Challenge: A 55-Year-Old With Impotence, Decreased Libido, and Hyponatremia"
},
{
"authors": "Mehtap Cakir, MD",
"content": [
"Upon physical examination, the patient's axillary temperature is 97.7ºF (36.5ºC). His pulse has a regular rhythm, with a heart rate of 62 beats/min. His blood pressure is 100/70 mm Hg. He appears apathetic and unwell. Head and neck examination reveals fine wrinkling of the perioral skin. His lungs are clear. His S1 and S2 heart sounds are normal. His abdomen is soft and nontender, and his peripheral pulses are weakly palpable.",
"Laboratory analysis reveals normochromic normocytic anemia, with a hemoglobin level of 11.8 g/dL (118 g/L; reference range, 13.5-18 g/dL), a hematocrit of 34% (0.34; reference range, 40%-54%) and a mean corpuscular volume of 91 μm3 (91 fL; reference range, 80-96 μm3). The remainder of the CBC count is normal, as are urinalysis findings and random blood glucose level.",
"The patient's renal function and liver function tests are normal. He has hyponatremia, with a serum sodium of 126 mEq/L (126 mmol/L; reference range of 136-145 mEq/L). His serum potassium level is normal. The patient is hospitalized for further evaluation of his hyponatremia and progressive symptoms. Cranial MRI is obtained (see below).",
"Figure 1.",
"Figure 1.",
"Figure 2.",
"Figure 2.",
"Figure 3.",
"Figure 3."
],
"date": "February 08, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/729/001/729001-thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/729/001/729001-thumb2.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/729/001/729001-thumb3.png"
}
],
"markdown": "# Endocrinology Case Challenge: A 55-Year-Old With Impotence, Decreased Libido, and Hyponatremia\n\n **Authors:** Mehtap Cakir, MD \n **Date:** February 08, 2022\n\n ## Content\n\n Upon physical examination, the patient's axillary temperature is 97.7ºF (36.5ºC). His pulse has a regular rhythm, with a heart rate of 62 beats/min. His blood pressure is 100/70 mm Hg. He appears apathetic and unwell. Head and neck examination reveals fine wrinkling of the perioral skin. His lungs are clear. His S1 and S2 heart sounds are normal. His abdomen is soft and nontender, and his peripheral pulses are weakly palpable.\nLaboratory analysis reveals normochromic normocytic anemia, with a hemoglobin level of 11.8 g/dL (118 g/L; reference range, 13.5-18 g/dL), a hematocrit of 34% (0.34; reference range, 40%-54%) and a mean corpuscular volume of 91 μm3 (91 fL; reference range, 80-96 μm3). The remainder of the CBC count is normal, as are urinalysis findings and random blood glucose level.\nThe patient's renal function and liver function tests are normal. He has hyponatremia, with a serum sodium of 126 mEq/L (126 mmol/L; reference range of 136-145 mEq/L). His serum potassium level is normal. The patient is hospitalized for further evaluation of his hyponatremia and progressive symptoms. Cranial MRI is obtained (see below).\nFigure 1.\nFigure 1.\nFigure 2.\nFigure 2.\nFigure 3.\nFigure 3.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 368110,
"choiceText": "Hypothyroidism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368111,
"choiceText": "Electrolyte loss due to vomiting",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368112,
"choiceText": "Hypopituitarism due to empty sella syndrome",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368113,
"choiceText": "Primary adrenal insufficiency",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 105503,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Endocrinology Case Challenge: A 55-Year-Old With Impotence, Decreased Libido, and Hyponatremia"
},
{
"authors": "Mehtap Cakir, MD",
"content": [
"The diagnosis of hypopituitarism resulting in hyponatremia was made on the basis of the patient's history, physical examination, and laboratory investigation. The fact that the patient had been able to reduce, and then stop using, his diabetes medications is notable. Hypoglycemia may be a clue to the development of hypoadrenalism or hypothyroidism in diabetic patients. This patient's decreased libido and impotence were probably due to gonadal failure; the fine wrinkles around his mouth were a sign of hypogonadism. The absence of both hyperkalemia and mucosal hyperpigmentation suggested secondary hypoadrenalism.",
"The patient's pituitary hormone levels were evaluated; his morning pituitary hormone profile was compatible with panhypopituitarism, with severe deficiencies in all hypothalamopituitary axes. Findings were as follows:",
"Insulin-like growth factor-1 (IGF-1) level - 62 ng/mL (62 μg/L; reference range, 78-258 ng/mL)",
"Growth hormone (GH) level - < 0.01 ng/mL (< 0.01 μg/L; reference range, <10 ng/mL)",
"Free thyroxine (T4) level - 0.39 ng/dL (5.02 pmol/L; reference range, 0.93-1.7 ng/dL)",
"Thyroid-stimulating hormone (TSH) level - 2.35 μIU/mL (2.35 μIU/L; reference range, 0.35-5.5 μIU/mL)",
"Follicle-stimulating hormone level - 0.94 mIU/mL (0.94 IU/L; reference range, 1.5-12.4 mIU/mL)",
"Luteinizing hormone level - 0.36 mIU/mL (0.36 IU/L; reference range, 1.7-8.6 mIU/mL)",
"Free testosterone level - 0.3 pg/mL (10.35 pmol/L; reference range, 8.69-54.69 pg/mL)",
"Cortisol level - 4.5 μg/dL (124.2 nmol/L; reference range, 6.2-19.4 μg/dL)",
"Prolactin level - 1.65 ng/mL (1.65 μg/L; reference range, 4-15.2 ng/mL)"
],
"date": "February 08, 2022",
"figures": [],
"markdown": "# Endocrinology Case Challenge: A 55-Year-Old With Impotence, Decreased Libido, and Hyponatremia\n\n **Authors:** Mehtap Cakir, MD \n **Date:** February 08, 2022\n\n ## Content\n\n The diagnosis of hypopituitarism resulting in hyponatremia was made on the basis of the patient's history, physical examination, and laboratory investigation. The fact that the patient had been able to reduce, and then stop using, his diabetes medications is notable. Hypoglycemia may be a clue to the development of hypoadrenalism or hypothyroidism in diabetic patients. This patient's decreased libido and impotence were probably due to gonadal failure; the fine wrinkles around his mouth were a sign of hypogonadism. The absence of both hyperkalemia and mucosal hyperpigmentation suggested secondary hypoadrenalism.\nThe patient's pituitary hormone levels were evaluated; his morning pituitary hormone profile was compatible with panhypopituitarism, with severe deficiencies in all hypothalamopituitary axes. Findings were as follows:\nInsulin-like growth factor-1 (IGF-1) level - 62 ng/mL (62 μg/L; reference range, 78-258 ng/mL)\nGrowth hormone (GH) level - < 0.01 ng/mL (< 0.01 μg/L; reference range, <10 ng/mL)\nFree thyroxine (T4) level - 0.39 ng/dL (5.02 pmol/L; reference range, 0.93-1.7 ng/dL)\nThyroid-stimulating hormone (TSH) level - 2.35 μIU/mL (2.35 μIU/L; reference range, 0.35-5.5 μIU/mL)\nFollicle-stimulating hormone level - 0.94 mIU/mL (0.94 IU/L; reference range, 1.5-12.4 mIU/mL)\nLuteinizing hormone level - 0.36 mIU/mL (0.36 IU/L; reference range, 1.7-8.6 mIU/mL)\nFree testosterone level - 0.3 pg/mL (10.35 pmol/L; reference range, 8.69-54.69 pg/mL)\nCortisol level - 4.5 μg/dL (124.2 nmol/L; reference range, 6.2-19.4 μg/dL)\nProlactin level - 1.65 ng/mL (1.65 μg/L; reference range, 4-15.2 ng/mL)\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 368110,
"choiceText": "Hypothyroidism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368111,
"choiceText": "Electrolyte loss due to vomiting",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368112,
"choiceText": "Hypopituitarism due to empty sella syndrome",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368113,
"choiceText": "Primary adrenal insufficiency",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 105503,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Endocrinology Case Challenge: A 55-Year-Old With Impotence, Decreased Libido, and Hyponatremia"
},
{
"authors": "Mehtap Cakir, MD",
"content": [
"A low free T4 level with an inappropriately normal TSH level is the hallmark of secondary hypothyroidism.[1] The same pattern may be seen in the gonadal axis, although this patient had a low testosterone level and low luteinizing hormone and follicle-stimulating hormone levels. Basal cortisol levels less than 5 μg/dL (138 nmol/L) are diagnostic of adrenal insufficiency, and stimulation tests are unnecessary. Prolactin deficiency is exceedingly rare; when present, it suggests complete pituitary destruction.[1] GH deficiency can be diagnosed without stimulation tests when there are deficiencies of 3 or more hypothalamopituitary axes. A low IGF-1 level for age and sex is also diagnostic of GH deficiency.",
"To identify the etiology of hypopituitarism, cranial MRI was performed. Coronal T2-weighted and sagittal and coronal T1-weighted scans revealed what is commonly described as an \"empty sella\" (Figures 1-3).",
"Figure 1.",
"Figure 1.",
"Figure 2.",
"Figure 2.",
"Figure 3.",
"Figure 3.",
"Empty sella is a condition in which the pituitary gland becomes compressed or flattened and the sella turcica appears empty on MRI. The term \"empty sella\" is a misnomer; the space is typically filled with cerebrospinal fluid. The condition has various causes, including anatomical defect, injury, tumor, and radiation therapy. The condition may be clinically asymptomatic.",
"Hyponatremia is defined as a serum sodium level <130 mmol/L. This is the most common electrolyte abnormality in hospitalized patients; the prevalence is 1%-46%, depending on the clinical setting, patient population, and the serum sodium level used to define it.[2,3] The rate at which hyponatremia develops is critical because the etiology and treatment of acute and chronic hyponatremia differs. Acute hyponatremia, which develops in less than 48 hours, is generally hospital-acquired and iatrogenic (although there are exceptions).",
"Chronic hyponatremia, which develops over more than 48 hours, is more likely to occur outside the hospital. Most symptoms of acute hyponatremia are neurologic, developing because of water movement into brain tissue, with resultant edema and reduction of brain osmolality.[3] Headache, nausea, vomiting, lethargy, confusion, and muscle cramps may be present in either mild cases of hyponatremia or when it develops slowly.[3] Chronic hyponatremia is particularly common in elderly persons and postmenopausal women.[3] Given the ability of the brain to adapt to hypo-osmolality, chronic hyponatremia is generally better tolerated than rapid-onset hyponatremia.",
"The etiology of hyponatremia includes renal, cardiac, hepatic, endocrine, and other conditions.[2] Hyponatremia may also be broadly considered to result from sodium depletion, excess water intake, or reduced renal free water clearance.[2] Sodium depletion may be due to extrarenal or renal volume loss. Conditions that cause extrarenal losses include burns, excessive perspiration, vomiting, and diarrhea. Renal volume loss may result from diuretic use, salt-wasting nephropathy, cerebral salt-wasting, and hypoadrenalism. Excess water intake can result from dipsogenic diabetes insipidus or the use of sodium-free, hypo-osmolar irrigating solutions. Reduced renal free water clearance may result from hypovolemia, cardiac failure, nephrotic syndrome, hypothyroidism, hypoadrenalism, syndrome of inappropriate antidiuresis hormone secretion, drugs, portal hypertension and ascites, renal failure, and hypoalbuminemia.[2,4]"
],
"date": "February 08, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/729/001/729001-thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/729/001/729001-thumb2.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/729/001/729001-thumb3.png"
}
],
"markdown": "# Endocrinology Case Challenge: A 55-Year-Old With Impotence, Decreased Libido, and Hyponatremia\n\n **Authors:** Mehtap Cakir, MD \n **Date:** February 08, 2022\n\n ## Content\n\n A low free T4 level with an inappropriately normal TSH level is the hallmark of secondary hypothyroidism.[1] The same pattern may be seen in the gonadal axis, although this patient had a low testosterone level and low luteinizing hormone and follicle-stimulating hormone levels. Basal cortisol levels less than 5 μg/dL (138 nmol/L) are diagnostic of adrenal insufficiency, and stimulation tests are unnecessary. Prolactin deficiency is exceedingly rare; when present, it suggests complete pituitary destruction.[1] GH deficiency can be diagnosed without stimulation tests when there are deficiencies of 3 or more hypothalamopituitary axes. A low IGF-1 level for age and sex is also diagnostic of GH deficiency.\nTo identify the etiology of hypopituitarism, cranial MRI was performed. Coronal T2-weighted and sagittal and coronal T1-weighted scans revealed what is commonly described as an \"empty sella\" (Figures 1-3).\nFigure 1.\nFigure 1.\nFigure 2.\nFigure 2.\nFigure 3.\nFigure 3.\nEmpty sella is a condition in which the pituitary gland becomes compressed or flattened and the sella turcica appears empty on MRI. The term \"empty sella\" is a misnomer; the space is typically filled with cerebrospinal fluid. The condition has various causes, including anatomical defect, injury, tumor, and radiation therapy. The condition may be clinically asymptomatic.\nHyponatremia is defined as a serum sodium level <130 mmol/L. This is the most common electrolyte abnormality in hospitalized patients; the prevalence is 1%-46%, depending on the clinical setting, patient population, and the serum sodium level used to define it.[2,3] The rate at which hyponatremia develops is critical because the etiology and treatment of acute and chronic hyponatremia differs. Acute hyponatremia, which develops in less than 48 hours, is generally hospital-acquired and iatrogenic (although there are exceptions).\nChronic hyponatremia, which develops over more than 48 hours, is more likely to occur outside the hospital. Most symptoms of acute hyponatremia are neurologic, developing because of water movement into brain tissue, with resultant edema and reduction of brain osmolality.[3] Headache, nausea, vomiting, lethargy, confusion, and muscle cramps may be present in either mild cases of hyponatremia or when it develops slowly.[3] Chronic hyponatremia is particularly common in elderly persons and postmenopausal women.[3] Given the ability of the brain to adapt to hypo-osmolality, chronic hyponatremia is generally better tolerated than rapid-onset hyponatremia.\nThe etiology of hyponatremia includes renal, cardiac, hepatic, endocrine, and other conditions.[2] Hyponatremia may also be broadly considered to result from sodium depletion, excess water intake, or reduced renal free water clearance.[2] Sodium depletion may be due to extrarenal or renal volume loss. Conditions that cause extrarenal losses include burns, excessive perspiration, vomiting, and diarrhea. Renal volume loss may result from diuretic use, salt-wasting nephropathy, cerebral salt-wasting, and hypoadrenalism. Excess water intake can result from dipsogenic diabetes insipidus or the use of sodium-free, hypo-osmolar irrigating solutions. Reduced renal free water clearance may result from hypovolemia, cardiac failure, nephrotic syndrome, hypothyroidism, hypoadrenalism, syndrome of inappropriate antidiuresis hormone secretion, drugs, portal hypertension and ascites, renal failure, and hypoalbuminemia.[2,4]\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n\n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Endocrinology Case Challenge: A 55-Year-Old With Impotence, Decreased Libido, and Hyponatremia"
},
{
"authors": "Mehtap Cakir, MD",
"content": [
"To narrow the differential diagnosis for hyponatremia, a complete medical history and review of systems should be obtained, followed by a thorough physical examination. The patient should be questioned about the use of diuretics and other drugs, including sulfonylureas, tricyclic antidepressants, vinca alkaloids, cyclophosphamide, dopamine agonists, selective serotonin reuptake inhibitors, opiates, phenothiazines, thioxanthenes, haloperidol, MDMA (\"ecstasy\"), chlorpropamide, cyclophosphamide, nonsteroidal anti-inflammatory drugs, acetaminophen, clofibrate, carbamazepine, and melphalan.[5] Information about the patient's daily water intake; possible renal, hepatic, or cardiac disease; possible diarrhea and vomiting; and possible history of trauma, radiotherapy, or surgery should also be obtained. Dyspnea, nocturia, and the presence of edema may provide additional clues about associated renal, cardiac, and hepatic disease.",
"Physical findings that suggest the presence of hypervolemia include rales, an S3 gallop, edema, and ascites. Mucosal hyperpigmentation is a sign of primary adrenal insufficiency. Hyperpigmentation is found in primary adrenal insufficiency because increased adrenocorticotropic hormone production leads to hyperstimulation of skin melanocytes. This does not occur in secondary adrenal insufficiency because secretion of adrenocorticotropic hormone is lost owing to pituitary destruction. Patients with hypothyroidism may have hoarseness, dry skin, an apathetic appearance, and periorbital edema.",
"The laboratory evaluation of hyponatremia should start by eliminating pseudohyponatremia due to hyperlipidemia, hyperglycemia, and hyperproteinemia as potential causes of a falsely low serum sodium level.[5] Once this entity is ruled out, further laboratory evaluation includes renal and liver function tests and measurement of serum electrolytes, serum osmolality, free T4, TSH, and cortisol.[6] Urinalysis, urinary osmolality, and electrocardiography are also useful diagnostic studies. Further evaluation is directed by the results of these basic tests.",
"Potassium is an important test for differentiating primary from secondary adrenal insufficiency. The potassium is elevated in primary adrenal insufficiency because aldosterone secretion from the adrenal gland is lost; however, it is normal in secondary adrenal insufficiency because the renin-angiotensin-aldosterone axis remains intact, thereby allowing normal potassium excretion.",
"Hypopituitarism may be overlooked in the broad differential diagnosis of hyponatremia. Several case reports and case series describe patients with hypopituitarism who are admitted to the hospital with hyponatremia.[7,8] Empty sella syndrome, pituitary surgery, pituitary radiotherapy, pituitary tumors, Sheehan syndrome, and other conditions can cause hypopituitarism.[1] This patient's hypopituitarism was due to empty sella syndrome.",
"Both hypothyroidism and adrenal failure contribute to hyponatremia in hypopituitarism. In hypothyroidism, free water clearance is reduced.[5] Plasma vasopressin levels are paradoxically normal or increased despite hypo-osmolality in hyponatremic patients with secondary adrenal failure.[5] Glucocorticoid deficiency also impairs the ability to excrete a water load appropriately.[5]",
"In patients with hypopituitarism and hypothyroidism, treatment with corticosteroids should be started before thyroid hormone replacement is started. Replacing thyroid hormone first increases glucocorticoid requirements during physiological stress, which could precipitate an adrenal crisis.[1]",
"In the patient in this case, intravenous corticosteroid and controlled fluid replacement were given first. Intravenous 3% hypertonic saline was not used because hyponatremia was chronic and mild, and the patient's mental status was relatively normal. On day 3 of corticosteroid replacement, thyroid hormone treatment was started with low-dose L-thyroxine; the dose was gradually increased. The patient's serum sodium level slowly normalized. His hospital discharge medications included oral prednisolone, thyroid hormone, and intramuscular testosterone."
],
"date": "February 08, 2022",
"figures": [],
"markdown": "# Endocrinology Case Challenge: A 55-Year-Old With Impotence, Decreased Libido, and Hyponatremia\n\n **Authors:** Mehtap Cakir, MD \n **Date:** February 08, 2022\n\n ## Content\n\n To narrow the differential diagnosis for hyponatremia, a complete medical history and review of systems should be obtained, followed by a thorough physical examination. The patient should be questioned about the use of diuretics and other drugs, including sulfonylureas, tricyclic antidepressants, vinca alkaloids, cyclophosphamide, dopamine agonists, selective serotonin reuptake inhibitors, opiates, phenothiazines, thioxanthenes, haloperidol, MDMA (\"ecstasy\"), chlorpropamide, cyclophosphamide, nonsteroidal anti-inflammatory drugs, acetaminophen, clofibrate, carbamazepine, and melphalan.[5] Information about the patient's daily water intake; possible renal, hepatic, or cardiac disease; possible diarrhea and vomiting; and possible history of trauma, radiotherapy, or surgery should also be obtained. Dyspnea, nocturia, and the presence of edema may provide additional clues about associated renal, cardiac, and hepatic disease.\nPhysical findings that suggest the presence of hypervolemia include rales, an S3 gallop, edema, and ascites. Mucosal hyperpigmentation is a sign of primary adrenal insufficiency. Hyperpigmentation is found in primary adrenal insufficiency because increased adrenocorticotropic hormone production leads to hyperstimulation of skin melanocytes. This does not occur in secondary adrenal insufficiency because secretion of adrenocorticotropic hormone is lost owing to pituitary destruction. Patients with hypothyroidism may have hoarseness, dry skin, an apathetic appearance, and periorbital edema.\nThe laboratory evaluation of hyponatremia should start by eliminating pseudohyponatremia due to hyperlipidemia, hyperglycemia, and hyperproteinemia as potential causes of a falsely low serum sodium level.[5] Once this entity is ruled out, further laboratory evaluation includes renal and liver function tests and measurement of serum electrolytes, serum osmolality, free T4, TSH, and cortisol.[6] Urinalysis, urinary osmolality, and electrocardiography are also useful diagnostic studies. Further evaluation is directed by the results of these basic tests.\nPotassium is an important test for differentiating primary from secondary adrenal insufficiency. The potassium is elevated in primary adrenal insufficiency because aldosterone secretion from the adrenal gland is lost; however, it is normal in secondary adrenal insufficiency because the renin-angiotensin-aldosterone axis remains intact, thereby allowing normal potassium excretion.\nHypopituitarism may be overlooked in the broad differential diagnosis of hyponatremia. Several case reports and case series describe patients with hypopituitarism who are admitted to the hospital with hyponatremia.[7,8] Empty sella syndrome, pituitary surgery, pituitary radiotherapy, pituitary tumors, Sheehan syndrome, and other conditions can cause hypopituitarism.[1] This patient's hypopituitarism was due to empty sella syndrome.\nBoth hypothyroidism and adrenal failure contribute to hyponatremia in hypopituitarism. In hypothyroidism, free water clearance is reduced.[5] Plasma vasopressin levels are paradoxically normal or increased despite hypo-osmolality in hyponatremic patients with secondary adrenal failure.[5] Glucocorticoid deficiency also impairs the ability to excrete a water load appropriately.[5]\nIn patients with hypopituitarism and hypothyroidism, treatment with corticosteroids should be started before thyroid hormone replacement is started. Replacing thyroid hormone first increases glucocorticoid requirements during physiological stress, which could precipitate an adrenal crisis.[1]\nIn the patient in this case, intravenous corticosteroid and controlled fluid replacement were given first. Intravenous 3% hypertonic saline was not used because hyponatremia was chronic and mild, and the patient's mental status was relatively normal. On day 3 of corticosteroid replacement, thyroid hormone treatment was started with low-dose L-thyroxine; the dose was gradually increased. The patient's serum sodium level slowly normalized. His hospital discharge medications included oral prednisolone, thyroid hormone, and intramuscular testosterone.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 368114,
"choiceText": "Normal IGF-1",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368115,
"choiceText": "Low serum cortisol",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368116,
"choiceText": "Low serum testosterone",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368117,
"choiceText": "Low free T4, normal TSH",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Low free T4 combined with a so-called “inappropriately” normal TSH level is diagnostic of secondary hypothyroidism. Low serum cortisol levels can be seen in both primary and secondary adrenal insufficiency. The same is true for low testosterone levels which can occur in both primary and secondary gonadal failure. Differentiating between primary and secondary gonadal failure is impossible without knowing the pituitary hormone levels. A normal IGF-1 level is not suggestive of hypopituitarism.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 105504,
"questionText": "Which laboratory abnormality suggests a secondary hormonal deficiency?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 368118,
"choiceText": "Hypoadrenalism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368119,
"choiceText": "Hypothyroidism",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368120,
"choiceText": "Syndrome of inappropriate antidiuresis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368121,
"choiceText": "Diuretic use",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368122,
"choiceText": "Heart failure",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Diuretic use causes hyponatremia by renal sodium loss. In all other conditions, renal free water clearance is reduced.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 105505,
"questionText": "Which of these etiologies causes hyponatremia due to sodium depletion?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Endocrinology Case Challenge: A 55-Year-Old With Impotence, Decreased Libido, and Hyponatremia"
},
{
"authors": "Mehtap Cakir, MD",
"content": [],
"date": "February 08, 2022",
"figures": [],
"markdown": "# Endocrinology Case Challenge: A 55-Year-Old With Impotence, Decreased Libido, and Hyponatremia\n\n **Authors:** Mehtap Cakir, MD \n **Date:** February 08, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 368114,
"choiceText": "Normal IGF-1",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368115,
"choiceText": "Low serum cortisol",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368116,
"choiceText": "Low serum testosterone",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368117,
"choiceText": "Low free T4, normal TSH",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Low free T4 combined with a so-called “inappropriately” normal TSH level is diagnostic of secondary hypothyroidism. Low serum cortisol levels can be seen in both primary and secondary adrenal insufficiency. The same is true for low testosterone levels which can occur in both primary and secondary gonadal failure. Differentiating between primary and secondary gonadal failure is impossible without knowing the pituitary hormone levels. A normal IGF-1 level is not suggestive of hypopituitarism.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 105504,
"questionText": "Which laboratory abnormality suggests a secondary hormonal deficiency?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 368118,
"choiceText": "Hypoadrenalism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368119,
"choiceText": "Hypothyroidism",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368120,
"choiceText": "Syndrome of inappropriate antidiuresis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368121,
"choiceText": "Diuretic use",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368122,
"choiceText": "Heart failure",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Diuretic use causes hyponatremia by renal sodium loss. In all other conditions, renal free water clearance is reduced.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 105505,
"questionText": "Which of these etiologies causes hyponatremia due to sodium depletion?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Endocrinology Case Challenge: A 55-Year-Old With Impotence, Decreased Libido, and Hyponatremia"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 368110,
"choiceText": "Hypothyroidism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368111,
"choiceText": "Electrolyte loss due to vomiting",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368112,
"choiceText": "Hypopituitarism due to empty sella syndrome",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368113,
"choiceText": "Primary adrenal insufficiency",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 105503,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 368114,
"choiceText": "Normal IGF-1",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368115,
"choiceText": "Low serum cortisol",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368116,
"choiceText": "Low serum testosterone",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368117,
"choiceText": "Low free T4, normal TSH",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Low free T4 combined with a so-called “inappropriately” normal TSH level is diagnostic of secondary hypothyroidism. Low serum cortisol levels can be seen in both primary and secondary adrenal insufficiency. The same is true for low testosterone levels which can occur in both primary and secondary gonadal failure. Differentiating between primary and secondary gonadal failure is impossible without knowing the pituitary hormone levels. A normal IGF-1 level is not suggestive of hypopituitarism.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 105504,
"questionText": "Which laboratory abnormality suggests a secondary hormonal deficiency?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 368118,
"choiceText": "Hypoadrenalism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368119,
"choiceText": "Hypothyroidism",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368120,
"choiceText": "Syndrome of inappropriate antidiuresis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368121,
"choiceText": "Diuretic use",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 368122,
"choiceText": "Heart failure",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Diuretic use causes hyponatremia by renal sodium loss. In all other conditions, renal free water clearance is reduced.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 105505,
"questionText": "Which of these etiologies causes hyponatremia due to sodium depletion?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
898100 | /viewarticle/898100 | [
{
"authors": "Jaime Shalkow, MD; Mayela E. García",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"The parents of a 5-month-old boy rush him to the emergency department (ED) in the middle of the night due to recent lethargy and severe abdominal distention. Prenatal ultrasonography findings were normal; he was born at 36 weeks' gestation via uncomplicated vaginal delivery, weighed 5.73 lb (2.6 kg), and was discharged home with his parents.",
"During the infant's first 3 months of life, he fed and grew properly, with normal development. Six weeks before the current episode, he developed sudden abdominal distention and decreased oral intake, with occasional postprandial vomiting of gastric contents, with no other major symptoms. Plain radiography revealed a large opacity on the right side of the abdomen (Figure 1). Doppler ultrasonography revealed a large, nonvascularized cystic mass on the undersurface of the liver (Figure 2). CT and MRI confirmed the presence of a large, septated, cystic mass under the liver, displacing the ascending colon downward (Figures 3-5).",
"Figure 1.",
"Figure 2.",
"Figure 3.",
"Figure 4.",
"Figure 5.",
"The patient's serum alpha-fetoprotein (AFP) level was 900 ng/mL. The rest of the blood work, including liver function, was normal. At the initial institution, abdominal lymphatic malformation was diagnosed, and the patient underwent fluoroscopy-guided percutaneous sclerosis of the lesion with doxycycline (Figure 6).",
"Figure 6.",
"Staples were used to fix the cyst to the abdominal wall in order to avoid drug leakage into the peritoneum. The patient was discharged home the next morning in good condition. After 3 weeks, abdominal distention and hyporexia persisted, and he was started on sildenafil (0.5 mg/kg/day) in an attempt to accelerate the clinical response. Two days later, the boy suddenly became unresponsive, flaccid, and pale, which is when his parents rushed him to the ED.",
"Staples were used to fix the cyst to the abdominal wall in order to avoid drug leakage into the peritoneum. The patient was discharged home the next morning in good condition. After 3 weeks, abdominal distention and hyporexia persisted, and he was started on sildenafil (0.5 mg/kg/day) in an attempt to accelerate the clinical response. Two days later, the boy suddenly became unresponsive, flaccid, and pale, which is when his parents rushed him to the ED."
],
"date": "February 08, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/898/100/898100-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/898/100/898100-Thumb2.jpg"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/898/100/898100-Thumb3.png"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/898/100/898100-Thumb4.png"
},
{
"caption": "Figure 5.",
"image_url": "https://img.medscapestatic.com/article/898/100/898100-Thumb5.jpg"
},
{
"caption": "Figure 6.",
"image_url": "https://img.medscapestatic.com/article/898/100/898100-Thumb6.jpg"
}
],
"markdown": "# 5-Month-Old Rushed to the ED for Severe Abdominal Distention\n\n **Authors:** Jaime Shalkow, MD; Mayela E. García \n **Date:** February 08, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nThe parents of a 5-month-old boy rush him to the emergency department (ED) in the middle of the night due to recent lethargy and severe abdominal distention. Prenatal ultrasonography findings were normal; he was born at 36 weeks' gestation via uncomplicated vaginal delivery, weighed 5.73 lb (2.6 kg), and was discharged home with his parents.\nDuring the infant's first 3 months of life, he fed and grew properly, with normal development. Six weeks before the current episode, he developed sudden abdominal distention and decreased oral intake, with occasional postprandial vomiting of gastric contents, with no other major symptoms. Plain radiography revealed a large opacity on the right side of the abdomen (Figure 1). Doppler ultrasonography revealed a large, nonvascularized cystic mass on the undersurface of the liver (Figure 2). CT and MRI confirmed the presence of a large, septated, cystic mass under the liver, displacing the ascending colon downward (Figures 3-5).\nFigure 1.\nFigure 2.\nFigure 3.\nFigure 4.\nFigure 5.\nThe patient's serum alpha-fetoprotein (AFP) level was 900 ng/mL. The rest of the blood work, including liver function, was normal. At the initial institution, abdominal lymphatic malformation was diagnosed, and the patient underwent fluoroscopy-guided percutaneous sclerosis of the lesion with doxycycline (Figure 6).\nFigure 6.\nStaples were used to fix the cyst to the abdominal wall in order to avoid drug leakage into the peritoneum. The patient was discharged home the next morning in good condition. After 3 weeks, abdominal distention and hyporexia persisted, and he was started on sildenafil (0.5 mg/kg/day) in an attempt to accelerate the clinical response. Two days later, the boy suddenly became unresponsive, flaccid, and pale, which is when his parents rushed him to the ED.\nStaples were used to fix the cyst to the abdominal wall in order to avoid drug leakage into the peritoneum. The patient was discharged home the next morning in good condition. After 3 weeks, abdominal distention and hyporexia persisted, and he was started on sildenafil (0.5 mg/kg/day) in an attempt to accelerate the clinical response. Two days later, the boy suddenly became unresponsive, flaccid, and pale, which is when his parents rushed him to the ED.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4.** \n \n\n**Figure 5.** \n \n\n**Figure 6.** \n \n\n\n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "5-Month-Old Rushed to the ED for Severe Abdominal Distention"
},
{
"authors": "Jaime Shalkow, MD; Mayela E. García",
"content": [
"Upon arrival to the hospital, the child looks extremely ill. He is immediately admitted to the ED shock room. He is very pale, flaccid, and unresponsive. The anterior fontanel is depressed, and his skin and mucous membranes are dry. Peripheral pulses (extremities) are not felt, but his carotid and femoral pulses are weak, with evident tachysphygmia. His heart rate is 210 beats/min, his respiratory rate is 45 breaths/min, his blood pressure is 50/40 mm Hg, and his temperature is 96.4°F (35.8°C).",
"The patient's abdomen is grossly distended, tense, and discolored. Bowel sounds cannot be heard. His alert status does not allow evaluation for rebound tenderness. Capillary refill time is 5 seconds. He becomes unconscious and is intubated and placed on a ventilator. Vascular access is achieved on the left femoral vein, and an intravenous bolus of Ringer solution (10 mL/kg) is given. An arterial line is placed on the femoral artery, and blood gas analysis reveals severe metabolic acidosis with elevated lactate level.",
"Blood tests reveal a hemoglobin level of 6 g/dL (reference range, 10-17 g/dL), leukocytosis of 14,000 cells/µL, neutrophilia of 73%, and platelet count of 60,000 cells/μL. Electrolyte analysis demonstrates hyperkalemia (potassium level, 5.9 mEq/L). The patient's blood pressure does not improve after the initial fluid bolus, and he is given a second one. Paracentesis reveals bloodstained free fluid."
],
"date": "February 08, 2022",
"figures": [],
"markdown": "# 5-Month-Old Rushed to the ED for Severe Abdominal Distention\n\n **Authors:** Jaime Shalkow, MD; Mayela E. García \n **Date:** February 08, 2022\n\n ## Content\n\n Upon arrival to the hospital, the child looks extremely ill. He is immediately admitted to the ED shock room. He is very pale, flaccid, and unresponsive. The anterior fontanel is depressed, and his skin and mucous membranes are dry. Peripheral pulses (extremities) are not felt, but his carotid and femoral pulses are weak, with evident tachysphygmia. His heart rate is 210 beats/min, his respiratory rate is 45 breaths/min, his blood pressure is 50/40 mm Hg, and his temperature is 96.4°F (35.8°C).\nThe patient's abdomen is grossly distended, tense, and discolored. Bowel sounds cannot be heard. His alert status does not allow evaluation for rebound tenderness. Capillary refill time is 5 seconds. He becomes unconscious and is intubated and placed on a ventilator. Vascular access is achieved on the left femoral vein, and an intravenous bolus of Ringer solution (10 mL/kg) is given. An arterial line is placed on the femoral artery, and blood gas analysis reveals severe metabolic acidosis with elevated lactate level.\nBlood tests reveal a hemoglobin level of 6 g/dL (reference range, 10-17 g/dL), leukocytosis of 14,000 cells/µL, neutrophilia of 73%, and platelet count of 60,000 cells/μL. Electrolyte analysis demonstrates hyperkalemia (potassium level, 5.9 mEq/L). The patient's blood pressure does not improve after the initial fluid bolus, and he is given a second one. Paracentesis reveals bloodstained free fluid.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1232920,
"choiceText": "Choledochal cyst",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232922,
"choiceText": "Portal hypertension",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232924,
"choiceText": "Abdominal vascular malformation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232926,
"choiceText": "Ruptured hepatic tumor",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232928,
"choiceText": "Malignant hemoperitoneum\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 392011,
"questionText": "Based on these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "5-Month-Old Rushed to the ED for Severe Abdominal Distention"
},
{
"authors": "Jaime Shalkow, MD; Mayela E. García",
"content": [
"The patient in this case presented with a ruptured hepatic tumor. Other diagnoses were ruled out.",
"A choledochal cyst is a congenital anomaly of the biliary tract, characterized by bile duct dilatation, involving the extra- and/or intrahepatic biliary radicles. Most cases are discovered at infancy, and it is more common in females (female-to-male ratio, 3:1-4:1). The classic clinical triad includes abdominal pain, jaundice, and a palpable right upper-quadrant abdominal mass. Patients might develop pancreatitis, cholangitis, and hepatocellular damage. These patients usually present with abnormal liver function test results, including an obstructive pattern with elevated hepatocellular enzyme, amylase, and lipase levels.[1,2] The patient in this case did not show any signs of pancreatitis or cholangitis, he was not jaundiced, and his liver function test results were normal.",
"Portal hypertension is a major complication of chronic liver disease. It results from increased vascular resistance and/or blood flow into the hepatic sinusoids, leading to a portal pressure gradient of 12 mm Hg or greater (normal pressure is 7-10 mm Hg). As a consequence, collateral vessels are formed, developing esophageal or gastric varices and hemorrhoids.",
"Portal hypertension is caused by a wide variety of conditions. The most common prehepatic cause of portal vein obstruction in children is thrombosis due to umbilical vein catheterization, omphalitis, or sepsis. Some intrahepatic causes include congenital hepatic fibrosis, cirrhosis due to primary liver disease or biliary atresia, and veno-occlusive hepatic disease, which may occur in children after hematopoietic stem cell transplantation. The main clinical manifestations are gastrointestinal hemorrhage, splenomegaly, and ascites. The condition is often clinically silent, but an important clue to its presence is an abnormal abdominal venous pattern (caput medusa).[3,4] The patient in this case did not have chronic liver disease, nor any clinical sign that suggested portal hypertension.",
"Vascular malformations are errors of vasculogenesis that occur at 4-7 weeks' gestation. They may involve a single type of vessel (eg, arterial, venous, capillary, lymphatic) or may be of mixed variety. They are classified by the predominant channel type and resultant rheologic character (fast versus slow flow).[5,6,7] The patient in this case was initially misdiagnosed as having an abdominal vascular malformation, on the basis of the cystic appearance of the lesion on imaging studies. However, a pure lymphatic malformation would not cause hemoperitoneum and shock. Sildenafil has been used with some success in certain lymphatic malformations. This child´s presentation could not be attributed to the drug.",
"Malignant hemoperitoneum is the presence of blood in the peritoneal cavity owing to a ruptured abdominal tumor. Acute abdomen is rare, occurring in less than 5% of patients. The diagnosis should be considered in patients with large abdominal masses, who develop distention, abdominal compartment syndrome, hypotension, decreased urine output, or anemia. Abdominal tumors may spontaneously rupture owing to fast enlargement and necrosis or capsular infiltration. They may also rupture owing to chemotherapy-induced necrosis.[8,9] The patient in this case did not have a history of abdominal cancer, nor had he received chemotherapy. The AFP level was certainly above the expected for age. However, malignant hepatic tumors, which in this age group are mostly hepatoblastomas, tend to elevate AFP levels much higher."
],
"date": "February 08, 2022",
"figures": [],
"markdown": "# 5-Month-Old Rushed to the ED for Severe Abdominal Distention\n\n **Authors:** Jaime Shalkow, MD; Mayela E. García \n **Date:** February 08, 2022\n\n ## Content\n\n The patient in this case presented with a ruptured hepatic tumor. Other diagnoses were ruled out.\nA choledochal cyst is a congenital anomaly of the biliary tract, characterized by bile duct dilatation, involving the extra- and/or intrahepatic biliary radicles. Most cases are discovered at infancy, and it is more common in females (female-to-male ratio, 3:1-4:1). The classic clinical triad includes abdominal pain, jaundice, and a palpable right upper-quadrant abdominal mass. Patients might develop pancreatitis, cholangitis, and hepatocellular damage. These patients usually present with abnormal liver function test results, including an obstructive pattern with elevated hepatocellular enzyme, amylase, and lipase levels.[1,2] The patient in this case did not show any signs of pancreatitis or cholangitis, he was not jaundiced, and his liver function test results were normal.\nPortal hypertension is a major complication of chronic liver disease. It results from increased vascular resistance and/or blood flow into the hepatic sinusoids, leading to a portal pressure gradient of 12 mm Hg or greater (normal pressure is 7-10 mm Hg). As a consequence, collateral vessels are formed, developing esophageal or gastric varices and hemorrhoids.\nPortal hypertension is caused by a wide variety of conditions. The most common prehepatic cause of portal vein obstruction in children is thrombosis due to umbilical vein catheterization, omphalitis, or sepsis. Some intrahepatic causes include congenital hepatic fibrosis, cirrhosis due to primary liver disease or biliary atresia, and veno-occlusive hepatic disease, which may occur in children after hematopoietic stem cell transplantation. The main clinical manifestations are gastrointestinal hemorrhage, splenomegaly, and ascites. The condition is often clinically silent, but an important clue to its presence is an abnormal abdominal venous pattern (caput medusa).[3,4] The patient in this case did not have chronic liver disease, nor any clinical sign that suggested portal hypertension.\nVascular malformations are errors of vasculogenesis that occur at 4-7 weeks' gestation. They may involve a single type of vessel (eg, arterial, venous, capillary, lymphatic) or may be of mixed variety. They are classified by the predominant channel type and resultant rheologic character (fast versus slow flow).[5,6,7] The patient in this case was initially misdiagnosed as having an abdominal vascular malformation, on the basis of the cystic appearance of the lesion on imaging studies. However, a pure lymphatic malformation would not cause hemoperitoneum and shock. Sildenafil has been used with some success in certain lymphatic malformations. This child´s presentation could not be attributed to the drug.\nMalignant hemoperitoneum is the presence of blood in the peritoneal cavity owing to a ruptured abdominal tumor. Acute abdomen is rare, occurring in less than 5% of patients. The diagnosis should be considered in patients with large abdominal masses, who develop distention, abdominal compartment syndrome, hypotension, decreased urine output, or anemia. Abdominal tumors may spontaneously rupture owing to fast enlargement and necrosis or capsular infiltration. They may also rupture owing to chemotherapy-induced necrosis.[8,9] The patient in this case did not have a history of abdominal cancer, nor had he received chemotherapy. The AFP level was certainly above the expected for age. However, malignant hepatic tumors, which in this age group are mostly hepatoblastomas, tend to elevate AFP levels much higher.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1232920,
"choiceText": "Choledochal cyst",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232922,
"choiceText": "Portal hypertension",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232924,
"choiceText": "Abdominal vascular malformation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232926,
"choiceText": "Ruptured hepatic tumor",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232928,
"choiceText": "Malignant hemoperitoneum\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 392011,
"questionText": "Based on these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "5-Month-Old Rushed to the ED for Severe Abdominal Distention"
},
{
"authors": "Jaime Shalkow, MD; Mayela E. García",
"content": [
"Mesenchymal hamartoma of the liver is the second most common benign hepatic tumor in children after hemangiomas, accounting for 8% of all liver masses in this age group.[10,11,12] The most common presentation is a palpable, nontender abdominal mass in an otherwise healthy-looking child, usually younger than 2 years,[10,11] with an average age of 15 months.[13,14] However, larger tumors can become symptomatic and cause vena cava obstruction, feeding difficulties, or respiratory distress. Mesenchymal hamartomas of the liver are most common in the right lobe (75%) and have a slight male predominance, with a 3:2 male-to-female ratio.[12,13] Their size ranges from tiny lesions to large tumors, sometimes up to 30 cm.[13,15] The mass is usually encapsulated.",
"Although some children present with mild AFP elevation, serum markers and liver function tests are unrevealing in most cases. High AFP levels return to normal after resection.[10,11,14]",
"The etiology of mesenchymal hamartomas of the liver is not fully understood; however, different theories have been proposed. Developmental defects, regional ischemia, or biliary obstruction, are considered possible causes.[16] An association with chromosomal anomalies has been linked to its pathogenesis, at the 19q13.4 region.[15,16] Although spontaneous regressions do occur, malignant transformation into undifferentiated or embryonal sarcoma of the liver has been also been reported, also involving the 19q13 chromosomal region.[17] Thus, primary complete surgical excision is considered the preferred treatment option.[18]",
"Histologically, mesenchymal hamartomas are heterogeneous lesions lined by bile duct epithelium, within either a dominant cyst or as a multicystic lesion. The cysts do not contain normal bile, nor do they communicate with the biliary tree.[18] Differential diagnoses for mesenchymal hamartomas include hepatoblastomas, infantile hemangioendothelioma, and embryonal sarcoma of the liver.[12,16]",
"Hepatoblastoma is the most common primary malignant liver tumor in children. It occurs most frequently during the first year of life, and the AFP level is elevated in most patients. By image, it is described as a well-circumscribed mass, slightly hypoattenuating to the adjacent liver. Calcifications and hemorrhage are also common findings.[13,18]",
"Infantile hemangioendothelioma is a benign but aggressive liver tumor that can occur in children younger than 6 months. Most are asymptomatic and incidentally discovered during abdominal imaging. They appear as a solid, highly vascularized, large, solitary or multifocal mass.[13,18] When large enough, they may cause congestive heart failure (CHF) , and severe thrombocytopenia (Kasabach-Merritt syndrome).",
"Embryonal sarcoma of the liver is a rare malignant hepatic tumor of childhood. It is an aggressive neoplasm of mesenchymal origin that is associated with an unfavorable prognosis. Typical presentation is individuals aged 8-18 years; a liver mass is accompanied by nausea, vomiting, jaundice, fever, and weight loss. The AFP level is not usually elevated. On imaging studies, they appear as a mixed solid and multiseptated cystic mass.[12,14]",
"For all liver tumors, initial imaging workup with ultrasonography confirms the location and characterizes the consistency as cystic, solid, or mixed. CT and MRI further delineate location, extent, and anatomy related to lesions or metastases.[11,19] These modalities facilitate surgical planning and may determine resectability.[18]",
"Mesenchymal hamartoma of the liver is a benign infant tumor of variable size, more commonly located in the right lobe and usually multicystic.[10,18] Areas of cystic degeneration may cause rapid progression by further fluid accumulation, which can lead to misdiagnosis as malignant.[13] Patients typically present with progressive abdominal distention and a nontender, palpable mass in the right upper quadrant. As tumor size increases, compression of surrounding structures may cause pain, anorexia, vomiting, jaundice, ascites, bowel obstruction, respiratory distress, or CHF.[10,11,18] The tumors can be prenatally detected by ultrasonography. Large tumors may cause severe hydrops, intestinal obstruction, or diaphragmatic elevation and risk for pulmonary hypoplasia. Compression of the inferior vena cava and umbilical vein place the fetus at risk for premature birth, CHF, and intrauterine death.[12,13,15]",
"Although biochemical liver markers are generally normal, in patients with mesenchymal hamartoma of the liver and elevated AFP levels at diagnosis, the marker becomes a helpful postoperative follow-up tool.[18] Imaging studies, such as ultrasonography, CT, and MRI, are useful not only for the initial diagnosis but also for pre- and posttreatment evaluation and follow-up.[19]",
"Ultrasonography is inexpensive and readily available; it displays important information about the mass, including location, consistence, and vascularity. On ultrasonography, mesenchymal hamartomas of the liver are seen as well-defined masses with cystic, solid, or mixed forms. Cysts are anechoic, separated by thin or thick echogenic septa.[11,19]",
"CT is used to confirm the diagnosis, clarify the segmental involvement, and determine the tumor's relationship with vascular and surrounding structures, permitting optimal planning of the surgical approach. Mesenchymal hamartomas of the liver are heterogeneous lesions on CT. Stromal components appear hypoattenuated to the surrounding liver parenchyma, whereas cystic components show water attenuation. Enhancement of the septa and stromal elements is observed after administration of contrast.[11,13,20]",
"Images of mesenchymal hamartomas of the liver at MRI vary. Cystic portions present with high signal intensity on T2-weighted images but variable signal intensity on T1-weighted images, depending on the protein content. Owing to fibrosis, solid portions may appear hypointense to the adjacent liver parenchyma on both T1- and T2-weighted images.[19,20]",
"Definitive diagnosis requires histologic confirmation. Fine-needle aspiration cytology may be helpful in excluding differential diagnoses in selected patients. However, it requires aspiration of adequate material and interpretation by an experienced pediatric cytopathologist. The specimen demonstrates clusters of hepatocytes and normal bile duct epithelium, admixed with bland mesenchymal or spindle-shaped cells in a myxoid background.[14,16,21] In most reported cases, mesenchymal hamartomas of the liver could not be diagnosed by this method[22]; thus, it is not usually used for preoperative diagnosis. Rather, the specimen is studied after complete resection.",
"Histologically, mesenchymal hamartoma of the livers are described as an enlargement of mesenchymal tissue, bile ducts, hepatic cords, and blood vessels within a liver mass, without atypical mitosis. Cysts are formed by dilated bile ducts, lying in a myxoid stroma with myofibroblast-like cells. Cords of normal hepatocytes stretch between the mesenchyme and the proliferating bile ducts.[10,16,20]"
],
"date": "February 08, 2022",
"figures": [],
"markdown": "# 5-Month-Old Rushed to the ED for Severe Abdominal Distention\n\n **Authors:** Jaime Shalkow, MD; Mayela E. García \n **Date:** February 08, 2022\n\n ## Content\n\n Mesenchymal hamartoma of the liver is the second most common benign hepatic tumor in children after hemangiomas, accounting for 8% of all liver masses in this age group.[10,11,12] The most common presentation is a palpable, nontender abdominal mass in an otherwise healthy-looking child, usually younger than 2 years,[10,11] with an average age of 15 months.[13,14] However, larger tumors can become symptomatic and cause vena cava obstruction, feeding difficulties, or respiratory distress. Mesenchymal hamartomas of the liver are most common in the right lobe (75%) and have a slight male predominance, with a 3:2 male-to-female ratio.[12,13] Their size ranges from tiny lesions to large tumors, sometimes up to 30 cm.[13,15] The mass is usually encapsulated.\nAlthough some children present with mild AFP elevation, serum markers and liver function tests are unrevealing in most cases. High AFP levels return to normal after resection.[10,11,14]\nThe etiology of mesenchymal hamartomas of the liver is not fully understood; however, different theories have been proposed. Developmental defects, regional ischemia, or biliary obstruction, are considered possible causes.[16] An association with chromosomal anomalies has been linked to its pathogenesis, at the 19q13.4 region.[15,16] Although spontaneous regressions do occur, malignant transformation into undifferentiated or embryonal sarcoma of the liver has been also been reported, also involving the 19q13 chromosomal region.[17] Thus, primary complete surgical excision is considered the preferred treatment option.[18]\nHistologically, mesenchymal hamartomas are heterogeneous lesions lined by bile duct epithelium, within either a dominant cyst or as a multicystic lesion. The cysts do not contain normal bile, nor do they communicate with the biliary tree.[18] Differential diagnoses for mesenchymal hamartomas include hepatoblastomas, infantile hemangioendothelioma, and embryonal sarcoma of the liver.[12,16]\nHepatoblastoma is the most common primary malignant liver tumor in children. It occurs most frequently during the first year of life, and the AFP level is elevated in most patients. By image, it is described as a well-circumscribed mass, slightly hypoattenuating to the adjacent liver. Calcifications and hemorrhage are also common findings.[13,18]\nInfantile hemangioendothelioma is a benign but aggressive liver tumor that can occur in children younger than 6 months. Most are asymptomatic and incidentally discovered during abdominal imaging. They appear as a solid, highly vascularized, large, solitary or multifocal mass.[13,18] When large enough, they may cause congestive heart failure (CHF) , and severe thrombocytopenia (Kasabach-Merritt syndrome).\nEmbryonal sarcoma of the liver is a rare malignant hepatic tumor of childhood. It is an aggressive neoplasm of mesenchymal origin that is associated with an unfavorable prognosis. Typical presentation is individuals aged 8-18 years; a liver mass is accompanied by nausea, vomiting, jaundice, fever, and weight loss. The AFP level is not usually elevated. On imaging studies, they appear as a mixed solid and multiseptated cystic mass.[12,14]\nFor all liver tumors, initial imaging workup with ultrasonography confirms the location and characterizes the consistency as cystic, solid, or mixed. CT and MRI further delineate location, extent, and anatomy related to lesions or metastases.[11,19] These modalities facilitate surgical planning and may determine resectability.[18]\nMesenchymal hamartoma of the liver is a benign infant tumor of variable size, more commonly located in the right lobe and usually multicystic.[10,18] Areas of cystic degeneration may cause rapid progression by further fluid accumulation, which can lead to misdiagnosis as malignant.[13] Patients typically present with progressive abdominal distention and a nontender, palpable mass in the right upper quadrant. As tumor size increases, compression of surrounding structures may cause pain, anorexia, vomiting, jaundice, ascites, bowel obstruction, respiratory distress, or CHF.[10,11,18] The tumors can be prenatally detected by ultrasonography. Large tumors may cause severe hydrops, intestinal obstruction, or diaphragmatic elevation and risk for pulmonary hypoplasia. Compression of the inferior vena cava and umbilical vein place the fetus at risk for premature birth, CHF, and intrauterine death.[12,13,15]\nAlthough biochemical liver markers are generally normal, in patients with mesenchymal hamartoma of the liver and elevated AFP levels at diagnosis, the marker becomes a helpful postoperative follow-up tool.[18] Imaging studies, such as ultrasonography, CT, and MRI, are useful not only for the initial diagnosis but also for pre- and posttreatment evaluation and follow-up.[19]\nUltrasonography is inexpensive and readily available; it displays important information about the mass, including location, consistence, and vascularity. On ultrasonography, mesenchymal hamartomas of the liver are seen as well-defined masses with cystic, solid, or mixed forms. Cysts are anechoic, separated by thin or thick echogenic septa.[11,19]\nCT is used to confirm the diagnosis, clarify the segmental involvement, and determine the tumor's relationship with vascular and surrounding structures, permitting optimal planning of the surgical approach. Mesenchymal hamartomas of the liver are heterogeneous lesions on CT. Stromal components appear hypoattenuated to the surrounding liver parenchyma, whereas cystic components show water attenuation. Enhancement of the septa and stromal elements is observed after administration of contrast.[11,13,20]\nImages of mesenchymal hamartomas of the liver at MRI vary. Cystic portions present with high signal intensity on T2-weighted images but variable signal intensity on T1-weighted images, depending on the protein content. Owing to fibrosis, solid portions may appear hypointense to the adjacent liver parenchyma on both T1- and T2-weighted images.[19,20]\nDefinitive diagnosis requires histologic confirmation. Fine-needle aspiration cytology may be helpful in excluding differential diagnoses in selected patients. However, it requires aspiration of adequate material and interpretation by an experienced pediatric cytopathologist. The specimen demonstrates clusters of hepatocytes and normal bile duct epithelium, admixed with bland mesenchymal or spindle-shaped cells in a myxoid background.[14,16,21] In most reported cases, mesenchymal hamartomas of the liver could not be diagnosed by this method[22]; thus, it is not usually used for preoperative diagnosis. Rather, the specimen is studied after complete resection.\nHistologically, mesenchymal hamartoma of the livers are described as an enlargement of mesenchymal tissue, bile ducts, hepatic cords, and blood vessels within a liver mass, without atypical mitosis. Cysts are formed by dilated bile ducts, lying in a myxoid stroma with myofibroblast-like cells. Cords of normal hepatocytes stretch between the mesenchyme and the proliferating bile ducts.[10,16,20]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "5-Month-Old Rushed to the ED for Severe Abdominal Distention"
},
{
"authors": "Jaime Shalkow, MD; Mayela E. García",
"content": [
"Complete surgical resection with free margins is considered the treatment of choice for mesenchymal hamartomas of the liver, to avoid relapse and malignant transformation. Anatomical resections following the segmental liver divisions are optimal. If the tumor is considered unresectable, enucleation and marsupialization are surgical alternatives.[11,12,18]",
"For large tumors in very young children in whom extended liver resection is indicated, successful results have been recently reported with preoperative portal vein embolization. This percutaneous procedure stimulates growth of the future liver remnant, with a success rate of 95%-100% in adults. Feasibility in infants requires expertise and appropriate-sized materials to warrant safety.[23]",
"Complete surgical resection offers an excellent prognosis and is curative in most cases.[10,11] Mortality is mostly related to surgical complications, such as hemorrhage, cardiac arrest, and pulmonary problems, including acute respiratory distress syndrome. The latter has been reported to occur in as many as 11% of patients.[16,22] For selected patients in whom resection is not feasible, decision of observation warrants a very close follow-up, given the risk for malignant transformation.",
"After complete surgical resection, most patients are cured and recurrences are seldom seen. Two or three follow-up CT scans are acceptable initially to identify early postoperative complications and monitor liver regeneration. However, after the first year, ultrasonography, liver function testing, and tumor marker level assays are most appropriate for follow-up.",
"In this patient, owing to a diagnosis of hypovolemic shock and hemoperitoneum, emergency exploratory laparotomy was initiated. The abdomen was approached through a transverse supraumbilical incision. A fair amount of bloody ascites was drained. A large, partially ruptured cystic mass was found descending from the right lobe of the liver, extending into the medial segment of the left hemiliver (Figure 7).",
"Figure 7.",
"Extended right hepatectomy was performed (segments 4-8), which achieved complete tumor resection. An incidental bile duct transection was repaired with a primary end-to-end anastomosis. The patient underwent cardiac arrest during surgery but was resuscitated with CPR. A closed active drain was placed near the anastomosis. Operating time was 13 hours, and blood loss was 340 mL, which required multiple packed red blood cells, platelets, and fresh frozen plasma transfusions.",
"The patient was transferred to the pediatric intensive care unit in critical condition but recovered uneventfully. He was transferred to the ward within 5 days, alert, neurologically intact, hemodynamically stable, and feeding by mouth. He was discharged home on postoperative day 11, without further complications, with normal blood tests, and tolerating oral intake.",
"In this patient, specimen histopathologic analysis revealed a cystic mesenchymal hamartoma of the liver (Figure 8), completely resected with free margins.",
"Figure 8.",
"The patient developed a biliary fistula that was managed conservatively with long-term drainage (the abdominal drain was left in place for 4 weeks) and octreotide. Follow-up ultrasonography revealed an infrahepatic fluid collection, without signs of peritonitis. The fistula spontaneously closed, without biliary stricture. Bilirubin, alkaline phosphatase, and liver enzyme levels remained normal.",
"At a follow-up visit 6 weeks later, the patient was doing well; he was asymptomatic, feeding properly, and gaining weight. His AFP level was 18 ng/mL (reference range, 10-17 g/dL). Ultrasonography revealed that the remaining left lateral sector of the liver had increased in volume to age-appropriate size, without bile duct dilatation. At a follow-up visit 30 months after hospital admission, he was healthy, with normal development and living a normal life without any sequelae."
],
"date": "February 08, 2022",
"figures": [
{
"caption": "Figure 7.",
"image_url": "https://img.medscapestatic.com/article/898/100/898100-Thumb7.png"
},
{
"caption": "Figure 8.",
"image_url": "https://img.medscapestatic.com/article/898/100/898100-Thumb8.png"
}
],
"markdown": "# 5-Month-Old Rushed to the ED for Severe Abdominal Distention\n\n **Authors:** Jaime Shalkow, MD; Mayela E. García \n **Date:** February 08, 2022\n\n ## Content\n\n Complete surgical resection with free margins is considered the treatment of choice for mesenchymal hamartomas of the liver, to avoid relapse and malignant transformation. Anatomical resections following the segmental liver divisions are optimal. If the tumor is considered unresectable, enucleation and marsupialization are surgical alternatives.[11,12,18]\nFor large tumors in very young children in whom extended liver resection is indicated, successful results have been recently reported with preoperative portal vein embolization. This percutaneous procedure stimulates growth of the future liver remnant, with a success rate of 95%-100% in adults. Feasibility in infants requires expertise and appropriate-sized materials to warrant safety.[23]\nComplete surgical resection offers an excellent prognosis and is curative in most cases.[10,11] Mortality is mostly related to surgical complications, such as hemorrhage, cardiac arrest, and pulmonary problems, including acute respiratory distress syndrome. The latter has been reported to occur in as many as 11% of patients.[16,22] For selected patients in whom resection is not feasible, decision of observation warrants a very close follow-up, given the risk for malignant transformation.\nAfter complete surgical resection, most patients are cured and recurrences are seldom seen. Two or three follow-up CT scans are acceptable initially to identify early postoperative complications and monitor liver regeneration. However, after the first year, ultrasonography, liver function testing, and tumor marker level assays are most appropriate for follow-up.\nIn this patient, owing to a diagnosis of hypovolemic shock and hemoperitoneum, emergency exploratory laparotomy was initiated. The abdomen was approached through a transverse supraumbilical incision. A fair amount of bloody ascites was drained. A large, partially ruptured cystic mass was found descending from the right lobe of the liver, extending into the medial segment of the left hemiliver (Figure 7).\nFigure 7.\nExtended right hepatectomy was performed (segments 4-8), which achieved complete tumor resection. An incidental bile duct transection was repaired with a primary end-to-end anastomosis. The patient underwent cardiac arrest during surgery but was resuscitated with CPR. A closed active drain was placed near the anastomosis. Operating time was 13 hours, and blood loss was 340 mL, which required multiple packed red blood cells, platelets, and fresh frozen plasma transfusions.\nThe patient was transferred to the pediatric intensive care unit in critical condition but recovered uneventfully. He was transferred to the ward within 5 days, alert, neurologically intact, hemodynamically stable, and feeding by mouth. He was discharged home on postoperative day 11, without further complications, with normal blood tests, and tolerating oral intake.\nIn this patient, specimen histopathologic analysis revealed a cystic mesenchymal hamartoma of the liver (Figure 8), completely resected with free margins.\nFigure 8.\nThe patient developed a biliary fistula that was managed conservatively with long-term drainage (the abdominal drain was left in place for 4 weeks) and octreotide. Follow-up ultrasonography revealed an infrahepatic fluid collection, without signs of peritonitis. The fistula spontaneously closed, without biliary stricture. Bilirubin, alkaline phosphatase, and liver enzyme levels remained normal.\nAt a follow-up visit 6 weeks later, the patient was doing well; he was asymptomatic, feeding properly, and gaining weight. His AFP level was 18 ng/mL (reference range, 10-17 g/dL). Ultrasonography revealed that the remaining left lateral sector of the liver had increased in volume to age-appropriate size, without bile duct dilatation. At a follow-up visit 30 months after hospital admission, he was healthy, with normal development and living a normal life without any sequelae.\n\n ## Figures\n\n **Figure 7.** \n \n\n**Figure 8.** \n \n\n\n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1232938,
"choiceText": "Mesenchymal hamartomas of the liver are more commonly located in the left lobe",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232940,
"choiceText": "Mesenchymal hamartomas of the liver are rarely multicystic",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232942,
"choiceText": "Mesenchymal hamartomas of the liver are routinely associated with notable changes in biochemical liver markers",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232944,
"choiceText": "Mesenchymal hamartomas of the liver require histologic confirmation for definitive diagnosis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Definitive diagnosis requires histologic confirmation. Fine-needle aspiration cytology may be helpful in excluding differential diagnoses in selected patients. However, it requires aspiration of adequate material and interpretation by an experienced pediatric cytopathologist. <br><br>\r\n\r\nMesenchymal hamartoma of the liver is a benign infant tumor of variable size, more commonly located in the right lobe, and usually multicystic. Although biochemical liver markers are generally normal, in patients with mesenchymal hamartoma of the liver and elevated AFP levels at diagnosis, the marker becomes a helpful postoperative follow-up tool.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 392015,
"questionText": "Which is most accurate about mesenchymal hamartomas of the liver?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1232946,
"choiceText": "Positron emission tomography",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232948,
"choiceText": "Nuclear liver scan",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232950,
"choiceText": "Ultrasonography",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232952,
"choiceText": "Magnetic resonance cholangiopancreatography\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "After complete surgical resection, most patients are cured and recurrences are seldom seen. Two or three follow-up CT scans are acceptable initially to identify early postoperative complications and monitor liver regeneration. However, after the first year, ultrasonography, liver function testing, and tumor marker level assays are most appropriate for follow-up.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 392017,
"questionText": "For patients treated with surgical resection for mesenchymal hamartoma of the liver, which is most appropriate for inclusion in follow-up visits after the first year?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "5-Month-Old Rushed to the ED for Severe Abdominal Distention"
},
{
"authors": "Jaime Shalkow, MD; Mayela E. García",
"content": [],
"date": "February 08, 2022",
"figures": [],
"markdown": "# 5-Month-Old Rushed to the ED for Severe Abdominal Distention\n\n **Authors:** Jaime Shalkow, MD; Mayela E. García \n **Date:** February 08, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1232938,
"choiceText": "Mesenchymal hamartomas of the liver are more commonly located in the left lobe",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232940,
"choiceText": "Mesenchymal hamartomas of the liver are rarely multicystic",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232942,
"choiceText": "Mesenchymal hamartomas of the liver are routinely associated with notable changes in biochemical liver markers",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232944,
"choiceText": "Mesenchymal hamartomas of the liver require histologic confirmation for definitive diagnosis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Definitive diagnosis requires histologic confirmation. Fine-needle aspiration cytology may be helpful in excluding differential diagnoses in selected patients. However, it requires aspiration of adequate material and interpretation by an experienced pediatric cytopathologist. <br><br>\r\n\r\nMesenchymal hamartoma of the liver is a benign infant tumor of variable size, more commonly located in the right lobe, and usually multicystic. Although biochemical liver markers are generally normal, in patients with mesenchymal hamartoma of the liver and elevated AFP levels at diagnosis, the marker becomes a helpful postoperative follow-up tool.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 392015,
"questionText": "Which is most accurate about mesenchymal hamartomas of the liver?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1232946,
"choiceText": "Positron emission tomography",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232948,
"choiceText": "Nuclear liver scan",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232950,
"choiceText": "Ultrasonography",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232952,
"choiceText": "Magnetic resonance cholangiopancreatography\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "After complete surgical resection, most patients are cured and recurrences are seldom seen. Two or three follow-up CT scans are acceptable initially to identify early postoperative complications and monitor liver regeneration. However, after the first year, ultrasonography, liver function testing, and tumor marker level assays are most appropriate for follow-up.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 392017,
"questionText": "For patients treated with surgical resection for mesenchymal hamartoma of the liver, which is most appropriate for inclusion in follow-up visits after the first year?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "5-Month-Old Rushed to the ED for Severe Abdominal Distention"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1232920,
"choiceText": "Choledochal cyst",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232922,
"choiceText": "Portal hypertension",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232924,
"choiceText": "Abdominal vascular malformation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232926,
"choiceText": "Ruptured hepatic tumor",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232928,
"choiceText": "Malignant hemoperitoneum\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 392011,
"questionText": "Based on these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1232938,
"choiceText": "Mesenchymal hamartomas of the liver are more commonly located in the left lobe",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232940,
"choiceText": "Mesenchymal hamartomas of the liver are rarely multicystic",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232942,
"choiceText": "Mesenchymal hamartomas of the liver are routinely associated with notable changes in biochemical liver markers",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232944,
"choiceText": "Mesenchymal hamartomas of the liver require histologic confirmation for definitive diagnosis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Definitive diagnosis requires histologic confirmation. Fine-needle aspiration cytology may be helpful in excluding differential diagnoses in selected patients. However, it requires aspiration of adequate material and interpretation by an experienced pediatric cytopathologist. <br><br>\r\n\r\nMesenchymal hamartoma of the liver is a benign infant tumor of variable size, more commonly located in the right lobe, and usually multicystic. Although biochemical liver markers are generally normal, in patients with mesenchymal hamartoma of the liver and elevated AFP levels at diagnosis, the marker becomes a helpful postoperative follow-up tool.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 392015,
"questionText": "Which is most accurate about mesenchymal hamartomas of the liver?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1232946,
"choiceText": "Positron emission tomography",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232948,
"choiceText": "Nuclear liver scan",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232950,
"choiceText": "Ultrasonography",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1232952,
"choiceText": "Magnetic resonance cholangiopancreatography\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "After complete surgical resection, most patients are cured and recurrences are seldom seen. Two or three follow-up CT scans are acceptable initially to identify early postoperative complications and monitor liver regeneration. However, after the first year, ultrasonography, liver function testing, and tumor marker level assays are most appropriate for follow-up.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 392017,
"questionText": "For patients treated with surgical resection for mesenchymal hamartoma of the liver, which is most appropriate for inclusion in follow-up visits after the first year?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
885135 | /viewarticle/885135 | [
{
"authors": "Greg P. Hansen, DO; Christo T. Philip, MD; Larissa I. Velez, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 23-year-old woman presents to the emergency department with a 3-day history of progressively worsening generalized muscle weakness and nonbilious emesis. She has been vomiting once or twice daily, mostly upon awakening. The emesis does not seem to be associated with oral intake. She is also experiencing intermittent hematuria, without any flank pain or dysuria. She denies having fever, diarrhea, chills, headache, abdominal pain, visual disturbances, or paresthesias.",
"Before the onset of symptoms, the patient was in good health, with a medical history significant only for renal colic 8 months before presentation. She had cosmetic rhinoplasty 2 years ago but otherwise has not had any prior major surgery. She has no known allergies and is not taking any medications. Her last menstrual period was 1 month ago. Results of a urine pregnancy test result are positive.",
"She recently moved to the United States from Mexico, works as a waitress, and does not use tobacco or illicit drugs."
],
"date": "February 02, 2022",
"figures": [],
"markdown": "# A 23-Year-Old Unaware She’s Pregnant With Hematuria, ECG Abnormalities\n\n **Authors:** Greg P. Hansen, DO; Christo T. Philip, MD; Larissa I. Velez, MD \n **Date:** February 02, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 23-year-old woman presents to the emergency department with a 3-day history of progressively worsening generalized muscle weakness and nonbilious emesis. She has been vomiting once or twice daily, mostly upon awakening. The emesis does not seem to be associated with oral intake. She is also experiencing intermittent hematuria, without any flank pain or dysuria. She denies having fever, diarrhea, chills, headache, abdominal pain, visual disturbances, or paresthesias.\nBefore the onset of symptoms, the patient was in good health, with a medical history significant only for renal colic 8 months before presentation. She had cosmetic rhinoplasty 2 years ago but otherwise has not had any prior major surgery. She has no known allergies and is not taking any medications. Her last menstrual period was 1 month ago. Results of a urine pregnancy test result are positive.\nShe recently moved to the United States from Mexico, works as a waitress, and does not use tobacco or illicit drugs.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A 23-Year-Old Unaware She’s Pregnant With Hematuria, ECG Abnormalities"
},
{
"authors": "Greg P. Hansen, DO; Christo T. Philip, MD; Larissa I. Velez, MD",
"content": [
"Upon physical examination, the patient's oral temperature is 99°F (37.2°C). Her pulse is regular, with a rate of 75 beats/min. Her blood pressure is 112/60 mm Hg, and she has a respiratory rate of 18 breaths/min with an oxygen saturation of 98% while breathing room air. She appears uncomfortable and generally fatigued, but is alert and oriented.",
"The patient's extraocular muscles are intact, with no nystagmus. Her pupils are symmetric and equally reactive to light, and the optic discs appear normal. Her mucous membranes are moist, and the remainder of the head, ear, nose, and throat examination is normal. Her lungs are clear to auscultation, and the patient exhibits normal respiratory effort. The heart rhythm is regular, without murmurs, rubs, or gallops. Her abdomen is nontender, without masses, and no costovertebral angle tenderness is noted. The extremities are without edema, and the radial pulses are strong bilaterally. The skin is clear, without rash, petechiae, or ecchymoses.",
"Cranial nerves II-XII are normal and symmetric. Otherwise, the neurologic examination reveals 2/5 strength throughout both upper and lower extremities, with 1/3 patellar, triceps, and Achilles reflexes bilaterally. The patient has negative Babinski and Hoffmann signs. Finger-to-nose coordination and gait could not be assessed as a result of her weakness.",
"An ECG (Figure 1), urine analysis, and basic metabolic panel are completed.",
"Figure 1.",
"She has a serum glucose concentration of 97 mg/dL (reference range, <140 mg/dL) and a hemoglobin level of 13.4 g/dL (reference range, 12-15.5 g/dL). As a result of a low bicarbonate finding on the metabolic panel, arterial blood gas measurement is subsequently performed; this shows a pH of 7.25 (neutral, 7), a partial pressure of carbon dioxide of 22 mm Hg (reference range, 38-42 mm Hg), a partial pressure of oxygen of 100 mm Hg (reference range, 75-100 mm Hg), and a bicarbonate level of 9 mEq/L (reference range, 23-30 mEq/L). The urine analysis shows a pH of 7 (reference range, 4.6-8), with moderate blood, negative nitrates, and small leukocytes.",
"Renal ultrasound is completed before admission (Figure 2).",
"Figure 2."
],
"date": "February 02, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/885/135/885135-thumb1.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/885/135/885135-thumb2.jpg"
}
],
"markdown": "# A 23-Year-Old Unaware She’s Pregnant With Hematuria, ECG Abnormalities\n\n **Authors:** Greg P. Hansen, DO; Christo T. Philip, MD; Larissa I. Velez, MD \n **Date:** February 02, 2022\n\n ## Content\n\n Upon physical examination, the patient's oral temperature is 99°F (37.2°C). Her pulse is regular, with a rate of 75 beats/min. Her blood pressure is 112/60 mm Hg, and she has a respiratory rate of 18 breaths/min with an oxygen saturation of 98% while breathing room air. She appears uncomfortable and generally fatigued, but is alert and oriented.\nThe patient's extraocular muscles are intact, with no nystagmus. Her pupils are symmetric and equally reactive to light, and the optic discs appear normal. Her mucous membranes are moist, and the remainder of the head, ear, nose, and throat examination is normal. Her lungs are clear to auscultation, and the patient exhibits normal respiratory effort. The heart rhythm is regular, without murmurs, rubs, or gallops. Her abdomen is nontender, without masses, and no costovertebral angle tenderness is noted. The extremities are without edema, and the radial pulses are strong bilaterally. The skin is clear, without rash, petechiae, or ecchymoses.\nCranial nerves II-XII are normal and symmetric. Otherwise, the neurologic examination reveals 2/5 strength throughout both upper and lower extremities, with 1/3 patellar, triceps, and Achilles reflexes bilaterally. The patient has negative Babinski and Hoffmann signs. Finger-to-nose coordination and gait could not be assessed as a result of her weakness.\nAn ECG (Figure 1), urine analysis, and basic metabolic panel are completed.\nFigure 1.\nShe has a serum glucose concentration of 97 mg/dL (reference range, <140 mg/dL) and a hemoglobin level of 13.4 g/dL (reference range, 12-15.5 g/dL). As a result of a low bicarbonate finding on the metabolic panel, arterial blood gas measurement is subsequently performed; this shows a pH of 7.25 (neutral, 7), a partial pressure of carbon dioxide of 22 mm Hg (reference range, 38-42 mm Hg), a partial pressure of oxygen of 100 mm Hg (reference range, 75-100 mm Hg), and a bicarbonate level of 9 mEq/L (reference range, 23-30 mEq/L). The urine analysis shows a pH of 7 (reference range, 4.6-8), with moderate blood, negative nitrates, and small leukocytes.\nRenal ultrasound is completed before admission (Figure 2).\nFigure 2.\n\n ## Figures\n\n **Figure 1.** \n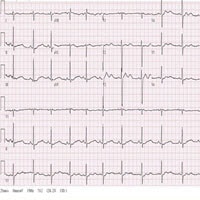 \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1134048,
"choiceText": "Cushing syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134050,
"choiceText": "Addison disease",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134052,
"choiceText": "Bartter syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134054,
"choiceText": "Distal renal tubular acidosis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 359781,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 23-Year-Old Unaware She’s Pregnant With Hematuria, ECG Abnormalities"
},
{
"authors": "Greg P. Hansen, DO; Christo T. Philip, MD; Larissa I. Velez, MD",
"content": [
"Distal renal tubular acidosis (RTA) was diagnosed on the basis of the patient's presentation of profound weakness, history of renal colic, ECG findings consistent with severe hypokalemia, renal ultrasound showing nephrocalcinosis, and arterial blood gas analysis showing profound metabolic acidosis.",
"Initial laboratory testing revealed a sodium level of 138 mEq/L (reference range, 135-145 mEq/L), potassium level of 1.6 mEq/L (reference range, 3.6-5 mEq/L), chloride level of 116 mEq/L (reference range, 98-109 mEq/L), bicarbonate level of 10 mEq/L (reference range, 22-31 mEq/L), anion gap of 12 mEq/L (reference range, 6-16 mEq/L), blood urea nitrogen level of 12 mg/dL (reference range, 7-21 mg/dL), and a creatinine level of 0.83 mg/dL (reference range, 0.6-1.2 mg/dL). These values were consistent with a nonanion gap metabolic acidosis, with associated hypokalemia and no evidence of chronic kidney disease. Her pregnancy-induced hyperemesis gravidarum was undoubtedly the inciting factor for the progression of hypokalemia to such a critical level.",
"The ECG (Figure 1) from the patient showed very prominent U waves, which are classically associated with hypokalemia; in cases where the U wave is taller than the T wave, severe hypokalemia is usually present.",
"The chest radiograph (not shown) showed subtle diffuse osteopenia. The patient's history of renal colic would be consistent with a history of urinary stones that often occurs in patients with RTA resulting from alkaline urine and hypercalciuria. The renal ultrasound (Figure 2) showed hyperechoic regions in the renal medulla consistent with nephrocalcinosis.",
"The arterial blood gas analysis demonstrated a profound metabolic acidosis with a pH of 7.25, further confirming the diagnosis. The type of RTA was characterized by looking at the urine pH, which in this patient was 7. This is consistent with type 1 RTA, also known as \"distal RTA.\"",
"Distal RTA is a rare renal disorder characterized by a nonanion gap hyperchloremic acidosis and hypokalemia. In this condition, the alpha intercalated cells of the cortical collecting duct of the distal nephron fail to secrete acid into the urine. This failure of acid secretion leads to an inability to acidify the urine to a pH < 5.5.",
"Because renal excretion is the primary means of eliminating acid from the body, a tendency toward systemic acidemia is noted. This leads to the clinical features of type 1 RTA, which include:",
"Normal anion gap hyperchloremic metabolic acidosis",
"Hypokalemia (from multiple mechanisms, but often severe during periods of stress)[1]",
"Nephrocalcinosis[2]",
"Nephrolithiasis (related to an inability to acidify urine, hypercalciuria, and low urinary citrate)",
"Loss of calcium from bones (which can cause rickets in children and osteomalacia in adults)",
"During periods of stress caused by illness, or in this particular case the vomiting of hyperemesis gravidum, patients can have episodes of profound hypokalemia, resulting in flaccid paralysis, rhabdomyolysis, cardiac arrest, and even death."
],
"date": "February 02, 2022",
"figures": [],
"markdown": "# A 23-Year-Old Unaware She’s Pregnant With Hematuria, ECG Abnormalities\n\n **Authors:** Greg P. Hansen, DO; Christo T. Philip, MD; Larissa I. Velez, MD \n **Date:** February 02, 2022\n\n ## Content\n\n Distal renal tubular acidosis (RTA) was diagnosed on the basis of the patient's presentation of profound weakness, history of renal colic, ECG findings consistent with severe hypokalemia, renal ultrasound showing nephrocalcinosis, and arterial blood gas analysis showing profound metabolic acidosis.\nInitial laboratory testing revealed a sodium level of 138 mEq/L (reference range, 135-145 mEq/L), potassium level of 1.6 mEq/L (reference range, 3.6-5 mEq/L), chloride level of 116 mEq/L (reference range, 98-109 mEq/L), bicarbonate level of 10 mEq/L (reference range, 22-31 mEq/L), anion gap of 12 mEq/L (reference range, 6-16 mEq/L), blood urea nitrogen level of 12 mg/dL (reference range, 7-21 mg/dL), and a creatinine level of 0.83 mg/dL (reference range, 0.6-1.2 mg/dL). These values were consistent with a nonanion gap metabolic acidosis, with associated hypokalemia and no evidence of chronic kidney disease. Her pregnancy-induced hyperemesis gravidarum was undoubtedly the inciting factor for the progression of hypokalemia to such a critical level.\nThe ECG (Figure 1) from the patient showed very prominent U waves, which are classically associated with hypokalemia; in cases where the U wave is taller than the T wave, severe hypokalemia is usually present.\nThe chest radiograph (not shown) showed subtle diffuse osteopenia. The patient's history of renal colic would be consistent with a history of urinary stones that often occurs in patients with RTA resulting from alkaline urine and hypercalciuria. The renal ultrasound (Figure 2) showed hyperechoic regions in the renal medulla consistent with nephrocalcinosis.\nThe arterial blood gas analysis demonstrated a profound metabolic acidosis with a pH of 7.25, further confirming the diagnosis. The type of RTA was characterized by looking at the urine pH, which in this patient was 7. This is consistent with type 1 RTA, also known as \"distal RTA.\"\nDistal RTA is a rare renal disorder characterized by a nonanion gap hyperchloremic acidosis and hypokalemia. In this condition, the alpha intercalated cells of the cortical collecting duct of the distal nephron fail to secrete acid into the urine. This failure of acid secretion leads to an inability to acidify the urine to a pH < 5.5.\nBecause renal excretion is the primary means of eliminating acid from the body, a tendency toward systemic acidemia is noted. This leads to the clinical features of type 1 RTA, which include:\nNormal anion gap hyperchloremic metabolic acidosis\nHypokalemia (from multiple mechanisms, but often severe during periods of stress)[1]\nNephrocalcinosis[2]\nNephrolithiasis (related to an inability to acidify urine, hypercalciuria, and low urinary citrate)\nLoss of calcium from bones (which can cause rickets in children and osteomalacia in adults)\nDuring periods of stress caused by illness, or in this particular case the vomiting of hyperemesis gravidum, patients can have episodes of profound hypokalemia, resulting in flaccid paralysis, rhabdomyolysis, cardiac arrest, and even death.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1134048,
"choiceText": "Cushing syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134050,
"choiceText": "Addison disease",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134052,
"choiceText": "Bartter syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134054,
"choiceText": "Distal renal tubular acidosis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 359781,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 23-Year-Old Unaware She’s Pregnant With Hematuria, ECG Abnormalities"
},
{
"authors": "Greg P. Hansen, DO; Christo T. Philip, MD; Larissa I. Velez, MD",
"content": [
"Type 1 RTA is either inherited or acquired. Inherited type 1 RTA can be either autosomal-dominant or autosomal-recessive. Autosomal-recessive type 1 RTA often presents in infancy, whereas autosomal-dominant type 1 RTA may not present until adolescence or young adulthood.[3] Some patients with autosomal recessive distal RTA have associated sensorineural hearing loss.[4] Mutations in the genes encoding carbonic anhydrase II, kidney anion exchanger 1, and subunits of the H+-ATPase have been identified in patients with distal RTA.[5] Some genetic disorders, such as Ehler-Danlos syndrome, Fabry disease, or Wilson disease, have also been associated with type 1 RTA.[6] In the acquired form, the disorder can be caused by drugs, autoimmune diseases, or by infection.[6] Some of the more common acquired forms are caused by Sjögren syndrome, lupus, hepatitis, treatment with amphotericin B,[7] toluene toxicity,[8] and chronic pyelonephritis.",
"The clinical manifestations of type 1 RTA depend upon the disease severity and whether it is acquired or inherited. Inherited type 1 RTA causes similar metabolic abnormalities, but it is more likely to result in decreased bone mineralization and growth retardation.[9] However, both forms feature hypokalemia, which results in muscle soreness, flaccid paralysis, and electrical cardiac disturbances. The most common cause of death related to type 1 RTA is hypokalemia-induced cardiac dysrhythmia.",
"Type 2 RTA (proximal RTA) is caused by an inability to reabsorb bicarbonate in the proximal tubules. Type 2 RTA may occur secondary to generalized dysfunction of the proximal tubules and can be associated with increased urinary excretion of glucose, uric acid, phosphate, amino acids, and protein.[10] The disorder most often occurs in the context of Fanconi syndrome, light chain nephropathy, multiple myeloma, or drug exposures.[10]",
"Because the clinical features of both type 1 and type 2 RTA can be similar, distinguishing between them can be a diagnostic challenge. However, these two causes of nonanion gap acidosis with hypokalemia can be distinguished relatively easily with some laboratory testing. The easiest and most readily obtained laboratory examination is the urine pH. In type 1 RTA, the distal tubule is unable to acidify the urine, resulting in a urine pH > 5.5. In contrast, distal acidification is intact in type 2 RTA; this, together with an ability of the proximal tubule to reabsorb filtered bicarbonate once its concentration has fallen below its abnormally low tubular reabsorptive capacity, results in a urine pH < 5.5. With these mechanisms, type 2 RTA usually does not cause as profound a serum acidosis as type 1 RTA. For example, a serum bicarbonate of < 10 mEq/L is not uncommon in type 1 RTA, whereas in type 2 RTA, the bicarbonate level is usually > 15 mEq/L.",
"Type 3 RTA is the rarest of the four forms and is basically a combination of both type 1 and type 2 RTA. Type 3 RTA is usually the result of an inherited carbonic anhydrase II mutation, and it gives rise to an autosomal-recessive syndrome of metabolic acidosis, hypokalemia, osteoporosis, cerebral calcification, and intellectual disability.",
"Type 4 RTA, also called \"hyperkalemic RTA,\" is caused by either aldosterone deficiency or resistance of the renal tubule to the actions of aldosterone. This form is readily distinguished from type 1 and type 2 RTA because type 4 RTA results in hyperkalemia rather than hypokalemia.",
"The diagnostic studies used to diagnose type 1 RTA include serum electrolytes, renal electrolytes, urinalysis, and 24-hour urine citrate and calcium measurements. In a patient with borderline acidosis and hypokalemia, an acid load test can often be diagnostic. This test entails giving an acid load of 0.1 g/kg of ammonium chloride or fludrocortisone/furosemide and then checking the urine pH 4-6 hours later.[11] The test is considered positive if the urine pH remains above 5.5. However, the acid load test is not advisable during periods of profound acidosis and should be used only for stable patients in otherwise nondiagnostic cases.",
"An ECG should be obtained if severe hypokalemia is suspected, which often presents as muscle weakness. Renal imaging can often show evidence of nephrolithiasis or nephrocalcinosis."
],
"date": "February 02, 2022",
"figures": [],
"markdown": "# A 23-Year-Old Unaware She’s Pregnant With Hematuria, ECG Abnormalities\n\n **Authors:** Greg P. Hansen, DO; Christo T. Philip, MD; Larissa I. Velez, MD \n **Date:** February 02, 2022\n\n ## Content\n\n Type 1 RTA is either inherited or acquired. Inherited type 1 RTA can be either autosomal-dominant or autosomal-recessive. Autosomal-recessive type 1 RTA often presents in infancy, whereas autosomal-dominant type 1 RTA may not present until adolescence or young adulthood.[3] Some patients with autosomal recessive distal RTA have associated sensorineural hearing loss.[4] Mutations in the genes encoding carbonic anhydrase II, kidney anion exchanger 1, and subunits of the H+-ATPase have been identified in patients with distal RTA.[5] Some genetic disorders, such as Ehler-Danlos syndrome, Fabry disease, or Wilson disease, have also been associated with type 1 RTA.[6] In the acquired form, the disorder can be caused by drugs, autoimmune diseases, or by infection.[6] Some of the more common acquired forms are caused by Sjögren syndrome, lupus, hepatitis, treatment with amphotericin B,[7] toluene toxicity,[8] and chronic pyelonephritis.\nThe clinical manifestations of type 1 RTA depend upon the disease severity and whether it is acquired or inherited. Inherited type 1 RTA causes similar metabolic abnormalities, but it is more likely to result in decreased bone mineralization and growth retardation.[9] However, both forms feature hypokalemia, which results in muscle soreness, flaccid paralysis, and electrical cardiac disturbances. The most common cause of death related to type 1 RTA is hypokalemia-induced cardiac dysrhythmia.\nType 2 RTA (proximal RTA) is caused by an inability to reabsorb bicarbonate in the proximal tubules. Type 2 RTA may occur secondary to generalized dysfunction of the proximal tubules and can be associated with increased urinary excretion of glucose, uric acid, phosphate, amino acids, and protein.[10] The disorder most often occurs in the context of Fanconi syndrome, light chain nephropathy, multiple myeloma, or drug exposures.[10]\nBecause the clinical features of both type 1 and type 2 RTA can be similar, distinguishing between them can be a diagnostic challenge. However, these two causes of nonanion gap acidosis with hypokalemia can be distinguished relatively easily with some laboratory testing. The easiest and most readily obtained laboratory examination is the urine pH. In type 1 RTA, the distal tubule is unable to acidify the urine, resulting in a urine pH > 5.5. In contrast, distal acidification is intact in type 2 RTA; this, together with an ability of the proximal tubule to reabsorb filtered bicarbonate once its concentration has fallen below its abnormally low tubular reabsorptive capacity, results in a urine pH < 5.5. With these mechanisms, type 2 RTA usually does not cause as profound a serum acidosis as type 1 RTA. For example, a serum bicarbonate of < 10 mEq/L is not uncommon in type 1 RTA, whereas in type 2 RTA, the bicarbonate level is usually > 15 mEq/L.\nType 3 RTA is the rarest of the four forms and is basically a combination of both type 1 and type 2 RTA. Type 3 RTA is usually the result of an inherited carbonic anhydrase II mutation, and it gives rise to an autosomal-recessive syndrome of metabolic acidosis, hypokalemia, osteoporosis, cerebral calcification, and intellectual disability.\nType 4 RTA, also called \"hyperkalemic RTA,\" is caused by either aldosterone deficiency or resistance of the renal tubule to the actions of aldosterone. This form is readily distinguished from type 1 and type 2 RTA because type 4 RTA results in hyperkalemia rather than hypokalemia.\nThe diagnostic studies used to diagnose type 1 RTA include serum electrolytes, renal electrolytes, urinalysis, and 24-hour urine citrate and calcium measurements. In a patient with borderline acidosis and hypokalemia, an acid load test can often be diagnostic. This test entails giving an acid load of 0.1 g/kg of ammonium chloride or fludrocortisone/furosemide and then checking the urine pH 4-6 hours later.[11] The test is considered positive if the urine pH remains above 5.5. However, the acid load test is not advisable during periods of profound acidosis and should be used only for stable patients in otherwise nondiagnostic cases.\nAn ECG should be obtained if severe hypokalemia is suspected, which often presents as muscle weakness. Renal imaging can often show evidence of nephrolithiasis or nephrocalcinosis.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A 23-Year-Old Unaware She’s Pregnant With Hematuria, ECG Abnormalities"
},
{
"authors": "Greg P. Hansen, DO; Christo T. Philip, MD; Larissa I. Velez, MD",
"content": [
"The cornerstone of medical treatment for type 1 RTA first entails addressing the underlying metabolic derangements. This is accomplished by replenishing potassium with oral and intravenous potassium chloride or potassium citrate. The latter is often more beneficial in patients with recurrent renal stones.[12] In addition, oral sodium bicarbonate (1-2 mEq/kg/d) can often help meet the alkali requirements and compensate for the lost bicarbonate. In inherited type 1 RTA, early medical therapy can mitigate growth retardation and bone demineralization.",
"The patient in this case was treated with large amounts of oral and intravenous potassium chloride and admitted to the medical intensive care unit for further management. During her 1-week hospitalization, the nephrology and obstetrics services were both consulted. The obstetrics service performed transabdominal ultrasound, which demonstrated an intrauterine 8-week embryo with normal cardiac motion. A regular regimen of oral potassium citrate, bicarbonate, folate, and prenatal vitamins was initiated.",
"On the day of discharge, the patient's electrolyte derangements had corrected with oral therapy, and her nausea was controlled with oral ondansetron. The patient was discharged home on hospital day 7, and she had a normal basic metabolic panel 3 weeks after discharge."
],
"date": "February 02, 2022",
"figures": [],
"markdown": "# A 23-Year-Old Unaware She’s Pregnant With Hematuria, ECG Abnormalities\n\n **Authors:** Greg P. Hansen, DO; Christo T. Philip, MD; Larissa I. Velez, MD \n **Date:** February 02, 2022\n\n ## Content\n\n The cornerstone of medical treatment for type 1 RTA first entails addressing the underlying metabolic derangements. This is accomplished by replenishing potassium with oral and intravenous potassium chloride or potassium citrate. The latter is often more beneficial in patients with recurrent renal stones.[12] In addition, oral sodium bicarbonate (1-2 mEq/kg/d) can often help meet the alkali requirements and compensate for the lost bicarbonate. In inherited type 1 RTA, early medical therapy can mitigate growth retardation and bone demineralization.\nThe patient in this case was treated with large amounts of oral and intravenous potassium chloride and admitted to the medical intensive care unit for further management. During her 1-week hospitalization, the nephrology and obstetrics services were both consulted. The obstetrics service performed transabdominal ultrasound, which demonstrated an intrauterine 8-week embryo with normal cardiac motion. A regular regimen of oral potassium citrate, bicarbonate, folate, and prenatal vitamins was initiated.\nOn the day of discharge, the patient's electrolyte derangements had corrected with oral therapy, and her nausea was controlled with oral ondansetron. The patient was discharged home on hospital day 7, and she had a normal basic metabolic panel 3 weeks after discharge.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1134056,
"choiceText": "Challenge with oral sodium bicarbonate, which should cause the urine pH to remain > 5.5 in type 1 RTA",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134058,
"choiceText": "Challenge with oral sodium bicarbonate, which should cause the urine pH to remain < 5.5 in type 1 RTA",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134060,
"choiceText": "Challenge with ammonium chloride, which should cause the urine pH to remain > 5.5 in type 1 RTA",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134062,
"choiceText": "Challenge with ammonium chloride, which should cause the urine pH to remain < 5.5 in type 1 RTA",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The diagnostic studies used to diagnose type 1 RTA include serum electrolytes, renal electrolytes, urinalysis, and 24-hour urine citrate and calcium measurements. In a patient with borderline acidosis and hypokalemia, an acid load test can often be diagnostic. This test entails giving an acid load of 0.1 g/kg of ammonium chloride or fludrocortisone/furosemide and then checking the urine pH 4-6 hours later. The test is considered positive if the urine pH remains above 5.5. However, the acid load test is not advisable during periods of profound acidosis and should be used only for stable patients in otherwise nondiagnostic cases.<br>\r\n<br>\r\nAn ECG should be obtained if severe hypokalemia is suspected, which often presents as muscle weakness. Renal imaging can often show evidence of nephrolithiasis or nephrocalcinosis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 359783,
"questionText": "In cases in which distinguishing between type and type 2 RTA is difficult, which is the test of choice, and what results are expected?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1134064,
"choiceText": "Hyperchloremic metabolic acidosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134066,
"choiceText": "Hyperkalemia",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134068,
"choiceText": "Nephrocalcinosis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134070,
"choiceText": "Osteomalacia",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134072,
"choiceText": "Ehler-Danlos syndrome, Sjögren syndrome, or exposure to toluene",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Type 4 RTA, also called \"hyperkalemic RTA,\" is caused by either aldosterone deficiency or resistance of the renal tubule to the actions of aldosterone. This form is readily distinguished from type 1 and type 2 RTA because type 4 RTA results in hyperkalemia rather than hypokalemia.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 359785,
"questionText": "Which of the following conditions is associated with type 4 RTA?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 23-Year-Old Unaware She’s Pregnant With Hematuria, ECG Abnormalities"
},
{
"authors": "Greg P. Hansen, DO; Christo T. Philip, MD; Larissa I. Velez, MD",
"content": [],
"date": "February 02, 2022",
"figures": [],
"markdown": "# A 23-Year-Old Unaware She’s Pregnant With Hematuria, ECG Abnormalities\n\n **Authors:** Greg P. Hansen, DO; Christo T. Philip, MD; Larissa I. Velez, MD \n **Date:** February 02, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1134056,
"choiceText": "Challenge with oral sodium bicarbonate, which should cause the urine pH to remain > 5.5 in type 1 RTA",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134058,
"choiceText": "Challenge with oral sodium bicarbonate, which should cause the urine pH to remain < 5.5 in type 1 RTA",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134060,
"choiceText": "Challenge with ammonium chloride, which should cause the urine pH to remain > 5.5 in type 1 RTA",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134062,
"choiceText": "Challenge with ammonium chloride, which should cause the urine pH to remain < 5.5 in type 1 RTA",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The diagnostic studies used to diagnose type 1 RTA include serum electrolytes, renal electrolytes, urinalysis, and 24-hour urine citrate and calcium measurements. In a patient with borderline acidosis and hypokalemia, an acid load test can often be diagnostic. This test entails giving an acid load of 0.1 g/kg of ammonium chloride or fludrocortisone/furosemide and then checking the urine pH 4-6 hours later. The test is considered positive if the urine pH remains above 5.5. However, the acid load test is not advisable during periods of profound acidosis and should be used only for stable patients in otherwise nondiagnostic cases.<br>\r\n<br>\r\nAn ECG should be obtained if severe hypokalemia is suspected, which often presents as muscle weakness. Renal imaging can often show evidence of nephrolithiasis or nephrocalcinosis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 359783,
"questionText": "In cases in which distinguishing between type and type 2 RTA is difficult, which is the test of choice, and what results are expected?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1134064,
"choiceText": "Hyperchloremic metabolic acidosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134066,
"choiceText": "Hyperkalemia",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134068,
"choiceText": "Nephrocalcinosis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134070,
"choiceText": "Osteomalacia",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134072,
"choiceText": "Ehler-Danlos syndrome, Sjögren syndrome, or exposure to toluene",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Type 4 RTA, also called \"hyperkalemic RTA,\" is caused by either aldosterone deficiency or resistance of the renal tubule to the actions of aldosterone. This form is readily distinguished from type 1 and type 2 RTA because type 4 RTA results in hyperkalemia rather than hypokalemia.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 359785,
"questionText": "Which of the following conditions is associated with type 4 RTA?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 23-Year-Old Unaware She’s Pregnant With Hematuria, ECG Abnormalities"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1134048,
"choiceText": "Cushing syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134050,
"choiceText": "Addison disease",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134052,
"choiceText": "Bartter syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134054,
"choiceText": "Distal renal tubular acidosis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 359781,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1134056,
"choiceText": "Challenge with oral sodium bicarbonate, which should cause the urine pH to remain > 5.5 in type 1 RTA",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134058,
"choiceText": "Challenge with oral sodium bicarbonate, which should cause the urine pH to remain < 5.5 in type 1 RTA",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134060,
"choiceText": "Challenge with ammonium chloride, which should cause the urine pH to remain > 5.5 in type 1 RTA",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134062,
"choiceText": "Challenge with ammonium chloride, which should cause the urine pH to remain < 5.5 in type 1 RTA",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The diagnostic studies used to diagnose type 1 RTA include serum electrolytes, renal electrolytes, urinalysis, and 24-hour urine citrate and calcium measurements. In a patient with borderline acidosis and hypokalemia, an acid load test can often be diagnostic. This test entails giving an acid load of 0.1 g/kg of ammonium chloride or fludrocortisone/furosemide and then checking the urine pH 4-6 hours later. The test is considered positive if the urine pH remains above 5.5. However, the acid load test is not advisable during periods of profound acidosis and should be used only for stable patients in otherwise nondiagnostic cases.<br>\r\n<br>\r\nAn ECG should be obtained if severe hypokalemia is suspected, which often presents as muscle weakness. Renal imaging can often show evidence of nephrolithiasis or nephrocalcinosis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 359783,
"questionText": "In cases in which distinguishing between type and type 2 RTA is difficult, which is the test of choice, and what results are expected?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1134064,
"choiceText": "Hyperchloremic metabolic acidosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134066,
"choiceText": "Hyperkalemia",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134068,
"choiceText": "Nephrocalcinosis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134070,
"choiceText": "Osteomalacia",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1134072,
"choiceText": "Ehler-Danlos syndrome, Sjögren syndrome, or exposure to toluene",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Type 4 RTA, also called \"hyperkalemic RTA,\" is caused by either aldosterone deficiency or resistance of the renal tubule to the actions of aldosterone. This form is readily distinguished from type 1 and type 2 RTA because type 4 RTA results in hyperkalemia rather than hypokalemia.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 359785,
"questionText": "Which of the following conditions is associated with type 4 RTA?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
736108 | /viewarticle/736108 | [
{
"authors": "Lee Neilson, MD; Elena Cecilia Rosca, MD, PhD; Simu Mihaela, MD, PhD; Chirileanu Ruxanda Dana, MD, PhD",
"content": [
"Editor's Note:\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.",
"A 72-year-old man is brought to the neurology clinic by his family after a 1-month history of episodic altered mental status, agitation, and hallucinations. The patient reports having insomnia, nonthreatening visual hallucinations (most frequently of people), and rarely, auditory hallucinations. His wife remarks, \"Some days he is not himself, and the next day he is fine.\"",
"Seven months earlier, the patient was diagnosed with Parkinson disease and started on a carbidopa/levodopa combination; however, he experienced only a mild response to medication.",
"His medical history includes asymptomatic lacunar infarcts, stage 2 hypertension, orthostatic hypotension, ischemic cardiomyopathy, coronary artery bypass surgery, and dyslipidemia. He has no history of underlying psychiatric disorder. His current medications include carbidopa/levodopa, clopidogrel, ramipril, metoprolol, spironolactone, furosemide, isosorbide dinitrate, and simvastatin. He does not smoke, drink alcohol, or use illicit drugs."
],
"date": "January 21, 2022",
"figures": [],
"markdown": "# Neurology Case Challenge: Visual and Auditory Hallucinations in a Patient With Parkinson Disease\n\n **Authors:** Lee Neilson, MD; Elena Cecilia Rosca, MD, PhD; Simu Mihaela, MD, PhD; Chirileanu Ruxanda Dana, MD, PhD \n **Date:** January 21, 2022\n\n ## Content\n\n Editor's Note:\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.\nA 72-year-old man is brought to the neurology clinic by his family after a 1-month history of episodic altered mental status, agitation, and hallucinations. The patient reports having insomnia, nonthreatening visual hallucinations (most frequently of people), and rarely, auditory hallucinations. His wife remarks, \"Some days he is not himself, and the next day he is fine.\"\nSeven months earlier, the patient was diagnosed with Parkinson disease and started on a carbidopa/levodopa combination; however, he experienced only a mild response to medication.\nHis medical history includes asymptomatic lacunar infarcts, stage 2 hypertension, orthostatic hypotension, ischemic cardiomyopathy, coronary artery bypass surgery, and dyslipidemia. He has no history of underlying psychiatric disorder. His current medications include carbidopa/levodopa, clopidogrel, ramipril, metoprolol, spironolactone, furosemide, isosorbide dinitrate, and simvastatin. He does not smoke, drink alcohol, or use illicit drugs.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Neurology Case Challenge: Visual and Auditory Hallucinations in a Patient With Parkinson Disease"
},
{
"authors": "Lee Neilson, MD; Elena Cecilia Rosca, MD, PhD; Simu Mihaela, MD, PhD; Chirileanu Ruxanda Dana, MD, PhD",
"content": [
"Upon physical examination, he appears well and has a temperature of 98.2°F (36.8°C), blood pressure of 130/77 mm Hg, and a regular pulse of 68 beats/min. The chest, cardiovascular, and abdominal examination findings are all normal. The neurologic examination shows the patient to be alert and oriented to person and place but not to time. He has some difficulty finding words to express himself and has impaired short-term memory (Mini Mental Status Examination = 25/30) as well as impaired concentration, as evidenced by losing his train of thought in the middle of a sentence. His affect is depressed and he has problems with executive function and visuospatial tasks.",
"Although his blink rate is reduced, the cranial nerve examination findings are otherwise unremarkable. The motor examination reveals mild rigidity at the neck in both arms, along with bradykinesia with finger taps, opening and closing of the hands, pronation-supination arm movement, and heel taps. Sensation, coordination, and reflex testing are unremarkable. Examination of the patient's gait shows a mildly hunched posture, shortened stride length, and postural instability.",
"The laboratory analysis, including a complete blood cell count, vitamin B12, folate, erythrocyte sedimentation rate, and liver, thyroid, and renal panels, is normal. His cholesterol is elevated at 248 mg/dL (reference range <200 mg/dL), but his high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, and triglyceride levels are all normal. Serologic tests for syphilis and HIV infection are negative. The CT scan of the brain below shows scattered lacunar infarcts and mild cortical atrophy without ventricular dilatation.",
"Figure 1."
],
"date": "January 21, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/736/108/736108-thumb1.png"
}
],
"markdown": "# Neurology Case Challenge: Visual and Auditory Hallucinations in a Patient With Parkinson Disease\n\n **Authors:** Lee Neilson, MD; Elena Cecilia Rosca, MD, PhD; Simu Mihaela, MD, PhD; Chirileanu Ruxanda Dana, MD, PhD \n **Date:** January 21, 2022\n\n ## Content\n\n Upon physical examination, he appears well and has a temperature of 98.2°F (36.8°C), blood pressure of 130/77 mm Hg, and a regular pulse of 68 beats/min. The chest, cardiovascular, and abdominal examination findings are all normal. The neurologic examination shows the patient to be alert and oriented to person and place but not to time. He has some difficulty finding words to express himself and has impaired short-term memory (Mini Mental Status Examination = 25/30) as well as impaired concentration, as evidenced by losing his train of thought in the middle of a sentence. His affect is depressed and he has problems with executive function and visuospatial tasks.\nAlthough his blink rate is reduced, the cranial nerve examination findings are otherwise unremarkable. The motor examination reveals mild rigidity at the neck in both arms, along with bradykinesia with finger taps, opening and closing of the hands, pronation-supination arm movement, and heel taps. Sensation, coordination, and reflex testing are unremarkable. Examination of the patient's gait shows a mildly hunched posture, shortened stride length, and postural instability.\nThe laboratory analysis, including a complete blood cell count, vitamin B12, folate, erythrocyte sedimentation rate, and liver, thyroid, and renal panels, is normal. His cholesterol is elevated at 248 mg/dL (reference range <200 mg/dL), but his high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, and triglyceride levels are all normal. Serologic tests for syphilis and HIV infection are negative. The CT scan of the brain below shows scattered lacunar infarcts and mild cortical atrophy without ventricular dilatation.\nFigure 1.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 388446,
"choiceText": "Vascular dementia",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388447,
"choiceText": "Parkinson disease dementia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388448,
"choiceText": "Dementia with Lewy bodies",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388449,
"choiceText": "Carbidopa/levodopa side effects",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388450,
"choiceText": "Alzheimer disease",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 112612,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Neurology Case Challenge: Visual and Auditory Hallucinations in a Patient With Parkinson Disease"
},
{
"authors": "Lee Neilson, MD; Elena Cecilia Rosca, MD, PhD; Simu Mihaela, MD, PhD; Chirileanu Ruxanda Dana, MD, PhD",
"content": [
"Dementia with Lewy bodies (DLB) was diagnosed based on the patient's history and the results of the neurologic and neuropsychologic examinations. The progression from delirium to frank parkinsonism to dementia shortly thereafter with episodes of altered mental status and visual and auditory hallucinations, is highly suggestive of the diagnosis.",
"DLB is the second most common neurodegenerative dementia after Alzheimer disease (AD), accounting for approximately 4.2% of dementia diagnoses in community settings and 7.5% of diagnoses in secondary care; however, these numbers are likely underestimates, as misdiagnosis is common.[1,2] It may present as a predominant dementia with some extrapyramidal signs or initially as parkinsonism with early-onset dementia, which is typically (although somewhat controversially) defined as dementia onset within 1 year.[3] Brief periods of confusion are present early in the disease course in a milieu of gradually worsening cognition, as well as impaired executive function and attention, with a tendency toward fluctuating cognitive performance. In fact, antecedent delirium increases the risk of progression to dementia, and evidence between delirium and DLB is mounting.[4]",
"The cognitive profile of a patient with DLB is typically early visuospatial impairment with rapid rate of decline; however, impairments in attention and executive function are also observed. Although memory function is less severe relative to AD, the rate of decline is similar.[5] Psychiatric symptoms are common. Hallucinations are prominent and rise to the level of a core clinical feature. The hallucinations tend to be visual but can occur in nonvisual modalities. Pareidolia, the perception of meaningful objects embedded visual scenes, is also characteristic of DLB.[6] Delusions, including delusional misidentification syndromes, are reported in as many as 50% of patients with DLB and may be an early finding.[7]",
"Currently, the definitive diagnosis of DLB rests on autopsy findings, with the presence of Lewy bodies situated in the substantia nigra and other brainstem nuclei (locus coeruleus, dorsal raphe, nucleus basalis of Meynert, dorsal motor nucleus of cranial nerve X) and the cerebral cortex (mainly in the amygdala and the entorhinal and anterior cingulate regions, but also in the neocortex).[8] Clinical diagnostic consensus criteria have, however, been developed for DLB.[9] The diagnosis of probable DLB requires a diagnosis of dementia in addition to 2 core features or 1 core feature and 1 indicative biomarker. Possible DLB can be diagnosed with either 1 core feature or indicative biomarker.",
"Core clinical features include the following:",
"Fluctuating cognition with pronounced variations in attention and alertness",
"Recurrent visual hallucinations",
"REM sleep behavior disorder (RBD)",
"Parkinsonism (presence of bradykinesia, rest tremor, or rigidity)",
"Indicative biomarkers include the following:",
"Reduced basal ganglia dopamine transporter uptake (single-photon emission computed tomography [SPECT] or positron-emission tomography [PET])",
"Abnormal (low uptake) 123iodine-MIBG myocardial scintigraphy",
"Polysomnographic confirmation of REM sleep without atonia",
"The cognitive fluctuations in DLB are deliriumlike, fluctuating from hour-to-hour and not perceived as \"good days and bad days\" nor a circadian phenomenon (ie, sundowning). RBD, in which the patient lashes out and shouts during vivid dreams, can often precede dementia by many years. Although comorbid posttraumatic stress disorder (PTSD) or concomitant use of selective serotonin reuptake inhibitors (SSRIs) may confound the ascertainment of true RBD, asking the question \"Have you ever seen the patient appear to act out their dreams while sleeping?\" can yield a positive predictive value of as high as 93%.[10]",
"Other supportive clinical features have been proposed. Although these lack diagnostic specificity, they are commonly present and may manifest early in the disease. These include the following:[11]",
"Severe sensitivity to antipsychotic agents",
"Postural instability",
"Repeated falls",
"Syncope or other transient episodes of unresponsiveness",
"Severe autonomic dysfunction (eg, constipation, orthostatic hypotension, urinary incontinence)",
"Hypersomnia",
"Hyposmia",
"Hallucinations in nonvisual modalities",
"Systematized delusions",
"Apathy",
"Anxiety",
"Depression",
"Occasional findings include supranuclear gaze palsy and myoclonus. Whereas the myoclonus of Parkinson disease is typically of small amplitude and may be confused with tremor, myoclonus in DLB can be of larger amplitude, more likely to occur at rest, and more prevalent.[12]",
"The current case fulfills the diagnostic criteria for probable DLB, with 3 core features."
],
"date": "January 21, 2022",
"figures": [],
"markdown": "# Neurology Case Challenge: Visual and Auditory Hallucinations in a Patient With Parkinson Disease\n\n **Authors:** Lee Neilson, MD; Elena Cecilia Rosca, MD, PhD; Simu Mihaela, MD, PhD; Chirileanu Ruxanda Dana, MD, PhD \n **Date:** January 21, 2022\n\n ## Content\n\n Dementia with Lewy bodies (DLB) was diagnosed based on the patient's history and the results of the neurologic and neuropsychologic examinations. The progression from delirium to frank parkinsonism to dementia shortly thereafter with episodes of altered mental status and visual and auditory hallucinations, is highly suggestive of the diagnosis.\nDLB is the second most common neurodegenerative dementia after Alzheimer disease (AD), accounting for approximately 4.2% of dementia diagnoses in community settings and 7.5% of diagnoses in secondary care; however, these numbers are likely underestimates, as misdiagnosis is common.[1,2] It may present as a predominant dementia with some extrapyramidal signs or initially as parkinsonism with early-onset dementia, which is typically (although somewhat controversially) defined as dementia onset within 1 year.[3] Brief periods of confusion are present early in the disease course in a milieu of gradually worsening cognition, as well as impaired executive function and attention, with a tendency toward fluctuating cognitive performance. In fact, antecedent delirium increases the risk of progression to dementia, and evidence between delirium and DLB is mounting.[4]\nThe cognitive profile of a patient with DLB is typically early visuospatial impairment with rapid rate of decline; however, impairments in attention and executive function are also observed. Although memory function is less severe relative to AD, the rate of decline is similar.[5] Psychiatric symptoms are common. Hallucinations are prominent and rise to the level of a core clinical feature. The hallucinations tend to be visual but can occur in nonvisual modalities. Pareidolia, the perception of meaningful objects embedded visual scenes, is also characteristic of DLB.[6] Delusions, including delusional misidentification syndromes, are reported in as many as 50% of patients with DLB and may be an early finding.[7]\nCurrently, the definitive diagnosis of DLB rests on autopsy findings, with the presence of Lewy bodies situated in the substantia nigra and other brainstem nuclei (locus coeruleus, dorsal raphe, nucleus basalis of Meynert, dorsal motor nucleus of cranial nerve X) and the cerebral cortex (mainly in the amygdala and the entorhinal and anterior cingulate regions, but also in the neocortex).[8] Clinical diagnostic consensus criteria have, however, been developed for DLB.[9] The diagnosis of probable DLB requires a diagnosis of dementia in addition to 2 core features or 1 core feature and 1 indicative biomarker. Possible DLB can be diagnosed with either 1 core feature or indicative biomarker.\nCore clinical features include the following:\nFluctuating cognition with pronounced variations in attention and alertness\nRecurrent visual hallucinations\nREM sleep behavior disorder (RBD)\nParkinsonism (presence of bradykinesia, rest tremor, or rigidity)\nIndicative biomarkers include the following:\nReduced basal ganglia dopamine transporter uptake (single-photon emission computed tomography [SPECT] or positron-emission tomography [PET])\nAbnormal (low uptake) 123iodine-MIBG myocardial scintigraphy\nPolysomnographic confirmation of REM sleep without atonia\nThe cognitive fluctuations in DLB are deliriumlike, fluctuating from hour-to-hour and not perceived as \"good days and bad days\" nor a circadian phenomenon (ie, sundowning). RBD, in which the patient lashes out and shouts during vivid dreams, can often precede dementia by many years. Although comorbid posttraumatic stress disorder (PTSD) or concomitant use of selective serotonin reuptake inhibitors (SSRIs) may confound the ascertainment of true RBD, asking the question \"Have you ever seen the patient appear to act out their dreams while sleeping?\" can yield a positive predictive value of as high as 93%.[10]\nOther supportive clinical features have been proposed. Although these lack diagnostic specificity, they are commonly present and may manifest early in the disease. These include the following:[11]\nSevere sensitivity to antipsychotic agents\nPostural instability\nRepeated falls\nSyncope or other transient episodes of unresponsiveness\nSevere autonomic dysfunction (eg, constipation, orthostatic hypotension, urinary incontinence)\nHypersomnia\nHyposmia\nHallucinations in nonvisual modalities\nSystematized delusions\nApathy\nAnxiety\nDepression\nOccasional findings include supranuclear gaze palsy and myoclonus. Whereas the myoclonus of Parkinson disease is typically of small amplitude and may be confused with tremor, myoclonus in DLB can be of larger amplitude, more likely to occur at rest, and more prevalent.[12]\nThe current case fulfills the diagnostic criteria for probable DLB, with 3 core features.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 388446,
"choiceText": "Vascular dementia",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388447,
"choiceText": "Parkinson disease dementia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388448,
"choiceText": "Dementia with Lewy bodies",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388449,
"choiceText": "Carbidopa/levodopa side effects",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388450,
"choiceText": "Alzheimer disease",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 112612,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Neurology Case Challenge: Visual and Auditory Hallucinations in a Patient With Parkinson Disease"
},
{
"authors": "Lee Neilson, MD; Elena Cecilia Rosca, MD, PhD; Simu Mihaela, MD, PhD; Chirileanu Ruxanda Dana, MD, PhD",
"content": [
"The main differential diagnostic consideration in DLB is Parkinson disease dementia (PDD) because the clinical features of DLB are very similar to those of PDD. They share many pathologic and clinical features, probably representing 2 clinical entities on a spectrum of Lewy body disease.[13] Although no clinical or pathologic basis can determine a definite time interval between the development of motor symptoms and the onset of dementia in differentiating DLB from PDD, to avoid confusion in clinical practice, a diagnosis of DLB should be made when dementia precedes or occurs within 1 year of the development of motor symptoms, whereas a diagnosis of PDD is appropriate when dementia develops within the context of established Parkinson disease.[9,14]",
"In this case, cognitive features appeared 7 months after extrapyramidal symptoms. Furthermore, the motor signs did not respond well to levodopa. Given these facts and the features described above, DLB was suspected.",
"Other entities in the differential diagnosis for this case include vascular dementia and AD. This patient had lacunar infarcts, which can cause vascular parkinsonism and dementia, but the neuroimaging results showed that the cerebrovascular disease was not of sufficient severity to account for all of his cognitive deficits. DLB can occasionally be confused with AD. In fact, half of all individuals with DLB are estimated to have sufficient pathology for a secondary neuropathological diagnosis of AD at autopsy.[15] However, patients with DLB more frequently have frontal lobe dysfunction, with marked impairment on tests of executive function and attention. In addition, those with DLB perform significantly worse on visuospatial tests than those with Parkinson disease, and their visual hallucinations are more prominent. Patients with AD also have poorer memory task performance. This disproportionate performance in different cognitive domains may help differentiate DLB from AD.[16] This patient's pattern of cognitive impairment, visual hallucinations, and fluctuating cognition favors a diagnosis of DLB.",
"Other potentially reversible or treatable causes of dementia must also be excluded. American Academy of Neurology (AAN) guidelines recommend screening for B12 deficiency, hypothyroidism, and depression. The normal vitamin B12 and folate levels ruled out these nutritional deficiencies. The normal thyroid panel excluded hypothyroidism as a cause for the patient's presentation. Testing for syphilis and HIV is typically reserved for situations with a high clinical suspicion, based on sexual history or travel to areas where exposure is more common. In this case, the patient’s results were negative.",
"The cerebral CT scan was performed to assess for structural pathology, such as a subdural hematoma (which can cause fluctuating cognition), a mass lesion (which can cause various symptoms and signs), or signs of normal pressure hydrocephalus (which presents as gait disturbance sometimes reminiscent of parkinsonian gait, dementia, and urinary incontinence and may require an MRI scan with a cerebrospinal fluid flow study for further imaging confirmation). Other indicators that warrant additional workup may include rapid decline in function, younger age of onset, prominent fluctuations, high-risk exposures, high-risk behaviors, unexplained neurological examination findings, and incongruent performance on neuropsychological testing.[17]",
"This patient's carbidopa/levodopa was stopped because this treatment can exacerbate behavioral or psychotic symptoms and because the patient had no demonstrable improvement. Only modest evidence is available for the treatment of DLB symptoms; however, expert consensus does offer some management strategies.[18] Data on the best treatment option for motor symptoms in patients with DLB are insufficient. Levodopa can improve motor function and is least likely to aggravate psychosis, but its risk-benefit ratio must be considered. The use of other Parkinson disease medications, such as anticholinergics, catechol-O-methyl-transferase inhibitors, monoamine oxidase inhibitors, and amantadine, may exacerbate cognitive impairments and should be avoided.[19] Zonisamide, a common antiseizure medication, has been shown to improve motor function without exacerbating psychiatric symptoms at doses of 25-50 mg/day when given as an adjunct to levodopa.[20]"
],
"date": "January 21, 2022",
"figures": [],
"markdown": "# Neurology Case Challenge: Visual and Auditory Hallucinations in a Patient With Parkinson Disease\n\n **Authors:** Lee Neilson, MD; Elena Cecilia Rosca, MD, PhD; Simu Mihaela, MD, PhD; Chirileanu Ruxanda Dana, MD, PhD \n **Date:** January 21, 2022\n\n ## Content\n\n The main differential diagnostic consideration in DLB is Parkinson disease dementia (PDD) because the clinical features of DLB are very similar to those of PDD. They share many pathologic and clinical features, probably representing 2 clinical entities on a spectrum of Lewy body disease.[13] Although no clinical or pathologic basis can determine a definite time interval between the development of motor symptoms and the onset of dementia in differentiating DLB from PDD, to avoid confusion in clinical practice, a diagnosis of DLB should be made when dementia precedes or occurs within 1 year of the development of motor symptoms, whereas a diagnosis of PDD is appropriate when dementia develops within the context of established Parkinson disease.[9,14]\nIn this case, cognitive features appeared 7 months after extrapyramidal symptoms. Furthermore, the motor signs did not respond well to levodopa. Given these facts and the features described above, DLB was suspected.\nOther entities in the differential diagnosis for this case include vascular dementia and AD. This patient had lacunar infarcts, which can cause vascular parkinsonism and dementia, but the neuroimaging results showed that the cerebrovascular disease was not of sufficient severity to account for all of his cognitive deficits. DLB can occasionally be confused with AD. In fact, half of all individuals with DLB are estimated to have sufficient pathology for a secondary neuropathological diagnosis of AD at autopsy.[15] However, patients with DLB more frequently have frontal lobe dysfunction, with marked impairment on tests of executive function and attention. In addition, those with DLB perform significantly worse on visuospatial tests than those with Parkinson disease, and their visual hallucinations are more prominent. Patients with AD also have poorer memory task performance. This disproportionate performance in different cognitive domains may help differentiate DLB from AD.[16] This patient's pattern of cognitive impairment, visual hallucinations, and fluctuating cognition favors a diagnosis of DLB.\nOther potentially reversible or treatable causes of dementia must also be excluded. American Academy of Neurology (AAN) guidelines recommend screening for B12 deficiency, hypothyroidism, and depression. The normal vitamin B12 and folate levels ruled out these nutritional deficiencies. The normal thyroid panel excluded hypothyroidism as a cause for the patient's presentation. Testing for syphilis and HIV is typically reserved for situations with a high clinical suspicion, based on sexual history or travel to areas where exposure is more common. In this case, the patient’s results were negative.\nThe cerebral CT scan was performed to assess for structural pathology, such as a subdural hematoma (which can cause fluctuating cognition), a mass lesion (which can cause various symptoms and signs), or signs of normal pressure hydrocephalus (which presents as gait disturbance sometimes reminiscent of parkinsonian gait, dementia, and urinary incontinence and may require an MRI scan with a cerebrospinal fluid flow study for further imaging confirmation). Other indicators that warrant additional workup may include rapid decline in function, younger age of onset, prominent fluctuations, high-risk exposures, high-risk behaviors, unexplained neurological examination findings, and incongruent performance on neuropsychological testing.[17]\nThis patient's carbidopa/levodopa was stopped because this treatment can exacerbate behavioral or psychotic symptoms and because the patient had no demonstrable improvement. Only modest evidence is available for the treatment of DLB symptoms; however, expert consensus does offer some management strategies.[18] Data on the best treatment option for motor symptoms in patients with DLB are insufficient. Levodopa can improve motor function and is least likely to aggravate psychosis, but its risk-benefit ratio must be considered. The use of other Parkinson disease medications, such as anticholinergics, catechol-O-methyl-transferase inhibitors, monoamine oxidase inhibitors, and amantadine, may exacerbate cognitive impairments and should be avoided.[19] Zonisamide, a common antiseizure medication, has been shown to improve motor function without exacerbating psychiatric symptoms at doses of 25-50 mg/day when given as an adjunct to levodopa.[20]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Neurology Case Challenge: Visual and Auditory Hallucinations in a Patient With Parkinson Disease"
},
{
"authors": "Lee Neilson, MD; Elena Cecilia Rosca, MD, PhD; Simu Mihaela, MD, PhD; Chirileanu Ruxanda Dana, MD, PhD",
"content": [
"In this patient, the cognitive impairments and neuropsychiatric symptoms (hallucinations, cognition fluctuations) were treated with donepezil 10 mg at bedtime. Acetylcholinesterase inhibitors are useful in treating the cognitive deficits of DLB. Robust evidence supports the efficacy of rivastigmine and donepezil; however, high-quality randomized controlled studies of galantamine are lacking. The evidence for adding mematine, an N-methyl D-asparatate receptor antagonist, is mixed.[18] Investigators reported that this agent appeared to improve global clinical status and behavioral symptoms of patients with mild to moderate DLB. Compared with patients who received placebo, a higher proportion of patients with PDD and DLB who were treated with memantine showed improvement or stabilization in their clinical global status (Alzheimer's Disease Cooperative Study-clinical global impression of change [ADCS-CGIC] scores) at the end of the study.[19] Mean neuropsychiatric inventory (NPI) total scores were also significantly higher in patients with DLB who received memantine, including single-item scores for delusions, hallucinations, sleeping or night-time behavior, and appetite or eating disorder. However, no significant differences were seen in any of the cognitive tests in patients with PDD at the end of the study. The incidence of adverse events and drug discontinuation was similar between the PDD or DLB treatment and placebo groups. The most common adverse event associated with memantine treatment compared with placebo was somnolence. The most common serious adverse events reported were stroke, falls, and worsening dementia.",
"The patient in this case also received quetiapine 25 mg/day for depression and hallucinations. Data are limited regarding the treatment of depression in DLB; however, SSRIs and serotonin-norepinephrine reuptake inhibitors (SNRIs) appear to be effective and tolerated well. Typical neuroleptics (eg, haloperidol) should be avoided in the treatment of psychosis, given the sensitivity of these patients to neuroleptics and the increased risk for neuroleptic malignant syndrome.[21] When psychosis is severe or distressing, atypical neuroleptics are preferred if a cholinesterase inhibitor is insufficient. Quetiapine is relatively safe. Clozapine may be more effective, but its use mandates hematologic monitoring.[22] Pimavanserin, a serotonin receptor modulator, is currently approved only for Parkinson disease psychosis. However, one phase 3 study showed that it was effective at preventing psychosis relapse in undifferentiated dementia; 7.1% of participants in that group had DLB.[23] A similar study comparing the efficacy of pimavanserin to quetiapine is underway in Parkinson disease.[24]"
],
"date": "January 21, 2022",
"figures": [],
"markdown": "# Neurology Case Challenge: Visual and Auditory Hallucinations in a Patient With Parkinson Disease\n\n **Authors:** Lee Neilson, MD; Elena Cecilia Rosca, MD, PhD; Simu Mihaela, MD, PhD; Chirileanu Ruxanda Dana, MD, PhD \n **Date:** January 21, 2022\n\n ## Content\n\n In this patient, the cognitive impairments and neuropsychiatric symptoms (hallucinations, cognition fluctuations) were treated with donepezil 10 mg at bedtime. Acetylcholinesterase inhibitors are useful in treating the cognitive deficits of DLB. Robust evidence supports the efficacy of rivastigmine and donepezil; however, high-quality randomized controlled studies of galantamine are lacking. The evidence for adding mematine, an N-methyl D-asparatate receptor antagonist, is mixed.[18] Investigators reported that this agent appeared to improve global clinical status and behavioral symptoms of patients with mild to moderate DLB. Compared with patients who received placebo, a higher proportion of patients with PDD and DLB who were treated with memantine showed improvement or stabilization in their clinical global status (Alzheimer's Disease Cooperative Study-clinical global impression of change [ADCS-CGIC] scores) at the end of the study.[19] Mean neuropsychiatric inventory (NPI) total scores were also significantly higher in patients with DLB who received memantine, including single-item scores for delusions, hallucinations, sleeping or night-time behavior, and appetite or eating disorder. However, no significant differences were seen in any of the cognitive tests in patients with PDD at the end of the study. The incidence of adverse events and drug discontinuation was similar between the PDD or DLB treatment and placebo groups. The most common adverse event associated with memantine treatment compared with placebo was somnolence. The most common serious adverse events reported were stroke, falls, and worsening dementia.\nThe patient in this case also received quetiapine 25 mg/day for depression and hallucinations. Data are limited regarding the treatment of depression in DLB; however, SSRIs and serotonin-norepinephrine reuptake inhibitors (SNRIs) appear to be effective and tolerated well. Typical neuroleptics (eg, haloperidol) should be avoided in the treatment of psychosis, given the sensitivity of these patients to neuroleptics and the increased risk for neuroleptic malignant syndrome.[21] When psychosis is severe or distressing, atypical neuroleptics are preferred if a cholinesterase inhibitor is insufficient. Quetiapine is relatively safe. Clozapine may be more effective, but its use mandates hematologic monitoring.[22] Pimavanserin, a serotonin receptor modulator, is currently approved only for Parkinson disease psychosis. However, one phase 3 study showed that it was effective at preventing psychosis relapse in undifferentiated dementia; 7.1% of participants in that group had DLB.[23] A similar study comparing the efficacy of pimavanserin to quetiapine is underway in Parkinson disease.[24]\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 388451,
"choiceText": "Depression",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388452,
"choiceText": "Recurrent visual hallucinations",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388453,
"choiceText": "Recurrent auditory hallucinations",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388454,
"choiceText": "Repeated falls",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "There are 4 <i>core</i> features of DLB: recurrent visual hallucinations, fluctuating cognition, RBD, and parkinsonism. Visual hallucinations are the most common psychotic symptom in DLB, although other types of hallucinations may also occur. The recurrent nature of the hallucinations is characteristic and helps distinguish DLB from hallucinatory experiences that may be circumstantially provoked by anticholinergic or dopaminergic drugs or other types of dementia (such as AD). Furthermore, visual hallucinations appearing early in the course of the disease are known to correlate with the presence of cortical Lewy bodies seen on brain sectioning. Depression is a supportive, but not a core, feature of DLB. The same is true for auditory hallucinations and repeated falls.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 112613,
"questionText": "Which is a core feature of DLB?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 388455,
"choiceText": "Levodopa",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388456,
"choiceText": "Galantamine",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388457,
"choiceText": "Haloperidol",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388458,
"choiceText": "Quetiapine",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Typical neuroleptics (haloperidol) should be avoided in patients with DLB because of the risk for severe neuroleptic sensitivity reactions, neuroleptic malignant syndrome, and parkinsonism. Patients with DLB are particularly vulnerable to severe neuroleptic sensitivity reactions, even with low-dose typical neuroleptics, with increased morbidity and mortality. These reactions are characterized by a sudden onset of sedation, increased confusion, rigidity, and immobility, often leading to a fatal outcome within a few days or weeks. No absolute contraindication to levodopa is noted in patients with DLB; however, it may exacerbate behavioral and psychiatric symptoms. Galantamine may be useful in treating cognitive impairments related to DLB and appears to be safe in this setting. Quetiapine, which is an atypical antipsychotic, is also considered safe for patients with DLB who have psychiatric symptoms.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 112614,
"questionText": "Which medication must be avoided in patients with DLB?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Neurology Case Challenge: Visual and Auditory Hallucinations in a Patient With Parkinson Disease"
},
{
"authors": "Lee Neilson, MD; Elena Cecilia Rosca, MD, PhD; Simu Mihaela, MD, PhD; Chirileanu Ruxanda Dana, MD, PhD",
"content": [],
"date": "January 21, 2022",
"figures": [],
"markdown": "# Neurology Case Challenge: Visual and Auditory Hallucinations in a Patient With Parkinson Disease\n\n **Authors:** Lee Neilson, MD; Elena Cecilia Rosca, MD, PhD; Simu Mihaela, MD, PhD; Chirileanu Ruxanda Dana, MD, PhD \n **Date:** January 21, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 388451,
"choiceText": "Depression",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388452,
"choiceText": "Recurrent visual hallucinations",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388453,
"choiceText": "Recurrent auditory hallucinations",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388454,
"choiceText": "Repeated falls",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "There are 4 <i>core</i> features of DLB: recurrent visual hallucinations, fluctuating cognition, RBD, and parkinsonism. Visual hallucinations are the most common psychotic symptom in DLB, although other types of hallucinations may also occur. The recurrent nature of the hallucinations is characteristic and helps distinguish DLB from hallucinatory experiences that may be circumstantially provoked by anticholinergic or dopaminergic drugs or other types of dementia (such as AD). Furthermore, visual hallucinations appearing early in the course of the disease are known to correlate with the presence of cortical Lewy bodies seen on brain sectioning. Depression is a supportive, but not a core, feature of DLB. The same is true for auditory hallucinations and repeated falls.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 112613,
"questionText": "Which is a core feature of DLB?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 388455,
"choiceText": "Levodopa",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388456,
"choiceText": "Galantamine",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388457,
"choiceText": "Haloperidol",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388458,
"choiceText": "Quetiapine",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Typical neuroleptics (haloperidol) should be avoided in patients with DLB because of the risk for severe neuroleptic sensitivity reactions, neuroleptic malignant syndrome, and parkinsonism. Patients with DLB are particularly vulnerable to severe neuroleptic sensitivity reactions, even with low-dose typical neuroleptics, with increased morbidity and mortality. These reactions are characterized by a sudden onset of sedation, increased confusion, rigidity, and immobility, often leading to a fatal outcome within a few days or weeks. No absolute contraindication to levodopa is noted in patients with DLB; however, it may exacerbate behavioral and psychiatric symptoms. Galantamine may be useful in treating cognitive impairments related to DLB and appears to be safe in this setting. Quetiapine, which is an atypical antipsychotic, is also considered safe for patients with DLB who have psychiatric symptoms.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 112614,
"questionText": "Which medication must be avoided in patients with DLB?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Neurology Case Challenge: Visual and Auditory Hallucinations in a Patient With Parkinson Disease"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 388446,
"choiceText": "Vascular dementia",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388447,
"choiceText": "Parkinson disease dementia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388448,
"choiceText": "Dementia with Lewy bodies",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388449,
"choiceText": "Carbidopa/levodopa side effects",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388450,
"choiceText": "Alzheimer disease",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 112612,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 388451,
"choiceText": "Depression",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388452,
"choiceText": "Recurrent visual hallucinations",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388453,
"choiceText": "Recurrent auditory hallucinations",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388454,
"choiceText": "Repeated falls",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "There are 4 <i>core</i> features of DLB: recurrent visual hallucinations, fluctuating cognition, RBD, and parkinsonism. Visual hallucinations are the most common psychotic symptom in DLB, although other types of hallucinations may also occur. The recurrent nature of the hallucinations is characteristic and helps distinguish DLB from hallucinatory experiences that may be circumstantially provoked by anticholinergic or dopaminergic drugs or other types of dementia (such as AD). Furthermore, visual hallucinations appearing early in the course of the disease are known to correlate with the presence of cortical Lewy bodies seen on brain sectioning. Depression is a supportive, but not a core, feature of DLB. The same is true for auditory hallucinations and repeated falls.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 112613,
"questionText": "Which is a core feature of DLB?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 388455,
"choiceText": "Levodopa",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388456,
"choiceText": "Galantamine",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388457,
"choiceText": "Haloperidol",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 388458,
"choiceText": "Quetiapine",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Typical neuroleptics (haloperidol) should be avoided in patients with DLB because of the risk for severe neuroleptic sensitivity reactions, neuroleptic malignant syndrome, and parkinsonism. Patients with DLB are particularly vulnerable to severe neuroleptic sensitivity reactions, even with low-dose typical neuroleptics, with increased morbidity and mortality. These reactions are characterized by a sudden onset of sedation, increased confusion, rigidity, and immobility, often leading to a fatal outcome within a few days or weeks. No absolute contraindication to levodopa is noted in patients with DLB; however, it may exacerbate behavioral and psychiatric symptoms. Galantamine may be useful in treating cognitive impairments related to DLB and appears to be safe in this setting. Quetiapine, which is an atypical antipsychotic, is also considered safe for patients with DLB who have psychiatric symptoms.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 112614,
"questionText": "Which medication must be avoided in patients with DLB?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
881373 | /viewarticle/881373 | [
{
"authors": "Peter Huynh, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 16-year-old girl presents to the emergency department with generalized pruritus, eye swelling, a full-body rash, and shortness of breath after playing basketball at school. She reports that she was playing basketball with her friends when she first noticed itchy palms. She stopped playing and washed her hands. The itch worsened and was followed by a rash and shortness of breath. She also felt that her throat was tightening, and she had difficulty swallowing. She was taken to the school nurse, paramedics were called, and she was brought to the local emergency department.",
"The patient has had several similar episodes within the past year and feels that the episodes are getting worse. The first episode occurred about 1 year ago while playing volleyball in a hot gym. She developed itchy palms and stopped to go drink some water; the itchiness went away without any medical attention. Recently, the episodes have been occurring more frequently and are more severe. Some episodes are associated with even mild physical exertion, especially when the temperature outside is hot. When she stops the physical activity, the symptoms typically go away. She cannot recall eating any specific foods that are related to her episodes. She is not taking any medications, vitamins, or herbal supplements.",
"The patient is otherwise healthy, with no significant medical history. She denies any malaise, fatigue, weight loss, nausea, vomiting, fever, or joint pain. She is in the 11th grade and does well in school, getting mostly A's and only a few B's. She wants to go to college. She has many friends at school. She enjoys biking, dancing, and texting. Occasionally, dancing causes her to feel itchy, but she just \"takes a break,\" and the itch goes away."
],
"date": "January 19, 2022",
"figures": [],
"markdown": "# A 16-Year-Old Girl With Full-Body Rash, Dyspnea, and Swelling\n\n **Authors:** Peter Huynh, MD \n **Date:** January 19, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 16-year-old girl presents to the emergency department with generalized pruritus, eye swelling, a full-body rash, and shortness of breath after playing basketball at school. She reports that she was playing basketball with her friends when she first noticed itchy palms. She stopped playing and washed her hands. The itch worsened and was followed by a rash and shortness of breath. She also felt that her throat was tightening, and she had difficulty swallowing. She was taken to the school nurse, paramedics were called, and she was brought to the local emergency department.\nThe patient has had several similar episodes within the past year and feels that the episodes are getting worse. The first episode occurred about 1 year ago while playing volleyball in a hot gym. She developed itchy palms and stopped to go drink some water; the itchiness went away without any medical attention. Recently, the episodes have been occurring more frequently and are more severe. Some episodes are associated with even mild physical exertion, especially when the temperature outside is hot. When she stops the physical activity, the symptoms typically go away. She cannot recall eating any specific foods that are related to her episodes. She is not taking any medications, vitamins, or herbal supplements.\nThe patient is otherwise healthy, with no significant medical history. She denies any malaise, fatigue, weight loss, nausea, vomiting, fever, or joint pain. She is in the 11th grade and does well in school, getting mostly A's and only a few B's. She wants to go to college. She has many friends at school. She enjoys biking, dancing, and texting. Occasionally, dancing causes her to feel itchy, but she just \"takes a break,\" and the itch goes away.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A 16-Year-Old Girl With Full-Body Rash, Dyspnea, and Swelling"
},
{
"authors": "Peter Huynh, MD",
"content": [
"Upon physical examination, the patient is a well-nourished, well-developed teen in mild respiratory distress. Her temperature is 98.6oF (37oC), respiratory rate is 30 breaths/min, heart rate is 110 beats/min, and blood pressure is 100/60 mm Hg. Periorbital angioedema and facial erythema are noted. Extraocular eye movements are within normal limits. Her nasal cavity shows normal nasal mucosa, septum, and turbinates bilaterally.",
"Upon throat examination, no erythema or exudates are present, and the tonsils are normal, without enlargement or inflammation. No neck stridor or jugular venous distension is observed. Auscultation of the lungs reveals bilateral diffuse wheezes. Cardiovascular examination reveals sinus tachycardia, regular rhythm, and an absence of murmurs.",
"The patient's extremities are warm and well-perfused. No lower-extremity edema, cyanosis, or clubbing is noted. A skin examination reveals diffuse urticaria and generalized warmth (Figure 1).",
"Figure 1.",
"She was given epinephrine (0.3 mg intramuscularly), diphenhydramine (50 mg intravenously), and methylprednisolone (125 mg intravenously). She was given nebulized albuterol for wheezing. Her symptoms resolved within 30 minutes."
],
"date": "January 19, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/881/373/881373-Thumb1.png"
}
],
"markdown": "# A 16-Year-Old Girl With Full-Body Rash, Dyspnea, and Swelling\n\n **Authors:** Peter Huynh, MD \n **Date:** January 19, 2022\n\n ## Content\n\n Upon physical examination, the patient is a well-nourished, well-developed teen in mild respiratory distress. Her temperature is 98.6oF (37oC), respiratory rate is 30 breaths/min, heart rate is 110 beats/min, and blood pressure is 100/60 mm Hg. Periorbital angioedema and facial erythema are noted. Extraocular eye movements are within normal limits. Her nasal cavity shows normal nasal mucosa, septum, and turbinates bilaterally.\nUpon throat examination, no erythema or exudates are present, and the tonsils are normal, without enlargement or inflammation. No neck stridor or jugular venous distension is observed. Auscultation of the lungs reveals bilateral diffuse wheezes. Cardiovascular examination reveals sinus tachycardia, regular rhythm, and an absence of murmurs.\nThe patient's extremities are warm and well-perfused. No lower-extremity edema, cyanosis, or clubbing is noted. A skin examination reveals diffuse urticaria and generalized warmth (Figure 1).\nFigure 1.\nShe was given epinephrine (0.3 mg intramuscularly), diphenhydramine (50 mg intravenously), and methylprednisolone (125 mg intravenously). She was given nebulized albuterol for wheezing. Her symptoms resolved within 30 minutes.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1103900,
"choiceText": "Hereditary angioedema",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103902,
"choiceText": "Cholinergic urticaria",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103904,
"choiceText": "Exercise-induced anaphylaxis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103906,
"choiceText": "Systemic mastocytosis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103924,
"choiceText": "Idiopathic anaphylaxis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 349835,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 16-Year-Old Girl With Full-Body Rash, Dyspnea, and Swelling"
},
{
"authors": "Peter Huynh, MD",
"content": [
"Exercise-induced anaphylaxis (EIA) is a rare disorder in which anaphylaxis occurs after physical activity.[1] The symptoms may include pruritus; hives; flushing; wheezing; and gastrointestinal involvement, including nausea, abdominal cramping, and diarrhea. If physical activity continues, patients may progress to more severe symptoms, including angioedema; laryngeal edema; hypotension; and, ultimately, cardiovascular collapse. Cessation of physical activity usually results in immediate improvement of symptoms. The typical age of onset of EIA is from adolescence to the third decade of life.",
"Patients with EIA often have prodromal symptoms that alert them to impending severe symptoms if physical activity continues.[2] Prodromal symptoms may include a feeling of fatigue, generalized warmth and pruritus, and cutaneous erythema. These early symptoms are followed by typical urticarial lesions and angioedema that can progress to gastrointestinal symptoms, laryngeal edema, and/or vascular collapse.",
"Symptoms may begin at any stage of exercise. Although cessation of the physical activity usually results in immediate improvement or resolution of symptoms, some patients may experience vascular collapse even after exercise cessation. The frequency of symptoms during exercise varies among patients with EIA. Most patients can exercise regularly and only occasionally experience attacks.",
"Vigorous forms of physical activity, such as jogging, tennis, dancing, and bicycling, are more commonly associated with EIA, although lower levels of exertion (eg, walking, yard work) are also capable of triggering attacks. In a long-term follow-up study, the physical activity most often associated with exercise-induced anaphylaxis was jogging.[3] Other reports have implicated running, soccer, raking leaves, shoveling snow, and horseback riding.[4]",
"EIA attacks may not be consistently elicited by the same type and intensity of physical activity in the same patient. Such cofactors as foods, alcohol, temperature, drugs (eg, aspirin, other nonsteroidal anti-inflammatory drugs), humidity, seasonal changes, and hormonal changes are important in the precipitation of attacks.",
"A distinct subset of EIA is food-dependent EIA (FDEIA), in which anaphylaxis develops only if physical activity occurs within a few hours after eating a specific food. Neither food intake nor physical activity by itself produces anaphylaxis.[5] The foods most commonly implicated in FDEIA include wheat, shellfish, tomatoes, peanuts, and corn.[6] However, the disorder has been reported with a wide variety of foods, including fruits, seeds, milk, soybean, lettuce, peas, beans, rice, and various meats. One case report described a patient who developed symptoms of anaphylaxis only after simultaneous ingestion of two foods (wheat and umeboshi) before exercise.[7] In the nonspecific form of FDEIA, eating any food before exercise induces anaphylaxis.[8]",
"Inhalant allergens have also been implicated in EIA. In a case report, a 14-year-old boy presented with severe EIA after ingestion of Penicillium mold-contaminated food and running at school.[9] In another case report, a 16-year-old girl presented with EIA after ingestion of wheat flour contaminated with storage mites.[10]"
],
"date": "January 19, 2022",
"figures": [],
"markdown": "# A 16-Year-Old Girl With Full-Body Rash, Dyspnea, and Swelling\n\n **Authors:** Peter Huynh, MD \n **Date:** January 19, 2022\n\n ## Content\n\n Exercise-induced anaphylaxis (EIA) is a rare disorder in which anaphylaxis occurs after physical activity.[1] The symptoms may include pruritus; hives; flushing; wheezing; and gastrointestinal involvement, including nausea, abdominal cramping, and diarrhea. If physical activity continues, patients may progress to more severe symptoms, including angioedema; laryngeal edema; hypotension; and, ultimately, cardiovascular collapse. Cessation of physical activity usually results in immediate improvement of symptoms. The typical age of onset of EIA is from adolescence to the third decade of life.\nPatients with EIA often have prodromal symptoms that alert them to impending severe symptoms if physical activity continues.[2] Prodromal symptoms may include a feeling of fatigue, generalized warmth and pruritus, and cutaneous erythema. These early symptoms are followed by typical urticarial lesions and angioedema that can progress to gastrointestinal symptoms, laryngeal edema, and/or vascular collapse.\nSymptoms may begin at any stage of exercise. Although cessation of the physical activity usually results in immediate improvement or resolution of symptoms, some patients may experience vascular collapse even after exercise cessation. The frequency of symptoms during exercise varies among patients with EIA. Most patients can exercise regularly and only occasionally experience attacks.\nVigorous forms of physical activity, such as jogging, tennis, dancing, and bicycling, are more commonly associated with EIA, although lower levels of exertion (eg, walking, yard work) are also capable of triggering attacks. In a long-term follow-up study, the physical activity most often associated with exercise-induced anaphylaxis was jogging.[3] Other reports have implicated running, soccer, raking leaves, shoveling snow, and horseback riding.[4]\nEIA attacks may not be consistently elicited by the same type and intensity of physical activity in the same patient. Such cofactors as foods, alcohol, temperature, drugs (eg, aspirin, other nonsteroidal anti-inflammatory drugs), humidity, seasonal changes, and hormonal changes are important in the precipitation of attacks.\nA distinct subset of EIA is food-dependent EIA (FDEIA), in which anaphylaxis develops only if physical activity occurs within a few hours after eating a specific food. Neither food intake nor physical activity by itself produces anaphylaxis.[5] The foods most commonly implicated in FDEIA include wheat, shellfish, tomatoes, peanuts, and corn.[6] However, the disorder has been reported with a wide variety of foods, including fruits, seeds, milk, soybean, lettuce, peas, beans, rice, and various meats. One case report described a patient who developed symptoms of anaphylaxis only after simultaneous ingestion of two foods (wheat and umeboshi) before exercise.[7] In the nonspecific form of FDEIA, eating any food before exercise induces anaphylaxis.[8]\nInhalant allergens have also been implicated in EIA. In a case report, a 14-year-old boy presented with severe EIA after ingestion of Penicillium mold-contaminated food and running at school.[9] In another case report, a 16-year-old girl presented with EIA after ingestion of wheat flour contaminated with storage mites.[10]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1103900,
"choiceText": "Hereditary angioedema",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103902,
"choiceText": "Cholinergic urticaria",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103904,
"choiceText": "Exercise-induced anaphylaxis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103906,
"choiceText": "Systemic mastocytosis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103924,
"choiceText": "Idiopathic anaphylaxis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 349835,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 16-Year-Old Girl With Full-Body Rash, Dyspnea, and Swelling"
},
{
"authors": "Peter Huynh, MD",
"content": [
"The differential diagnosis for EIA includes cholinergic urticaria, idiopathic cold urticaria, mastocytosis, cardiovascular disorders, food allergy exacerbated by exercise, and angioedema.",
"Cholinergic urticaria is a form of physical urticaria that can be precipitated by exercise. The skin lesions are distinctive and appear as 2- to 4-mm pruritic wheals surrounded by extensive areas of macular erythema. Rare reports describe patients with cholinergic urticaria who develop recurrent episodes of hypotension, which may mimic EIA. Key distinguishing features include the size of the skin lesions and the underlying pathophysiologic features. Cholinergic urticaria usually produces pinpoint hives, which may coalesce to larger lesions; in contrast, EIA produces giant hives.",
"Passive heat challenges are valuable in differentiating between cholinergic urticaria and EIA.[11] In cholinergic urticaria, passive heating (eg, hot baths, saunas) with an increase in core body temperature of more than 1.26°F (0.7°C) causes histamine release, urticaria, and anaphylactic symptoms. In contrast, patients with EIA do not react with passive heating.",
"Idiopathic cold urticaria is a form of physical urticaria characterized by the development of urticaria and/or angioedema after cold exposure. Other organ systems may become involved, which may progress to frank anaphylaxis. Anaphylaxis has resulted in deaths either directly from the anaphylactic reaction or by drowning when swimming in cold water.[12] Patients with idiopathic cold urticaria who experience symptoms from exercising in cold weather may be misdiagnosed with EIA. Ascertaining whether passive cold exposure in the absence of exercise can elicit symptoms is important.",
"An ice-cube challenge test is useful in differentiating between cold-induced urticaria and EIA. This test entails the application of an ice cube for a certain period (usually 10 minutes), followed by a period of rewarming. Patients with idiopathic cold urticaria develop a wheal at the ice-cube site after the skin is rewarmed.",
"Mastocytosis is a disorder characterized by mast cell proliferation and accumulation within various organs, most commonly the skin.[13] Patients with mastocytosis are susceptible to anaphylaxis from various triggers, including exercise.",
"A useful distinguishing feature between EIA and mastocytosis is the serum tryptase level. Patients with mastocytosis have persistent elevation in serum tryptase levels, whereas patients with anaphylaxis from other causes (EIA and FDEIA) demonstrate elevation of tryptase only during acute attacks. In addition, patients with mastocytosis may have characteristic cutaneous findings of urticaria pigmentosa, characterized by oval or round red-brown macules, papules, or plaques. Gently stroking normal skin may produce raised wheals and a burning or itching sensation (Darier sign).",
"Cardiac events, such as myocardial infarction and arrhythmias, can cause sudden fatigue, dyspnea, and vascular collapse during exercise. However, cardiovascular disorders do not cause pruritus, urticaria, angioedema, and laryngeal edema.",
"Patients with food allergy may have more severe and frequent reactions with concomitant exercise. Exercise increases gastrointestinal permeability, which may allow increased entry of intact or incompletely digested allergens into the circulation. In the case of FDEIA, demonstrating that patients can tolerate the offending food in the absence of physical activity is essential. A formal food challenge may be helpful in this regard.",
"Hereditary angioedema is an inherited disease resulting from a deficiency or dysfunction of the C1 inhibitor enzyme.[14] Acquired angioedema is caused by autoimmune interference with C1 inhibitor enzyme function.[15] Both the hereditary and acquired forms are characterized by recurrent episodes of angioedema, without urticaria or pruritus, which most often affect the skin or the mucosal tissues of the upper respiratory and gastrointestinal tracts. Angioedema attacks may be precipitated by exercise, stress, and cold exposure. A key distinction between hereditary or acquired angioedema and EIA is the absence of urticaria and pruritus in hereditary and acquired angioedema."
],
"date": "January 19, 2022",
"figures": [],
"markdown": "# A 16-Year-Old Girl With Full-Body Rash, Dyspnea, and Swelling\n\n **Authors:** Peter Huynh, MD \n **Date:** January 19, 2022\n\n ## Content\n\n The differential diagnosis for EIA includes cholinergic urticaria, idiopathic cold urticaria, mastocytosis, cardiovascular disorders, food allergy exacerbated by exercise, and angioedema.\nCholinergic urticaria is a form of physical urticaria that can be precipitated by exercise. The skin lesions are distinctive and appear as 2- to 4-mm pruritic wheals surrounded by extensive areas of macular erythema. Rare reports describe patients with cholinergic urticaria who develop recurrent episodes of hypotension, which may mimic EIA. Key distinguishing features include the size of the skin lesions and the underlying pathophysiologic features. Cholinergic urticaria usually produces pinpoint hives, which may coalesce to larger lesions; in contrast, EIA produces giant hives.\nPassive heat challenges are valuable in differentiating between cholinergic urticaria and EIA.[11] In cholinergic urticaria, passive heating (eg, hot baths, saunas) with an increase in core body temperature of more than 1.26°F (0.7°C) causes histamine release, urticaria, and anaphylactic symptoms. In contrast, patients with EIA do not react with passive heating.\nIdiopathic cold urticaria is a form of physical urticaria characterized by the development of urticaria and/or angioedema after cold exposure. Other organ systems may become involved, which may progress to frank anaphylaxis. Anaphylaxis has resulted in deaths either directly from the anaphylactic reaction or by drowning when swimming in cold water.[12] Patients with idiopathic cold urticaria who experience symptoms from exercising in cold weather may be misdiagnosed with EIA. Ascertaining whether passive cold exposure in the absence of exercise can elicit symptoms is important.\nAn ice-cube challenge test is useful in differentiating between cold-induced urticaria and EIA. This test entails the application of an ice cube for a certain period (usually 10 minutes), followed by a period of rewarming. Patients with idiopathic cold urticaria develop a wheal at the ice-cube site after the skin is rewarmed.\nMastocytosis is a disorder characterized by mast cell proliferation and accumulation within various organs, most commonly the skin.[13] Patients with mastocytosis are susceptible to anaphylaxis from various triggers, including exercise.\nA useful distinguishing feature between EIA and mastocytosis is the serum tryptase level. Patients with mastocytosis have persistent elevation in serum tryptase levels, whereas patients with anaphylaxis from other causes (EIA and FDEIA) demonstrate elevation of tryptase only during acute attacks. In addition, patients with mastocytosis may have characteristic cutaneous findings of urticaria pigmentosa, characterized by oval or round red-brown macules, papules, or plaques. Gently stroking normal skin may produce raised wheals and a burning or itching sensation (Darier sign).\nCardiac events, such as myocardial infarction and arrhythmias, can cause sudden fatigue, dyspnea, and vascular collapse during exercise. However, cardiovascular disorders do not cause pruritus, urticaria, angioedema, and laryngeal edema.\nPatients with food allergy may have more severe and frequent reactions with concomitant exercise. Exercise increases gastrointestinal permeability, which may allow increased entry of intact or incompletely digested allergens into the circulation. In the case of FDEIA, demonstrating that patients can tolerate the offending food in the absence of physical activity is essential. A formal food challenge may be helpful in this regard.\nHereditary angioedema is an inherited disease resulting from a deficiency or dysfunction of the C1 inhibitor enzyme.[14] Acquired angioedema is caused by autoimmune interference with C1 inhibitor enzyme function.[15] Both the hereditary and acquired forms are characterized by recurrent episodes of angioedema, without urticaria or pruritus, which most often affect the skin or the mucosal tissues of the upper respiratory and gastrointestinal tracts. Angioedema attacks may be precipitated by exercise, stress, and cold exposure. A key distinction between hereditary or acquired angioedema and EIA is the absence of urticaria and pruritus in hereditary and acquired angioedema.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A 16-Year-Old Girl With Full-Body Rash, Dyspnea, and Swelling"
},
{
"authors": "Peter Huynh, MD",
"content": [
"Intramuscular epinephrine is the drug of choice for acute attacks of EIA or FDEIA. Early administration of intramuscular epinephrine is associated with decreased mortality in patients with anaphylaxis.[16]",
"Other medications play an ancillary role in the treatment of anaphylaxis. H1-antihistamines relieve itch and hives, but they do not relieve airway obstruction or shock. Beta-2–adrenergic agonists relieve bronchospasm, but they do not relieve upper-airway obstruction or shock. Glucocorticoids might prevent protracted or biphasic symptoms, but they do not provide rapid relief of upper or lower-airway obstruction, shock, or other symptoms of anaphylaxis.",
"Long-term management of EIA and FDEIA must be individualized to each patient because the severity, frequency, and intensity of exercise needed to trigger anaphylaxis and the possible association with other cotriggers all vary. Other medications, such as oral steroids, leukotriene-modifying agents, and omalizumab, are either unstudied or reported only in isolated cases.",
"Patients must understand the emergent nature of EIA and the proper use of emergency injectable epinephrine. Instruct patients with EIA to recognize the early warning signs and symptoms and stop physical activity to prevent progression of the syndrome. This includes limiting exercise and being cautious in temperature extremes.",
"Patients with FDEIA or medicine-dependent EIA need to be aware of the offending food or medication (if specific ones can be identified) and know how long to refrain from exercise after eating. Educate patients with EIA about the need to exercise with a partner who is aware of EIA and the emergent nature of an episode.",
"The prognosis of patients with EIA is generally favorable. Most patients experience fewer and less severe attacks over time. Although rare, several fatalities have been attributed to EIA or FDEIA.[17,18,19] No cure for these disorders is known. With appropriate lifestyle changes, however, patients may be able to reduce or eliminate episodes of anaphylaxis, and prompt intervention can abort episodes that do occur.",
"The patient in this case was counseled and given appropriate instructions on necessary preparations and interventions, as described above."
],
"date": "January 19, 2022",
"figures": [],
"markdown": "# A 16-Year-Old Girl With Full-Body Rash, Dyspnea, and Swelling\n\n **Authors:** Peter Huynh, MD \n **Date:** January 19, 2022\n\n ## Content\n\n Intramuscular epinephrine is the drug of choice for acute attacks of EIA or FDEIA. Early administration of intramuscular epinephrine is associated with decreased mortality in patients with anaphylaxis.[16]\nOther medications play an ancillary role in the treatment of anaphylaxis. H1-antihistamines relieve itch and hives, but they do not relieve airway obstruction or shock. Beta-2–adrenergic agonists relieve bronchospasm, but they do not relieve upper-airway obstruction or shock. Glucocorticoids might prevent protracted or biphasic symptoms, but they do not provide rapid relief of upper or lower-airway obstruction, shock, or other symptoms of anaphylaxis.\nLong-term management of EIA and FDEIA must be individualized to each patient because the severity, frequency, and intensity of exercise needed to trigger anaphylaxis and the possible association with other cotriggers all vary. Other medications, such as oral steroids, leukotriene-modifying agents, and omalizumab, are either unstudied or reported only in isolated cases.\nPatients must understand the emergent nature of EIA and the proper use of emergency injectable epinephrine. Instruct patients with EIA to recognize the early warning signs and symptoms and stop physical activity to prevent progression of the syndrome. This includes limiting exercise and being cautious in temperature extremes.\nPatients with FDEIA or medicine-dependent EIA need to be aware of the offending food or medication (if specific ones can be identified) and know how long to refrain from exercise after eating. Educate patients with EIA about the need to exercise with a partner who is aware of EIA and the emergent nature of an episode.\nThe prognosis of patients with EIA is generally favorable. Most patients experience fewer and less severe attacks over time. Although rare, several fatalities have been attributed to EIA or FDEIA.[17,18,19] No cure for these disorders is known. With appropriate lifestyle changes, however, patients may be able to reduce or eliminate episodes of anaphylaxis, and prompt intervention can abort episodes that do occur.\nThe patient in this case was counseled and given appropriate instructions on necessary preparations and interventions, as described above.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1103908,
"choiceText": "Albuterol",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103910,
"choiceText": "Antihistamines",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103912,
"choiceText": "Glucocorticosteroids",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103914,
"choiceText": "Epinephrine",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Intramuscular epinephrine is the drug of choice for acute attacks of EIA or FDEIA. Early administration of intramuscular epinephrine is associated with decreased mortality in patients with anaphylaxis.<br/><br/>\r\nOther medications play an ancillary role in the treatment of anaphylaxis. H1-antihistamines relieve itch and hives, but they do not relieve airway obstruction or shock. Beta-2–adrenergic agonists relieve bronchospasm, but they do not relieve upper-airway obstruction or shock. Glucocorticoids might prevent protracted or biphasic symptoms, but they do not provide rapid relief of upper or lower-airway obstruction, shock, or other symptoms of anaphylaxis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 349837,
"questionText": "Which is the drug of choice for the treatment of EIA?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1103916,
"choiceText": "Egg",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103918,
"choiceText": "Milk",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103920,
"choiceText": "Soy",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103922,
"choiceText": "Wheat",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The foods most commonly implicated in FDEIA include wheat, shellfish, tomatoes, peanuts, and corn. ",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 349839,
"questionText": "Which food is more commonly associated with FDEIA?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 16-Year-Old Girl With Full-Body Rash, Dyspnea, and Swelling"
},
{
"authors": "Peter Huynh, MD",
"content": [],
"date": "January 19, 2022",
"figures": [],
"markdown": "# A 16-Year-Old Girl With Full-Body Rash, Dyspnea, and Swelling\n\n **Authors:** Peter Huynh, MD \n **Date:** January 19, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1103908,
"choiceText": "Albuterol",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103910,
"choiceText": "Antihistamines",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103912,
"choiceText": "Glucocorticosteroids",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103914,
"choiceText": "Epinephrine",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Intramuscular epinephrine is the drug of choice for acute attacks of EIA or FDEIA. Early administration of intramuscular epinephrine is associated with decreased mortality in patients with anaphylaxis.<br/><br/>\r\nOther medications play an ancillary role in the treatment of anaphylaxis. H1-antihistamines relieve itch and hives, but they do not relieve airway obstruction or shock. Beta-2–adrenergic agonists relieve bronchospasm, but they do not relieve upper-airway obstruction or shock. Glucocorticoids might prevent protracted or biphasic symptoms, but they do not provide rapid relief of upper or lower-airway obstruction, shock, or other symptoms of anaphylaxis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 349837,
"questionText": "Which is the drug of choice for the treatment of EIA?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1103916,
"choiceText": "Egg",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103918,
"choiceText": "Milk",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103920,
"choiceText": "Soy",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103922,
"choiceText": "Wheat",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The foods most commonly implicated in FDEIA include wheat, shellfish, tomatoes, peanuts, and corn. ",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 349839,
"questionText": "Which food is more commonly associated with FDEIA?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 16-Year-Old Girl With Full-Body Rash, Dyspnea, and Swelling"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1103900,
"choiceText": "Hereditary angioedema",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103902,
"choiceText": "Cholinergic urticaria",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103904,
"choiceText": "Exercise-induced anaphylaxis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103906,
"choiceText": "Systemic mastocytosis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103924,
"choiceText": "Idiopathic anaphylaxis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 349835,
"questionText": "On the basis of these findings only, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1103908,
"choiceText": "Albuterol",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103910,
"choiceText": "Antihistamines",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103912,
"choiceText": "Glucocorticosteroids",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103914,
"choiceText": "Epinephrine",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Intramuscular epinephrine is the drug of choice for acute attacks of EIA or FDEIA. Early administration of intramuscular epinephrine is associated with decreased mortality in patients with anaphylaxis.<br/><br/>\r\nOther medications play an ancillary role in the treatment of anaphylaxis. H1-antihistamines relieve itch and hives, but they do not relieve airway obstruction or shock. Beta-2–adrenergic agonists relieve bronchospasm, but they do not relieve upper-airway obstruction or shock. Glucocorticoids might prevent protracted or biphasic symptoms, but they do not provide rapid relief of upper or lower-airway obstruction, shock, or other symptoms of anaphylaxis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 349837,
"questionText": "Which is the drug of choice for the treatment of EIA?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1103916,
"choiceText": "Egg",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103918,
"choiceText": "Milk",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103920,
"choiceText": "Soy",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1103922,
"choiceText": "Wheat",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The foods most commonly implicated in FDEIA include wheat, shellfish, tomatoes, peanuts, and corn. ",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 349839,
"questionText": "Which food is more commonly associated with FDEIA?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
915146 | /viewarticle/915146 | [
{
"authors": "Amanda L. Blackmon, DO, MS; Lauren Pinter-Brown, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 77-year-old retired teacher presents to the emergency department with dizziness, imbalance, nausea/vomiting, and a constant headache for the past 2 weeks. He describes his headache as diffuse and throbbing. His history is significant for hepatitis C; hypothyroidism; Helicobacter pylori infection; and mantle cell lymphoma, which was diagnosed 2 years ago and is currently in remission. The patient is taking rituximab for maintenance therapy. He takes lorazepam nightly for sleep.",
"The patient reports having traveled to Brazil 3 weeks ago. His family describes the patient as having been more confused than usual. He has been around his grandchildren, who attend a daycare center. He has a 40–pack-year smoking history and quit smoking 30 years ago. He reports occasional alcohol use and denies illicit drug use. He currently lives with his significant other. He is HIV negative. His vaccination status is unknown."
],
"date": "January 05, 2022",
"figures": [],
"markdown": "# A Retired Teacher With a Constant Headache and Vomiting\n\n **Authors:** Amanda L. Blackmon, DO, MS; Lauren Pinter-Brown, MD \n **Date:** January 05, 2022\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 77-year-old retired teacher presents to the emergency department with dizziness, imbalance, nausea/vomiting, and a constant headache for the past 2 weeks. He describes his headache as diffuse and throbbing. His history is significant for hepatitis C; hypothyroidism; Helicobacter pylori infection; and mantle cell lymphoma, which was diagnosed 2 years ago and is currently in remission. The patient is taking rituximab for maintenance therapy. He takes lorazepam nightly for sleep.\nThe patient reports having traveled to Brazil 3 weeks ago. His family describes the patient as having been more confused than usual. He has been around his grandchildren, who attend a daycare center. He has a 40–pack-year smoking history and quit smoking 30 years ago. He reports occasional alcohol use and denies illicit drug use. He currently lives with his significant other. He is HIV negative. His vaccination status is unknown.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A Retired Teacher With a Constant Headache and Vomiting"
},
{
"authors": "Amanda L. Blackmon, DO, MS; Lauren Pinter-Brown, MD",
"content": [
"Upon physical examination, the patient is afebrile and hemodynamically stable. He is a well-appearing elderly man in mild distress. He is normocephalic and atraumatic. His mucous membranes are moist, and no tonsillar enlargement is noted. His pupils are equal and round and reactive to light and accommodation. His extraocular movements are intact. Neurologic examination reveals no focal deficit. His motor strength is 5/5 in bilateral upper and lower extremities. He has no lymphadenopathy or hepatosplenomegaly.",
"Laboratory studies are unrevealing and include the following:",
"White blood cell count: 6,100 cells/µL (75% neutrophils); reference range, 4,000-11,000 cells/µL (55% to 70% neutrophils)",
"Hemoglobin B level: 13.4 g/dL (reference range, 13.5-17.5 g/dL)",
"Platelet count: 163,000 cells/µL (reference range, 150,000-450,000 cells/µL)",
"Sodium level: 136 mmol/L (reference range, 135-145 mmol/L)",
"Potassium level: 3.7 mmol/L (reference range, 3.6-5.2 mmol/L)",
"Chloride level: 107 mmol/L (reference range, 96-106 mmol/L)",
"Bicarbonate level: 26 mmol/L (reference range, 23-30 mmol/L)",
"Blood urea nitrogen level: 23 mg/dL (reference range, 6-24 mg/dL)",
"Creatinine level: 0.9 mg/dL (reference range, 0.6-1.2 mg/dL)",
"Glucose level: 85 mg/dL (reference range, <140 mg/dL)",
"Alkaline phosphatase level: 57 IU/L (reference range, 44-147 IU/L)",
"Alanine aminotransferase level: 11 U/L (reference range, 4-36 IU/L)",
"Aspartate aminotransferase level: 12 U/L (reference range, 8-33 U/L)",
"Total bilirubin level: 0.8 mg/dL (reference range, 0.1-1.2 mg/dL)",
"Albumin level: 4.2 g/dL (reference range, 3.5-5.5 g/dL)",
"Total protein level: 6.7 g/dL (reference range, 6-8.3 g/dL)",
"Thyroid-stimulating hormone level: 1.18 mU/L (reference range, 0.45-4.5 mU/L)",
"International normalized ratio: 0.97 (reference range, <1.1)",
"Partial thromboplastin time: 24.3 s (reference range, 60-70 s)",
"Lactate dehydrogenase (LDH) level: 235 U/L (reference range, 140-280 U/L)",
"MRI of the brain reveals mild to moderate hydrocephalus (Figure 1).",
"Figure 1.",
"A high-volume lumbar puncture is performed. Opening pressure was 27 cm H2O. Cerebrospinal fluid (CSF) analysis reveals 338 nucleated cells, 38% lymphocytes, 51% others, 11 red blood cells, a protein level of 1530 mg/dL, and a glucose level of 20 mg/dL. The patient's headache improved after the high-volume lumbar puncture."
],
"date": "January 05, 2022",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/915/146/915146-Thumb1.png"
}
],
"markdown": "# A Retired Teacher With a Constant Headache and Vomiting\n\n **Authors:** Amanda L. Blackmon, DO, MS; Lauren Pinter-Brown, MD \n **Date:** January 05, 2022\n\n ## Content\n\n Upon physical examination, the patient is afebrile and hemodynamically stable. He is a well-appearing elderly man in mild distress. He is normocephalic and atraumatic. His mucous membranes are moist, and no tonsillar enlargement is noted. His pupils are equal and round and reactive to light and accommodation. His extraocular movements are intact. Neurologic examination reveals no focal deficit. His motor strength is 5/5 in bilateral upper and lower extremities. He has no lymphadenopathy or hepatosplenomegaly.\nLaboratory studies are unrevealing and include the following:\nWhite blood cell count: 6,100 cells/µL (75% neutrophils); reference range, 4,000-11,000 cells/µL (55% to 70% neutrophils)\nHemoglobin B level: 13.4 g/dL (reference range, 13.5-17.5 g/dL)\nPlatelet count: 163,000 cells/µL (reference range, 150,000-450,000 cells/µL)\nSodium level: 136 mmol/L (reference range, 135-145 mmol/L)\nPotassium level: 3.7 mmol/L (reference range, 3.6-5.2 mmol/L)\nChloride level: 107 mmol/L (reference range, 96-106 mmol/L)\nBicarbonate level: 26 mmol/L (reference range, 23-30 mmol/L)\nBlood urea nitrogen level: 23 mg/dL (reference range, 6-24 mg/dL)\nCreatinine level: 0.9 mg/dL (reference range, 0.6-1.2 mg/dL)\nGlucose level: 85 mg/dL (reference range, <140 mg/dL)\nAlkaline phosphatase level: 57 IU/L (reference range, 44-147 IU/L)\nAlanine aminotransferase level: 11 U/L (reference range, 4-36 IU/L)\nAspartate aminotransferase level: 12 U/L (reference range, 8-33 U/L)\nTotal bilirubin level: 0.8 mg/dL (reference range, 0.1-1.2 mg/dL)\nAlbumin level: 4.2 g/dL (reference range, 3.5-5.5 g/dL)\nTotal protein level: 6.7 g/dL (reference range, 6-8.3 g/dL)\nThyroid-stimulating hormone level: 1.18 mU/L (reference range, 0.45-4.5 mU/L)\nInternational normalized ratio: 0.97 (reference range, <1.1)\nPartial thromboplastin time: 24.3 s (reference range, 60-70 s)\nLactate dehydrogenase (LDH) level: 235 U/L (reference range, 140-280 U/L)\nMRI of the brain reveals mild to moderate hydrocephalus (Figure 1).\nFigure 1.\nA high-volume lumbar puncture is performed. Opening pressure was 27 cm H2O. Cerebrospinal fluid (CSF) analysis reveals 338 nucleated cells, 38% lymphocytes, 51% others, 11 red blood cells, a protein level of 1530 mg/dL, and a glucose level of 20 mg/dL. The patient's headache improved after the high-volume lumbar puncture.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1381206,
"choiceText": "Normal-pressure hydrocephalus",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381208,
"choiceText": "Cryptococcal meningitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381210,
"choiceText": "Mumps ",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381212,
"choiceText": "Leptomeningeal disease ",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381214,
"choiceText": "Lymphocytic choriomeningitis\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 441055,
"questionText": "Based on only these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Retired Teacher With a Constant Headache and Vomiting"
},
{
"authors": "Amanda L. Blackmon, DO, MS; Lauren Pinter-Brown, MD",
"content": [
"CSF flow cytometry revealed 48% kappa-restricted CD5-positive B-cell population, consistent with involvement of mantle cell lymphoma. These cells express CD20, CD19, CD5, and CD38. Bone marrow biopsy performed showed low-normocellular marrow with active trilineage hematopoiesis and no morphologic or immunophenotypic (flow cytometry) evidence of a B-cell lymphoma. CT of the chest, abdomen, and pelvis with contrast were negative for any suspicious lymphadenopathy. The CSF was the only site of recurrence.",
"Mantle cell lymphoma was diagnosed in this patient 2 years before this presentation. At the time, he had surveillance abdominal ultrasonography owing to his history of hepatitis C. A complete blood cell count at the time revealed leukocytosis/lymphocytosis. Flow cytometry on peripheral blood revealed a 32% abnormal B-cell population, which express CD20, CD19, and CD5. It also revealed surface kappa light-chain restriction. The cells did not express CD10, CD23, and CD38.",
"At the time of diagnosis, bone marrow biopsy revealed 50% involvement of mantle cell lymphoma. Immunohistochemistry was positive for CD19, CD20, CD5, and cyclin Dl; Ki-67 was not increased. PET at diagnosis revealed splenomegaly with a standard uptake value of 4.6 and mildly fluoro-D-glucose (FDG)–avid, nonenlarged lymph nodes diffusely in his cervical, thoracic, and abdominal/pelvic regions.",
"He was initially observed for approximately 6 months off treatment and was then treated with rituximab-lenalidomide for 2 months; however, he could not tolerate this treatment owing to a grade 3 rash. He completed six cycles of rituximab-bendamustine, with cytarabine (500 mg) added to cycles 5 and 6 owing to a plateau in response (size of spleen). His end-of-treatment scan showed a complete response. He was started on rituximab maintenance every 2 months, which he maintained for 1.5 years before his presentation with hydrocephalus.",
"Mantle cell lymphoma is a rare form of non-Hodgkin lymphoma (NHL). It is a mature B-cell neoplasm of small to medium-sized cells with a variable disease course. It is associated with poor long-term survival compared with other mature B-cell cancers. Mantle cell lymphoma represents about 7% of NHLs, with a median age at diagnosis of 60 years, male predominance, and median survival of 3-5 years.[1] Mantle cell lymphoma usually responds to initial treatment with chemoimmunotherapy; however, most patients have relapse and have poor outcomes.[2] A small number of patients have indolent disease; however, this population remains difficult to predict.",
"Mantle cell lymphoma is classically defined by the acquired translocation(11;14)(q13;q32) of pre-B cells in the bone marrow, which results in the constitutive expression of cyclin D1; this leads to cell cycle dysregulation.[3] This translocation transposes the CCDN1 gene under control of immunoglobulin heavy chain locus (14q32), which leads to the constitutive expression of cyclin D. This translocation alone is not responsible for the development of mantle cell lymphoma; however, it leads to genetic instability and subsequent genetic aberrations, which are implicated in the aggressive disease course.",
"Two different forms of mantle cell lymphoma are recognized. Classical mantle cell lymphoma is generated from B cells that express SOX11 and is characterized by minimal IgVH somatic hypermutation and genetic instability. SOX11 is a transcription factor usually absent in B cells that affects cell cycle regulatory genes, DNA repair mechanisms, and cell survival mechanisms, leading to arrest of B-cell differentiation and proliferation of abnormal cells.[3] Classical mantle cell lymphoma tends to be more aggressive, and patients are more symptomatic at diagnosis. Lymph node involvement is noted, and extranodal involvement is typically present, often in the gastrointestinal tract.",
"The second form of mantle cell lymphoma is known as the leukemic non-nodal variant and accounts for 10%-20% of cases.[4] It is generated from post-germinal center, SOX11-negative B cells that are IgVH hypermutated and is more genetically stable. The leukemic variant of mantle cell lymphoma typically involves the peripheral blood and spleen, sparing the lymph nodes. This form is often clinically indolent but can involve further mutations (TP53) that can lead to a more aggressive disease course.[3] As more mutations are acquired, this may lead to the blastoid and pleomorphic variants. The blastoid variant is classified by medium-sized lymphocytes, with indistinct cytoplasm and dispersed chromatin. Classical mantle cell lymphoma generally has morphologically smaller lymphocytes and condensed chromatin.[5]",
"On the basis of our patient's initial presentation with splenomegaly and lymphocytosis with nonenlarged, mildly FDG-avid lymphadenopathy, he may have the leukemic variant that is theoretically associated with indolent disease. A pathology review of the SOX11 and p53 IHC status in the bone marrow was requested."
],
"date": "January 05, 2022",
"figures": [],
"markdown": "# A Retired Teacher With a Constant Headache and Vomiting\n\n **Authors:** Amanda L. Blackmon, DO, MS; Lauren Pinter-Brown, MD \n **Date:** January 05, 2022\n\n ## Content\n\n CSF flow cytometry revealed 48% kappa-restricted CD5-positive B-cell population, consistent with involvement of mantle cell lymphoma. These cells express CD20, CD19, CD5, and CD38. Bone marrow biopsy performed showed low-normocellular marrow with active trilineage hematopoiesis and no morphologic or immunophenotypic (flow cytometry) evidence of a B-cell lymphoma. CT of the chest, abdomen, and pelvis with contrast were negative for any suspicious lymphadenopathy. The CSF was the only site of recurrence.\nMantle cell lymphoma was diagnosed in this patient 2 years before this presentation. At the time, he had surveillance abdominal ultrasonography owing to his history of hepatitis C. A complete blood cell count at the time revealed leukocytosis/lymphocytosis. Flow cytometry on peripheral blood revealed a 32% abnormal B-cell population, which express CD20, CD19, and CD5. It also revealed surface kappa light-chain restriction. The cells did not express CD10, CD23, and CD38.\nAt the time of diagnosis, bone marrow biopsy revealed 50% involvement of mantle cell lymphoma. Immunohistochemistry was positive for CD19, CD20, CD5, and cyclin Dl; Ki-67 was not increased. PET at diagnosis revealed splenomegaly with a standard uptake value of 4.6 and mildly fluoro-D-glucose (FDG)–avid, nonenlarged lymph nodes diffusely in his cervical, thoracic, and abdominal/pelvic regions.\nHe was initially observed for approximately 6 months off treatment and was then treated with rituximab-lenalidomide for 2 months; however, he could not tolerate this treatment owing to a grade 3 rash. He completed six cycles of rituximab-bendamustine, with cytarabine (500 mg) added to cycles 5 and 6 owing to a plateau in response (size of spleen). His end-of-treatment scan showed a complete response. He was started on rituximab maintenance every 2 months, which he maintained for 1.5 years before his presentation with hydrocephalus.\nMantle cell lymphoma is a rare form of non-Hodgkin lymphoma (NHL). It is a mature B-cell neoplasm of small to medium-sized cells with a variable disease course. It is associated with poor long-term survival compared with other mature B-cell cancers. Mantle cell lymphoma represents about 7% of NHLs, with a median age at diagnosis of 60 years, male predominance, and median survival of 3-5 years.[1] Mantle cell lymphoma usually responds to initial treatment with chemoimmunotherapy; however, most patients have relapse and have poor outcomes.[2] A small number of patients have indolent disease; however, this population remains difficult to predict.\nMantle cell lymphoma is classically defined by the acquired translocation(11;14)(q13;q32) of pre-B cells in the bone marrow, which results in the constitutive expression of cyclin D1; this leads to cell cycle dysregulation.[3] This translocation transposes the CCDN1 gene under control of immunoglobulin heavy chain locus (14q32), which leads to the constitutive expression of cyclin D. This translocation alone is not responsible for the development of mantle cell lymphoma; however, it leads to genetic instability and subsequent genetic aberrations, which are implicated in the aggressive disease course.\nTwo different forms of mantle cell lymphoma are recognized. Classical mantle cell lymphoma is generated from B cells that express SOX11 and is characterized by minimal IgVH somatic hypermutation and genetic instability. SOX11 is a transcription factor usually absent in B cells that affects cell cycle regulatory genes, DNA repair mechanisms, and cell survival mechanisms, leading to arrest of B-cell differentiation and proliferation of abnormal cells.[3] Classical mantle cell lymphoma tends to be more aggressive, and patients are more symptomatic at diagnosis. Lymph node involvement is noted, and extranodal involvement is typically present, often in the gastrointestinal tract.\nThe second form of mantle cell lymphoma is known as the leukemic non-nodal variant and accounts for 10%-20% of cases.[4] It is generated from post-germinal center, SOX11-negative B cells that are IgVH hypermutated and is more genetically stable. The leukemic variant of mantle cell lymphoma typically involves the peripheral blood and spleen, sparing the lymph nodes. This form is often clinically indolent but can involve further mutations (TP53) that can lead to a more aggressive disease course.[3] As more mutations are acquired, this may lead to the blastoid and pleomorphic variants. The blastoid variant is classified by medium-sized lymphocytes, with indistinct cytoplasm and dispersed chromatin. Classical mantle cell lymphoma generally has morphologically smaller lymphocytes and condensed chromatin.[5]\nOn the basis of our patient's initial presentation with splenomegaly and lymphocytosis with nonenlarged, mildly FDG-avid lymphadenopathy, he may have the leukemic variant that is theoretically associated with indolent disease. A pathology review of the SOX11 and p53 IHC status in the bone marrow was requested.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1381206,
"choiceText": "Normal-pressure hydrocephalus",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381208,
"choiceText": "Cryptococcal meningitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381210,
"choiceText": "Mumps ",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381212,
"choiceText": "Leptomeningeal disease ",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381214,
"choiceText": "Lymphocytic choriomeningitis\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 441055,
"questionText": "Based on only these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Retired Teacher With a Constant Headache and Vomiting"
},
{
"authors": "Amanda L. Blackmon, DO, MS; Lauren Pinter-Brown, MD",
"content": [
"Clinically, mantle cell lymphoma has a wide range of presenting symptoms. Patients may be asymptomatic, with monoclonal MCL-type lymphocytosis. Some patients have extranodal disease and present with gastrointestinal symptoms. Other patients have B symptoms; cytopenias; splenomegaly; and, rarely, neurologic symptoms with central nervous system (CNS) involvement. Most classical, nodal forms of mantle cell lymphoma are more advanced and symptomatic at the time of diagnosis and require up-front treatment with systemic therapy. Mantle cell lymphoma can also transform from one variant to another, usually classical to blastoid.",
"The current method used for prognostication includes the Mantle Cell Lymphoma International Prognostic Index (MIPI) risk score, which takes into account performance status, age, LDH level, and white blood cell count, with or without Ki67; on the basis of the number of positive risk factors, a risk category is assigned. Our patient has a simplified MIPI score of 4, making him intermediate-risk, with 58 months as a likely median survival and 35% 5-year overall survival (OS). Ki-67 is reported as a percentage, which is a marker of cell division, with higher numbers associated with more aggressive disease; > 30% is often used as a cutoff for more aggressive disease, although the percentage remains subjective on the numbers of cells that stain positive.[6] This patient's Ki-67 percentage was not increased on his initial bone marrow biopsy at the time of diagnosis.",
"Other factors that have been associated with worse clinical outcomes include complex karyotype, TP53 mutations or overexpression, MYC translocation or overexpression, and unmutated IgVH status. Additional prognostic factors that have been proposed include minimal residual disease testing, circulating tumor DNA, and specific mutations (eg, CDKN2A, ATM, MYC, NOTCH1, NOTCH2, BIRC3, BTK), as well as sequencing panels used to determine a prognostic score.[4,7] Some of these factors may also be correlated to response to certain systemic treatments.[4] Clot and colleagues[7] describe a molecular assay along with genomic complexity that may accurately predict the subtype of mantle cell lymphoma and aid in prognosis.",
"At the time of diagnosis, patients usually have advanced disease and are symptomatic, with widespread lymphadenopathy. The mainstay of treatment has been induction with chemoimmunotherapy with or without radiation. Regimens include the following:",
"Bendamustine plus rituximab (BR)",
"Rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP)/rituximab plus cyclophosphamide, vincristine, and prednisone (R-CVP)",
"Rituximab plus fractionated cyclophosphamide, vincristine, doxorubicin and dexamethasone (R-hyperCVAD)",
"Rituximab plus dexamethasone, cytarabine, and cisplatin (R-DHAP)",
"NORDIC protocol (especially in younger, healthier patients who can endure the side effects of myelosuppression, associated infections, development of myelodysplastic syndrome, and other toxicities)",
"The BRIGHT study compared BR with R-CHOP and found similar efficacy and less toxicity in the BR group; however, a higher rate of secondary cancers was observed in the BR group.[8] Autologous and allogenic hematopoietic stem cell transplant (HSCT) are often considered, with the hope of a more durable remission. In patients who are not eligible for transplant, rituximab maintenance every 8 weeks for 3 years is used, on the basis of a European trial with longer progression-free survival and OS compared with interferon.[9,10]",
"These induction treatments are often difficult for elderly patients. Martin and colleagues[11] reviewed nonchemotherapy strategies in mantle cell lymphoma. Several studies of these agents in a first-line setting are under way, and predictive markers are being evaluated to determine which patients may benefit more from these treatments. Avoiding chemotherapy is not recommended at this time, although better treatment regimens are clearly needed.",
"Other than the induction chemotherapy regiments mentioned above, other agents are often used as second-line treatments. These include bortezomib-rituximab, lenalidomide-rituximab, and temsirolimus. The BTK inhibitors ibrutinib and acalabrutinib and the BCL-2 inhibitor venetoclax have also been used. CD19 CAR-T clinical trials are under way for patients with disease that is refractory to other treatment; however, patients with CNS involvement are generally excluded owing to the neurotoxicity associated with treatment.",
"A subset of patients may be able to pursue a watchful waiting strategy; these are usually patients with good performance status who are asymptomatic, do not have B symptoms, have normal LDH levels, have non-nodal disease, and have low Ki-67 percentages. This observation strategy was studied by a Canadian group that evaluated 440 patients, 75 of whom were observed for 3 or more months.[12] The median time to treatment was 35 months, and the OS in this group was longer than that in the early treatment group."
],
"date": "January 05, 2022",
"figures": [],
"markdown": "# A Retired Teacher With a Constant Headache and Vomiting\n\n **Authors:** Amanda L. Blackmon, DO, MS; Lauren Pinter-Brown, MD \n **Date:** January 05, 2022\n\n ## Content\n\n Clinically, mantle cell lymphoma has a wide range of presenting symptoms. Patients may be asymptomatic, with monoclonal MCL-type lymphocytosis. Some patients have extranodal disease and present with gastrointestinal symptoms. Other patients have B symptoms; cytopenias; splenomegaly; and, rarely, neurologic symptoms with central nervous system (CNS) involvement. Most classical, nodal forms of mantle cell lymphoma are more advanced and symptomatic at the time of diagnosis and require up-front treatment with systemic therapy. Mantle cell lymphoma can also transform from one variant to another, usually classical to blastoid.\nThe current method used for prognostication includes the Mantle Cell Lymphoma International Prognostic Index (MIPI) risk score, which takes into account performance status, age, LDH level, and white blood cell count, with or without Ki67; on the basis of the number of positive risk factors, a risk category is assigned. Our patient has a simplified MIPI score of 4, making him intermediate-risk, with 58 months as a likely median survival and 35% 5-year overall survival (OS). Ki-67 is reported as a percentage, which is a marker of cell division, with higher numbers associated with more aggressive disease; > 30% is often used as a cutoff for more aggressive disease, although the percentage remains subjective on the numbers of cells that stain positive.[6] This patient's Ki-67 percentage was not increased on his initial bone marrow biopsy at the time of diagnosis.\nOther factors that have been associated with worse clinical outcomes include complex karyotype, TP53 mutations or overexpression, MYC translocation or overexpression, and unmutated IgVH status. Additional prognostic factors that have been proposed include minimal residual disease testing, circulating tumor DNA, and specific mutations (eg, CDKN2A, ATM, MYC, NOTCH1, NOTCH2, BIRC3, BTK), as well as sequencing panels used to determine a prognostic score.[4,7] Some of these factors may also be correlated to response to certain systemic treatments.[4] Clot and colleagues[7] describe a molecular assay along with genomic complexity that may accurately predict the subtype of mantle cell lymphoma and aid in prognosis.\nAt the time of diagnosis, patients usually have advanced disease and are symptomatic, with widespread lymphadenopathy. The mainstay of treatment has been induction with chemoimmunotherapy with or without radiation. Regimens include the following:\nBendamustine plus rituximab (BR)\nRituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP)/rituximab plus cyclophosphamide, vincristine, and prednisone (R-CVP)\nRituximab plus fractionated cyclophosphamide, vincristine, doxorubicin and dexamethasone (R-hyperCVAD)\nRituximab plus dexamethasone, cytarabine, and cisplatin (R-DHAP)\nNORDIC protocol (especially in younger, healthier patients who can endure the side effects of myelosuppression, associated infections, development of myelodysplastic syndrome, and other toxicities)\nThe BRIGHT study compared BR with R-CHOP and found similar efficacy and less toxicity in the BR group; however, a higher rate of secondary cancers was observed in the BR group.[8] Autologous and allogenic hematopoietic stem cell transplant (HSCT) are often considered, with the hope of a more durable remission. In patients who are not eligible for transplant, rituximab maintenance every 8 weeks for 3 years is used, on the basis of a European trial with longer progression-free survival and OS compared with interferon.[9,10]\nThese induction treatments are often difficult for elderly patients. Martin and colleagues[11] reviewed nonchemotherapy strategies in mantle cell lymphoma. Several studies of these agents in a first-line setting are under way, and predictive markers are being evaluated to determine which patients may benefit more from these treatments. Avoiding chemotherapy is not recommended at this time, although better treatment regimens are clearly needed.\nOther than the induction chemotherapy regiments mentioned above, other agents are often used as second-line treatments. These include bortezomib-rituximab, lenalidomide-rituximab, and temsirolimus. The BTK inhibitors ibrutinib and acalabrutinib and the BCL-2 inhibitor venetoclax have also been used. CD19 CAR-T clinical trials are under way for patients with disease that is refractory to other treatment; however, patients with CNS involvement are generally excluded owing to the neurotoxicity associated with treatment.\nA subset of patients may be able to pursue a watchful waiting strategy; these are usually patients with good performance status who are asymptomatic, do not have B symptoms, have normal LDH levels, have non-nodal disease, and have low Ki-67 percentages. This observation strategy was studied by a Canadian group that evaluated 440 patients, 75 of whom were observed for 3 or more months.[12] The median time to treatment was 35 months, and the OS in this group was longer than that in the early treatment group.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A Retired Teacher With a Constant Headache and Vomiting"
},
{
"authors": "Amanda L. Blackmon, DO, MS; Lauren Pinter-Brown, MD",
"content": [
"CNS involvement in mantle cell lymphoma usually presents in patients with relapse, leading to the question of which patients require CNS prophylaxis. No guidelines regarding patients who should receive prophylaxis have been established. However, blastoid histology, high Ki-67 percentage, high LDH level, and high risk score may suggest the need to consider prophylactic CNS treatment.[13] Once patients have a CNS relapse, it usually accompanies a systemic relapse. Of note, mantle cell lymphoma has more of a predilection for leptomeningeal disease, compared with diffuse large B-cell lymphoma, in which parenchymal relapse is more frequent.",
"In a study by Cheah and colleagues,[2] the incidence of CNS involvement was 0.9% at diagnosis and 4.1% overall. The median overall survival at the time of CNS involvement was 3.7 months.",
"CNS involvement can be treated several ways, including certain chemotherapy that crosses the blood-brain barrier; intrathecal chemotherapy; and radiation for patients with refractory disease, usually parenchymal disease. Systemic chemotherapy often includes high-dose methotrexate or cytarabine, which can be used as monotherapy or in conjunction with R-CHOP. Intrathecal chemotherapy can consist of triple therapy with methotrexate, cytarabine, and hydrocortisone; however, methotrexate and liposomal cytarabine can be used, as well as methotrexate alone. Triple therapy rapidly clears from the CSF and thus requires administration two or three times per week until the CSF is cleared. This is generally the approach used by the authors of this case. Liposomal cytarabine has a longer half-life and has been associated with more case reports of adverse events.",
"HSCT has been used as consolidation therapy in patients with CNS involvement, which has shown longer rates of remission (>12 mo) in the small subset of patients who are eligible for HSCT.[2] Ibrutinib has been discussed in case reports, inducing a rapid, dramatic, and sustained response in a patient with mantle cell lymphoma who had symptomatic CNS relapse.[14] Whether patients with high-risk disease should be given CNS prophylaxis given the rarity of CNS involvement is unclear; however, it should be considered in patients with high-risk disease who receive regimens that do not cross the blood-brain barrier.",
"The patient in this case received intrathecal chemotherapy with methotrexate/cytarabine/hydrocortisone three times weekly followed by leucovorin for 3 weeks when his CSF had cleared by cell count and cytology. After clearance, he received weekly intrathecal triple therapy for 4 weeks and then tapered to every 2 weeks for 1 month. He developed diarrhea and gait imbalance. MRI of the brain and spine was performed, given that his CSF remained clear (Figure 2).",
"Figure 2.",
"The spinal MRI was unremarkable. MRI of the brain revealed periventricular white matter changes consistent with leukoencephalopathy. He has also demonstrated mild bilateral weakness and reserved deep tendon reflexes.",
"Neurotoxicity associated with various intrathecal chemotherapies has been described in a limited number of case reports. Whether the specific agent used has a causative effect is unclear; intrathecal chemotherapy often consists of more than one agent or is given in combination with systemic chemotherapy, which may cause heightened toxicity.[15] Another question is whether the vehicle used to carry the chemotherapy could have an independent association with neurologic toxicity.[16] The disease being treated may also alter the toxicity profile.",
"A series of case reports describe treatment with liposomal cytarabine, especially when used in combination with systemic chemotherapy that crosses the blood-brain barrier (ie, methotrexate); this causes significant neurotoxicity that is not always reversible and can lead to death in rare cases.[17] Intrathecal methotrexate has been associated with leukoencephalopathy/neurotoxicity leading to seizures, confusion, and headache, as well as posterior reversible leukoencephalopathy syndrome.[18,19,20]",
"The amount of intrathecal chemotherapy needed to ensure that lymphoma is adequately treated and avoid detrimental side effects remains unknown. The accumulated dose may not be the only factor associated with toxicity. This toxicity can be reversible, as in this patient's case, and may not occur with rechallenge."
],
"date": "January 05, 2022",
"figures": [
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/915/146/915146-Thumb2.png"
}
],
"markdown": "# A Retired Teacher With a Constant Headache and Vomiting\n\n **Authors:** Amanda L. Blackmon, DO, MS; Lauren Pinter-Brown, MD \n **Date:** January 05, 2022\n\n ## Content\n\n CNS involvement in mantle cell lymphoma usually presents in patients with relapse, leading to the question of which patients require CNS prophylaxis. No guidelines regarding patients who should receive prophylaxis have been established. However, blastoid histology, high Ki-67 percentage, high LDH level, and high risk score may suggest the need to consider prophylactic CNS treatment.[13] Once patients have a CNS relapse, it usually accompanies a systemic relapse. Of note, mantle cell lymphoma has more of a predilection for leptomeningeal disease, compared with diffuse large B-cell lymphoma, in which parenchymal relapse is more frequent.\nIn a study by Cheah and colleagues,[2] the incidence of CNS involvement was 0.9% at diagnosis and 4.1% overall. The median overall survival at the time of CNS involvement was 3.7 months.\nCNS involvement can be treated several ways, including certain chemotherapy that crosses the blood-brain barrier; intrathecal chemotherapy; and radiation for patients with refractory disease, usually parenchymal disease. Systemic chemotherapy often includes high-dose methotrexate or cytarabine, which can be used as monotherapy or in conjunction with R-CHOP. Intrathecal chemotherapy can consist of triple therapy with methotrexate, cytarabine, and hydrocortisone; however, methotrexate and liposomal cytarabine can be used, as well as methotrexate alone. Triple therapy rapidly clears from the CSF and thus requires administration two or three times per week until the CSF is cleared. This is generally the approach used by the authors of this case. Liposomal cytarabine has a longer half-life and has been associated with more case reports of adverse events.\nHSCT has been used as consolidation therapy in patients with CNS involvement, which has shown longer rates of remission (>12 mo) in the small subset of patients who are eligible for HSCT.[2] Ibrutinib has been discussed in case reports, inducing a rapid, dramatic, and sustained response in a patient with mantle cell lymphoma who had symptomatic CNS relapse.[14] Whether patients with high-risk disease should be given CNS prophylaxis given the rarity of CNS involvement is unclear; however, it should be considered in patients with high-risk disease who receive regimens that do not cross the blood-brain barrier.\nThe patient in this case received intrathecal chemotherapy with methotrexate/cytarabine/hydrocortisone three times weekly followed by leucovorin for 3 weeks when his CSF had cleared by cell count and cytology. After clearance, he received weekly intrathecal triple therapy for 4 weeks and then tapered to every 2 weeks for 1 month. He developed diarrhea and gait imbalance. MRI of the brain and spine was performed, given that his CSF remained clear (Figure 2).\nFigure 2.\nThe spinal MRI was unremarkable. MRI of the brain revealed periventricular white matter changes consistent with leukoencephalopathy. He has also demonstrated mild bilateral weakness and reserved deep tendon reflexes.\nNeurotoxicity associated with various intrathecal chemotherapies has been described in a limited number of case reports. Whether the specific agent used has a causative effect is unclear; intrathecal chemotherapy often consists of more than one agent or is given in combination with systemic chemotherapy, which may cause heightened toxicity.[15] Another question is whether the vehicle used to carry the chemotherapy could have an independent association with neurologic toxicity.[16] The disease being treated may also alter the toxicity profile.\nA series of case reports describe treatment with liposomal cytarabine, especially when used in combination with systemic chemotherapy that crosses the blood-brain barrier (ie, methotrexate); this causes significant neurotoxicity that is not always reversible and can lead to death in rare cases.[17] Intrathecal methotrexate has been associated with leukoencephalopathy/neurotoxicity leading to seizures, confusion, and headache, as well as posterior reversible leukoencephalopathy syndrome.[18,19,20]\nThe amount of intrathecal chemotherapy needed to ensure that lymphoma is adequately treated and avoid detrimental side effects remains unknown. The accumulated dose may not be the only factor associated with toxicity. This toxicity can be reversible, as in this patient's case, and may not occur with rechallenge.\n\n ## Figures\n\n **Figure 2.** \n \n\n\n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1381216,
"choiceText": "True",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381218,
"choiceText": "False",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "A subset of patients may be able to pursue a watchful waiting strategy; these are usually patients with good performance status who are asymptomatic, do not have B symptoms, have normal LDH levels, have non-nodal disease, and have low Ki-67 percentages.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 441057,
"questionText": "True or false: All patients with mantle cell lymphoma should be treated starting at the time of diagnosis.",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1381220,
"choiceText": "A Ki-67 of 50%",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381222,
"choiceText": "Blastoid variant",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381224,
"choiceText": "IgVH mutated status",
"correct": true,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381226,
"choiceText": "Complex karyotype",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381228,
"choiceText": "<i>TP53</i> mutated status\r\n",
"correct": false,
"displayOrder": 5,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "An IgVH hypermutated status is a good prognostic factor and is often seen in the leukemic variant. Factors that have been associated with worse clinical outcomes include complex karyotype, <i>TP53</i> mutations or overexpression, and <i>MYC</i> translocation or overexpression.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 441059,
"questionText": "Which of the following is considered a good prognostic factor associated with mantle cell lymphoma?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Retired Teacher With a Constant Headache and Vomiting"
},
{
"authors": "Amanda L. Blackmon, DO, MS; Lauren Pinter-Brown, MD",
"content": [],
"date": "January 05, 2022",
"figures": [],
"markdown": "# A Retired Teacher With a Constant Headache and Vomiting\n\n **Authors:** Amanda L. Blackmon, DO, MS; Lauren Pinter-Brown, MD \n **Date:** January 05, 2022\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1381216,
"choiceText": "True",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381218,
"choiceText": "False",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "A subset of patients may be able to pursue a watchful waiting strategy; these are usually patients with good performance status who are asymptomatic, do not have B symptoms, have normal LDH levels, have non-nodal disease, and have low Ki-67 percentages.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 441057,
"questionText": "True or false: All patients with mantle cell lymphoma should be treated starting at the time of diagnosis.",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1381220,
"choiceText": "A Ki-67 of 50%",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381222,
"choiceText": "Blastoid variant",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381224,
"choiceText": "IgVH mutated status",
"correct": true,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381226,
"choiceText": "Complex karyotype",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381228,
"choiceText": "<i>TP53</i> mutated status\r\n",
"correct": false,
"displayOrder": 5,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "An IgVH hypermutated status is a good prognostic factor and is often seen in the leukemic variant. Factors that have been associated with worse clinical outcomes include complex karyotype, <i>TP53</i> mutations or overexpression, and <i>MYC</i> translocation or overexpression.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 441059,
"questionText": "Which of the following is considered a good prognostic factor associated with mantle cell lymphoma?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Retired Teacher With a Constant Headache and Vomiting"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1381206,
"choiceText": "Normal-pressure hydrocephalus",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381208,
"choiceText": "Cryptococcal meningitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381210,
"choiceText": "Mumps ",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381212,
"choiceText": "Leptomeningeal disease ",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381214,
"choiceText": "Lymphocytic choriomeningitis\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 441055,
"questionText": "Based on only these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1381216,
"choiceText": "True",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381218,
"choiceText": "False",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "A subset of patients may be able to pursue a watchful waiting strategy; these are usually patients with good performance status who are asymptomatic, do not have B symptoms, have normal LDH levels, have non-nodal disease, and have low Ki-67 percentages.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 441057,
"questionText": "True or false: All patients with mantle cell lymphoma should be treated starting at the time of diagnosis.",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1381220,
"choiceText": "A Ki-67 of 50%",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381222,
"choiceText": "Blastoid variant",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381224,
"choiceText": "IgVH mutated status",
"correct": true,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381226,
"choiceText": "Complex karyotype",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1381228,
"choiceText": "<i>TP53</i> mutated status\r\n",
"correct": false,
"displayOrder": 5,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "An IgVH hypermutated status is a good prognostic factor and is often seen in the leukemic variant. Factors that have been associated with worse clinical outcomes include complex karyotype, <i>TP53</i> mutations or overexpression, and <i>MYC</i> translocation or overexpression.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 441059,
"questionText": "Which of the following is considered a good prognostic factor associated with mantle cell lymphoma?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
877077 | /viewarticle/877077 | [
{
"authors": "Alfredo Musumeci, MD, PhD; Michele Alzetta, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 42-year-old comatose man is brought to the emergency department (ED) by ambulance. He had recently been hospitalized for decompensated hepatitis C virus liver cirrhosis at another hospital, from which he left against medical advice. In the hours before admission to the ED, the patient experienced two witnessed episodes of loss of consciousness associated with urinary incontinence and myoclonic jerks.",
"The patient's prescribed medications include abacavir, lamivudine, and zidovudine daily for HIV infection. He also takes furosemide (50 mg), potassium canrenoate (an aldosterone antagonist), lorazepam, and methadone (90 mg); the latter is for the management of heroin addiction."
],
"date": "December 14, 2021",
"figures": [],
"markdown": "# Seizures in a 42-Year-Old Who Left a Hospital Against Advice\n\n **Authors:** Alfredo Musumeci, MD, PhD; Michele Alzetta, MD \n **Date:** December 14, 2021\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 42-year-old comatose man is brought to the emergency department (ED) by ambulance. He had recently been hospitalized for decompensated hepatitis C virus liver cirrhosis at another hospital, from which he left against medical advice. In the hours before admission to the ED, the patient experienced two witnessed episodes of loss of consciousness associated with urinary incontinence and myoclonic jerks.\nThe patient's prescribed medications include abacavir, lamivudine, and zidovudine daily for HIV infection. He also takes furosemide (50 mg), potassium canrenoate (an aldosterone antagonist), lorazepam, and methadone (90 mg); the latter is for the management of heroin addiction.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Seizures in a 42-Year-Old Who Left a Hospital Against Advice"
},
{
"authors": "Alfredo Musumeci, MD, PhD; Michele Alzetta, MD",
"content": [
"Upon physical examination, the patient is lethargic, and his Glasgow Coma Scale score is 6 (eye opening response, 1; verbal response, 1; motor response, 4). His pupils are normal in size and bilaterally reactive to light. He has a temperature of 96.8°F (36.5°C), a blood pressure of 90/54 mm Hg, and a pulse rate of 86 beats/min. His respiratory rate is 18 breaths/min, and he has an oxygen saturation of 98% while breathing room air.",
"Upon auscultation, the lung fields are clear bilaterally, and normal heart sounds are heard. His peripheral pulses are palpable; however, bilateral lower extremity pitting edema is present. The abdomen is distended, tense, and with ascites. His sclerae are noted to be icteric.",
"Laboratory tests are ordered, with pertinent findings that include a hemoglobin level of 11.1 g/dL (reference range, 13.5-17.5 g/dL) and a platelet count of 24 × 109/L (reference range, 136-436 × 109/L).",
"A chemistry panel reveals the following:",
"Sodium level: 134 mEq/L (134 mmol/L; reference range, 135-145 mEq/L)",
"Potassium level: 3.2 mEq/L (3.2 mmol/L; reference range, 3.5-5 mEq/L)",
"Creatinine level: 0.6 mg/dL (53.04 µmol/L; reference range, 0.7-1.2 mg/dL)",
"Glucose level: 148 mg/dL (8.21 mmol/L; reference range, <140 mg/dL)",
"Bilirubin level: 4.7 mg/dL (80.37 µmol/L; reference range, 0.3-1 mg/dL)",
"Magnesium level: 1.3 mg/dL (0.53 mmol/L; reference range, 1.5-2.5 mg/dL)",
"Ammonium level: 153.3 µg/dL (90 μmol/L; reference range, 11-79 µg/dL)",
"Ionized calcium level: 3.96 mg/dL (0.99 mmol/L; reference range 4.6-5.6 mg/dL)",
"His troponin level is 0.07 ng/mL (0.07 μg/L; reference range, <0.12 ng/mL). Serum alcohol testing results are negative, and a urine toxicology screen is negative for cannabinoids, cocaine, and opiates (note that methadone usage may not cause a positive opiate result). A CT scan of the brain is negative for acute abnormalities.",
"The patient is initially thought to have had a seizure and is cautiously given benzodiazepines to prevent a recurrence.",
"An electrocardiogram (ECG) is then performed (Figure 1). Soon afterwards, an abnormal tracing is seen on the cardiac monitor (Figure 2), and the patient becomes pulseless and apneic and requires cardiopulmonary resuscitation.",
"Figure 1.",
"Figure 2."
],
"date": "December 14, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/877/077/877077-Thumb1.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/877/077/877077-Thumb2.jpg"
}
],
"markdown": "# Seizures in a 42-Year-Old Who Left a Hospital Against Advice\n\n **Authors:** Alfredo Musumeci, MD, PhD; Michele Alzetta, MD \n **Date:** December 14, 2021\n\n ## Content\n\n Upon physical examination, the patient is lethargic, and his Glasgow Coma Scale score is 6 (eye opening response, 1; verbal response, 1; motor response, 4). His pupils are normal in size and bilaterally reactive to light. He has a temperature of 96.8°F (36.5°C), a blood pressure of 90/54 mm Hg, and a pulse rate of 86 beats/min. His respiratory rate is 18 breaths/min, and he has an oxygen saturation of 98% while breathing room air.\nUpon auscultation, the lung fields are clear bilaterally, and normal heart sounds are heard. His peripheral pulses are palpable; however, bilateral lower extremity pitting edema is present. The abdomen is distended, tense, and with ascites. His sclerae are noted to be icteric.\nLaboratory tests are ordered, with pertinent findings that include a hemoglobin level of 11.1 g/dL (reference range, 13.5-17.5 g/dL) and a platelet count of 24 × 109/L (reference range, 136-436 × 109/L).\nA chemistry panel reveals the following:\nSodium level: 134 mEq/L (134 mmol/L; reference range, 135-145 mEq/L)\nPotassium level: 3.2 mEq/L (3.2 mmol/L; reference range, 3.5-5 mEq/L)\nCreatinine level: 0.6 mg/dL (53.04 µmol/L; reference range, 0.7-1.2 mg/dL)\nGlucose level: 148 mg/dL (8.21 mmol/L; reference range, <140 mg/dL)\nBilirubin level: 4.7 mg/dL (80.37 µmol/L; reference range, 0.3-1 mg/dL)\nMagnesium level: 1.3 mg/dL (0.53 mmol/L; reference range, 1.5-2.5 mg/dL)\nAmmonium level: 153.3 µg/dL (90 μmol/L; reference range, 11-79 µg/dL)\nIonized calcium level: 3.96 mg/dL (0.99 mmol/L; reference range 4.6-5.6 mg/dL)\nHis troponin level is 0.07 ng/mL (0.07 μg/L; reference range, <0.12 ng/mL). Serum alcohol testing results are negative, and a urine toxicology screen is negative for cannabinoids, cocaine, and opiates (note that methadone usage may not cause a positive opiate result). A CT scan of the brain is negative for acute abnormalities.\nThe patient is initially thought to have had a seizure and is cautiously given benzodiazepines to prevent a recurrence.\nAn electrocardiogram (ECG) is then performed (Figure 1). Soon afterwards, an abnormal tracing is seen on the cardiac monitor (Figure 2), and the patient becomes pulseless and apneic and requires cardiopulmonary resuscitation.\nFigure 1.\nFigure 2.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1073616,
"choiceText": "Supraventricular tachycardia (SVT)\r\n",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073618,
"choiceText": "Torsade de pointes",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073620,
"choiceText": "Ventricular fibrillation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073622,
"choiceText": "SVT with aberrancy\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 339965,
"questionText": "Which rhythm is being demonstrated in Figure 2?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Seizures in a 42-Year-Old Who Left a Hospital Against Advice"
},
{
"authors": "Alfredo Musumeci, MD, PhD; Michele Alzetta, MD",
"content": [
"The cardiac rhythm strip (Figure 2) demonstrated torsade de pointes (French for \"twisting of the points\"), otherwise known as simply \"torsades\" or polymorphic ventricular tachycardia.",
"Figure 1.",
"Figure 2.",
"The initial ECG (Figure 1), which was obtained before the development of the torsades, revealed a prolonged QT interval (544 msec), with a QT interval corrected for the heart rate (QTc) of 647 msec. Moreover, notched T waves were noted in leads II, III, aVF, and V1-V6. A prolonged QT interval is often noted incidentally on an ECG in an asymptomatic patient; however, in a patient who presents with palpitations, presyncope, syncope, or cardiac arrest, the presence of a prolonged QT interval should raise particular concern for torsade de pointes.",
"QT prolongation can be either acquired or congenital. A thorough clinical history-taking and knowledge of the patient's current medications is very important for this differentiation. Congenital long QT syndrome (LQTS) is a disorder characterized by abnormal QT-interval prolongation on the ECG caused by cardiac myocyte ion channel gene mutations, with a propensity to ventricular tachyarrhythmias. Patients are typically young and may present with syncope or sudden death.[1,2]",
"Acquired QT interval prolongation may be drug-induced, or it may be caused by certain electrolyte derangements, such as hypomagnesemia, hypokalemia, and hypocalcemia. Many drugs have been implicated, including class 1A antiarrhythmic drugs such as quinidine and procainamide and class III antiarrhythmics such as amiodarone and sotalol. Other drugs that have been implicated include antihistamines (terfenadine, astemizole), macrolide antibiotics (erythromycin, clarithromycin, clindamycin), pentamidine, serotonin receptor antagonists (ketanserin), diuretics (indapamide), certain fluoroquinolone antibiotics, tricyclic antidepressants, antipsychotics (phenothiazines, haloperidol, mesoridazine, pimozide, thioridazine, ziprasidone), gastrointestinal motility enhancers (cisapride, domperidone), inotropes (amrinone, milrinone), toxins (organophosphates, arsenic), protease inhibitors, and methadone.[3,4,5,6,7,8,9,10]"
],
"date": "December 14, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/877/077/877077-Thumb1.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/877/077/877077-Thumb2.jpg"
}
],
"markdown": "# Seizures in a 42-Year-Old Who Left a Hospital Against Advice\n\n **Authors:** Alfredo Musumeci, MD, PhD; Michele Alzetta, MD \n **Date:** December 14, 2021\n\n ## Content\n\n The cardiac rhythm strip (Figure 2) demonstrated torsade de pointes (French for \"twisting of the points\"), otherwise known as simply \"torsades\" or polymorphic ventricular tachycardia.\nFigure 1.\nFigure 2.\nThe initial ECG (Figure 1), which was obtained before the development of the torsades, revealed a prolonged QT interval (544 msec), with a QT interval corrected for the heart rate (QTc) of 647 msec. Moreover, notched T waves were noted in leads II, III, aVF, and V1-V6. A prolonged QT interval is often noted incidentally on an ECG in an asymptomatic patient; however, in a patient who presents with palpitations, presyncope, syncope, or cardiac arrest, the presence of a prolonged QT interval should raise particular concern for torsade de pointes.\nQT prolongation can be either acquired or congenital. A thorough clinical history-taking and knowledge of the patient's current medications is very important for this differentiation. Congenital long QT syndrome (LQTS) is a disorder characterized by abnormal QT-interval prolongation on the ECG caused by cardiac myocyte ion channel gene mutations, with a propensity to ventricular tachyarrhythmias. Patients are typically young and may present with syncope or sudden death.[1,2]\nAcquired QT interval prolongation may be drug-induced, or it may be caused by certain electrolyte derangements, such as hypomagnesemia, hypokalemia, and hypocalcemia. Many drugs have been implicated, including class 1A antiarrhythmic drugs such as quinidine and procainamide and class III antiarrhythmics such as amiodarone and sotalol. Other drugs that have been implicated include antihistamines (terfenadine, astemizole), macrolide antibiotics (erythromycin, clarithromycin, clindamycin), pentamidine, serotonin receptor antagonists (ketanserin), diuretics (indapamide), certain fluoroquinolone antibiotics, tricyclic antidepressants, antipsychotics (phenothiazines, haloperidol, mesoridazine, pimozide, thioridazine, ziprasidone), gastrointestinal motility enhancers (cisapride, domperidone), inotropes (amrinone, milrinone), toxins (organophosphates, arsenic), protease inhibitors, and methadone.[3,4,5,6,7,8,9,10]\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1073616,
"choiceText": "Supraventricular tachycardia (SVT)\r\n",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073618,
"choiceText": "Torsade de pointes",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073620,
"choiceText": "Ventricular fibrillation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073622,
"choiceText": "SVT with aberrancy\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 339965,
"questionText": "Which rhythm is being demonstrated in Figure 2?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Seizures in a 42-Year-Old Who Left a Hospital Against Advice"
},
{
"authors": "Alfredo Musumeci, MD, PhD; Michele Alzetta, MD",
"content": [
"Drug-induced prolongation of the QT interval is directly linked to a modification in myocardial cell repolarization, which is mediated by the efflux of potassium ions. The shape of the action potential depends on the balance between sodium and calcium inflow and potassium outflow. Two subtypes of the delayed rectifier K+ current, IKr (rapid) and IKs (slow), are responsible for repolarization. The human ether-a-go-go related gene (hERG; also termed KCNH2) codes for a protein known as the Kv 11.1 potassium ion channel, which mediates the repolarizing potassium current IKr.",
"Blockage of the hERG-encoded potassium channels has been implicated as a cause of drug-induced QT prolongation. A strong correlation is noted between IKr blockade and ventricular arrhythmia or sudden death. Drugs that block the IKr channel increase the QT interval and allow inward current, particularly calcium, to reactivate, leading to early after-depolarizations in cardiac tissue that may result in torsades. Other drugs implicated in QT prolongation have no effect on the potassium channels; therefore, additional cardiac mechanisms can play a significant role.[3,4,5,10]",
"Some medications prolong the QT interval at specific doses, whereas others may act at any dose. Several agents are metabolized by the hepatic cytochrome P450 3A4 (CYP3A4) system, and drug-drug interactions and consequent QT prolongation can causes torsades. Drug interactions in this setting are primarily pharmacokinetic.",
"When administering a drug that potentially prolongs the QT interval, numerous predisposing factors for torsades development must be considered, including advanced age, obesity, poor nutrition (anorexia nervosa, starvation diets, alcoholism), bradycardia (<50 beats/min), cerebrovascular disease (intracranial and subarachnoid hemorrhage, stroke, intracranial trauma, thalamic hematoma), congenital long QT syndrome, heart failure (cardiomyopathy, dilated or hypertrophic), hypoglycemia, hypothermia, hypothyroidism, myocardial ischemia or infarction, organophosphate exposure, pheochromocytoma, pituitary insufficiency, coadministration of other QT prolonging agents, and hypoxia.",
"If a drug-to-drug interaction is suspected, the drug should be withdrawn. Ehret and colleagues[9] studied a population of active or former intravenous drug abusers and suggested that methadone (even at low doses), CYP3A4 inhibitors, and hepatic dysfunction contributed to prolongation of QT. Methadone delays cardiac repolarization by blocking the flow of potassium ions through the hERG channels, but no evidence suggests interaction between this drug and nucleoside reverse transcriptase inhibitors.[4,5,7,9,10,11]",
"Torsade de pointes is characterized by QRS complexes that vary in axis and amplitude over the isoelectric line (\"twisting around the points,\" as the name implies). Other associated characteristics include the presence of long and short beat-to-beat (RR) interval onset after an early premature ventricular contraction.",
"A relationship between the degree of QT interval prolongation and the development of torsades is noted. The QT interval varies directly with heart rate, and a correction is required in order to compensate for heart rate. A commonly used correction (QTc) is the Bazett correction (QTc=QT/√RR), wherein QT is the longest QT interval measured on the ECG, and RR is an average RR interval. QT measurement should be made manually from a 12-lead ECG, and it is calculated from the beginning of the QRS complex to the end of the T wave and averaged over three to five beats in a single lead. Prominent U waves should be included in the measurement if they merge into the T wave. It is advisable to assess QT during peak plasma concentration of any ingested QT-prolonging substances and to correct it for heart rate while looking for other warning signs, including the appearance of prominent U waves, extrasystoles, and U wave augmentation after extrasystole.",
"Corrected QT is considered prolonged if it is beyond 440 msec for adult males, 460 msec for adult females, and 500 msec in the presence of ventricular depolarization abnormalities (ie, bundle branch blocks or intraventricular conduction delay greater than 120 msec). The uncorrected QT interval should also be considered, however, as a very long QT (>600 msec) after drug exposure is a marker of an increased risk for torsades.[2,4,10,12]"
],
"date": "December 14, 2021",
"figures": [],
"markdown": "# Seizures in a 42-Year-Old Who Left a Hospital Against Advice\n\n **Authors:** Alfredo Musumeci, MD, PhD; Michele Alzetta, MD \n **Date:** December 14, 2021\n\n ## Content\n\n Drug-induced prolongation of the QT interval is directly linked to a modification in myocardial cell repolarization, which is mediated by the efflux of potassium ions. The shape of the action potential depends on the balance between sodium and calcium inflow and potassium outflow. Two subtypes of the delayed rectifier K+ current, IKr (rapid) and IKs (slow), are responsible for repolarization. The human ether-a-go-go related gene (hERG; also termed KCNH2) codes for a protein known as the Kv 11.1 potassium ion channel, which mediates the repolarizing potassium current IKr.\nBlockage of the hERG-encoded potassium channels has been implicated as a cause of drug-induced QT prolongation. A strong correlation is noted between IKr blockade and ventricular arrhythmia or sudden death. Drugs that block the IKr channel increase the QT interval and allow inward current, particularly calcium, to reactivate, leading to early after-depolarizations in cardiac tissue that may result in torsades. Other drugs implicated in QT prolongation have no effect on the potassium channels; therefore, additional cardiac mechanisms can play a significant role.[3,4,5,10]\nSome medications prolong the QT interval at specific doses, whereas others may act at any dose. Several agents are metabolized by the hepatic cytochrome P450 3A4 (CYP3A4) system, and drug-drug interactions and consequent QT prolongation can causes torsades. Drug interactions in this setting are primarily pharmacokinetic.\nWhen administering a drug that potentially prolongs the QT interval, numerous predisposing factors for torsades development must be considered, including advanced age, obesity, poor nutrition (anorexia nervosa, starvation diets, alcoholism), bradycardia (<50 beats/min), cerebrovascular disease (intracranial and subarachnoid hemorrhage, stroke, intracranial trauma, thalamic hematoma), congenital long QT syndrome, heart failure (cardiomyopathy, dilated or hypertrophic), hypoglycemia, hypothermia, hypothyroidism, myocardial ischemia or infarction, organophosphate exposure, pheochromocytoma, pituitary insufficiency, coadministration of other QT prolonging agents, and hypoxia.\nIf a drug-to-drug interaction is suspected, the drug should be withdrawn. Ehret and colleagues[9] studied a population of active or former intravenous drug abusers and suggested that methadone (even at low doses), CYP3A4 inhibitors, and hepatic dysfunction contributed to prolongation of QT. Methadone delays cardiac repolarization by blocking the flow of potassium ions through the hERG channels, but no evidence suggests interaction between this drug and nucleoside reverse transcriptase inhibitors.[4,5,7,9,10,11]\nTorsade de pointes is characterized by QRS complexes that vary in axis and amplitude over the isoelectric line (\"twisting around the points,\" as the name implies). Other associated characteristics include the presence of long and short beat-to-beat (RR) interval onset after an early premature ventricular contraction.\nA relationship between the degree of QT interval prolongation and the development of torsades is noted. The QT interval varies directly with heart rate, and a correction is required in order to compensate for heart rate. A commonly used correction (QTc) is the Bazett correction (QTc=QT/√RR), wherein QT is the longest QT interval measured on the ECG, and RR is an average RR interval. QT measurement should be made manually from a 12-lead ECG, and it is calculated from the beginning of the QRS complex to the end of the T wave and averaged over three to five beats in a single lead. Prominent U waves should be included in the measurement if they merge into the T wave. It is advisable to assess QT during peak plasma concentration of any ingested QT-prolonging substances and to correct it for heart rate while looking for other warning signs, including the appearance of prominent U waves, extrasystoles, and U wave augmentation after extrasystole.\nCorrected QT is considered prolonged if it is beyond 440 msec for adult males, 460 msec for adult females, and 500 msec in the presence of ventricular depolarization abnormalities (ie, bundle branch blocks or intraventricular conduction delay greater than 120 msec). The uncorrected QT interval should also be considered, however, as a very long QT (>600 msec) after drug exposure is a marker of an increased risk for torsades.[2,4,10,12]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Seizures in a 42-Year-Old Who Left a Hospital Against Advice"
},
{
"authors": "Alfredo Musumeci, MD, PhD; Michele Alzetta, MD",
"content": [
"The patient in this case was initially treated with 2 g of intravenous magnesium sulfate and 1 g of calcium chloride. Despite this, he developed recurrent torsade de pointes. He underwent repeated defibrillation followed by irregular rhythms, including premature atrial complexes and ventricular bigeminy. The recurrent episodes of torsade de pointes were then treated with an intravenous bolus of lidocaine followed by a 2-mg/min infusion. Normal sinus rhythm then returned, and the patient slowly improved and regained consciousness.",
"In this case, the cause of the patient's QT prolongation was likely multifactorial and probably included the chronic use of methadone and electrolyte derangement. Slight hypomagnesemia, hypocalcemia, and hypokalemia were noted. These mild electrolyte abnormalities alone are not sufficient to result in torsade de pointes, as evidenced by the persistence of episodic torsade de pointes despite electrolyte replacement. Once the methadone was withdrawn, however, no further episodes of torsade de pointes occurred, and the QT interval normalized.",
"Immediate treatment for patients who develop torsades can be categorized into pharmacologic and nonpharmacologic approaches. Intravenous magnesium sulfate (2-g bolus followed by an infusion of 2-4 mg/min) is the initial therapy, regardless of the serum levels of magnesium. If the patient is hemodynamically unstable, and the torsades persists, or if ventricular fibrillation develops, immediate unsynchronized defibrillation is indicated. Serum potassium levels should be maintained in the high-normal range (4.5-5 mmol/L). Overdrive transvenous pacing shortens the QT interval and is highly effective in preventing recurrences, especially in the setting of bradycardia. Maintaining a heart rate greater than 70 beats/min protects against drug-induced torsades.[10]",
"Isoproterenol is useful if temporary pacing is unavailable or while preparing for transvenous catheter insertion. It is contraindicated in patients with congenital LQTS and in ischemic heart disease. Additional treatments include discontinuation of any drug known to cause QT prolongation, correction of electrolyte disturbances, and monitoring the cardiac rhythm until the patient is considered out of risk. Beta-blockers can help prevent symptoms in most people with long QT syndrome, but they do not substantially shorten the QT interval. This class of drugs slows the heart rate and helps prevent tachyarrhythmia. Long-acting preparations such as nadolol and atenolol are usually used. The use of implantable cardioverter-defibrillators (ICDs) is widely considered in patients at high risk for sudden death.[6,13]",
"This case illustrates an incident of likely drug-induced torsade de pointes resulting from methadone usage in the setting of electrolyte abnormalities. The case highlights the need for an evaluation for potential cardiogenic causes of syncope in patients who present with an abnormal ECG."
],
"date": "December 14, 2021",
"figures": [],
"markdown": "# Seizures in a 42-Year-Old Who Left a Hospital Against Advice\n\n **Authors:** Alfredo Musumeci, MD, PhD; Michele Alzetta, MD \n **Date:** December 14, 2021\n\n ## Content\n\n The patient in this case was initially treated with 2 g of intravenous magnesium sulfate and 1 g of calcium chloride. Despite this, he developed recurrent torsade de pointes. He underwent repeated defibrillation followed by irregular rhythms, including premature atrial complexes and ventricular bigeminy. The recurrent episodes of torsade de pointes were then treated with an intravenous bolus of lidocaine followed by a 2-mg/min infusion. Normal sinus rhythm then returned, and the patient slowly improved and regained consciousness.\nIn this case, the cause of the patient's QT prolongation was likely multifactorial and probably included the chronic use of methadone and electrolyte derangement. Slight hypomagnesemia, hypocalcemia, and hypokalemia were noted. These mild electrolyte abnormalities alone are not sufficient to result in torsade de pointes, as evidenced by the persistence of episodic torsade de pointes despite electrolyte replacement. Once the methadone was withdrawn, however, no further episodes of torsade de pointes occurred, and the QT interval normalized.\nImmediate treatment for patients who develop torsades can be categorized into pharmacologic and nonpharmacologic approaches. Intravenous magnesium sulfate (2-g bolus followed by an infusion of 2-4 mg/min) is the initial therapy, regardless of the serum levels of magnesium. If the patient is hemodynamically unstable, and the torsades persists, or if ventricular fibrillation develops, immediate unsynchronized defibrillation is indicated. Serum potassium levels should be maintained in the high-normal range (4.5-5 mmol/L). Overdrive transvenous pacing shortens the QT interval and is highly effective in preventing recurrences, especially in the setting of bradycardia. Maintaining a heart rate greater than 70 beats/min protects against drug-induced torsades.[10]\nIsoproterenol is useful if temporary pacing is unavailable or while preparing for transvenous catheter insertion. It is contraindicated in patients with congenital LQTS and in ischemic heart disease. Additional treatments include discontinuation of any drug known to cause QT prolongation, correction of electrolyte disturbances, and monitoring the cardiac rhythm until the patient is considered out of risk. Beta-blockers can help prevent symptoms in most people with long QT syndrome, but they do not substantially shorten the QT interval. This class of drugs slows the heart rate and helps prevent tachyarrhythmia. Long-acting preparations such as nadolol and atenolol are usually used. The use of implantable cardioverter-defibrillators (ICDs) is widely considered in patients at high risk for sudden death.[6,13]\nThis case illustrates an incident of likely drug-induced torsade de pointes resulting from methadone usage in the setting of electrolyte abnormalities. The case highlights the need for an evaluation for potential cardiogenic causes of syncope in patients who present with an abnormal ECG.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1073624,
"choiceText": "A 63-year-old woman with a 2-day history of vomiting and watery diarrhea",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073626,
"choiceText": "A 38-year-old man with a history of schizophrenia recently treated with erythromycin for a sinus infection",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073628,
"choiceText": "A 58-year-old man status post-percutaneous coronary intervention initiated on clopidogrel and atorvastatin",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073630,
"choiceText": "A 23-year-old woman deeply intoxicated after binge drinking",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073632,
"choiceText": "A 45-year-old diabetic woman with a blood glucose of 458 mg/dL (25.4 mmol/L) and no urine ketones\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Acquired QT interval prolongation may be drug-induced, or it may be caused by certain electrolyte derangements, such as hypomagnesemia, hypokalemia, and hypocalcemia. Many drugs have been implicated, including class 1A antiarrhythmic drugs such as quinidine and procainamide and class III antiarrhythmics such as amiodarone and sotalol. Other drugs that have been implicated include antihistamines (terfenadine, astemizole), macrolide antibiotics (erythromycin, clarithromycin, clindamycin), pentamidine, serotonin receptor antagonists (ketanserin), diuretics (indapamide), certain fluoroquinolone antibiotics, tricyclic antidepressants, antipsychotics (phenothiazines, haloperidol, mesoridazine, pimozide, thioridazine, ziprasidone), gastrointestinal motility enhancers (cisapride, domperidone), inotropes (amrinone, milrinone), toxins (organophosphates, arsenic), protease inhibitors, and methadone.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 339967,
"questionText": "A patient presents to the ED after a syncopal episode and is found to have a prolonged QT interval; subsequently, the patient develops torsade de pointes. Which clinical scenario is most likely to result in this condition?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1073634,
"choiceText": "Unsynchronized cardioversion",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073636,
"choiceText": "Transvenous pacing",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073638,
"choiceText": "Intravenous potassium",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073640,
"choiceText": "Intravenous magnesium sulfate",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073642,
"choiceText": "Intravenous isoproterenol",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Immediate treatment for patients who develop torsades can be categorized into pharmacologic and nonpharmacologic approaches. Intravenous magnesium sulfate (2-g bolus followed by an infusion of 2-4 mg/min) is the initial therapy, regardless of the serum levels of magnesium.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 339969,
"questionText": "Which is the best initial therapy for torsade de pointes without hemodynamic instability for the same patient described in the above question?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Seizures in a 42-Year-Old Who Left a Hospital Against Advice"
},
{
"authors": "Alfredo Musumeci, MD, PhD; Michele Alzetta, MD",
"content": [],
"date": "December 14, 2021",
"figures": [],
"markdown": "# Seizures in a 42-Year-Old Who Left a Hospital Against Advice\n\n **Authors:** Alfredo Musumeci, MD, PhD; Michele Alzetta, MD \n **Date:** December 14, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1073624,
"choiceText": "A 63-year-old woman with a 2-day history of vomiting and watery diarrhea",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073626,
"choiceText": "A 38-year-old man with a history of schizophrenia recently treated with erythromycin for a sinus infection",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073628,
"choiceText": "A 58-year-old man status post-percutaneous coronary intervention initiated on clopidogrel and atorvastatin",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073630,
"choiceText": "A 23-year-old woman deeply intoxicated after binge drinking",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073632,
"choiceText": "A 45-year-old diabetic woman with a blood glucose of 458 mg/dL (25.4 mmol/L) and no urine ketones\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Acquired QT interval prolongation may be drug-induced, or it may be caused by certain electrolyte derangements, such as hypomagnesemia, hypokalemia, and hypocalcemia. Many drugs have been implicated, including class 1A antiarrhythmic drugs such as quinidine and procainamide and class III antiarrhythmics such as amiodarone and sotalol. Other drugs that have been implicated include antihistamines (terfenadine, astemizole), macrolide antibiotics (erythromycin, clarithromycin, clindamycin), pentamidine, serotonin receptor antagonists (ketanserin), diuretics (indapamide), certain fluoroquinolone antibiotics, tricyclic antidepressants, antipsychotics (phenothiazines, haloperidol, mesoridazine, pimozide, thioridazine, ziprasidone), gastrointestinal motility enhancers (cisapride, domperidone), inotropes (amrinone, milrinone), toxins (organophosphates, arsenic), protease inhibitors, and methadone.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 339967,
"questionText": "A patient presents to the ED after a syncopal episode and is found to have a prolonged QT interval; subsequently, the patient develops torsade de pointes. Which clinical scenario is most likely to result in this condition?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1073634,
"choiceText": "Unsynchronized cardioversion",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073636,
"choiceText": "Transvenous pacing",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073638,
"choiceText": "Intravenous potassium",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073640,
"choiceText": "Intravenous magnesium sulfate",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073642,
"choiceText": "Intravenous isoproterenol",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Immediate treatment for patients who develop torsades can be categorized into pharmacologic and nonpharmacologic approaches. Intravenous magnesium sulfate (2-g bolus followed by an infusion of 2-4 mg/min) is the initial therapy, regardless of the serum levels of magnesium.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 339969,
"questionText": "Which is the best initial therapy for torsade de pointes without hemodynamic instability for the same patient described in the above question?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Seizures in a 42-Year-Old Who Left a Hospital Against Advice"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1073616,
"choiceText": "Supraventricular tachycardia (SVT)\r\n",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073618,
"choiceText": "Torsade de pointes",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073620,
"choiceText": "Ventricular fibrillation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073622,
"choiceText": "SVT with aberrancy\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 339965,
"questionText": "Which rhythm is being demonstrated in Figure 2?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1073624,
"choiceText": "A 63-year-old woman with a 2-day history of vomiting and watery diarrhea",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073626,
"choiceText": "A 38-year-old man with a history of schizophrenia recently treated with erythromycin for a sinus infection",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073628,
"choiceText": "A 58-year-old man status post-percutaneous coronary intervention initiated on clopidogrel and atorvastatin",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073630,
"choiceText": "A 23-year-old woman deeply intoxicated after binge drinking",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073632,
"choiceText": "A 45-year-old diabetic woman with a blood glucose of 458 mg/dL (25.4 mmol/L) and no urine ketones\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Acquired QT interval prolongation may be drug-induced, or it may be caused by certain electrolyte derangements, such as hypomagnesemia, hypokalemia, and hypocalcemia. Many drugs have been implicated, including class 1A antiarrhythmic drugs such as quinidine and procainamide and class III antiarrhythmics such as amiodarone and sotalol. Other drugs that have been implicated include antihistamines (terfenadine, astemizole), macrolide antibiotics (erythromycin, clarithromycin, clindamycin), pentamidine, serotonin receptor antagonists (ketanserin), diuretics (indapamide), certain fluoroquinolone antibiotics, tricyclic antidepressants, antipsychotics (phenothiazines, haloperidol, mesoridazine, pimozide, thioridazine, ziprasidone), gastrointestinal motility enhancers (cisapride, domperidone), inotropes (amrinone, milrinone), toxins (organophosphates, arsenic), protease inhibitors, and methadone.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 339967,
"questionText": "A patient presents to the ED after a syncopal episode and is found to have a prolonged QT interval; subsequently, the patient develops torsade de pointes. Which clinical scenario is most likely to result in this condition?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1073634,
"choiceText": "Unsynchronized cardioversion",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073636,
"choiceText": "Transvenous pacing",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073638,
"choiceText": "Intravenous potassium",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073640,
"choiceText": "Intravenous magnesium sulfate",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1073642,
"choiceText": "Intravenous isoproterenol",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Immediate treatment for patients who develop torsades can be categorized into pharmacologic and nonpharmacologic approaches. Intravenous magnesium sulfate (2-g bolus followed by an infusion of 2-4 mg/min) is the initial therapy, regardless of the serum levels of magnesium.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 339969,
"questionText": "Which is the best initial therapy for torsade de pointes without hemodynamic instability for the same patient described in the above question?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
882078 | /viewarticle/882078 | [
{
"authors": "Gerard J. Fitzmaurice, BSc, MBBCh BAO; Robin Brown, MD, FRCS; Mark E. O'Donnell, DSEM, MFSEM, MRCS; Fionnuala Mone, MBBCh BAO; Angela McGreevy, MBBCh BAO",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 27-year-old man presents to the emergency department with a 2-day history of hyperemesis followed by episodes of hematemesis. He is experiencing worsening epigastric pain, diarrhea, and myalgia. The patient also describes night sweats and rigors. No melena or hematochezia is reported.",
"The patient is a binge drinker and consumed approximately 21 cans of beer 3 days ago. The patient's relevant medical history includes esophagitis, which was diagnosed last year and was treated with a long-term proton pump inhibitor. He has no known drug allergies and has not taken any other medications recently. He does not use any illegal substances.",
"He has a significant family history of hypertrophic obstructive cardiomyopathy. He works as a laborer and has smoked 10 cigarettes a day for the past 6 years. Soon after presenting in the emergency department, the patient collapses."
],
"date": "November 30, 2021",
"figures": [],
"markdown": "# After Drinking 21 Beers, a 27-Year-Old Can’t Stop Vomiting\n\n **Authors:** Gerard J. Fitzmaurice, BSc, MBBCh BAO; Robin Brown, MD, FRCS; Mark E. O'Donnell, DSEM, MFSEM, MRCS; Fionnuala Mone, MBBCh BAO; Angela McGreevy, MBBCh BAO \n **Date:** November 30, 2021\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 27-year-old man presents to the emergency department with a 2-day history of hyperemesis followed by episodes of hematemesis. He is experiencing worsening epigastric pain, diarrhea, and myalgia. The patient also describes night sweats and rigors. No melena or hematochezia is reported.\nThe patient is a binge drinker and consumed approximately 21 cans of beer 3 days ago. The patient's relevant medical history includes esophagitis, which was diagnosed last year and was treated with a long-term proton pump inhibitor. He has no known drug allergies and has not taken any other medications recently. He does not use any illegal substances.\nHe has a significant family history of hypertrophic obstructive cardiomyopathy. He works as a laborer and has smoked 10 cigarettes a day for the past 6 years. Soon after presenting in the emergency department, the patient collapses.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "After Drinking 21 Beers, a 27-Year-Old Can’t Stop Vomiting"
},
{
"authors": "Gerard J. Fitzmaurice, BSc, MBBCh BAO; Robin Brown, MD, FRCS; Mark E. O'Donnell, DSEM, MFSEM, MRCS; Fionnuala Mone, MBBCh BAO; Angela McGreevy, MBBCh BAO",
"content": [
"Upon physical examination, the patient has a temperature of 99.5°F (37.5°C). He is in sinus tachycardia, with a heart rate of 130 beats/min, and his blood pressure is 118/82 mm Hg. The patient is severely dehydrated and agitated, with tenderness to palpation noted in the upper chest and neck. The lungs are clear to auscultation, and heart sounds S1 and S2 are heard, with no murmurs or added sounds. His abdomen is soft, with a tender epigastrium.",
"The initial work-up includes laboratory investigations. The clinically significant results are as follows:",
"White blood cell count: 17.9 × 103 cells/µL (reference range, 4-11 x 103 cells/µL)",
"Sodium level: 147 mEq/L (reference range, 135-145 mEq/L)",
"Potassium level: 2.6 mEq/L (reference range, 3.5-5 mEq/L)",
"Blood urea nitrogen level: 14.5 mg/dL (reference range, 7-19 mg/dL)",
"Creatinine level: 1.71 mg/dL (reference range, 0.8-1.7 mg/dL)",
"Liver function test results are slightly deranged, with the main abnormality being an increased gamma-glutamyltransferase level of 716 U/L (reference range, 11-51 U/L). An ECG is performed and shows a prolonged QT interval, with ST depression in the inferior and anterolateral leads.",
"The patient is diagnosed with multiorgan failure caused by sepsis, and he is transferred to the high-dependency unit. He is treated with vigorous fluid resuscitation and broad-spectrum intravenous (IV) antibiotics. Further probing of the history reveals that he has vomited 30 times in the past 24 hours.",
"An erect posteroanterior chest radiograph is urgently obtained (Figure 1). An abnormality on the chest radiograph prompts CT of the chest (Figure 2) and the abdomen (not pictured).",
"Figure 1.",
"Figure 2."
],
"date": "November 30, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/882/078/882078-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/882/078/882078-Thumb2.png"
}
],
"markdown": "# After Drinking 21 Beers, a 27-Year-Old Can’t Stop Vomiting\n\n **Authors:** Gerard J. Fitzmaurice, BSc, MBBCh BAO; Robin Brown, MD, FRCS; Mark E. O'Donnell, DSEM, MFSEM, MRCS; Fionnuala Mone, MBBCh BAO; Angela McGreevy, MBBCh BAO \n **Date:** November 30, 2021\n\n ## Content\n\n Upon physical examination, the patient has a temperature of 99.5°F (37.5°C). He is in sinus tachycardia, with a heart rate of 130 beats/min, and his blood pressure is 118/82 mm Hg. The patient is severely dehydrated and agitated, with tenderness to palpation noted in the upper chest and neck. The lungs are clear to auscultation, and heart sounds S1 and S2 are heard, with no murmurs or added sounds. His abdomen is soft, with a tender epigastrium.\nThe initial work-up includes laboratory investigations. The clinically significant results are as follows:\nWhite blood cell count: 17.9 × 103 cells/µL (reference range, 4-11 x 103 cells/µL)\nSodium level: 147 mEq/L (reference range, 135-145 mEq/L)\nPotassium level: 2.6 mEq/L (reference range, 3.5-5 mEq/L)\nBlood urea nitrogen level: 14.5 mg/dL (reference range, 7-19 mg/dL)\nCreatinine level: 1.71 mg/dL (reference range, 0.8-1.7 mg/dL)\nLiver function test results are slightly deranged, with the main abnormality being an increased gamma-glutamyltransferase level of 716 U/L (reference range, 11-51 U/L). An ECG is performed and shows a prolonged QT interval, with ST depression in the inferior and anterolateral leads.\nThe patient is diagnosed with multiorgan failure caused by sepsis, and he is transferred to the high-dependency unit. He is treated with vigorous fluid resuscitation and broad-spectrum intravenous (IV) antibiotics. Further probing of the history reveals that he has vomited 30 times in the past 24 hours.\nAn erect posteroanterior chest radiograph is urgently obtained (Figure 1). An abnormality on the chest radiograph prompts CT of the chest (Figure 2) and the abdomen (not pictured).\nFigure 1.\nFigure 2.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1115308,
"choiceText": "Pneumothorax",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115310,
"choiceText": "Boerhaave syndrome",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115312,
"choiceText": "Mallory-Weiss syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115314,
"choiceText": "Aortic dissection",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353489,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": true,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "After Drinking 21 Beers, a 27-Year-Old Can’t Stop Vomiting"
},
{
"authors": "Gerard J. Fitzmaurice, BSc, MBBCh BAO; Robin Brown, MD, FRCS; Mark E. O'Donnell, DSEM, MFSEM, MRCS; Fionnuala Mone, MBBCh BAO; Angela McGreevy, MBBCh BAO",
"content": [
"This 27-year-old man presented in an acutely deteriorating state and was quickly diagnosed with multiorgan failure caused by underlying sepsis. The erect chest radiograph was a key diagnostic tool in this case because it demonstrated air along the left heart border and the aortic knob, representing pneumomediastinum and/or pneumopericardiac air (Figure 1). This finding led to urgent CT of the chest and abdomen, which found free air within the mediastinum and the pericardial sac (Figure 2).",
"Figure 1.",
"Figure 2.",
"The patient then underwent a contrast-enhanced swallow study (not available), which failed to demonstrate a patent esophageal leak, thus indicating that the rupture had probably occurred earlier.",
"Boerhaave syndrome, or spontaneous esophageal rupture, is a rare but serious condition with a mortality rate ranging from 25% to 89%. If treatment is instituted within 24 hours of the appearance of symptoms, the mortality rate is 25%; however, mortality rates rise to greater than 65% after 24 hours without treatment and 75%-89% after 48 hours without treatment.[1]",
"The syndrome is characterized by a complete transmural rupture of the esophagus resulting from barogenic trauma (ie, forceful vomiting).[2] A sudden rise in intraluminal pressure caused by uncoordinated vomiting with pyloric closure and diaphragmatic contraction against a contracted cricopharyngeal muscle is theorized to be the underlying cause of Boerhaave syndrome.[3] Perforation usually occurs at the weakest point of the esophagus; therefore, the most common site of rupture is the left posterolateral wall of the lower third of the esophagus. This is seen in 90% of patients.[4]",
"Although Boerhaave syndrome is relatively rare (accounting for only 16% of all traumatic ruptures of the esophagus), it has been associated with a heterogeneous population, affecting all races worldwide.[2,3] An association has been noted between overindulgence in alcohol and food, as is expected from a condition that is associated with vomiting.[3] Boerhaave syndrome has a significantly increased incidence in men compared with women, with a ratio of approximately 2:1.[3] It is also more common in middle-aged individuals; 80% of patients are middle-aged men.[3] Despite this, studies consistently report that Boerhaave syndrome affects all age groups, from neonates to those aged 90 years.[2,3]"
],
"date": "November 30, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/882/078/882078-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/882/078/882078-Thumb2.png"
}
],
"markdown": "# After Drinking 21 Beers, a 27-Year-Old Can’t Stop Vomiting\n\n **Authors:** Gerard J. Fitzmaurice, BSc, MBBCh BAO; Robin Brown, MD, FRCS; Mark E. O'Donnell, DSEM, MFSEM, MRCS; Fionnuala Mone, MBBCh BAO; Angela McGreevy, MBBCh BAO \n **Date:** November 30, 2021\n\n ## Content\n\n This 27-year-old man presented in an acutely deteriorating state and was quickly diagnosed with multiorgan failure caused by underlying sepsis. The erect chest radiograph was a key diagnostic tool in this case because it demonstrated air along the left heart border and the aortic knob, representing pneumomediastinum and/or pneumopericardiac air (Figure 1). This finding led to urgent CT of the chest and abdomen, which found free air within the mediastinum and the pericardial sac (Figure 2).\nFigure 1.\nFigure 2.\nThe patient then underwent a contrast-enhanced swallow study (not available), which failed to demonstrate a patent esophageal leak, thus indicating that the rupture had probably occurred earlier.\nBoerhaave syndrome, or spontaneous esophageal rupture, is a rare but serious condition with a mortality rate ranging from 25% to 89%. If treatment is instituted within 24 hours of the appearance of symptoms, the mortality rate is 25%; however, mortality rates rise to greater than 65% after 24 hours without treatment and 75%-89% after 48 hours without treatment.[1]\nThe syndrome is characterized by a complete transmural rupture of the esophagus resulting from barogenic trauma (ie, forceful vomiting).[2] A sudden rise in intraluminal pressure caused by uncoordinated vomiting with pyloric closure and diaphragmatic contraction against a contracted cricopharyngeal muscle is theorized to be the underlying cause of Boerhaave syndrome.[3] Perforation usually occurs at the weakest point of the esophagus; therefore, the most common site of rupture is the left posterolateral wall of the lower third of the esophagus. This is seen in 90% of patients.[4]\nAlthough Boerhaave syndrome is relatively rare (accounting for only 16% of all traumatic ruptures of the esophagus), it has been associated with a heterogeneous population, affecting all races worldwide.[2,3] An association has been noted between overindulgence in alcohol and food, as is expected from a condition that is associated with vomiting.[3] Boerhaave syndrome has a significantly increased incidence in men compared with women, with a ratio of approximately 2:1.[3] It is also more common in middle-aged individuals; 80% of patients are middle-aged men.[3] Despite this, studies consistently report that Boerhaave syndrome affects all age groups, from neonates to those aged 90 years.[2,3]\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1115308,
"choiceText": "Pneumothorax",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115310,
"choiceText": "Boerhaave syndrome",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115312,
"choiceText": "Mallory-Weiss syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115314,
"choiceText": "Aortic dissection",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353489,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": true,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "After Drinking 21 Beers, a 27-Year-Old Can’t Stop Vomiting"
},
{
"authors": "Gerard J. Fitzmaurice, BSc, MBBCh BAO; Robin Brown, MD, FRCS; Mark E. O'Donnell, DSEM, MFSEM, MRCS; Fionnuala Mone, MBBCh BAO; Angela McGreevy, MBBCh BAO",
"content": [
"The clinical presentation of Boerhaave syndrome typically includes a history of nausea and vomiting, followed by severe lower thoracic and epigastric pain. The pain may radiate to the back or to the left shoulder, and it may be worsened by swallowing. Hematemesis is typically not a symptom with esophageal rupture, and this can help to differentiate it from a Mallory-Weiss tear. Shortness of breath can also be a common symptom, resulting from pleuritic chest pain or a pleural effusion.[3]",
"The Mackler triad is the classic presentation of vomiting, lower chest pain, and subcutaneous emphysema that is seen in Boerhaave syndrome[2,3]; however, this sign is seen only in approximately one half of patients at the initial presentation (typically in those who present later).[3] Other classic findings include tachypnea and abdominal rigidity.[3] Atypical findings include peripheral cyanosis, hoarseness caused by involvement of the recurrent laryngeal nerve, tracheal shift, cervical vein distention, and proptosis.[3] Nonspecific findings include tachycardia, diaphoresis, fever, and hypotension, especially as the condition evolves.[3]",
"The Hamman crunch, a crackling sound heard on upon auscultation of the chest, demonstrates pneumomediastinum and can be present in 20% of patients.[3] More advanced stages of rupture typically present as sepsis with progression toward multiorgan failure.[3] Despite these symptoms and signs, the clinical presentation can vary, and often the classic triad of symptoms and signs (ie, the Mackler triad) can be absent, which can make establishing the diagnosis difficult.[5,6,7] This multitude of presenting symptoms and clinical signs leads to a wide differential diagnosis, including acute coronary syndrome, aortic dissection, Mallory-Weiss tear, pericarditis, acute pancreatitis, and spontaneous pneumothorax.[3]",
"The initial workup should involve basic laboratory investigations; however, these tests are often nonspecific and may simply show elevated inflammatory markers and, perhaps, deranged liver function (in keeping with significant alcohol intake). An early ECG is mandatory to exclude myocardial infarction. Erect chest radiography is the initial radiographic investigation; as many as 90% of patients have an abnormal finding after esophageal perforation.[2,3]",
"The most common abnormality is a unilateral pleural effusion (usually on the left side), which reflects the fact that most ruptures affect the left lower esophagus.[3] Other findings can include pneumothorax, hydropneumothorax, pneumomediastinum, subcutaneous emphysema, or mediastinal widening.[3]",
"CT scanning allows visualization of the surrounding structures to assist with the elimination of other diagnoses, and it can demonstrate periesophageal air, which can be suggestive of a perforation[2,3]; however, the mainstay of investigation used to determine the exact location and size of an esophageal perforation is an esophageal swallow or esophagraphy with, preferably, water-soluble contrast.[8,9] Esophagraphy has a sensitivity of as much as 90%; however, it also has a false-negative result in as many as 20% of cases.[3]"
],
"date": "November 30, 2021",
"figures": [],
"markdown": "# After Drinking 21 Beers, a 27-Year-Old Can’t Stop Vomiting\n\n **Authors:** Gerard J. Fitzmaurice, BSc, MBBCh BAO; Robin Brown, MD, FRCS; Mark E. O'Donnell, DSEM, MFSEM, MRCS; Fionnuala Mone, MBBCh BAO; Angela McGreevy, MBBCh BAO \n **Date:** November 30, 2021\n\n ## Content\n\n The clinical presentation of Boerhaave syndrome typically includes a history of nausea and vomiting, followed by severe lower thoracic and epigastric pain. The pain may radiate to the back or to the left shoulder, and it may be worsened by swallowing. Hematemesis is typically not a symptom with esophageal rupture, and this can help to differentiate it from a Mallory-Weiss tear. Shortness of breath can also be a common symptom, resulting from pleuritic chest pain or a pleural effusion.[3]\nThe Mackler triad is the classic presentation of vomiting, lower chest pain, and subcutaneous emphysema that is seen in Boerhaave syndrome[2,3]; however, this sign is seen only in approximately one half of patients at the initial presentation (typically in those who present later).[3] Other classic findings include tachypnea and abdominal rigidity.[3] Atypical findings include peripheral cyanosis, hoarseness caused by involvement of the recurrent laryngeal nerve, tracheal shift, cervical vein distention, and proptosis.[3] Nonspecific findings include tachycardia, diaphoresis, fever, and hypotension, especially as the condition evolves.[3]\nThe Hamman crunch, a crackling sound heard on upon auscultation of the chest, demonstrates pneumomediastinum and can be present in 20% of patients.[3] More advanced stages of rupture typically present as sepsis with progression toward multiorgan failure.[3] Despite these symptoms and signs, the clinical presentation can vary, and often the classic triad of symptoms and signs (ie, the Mackler triad) can be absent, which can make establishing the diagnosis difficult.[5,6,7] This multitude of presenting symptoms and clinical signs leads to a wide differential diagnosis, including acute coronary syndrome, aortic dissection, Mallory-Weiss tear, pericarditis, acute pancreatitis, and spontaneous pneumothorax.[3]\nThe initial workup should involve basic laboratory investigations; however, these tests are often nonspecific and may simply show elevated inflammatory markers and, perhaps, deranged liver function (in keeping with significant alcohol intake). An early ECG is mandatory to exclude myocardial infarction. Erect chest radiography is the initial radiographic investigation; as many as 90% of patients have an abnormal finding after esophageal perforation.[2,3]\nThe most common abnormality is a unilateral pleural effusion (usually on the left side), which reflects the fact that most ruptures affect the left lower esophagus.[3] Other findings can include pneumothorax, hydropneumothorax, pneumomediastinum, subcutaneous emphysema, or mediastinal widening.[3]\nCT scanning allows visualization of the surrounding structures to assist with the elimination of other diagnoses, and it can demonstrate periesophageal air, which can be suggestive of a perforation[2,3]; however, the mainstay of investigation used to determine the exact location and size of an esophageal perforation is an esophageal swallow or esophagraphy with, preferably, water-soluble contrast.[8,9] Esophagraphy has a sensitivity of as much as 90%; however, it also has a false-negative result in as many as 20% of cases.[3]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "After Drinking 21 Beers, a 27-Year-Old Can’t Stop Vomiting"
},
{
"authors": "Gerard J. Fitzmaurice, BSc, MBBCh BAO; Robin Brown, MD, FRCS; Mark E. O'Donnell, DSEM, MFSEM, MRCS; Fionnuala Mone, MBBCh BAO; Angela McGreevy, MBBCh BAO",
"content": [
"Immediate medical management involves stabilizing the patient with IV fluid resuscitation, nasogastric suction, broad-spectrum antibiotics, and narcotic analgesics.[3]",
"Options for treatment of Boerhaave syndrome include conservative management or surgical intervention. Unfortunately, a delay between the onset of symptoms and presentation and diagnosis is typical.[2] Clinical features that support conservative therapy include an absence of clinical signs of infection; a contained perforation in the mediastinum and the visceral pleura, without penetration to another body cavity; and a perforation with the contrast medium draining back into the esophagus.",
"Some experts believe that if treatment is instituted more than 24 hours after the perforation, the mode of treatment does not influence the outcome and can therefore be conservative management, placement of a tube thoracostomy (drainage), repair, or diversion. Conservative management involves administration of IV fluids and broad-spectrum antibiotics, nasogastric suction, keeping the patient NPO, and early nutritional support (jejunostomy feeding is favored).[2,3]",
"Surgical intervention is favored when the diagnosis is made early (within the first 24 hours after perforation).[2,10] Surgical techniques used for treating esophageal rupture include the following:",
"Tube thoracostomy (drainage with a chest tube or operative drainage alone)",
"Primary repair",
"Primary repair with reinforcement (pleura, intercostal muscle, diaphragm, pericardial fat, pleural flap)",
"Diversion",
"Diversion and exclusion",
"Esophageal resection",
"Thoracoscopic repair",
"Esophageal stent",
"Endoscopic placement of fibrin sealant",
"Possible complications of surgical intervention include leaks, sepsis, respiratory failure, mediastinitis, shock, empyema formation, esophagotracheal/esophagobronchial fistula formation, and death.[3]",
"As previously stated, in Boerhaave syndrome the prognosis is directly related to the time to diagnosis and appropriate intervention. Intervention within 24 hours of symptoms has a survival rate of 75%; this rate drops to 35% with a 24-hour delay, then to 11%-25% if diagnosis and treatment are delayed by 48 hours.[3]",
"In this patient, immediate fluid resuscitation was initiated, with administration of IV cefuroxime and metronidazole. Because of the 20% false-negative rate of an initial esophagram, the study was repeated, and it again confirmed the original finding of no evidence of a leak.",
"The patient was treated conservatively with broad-spectrum IV antibiotics, kept NPO with nutritional feeding through a jejunostomy tube, and given adequate hydration through IV fluids (with urine output monitoring). He improved significantly; repeat CT of the chest demonstrated a normal mediastinum. After hospitalization for 10 days, he was discharged to home in good health."
],
"date": "November 30, 2021",
"figures": [],
"markdown": "# After Drinking 21 Beers, a 27-Year-Old Can’t Stop Vomiting\n\n **Authors:** Gerard J. Fitzmaurice, BSc, MBBCh BAO; Robin Brown, MD, FRCS; Mark E. O'Donnell, DSEM, MFSEM, MRCS; Fionnuala Mone, MBBCh BAO; Angela McGreevy, MBBCh BAO \n **Date:** November 30, 2021\n\n ## Content\n\n Immediate medical management involves stabilizing the patient with IV fluid resuscitation, nasogastric suction, broad-spectrum antibiotics, and narcotic analgesics.[3]\nOptions for treatment of Boerhaave syndrome include conservative management or surgical intervention. Unfortunately, a delay between the onset of symptoms and presentation and diagnosis is typical.[2] Clinical features that support conservative therapy include an absence of clinical signs of infection; a contained perforation in the mediastinum and the visceral pleura, without penetration to another body cavity; and a perforation with the contrast medium draining back into the esophagus.\nSome experts believe that if treatment is instituted more than 24 hours after the perforation, the mode of treatment does not influence the outcome and can therefore be conservative management, placement of a tube thoracostomy (drainage), repair, or diversion. Conservative management involves administration of IV fluids and broad-spectrum antibiotics, nasogastric suction, keeping the patient NPO, and early nutritional support (jejunostomy feeding is favored).[2,3]\nSurgical intervention is favored when the diagnosis is made early (within the first 24 hours after perforation).[2,10] Surgical techniques used for treating esophageal rupture include the following:\nTube thoracostomy (drainage with a chest tube or operative drainage alone)\nPrimary repair\nPrimary repair with reinforcement (pleura, intercostal muscle, diaphragm, pericardial fat, pleural flap)\nDiversion\nDiversion and exclusion\nEsophageal resection\nThoracoscopic repair\nEsophageal stent\nEndoscopic placement of fibrin sealant\nPossible complications of surgical intervention include leaks, sepsis, respiratory failure, mediastinitis, shock, empyema formation, esophagotracheal/esophagobronchial fistula formation, and death.[3]\nAs previously stated, in Boerhaave syndrome the prognosis is directly related to the time to diagnosis and appropriate intervention. Intervention within 24 hours of symptoms has a survival rate of 75%; this rate drops to 35% with a 24-hour delay, then to 11%-25% if diagnosis and treatment are delayed by 48 hours.[3]\nIn this patient, immediate fluid resuscitation was initiated, with administration of IV cefuroxime and metronidazole. Because of the 20% false-negative rate of an initial esophagram, the study was repeated, and it again confirmed the original finding of no evidence of a leak.\nThe patient was treated conservatively with broad-spectrum IV antibiotics, kept NPO with nutritional feeding through a jejunostomy tube, and given adequate hydration through IV fluids (with urine output monitoring). He improved significantly; repeat CT of the chest demonstrated a normal mediastinum. After hospitalization for 10 days, he was discharged to home in good health.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1115332,
"choiceText": "Hematemesis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115334,
"choiceText": "Severe lower abdominal pain",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115336,
"choiceText": "Vomiting",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115338,
"choiceText": "Diarrhea",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115340,
"choiceText": "Bradypnea",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The clinical presentation of Boerhaave syndrome typically includes a history of vomiting, followed by severe lower thoracic and epigastric pain. The pain may radiate to the back or to the left shoulder, and it may be worsened by swallowing. Hematemesis is typically not a symptom with esophageal rupture, and this can help to differentiate it from a Mallory-Weiss tear.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353495,
"questionText": "Which is a common symptom associated with Boerhaave syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": true,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1115350,
"choiceText": "Pneumothorax",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115352,
"choiceText": "Pneumomediastinum",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115354,
"choiceText": "Unilateral pleural effusion, usually left-sided",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115356,
"choiceText": "Mediastinal widening",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115358,
"choiceText": "Subcutaneous emphysema",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Erect chest radiography is the initial radiographic investigation; as many as 90% of patients have an abnormal finding following an esophageal perforation. The most common abnormality is a unilateral pleural effusion (usually on the left side), which reflects the fact that most ruptures affect the left lower esophagus.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353499,
"questionText": "Which is the most common finding on an erect posteroanterior chest radiograph after esophageal rupture?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": true,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "After Drinking 21 Beers, a 27-Year-Old Can’t Stop Vomiting"
},
{
"authors": "Gerard J. Fitzmaurice, BSc, MBBCh BAO; Robin Brown, MD, FRCS; Mark E. O'Donnell, DSEM, MFSEM, MRCS; Fionnuala Mone, MBBCh BAO; Angela McGreevy, MBBCh BAO",
"content": [],
"date": "November 30, 2021",
"figures": [],
"markdown": "# After Drinking 21 Beers, a 27-Year-Old Can’t Stop Vomiting\n\n **Authors:** Gerard J. Fitzmaurice, BSc, MBBCh BAO; Robin Brown, MD, FRCS; Mark E. O'Donnell, DSEM, MFSEM, MRCS; Fionnuala Mone, MBBCh BAO; Angela McGreevy, MBBCh BAO \n **Date:** November 30, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1115332,
"choiceText": "Hematemesis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115334,
"choiceText": "Severe lower abdominal pain",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115336,
"choiceText": "Vomiting",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115338,
"choiceText": "Diarrhea",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115340,
"choiceText": "Bradypnea",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The clinical presentation of Boerhaave syndrome typically includes a history of vomiting, followed by severe lower thoracic and epigastric pain. The pain may radiate to the back or to the left shoulder, and it may be worsened by swallowing. Hematemesis is typically not a symptom with esophageal rupture, and this can help to differentiate it from a Mallory-Weiss tear.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353495,
"questionText": "Which is a common symptom associated with Boerhaave syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": true,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1115350,
"choiceText": "Pneumothorax",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115352,
"choiceText": "Pneumomediastinum",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115354,
"choiceText": "Unilateral pleural effusion, usually left-sided",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115356,
"choiceText": "Mediastinal widening",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115358,
"choiceText": "Subcutaneous emphysema",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Erect chest radiography is the initial radiographic investigation; as many as 90% of patients have an abnormal finding following an esophageal perforation. The most common abnormality is a unilateral pleural effusion (usually on the left side), which reflects the fact that most ruptures affect the left lower esophagus.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353499,
"questionText": "Which is the most common finding on an erect posteroanterior chest radiograph after esophageal rupture?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": true,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "After Drinking 21 Beers, a 27-Year-Old Can’t Stop Vomiting"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1115308,
"choiceText": "Pneumothorax",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115310,
"choiceText": "Boerhaave syndrome",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115312,
"choiceText": "Mallory-Weiss syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115314,
"choiceText": "Aortic dissection",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353489,
"questionText": "On the basis of only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": true,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1115332,
"choiceText": "Hematemesis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115334,
"choiceText": "Severe lower abdominal pain",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115336,
"choiceText": "Vomiting",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115338,
"choiceText": "Diarrhea",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115340,
"choiceText": "Bradypnea",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The clinical presentation of Boerhaave syndrome typically includes a history of vomiting, followed by severe lower thoracic and epigastric pain. The pain may radiate to the back or to the left shoulder, and it may be worsened by swallowing. Hematemesis is typically not a symptom with esophageal rupture, and this can help to differentiate it from a Mallory-Weiss tear.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353495,
"questionText": "Which is a common symptom associated with Boerhaave syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": true,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1115350,
"choiceText": "Pneumothorax",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115352,
"choiceText": "Pneumomediastinum",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115354,
"choiceText": "Unilateral pleural effusion, usually left-sided",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115356,
"choiceText": "Mediastinal widening",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1115358,
"choiceText": "Subcutaneous emphysema",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Erect chest radiography is the initial radiographic investigation; as many as 90% of patients have an abnormal finding following an esophageal perforation. The most common abnormality is a unilateral pleural effusion (usually on the left side), which reflects the fact that most ruptures affect the left lower esophagus.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 353499,
"questionText": "Which is the most common finding on an erect posteroanterior chest radiograph after esophageal rupture?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": true,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
832279 | /viewarticle/832279 | [
{
"authors": "Dora E. Izaguirre, MD; Jesus Lanza, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 47-year-old man with no history of significant illness presents to his primary care physician with progressive dyspnea over the past two years. According to the patient, his dyspnea worsens with exertion. He has an associated intermittent productive cough with yellowish sputum that has responded to a short course of antibiotics in the past. No associated chest pain, hemoptysis, fever, night sweats, or weight loss is reported.",
"Upon initial presentation to his primary care physician at the time of symptom onset, the patient was prescribed albuterol for possible asthma, which resulted in mild improvement of his symptoms. His shortness of breath has recently gotten worse, to the point that he is limited to light activities around the house; he previously played golf on the weekends. His family history includes other members with similar symptoms and \"liver problems.\" He previously smoked one pack of cigarettes a week for the past 10 years but quit six months ago. He does not drink alcohol in excess and does not use illicit drugs. He does not take any medications or vitamin supplements."
],
"date": "November 19, 2021",
"figures": [],
"markdown": "# A 47-Year-Old With Progressive Dyspnea and Weepy Nodules\n\n **Authors:** Dora E. Izaguirre, MD; Jesus Lanza, MD \n **Date:** November 19, 2021\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 47-year-old man with no history of significant illness presents to his primary care physician with progressive dyspnea over the past two years. According to the patient, his dyspnea worsens with exertion. He has an associated intermittent productive cough with yellowish sputum that has responded to a short course of antibiotics in the past. No associated chest pain, hemoptysis, fever, night sweats, or weight loss is reported.\nUpon initial presentation to his primary care physician at the time of symptom onset, the patient was prescribed albuterol for possible asthma, which resulted in mild improvement of his symptoms. His shortness of breath has recently gotten worse, to the point that he is limited to light activities around the house; he previously played golf on the weekends. His family history includes other members with similar symptoms and \"liver problems.\" He previously smoked one pack of cigarettes a week for the past 10 years but quit six months ago. He does not drink alcohol in excess and does not use illicit drugs. He does not take any medications or vitamin supplements.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A 47-Year-Old With Progressive Dyspnea and Weepy Nodules"
},
{
"authors": "Dora E. Izaguirre, MD; Jesus Lanza, MD",
"content": [
"Physical examination reveals an alert and oriented male with a regular pulse of 94 beats/min, blood pressure of 130/85 mm Hg, respiratory rate of 22 breath/min, temperature of 98.8°F, and O2 saturation of 92% on room air. The neck is supple, without jugular venous distention or lymphadenopathy. Cardiac examination reveals normal S1 and S2 findings, and no audible murmurs, rubs, or gallops are noted. Chest examination shows bilateral equal decreased air entry with scattered wheezes, but no rhonchi or rales are heard upon auscultation.",
"The abdomen is soft, nontender, and nondistended, with evidence of mild hepatomegaly. No lower-extremity edema, cyanosis, or clubbing is seen. The peripheral arterial pulses are palpable. Skin examination reveals painful and weepy cutaneous nodules on the patient's right forearm (Figure 1).",
"Figure 1.",
"Neurologic examination findings are normal. Laboratory work-up, including a complete blood count, and a comprehensive metabolic panel showed mild elevation of aminotransferases. The cytoplasmic antineutrophil cytoplasmic antibody (C-ANCA) titer was positive, and serum levels of alpha-1 antitrypsin (AAT) were 10 µmol/L (reference range, 20-60 µmol/L).",
"Pulmonary function testing revealed an FEV1 of 1.82 L (52% of predicted), with an FEV1/FVC ratio of 68%. FEV1 didn't improve with albuterol treatment (postbronchodilator increase in FEV1 of 9%). He was also found to have a reduced diffusing capacity or transfer factor of the lung for carbon monoxide (DLCO) of 17.72 mL/min/mm Hg (62% of predicted) and evidence of air trapping with a residual volume of 3.26 L (127% of predicted). Chest radiography (Figure 2) revealed hyperlucent areas in bilateral lower lobes. Chest CT is shown in Figure 3.",
"Figure 2.",
"Figure 3."
],
"date": "November 19, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/832/279/832279-thumb-1.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/832/279/832279-thumb-3.jpg"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/832/279/832279-thumb-2.jpg"
}
],
"markdown": "# A 47-Year-Old With Progressive Dyspnea and Weepy Nodules\n\n **Authors:** Dora E. Izaguirre, MD; Jesus Lanza, MD \n **Date:** November 19, 2021\n\n ## Content\n\n Physical examination reveals an alert and oriented male with a regular pulse of 94 beats/min, blood pressure of 130/85 mm Hg, respiratory rate of 22 breath/min, temperature of 98.8°F, and O2 saturation of 92% on room air. The neck is supple, without jugular venous distention or lymphadenopathy. Cardiac examination reveals normal S1 and S2 findings, and no audible murmurs, rubs, or gallops are noted. Chest examination shows bilateral equal decreased air entry with scattered wheezes, but no rhonchi or rales are heard upon auscultation.\nThe abdomen is soft, nontender, and nondistended, with evidence of mild hepatomegaly. No lower-extremity edema, cyanosis, or clubbing is seen. The peripheral arterial pulses are palpable. Skin examination reveals painful and weepy cutaneous nodules on the patient's right forearm (Figure 1).\nFigure 1.\nNeurologic examination findings are normal. Laboratory work-up, including a complete blood count, and a comprehensive metabolic panel showed mild elevation of aminotransferases. The cytoplasmic antineutrophil cytoplasmic antibody (C-ANCA) titer was positive, and serum levels of alpha-1 antitrypsin (AAT) were 10 µmol/L (reference range, 20-60 µmol/L).\nPulmonary function testing revealed an FEV1 of 1.82 L (52% of predicted), with an FEV1/FVC ratio of 68%. FEV1 didn't improve with albuterol treatment (postbronchodilator increase in FEV1 of 9%). He was also found to have a reduced diffusing capacity or transfer factor of the lung for carbon monoxide (DLCO) of 17.72 mL/min/mm Hg (62% of predicted) and evidence of air trapping with a residual volume of 3.26 L (127% of predicted). Chest radiography (Figure 2) revealed hyperlucent areas in bilateral lower lobes. Chest CT is shown in Figure 3.\nFigure 2.\nFigure 3.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 774277,
"choiceText": "Autoimmune hepatitis (AIH)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774279,
"choiceText": "Chronic bronchitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774281,
"choiceText": "AAT deficiency (AATD)",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774283,
"choiceText": "Bronchiectasis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774285,
"choiceText": "Wegener granulomatosis (granulomatosis with polyangiitis)",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 242539,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 47-Year-Old With Progressive Dyspnea and Weepy Nodules"
},
{
"authors": "Dora E. Izaguirre, MD; Jesus Lanza, MD",
"content": [
"AATD should be suspected in any person who presents with early-onset emphysema or chronic obstructive pulmonary disease (COPD), regardless of his or her smoking history. In patients with AATD, liver function test results are elevated; however, this abnormality is not specific in these patients. AATD is an autosomal codominant disease; therefore, the family history of similar symptoms in this patient suggests the possibility of AATD. C-ANCA vasculitis has been systematically associated with AATD.[1]",
"This patient presented with an AAT level of 10 µmol/L. AAT levels below 11 µmol/L are consistent with AATD; however, low AAT levels alone have low sensitivity for the diagnosis of AATD.[2,3]",
"Standard pulmonary tests play an important role in determining the severity of lung disease, which is characterized by increased total lung capacity, reduced FEV1, and reduced FEV1/FVC ratio. This patient presented a FEV1 of 1.82 L (52% of predicted), with an FEV1/FVC ratio that was 68% of predicted.",
"The chest radiograph in this patient revealed hyperlucent areas in bilateral lower lobes; flattening of diaphragms may also be observed.[3] High-resolution CT (HRCT) of the chest revealed middle- and lower-lobe emphysema. In patients with mild forms of AATD, this finding may be missed on HRCT. However, in patients with moderate or severe forms of AATD, loss of lung basal parenchyma hyperlucencies are characteristic. Panacinar emphysema with predominantly lower-lobe distribution is a classic finding in patients with AATD; however, in severe forms, it might be indistinguishable from centrilobular emphysema.",
"A diagnosis of AIH is unlikely because the usual presentation is in young women with no family history of similar symptoms. In addition, in patients with AIH, serum antinuclear antibody or anti–smooth-muscle antibody findings are positive, and AAT levels and phenotype are within normal limits.",
"Chronic bronchitis is unlikely because the patient's clinical history does not include sputum production for at least three months per year for two consecutive years. In addition, AAT levels and phenotype are normal in chronic bronchitis.",
"Bronchiectasis is unlikely because patients present with a chronic history of respiratory symptoms (eg, cough with thick mucopurulent sputum production), and HRCT findings in these patients include bronchial wall thickening and luminal dilatation. In addition, AAT levels and phenotype are normal in bronchiectasis.",
"Granulomatosis with polyangiitis, previously known as \"Wegener granulomatosis,\" is unlikely because positive C-ANCA results are not specific for this diagnosis. In addition, granulomatosis with polyangiitis presents as a vasculitic syndrome that predominantly affects the kidney, lungs, and upper airway and also has blood test findings, radiographic findings, and biopsy results that differ from those in patients with AATD."
],
"date": "November 19, 2021",
"figures": [],
"markdown": "# A 47-Year-Old With Progressive Dyspnea and Weepy Nodules\n\n **Authors:** Dora E. Izaguirre, MD; Jesus Lanza, MD \n **Date:** November 19, 2021\n\n ## Content\n\n AATD should be suspected in any person who presents with early-onset emphysema or chronic obstructive pulmonary disease (COPD), regardless of his or her smoking history. In patients with AATD, liver function test results are elevated; however, this abnormality is not specific in these patients. AATD is an autosomal codominant disease; therefore, the family history of similar symptoms in this patient suggests the possibility of AATD. C-ANCA vasculitis has been systematically associated with AATD.[1]\nThis patient presented with an AAT level of 10 µmol/L. AAT levels below 11 µmol/L are consistent with AATD; however, low AAT levels alone have low sensitivity for the diagnosis of AATD.[2,3]\nStandard pulmonary tests play an important role in determining the severity of lung disease, which is characterized by increased total lung capacity, reduced FEV1, and reduced FEV1/FVC ratio. This patient presented a FEV1 of 1.82 L (52% of predicted), with an FEV1/FVC ratio that was 68% of predicted.\nThe chest radiograph in this patient revealed hyperlucent areas in bilateral lower lobes; flattening of diaphragms may also be observed.[3] High-resolution CT (HRCT) of the chest revealed middle- and lower-lobe emphysema. In patients with mild forms of AATD, this finding may be missed on HRCT. However, in patients with moderate or severe forms of AATD, loss of lung basal parenchyma hyperlucencies are characteristic. Panacinar emphysema with predominantly lower-lobe distribution is a classic finding in patients with AATD; however, in severe forms, it might be indistinguishable from centrilobular emphysema.\nA diagnosis of AIH is unlikely because the usual presentation is in young women with no family history of similar symptoms. In addition, in patients with AIH, serum antinuclear antibody or anti–smooth-muscle antibody findings are positive, and AAT levels and phenotype are within normal limits.\nChronic bronchitis is unlikely because the patient's clinical history does not include sputum production for at least three months per year for two consecutive years. In addition, AAT levels and phenotype are normal in chronic bronchitis.\nBronchiectasis is unlikely because patients present with a chronic history of respiratory symptoms (eg, cough with thick mucopurulent sputum production), and HRCT findings in these patients include bronchial wall thickening and luminal dilatation. In addition, AAT levels and phenotype are normal in bronchiectasis.\nGranulomatosis with polyangiitis, previously known as \"Wegener granulomatosis,\" is unlikely because positive C-ANCA results are not specific for this diagnosis. In addition, granulomatosis with polyangiitis presents as a vasculitic syndrome that predominantly affects the kidney, lungs, and upper airway and also has blood test findings, radiographic findings, and biopsy results that differ from those in patients with AATD.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 774277,
"choiceText": "Autoimmune hepatitis (AIH)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774279,
"choiceText": "Chronic bronchitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774281,
"choiceText": "AAT deficiency (AATD)",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774283,
"choiceText": "Bronchiectasis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774285,
"choiceText": "Wegener granulomatosis (granulomatosis with polyangiitis)",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 242539,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 47-Year-Old With Progressive Dyspnea and Weepy Nodules"
},
{
"authors": "Dora E. Izaguirre, MD; Jesus Lanza, MD",
"content": [
"AATD was first described by Laurell and Eriksson in 1963.[1,4] The condition often goes undiagnosed, even though it is a relatively common genetic condition. COPD and liver disease are common in persons with AATD. Approximately 1%-5% of patients diagnosed with COPD are believed to have AATD.[5] The incidence of liver disease increases over time.",
"AATD is one of the most common genetic diseases that causes death in adult white persons. Severe AATD is found in approximately 70,000-100,000 people. At least one deficient gene is present in an estimated 25 million individuals, although fewer than 10% are identified.[1,2,4,6]",
"Specific morbidity and mortality rates are unclear. Not all individuals with homozygous deficiency display emphysema or cirrhosis, and the condition commonly goes undetected. Patients describe having symptoms for several years that were examined by multiple physicians before diagnosis. The median time between symptom presentation and diagnosis is estimated to be 8 years. Symptomatic patients have a high mortality rate.",
"Early symptoms of AATD include wheezing, intermittent cough, and sputum production. Dyspnea in AATD is initially evident only with high exertion. Eventually, the condition limits even milder exertion.",
"Dyspnea develops 20-30 years earlier in individuals with AATD than in individuals who smoke. Smoking accelerates emphysema progression in AATD; symptoms are evident 10 years earlier in individuals with AATD who smoke regularly. Infections and exposure to dust or fumes can also increase the onset of symptoms or worsen disease progression.",
"AATD emphysema cannot be confirmed by a single physical sign, and most signs associated with emphysema from any cause are easily missed. Individuals with unexplained liver disease should be investigated for AATD, regardless of whether respiratory symptoms are present. Chronic liver disease and panniculitis must be investigated. Hepatomegaly is not specific for AATD but may also be present.",
"Elevated levels of bilirubin, aspartate transaminase, and alanine aminotransferase may be observed but are nonspecific and nonsensitive for AATD. Serum levels of AAT below 11 µmol/L suggest AATD; however, this finding alone lacks the sensitivity and specificity to confirm the diagnosis.",
"Pulmonary function tests are also not sensitive or specific for AATD; however, they are important in diagnosing obstructive lung disease and determining severity of emphysema. These results typically include increased total lung capacity, reduced FEV1, reduced FVC, and reduced FEV1/FVC ratio.",
"DNA tests are used to determine specific mutations.[3] Isoelectric focusing (IEF) phenotyping is the criterion standard in the diagnosis of AATD; however, it requires complex interpretation.",
"Findings on liver histopathology have been shown to vary, depending on the classification and staging of disease. The presence of periodic acid-Schiff-positive globules may suggest AATD, but further investigation is recommended.",
"Bibasilar hyperlucent fields and flattened diaphragms are seen on chest radiography. Mild forms may be missed on HRCT; when the disease is moderate, determining the panlobular nature of the process and the characteristic lower zone predominance is possible. Severe forms can be indistinguishable from severe centrilobular emphysema. Unspecific changes related with cirrhosis or hepatocellular carcinoma may be observed on CT of the abdomen.[3]"
],
"date": "November 19, 2021",
"figures": [],
"markdown": "# A 47-Year-Old With Progressive Dyspnea and Weepy Nodules\n\n **Authors:** Dora E. Izaguirre, MD; Jesus Lanza, MD \n **Date:** November 19, 2021\n\n ## Content\n\n AATD was first described by Laurell and Eriksson in 1963.[1,4] The condition often goes undiagnosed, even though it is a relatively common genetic condition. COPD and liver disease are common in persons with AATD. Approximately 1%-5% of patients diagnosed with COPD are believed to have AATD.[5] The incidence of liver disease increases over time.\nAATD is one of the most common genetic diseases that causes death in adult white persons. Severe AATD is found in approximately 70,000-100,000 people. At least one deficient gene is present in an estimated 25 million individuals, although fewer than 10% are identified.[1,2,4,6]\nSpecific morbidity and mortality rates are unclear. Not all individuals with homozygous deficiency display emphysema or cirrhosis, and the condition commonly goes undetected. Patients describe having symptoms for several years that were examined by multiple physicians before diagnosis. The median time between symptom presentation and diagnosis is estimated to be 8 years. Symptomatic patients have a high mortality rate.\nEarly symptoms of AATD include wheezing, intermittent cough, and sputum production. Dyspnea in AATD is initially evident only with high exertion. Eventually, the condition limits even milder exertion.\nDyspnea develops 20-30 years earlier in individuals with AATD than in individuals who smoke. Smoking accelerates emphysema progression in AATD; symptoms are evident 10 years earlier in individuals with AATD who smoke regularly. Infections and exposure to dust or fumes can also increase the onset of symptoms or worsen disease progression.\nAATD emphysema cannot be confirmed by a single physical sign, and most signs associated with emphysema from any cause are easily missed. Individuals with unexplained liver disease should be investigated for AATD, regardless of whether respiratory symptoms are present. Chronic liver disease and panniculitis must be investigated. Hepatomegaly is not specific for AATD but may also be present.\nElevated levels of bilirubin, aspartate transaminase, and alanine aminotransferase may be observed but are nonspecific and nonsensitive for AATD. Serum levels of AAT below 11 µmol/L suggest AATD; however, this finding alone lacks the sensitivity and specificity to confirm the diagnosis.\nPulmonary function tests are also not sensitive or specific for AATD; however, they are important in diagnosing obstructive lung disease and determining severity of emphysema. These results typically include increased total lung capacity, reduced FEV1, reduced FVC, and reduced FEV1/FVC ratio.\nDNA tests are used to determine specific mutations.[3] Isoelectric focusing (IEF) phenotyping is the criterion standard in the diagnosis of AATD; however, it requires complex interpretation.\nFindings on liver histopathology have been shown to vary, depending on the classification and staging of disease. The presence of periodic acid-Schiff-positive globules may suggest AATD, but further investigation is recommended.\nBibasilar hyperlucent fields and flattened diaphragms are seen on chest radiography. Mild forms may be missed on HRCT; when the disease is moderate, determining the panlobular nature of the process and the characteristic lower zone predominance is possible. Severe forms can be indistinguishable from severe centrilobular emphysema. Unspecific changes related with cirrhosis or hepatocellular carcinoma may be observed on CT of the abdomen.[3]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A 47-Year-Old With Progressive Dyspnea and Weepy Nodules"
},
{
"authors": "Dora E. Izaguirre, MD; Jesus Lanza, MD",
"content": [
"Preventing or slowing the progression of lung disease is the primary focus of treatment. As such, discouraging smoking and treating asthma and respiratory infection is important.",
"Replacing or supplementing the deficient enzyme in patients with plasma AAT levels less than 11 µmol/L is recommended. Most patients are identified after they develop lung disease; the aim of treating AATD emphysema is similar to that associated with any form of emphysema. Patients who also have liver disease must be considered for potential complications.",
"Volume reduction surgery, as well as lung and liver transplantation, should be offered to patients with advanced disease who do not appropriately respond to medical management.",
"Annual pulmonary function monitoring allows for better counseling and planning for interventions, such as initiation of replacement therapy (if not already started) or transplantation. Annual influenza vaccination is recommended, as is pneumococcal vaccination every 5 years. Liver function should be periodically monitored in all individuals with the PiZZ genotype. For those with established liver disease, monitoring with ultrasonography every 6-12 months is recommended to detect fibrotic changes and carcinoma.",
"Complications in patients with AATD are similar to those in patients with COPD and emphysema associated with cigarette smoking. These include acute exacerbation of airflow obstruction, pneumothorax, pneumonia, and respiratory failure.",
"In patients with AATD that was diagnosed on screening, the prognosis is often similar to that of healthy people. In contrast, patients whose disease was diagnosed on the basis of clinical manifestations have a more limited prognosis.",
"Upon further investigation of the patient in this case, phenotype ZZ was determined. AAT replacement therapy was started. The patient's symptoms improved dramatically, and further visits have been scheduled to follow up on the evolution of his disease."
],
"date": "November 19, 2021",
"figures": [],
"markdown": "# A 47-Year-Old With Progressive Dyspnea and Weepy Nodules\n\n **Authors:** Dora E. Izaguirre, MD; Jesus Lanza, MD \n **Date:** November 19, 2021\n\n ## Content\n\n Preventing or slowing the progression of lung disease is the primary focus of treatment. As such, discouraging smoking and treating asthma and respiratory infection is important.\nReplacing or supplementing the deficient enzyme in patients with plasma AAT levels less than 11 µmol/L is recommended. Most patients are identified after they develop lung disease; the aim of treating AATD emphysema is similar to that associated with any form of emphysema. Patients who also have liver disease must be considered for potential complications.\nVolume reduction surgery, as well as lung and liver transplantation, should be offered to patients with advanced disease who do not appropriately respond to medical management.\nAnnual pulmonary function monitoring allows for better counseling and planning for interventions, such as initiation of replacement therapy (if not already started) or transplantation. Annual influenza vaccination is recommended, as is pneumococcal vaccination every 5 years. Liver function should be periodically monitored in all individuals with the PiZZ genotype. For those with established liver disease, monitoring with ultrasonography every 6-12 months is recommended to detect fibrotic changes and carcinoma.\nComplications in patients with AATD are similar to those in patients with COPD and emphysema associated with cigarette smoking. These include acute exacerbation of airflow obstruction, pneumothorax, pneumonia, and respiratory failure.\nIn patients with AATD that was diagnosed on screening, the prognosis is often similar to that of healthy people. In contrast, patients whose disease was diagnosed on the basis of clinical manifestations have a more limited prognosis.\nUpon further investigation of the patient in this case, phenotype ZZ was determined. AAT replacement therapy was started. The patient's symptoms improved dramatically, and further visits have been scheduled to follow up on the evolution of his disease.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 774287,
"choiceText": "Serum AAT levels",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774289,
"choiceText": "Chest CT",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774291,
"choiceText": "Posteroanterior and lateral chest radiography",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774293,
"choiceText": "AAT phenotype determined by IEF ",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774295,
"choiceText": "Spirometry",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Although each of these tests may contribute some information about emphysema, none is specific or sensitive for AATD. AAT levels may be falsely elevated in any inflammatory condition that involves an acute-phase protein. Therefore, the criterion standard for diagnosis of AATD is phenotype analysis using IEF.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 242541,
"questionText": "Which of these tests is considered the criterion standard for the diagnosis of AATD?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 774297,
"choiceText": "Smoking cessation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774299,
"choiceText": "AAT enzyme replacement",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774301,
"choiceText": "Influenza and pneumococcal vaccination",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774303,
"choiceText": "Liver and lung transplantation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774305,
"choiceText": "All of the above",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "All of the options mentioned constitute part of the management of AATD. In patients with advanced disease, liver and lung transplantation should be offered.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 242543,
"questionText": "Which intervention is part of long-term management of patients with AATD?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 47-Year-Old With Progressive Dyspnea and Weepy Nodules"
},
{
"authors": "Dora E. Izaguirre, MD; Jesus Lanza, MD",
"content": [],
"date": "November 19, 2021",
"figures": [],
"markdown": "# A 47-Year-Old With Progressive Dyspnea and Weepy Nodules\n\n **Authors:** Dora E. Izaguirre, MD; Jesus Lanza, MD \n **Date:** November 19, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 774287,
"choiceText": "Serum AAT levels",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774289,
"choiceText": "Chest CT",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774291,
"choiceText": "Posteroanterior and lateral chest radiography",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774293,
"choiceText": "AAT phenotype determined by IEF ",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774295,
"choiceText": "Spirometry",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Although each of these tests may contribute some information about emphysema, none is specific or sensitive for AATD. AAT levels may be falsely elevated in any inflammatory condition that involves an acute-phase protein. Therefore, the criterion standard for diagnosis of AATD is phenotype analysis using IEF.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 242541,
"questionText": "Which of these tests is considered the criterion standard for the diagnosis of AATD?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 774297,
"choiceText": "Smoking cessation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774299,
"choiceText": "AAT enzyme replacement",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774301,
"choiceText": "Influenza and pneumococcal vaccination",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774303,
"choiceText": "Liver and lung transplantation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774305,
"choiceText": "All of the above",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "All of the options mentioned constitute part of the management of AATD. In patients with advanced disease, liver and lung transplantation should be offered.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 242543,
"questionText": "Which intervention is part of long-term management of patients with AATD?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 47-Year-Old With Progressive Dyspnea and Weepy Nodules"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 774277,
"choiceText": "Autoimmune hepatitis (AIH)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774279,
"choiceText": "Chronic bronchitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774281,
"choiceText": "AAT deficiency (AATD)",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774283,
"choiceText": "Bronchiectasis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774285,
"choiceText": "Wegener granulomatosis (granulomatosis with polyangiitis)",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 242539,
"questionText": "Based on only these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 774287,
"choiceText": "Serum AAT levels",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774289,
"choiceText": "Chest CT",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774291,
"choiceText": "Posteroanterior and lateral chest radiography",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774293,
"choiceText": "AAT phenotype determined by IEF ",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774295,
"choiceText": "Spirometry",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Although each of these tests may contribute some information about emphysema, none is specific or sensitive for AATD. AAT levels may be falsely elevated in any inflammatory condition that involves an acute-phase protein. Therefore, the criterion standard for diagnosis of AATD is phenotype analysis using IEF.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 242541,
"questionText": "Which of these tests is considered the criterion standard for the diagnosis of AATD?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 774297,
"choiceText": "Smoking cessation",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774299,
"choiceText": "AAT enzyme replacement",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774301,
"choiceText": "Influenza and pneumococcal vaccination",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774303,
"choiceText": "Liver and lung transplantation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 774305,
"choiceText": "All of the above",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "All of the options mentioned constitute part of the management of AATD. In patients with advanced disease, liver and lung transplantation should be offered.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 242543,
"questionText": "Which intervention is part of long-term management of patients with AATD?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
962080 | /viewarticle/962080 | [
{
"authors": "Mark Davis, MD; Nandita Kakar",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 70-year-old man presents with a history of initial fullness in the left medial epitrochlear region that developed over approximately 2 months into a golf ball–sized mass. The mass is nontender, with no drainage. The overlying skin is normal, and the patient does not recall any trauma. He describes no other symptoms and denies fever, sweats, or weight loss, as well as any loss of muscular function or tingling, burning, or pain sensations of the left arm. The mass causes mild to no discomfort, and the patient is mainly concerned about its rapid progression.",
"He has a past medical history of familial hypercholesterolemia and gastroesophageal reflux disease (GERD) with esophagitis, which are managed with atorvastatin and omeprazole, respectively. He has never smoked tobacco or used alcohol or illicit substances. His surgical history includes a hernia repair and a tonsillectomy. He has a family history of heart disease and Alzheimer's disease."
],
"date": "November 08, 2021",
"figures": [],
"markdown": "# What's Causing This Rapidly Growing, Golf Ball–Sized Mass?\n\n **Authors:** Mark Davis, MD; Nandita Kakar \n **Date:** November 08, 2021\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 70-year-old man presents with a history of initial fullness in the left medial epitrochlear region that developed over approximately 2 months into a golf ball–sized mass. The mass is nontender, with no drainage. The overlying skin is normal, and the patient does not recall any trauma. He describes no other symptoms and denies fever, sweats, or weight loss, as well as any loss of muscular function or tingling, burning, or pain sensations of the left arm. The mass causes mild to no discomfort, and the patient is mainly concerned about its rapid progression.\nHe has a past medical history of familial hypercholesterolemia and gastroesophageal reflux disease (GERD) with esophagitis, which are managed with atorvastatin and omeprazole, respectively. He has never smoked tobacco or used alcohol or illicit substances. His surgical history includes a hernia repair and a tonsillectomy. He has a family history of heart disease and Alzheimer's disease.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "What's Causing This Rapidly Growing, Golf Ball–Sized Mass?"
},
{
"authors": "Mark Davis, MD; Nandita Kakar",
"content": [
"The patient is oriented to person, place, and time but is in acute distress in regard to the rapid development of the mass. His height is 5 ft 10 in (177.8 cm), and his weight is 216 lb (97.98 kg), with a body mass index of 31 kg/m2. His oral temperature is 98.7°F (37°C). His pulse is 80 beats/min and regular, his respiration rate is 16 breaths/min and unlabored, and his blood pressure is 112/70 mm Hg in the left upper extremity when he is seated. His oxygen saturation measured by pulse oximetry is 97% on room air.",
"Heart sounds are normal, and the rate and rhythm are regular. The lung examination reveals no dullness or hyperresonance to percussion, and breath sounds are normal across all lung fields. The abdomen is nontender, with no guarding or organomegaly, and bowel sounds are normal. A firm 4 cm × 3 cm mass is noted in the epitrochlear region of the left elbow. The extremities exhibit normal tone and motor strength, with no contractures, malalignment, tenderness, or bony abnormalities. No cyanosis, edema, or varicosities are noted in any of the extremities. Inspection and palpation of the skin reveal no abnormalities.",
"A CT scan with contrast shows a 4.0 cm × 3.1 cm soft tissue density in the medial, supracondylar region of the left arm, slightly above the elbow. The mass does not exhibit significant enhancement. It exerts a mass effect on the adjacent basilic vein with extrinsic compression. The fat planes between the mass and the underlying musculature appear preserved, with no infiltration, but some induration in the adjacent fat is noted. The surrounding soft tissue and bones appear normal. The CT scan results are highly suggestive of a soft tissue mass that probably requires pathologic examination. See the images below.",
"Figure 1.",
"Figure 2.",
"The mass is excised. The surgical pathology specimen consists of a 1.9 cm × 1.4 cm × 0.3 cm oval portion of homogeneous, glistening yellow-tan adipose tissue and a 4.4 cm × 3.7 cm × 3.2 cm oval portion of soft, gelatinous pink-gray tissue. The adipose tissue in the specimen is part of the overlying skin that was removed for appropriate closure of the incision."
],
"date": "November 08, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/962/080/962080-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/962/080/962080-Thumb2.png"
}
],
"markdown": "# What's Causing This Rapidly Growing, Golf Ball–Sized Mass?\n\n **Authors:** Mark Davis, MD; Nandita Kakar \n **Date:** November 08, 2021\n\n ## Content\n\n The patient is oriented to person, place, and time but is in acute distress in regard to the rapid development of the mass. His height is 5 ft 10 in (177.8 cm), and his weight is 216 lb (97.98 kg), with a body mass index of 31 kg/m2. His oral temperature is 98.7°F (37°C). His pulse is 80 beats/min and regular, his respiration rate is 16 breaths/min and unlabored, and his blood pressure is 112/70 mm Hg in the left upper extremity when he is seated. His oxygen saturation measured by pulse oximetry is 97% on room air.\nHeart sounds are normal, and the rate and rhythm are regular. The lung examination reveals no dullness or hyperresonance to percussion, and breath sounds are normal across all lung fields. The abdomen is nontender, with no guarding or organomegaly, and bowel sounds are normal. A firm 4 cm × 3 cm mass is noted in the epitrochlear region of the left elbow. The extremities exhibit normal tone and motor strength, with no contractures, malalignment, tenderness, or bony abnormalities. No cyanosis, edema, or varicosities are noted in any of the extremities. Inspection and palpation of the skin reveal no abnormalities.\nA CT scan with contrast shows a 4.0 cm × 3.1 cm soft tissue density in the medial, supracondylar region of the left arm, slightly above the elbow. The mass does not exhibit significant enhancement. It exerts a mass effect on the adjacent basilic vein with extrinsic compression. The fat planes between the mass and the underlying musculature appear preserved, with no infiltration, but some induration in the adjacent fat is noted. The surrounding soft tissue and bones appear normal. The CT scan results are highly suggestive of a soft tissue mass that probably requires pathologic examination. See the images below.\nFigure 1.\nFigure 2.\nThe mass is excised. The surgical pathology specimen consists of a 1.9 cm × 1.4 cm × 0.3 cm oval portion of homogeneous, glistening yellow-tan adipose tissue and a 4.4 cm × 3.7 cm × 3.2 cm oval portion of soft, gelatinous pink-gray tissue. The adipose tissue in the specimen is part of the overlying skin that was removed for appropriate closure of the incision.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1635247,
"choiceText": "Lipoma",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635248,
"choiceText": "Rheumatoid nodule",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635249,
"choiceText": "Infectious mononucleosis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635250,
"choiceText": "Diffuse large B-cell lymphoma",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 526075,
"questionText": "On the basis of these findings only, what is the most probable diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "What's Causing This Rapidly Growing, Golf Ball–Sized Mass?"
},
{
"authors": "Mark Davis, MD; Nandita Kakar",
"content": [
"The initial differential diagnosis for this patient consisted of a lipoma, a sarcoma, a rheumatoid nodule, and a lymphoma. Lipomas are common, benign tumors of mature fat that may be subcutaneous, intramuscular, or extramuscular. They are often stable, mobile, and painless. Upon removal, the mass did not resemble a lipoma because no gross adipose tissue was visible. Thus, a sarcoma rose higher on the differential diagnosis list. A sarcoma is a tumor of mesenchymal origin that starts in connective tissue or bone and can be either benign or malignant. The presence of a sarcoma can be confirmed only by pathologic examination.",
"A rheumatoid nodule was low on the comprehensive differential list for this patient because he had no history of rheumatoid arthritis or the commonly associated joint pain and stiffness. Rheumatoid nodules are subcutaneous lumps of inflammatory tissue that typically form over areas of repeated trauma and pressure. The medial location of the patient's mass also made this diagnosis unlikely.",
"A lymphoma originates from lymphoid tissues and is classified as Hodgkin or non-Hodgkin. A Hodgkin lymphoma is localized in a single group of lymph nodes, whereas a non-Hodgkin lymphoma involves multiple lymph nodes or features extranodal involvement and has a poorer prognosis. The epitrochlear location of this patient's mass indicates possible involvement of the lymph nodes in that region. These differential diagnoses cannot be ruled out until a pathologic study after excision reveals the cytology of the mass.",
"Microscopic examination revealed diffuse and vaguely nodular lymphoid proliferation. The immunochemical stain studies performed for this patient showed the expression of B-cell markers. The atypical lymphocytes were positive for the following biomarkers: CD-20, PAX5, BCL2 (B-cell lymphoma-2) (expressed in 100% of lymphoma cells), MUM1 (multiple myeloma oncogene 1), BCL6 (B-cell lymphoma-6), CD-10, a patchy differentiation of c-MYC, and small foci of follicular dendritic network remnants of CD-21.",
"The presence of B-cell markers raises concern for numerous immune-related diseases. These diseases are classified on the basis of the presence of specific markers and gene mutations. Infectious mononucleosis is caused by a virus that binds to B cells via CD-21 and can result in atypical lymphocytes in the bloodstream. This disease can be ruled out after interpretation of the pathologic studies, as well as by the patient's lack of characteristic symptoms such pharyngitis, fever, and fatigue.",
"Burkitt lymphoma is subtype of non-Hodgkin lymphoma that commonly occurs in adolescents or young adults and is associated with c-MYC, which is a transcription factor that can acquire a gain of function mutation to develop into an oncogene. This biomarker was present in the pathologic study of the patient's mass, which raised suspicion for a double-hit lymphoma. The larger presence of BCL2 and BCL6 suggested diffuse large B-cell lymphoma (DLBCL) because mutations in these genes are found in this subtype of non-Hodgkin lymphoma; however, the presence of c-MYC must be considered.",
"Fluorescence in situ hybridization studies, which identify the presence of chromosomal regions, were performed for BCL2, BCL6, and c-MYC translocations to rule out double-hit lymphoma, which was, in fact, excluded. The various types of non-Hodgkin lymphomas are classified by their genetic makeup. Overall, the findings in this patient were most consistent with the germinal center subtype of DLBCL, with mutations in BCL2 and BCL6 genes. A Ki67 stain showed a high proliferation rate of 70%."
],
"date": "November 08, 2021",
"figures": [],
"markdown": "# What's Causing This Rapidly Growing, Golf Ball–Sized Mass?\n\n **Authors:** Mark Davis, MD; Nandita Kakar \n **Date:** November 08, 2021\n\n ## Content\n\n The initial differential diagnosis for this patient consisted of a lipoma, a sarcoma, a rheumatoid nodule, and a lymphoma. Lipomas are common, benign tumors of mature fat that may be subcutaneous, intramuscular, or extramuscular. They are often stable, mobile, and painless. Upon removal, the mass did not resemble a lipoma because no gross adipose tissue was visible. Thus, a sarcoma rose higher on the differential diagnosis list. A sarcoma is a tumor of mesenchymal origin that starts in connective tissue or bone and can be either benign or malignant. The presence of a sarcoma can be confirmed only by pathologic examination.\nA rheumatoid nodule was low on the comprehensive differential list for this patient because he had no history of rheumatoid arthritis or the commonly associated joint pain and stiffness. Rheumatoid nodules are subcutaneous lumps of inflammatory tissue that typically form over areas of repeated trauma and pressure. The medial location of the patient's mass also made this diagnosis unlikely.\nA lymphoma originates from lymphoid tissues and is classified as Hodgkin or non-Hodgkin. A Hodgkin lymphoma is localized in a single group of lymph nodes, whereas a non-Hodgkin lymphoma involves multiple lymph nodes or features extranodal involvement and has a poorer prognosis. The epitrochlear location of this patient's mass indicates possible involvement of the lymph nodes in that region. These differential diagnoses cannot be ruled out until a pathologic study after excision reveals the cytology of the mass.\nMicroscopic examination revealed diffuse and vaguely nodular lymphoid proliferation. The immunochemical stain studies performed for this patient showed the expression of B-cell markers. The atypical lymphocytes were positive for the following biomarkers: CD-20, PAX5, BCL2 (B-cell lymphoma-2) (expressed in 100% of lymphoma cells), MUM1 (multiple myeloma oncogene 1), BCL6 (B-cell lymphoma-6), CD-10, a patchy differentiation of c-MYC, and small foci of follicular dendritic network remnants of CD-21.\nThe presence of B-cell markers raises concern for numerous immune-related diseases. These diseases are classified on the basis of the presence of specific markers and gene mutations. Infectious mononucleosis is caused by a virus that binds to B cells via CD-21 and can result in atypical lymphocytes in the bloodstream. This disease can be ruled out after interpretation of the pathologic studies, as well as by the patient's lack of characteristic symptoms such pharyngitis, fever, and fatigue.\nBurkitt lymphoma is subtype of non-Hodgkin lymphoma that commonly occurs in adolescents or young adults and is associated with c-MYC, which is a transcription factor that can acquire a gain of function mutation to develop into an oncogene. This biomarker was present in the pathologic study of the patient's mass, which raised suspicion for a double-hit lymphoma. The larger presence of BCL2 and BCL6 suggested diffuse large B-cell lymphoma (DLBCL) because mutations in these genes are found in this subtype of non-Hodgkin lymphoma; however, the presence of c-MYC must be considered.\nFluorescence in situ hybridization studies, which identify the presence of chromosomal regions, were performed for BCL2, BCL6, and c-MYC translocations to rule out double-hit lymphoma, which was, in fact, excluded. The various types of non-Hodgkin lymphomas are classified by their genetic makeup. Overall, the findings in this patient were most consistent with the germinal center subtype of DLBCL, with mutations in BCL2 and BCL6 genes. A Ki67 stain showed a high proliferation rate of 70%.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1635247,
"choiceText": "Lipoma",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635248,
"choiceText": "Rheumatoid nodule",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635249,
"choiceText": "Infectious mononucleosis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635250,
"choiceText": "Diffuse large B-cell lymphoma",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 526075,
"questionText": "On the basis of these findings only, what is the most probable diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "What's Causing This Rapidly Growing, Golf Ball–Sized Mass?"
},
{
"authors": "Mark Davis, MD; Nandita Kakar",
"content": [
"The outlook and treatment of DLBCL may differ on the basis of the cell of origin. Some start from germinal centers of lymphoid tissue, whereas others do not. Immunohistochemistry helps to identify the proteins specific to each subtype. DLBCL often involves CD-20, which is a membrane-embedded surface molecule that plays a role in the development and differentiation of B cells into plasma cells for the production of antibodies. CD-10 is an important biomarker that is unique to germinal center B cells, thus confirming this patient's tumor as the germinal center subtype of DLBCL.[1]",
"Chest, abdominal, and pelvic CT were performed to detect the primary neoplasm. The CT studies did not reveal any other masses. PET was subsequently performed to investigate metabolically active tissue in the patient. A morphologically normal-appearing left axillary lymph node was found to have metabolic activity, with a maximum standardized uptake value of 4.3, which could suggest cancer. Standardized uptake value is a measurement of glucose uptake from the radioactive tracer in the patient's tissue, which signifies metabolic activity that can be compared with other sites in the body to identify cell proliferation.[1] See the image below.",
"Figure 3.",
"DLBCL is the most common non-Hodgkin lymphoma in the United States. DLBCL is a B-lymphocyte neoplasm that can develop in the lymph nodes; however, 31.6% of cases present in extranodal sites such as the gastrointestinal tract, thyroid, testes, or in any organ of the body.[2]",
"BCL2 inhibits apoptosis in the intrinsic programmed cell death pathway. This gene can undergo a gain of function mutation, converting the gene into an oncogene, which is commonly known as the translocation t(14;18). The overexpression of BCL2 is associated with a poor prognosis in DLBCL, but its effects vary depending on the stage of the disease.[3] BCL6 is a transcription factor that acts as a repressor of transcription of B cells. This gene is found to be hypermutated and translocated in the pathogenesis of DLBCL.",
"Germinal centers are dependent on BCL6 for initiation and maintenance.[4] Germinal centers are sites in follicles of lymph nodes involved in the production of mature B cells and high-affinity antibodies that can provide protection against reinfection. Mutations in these genes result in the progressive clonal expansion of mature B cells. These mutations may result from chromosomal translocations, infections, environmental factors, immunocompromised states, and/or chronic inflammation.[5]",
"Low-grade DLBCL can present as painless lymphadenopathy, with the commonly associated symptoms of fatigue and weakness. High-grade DLBCL can present with these symptoms, along with fever, night sweats, and weight loss, which are known as \"B symptoms.\" Extranodal tumors can be resected surgically, as was done in this patient. The suspected activity in additional lymph nodes, which was revealed by the PET scan, requires medical treatment with chemotherapy."
],
"date": "November 08, 2021",
"figures": [
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/962/080/962080-Thumb3.png"
}
],
"markdown": "# What's Causing This Rapidly Growing, Golf Ball–Sized Mass?\n\n **Authors:** Mark Davis, MD; Nandita Kakar \n **Date:** November 08, 2021\n\n ## Content\n\n The outlook and treatment of DLBCL may differ on the basis of the cell of origin. Some start from germinal centers of lymphoid tissue, whereas others do not. Immunohistochemistry helps to identify the proteins specific to each subtype. DLBCL often involves CD-20, which is a membrane-embedded surface molecule that plays a role in the development and differentiation of B cells into plasma cells for the production of antibodies. CD-10 is an important biomarker that is unique to germinal center B cells, thus confirming this patient's tumor as the germinal center subtype of DLBCL.[1]\nChest, abdominal, and pelvic CT were performed to detect the primary neoplasm. The CT studies did not reveal any other masses. PET was subsequently performed to investigate metabolically active tissue in the patient. A morphologically normal-appearing left axillary lymph node was found to have metabolic activity, with a maximum standardized uptake value of 4.3, which could suggest cancer. Standardized uptake value is a measurement of glucose uptake from the radioactive tracer in the patient's tissue, which signifies metabolic activity that can be compared with other sites in the body to identify cell proliferation.[1] See the image below.\nFigure 3.\nDLBCL is the most common non-Hodgkin lymphoma in the United States. DLBCL is a B-lymphocyte neoplasm that can develop in the lymph nodes; however, 31.6% of cases present in extranodal sites such as the gastrointestinal tract, thyroid, testes, or in any organ of the body.[2]\nBCL2 inhibits apoptosis in the intrinsic programmed cell death pathway. This gene can undergo a gain of function mutation, converting the gene into an oncogene, which is commonly known as the translocation t(14;18). The overexpression of BCL2 is associated with a poor prognosis in DLBCL, but its effects vary depending on the stage of the disease.[3] BCL6 is a transcription factor that acts as a repressor of transcription of B cells. This gene is found to be hypermutated and translocated in the pathogenesis of DLBCL.\nGerminal centers are dependent on BCL6 for initiation and maintenance.[4] Germinal centers are sites in follicles of lymph nodes involved in the production of mature B cells and high-affinity antibodies that can provide protection against reinfection. Mutations in these genes result in the progressive clonal expansion of mature B cells. These mutations may result from chromosomal translocations, infections, environmental factors, immunocompromised states, and/or chronic inflammation.[5]\nLow-grade DLBCL can present as painless lymphadenopathy, with the commonly associated symptoms of fatigue and weakness. High-grade DLBCL can present with these symptoms, along with fever, night sweats, and weight loss, which are known as \"B symptoms.\" Extranodal tumors can be resected surgically, as was done in this patient. The suspected activity in additional lymph nodes, which was revealed by the PET scan, requires medical treatment with chemotherapy.\n\n ## Figures\n\n **Figure 3.** \n \n\n\n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "What's Causing This Rapidly Growing, Golf Ball–Sized Mass?"
},
{
"authors": "Mark Davis, MD; Nandita Kakar",
"content": [
"Depending on the stage of the cancer, the treatment options include chemotherapy, radiation therapy, corticosteroids, immunomodulators, targeted gene therapy, and blood cell transplant. R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone) is the most common combination regimen that is used to treat DLBCL. Rituximab is a monoclonal antibody that targets CD-20; the other medications in the regimen include alkylating agents and anthracyclines. These medications have many adverse effects (cardiotoxic effects in particular) that must be considered in patients older than 60 years. Alternative regimens have been investigated to prevent these effects, including decreased doses and pegylation.[6]",
"The clinical diagnosis of DLBCL can be challenging, especially in a patient who does not present with many symptoms. However, any rapidly growing mass should be suspected of being cancer until proven otherwise. Although the absence of fever, night sweats, and weight loss in this patient weighs against the diagnosis of a lymphoma, the location of the mass is precisely in the epitrochlear lymph node region. This clinical sign should raise suspicion for a lymphoma, with timely diagnostic testing to direct treatment.",
"This patient has clinical stage IA disease, which indicates that the cancer is in one lymph node region, with a primary epitrochlear lymph node origin. He is being treated with rituximab. A port was placed to receive chemotherapy, and he is expected to have a good prognosis."
],
"date": "November 08, 2021",
"figures": [],
"markdown": "# What's Causing This Rapidly Growing, Golf Ball–Sized Mass?\n\n **Authors:** Mark Davis, MD; Nandita Kakar \n **Date:** November 08, 2021\n\n ## Content\n\n Depending on the stage of the cancer, the treatment options include chemotherapy, radiation therapy, corticosteroids, immunomodulators, targeted gene therapy, and blood cell transplant. R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone) is the most common combination regimen that is used to treat DLBCL. Rituximab is a monoclonal antibody that targets CD-20; the other medications in the regimen include alkylating agents and anthracyclines. These medications have many adverse effects (cardiotoxic effects in particular) that must be considered in patients older than 60 years. Alternative regimens have been investigated to prevent these effects, including decreased doses and pegylation.[6]\nThe clinical diagnosis of DLBCL can be challenging, especially in a patient who does not present with many symptoms. However, any rapidly growing mass should be suspected of being cancer until proven otherwise. Although the absence of fever, night sweats, and weight loss in this patient weighs against the diagnosis of a lymphoma, the location of the mass is precisely in the epitrochlear lymph node region. This clinical sign should raise suspicion for a lymphoma, with timely diagnostic testing to direct treatment.\nThis patient has clinical stage IA disease, which indicates that the cancer is in one lymph node region, with a primary epitrochlear lymph node origin. He is being treated with rituximab. A port was placed to receive chemotherapy, and he is expected to have a good prognosis.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1635251,
"choiceText": "c-MYC",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635252,
"choiceText": "BCL2",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635253,
"choiceText": "CD-20",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635254,
"choiceText": "BCL2 and BCL6",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635255,
"choiceText": "CD-21",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "BCL2 and BCL6 are markers linked to the germinal centers of B cells. B cells undergo various stages of maturation in germinal centers to assemble immunoglobulins. During this process, B cells are susceptible to the development of chromosomal translocations or gene mutations. The BCL2 and BCL6 markers are involved in the regulation of this process, and their dysfunction can lead to the selective growth of a malignant clone.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 526076,
"questionText": "Which markers are most commonly associated with DLBCL?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1635256,
"choiceText": "CT ",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635257,
"choiceText": "MRI",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635258,
"choiceText": "PET",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635259,
"choiceText": "Ultrasonography",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nPET is the most helpful test to stage cancer. A radioactive tracer is used to detect the levels of metabolic activity in the body's tissues. Cancerous cells have a higher metabolic rate than noncancerous cells, which is useful in detecting a disease that may not be grossly visible or evident on CT.\r\n\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 526077,
"questionText": "Which test is most helpful for staging DLBCL?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "What's Causing This Rapidly Growing, Golf Ball–Sized Mass?"
},
{
"authors": "Mark Davis, MD; Nandita Kakar",
"content": [
"Follow Medscape on Facebook, Twitter, Instagram, and YouTube"
],
"date": "November 08, 2021",
"figures": [],
"markdown": "# What's Causing This Rapidly Growing, Golf Ball–Sized Mass?\n\n **Authors:** Mark Davis, MD; Nandita Kakar \n **Date:** November 08, 2021\n\n ## Content\n\n Follow Medscape on Facebook, Twitter, Instagram, and YouTube\n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1635251,
"choiceText": "c-MYC",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635252,
"choiceText": "BCL2",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635253,
"choiceText": "CD-20",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635254,
"choiceText": "BCL2 and BCL6",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635255,
"choiceText": "CD-21",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "BCL2 and BCL6 are markers linked to the germinal centers of B cells. B cells undergo various stages of maturation in germinal centers to assemble immunoglobulins. During this process, B cells are susceptible to the development of chromosomal translocations or gene mutations. The BCL2 and BCL6 markers are involved in the regulation of this process, and their dysfunction can lead to the selective growth of a malignant clone.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 526076,
"questionText": "Which markers are most commonly associated with DLBCL?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1635256,
"choiceText": "CT ",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635257,
"choiceText": "MRI",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635258,
"choiceText": "PET",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635259,
"choiceText": "Ultrasonography",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nPET is the most helpful test to stage cancer. A radioactive tracer is used to detect the levels of metabolic activity in the body's tissues. Cancerous cells have a higher metabolic rate than noncancerous cells, which is useful in detecting a disease that may not be grossly visible or evident on CT.\r\n\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 526077,
"questionText": "Which test is most helpful for staging DLBCL?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "What's Causing This Rapidly Growing, Golf Ball–Sized Mass?"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1635247,
"choiceText": "Lipoma",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635248,
"choiceText": "Rheumatoid nodule",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635249,
"choiceText": "Infectious mononucleosis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635250,
"choiceText": "Diffuse large B-cell lymphoma",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 526075,
"questionText": "On the basis of these findings only, what is the most probable diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1635251,
"choiceText": "c-MYC",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635252,
"choiceText": "BCL2",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635253,
"choiceText": "CD-20",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635254,
"choiceText": "BCL2 and BCL6",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635255,
"choiceText": "CD-21",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "BCL2 and BCL6 are markers linked to the germinal centers of B cells. B cells undergo various stages of maturation in germinal centers to assemble immunoglobulins. During this process, B cells are susceptible to the development of chromosomal translocations or gene mutations. The BCL2 and BCL6 markers are involved in the regulation of this process, and their dysfunction can lead to the selective growth of a malignant clone.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 526076,
"questionText": "Which markers are most commonly associated with DLBCL?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1635256,
"choiceText": "CT ",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635257,
"choiceText": "MRI",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635258,
"choiceText": "PET",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1635259,
"choiceText": "Ultrasonography",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nPET is the most helpful test to stage cancer. A radioactive tracer is used to detect the levels of metabolic activity in the body's tissues. Cancerous cells have a higher metabolic rate than noncancerous cells, which is useful in detecting a disease that may not be grossly visible or evident on CT.\r\n\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 526077,
"questionText": "Which test is most helpful for staging DLBCL?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
717114 | /viewarticle/717114 | [
{
"authors": "Thomas J. Hemingway, MD; Rick G. Kulkarni, MD, FACEP",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 30-year-old man of Japanese descent presents to the emergency department (ED) after experiencing a syncopal event at home. His wife, who has accompanied him to the ED, witnessed the event. She states that they had been talking in the kitchen when her husband complained of feeling dizzy. He then became nauseous and slumped over onto the table; before she could get up and help him, he fell out of his chair and hit his head on the floor. After some time lying on the floor, he regained consciousness.",
"The wife did not notice any seizurelike activity (including no jerky body movements, tongue biting, or incontinence) while her husband was unconscious. When he regained consciousness, he was immediately fully awake, alert, and conversant; no period of confusion or garbled speech was noted.",
"The patient reports that he has had many similar episodes in the past several years, but he has never sought medical evaluation for them. At the time of presentation, the patient has no specific complaints other than a bruise on his forehead and mild embarrassment. The patient's family history is significant for an uncle who died in his 30s without apparent cause."
],
"date": "November 02, 2021",
"figures": [],
"markdown": "# Recurrent Syncope in a 30-Year-Old Whose Uncle Died Suddenly\n\n **Authors:** Thomas J. Hemingway, MD; Rick G. Kulkarni, MD, FACEP \n **Date:** November 02, 2021\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 30-year-old man of Japanese descent presents to the emergency department (ED) after experiencing a syncopal event at home. His wife, who has accompanied him to the ED, witnessed the event. She states that they had been talking in the kitchen when her husband complained of feeling dizzy. He then became nauseous and slumped over onto the table; before she could get up and help him, he fell out of his chair and hit his head on the floor. After some time lying on the floor, he regained consciousness.\nThe wife did not notice any seizurelike activity (including no jerky body movements, tongue biting, or incontinence) while her husband was unconscious. When he regained consciousness, he was immediately fully awake, alert, and conversant; no period of confusion or garbled speech was noted.\nThe patient reports that he has had many similar episodes in the past several years, but he has never sought medical evaluation for them. At the time of presentation, the patient has no specific complaints other than a bruise on his forehead and mild embarrassment. The patient's family history is significant for an uncle who died in his 30s without apparent cause.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Recurrent Syncope in a 30-Year-Old Whose Uncle Died Suddenly"
},
{
"authors": "Thomas J. Hemingway, MD; Rick G. Kulkarni, MD, FACEP",
"content": [
"Upon physical examination, the patient is awake and alert. His vital signs are stable, with a heart rate of 82 beats/min and a blood pressure of 135/85 mm Hg. His respirations are 12 breaths/min, and an oxygen reading on room air is 100%. He has a 3-cm area of ecchymosis on his left forehead, with no underlying hematoma or tenderness to palpation.",
"No laceration is noted over the area of bruising. The cardiac examination reveals a regular rhythm with no significant murmurs or gallops. The chest examination demonstrates easy, nonlabored respirations, with no abnormal breath sounds. The neurologic examination is also unremarkable, including a normal cranial nerve inspection, normal gross motor and sensory function, no pronator drift, and normal speech. He is able to walk without difficulty.",
"A panel of laboratory investigative blood work is drawn. An electrocardiogram (ECG) is ordered (see Figure 1). The results of the complete blood cell (CBC) count as well as a basic metabolic panel and other laboratory findings are unremarkable.",
"Figure 1."
],
"date": "November 02, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/717/114/717114-thumb1.png"
}
],
"markdown": "# Recurrent Syncope in a 30-Year-Old Whose Uncle Died Suddenly\n\n **Authors:** Thomas J. Hemingway, MD; Rick G. Kulkarni, MD, FACEP \n **Date:** November 02, 2021\n\n ## Content\n\n Upon physical examination, the patient is awake and alert. His vital signs are stable, with a heart rate of 82 beats/min and a blood pressure of 135/85 mm Hg. His respirations are 12 breaths/min, and an oxygen reading on room air is 100%. He has a 3-cm area of ecchymosis on his left forehead, with no underlying hematoma or tenderness to palpation.\nNo laceration is noted over the area of bruising. The cardiac examination reveals a regular rhythm with no significant murmurs or gallops. The chest examination demonstrates easy, nonlabored respirations, with no abnormal breath sounds. The neurologic examination is also unremarkable, including a normal cranial nerve inspection, normal gross motor and sensory function, no pronator drift, and normal speech. He is able to walk without difficulty.\nA panel of laboratory investigative blood work is drawn. An electrocardiogram (ECG) is ordered (see Figure 1). The results of the complete blood cell (CBC) count as well as a basic metabolic panel and other laboratory findings are unremarkable.\nFigure 1.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 329777,
"choiceText": "Brugada syndrome",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329778,
"choiceText": "ST-segment elevation myocardial infarction",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329779,
"choiceText": "Wolff-Parkinson-White syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329780,
"choiceText": "Ventricular tachycardia",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 92163,
"questionText": "Based only on this information, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Recurrent Syncope in a 30-Year-Old Whose Uncle Died Suddenly"
},
{
"authors": "Thomas J. Hemingway, MD; Rick G. Kulkarni, MD, FACEP",
"content": [
"The patient presented with ECG findings of a characteristic downsloping ST-segment elevation in leads V1-V3, accompanied by a QRS morphology resembling that of a right bundle branch block (RBBB); these findings on an ECG are known as the Brugada pattern. In combination with the patient's history of previous multiple episodes of unexplained syncope, as well as a close family member with likely sudden cardiac death (SCD), the presentation was strongly suggestive of a diagnosis of Brugada syndrome.",
"The vast majority of individuals who experience SCD are patients with coronary artery disease (CAD) or structural heart disease, such as hypertrophic cardiomyopathy, anomalous coronary artery origins, or arrhythmogenic right ventricular dysplasia. SCD is uncommon in individuals without a history of CAD or of a structurally abnormal heart (such as with hypertrophic cardiomyopathy or dilated cardiomyopathy). In the minority of patients who experience SCD that have a structurally normal heart and no evidence of CAD, the causes include Brugada syndrome, long QT syndrome, and preexcitation syndromes.",
"About 5% of the survivors of cardiac arrest have no clinically identified cardiac abnormality; about half of those cases are thought to be caused by Brugada syndrome.[1] Commotio cordis as a result of blunt trauma to the chest may also lead to SCD in an individual with a normal heart.[2]",
"Brugada syndrome was originally described in 1992. It consists of the Brugada pattern (seen on ECG) and 1 or more of the following associated clinical features:",
"Syncopal episodes",
"Documented ventricular fibrillation (VF)",
"Self-terminating polymorphic ventricular tachycardia (VT)",
"Family history of SCD in a relative younger than 45 years",
"Evidence of ST-segment elevation in family members",
"The syndrome is characteristically caused by an autosomal-dominant genetic defect that results in dysfunction or loss of function of the sodium channel.",
"Dysfunction of the cardiac sodium ion channels underlies the clinical manifestations of Brugada syndrome by reducing the sodium current available during phases 0 (upstroke) and 1 (early repolarization) of the cardiac action potential. The condition most commonly affects middle-aged men (with an average presentation of age 30 y), and it can be recognized by its characteristic ECG pattern. Individuals with Brugada syndrome are prone to develop malignant ventricular tachyarrhythmias, which may lead to syncope, cardiac arrest, or SCD.[3]"
],
"date": "November 02, 2021",
"figures": [],
"markdown": "# Recurrent Syncope in a 30-Year-Old Whose Uncle Died Suddenly\n\n **Authors:** Thomas J. Hemingway, MD; Rick G. Kulkarni, MD, FACEP \n **Date:** November 02, 2021\n\n ## Content\n\n The patient presented with ECG findings of a characteristic downsloping ST-segment elevation in leads V1-V3, accompanied by a QRS morphology resembling that of a right bundle branch block (RBBB); these findings on an ECG are known as the Brugada pattern. In combination with the patient's history of previous multiple episodes of unexplained syncope, as well as a close family member with likely sudden cardiac death (SCD), the presentation was strongly suggestive of a diagnosis of Brugada syndrome.\nThe vast majority of individuals who experience SCD are patients with coronary artery disease (CAD) or structural heart disease, such as hypertrophic cardiomyopathy, anomalous coronary artery origins, or arrhythmogenic right ventricular dysplasia. SCD is uncommon in individuals without a history of CAD or of a structurally abnormal heart (such as with hypertrophic cardiomyopathy or dilated cardiomyopathy). In the minority of patients who experience SCD that have a structurally normal heart and no evidence of CAD, the causes include Brugada syndrome, long QT syndrome, and preexcitation syndromes.\nAbout 5% of the survivors of cardiac arrest have no clinically identified cardiac abnormality; about half of those cases are thought to be caused by Brugada syndrome.[1] Commotio cordis as a result of blunt trauma to the chest may also lead to SCD in an individual with a normal heart.[2]\nBrugada syndrome was originally described in 1992. It consists of the Brugada pattern (seen on ECG) and 1 or more of the following associated clinical features:\nSyncopal episodes\nDocumented ventricular fibrillation (VF)\nSelf-terminating polymorphic ventricular tachycardia (VT)\nFamily history of SCD in a relative younger than 45 years\nEvidence of ST-segment elevation in family members\nThe syndrome is characteristically caused by an autosomal-dominant genetic defect that results in dysfunction or loss of function of the sodium channel.\nDysfunction of the cardiac sodium ion channels underlies the clinical manifestations of Brugada syndrome by reducing the sodium current available during phases 0 (upstroke) and 1 (early repolarization) of the cardiac action potential. The condition most commonly affects middle-aged men (with an average presentation of age 30 y), and it can be recognized by its characteristic ECG pattern. Individuals with Brugada syndrome are prone to develop malignant ventricular tachyarrhythmias, which may lead to syncope, cardiac arrest, or SCD.[3]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 329777,
"choiceText": "Brugada syndrome",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329778,
"choiceText": "ST-segment elevation myocardial infarction",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329779,
"choiceText": "Wolff-Parkinson-White syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329780,
"choiceText": "Ventricular tachycardia",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 92163,
"questionText": "Based only on this information, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Recurrent Syncope in a 30-Year-Old Whose Uncle Died Suddenly"
},
{
"authors": "Thomas J. Hemingway, MD; Rick G. Kulkarni, MD, FACEP",
"content": [
"The prevalence of Brugada syndrome depends on the age, sex, and ethnicity of the population. In some countries in Southeast Asia, the syndrome accounts for 40%-50% of all cases of idiopathic VF; in the United States, the prevalence is much lower, although the incidence is not well established overall because of the relatively recent identification of the condition itself.",
"The genetic basis for Brugada syndrome is under continued investigation; approximately 20%-30% of cases demonstrate a loss-of-function mutation in the SCN5A gene. Another locus on chromosome 3 has also been reported, but the genetic cause for most Brugada syndrome cases remains unknown. Several clinical conditions may unmask or exacerbate the ECG pattern of Brugada syndrome, including the pharmacologic use of sodium-channel blockers, alpha-adrenergic agonists, beta-adrenergic blockers, and heterocyclic antidepressant agents. A febrile state, active use of certain substances (such as cocaine and alcohol), as well as many electrolyte disturbances have also been implicated (including hyperkalemia, hypokalemia, and hypercalcemia).[4,5,6]",
"The diagnosis of Brugada syndrome should be considered in patients with a personal or family history of SCD, even if the initial ECG is normal. Intermittent or concealed forms of Brugada syndrome can often be diagnosed by provocative administration of antiarrhythmic agents that block the sodium channel in the electrophysiology laboratory. In fact, the abnormality may only be revealed with the administration of such provocative drugs (eg, flecainide, procainamide).",
"The ECG abnormalities may disappear with exercise. The effects of these pharmaceutical agents and of exercise are consistent with the molecular mechanism of a reduced sodium current as the proposed explanation for Brugada syndrome. If the patient's history or ECG findings suggest this condition, a cardiologist specializing in electrophysiology should be consulted.[6]"
],
"date": "November 02, 2021",
"figures": [],
"markdown": "# Recurrent Syncope in a 30-Year-Old Whose Uncle Died Suddenly\n\n **Authors:** Thomas J. Hemingway, MD; Rick G. Kulkarni, MD, FACEP \n **Date:** November 02, 2021\n\n ## Content\n\n The prevalence of Brugada syndrome depends on the age, sex, and ethnicity of the population. In some countries in Southeast Asia, the syndrome accounts for 40%-50% of all cases of idiopathic VF; in the United States, the prevalence is much lower, although the incidence is not well established overall because of the relatively recent identification of the condition itself.\nThe genetic basis for Brugada syndrome is under continued investigation; approximately 20%-30% of cases demonstrate a loss-of-function mutation in the SCN5A gene. Another locus on chromosome 3 has also been reported, but the genetic cause for most Brugada syndrome cases remains unknown. Several clinical conditions may unmask or exacerbate the ECG pattern of Brugada syndrome, including the pharmacologic use of sodium-channel blockers, alpha-adrenergic agonists, beta-adrenergic blockers, and heterocyclic antidepressant agents. A febrile state, active use of certain substances (such as cocaine and alcohol), as well as many electrolyte disturbances have also been implicated (including hyperkalemia, hypokalemia, and hypercalcemia).[4,5,6]\nThe diagnosis of Brugada syndrome should be considered in patients with a personal or family history of SCD, even if the initial ECG is normal. Intermittent or concealed forms of Brugada syndrome can often be diagnosed by provocative administration of antiarrhythmic agents that block the sodium channel in the electrophysiology laboratory. In fact, the abnormality may only be revealed with the administration of such provocative drugs (eg, flecainide, procainamide).\nThe ECG abnormalities may disappear with exercise. The effects of these pharmaceutical agents and of exercise are consistent with the molecular mechanism of a reduced sodium current as the proposed explanation for Brugada syndrome. If the patient's history or ECG findings suggest this condition, a cardiologist specializing in electrophysiology should be consulted.[6]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Recurrent Syncope in a 30-Year-Old Whose Uncle Died Suddenly"
},
{
"authors": "Thomas J. Hemingway, MD; Rick G. Kulkarni, MD, FACEP",
"content": [
"Not all patients who present with syncope require admission; however, patients who have had syncopal episodes in the setting of ECG abnormalities or have a family history of SCD should be admitted to the hospital. In patients with Brugada syndrome, an automatic implantable cardioverter defibrillator (AICD), the only treatment that has been proven effective for this condition, should be considered. No proven pharmacologic agents have reliably reduced the occurrence of VT or VF, or that have prevented sudden death in a prospective manner.",
"The indications for AICD implantation were published in the report of the Second Consensus Conference on Brugada syndrome,[4] with consensus only achieved for patients with a history for Brugada syndrome and a history of cardiac arrest requiring an AICD; close follow-up without intervention was recommended for asymptomatic patients with no family history of SCD. In suspected cases with a \"concealed\" Brugada pattern on the ECG, procainamide may be administered to bring out the characteristic ECG abnormalities.",
"Additionally, programmed electrical stimulation to induce VT/VF during an electrophysiology study (EPS) may also be used to determine the need for AICD placement in these patients. Given the genetic pattern of autosomal dominance, the treating cardiologist should arrange for an evaluation of the patient's family members. Some clinicians also recommend restrictions in physical activity for patients with Brugada syndrome because of a potential increased risk of developing VF as a result of increased vagal tone during the recovery period after exercise.[7] Whether patients who are asymptomatic carriers of SCN5A mutations should also be restricted from participation in sports.[6]",
"The patient in this case was admitted to an inpatient monitored setting after consultation with an electrophysiologist. Given the clinical presentation, including the positive family history of SCD and the characteristic changes of the Brugada pattern noted on the ECG, the decision was made to place an AICD without a formal EPS. The patient was discharged to home on postprocedure day 2 with follow-up. He was also advised to contact his family members to alert them to his diagnosis and treatment.",
"Special thanks are extended to Dr. John Vozenilek, MD, FACEP, for his contributions to the publication of this case, and to EMedHome.com, for contributing the ECG image."
],
"date": "November 02, 2021",
"figures": [],
"markdown": "# Recurrent Syncope in a 30-Year-Old Whose Uncle Died Suddenly\n\n **Authors:** Thomas J. Hemingway, MD; Rick G. Kulkarni, MD, FACEP \n **Date:** November 02, 2021\n\n ## Content\n\n Not all patients who present with syncope require admission; however, patients who have had syncopal episodes in the setting of ECG abnormalities or have a family history of SCD should be admitted to the hospital. In patients with Brugada syndrome, an automatic implantable cardioverter defibrillator (AICD), the only treatment that has been proven effective for this condition, should be considered. No proven pharmacologic agents have reliably reduced the occurrence of VT or VF, or that have prevented sudden death in a prospective manner.\nThe indications for AICD implantation were published in the report of the Second Consensus Conference on Brugada syndrome,[4] with consensus only achieved for patients with a history for Brugada syndrome and a history of cardiac arrest requiring an AICD; close follow-up without intervention was recommended for asymptomatic patients with no family history of SCD. In suspected cases with a \"concealed\" Brugada pattern on the ECG, procainamide may be administered to bring out the characteristic ECG abnormalities.\nAdditionally, programmed electrical stimulation to induce VT/VF during an electrophysiology study (EPS) may also be used to determine the need for AICD placement in these patients. Given the genetic pattern of autosomal dominance, the treating cardiologist should arrange for an evaluation of the patient's family members. Some clinicians also recommend restrictions in physical activity for patients with Brugada syndrome because of a potential increased risk of developing VF as a result of increased vagal tone during the recovery period after exercise.[7] Whether patients who are asymptomatic carriers of SCN5A mutations should also be restricted from participation in sports.[6]\nThe patient in this case was admitted to an inpatient monitored setting after consultation with an electrophysiologist. Given the clinical presentation, including the positive family history of SCD and the characteristic changes of the Brugada pattern noted on the ECG, the decision was made to place an AICD without a formal EPS. The patient was discharged to home on postprocedure day 2 with follow-up. He was also advised to contact his family members to alert them to his diagnosis and treatment.\nSpecial thanks are extended to Dr. John Vozenilek, MD, FACEP, for his contributions to the publication of this case, and to EMedHome.com, for contributing the ECG image.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 329786,
"choiceText": "Prolonged QT interval",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329787,
"choiceText": "QRS morphology resembling a left bundle branch block",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329788,
"choiceText": "Positive deflection of the T-wave in the affected precordial leads",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329789,
"choiceText": "Downsloping ST-segment elevations in V1-V3",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329790,
"choiceText": "None of the above",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The characteristic Brugada pattern on ECG is recognizable by a downsloping ST-segment elevation in leads V1-V3 and a QRS resembling a RBBB. Brugada syndrome is distinguished from benign early repolarization (BER) in that Brugada syndrome has a downsloping precordial ST-segment elevation that is typically followed by a negative T wave, whereas BER usually has a positive T wave. A prolonged QT interval is not typically associated with Brugada syndrome, although it can be another cause of syncope.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 92167,
"questionText": "Which of the following ECG abnormalities is typically associated with the Brugada pattern?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 329791,
"choiceText": "History of palpitations",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329792,
"choiceText": "Family history of hypertension in individuals younger than 45 years",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329793,
"choiceText": "Evidence of ST segment depression in family members",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329794,
"choiceText": "History of syncopal episodes",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329795,
"choiceText": "Previously documented atrial fibrillation",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Brugada syndrome consists of the Brugada pattern and 1 or more of the following associated clinical features: syncopal episodes, documented VF, self-terminating polymorphic VT, a family history of SCD in a relative younger than 45 years, and evidence of ST-segment elevation in family members. A history of palpitation is not required for diagnosis.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 92168,
"questionText": "Which of the following associated features is required to define Brugada syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Recurrent Syncope in a 30-Year-Old Whose Uncle Died Suddenly"
},
{
"authors": "Thomas J. Hemingway, MD; Rick G. Kulkarni, MD, FACEP",
"content": [],
"date": "November 02, 2021",
"figures": [],
"markdown": "# Recurrent Syncope in a 30-Year-Old Whose Uncle Died Suddenly\n\n **Authors:** Thomas J. Hemingway, MD; Rick G. Kulkarni, MD, FACEP \n **Date:** November 02, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 329786,
"choiceText": "Prolonged QT interval",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329787,
"choiceText": "QRS morphology resembling a left bundle branch block",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329788,
"choiceText": "Positive deflection of the T-wave in the affected precordial leads",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329789,
"choiceText": "Downsloping ST-segment elevations in V1-V3",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329790,
"choiceText": "None of the above",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The characteristic Brugada pattern on ECG is recognizable by a downsloping ST-segment elevation in leads V1-V3 and a QRS resembling a RBBB. Brugada syndrome is distinguished from benign early repolarization (BER) in that Brugada syndrome has a downsloping precordial ST-segment elevation that is typically followed by a negative T wave, whereas BER usually has a positive T wave. A prolonged QT interval is not typically associated with Brugada syndrome, although it can be another cause of syncope.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 92167,
"questionText": "Which of the following ECG abnormalities is typically associated with the Brugada pattern?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 329791,
"choiceText": "History of palpitations",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329792,
"choiceText": "Family history of hypertension in individuals younger than 45 years",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329793,
"choiceText": "Evidence of ST segment depression in family members",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329794,
"choiceText": "History of syncopal episodes",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329795,
"choiceText": "Previously documented atrial fibrillation",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Brugada syndrome consists of the Brugada pattern and 1 or more of the following associated clinical features: syncopal episodes, documented VF, self-terminating polymorphic VT, a family history of SCD in a relative younger than 45 years, and evidence of ST-segment elevation in family members. A history of palpitation is not required for diagnosis.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 92168,
"questionText": "Which of the following associated features is required to define Brugada syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Recurrent Syncope in a 30-Year-Old Whose Uncle Died Suddenly"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 329777,
"choiceText": "Brugada syndrome",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329778,
"choiceText": "ST-segment elevation myocardial infarction",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329779,
"choiceText": "Wolff-Parkinson-White syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329780,
"choiceText": "Ventricular tachycardia",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 92163,
"questionText": "Based only on this information, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 329786,
"choiceText": "Prolonged QT interval",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329787,
"choiceText": "QRS morphology resembling a left bundle branch block",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329788,
"choiceText": "Positive deflection of the T-wave in the affected precordial leads",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329789,
"choiceText": "Downsloping ST-segment elevations in V1-V3",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329790,
"choiceText": "None of the above",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The characteristic Brugada pattern on ECG is recognizable by a downsloping ST-segment elevation in leads V1-V3 and a QRS resembling a RBBB. Brugada syndrome is distinguished from benign early repolarization (BER) in that Brugada syndrome has a downsloping precordial ST-segment elevation that is typically followed by a negative T wave, whereas BER usually has a positive T wave. A prolonged QT interval is not typically associated with Brugada syndrome, although it can be another cause of syncope.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 92167,
"questionText": "Which of the following ECG abnormalities is typically associated with the Brugada pattern?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 329791,
"choiceText": "History of palpitations",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329792,
"choiceText": "Family history of hypertension in individuals younger than 45 years",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329793,
"choiceText": "Evidence of ST segment depression in family members",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329794,
"choiceText": "History of syncopal episodes",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 329795,
"choiceText": "Previously documented atrial fibrillation",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Brugada syndrome consists of the Brugada pattern and 1 or more of the following associated clinical features: syncopal episodes, documented VF, self-terminating polymorphic VT, a family history of SCD in a relative younger than 45 years, and evidence of ST-segment elevation in family members. A history of palpitation is not required for diagnosis.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 92168,
"questionText": "Which of the following associated features is required to define Brugada syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
878930 | /viewarticle/878930 | [
{
"authors": "James Robert Brasic, MD, MPH",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 33-year-old woman presents with her parents for a routine clinic visit and to refill her medications. Presently, she lives with her parents, who are her primary caregivers and on whom she is completely dependent. She has profound intellectual impairment and is thought to have the mental capacity of an 18-month-old child. No other family members are affected.",
"According to her parents, her birth history was unremarkable. Phenotypically normal, the patient developed and grew appropriately her first year of life. However, as a toddler, she began to lose previously acquired skills (developmental regression) and failed to attain further developmental milestones. She did not learn to talk and was diagnosed with profound intellectual disability. She received special education services to assist her with adaptive functioning.",
"In early childhood, she was diagnosed with a seizure disorder, which has been medically treated with the anticonvulsants carbamazepine and valproic acid. She has a history of orthopedic concerns. Skeletal abnormalities of note include a history of marked scoliosis and a left-sided coxa valga, which was treated by a lift in her left shoe. To treat her scoliosis, rods were placed in lateral position along her spine.",
"The patient lives with her parents, who observe her closely 24 hours a day. She can walk by herself, with an ataxic, rigid gait. She must be constantly observed in order to be directed verbally and physically to the appropriate path. She cannot go to unfamiliar places without supervision from a responsible adult. She is also able to feed herself and has been trained to cut food into smaller pieces and use utensils."
],
"date": "October 20, 2021",
"figures": [],
"markdown": "# A Nonverbal 33-Year-Old Woman With Intellectual Impairment\n\n **Authors:** James Robert Brasic, MD, MPH \n **Date:** October 20, 2021\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 33-year-old woman presents with her parents for a routine clinic visit and to refill her medications. Presently, she lives with her parents, who are her primary caregivers and on whom she is completely dependent. She has profound intellectual impairment and is thought to have the mental capacity of an 18-month-old child. No other family members are affected.\nAccording to her parents, her birth history was unremarkable. Phenotypically normal, the patient developed and grew appropriately her first year of life. However, as a toddler, she began to lose previously acquired skills (developmental regression) and failed to attain further developmental milestones. She did not learn to talk and was diagnosed with profound intellectual disability. She received special education services to assist her with adaptive functioning.\nIn early childhood, she was diagnosed with a seizure disorder, which has been medically treated with the anticonvulsants carbamazepine and valproic acid. She has a history of orthopedic concerns. Skeletal abnormalities of note include a history of marked scoliosis and a left-sided coxa valga, which was treated by a lift in her left shoe. To treat her scoliosis, rods were placed in lateral position along her spine.\nThe patient lives with her parents, who observe her closely 24 hours a day. She can walk by herself, with an ataxic, rigid gait. She must be constantly observed in order to be directed verbally and physically to the appropriate path. She cannot go to unfamiliar places without supervision from a responsible adult. She is also able to feed herself and has been trained to cut food into smaller pieces and use utensils.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A Nonverbal 33-Year-Old Woman With Intellectual Impairment"
},
{
"authors": "James Robert Brasic, MD, MPH",
"content": [
"Upon examination, the patient is a well-developed, well-nourished young woman in no acute respiratory distress. She is awake, alert, and nonverbal.",
"The patient seems to understand and respond nonverbally to some commands but does not respond to others. She has episodes of repeated eye-blinking, followed by eye staring and unresponsiveness that lasts for several seconds. At times, she maintains a rigid posture without responding to environmental stimuli that lasts for several seconds. At other times, she stands and responds to commands instructed by the examiner. This may reflect apraxia or minor seizures, as she had been treated for seizures in the past.",
"When asked to stand still, the patient maintains that position. Her extremities are rigid. She resists being assisted by others to walk to other locations. She exhibits nonpurposeful stereotypic hand movements. Her hands are primarily held midline in a cupped position. Hand-wringing, clapping, and hand-rubbing are repeated behaviors that are noted, although she appears to have a limited range of motion to her upper extremities. She exhibits bouts of fluctuating awareness. An example of these behaviors is shown in the video below.",
"At age 29 years, an anterior-posterior radiograph of the patient's pelvis demonstrated a left-sided coxa valga (Figure 1). Both femoral heads are normally seated within the acetabula. The inferior extent of the spinal rods overlies her sacral region. In addition, bone graft material extends bilaterally about the spine.",
"Figure 1.",
"At age 33 years, a radiographic study of the patient's spine was obtained (Figure 2). Merged anterior-posterior and lateral views are presented in the image. Posterior spinal fusion of T3 to the sacrum is demonstrated. Screws, rods, crossbars, hooks, and bone graft material are present bilaterally. The hardware is intact. Significant scoliosis is absent from the images.",
"Figure 2."
],
"date": "October 20, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/878/930/878930-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/878/930/878930-Thumb2.png"
}
],
"markdown": "# A Nonverbal 33-Year-Old Woman With Intellectual Impairment\n\n **Authors:** James Robert Brasic, MD, MPH \n **Date:** October 20, 2021\n\n ## Content\n\n Upon examination, the patient is a well-developed, well-nourished young woman in no acute respiratory distress. She is awake, alert, and nonverbal.\nThe patient seems to understand and respond nonverbally to some commands but does not respond to others. She has episodes of repeated eye-blinking, followed by eye staring and unresponsiveness that lasts for several seconds. At times, she maintains a rigid posture without responding to environmental stimuli that lasts for several seconds. At other times, she stands and responds to commands instructed by the examiner. This may reflect apraxia or minor seizures, as she had been treated for seizures in the past.\nWhen asked to stand still, the patient maintains that position. Her extremities are rigid. She resists being assisted by others to walk to other locations. She exhibits nonpurposeful stereotypic hand movements. Her hands are primarily held midline in a cupped position. Hand-wringing, clapping, and hand-rubbing are repeated behaviors that are noted, although she appears to have a limited range of motion to her upper extremities. She exhibits bouts of fluctuating awareness. An example of these behaviors is shown in the video below.\nAt age 29 years, an anterior-posterior radiograph of the patient's pelvis demonstrated a left-sided coxa valga (Figure 1). Both femoral heads are normally seated within the acetabula. The inferior extent of the spinal rods overlies her sacral region. In addition, bone graft material extends bilaterally about the spine.\nFigure 1.\nAt age 33 years, a radiographic study of the patient's spine was obtained (Figure 2). Merged anterior-posterior and lateral views are presented in the image. Posterior spinal fusion of T3 to the sacrum is demonstrated. Screws, rods, crossbars, hooks, and bone graft material are present bilaterally. The hardware is intact. Significant scoliosis is absent from the images.\nFigure 2.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1088550,
"choiceText": "Cornelia de Lange syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088552,
"choiceText": "Down syndrome",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088554,
"choiceText": "Fragile X syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088556,
"choiceText": "Rett syndrome\r\n",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 344857,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Nonverbal 33-Year-Old Woman With Intellectual Impairment"
},
{
"authors": "James Robert Brasic, MD, MPH",
"content": [
"Rett syndrome is a progressive neurodevelopmental disorder that almost exclusively affects females.[1,2,3] This rare disorder was described in 1966 by Dr Andreas Rett, an Austrian pediatric neurologist. Now considered to be a syndrome of neurodevelopmental arrest, patients experience developmental regression after a period of 6-18 months of normal development. Subsequent stages of disease progression occur and are described as rapid developmental regression (onset 1-4 years), pseudostationary or plateau period (onset 2-10 years) and late motor deterioration, during which ambulatory ability decreases or ceases (approximate onset ≥ 10 y). This case illustrates progression to the fourth clinical stage of Rett syndrome, as demonstrated by the patient's marked scoliosis and radiographic evidence of orthopedic interventions.",
"In the United States, classic Rett syndrome affects 1 in 10,000 to 1 in 15,000 girls by age 12 years.[4] Undiagnosed and misdiagnosed cases make it difficult to determine the exact frequency in various populations.",
"Patients are phenotypically normal at birth. Growth and development seem normal during the first year of life. Subsequently, a deceleration in head growth can occur (acquired microcephaly). Girls with Rett syndrome lose previously acquired motor and language skills. Impaired control of voluntary movements (gait ataxia) is common, as is apraxia. Nonpurposeful stereotypic hand movements, such as hand-wringing, hand-squeezing, clapping, hand-rubbing, and repetitive hand-to-mouth movement, are distinctive, along with progressive rigidity.[5,6,7,8] A longer example of these types of behaviors that includes more detail is provided in the video below.",
"Affected females may display autistic mannerisms, feeding and swallowing difficulties, and, as in the patient in this case, a seizure disorder. Females with Rett syndrome generally have profound intellectual disability. Average life expectancy can be into the mid-40s. An increased risk for sudden death due to electrophysiologic cardiac irregularities, such as prolonged QT interval and T-wave abnormalities, is noted. Poor seizure control, aspiration pneumonia, and malnutrition are contributing factors to morbidity and mortality.",
"Most males born with Rett syndrome die in infancy. Those who survive past infancy are severely affected and are described to have a variant condition called \"MECP2-related severe neonatal encephalopathy.\" Rett syndrome is inherited as an X-linked dominant disorder. Cases are sporadic and are typically caused by a de novo mutational event on the X chromosome. This syndrome is caused by mutations in MECP2, a gene located on Xq28, that encodes for methyl-CpG–binding protein 2 (MeCP2).[1,2] Abnormal function of the MECP2 gene hinders normal production of the MeCP2 protein. This protein is critical for neuronal maturation, elaboration of synapses, and pruning of the nervous system in childhood.[9,10,11] In addition, cholinergic neurotransmission is defective in Rett syndrome.[12]",
"In patients with Rett syndrome, random X-chromosome inactivation (lyonization) affects the clinical severity of the disorder.[13,14,15,16] X-chromosome inactivation is considered skewed when more than 80% of cells reflect a single allele.[17,18,19,20] Hence, a higher percentage of an active abnormal X allele dictates a worse clinical presentation for the patient.",
"In summary, Rett syndrome is diagnosed by obtaining a clear developmental history, clinical exam, and observation of characteristic behaviors, as described in these diagnostic criteria. Rett Syndrome is primarily a clinical diagnosis. Patients diagnosed with Rett syndrome do not all carry MECP2 mutations; conversely, MECP2 mutations have been identified in patients who do not fit the clinical criteria for Rett syndrome. The consistent feature for classic Rett syndrome is a timeline of clear developmental regression, followed by limited recovery or stabilization (plateau period). That is then followed by subsequent motor deterioration. Other key criteria include loss of purposeful hand skills, stereotypic hand movements, loss of spoken language, and gait abnormalities. Deceleration of head growth can occur; however it is not considered diagnostic. Fulfillment of these diagnostic criteria can assist in the clinical diagnosis of Rett syndrome and its variant or atypical forms. Molecular genetic testing can detect mutations in the MECP2 gene and help confirm the suspected diagnosis."
],
"date": "October 20, 2021",
"figures": [],
"markdown": "# A Nonverbal 33-Year-Old Woman With Intellectual Impairment\n\n **Authors:** James Robert Brasic, MD, MPH \n **Date:** October 20, 2021\n\n ## Content\n\n Rett syndrome is a progressive neurodevelopmental disorder that almost exclusively affects females.[1,2,3] This rare disorder was described in 1966 by Dr Andreas Rett, an Austrian pediatric neurologist. Now considered to be a syndrome of neurodevelopmental arrest, patients experience developmental regression after a period of 6-18 months of normal development. Subsequent stages of disease progression occur and are described as rapid developmental regression (onset 1-4 years), pseudostationary or plateau period (onset 2-10 years) and late motor deterioration, during which ambulatory ability decreases or ceases (approximate onset ≥ 10 y). This case illustrates progression to the fourth clinical stage of Rett syndrome, as demonstrated by the patient's marked scoliosis and radiographic evidence of orthopedic interventions.\nIn the United States, classic Rett syndrome affects 1 in 10,000 to 1 in 15,000 girls by age 12 years.[4] Undiagnosed and misdiagnosed cases make it difficult to determine the exact frequency in various populations.\nPatients are phenotypically normal at birth. Growth and development seem normal during the first year of life. Subsequently, a deceleration in head growth can occur (acquired microcephaly). Girls with Rett syndrome lose previously acquired motor and language skills. Impaired control of voluntary movements (gait ataxia) is common, as is apraxia. Nonpurposeful stereotypic hand movements, such as hand-wringing, hand-squeezing, clapping, hand-rubbing, and repetitive hand-to-mouth movement, are distinctive, along with progressive rigidity.[5,6,7,8] A longer example of these types of behaviors that includes more detail is provided in the video below.\nAffected females may display autistic mannerisms, feeding and swallowing difficulties, and, as in the patient in this case, a seizure disorder. Females with Rett syndrome generally have profound intellectual disability. Average life expectancy can be into the mid-40s. An increased risk for sudden death due to electrophysiologic cardiac irregularities, such as prolonged QT interval and T-wave abnormalities, is noted. Poor seizure control, aspiration pneumonia, and malnutrition are contributing factors to morbidity and mortality.\nMost males born with Rett syndrome die in infancy. Those who survive past infancy are severely affected and are described to have a variant condition called \"MECP2-related severe neonatal encephalopathy.\" Rett syndrome is inherited as an X-linked dominant disorder. Cases are sporadic and are typically caused by a de novo mutational event on the X chromosome. This syndrome is caused by mutations in MECP2, a gene located on Xq28, that encodes for methyl-CpG–binding protein 2 (MeCP2).[1,2] Abnormal function of the MECP2 gene hinders normal production of the MeCP2 protein. This protein is critical for neuronal maturation, elaboration of synapses, and pruning of the nervous system in childhood.[9,10,11] In addition, cholinergic neurotransmission is defective in Rett syndrome.[12]\nIn patients with Rett syndrome, random X-chromosome inactivation (lyonization) affects the clinical severity of the disorder.[13,14,15,16] X-chromosome inactivation is considered skewed when more than 80% of cells reflect a single allele.[17,18,19,20] Hence, a higher percentage of an active abnormal X allele dictates a worse clinical presentation for the patient.\nIn summary, Rett syndrome is diagnosed by obtaining a clear developmental history, clinical exam, and observation of characteristic behaviors, as described in these diagnostic criteria. Rett Syndrome is primarily a clinical diagnosis. Patients diagnosed with Rett syndrome do not all carry MECP2 mutations; conversely, MECP2 mutations have been identified in patients who do not fit the clinical criteria for Rett syndrome. The consistent feature for classic Rett syndrome is a timeline of clear developmental regression, followed by limited recovery or stabilization (plateau period). That is then followed by subsequent motor deterioration. Other key criteria include loss of purposeful hand skills, stereotypic hand movements, loss of spoken language, and gait abnormalities. Deceleration of head growth can occur; however it is not considered diagnostic. Fulfillment of these diagnostic criteria can assist in the clinical diagnosis of Rett syndrome and its variant or atypical forms. Molecular genetic testing can detect mutations in the MECP2 gene and help confirm the suspected diagnosis.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1088550,
"choiceText": "Cornelia de Lange syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088552,
"choiceText": "Down syndrome",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088554,
"choiceText": "Fragile X syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088556,
"choiceText": "Rett syndrome\r\n",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 344857,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Nonverbal 33-Year-Old Woman With Intellectual Impairment"
},
{
"authors": "James Robert Brasic, MD, MPH",
"content": [
"Cornelia de Lange syndrome is a genetic disorder with phenotypic features apparent at birth. Patients with this syndrome have characteristic dysmorphic facies that include microbrachycephaly; synophrys; curly, unusually long eyelashes; a depressed nasal bridge; anteverted nares; maxillary prognathism; and micrognathia. Prenatal and postnatal growth deficiency, feeding difficulties, hypertonicity, motor delays, behavioral problems, and genitourinary and skeletal malformations are reported.[21] Intellectual disability can range from moderate to profound. A wide spectrum of phenotypic variation is observed.",
"Cornelia de Lange syndrome can be inherited as an autosomal dominant (gene location 5p13.2) or as an X-linked dominant condition. Males and females are both affected. The occurrence rate in the United States is about 1 in 10,000 live births. Many cases of Cornelia de Lange syndrome have been cited in the medical literature, and include case studies citing multiple affected siblings within families.",
"Down syndrome (also known as trisomy 21) is the most common human chromosome disorder and is caused by the presence of three copies of chromosome 21 in the patient's genotype. The population frequency in the United States is estimated to be 1 in 700 live births. It is a common cause of intellectual disability, and wide phenotypic variation is observed. Down syndrome is easily diagnosed by karyotype analysis. Interphase fluorescence in situ hybridization facilitates rapid diagnosis of Down syndrome. Laboratory assessments include investigations for possible mosaicism of trisomy 21.[22]",
"Patients with Down syndrome have a well-defined phenotype. Clinical findings include flattened occiput, shortened neck, midface hypoplasia, ocular findings (eg, epicanthal folds, upward slanting palpebral fissures, Brushfield spots), flattened nasal bridge, micrognathia, tongue protrusion, and low-set ears. Additional physical features can be extremity shortening; short, broad hands; single transverse palmar crease; noted extensibility and flexibility of joints; hypotonia; and diastasis recti. Patients are often diagnosed with hypothyroidism and cardiac and gastrointestinal problems. Congenital heart defects are diagnosed by echocardiography.[22]",
"Children with Down syndrome often have auditory and ocular concerns. Brainstem auditory evoked responses or auditory brainstem responses are used to identify hearing deficits. Ophthalmologic examinations identify visual deficits.",
"Cognitive delays may be present, along with problems associated with motor, language, and social development.[22] Intellectual disability can range from moderate to severe. An enriching home environment, early intervention, and integrated education efforts have shown a strong positive influence for children with Down syndrome. Genetic counseling, and continuity of medical care, benefit patients and their families. A comprehensive medical team approach is warranted to address involvement of various organ systems, such as the cardiac, endocrinologic, gastrointestinal, skeletal, and neurologic systems.[22]",
"Adolescents with Down syndrome merit counseling as they transition to adulthood. Caregivers can help them understand their physical activity limitations. Participating in rewarding physical activities, such as the Special Olympics, should be encouraged. Patients also may benefit from vocational training. Intellectual disabilities may limit their ability to advance to higher education. Providing long-term medical services and supportive living arrangements are warranted, as the average lifespan for these patients living in the United States is 60 years."
],
"date": "October 20, 2021",
"figures": [],
"markdown": "# A Nonverbal 33-Year-Old Woman With Intellectual Impairment\n\n **Authors:** James Robert Brasic, MD, MPH \n **Date:** October 20, 2021\n\n ## Content\n\n Cornelia de Lange syndrome is a genetic disorder with phenotypic features apparent at birth. Patients with this syndrome have characteristic dysmorphic facies that include microbrachycephaly; synophrys; curly, unusually long eyelashes; a depressed nasal bridge; anteverted nares; maxillary prognathism; and micrognathia. Prenatal and postnatal growth deficiency, feeding difficulties, hypertonicity, motor delays, behavioral problems, and genitourinary and skeletal malformations are reported.[21] Intellectual disability can range from moderate to profound. A wide spectrum of phenotypic variation is observed.\nCornelia de Lange syndrome can be inherited as an autosomal dominant (gene location 5p13.2) or as an X-linked dominant condition. Males and females are both affected. The occurrence rate in the United States is about 1 in 10,000 live births. Many cases of Cornelia de Lange syndrome have been cited in the medical literature, and include case studies citing multiple affected siblings within families.\nDown syndrome (also known as trisomy 21) is the most common human chromosome disorder and is caused by the presence of three copies of chromosome 21 in the patient's genotype. The population frequency in the United States is estimated to be 1 in 700 live births. It is a common cause of intellectual disability, and wide phenotypic variation is observed. Down syndrome is easily diagnosed by karyotype analysis. Interphase fluorescence in situ hybridization facilitates rapid diagnosis of Down syndrome. Laboratory assessments include investigations for possible mosaicism of trisomy 21.[22]\nPatients with Down syndrome have a well-defined phenotype. Clinical findings include flattened occiput, shortened neck, midface hypoplasia, ocular findings (eg, epicanthal folds, upward slanting palpebral fissures, Brushfield spots), flattened nasal bridge, micrognathia, tongue protrusion, and low-set ears. Additional physical features can be extremity shortening; short, broad hands; single transverse palmar crease; noted extensibility and flexibility of joints; hypotonia; and diastasis recti. Patients are often diagnosed with hypothyroidism and cardiac and gastrointestinal problems. Congenital heart defects are diagnosed by echocardiography.[22]\nChildren with Down syndrome often have auditory and ocular concerns. Brainstem auditory evoked responses or auditory brainstem responses are used to identify hearing deficits. Ophthalmologic examinations identify visual deficits.\nCognitive delays may be present, along with problems associated with motor, language, and social development.[22] Intellectual disability can range from moderate to severe. An enriching home environment, early intervention, and integrated education efforts have shown a strong positive influence for children with Down syndrome. Genetic counseling, and continuity of medical care, benefit patients and their families. A comprehensive medical team approach is warranted to address involvement of various organ systems, such as the cardiac, endocrinologic, gastrointestinal, skeletal, and neurologic systems.[22]\nAdolescents with Down syndrome merit counseling as they transition to adulthood. Caregivers can help them understand their physical activity limitations. Participating in rewarding physical activities, such as the Special Olympics, should be encouraged. Patients also may benefit from vocational training. Intellectual disabilities may limit their ability to advance to higher education. Providing long-term medical services and supportive living arrangements are warranted, as the average lifespan for these patients living in the United States is 60 years.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A Nonverbal 33-Year-Old Woman With Intellectual Impairment"
},
{
"authors": "James Robert Brasic, MD, MPH",
"content": [
"Fragile X syndrome is an X-linked dominant genetic disorder and is considered the most common etiology for inherited intellectual disability and autistic behaviors. Both males and females can be affected, but the impact on cognitive ability differs between the sexes. Given the X-linked inheritance, males are more seriously affected and have moderate intellectual disability, whereas females have mild impairment. In the United States, fragile X syndrome affects about 1 in 4000 males and 1 in 8000 females.[23]",
"Females with fragile X syndrome have a normal appearance, whereas affected males have distinctive phenotypic features. Salient craniofacial findings include macrocephaly; a long face; prominent forehead and chin; and large, protruding ears. Macroorchidism is seen in postpubertal males. Delayed motor development, language delay, hyperactivity, and autistic mannerisms are described in affected males with moderate intellectual disability.[24,25]",
"Fragile X syndrome is caused by a mutation in the FMR1 gene located on the X chromosome (Xq27.3). For patients, the severity of the syndrome is determined by the number of trinucleotide repeats (CGG) present within the FMR1 gene. Expansion of CGG repeats leads to an inability to produce the FMRP, a protein involved in cerebral neuronal function.",
"Early intervention programs to address intellectual deficits in patients with fragile X syndrome can help facilitate optimal growth and development. Newborn screening for fragile X syndrome has been considered, although presently, it is not available as part of the newborn screening program in the United States. Medications to address behavioral concerns and improve quality of life for patients with fragile X syndrome have been investigated.[24,25,26]",
"The female patient in this case challenge participated in an investigation to examine acetylcholine in the brains of women with Rett syndrome and healthy men and women.[27] Men with Rett syndrome are extremely rare. Because males have only one X chromosome, the defect of this X-linked condition is apparently lethal in utero, leading to miscarriages. The density of the acetylcholine vesicular transporters in the living human brain can be estimated by single-photon emission computed tomography after the administration of (-)-(2R,3R)-2-hydroxy-3-(4-phenylpiperidino)-5-[123I]iodotetralin, (-)-5-[123I]iodobenzovesamicol ([123I]IBVM).[27] The scans of the patient and three other women with Rett syndrome exhibited reduced uptake in the brain, in contrast to the scans of eight healthy men and women (Figure 3).",
"Figure 3.",
"The lower panels in the image demonstrate the average representations of the women with Rett syndrome, whereas the upper panels show the averaged images of the healthy adults. The right side of each picture corresponds to the right side of the brain. The top of each image corresponds to the anterior (front) of the brain. The panels represent transverse images at the level of the cerebellum (left), striatum (middle), and cingulate gyrus (right). Reduced uptake is demonstrated in the vermis (left lower panel), the striatum (middle lower panel), and in bilateral precentral cortices (left lower panel) and middle cingulate (right lower panel). The changes do not attain statistical significance, probably owing to the small sample sizes.[27]",
"Although this patient has the ability to feed herself and to walk without assistance, most patients diagnosed with Rett syndrome require assistance with eating, walking, dressing, toileting, and other basic activities of daily living. People with Rett syndrome typically require assistance and supervision for their entire lives owing to their profound intellectual disability, as is the situation with the patient described in this case."
],
"date": "October 20, 2021",
"figures": [
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/878/930/878930-Thumb3.png"
}
],
"markdown": "# A Nonverbal 33-Year-Old Woman With Intellectual Impairment\n\n **Authors:** James Robert Brasic, MD, MPH \n **Date:** October 20, 2021\n\n ## Content\n\n Fragile X syndrome is an X-linked dominant genetic disorder and is considered the most common etiology for inherited intellectual disability and autistic behaviors. Both males and females can be affected, but the impact on cognitive ability differs between the sexes. Given the X-linked inheritance, males are more seriously affected and have moderate intellectual disability, whereas females have mild impairment. In the United States, fragile X syndrome affects about 1 in 4000 males and 1 in 8000 females.[23]\nFemales with fragile X syndrome have a normal appearance, whereas affected males have distinctive phenotypic features. Salient craniofacial findings include macrocephaly; a long face; prominent forehead and chin; and large, protruding ears. Macroorchidism is seen in postpubertal males. Delayed motor development, language delay, hyperactivity, and autistic mannerisms are described in affected males with moderate intellectual disability.[24,25]\nFragile X syndrome is caused by a mutation in the FMR1 gene located on the X chromosome (Xq27.3). For patients, the severity of the syndrome is determined by the number of trinucleotide repeats (CGG) present within the FMR1 gene. Expansion of CGG repeats leads to an inability to produce the FMRP, a protein involved in cerebral neuronal function.\nEarly intervention programs to address intellectual deficits in patients with fragile X syndrome can help facilitate optimal growth and development. Newborn screening for fragile X syndrome has been considered, although presently, it is not available as part of the newborn screening program in the United States. Medications to address behavioral concerns and improve quality of life for patients with fragile X syndrome have been investigated.[24,25,26]\nThe female patient in this case challenge participated in an investigation to examine acetylcholine in the brains of women with Rett syndrome and healthy men and women.[27] Men with Rett syndrome are extremely rare. Because males have only one X chromosome, the defect of this X-linked condition is apparently lethal in utero, leading to miscarriages. The density of the acetylcholine vesicular transporters in the living human brain can be estimated by single-photon emission computed tomography after the administration of (-)-(2R,3R)-2-hydroxy-3-(4-phenylpiperidino)-5-[123I]iodotetralin, (-)-5-[123I]iodobenzovesamicol ([123I]IBVM).[27] The scans of the patient and three other women with Rett syndrome exhibited reduced uptake in the brain, in contrast to the scans of eight healthy men and women (Figure 3).\nFigure 3.\nThe lower panels in the image demonstrate the average representations of the women with Rett syndrome, whereas the upper panels show the averaged images of the healthy adults. The right side of each picture corresponds to the right side of the brain. The top of each image corresponds to the anterior (front) of the brain. The panels represent transverse images at the level of the cerebellum (left), striatum (middle), and cingulate gyrus (right). Reduced uptake is demonstrated in the vermis (left lower panel), the striatum (middle lower panel), and in bilateral precentral cortices (left lower panel) and middle cingulate (right lower panel). The changes do not attain statistical significance, probably owing to the small sample sizes.[27]\nAlthough this patient has the ability to feed herself and to walk without assistance, most patients diagnosed with Rett syndrome require assistance with eating, walking, dressing, toileting, and other basic activities of daily living. People with Rett syndrome typically require assistance and supervision for their entire lives owing to their profound intellectual disability, as is the situation with the patient described in this case.\n\n ## Figures\n\n **Figure 3.** \n \n\n\n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1088558,
"choiceText": "Profound intellectual disability",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088560,
"choiceText": "Borderline intellectual disability",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088562,
"choiceText": "Normal intellectual ability",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088564,
"choiceText": "Varies from borderline intellectual disability to normal ability",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "People with Rett syndrome have profound intellectual and developmental disabilities. Most require caregiver assistance for eating, dressing, toileting, walking, and other basic activities of daily living. People with Rett syndrome depend on assistance and supervision throughout their lives.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 344859,
"questionText": "Which best describes the intellectual functioning of people with Rett syndrome?\r\n",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1088566,
"choiceText": "Cornelia de Lange syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088568,
"choiceText": "Down syndrome",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088570,
"choiceText": "Fragile X syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088572,
"choiceText": "Rett syndrome",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088574,
"choiceText": "All of the above",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088576,
"choiceText": "None of the above\r\n",
"correct": false,
"displayOrder": 6,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Cornelia de Lange syndrome, Down syndrome, fragile X syndrome, and Rett syndrome are all neurodevelopmental disorders associated with intellectual impairments.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 344861,
"questionText": "Which is/are associated with a level of intellectual deficit?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Nonverbal 33-Year-Old Woman With Intellectual Impairment"
},
{
"authors": "James Robert Brasic, MD, MPH",
"content": [],
"date": "October 20, 2021",
"figures": [],
"markdown": "# A Nonverbal 33-Year-Old Woman With Intellectual Impairment\n\n **Authors:** James Robert Brasic, MD, MPH \n **Date:** October 20, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1088558,
"choiceText": "Profound intellectual disability",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088560,
"choiceText": "Borderline intellectual disability",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088562,
"choiceText": "Normal intellectual ability",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088564,
"choiceText": "Varies from borderline intellectual disability to normal ability",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "People with Rett syndrome have profound intellectual and developmental disabilities. Most require caregiver assistance for eating, dressing, toileting, walking, and other basic activities of daily living. People with Rett syndrome depend on assistance and supervision throughout their lives.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 344859,
"questionText": "Which best describes the intellectual functioning of people with Rett syndrome?\r\n",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1088566,
"choiceText": "Cornelia de Lange syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088568,
"choiceText": "Down syndrome",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088570,
"choiceText": "Fragile X syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088572,
"choiceText": "Rett syndrome",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088574,
"choiceText": "All of the above",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088576,
"choiceText": "None of the above\r\n",
"correct": false,
"displayOrder": 6,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Cornelia de Lange syndrome, Down syndrome, fragile X syndrome, and Rett syndrome are all neurodevelopmental disorders associated with intellectual impairments.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 344861,
"questionText": "Which is/are associated with a level of intellectual deficit?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Nonverbal 33-Year-Old Woman With Intellectual Impairment"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1088550,
"choiceText": "Cornelia de Lange syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088552,
"choiceText": "Down syndrome",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088554,
"choiceText": "Fragile X syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088556,
"choiceText": "Rett syndrome\r\n",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 344857,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1088558,
"choiceText": "Profound intellectual disability",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088560,
"choiceText": "Borderline intellectual disability",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088562,
"choiceText": "Normal intellectual ability",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088564,
"choiceText": "Varies from borderline intellectual disability to normal ability",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "People with Rett syndrome have profound intellectual and developmental disabilities. Most require caregiver assistance for eating, dressing, toileting, walking, and other basic activities of daily living. People with Rett syndrome depend on assistance and supervision throughout their lives.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 344859,
"questionText": "Which best describes the intellectual functioning of people with Rett syndrome?\r\n",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1088566,
"choiceText": "Cornelia de Lange syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088568,
"choiceText": "Down syndrome",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088570,
"choiceText": "Fragile X syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088572,
"choiceText": "Rett syndrome",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088574,
"choiceText": "All of the above",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1088576,
"choiceText": "None of the above\r\n",
"correct": false,
"displayOrder": 6,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Cornelia de Lange syndrome, Down syndrome, fragile X syndrome, and Rett syndrome are all neurodevelopmental disorders associated with intellectual impairments.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 344861,
"questionText": "Which is/are associated with a level of intellectual deficit?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
960397 | /viewarticle/960397 | [
{
"authors": "Paige A. Hargis, BS; Katie S. Murray, DO, MS",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 60-year-old man presents to his primary care physician with a 2-week history of gross hematuria. He has had no recent illness or exposure to sick contacts. He reports no fever or chills, shortness of breath, abdominal or flank pain, diarrhea or constipation, nausea or vomiting, fatigue, weight loss, lightheadedness, or weakness. He also denies urinary tract symptoms, including dysuria, frequency, urgency, weak stream, and incomplete emptying.",
"His past medical history is significant for rheumatic fever, mitral valve replacement, and lifelong anticoagulation with warfarin. Otherwise, he states that he is relatively healthy. He missed his most recent appointment with his cardiologist but plans to see him in 2 weeks for follow-up.",
"The patient is married and works as a mail carrier. He has a 15–pack-year smoking history, although he quit more than 10 years ago. He does not consume alcohol or use illicit drugs. His father received a diagnosis of prostate cancer in his 80s, and his sister recently received a diagnosis of lupus."
],
"date": "October 12, 2021",
"figures": [],
"markdown": "# A Mail Carrier With Gross Hematuria Whose Sister Has Lupus\n\n **Authors:** Paige A. Hargis, BS; Katie S. Murray, DO, MS \n **Date:** October 12, 2021\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 60-year-old man presents to his primary care physician with a 2-week history of gross hematuria. He has had no recent illness or exposure to sick contacts. He reports no fever or chills, shortness of breath, abdominal or flank pain, diarrhea or constipation, nausea or vomiting, fatigue, weight loss, lightheadedness, or weakness. He also denies urinary tract symptoms, including dysuria, frequency, urgency, weak stream, and incomplete emptying.\nHis past medical history is significant for rheumatic fever, mitral valve replacement, and lifelong anticoagulation with warfarin. Otherwise, he states that he is relatively healthy. He missed his most recent appointment with his cardiologist but plans to see him in 2 weeks for follow-up.\nThe patient is married and works as a mail carrier. He has a 15–pack-year smoking history, although he quit more than 10 years ago. He does not consume alcohol or use illicit drugs. His father received a diagnosis of prostate cancer in his 80s, and his sister recently received a diagnosis of lupus.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A Mail Carrier With Gross Hematuria Whose Sister Has Lupus"
},
{
"authors": "Paige A. Hargis, BS; Katie S. Murray, DO, MS",
"content": [
"Upon physical examination, the patient appears well. His temperature is 98.5 °F (36.9 °C), his blood pressure is 134/89 mm Hg, his heart rate is 76 beats/min, and his respiration rate is 14 breaths/min. Pulse oximetry shows an oxygen saturation of 99% on room air. The lungs are clear to auscultation, and breath sounds are equal. Results of the cardiac examination are unremarkable. No tenderness to palpation of the abdomen or pelvis is noted. Flank tenderness is not appreciated. Capillary refill time is < 2 seconds. Some bruising is observed on the upper extremities, but the rest of the examination reveals no obvious signs of bleeding.",
"Laboratory studies show the following values:",
"White blood cell (WBC) count: 9.07 × 109 cells/L (reference range, 4-11 × 109 cells/L)",
"Hemoglobin level: 12.0 g/dL (reference range, 13.5-15.5 g/dL)",
"Hematocrit: 41.3% (reference range, 45%-52%)",
"Platelet count: 304 × 109 cells/L (reference range, 150-400 × 109 cells/L)",
"Glucose level: 106 mg/dL (reference range, <160 mg/dL)",
"Blood urea nitrogen: 18 mg/dL (reference range, 8-24 mg/dL)",
"Creatinine level: 1.04 mg/dL (reference range, 0.9-1.3 mg/dL)",
"International normalized ratio (INR): 3.2 (reference range, 2-3)",
"Urinalysis findings are as follows:",
"Grossly bloody urine",
"Red blood cell (RBC) count: > 30 RBCs per high-power field (HPF) (reference range, ≤ 2 RBCs/HPF)",
"WBC count: 20-50 WBCs/HPF (reference range, ≤ 2-5 WBCs/HPF)",
"Leukocyte esterase and nitrites: Negative",
"Few epithelial cells",
"No bacteria",
"The patient's anticoagulation regimen is adjusted, and subsequent ultrasound does not show any masses, hydronephrosis, or stones.",
"The patient is referred to a urologist for further evaluation and workup. Two weeks after the initial urology visit, cystoscopy is performed. The findings resemble those shown below in a different patient (Figure 1).",
"Figure 1."
],
"date": "October 12, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/960/397/960397-Thumb1.jpg"
}
],
"markdown": "# A Mail Carrier With Gross Hematuria Whose Sister Has Lupus\n\n **Authors:** Paige A. Hargis, BS; Katie S. Murray, DO, MS \n **Date:** October 12, 2021\n\n ## Content\n\n Upon physical examination, the patient appears well. His temperature is 98.5 °F (36.9 °C), his blood pressure is 134/89 mm Hg, his heart rate is 76 beats/min, and his respiration rate is 14 breaths/min. Pulse oximetry shows an oxygen saturation of 99% on room air. The lungs are clear to auscultation, and breath sounds are equal. Results of the cardiac examination are unremarkable. No tenderness to palpation of the abdomen or pelvis is noted. Flank tenderness is not appreciated. Capillary refill time is < 2 seconds. Some bruising is observed on the upper extremities, but the rest of the examination reveals no obvious signs of bleeding.\nLaboratory studies show the following values:\nWhite blood cell (WBC) count: 9.07 × 109 cells/L (reference range, 4-11 × 109 cells/L)\nHemoglobin level: 12.0 g/dL (reference range, 13.5-15.5 g/dL)\nHematocrit: 41.3% (reference range, 45%-52%)\nPlatelet count: 304 × 109 cells/L (reference range, 150-400 × 109 cells/L)\nGlucose level: 106 mg/dL (reference range, <160 mg/dL)\nBlood urea nitrogen: 18 mg/dL (reference range, 8-24 mg/dL)\nCreatinine level: 1.04 mg/dL (reference range, 0.9-1.3 mg/dL)\nInternational normalized ratio (INR): 3.2 (reference range, 2-3)\nUrinalysis findings are as follows:\nGrossly bloody urine\nRed blood cell (RBC) count: > 30 RBCs per high-power field (HPF) (reference range, ≤ 2 RBCs/HPF)\nWBC count: 20-50 WBCs/HPF (reference range, ≤ 2-5 WBCs/HPF)\nLeukocyte esterase and nitrites: Negative\nFew epithelial cells\nNo bacteria\nThe patient's anticoagulation regimen is adjusted, and subsequent ultrasound does not show any masses, hydronephrosis, or stones.\nThe patient is referred to a urologist for further evaluation and workup. Two weeks after the initial urology visit, cystoscopy is performed. The findings resemble those shown below in a different patient (Figure 1).\nFigure 1.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1629088,
"choiceText": "Benign prostatic hyperplasia",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629089,
"choiceText": "Anticoagulation-associated hematuria",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629090,
"choiceText": "Urothelial cell carcinoma",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629091,
"choiceText": "Urolithiasis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629092,
"choiceText": "Cystitis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 523948,
"questionText": "On the basis of these findings only, what is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Mail Carrier With Gross Hematuria Whose Sister Has Lupus"
},
{
"authors": "Paige A. Hargis, BS; Katie S. Murray, DO, MS",
"content": [
"The differential diagnosis for hematuria is wide and involves mostly pathologies associated with the urinary tract. Conditions in the differential include the following:",
"Urinary tract infection",
"Hemorrhagic cystitis",
"Radiation cystitis",
"Prostatitis",
"Benign prostatic hyperplasia",
"Prostate cancer",
"Nephrolithiasis",
"Renal cancers",
"Glomerular and nonglomerular disease",
"Other pelvic cancers",
"Diverticulitis",
"Trauma",
"Exercise",
"Bleeding tendency",
"Idiopathic",
"All of the choices presented are possible etiologies for hematuria. Benign prostatic hyperplasia is usually accompanied by lower urinary tract symptoms, such as frequency, urgency, weak stream, and incomplete emptying, which were not present in this patient. Therefore, this diagnosis is less likely. Urolithiasis is often associated with dysuria, nausea or vomiting, and back or abdominal pain that may radiate toward the groin. The absence of these symptoms and a normal renal ultrasound reduces the likelihood of this diagnosis.",
"Cystitis can also cause pain and burning with urination, and urine testing typically shows an elevated WBC count, bacteriuria, nitrites, and a positive leukocyte esterase test. Although this patient had an elevated urine WBC count, he did not have the other characteristic urinalysis findings.",
"Anticoagulation-associated hematuria is a reasonable differential diagnosis for this patient's hematuria. However, it is more likely to be a consideration when the INR is > 4, and this patient's INR was 3.2.[1]",
"Gross hematuria in a man in his 60s with a history of cigarette smoking warrants strong suspicion for bladder cancer until proven otherwise. In addition, the cystoscopy images show a lesion on the bladder wall that supports the diagnosis of cancer. Therefore, urothelial cell carcinoma is the most likely diagnosis at this time.",
"In 2020, an estimated 81,400 new cases of urinary bladder cancer occurred, with an estimated 17,980 deaths.[2] Bladder cancer is the seventh most common cancer throughout the world, and it is the fourth most common cancer in men in the United States. Men are affected about three times more often than women.[3,4]",
"Urothelial carcinoma is by far the most common type of bladder cancer, occurring in about 90% of cases. Other types of bladder cancer include squamous cell carcinoma and adenocarcinoma. Tobacco use is the leading risk factor for the development of bladder cancer; approximately half of patients with a diagnosis of bladder cancer report a history of smoking. Other notable risk factors include exposure to dyes and rubbers, such as 4-aminobiphenyl, o-toluidine, and benzidine; chemotherapeutic agents (cyclophosphamide); and pelvic radiation therapy.[5]",
"About 80% of patients with bladder cancer report hematuria, which is the most common presenting symptom.[5] Other lower urinary tract symptoms may include dysuria, urgency, and frequency, or flank pain secondary to obstruction of the urinary tract. A pelvic mass is an atypical finding in a patient who presents with bladder cancer. In addition to generalized symptoms, such as fatigue, weight loss, and abdominal or bone pain, a mass is usually associated with metastasis.[6]"
],
"date": "October 12, 2021",
"figures": [],
"markdown": "# A Mail Carrier With Gross Hematuria Whose Sister Has Lupus\n\n **Authors:** Paige A. Hargis, BS; Katie S. Murray, DO, MS \n **Date:** October 12, 2021\n\n ## Content\n\n The differential diagnosis for hematuria is wide and involves mostly pathologies associated with the urinary tract. Conditions in the differential include the following:\nUrinary tract infection\nHemorrhagic cystitis\nRadiation cystitis\nProstatitis\nBenign prostatic hyperplasia\nProstate cancer\nNephrolithiasis\nRenal cancers\nGlomerular and nonglomerular disease\nOther pelvic cancers\nDiverticulitis\nTrauma\nExercise\nBleeding tendency\nIdiopathic\nAll of the choices presented are possible etiologies for hematuria. Benign prostatic hyperplasia is usually accompanied by lower urinary tract symptoms, such as frequency, urgency, weak stream, and incomplete emptying, which were not present in this patient. Therefore, this diagnosis is less likely. Urolithiasis is often associated with dysuria, nausea or vomiting, and back or abdominal pain that may radiate toward the groin. The absence of these symptoms and a normal renal ultrasound reduces the likelihood of this diagnosis.\nCystitis can also cause pain and burning with urination, and urine testing typically shows an elevated WBC count, bacteriuria, nitrites, and a positive leukocyte esterase test. Although this patient had an elevated urine WBC count, he did not have the other characteristic urinalysis findings.\nAnticoagulation-associated hematuria is a reasonable differential diagnosis for this patient's hematuria. However, it is more likely to be a consideration when the INR is > 4, and this patient's INR was 3.2.[1]\nGross hematuria in a man in his 60s with a history of cigarette smoking warrants strong suspicion for bladder cancer until proven otherwise. In addition, the cystoscopy images show a lesion on the bladder wall that supports the diagnosis of cancer. Therefore, urothelial cell carcinoma is the most likely diagnosis at this time.\nIn 2020, an estimated 81,400 new cases of urinary bladder cancer occurred, with an estimated 17,980 deaths.[2] Bladder cancer is the seventh most common cancer throughout the world, and it is the fourth most common cancer in men in the United States. Men are affected about three times more often than women.[3,4]\nUrothelial carcinoma is by far the most common type of bladder cancer, occurring in about 90% of cases. Other types of bladder cancer include squamous cell carcinoma and adenocarcinoma. Tobacco use is the leading risk factor for the development of bladder cancer; approximately half of patients with a diagnosis of bladder cancer report a history of smoking. Other notable risk factors include exposure to dyes and rubbers, such as 4-aminobiphenyl, o-toluidine, and benzidine; chemotherapeutic agents (cyclophosphamide); and pelvic radiation therapy.[5]\nAbout 80% of patients with bladder cancer report hematuria, which is the most common presenting symptom.[5] Other lower urinary tract symptoms may include dysuria, urgency, and frequency, or flank pain secondary to obstruction of the urinary tract. A pelvic mass is an atypical finding in a patient who presents with bladder cancer. In addition to generalized symptoms, such as fatigue, weight loss, and abdominal or bone pain, a mass is usually associated with metastasis.[6]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1629088,
"choiceText": "Benign prostatic hyperplasia",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629089,
"choiceText": "Anticoagulation-associated hematuria",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629090,
"choiceText": "Urothelial cell carcinoma",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629091,
"choiceText": "Urolithiasis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629092,
"choiceText": "Cystitis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 523948,
"questionText": "On the basis of these findings only, what is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Mail Carrier With Gross Hematuria Whose Sister Has Lupus"
},
{
"authors": "Paige A. Hargis, BS; Katie S. Murray, DO, MS",
"content": [
"Although painless hematuria should prompt suspicion of a possible underlying bladder carcinoma, other pertinent aspects of a patient's medical history may influence a provisional diagnosis and subsequently delay necessary workup. For example, in this case, the patient is receiving long-term anticoagulation, which is known to have the possible adverse effect of hematuria.[1] This situation can result in delayed referral to a urologist for further workup.",
"Anticoagulation-associated hematuria and the likelihood of underlying bladder cancer have been the subject of debate. Some studies have shown that the cause of hematuria in patients who are receiving anticoagulation is more commonly nonurologic.[1,7] However, Wallis and colleagues[8] found that patients with anticoagulation-associated hematuria were more likely to receive a diagnosis of bladder cancer than were both patients who were not taking antithrombotic medication and the general population. The risk for cancer as the underlying cause of anticoagulation-associated hematuria is not negligible. Thus, investigators recommend prompt urologic evaluation to prevent a potential detrimental delay in bladder cancer diagnosis.[1,9]Despite patients being on anticoagulation, the presence of gross hematuria should be evaluated with upper tract imaging and cystoscopy, especially among those with risk factors.",
"Timely diagnosis is important because bladder cancer can be associated with significant morbidity and mortality.[6] The clinical stage of the primary bladder tumor is one of the most important factors in determining prognosis and survival. Features that contribute to the clinical stage, such as depth of tumor invasion, are time sensitive, and delays in diagnosis are associated with worse outcomes. One study found that patients who were referred to a specialist within 14 days of symptom onset had higher survival rates than those whose evaluation was delayed past 2 weeks.[10] Therefore, early detection and diagnosis with timely intervention in patients with risk factors and clinical signs suggestive of possible bladder cancer are crucial in optimizing long-term outcomes.",
"Currently, routine screening for bladder cancer is not recommended in asymptomatic adults.[11] However, symptoms of bladder cancer, particularly hematuria, are an indication for a thorough evaluation of the urinary tract in most cases. Various diagnostic studies can be used in the evaluation of bladder cancer. Urine cytology can be useful in this setting by identifying malignant cells.[12] Reasonable imaging modalities include ultrasonography, intravenous urography, CT, and MRI. The ultrasound scan (Figure 2) and the CT scan (Figure 3) shown here reveal masses in the bladders of different patients.",
"Figure 2.",
"Figure 3.",
"Ultrasonography is typically readily available, cost-effective, and noninvasive. Its role has been evaluated in several studies, with conflicting evidence regarding its ability to identify bladder tumors.[13] In addition, the quality of imaging is operator dependent and may be limited by other factors, such as patient body habitus. Therefore, although any of these imaging studies may be obtained, cystoscopy remains the gold standard for the initial evaluation of bladder cancer.[3] It is the ideal diagnostic study because it allows for direct visualization of the bladder and any lesions or tumors that may have otherwise been difficult to detect or that were missed on imaging. The cystoscopy image shown below reveals urothelial cell carcinoma of the bladder in a different patient (Figure 4).",
"Figure 1.",
"Cystoscopy also provides information on tumor features, including location, size, and characteristics that allow classification of the tumor. Biopsy or resection of the tumor should be performed during cystoscopy to permit definitive diagnosis and histologic assessment of the depth of tumor invasion into the bladder wall muscle, which helps guide management.[5]"
],
"date": "October 12, 2021",
"figures": [
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/960/397/960397-Thumb2.jpg"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/960/397/960397-Thumb3.jpg"
},
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/960/397/960397-Thumb1.jpg"
}
],
"markdown": "# A Mail Carrier With Gross Hematuria Whose Sister Has Lupus\n\n **Authors:** Paige A. Hargis, BS; Katie S. Murray, DO, MS \n **Date:** October 12, 2021\n\n ## Content\n\n Although painless hematuria should prompt suspicion of a possible underlying bladder carcinoma, other pertinent aspects of a patient's medical history may influence a provisional diagnosis and subsequently delay necessary workup. For example, in this case, the patient is receiving long-term anticoagulation, which is known to have the possible adverse effect of hematuria.[1] This situation can result in delayed referral to a urologist for further workup.\nAnticoagulation-associated hematuria and the likelihood of underlying bladder cancer have been the subject of debate. Some studies have shown that the cause of hematuria in patients who are receiving anticoagulation is more commonly nonurologic.[1,7] However, Wallis and colleagues[8] found that patients with anticoagulation-associated hematuria were more likely to receive a diagnosis of bladder cancer than were both patients who were not taking antithrombotic medication and the general population. The risk for cancer as the underlying cause of anticoagulation-associated hematuria is not negligible. Thus, investigators recommend prompt urologic evaluation to prevent a potential detrimental delay in bladder cancer diagnosis.[1,9]Despite patients being on anticoagulation, the presence of gross hematuria should be evaluated with upper tract imaging and cystoscopy, especially among those with risk factors.\nTimely diagnosis is important because bladder cancer can be associated with significant morbidity and mortality.[6] The clinical stage of the primary bladder tumor is one of the most important factors in determining prognosis and survival. Features that contribute to the clinical stage, such as depth of tumor invasion, are time sensitive, and delays in diagnosis are associated with worse outcomes. One study found that patients who were referred to a specialist within 14 days of symptom onset had higher survival rates than those whose evaluation was delayed past 2 weeks.[10] Therefore, early detection and diagnosis with timely intervention in patients with risk factors and clinical signs suggestive of possible bladder cancer are crucial in optimizing long-term outcomes.\nCurrently, routine screening for bladder cancer is not recommended in asymptomatic adults.[11] However, symptoms of bladder cancer, particularly hematuria, are an indication for a thorough evaluation of the urinary tract in most cases. Various diagnostic studies can be used in the evaluation of bladder cancer. Urine cytology can be useful in this setting by identifying malignant cells.[12] Reasonable imaging modalities include ultrasonography, intravenous urography, CT, and MRI. The ultrasound scan (Figure 2) and the CT scan (Figure 3) shown here reveal masses in the bladders of different patients.\nFigure 2.\nFigure 3.\nUltrasonography is typically readily available, cost-effective, and noninvasive. Its role has been evaluated in several studies, with conflicting evidence regarding its ability to identify bladder tumors.[13] In addition, the quality of imaging is operator dependent and may be limited by other factors, such as patient body habitus. Therefore, although any of these imaging studies may be obtained, cystoscopy remains the gold standard for the initial evaluation of bladder cancer.[3] It is the ideal diagnostic study because it allows for direct visualization of the bladder and any lesions or tumors that may have otherwise been difficult to detect or that were missed on imaging. The cystoscopy image shown below reveals urothelial cell carcinoma of the bladder in a different patient (Figure 4).\nFigure 1.\nCystoscopy also provides information on tumor features, including location, size, and characteristics that allow classification of the tumor. Biopsy or resection of the tumor should be performed during cystoscopy to permit definitive diagnosis and histologic assessment of the depth of tumor invasion into the bladder wall muscle, which helps guide management.[5]\n\n ## Figures\n\n **Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 1.** \n \n\n\n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A Mail Carrier With Gross Hematuria Whose Sister Has Lupus"
},
{
"authors": "Paige A. Hargis, BS; Katie S. Murray, DO, MS",
"content": [
"The complications of bladder cancer are typically related to tumor burden or symptoms associated with treatment.[3] Progressive bladder cancer can cause constitutional symptoms, such as fatigue, anorexia, weight loss, and weakness. Metastatic disease can lead to the development of other symptoms depending on the location of metastasis; for example, bone metastasis can result in localized bone pain. Tumors can progress to cause symptoms of mass effect, such as urinary tract obstruction that causes hydronephrosis and eventual kidney failure. Patients may also develop symptoms related to adverse effects of chemotherapy or radiation treatment. Potential complications of surgery include urinary incontinence, erectile dysfunction, and vaginal narrowing.",
"A shared decision-making approach to discuss the treatment of bladder cancer with patients is critical.[11] Management is largely determined by the stage of the tumor, particularly whether it has invaded the muscle; other tumor characteristics; and the patient's surgical candidacy.[3] Algorithms can help guide standardized therapy in patients with bladder cancer.[11] In general, the options are surgery; chemotherapy; radiation therapy; immunotherapy; targeted therapy; or, more commonly, a combination of these treatments.[14] Common surgical interventions include transurethral resection of bladder tumor (TURBT), partial cystectomy, or radical cystectomy with urinary diversion. The video shows TURBT being performed in a different patient with bladder cancer.",
"Systemic or intravesical chemotherapy may be used, including as adjuvant or neoadjuvant therapy. Intravesical immunotherapy with bacillus Calmette-Guérin (BCG) vaccine has been associated with high survival rates in patients at elevated risk.[15] Radiation therapy may be used, usually in conjunction with chemotherapy, owing to high recurrence rates reported in patients treated with radiation alone.[11] Immunotherapy, including checkpoint inhibitors, is typically indicated in patients with refractory cancer.[11] Overall, the treatment of bladder cancer is complex, and many different factors are taken into account when determining the appropriate management strategy for each patient.",
"In this case, the patient received a diagnosis of T1 high-grade urothelial carcinoma, an aggressive form of bladder cancer. TURBT was performed, with repeated resection at 4 weeks and subsequent intravesical BCG treatment. Surveillance cystoscopy at 6 months showed no tumor recurrence.",
"This case is an example of a patient who received a delayed cancer diagnosis because of the bias toward a diagnosis of benign hematuria in a patient on anticoagulation therapy. This patient did not present with many notable symptoms, which made benign anticoagulation-associated hematuria an appealing differential diagnosis. However, painless hematuria may be the only presenting symptom in a patient with underlying bladder cancer. Owing to the potential morbidity and mortality that can be associated with bladder cancer, prompt evaluation and a thorough workup of hematuria, including cystoscopy, are necessary to rule out severe disease."
],
"date": "October 12, 2021",
"figures": [],
"markdown": "# A Mail Carrier With Gross Hematuria Whose Sister Has Lupus\n\n **Authors:** Paige A. Hargis, BS; Katie S. Murray, DO, MS \n **Date:** October 12, 2021\n\n ## Content\n\n The complications of bladder cancer are typically related to tumor burden or symptoms associated with treatment.[3] Progressive bladder cancer can cause constitutional symptoms, such as fatigue, anorexia, weight loss, and weakness. Metastatic disease can lead to the development of other symptoms depending on the location of metastasis; for example, bone metastasis can result in localized bone pain. Tumors can progress to cause symptoms of mass effect, such as urinary tract obstruction that causes hydronephrosis and eventual kidney failure. Patients may also develop symptoms related to adverse effects of chemotherapy or radiation treatment. Potential complications of surgery include urinary incontinence, erectile dysfunction, and vaginal narrowing.\nA shared decision-making approach to discuss the treatment of bladder cancer with patients is critical.[11] Management is largely determined by the stage of the tumor, particularly whether it has invaded the muscle; other tumor characteristics; and the patient's surgical candidacy.[3] Algorithms can help guide standardized therapy in patients with bladder cancer.[11] In general, the options are surgery; chemotherapy; radiation therapy; immunotherapy; targeted therapy; or, more commonly, a combination of these treatments.[14] Common surgical interventions include transurethral resection of bladder tumor (TURBT), partial cystectomy, or radical cystectomy with urinary diversion. The video shows TURBT being performed in a different patient with bladder cancer.\nSystemic or intravesical chemotherapy may be used, including as adjuvant or neoadjuvant therapy. Intravesical immunotherapy with bacillus Calmette-Guérin (BCG) vaccine has been associated with high survival rates in patients at elevated risk.[15] Radiation therapy may be used, usually in conjunction with chemotherapy, owing to high recurrence rates reported in patients treated with radiation alone.[11] Immunotherapy, including checkpoint inhibitors, is typically indicated in patients with refractory cancer.[11] Overall, the treatment of bladder cancer is complex, and many different factors are taken into account when determining the appropriate management strategy for each patient.\nIn this case, the patient received a diagnosis of T1 high-grade urothelial carcinoma, an aggressive form of bladder cancer. TURBT was performed, with repeated resection at 4 weeks and subsequent intravesical BCG treatment. Surveillance cystoscopy at 6 months showed no tumor recurrence.\nThis case is an example of a patient who received a delayed cancer diagnosis because of the bias toward a diagnosis of benign hematuria in a patient on anticoagulation therapy. This patient did not present with many notable symptoms, which made benign anticoagulation-associated hematuria an appealing differential diagnosis. However, painless hematuria may be the only presenting symptom in a patient with underlying bladder cancer. Owing to the potential morbidity and mortality that can be associated with bladder cancer, prompt evaluation and a thorough workup of hematuria, including cystoscopy, are necessary to rule out severe disease.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1629093,
"choiceText": "Smoking",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629094,
"choiceText": "Alcohol use",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629095,
"choiceText": "Chronic urinary tract infections",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629096,
"choiceText": "Age",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Smoking is the greatest risk factor for the development of bladder cancer. Approximately half of bladder cancer diagnoses occur in patients with a history of cigarette smoking.<sup>[5]</sup> Alcohol consumption does not significantly increase the risk for bladder cancer. Chronic bladder irritation or inflammation and increasing age are other risk factors that can be associated with the development of bladder cancer, but to a lesser extent than smoking.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 523949,
"questionText": "Which risk factor is most likely to be associated with a diagnosis of bladder cancer?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1629097,
"choiceText": "Ultrasonography",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629098,
"choiceText": "CT",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629099,
"choiceText": "MRI",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629100,
"choiceText": "Cystoscopy",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Cystoscopy allows for direct visualization of the tumor and is the gold standard for diagnosing bladder cancer. In addition, cystoscopy permits visualization of tumor features, such as whether it is papillary or sessile, the size of the tumor, and the presence of multiple tumors.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 523950,
"questionText": "Which diagnostic modality in the workup of bladder cancer allows for the best visualization of the tumor?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Mail Carrier With Gross Hematuria Whose Sister Has Lupus"
},
{
"authors": "Paige A. Hargis, BS; Katie S. Murray, DO, MS",
"content": [],
"date": "October 12, 2021",
"figures": [],
"markdown": "# A Mail Carrier With Gross Hematuria Whose Sister Has Lupus\n\n **Authors:** Paige A. Hargis, BS; Katie S. Murray, DO, MS \n **Date:** October 12, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1629093,
"choiceText": "Smoking",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629094,
"choiceText": "Alcohol use",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629095,
"choiceText": "Chronic urinary tract infections",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629096,
"choiceText": "Age",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Smoking is the greatest risk factor for the development of bladder cancer. Approximately half of bladder cancer diagnoses occur in patients with a history of cigarette smoking.<sup>[5]</sup> Alcohol consumption does not significantly increase the risk for bladder cancer. Chronic bladder irritation or inflammation and increasing age are other risk factors that can be associated with the development of bladder cancer, but to a lesser extent than smoking.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 523949,
"questionText": "Which risk factor is most likely to be associated with a diagnosis of bladder cancer?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1629097,
"choiceText": "Ultrasonography",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629098,
"choiceText": "CT",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629099,
"choiceText": "MRI",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629100,
"choiceText": "Cystoscopy",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Cystoscopy allows for direct visualization of the tumor and is the gold standard for diagnosing bladder cancer. In addition, cystoscopy permits visualization of tumor features, such as whether it is papillary or sessile, the size of the tumor, and the presence of multiple tumors.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 523950,
"questionText": "Which diagnostic modality in the workup of bladder cancer allows for the best visualization of the tumor?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Mail Carrier With Gross Hematuria Whose Sister Has Lupus"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1629088,
"choiceText": "Benign prostatic hyperplasia",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629089,
"choiceText": "Anticoagulation-associated hematuria",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629090,
"choiceText": "Urothelial cell carcinoma",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629091,
"choiceText": "Urolithiasis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629092,
"choiceText": "Cystitis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 523948,
"questionText": "On the basis of these findings only, what is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1629093,
"choiceText": "Smoking",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629094,
"choiceText": "Alcohol use",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629095,
"choiceText": "Chronic urinary tract infections",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629096,
"choiceText": "Age",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Smoking is the greatest risk factor for the development of bladder cancer. Approximately half of bladder cancer diagnoses occur in patients with a history of cigarette smoking.<sup>[5]</sup> Alcohol consumption does not significantly increase the risk for bladder cancer. Chronic bladder irritation or inflammation and increasing age are other risk factors that can be associated with the development of bladder cancer, but to a lesser extent than smoking.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 523949,
"questionText": "Which risk factor is most likely to be associated with a diagnosis of bladder cancer?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1629097,
"choiceText": "Ultrasonography",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629098,
"choiceText": "CT",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629099,
"choiceText": "MRI",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1629100,
"choiceText": "Cystoscopy",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Cystoscopy allows for direct visualization of the tumor and is the gold standard for diagnosing bladder cancer. In addition, cystoscopy permits visualization of tumor features, such as whether it is papillary or sessile, the size of the tumor, and the presence of multiple tumors.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 523950,
"questionText": "Which diagnostic modality in the workup of bladder cancer allows for the best visualization of the tumor?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
865890 | /viewarticle/865890 | [
{
"authors": "Manuel Salinas, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 23-year-old man is brought to the hospital by his family with complaints of malaise, fatigue, a 22-lb (10-kg) weight loss, and a 10-month history of diminished appetite. He also complains of painful tongue erosions which are covered with a white, creamy exudate. Three days after admission to the hospital, the patient's mental status progressively declines, evolving from drowsiness to confusion. He is eventually found by the nursing staff to be stuporous. Soon afterwards, the patient experiences generalized tonic-clonic seizures and sudden dense left hemiparesis.",
"At the time that the patient develops altered mental status, his family states that he has also been having increasingly severe headaches without neck stiffness or fevers. The patient has not had any known trauma. He does not have any known risk factors for tuberculosis nor has he had any ill contacts. He has no previously diagnosed medical conditions and has not been taking any medications. No significant family history is reported. His social history is remarkable only for sexual relationships with men."
],
"date": "October 05, 2021",
"figures": [],
"markdown": "# A Sexually Active 23-Year-Old With Seizures and Tongue Pain\n\n **Authors:** Manuel Salinas, MD \n **Date:** October 05, 2021\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 23-year-old man is brought to the hospital by his family with complaints of malaise, fatigue, a 22-lb (10-kg) weight loss, and a 10-month history of diminished appetite. He also complains of painful tongue erosions which are covered with a white, creamy exudate. Three days after admission to the hospital, the patient's mental status progressively declines, evolving from drowsiness to confusion. He is eventually found by the nursing staff to be stuporous. Soon afterwards, the patient experiences generalized tonic-clonic seizures and sudden dense left hemiparesis.\nAt the time that the patient develops altered mental status, his family states that he has also been having increasingly severe headaches without neck stiffness or fevers. The patient has not had any known trauma. He does not have any known risk factors for tuberculosis nor has he had any ill contacts. He has no previously diagnosed medical conditions and has not been taking any medications. No significant family history is reported. His social history is remarkable only for sexual relationships with men.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A Sexually Active 23-Year-Old With Seizures and Tongue Pain"
},
{
"authors": "Manuel Salinas, MD",
"content": [
"Upon physical examination, during the development of his altered mental status, the patient's temperature is 97.7°F (36.5°C), his pulse is regular at a rate of 100 beats/min, his blood pressure is 100/50 mm Hg, and his respiratory rate is 16 breaths/min. A normal S1 and S2 are auscultated, with no murmurs or rubs. His lungs are clear in all fields. Palpation of the abdomen reveals no tenderness, masses, or enlargement of the liver or spleen. His mucous membranes are pale and the tongue has diffuse, creamy white exudates, which, when scraped, leave a bleeding, ulcerative surface. The neurologic examination reveals stupor, a dense left-sided hemiparesis, seventh cranial nerve palsy, and an extensor plantar response on the left. No pupillary abnormalities are noted.",
"Laboratory testing is performed and includes a complete blood count (CBC) that reveals anemia with a hemoglobin concentration of 9.4 g/dL (94 g/L) and a hematocrit of 29% (0.29). His white blood cell (WBC) count is within the reference range, except for 63% (0.63) lymphocytes. The erythrocyte (globular) sedimentation rate is elevated at 62 mm/hr. Complete metabolic panel findings, including electrolytes and liver enzymes, are normal. Cerebrospinal fluid is not initially obtained because of a concern for increased intracranial pressure.",
"A CT scan of the brain is performed (Figures 1-4).",
"Figure 1.",
"Figure 2.",
"Figure 3.",
"Figure 4."
],
"date": "October 05, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/865/890/865890-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/865/890/865890-Thumb2.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/865/890/865890-Thumb3.png"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/865/890/865890-Thumb4.png"
}
],
"markdown": "# A Sexually Active 23-Year-Old With Seizures and Tongue Pain\n\n **Authors:** Manuel Salinas, MD \n **Date:** October 05, 2021\n\n ## Content\n\n Upon physical examination, during the development of his altered mental status, the patient's temperature is 97.7°F (36.5°C), his pulse is regular at a rate of 100 beats/min, his blood pressure is 100/50 mm Hg, and his respiratory rate is 16 breaths/min. A normal S1 and S2 are auscultated, with no murmurs or rubs. His lungs are clear in all fields. Palpation of the abdomen reveals no tenderness, masses, or enlargement of the liver or spleen. His mucous membranes are pale and the tongue has diffuse, creamy white exudates, which, when scraped, leave a bleeding, ulcerative surface. The neurologic examination reveals stupor, a dense left-sided hemiparesis, seventh cranial nerve palsy, and an extensor plantar response on the left. No pupillary abnormalities are noted.\nLaboratory testing is performed and includes a complete blood count (CBC) that reveals anemia with a hemoglobin concentration of 9.4 g/dL (94 g/L) and a hematocrit of 29% (0.29). His white blood cell (WBC) count is within the reference range, except for 63% (0.63) lymphocytes. The erythrocyte (globular) sedimentation rate is elevated at 62 mm/hr. Complete metabolic panel findings, including electrolytes and liver enzymes, are normal. Cerebrospinal fluid is not initially obtained because of a concern for increased intracranial pressure.\nA CT scan of the brain is performed (Figures 1-4).\nFigure 1.\nFigure 2.\nFigure 3.\nFigure 4.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 986341,
"choiceText": "Central nervous system (CNS) toxoplasmosis",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986343,
"choiceText": "Glioblastoma multiforme",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986345,
"choiceText": "Subarachnoid hemorrhage",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986347,
"choiceText": "CNS lymphoma",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 312143,
"questionText": "Based only on these findings, which is the most likely diagnosis?<br/><br/>\r\n<em>Hint: The patient's social history is critical to the diagnosis</em>.",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Sexually Active 23-Year-Old With Seizures and Tongue Pain"
},
{
"authors": "Manuel Salinas, MD",
"content": [
"The noncontrast CT scan revealed large, hypodense lesions located in the right frontal cerebral hemisphere, bilateral thalami, and basal ganglia extending into the centrum semiovale, with mild compression of the right lateral ventricle. Subsequent administration of contrast resulted in enhancement of the peripheral zone of the lesions in a typical ring pattern, suggesting CNS toxoplasmosis (images not available).",
"Toxoplasmosis is caused by the protozoan Toxoplasma gondii.[1,2] The organism is a ubiquitous coccidian parasite that infects more than 50% of individuals in some populations but does not commonly cause active disease. It has the following three forms:",
"Oocysts, which are excreted in cat feces (the definitive host)",
"Tachyzoites, which multiply intracellularly",
"Tissue cysts, the end product of this intracellular multiplication, which can persist as viable parasites in the brain and striated muscles throughout the life of the host",
"Toxoplasmosis infection usually occurs via the ingestion of oocysts or tissue cysts. The infection has four stages: acute, subacute, chronic, and reactivation. After the organisms invade and multiply within the GI tract, they spread through the lymphatic system and the bloodstream to distant organs (acute stage). Cellular and humoral immune responses then suppress disease progression and limit the parasite burden in organs. In immunocompetent hosts, the parasite encysts and persists without any inflammatory process (chronic stage). When the host becomes immunocompromised, bradyzoites are released and the parasite becomes an opportunistic agent causing disease.",
"CNS manifestations are the most frequent form of disease and occur in 10%-25% of individuals with AIDS. The affinity of T gondii for brain tissue has been conferred to low local immunity. These manifestations are initially protean and may develop insidiously. Focal neurologic signs may arise, accompanied by generalized cerebral dysfunction (drowsiness progressing into coma). Seizures may be present and may be generalized or focal. Hemianopia, aphasia, ataxia, and cranial nerve palsies may also be observed. Low-grade fever and progressive headaches are frequent symptoms. The clinical signs of CNS toxoplasmosis are typically vague and vary among patients; thus, confirming the diagnosis with radiologic and serologic studies is important.[1.2]"
],
"date": "October 05, 2021",
"figures": [],
"markdown": "# A Sexually Active 23-Year-Old With Seizures and Tongue Pain\n\n **Authors:** Manuel Salinas, MD \n **Date:** October 05, 2021\n\n ## Content\n\n The noncontrast CT scan revealed large, hypodense lesions located in the right frontal cerebral hemisphere, bilateral thalami, and basal ganglia extending into the centrum semiovale, with mild compression of the right lateral ventricle. Subsequent administration of contrast resulted in enhancement of the peripheral zone of the lesions in a typical ring pattern, suggesting CNS toxoplasmosis (images not available).\nToxoplasmosis is caused by the protozoan Toxoplasma gondii.[1,2] The organism is a ubiquitous coccidian parasite that infects more than 50% of individuals in some populations but does not commonly cause active disease. It has the following three forms:\nOocysts, which are excreted in cat feces (the definitive host)\nTachyzoites, which multiply intracellularly\nTissue cysts, the end product of this intracellular multiplication, which can persist as viable parasites in the brain and striated muscles throughout the life of the host\nToxoplasmosis infection usually occurs via the ingestion of oocysts or tissue cysts. The infection has four stages: acute, subacute, chronic, and reactivation. After the organisms invade and multiply within the GI tract, they spread through the lymphatic system and the bloodstream to distant organs (acute stage). Cellular and humoral immune responses then suppress disease progression and limit the parasite burden in organs. In immunocompetent hosts, the parasite encysts and persists without any inflammatory process (chronic stage). When the host becomes immunocompromised, bradyzoites are released and the parasite becomes an opportunistic agent causing disease.\nCNS manifestations are the most frequent form of disease and occur in 10%-25% of individuals with AIDS. The affinity of T gondii for brain tissue has been conferred to low local immunity. These manifestations are initially protean and may develop insidiously. Focal neurologic signs may arise, accompanied by generalized cerebral dysfunction (drowsiness progressing into coma). Seizures may be present and may be generalized or focal. Hemianopia, aphasia, ataxia, and cranial nerve palsies may also be observed. Low-grade fever and progressive headaches are frequent symptoms. The clinical signs of CNS toxoplasmosis are typically vague and vary among patients; thus, confirming the diagnosis with radiologic and serologic studies is important.[1.2]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 986341,
"choiceText": "Central nervous system (CNS) toxoplasmosis",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986343,
"choiceText": "Glioblastoma multiforme",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986345,
"choiceText": "Subarachnoid hemorrhage",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986347,
"choiceText": "CNS lymphoma",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 312143,
"questionText": "Based only on these findings, which is the most likely diagnosis?<br/><br/>\r\n<em>Hint: The patient's social history is critical to the diagnosis</em>.",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Sexually Active 23-Year-Old With Seizures and Tongue Pain"
},
{
"authors": "Manuel Salinas, MD",
"content": [
"Many other conditions may mimic CNS toxoplasmosis, such as chronic meningitis (especially from fungi or syphilis), cytomegalovirus encephalitis, herpes simplex encephalitis, HIV encephalitis, primary CNS lymphoma, progressive multifocal leukoencephalopathy, and malignancy (brain metastases). In patients with focal neurologic abnormalities, the presence of cerebrovascular disease (stroke) may need to be ruled out.[1.2]",
"Although serologic data are essential for confirmation, such tests are not solely diagnostic because the antibody is present in relatively high numbers in many populations. Rising serum immunoglobulin G titers are usually observed, and an immunoglobulin M antibody response is seen in cases of newly acquired toxoplasmosis. Antibody levels may be unexpectedly low in patients with AIDS, even in the presence of active disease. Isolation of T gondii from blood or body fluids or identification of tachyzoites in tissue sections or smears of body fluids (such as cerebrospinal fluid) signify acute infection. Polymerase chain reaction (PCR) amplification for the detection of T gondii DNA may also be used to clearly establish acute infection.[2]",
"Imaging is essential in the diagnosis of CNS toxoplasmosis. CT scans may reveal single or multiple bilateral, hypodense lesions with possible mass effect. In 70%-80% of cases, the lesions enhance in a homogeneous or ring pattern with contrast. Diffuse toxoplasmosis may appear on images as either normal or with findings suggestive of HIV encephalitis.",
"MRI is more sensitive in disclosing multiple lesions. When a single lesion is found in a patient with AIDS and clinical manifestations of CNS involvement, primary lymphoma is more likely, but this does not rule out toxoplasmosis. Multiple lesions may be incorrectly interpreted as multiple metastases in patients without a known history of HIV infection, so HIV and CNS toxoplasmosis must be considered in individuals with these findings and HIV risk factors.",
"Ultimately, single-photon emission computed tomography (SPECT) may be useful in differentiating lymphoma from toxoplasmosis. Whenever the diagnosis is uncertain, a brain biopsy is advocated. This option most often arises in the setting of a single mass lesion with negative serologic results and no response to empiric therapy.[1,2]"
],
"date": "October 05, 2021",
"figures": [],
"markdown": "# A Sexually Active 23-Year-Old With Seizures and Tongue Pain\n\n **Authors:** Manuel Salinas, MD \n **Date:** October 05, 2021\n\n ## Content\n\n Many other conditions may mimic CNS toxoplasmosis, such as chronic meningitis (especially from fungi or syphilis), cytomegalovirus encephalitis, herpes simplex encephalitis, HIV encephalitis, primary CNS lymphoma, progressive multifocal leukoencephalopathy, and malignancy (brain metastases). In patients with focal neurologic abnormalities, the presence of cerebrovascular disease (stroke) may need to be ruled out.[1.2]\nAlthough serologic data are essential for confirmation, such tests are not solely diagnostic because the antibody is present in relatively high numbers in many populations. Rising serum immunoglobulin G titers are usually observed, and an immunoglobulin M antibody response is seen in cases of newly acquired toxoplasmosis. Antibody levels may be unexpectedly low in patients with AIDS, even in the presence of active disease. Isolation of T gondii from blood or body fluids or identification of tachyzoites in tissue sections or smears of body fluids (such as cerebrospinal fluid) signify acute infection. Polymerase chain reaction (PCR) amplification for the detection of T gondii DNA may also be used to clearly establish acute infection.[2]\nImaging is essential in the diagnosis of CNS toxoplasmosis. CT scans may reveal single or multiple bilateral, hypodense lesions with possible mass effect. In 70%-80% of cases, the lesions enhance in a homogeneous or ring pattern with contrast. Diffuse toxoplasmosis may appear on images as either normal or with findings suggestive of HIV encephalitis.\nMRI is more sensitive in disclosing multiple lesions. When a single lesion is found in a patient with AIDS and clinical manifestations of CNS involvement, primary lymphoma is more likely, but this does not rule out toxoplasmosis. Multiple lesions may be incorrectly interpreted as multiple metastases in patients without a known history of HIV infection, so HIV and CNS toxoplasmosis must be considered in individuals with these findings and HIV risk factors.\nUltimately, single-photon emission computed tomography (SPECT) may be useful in differentiating lymphoma from toxoplasmosis. Whenever the diagnosis is uncertain, a brain biopsy is advocated. This option most often arises in the setting of a single mass lesion with negative serologic results and no response to empiric therapy.[1,2]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A Sexually Active 23-Year-Old With Seizures and Tongue Pain"
},
{
"authors": "Manuel Salinas, MD",
"content": [
"Toxoplasmosis treatment is often empiric in the appropriate clinical setting, pending confirmatory testing. The standard regimen for treating acute infection is a combination of three drugs given for 6 weeks: pyrimethamine, sulfadiazine, and folinic acid. Cotrimoxazole (trimethoprim-sulfamethoxazole) can be used as an alternative regimen; it is better tolerated with no differences in the clinical outcomes.",
"In cases of allergy to sulfa drugs, clindamycin, clarithromycin, azithromycin, or atovaquone combined with pyrimethamine and folinic acid are viable alternatives. The treatment of acute infection should last 4-6 weeks and is followed by long-term suppressive therapy at reduced doses. The initiation of highly active antiretroviral therapy (HAART) for HIV is as important as the treatment of acute infection. Suppressive therapy should continue until CD4 counts remain > 200 cells/µL and lesions are no longer detected on MRI.[3,4]",
"In this patient, the history of sex with men combined with the physical finding of lesions on the tongue, compatible with thrush, led to the suspicion of HIV infection. Because the neurologic state of the patient had declined and there was a possibility of immunodeficiency, a decision was made to treat for bacterial meningitis and to also treat empirically for CNS toxoplasmosis, given the results of the noncontrast CT scan of the head, pending the serologic results. A lumbar puncture was considered but was deferred as a result of concern for neurologic complications stemming from evidence of increased intracranial pressure on the noncontrast CT scan of the head. HAART was also initiated empirically.",
"With treatment, the patient's mental status improved and, over a period of time, he progressively returned to normal mentation. HIV infection was confirmed by serologic studies (ie, enzyme-linked immunosorbent assay [ELISA] and Western blot), and the patient was noted to have a decreased CD4 count (< 150 cells/µL). A week later, therapy with pyrimethamine, sulfadiazine, and folinic acid was initiated. The patient was eventually discharged with only a mild language disturbance and a discreet motor deficit in his left leg."
],
"date": "October 05, 2021",
"figures": [],
"markdown": "# A Sexually Active 23-Year-Old With Seizures and Tongue Pain\n\n **Authors:** Manuel Salinas, MD \n **Date:** October 05, 2021\n\n ## Content\n\n Toxoplasmosis treatment is often empiric in the appropriate clinical setting, pending confirmatory testing. The standard regimen for treating acute infection is a combination of three drugs given for 6 weeks: pyrimethamine, sulfadiazine, and folinic acid. Cotrimoxazole (trimethoprim-sulfamethoxazole) can be used as an alternative regimen; it is better tolerated with no differences in the clinical outcomes.\nIn cases of allergy to sulfa drugs, clindamycin, clarithromycin, azithromycin, or atovaquone combined with pyrimethamine and folinic acid are viable alternatives. The treatment of acute infection should last 4-6 weeks and is followed by long-term suppressive therapy at reduced doses. The initiation of highly active antiretroviral therapy (HAART) for HIV is as important as the treatment of acute infection. Suppressive therapy should continue until CD4 counts remain > 200 cells/µL and lesions are no longer detected on MRI.[3,4]\nIn this patient, the history of sex with men combined with the physical finding of lesions on the tongue, compatible with thrush, led to the suspicion of HIV infection. Because the neurologic state of the patient had declined and there was a possibility of immunodeficiency, a decision was made to treat for bacterial meningitis and to also treat empirically for CNS toxoplasmosis, given the results of the noncontrast CT scan of the head, pending the serologic results. A lumbar puncture was considered but was deferred as a result of concern for neurologic complications stemming from evidence of increased intracranial pressure on the noncontrast CT scan of the head. HAART was also initiated empirically.\nWith treatment, the patient's mental status improved and, over a period of time, he progressively returned to normal mentation. HIV infection was confirmed by serologic studies (ie, enzyme-linked immunosorbent assay [ELISA] and Western blot), and the patient was noted to have a decreased CD4 count (< 150 cells/µL). A week later, therapy with pyrimethamine, sulfadiazine, and folinic acid was initiated. The patient was eventually discharged with only a mild language disturbance and a discreet motor deficit in his left leg.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 986349,
"choiceText": "Seizures",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986351,
"choiceText": "Focal neurologic deficit ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986353,
"choiceText": "Language disturbances",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986355,
"choiceText": "Coma",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986357,
"choiceText": "All of the above",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Toxoplasmosis involvement in the CNS can be expressed by almost any neurologic symptom. The natural history of CNS toxoplasmosis includes vague constitutional symptoms followed by confusion and drowsiness, seizures, focal weakness, and language disturbances. If no treatment is started, progression to coma in days to weeks is inevitable. Personality and mental status changes, hemiparesis, hemianopia, aphasia, ataxia, and cranial nerve palsies are common.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 312145,
"questionText": "Which of the following clinical manifestations is commonly seen in cases of CNS toxoplasmosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 986359,
"choiceText": "Cerebral metastases",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986361,
"choiceText": "Primary CNS lymphoma",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986363,
"choiceText": "Progressive multifocal leukoencephalopathy",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986365,
"choiceText": "Cytomegalovirus encephalitis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986367,
"choiceText": "Stroke",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "SPECT may be useful in differentiating lymphoma from toxoplasmosis. Whenever the diagnosis is uncertain, a brain biopsy is advocated. This option most often arises in the setting of a single mass lesion with negative serologic results and no response to empiric therapy.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 312147,
"questionText": "Which of the following conditions is most likely in a patient with AIDS and a single mass lesion found on cranial imaging studies?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Sexually Active 23-Year-Old With Seizures and Tongue Pain"
},
{
"authors": "Manuel Salinas, MD",
"content": [],
"date": "October 05, 2021",
"figures": [],
"markdown": "# A Sexually Active 23-Year-Old With Seizures and Tongue Pain\n\n **Authors:** Manuel Salinas, MD \n **Date:** October 05, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 986349,
"choiceText": "Seizures",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986351,
"choiceText": "Focal neurologic deficit ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986353,
"choiceText": "Language disturbances",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986355,
"choiceText": "Coma",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986357,
"choiceText": "All of the above",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Toxoplasmosis involvement in the CNS can be expressed by almost any neurologic symptom. The natural history of CNS toxoplasmosis includes vague constitutional symptoms followed by confusion and drowsiness, seizures, focal weakness, and language disturbances. If no treatment is started, progression to coma in days to weeks is inevitable. Personality and mental status changes, hemiparesis, hemianopia, aphasia, ataxia, and cranial nerve palsies are common.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 312145,
"questionText": "Which of the following clinical manifestations is commonly seen in cases of CNS toxoplasmosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 986359,
"choiceText": "Cerebral metastases",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986361,
"choiceText": "Primary CNS lymphoma",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986363,
"choiceText": "Progressive multifocal leukoencephalopathy",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986365,
"choiceText": "Cytomegalovirus encephalitis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986367,
"choiceText": "Stroke",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "SPECT may be useful in differentiating lymphoma from toxoplasmosis. Whenever the diagnosis is uncertain, a brain biopsy is advocated. This option most often arises in the setting of a single mass lesion with negative serologic results and no response to empiric therapy.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 312147,
"questionText": "Which of the following conditions is most likely in a patient with AIDS and a single mass lesion found on cranial imaging studies?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Sexually Active 23-Year-Old With Seizures and Tongue Pain"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 986341,
"choiceText": "Central nervous system (CNS) toxoplasmosis",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986343,
"choiceText": "Glioblastoma multiforme",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986345,
"choiceText": "Subarachnoid hemorrhage",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986347,
"choiceText": "CNS lymphoma",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 312143,
"questionText": "Based only on these findings, which is the most likely diagnosis?<br/><br/>\r\n<em>Hint: The patient's social history is critical to the diagnosis</em>.",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 986349,
"choiceText": "Seizures",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986351,
"choiceText": "Focal neurologic deficit ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986353,
"choiceText": "Language disturbances",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986355,
"choiceText": "Coma",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986357,
"choiceText": "All of the above",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Toxoplasmosis involvement in the CNS can be expressed by almost any neurologic symptom. The natural history of CNS toxoplasmosis includes vague constitutional symptoms followed by confusion and drowsiness, seizures, focal weakness, and language disturbances. If no treatment is started, progression to coma in days to weeks is inevitable. Personality and mental status changes, hemiparesis, hemianopia, aphasia, ataxia, and cranial nerve palsies are common.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 312145,
"questionText": "Which of the following clinical manifestations is commonly seen in cases of CNS toxoplasmosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 986359,
"choiceText": "Cerebral metastases",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986361,
"choiceText": "Primary CNS lymphoma",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986363,
"choiceText": "Progressive multifocal leukoencephalopathy",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986365,
"choiceText": "Cytomegalovirus encephalitis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 986367,
"choiceText": "Stroke",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "SPECT may be useful in differentiating lymphoma from toxoplasmosis. Whenever the diagnosis is uncertain, a brain biopsy is advocated. This option most often arises in the setting of a single mass lesion with negative serologic results and no response to empiric therapy.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 312147,
"questionText": "Which of the following conditions is most likely in a patient with AIDS and a single mass lesion found on cranial imaging studies?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
861792 | /viewarticle/861792 | [
{
"authors": "Andrea Bianchin, MD; Moreno Agostini, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 30-year-old woman presents to the emergency department with malaise, diffuse myalgia, and a rash that has spread all over her body (Figures 1 and 2).",
"Figure 1.",
"Figure 2.",
"Her symptoms began the day before presentation and initially improved with ibuprofen. Her boyfriend, who has accompanied her to the emergency department, adds that she has been vomiting, has appeared to be in pain with movement, and has had intermittent confusion during the night.",
"The patient has developed a headache of moderate intensity that is diffuse, radiates to her neck, and worsens with movement. She does not have any photophobia or dizziness, and she has not experienced any seizures. She denies having subjective fever, abdominal pain, hematemesis, or diarrhea. She has not had any urinary symptoms or low back pain. She denies having cough or shortness of breath.",
"The patient's medical history is remarkable only for trauma that occurred 3 months ago and resulted in rib fractures and blunt abdominal trauma. At that time, she underwent exploratory laparotomy, with suture repair of liver lacerations and a right kidney laceration; she has been doing well since then. The patient does not have any chronic medical conditions and does not take any regular medications. She smokes cigarettes but denies heavy alcohol use or illicit drug use."
],
"date": "September 22, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/861/792/861792-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/861/792/861792-Thumb2.png"
}
],
"markdown": "# A 30-Year-Old With a Full-Body Rash, Vomiting, and Confusion\n\n **Authors:** Andrea Bianchin, MD; Moreno Agostini, MD \n **Date:** September 22, 2021\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 30-year-old woman presents to the emergency department with malaise, diffuse myalgia, and a rash that has spread all over her body (Figures 1 and 2).\nFigure 1.\nFigure 2.\nHer symptoms began the day before presentation and initially improved with ibuprofen. Her boyfriend, who has accompanied her to the emergency department, adds that she has been vomiting, has appeared to be in pain with movement, and has had intermittent confusion during the night.\nThe patient has developed a headache of moderate intensity that is diffuse, radiates to her neck, and worsens with movement. She does not have any photophobia or dizziness, and she has not experienced any seizures. She denies having subjective fever, abdominal pain, hematemesis, or diarrhea. She has not had any urinary symptoms or low back pain. She denies having cough or shortness of breath.\nThe patient's medical history is remarkable only for trauma that occurred 3 months ago and resulted in rib fractures and blunt abdominal trauma. At that time, she underwent exploratory laparotomy, with suture repair of liver lacerations and a right kidney laceration; she has been doing well since then. The patient does not have any chronic medical conditions and does not take any regular medications. She smokes cigarettes but denies heavy alcohol use or illicit drug use.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A 30-Year-Old With a Full-Body Rash, Vomiting, and Confusion"
},
{
"authors": "Andrea Bianchin, MD; Moreno Agostini, MD",
"content": [
"Upon physical examination, the patient appears drowsy and uncomfortable. Her oral temperature is 100.9°F [38.3°C]. She is tachycardic and hypotensive, with a heart rate of 120 beats/min and a blood pressure of 80/60 mm Hg. Her respiratory rate and oxygen saturation are normal (at 16 breaths/min and 99% while breathing room air, respectively). She grimaces in pain with movement of the joints—particularly with movement of her neck, which is limited. Her pupils are 3 mm and equally reactive. Her neurologic examination findings, including a cranial nerve inspection, are normal (except for her drowsy mental status).",
"The patient has a nonpainful purpuric rash on her arms, trunk, and face consisting of patchy macules approximately 1-4 cm in diameter (Figures 1 and 2).",
"Figure 1.",
"Figure 1.",
"Figure 2.",
"No cervical, axillary, or inguinal lymphadenopathy is noted. Her lungs are clear, and her heart sounds are normal, without any murmurs or gallops. She has a soft and nontender abdomen, with no splenomegaly. No midline spinal tenderness or costovertebral angle tenderness is detected. No evidence suggests joint involvement, and no tenderness or swelling is noted. The remainder of the examination is unremarkable.",
"Laboratory studies show an elevated white blood cell count of 17.6 × 103 cells/µL, a hemoglobin level of 13.6 g/dL (reference range, 12-15.5 g/dL), and a platelet count of 54 × 103 cells/µL (reference range, 15-40 × 103 cells/µL). Her creatinine level is 3.3 mg/dL (reference range, 0.74-1.35 mg/dL), and her blood urea nitrogen level is 57 mg/dL (reference range, 10-20 mg/dL). Electrolyte concentrations and hepatic studies are normal.",
"The patient's myoglobin and creatine kinase concentrations are elevated, at 332 µg/L and 149 U/L, respectively. The C-reactive protein level is high, at 22 mg/dL. The partial thromboplastin time is elevated at > 120 seconds, and the international normalized ratio is 2.14. The D-dimer value is markedly elevated, at > 10 µg/mL. A serum pregnancy test is negative.",
"Arterial blood gas analysis shows a pH of 7.3 (reference range, 7.35-7.45), a lactate level of 64.9 mg/dL (reference range, 4.5-19.8 mg/dL), a partial pressure of carbon dioxide of 35.4 mm Hg (reference range, 35-45 mm/Hg), a partial pressure of oxygen of 318 mm Hg (reference range, 75-100 mm Hg), and an oxygen saturation of 99.3% (reference range, ≥ 95%) while using an oxygen mask at 10 L/min. Blood is drawn for culture and sent to the laboratory."
],
"date": "September 22, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/861/792/861792-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/861/792/861792-Thumb2.png"
}
],
"markdown": "# A 30-Year-Old With a Full-Body Rash, Vomiting, and Confusion\n\n **Authors:** Andrea Bianchin, MD; Moreno Agostini, MD \n **Date:** September 22, 2021\n\n ## Content\n\n Upon physical examination, the patient appears drowsy and uncomfortable. Her oral temperature is 100.9°F [38.3°C]. She is tachycardic and hypotensive, with a heart rate of 120 beats/min and a blood pressure of 80/60 mm Hg. Her respiratory rate and oxygen saturation are normal (at 16 breaths/min and 99% while breathing room air, respectively). She grimaces in pain with movement of the joints—particularly with movement of her neck, which is limited. Her pupils are 3 mm and equally reactive. Her neurologic examination findings, including a cranial nerve inspection, are normal (except for her drowsy mental status).\nThe patient has a nonpainful purpuric rash on her arms, trunk, and face consisting of patchy macules approximately 1-4 cm in diameter (Figures 1 and 2).\nFigure 1.\nFigure 1.\nFigure 2.\nNo cervical, axillary, or inguinal lymphadenopathy is noted. Her lungs are clear, and her heart sounds are normal, without any murmurs or gallops. She has a soft and nontender abdomen, with no splenomegaly. No midline spinal tenderness or costovertebral angle tenderness is detected. No evidence suggests joint involvement, and no tenderness or swelling is noted. The remainder of the examination is unremarkable.\nLaboratory studies show an elevated white blood cell count of 17.6 × 103 cells/µL, a hemoglobin level of 13.6 g/dL (reference range, 12-15.5 g/dL), and a platelet count of 54 × 103 cells/µL (reference range, 15-40 × 103 cells/µL). Her creatinine level is 3.3 mg/dL (reference range, 0.74-1.35 mg/dL), and her blood urea nitrogen level is 57 mg/dL (reference range, 10-20 mg/dL). Electrolyte concentrations and hepatic studies are normal.\nThe patient's myoglobin and creatine kinase concentrations are elevated, at 332 µg/L and 149 U/L, respectively. The C-reactive protein level is high, at 22 mg/dL. The partial thromboplastin time is elevated at > 120 seconds, and the international normalized ratio is 2.14. The D-dimer value is markedly elevated, at > 10 µg/mL. A serum pregnancy test is negative.\nArterial blood gas analysis shows a pH of 7.3 (reference range, 7.35-7.45), a lactate level of 64.9 mg/dL (reference range, 4.5-19.8 mg/dL), a partial pressure of carbon dioxide of 35.4 mm Hg (reference range, 35-45 mm/Hg), a partial pressure of oxygen of 318 mm Hg (reference range, 75-100 mm Hg), and an oxygen saturation of 99.3% (reference range, ≥ 95%) while using an oxygen mask at 10 L/min. Blood is drawn for culture and sent to the laboratory.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 957705,
"choiceText": "Toxic shock syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957707,
"choiceText": "Waterhouse-Friderichsen syndrome",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957709,
"choiceText": "Acute necrotizing pancreatitis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957711,
"choiceText": "Acute respiratory distress syndrome\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 302893,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 30-Year-Old With a Full-Body Rash, Vomiting, and Confusion"
},
{
"authors": "Andrea Bianchin, MD; Moreno Agostini, MD",
"content": [
"Waterhouse-Friderichsen syndrome is a severe complication of Neisseria meningitidis infection. N meningitidis is a gram-negative aerobic diplococcus with a particular affinity for the bloodstream and meninges. Infection with N meningitidis may cause clinical conditions ranging from fever and bacteremia to life-threatening septic shock.",
"N meningitidis is a commensal bacterium in many humans that resides in the nasopharynx and colonizes up to 25% of healthy people, without causing illness. It is transmitted by aerosolized respiratory particles and secretions.",
"The reason why some people who carry invasive strains of the bacteria become ill whereas others do not is unclear. A particular virulence factor may be a cause but is not fully understood. Crowded living conditions, such as college dormitories and military barracks, increase the risk for transmission. Other risk factors include smoking and upper respiratory tract infection, as well as systemic diseases, such as multiple myeloma, nephrotic syndrome, or systemic lupus erythematosus.",
"Immune defects, deficiency of humoral immunity or the complement-mediated immune system, and anatomical or functional asplenia predispose patients to N meningitidis infection, with a relative risk of 500 in asplenic patients. Outbreaks of N meningitidis infection appear to be seasonal, occurring most often in spring and winter. The yearly incidence of the disease is about 1 case per 100,000 people.[1,2,3,4,5]",
"N meningitidis spreads through the inhalation of respiratory secretions transmitted by a carrier. The onset of symptoms occurs approximately 3-4 days after inoculation. The patient typically begins to have symptoms of a respiratory illness, followed by fever, headache, and vomiting; this rapidly progresses to the development of mental status changes (such as lethargy or confusion).",
"Meningeal infection probably results from hematogenous spread; N meningitidis can be isolated via blood cultures in approximately 75% of patients. Meningococcal sepsis with multisystem involvement, however, occurs in only one fifth of cases of meningitis caused by N meningitidis.",
"The mortality rate of meningococcal sepsis is very high; it is even more lethal than isolated meningococcal meningitis. Waterhouse-Friderichsen syndrome is one of the most severe complications of meningococcal infection. Although often classified by the presence of multiorgan dysfunction in the presence of meningococcal infection, the syndrome is typically more specifically defined by the presence of hemorrhage into the adrenal glands.[2,3,4]",
"A typical purpuric rash may be seen as a result of septicemia. This usually first appears on the trunk and lower extremities and subsequently spreads throughout the body surface. The development of purpura fulminans (PF) - a life-threatening hemorrhagic condition characterized by hypotension, disseminated intravascular coagulation (DIC), and purpura - indicates a poor prognosis.",
"Although the presence of PF is classic for meningococcal infection, multiple causes may be responsible and should also be considered. Three general categories of PF are recognized: acute infectious PF, idiopathic PF, and abnormalities of the coagulation system. In fact, most PF cases are caused by coagulation abnormalities. Occasionally, meningococcal infection causes only focal disease, such as conjunctivitis, septic arthritis, urethritis, purulent pericarditis, or respiratory tract infection (eg, pneumonia, epiglottitis, and otitis media).[2]"
],
"date": "September 22, 2021",
"figures": [],
"markdown": "# A 30-Year-Old With a Full-Body Rash, Vomiting, and Confusion\n\n **Authors:** Andrea Bianchin, MD; Moreno Agostini, MD \n **Date:** September 22, 2021\n\n ## Content\n\n Waterhouse-Friderichsen syndrome is a severe complication of Neisseria meningitidis infection. N meningitidis is a gram-negative aerobic diplococcus with a particular affinity for the bloodstream and meninges. Infection with N meningitidis may cause clinical conditions ranging from fever and bacteremia to life-threatening septic shock.\nN meningitidis is a commensal bacterium in many humans that resides in the nasopharynx and colonizes up to 25% of healthy people, without causing illness. It is transmitted by aerosolized respiratory particles and secretions.\nThe reason why some people who carry invasive strains of the bacteria become ill whereas others do not is unclear. A particular virulence factor may be a cause but is not fully understood. Crowded living conditions, such as college dormitories and military barracks, increase the risk for transmission. Other risk factors include smoking and upper respiratory tract infection, as well as systemic diseases, such as multiple myeloma, nephrotic syndrome, or systemic lupus erythematosus.\nImmune defects, deficiency of humoral immunity or the complement-mediated immune system, and anatomical or functional asplenia predispose patients to N meningitidis infection, with a relative risk of 500 in asplenic patients. Outbreaks of N meningitidis infection appear to be seasonal, occurring most often in spring and winter. The yearly incidence of the disease is about 1 case per 100,000 people.[1,2,3,4,5]\nN meningitidis spreads through the inhalation of respiratory secretions transmitted by a carrier. The onset of symptoms occurs approximately 3-4 days after inoculation. The patient typically begins to have symptoms of a respiratory illness, followed by fever, headache, and vomiting; this rapidly progresses to the development of mental status changes (such as lethargy or confusion).\nMeningeal infection probably results from hematogenous spread; N meningitidis can be isolated via blood cultures in approximately 75% of patients. Meningococcal sepsis with multisystem involvement, however, occurs in only one fifth of cases of meningitis caused by N meningitidis.\nThe mortality rate of meningococcal sepsis is very high; it is even more lethal than isolated meningococcal meningitis. Waterhouse-Friderichsen syndrome is one of the most severe complications of meningococcal infection. Although often classified by the presence of multiorgan dysfunction in the presence of meningococcal infection, the syndrome is typically more specifically defined by the presence of hemorrhage into the adrenal glands.[2,3,4]\nA typical purpuric rash may be seen as a result of septicemia. This usually first appears on the trunk and lower extremities and subsequently spreads throughout the body surface. The development of purpura fulminans (PF) - a life-threatening hemorrhagic condition characterized by hypotension, disseminated intravascular coagulation (DIC), and purpura - indicates a poor prognosis.\nAlthough the presence of PF is classic for meningococcal infection, multiple causes may be responsible and should also be considered. Three general categories of PF are recognized: acute infectious PF, idiopathic PF, and abnormalities of the coagulation system. In fact, most PF cases are caused by coagulation abnormalities. Occasionally, meningococcal infection causes only focal disease, such as conjunctivitis, septic arthritis, urethritis, purulent pericarditis, or respiratory tract infection (eg, pneumonia, epiglottitis, and otitis media).[2]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 957705,
"choiceText": "Toxic shock syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957707,
"choiceText": "Waterhouse-Friderichsen syndrome",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957709,
"choiceText": "Acute necrotizing pancreatitis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957711,
"choiceText": "Acute respiratory distress syndrome\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 302893,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 30-Year-Old With a Full-Body Rash, Vomiting, and Confusion"
},
{
"authors": "Andrea Bianchin, MD; Moreno Agostini, MD",
"content": [
"The diagnosis of Waterhouse-Friderichsen syndrome (or of meningococcal sepsis in general) must be made early and should be based on the clinical features of fever, purpuric rash, altered mental status, meningeal signs, hypotension, and septic shock. Specific testing should be used for confirmation and for guiding subsequent treatment, but it should not delay the initiation of therapy. An effort should be made to obtain blood cultures before administering antibiotics to the patient. The results are not typically available for 12-24 hours; however, they may guide subsequent therapy. Lumbar puncture should be performed early in the course of treatment, but it should not delay the administration of antibiotics. Cerebrospinal fluid analysis should include a cell count and differential, culture, Gram stain, and protein and glucose concentrations.",
"The presence of meningitis is identified by leukocytosis with polymorphonuclear predominance, an elevated protein concentration, and a low glucose concentration. Gram stains are often negative in meningitis. Cultures may also be obtained from synovial, pleural, or pericardial fluid, if appropriate.",
"Methods for identifying meningococcus other than culture are available, such as antigen detection from biological fluids. This method is rapid and can provide an exact identification of the serogroup, but it commonly produces false-negative results. Polymerase chain reaction can also identify specific serogroups and does not require the presence of a live organism.[4]",
"Without prompt treatment, the mortality rate of Waterhouse-Friderichsen syndrome approaches 100%. Even with rapid and optimal medical therapy, approximately 40% of patients with meningococcal sepsis do not survive. When DIC is present, the mortality rate is as high as 90%. The overall mortality of meningococcal disease is 10%-20%, with the same percentage of survivors having permanent neurologic sequelae (ie, neurologic disability, loss of a limb, and hearing impairment).[4,5]",
"The most important therapeutic point for meningococcal infection is early administration of appropriate antibiotics. Empirical antibiotics should be administered whenever meningococcal infection is suspected because delays in therapy expose patients to risk for severe illness, permanent disability, or death.",
"Common antimicrobial agents are active against Neisseria species. Penicillin G is usually the first-line antibiotic therapy; it has a low prevalence of resistance. In areas where penicillin-resistant strains have been identified, such as the United Kingdom or Spain, a third-generation cephalosporin can be used instead. Initial treatment with broad-spectrum antibiotics is recommended in all sepsis cases because antibiotic treatment can later be changed once a specific organism is identified.",
"Early goal-directed therapy should be initiated, with a particular focus on fluid administration and maintenance of adequate blood pressure. The efficacy of corticosteroid treatment is controversial, but it is typically recommended in cases of sepsis and meningitis. Debridement of skin and subcutaneous tissues, with subsequent skin grafting or limb amputation, may be necessary if septicemia results in peripheral hypoperfusion with skin and bone necrosis.",
"In cases of fulminant meningococcemia, patients should be immediately transferred to an intensive care unit for aggressive fluid therapy, vasopressor support, and intensive hemodynamic monitoring. Activated protein C may be of use in a very limited number of patients.",
"Treatment of DIC includes administration of fresh frozen plasma. Additional treatments currently under investigation include monoclonal antibodies to inflammatory mediators, such as endotoxins, tumor necrosis factor, interleukins, and interferon gamma.[4,5]"
],
"date": "September 22, 2021",
"figures": [],
"markdown": "# A 30-Year-Old With a Full-Body Rash, Vomiting, and Confusion\n\n **Authors:** Andrea Bianchin, MD; Moreno Agostini, MD \n **Date:** September 22, 2021\n\n ## Content\n\n The diagnosis of Waterhouse-Friderichsen syndrome (or of meningococcal sepsis in general) must be made early and should be based on the clinical features of fever, purpuric rash, altered mental status, meningeal signs, hypotension, and septic shock. Specific testing should be used for confirmation and for guiding subsequent treatment, but it should not delay the initiation of therapy. An effort should be made to obtain blood cultures before administering antibiotics to the patient. The results are not typically available for 12-24 hours; however, they may guide subsequent therapy. Lumbar puncture should be performed early in the course of treatment, but it should not delay the administration of antibiotics. Cerebrospinal fluid analysis should include a cell count and differential, culture, Gram stain, and protein and glucose concentrations.\nThe presence of meningitis is identified by leukocytosis with polymorphonuclear predominance, an elevated protein concentration, and a low glucose concentration. Gram stains are often negative in meningitis. Cultures may also be obtained from synovial, pleural, or pericardial fluid, if appropriate.\nMethods for identifying meningococcus other than culture are available, such as antigen detection from biological fluids. This method is rapid and can provide an exact identification of the serogroup, but it commonly produces false-negative results. Polymerase chain reaction can also identify specific serogroups and does not require the presence of a live organism.[4]\nWithout prompt treatment, the mortality rate of Waterhouse-Friderichsen syndrome approaches 100%. Even with rapid and optimal medical therapy, approximately 40% of patients with meningococcal sepsis do not survive. When DIC is present, the mortality rate is as high as 90%. The overall mortality of meningococcal disease is 10%-20%, with the same percentage of survivors having permanent neurologic sequelae (ie, neurologic disability, loss of a limb, and hearing impairment).[4,5]\nThe most important therapeutic point for meningococcal infection is early administration of appropriate antibiotics. Empirical antibiotics should be administered whenever meningococcal infection is suspected because delays in therapy expose patients to risk for severe illness, permanent disability, or death.\nCommon antimicrobial agents are active against Neisseria species. Penicillin G is usually the first-line antibiotic therapy; it has a low prevalence of resistance. In areas where penicillin-resistant strains have been identified, such as the United Kingdom or Spain, a third-generation cephalosporin can be used instead. Initial treatment with broad-spectrum antibiotics is recommended in all sepsis cases because antibiotic treatment can later be changed once a specific organism is identified.\nEarly goal-directed therapy should be initiated, with a particular focus on fluid administration and maintenance of adequate blood pressure. The efficacy of corticosteroid treatment is controversial, but it is typically recommended in cases of sepsis and meningitis. Debridement of skin and subcutaneous tissues, with subsequent skin grafting or limb amputation, may be necessary if septicemia results in peripheral hypoperfusion with skin and bone necrosis.\nIn cases of fulminant meningococcemia, patients should be immediately transferred to an intensive care unit for aggressive fluid therapy, vasopressor support, and intensive hemodynamic monitoring. Activated protein C may be of use in a very limited number of patients.\nTreatment of DIC includes administration of fresh frozen plasma. Additional treatments currently under investigation include monoclonal antibodies to inflammatory mediators, such as endotoxins, tumor necrosis factor, interleukins, and interferon gamma.[4,5]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A 30-Year-Old With a Full-Body Rash, Vomiting, and Confusion"
},
{
"authors": "Andrea Bianchin, MD; Moreno Agostini, MD",
"content": [
"All persons who have been in close contact with a patient with meningococcal infection are at elevated risk of contracting the disease. Meningococci are spread via respiratory secretions, and they are easily transmitted to close contacts. For this reason, all household members, classmates, medical staff, or anyone else recently associated with the patient must be considered at risk of acquiring the disease.",
"The probability of transmission varies with the duration and closeness of exposure; it is highest during the first few days after the onset of disease. The risk for transmission is higher with actions that result in direct exposure of secretions to mucous membranes, including kissing; mouth-to-mouth resuscitation; and sharing of food, glasses, bottles, or cigarettes.",
"People who have stayed more than 8 hours in close proximity to an infected patient or who have had direct contact with a patient's secretions within 1 week before the onset of symptoms should receive prophylactic treatment. Chemoprophylaxis should be given as soon as possible, because the efficacy of prophylaxis is very low if antibiotics are not started within 10-14 days after exposure. Cultures of oropharyngeal or nasopharyngeal tissue are not useful for determining whether or not antibiotics are necessary, and waiting for the results of these examinations can cause an inappropriate delay in the administration of prophylactic treatment.",
"Rifampin, ciprofloxacin, or ceftriaxone are all effective choices for prophylaxis. The duration of chemoprophylaxis should be 1-2 days, depending on the antibiotic used. Ciprofloxacin and ceftriaxone require a single-dose treatment, and rifampin may be given twice daily for four doses.[1,3,5]",
"Several vaccines are available for controlling outbreaks of N meningitidis. The quadrivalent polysaccharide vaccine (Menomune®) was the first meningococcal vaccine approved by the US Food and Drug Administration (FDA) for serogroups A, C, Y, and W-135; however, this vaccine has largely been replaced by two quadrivalent conjugate vaccines (Menactra®, Menveo®) for most populations. Two meningococcal vaccines for serogroup B are also available in the United States (Bexsero®, Trumenba®).",
"Routine vaccination with Menactra or Menveo is recommended for young adolescents beginning at age 11-12 years, with a booster dose at age 16-23 years.[6] Serogroup B vaccines are not recommended for routine vaccination by the Centers for Disease Control and Prevention (CDC), but adolescents and young adults may receive Trumenba (three doses) or Bexsero (two doses) at age 16-23 years.[6,7]",
"For outbreak situations, meningococcal vaccines A/C/Y and W-135 plus serogroup B administration are recommended in the presence of at least three cases during 3 months or less, or when 10 cases occur per 100,000 people in larger communities. These vaccines are also recommended for high-risk individuals (eg, complement deficiencies, asplenia, microbiologists routinely exposed).[6,8,9,10]",
"The patient in this case was admitted to the intensive care unit after early initiation of intravenous ceftriaxone. The patient's blood cultures grew serogroup C N meningitidis. A few hours after admission, petechial lesions appeared and rapidly spread throughout her trunk, legs, back, and face. The lesions became progressively larger and hemorrhagic (Figures 3 and 4).",
"Figure 3.",
"Figure 4.",
"Aggressive fluid therapy, vasopressor support, fresh frozen plasma, and activated protein C therapy were given. The patient required mechanical ventilation after developing acute respiratory failure. Renal failure soon followed, and dialysis was initiated. Her hands and feet became increasingly cyanotic (Figure 5).",
"Figure 5.",
"Despite aggressive therapy, multiple organ dysfunction and DIC progressed; the patient died 4 days after admission. The postmortem examination confirmed meningococcal sepsis and revealed acute purulent meningitis, adrenal apoplexy, thrombotic microangiopathy, purpura confluens, and epidermolysis bullosa; these findings are consistent with a diagnosis of Waterhouse-Friderichsen syndrome."
],
"date": "September 22, 2021",
"figures": [
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/861/792/861792-Thumb3.png"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/861/792/861792-Thumb4.png"
},
{
"caption": "Figure 5.",
"image_url": "https://img.medscapestatic.com/article/861/792/861792-Thumb5.png"
}
],
"markdown": "# A 30-Year-Old With a Full-Body Rash, Vomiting, and Confusion\n\n **Authors:** Andrea Bianchin, MD; Moreno Agostini, MD \n **Date:** September 22, 2021\n\n ## Content\n\n All persons who have been in close contact with a patient with meningococcal infection are at elevated risk of contracting the disease. Meningococci are spread via respiratory secretions, and they are easily transmitted to close contacts. For this reason, all household members, classmates, medical staff, or anyone else recently associated with the patient must be considered at risk of acquiring the disease.\nThe probability of transmission varies with the duration and closeness of exposure; it is highest during the first few days after the onset of disease. The risk for transmission is higher with actions that result in direct exposure of secretions to mucous membranes, including kissing; mouth-to-mouth resuscitation; and sharing of food, glasses, bottles, or cigarettes.\nPeople who have stayed more than 8 hours in close proximity to an infected patient or who have had direct contact with a patient's secretions within 1 week before the onset of symptoms should receive prophylactic treatment. Chemoprophylaxis should be given as soon as possible, because the efficacy of prophylaxis is very low if antibiotics are not started within 10-14 days after exposure. Cultures of oropharyngeal or nasopharyngeal tissue are not useful for determining whether or not antibiotics are necessary, and waiting for the results of these examinations can cause an inappropriate delay in the administration of prophylactic treatment.\nRifampin, ciprofloxacin, or ceftriaxone are all effective choices for prophylaxis. The duration of chemoprophylaxis should be 1-2 days, depending on the antibiotic used. Ciprofloxacin and ceftriaxone require a single-dose treatment, and rifampin may be given twice daily for four doses.[1,3,5]\nSeveral vaccines are available for controlling outbreaks of N meningitidis. The quadrivalent polysaccharide vaccine (Menomune®) was the first meningococcal vaccine approved by the US Food and Drug Administration (FDA) for serogroups A, C, Y, and W-135; however, this vaccine has largely been replaced by two quadrivalent conjugate vaccines (Menactra®, Menveo®) for most populations. Two meningococcal vaccines for serogroup B are also available in the United States (Bexsero®, Trumenba®).\nRoutine vaccination with Menactra or Menveo is recommended for young adolescents beginning at age 11-12 years, with a booster dose at age 16-23 years.[6] Serogroup B vaccines are not recommended for routine vaccination by the Centers for Disease Control and Prevention (CDC), but adolescents and young adults may receive Trumenba (three doses) or Bexsero (two doses) at age 16-23 years.[6,7]\nFor outbreak situations, meningococcal vaccines A/C/Y and W-135 plus serogroup B administration are recommended in the presence of at least three cases during 3 months or less, or when 10 cases occur per 100,000 people in larger communities. These vaccines are also recommended for high-risk individuals (eg, complement deficiencies, asplenia, microbiologists routinely exposed).[6,8,9,10]\nThe patient in this case was admitted to the intensive care unit after early initiation of intravenous ceftriaxone. The patient's blood cultures grew serogroup C N meningitidis. A few hours after admission, petechial lesions appeared and rapidly spread throughout her trunk, legs, back, and face. The lesions became progressively larger and hemorrhagic (Figures 3 and 4).\nFigure 3.\nFigure 4.\nAggressive fluid therapy, vasopressor support, fresh frozen plasma, and activated protein C therapy were given. The patient required mechanical ventilation after developing acute respiratory failure. Renal failure soon followed, and dialysis was initiated. Her hands and feet became increasingly cyanotic (Figure 5).\nFigure 5.\nDespite aggressive therapy, multiple organ dysfunction and DIC progressed; the patient died 4 days after admission. The postmortem examination confirmed meningococcal sepsis and revealed acute purulent meningitis, adrenal apoplexy, thrombotic microangiopathy, purpura confluens, and epidermolysis bullosa; these findings are consistent with a diagnosis of Waterhouse-Friderichsen syndrome.\n\n ## Figures\n\n **Figure 3.** \n \n\n**Figure 4.** \n \n\n**Figure 5.** \n \n\n\n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 957713,
"choiceText": "Waterhouse-Friderichsen syndrome is a complication of <i>N meningitidis</i> infection",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957715,
"choiceText": "<i>N meningitidis</i> is a gram-positive aerobic diplococcus",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957717,
"choiceText": "<i>N meningitidis</i> usually causes severe illness in all individuals it colonizes",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957719,
"choiceText": "<i>N meningitidis</i> is transmitted through direct contact\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Waterhouse-Friderichsen syndrome is a severe complication of <i>N meningitidis</i> infection. <i>N meningitidis</i> is a gram-negative aerobic diplococcus with a particular affinity for the bloodstream and meninges. Infection may cause clinical conditions ranging from fever and bacteremia to life-threatening septic shock.<br>\r\n<br><i>N meningitidis</i> is a commensal bacterium in many humans that resides in the nasopharynx and colonizes up to 25% of healthy people, without causing illness. It is transmitted by aerosolized respiratory particles and secretions.<br>\r\n<br>The reason why some people who carry invasive strains of the bacteria become ill whereas others do not is unclear. <i>N meningitidis</i> spreads through the inhalation of respiratory secretions transmitted by a carrier.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 302895,
"questionText": "Which statement is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 957721,
"choiceText": "A third-generation cephalosporin is required in areas where penicillin-resistant strains of <i>Neisseria</i> species have been identified ",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957723,
"choiceText": "Most common antimicrobial agents are inactive against <i>Neisseria</i> species",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957725,
"choiceText": "Penicillin is now contraindicated in most patients with meningococcal infection",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957727,
"choiceText": "Antibiotics should be administered only after definitive diagnosis in cases of suspected meningococcal infection",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Common antimicrobial agents are active against <i>Neisseria</i> species. Penicillin G is usually the first-line antibiotic therapy; it has a low prevalence of resistance. In areas where penicillin-resistant strains have been identified, such as the United Kingdom or Spain, a third-generation cephalosporin can be used instead. Initial treatment with broad-spectrum antibiotics is recommended in all sepsis cases because antibiotic treatment can later be changed once a specific organism is identified. \r\n<br><br>\r\nThe most important therapeutic point for meningococcal infection is early administration of appropriate antibiotics. Empirical antibiotics should be administered whenever meningococcal infection is suspected because delays in therapy expose patients to a risk for severe illness, permanent disability, or death.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 302897,
"questionText": "Which statement is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 30-Year-Old With a Full-Body Rash, Vomiting, and Confusion"
},
{
"authors": "Andrea Bianchin, MD; Moreno Agostini, MD",
"content": [],
"date": "September 22, 2021",
"figures": [],
"markdown": "# A 30-Year-Old With a Full-Body Rash, Vomiting, and Confusion\n\n **Authors:** Andrea Bianchin, MD; Moreno Agostini, MD \n **Date:** September 22, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 957713,
"choiceText": "Waterhouse-Friderichsen syndrome is a complication of <i>N meningitidis</i> infection",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957715,
"choiceText": "<i>N meningitidis</i> is a gram-positive aerobic diplococcus",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957717,
"choiceText": "<i>N meningitidis</i> usually causes severe illness in all individuals it colonizes",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957719,
"choiceText": "<i>N meningitidis</i> is transmitted through direct contact\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Waterhouse-Friderichsen syndrome is a severe complication of <i>N meningitidis</i> infection. <i>N meningitidis</i> is a gram-negative aerobic diplococcus with a particular affinity for the bloodstream and meninges. Infection may cause clinical conditions ranging from fever and bacteremia to life-threatening septic shock.<br>\r\n<br><i>N meningitidis</i> is a commensal bacterium in many humans that resides in the nasopharynx and colonizes up to 25% of healthy people, without causing illness. It is transmitted by aerosolized respiratory particles and secretions.<br>\r\n<br>The reason why some people who carry invasive strains of the bacteria become ill whereas others do not is unclear. <i>N meningitidis</i> spreads through the inhalation of respiratory secretions transmitted by a carrier.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 302895,
"questionText": "Which statement is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 957721,
"choiceText": "A third-generation cephalosporin is required in areas where penicillin-resistant strains of <i>Neisseria</i> species have been identified ",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957723,
"choiceText": "Most common antimicrobial agents are inactive against <i>Neisseria</i> species",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957725,
"choiceText": "Penicillin is now contraindicated in most patients with meningococcal infection",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957727,
"choiceText": "Antibiotics should be administered only after definitive diagnosis in cases of suspected meningococcal infection",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Common antimicrobial agents are active against <i>Neisseria</i> species. Penicillin G is usually the first-line antibiotic therapy; it has a low prevalence of resistance. In areas where penicillin-resistant strains have been identified, such as the United Kingdom or Spain, a third-generation cephalosporin can be used instead. Initial treatment with broad-spectrum antibiotics is recommended in all sepsis cases because antibiotic treatment can later be changed once a specific organism is identified. \r\n<br><br>\r\nThe most important therapeutic point for meningococcal infection is early administration of appropriate antibiotics. Empirical antibiotics should be administered whenever meningococcal infection is suspected because delays in therapy expose patients to a risk for severe illness, permanent disability, or death.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 302897,
"questionText": "Which statement is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 30-Year-Old With a Full-Body Rash, Vomiting, and Confusion"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 957705,
"choiceText": "Toxic shock syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957707,
"choiceText": "Waterhouse-Friderichsen syndrome",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957709,
"choiceText": "Acute necrotizing pancreatitis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957711,
"choiceText": "Acute respiratory distress syndrome\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 302893,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 957713,
"choiceText": "Waterhouse-Friderichsen syndrome is a complication of <i>N meningitidis</i> infection",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957715,
"choiceText": "<i>N meningitidis</i> is a gram-positive aerobic diplococcus",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957717,
"choiceText": "<i>N meningitidis</i> usually causes severe illness in all individuals it colonizes",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957719,
"choiceText": "<i>N meningitidis</i> is transmitted through direct contact\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Waterhouse-Friderichsen syndrome is a severe complication of <i>N meningitidis</i> infection. <i>N meningitidis</i> is a gram-negative aerobic diplococcus with a particular affinity for the bloodstream and meninges. Infection may cause clinical conditions ranging from fever and bacteremia to life-threatening septic shock.<br>\r\n<br><i>N meningitidis</i> is a commensal bacterium in many humans that resides in the nasopharynx and colonizes up to 25% of healthy people, without causing illness. It is transmitted by aerosolized respiratory particles and secretions.<br>\r\n<br>The reason why some people who carry invasive strains of the bacteria become ill whereas others do not is unclear. <i>N meningitidis</i> spreads through the inhalation of respiratory secretions transmitted by a carrier.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 302895,
"questionText": "Which statement is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 957721,
"choiceText": "A third-generation cephalosporin is required in areas where penicillin-resistant strains of <i>Neisseria</i> species have been identified ",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957723,
"choiceText": "Most common antimicrobial agents are inactive against <i>Neisseria</i> species",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957725,
"choiceText": "Penicillin is now contraindicated in most patients with meningococcal infection",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 957727,
"choiceText": "Antibiotics should be administered only after definitive diagnosis in cases of suspected meningococcal infection",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Common antimicrobial agents are active against <i>Neisseria</i> species. Penicillin G is usually the first-line antibiotic therapy; it has a low prevalence of resistance. In areas where penicillin-resistant strains have been identified, such as the United Kingdom or Spain, a third-generation cephalosporin can be used instead. Initial treatment with broad-spectrum antibiotics is recommended in all sepsis cases because antibiotic treatment can later be changed once a specific organism is identified. \r\n<br><br>\r\nThe most important therapeutic point for meningococcal infection is early administration of appropriate antibiotics. Empirical antibiotics should be administered whenever meningococcal infection is suspected because delays in therapy expose patients to a risk for severe illness, permanent disability, or death.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 302897,
"questionText": "Which statement is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
957245 | /viewarticle/957245 | [
{
"authors": "Vikramjit Kanwar, MBBS, MBA; Shyam Srinivasan, MBBS, DM",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 28-month-old girl has recently become irritable and \"clingy\" with difficulty sleeping and occasional high-pitched crying. Her mother reports that her speech has decreased and she is clumsier. The girl also complains of \"ouchy\" and points to her navel but is not constipated.",
"She is an only child born by normal vaginal delivery at full term, and she has met the normal developmental milestones until recently. Her immunizations are up to date. Her symptoms started a month ago when her grandmother relocated to a different state. Her pediatrician suspected that her symptoms resulted from the anxiety of losing contact with \"nana\" and reassured her mother that she should \"watch and wait.\" However, the child grew increasingly unsteady when she walked, to the point of losing her balance and falling over, and her eyes developed intermittent chaotic and jerky movements. The mother was alarmed and contacted the pediatrician, who directed her to the emergency department.",
"The mother and child live in an older part of Philadelphia. The only significant illness recorded for the child is an episode of iron deficiency anemia at the age of 12 months when the child was drinking four bottles of cow's milk a day, eating dirt, and chewing on the doorframe. Laboratory testing confirmed she had microcytic hypochromic anemia and a profoundly low ferritin level that resolved with dietary counseling and a therapeutic course of ferrous sulfate. She has had the usual childhood coughs, colds, and mild viral illnesses, including a \"strep throat\" infection, but she has not had any such illnesses during the previous 2 months. She has no history of weight loss, fever, headache, rashes, joint swelling, pallor, or bruising."
],
"date": "September 02, 2021",
"figures": [],
"markdown": "# Decreased Speech and Jerky Eye Movements in a 'Clumsy' Toddler\n\n **Authors:** Vikramjit Kanwar, MBBS, MBA; Shyam Srinivasan, MBBS, DM \n **Date:** September 02, 2021\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 28-month-old girl has recently become irritable and \"clingy\" with difficulty sleeping and occasional high-pitched crying. Her mother reports that her speech has decreased and she is clumsier. The girl also complains of \"ouchy\" and points to her navel but is not constipated.\nShe is an only child born by normal vaginal delivery at full term, and she has met the normal developmental milestones until recently. Her immunizations are up to date. Her symptoms started a month ago when her grandmother relocated to a different state. Her pediatrician suspected that her symptoms resulted from the anxiety of losing contact with \"nana\" and reassured her mother that she should \"watch and wait.\" However, the child grew increasingly unsteady when she walked, to the point of losing her balance and falling over, and her eyes developed intermittent chaotic and jerky movements. The mother was alarmed and contacted the pediatrician, who directed her to the emergency department.\nThe mother and child live in an older part of Philadelphia. The only significant illness recorded for the child is an episode of iron deficiency anemia at the age of 12 months when the child was drinking four bottles of cow's milk a day, eating dirt, and chewing on the doorframe. Laboratory testing confirmed she had microcytic hypochromic anemia and a profoundly low ferritin level that resolved with dietary counseling and a therapeutic course of ferrous sulfate. She has had the usual childhood coughs, colds, and mild viral illnesses, including a \"strep throat\" infection, but she has not had any such illnesses during the previous 2 months. She has no history of weight loss, fever, headache, rashes, joint swelling, pallor, or bruising.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Decreased Speech and Jerky Eye Movements in a 'Clumsy' Toddler"
},
{
"authors": "Vikramjit Kanwar, MBBS, MBA; Shyam Srinivasan, MBBS, DM",
"content": [
"Upon examination, the patient is alert but irritable and difficult to console. See an example of this behavior in a different patient in the video clip below.",
"Video 1.",
"Her vital signs are normal, including a heart rate of 108 beats/minute, a respiration rate of 28 breaths/minute, and a blood pressure of 96/58 mm Hg. Her oxygen saturation is 98% on room air. She is afebrile. No pallor, icterus, lymphadenopathy, cyanosis, clubbing, or rashes are noted. Results of the neurologic examination are remarkable for intermittent jerking movements of her arms and legs, with an unsteady ataxic gait. See an example of this behavior in a different patient in the video clip below.",
"Video 2.",
"Her pupils are equal and react to light, and other cranial nerves appear intact. However, she has intermittent conjugate jerky eye movements that are not confined to a particular direction. See an example of this behavior in a different patient in the video clip below.",
"Video 3.",
"Power and tone are difficult to assess, but deep tendon reflexes are present and symmetrical, with downgoing plantar responses and no meningeal signs. Her chest is clear to auscultation. The cardiovascular examination reveals normal first and second heart sounds, with a low-pitched grade 2/6 systolic murmur at the left lower sternal border. Her abdomen is soft and nontender with no hepatosplenomegaly and no palpable masses.",
"Initial test results include a complete blood cell count that is notable for a hemoglobin level of 11.2 g/dL (reference range, 12.6-17.4 g/dL); normal total white blood cell count, differential, and platelet counts; and a peripheral blood smear that shows no abnormalities. Serum electrolyte, creatinine, and liver enzyme levels are within the normal range. The results of a routine urine examination are normal, and the urine vanillylmandelic acid (VMA) level is also in the normal range.",
"An abdominal ultrasound scan shows no abnormal masses. A CT scan of the brain with and without contrast reveals no evidence of a tumor, hydrocephalus, or intracranial bleeding. The findings of a lumbar puncture are:",
"Appearance of cerebrospinal fluid (CSF): Clear",
"Pressure: Normal",
"White blood cell count: 3 cells/µL, all lymphocytes (reference range, 0-5 cells/µL [< 2 polymorphonucleocytes])",
"Protein and glucose levels: Normal",
"An MRI scan of the brain with contrast shows no evidence of a space-occupying lesion; a formal report is pending."
],
"date": "September 02, 2021",
"figures": [],
"markdown": "# Decreased Speech and Jerky Eye Movements in a 'Clumsy' Toddler\n\n **Authors:** Vikramjit Kanwar, MBBS, MBA; Shyam Srinivasan, MBBS, DM \n **Date:** September 02, 2021\n\n ## Content\n\n Upon examination, the patient is alert but irritable and difficult to console. See an example of this behavior in a different patient in the video clip below.\nVideo 1.\nHer vital signs are normal, including a heart rate of 108 beats/minute, a respiration rate of 28 breaths/minute, and a blood pressure of 96/58 mm Hg. Her oxygen saturation is 98% on room air. She is afebrile. No pallor, icterus, lymphadenopathy, cyanosis, clubbing, or rashes are noted. Results of the neurologic examination are remarkable for intermittent jerking movements of her arms and legs, with an unsteady ataxic gait. See an example of this behavior in a different patient in the video clip below.\nVideo 2.\nHer pupils are equal and react to light, and other cranial nerves appear intact. However, she has intermittent conjugate jerky eye movements that are not confined to a particular direction. See an example of this behavior in a different patient in the video clip below.\nVideo 3.\nPower and tone are difficult to assess, but deep tendon reflexes are present and symmetrical, with downgoing plantar responses and no meningeal signs. Her chest is clear to auscultation. The cardiovascular examination reveals normal first and second heart sounds, with a low-pitched grade 2/6 systolic murmur at the left lower sternal border. Her abdomen is soft and nontender with no hepatosplenomegaly and no palpable masses.\nInitial test results include a complete blood cell count that is notable for a hemoglobin level of 11.2 g/dL (reference range, 12.6-17.4 g/dL); normal total white blood cell count, differential, and platelet counts; and a peripheral blood smear that shows no abnormalities. Serum electrolyte, creatinine, and liver enzyme levels are within the normal range. The results of a routine urine examination are normal, and the urine vanillylmandelic acid (VMA) level is also in the normal range.\nAn abdominal ultrasound scan shows no abnormal masses. A CT scan of the brain with and without contrast reveals no evidence of a tumor, hydrocephalus, or intracranial bleeding. The findings of a lumbar puncture are:\nAppearance of cerebrospinal fluid (CSF): Clear\nPressure: Normal\nWhite blood cell count: 3 cells/µL, all lymphocytes (reference range, 0-5 cells/µL [< 2 polymorphonucleocytes])\nProtein and glucose levels: Normal\nAn MRI scan of the brain with contrast shows no evidence of a space-occupying lesion; a formal report is pending.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1616449,
"choiceText": "Lead-related neurotoxicity",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616450,
"choiceText": "Sydenham (rheumatic) chorea",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616451,
"choiceText": "Postviral cerebellar ataxia",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616452,
"choiceText": "Opsoclonus-myoclonus ataxia syndrome",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 519320,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Decreased Speech and Jerky Eye Movements in a 'Clumsy' Toddler"
},
{
"authors": "Vikramjit Kanwar, MBBS, MBA; Shyam Srinivasan, MBBS, DM",
"content": [
"Acute ataxia is a rare finding in a toddler.[1] In this case, the prodrome of behavioral changes, the association with myoclonic jerks, and the presence of intermittent rapid, conjugate, multidirectional eye movements (opsoclonus) helped establish the diagnosis of opsoclonus-myoclonus ataxia syndrome (OMAS), also known as \"dancing eyes and dancing feet syndrome.\"[2,3] OMAS primarily affects toddlers and is commonly associated with the presence of a neuroblastoma. Of the 650 children who receive a diagnosis of neuroblastoma each year in North America, 2%-4% have OMAS.[4] In 2004, an international task force recommended that three of these four criteria be present to diagnose neuroblastoma with OMAS[5]:",
"Opsoclonus",
"Myoclonus and ataxia",
"Behavioral change and/or sleep disturbance",
"Neuroblastoma",
"All the classic findings of OMAS do not need to be present to make a diagnosis, so OMAS should be considered in any toddler or preschool child who has unexplained ataxia of sudden onset.[1,2] In the patient in this case, a whole body MRI scan showed a 2.6 × 2.2 × 1.1-cm tumor in the left paravertebral area at the level of D9. Similar MRI findings are shown below in a different patient (Figure 1). Resection of the tumor confirmed a ganglioneuroblastoma (neuroblastoma mixed with elements of maturation) with dense lymphocytic infiltration. The histopathologic findings resemble those seen below (Figure 2). No N-myc amplification, evidence of spread, or elevation in urine catecholamine levels was noted, which is consistent with the low grade of the tumor.[6]",
"Figure 1.",
"Figure 2.",
"Surgical resection temporarily ameliorated the patient's symptoms. Although the expected long-term survival rate for a patient who has a neuroblastoma and OMAS is excellent, the main concern is the high likelihood of significant residual neurologic deficits, including developmental delay and learning disabilities, which are found in 70%-80% of patients who do not receive further therapy.[7]",
"The other differential diagnoses considered in this case were lead-related neurotoxicity, Sydenham (rheumatic) chorea, and postviral cerebellar ataxia. Lead toxicity in children leads to 1500 emergency department visits per year in the United States. In older homes, lead-containing paint in deeper layers can allow children with pica to ingest sufficient quantities to have ill effects. Blood lead levels of > 70 µg/dL (fortunately, rarely encountered) are needed to cause acute toxicity with vomiting, clumsiness, irritability, ataxia, and even seizures and coma.[8] In this patient, the absence of recent pica and the presence of opsoclonus and myoclonus excluded this diagnosis.",
"Sydenham chorea, which occurs in 10%-30% of patients with rheumatic fever, is rare in the United States and is triggered by anti–basal ganglia antibodies. It is the most common cause of childhood chorea and is characterized by an abrupt onset of jerky involuntary movements (St Vitus' dance), along with dysarthria and tics. Although behavioral changes and gait disturbances are seen in patients with Sydenham chorea, ataxia, myoclonus, and opsoclonus are not. In addition, despite this patient's recent history of \"strep throat,\" acute rheumatic fever and Sydenham chorea do not occur in children younger than 5 years.[9]",
"Postinfectious cerebellar ataxia (PICA) affects 700 children each year in the United States and is the most common cause of acute childhood ataxia. The nystagmus of PICA comprises horizontal eye movements, which are distinct from the chaotic eye movements of opsoclonus in this patient. There is invariably a history of a viral illness within 3-4 weeks preceding the onset of symptoms, which was also not seen in this case. Nevertheless, patients with OMAS sometimes receive a diagnosis of PICA, especially if opsoclonus and/or myoclonus is not prominent. The correct diagnosis is made when more classic signs of OMAS appear or when the ataxia fails to resolve in a few weeks (the expected course in a patient with PICA).[1,10]"
],
"date": "September 02, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/957/245/957245-Thumb1.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/957/245/957245-Thumb2.jpg"
}
],
"markdown": "# Decreased Speech and Jerky Eye Movements in a 'Clumsy' Toddler\n\n **Authors:** Vikramjit Kanwar, MBBS, MBA; Shyam Srinivasan, MBBS, DM \n **Date:** September 02, 2021\n\n ## Content\n\n Acute ataxia is a rare finding in a toddler.[1] In this case, the prodrome of behavioral changes, the association with myoclonic jerks, and the presence of intermittent rapid, conjugate, multidirectional eye movements (opsoclonus) helped establish the diagnosis of opsoclonus-myoclonus ataxia syndrome (OMAS), also known as \"dancing eyes and dancing feet syndrome.\"[2,3] OMAS primarily affects toddlers and is commonly associated with the presence of a neuroblastoma. Of the 650 children who receive a diagnosis of neuroblastoma each year in North America, 2%-4% have OMAS.[4] In 2004, an international task force recommended that three of these four criteria be present to diagnose neuroblastoma with OMAS[5]:\nOpsoclonus\nMyoclonus and ataxia\nBehavioral change and/or sleep disturbance\nNeuroblastoma\nAll the classic findings of OMAS do not need to be present to make a diagnosis, so OMAS should be considered in any toddler or preschool child who has unexplained ataxia of sudden onset.[1,2] In the patient in this case, a whole body MRI scan showed a 2.6 × 2.2 × 1.1-cm tumor in the left paravertebral area at the level of D9. Similar MRI findings are shown below in a different patient (Figure 1). Resection of the tumor confirmed a ganglioneuroblastoma (neuroblastoma mixed with elements of maturation) with dense lymphocytic infiltration. The histopathologic findings resemble those seen below (Figure 2). No N-myc amplification, evidence of spread, or elevation in urine catecholamine levels was noted, which is consistent with the low grade of the tumor.[6]\nFigure 1.\nFigure 2.\nSurgical resection temporarily ameliorated the patient's symptoms. Although the expected long-term survival rate for a patient who has a neuroblastoma and OMAS is excellent, the main concern is the high likelihood of significant residual neurologic deficits, including developmental delay and learning disabilities, which are found in 70%-80% of patients who do not receive further therapy.[7]\nThe other differential diagnoses considered in this case were lead-related neurotoxicity, Sydenham (rheumatic) chorea, and postviral cerebellar ataxia. Lead toxicity in children leads to 1500 emergency department visits per year in the United States. In older homes, lead-containing paint in deeper layers can allow children with pica to ingest sufficient quantities to have ill effects. Blood lead levels of > 70 µg/dL (fortunately, rarely encountered) are needed to cause acute toxicity with vomiting, clumsiness, irritability, ataxia, and even seizures and coma.[8] In this patient, the absence of recent pica and the presence of opsoclonus and myoclonus excluded this diagnosis.\nSydenham chorea, which occurs in 10%-30% of patients with rheumatic fever, is rare in the United States and is triggered by anti–basal ganglia antibodies. It is the most common cause of childhood chorea and is characterized by an abrupt onset of jerky involuntary movements (St Vitus' dance), along with dysarthria and tics. Although behavioral changes and gait disturbances are seen in patients with Sydenham chorea, ataxia, myoclonus, and opsoclonus are not. In addition, despite this patient's recent history of \"strep throat,\" acute rheumatic fever and Sydenham chorea do not occur in children younger than 5 years.[9]\nPostinfectious cerebellar ataxia (PICA) affects 700 children each year in the United States and is the most common cause of acute childhood ataxia. The nystagmus of PICA comprises horizontal eye movements, which are distinct from the chaotic eye movements of opsoclonus in this patient. There is invariably a history of a viral illness within 3-4 weeks preceding the onset of symptoms, which was also not seen in this case. Nevertheless, patients with OMAS sometimes receive a diagnosis of PICA, especially if opsoclonus and/or myoclonus is not prominent. The correct diagnosis is made when more classic signs of OMAS appear or when the ataxia fails to resolve in a few weeks (the expected course in a patient with PICA).[1,10]\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1616449,
"choiceText": "Lead-related neurotoxicity",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616450,
"choiceText": "Sydenham (rheumatic) chorea",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616451,
"choiceText": "Postviral cerebellar ataxia",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616452,
"choiceText": "Opsoclonus-myoclonus ataxia syndrome",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 519320,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Decreased Speech and Jerky Eye Movements in a 'Clumsy' Toddler"
},
{
"authors": "Vikramjit Kanwar, MBBS, MBA; Shyam Srinivasan, MBBS, DM",
"content": [
"OMAS was first described in 1963 by Kinsbourne based on six patients and may present primarily with acute/subacute ataxia with minimal myoclonus and delayed opsoclonus.[1,2,3,4,5] Thus, a high index of suspicion is needed to make the diagnosis. Motor findings are frequently preceded by weeks of behavioral changes ranging from irritability with the inability to be consoled, loss of speech, and sleep disturbances to apathy and the reduction of social and playing activities. The ataxia is acute in onset, and toddlers may lose the ability to walk or sit within days. The associated myoclonus may involve all parts of the body, ranging from mild tremors (polymyoclonia) to coarse multifocal jerks, and it is exacerbated by attempts to move or emotional distress. Opsoclonus may be late in onset, appearing several weeks after the onset of ataxia and comprising intermittent rapid, conjugate, multidirectional eye movements. These movements can be provoked by a change in gaze fixation, usually from far to near.[11]",
"Although finding a neuroblastoma in conjunction with at least two of the characteristic neurologic findings is diagnostic, Pranzatelli and colleagues[4] from the United States confirmed in their series (N = 356) that 50% of children with OMAS did not have a detectable neuroblastoma. Series of patients with OMAS reported from around the world mirrored this finding; the proportion of patients lacking an identifiable neuroblastoma was 18 of 36 patients (50%) in South India, 12 of 34 patients (36%) in France, and 11 of 15 patients (74%) in the United Kingdom.[12,13,14,15] A fine-cut CT scan or a whole body MRI scan may reveal small paravertebral tumors, and the routine use of these modalities might improve the detection rate.[15,16] Nevertheless, it is hypothesized that in many patients the tumor has already involuted owing to an autoimmune mechanism, and the persistent neurologic symptoms of OMAS represent a \"hit and run\" phenomenon.[4] Serum immunoglobulin from patients with OMAS has been shown to suppress the growth of neuroblastoma cell lines, which supports this hypothesis.",
"The mechanism for coincident OMAS and neuroblastoma remains speculative. Although the level of antineuronal antibodies increases, a causative antibody is still elusive.[17] Indirect evidence that OMAS is immunologically mediated includes the presence of hypergammaglobulinemia, CSF with pleocytosis, and abnormalities in the CSF immunoglobulin G index that persist for years after diagnosis, as well as a significant response to corticosteroids, immunosuppressive medications, and chemotherapy.[4,5]",
"In the United States, the Pediatric Oncology Group reviewed data from 29 children who had received a diagnosis of neuroblastoma and OMAS between 1983 and 1993. Most of the patients had low-stage (n = 21) and intermediate-stage (n = 7) tumors, usually in the paraspinal region. The treatment for neuroblastoma was surgery alone in 19 of 29 patients; the rest also received chemotherapy. Surgery transiently improved acute symptoms, which was also observed by Japanese researchers in a more recent study (n = 5); however, complete resolution of OMAS was rare.[7,18] Twenty children (69%) had persistent neurologic deficits, including speech delay, cognitive deficits, motor delay, and behavioral problems, but 6 of 9 children who received chemotherapy had a complete recovery from OMAS without neurologic sequelae.[7]",
"Building on these data, the Children's Oncology Group (COG) from North America, Australia, and New Zealand conducted the landmark study COG-ANBL00P3, in which a total of 53 patients with neuroblastoma-associated OMAS were enrolled from 2004 to 2013.[19] In the entire cohort, 83% of patients had low-risk disease, the male to female ratio was 1:1.7, and the median age of diagnosis was 18.9 months. All patients received prednisone for at least 2 months and cyclophosphamide monthly for 6 months (intermediate/high-risk patients received only their scheduled chemotherapy). In addition, patients were prospectively randomized to receive intravenous immunoglobulin (IVIG) as an immune modulator. The 26 patients assigned to that arm were given IVIG monthly for 6 months, and it was continued bimonthly until 12 months.",
"The response rate for those who had received IVIG was markedly superior to the rate for those who did not (21 of 26 patients [80.8%] vs 11 of 27 patients [40.7%], P = .0029), and the three-agent combination emerged as a standard regimen. Additional follow-up will be needed to assess the impact on long-term neurologic sequelae. The 3-year event-free survival of the cohort was 94.1%.",
"The International Society of Pediatric Oncology European Neuroblastoma Group has a similar trial with dexamethasone, cyclophosphamide, and rituximab; the outcomes are awaited.[11] In Toronto, Canada, a limited pilot study looked at pulsed methylprednisolone and rituximab in reducing the duration of immune suppression.[20]"
],
"date": "September 02, 2021",
"figures": [],
"markdown": "# Decreased Speech and Jerky Eye Movements in a 'Clumsy' Toddler\n\n **Authors:** Vikramjit Kanwar, MBBS, MBA; Shyam Srinivasan, MBBS, DM \n **Date:** September 02, 2021\n\n ## Content\n\n OMAS was first described in 1963 by Kinsbourne based on six patients and may present primarily with acute/subacute ataxia with minimal myoclonus and delayed opsoclonus.[1,2,3,4,5] Thus, a high index of suspicion is needed to make the diagnosis. Motor findings are frequently preceded by weeks of behavioral changes ranging from irritability with the inability to be consoled, loss of speech, and sleep disturbances to apathy and the reduction of social and playing activities. The ataxia is acute in onset, and toddlers may lose the ability to walk or sit within days. The associated myoclonus may involve all parts of the body, ranging from mild tremors (polymyoclonia) to coarse multifocal jerks, and it is exacerbated by attempts to move or emotional distress. Opsoclonus may be late in onset, appearing several weeks after the onset of ataxia and comprising intermittent rapid, conjugate, multidirectional eye movements. These movements can be provoked by a change in gaze fixation, usually from far to near.[11]\nAlthough finding a neuroblastoma in conjunction with at least two of the characteristic neurologic findings is diagnostic, Pranzatelli and colleagues[4] from the United States confirmed in their series (N = 356) that 50% of children with OMAS did not have a detectable neuroblastoma. Series of patients with OMAS reported from around the world mirrored this finding; the proportion of patients lacking an identifiable neuroblastoma was 18 of 36 patients (50%) in South India, 12 of 34 patients (36%) in France, and 11 of 15 patients (74%) in the United Kingdom.[12,13,14,15] A fine-cut CT scan or a whole body MRI scan may reveal small paravertebral tumors, and the routine use of these modalities might improve the detection rate.[15,16] Nevertheless, it is hypothesized that in many patients the tumor has already involuted owing to an autoimmune mechanism, and the persistent neurologic symptoms of OMAS represent a \"hit and run\" phenomenon.[4] Serum immunoglobulin from patients with OMAS has been shown to suppress the growth of neuroblastoma cell lines, which supports this hypothesis.\nThe mechanism for coincident OMAS and neuroblastoma remains speculative. Although the level of antineuronal antibodies increases, a causative antibody is still elusive.[17] Indirect evidence that OMAS is immunologically mediated includes the presence of hypergammaglobulinemia, CSF with pleocytosis, and abnormalities in the CSF immunoglobulin G index that persist for years after diagnosis, as well as a significant response to corticosteroids, immunosuppressive medications, and chemotherapy.[4,5]\nIn the United States, the Pediatric Oncology Group reviewed data from 29 children who had received a diagnosis of neuroblastoma and OMAS between 1983 and 1993. Most of the patients had low-stage (n = 21) and intermediate-stage (n = 7) tumors, usually in the paraspinal region. The treatment for neuroblastoma was surgery alone in 19 of 29 patients; the rest also received chemotherapy. Surgery transiently improved acute symptoms, which was also observed by Japanese researchers in a more recent study (n = 5); however, complete resolution of OMAS was rare.[7,18] Twenty children (69%) had persistent neurologic deficits, including speech delay, cognitive deficits, motor delay, and behavioral problems, but 6 of 9 children who received chemotherapy had a complete recovery from OMAS without neurologic sequelae.[7]\nBuilding on these data, the Children's Oncology Group (COG) from North America, Australia, and New Zealand conducted the landmark study COG-ANBL00P3, in which a total of 53 patients with neuroblastoma-associated OMAS were enrolled from 2004 to 2013.[19] In the entire cohort, 83% of patients had low-risk disease, the male to female ratio was 1:1.7, and the median age of diagnosis was 18.9 months. All patients received prednisone for at least 2 months and cyclophosphamide monthly for 6 months (intermediate/high-risk patients received only their scheduled chemotherapy). In addition, patients were prospectively randomized to receive intravenous immunoglobulin (IVIG) as an immune modulator. The 26 patients assigned to that arm were given IVIG monthly for 6 months, and it was continued bimonthly until 12 months.\nThe response rate for those who had received IVIG was markedly superior to the rate for those who did not (21 of 26 patients [80.8%] vs 11 of 27 patients [40.7%], P = .0029), and the three-agent combination emerged as a standard regimen. Additional follow-up will be needed to assess the impact on long-term neurologic sequelae. The 3-year event-free survival of the cohort was 94.1%.\nThe International Society of Pediatric Oncology European Neuroblastoma Group has a similar trial with dexamethasone, cyclophosphamide, and rituximab; the outcomes are awaited.[11] In Toronto, Canada, a limited pilot study looked at pulsed methylprednisolone and rituximab in reducing the duration of immune suppression.[20]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Decreased Speech and Jerky Eye Movements in a 'Clumsy' Toddler"
},
{
"authors": "Vikramjit Kanwar, MBBS, MBA; Shyam Srinivasan, MBBS, DM",
"content": [
"Given the high likelihood of symptomatic relapses and long-term neurologic sequelae in OMAS, the patient in this case received prednisone, monthly intravenous cyclophosphamide, and IVIG for 6 months. She had an excellent response within a few weeks of the start of therapy. Her prednisone dosage was tapered after 2 months; however, because her symptoms recurred, the corticosteroid was continued for 6 months, after which the dosage was slowly reduced and then stopped. Fortunately, she responded well.",
"For the small number of patients whose disorder is refractory to therapy, adrenocorticotropic hormone therapy is considered potentially more effective than corticosteroid treatment, and rituximab has also been used. Case reports of other modalities reported to provide benefit in persistently symptomatic patients include therapeutic plasma exchange and even autologous stem cell transplant; however, these treatments are not considered the standard of care.[21,22]",
"For the past 2 years, this patient has not required medication and has had no further relapses. She is a happy, healthy little girl who was just enrolled in kindergarten. Because of concerns about recurrence and long-term deficits, she is undergoing follow-up with a pediatric neurologist who is familiar with OMAS and who uses a standardized metric to document her signs and symptoms.[23]"
],
"date": "September 02, 2021",
"figures": [],
"markdown": "# Decreased Speech and Jerky Eye Movements in a 'Clumsy' Toddler\n\n **Authors:** Vikramjit Kanwar, MBBS, MBA; Shyam Srinivasan, MBBS, DM \n **Date:** September 02, 2021\n\n ## Content\n\n Given the high likelihood of symptomatic relapses and long-term neurologic sequelae in OMAS, the patient in this case received prednisone, monthly intravenous cyclophosphamide, and IVIG for 6 months. She had an excellent response within a few weeks of the start of therapy. Her prednisone dosage was tapered after 2 months; however, because her symptoms recurred, the corticosteroid was continued for 6 months, after which the dosage was slowly reduced and then stopped. Fortunately, she responded well.\nFor the small number of patients whose disorder is refractory to therapy, adrenocorticotropic hormone therapy is considered potentially more effective than corticosteroid treatment, and rituximab has also been used. Case reports of other modalities reported to provide benefit in persistently symptomatic patients include therapeutic plasma exchange and even autologous stem cell transplant; however, these treatments are not considered the standard of care.[21,22]\nFor the past 2 years, this patient has not required medication and has had no further relapses. She is a happy, healthy little girl who was just enrolled in kindergarten. Because of concerns about recurrence and long-term deficits, she is undergoing follow-up with a pediatric neurologist who is familiar with OMAS and who uses a standardized metric to document her signs and symptoms.[23]\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1616453,
"choiceText": "Demonstrating that a neuroblastoma is present is essential to confirming the diagnosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616454,
"choiceText": "The neuroblastoma found is usually of a high stage and grade",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616455,
"choiceText": "Children older than 4 years are rarely affected",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616456,
"choiceText": "Measurement of urine VMA level is a reliable screening test",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "An international task force recommended that three of four of these criteria be present to diagnose neuroblastoma with OMAS: (1) opsoclonus, (2) myoclonus and ataxia, (3) behavioral change and/or sleep disturbance, and (4) neuroblastoma.<sup>[5]</sup>Patients with OMAS have various neurologic findings, and opsoclonus, myoclonic jerks, and ataxia may not all be present, which means a high index of suspicion is often needed. Although finding a neuroblastoma in conjunction with at least two of these neurologic findings virtually confirms the diagnosis, half of patients with OMAS do not have a detectable neuroblastoma.\r\n<br><br>\r\nAn objective test would be of great help, but the urine VMA test results are often negative, and I<sup>123/131</sup>-methyliodobenzylguanadine (MIBG) scanning does not usually reveal these minimally aggressive tumors. Whole body MRI or fine-cut CT scans can better detect small paravertebral tumors, but their use depends on their availability. When a neuroblastoma is found, the majority are low stage and associated with low-grade disease; this observation was confirmed in the COG-ANBL00P3 study.<sup>[19]</sup>\r\n<br><br>\r\nThe age of onset of OMAS is after the first 6 months of life, and most commonly during the second year. Only rarely is the syndrome reported beyond the third year of life; the oldest patient in the COG study was a 4-year-old child.\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 519321,
"questionText": "Which of the following statements is most accurate regarding the diagnosis of OMAS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1616457,
"choiceText": "A combination of cyclophosphamide, a corticosteroid, and IVIG shows significant benefit",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616458,
"choiceText": "Treatment with immune modulators has been proved to improve long-term outcomes ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616459,
"choiceText": "Autologous stem cell transplant is an essential component of treatment",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616460,
"choiceText": "Surgical resection of the primary tumor is essential for a cure",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The COG conducted a prospective randomized phase 3 clinical trial (COG-ANBL00P3) for children with neuroblastoma-associated OMAS, which demonstrated that the administration of prednisone, chemotherapy, and IVIG resulted in an 80% response rate for OMAS without compromising a neuroblastoma 3-year event-free survival of 94.1%. This study established this combination of agents as standard therapy for OMAS in North America. The SIOPEN trial uses a similar approach with dexamethasone, cyclophosphamide, and rituximab as an immune modulator (rather than IVIG). Subjects whose disorder failed to respond to protocol therapy after 2 months were designated nonresponders and received adrenocorticotropic hormone therapy.<br><br>\r\nChildren with OMAS with relentless symptoms who have benefited from therapeutic plasma exchange or autologous stem cell transplant have been reported. Although these treatments provided resolution of symptoms that were refractory to conventional therapy, they are not considered part of the standard care for patients with OMAS. A transient improvement in the acute symptoms of OMAS can occur after surgery for an identified neuroblastoma; however, complete resolution is rare without further therapy, and surgical removal alone is inadequate in curing OMAS.\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 519322,
"questionText": "Which of the following statements is most accurate regarding the treatment of OMAS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Decreased Speech and Jerky Eye Movements in a 'Clumsy' Toddler"
},
{
"authors": "Vikramjit Kanwar, MBBS, MBA; Shyam Srinivasan, MBBS, DM",
"content": [],
"date": "September 02, 2021",
"figures": [],
"markdown": "# Decreased Speech and Jerky Eye Movements in a 'Clumsy' Toddler\n\n **Authors:** Vikramjit Kanwar, MBBS, MBA; Shyam Srinivasan, MBBS, DM \n **Date:** September 02, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1616453,
"choiceText": "Demonstrating that a neuroblastoma is present is essential to confirming the diagnosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616454,
"choiceText": "The neuroblastoma found is usually of a high stage and grade",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616455,
"choiceText": "Children older than 4 years are rarely affected",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616456,
"choiceText": "Measurement of urine VMA level is a reliable screening test",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "An international task force recommended that three of four of these criteria be present to diagnose neuroblastoma with OMAS: (1) opsoclonus, (2) myoclonus and ataxia, (3) behavioral change and/or sleep disturbance, and (4) neuroblastoma.<sup>[5]</sup>Patients with OMAS have various neurologic findings, and opsoclonus, myoclonic jerks, and ataxia may not all be present, which means a high index of suspicion is often needed. Although finding a neuroblastoma in conjunction with at least two of these neurologic findings virtually confirms the diagnosis, half of patients with OMAS do not have a detectable neuroblastoma.\r\n<br><br>\r\nAn objective test would be of great help, but the urine VMA test results are often negative, and I<sup>123/131</sup>-methyliodobenzylguanadine (MIBG) scanning does not usually reveal these minimally aggressive tumors. Whole body MRI or fine-cut CT scans can better detect small paravertebral tumors, but their use depends on their availability. When a neuroblastoma is found, the majority are low stage and associated with low-grade disease; this observation was confirmed in the COG-ANBL00P3 study.<sup>[19]</sup>\r\n<br><br>\r\nThe age of onset of OMAS is after the first 6 months of life, and most commonly during the second year. Only rarely is the syndrome reported beyond the third year of life; the oldest patient in the COG study was a 4-year-old child.\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 519321,
"questionText": "Which of the following statements is most accurate regarding the diagnosis of OMAS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1616457,
"choiceText": "A combination of cyclophosphamide, a corticosteroid, and IVIG shows significant benefit",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616458,
"choiceText": "Treatment with immune modulators has been proved to improve long-term outcomes ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616459,
"choiceText": "Autologous stem cell transplant is an essential component of treatment",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616460,
"choiceText": "Surgical resection of the primary tumor is essential for a cure",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The COG conducted a prospective randomized phase 3 clinical trial (COG-ANBL00P3) for children with neuroblastoma-associated OMAS, which demonstrated that the administration of prednisone, chemotherapy, and IVIG resulted in an 80% response rate for OMAS without compromising a neuroblastoma 3-year event-free survival of 94.1%. This study established this combination of agents as standard therapy for OMAS in North America. The SIOPEN trial uses a similar approach with dexamethasone, cyclophosphamide, and rituximab as an immune modulator (rather than IVIG). Subjects whose disorder failed to respond to protocol therapy after 2 months were designated nonresponders and received adrenocorticotropic hormone therapy.<br><br>\r\nChildren with OMAS with relentless symptoms who have benefited from therapeutic plasma exchange or autologous stem cell transplant have been reported. Although these treatments provided resolution of symptoms that were refractory to conventional therapy, they are not considered part of the standard care for patients with OMAS. A transient improvement in the acute symptoms of OMAS can occur after surgery for an identified neuroblastoma; however, complete resolution is rare without further therapy, and surgical removal alone is inadequate in curing OMAS.\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 519322,
"questionText": "Which of the following statements is most accurate regarding the treatment of OMAS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Decreased Speech and Jerky Eye Movements in a 'Clumsy' Toddler"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1616449,
"choiceText": "Lead-related neurotoxicity",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616450,
"choiceText": "Sydenham (rheumatic) chorea",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616451,
"choiceText": "Postviral cerebellar ataxia",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616452,
"choiceText": "Opsoclonus-myoclonus ataxia syndrome",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 519320,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1616453,
"choiceText": "Demonstrating that a neuroblastoma is present is essential to confirming the diagnosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616454,
"choiceText": "The neuroblastoma found is usually of a high stage and grade",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616455,
"choiceText": "Children older than 4 years are rarely affected",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616456,
"choiceText": "Measurement of urine VMA level is a reliable screening test",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "An international task force recommended that three of four of these criteria be present to diagnose neuroblastoma with OMAS: (1) opsoclonus, (2) myoclonus and ataxia, (3) behavioral change and/or sleep disturbance, and (4) neuroblastoma.<sup>[5]</sup>Patients with OMAS have various neurologic findings, and opsoclonus, myoclonic jerks, and ataxia may not all be present, which means a high index of suspicion is often needed. Although finding a neuroblastoma in conjunction with at least two of these neurologic findings virtually confirms the diagnosis, half of patients with OMAS do not have a detectable neuroblastoma.\r\n<br><br>\r\nAn objective test would be of great help, but the urine VMA test results are often negative, and I<sup>123/131</sup>-methyliodobenzylguanadine (MIBG) scanning does not usually reveal these minimally aggressive tumors. Whole body MRI or fine-cut CT scans can better detect small paravertebral tumors, but their use depends on their availability. When a neuroblastoma is found, the majority are low stage and associated with low-grade disease; this observation was confirmed in the COG-ANBL00P3 study.<sup>[19]</sup>\r\n<br><br>\r\nThe age of onset of OMAS is after the first 6 months of life, and most commonly during the second year. Only rarely is the syndrome reported beyond the third year of life; the oldest patient in the COG study was a 4-year-old child.\r\n",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 519321,
"questionText": "Which of the following statements is most accurate regarding the diagnosis of OMAS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1616457,
"choiceText": "A combination of cyclophosphamide, a corticosteroid, and IVIG shows significant benefit",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616458,
"choiceText": "Treatment with immune modulators has been proved to improve long-term outcomes ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616459,
"choiceText": "Autologous stem cell transplant is an essential component of treatment",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1616460,
"choiceText": "Surgical resection of the primary tumor is essential for a cure",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The COG conducted a prospective randomized phase 3 clinical trial (COG-ANBL00P3) for children with neuroblastoma-associated OMAS, which demonstrated that the administration of prednisone, chemotherapy, and IVIG resulted in an 80% response rate for OMAS without compromising a neuroblastoma 3-year event-free survival of 94.1%. This study established this combination of agents as standard therapy for OMAS in North America. The SIOPEN trial uses a similar approach with dexamethasone, cyclophosphamide, and rituximab as an immune modulator (rather than IVIG). Subjects whose disorder failed to respond to protocol therapy after 2 months were designated nonresponders and received adrenocorticotropic hormone therapy.<br><br>\r\nChildren with OMAS with relentless symptoms who have benefited from therapeutic plasma exchange or autologous stem cell transplant have been reported. Although these treatments provided resolution of symptoms that were refractory to conventional therapy, they are not considered part of the standard care for patients with OMAS. A transient improvement in the acute symptoms of OMAS can occur after surgery for an identified neuroblastoma; however, complete resolution is rare without further therapy, and surgical removal alone is inadequate in curing OMAS.\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 519322,
"questionText": "Which of the following statements is most accurate regarding the treatment of OMAS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
852434 | /viewarticle/852434 | [
{
"authors": "Noah Gudel, DO; Alyn Hatter, DO, MS; Stanley L. Fox, MD; Marilyn W. Edmunds, PhD, CRNP",
"content": [
"Editor's Note:\n\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.",
"A 50-year-old woman presents due to a persistent cough and dyspnea, despite receiving oral antibiotic therapy for a presumed exacerbation of chronic obstructive pulmonary disease (COPD). She reports moderate sputum production and occasional mild hemoptysis. She denies any recent contact with ill persons or recent travel. She additionally reports frequent and often heavy epistaxis. She denies having fevers, night sweats, or unintentional weight loss. She has not experienced any recent diarrhea, melena, or hematochezia.",
"In addition to a medical history of seizures, seasonal allergies, hypertension, impaired gastric motility, anxiety, depression, and gastroesophageal reflux disease, she has a longstanding history of COPD, which is normally well-controlled with inhaled fluticasone/salmeterol and albuterol.",
"The patient's other home medications include ethosuximide, loratadine, verapamil, metoclopramide, promethazine, alprazolam, temazepam, duloxetine, esomeprazole, aminocaproic acid, ferrous sulfate, and a multivitamin. Her surgical history includes a cholecystectomy, knee arthroscopy, and a partial hysterectomy for cervical carcinoma.",
"The patient's family history does not contribute to this admission, but it is significant in the pathologic process (see Figures 1-3). The patient is a current smoker but does not use any illicit drugs.",
"Figure 1.",
"Figure 1.",
"Figure 2.",
"Figure 2.",
"Figure 3.",
"Figure 3."
],
"date": "August 20, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/852/434/852434-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/852/434/852434-Thumb2.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/852/434/852434-Thumb3.png"
}
],
"markdown": "# A 50-Year-Old With Telangiectasia, Cough, and Epistaxis\n\n **Authors:** Noah Gudel, DO; Alyn Hatter, DO, MS; Stanley L. Fox, MD; Marilyn W. Edmunds, PhD, CRNP \n **Date:** August 20, 2021\n\n ## Content\n\n Editor's Note:\n\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.\nA 50-year-old woman presents due to a persistent cough and dyspnea, despite receiving oral antibiotic therapy for a presumed exacerbation of chronic obstructive pulmonary disease (COPD). She reports moderate sputum production and occasional mild hemoptysis. She denies any recent contact with ill persons or recent travel. She additionally reports frequent and often heavy epistaxis. She denies having fevers, night sweats, or unintentional weight loss. She has not experienced any recent diarrhea, melena, or hematochezia.\nIn addition to a medical history of seizures, seasonal allergies, hypertension, impaired gastric motility, anxiety, depression, and gastroesophageal reflux disease, she has a longstanding history of COPD, which is normally well-controlled with inhaled fluticasone/salmeterol and albuterol.\nThe patient's other home medications include ethosuximide, loratadine, verapamil, metoclopramide, promethazine, alprazolam, temazepam, duloxetine, esomeprazole, aminocaproic acid, ferrous sulfate, and a multivitamin. Her surgical history includes a cholecystectomy, knee arthroscopy, and a partial hysterectomy for cervical carcinoma.\nThe patient's family history does not contribute to this admission, but it is significant in the pathologic process (see Figures 1-3). The patient is a current smoker but does not use any illicit drugs.\nFigure 1.\nFigure 1.\nFigure 2.\nFigure 2.\nFigure 3.\nFigure 3.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n\n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A 50-Year-Old With Telangiectasia, Cough, and Epistaxis"
},
{
"authors": "Noah Gudel, DO; Alyn Hatter, DO, MS; Stanley L. Fox, MD; Marilyn W. Edmunds, PhD, CRNP",
"content": [
"The physical examination reveals a 50-year-old woman in no acute distress. Her oral temperature is 99.4°F (37.4°C). Her pulse is 80 beats/min, and her blood pressure is 111/63 mm Hg. A pulse oximetry examination reveals a room air saturation of 97%. Examination of the lungs shows bilateral rhonchi and mild wheezing. Examination of the cardiovascular system is unremarkable, as is the abdominal examination. Examination of the skin is remarkable for the pathologic process revealed in the images seen in Figures 1-3. She is also noted to have multiple superficial nonbleeding vessels on the nasal septum.",
"Figure 1.",
"Figure 1.",
"Figure 2.",
"Figure 2.",
"Figure 3.",
"Figure 3.",
"Portable chest x-ray is obtained and does not reveal any effusions or infiltrates. A complete blood cell count shows an increased white blood cell count of 15.6 x 103/µL (15.6 x 109/L; reference range: 4.4-11.3 x 103/µL), as well as a microcytic, hypochromic anemia (with a hemoglobin of 9.2 g/dL [92 g/L], a mean corpuscular volume of 76 μ/m3 [76 fL], and a mean corpuscular hemoglobin of 21.6 pg/cell)."
],
"date": "August 20, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/852/434/852434-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/852/434/852434-Thumb2.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/852/434/852434-Thumb3.png"
}
],
"markdown": "# A 50-Year-Old With Telangiectasia, Cough, and Epistaxis\n\n **Authors:** Noah Gudel, DO; Alyn Hatter, DO, MS; Stanley L. Fox, MD; Marilyn W. Edmunds, PhD, CRNP \n **Date:** August 20, 2021\n\n ## Content\n\n The physical examination reveals a 50-year-old woman in no acute distress. Her oral temperature is 99.4°F (37.4°C). Her pulse is 80 beats/min, and her blood pressure is 111/63 mm Hg. A pulse oximetry examination reveals a room air saturation of 97%. Examination of the lungs shows bilateral rhonchi and mild wheezing. Examination of the cardiovascular system is unremarkable, as is the abdominal examination. Examination of the skin is remarkable for the pathologic process revealed in the images seen in Figures 1-3. She is also noted to have multiple superficial nonbleeding vessels on the nasal septum.\nFigure 1.\nFigure 1.\nFigure 2.\nFigure 2.\nFigure 3.\nFigure 3.\nPortable chest x-ray is obtained and does not reveal any effusions or infiltrates. A complete blood cell count shows an increased white blood cell count of 15.6 x 103/µL (15.6 x 109/L; reference range: 4.4-11.3 x 103/µL), as well as a microcytic, hypochromic anemia (with a hemoglobin of 9.2 g/dL [92 g/L], a mean corpuscular volume of 76 μ/m3 [76 fL], and a mean corpuscular hemoglobin of 21.6 pg/cell).\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 898331,
"choiceText": "Dermatomyositis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898333,
"choiceText": "von Willebrand disease",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898335,
"choiceText": "Osler-Weber-Rendu syndrome",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898337,
"choiceText": "Louis-Bar syndrome\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 283117,
"questionText": "Based only on these findings, which condition is most likely responsible for her abnormal skin findings?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 50-Year-Old With Telangiectasia, Cough, and Epistaxis"
},
{
"authors": "Noah Gudel, DO; Alyn Hatter, DO, MS; Stanley L. Fox, MD; Marilyn W. Edmunds, PhD, CRNP",
"content": [
"Osler-Weber-Rendu syndrome (also known as hereditary hemorrhagic telangiectasia [HHT]) is inherited in an autosomal dominant manner.[1] The disease is characterized by mucocutaneous and visceral telangiectases and arteriovenous malformations (AVM). Although epistaxis is the most common symptom, serious complications can arise as a result of large telangiectases and AVMs affecting the central nervous system (CNS), lungs, liver, spleen, and GI mucosa.",
"Osler-Weber-Rendu syndrome has been reported in all racial groups, and its prevalence varies among populations. For example, 1 case per 8345 persons is reported in France. Even greater frequencies have been reported for the Dutch Antilles.[2] The estimated frequency in the US state of Vermont is 1 per 16,500 persons.[2] Away from these discrete populations, however, Osler-Weber-Rendu syndrome is a rare condition that is estimated to affect 1-2 persons per 100,000 population in the United States.[2] It affects men and women equally. Although Osler-Weber-Rendu syndrome can manifest in childhood, it more commonly appears in adolescents and young adults.[2]",
"The prognosis for most patients is generally good when sources of bleeding can be found and controlled. Recurrent epistaxis and GI mucosal bleeds can result in melena and iron-deficiency anemia.[2] Nosebleeds tend to become more serious with age, with 10%-30% of patients requiring blood transfusion.[2] Patients with pulmonary AVMs and extensive GI telangiectases are at risk for life-threatening hemorrhage at these sites.[2] In patients who have pulmonary AVMs, the risk for stroke is estimated to be 2% per year, while the incidence of brain abscess is estimated to be 1% per year.[2] These patients are at risk for paradoxical bland and septic emboli.[2] Cases have been reported of extensive hepatic involvement, with some patients requiring liver transplantation.[3] Despite the numerous potential complications associated with Osler-Weber-Rendu syndrome, only 10% of these patients die from complications of the disease.[2]"
],
"date": "August 20, 2021",
"figures": [],
"markdown": "# A 50-Year-Old With Telangiectasia, Cough, and Epistaxis\n\n **Authors:** Noah Gudel, DO; Alyn Hatter, DO, MS; Stanley L. Fox, MD; Marilyn W. Edmunds, PhD, CRNP \n **Date:** August 20, 2021\n\n ## Content\n\n Osler-Weber-Rendu syndrome (also known as hereditary hemorrhagic telangiectasia [HHT]) is inherited in an autosomal dominant manner.[1] The disease is characterized by mucocutaneous and visceral telangiectases and arteriovenous malformations (AVM). Although epistaxis is the most common symptom, serious complications can arise as a result of large telangiectases and AVMs affecting the central nervous system (CNS), lungs, liver, spleen, and GI mucosa.\nOsler-Weber-Rendu syndrome has been reported in all racial groups, and its prevalence varies among populations. For example, 1 case per 8345 persons is reported in France. Even greater frequencies have been reported for the Dutch Antilles.[2] The estimated frequency in the US state of Vermont is 1 per 16,500 persons.[2] Away from these discrete populations, however, Osler-Weber-Rendu syndrome is a rare condition that is estimated to affect 1-2 persons per 100,000 population in the United States.[2] It affects men and women equally. Although Osler-Weber-Rendu syndrome can manifest in childhood, it more commonly appears in adolescents and young adults.[2]\nThe prognosis for most patients is generally good when sources of bleeding can be found and controlled. Recurrent epistaxis and GI mucosal bleeds can result in melena and iron-deficiency anemia.[2] Nosebleeds tend to become more serious with age, with 10%-30% of patients requiring blood transfusion.[2] Patients with pulmonary AVMs and extensive GI telangiectases are at risk for life-threatening hemorrhage at these sites.[2] In patients who have pulmonary AVMs, the risk for stroke is estimated to be 2% per year, while the incidence of brain abscess is estimated to be 1% per year.[2] These patients are at risk for paradoxical bland and septic emboli.[2] Cases have been reported of extensive hepatic involvement, with some patients requiring liver transplantation.[3] Despite the numerous potential complications associated with Osler-Weber-Rendu syndrome, only 10% of these patients die from complications of the disease.[2]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 898331,
"choiceText": "Dermatomyositis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898333,
"choiceText": "von Willebrand disease",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898335,
"choiceText": "Osler-Weber-Rendu syndrome",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898337,
"choiceText": "Louis-Bar syndrome\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 283117,
"questionText": "Based only on these findings, which condition is most likely responsible for her abnormal skin findings?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 50-Year-Old With Telangiectasia, Cough, and Epistaxis"
},
{
"authors": "Noah Gudel, DO; Alyn Hatter, DO, MS; Stanley L. Fox, MD; Marilyn W. Edmunds, PhD, CRNP",
"content": [
"The first gene found to be responsible for Osler-Weber-Rendu syndrome was mapped to chromosome 9q33 and identified as ENG (endoglin).[4] Endoglin serves as a transforming growth factor beta binding protein. Various mutations have been reported at this site, which represents the most common form of Osler-Weber-Rendu syndrome. Subsequently, other genes have been mapped to chromosomes 12q13, 5q31-32, and 7p14, leading to Osler-Weber-Rendu syndrome types 2 through 4, respectively.[5] Osler-Weber-Rendu syndrome type 2 is defined by a mutation in the ALK1 gene, which produces an activin-like tyrosine kinase. Both ENG and ALK1 gene products help mediate vascular remodeling by endothelial cells[1,5]; therefore, the lesions in Osler-Weber-Rendu syndrome are thought to develop from faulty repair mechanisms in damaged vasculature.[6]",
"Traditionally, the diagnosis was made on the basis of the classic triad of epistaxis, telangiectasia, and family history. In 1999, the Scientific Advisory Board of Osler-Weber-Rendu-HHT Foundation International published stringent criteria to help guide the diagnosis of Osler-Weber-Rendu syndrome.[1] The criteria include the following[2]:",
"Epistaxis: Spontaneous, recurrent nose bleeds",
"Telangiectases: Multiple and at characteristic sites (lips, oral cavity, fingers, nose)",
"Visceral lesions: Such as GI telangiectasia (with or without bleeding), pulmonary AVM, hepatic AVM, cerebral AVM, spinal AVM",
"Family history: A first-degree relative with Osler-Weber-Rendu syndrome according to these criteria",
"A diagnosis of Osler-Weber-Rendu syndrome is considered definite if three criteria are present, possible or suspected if two criteria are present, and unlikely if fewer than two criteria are met.[1] A clinical diagnosis in children may be difficult because epistaxis may present years before cutaneous telangiectasia.",
"Skin biopsy findings can be used to help confirm the diagnosis. A punch biopsy is usually adequate. The findings are localized in the dermal upper-horizontal plexus; dilated capillaries and new vessel formation are the classic features associated with this diagnosis. In the dermis, the walls of dilated vessels may be thickened.[2]",
"The presenting symptom is recurrent epistaxis, which is seen in 95% of patients.[2] Telangiectases often appear after puberty and in characteristic locations.[2] The lips and oral mucosa are nearly always involved. Telangiectases may be scattered about the face, nose, ears, trunk, and arms. The fingers and hands are also frequently involved. Although not pathognomonic, dilated capillaries in the nail bed and nail folds are characteristic of Osler-Weber-Rendu syndrome.[2,7] Telangiectases can be seen throughout the GI mucosa with endoscopy.[2]",
"Patients with severe pulmonary AVMs can develop right-to-left shunting with hypoxemia, cyanosis, and clubbing of the digits.[2] In the obstetric patient, pulmonary AVMs can hemorrhage, leading to life-threatening complications for both the mother and fetus.[2] When AVMs develop in the CNS or spinal canal, patients can be affected by stroke, seizure, or focal neurologic signs.[2] Extensive hepatic involvement is seen in 8%-31% of patients with Osler-Weber-Rendu syndrome.[2] Fistulae in the liver can cause portal hypertension, cirrhosis, and hepatomegaly with high-output heart failure.[2,3]",
"When multiple cutaneous telangiectases are present, the differential diagnosis could include essential telangiectasia, ataxia-telangiectasia, CREST (calcinosis, Raynaud phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia) syndrome, and rosacea.[2,8] When Osler-Weber-Rendu syndrome is diagnosed, patients should be monitored for melena and iron-deficiency anemia.[2] Liver studies including transaminases and bilirubin levels should be performed regularly in patients with known or suspected hepatic involvement. MRI and CT scanning may be needed to evaluate the extent of AVMs in the viscera and meninges.[2] Angiography is often used when surgical interventions are considered.[2]"
],
"date": "August 20, 2021",
"figures": [],
"markdown": "# A 50-Year-Old With Telangiectasia, Cough, and Epistaxis\n\n **Authors:** Noah Gudel, DO; Alyn Hatter, DO, MS; Stanley L. Fox, MD; Marilyn W. Edmunds, PhD, CRNP \n **Date:** August 20, 2021\n\n ## Content\n\n The first gene found to be responsible for Osler-Weber-Rendu syndrome was mapped to chromosome 9q33 and identified as ENG (endoglin).[4] Endoglin serves as a transforming growth factor beta binding protein. Various mutations have been reported at this site, which represents the most common form of Osler-Weber-Rendu syndrome. Subsequently, other genes have been mapped to chromosomes 12q13, 5q31-32, and 7p14, leading to Osler-Weber-Rendu syndrome types 2 through 4, respectively.[5] Osler-Weber-Rendu syndrome type 2 is defined by a mutation in the ALK1 gene, which produces an activin-like tyrosine kinase. Both ENG and ALK1 gene products help mediate vascular remodeling by endothelial cells[1,5]; therefore, the lesions in Osler-Weber-Rendu syndrome are thought to develop from faulty repair mechanisms in damaged vasculature.[6]\nTraditionally, the diagnosis was made on the basis of the classic triad of epistaxis, telangiectasia, and family history. In 1999, the Scientific Advisory Board of Osler-Weber-Rendu-HHT Foundation International published stringent criteria to help guide the diagnosis of Osler-Weber-Rendu syndrome.[1] The criteria include the following[2]:\nEpistaxis: Spontaneous, recurrent nose bleeds\nTelangiectases: Multiple and at characteristic sites (lips, oral cavity, fingers, nose)\nVisceral lesions: Such as GI telangiectasia (with or without bleeding), pulmonary AVM, hepatic AVM, cerebral AVM, spinal AVM\nFamily history: A first-degree relative with Osler-Weber-Rendu syndrome according to these criteria\nA diagnosis of Osler-Weber-Rendu syndrome is considered definite if three criteria are present, possible or suspected if two criteria are present, and unlikely if fewer than two criteria are met.[1] A clinical diagnosis in children may be difficult because epistaxis may present years before cutaneous telangiectasia.\nSkin biopsy findings can be used to help confirm the diagnosis. A punch biopsy is usually adequate. The findings are localized in the dermal upper-horizontal plexus; dilated capillaries and new vessel formation are the classic features associated with this diagnosis. In the dermis, the walls of dilated vessels may be thickened.[2]\nThe presenting symptom is recurrent epistaxis, which is seen in 95% of patients.[2] Telangiectases often appear after puberty and in characteristic locations.[2] The lips and oral mucosa are nearly always involved. Telangiectases may be scattered about the face, nose, ears, trunk, and arms. The fingers and hands are also frequently involved. Although not pathognomonic, dilated capillaries in the nail bed and nail folds are characteristic of Osler-Weber-Rendu syndrome.[2,7] Telangiectases can be seen throughout the GI mucosa with endoscopy.[2]\nPatients with severe pulmonary AVMs can develop right-to-left shunting with hypoxemia, cyanosis, and clubbing of the digits.[2] In the obstetric patient, pulmonary AVMs can hemorrhage, leading to life-threatening complications for both the mother and fetus.[2] When AVMs develop in the CNS or spinal canal, patients can be affected by stroke, seizure, or focal neurologic signs.[2] Extensive hepatic involvement is seen in 8%-31% of patients with Osler-Weber-Rendu syndrome.[2] Fistulae in the liver can cause portal hypertension, cirrhosis, and hepatomegaly with high-output heart failure.[2,3]\nWhen multiple cutaneous telangiectases are present, the differential diagnosis could include essential telangiectasia, ataxia-telangiectasia, CREST (calcinosis, Raynaud phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia) syndrome, and rosacea.[2,8] When Osler-Weber-Rendu syndrome is diagnosed, patients should be monitored for melena and iron-deficiency anemia.[2] Liver studies including transaminases and bilirubin levels should be performed regularly in patients with known or suspected hepatic involvement. MRI and CT scanning may be needed to evaluate the extent of AVMs in the viscera and meninges.[2] Angiography is often used when surgical interventions are considered.[2]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A 50-Year-Old With Telangiectasia, Cough, and Epistaxis"
},
{
"authors": "Noah Gudel, DO; Alyn Hatter, DO, MS; Stanley L. Fox, MD; Marilyn W. Edmunds, PhD, CRNP",
"content": [
"Management of Osler-Weber-Rendu syndrome is mostly supportive. Nasal packing and cautery may be required for routine epistaxis. Autologous skin grafting of the nasal septum, called septal dermoplasty, can be used in severe cases of recurrent epistaxis.[2] Blood transfusions and iron replacement may be needed in some patients. Aminocaproic acid is an antifibrinolytic used to prevent and treat mucosal bleeding.[2] Oral contraceptives can also be helpful in treating the chronic, obscure GI bleed.[2]",
"Electrocautery and neodymium:yttrium-aluminum-garnet (Nd:YAG) laser ablation have been used to treat cutaneous skin lesions as well as mucosal telangiectases.[2] Transluminal embolization of pulmonary fistulae is an effective therapy for patients with bilateral lung involvement.[2] Solitary lesions, as well as symptomatic lesions in the setting of diffuse disease, can be resected surgically.[2] Neurovascular surgery is indicated in select CNS AVMs.[2] As with any genetic disease, family counseling and education about inheritance should be included in the management of the condition.",
"During this patient's acute presentation related to her COPD, the incidental finding of telangiectases led to a diagnosis of Osler-Weber-Rendu syndrome. She received smoking-cessation counseling while hospitalized and was discharged to home, in stable condition, after several days of oxygen supplementation, antibiotics, and corticosteroids for her COPD exacerbation."
],
"date": "August 20, 2021",
"figures": [],
"markdown": "# A 50-Year-Old With Telangiectasia, Cough, and Epistaxis\n\n **Authors:** Noah Gudel, DO; Alyn Hatter, DO, MS; Stanley L. Fox, MD; Marilyn W. Edmunds, PhD, CRNP \n **Date:** August 20, 2021\n\n ## Content\n\n Management of Osler-Weber-Rendu syndrome is mostly supportive. Nasal packing and cautery may be required for routine epistaxis. Autologous skin grafting of the nasal septum, called septal dermoplasty, can be used in severe cases of recurrent epistaxis.[2] Blood transfusions and iron replacement may be needed in some patients. Aminocaproic acid is an antifibrinolytic used to prevent and treat mucosal bleeding.[2] Oral contraceptives can also be helpful in treating the chronic, obscure GI bleed.[2]\nElectrocautery and neodymium:yttrium-aluminum-garnet (Nd:YAG) laser ablation have been used to treat cutaneous skin lesions as well as mucosal telangiectases.[2] Transluminal embolization of pulmonary fistulae is an effective therapy for patients with bilateral lung involvement.[2] Solitary lesions, as well as symptomatic lesions in the setting of diffuse disease, can be resected surgically.[2] Neurovascular surgery is indicated in select CNS AVMs.[2] As with any genetic disease, family counseling and education about inheritance should be included in the management of the condition.\nDuring this patient's acute presentation related to her COPD, the incidental finding of telangiectases led to a diagnosis of Osler-Weber-Rendu syndrome. She received smoking-cessation counseling while hospitalized and was discharged to home, in stable condition, after several days of oxygen supplementation, antibiotics, and corticosteroids for her COPD exacerbation.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 898339,
"choiceText": "GI bleeding",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898341,
"choiceText": "Hemoptysis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898343,
"choiceText": "Epistaxis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898345,
"choiceText": "Hemorrhagic stroke\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Often diagnosed in the teenage years, this condition commonly presents with epistaxis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 283119,
"questionText": "Which of the following is the most common presenting symptom seen in patients with Osler-Weber-Rendu syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 898347,
"choiceText": "It should always involve a vascular consult for possible embolization",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898349,
"choiceText": "It should include a routine gastroenterology consult to rule out bleeding from a GI AVM",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898351,
"choiceText": "It is mostly supportive",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898353,
"choiceText": "Regular platelet transfusions are typically required\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Management of Osler-Weber-Rendu syndrome is mostly supportive. Nasal packing and cautery may be required for routine epistaxis. Autologous skin grafting of the nasal septum, called septal dermoplasty, can be used in severe cases of recurrent epistaxis. Blood transfusions and iron replacement may be needed in some patients. Aminocaproic acid is an antifibrinolytic used to prevent and treat mucosal bleeding. Oral contraceptives can also be helpful in treating the chronic, obscure GI bleed.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 283121,
"questionText": "Which of the following is most accurate regarding the management of patients with Osler-Weber-Rendu syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 50-Year-Old With Telangiectasia, Cough, and Epistaxis"
},
{
"authors": "Noah Gudel, DO; Alyn Hatter, DO, MS; Stanley L. Fox, MD; Marilyn W. Edmunds, PhD, CRNP",
"content": [],
"date": "August 20, 2021",
"figures": [],
"markdown": "# A 50-Year-Old With Telangiectasia, Cough, and Epistaxis\n\n **Authors:** Noah Gudel, DO; Alyn Hatter, DO, MS; Stanley L. Fox, MD; Marilyn W. Edmunds, PhD, CRNP \n **Date:** August 20, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 898339,
"choiceText": "GI bleeding",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898341,
"choiceText": "Hemoptysis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898343,
"choiceText": "Epistaxis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898345,
"choiceText": "Hemorrhagic stroke\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Often diagnosed in the teenage years, this condition commonly presents with epistaxis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 283119,
"questionText": "Which of the following is the most common presenting symptom seen in patients with Osler-Weber-Rendu syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 898347,
"choiceText": "It should always involve a vascular consult for possible embolization",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898349,
"choiceText": "It should include a routine gastroenterology consult to rule out bleeding from a GI AVM",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898351,
"choiceText": "It is mostly supportive",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898353,
"choiceText": "Regular platelet transfusions are typically required\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Management of Osler-Weber-Rendu syndrome is mostly supportive. Nasal packing and cautery may be required for routine epistaxis. Autologous skin grafting of the nasal septum, called septal dermoplasty, can be used in severe cases of recurrent epistaxis. Blood transfusions and iron replacement may be needed in some patients. Aminocaproic acid is an antifibrinolytic used to prevent and treat mucosal bleeding. Oral contraceptives can also be helpful in treating the chronic, obscure GI bleed.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 283121,
"questionText": "Which of the following is most accurate regarding the management of patients with Osler-Weber-Rendu syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 50-Year-Old With Telangiectasia, Cough, and Epistaxis"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 898331,
"choiceText": "Dermatomyositis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898333,
"choiceText": "von Willebrand disease",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898335,
"choiceText": "Osler-Weber-Rendu syndrome",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898337,
"choiceText": "Louis-Bar syndrome\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 283117,
"questionText": "Based only on these findings, which condition is most likely responsible for her abnormal skin findings?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 898339,
"choiceText": "GI bleeding",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898341,
"choiceText": "Hemoptysis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898343,
"choiceText": "Epistaxis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898345,
"choiceText": "Hemorrhagic stroke\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Often diagnosed in the teenage years, this condition commonly presents with epistaxis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 283119,
"questionText": "Which of the following is the most common presenting symptom seen in patients with Osler-Weber-Rendu syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 898347,
"choiceText": "It should always involve a vascular consult for possible embolization",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898349,
"choiceText": "It should include a routine gastroenterology consult to rule out bleeding from a GI AVM",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898351,
"choiceText": "It is mostly supportive",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 898353,
"choiceText": "Regular platelet transfusions are typically required\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Management of Osler-Weber-Rendu syndrome is mostly supportive. Nasal packing and cautery may be required for routine epistaxis. Autologous skin grafting of the nasal septum, called septal dermoplasty, can be used in severe cases of recurrent epistaxis. Blood transfusions and iron replacement may be needed in some patients. Aminocaproic acid is an antifibrinolytic used to prevent and treat mucosal bleeding. Oral contraceptives can also be helpful in treating the chronic, obscure GI bleed.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 283121,
"questionText": "Which of the following is most accurate regarding the management of patients with Osler-Weber-Rendu syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
955983 | /viewarticle/955983 | [
{
"authors": "Dushyant Singh Dahiya, MD; Farah Wani, MD; Tin Wong; Asim Kichloo, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 50-year-old man with hypertension and type 2 diabetes mellitus presents to the emergency department (ED) with a 4-day history of epigastric pain. About 1 year earlier, he received a diagnosis of end-stage renal disease (ESRD) secondary to diabetic nephropathy and started hemodialysis. Approximately 8 months later, he transitioned to continuous ambulatory peritoneal dialysis (PD) to accommodate his travel plans.",
"The patient flew to Michigan about 2 weeks ago to visit his grandchildren, who had \"the flu,\" for a week. He was highly compliant with PD throughout the trip and did not have any complaints.",
"About 4 days ago, he noted the onset of mild epigastric pain, which he initially attributed to overeating throughout the trip and which he tried to manage with over-the-counter calcium carbonate. However, during the next few days, the pain worsened, and he started to develop shortness of breath, prompting him to present to the ED.",
"He describes the pain as sharp, nonradiating, and diffuse but most prominent in the epigastric region. He rates the intensity of the pain at 7/10. Movement, deep breathing, and coughing exacerbate the pain. He reports no specific relieving factors or positional variations of the pain. He also feels nauseated and warm but did not check his temperature at home."
],
"date": "August 16, 2021",
"figures": [],
"markdown": "# After Travel, a 50-Year-Old Grandfather Has Dyspnea, Fever\n\n **Authors:** Dushyant Singh Dahiya, MD; Farah Wani, MD; Tin Wong; Asim Kichloo, MD \n **Date:** August 16, 2021\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 50-year-old man with hypertension and type 2 diabetes mellitus presents to the emergency department (ED) with a 4-day history of epigastric pain. About 1 year earlier, he received a diagnosis of end-stage renal disease (ESRD) secondary to diabetic nephropathy and started hemodialysis. Approximately 8 months later, he transitioned to continuous ambulatory peritoneal dialysis (PD) to accommodate his travel plans.\nThe patient flew to Michigan about 2 weeks ago to visit his grandchildren, who had \"the flu,\" for a week. He was highly compliant with PD throughout the trip and did not have any complaints.\nAbout 4 days ago, he noted the onset of mild epigastric pain, which he initially attributed to overeating throughout the trip and which he tried to manage with over-the-counter calcium carbonate. However, during the next few days, the pain worsened, and he started to develop shortness of breath, prompting him to present to the ED.\nHe describes the pain as sharp, nonradiating, and diffuse but most prominent in the epigastric region. He rates the intensity of the pain at 7/10. Movement, deep breathing, and coughing exacerbate the pain. He reports no specific relieving factors or positional variations of the pain. He also feels nauseated and warm but did not check his temperature at home.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "After Travel, a 50-Year-Old Grandfather Has Dyspnea, Fever"
},
{
"authors": "Dushyant Singh Dahiya, MD; Farah Wani, MD; Tin Wong; Asim Kichloo, MD",
"content": [
"Upon examination, the patient appears to be in moderate distress. His temperature is 101.5°F (38.6°C); respiration rate is 22 breaths/min, with a peripheral capillary oxygen saturation of 92% on room air; heart rate is 88 beats/min; and blood pressure is 160/90 mm Hg. His body mass index is 27 kg/m2.",
"Examination of the respiratory system is limited owing to significant pain on deep inspiration. His lungs are grossly clear to auscultation bilaterally, except for reduced air entry at the lung bases. The cardiac examination reveals tachycardia, with normal heart sounds and no murmurs. The patient's abdomen is nondistended, and examination shows diffuse tenderness to light palpation, guarding, and positive rebound tenderness. He has a negative Murphy sign.",
"A PD catheter with a dressed site is noted; no erythema or warmth is observed around the region. For context, Figure 1 shows a similar PD catheter site in a different patient. Mild 1+ bilateral pedal edema is noted from the mid-tibial region down to the ankles. The remainder of the physical examination findings are unremarkable.",
"Figure 1.",
"Laboratory investigations reveal a hemoglobin level of 11.5 g/dL (reference range, 13.5-17.5 g/dL) and a hematocrit of 33.1% (reference range, 41%-50%). Mean corpuscular volume and mean corpuscular hemoglobin concentration are both normal. Other laboratory values are as follows:",
"White blood cell (WBC) count: 15,000 cells/µL (reference range, 4000-11,000 cells/µL), with 80% neutrophils and decreased lymphocytes (10%)",
"Platelet count: 200,000 cells/µL (reference range, 150,000-400,000 cells/µL)",
"Troponin level: 0.45 ng/mL (reference range, < 0.4 ng/mL)",
"Brain-type natriuretic peptide level: 283 pg/mL (reference range, < 100 pg/mL)",
"The results of a basic metabolic panel are grossly elevated, with the following findings:",
"Sodium level: 150 mmol/L (reference range, 135-147 mmol/L)",
"Potassium level: 5.6 mmol/L (reference range, 3.5-5.0 mmol/L)",
"Chloride level: 115 mmol/L (reference range, 98-106 mmol/L)",
"Carbon dioxide level: 33 mmol/L (reference range, 23-29 mmol/L)",
"Blood urea nitrogen level: 45 mg/dL (reference range, 8-24 mg/dL)",
"Creatinine level: 1.7 mg/dL (reference range, 0.9-1.3 mg/dL)",
"The total serum protein level is 5.5 g/dL (reference range, 6.4-8.3 g/dL), and the serum lactate dehydrogenase level is 150 U/L (reference range, 140-280 U/L; upper limit of normal, 222 U/L).",
"ECG shows nonspecific T-wave changes. Figure 2 is an example of similar ECG findings in another patient.",
"Figure 2.",
"Echocardiography performed 6 months earlier revealed a left ventricular ejection fraction of 60%. Chest radiography shows a mild pleural effusion. Because the patient has an elevated D-dimer level, CT angiography of the chest is obtained. Figure 3 shows results similar to those in this case in a different patient. Fluid analysis from the PD is performed, and the results are pending.",
"Figure 3."
],
"date": "August 16, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/955/983/955983-Thumb1.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/955/983/955983-Thumb2.jpg"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/955/983/955983-Thumb3.jpg"
}
],
"markdown": "# After Travel, a 50-Year-Old Grandfather Has Dyspnea, Fever\n\n **Authors:** Dushyant Singh Dahiya, MD; Farah Wani, MD; Tin Wong; Asim Kichloo, MD \n **Date:** August 16, 2021\n\n ## Content\n\n Upon examination, the patient appears to be in moderate distress. His temperature is 101.5°F (38.6°C); respiration rate is 22 breaths/min, with a peripheral capillary oxygen saturation of 92% on room air; heart rate is 88 beats/min; and blood pressure is 160/90 mm Hg. His body mass index is 27 kg/m2.\nExamination of the respiratory system is limited owing to significant pain on deep inspiration. His lungs are grossly clear to auscultation bilaterally, except for reduced air entry at the lung bases. The cardiac examination reveals tachycardia, with normal heart sounds and no murmurs. The patient's abdomen is nondistended, and examination shows diffuse tenderness to light palpation, guarding, and positive rebound tenderness. He has a negative Murphy sign.\nA PD catheter with a dressed site is noted; no erythema or warmth is observed around the region. For context, Figure 1 shows a similar PD catheter site in a different patient. Mild 1+ bilateral pedal edema is noted from the mid-tibial region down to the ankles. The remainder of the physical examination findings are unremarkable.\nFigure 1.\nLaboratory investigations reveal a hemoglobin level of 11.5 g/dL (reference range, 13.5-17.5 g/dL) and a hematocrit of 33.1% (reference range, 41%-50%). Mean corpuscular volume and mean corpuscular hemoglobin concentration are both normal. Other laboratory values are as follows:\nWhite blood cell (WBC) count: 15,000 cells/µL (reference range, 4000-11,000 cells/µL), with 80% neutrophils and decreased lymphocytes (10%)\nPlatelet count: 200,000 cells/µL (reference range, 150,000-400,000 cells/µL)\nTroponin level: 0.45 ng/mL (reference range, < 0.4 ng/mL)\nBrain-type natriuretic peptide level: 283 pg/mL (reference range, < 100 pg/mL)\nThe results of a basic metabolic panel are grossly elevated, with the following findings:\nSodium level: 150 mmol/L (reference range, 135-147 mmol/L)\nPotassium level: 5.6 mmol/L (reference range, 3.5-5.0 mmol/L)\nChloride level: 115 mmol/L (reference range, 98-106 mmol/L)\nCarbon dioxide level: 33 mmol/L (reference range, 23-29 mmol/L)\nBlood urea nitrogen level: 45 mg/dL (reference range, 8-24 mg/dL)\nCreatinine level: 1.7 mg/dL (reference range, 0.9-1.3 mg/dL)\nThe total serum protein level is 5.5 g/dL (reference range, 6.4-8.3 g/dL), and the serum lactate dehydrogenase level is 150 U/L (reference range, 140-280 U/L; upper limit of normal, 222 U/L).\nECG shows nonspecific T-wave changes. Figure 2 is an example of similar ECG findings in another patient.\nFigure 2.\nEchocardiography performed 6 months earlier revealed a left ventricular ejection fraction of 60%. Chest radiography shows a mild pleural effusion. Because the patient has an elevated D-dimer level, CT angiography of the chest is obtained. Figure 3 shows results similar to those in this case in a different patient. Fluid analysis from the PD is performed, and the results are pending.\nFigure 3.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n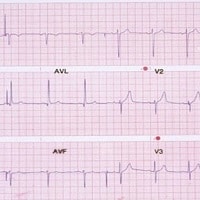 \n\n**Figure 3.** \n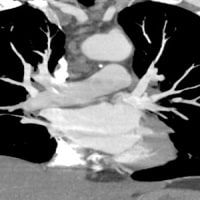 \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1612086,
"choiceText": "Acute myocardial infarction",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612087,
"choiceText": "Perforation of peptic ulcer",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612088,
"choiceText": "Hypertensive urgency",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612089,
"choiceText": "Acute peritonitis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612090,
"choiceText": "Acute pericarditis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 517840,
"questionText": "On the basis of these findings only, what is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "After Travel, a 50-Year-Old Grandfather Has Dyspnea, Fever"
},
{
"authors": "Dushyant Singh Dahiya, MD; Farah Wani, MD; Tin Wong; Asim Kichloo, MD",
"content": [
"This patient's acute-onset, diffuse abdominal pain; abdominal tenderness on palpation; and history of PD all pointed to a diagnosis of acute peritonitis. Initially, broad-spectrum antibiotic coverage was provided with vancomycin and cefotaxime. The peritoneal fluid analysis was positive for Staphylococcus epidermidis, which was sensitive to cefotaxime. Hence, vancomycin was discontinued and cefotaxime was continued for a total of 5 days. The patient's symptoms resolved completely, and he was eventually discharged home.",
"Peritonitis is a common complication of PD[1]; the PD catheter serves as a highly effective portal of entry for bacteria into the abdomen. Ever since Dr Henry Tenckhoff invented the first indwelling catheter in 1968, patients undergoing PD have reportedly averaged six episodes of peritonitis per year.[2] However, the rate of peritonitis in patients receiving PD is on a downward trend. Over the years, the rate declined to 4.4 episodes per patient-year in 1979 and to 1.4 episodes per patient-year in 1989 (1 year after the introduction of the twin-bag system). In 2010, the rate of peritonitis was reported to be 0.95 episode per patient-year.[3] Despite this marked reduction over time, peritonitis continues to be problematic because of its association with significant morbidity (16%) and mortality (5%).[2]",
"The most common presenting symptoms in patients with peritonitis who are undergoing PD include the following[4,5]:",
"Abdominal pain (79%-88%)",
"Cloudy effluent (84%)",
"Fever (29%-53%)",
"Nausea or vomiting (31%-51%)",
"Less frequently, peritonitis may also present with signs of systemic infection, such as hypotension, which is seen in about 18% of patients.[4,5] Streptococcal and fungal peritonitis have been associated with severe abdominal pain.[6,7]",
"A definitive diagnosis of peritonitis requires cultures of the dialysate fluid; however, patients receiving PD should have a presumptive diagnosis of peritonitis if they present with abdominal pain or cloudy effluent during dialysis.[8] In addition, sudden difficulty in performing regular peritoneal exchanges should always prompt peritonitis as a differential diagnosis in this patient population. Furthermore, these patients should receive immediate empirical antibiotic treatment until a diagnosis is confirmed or excluded.[8] Overall, coagulase-negative staphylococci (S epidermidis) are the most common organism implicated in the development of acute peritonitis in patients undergoing PD."
],
"date": "August 16, 2021",
"figures": [],
"markdown": "# After Travel, a 50-Year-Old Grandfather Has Dyspnea, Fever\n\n **Authors:** Dushyant Singh Dahiya, MD; Farah Wani, MD; Tin Wong; Asim Kichloo, MD \n **Date:** August 16, 2021\n\n ## Content\n\n This patient's acute-onset, diffuse abdominal pain; abdominal tenderness on palpation; and history of PD all pointed to a diagnosis of acute peritonitis. Initially, broad-spectrum antibiotic coverage was provided with vancomycin and cefotaxime. The peritoneal fluid analysis was positive for Staphylococcus epidermidis, which was sensitive to cefotaxime. Hence, vancomycin was discontinued and cefotaxime was continued for a total of 5 days. The patient's symptoms resolved completely, and he was eventually discharged home.\nPeritonitis is a common complication of PD[1]; the PD catheter serves as a highly effective portal of entry for bacteria into the abdomen. Ever since Dr Henry Tenckhoff invented the first indwelling catheter in 1968, patients undergoing PD have reportedly averaged six episodes of peritonitis per year.[2] However, the rate of peritonitis in patients receiving PD is on a downward trend. Over the years, the rate declined to 4.4 episodes per patient-year in 1979 and to 1.4 episodes per patient-year in 1989 (1 year after the introduction of the twin-bag system). In 2010, the rate of peritonitis was reported to be 0.95 episode per patient-year.[3] Despite this marked reduction over time, peritonitis continues to be problematic because of its association with significant morbidity (16%) and mortality (5%).[2]\nThe most common presenting symptoms in patients with peritonitis who are undergoing PD include the following[4,5]:\nAbdominal pain (79%-88%)\nCloudy effluent (84%)\nFever (29%-53%)\nNausea or vomiting (31%-51%)\nLess frequently, peritonitis may also present with signs of systemic infection, such as hypotension, which is seen in about 18% of patients.[4,5] Streptococcal and fungal peritonitis have been associated with severe abdominal pain.[6,7]\nA definitive diagnosis of peritonitis requires cultures of the dialysate fluid; however, patients receiving PD should have a presumptive diagnosis of peritonitis if they present with abdominal pain or cloudy effluent during dialysis.[8] In addition, sudden difficulty in performing regular peritoneal exchanges should always prompt peritonitis as a differential diagnosis in this patient population. Furthermore, these patients should receive immediate empirical antibiotic treatment until a diagnosis is confirmed or excluded.[8] Overall, coagulase-negative staphylococci (S epidermidis) are the most common organism implicated in the development of acute peritonitis in patients undergoing PD.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1612086,
"choiceText": "Acute myocardial infarction",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612087,
"choiceText": "Perforation of peptic ulcer",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612088,
"choiceText": "Hypertensive urgency",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612089,
"choiceText": "Acute peritonitis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612090,
"choiceText": "Acute pericarditis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 517840,
"questionText": "On the basis of these findings only, what is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "After Travel, a 50-Year-Old Grandfather Has Dyspnea, Fever"
},
{
"authors": "Dushyant Singh Dahiya, MD; Farah Wani, MD; Tin Wong; Asim Kichloo, MD",
"content": [
"In cases of a negative effluent culture, peritonitis in patients receiving PD can be diagnosed if the patient presents with a clinical picture of peritonitis and the peritoneal fluid analysis demonstrates a WBC count > 100 cells/µL with > 50% neutrophils.[8] The corrected Light criteria are also an important diagnostic tool in peritonitis and can be used to determine whether the peritoneal fluid is transudative or exudative; this finding may help to rule out other possible etiologies.[9]",
"In this case, the patient's positive rebound tenderness on physical examination favored a diagnosis of peritonitis. In patients who are receiving PD, it is vital to inspect the catheter site to rule out an obvious infection of the exit site.",
"It is well established that dialysis-related peritonitis can occur in patients receiving PD. However, some of these patients can develop non–dialysis-related peritonitis, often referred to as \"secondary peritonitis.\" Common causes of secondary peritonitis include cholecystitis, appendicitis, ruptured diverticulum, bowel disimpaction procedure, bowel perforation, bowel ischemia, and incarcerated hernias. In addition, bacterial seeding of the peritoneum from the blood and vagina can lead to secondary peritonitis. The most common presenting features that may aid in the diagnosis of secondary peritonitis include feculent material in the dialysate and additional localized pain.[8,10,11,12]",
"In this case, although the patient has elevated serum markers for myocardial infarction (troponin), congestive heart failure (brain-type natriuretic peptide), and pulmonary embolism (D-dimer), it is important to note his ESRD. Patients with renal failure have significantly decreased clearance of metabolic waste products and biomarkers from the blood compared with healthy persons. On repeated laboratory investigations, these serum markers are consistently elevated. Therefore, acute processes such as myocardial infarction and pulmonary embolism are far less likely. Nonetheless, it is important to perform further diagnostic workup in cases with high clinical suspicion. In this patient, the results of additional investigations, such as ECG, echocardiography, and chest CT angiography, were unremarkable.",
"Patients with perforated peptic ulcers may initially present with sudden-onset, severe epigastric pain; vomiting; tachycardia; abdominal rigidity; and right lower-quadrant tenderness (fluid tracking along the right paracolic gutter), which may rapidly evolve (over > 12 h) to abdominal distention, fever, and circulatory collapse. This presentation was not observed in the patient in this case. In addition, perforated peptic ulcers tend to occur in elderly patients with multiple comorbidities and are associated with the use of corticosteroids or nonsteroidal anti-inflammatory drugs.",
"A hypertensive urgency is defined as a blood pressure ≥ 180/120 mm Hg without end-organ damage; this patient does not meet these criteria. His elevated blood pressure may be secondary to abdominal pain and in part due to his ESRD.",
"This patient was exposed to viral infections during his recent trip. Although viral infections are commonly associated with acute pericarditis, this diagnosis can be ruled out because the patient does not describe acute retrosternal, sharp, pleuritic chest pain that improves on leaning forward. In addition, a pericardial friction rub (highly specific and pathognomonic for acute pericarditis) and classic changes, which include widespread concave upward ST-segment elevation and PR-segment depression without T-wave inversions, were absent on his ECG."
],
"date": "August 16, 2021",
"figures": [],
"markdown": "# After Travel, a 50-Year-Old Grandfather Has Dyspnea, Fever\n\n **Authors:** Dushyant Singh Dahiya, MD; Farah Wani, MD; Tin Wong; Asim Kichloo, MD \n **Date:** August 16, 2021\n\n ## Content\n\n In cases of a negative effluent culture, peritonitis in patients receiving PD can be diagnosed if the patient presents with a clinical picture of peritonitis and the peritoneal fluid analysis demonstrates a WBC count > 100 cells/µL with > 50% neutrophils.[8] The corrected Light criteria are also an important diagnostic tool in peritonitis and can be used to determine whether the peritoneal fluid is transudative or exudative; this finding may help to rule out other possible etiologies.[9]\nIn this case, the patient's positive rebound tenderness on physical examination favored a diagnosis of peritonitis. In patients who are receiving PD, it is vital to inspect the catheter site to rule out an obvious infection of the exit site.\nIt is well established that dialysis-related peritonitis can occur in patients receiving PD. However, some of these patients can develop non–dialysis-related peritonitis, often referred to as \"secondary peritonitis.\" Common causes of secondary peritonitis include cholecystitis, appendicitis, ruptured diverticulum, bowel disimpaction procedure, bowel perforation, bowel ischemia, and incarcerated hernias. In addition, bacterial seeding of the peritoneum from the blood and vagina can lead to secondary peritonitis. The most common presenting features that may aid in the diagnosis of secondary peritonitis include feculent material in the dialysate and additional localized pain.[8,10,11,12]\nIn this case, although the patient has elevated serum markers for myocardial infarction (troponin), congestive heart failure (brain-type natriuretic peptide), and pulmonary embolism (D-dimer), it is important to note his ESRD. Patients with renal failure have significantly decreased clearance of metabolic waste products and biomarkers from the blood compared with healthy persons. On repeated laboratory investigations, these serum markers are consistently elevated. Therefore, acute processes such as myocardial infarction and pulmonary embolism are far less likely. Nonetheless, it is important to perform further diagnostic workup in cases with high clinical suspicion. In this patient, the results of additional investigations, such as ECG, echocardiography, and chest CT angiography, were unremarkable.\nPatients with perforated peptic ulcers may initially present with sudden-onset, severe epigastric pain; vomiting; tachycardia; abdominal rigidity; and right lower-quadrant tenderness (fluid tracking along the right paracolic gutter), which may rapidly evolve (over > 12 h) to abdominal distention, fever, and circulatory collapse. This presentation was not observed in the patient in this case. In addition, perforated peptic ulcers tend to occur in elderly patients with multiple comorbidities and are associated with the use of corticosteroids or nonsteroidal anti-inflammatory drugs.\nA hypertensive urgency is defined as a blood pressure ≥ 180/120 mm Hg without end-organ damage; this patient does not meet these criteria. His elevated blood pressure may be secondary to abdominal pain and in part due to his ESRD.\nThis patient was exposed to viral infections during his recent trip. Although viral infections are commonly associated with acute pericarditis, this diagnosis can be ruled out because the patient does not describe acute retrosternal, sharp, pleuritic chest pain that improves on leaning forward. In addition, a pericardial friction rub (highly specific and pathognomonic for acute pericarditis) and classic changes, which include widespread concave upward ST-segment elevation and PR-segment depression without T-wave inversions, were absent on his ECG.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "After Travel, a 50-Year-Old Grandfather Has Dyspnea, Fever"
},
{
"authors": "Dushyant Singh Dahiya, MD; Farah Wani, MD; Tin Wong; Asim Kichloo, MD",
"content": [
"It is essential to initiate empirical antibiotic therapy after peritoneal fluid is collected for analysis, Gram staining, and culture. Intraperitoneal administration is preferred over the intravenous route for optimal local antibiotic concentration, unless a systemic infection is also suspected.[8] The antibiotic of choice should cover both gram-positive and gram-negative organisms and should be selected on the basis of the local antibiogram.",
"According to current recommendations, vancomycin or first-generation cephalosporins are used to cover for gram-positive organisms, whereas third- or fourth-generation cephalosporins, aminoglycosides, or aztreonam can be used for gram-negative organisms.[8] Further adjustments in the antibiotic regimen may be required upon Gram staining, fluid culture, and sensitivity results. If Gram staining reveals yeast or other fungi, antifungal therapy should be started immediately and the patient should be prepared for possible transition to hemodialysis.[8] It is recommended that patients be admitted to the hospital and monitored for clinical improvement within 48 hours of initiation of the antibiotic regimen.[13]",
"In special circumstances, PD catheter removal may be required. Indications for PD catheter removal include the following[7,13]:",
"Refractory peritonitis that fails to respond to antibiotics within 5 days of initiation",
"Relapsing peritonitis within 4 weeks of completion of the antibiotic regimen",
"Fungal or mycobacterial peritonitis",
"Peritonitis associated with intra-abdominal pathology, such as abscess, perforation, or infarcted bowel",
"Culture-negative peritonitis with persistent symptoms and a high peritoneal WBC count",
"Catheter removal with simultaneous replacement, upon clearing of the dialysate, is acceptable only for relapsing peritonitis.[7]"
],
"date": "August 16, 2021",
"figures": [],
"markdown": "# After Travel, a 50-Year-Old Grandfather Has Dyspnea, Fever\n\n **Authors:** Dushyant Singh Dahiya, MD; Farah Wani, MD; Tin Wong; Asim Kichloo, MD \n **Date:** August 16, 2021\n\n ## Content\n\n It is essential to initiate empirical antibiotic therapy after peritoneal fluid is collected for analysis, Gram staining, and culture. Intraperitoneal administration is preferred over the intravenous route for optimal local antibiotic concentration, unless a systemic infection is also suspected.[8] The antibiotic of choice should cover both gram-positive and gram-negative organisms and should be selected on the basis of the local antibiogram.\nAccording to current recommendations, vancomycin or first-generation cephalosporins are used to cover for gram-positive organisms, whereas third- or fourth-generation cephalosporins, aminoglycosides, or aztreonam can be used for gram-negative organisms.[8] Further adjustments in the antibiotic regimen may be required upon Gram staining, fluid culture, and sensitivity results. If Gram staining reveals yeast or other fungi, antifungal therapy should be started immediately and the patient should be prepared for possible transition to hemodialysis.[8] It is recommended that patients be admitted to the hospital and monitored for clinical improvement within 48 hours of initiation of the antibiotic regimen.[13]\nIn special circumstances, PD catheter removal may be required. Indications for PD catheter removal include the following[7,13]:\nRefractory peritonitis that fails to respond to antibiotics within 5 days of initiation\nRelapsing peritonitis within 4 weeks of completion of the antibiotic regimen\nFungal or mycobacterial peritonitis\nPeritonitis associated with intra-abdominal pathology, such as abscess, perforation, or infarcted bowel\nCulture-negative peritonitis with persistent symptoms and a high peritoneal WBC count\nCatheter removal with simultaneous replacement, upon clearing of the dialysate, is acceptable only for relapsing peritonitis.[7]\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1612097,
"choiceText": "<i>Escherichia coli</i>",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612098,
"choiceText": "<i>Candida albicans</i>",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612099,
"choiceText": "<i>Staphylococcus aureus</i>",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612100,
"choiceText": "<i>Staphylococcus epidermidis</i>",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "About 45%-65% of cases of acute peritonitis are secondary to gram-positive bacteria, followed by gram-negative bacteria (15%-35%) and fungi (3%-5%); <i>Candida</i> species are the most common fungal pathogens.<sup>[14-17]</sup> Of the gram-positive bacteria, coagulase-negative staphylococci <i>(S epidermidis)</i> are most frequently implicated.<sup>[16]</sup> Contamination of the peritoneal fluid may occur when performing exchanges or connecting and disconnecting from the transfer set. The most common gram-negative organism leading to acute peritonitis is <i>E coli</i>, followed by <i>Klebsiella</i> species.<sup>[16]</sup> Contamination with gram-negative bacteria may come from the bowel, urinary tract, skin, contaminated water, or animal contact.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 517842,
"questionText": "Which is the most common organism implicated in acute peritonitis in patients undergoing PD?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1612103,
"choiceText": "Dialysate culture positive for methicillin-resistant <i>Staphylococcus aureus</i> (MRSA)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612104,
"choiceText": "Dialysate culture positive for fungal infection",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612105,
"choiceText": "Fever (temperature > 102 °F [38.9 °C])",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612106,
"choiceText": "Dialysate fluid with a WBC count > 500 cells/µL with > 50% neutrophils",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Although peritonitis in patients receiving PD is more commonly caused by bacteria than by fungi, fungal peritonitis carries higher morbidity and mortality (15%-45%) than bacterial infections.<sup>[18-20]</sup> Complications include sclerosing peritonitis, adhesions with resulting bowel obstructions or strictures, bowel wall invasion, and abscess formation.<sup>[21]</sup> \r\n<br><br>\r\nAccording to the 2010 guidelines of the International Society for Peritoneal Dialysis, removal of the peritoneal catheter is indicated in the following circumstances: refractory peritonitis that does not respond to antibiotics within 5 days of initiation; relapsing peritonitis within 4 weeks of completion of an antibiotic regimen; fungal or mycobacterial peritonitis; peritonitis associated with intra-abdominal pathology, such as abscess, perforation, or infarcted bowel; and culture-negative peritonitis with persistent symptoms and a high peritoneal WBC count.<sup>[7,13]</sup>\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 517845,
"questionText": "Which is an indication for peritoneal catheter removal in the setting of peritonitis in patients receiving PD?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "After Travel, a 50-Year-Old Grandfather Has Dyspnea, Fever"
},
{
"authors": "Dushyant Singh Dahiya, MD; Farah Wani, MD; Tin Wong; Asim Kichloo, MD",
"content": [],
"date": "August 16, 2021",
"figures": [],
"markdown": "# After Travel, a 50-Year-Old Grandfather Has Dyspnea, Fever\n\n **Authors:** Dushyant Singh Dahiya, MD; Farah Wani, MD; Tin Wong; Asim Kichloo, MD \n **Date:** August 16, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1612097,
"choiceText": "<i>Escherichia coli</i>",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612098,
"choiceText": "<i>Candida albicans</i>",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612099,
"choiceText": "<i>Staphylococcus aureus</i>",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612100,
"choiceText": "<i>Staphylococcus epidermidis</i>",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "About 45%-65% of cases of acute peritonitis are secondary to gram-positive bacteria, followed by gram-negative bacteria (15%-35%) and fungi (3%-5%); <i>Candida</i> species are the most common fungal pathogens.<sup>[14-17]</sup> Of the gram-positive bacteria, coagulase-negative staphylococci <i>(S epidermidis)</i> are most frequently implicated.<sup>[16]</sup> Contamination of the peritoneal fluid may occur when performing exchanges or connecting and disconnecting from the transfer set. The most common gram-negative organism leading to acute peritonitis is <i>E coli</i>, followed by <i>Klebsiella</i> species.<sup>[16]</sup> Contamination with gram-negative bacteria may come from the bowel, urinary tract, skin, contaminated water, or animal contact.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 517842,
"questionText": "Which is the most common organism implicated in acute peritonitis in patients undergoing PD?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1612103,
"choiceText": "Dialysate culture positive for methicillin-resistant <i>Staphylococcus aureus</i> (MRSA)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612104,
"choiceText": "Dialysate culture positive for fungal infection",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612105,
"choiceText": "Fever (temperature > 102 °F [38.9 °C])",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612106,
"choiceText": "Dialysate fluid with a WBC count > 500 cells/µL with > 50% neutrophils",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Although peritonitis in patients receiving PD is more commonly caused by bacteria than by fungi, fungal peritonitis carries higher morbidity and mortality (15%-45%) than bacterial infections.<sup>[18-20]</sup> Complications include sclerosing peritonitis, adhesions with resulting bowel obstructions or strictures, bowel wall invasion, and abscess formation.<sup>[21]</sup> \r\n<br><br>\r\nAccording to the 2010 guidelines of the International Society for Peritoneal Dialysis, removal of the peritoneal catheter is indicated in the following circumstances: refractory peritonitis that does not respond to antibiotics within 5 days of initiation; relapsing peritonitis within 4 weeks of completion of an antibiotic regimen; fungal or mycobacterial peritonitis; peritonitis associated with intra-abdominal pathology, such as abscess, perforation, or infarcted bowel; and culture-negative peritonitis with persistent symptoms and a high peritoneal WBC count.<sup>[7,13]</sup>\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 517845,
"questionText": "Which is an indication for peritoneal catheter removal in the setting of peritonitis in patients receiving PD?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "After Travel, a 50-Year-Old Grandfather Has Dyspnea, Fever"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1612086,
"choiceText": "Acute myocardial infarction",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612087,
"choiceText": "Perforation of peptic ulcer",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612088,
"choiceText": "Hypertensive urgency",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612089,
"choiceText": "Acute peritonitis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612090,
"choiceText": "Acute pericarditis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 517840,
"questionText": "On the basis of these findings only, what is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1612097,
"choiceText": "<i>Escherichia coli</i>",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612098,
"choiceText": "<i>Candida albicans</i>",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612099,
"choiceText": "<i>Staphylococcus aureus</i>",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612100,
"choiceText": "<i>Staphylococcus epidermidis</i>",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "About 45%-65% of cases of acute peritonitis are secondary to gram-positive bacteria, followed by gram-negative bacteria (15%-35%) and fungi (3%-5%); <i>Candida</i> species are the most common fungal pathogens.<sup>[14-17]</sup> Of the gram-positive bacteria, coagulase-negative staphylococci <i>(S epidermidis)</i> are most frequently implicated.<sup>[16]</sup> Contamination of the peritoneal fluid may occur when performing exchanges or connecting and disconnecting from the transfer set. The most common gram-negative organism leading to acute peritonitis is <i>E coli</i>, followed by <i>Klebsiella</i> species.<sup>[16]</sup> Contamination with gram-negative bacteria may come from the bowel, urinary tract, skin, contaminated water, or animal contact.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 517842,
"questionText": "Which is the most common organism implicated in acute peritonitis in patients undergoing PD?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1612103,
"choiceText": "Dialysate culture positive for methicillin-resistant <i>Staphylococcus aureus</i> (MRSA)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612104,
"choiceText": "Dialysate culture positive for fungal infection",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612105,
"choiceText": "Fever (temperature > 102 °F [38.9 °C])",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1612106,
"choiceText": "Dialysate fluid with a WBC count > 500 cells/µL with > 50% neutrophils",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Although peritonitis in patients receiving PD is more commonly caused by bacteria than by fungi, fungal peritonitis carries higher morbidity and mortality (15%-45%) than bacterial infections.<sup>[18-20]</sup> Complications include sclerosing peritonitis, adhesions with resulting bowel obstructions or strictures, bowel wall invasion, and abscess formation.<sup>[21]</sup> \r\n<br><br>\r\nAccording to the 2010 guidelines of the International Society for Peritoneal Dialysis, removal of the peritoneal catheter is indicated in the following circumstances: refractory peritonitis that does not respond to antibiotics within 5 days of initiation; relapsing peritonitis within 4 weeks of completion of an antibiotic regimen; fungal or mycobacterial peritonitis; peritonitis associated with intra-abdominal pathology, such as abscess, perforation, or infarcted bowel; and culture-negative peritonitis with persistent symptoms and a high peritoneal WBC count.<sup>[7,13]</sup>\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 517845,
"questionText": "Which is an indication for peritoneal catheter removal in the setting of peritonitis in patients receiving PD?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
860310 | /viewarticle/860310 | [
{
"authors": "Elizabeth K. Satter, MD, MPH",
"content": [
"Editor's Note:\n\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.",
"A 40-year-old man presents with a 20-year history of recurrent painful nodules on his bilateral buttocks, gluteal cleft, and medial aspect of his upper thighs. The lesions often spontaneously rupture and result in sinus tracts or scarring. The patient previously had an excision of a diffusely involved area on his left buttock followed by a split-thickness skin graft; however, within 6-8 months, new lesions developed at the site of prior treatment.",
"The patient is otherwise healthy, with no history of facial or back acne, pseudofolliculitis barbae, or dissecting scalp folliculitis. The patient does not have arthralgia, gastrointestinal or genitourinary symptoms, and fever or chills. He does not smoke, and his total body mass index is within normal limit. No family history of similar lesions is reported."
],
"date": "July 27, 2021",
"figures": [],
"markdown": "# A 40-Year-Old Man With Painful, Rupturing Lesions\n\n **Authors:** Elizabeth K. Satter, MD, MPH \n **Date:** July 27, 2021\n\n ## Content\n\n Editor's Note:\n\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.\nA 40-year-old man presents with a 20-year history of recurrent painful nodules on his bilateral buttocks, gluteal cleft, and medial aspect of his upper thighs. The lesions often spontaneously rupture and result in sinus tracts or scarring. The patient previously had an excision of a diffusely involved area on his left buttock followed by a split-thickness skin graft; however, within 6-8 months, new lesions developed at the site of prior treatment.\nThe patient is otherwise healthy, with no history of facial or back acne, pseudofolliculitis barbae, or dissecting scalp folliculitis. The patient does not have arthralgia, gastrointestinal or genitourinary symptoms, and fever or chills. He does not smoke, and his total body mass index is within normal limit. No family history of similar lesions is reported.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A 40-Year-Old Man With Painful, Rupturing Lesions"
},
{
"authors": "Elizabeth K. Satter, MD, MPH",
"content": [
"Upon examination, the patient is afebrile. He appears to be in a fair amount of discomfort while seated. On his left buttock is a large, indurated, hyperpigmented plaque with multiple coalescent erythematous and often fluctuant nodules. Scattered sinus tracts containing purulent material are observed, admixed with hyperpigmented hypertrophic and depressed scars (Figure). Similar lesions are noted on the right buttock and medial thighs, but the degree of involvement is significantly less. No lesions are seen in the axilla, and the rest of the physical examination is unremarkable.",
"Figure.",
"Figure.",
"Because the patient's presentation is unusual, a punch biopsy is performed and reveals an epithelial-lined sinus tract filled with keratin debris and neutrophils. The adjacent dermis is fibrotic and contains a mixed inflammatory infiltrate composed of lymphocytes, histiocytes, and plasma cells, as well as focal collections of neutrophils. Tissue cultures are negative."
],
"date": "July 27, 2021",
"figures": [
{
"caption": "Figure.",
"image_url": "https://img.medscapestatic.com/article/860/310/860310-Thumb1.png"
}
],
"markdown": "# A 40-Year-Old Man With Painful, Rupturing Lesions\n\n **Authors:** Elizabeth K. Satter, MD, MPH \n **Date:** July 27, 2021\n\n ## Content\n\n Upon examination, the patient is afebrile. He appears to be in a fair amount of discomfort while seated. On his left buttock is a large, indurated, hyperpigmented plaque with multiple coalescent erythematous and often fluctuant nodules. Scattered sinus tracts containing purulent material are observed, admixed with hyperpigmented hypertrophic and depressed scars (Figure). Similar lesions are noted on the right buttock and medial thighs, but the degree of involvement is significantly less. No lesions are seen in the axilla, and the rest of the physical examination is unremarkable.\nFigure.\nFigure.\nBecause the patient's presentation is unusual, a punch biopsy is performed and reveals an epithelial-lined sinus tract filled with keratin debris and neutrophils. The adjacent dermis is fibrotic and contains a mixed inflammatory infiltrate composed of lymphocytes, histiocytes, and plasma cells, as well as focal collections of neutrophils. Tissue cultures are negative.\n\n ## Figures\n\n **Figure.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 950249,
"choiceText": "Granuloma inguinale",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950251,
"choiceText": "Lymphogranuloma venereum",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950253,
"choiceText": "Cutaneous Crohn disease",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950255,
"choiceText": "Hidradenitis suppurativa",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950257,
"choiceText": "Recurrent furunculosis\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 300635,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 40-Year-Old Man With Painful, Rupturing Lesions"
},
{
"authors": "Elizabeth K. Satter, MD, MPH",
"content": [
"Hidradenitis suppurativa is a chronic and relapsing inflammatory disorder of the pilosebaceous glands that tends to occur in apocrine-rich anatomical regions. The inciting event is hypothesized to be occlusion of the follicular infundibulum, followed by follicular rupture associated with a vigorous inflammatory response. The pathologic role of microorganisms is debatable; however, bacteria may play a role in eliciting an autoinflammatory response via the innate immune system.[1,2,3,4,5,6,7]",
"Hidradenitis suppurativa is part of the follicular occlusion tetrad, which includes dissecting cellulitis of the scalp, acne conglobata, and pilonidal cysts. Owing to the similarities of these conditions, \"acne inversa\" has been used as an all-inclusive term.[6]",
"Initially, hidradenitis suppurativa presents as open comedones, often with two or more openings, admixed with tender erythematous papules to nodules. Subsequently, lesions become fluctuant and spontaneously drain, then sinus tracts develop. As the condition progresses, the lesions become more numerous, associated with interconnection of the sinus tracts and significant scarring.",
"The estimated prevalence of hidradenitis suppurativa in the United States is 1%-2%; however, not all patients seek medical help, often owing to embarrassment.[1,2] The typical age of onset is in the second and third decades.[1] Women are three times more likely than men to have hidradenitis suppurativa; however, men have a greater tendency for atypical locations, have more severe disease, and often have associated acne.[1,2,3,4,5]",
"Most cases are sporadic, but a familial form with autosomal dominant inheritance has been reported.[1] Less commonly, hidradenitis suppurativa can be seen in patients with rare systemic autoinflammatory syndromes, such as the synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome and the pyogenic arthritis, pyoderma gangrenosum, and acne (PAPA) syndrome.",
"Because lesions often develop postpubertally, androgens have been postulated to play a role. Most patients have a normal androgen profile[1,2,4]; thus, the defect is hypothesized to lie at the androgen receptor level.[4] Although obesity and smoking are often cited as contributory factors, their role in the pathogenesis has not been established; lifestyle modifications may, but do not necessarily, improve the condition.[1,2,3]",
"A diagnosis of hidradenitis suppurativa is typically based on characteristic history and clinical morphology. In patients who have an atypical presentation, a biopsy can be performed. Histologically, early lesions show follicular hyperkeratosis and plugging of the infundibulum, followed by follicular dilation and epithelial hyperplasia. Ruptured hair follicles elicit a brisk mixed inflammatory infiltrate, and abscesses often develop. Late lesions show epithelial-lined sinus tracts and scarring.",
"Cultures do not need to be performed from ruptured lesions because they are often colonized by various bacterial species. Tissue cultures of early intact lesions may provide more information; however, they are frequently sterile.[3]"
],
"date": "July 27, 2021",
"figures": [],
"markdown": "# A 40-Year-Old Man With Painful, Rupturing Lesions\n\n **Authors:** Elizabeth K. Satter, MD, MPH \n **Date:** July 27, 2021\n\n ## Content\n\n Hidradenitis suppurativa is a chronic and relapsing inflammatory disorder of the pilosebaceous glands that tends to occur in apocrine-rich anatomical regions. The inciting event is hypothesized to be occlusion of the follicular infundibulum, followed by follicular rupture associated with a vigorous inflammatory response. The pathologic role of microorganisms is debatable; however, bacteria may play a role in eliciting an autoinflammatory response via the innate immune system.[1,2,3,4,5,6,7]\nHidradenitis suppurativa is part of the follicular occlusion tetrad, which includes dissecting cellulitis of the scalp, acne conglobata, and pilonidal cysts. Owing to the similarities of these conditions, \"acne inversa\" has been used as an all-inclusive term.[6]\nInitially, hidradenitis suppurativa presents as open comedones, often with two or more openings, admixed with tender erythematous papules to nodules. Subsequently, lesions become fluctuant and spontaneously drain, then sinus tracts develop. As the condition progresses, the lesions become more numerous, associated with interconnection of the sinus tracts and significant scarring.\nThe estimated prevalence of hidradenitis suppurativa in the United States is 1%-2%; however, not all patients seek medical help, often owing to embarrassment.[1,2] The typical age of onset is in the second and third decades.[1] Women are three times more likely than men to have hidradenitis suppurativa; however, men have a greater tendency for atypical locations, have more severe disease, and often have associated acne.[1,2,3,4,5]\nMost cases are sporadic, but a familial form with autosomal dominant inheritance has been reported.[1] Less commonly, hidradenitis suppurativa can be seen in patients with rare systemic autoinflammatory syndromes, such as the synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome and the pyogenic arthritis, pyoderma gangrenosum, and acne (PAPA) syndrome.\nBecause lesions often develop postpubertally, androgens have been postulated to play a role. Most patients have a normal androgen profile[1,2,4]; thus, the defect is hypothesized to lie at the androgen receptor level.[4] Although obesity and smoking are often cited as contributory factors, their role in the pathogenesis has not been established; lifestyle modifications may, but do not necessarily, improve the condition.[1,2,3]\nA diagnosis of hidradenitis suppurativa is typically based on characteristic history and clinical morphology. In patients who have an atypical presentation, a biopsy can be performed. Histologically, early lesions show follicular hyperkeratosis and plugging of the infundibulum, followed by follicular dilation and epithelial hyperplasia. Ruptured hair follicles elicit a brisk mixed inflammatory infiltrate, and abscesses often develop. Late lesions show epithelial-lined sinus tracts and scarring.\nCultures do not need to be performed from ruptured lesions because they are often colonized by various bacterial species. Tissue cultures of early intact lesions may provide more information; however, they are frequently sterile.[3]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 950249,
"choiceText": "Granuloma inguinale",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950251,
"choiceText": "Lymphogranuloma venereum",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950253,
"choiceText": "Cutaneous Crohn disease",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950255,
"choiceText": "Hidradenitis suppurativa",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950257,
"choiceText": "Recurrent furunculosis\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 300635,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 40-Year-Old Man With Painful, Rupturing Lesions"
},
{
"authors": "Elizabeth K. Satter, MD, MPH",
"content": [
"The differential diagnosis of indurated suppurative genital lesions include Bartholin gland abscess, cutaneous Crohn disease, and pilonidal cysts. The differential also includes lymphogranuloma venereum, granuloma inguinale, and scrofuloderma, as well as other infectious or neoplastic processes of the lymph nodes; however, these latter conditions are uncommon, especially in the United States.[2,3] After performing a comprehensive review, Alikhan and colleagues[7] concluded that a diagnosis of hidradenitis suppurativa is most likely if a patient has multiple recurrent lesions, particularly if bilateral, and located along the milk line.",
"The severity of hidradenitis suppurativa can be classified using various scoring systems. The most established and simplest system was initially described by Hurley[8] in 1989. Most patients have disease that is classified as Hurley stage I, which is characterized by single or multiple isolated abscesses without sinus tracts or scarring. Stage II disease manifests as recurrent abscesses, with single or multiple widely separated lesions that have limited sinus tract formation. Hurley stage III is the most severe, yet least common, presentation. Patients present with multiple abscesses and interconnected sinus tracts that are located across a broad area associated with extensive scarring.",
"Although the Hurley staging system is easy to use, it does not address response to treatment or disease progression; therefore, the Sartorius system was designed to provide a numerical score based on physical findings.[9] The score is based on the number of anatomical regions involved (3 points per region); number of lesions (2 points for each nodule, 4 points for each fistula, and 1 point for each scar); and longest distance between 2 lesions (2-4 points), with 6 additional points given if the lesions are not clearly separated by normal skin.[9]",
"Some evaluators suggest using a modified Sartorius system, which additionally includes the presence of pain, discharge, or odor. However, given the complexities of the Sartorius system, it may better suited to quantify disease in a research setting.",
"Chiricozzi and colleagues[10] proposed the Acne Inversa Severity Index (AISI), which was designed to combine the physician's clinical evaluation (type of lesions and the affected body sites) with the patient's quality-of-life ratings (pain, discomfort, and disability due to hidradenitis suppurativa). The authors claim that AISI is a simple, rapid, yet accurate method that better quantitates the severity of the disease in both clinical and research settings.[10]"
],
"date": "July 27, 2021",
"figures": [],
"markdown": "# A 40-Year-Old Man With Painful, Rupturing Lesions\n\n **Authors:** Elizabeth K. Satter, MD, MPH \n **Date:** July 27, 2021\n\n ## Content\n\n The differential diagnosis of indurated suppurative genital lesions include Bartholin gland abscess, cutaneous Crohn disease, and pilonidal cysts. The differential also includes lymphogranuloma venereum, granuloma inguinale, and scrofuloderma, as well as other infectious or neoplastic processes of the lymph nodes; however, these latter conditions are uncommon, especially in the United States.[2,3] After performing a comprehensive review, Alikhan and colleagues[7] concluded that a diagnosis of hidradenitis suppurativa is most likely if a patient has multiple recurrent lesions, particularly if bilateral, and located along the milk line.\nThe severity of hidradenitis suppurativa can be classified using various scoring systems. The most established and simplest system was initially described by Hurley[8] in 1989. Most patients have disease that is classified as Hurley stage I, which is characterized by single or multiple isolated abscesses without sinus tracts or scarring. Stage II disease manifests as recurrent abscesses, with single or multiple widely separated lesions that have limited sinus tract formation. Hurley stage III is the most severe, yet least common, presentation. Patients present with multiple abscesses and interconnected sinus tracts that are located across a broad area associated with extensive scarring.\nAlthough the Hurley staging system is easy to use, it does not address response to treatment or disease progression; therefore, the Sartorius system was designed to provide a numerical score based on physical findings.[9] The score is based on the number of anatomical regions involved (3 points per region); number of lesions (2 points for each nodule, 4 points for each fistula, and 1 point for each scar); and longest distance between 2 lesions (2-4 points), with 6 additional points given if the lesions are not clearly separated by normal skin.[9]\nSome evaluators suggest using a modified Sartorius system, which additionally includes the presence of pain, discharge, or odor. However, given the complexities of the Sartorius system, it may better suited to quantify disease in a research setting.\nChiricozzi and colleagues[10] proposed the Acne Inversa Severity Index (AISI), which was designed to combine the physician's clinical evaluation (type of lesions and the affected body sites) with the patient's quality-of-life ratings (pain, discomfort, and disability due to hidradenitis suppurativa). The authors claim that AISI is a simple, rapid, yet accurate method that better quantitates the severity of the disease in both clinical and research settings.[10]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A 40-Year-Old Man With Painful, Rupturing Lesions"
},
{
"authors": "Elizabeth K. Satter, MD, MPH",
"content": [
"Treatment of hidradenitis suppurativa is often challenging. Despite the introduction of new therapeutic options, large clinical trials are few. Early diagnosis and treatment is essential because more effective control can be achieved in early disease, with the goal of treatment being to reduce disease burden; prevent development of new lesions; and avoid, or at least limit, scarring. Unfortunately, patients typically do not seek medical attention when they have early limited disease or are misdiagnosed with suppurative folliculitis, carbuncles, or inflamed epidermal or pilonidal cysts and treated with incision and drainage.",
"Several comprehensive reviews have evaluated different treatment options based on clinical stage; however, no treatment gained US Food and Drug Administration (FDA) approval for hidradenitis suppurativa until May 2015, when the FDA granted adalimumab orphan status for treatment of patients with Hurley stage II or III disease.[11,12] First-line medical therapy for patients with Hurley stage I or II disease should include topical antimicrobials (eg, benzoyl peroxide washes, bleach baths, bleach soaks) and clindamycin lotion, along with short courses of oral doxycycline, minocycline, or the combination of clindamycin and rifampin for acute flares. Dapsone has also been used; however, studies are limited and have shown variable results.[11,12] Antibiotics are believed to be beneficial, not just for their bactericidal properties but also their anti-inflammatory and immunomodulatory effects. However, similar to acne treatment, long-term antibiotic therapy is not recommended owing to development of bacterial resistance.",
"Although hidradenitis suppurativa resembles nodular acne, oral retinoids have had limited success. Antiandrogen therapy may be beneficial for females with hidradenitis suppurativa, especially those who experience flares of their symptoms with menstruation.[11,12] Methotrexate, metformin, and various biologic agents (adalimumab, anakinra, etanercept, infliximab, and ustekinumab) are typically reserved for patients in whom other approaches have been tried and failed.[11,12,13]",
"Surgical options depend on the stage of disease. Incision and drainage is not recommended because recurrence is almost universal. For limited stage I and II disease, a \"deroofing\" procedure with curettage of the base is a good treatment option and is associated with a lower likelihood of recurrence.[14] For patients with Hurley stage III or refractory hidradenitis suppurativa, surgery is the best option. Patients with more extensive disease require wide excision, followed by split-thickness skin grafts or local fasciocutaneous flaps; the latter often provide better functional results.[15] Lasers designed to help with hair reduction have also been used with some success.",
"In conclusion, hidradenitis suppurativa remains a challenging, chronic debilitating condition; therefore, patient education and support groups are essential. Treatment often consists of a combination of lifestyle modifications (eg, weight loss, avoidance of tight-fitting clothes and skin trauma, keeping skin cool, warm compresses), topical therapies, laser hair reduction, systemic agents, or surgery.",
"The patient in this case was classified as having Hurley stage III hidradenitis suppurativa. Because he experienced recurrence and contractures, after local excision and grafting, he was referred for wide excision followed by closure of the defect with a local fasciocutaneous advancement flap."
],
"date": "July 27, 2021",
"figures": [],
"markdown": "# A 40-Year-Old Man With Painful, Rupturing Lesions\n\n **Authors:** Elizabeth K. Satter, MD, MPH \n **Date:** July 27, 2021\n\n ## Content\n\n Treatment of hidradenitis suppurativa is often challenging. Despite the introduction of new therapeutic options, large clinical trials are few. Early diagnosis and treatment is essential because more effective control can be achieved in early disease, with the goal of treatment being to reduce disease burden; prevent development of new lesions; and avoid, or at least limit, scarring. Unfortunately, patients typically do not seek medical attention when they have early limited disease or are misdiagnosed with suppurative folliculitis, carbuncles, or inflamed epidermal or pilonidal cysts and treated with incision and drainage.\nSeveral comprehensive reviews have evaluated different treatment options based on clinical stage; however, no treatment gained US Food and Drug Administration (FDA) approval for hidradenitis suppurativa until May 2015, when the FDA granted adalimumab orphan status for treatment of patients with Hurley stage II or III disease.[11,12] First-line medical therapy for patients with Hurley stage I or II disease should include topical antimicrobials (eg, benzoyl peroxide washes, bleach baths, bleach soaks) and clindamycin lotion, along with short courses of oral doxycycline, minocycline, or the combination of clindamycin and rifampin for acute flares. Dapsone has also been used; however, studies are limited and have shown variable results.[11,12] Antibiotics are believed to be beneficial, not just for their bactericidal properties but also their anti-inflammatory and immunomodulatory effects. However, similar to acne treatment, long-term antibiotic therapy is not recommended owing to development of bacterial resistance.\nAlthough hidradenitis suppurativa resembles nodular acne, oral retinoids have had limited success. Antiandrogen therapy may be beneficial for females with hidradenitis suppurativa, especially those who experience flares of their symptoms with menstruation.[11,12] Methotrexate, metformin, and various biologic agents (adalimumab, anakinra, etanercept, infliximab, and ustekinumab) are typically reserved for patients in whom other approaches have been tried and failed.[11,12,13]\nSurgical options depend on the stage of disease. Incision and drainage is not recommended because recurrence is almost universal. For limited stage I and II disease, a \"deroofing\" procedure with curettage of the base is a good treatment option and is associated with a lower likelihood of recurrence.[14] For patients with Hurley stage III or refractory hidradenitis suppurativa, surgery is the best option. Patients with more extensive disease require wide excision, followed by split-thickness skin grafts or local fasciocutaneous flaps; the latter often provide better functional results.[15] Lasers designed to help with hair reduction have also been used with some success.\nIn conclusion, hidradenitis suppurativa remains a challenging, chronic debilitating condition; therefore, patient education and support groups are essential. Treatment often consists of a combination of lifestyle modifications (eg, weight loss, avoidance of tight-fitting clothes and skin trauma, keeping skin cool, warm compresses), topical therapies, laser hair reduction, systemic agents, or surgery.\nThe patient in this case was classified as having Hurley stage III hidradenitis suppurativa. Because he experienced recurrence and contractures, after local excision and grafting, he was referred for wide excision followed by closure of the defect with a local fasciocutaneous advancement flap.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 950259,
"choiceText": "The primary pathogenesis of hidradenitis suppurativa is apocrine gland dysfunction",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950261,
"choiceText": "Apocrine gland inflammation is hypothesized to be the inciting event that leads to follicular occlusion and the characteristic lesions of hidradenitis suppurativa",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950263,
"choiceText": "Smoking and obesity have been definitively established as playing a large role in the pathogenesis of hidradenitis suppurativa in many patients",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950265,
"choiceText": "The primary etiology of hidradenitis suppurativa is follicular occlusion, followed by follicular rupture and a brisk inflammatory response",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The inciting event is hypothesized to be occlusion of the follicular infundibulum, followed by follicular rupture associated with a vigorous inflammatory response. The pathologic role of microorganisms is debatable; however, bacteria may play a role in eliciting an autoinflammatory response via the innate immune system.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 300637,
"questionText": "Which of the following statements about hidradenitis suppurativa is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 950267,
"choiceText": "Lifestyle modifications have <i>not</i> been proven to alter the course of hidradenitis suppurativa",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950269,
"choiceText": "Because the etiology of hidradenitis suppurativa has now been elucidated, targeted biologic therapies are considered the first-line therapy for all patients with severe disease",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950271,
"choiceText": "Patients classified as having Hurley stage III hidradenitis suppurativa are best treated with topical agents",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950273,
"choiceText": "Surgery should be considered, along with pharmacologic therapy, when developing an individualized treatment plan in most patients with hidradenitis suppurativa",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Treatment often consists of a combination of lifestyle modifications (eg, weight loss, avoidance of tight-fitting clothes and skin trauma, keeping skin cool, warm compresses), topical therapies, laser hair reduction, systemic agents, or surgery.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 300639,
"questionText": "Which of the following statements most accurately describes the therapeutic options for hidradenitis suppurativa?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 40-Year-Old Man With Painful, Rupturing Lesions"
},
{
"authors": "Elizabeth K. Satter, MD, MPH",
"content": [],
"date": "July 27, 2021",
"figures": [],
"markdown": "# A 40-Year-Old Man With Painful, Rupturing Lesions\n\n **Authors:** Elizabeth K. Satter, MD, MPH \n **Date:** July 27, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 950259,
"choiceText": "The primary pathogenesis of hidradenitis suppurativa is apocrine gland dysfunction",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950261,
"choiceText": "Apocrine gland inflammation is hypothesized to be the inciting event that leads to follicular occlusion and the characteristic lesions of hidradenitis suppurativa",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950263,
"choiceText": "Smoking and obesity have been definitively established as playing a large role in the pathogenesis of hidradenitis suppurativa in many patients",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950265,
"choiceText": "The primary etiology of hidradenitis suppurativa is follicular occlusion, followed by follicular rupture and a brisk inflammatory response",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The inciting event is hypothesized to be occlusion of the follicular infundibulum, followed by follicular rupture associated with a vigorous inflammatory response. The pathologic role of microorganisms is debatable; however, bacteria may play a role in eliciting an autoinflammatory response via the innate immune system.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 300637,
"questionText": "Which of the following statements about hidradenitis suppurativa is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 950267,
"choiceText": "Lifestyle modifications have <i>not</i> been proven to alter the course of hidradenitis suppurativa",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950269,
"choiceText": "Because the etiology of hidradenitis suppurativa has now been elucidated, targeted biologic therapies are considered the first-line therapy for all patients with severe disease",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950271,
"choiceText": "Patients classified as having Hurley stage III hidradenitis suppurativa are best treated with topical agents",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950273,
"choiceText": "Surgery should be considered, along with pharmacologic therapy, when developing an individualized treatment plan in most patients with hidradenitis suppurativa",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Treatment often consists of a combination of lifestyle modifications (eg, weight loss, avoidance of tight-fitting clothes and skin trauma, keeping skin cool, warm compresses), topical therapies, laser hair reduction, systemic agents, or surgery.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 300639,
"questionText": "Which of the following statements most accurately describes the therapeutic options for hidradenitis suppurativa?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 40-Year-Old Man With Painful, Rupturing Lesions"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 950249,
"choiceText": "Granuloma inguinale",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950251,
"choiceText": "Lymphogranuloma venereum",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950253,
"choiceText": "Cutaneous Crohn disease",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950255,
"choiceText": "Hidradenitis suppurativa",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950257,
"choiceText": "Recurrent furunculosis\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 300635,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 950259,
"choiceText": "The primary pathogenesis of hidradenitis suppurativa is apocrine gland dysfunction",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950261,
"choiceText": "Apocrine gland inflammation is hypothesized to be the inciting event that leads to follicular occlusion and the characteristic lesions of hidradenitis suppurativa",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950263,
"choiceText": "Smoking and obesity have been definitively established as playing a large role in the pathogenesis of hidradenitis suppurativa in many patients",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950265,
"choiceText": "The primary etiology of hidradenitis suppurativa is follicular occlusion, followed by follicular rupture and a brisk inflammatory response",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The inciting event is hypothesized to be occlusion of the follicular infundibulum, followed by follicular rupture associated with a vigorous inflammatory response. The pathologic role of microorganisms is debatable; however, bacteria may play a role in eliciting an autoinflammatory response via the innate immune system.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 300637,
"questionText": "Which of the following statements about hidradenitis suppurativa is most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 950267,
"choiceText": "Lifestyle modifications have <i>not</i> been proven to alter the course of hidradenitis suppurativa",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950269,
"choiceText": "Because the etiology of hidradenitis suppurativa has now been elucidated, targeted biologic therapies are considered the first-line therapy for all patients with severe disease",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950271,
"choiceText": "Patients classified as having Hurley stage III hidradenitis suppurativa are best treated with topical agents",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 950273,
"choiceText": "Surgery should be considered, along with pharmacologic therapy, when developing an individualized treatment plan in most patients with hidradenitis suppurativa",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Treatment often consists of a combination of lifestyle modifications (eg, weight loss, avoidance of tight-fitting clothes and skin trauma, keeping skin cool, warm compresses), topical therapies, laser hair reduction, systemic agents, or surgery.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 300639,
"questionText": "Which of the following statements most accurately describes the therapeutic options for hidradenitis suppurativa?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
954850 | /viewarticle/954850 | [
{
"authors": "Paul P. Rega, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 53-year-old woman comes to the emergency department (ED) in the middle of the night with a 1-day history of diffuse, constant, and worsening abdominal pain. The pain is not associated with fever, nausea, vomiting, constipation, diarrhea, or urinary symptoms. Her review of symptoms is positive only for visual blurriness and xerostomia.",
"The patient takes atorvastatin and atenolol/chlorthalidone. She has no recent history of trauma or hospitalizations. Past surgeries include an appendectomy at 10 years of age and a hysterectomy at 42 years of age.",
"She lives with her husband and adult son, and they all work from home on their social media business. Her husband and son are not ill, although they have generally shared the same environment and foods. They have been living in isolation as much as possible for fear of contracting SARS-CoV-2. The COVID-19 pandemic has significantly affected their private lives; however, new projects such as painting lessons, canning workshops, and jewelry-making have enhanced their physical and mental health. None of the family has been tested for the virus, and they have not yet been vaccinated."
],
"date": "July 20, 2021",
"figures": [],
"markdown": "# A 53-Year-Old Social Media Worker With Dysphonia and Paresis\n\n **Authors:** Paul P. Rega, MD \n **Date:** July 20, 2021\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 53-year-old woman comes to the emergency department (ED) in the middle of the night with a 1-day history of diffuse, constant, and worsening abdominal pain. The pain is not associated with fever, nausea, vomiting, constipation, diarrhea, or urinary symptoms. Her review of symptoms is positive only for visual blurriness and xerostomia.\nThe patient takes atorvastatin and atenolol/chlorthalidone. She has no recent history of trauma or hospitalizations. Past surgeries include an appendectomy at 10 years of age and a hysterectomy at 42 years of age.\nShe lives with her husband and adult son, and they all work from home on their social media business. Her husband and son are not ill, although they have generally shared the same environment and foods. They have been living in isolation as much as possible for fear of contracting SARS-CoV-2. The COVID-19 pandemic has significantly affected their private lives; however, new projects such as painting lessons, canning workshops, and jewelry-making have enhanced their physical and mental health. None of the family has been tested for the virus, and they have not yet been vaccinated.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A 53-Year-Old Social Media Worker With Dysphonia and Paresis"
},
{
"authors": "Paul P. Rega, MD",
"content": [
"The patient's initial vital signs in the ED include a temperature of 98.6 °F, heart rate of 102 beats/minute with sinus tachycardia, blood pressure of 116/50 mm Hg, and respiration rate of 18 breaths/minute. Her oxygen saturation level is 99%. Her score on the Glasgow Coma Scale is 15. She rates the level of her pain at 7 out of 10.",
"Once the patient is undressed and placed in a gown, a physical examination is performed. The results are normal except for a mildly distended abdomen with voluntary guarding along the lower quadrants. No rebound tenderness is noted. The mucous membranes are slightly dry. The results of the neurologic examination are grossly intact.",
"An intravenous (IV) line is inserted, and blood is drawn for laboratory studies. The results of a complete blood cell count, comprehensive metabolic panel, and urinalysis are normal. Plain abdominal radiography reveals distended loops of bowel and air-fluid levels. Similar radiographic findings are shown below in a different patient (Figure 1).",
"Figure 1.",
"An abdominal CT scan with IV contrast confirms the dilated loops of small bowel but reveals no evidence of a mechanical obstruction. Figure 2 shows an example of an intestinal obstruction on a CT scan in a different patient.",
"Figure 2.",
"After a consultation finds no evidence of an acute abdomen requiring surgery, the patient is sent to the ED observation unit for placement of a nasogastric tube, IV hydration, analgesia, and monitoring.",
"Over the course of 4-5 hours in the observation unit, the patient begins to see double, and her speech becomes less intelligible. She also complains of shortness of breath. Her temperature is 98.2 °F, heart rate is 52 beats/minute, blood pressure is 92/52 mm Hg, and respiration rate is 28 breaths/minute. Her oxygen saturation level is 97%. Her score on the Glasgow Coma Scale is 14-15. She rates the level of her pain at 2 out of 10.",
"The physician on duty is unable to see the patient immediately and orders a CT scan of the brain, repeated blood tests, and arterial blood gas analysis. The results of the brain CT scan are normal. The arterial blood gas analysis demonstrates a moderate respiratory acidosis. The findings are:",
"Arterial blood pH: 7.32 (reference range, 7.35-7.45)",
"Partial pressure of oxygen (Po2): 94 mm Hg (reference range, 75-100 mm Hg)",
"Partial pressure of carbon dioxide (Pco2): 56 mm Hg (reference range, 35-45 mm Hg)",
"When the physician returns to see the patient, he notes bilateral ptosis, dysphonia, dysarthria, and bilateral cranial nerve VI paresis."
],
"date": "July 20, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/954/850/954850-Thumb1.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/954/850/954850-Thumb2.jpg"
}
],
"markdown": "# A 53-Year-Old Social Media Worker With Dysphonia and Paresis\n\n **Authors:** Paul P. Rega, MD \n **Date:** July 20, 2021\n\n ## Content\n\n The patient's initial vital signs in the ED include a temperature of 98.6 °F, heart rate of 102 beats/minute with sinus tachycardia, blood pressure of 116/50 mm Hg, and respiration rate of 18 breaths/minute. Her oxygen saturation level is 99%. Her score on the Glasgow Coma Scale is 15. She rates the level of her pain at 7 out of 10.\nOnce the patient is undressed and placed in a gown, a physical examination is performed. The results are normal except for a mildly distended abdomen with voluntary guarding along the lower quadrants. No rebound tenderness is noted. The mucous membranes are slightly dry. The results of the neurologic examination are grossly intact.\nAn intravenous (IV) line is inserted, and blood is drawn for laboratory studies. The results of a complete blood cell count, comprehensive metabolic panel, and urinalysis are normal. Plain abdominal radiography reveals distended loops of bowel and air-fluid levels. Similar radiographic findings are shown below in a different patient (Figure 1).\nFigure 1.\nAn abdominal CT scan with IV contrast confirms the dilated loops of small bowel but reveals no evidence of a mechanical obstruction. Figure 2 shows an example of an intestinal obstruction on a CT scan in a different patient.\nFigure 2.\nAfter a consultation finds no evidence of an acute abdomen requiring surgery, the patient is sent to the ED observation unit for placement of a nasogastric tube, IV hydration, analgesia, and monitoring.\nOver the course of 4-5 hours in the observation unit, the patient begins to see double, and her speech becomes less intelligible. She also complains of shortness of breath. Her temperature is 98.2 °F, heart rate is 52 beats/minute, blood pressure is 92/52 mm Hg, and respiration rate is 28 breaths/minute. Her oxygen saturation level is 97%. Her score on the Glasgow Coma Scale is 14-15. She rates the level of her pain at 2 out of 10.\nThe physician on duty is unable to see the patient immediately and orders a CT scan of the brain, repeated blood tests, and arterial blood gas analysis. The results of the brain CT scan are normal. The arterial blood gas analysis demonstrates a moderate respiratory acidosis. The findings are:\nArterial blood pH: 7.32 (reference range, 7.35-7.45)\nPartial pressure of oxygen (Po2): 94 mm Hg (reference range, 75-100 mm Hg)\nPartial pressure of carbon dioxide (Pco2): 56 mm Hg (reference range, 35-45 mm Hg)\nWhen the physician returns to see the patient, he notes bilateral ptosis, dysphonia, dysarthria, and bilateral cranial nerve VI paresis.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1605352,
"choiceText": "Tolosa-Hunt syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605353,
"choiceText": "Guillain-Barré syndrome ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605354,
"choiceText": "Tick paralysis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605355,
"choiceText": "Foodborne botulism",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 515502,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 53-Year-Old Social Media Worker With Dysphonia and Paresis"
},
{
"authors": "Paul P. Rega, MD",
"content": [
"Tolosa-Hunt syndrome is a granulomatous inflammatory process near the cavernous sinus or within certain areas of the orbits. The disease manifests with one or more episodes of unilateral ocular pain in addition to paralysis of cranial nerves III, IV, and/or V. In contrast to this patient's presentation, there is typically no gastrointestinal prodrome or progression of the neurologic manifestations beyond the ocular nerves.",
"An association between SARS-CoV-2 infection and Guillain-Barré syndrome has been described in the recent literature.[1] Classically, Guillain-Barré syndrome is a demyelinating polyneuropathy associated with an acute ascending paralysis. Gastrointestinal symptoms, like what occurred in this patient, are not part of the prodrome in Guillain-Barré syndrome.",
"In North America, tick paralysis is common during the spring and summer when ticks are most active. Owing to the pandemic, this patient's activities have been primarily indoors rather than outdoors, where tick bites are more likely to occur. Furthermore, when this patient was undressed and placed in a gown in the ED, a tick would likely have been discovered. The neurologic manifestations occur while the tick is attached. Once the tick is removed, the paralysis resolves. The prodrome is an influenza-like illness, and acute abdominal pain is not a typical presentation. The second stage is an ascending paralysis, not a descending paralysis. Patients are ataxic and exhibit lower extremity muscular weakness.",
"Botulism is a neuromuscular disease caused by toxins generated by the anaerobic, Gram-positive bacterium Clostridium botulinum (Figure 3). Six syndromes are recognized: infant, foodborne, wound, adult colonization, inhalational, and iatrogenic. Of the eight neurotoxins (A to H), toxins A, B, and E (F, rarely) affect humans.[2,3] Type H was discovered in 1977.[4] These neurotoxins are considered the most potent biologic poison known.[2,3]",
"Figure 3.",
"From 2011 to 2015, 162 cases of botulism were reported annually (mean). Infant botulism, foodborne botulism, and wound botulism occurred in 71%-88%, 1%-20%, and 5%-10% of these cases, respectively.[3] For foodborne botulism, the incubation period from first exposure to symptom onset can be from 12 to 72 hours (range, 2 hours to 8 days). The classic manifestations begin with a symmetrical paresis or paralysis starting from head to toe. The initial symptoms of botulism poisoning include ptosis, dysphonia, dysphagia, dysarthria, xerostomia, and visual difficulties (ie, bulbar manifestations).[2,3]"
],
"date": "July 20, 2021",
"figures": [
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/954/850/954850-Thumb3.jpg"
}
],
"markdown": "# A 53-Year-Old Social Media Worker With Dysphonia and Paresis\n\n **Authors:** Paul P. Rega, MD \n **Date:** July 20, 2021\n\n ## Content\n\n Tolosa-Hunt syndrome is a granulomatous inflammatory process near the cavernous sinus or within certain areas of the orbits. The disease manifests with one or more episodes of unilateral ocular pain in addition to paralysis of cranial nerves III, IV, and/or V. In contrast to this patient's presentation, there is typically no gastrointestinal prodrome or progression of the neurologic manifestations beyond the ocular nerves.\nAn association between SARS-CoV-2 infection and Guillain-Barré syndrome has been described in the recent literature.[1] Classically, Guillain-Barré syndrome is a demyelinating polyneuropathy associated with an acute ascending paralysis. Gastrointestinal symptoms, like what occurred in this patient, are not part of the prodrome in Guillain-Barré syndrome.\nIn North America, tick paralysis is common during the spring and summer when ticks are most active. Owing to the pandemic, this patient's activities have been primarily indoors rather than outdoors, where tick bites are more likely to occur. Furthermore, when this patient was undressed and placed in a gown in the ED, a tick would likely have been discovered. The neurologic manifestations occur while the tick is attached. Once the tick is removed, the paralysis resolves. The prodrome is an influenza-like illness, and acute abdominal pain is not a typical presentation. The second stage is an ascending paralysis, not a descending paralysis. Patients are ataxic and exhibit lower extremity muscular weakness.\nBotulism is a neuromuscular disease caused by toxins generated by the anaerobic, Gram-positive bacterium Clostridium botulinum (Figure 3). Six syndromes are recognized: infant, foodborne, wound, adult colonization, inhalational, and iatrogenic. Of the eight neurotoxins (A to H), toxins A, B, and E (F, rarely) affect humans.[2,3] Type H was discovered in 1977.[4] These neurotoxins are considered the most potent biologic poison known.[2,3]\nFigure 3.\nFrom 2011 to 2015, 162 cases of botulism were reported annually (mean). Infant botulism, foodborne botulism, and wound botulism occurred in 71%-88%, 1%-20%, and 5%-10% of these cases, respectively.[3] For foodborne botulism, the incubation period from first exposure to symptom onset can be from 12 to 72 hours (range, 2 hours to 8 days). The classic manifestations begin with a symmetrical paresis or paralysis starting from head to toe. The initial symptoms of botulism poisoning include ptosis, dysphonia, dysphagia, dysarthria, xerostomia, and visual difficulties (ie, bulbar manifestations).[2,3]\n\n ## Figures\n\n **Figure 3.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1605352,
"choiceText": "Tolosa-Hunt syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605353,
"choiceText": "Guillain-Barré syndrome ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605354,
"choiceText": "Tick paralysis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605355,
"choiceText": "Foodborne botulism",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 515502,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 53-Year-Old Social Media Worker With Dysphonia and Paresis"
},
{
"authors": "Paul P. Rega, MD",
"content": [
"Although death was a frequent outcome in the past, it rarely occurs today. Before 1950 or so, foodborne botulism carried a mortality rate of 60%-70%. That rate dropped to 3% for all the different types of botulism between 1975 and 2009.[3] Two principal causes of early death are complete airway obstruction from a food bolus as the muscles of deglutition become paralyzed and suffocation with paralysis of the diaphragm and intercostal muscles.[2]",
"Once introduced into the body, the toxin enters the neuronal cells at the voluntary motor and autonomic neuromuscular junctions. There, it disrupts the release of neurotransmitter (acetylcholine) across the junction. With acetylcholine transmission blocked, the receptor sites of the motor and autonomic cells lie vacant. Flaccid paralysis occurs.[2,3] This process cannot be reversed. It may take months for the regeneration of the neurotransmitter mechanics.[2]",
"The initial manifestations of botulism may be misleading. A patient who presents at the early stage may be alert and afebrile. The patient may sense the minute anatomic changes, but these subjective concerns are subtle and may be attributed to more typical maladies. Common misdiagnoses at this stage include alcohol or drug intoxication and psychiatric disorders.[2] Later, the neurologic signs become dominant, and botulism may be misdiagnosed as stroke, Tolosa-Hunt syndrome, meningitis, myasthenia gravis, tick paralysis, or Guillain-Barré syndrome.[1,2,5,6,7]",
"Rarely, the gastrointestinal manifestations of botulism may predate or obscure the classic neurologic symptoms.[2,3] Botulism has been mistaken for acute bowel obstruction.[8,9] It is not until the neurologic manifestations come to the forefront that the correct diagnosis is made. In the patient in this case, the early ptosis was mistaken for lack of sleep and the xerostomia for dehydration. Nevertheless, the workup for a bowel obstruction (ie, abdominal radiographs and a CT scan of the abdomen with contrast) was reasonable because it is a more common disorder.",
"In-depth questioning of this patient revealed that several days before she came to the ED, she opened and tasted a batch of canned jalapeño peppers she had made a few months earlier. She was planning to take them to a parish food drive. Her husband and son did not consume any of the peppers.",
"Once botulism is included in the differential diagnosis, three actions must occur. First, the patient's status must be NPO to prevent aspiration. Second, assessment of respiratory capabilities is critical. It can be accomplished through various measurements, such as negative inspiratory force, vital capacity, blood gas analysis, or capnography.[1,2] Carbon dioxide retention requires immediate consideration of aggressive airway management to counter respiratory paralysis and cardiorespiratory arrest. Third, the local public health department and the Centers for Disease Control and Prevention (CDC) must be notified. Any case of botulism in a community is a public health emergency. An urgent epidemiologic investigation must begin to search for additional cases and the source of the outbreak (eg, restaurants).[2]",
"Meanwhile, electrodiagnostic studies may be used to evaluate muscle weakness.[2] Laboratory studies to confirm botulism include testing for neurotoxin in the serum, stool, and gastric juices; identifying clostridia in stool or wound cultures; and investigating the suspected sources of the toxin release. The mouse bioassay remains the gold standard. Real-time polymerase chain reaction and mass spectrometry are also helpful.[2] However, waiting for the results of these studies cannot delay communication with the CDC once botulism is suspected.",
"The CDC has the responsibility for releasing Botulinum Antitoxin Heptavalent (A, B, C, D, E, F, G) (Equine) (BAT). It is free and is available to clinicians 24 hours a day, 7 days a week.[2] Early administration of the antitoxin is associated with fewer days in the hospital and intensive care unit and a reduced need for mechanical ventilation support.[2,10,11] BAT neutralizes only the toxin circulating in the bloodstream that has yet to be incorporated into the cells.[1] In 2015, at a botulism mass casualty incident at a potluck meal in Lancaster, Ohio, the antitoxin was requested at 10 AM but did not arrive until midnight.[12,13] Therefore, the CDC should be contacted expeditiously. Note that Botulism Immune Globulin Intravenous (Human) (BIG-IV) (BabyBIG), the specific immunoglobulin G for infants with botulism who are younger than 1 year of age, is requested through the California Department of Public Health Infant Botulism Treatment and Prevention Program.[2,14]"
],
"date": "July 20, 2021",
"figures": [],
"markdown": "# A 53-Year-Old Social Media Worker With Dysphonia and Paresis\n\n **Authors:** Paul P. Rega, MD \n **Date:** July 20, 2021\n\n ## Content\n\n Although death was a frequent outcome in the past, it rarely occurs today. Before 1950 or so, foodborne botulism carried a mortality rate of 60%-70%. That rate dropped to 3% for all the different types of botulism between 1975 and 2009.[3] Two principal causes of early death are complete airway obstruction from a food bolus as the muscles of deglutition become paralyzed and suffocation with paralysis of the diaphragm and intercostal muscles.[2]\nOnce introduced into the body, the toxin enters the neuronal cells at the voluntary motor and autonomic neuromuscular junctions. There, it disrupts the release of neurotransmitter (acetylcholine) across the junction. With acetylcholine transmission blocked, the receptor sites of the motor and autonomic cells lie vacant. Flaccid paralysis occurs.[2,3] This process cannot be reversed. It may take months for the regeneration of the neurotransmitter mechanics.[2]\nThe initial manifestations of botulism may be misleading. A patient who presents at the early stage may be alert and afebrile. The patient may sense the minute anatomic changes, but these subjective concerns are subtle and may be attributed to more typical maladies. Common misdiagnoses at this stage include alcohol or drug intoxication and psychiatric disorders.[2] Later, the neurologic signs become dominant, and botulism may be misdiagnosed as stroke, Tolosa-Hunt syndrome, meningitis, myasthenia gravis, tick paralysis, or Guillain-Barré syndrome.[1,2,5,6,7]\nRarely, the gastrointestinal manifestations of botulism may predate or obscure the classic neurologic symptoms.[2,3] Botulism has been mistaken for acute bowel obstruction.[8,9] It is not until the neurologic manifestations come to the forefront that the correct diagnosis is made. In the patient in this case, the early ptosis was mistaken for lack of sleep and the xerostomia for dehydration. Nevertheless, the workup for a bowel obstruction (ie, abdominal radiographs and a CT scan of the abdomen with contrast) was reasonable because it is a more common disorder.\nIn-depth questioning of this patient revealed that several days before she came to the ED, she opened and tasted a batch of canned jalapeño peppers she had made a few months earlier. She was planning to take them to a parish food drive. Her husband and son did not consume any of the peppers.\nOnce botulism is included in the differential diagnosis, three actions must occur. First, the patient's status must be NPO to prevent aspiration. Second, assessment of respiratory capabilities is critical. It can be accomplished through various measurements, such as negative inspiratory force, vital capacity, blood gas analysis, or capnography.[1,2] Carbon dioxide retention requires immediate consideration of aggressive airway management to counter respiratory paralysis and cardiorespiratory arrest. Third, the local public health department and the Centers for Disease Control and Prevention (CDC) must be notified. Any case of botulism in a community is a public health emergency. An urgent epidemiologic investigation must begin to search for additional cases and the source of the outbreak (eg, restaurants).[2]\nMeanwhile, electrodiagnostic studies may be used to evaluate muscle weakness.[2] Laboratory studies to confirm botulism include testing for neurotoxin in the serum, stool, and gastric juices; identifying clostridia in stool or wound cultures; and investigating the suspected sources of the toxin release. The mouse bioassay remains the gold standard. Real-time polymerase chain reaction and mass spectrometry are also helpful.[2] However, waiting for the results of these studies cannot delay communication with the CDC once botulism is suspected.\nThe CDC has the responsibility for releasing Botulinum Antitoxin Heptavalent (A, B, C, D, E, F, G) (Equine) (BAT). It is free and is available to clinicians 24 hours a day, 7 days a week.[2] Early administration of the antitoxin is associated with fewer days in the hospital and intensive care unit and a reduced need for mechanical ventilation support.[2,10,11] BAT neutralizes only the toxin circulating in the bloodstream that has yet to be incorporated into the cells.[1] In 2015, at a botulism mass casualty incident at a potluck meal in Lancaster, Ohio, the antitoxin was requested at 10 AM but did not arrive until midnight.[12,13] Therefore, the CDC should be contacted expeditiously. Note that Botulism Immune Globulin Intravenous (Human) (BIG-IV) (BabyBIG), the specific immunoglobulin G for infants with botulism who are younger than 1 year of age, is requested through the California Department of Public Health Infant Botulism Treatment and Prevention Program.[2,14]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A 53-Year-Old Social Media Worker With Dysphonia and Paresis"
},
{
"authors": "Paul P. Rega, MD",
"content": [
"The patient in this case received the botulinum antitoxin, and her clinical manifestations resolved almost completely within 24 hours. She did not need intubation or mechanical ventilation support.",
"Any patient with a presumptive diagnosis of botulism may require invasive airway management, owing to impending paralysis. Patients who may have a difficult airway should be identified early. Such patients include those who have short necks, obvious nuchal and/or facial abnormalities, or disconcerting results on an airway assessment tool (eg, the Mallampati score). For this type of patient, an elective intubation is safer than an emergency intubation.",
"Another situation that must be planned for is a community-wide outbreak with limited healthcare resources. Between 1977 and 2015, there were six foodborne botulism outbreaks involving multiple patients. The smallest outbreak (16 people) occurred in Texas in 2001 and was caused by contaminated chili at a church function. The highest caseload was 58 patients in Michigan in 1977. In this outbreak, home-canned peppers served at a local restaurant contained the botulinum toxin (Figure 4).[12]",
"Figure 4.",
"As patients involved in an outbreak arrive at an ED, there may be a paucity of respiratory therapists and equipment to evaluate progressive respiratory failure expediently. One solution is the single-breath counting test.[15] Its functionality is not limited by skill set, equipment needs, or geography. The next step is to triage certain patients to outlying institutions to avoid compromising healthcare capabilities at the initial hospital. Reverse triage may be the safest method; that is, transporting the intubated patients whose condition is less likely to deteriorate en route.",
"Botulism is a complicated disease for both patients and their communities. It must be managed with equal measures of skill and flexibility."
],
"date": "July 20, 2021",
"figures": [
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/954/850/954850-Thumb4.jpg"
}
],
"markdown": "# A 53-Year-Old Social Media Worker With Dysphonia and Paresis\n\n **Authors:** Paul P. Rega, MD \n **Date:** July 20, 2021\n\n ## Content\n\n The patient in this case received the botulinum antitoxin, and her clinical manifestations resolved almost completely within 24 hours. She did not need intubation or mechanical ventilation support.\nAny patient with a presumptive diagnosis of botulism may require invasive airway management, owing to impending paralysis. Patients who may have a difficult airway should be identified early. Such patients include those who have short necks, obvious nuchal and/or facial abnormalities, or disconcerting results on an airway assessment tool (eg, the Mallampati score). For this type of patient, an elective intubation is safer than an emergency intubation.\nAnother situation that must be planned for is a community-wide outbreak with limited healthcare resources. Between 1977 and 2015, there were six foodborne botulism outbreaks involving multiple patients. The smallest outbreak (16 people) occurred in Texas in 2001 and was caused by contaminated chili at a church function. The highest caseload was 58 patients in Michigan in 1977. In this outbreak, home-canned peppers served at a local restaurant contained the botulinum toxin (Figure 4).[12]\nFigure 4.\nAs patients involved in an outbreak arrive at an ED, there may be a paucity of respiratory therapists and equipment to evaluate progressive respiratory failure expediently. One solution is the single-breath counting test.[15] Its functionality is not limited by skill set, equipment needs, or geography. The next step is to triage certain patients to outlying institutions to avoid compromising healthcare capabilities at the initial hospital. Reverse triage may be the safest method; that is, transporting the intubated patients whose condition is less likely to deteriorate en route.\nBotulism is a complicated disease for both patients and their communities. It must be managed with equal measures of skill and flexibility.\n\n ## Figures\n\n **Figure 4.** \n \n\n\n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1605356,
"choiceText": "Neurotoxins A, B, and E",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605357,
"choiceText": "Neurotoxins A and B only",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605358,
"choiceText": "Neurotoxins C and D only",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605359,
"choiceText": "Neurotoxin D, E, and F",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Of the eight C <i>botulinum</i> toxins (A to H), the ones that are likely to be poisonous to humans are A, B, and E, and rarely F. Type A produces the most severe syndromes. Type E is usually associated with botulism caused by consumption of aquatic food. Neurotoxin H was the last one discovered in 1977.<sup>[2]</sup>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 515503,
"questionText": "Which botulinum toxins are most deleterious to humans?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1605360,
"choiceText": "It is an antibiotic cocktail for infants with a diagnosis of wound botulism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605361,
"choiceText": "It is indicated for infants and children aged 1-5 years",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605362,
"choiceText": "The CDC administers BabyBIG",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605363,
"choiceText": "It is indicated for infants up to 1 year of age who have a diagnosis of botulism\r\n\r\n",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "BabyBIG is an orphan drug that consists of human-derived anti–botulism toxin antibodies. It has been approved by the US Food and Drug Administration for the treatment of infant botulism types A and B in infants younger than 1 year. The treating physician can obtain BabyBIG by contacting the California Department of Public Health's Infant Botulism Treatment and Prevention Program. It has been administered to more than 1500 infants with botulism and, compared with control patients, resulted in a 3.5-week decrease in length of hospitalization.<sup>[10,14]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 515504,
"questionText": "Which of the following statements about BabyBIG is the most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 53-Year-Old Social Media Worker With Dysphonia and Paresis"
},
{
"authors": "Paul P. Rega, MD",
"content": [],
"date": "July 20, 2021",
"figures": [],
"markdown": "# A 53-Year-Old Social Media Worker With Dysphonia and Paresis\n\n **Authors:** Paul P. Rega, MD \n **Date:** July 20, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1605356,
"choiceText": "Neurotoxins A, B, and E",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605357,
"choiceText": "Neurotoxins A and B only",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605358,
"choiceText": "Neurotoxins C and D only",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605359,
"choiceText": "Neurotoxin D, E, and F",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Of the eight C <i>botulinum</i> toxins (A to H), the ones that are likely to be poisonous to humans are A, B, and E, and rarely F. Type A produces the most severe syndromes. Type E is usually associated with botulism caused by consumption of aquatic food. Neurotoxin H was the last one discovered in 1977.<sup>[2]</sup>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 515503,
"questionText": "Which botulinum toxins are most deleterious to humans?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1605360,
"choiceText": "It is an antibiotic cocktail for infants with a diagnosis of wound botulism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605361,
"choiceText": "It is indicated for infants and children aged 1-5 years",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605362,
"choiceText": "The CDC administers BabyBIG",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605363,
"choiceText": "It is indicated for infants up to 1 year of age who have a diagnosis of botulism\r\n\r\n",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "BabyBIG is an orphan drug that consists of human-derived anti–botulism toxin antibodies. It has been approved by the US Food and Drug Administration for the treatment of infant botulism types A and B in infants younger than 1 year. The treating physician can obtain BabyBIG by contacting the California Department of Public Health's Infant Botulism Treatment and Prevention Program. It has been administered to more than 1500 infants with botulism and, compared with control patients, resulted in a 3.5-week decrease in length of hospitalization.<sup>[10,14]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 515504,
"questionText": "Which of the following statements about BabyBIG is the most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 53-Year-Old Social Media Worker With Dysphonia and Paresis"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1605352,
"choiceText": "Tolosa-Hunt syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605353,
"choiceText": "Guillain-Barré syndrome ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605354,
"choiceText": "Tick paralysis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605355,
"choiceText": "Foodborne botulism",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 515502,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1605356,
"choiceText": "Neurotoxins A, B, and E",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605357,
"choiceText": "Neurotoxins A and B only",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605358,
"choiceText": "Neurotoxins C and D only",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605359,
"choiceText": "Neurotoxin D, E, and F",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Of the eight C <i>botulinum</i> toxins (A to H), the ones that are likely to be poisonous to humans are A, B, and E, and rarely F. Type A produces the most severe syndromes. Type E is usually associated with botulism caused by consumption of aquatic food. Neurotoxin H was the last one discovered in 1977.<sup>[2]</sup>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 515503,
"questionText": "Which botulinum toxins are most deleterious to humans?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1605360,
"choiceText": "It is an antibiotic cocktail for infants with a diagnosis of wound botulism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605361,
"choiceText": "It is indicated for infants and children aged 1-5 years",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605362,
"choiceText": "The CDC administers BabyBIG",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1605363,
"choiceText": "It is indicated for infants up to 1 year of age who have a diagnosis of botulism\r\n\r\n",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "BabyBIG is an orphan drug that consists of human-derived anti–botulism toxin antibodies. It has been approved by the US Food and Drug Administration for the treatment of infant botulism types A and B in infants younger than 1 year. The treating physician can obtain BabyBIG by contacting the California Department of Public Health's Infant Botulism Treatment and Prevention Program. It has been administered to more than 1500 infants with botulism and, compared with control patients, resulted in a 3.5-week decrease in length of hospitalization.<sup>[10,14]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 515504,
"questionText": "Which of the following statements about BabyBIG is the most accurate?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
731206 | /viewarticle/731206 | [
{
"authors": "Ajith Goonetilleke, MB BS, FRCP",
"content": [
"Editor's Note:\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 34-year-old woman presents to the emergency department (ED) with a 3-day history of pain around the right ear extending to the temple. She was sitting at work today when she suddenly experienced dizziness, a feeling of discomfort in the throat, and a burning sensation in the left arm and leg. When she tried to stand and walk, her right arm and leg did not move in a normal, coordinated manner.",
"The patient was previously healthy and does not take any regular medications. She does not smoke or drink. She does vigorous aerobic exercises on an almost daily basis. Her mother and numerous relatives on her mother's side have hypertension."
],
"date": "July 02, 2021",
"figures": [],
"markdown": "# An Accountant Who Loves Aerobics With Hiccups and Incoordination\n\n **Authors:** Ajith Goonetilleke, MB BS, FRCP \n **Date:** July 02, 2021\n\n ## Content\n\n Editor's Note:\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 34-year-old woman presents to the emergency department (ED) with a 3-day history of pain around the right ear extending to the temple. She was sitting at work today when she suddenly experienced dizziness, a feeling of discomfort in the throat, and a burning sensation in the left arm and leg. When she tried to stand and walk, her right arm and leg did not move in a normal, coordinated manner.\nThe patient was previously healthy and does not take any regular medications. She does not smoke or drink. She does vigorous aerobic exercises on an almost daily basis. Her mother and numerous relatives on her mother's side have hypertension.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "An Accountant Who Loves Aerobics With Hiccups and Incoordination"
},
{
"authors": "Ajith Goonetilleke, MB BS, FRCP",
"content": [
"Upon physical examination, the patient has an oral temperature of 98.6°F (37°C). Her pulse is regular with a rate of 86 beats/min. Her blood pressure is 164/90 mm Hg, and her heart sounds are normal and without added sounds. No arterial bruits are auscultated in her neck.",
"She is noted to have prolonged bouts of hiccuping. She is unable to stand due to a severe feeling of imbalance. Right-sided ptosis and miosis is observed. She has a sustained horizontal gaze-evoked nystagmus looking to the left and right, with a downbeating nystagmus on downward gaze. Decreased sensation of pinprick and temperature on the right side of the face is noted. The right side also has reduced movement of the palate, and the gag reflex is diminished. The tongue movements are normal.",
"The power is normal in all 4 limbs, the deep tendon reflexes are normal, and the plantar responses are downgoing bilaterally (no Babinski sign). Moderate ataxia affects the right arm and leg. Sensation to pinprick and temperature is decreased on the left arm, leg, and trunk. The joint position and vibration sense are intact bilaterally.",
"Routine laboratory analysis findings, including a complete blood cell count, a basic metabolic panel, and a lipid profile, are normal. Noncontrast CT scan of the head findings are normal. MRI of the brain is obtained (Figure 1).",
"Figure 1."
],
"date": "July 02, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/730/607/730607-thumb1.png"
}
],
"markdown": "# An Accountant Who Loves Aerobics With Hiccups and Incoordination\n\n **Authors:** Ajith Goonetilleke, MB BS, FRCP \n **Date:** July 02, 2021\n\n ## Content\n\n Upon physical examination, the patient has an oral temperature of 98.6°F (37°C). Her pulse is regular with a rate of 86 beats/min. Her blood pressure is 164/90 mm Hg, and her heart sounds are normal and without added sounds. No arterial bruits are auscultated in her neck.\nShe is noted to have prolonged bouts of hiccuping. She is unable to stand due to a severe feeling of imbalance. Right-sided ptosis and miosis is observed. She has a sustained horizontal gaze-evoked nystagmus looking to the left and right, with a downbeating nystagmus on downward gaze. Decreased sensation of pinprick and temperature on the right side of the face is noted. The right side also has reduced movement of the palate, and the gag reflex is diminished. The tongue movements are normal.\nThe power is normal in all 4 limbs, the deep tendon reflexes are normal, and the plantar responses are downgoing bilaterally (no Babinski sign). Moderate ataxia affects the right arm and leg. Sensation to pinprick and temperature is decreased on the left arm, leg, and trunk. The joint position and vibration sense are intact bilaterally.\nRoutine laboratory analysis findings, including a complete blood cell count, a basic metabolic panel, and a lipid profile, are normal. Noncontrast CT scan of the head findings are normal. MRI of the brain is obtained (Figure 1).\nFigure 1.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 373030,
"choiceText": "Right-sided lateral pontine stroke (ie, Marie-Foix syndrome)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373031,
"choiceText": "Right-sided lateral medullary stroke (ie, Wallenberg syndrome) ",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373032,
"choiceText": "Right-sided medial medullary stroke (ie, Dejerine syndrome)",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373033,
"choiceText": "Right-sided hemi-medullary stroke (ie, Babinski-Nageotte syndrome)",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373034,
"choiceText": "Left-sided medial medullary stroke",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 107221,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "An Accountant Who Loves Aerobics With Hiccups and Incoordination"
},
{
"authors": "Ajith Goonetilleke, MB BS, FRCP",
"content": [
"The patient in this case was diagnosed with a lateral medullary stroke on the right with Wallenberg syndrome.",
"Neurons relaying pain and temperature sensation from the right side of the face synapse in the descending spinal nucleus of the trigeminal nerve, which lies in the dorsolateral aspect of the brainstem (Figure 2).",
"Figure 2.",
"Thereafter, the pathway crosses (as the quintothalamic tracts) and ascends to the thalamus. For the limbs and trunk, the neurons of the spinothalamic tract from the left side of the body pass into the spinal cord, where they ascend for 1 or 2 levels (via Lissauer's tract) and then synapse. The second-order neurons then cross to the right side of the spinal cord (via the anterior commissure, just anterior to the central canal of the cord) and then ascend in the anterolateral aspect of the spinal cord up into the right side of the brainstem. In the brainstem, the spinothalamic tract lies laterally.",
"This patient had impairment of pain and temperature (ie, spinothalamic) sensation on the right side of the face and the left side of the body. These contralateral findings are characteristic of a right lateral medullary lesion. The patient also had reduced palatal movements and gag reflex on the right side indicative of involvement of the right IX (glossopharyngeal) and X (vagus) cranial nerves. These cranial nerves, as well as the descending sympathetic fibers (patient had a right-sided Horner sign), are also found in the dorsolateral aspect of the right side of the medulla (Figure 3).",
"Figure 3.",
"The presence of vertigo and right-sided ataxia was due to involvement of the vestibular nucleus and cerebellar pathways (as they pass into the cerebellum through the inferior cerebellar peduncle), respectively, on the right side. The nucleus and the fascicles of the hypoglossal nerve lie medially within the medulla, and the pyramidal pathways lie anteromedially as they pass through the medulla. The joint position and vibration sense modalities pass up the spinal cord on the ipsilateral side and then synapse at the gracile and cuneate nuclei in the lower part of the medulla. The dorsal column pathways then cross (as the internal arcuate fibres) at the level of the lower medulla and pass up the medial aspect of the brainstem as the medial lemnisci. The normal tongue movements and the preserved pyramidal and dorsal column function in this patient indicated that there was sparing of the medial medulla; therefore, this patient had a right-sided lateral medullary syndrome (ie, Wallenberg syndrome), which was determined by brain MRI to be a stroke. The T2-weighted coronal scan showed a high signal abnormality in the right side of the medulla (black arrow, Figure 1).",
"Figure 1.",
"The presence of prominent right ear pain for 3 days prior to developing neurologic deficits was suggestive of a vertebral artery dissection. In fact, stroke preceded by headache or neck pain should always raise suspicion for cervical arterial dissection. The patient performed vigorous aerobic exercises on an almost daily basis, and these exercises included repetitive high-energy lateral neck flexions. This is likely to have been the cause of an arterial dissection. The diagnosis made was of a dissection of the right vertebral artery and a subsequent infarction of the dorsolateral aspect of the right medulla."
],
"date": "July 02, 2021",
"figures": [
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/730/607/730607-thumb2.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/730/607/730607-thumb3.png"
},
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/730/607/730607-thumb1.png"
}
],
"markdown": "# An Accountant Who Loves Aerobics With Hiccups and Incoordination\n\n **Authors:** Ajith Goonetilleke, MB BS, FRCP \n **Date:** July 02, 2021\n\n ## Content\n\n The patient in this case was diagnosed with a lateral medullary stroke on the right with Wallenberg syndrome.\nNeurons relaying pain and temperature sensation from the right side of the face synapse in the descending spinal nucleus of the trigeminal nerve, which lies in the dorsolateral aspect of the brainstem (Figure 2).\nFigure 2.\nThereafter, the pathway crosses (as the quintothalamic tracts) and ascends to the thalamus. For the limbs and trunk, the neurons of the spinothalamic tract from the left side of the body pass into the spinal cord, where they ascend for 1 or 2 levels (via Lissauer's tract) and then synapse. The second-order neurons then cross to the right side of the spinal cord (via the anterior commissure, just anterior to the central canal of the cord) and then ascend in the anterolateral aspect of the spinal cord up into the right side of the brainstem. In the brainstem, the spinothalamic tract lies laterally.\nThis patient had impairment of pain and temperature (ie, spinothalamic) sensation on the right side of the face and the left side of the body. These contralateral findings are characteristic of a right lateral medullary lesion. The patient also had reduced palatal movements and gag reflex on the right side indicative of involvement of the right IX (glossopharyngeal) and X (vagus) cranial nerves. These cranial nerves, as well as the descending sympathetic fibers (patient had a right-sided Horner sign), are also found in the dorsolateral aspect of the right side of the medulla (Figure 3).\nFigure 3.\nThe presence of vertigo and right-sided ataxia was due to involvement of the vestibular nucleus and cerebellar pathways (as they pass into the cerebellum through the inferior cerebellar peduncle), respectively, on the right side. The nucleus and the fascicles of the hypoglossal nerve lie medially within the medulla, and the pyramidal pathways lie anteromedially as they pass through the medulla. The joint position and vibration sense modalities pass up the spinal cord on the ipsilateral side and then synapse at the gracile and cuneate nuclei in the lower part of the medulla. The dorsal column pathways then cross (as the internal arcuate fibres) at the level of the lower medulla and pass up the medial aspect of the brainstem as the medial lemnisci. The normal tongue movements and the preserved pyramidal and dorsal column function in this patient indicated that there was sparing of the medial medulla; therefore, this patient had a right-sided lateral medullary syndrome (ie, Wallenberg syndrome), which was determined by brain MRI to be a stroke. The T2-weighted coronal scan showed a high signal abnormality in the right side of the medulla (black arrow, Figure 1).\nFigure 1.\nThe presence of prominent right ear pain for 3 days prior to developing neurologic deficits was suggestive of a vertebral artery dissection. In fact, stroke preceded by headache or neck pain should always raise suspicion for cervical arterial dissection. The patient performed vigorous aerobic exercises on an almost daily basis, and these exercises included repetitive high-energy lateral neck flexions. This is likely to have been the cause of an arterial dissection. The diagnosis made was of a dissection of the right vertebral artery and a subsequent infarction of the dorsolateral aspect of the right medulla.\n\n ## Figures\n\n **Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 1.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 373030,
"choiceText": "Right-sided lateral pontine stroke (ie, Marie-Foix syndrome)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373031,
"choiceText": "Right-sided lateral medullary stroke (ie, Wallenberg syndrome) ",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373032,
"choiceText": "Right-sided medial medullary stroke (ie, Dejerine syndrome)",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373033,
"choiceText": "Right-sided hemi-medullary stroke (ie, Babinski-Nageotte syndrome)",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373034,
"choiceText": "Left-sided medial medullary stroke",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 107221,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "An Accountant Who Loves Aerobics With Hiccups and Incoordination"
},
{
"authors": "Ajith Goonetilleke, MB BS, FRCP",
"content": [
"The lateral medullary syndrome (also called Wallenberg or posterior inferior cerebellar artery [PICA] syndrome) was first described by Gaspard Vieusseux in 1808. Subsequent clinical (1895) and autopsy (1901) descriptions by Wallenberg led to the syndrome being associated with his name. The loss of pain and temperature sensation on the ipsilateral side of the face and contralateral side of the body is characteristic of this condition. Other clinical features include intractable hiccups, vertigo, Horner syndrome, nystagmus, dysarthria, dysphagia, and ipsilateral ataxia.",
"The blood supply to the medulla is mainly from the vertebral arteries. At the level of the lower medulla, each vertebral artery gives off a variable branch named the posterior inferior cerebellar artery (which may be absent in up to 25% of the population) that supplies the dorsolateral aspects of the medulla. At a higher level, approaching the pontomedullary junction, each vertebral artery also contributes branches to form the anterior spinal artery, which descends over the anterior surface of the medulla and supplies the medial aspects of the medulla.",
"Most cases of Wallenberg syndrome are therefore due to vascular events, whereby the dorsolateral aspect of the medulla may be involved, with sparing of the medial medulla due to an intact anterior spinal artery supply. Definitive pathologic[1] and more recent MRI[2] studies indicate that lateral medullary infarctions occur due to involvement of the vertebral artery in 38% of cases. PICA is involved 14%-24% of the time, and both arteries are involved in 26% of cases. No abnormality is found in either vessel only 12%-19% of the time.",
"Intravenous thrombolysis (IVT) is an acute treatment of the lateral medullary syndrome. Studies show that IVT using recombinant tissue plasminogen activator (tPA) is efficacious for acute ischemic stroke. Dissection is not an absolute contraindication to IVT; however, if a vertebral artery dissection extends intracranially (which is uncommon), caution is advised due to an increased risk for bleeding. The ECASS 3 trial demonstrated benefit of IVT given up to 4.5 hours after symptom onset in ischemic stroke, although certain patients were excluded from this trial and tPA has not received FDA approval for use in this later time frame.[3] Newer, invasive, stent-based techniques exist for stroke and dissection treatment, though they are available at very few centers. If a patient with a nonhemorrhagic stroke is seen beyond the time window for IVT, then aspirin may be given. In this case, vertebral artery dissection was present, anticoagulation with heparin and subsequently warfarin was indicated.",
"The mechanism of the intractable hiccups that is often observed in the lateral medullary syndrome is poorly understood. Occasionally, gabapentin or chlorpromazine is effective. Patients may experience disturbed vision due to persistent nystagmus, and this may be helped by gabapentin or memantine.[4]"
],
"date": "July 02, 2021",
"figures": [],
"markdown": "# An Accountant Who Loves Aerobics With Hiccups and Incoordination\n\n **Authors:** Ajith Goonetilleke, MB BS, FRCP \n **Date:** July 02, 2021\n\n ## Content\n\n The lateral medullary syndrome (also called Wallenberg or posterior inferior cerebellar artery [PICA] syndrome) was first described by Gaspard Vieusseux in 1808. Subsequent clinical (1895) and autopsy (1901) descriptions by Wallenberg led to the syndrome being associated with his name. The loss of pain and temperature sensation on the ipsilateral side of the face and contralateral side of the body is characteristic of this condition. Other clinical features include intractable hiccups, vertigo, Horner syndrome, nystagmus, dysarthria, dysphagia, and ipsilateral ataxia.\nThe blood supply to the medulla is mainly from the vertebral arteries. At the level of the lower medulla, each vertebral artery gives off a variable branch named the posterior inferior cerebellar artery (which may be absent in up to 25% of the population) that supplies the dorsolateral aspects of the medulla. At a higher level, approaching the pontomedullary junction, each vertebral artery also contributes branches to form the anterior spinal artery, which descends over the anterior surface of the medulla and supplies the medial aspects of the medulla.\nMost cases of Wallenberg syndrome are therefore due to vascular events, whereby the dorsolateral aspect of the medulla may be involved, with sparing of the medial medulla due to an intact anterior spinal artery supply. Definitive pathologic[1] and more recent MRI[2] studies indicate that lateral medullary infarctions occur due to involvement of the vertebral artery in 38% of cases. PICA is involved 14%-24% of the time, and both arteries are involved in 26% of cases. No abnormality is found in either vessel only 12%-19% of the time.\nIntravenous thrombolysis (IVT) is an acute treatment of the lateral medullary syndrome. Studies show that IVT using recombinant tissue plasminogen activator (tPA) is efficacious for acute ischemic stroke. Dissection is not an absolute contraindication to IVT; however, if a vertebral artery dissection extends intracranially (which is uncommon), caution is advised due to an increased risk for bleeding. The ECASS 3 trial demonstrated benefit of IVT given up to 4.5 hours after symptom onset in ischemic stroke, although certain patients were excluded from this trial and tPA has not received FDA approval for use in this later time frame.[3] Newer, invasive, stent-based techniques exist for stroke and dissection treatment, though they are available at very few centers. If a patient with a nonhemorrhagic stroke is seen beyond the time window for IVT, then aspirin may be given. In this case, vertebral artery dissection was present, anticoagulation with heparin and subsequently warfarin was indicated.\nThe mechanism of the intractable hiccups that is often observed in the lateral medullary syndrome is poorly understood. Occasionally, gabapentin or chlorpromazine is effective. Patients may experience disturbed vision due to persistent nystagmus, and this may be helped by gabapentin or memantine.[4]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "An Accountant Who Loves Aerobics With Hiccups and Incoordination"
},
{
"authors": "Ajith Goonetilleke, MB BS, FRCP",
"content": [
"Cervical artery dissections (CADs) may involve the carotid or vertebral arteries. They are implicated in 2% of all ischemic strokes but in up to 10%-25% of cases in young and middle-aged patients. CAD may occur spontaneously, and several inheritable connective tissue disorders (eg, Ehlers-Danlos syndrome type IV, Marfan syndrome, autosomal dominant polycystic kidney disease, and osteogenesis imperfecta) are associated with an increased risk. Familial arterial dissections have been associated with generalized lentiginosis, coarctation of the aorta, bicuspid aortic valve, and aortic root dilatation.",
"Traumatic CAD occurs most frequently following motor vehicle accidents. Less violent forms of trauma have also been implicated in CAD, especially cervical spine chiropractic manipulations. Other forms of trauma implicated in CAD include contact sports, yoga, calisthenics, vigorous aerobic exercise, ceiling painting, tonic-clonic seizures, and riding on roller coasters. The mechanism of stroke in CAD is usually thromboembolic due to disruption of normal blood flow in the region of dissection. Partial or total occlusion of the vessel that then results in low blood flow and watershed ischemia is less common. The presence of a CAD may be confirmed by formal cerebral angiography, but less invasive procedures such as MR angiography, CT angiography, or duplex Doppler studies are diagnostic in a high proportion of patients.",
"The patient in this case presented acutely to the ED, had a normal CT head scan, and was within the time window to receive treatment with IVT. She was given 0.9 mg/kg of recombinant tPA intravenously 3 hours and 15 minutes after the onset of her stroke. She remained well, and 24 hours later she was started on oral aspirin therapy. Her intractable hiccups were treated with oral chlorpromazine and resolved after 2 weeks. Because she was experiencing an intrusive burning sensation affecting the left side of her body as well as disturbed vision due to persistent nystagmus, she was started on gabapentin therapy. Both of these symptoms were controlled well with gabapentin at 1800 mg per day. The patient's dysphagia and right-sided limb ataxia improved such that she was able to eat a normal diet and walk within 1 week of hospital admission. The patient was discharged to home and was able to return to her employment as an accountant 10 weeks after her stroke."
],
"date": "July 02, 2021",
"figures": [],
"markdown": "# An Accountant Who Loves Aerobics With Hiccups and Incoordination\n\n **Authors:** Ajith Goonetilleke, MB BS, FRCP \n **Date:** July 02, 2021\n\n ## Content\n\n Cervical artery dissections (CADs) may involve the carotid or vertebral arteries. They are implicated in 2% of all ischemic strokes but in up to 10%-25% of cases in young and middle-aged patients. CAD may occur spontaneously, and several inheritable connective tissue disorders (eg, Ehlers-Danlos syndrome type IV, Marfan syndrome, autosomal dominant polycystic kidney disease, and osteogenesis imperfecta) are associated with an increased risk. Familial arterial dissections have been associated with generalized lentiginosis, coarctation of the aorta, bicuspid aortic valve, and aortic root dilatation.\nTraumatic CAD occurs most frequently following motor vehicle accidents. Less violent forms of trauma have also been implicated in CAD, especially cervical spine chiropractic manipulations. Other forms of trauma implicated in CAD include contact sports, yoga, calisthenics, vigorous aerobic exercise, ceiling painting, tonic-clonic seizures, and riding on roller coasters. The mechanism of stroke in CAD is usually thromboembolic due to disruption of normal blood flow in the region of dissection. Partial or total occlusion of the vessel that then results in low blood flow and watershed ischemia is less common. The presence of a CAD may be confirmed by formal cerebral angiography, but less invasive procedures such as MR angiography, CT angiography, or duplex Doppler studies are diagnostic in a high proportion of patients.\nThe patient in this case presented acutely to the ED, had a normal CT head scan, and was within the time window to receive treatment with IVT. She was given 0.9 mg/kg of recombinant tPA intravenously 3 hours and 15 minutes after the onset of her stroke. She remained well, and 24 hours later she was started on oral aspirin therapy. Her intractable hiccups were treated with oral chlorpromazine and resolved after 2 weeks. Because she was experiencing an intrusive burning sensation affecting the left side of her body as well as disturbed vision due to persistent nystagmus, she was started on gabapentin therapy. Both of these symptoms were controlled well with gabapentin at 1800 mg per day. The patient's dysphagia and right-sided limb ataxia improved such that she was able to eat a normal diet and walk within 1 week of hospital admission. The patient was discharged to home and was able to return to her employment as an accountant 10 weeks after her stroke.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 373035,
"choiceText": "Echocardiography",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373036,
"choiceText": "Genetic testing for Marfan syndrome",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373037,
"choiceText": "MRI head scan and MR angiography",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373038,
"choiceText": "Lumbar puncture",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "MRI studies are considered the noninvasive imaging modality of choice in this situation. CT angiography is also acceptable but will not identify the stroke. The images obtained from the MRI scan of the head may directly detect the pathologic lesion. In the patient presented in the case, the T1-weighted and fluid-attenuated inversion recovery (FLAIR) sequences of the MRI showed a bright signal across the right vertebral artery wall. It also demonstrated the right lateral medullary infarction. These features are highly suggestive of fresh blood and/or recent thrombus throughout the vessel wall seen in arterial dissection. Conditions associated with an arterial dissection may be demonstrated by an echocardiogram and appropriate genetic testing (eg, for Marfan syndrome) but will not help in confirming the presence of an arterial dissection. A lumbar puncture has no role in stroke or dissection evaluation.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 107222,
"questionText": "You are seeing a patient in whom you suspect a brainstem stroke due to a vertebral artery dissection. Which investigation is most appropriate after an initial noncontrast CT scan of the head?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 373039,
"choiceText": "Hemiplegia",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373040,
"choiceText": "Contralateral ataxia",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373041,
"choiceText": "Ipsilateral decreased temperature sensation on the face",
"correct": true,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373042,
"choiceText": "Contralateral decreased pinprick sensation on the face",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The loss of pain and temperature sensation on the ipsilateral side of the face and contralateral side of the body is characteristic of Wallenberg syndrome. Other clinical features include intractable hiccups, vertigo, Horner syndrome, nystagmus, dysarthria, dysphagia and ipsilateral ataxia.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 107223,
"questionText": "The patient described above is found to have a vertebral artery dissection and stroke with Wallenberg syndrome. Which symptom or sign would you expect to find in this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "An Accountant Who Loves Aerobics With Hiccups and Incoordination"
},
{
"authors": "Ajith Goonetilleke, MB BS, FRCP",
"content": [],
"date": "July 02, 2021",
"figures": [],
"markdown": "# An Accountant Who Loves Aerobics With Hiccups and Incoordination\n\n **Authors:** Ajith Goonetilleke, MB BS, FRCP \n **Date:** July 02, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 373035,
"choiceText": "Echocardiography",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373036,
"choiceText": "Genetic testing for Marfan syndrome",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373037,
"choiceText": "MRI head scan and MR angiography",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373038,
"choiceText": "Lumbar puncture",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "MRI studies are considered the noninvasive imaging modality of choice in this situation. CT angiography is also acceptable but will not identify the stroke. The images obtained from the MRI scan of the head may directly detect the pathologic lesion. In the patient presented in the case, the T1-weighted and fluid-attenuated inversion recovery (FLAIR) sequences of the MRI showed a bright signal across the right vertebral artery wall. It also demonstrated the right lateral medullary infarction. These features are highly suggestive of fresh blood and/or recent thrombus throughout the vessel wall seen in arterial dissection. Conditions associated with an arterial dissection may be demonstrated by an echocardiogram and appropriate genetic testing (eg, for Marfan syndrome) but will not help in confirming the presence of an arterial dissection. A lumbar puncture has no role in stroke or dissection evaluation.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 107222,
"questionText": "You are seeing a patient in whom you suspect a brainstem stroke due to a vertebral artery dissection. Which investigation is most appropriate after an initial noncontrast CT scan of the head?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 373039,
"choiceText": "Hemiplegia",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373040,
"choiceText": "Contralateral ataxia",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373041,
"choiceText": "Ipsilateral decreased temperature sensation on the face",
"correct": true,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373042,
"choiceText": "Contralateral decreased pinprick sensation on the face",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The loss of pain and temperature sensation on the ipsilateral side of the face and contralateral side of the body is characteristic of Wallenberg syndrome. Other clinical features include intractable hiccups, vertigo, Horner syndrome, nystagmus, dysarthria, dysphagia and ipsilateral ataxia.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 107223,
"questionText": "The patient described above is found to have a vertebral artery dissection and stroke with Wallenberg syndrome. Which symptom or sign would you expect to find in this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "An Accountant Who Loves Aerobics With Hiccups and Incoordination"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 373030,
"choiceText": "Right-sided lateral pontine stroke (ie, Marie-Foix syndrome)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373031,
"choiceText": "Right-sided lateral medullary stroke (ie, Wallenberg syndrome) ",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373032,
"choiceText": "Right-sided medial medullary stroke (ie, Dejerine syndrome)",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373033,
"choiceText": "Right-sided hemi-medullary stroke (ie, Babinski-Nageotte syndrome)",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373034,
"choiceText": "Left-sided medial medullary stroke",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 107221,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 373035,
"choiceText": "Echocardiography",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373036,
"choiceText": "Genetic testing for Marfan syndrome",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373037,
"choiceText": "MRI head scan and MR angiography",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373038,
"choiceText": "Lumbar puncture",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "MRI studies are considered the noninvasive imaging modality of choice in this situation. CT angiography is also acceptable but will not identify the stroke. The images obtained from the MRI scan of the head may directly detect the pathologic lesion. In the patient presented in the case, the T1-weighted and fluid-attenuated inversion recovery (FLAIR) sequences of the MRI showed a bright signal across the right vertebral artery wall. It also demonstrated the right lateral medullary infarction. These features are highly suggestive of fresh blood and/or recent thrombus throughout the vessel wall seen in arterial dissection. Conditions associated with an arterial dissection may be demonstrated by an echocardiogram and appropriate genetic testing (eg, for Marfan syndrome) but will not help in confirming the presence of an arterial dissection. A lumbar puncture has no role in stroke or dissection evaluation.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 107222,
"questionText": "You are seeing a patient in whom you suspect a brainstem stroke due to a vertebral artery dissection. Which investigation is most appropriate after an initial noncontrast CT scan of the head?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 373039,
"choiceText": "Hemiplegia",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373040,
"choiceText": "Contralateral ataxia",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373041,
"choiceText": "Ipsilateral decreased temperature sensation on the face",
"correct": true,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 373042,
"choiceText": "Contralateral decreased pinprick sensation on the face",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The loss of pain and temperature sensation on the ipsilateral side of the face and contralateral side of the body is characteristic of Wallenberg syndrome. Other clinical features include intractable hiccups, vertigo, Horner syndrome, nystagmus, dysarthria, dysphagia and ipsilateral ataxia.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 107223,
"questionText": "The patient described above is found to have a vertebral artery dissection and stroke with Wallenberg syndrome. Which symptom or sign would you expect to find in this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
855224 | /viewarticle/855224 | [
{
"authors": "Jun H. Lee, MD; Marc D. Basson, MD, PhD",
"content": [
"Editor's Note:\n\n\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.",
"A 66-year-old woman with a history of factor V Leiden thrombophilia presents to the emergency department (ED) with deep venous thrombosis (DVT) after a 6-hour plane flight within the continental United States. During evaluation, she is found to be mildly anemic. Upon further discussion, she reports her bowel movements have increased from once daily to two to three times daily and have become slightly looser than normal over the past month. She also notes that in the past 2 weeks, her abdomen has felt \"bloated and hard.\" She did not notice blood or mucus in her stool and denies pelvic or rectal pain, change in the stool caliber, recent weight loss, regular consumption of aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs), or any history of stomach ulcers.",
"The patient is an ex-smoker who is fit for her age and enjoys regular aerobic exercise. She lives alone and has two grown children who live overseas; however, she has not recently traveled abroad. She eats balanced meals, with regular consumption of red meat and vegetables. She takes no regular medications and has never had surgery. She has not been recently ill and has no history of recent antibiotic use. No family history of bowel cancer is noted; one of her daughters was diagnosed with ulcerative colitis as a teenager."
],
"date": "June 29, 2021",
"figures": [],
"markdown": "# A Woman With DVT After a Flight, Anemia, and Bowel Changes\n\n **Authors:** Jun H. Lee, MD; Marc D. Basson, MD, PhD \n **Date:** June 29, 2021\n\n ## Content\n\n Editor's Note:\n\n\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.\nA 66-year-old woman with a history of factor V Leiden thrombophilia presents to the emergency department (ED) with deep venous thrombosis (DVT) after a 6-hour plane flight within the continental United States. During evaluation, she is found to be mildly anemic. Upon further discussion, she reports her bowel movements have increased from once daily to two to three times daily and have become slightly looser than normal over the past month. She also notes that in the past 2 weeks, her abdomen has felt \"bloated and hard.\" She did not notice blood or mucus in her stool and denies pelvic or rectal pain, change in the stool caliber, recent weight loss, regular consumption of aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs), or any history of stomach ulcers.\nThe patient is an ex-smoker who is fit for her age and enjoys regular aerobic exercise. She lives alone and has two grown children who live overseas; however, she has not recently traveled abroad. She eats balanced meals, with regular consumption of red meat and vegetables. She takes no regular medications and has never had surgery. She has not been recently ill and has no history of recent antibiotic use. No family history of bowel cancer is noted; one of her daughters was diagnosed with ulcerative colitis as a teenager.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A Woman With DVT After a Flight, Anemia, and Bowel Changes"
},
{
"authors": "Jun H. Lee, MD; Marc D. Basson, MD, PhD",
"content": [
"Upon examination, the patient is a petite woman who appears well-nourished and hydrated. Her heart rate is 71 beats/min, her blood pressure is 131/72 mm Hg, her respiratory rate is 15 breaths/min, and her temperature is 99.0°F (37.2°C). Her conjunctivae are pink, and her extremities are warm and well perfused. No skin lesions or lymphadenopathy are present. No skin changes or lumps are palpable in either breast. Heart sounds are normal, and breath sounds are clear bilaterally.",
"Her abdomen is nondistended and soft to palpation with mild generalized tenderness, without guarding or peritoneal signs or palpable masses. Bowel sounds are normal. Neither obvious blood nor mucus nor a mass is apparent during rectal examination. No perianal skin tags, fissures, fistulae, or abscesses are found.",
"Distal pulses are present throughout.",
"The laboratory test results are as follows:",
"Hemoglobin level: 8 g/dL (reference range, 12-15.5 g/dL)",
"Mean corpuscular volume: 84 fL (reference range, 80-100 fL)",
"Hematocrit level: 25% (reference range, 36% to 48%)",
"Platelet count: 310,000/mcL (reference range, 150,000-400,000/mcL)",
"White blood cell count: 10,700/mcL (reference range, 4,500-11,000/mcL)",
"Ferritin level: 92 ng/mL (reference range, 10-120 ng/mL)",
"C-reactive protein level: 110 mg/dL (reference range, <10 mg/L)",
"Alkaline phosphatase level: 35 U/L (reference range, 44-147 U/L)",
"Albumin level: 3.7 g/dL (reference range, 3.4-5.4 g/dL)",
"Sodium level: 141 mEq/L (reference range, 135-145 mEq/L)",
"Potassium level: 4.6 mEq/L (reference range, 3.6-5.2 mEq/L)",
"Creatinine level: 1 mg/dL (reference range, 0.7-1.2 mg/dL)",
"Urea nitrogen level: 10 mg/dL (reference range, 7-20 mg/dL)",
"Urinalysis is negative for blood, protein, and white blood cells. The specific gravity is 1.012. Stool examination for ova, parasite, and Clostridium difficile toxin are all negative.",
"Colonoscopy shows a continuous edematous, hyperemic, and friable mucosa of a granular pattern in the rectosigmoid (Figure 1). No masses are found. Although this patient did not have surgical resection at this time, a typical gross appearance of disease is seen (Figure 2).",
"Figure 1.",
"Figure 1.",
"Figure 2.",
"Figure 2.",
"Figure 3.",
"Figure 3.",
"Figure 4.",
"Figure 4."
],
"date": "June 29, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/855/224/855224-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/855/224/855224-Thumb2.jpg"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/855/224/855224-Thumb3.png"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/855/224/855224-Thumb4.png"
}
],
"markdown": "# A Woman With DVT After a Flight, Anemia, and Bowel Changes\n\n **Authors:** Jun H. Lee, MD; Marc D. Basson, MD, PhD \n **Date:** June 29, 2021\n\n ## Content\n\n Upon examination, the patient is a petite woman who appears well-nourished and hydrated. Her heart rate is 71 beats/min, her blood pressure is 131/72 mm Hg, her respiratory rate is 15 breaths/min, and her temperature is 99.0°F (37.2°C). Her conjunctivae are pink, and her extremities are warm and well perfused. No skin lesions or lymphadenopathy are present. No skin changes or lumps are palpable in either breast. Heart sounds are normal, and breath sounds are clear bilaterally.\nHer abdomen is nondistended and soft to palpation with mild generalized tenderness, without guarding or peritoneal signs or palpable masses. Bowel sounds are normal. Neither obvious blood nor mucus nor a mass is apparent during rectal examination. No perianal skin tags, fissures, fistulae, or abscesses are found.\nDistal pulses are present throughout.\nThe laboratory test results are as follows:\nHemoglobin level: 8 g/dL (reference range, 12-15.5 g/dL)\nMean corpuscular volume: 84 fL (reference range, 80-100 fL)\nHematocrit level: 25% (reference range, 36% to 48%)\nPlatelet count: 310,000/mcL (reference range, 150,000-400,000/mcL)\nWhite blood cell count: 10,700/mcL (reference range, 4,500-11,000/mcL)\nFerritin level: 92 ng/mL (reference range, 10-120 ng/mL)\nC-reactive protein level: 110 mg/dL (reference range, <10 mg/L)\nAlkaline phosphatase level: 35 U/L (reference range, 44-147 U/L)\nAlbumin level: 3.7 g/dL (reference range, 3.4-5.4 g/dL)\nSodium level: 141 mEq/L (reference range, 135-145 mEq/L)\nPotassium level: 4.6 mEq/L (reference range, 3.6-5.2 mEq/L)\nCreatinine level: 1 mg/dL (reference range, 0.7-1.2 mg/dL)\nUrea nitrogen level: 10 mg/dL (reference range, 7-20 mg/dL)\nUrinalysis is negative for blood, protein, and white blood cells. The specific gravity is 1.012. Stool examination for ova, parasite, and Clostridium difficile toxin are all negative.\nColonoscopy shows a continuous edematous, hyperemic, and friable mucosa of a granular pattern in the rectosigmoid (Figure 1). No masses are found. Although this patient did not have surgical resection at this time, a typical gross appearance of disease is seen (Figure 2).\nFigure 1.\nFigure 1.\nFigure 2.\nFigure 2.\nFigure 3.\nFigure 3.\nFigure 4.\nFigure 4.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 917383,
"choiceText": "Crohn disease",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917385,
"choiceText": "Ischemic colitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917387,
"choiceText": "Pseudomembranous colitis\r\n",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917389,
"choiceText": "Ulcerative colitis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917391,
"choiceText": "Colon cancer",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 289549,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Woman With DVT After a Flight, Anemia, and Bowel Changes"
},
{
"authors": "Jun H. Lee, MD; Marc D. Basson, MD, PhD",
"content": [
"The combination of the history and clinical workup suggests ulcerative colitis (UC) as the most likely diagnosis. UC is the most common inflammatory bowel disease (IBD). It is most prevalent in the developed world, such as Europe and North America, where the incidence ranges from 0.6 to more than 20 cases per 100,000 person years. This means that 1 in 200 people have UC in developed countries. The prevalence of the disease worldwide is 5-500 people per 100,000 person years and rising.[1] UC onset has a bimodal distribution; the first peak occurs in the thirties, and the second peak occurs between 50 and 70 years. Twelve percent of patients present for the first time with symptoms when older than 60 years.[2] No sex-based differences are noted.[1]",
"Smoking has been known to be protective of developing UC.[1] However, greater proportions of elderly patients were ex-smokers compared with their younger counterparts. In contrast, genetic factors seem to play a greater role in the younger UC population, where a stronger family history of UC is noted compared with the elderly patient population.[3]",
"The rectum is involved in 95% of cases. Thus, the commonest presenting complaints are bloody diarrhea with or without mucus, urgency, and tenesmus.[1,4] However, elderly patients more frequently present with bleeding, weight loss, fever, and constipation.[5,6] Extraintestinal involvement is present in 10%-30% of patients. This includes the skin (5%), eye (5%), small and large joints (20%), and the liver (5%).[1,4] Although these manifestations occur later in the disease process, one study showed that more than 30% of patients had one of the extraintestinal abnormalities present at the time of diagnosis.[7] A thorough examination of the patient when suspecting UC as a potential diagnosis is important.",
"Extraintestinal involvement is as follows:",
"Skin: Erythema nodosum, pyoderma gangrenosum",
"Eye: Uveitis, iritis, episcleritis, scleritis",
"Joints: Seronegative arthritis, sacroiliitis",
"Liver: Autoimmune liver disease, primary sclerosing cholangitis"
],
"date": "June 29, 2021",
"figures": [],
"markdown": "# A Woman With DVT After a Flight, Anemia, and Bowel Changes\n\n **Authors:** Jun H. Lee, MD; Marc D. Basson, MD, PhD \n **Date:** June 29, 2021\n\n ## Content\n\n The combination of the history and clinical workup suggests ulcerative colitis (UC) as the most likely diagnosis. UC is the most common inflammatory bowel disease (IBD). It is most prevalent in the developed world, such as Europe and North America, where the incidence ranges from 0.6 to more than 20 cases per 100,000 person years. This means that 1 in 200 people have UC in developed countries. The prevalence of the disease worldwide is 5-500 people per 100,000 person years and rising.[1] UC onset has a bimodal distribution; the first peak occurs in the thirties, and the second peak occurs between 50 and 70 years. Twelve percent of patients present for the first time with symptoms when older than 60 years.[2] No sex-based differences are noted.[1]\nSmoking has been known to be protective of developing UC.[1] However, greater proportions of elderly patients were ex-smokers compared with their younger counterparts. In contrast, genetic factors seem to play a greater role in the younger UC population, where a stronger family history of UC is noted compared with the elderly patient population.[3]\nThe rectum is involved in 95% of cases. Thus, the commonest presenting complaints are bloody diarrhea with or without mucus, urgency, and tenesmus.[1,4] However, elderly patients more frequently present with bleeding, weight loss, fever, and constipation.[5,6] Extraintestinal involvement is present in 10%-30% of patients. This includes the skin (5%), eye (5%), small and large joints (20%), and the liver (5%).[1,4] Although these manifestations occur later in the disease process, one study showed that more than 30% of patients had one of the extraintestinal abnormalities present at the time of diagnosis.[7] A thorough examination of the patient when suspecting UC as a potential diagnosis is important.\nExtraintestinal involvement is as follows:\nSkin: Erythema nodosum, pyoderma gangrenosum\nEye: Uveitis, iritis, episcleritis, scleritis\nJoints: Seronegative arthritis, sacroiliitis\nLiver: Autoimmune liver disease, primary sclerosing cholangitis\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 917383,
"choiceText": "Crohn disease",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917385,
"choiceText": "Ischemic colitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917387,
"choiceText": "Pseudomembranous colitis\r\n",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917389,
"choiceText": "Ulcerative colitis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917391,
"choiceText": "Colon cancer",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 289549,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Woman With DVT After a Flight, Anemia, and Bowel Changes"
},
{
"authors": "Jun H. Lee, MD; Marc D. Basson, MD, PhD",
"content": [
"Endoscopy and biopsy is the criterion standard for diagnosing UC. Colonoscopy is more often used because it provides a more thorough view of the whole colon. The gross appearance on endoscopy and histology is used to differentiate between UC and other types of colitis.[4] Still, differentiating or even confirming a diagnosis of IBD is difficult. One study showed that more than 40% of people who were initially diagnosed with indeterminate colitis were found to have UC later on.[8] In that study, 9% of patients initially diagnosed with UC or Crohn disease (CD) had their diagnosis changed, and about 5% of people initially diagnosed with UC were rediagnosed with CD.[8] Vigilance for any changes in symptoms or signs that may warrant re-evaluation of the patient is important.",
"Key points to differentiate between different causes of colitis are as follows:",
"UC: Continuous inflammation extending proximally from rectum, erythematous, friable, granular appearance, shallow ulcerations, mucosal or submucosal involvement only, crypt abscesses, lymphocytes in lamina propria; most always involves rectum; varying severity of diarrhea",
"CD: Skip lesions, cobblestone appearance, granulomas, transmural inflammation; rectum less commonly involved, can involve any part of the gastrointestinal tract; perianal disease; abdominal pain common; diarrhea less severe",
"Ischemic colitis: Acute onset, petechial hemorrhage within areas of pallor, dusky, mucosal fibrosis, crypt atrophy; elderly patients; vascular disease; often painful",
"Infectious colitis: Acute onset, mucosal erosions, positive serology and stool examination; travel history; food poisoning",
"Pseudomembranous colitis: Multiple yellow mushroom-like plaques; recent antibiotic use; C difficile toxin-positive stool",
"Efforts have been made to determine if serologic markers can be used to differentiate between UC and CD. Determinations of perinuclear antineutrophilic cytoplasmic antibodies and anti-Saccharomyces cerevisiae antibodies together were specific but not sensitive for diagnosing UC.[9] Thus, no validated blood tests can facilitate the diagnosis of UC at this time.",
"The histologic results and the gross appearance within the colon in this patient's case correspond best with UC. The continuous nature of the lesion with a granular pattern and crypt abscesses are textbook diagnostic criteria for UC. Although this patient has a background of thrombophilia and was admitted with a DVT, ischemic colitis is more commonly due to arterial blockage rather than venous thrombosis. The thrombotic episode may have been secondary to the ongoing inflammatory state as patients with IBD are at higher risk of developing a thrombotic episode.[10] She also does not have a history of vasculopathy or signs of dehydration, as her blood urea nitrogen/creatinine ratio and urine-specific gravity are normal. Thus, ischemic colitis is less likely in this case. Infectious or pseudomembranous colitis are also less likely because of the negative stool test and lack of recent antibiotic use or trip abroad in her history. Although differentiating between UC and CD is difficult with history and examination alone, perianal disease is more commonly seen in patients with CD, which makes the diagnosis of CD less likely here. Lastly, colon cancer is unlikely in this case due to the shorter history of presentation and no associated weight loss or palpable mass."
],
"date": "June 29, 2021",
"figures": [],
"markdown": "# A Woman With DVT After a Flight, Anemia, and Bowel Changes\n\n **Authors:** Jun H. Lee, MD; Marc D. Basson, MD, PhD \n **Date:** June 29, 2021\n\n ## Content\n\n Endoscopy and biopsy is the criterion standard for diagnosing UC. Colonoscopy is more often used because it provides a more thorough view of the whole colon. The gross appearance on endoscopy and histology is used to differentiate between UC and other types of colitis.[4] Still, differentiating or even confirming a diagnosis of IBD is difficult. One study showed that more than 40% of people who were initially diagnosed with indeterminate colitis were found to have UC later on.[8] In that study, 9% of patients initially diagnosed with UC or Crohn disease (CD) had their diagnosis changed, and about 5% of people initially diagnosed with UC were rediagnosed with CD.[8] Vigilance for any changes in symptoms or signs that may warrant re-evaluation of the patient is important.\nKey points to differentiate between different causes of colitis are as follows:\nUC: Continuous inflammation extending proximally from rectum, erythematous, friable, granular appearance, shallow ulcerations, mucosal or submucosal involvement only, crypt abscesses, lymphocytes in lamina propria; most always involves rectum; varying severity of diarrhea\nCD: Skip lesions, cobblestone appearance, granulomas, transmural inflammation; rectum less commonly involved, can involve any part of the gastrointestinal tract; perianal disease; abdominal pain common; diarrhea less severe\nIschemic colitis: Acute onset, petechial hemorrhage within areas of pallor, dusky, mucosal fibrosis, crypt atrophy; elderly patients; vascular disease; often painful\nInfectious colitis: Acute onset, mucosal erosions, positive serology and stool examination; travel history; food poisoning\nPseudomembranous colitis: Multiple yellow mushroom-like plaques; recent antibiotic use; C difficile toxin-positive stool\nEfforts have been made to determine if serologic markers can be used to differentiate between UC and CD. Determinations of perinuclear antineutrophilic cytoplasmic antibodies and anti-Saccharomyces cerevisiae antibodies together were specific but not sensitive for diagnosing UC.[9] Thus, no validated blood tests can facilitate the diagnosis of UC at this time.\nThe histologic results and the gross appearance within the colon in this patient's case correspond best with UC. The continuous nature of the lesion with a granular pattern and crypt abscesses are textbook diagnostic criteria for UC. Although this patient has a background of thrombophilia and was admitted with a DVT, ischemic colitis is more commonly due to arterial blockage rather than venous thrombosis. The thrombotic episode may have been secondary to the ongoing inflammatory state as patients with IBD are at higher risk of developing a thrombotic episode.[10] She also does not have a history of vasculopathy or signs of dehydration, as her blood urea nitrogen/creatinine ratio and urine-specific gravity are normal. Thus, ischemic colitis is less likely in this case. Infectious or pseudomembranous colitis are also less likely because of the negative stool test and lack of recent antibiotic use or trip abroad in her history. Although differentiating between UC and CD is difficult with history and examination alone, perianal disease is more commonly seen in patients with CD, which makes the diagnosis of CD less likely here. Lastly, colon cancer is unlikely in this case due to the shorter history of presentation and no associated weight loss or palpable mass.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A Woman With DVT After a Flight, Anemia, and Bowel Changes"
},
{
"authors": "Jun H. Lee, MD; Marc D. Basson, MD, PhD",
"content": [
"The location of the lesion is important as it helps to determine the best route of administration for therapeutic intervention in patients with UC. Lesions are found in the rectum (proctitis) in 30%-35% of patients, extend up to the splenic flexure (left-sided colitis) in 30%-45% of patients, and involve the whole colon (pancolitis) in 20%-25% of patients.[11,12] In addition, the severity of the disease also plays a role in choosing the right treatment.",
"Classification is as follows:",
"Mild: <4 stools/day, no systemic signs of toxicity, normal erythrocyte sedimentation rate (ESR)",
"Moderate: >4 stools/day, minimal signs of toxicity",
"Severe: > 6 stools/day, signs of toxicity (eg, fever, increased blood pressure), increased ESR",
"Table 1. Management According to Severity and Site of Disease",
"5-ASA = 5-aminosalicylic acid; TNF = tumor necrosis factor; IV = intravenous. Data from Kornbluth A, et al.[13]",
"A newer formulation of mesalazine, which has replaced sulfasalazine as the mainstay of treatment for IBD, reaches the commonly affected left colon better than previous formulations. It has been engineered so that the drug does not get absorbed until it reaches the left colon. Furthermore, because the compound is released slowly over 24 hours, patients only have to take the drug once a day, increasing compliance with the medication regimen.[15]",
"Unlike what was observed in the past, recent studies have shown that elderly patients are more likely to be in clinical remission and successfully tapered off of steroids within the first year. This may reflect a relative decrease in immunocompetence with age. As the immune system weakens, the overall cell-mediated immune response declines, which makes elderly patients more susceptible to developing UC. However, the relatively immunodeficient state leads to aberrant immune response that normally leads to flare ups, ultimately facilitating more frequent and stable clinical remission than observed in younger cohorts who are able to mount a full immune response.[3]",
"Additional studies on the pathogenesis of UC suggest that enteric microbiota dysbiosis may contribute to the development of the disease. The presence of normal pathogens within the gut is disrupted, which, in turn, prevents these organisms from protecting against nonresident pathogens. This may lead to the development of IBD. Some researchers have proposed replacing fecal microbiota from a healthy donor as a form of treatment. So far, the results of fecal transplantation are mixed and require further testing.[16]",
"When the patient does not respond to medical treatment, then surgery is required. Unlike in CD, surgery is curative for UC. Surgeons most often perform a proctocolectomy with ileal pouch anal anastomosis, although very ill patients may receive lesser procedures, including proctocolectomy with ileostomy or even total abdominal colectomy with ileostomy, leaving the rectal stump behind in the pelvis.[1,4,13] Surgery is more commonly used as a first-line treatment for complications secondary to UC, such as fulminant colitis, toxic megacolon, strictures, or colon cancer. Although all are potentially quite serious, guidelines are set up specifically to monitor for colonic dysplasia. The risk for colon cancer increases up to 30% after 30 years of disease. Early onset, greater extent of disease, and family history of colon cancer all increase the risk. Current guidelines recommend annual colonoscopy 8 years from the time of diagnosis and every 1-3 years thereafter, depending on the findings.[4,13] However, it is not certain that screening actually improves survival rates.[17]",
"The patient in this case was treated with oral mesalazine, to which she responded well, and she went into remission without the need for steroid treatment."
],
"date": "June 29, 2021",
"figures": [],
"markdown": "# A Woman With DVT After a Flight, Anemia, and Bowel Changes\n\n **Authors:** Jun H. Lee, MD; Marc D. Basson, MD, PhD \n **Date:** June 29, 2021\n\n ## Content\n\n The location of the lesion is important as it helps to determine the best route of administration for therapeutic intervention in patients with UC. Lesions are found in the rectum (proctitis) in 30%-35% of patients, extend up to the splenic flexure (left-sided colitis) in 30%-45% of patients, and involve the whole colon (pancolitis) in 20%-25% of patients.[11,12] In addition, the severity of the disease also plays a role in choosing the right treatment.\nClassification is as follows:\nMild: <4 stools/day, no systemic signs of toxicity, normal erythrocyte sedimentation rate (ESR)\nModerate: >4 stools/day, minimal signs of toxicity\nSevere: > 6 stools/day, signs of toxicity (eg, fever, increased blood pressure), increased ESR\nTable 1. Management According to Severity and Site of Disease\n5-ASA = 5-aminosalicylic acid; TNF = tumor necrosis factor; IV = intravenous. Data from Kornbluth A, et al.[13]\nA newer formulation of mesalazine, which has replaced sulfasalazine as the mainstay of treatment for IBD, reaches the commonly affected left colon better than previous formulations. It has been engineered so that the drug does not get absorbed until it reaches the left colon. Furthermore, because the compound is released slowly over 24 hours, patients only have to take the drug once a day, increasing compliance with the medication regimen.[15]\nUnlike what was observed in the past, recent studies have shown that elderly patients are more likely to be in clinical remission and successfully tapered off of steroids within the first year. This may reflect a relative decrease in immunocompetence with age. As the immune system weakens, the overall cell-mediated immune response declines, which makes elderly patients more susceptible to developing UC. However, the relatively immunodeficient state leads to aberrant immune response that normally leads to flare ups, ultimately facilitating more frequent and stable clinical remission than observed in younger cohorts who are able to mount a full immune response.[3]\nAdditional studies on the pathogenesis of UC suggest that enteric microbiota dysbiosis may contribute to the development of the disease. The presence of normal pathogens within the gut is disrupted, which, in turn, prevents these organisms from protecting against nonresident pathogens. This may lead to the development of IBD. Some researchers have proposed replacing fecal microbiota from a healthy donor as a form of treatment. So far, the results of fecal transplantation are mixed and require further testing.[16]\nWhen the patient does not respond to medical treatment, then surgery is required. Unlike in CD, surgery is curative for UC. Surgeons most often perform a proctocolectomy with ileal pouch anal anastomosis, although very ill patients may receive lesser procedures, including proctocolectomy with ileostomy or even total abdominal colectomy with ileostomy, leaving the rectal stump behind in the pelvis.[1,4,13] Surgery is more commonly used as a first-line treatment for complications secondary to UC, such as fulminant colitis, toxic megacolon, strictures, or colon cancer. Although all are potentially quite serious, guidelines are set up specifically to monitor for colonic dysplasia. The risk for colon cancer increases up to 30% after 30 years of disease. Early onset, greater extent of disease, and family history of colon cancer all increase the risk. Current guidelines recommend annual colonoscopy 8 years from the time of diagnosis and every 1-3 years thereafter, depending on the findings.[4,13] However, it is not certain that screening actually improves survival rates.[17]\nThe patient in this case was treated with oral mesalazine, to which she responded well, and she went into remission without the need for steroid treatment.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 917393,
"choiceText": "Oral 5-ASA only",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917395,
"choiceText": "Oral steroids only",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917397,
"choiceText": "Oral 5-ASA and 5-ASA suppository combination\r\n",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917399,
"choiceText": "Azathioprine",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nPatients with proctitis or left-sided colitis who do not respond to 5-ASA suppository alone should try a combination of both oral and suppository forms of 5-ASA before adding oral steroids or azathioprine, which are more aggressive treatments.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 289551,
"questionText": "A 25-year-old man with proctitis has been treated with 5-aminosalicylic acid (5-ASA) suppository alone without relief from his symptoms. Which should be the next step?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 917401,
"choiceText": "2 years",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917403,
"choiceText": "5-10 years",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917405,
"choiceText": "> 10 years\r\n\r\n",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917407,
"choiceText": "Colonoscopy for screening is unnecessary because she is in remission",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "An increased risk for colon cancer is present in patients with UC. Current guidelines recommend annual colonoscopy 8 years from the time of diagnosis and every 1-3 years thereafter, depending on the findings. ",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 289553,
"questionText": "A 45-year-old woman was diagnosed with UC when she was 39 years old. She has responded well to her treatment and has been in remission for years. When should she have a colonoscopy to screen for colon cancer?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Woman With DVT After a Flight, Anemia, and Bowel Changes"
},
{
"authors": "Jun H. Lee, MD; Marc D. Basson, MD, PhD",
"content": [],
"date": "June 29, 2021",
"figures": [],
"markdown": "# A Woman With DVT After a Flight, Anemia, and Bowel Changes\n\n **Authors:** Jun H. Lee, MD; Marc D. Basson, MD, PhD \n **Date:** June 29, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 917393,
"choiceText": "Oral 5-ASA only",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917395,
"choiceText": "Oral steroids only",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917397,
"choiceText": "Oral 5-ASA and 5-ASA suppository combination\r\n",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917399,
"choiceText": "Azathioprine",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nPatients with proctitis or left-sided colitis who do not respond to 5-ASA suppository alone should try a combination of both oral and suppository forms of 5-ASA before adding oral steroids or azathioprine, which are more aggressive treatments.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 289551,
"questionText": "A 25-year-old man with proctitis has been treated with 5-aminosalicylic acid (5-ASA) suppository alone without relief from his symptoms. Which should be the next step?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 917401,
"choiceText": "2 years",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917403,
"choiceText": "5-10 years",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917405,
"choiceText": "> 10 years\r\n\r\n",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917407,
"choiceText": "Colonoscopy for screening is unnecessary because she is in remission",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "An increased risk for colon cancer is present in patients with UC. Current guidelines recommend annual colonoscopy 8 years from the time of diagnosis and every 1-3 years thereafter, depending on the findings. ",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 289553,
"questionText": "A 45-year-old woman was diagnosed with UC when she was 39 years old. She has responded well to her treatment and has been in remission for years. When should she have a colonoscopy to screen for colon cancer?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Woman With DVT After a Flight, Anemia, and Bowel Changes"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 917383,
"choiceText": "Crohn disease",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917385,
"choiceText": "Ischemic colitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917387,
"choiceText": "Pseudomembranous colitis\r\n",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917389,
"choiceText": "Ulcerative colitis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917391,
"choiceText": "Colon cancer",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 289549,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 917393,
"choiceText": "Oral 5-ASA only",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917395,
"choiceText": "Oral steroids only",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917397,
"choiceText": "Oral 5-ASA and 5-ASA suppository combination\r\n",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917399,
"choiceText": "Azathioprine",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nPatients with proctitis or left-sided colitis who do not respond to 5-ASA suppository alone should try a combination of both oral and suppository forms of 5-ASA before adding oral steroids or azathioprine, which are more aggressive treatments.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 289551,
"questionText": "A 25-year-old man with proctitis has been treated with 5-aminosalicylic acid (5-ASA) suppository alone without relief from his symptoms. Which should be the next step?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 917401,
"choiceText": "2 years",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917403,
"choiceText": "5-10 years",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917405,
"choiceText": "> 10 years\r\n\r\n",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 917407,
"choiceText": "Colonoscopy for screening is unnecessary because she is in remission",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "An increased risk for colon cancer is present in patients with UC. Current guidelines recommend annual colonoscopy 8 years from the time of diagnosis and every 1-3 years thereafter, depending on the findings. ",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 289553,
"questionText": "A 45-year-old woman was diagnosed with UC when she was 39 years old. She has responded well to her treatment and has been in remission for years. When should she have a colonoscopy to screen for colon cancer?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
857130 | /viewarticle/857130 | [
{
"authors": "Ingrid Chen, MD; Dieu-Thu Nguyen-Khoa, MD",
"content": [
"Editor's Note:",
"The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.",
"An 18-year-old with no significant medical history presents to the emergency department with sudden-onset chest pain that awakened him from sleep at 4 AM. The pain is located in the midsubsternal region and radiates to his neck. The patient describes it as a sharp pain; when asked to rate the pain on a scale of increasing severity from 1 to 10, he states that it is an 8. The pain worsens with inspiration and is associated with shortness of breath.",
"The patient denies having any fevers, chills, cough, hemoptysis, nausea, or vomiting. He has not had any recent trauma or surgeries. The patient has an 8–pack-year history of smoking cigarettes. He describes occasional marijuana use and remote experimentation with inhaled methamphetamines. He states that he does not use alcohol. He is not currently taking any medications and does not have any known allergies to medications."
],
"date": "June 11, 2021",
"figures": [],
"markdown": "# A Marijuana User With Sudden Chest Pain Radiating to His Neck\n\n **Authors:** Ingrid Chen, MD; Dieu-Thu Nguyen-Khoa, MD \n **Date:** June 11, 2021\n\n ## Content\n\n Editor's Note:\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.\nAn 18-year-old with no significant medical history presents to the emergency department with sudden-onset chest pain that awakened him from sleep at 4 AM. The pain is located in the midsubsternal region and radiates to his neck. The patient describes it as a sharp pain; when asked to rate the pain on a scale of increasing severity from 1 to 10, he states that it is an 8. The pain worsens with inspiration and is associated with shortness of breath.\nThe patient denies having any fevers, chills, cough, hemoptysis, nausea, or vomiting. He has not had any recent trauma or surgeries. The patient has an 8–pack-year history of smoking cigarettes. He describes occasional marijuana use and remote experimentation with inhaled methamphetamines. He states that he does not use alcohol. He is not currently taking any medications and does not have any known allergies to medications.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A Marijuana User With Sudden Chest Pain Radiating to His Neck"
},
{
"authors": "Ingrid Chen, MD; Dieu-Thu Nguyen-Khoa, MD",
"content": [
"Upon physical examination, the patient is noted to be a well-developed, well-nourished male in no acute distress. He does not appear to be tachypneic or cyanotic. Vital signs show a temperature of 98.1°F (36.7°C), a blood pressure of 94/58 mm Hg, a heart rate of 67 beats/min, a respiratory rate of 20 breaths/min, and an oxygen saturation of 95% while breathing room air.",
"No jugular venous distention is noted, and the patient has a normal respiratory effort. The lungs are clear to auscultation bilaterally, without any wheezes, rales, or rhonchi. The heart examination reveals a regular rate and rhythm, with normal S1 and S2 heart sounds and no murmurs, rubs, or gallops. The abdomen is soft, nontender, and nondistended. His extremities do not exhibit any clubbing, cyanosis, or edema. No subcutaneous crepitus is appreciated on examination of the skin.",
"The initial laboratory findings show the following:",
"White blood cell count: 11 × 103 cells/μL (reference range, 3.8-10.9 × 103 cells/μL), with neutrophils at 73.9% (reference range, 41.8%-77%)",
"Hemoglobin level: 15.1 g/dL (normal range, 13.6-17.3 g/dL)",
"Hematocrit: 44% (reference range, 39.8%-50.7%)",
"Platelet count: 263 × 103 cells/μL (reference range, 141-401 × 103 cells/μL)",
"Basic metabolic panel findings are normal. Urine toxicology screen results are negative. The erythrocyte sedimentation rate is 5 mm/h (reference range, < 15 mm/h). An ECG is obtained (not shown here), which reveals a normal sinus rhythm with a heart rate of 55 beats/min and no ST-segment or T-wave abnormalities.",
"Plain chest radiographs are obtained (Figures 1 and 2).",
"Figure 1.",
"Figure 1.",
"Figure 2.",
"Figure 2."
],
"date": "June 11, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/857/130/857130-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/857/130/857130-Thumb2.png"
}
],
"markdown": "# A Marijuana User With Sudden Chest Pain Radiating to His Neck\n\n **Authors:** Ingrid Chen, MD; Dieu-Thu Nguyen-Khoa, MD \n **Date:** June 11, 2021\n\n ## Content\n\n Upon physical examination, the patient is noted to be a well-developed, well-nourished male in no acute distress. He does not appear to be tachypneic or cyanotic. Vital signs show a temperature of 98.1°F (36.7°C), a blood pressure of 94/58 mm Hg, a heart rate of 67 beats/min, a respiratory rate of 20 breaths/min, and an oxygen saturation of 95% while breathing room air.\nNo jugular venous distention is noted, and the patient has a normal respiratory effort. The lungs are clear to auscultation bilaterally, without any wheezes, rales, or rhonchi. The heart examination reveals a regular rate and rhythm, with normal S1 and S2 heart sounds and no murmurs, rubs, or gallops. The abdomen is soft, nontender, and nondistended. His extremities do not exhibit any clubbing, cyanosis, or edema. No subcutaneous crepitus is appreciated on examination of the skin.\nThe initial laboratory findings show the following:\nWhite blood cell count: 11 × 103 cells/μL (reference range, 3.8-10.9 × 103 cells/μL), with neutrophils at 73.9% (reference range, 41.8%-77%)\nHemoglobin level: 15.1 g/dL (normal range, 13.6-17.3 g/dL)\nHematocrit: 44% (reference range, 39.8%-50.7%)\nPlatelet count: 263 × 103 cells/μL (reference range, 141-401 × 103 cells/μL)\nBasic metabolic panel findings are normal. Urine toxicology screen results are negative. The erythrocyte sedimentation rate is 5 mm/h (reference range, < 15 mm/h). An ECG is obtained (not shown here), which reveals a normal sinus rhythm with a heart rate of 55 beats/min and no ST-segment or T-wave abnormalities.\nPlain chest radiographs are obtained (Figures 1 and 2).\nFigure 1.\nFigure 1.\nFigure 2.\nFigure 2.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 934685,
"choiceText": "Pulmonary embolism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934687,
"choiceText": "Pneumomediastinum",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934689,
"choiceText": "Aortic dissection",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934691,
"choiceText": "Pericarditis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 295701,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Marijuana User With Sudden Chest Pain Radiating to His Neck"
},
{
"authors": "Ingrid Chen, MD; Dieu-Thu Nguyen-Khoa, MD",
"content": [
"The chest radiograph showed linear and curvilinear radiolucencies in the anterior mediastinum and possibly pericardium suggestive of pneumomediastinum and minimal pneumopericardium. CT of the chest was subsequently obtained, which confirmed the presence of pneumomediastinum (Figures 3 and 4) and pneumopericardium, with air tracking superiorly along the right carotid sheath (not included in the images provided).",
"Figure 3.",
"Figure 3.",
"Figure 4.",
"Figure 4.",
"No evidence of pneumothorax, bullous changes, or bronchopleural fistula was found. The remaining portions of the lungs were normal, with no areas of focal consolidation or pleural effusion.",
"The esophagus and trachea appeared normal. No mediastinal or hilar lymphadenopathy was noted. The vascular and bone structures had no abnormalities.",
"A diagnosis of pneumomediastinum and pneumopericardium was established based on the imaging studies, and the patient was admitted to the hospital for observation.",
"Spontaneous pneumomediastinum is defined as the presence of free air in the mediastinum without any apparent precipitating cause. Secondary pneumomediastinum is caused by certain events, such as trauma, infections in the intrathoracic or oropharyngeal spaces, or disruption of the aerodigestive tract. Spontaneous pneumomediastinum is a rare, usually self-limited disease primarily affecting young men. More than 75% of reported cases occur in males, with a mean age of 20 years.",
"The prevalence of spontaneous pneumomediastinum has not been clearly established because the only published reports available are case studies or small case series. Newcomb and Clarke[1] reported an incidence of 1 in 29,670 emergency department presentations, whereas the figure observed in a study by Macia and colleagues[2] was 1 in 44,511. Other sources have found the incidence of spontaneous pneumomediastinum to be between 1 in 800 and 1 in 42,000 hospital admissions. The incidence of this disease could be underestimated, given that it frequently goes unrecognized. The clinical presentation of spontaneous pneumomediastinum can often be subtle, and the diagnosis is sometimes missed or delayed.[1,2,3,4,5,6,7]"
],
"date": "June 11, 2021",
"figures": [
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/857/130/857130-Thumb3.png"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/857/130/857130-Thumb4.png"
}
],
"markdown": "# A Marijuana User With Sudden Chest Pain Radiating to His Neck\n\n **Authors:** Ingrid Chen, MD; Dieu-Thu Nguyen-Khoa, MD \n **Date:** June 11, 2021\n\n ## Content\n\n The chest radiograph showed linear and curvilinear radiolucencies in the anterior mediastinum and possibly pericardium suggestive of pneumomediastinum and minimal pneumopericardium. CT of the chest was subsequently obtained, which confirmed the presence of pneumomediastinum (Figures 3 and 4) and pneumopericardium, with air tracking superiorly along the right carotid sheath (not included in the images provided).\nFigure 3.\nFigure 3.\nFigure 4.\nFigure 4.\nNo evidence of pneumothorax, bullous changes, or bronchopleural fistula was found. The remaining portions of the lungs were normal, with no areas of focal consolidation or pleural effusion.\nThe esophagus and trachea appeared normal. No mediastinal or hilar lymphadenopathy was noted. The vascular and bone structures had no abnormalities.\nA diagnosis of pneumomediastinum and pneumopericardium was established based on the imaging studies, and the patient was admitted to the hospital for observation.\nSpontaneous pneumomediastinum is defined as the presence of free air in the mediastinum without any apparent precipitating cause. Secondary pneumomediastinum is caused by certain events, such as trauma, infections in the intrathoracic or oropharyngeal spaces, or disruption of the aerodigestive tract. Spontaneous pneumomediastinum is a rare, usually self-limited disease primarily affecting young men. More than 75% of reported cases occur in males, with a mean age of 20 years.\nThe prevalence of spontaneous pneumomediastinum has not been clearly established because the only published reports available are case studies or small case series. Newcomb and Clarke[1] reported an incidence of 1 in 29,670 emergency department presentations, whereas the figure observed in a study by Macia and colleagues[2] was 1 in 44,511. Other sources have found the incidence of spontaneous pneumomediastinum to be between 1 in 800 and 1 in 42,000 hospital admissions. The incidence of this disease could be underestimated, given that it frequently goes unrecognized. The clinical presentation of spontaneous pneumomediastinum can often be subtle, and the diagnosis is sometimes missed or delayed.[1,2,3,4,5,6,7]\n\n ## Figures\n\n **Figure 3.** \n \n\n**Figure 4.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 934685,
"choiceText": "Pulmonary embolism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934687,
"choiceText": "Pneumomediastinum",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934689,
"choiceText": "Aortic dissection",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934691,
"choiceText": "Pericarditis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 295701,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Marijuana User With Sudden Chest Pain Radiating to His Neck"
},
{
"authors": "Ingrid Chen, MD; Dieu-Thu Nguyen-Khoa, MD",
"content": [
"The most commonly proposed cause of pneumomediastinum is alveolar rupture, which occurs in the presence of elevated intra-alveolar pressure or damage to the alveolar walls. An increased pressure gradient between the intra-alveolar and interstitial spaces leads to air leakage from small alveolar openings and ruptured alveoli into the perivascular spaces, which in turn leads to interstitial emphysema. The pressure gradient then favors dissection of air along the vascular sheaths toward the hilum. Air can then decompress into the subcutaneous tissues and the deep cervical spaces, eventually spreading into the pericardial space and leading to pneumopericardium. Dissection of free air into the pericardial space is a common complication of barotrauma in neonates, but it is rare in adults, in whom the apposition of the pericardial layers is very tight.[1,2,3,7]",
"Various conditions can cause elevated intra-alveolar pressure, including airway obstruction (eg, mucus plugging in an asthmatic person or the presence of a foreign body), mechanical ventilation, blunt trauma, coughing, emesis, or the Valsalva maneuver (eg, during parturition). Certain conditions that can cause damage to the alveolar walls include pneumonitis, emphysema, lung fibrosis, and acute respiratory distress syndrome.[1,2,3,4] More recently, COVID-19 has also been associated with the development of pneumomediastinum.[8,9]",
"To diagnose spontaneous pneumomediastinum, the clinician must rule out causes of secondary pneumomediastinum. This is particularly vital because alternative causes of pneumomediastinum are potentially life-threatening. Determine whether the patient has had recent dental surgery or procedures of the upper digestive tract and evaluate for underlying conditions that can lead to pneumomediastinum, such as gas-producing infections of the head, neck, or abdomen or neoplasms disrupting the mucosal integrity of the esophagus. Esophageal rupture must be ruled out by obtaining an esophagram when indicated. Events or conditions known to precipitate spontaneous pneumomediastinum include vomiting (especially retching), asthma exacerbation, coughing, or physical activity.[1,3,5,7]",
"Pneumomediastinum has also been found to be associated with inhalational drug use. In theory, this is thought to be caused by barotrauma from prolonged forceful breath holding. Cocaine and marijuana users perform a Valsalva-type maneuver during deep inhalation of the respective substance (often through a water pipe), leading to an increase in intra-alveolar pressure and subsequent alveolar rupture. No evidence suggests a direct pharmacologic effect of illicit drugs on spontaneous pneumomediastinum.[1,2,3,4]",
"Patients with spontaneous pneumomediastinum most commonly present with chest pain, dyspnea, and neck pain or discomfort. Chest pain is the most common symptom; it typically presents as an acute, retrosternal, pleuritic pain that may radiate to the neck, back, or shoulders. Other, less common symptoms include odynophagia, dysphagia, dysphonia, cough, back pain, or abdominal pain. Physical examination may reveal signs of respiratory distress; subcutaneous emphysema; and the Hamman sign, which is pathognomonic for pneumomediastinum.",
"The Hamman sign is crunching, crackling, or bubbling sounds that are synchronous with the heartbeat on auscultation; this signifies air in the mediastinum. The prevalence of the Hamman sign is highly variable; however, subcutaneous emphysema, mainly at the neck, is a more frequent finding that is seen in 40%-100% of cases.[1,2,3,4,5,7]",
"The differential diagnosis of spontaneous pneumomediastinum is broad and includes musculoskeletal disorders, acute coronary syndrome, pericarditis, pneumothorax, pulmonary embolism, tracheobronchial tree rupture, and Boerhaave syndrome. Tracheobronchial tree rupture and Boerhaave syndrome are potentially life-threatening conditions. Boerhaave syndrome can be ruled out with contrast-enhanced esophagography if it is suspected; whereas suspected tracheobronchial tree rupture can be ruled out with bronchoscopy.[1,2,3]"
],
"date": "June 11, 2021",
"figures": [],
"markdown": "# A Marijuana User With Sudden Chest Pain Radiating to His Neck\n\n **Authors:** Ingrid Chen, MD; Dieu-Thu Nguyen-Khoa, MD \n **Date:** June 11, 2021\n\n ## Content\n\n The most commonly proposed cause of pneumomediastinum is alveolar rupture, which occurs in the presence of elevated intra-alveolar pressure or damage to the alveolar walls. An increased pressure gradient between the intra-alveolar and interstitial spaces leads to air leakage from small alveolar openings and ruptured alveoli into the perivascular spaces, which in turn leads to interstitial emphysema. The pressure gradient then favors dissection of air along the vascular sheaths toward the hilum. Air can then decompress into the subcutaneous tissues and the deep cervical spaces, eventually spreading into the pericardial space and leading to pneumopericardium. Dissection of free air into the pericardial space is a common complication of barotrauma in neonates, but it is rare in adults, in whom the apposition of the pericardial layers is very tight.[1,2,3,7]\nVarious conditions can cause elevated intra-alveolar pressure, including airway obstruction (eg, mucus plugging in an asthmatic person or the presence of a foreign body), mechanical ventilation, blunt trauma, coughing, emesis, or the Valsalva maneuver (eg, during parturition). Certain conditions that can cause damage to the alveolar walls include pneumonitis, emphysema, lung fibrosis, and acute respiratory distress syndrome.[1,2,3,4] More recently, COVID-19 has also been associated with the development of pneumomediastinum.[8,9]\nTo diagnose spontaneous pneumomediastinum, the clinician must rule out causes of secondary pneumomediastinum. This is particularly vital because alternative causes of pneumomediastinum are potentially life-threatening. Determine whether the patient has had recent dental surgery or procedures of the upper digestive tract and evaluate for underlying conditions that can lead to pneumomediastinum, such as gas-producing infections of the head, neck, or abdomen or neoplasms disrupting the mucosal integrity of the esophagus. Esophageal rupture must be ruled out by obtaining an esophagram when indicated. Events or conditions known to precipitate spontaneous pneumomediastinum include vomiting (especially retching), asthma exacerbation, coughing, or physical activity.[1,3,5,7]\nPneumomediastinum has also been found to be associated with inhalational drug use. In theory, this is thought to be caused by barotrauma from prolonged forceful breath holding. Cocaine and marijuana users perform a Valsalva-type maneuver during deep inhalation of the respective substance (often through a water pipe), leading to an increase in intra-alveolar pressure and subsequent alveolar rupture. No evidence suggests a direct pharmacologic effect of illicit drugs on spontaneous pneumomediastinum.[1,2,3,4]\nPatients with spontaneous pneumomediastinum most commonly present with chest pain, dyspnea, and neck pain or discomfort. Chest pain is the most common symptom; it typically presents as an acute, retrosternal, pleuritic pain that may radiate to the neck, back, or shoulders. Other, less common symptoms include odynophagia, dysphagia, dysphonia, cough, back pain, or abdominal pain. Physical examination may reveal signs of respiratory distress; subcutaneous emphysema; and the Hamman sign, which is pathognomonic for pneumomediastinum.\nThe Hamman sign is crunching, crackling, or bubbling sounds that are synchronous with the heartbeat on auscultation; this signifies air in the mediastinum. The prevalence of the Hamman sign is highly variable; however, subcutaneous emphysema, mainly at the neck, is a more frequent finding that is seen in 40%-100% of cases.[1,2,3,4,5,7]\nThe differential diagnosis of spontaneous pneumomediastinum is broad and includes musculoskeletal disorders, acute coronary syndrome, pericarditis, pneumothorax, pulmonary embolism, tracheobronchial tree rupture, and Boerhaave syndrome. Tracheobronchial tree rupture and Boerhaave syndrome are potentially life-threatening conditions. Boerhaave syndrome can be ruled out with contrast-enhanced esophagography if it is suspected; whereas suspected tracheobronchial tree rupture can be ruled out with bronchoscopy.[1,2,3]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A Marijuana User With Sudden Chest Pain Radiating to His Neck"
},
{
"authors": "Ingrid Chen, MD; Dieu-Thu Nguyen-Khoa, MD",
"content": [
"The diagnosis of pneumomediastinum is confirmed by obtaining posteroanterior and lateral chest radiographs. Posteroanterior chest radiographs typically reveal radiolucency between the left heart border and the mediastinal pleura. A lateral view should always be obtained because, if only a posteroanterior radiograph is taken, the diagnosis is missed in as many as 50% of cases. When air is limited in quantity, the only sign of pneumomediastinum on plain chest radiography may be a radiolucent band (hyperlucency) in the retrosternal area, which can only be seen in the lateral view. As many as 30% of patients with spontaneous pneumomediastinum present with a normal radiograph; therefore, if the clinical suspicion is high but the diagnosis is unclear, CT of the chest can be obtained.[1,2,3]",
"Spontaneous pneumomediastinum is almost always a benign, self-limited condition. The treatment consists of supportive measures, including rest, oxygen, and analgesics. Breathing 100% oxygen helps to enhance reabsorption of the free air by increasing the gradient of nitrogen between the alveoli and the tissues. Antibiotic therapy is not required for spontaneous pneumomediastinum. Patients respond well to supportive treatment, and pain typically resolves within 1-2 days. Follow-up chest radiography should be obtained within 12-24 hours. The chest radiograph findings usually return to normal within 1 week. Significant complications are virtually nonexistent, and most published series have not reported any cases of recurrence.[1,2,3,4,5,7]",
"This patient in this case was admitted to the hospital for observation, and supportive treatment with supplemental oxygen and analgesics was initiated. Findings of an evaluation by an ear, nose, and throat surgeon were normal. In addition, CT of the neck was obtained and was found to be normal. Repeat CT of the chest obtained the day after admission showed no interval progression in the pneumomediastinum and pneumopericardium.",
"The patient's pain and shortness of breath resolved within 24 hours, and he was subsequently discharged to home after a 2-day hospital stay. CT of the chest performed 3 days after discharge showed mild improvement in the pneumomediastinum and resolution of the pneumopericardium (Figures 5 and 6).",
"Figure 5.",
"Figure 5.",
"Figure 6.",
"Figure 6.",
"At the time of discharge, the patient was instructed to refrain from future drug use and smoking, and to avoid air travel or prolonged stays at high altitudes for 1 month. Physical activity was not restricted, except for scuba diving, which he was directed not to do for at least 6 months. These suggestions were based on the theoretical risk for recurrence of spontaneous pneumomediastinum. The actual rate and risk factors for recurrence are not known, so recommendations on avoidance of potential high risk activities must be individualized on the basis of patient factors and known information about the recurrence of pneumothorax."
],
"date": "June 11, 2021",
"figures": [
{
"caption": "Figure 5.",
"image_url": "https://img.medscapestatic.com/article/857/130/857130-Thumb5.png"
},
{
"caption": "Figure 6.",
"image_url": "https://img.medscapestatic.com/article/857/130/857130-Thumb6.png"
}
],
"markdown": "# A Marijuana User With Sudden Chest Pain Radiating to His Neck\n\n **Authors:** Ingrid Chen, MD; Dieu-Thu Nguyen-Khoa, MD \n **Date:** June 11, 2021\n\n ## Content\n\n The diagnosis of pneumomediastinum is confirmed by obtaining posteroanterior and lateral chest radiographs. Posteroanterior chest radiographs typically reveal radiolucency between the left heart border and the mediastinal pleura. A lateral view should always be obtained because, if only a posteroanterior radiograph is taken, the diagnosis is missed in as many as 50% of cases. When air is limited in quantity, the only sign of pneumomediastinum on plain chest radiography may be a radiolucent band (hyperlucency) in the retrosternal area, which can only be seen in the lateral view. As many as 30% of patients with spontaneous pneumomediastinum present with a normal radiograph; therefore, if the clinical suspicion is high but the diagnosis is unclear, CT of the chest can be obtained.[1,2,3]\nSpontaneous pneumomediastinum is almost always a benign, self-limited condition. The treatment consists of supportive measures, including rest, oxygen, and analgesics. Breathing 100% oxygen helps to enhance reabsorption of the free air by increasing the gradient of nitrogen between the alveoli and the tissues. Antibiotic therapy is not required for spontaneous pneumomediastinum. Patients respond well to supportive treatment, and pain typically resolves within 1-2 days. Follow-up chest radiography should be obtained within 12-24 hours. The chest radiograph findings usually return to normal within 1 week. Significant complications are virtually nonexistent, and most published series have not reported any cases of recurrence.[1,2,3,4,5,7]\nThis patient in this case was admitted to the hospital for observation, and supportive treatment with supplemental oxygen and analgesics was initiated. Findings of an evaluation by an ear, nose, and throat surgeon were normal. In addition, CT of the neck was obtained and was found to be normal. Repeat CT of the chest obtained the day after admission showed no interval progression in the pneumomediastinum and pneumopericardium.\nThe patient's pain and shortness of breath resolved within 24 hours, and he was subsequently discharged to home after a 2-day hospital stay. CT of the chest performed 3 days after discharge showed mild improvement in the pneumomediastinum and resolution of the pneumopericardium (Figures 5 and 6).\nFigure 5.\nFigure 5.\nFigure 6.\nFigure 6.\nAt the time of discharge, the patient was instructed to refrain from future drug use and smoking, and to avoid air travel or prolonged stays at high altitudes for 1 month. Physical activity was not restricted, except for scuba diving, which he was directed not to do for at least 6 months. These suggestions were based on the theoretical risk for recurrence of spontaneous pneumomediastinum. The actual rate and risk factors for recurrence are not known, so recommendations on avoidance of potential high risk activities must be individualized on the basis of patient factors and known information about the recurrence of pneumothorax.\n\n ## Figures\n\n **Figure 5.** \n \n\n**Figure 6.** \n \n\n\n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 934693,
"choiceText": "Lateral view",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934695,
"choiceText": "Posteroanterior view",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934697,
"choiceText": "Posteroanterior and lateral views",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934699,
"choiceText": "Oblique view",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934701,
"choiceText": "Anterolateral views\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The diagnosis of pneumomediastinum is confirmed by obtaining posteroanterior and lateral chest radiographs. Posteroanterior chest radiographs typically reveal radiolucency between the left heart border and the mediastinal pleura. A lateral view should always be obtained because if only a posteroanterior radiograph is taken, the diagnosis is missed in as many as 50% of cases.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 295703,
"questionText": "Which of the following views is recommended to establish a diagnosis of pneumomediastinum on chest radiography?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 934703,
"choiceText": "A hypodense line in the mediastinum on posteroanterior chest radiography",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934705,
"choiceText": "Bluish discoloration on the lips of patients with spontaneous pneumomediastinum, resulting from a lack of oxygenation",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934707,
"choiceText": "A gurgling sound coming from a patient's stomach as a result of air escaping from the mediastinum",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934709,
"choiceText": "Crunching, crackling, or bubbling sounds that are synchronous with the heartbeat on auscultation",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934711,
"choiceText": "None of the above\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The Hamman sign is crunching, crackling, or bubbling sounds that are synchronous with the heartbeat on auscultation; this signifies air in the mediastinum. The prevalence of the Hamman sign is highly variable; however, subcutaneous emphysema, mainly at the neck, is a more frequent finding that is seen in 40%-100% of cases.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 295705,
"questionText": "Which of these is the Hamman sign?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Marijuana User With Sudden Chest Pain Radiating to His Neck"
},
{
"authors": "Ingrid Chen, MD; Dieu-Thu Nguyen-Khoa, MD",
"content": [],
"date": "June 11, 2021",
"figures": [],
"markdown": "# A Marijuana User With Sudden Chest Pain Radiating to His Neck\n\n **Authors:** Ingrid Chen, MD; Dieu-Thu Nguyen-Khoa, MD \n **Date:** June 11, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 934693,
"choiceText": "Lateral view",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934695,
"choiceText": "Posteroanterior view",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934697,
"choiceText": "Posteroanterior and lateral views",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934699,
"choiceText": "Oblique view",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934701,
"choiceText": "Anterolateral views\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The diagnosis of pneumomediastinum is confirmed by obtaining posteroanterior and lateral chest radiographs. Posteroanterior chest radiographs typically reveal radiolucency between the left heart border and the mediastinal pleura. A lateral view should always be obtained because if only a posteroanterior radiograph is taken, the diagnosis is missed in as many as 50% of cases.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 295703,
"questionText": "Which of the following views is recommended to establish a diagnosis of pneumomediastinum on chest radiography?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 934703,
"choiceText": "A hypodense line in the mediastinum on posteroanterior chest radiography",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934705,
"choiceText": "Bluish discoloration on the lips of patients with spontaneous pneumomediastinum, resulting from a lack of oxygenation",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934707,
"choiceText": "A gurgling sound coming from a patient's stomach as a result of air escaping from the mediastinum",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934709,
"choiceText": "Crunching, crackling, or bubbling sounds that are synchronous with the heartbeat on auscultation",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934711,
"choiceText": "None of the above\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The Hamman sign is crunching, crackling, or bubbling sounds that are synchronous with the heartbeat on auscultation; this signifies air in the mediastinum. The prevalence of the Hamman sign is highly variable; however, subcutaneous emphysema, mainly at the neck, is a more frequent finding that is seen in 40%-100% of cases.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 295705,
"questionText": "Which of these is the Hamman sign?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Marijuana User With Sudden Chest Pain Radiating to His Neck"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 934685,
"choiceText": "Pulmonary embolism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934687,
"choiceText": "Pneumomediastinum",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934689,
"choiceText": "Aortic dissection",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934691,
"choiceText": "Pericarditis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 295701,
"questionText": "Based only on these findings, which is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 934693,
"choiceText": "Lateral view",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934695,
"choiceText": "Posteroanterior view",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934697,
"choiceText": "Posteroanterior and lateral views",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934699,
"choiceText": "Oblique view",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934701,
"choiceText": "Anterolateral views\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The diagnosis of pneumomediastinum is confirmed by obtaining posteroanterior and lateral chest radiographs. Posteroanterior chest radiographs typically reveal radiolucency between the left heart border and the mediastinal pleura. A lateral view should always be obtained because if only a posteroanterior radiograph is taken, the diagnosis is missed in as many as 50% of cases.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 295703,
"questionText": "Which of the following views is recommended to establish a diagnosis of pneumomediastinum on chest radiography?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 934703,
"choiceText": "A hypodense line in the mediastinum on posteroanterior chest radiography",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934705,
"choiceText": "Bluish discoloration on the lips of patients with spontaneous pneumomediastinum, resulting from a lack of oxygenation",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934707,
"choiceText": "A gurgling sound coming from a patient's stomach as a result of air escaping from the mediastinum",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934709,
"choiceText": "Crunching, crackling, or bubbling sounds that are synchronous with the heartbeat on auscultation",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 934711,
"choiceText": "None of the above\r\n",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The Hamman sign is crunching, crackling, or bubbling sounds that are synchronous with the heartbeat on auscultation; this signifies air in the mediastinum. The prevalence of the Hamman sign is highly variable; however, subcutaneous emphysema, mainly at the neck, is a more frequent finding that is seen in 40%-100% of cases.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 295705,
"questionText": "Which of these is the Hamman sign?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
840963 | /viewarticle/840963 | [
{
"authors": "Eva Nourbakhsh, MD; Kenneth M. Nugent, MD; Rishi Raj, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.",
"A 70-year-old woman was recently treated in the hospital for a right hip fracture, weakness, and chronic atrial fibrillation with a rapid ventricular response. Two days after she was discharged to a long-term care facility, she is readmitted for urinary retention and recurrent tachycardia. In addition, she complains of generalized weakness and midline lower abdominal pain.",
"She denies any previous history of urinary retention as well as experiencing any fever, dysuria, hematuria, vomiting, trouble breathing, or chest pain in association with this presentation. Her medical and surgical history includes a stroke with left hemiparesis, hypertension, atrial fibrillation, epilepsy, and hemiarthroplasty; she is nonambulatory secondary to the stroke.",
"Her medications include atorvastatin, enoxaparin, levetiracetam, metoprolol, omeprazole, and warfarin (7.5 mg daily)."
],
"date": "April 30, 2021",
"figures": [],
"markdown": "# Abdominal Pain, Anemia, and Oliguria in a Distressed Woman\n\n **Authors:** Eva Nourbakhsh, MD; Kenneth M. Nugent, MD; Rishi Raj, MD \n **Date:** April 30, 2021\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.\nA 70-year-old woman was recently treated in the hospital for a right hip fracture, weakness, and chronic atrial fibrillation with a rapid ventricular response. Two days after she was discharged to a long-term care facility, she is readmitted for urinary retention and recurrent tachycardia. In addition, she complains of generalized weakness and midline lower abdominal pain.\nShe denies any previous history of urinary retention as well as experiencing any fever, dysuria, hematuria, vomiting, trouble breathing, or chest pain in association with this presentation. Her medical and surgical history includes a stroke with left hemiparesis, hypertension, atrial fibrillation, epilepsy, and hemiarthroplasty; she is nonambulatory secondary to the stroke.\nHer medications include atorvastatin, enoxaparin, levetiracetam, metoprolol, omeprazole, and warfarin (7.5 mg daily).\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Abdominal Pain, Anemia, and Oliguria in a Distressed Woman"
},
{
"authors": "Eva Nourbakhsh, MD; Kenneth M. Nugent, MD; Rishi Raj, MD",
"content": [
"Upon physical examination, the patient is in distress secondary to her abdominal pain. She is hypotensive, with a blood pressure of 73/45 mm Hg, and tachycardic, with a heart rate of 180 beats/min. No fever is noted (temperature, 98.9°F [37.2°C]). Her oxygen saturation is 97% on 2 L/min. Her head, neck, and pulmonary examination findings are all normal. The heart rate is rapid and periodically irregular, but no jugular venous distention or peripheral edema is detected.",
"She has abdominal wall bruising from enoxaparin injections. The abdomen is firm and diffusely tender to palpation, without rebound or guarding, and hypoactive bowel sounds are noted. On neurologic examination, an unchanged chronic left hemiparesis is found. The rest of the physical examination is unremarkable.",
"A complete blood count and metabolic panel reveal leukocytosis (28.1 kU/L), anemia (hemoglobin level, 7.3 g/dL; hematocrit, 21.1%), hyperkalemia (serum potassium, 5.9 mmol/L), renal insufficiency (creatinine level, 1.6 mg/dL; blood urea nitrogen, 32 mg/dL; estimated glomerular filtration rate, 32 mL/min/1.73 m2), and an anion gap metabolic acidosis (carbon dioxide level, 15 mmol/L; anion gap, 23 mEq/L). Her liver enzymes are mildly elevated, with an alkaline phosphatase level of 126 IU/L, an alanine aminotransferase level of 73 IU/L, and an aspartate aminotransferase level of 129 IU/L.",
"Her prothrombin time is 18.2 sec, correlating with an international normalized ratio of 1.62. The cardiac enzymes include a total creatinine kinase (CK) level of 21 IU/L, CK-MB isoenzyme level of 1.8 ng/mL, and troponin-t level of 0.19 ng/mL.",
"Electrocardiography (ECG) shows atrial fibrillation with a rapid ventricular response but no evidence of acute ischemia. Chest radiography does not reveal any acute disease process. CT scanning of the abdomen and pelvis reveals a large 15 cm x 13 cm hypodense mass posterior to the left rectus abdominis muscle, with dependent hyperdensities and a collapsed inferior vena cava (Figure 1; Figure 2).",
"Figure 1.",
"Figure 1.",
"Figure 2.",
"Figure 2.",
"The patient is immediately placed on a cardiac monitor, and a 500-mL normal saline bolus is administered; slight improvement is seen in both her heart rate and blood pressure. Because of this, medical management is continued rather than emergent cardioversion. A Foley catheter is placed, but no urine output is seen. After a second and third 500-mL bolus, the blood pressure remains low, but the heart rate has dropped to 129 beats/min. A diltiazem drip is initiated for control of her atrial fibrillation.",
"During the first 24 hours of intensive therapy, she receives a total of 4250 mL of normal saline, 3 units of packed red blood cells, and 4 units of fresh frozen plasma. Norepinephrine is started for persistent hypotension despite fluid and blood resuscitation. At this point, the patient's abdomen is noted to be somewhat tense and more painful, so an intra-abdominal pressure (IAP) measurement is performed and is found to be 24 mm Hg. A consultation with the surgery department is ordered, and supportive measures are continued. Six hours later, the IAP has increased to 38 mm Hg."
],
"date": "April 30, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/840/963/840963-thumb-1.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/840/963/840963-thumb-2.jpg"
}
],
"markdown": "# Abdominal Pain, Anemia, and Oliguria in a Distressed Woman\n\n **Authors:** Eva Nourbakhsh, MD; Kenneth M. Nugent, MD; Rishi Raj, MD \n **Date:** April 30, 2021\n\n ## Content\n\n Upon physical examination, the patient is in distress secondary to her abdominal pain. She is hypotensive, with a blood pressure of 73/45 mm Hg, and tachycardic, with a heart rate of 180 beats/min. No fever is noted (temperature, 98.9°F [37.2°C]). Her oxygen saturation is 97% on 2 L/min. Her head, neck, and pulmonary examination findings are all normal. The heart rate is rapid and periodically irregular, but no jugular venous distention or peripheral edema is detected.\nShe has abdominal wall bruising from enoxaparin injections. The abdomen is firm and diffusely tender to palpation, without rebound or guarding, and hypoactive bowel sounds are noted. On neurologic examination, an unchanged chronic left hemiparesis is found. The rest of the physical examination is unremarkable.\nA complete blood count and metabolic panel reveal leukocytosis (28.1 kU/L), anemia (hemoglobin level, 7.3 g/dL; hematocrit, 21.1%), hyperkalemia (serum potassium, 5.9 mmol/L), renal insufficiency (creatinine level, 1.6 mg/dL; blood urea nitrogen, 32 mg/dL; estimated glomerular filtration rate, 32 mL/min/1.73 m2), and an anion gap metabolic acidosis (carbon dioxide level, 15 mmol/L; anion gap, 23 mEq/L). Her liver enzymes are mildly elevated, with an alkaline phosphatase level of 126 IU/L, an alanine aminotransferase level of 73 IU/L, and an aspartate aminotransferase level of 129 IU/L.\nHer prothrombin time is 18.2 sec, correlating with an international normalized ratio of 1.62. The cardiac enzymes include a total creatinine kinase (CK) level of 21 IU/L, CK-MB isoenzyme level of 1.8 ng/mL, and troponin-t level of 0.19 ng/mL.\nElectrocardiography (ECG) shows atrial fibrillation with a rapid ventricular response but no evidence of acute ischemia. Chest radiography does not reveal any acute disease process. CT scanning of the abdomen and pelvis reveals a large 15 cm x 13 cm hypodense mass posterior to the left rectus abdominis muscle, with dependent hyperdensities and a collapsed inferior vena cava (Figure 1; Figure 2).\nFigure 1.\nFigure 1.\nFigure 2.\nFigure 2.\nThe patient is immediately placed on a cardiac monitor, and a 500-mL normal saline bolus is administered; slight improvement is seen in both her heart rate and blood pressure. Because of this, medical management is continued rather than emergent cardioversion. A Foley catheter is placed, but no urine output is seen. After a second and third 500-mL bolus, the blood pressure remains low, but the heart rate has dropped to 129 beats/min. A diltiazem drip is initiated for control of her atrial fibrillation.\nDuring the first 24 hours of intensive therapy, she receives a total of 4250 mL of normal saline, 3 units of packed red blood cells, and 4 units of fresh frozen plasma. Norepinephrine is started for persistent hypotension despite fluid and blood resuscitation. At this point, the patient's abdomen is noted to be somewhat tense and more painful, so an intra-abdominal pressure (IAP) measurement is performed and is found to be 24 mm Hg. A consultation with the surgery department is ordered, and supportive measures are continued. Six hours later, the IAP has increased to 38 mm Hg.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 819545,
"choiceText": "Spontaneous retroperitoneal hematoma",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819547,
"choiceText": "Abdominal compartment syndrome",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819549,
"choiceText": "Abdominal wall abscess",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819551,
"choiceText": "Septic shock",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 257387,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Abdominal Pain, Anemia, and Oliguria in a Distressed Woman"
},
{
"authors": "Eva Nourbakhsh, MD; Kenneth M. Nugent, MD; Rishi Raj, MD",
"content": [
"This patient presented with refractory hypotension, oliguria, metabolic acidosis, and anemia. A CT scan revealed a large abdominal wall hematoma, with collapse of the inferior vena cava. Her bladder pressure was initially high and further increased during a relatively short period of observation. The diagnosis of abdominal compartment syndrome (ACS) was made based on the multiorgan failure, evidence of abdominal wall hematoma secondary to anticoagulants, and increasing IAPs.",
"Compartment syndrome (CS) refers to a fixed compartment that becomes subject to increased pressure, whether from injury or other means, leading to reduced capillary circulation or outright venous collapse followed by ischemia and organ dysfunction. CS occurs most frequently in the extremities, but it may also occur in the abdomen and the organs. ACS often presents with pain and complaint of distended or bloated abdomen; however, it often occurs in unconscious patients and goes unnoticed. In the comatose patient, signs include a distended or overly \"round\" abdomen and vital sign deterioration with tachycardia and hypotension; if untreated, this leads to multiorgan failure and shock later.",
"ACS is defined as the adverse physiologic consequences that occur with an acute increase in IAP. The consensus statement from the World Society of the Abdominal Compartment Syndrome defines intra-abdominal hypertension (IAH) as an IAP of 12 mm Hg or higher and ACS as a sustained IAP of 20 mm Hg or higher associated with new organ dysfunction or failure.[1] The organ dysfunction occurs as a result of direct compression of hollow systems.[2] These structures collapse under high pressure, and thrombosis or bowel wall edema occurs, leading to translocation of bacterial products and additional fluid accumulation that further increases IAP.",
"At the cellular level, oxygen delivery is impaired, which causes ischemia and anaerobic metabolism. Vasoactive substances, such as histamine and serotonin, increase endothelial permeability, and this capillary leakage impairs red cell transport and oxygen delivery.",
"ACS can be divided into primary, secondary, and chronic forms. Primary or acute presentations occur when an intra-abdominal pathology is directly responsible for the CS. Examples of this include penetrating trauma, intraperitoneal hemorrhage, pancreatitis, pelvic fracture, rupture of an abdominal aortic aneurysm, and a perforated peptic ulcer. Secondary presentations occur when no visible intra-abdominal injury is present but injuries outside of the abdomen cause fluid accumulation; examples of this include large-volume resuscitation (>3 L), large areas of full-thickness burns, postoperative packing and primary fascial closure, and sepsis. Chronic ACS can develop in cases of cirrhosis with excessive ascites.[3]"
],
"date": "April 30, 2021",
"figures": [],
"markdown": "# Abdominal Pain, Anemia, and Oliguria in a Distressed Woman\n\n **Authors:** Eva Nourbakhsh, MD; Kenneth M. Nugent, MD; Rishi Raj, MD \n **Date:** April 30, 2021\n\n ## Content\n\n This patient presented with refractory hypotension, oliguria, metabolic acidosis, and anemia. A CT scan revealed a large abdominal wall hematoma, with collapse of the inferior vena cava. Her bladder pressure was initially high and further increased during a relatively short period of observation. The diagnosis of abdominal compartment syndrome (ACS) was made based on the multiorgan failure, evidence of abdominal wall hematoma secondary to anticoagulants, and increasing IAPs.\nCompartment syndrome (CS) refers to a fixed compartment that becomes subject to increased pressure, whether from injury or other means, leading to reduced capillary circulation or outright venous collapse followed by ischemia and organ dysfunction. CS occurs most frequently in the extremities, but it may also occur in the abdomen and the organs. ACS often presents with pain and complaint of distended or bloated abdomen; however, it often occurs in unconscious patients and goes unnoticed. In the comatose patient, signs include a distended or overly \"round\" abdomen and vital sign deterioration with tachycardia and hypotension; if untreated, this leads to multiorgan failure and shock later.\nACS is defined as the adverse physiologic consequences that occur with an acute increase in IAP. The consensus statement from the World Society of the Abdominal Compartment Syndrome defines intra-abdominal hypertension (IAH) as an IAP of 12 mm Hg or higher and ACS as a sustained IAP of 20 mm Hg or higher associated with new organ dysfunction or failure.[1] The organ dysfunction occurs as a result of direct compression of hollow systems.[2] These structures collapse under high pressure, and thrombosis or bowel wall edema occurs, leading to translocation of bacterial products and additional fluid accumulation that further increases IAP.\nAt the cellular level, oxygen delivery is impaired, which causes ischemia and anaerobic metabolism. Vasoactive substances, such as histamine and serotonin, increase endothelial permeability, and this capillary leakage impairs red cell transport and oxygen delivery.\nACS can be divided into primary, secondary, and chronic forms. Primary or acute presentations occur when an intra-abdominal pathology is directly responsible for the CS. Examples of this include penetrating trauma, intraperitoneal hemorrhage, pancreatitis, pelvic fracture, rupture of an abdominal aortic aneurysm, and a perforated peptic ulcer. Secondary presentations occur when no visible intra-abdominal injury is present but injuries outside of the abdomen cause fluid accumulation; examples of this include large-volume resuscitation (>3 L), large areas of full-thickness burns, postoperative packing and primary fascial closure, and sepsis. Chronic ACS can develop in cases of cirrhosis with excessive ascites.[3]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 819545,
"choiceText": "Spontaneous retroperitoneal hematoma",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819547,
"choiceText": "Abdominal compartment syndrome",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819549,
"choiceText": "Abdominal wall abscess",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819551,
"choiceText": "Septic shock",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 257387,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Abdominal Pain, Anemia, and Oliguria in a Distressed Woman"
},
{
"authors": "Eva Nourbakhsh, MD; Kenneth M. Nugent, MD; Rishi Raj, MD",
"content": [
"Risk factors for ACS include the following:[4]",
"Diminished abdominal wall compliance in patients who undergo abdominal surgery, have major trauma or burns, or have a high body mass index with central obesity",
"Patients on mechanical ventilation",
"Increased intraluminal content secondary to gastroparesis, ileus, colonic pseudo-obstruction, or intra-abdominal or retroperitoneal tumors",
"Increased abdominal contents in hemoperitoneum, pneumoperitoneum, or ascites",
"Capillary leak and fluid resuscitation in acidosis or hypotension",
"Hypothermia",
"Massive transfusion (>10 units in 24 hours)",
"Massive fluid resuscitation (>5 L/24 hours)",
"Pancreatitis",
"Sepsis",
"Damage control laparotomy",
"Several case reports have been published on enoxaparin-associated retroperitoneal bleeding and ACS.[5,6]",
"Patients with two or more risk factors or with new or progressive organ failure should be screened for ACS. Investigations for ACS should include abdominal radiography to look for free air or bowel obstruction and an abdominal CT scan to look for the \"round-belly\" sign (abdominal distention with an increased anteroposterior-to-transverse abdominal diameter (ratio >0.80), collapse of the vena cava, or bowel wall thickening.",
"In addition, an IAP measurement should be performed. Bladder pressure can be monitored fairly easily by connecting a transurethral Foley catheter to a pressure transducer. Changes in intraperitoneal pressure are reflected by parallel change in intraluminal bladder pressure.[1] IAPs have the following usual ranges based on the patient's condition:",
"Healthy adults: 0-5 mm Hg",
"Critically ill adults: 5-7 mm Hg",
"Post-laparotomy patients: 10-15 mm Hg",
"Patients with septic shock: 15-25 mm Hg",
"Patients with an acute surgical abdomen: 25-40 mm Hg",
"Burch and associates classified patients into the following categories on the basis of IAP measurement via bladder catheterization[7]:",
"Grade I: 10-15 cm H2O",
"Grade II: 15-25 cm H2O",
"Grade III: 25-35 cm H2O",
"Grade IV: >35 cm H2O",
"A multicenter, prospective, epidemiologic study reported that the mean IAP in all intensive care unit admissions was 10 ± 4.8 mm Hg. A total of 67.9% of patients had a normal IAP (<12 mm Hg), 32.1% had IAH >12 mm Hg, and 4.2% had ACS. The prevalence of ACS in patients with IAH was 12.9%. The mortality rate was significantly higher in the group with IAH compared with the non-IAH group.[8]",
"The hemodynamic consequences of IAH include a fall in cardiac output and stroke volume; a decrease in celiac, superior mesenteric, and renal artery blood flow; an increase in oxygen consumption; and a decrease in pH and arterial partial pressure of oxygen. The reduction in cardiac output is probably explained by compression of the inferior vena cava leading to a reduction in venous return (as seen in this case). Additionally, an increase in afterload may contribute to systemic hypotension.[9]",
"Increased IAP impairs pulmonary function through mechanical effects. As IAP increases, the diaphragm is forced higher into the chest and decreases lung and chest wall compliance. Adequate ventilation with a mechanical ventilator then requires increased airway pressures.[4] IAH decreases renal plasma flow and the glomerular filtration rate. The pathophysiology of these IAH effects is uncertain but does not necessarily reflect the decreased cardiac output. Shunting of blood away from the renal cortex into the medulla, reduced renal blood flow, direct compression of the kidneys or renal veins, and high levels of antidiuretic hormone may explain renal impairment.[2] Abdominal perfusion pressure (APP) is used to assess the severity and adequacy of abdominal blood flow. It can be calculated by subtracting the IAP from the mean arterial pressure. APP should be kept above 50-60 mm Hg. APP is superior to IAP, arterial pH, base deficit, and arterial lactate in predicting organ failure and patient outcome."
],
"date": "April 30, 2021",
"figures": [],
"markdown": "# Abdominal Pain, Anemia, and Oliguria in a Distressed Woman\n\n **Authors:** Eva Nourbakhsh, MD; Kenneth M. Nugent, MD; Rishi Raj, MD \n **Date:** April 30, 2021\n\n ## Content\n\n Risk factors for ACS include the following:[4]\nDiminished abdominal wall compliance in patients who undergo abdominal surgery, have major trauma or burns, or have a high body mass index with central obesity\nPatients on mechanical ventilation\nIncreased intraluminal content secondary to gastroparesis, ileus, colonic pseudo-obstruction, or intra-abdominal or retroperitoneal tumors\nIncreased abdominal contents in hemoperitoneum, pneumoperitoneum, or ascites\nCapillary leak and fluid resuscitation in acidosis or hypotension\nHypothermia\nMassive transfusion (>10 units in 24 hours)\nMassive fluid resuscitation (>5 L/24 hours)\nPancreatitis\nSepsis\nDamage control laparotomy\nSeveral case reports have been published on enoxaparin-associated retroperitoneal bleeding and ACS.[5,6]\nPatients with two or more risk factors or with new or progressive organ failure should be screened for ACS. Investigations for ACS should include abdominal radiography to look for free air or bowel obstruction and an abdominal CT scan to look for the \"round-belly\" sign (abdominal distention with an increased anteroposterior-to-transverse abdominal diameter (ratio >0.80), collapse of the vena cava, or bowel wall thickening.\nIn addition, an IAP measurement should be performed. Bladder pressure can be monitored fairly easily by connecting a transurethral Foley catheter to a pressure transducer. Changes in intraperitoneal pressure are reflected by parallel change in intraluminal bladder pressure.[1] IAPs have the following usual ranges based on the patient's condition:\nHealthy adults: 0-5 mm Hg\nCritically ill adults: 5-7 mm Hg\nPost-laparotomy patients: 10-15 mm Hg\nPatients with septic shock: 15-25 mm Hg\nPatients with an acute surgical abdomen: 25-40 mm Hg\nBurch and associates classified patients into the following categories on the basis of IAP measurement via bladder catheterization[7]:\nGrade I: 10-15 cm H2O\nGrade II: 15-25 cm H2O\nGrade III: 25-35 cm H2O\nGrade IV: >35 cm H2O\nA multicenter, prospective, epidemiologic study reported that the mean IAP in all intensive care unit admissions was 10 ± 4.8 mm Hg. A total of 67.9% of patients had a normal IAP (<12 mm Hg), 32.1% had IAH >12 mm Hg, and 4.2% had ACS. The prevalence of ACS in patients with IAH was 12.9%. The mortality rate was significantly higher in the group with IAH compared with the non-IAH group.[8]\nThe hemodynamic consequences of IAH include a fall in cardiac output and stroke volume; a decrease in celiac, superior mesenteric, and renal artery blood flow; an increase in oxygen consumption; and a decrease in pH and arterial partial pressure of oxygen. The reduction in cardiac output is probably explained by compression of the inferior vena cava leading to a reduction in venous return (as seen in this case). Additionally, an increase in afterload may contribute to systemic hypotension.[9]\nIncreased IAP impairs pulmonary function through mechanical effects. As IAP increases, the diaphragm is forced higher into the chest and decreases lung and chest wall compliance. Adequate ventilation with a mechanical ventilator then requires increased airway pressures.[4] IAH decreases renal plasma flow and the glomerular filtration rate. The pathophysiology of these IAH effects is uncertain but does not necessarily reflect the decreased cardiac output. Shunting of blood away from the renal cortex into the medulla, reduced renal blood flow, direct compression of the kidneys or renal veins, and high levels of antidiuretic hormone may explain renal impairment.[2] Abdominal perfusion pressure (APP) is used to assess the severity and adequacy of abdominal blood flow. It can be calculated by subtracting the IAP from the mean arterial pressure. APP should be kept above 50-60 mm Hg. APP is superior to IAP, arterial pH, base deficit, and arterial lactate in predicting organ failure and patient outcome.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Abdominal Pain, Anemia, and Oliguria in a Distressed Woman"
},
{
"authors": "Eva Nourbakhsh, MD; Kenneth M. Nugent, MD; Rishi Raj, MD",
"content": [
"The treatment of ACS is multifactorial and depends on both the severity and the primary cause. Because a wide variety of patients may develop IAH/ACS, no one management strategy can be uniformly applied. Appropriate IAH/ACS management is based on three principles: serial monitoring of IAP, optimization of systemic perfusion and organ function, and prompt surgical decompression for refractory IAH. Most patients with Grade III pressures and all patients with Grade IV pressures should have surgical decompression. Nonsurgical strategies are appropriate, at least initially, for Grades I and II. These modalities may include body positioning, nasogastric and colonic decompression, fluid resuscitation, diuretics and continuous renal replacement therapies, as well as percutaneous catheter decompression.[4]",
"After reversal of her warfarin-induced coagulopathy with plasma and vitamin K, the patient in this case was taken to the operating room for evacuation of a large abdominal wall hematoma. No active bleeding was found. The wound was packed for hemostasis, and the abdominal cavity was left open to ensure that the IAP remained low. The following day, after improvement of her condition, she was taken back to the operating room for removal of the packing and for closure of the abdominal cavity. Another blood clot was found, but no active arterial or venous bleed was noted. A Jackson-Pratt tube and a wound vacuum-assisted closure (VAC) were placed. The patient's clinical status and multiorgan failure resolved, and she was discharged to a long-term acute care facility with the wound VAC in place."
],
"date": "April 30, 2021",
"figures": [],
"markdown": "# Abdominal Pain, Anemia, and Oliguria in a Distressed Woman\n\n **Authors:** Eva Nourbakhsh, MD; Kenneth M. Nugent, MD; Rishi Raj, MD \n **Date:** April 30, 2021\n\n ## Content\n\n The treatment of ACS is multifactorial and depends on both the severity and the primary cause. Because a wide variety of patients may develop IAH/ACS, no one management strategy can be uniformly applied. Appropriate IAH/ACS management is based on three principles: serial monitoring of IAP, optimization of systemic perfusion and organ function, and prompt surgical decompression for refractory IAH. Most patients with Grade III pressures and all patients with Grade IV pressures should have surgical decompression. Nonsurgical strategies are appropriate, at least initially, for Grades I and II. These modalities may include body positioning, nasogastric and colonic decompression, fluid resuscitation, diuretics and continuous renal replacement therapies, as well as percutaneous catheter decompression.[4]\nAfter reversal of her warfarin-induced coagulopathy with plasma and vitamin K, the patient in this case was taken to the operating room for evacuation of a large abdominal wall hematoma. No active bleeding was found. The wound was packed for hemostasis, and the abdominal cavity was left open to ensure that the IAP remained low. The following day, after improvement of her condition, she was taken back to the operating room for removal of the packing and for closure of the abdominal cavity. Another blood clot was found, but no active arterial or venous bleed was noted. A Jackson-Pratt tube and a wound vacuum-assisted closure (VAC) were placed. The patient's clinical status and multiorgan failure resolved, and she was discharged to a long-term acute care facility with the wound VAC in place.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 819553,
"choiceText": "A 28-year-old man with acute appendicitis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819555,
"choiceText": "A 72-year-old woman with an asymptomatic abdominal aortic aneurysm",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819557,
"choiceText": "A 66-year-old woman with a chronic obstructive pulmonary disease exacerbation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819559,
"choiceText": "A 58-year-old man with ascites secondary to liver cirrhosis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Patients with two or more risk factors or with new or progressive organ failure should be screened for ACS. Among the various risk factors are increased abdominal contents in hemoperitoneum, pneumoperitoneum, or ascites.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 257389,
"questionText": "You are examining the four patients seen in the answer choices below. Which of these patients is most at risk of developing IAH or ACS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 819561,
"choiceText": "Central venous pressure",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819563,
"choiceText": "Serial kidney, ureter, and bladder radiography",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819565,
"choiceText": "Bladder pressure recordings",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819567,
"choiceText": "Serial arterial blood gas with lactate",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Bladder pressure can be monitored by connecting a transurethral Foley catheter to a pressure transducer. Changes in intraperitoneal pressure are reflected by parallel change in intraluminal bladder pressure.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 257391,
"questionText": "You suspect a patient has IAH or ACS. Which of these represents the best means by which to monitor this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Abdominal Pain, Anemia, and Oliguria in a Distressed Woman"
},
{
"authors": "Eva Nourbakhsh, MD; Kenneth M. Nugent, MD; Rishi Raj, MD",
"content": [],
"date": "April 30, 2021",
"figures": [],
"markdown": "# Abdominal Pain, Anemia, and Oliguria in a Distressed Woman\n\n **Authors:** Eva Nourbakhsh, MD; Kenneth M. Nugent, MD; Rishi Raj, MD \n **Date:** April 30, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 819553,
"choiceText": "A 28-year-old man with acute appendicitis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819555,
"choiceText": "A 72-year-old woman with an asymptomatic abdominal aortic aneurysm",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819557,
"choiceText": "A 66-year-old woman with a chronic obstructive pulmonary disease exacerbation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819559,
"choiceText": "A 58-year-old man with ascites secondary to liver cirrhosis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Patients with two or more risk factors or with new or progressive organ failure should be screened for ACS. Among the various risk factors are increased abdominal contents in hemoperitoneum, pneumoperitoneum, or ascites.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 257389,
"questionText": "You are examining the four patients seen in the answer choices below. Which of these patients is most at risk of developing IAH or ACS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 819561,
"choiceText": "Central venous pressure",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819563,
"choiceText": "Serial kidney, ureter, and bladder radiography",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819565,
"choiceText": "Bladder pressure recordings",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819567,
"choiceText": "Serial arterial blood gas with lactate",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Bladder pressure can be monitored by connecting a transurethral Foley catheter to a pressure transducer. Changes in intraperitoneal pressure are reflected by parallel change in intraluminal bladder pressure.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 257391,
"questionText": "You suspect a patient has IAH or ACS. Which of these represents the best means by which to monitor this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Abdominal Pain, Anemia, and Oliguria in a Distressed Woman"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 819545,
"choiceText": "Spontaneous retroperitoneal hematoma",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819547,
"choiceText": "Abdominal compartment syndrome",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819549,
"choiceText": "Abdominal wall abscess",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819551,
"choiceText": "Septic shock",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 257387,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 819553,
"choiceText": "A 28-year-old man with acute appendicitis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819555,
"choiceText": "A 72-year-old woman with an asymptomatic abdominal aortic aneurysm",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819557,
"choiceText": "A 66-year-old woman with a chronic obstructive pulmonary disease exacerbation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819559,
"choiceText": "A 58-year-old man with ascites secondary to liver cirrhosis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Patients with two or more risk factors or with new or progressive organ failure should be screened for ACS. Among the various risk factors are increased abdominal contents in hemoperitoneum, pneumoperitoneum, or ascites.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 257389,
"questionText": "You are examining the four patients seen in the answer choices below. Which of these patients is most at risk of developing IAH or ACS?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 819561,
"choiceText": "Central venous pressure",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819563,
"choiceText": "Serial kidney, ureter, and bladder radiography",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819565,
"choiceText": "Bladder pressure recordings",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 819567,
"choiceText": "Serial arterial blood gas with lactate",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Bladder pressure can be monitored by connecting a transurethral Foley catheter to a pressure transducer. Changes in intraperitoneal pressure are reflected by parallel change in intraluminal bladder pressure.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 257391,
"questionText": "You suspect a patient has IAH or ACS. Which of these represents the best means by which to monitor this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
948838 | /viewarticle/948838 | [
{
"authors": "Asim Kichloo, MD; Dushyant Singh Dahiya, MD; Farah Wani, MD; Khalil Kanjwal, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us .",
"A 67-year-old man presents to the emergency department (ED) with worsening dyspnea and fatigue. He also reports a change in the color of his stools. The patient has a history of extensive smoking, atrial fibrillation, and a recent percutaneous coronary intervention (PCI) for an ST-segment elevation myocardial infarction (STEMI).",
"One day before he presented to the ED, the patient experienced sudden onset of progressively worsening dyspnea upon exertion, which was accompanied by increased fatigue. The shortness of breath occurred while he was walking around the house and climbing a flight of stairs. Sitting down eased his symptoms. He states that the dyspnea upon exertion represents an increase from his baseline condition.",
"The patient says that he has used two pillows while sleeping for \"as long as I can remember.\" He does not recall any episodes of waking up at night and gasping for air. He denies any fever, chills, cough, recent sick contacts, or respiratory tract infections. He does not have any chest pain or leg swelling.",
"The patient also reports that his stools have become darker over the past 3 days; the consistency is normal. He has not had any associated abdominal pain, painful defecation, recent diarrhea, or change in his bowel and bladder habits. He does not take over-the-counter pain medications. The results of a colonoscopy 2 years prior were normal. He has not had similar stool darkening in the past.",
"For more than 30 years, the patient smoked two packs of cigarettes per day. He received a diagnosis of chronic obstructive pulmonary disease (COPD). He does not take any medications for COPD or use oxygen at home. He has no history of substance use (including marijuana) or alcohol consumption.",
"He takes apixaban for atrial fibrillation, which was diagnosed 5 years earlier. He underwent PCI for a STEMI with placement of a drug-eluting stent in the right coronary artery 45 days ago. Aspirin and clopidogrel were started after the procedure. He does not take any other medications.",
"The patient has a family history of inflammatory bowel disease (IBD) in his father and diverticulosis in his mother."
],
"date": "April 12, 2021",
"figures": [],
"markdown": "# Strange Stool Color and Fatigue in a Man With COPD and Atrial Fibrillation\n\n **Authors:** Asim Kichloo, MD; Dushyant Singh Dahiya, MD; Farah Wani, MD; Khalil Kanjwal, MD \n **Date:** April 12, 2021\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us .\nA 67-year-old man presents to the emergency department (ED) with worsening dyspnea and fatigue. He also reports a change in the color of his stools. The patient has a history of extensive smoking, atrial fibrillation, and a recent percutaneous coronary intervention (PCI) for an ST-segment elevation myocardial infarction (STEMI).\nOne day before he presented to the ED, the patient experienced sudden onset of progressively worsening dyspnea upon exertion, which was accompanied by increased fatigue. The shortness of breath occurred while he was walking around the house and climbing a flight of stairs. Sitting down eased his symptoms. He states that the dyspnea upon exertion represents an increase from his baseline condition.\nThe patient says that he has used two pillows while sleeping for \"as long as I can remember.\" He does not recall any episodes of waking up at night and gasping for air. He denies any fever, chills, cough, recent sick contacts, or respiratory tract infections. He does not have any chest pain or leg swelling.\nThe patient also reports that his stools have become darker over the past 3 days; the consistency is normal. He has not had any associated abdominal pain, painful defecation, recent diarrhea, or change in his bowel and bladder habits. He does not take over-the-counter pain medications. The results of a colonoscopy 2 years prior were normal. He has not had similar stool darkening in the past.\nFor more than 30 years, the patient smoked two packs of cigarettes per day. He received a diagnosis of chronic obstructive pulmonary disease (COPD). He does not take any medications for COPD or use oxygen at home. He has no history of substance use (including marijuana) or alcohol consumption.\nHe takes apixaban for atrial fibrillation, which was diagnosed 5 years earlier. He underwent PCI for a STEMI with placement of a drug-eluting stent in the right coronary artery 45 days ago. Aspirin and clopidogrel were started after the procedure. He does not take any other medications.\nThe patient has a family history of inflammatory bowel disease (IBD) in his father and diverticulosis in his mother.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Strange Stool Color and Fatigue in a Man With COPD and Atrial Fibrillation"
},
{
"authors": "Asim Kichloo, MD; Dushyant Singh Dahiya, MD; Farah Wani, MD; Khalil Kanjwal, MD",
"content": [
"In the ED, the patient has a temperature of 98 °F (36.7 °C), a heart rate of 120 beats/min, a respiration rate of 18 breaths/min, and a blood pressure of 86/60 mm Hg. His oxygen saturation is 98% on room air.",
"Upon physical examination, his extremities are pale and cold. No peripheral edema is noted. Peripheral pulses are weak but palpable in all limbs. His abdomen is soft and nontender, with normal bowel sounds. Tachycardia is noted on auscultation of the chest, and rhonchi are audible in all lung fields.",
"Laboratory investigations reveal the following values:",
"Hemoglobin level: 6.9 g/dL (reference range, 13.5-17.5 g/dL)",
"Hematocrit: 40% (reference range, 41-50%)",
"White blood cell count: 7000 cells/µL (reference range, 4000-11,000 cells/µL)",
"Platelet count: 177,000 cells/µL (reference range, 150,000-400,000 cells/µL)",
"The fecal occult blood test result is positive. All other laboratory values are unremarkable. An ECG shows sinus tachycardia and no ST-segment changes. Echocardiography reveals a left ventricular ejection fraction of 60%-65%. Esophagogastroduodenoscopy (EGD) is performed. Figure 1 shows similar results as were seen in this case in another patient. Colonoscopy is also performed. Figure 2 is an example of similar findings as were seen in this case in another patient.",
"Figure 1.",
"Figure 2."
],
"date": "April 12, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/948/838/948838-Thumb1.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/948/838/948838-Thumb2.jpg"
}
],
"markdown": "# Strange Stool Color and Fatigue in a Man With COPD and Atrial Fibrillation\n\n **Authors:** Asim Kichloo, MD; Dushyant Singh Dahiya, MD; Farah Wani, MD; Khalil Kanjwal, MD \n **Date:** April 12, 2021\n\n ## Content\n\n In the ED, the patient has a temperature of 98 °F (36.7 °C), a heart rate of 120 beats/min, a respiration rate of 18 breaths/min, and a blood pressure of 86/60 mm Hg. His oxygen saturation is 98% on room air.\nUpon physical examination, his extremities are pale and cold. No peripheral edema is noted. Peripheral pulses are weak but palpable in all limbs. His abdomen is soft and nontender, with normal bowel sounds. Tachycardia is noted on auscultation of the chest, and rhonchi are audible in all lung fields.\nLaboratory investigations reveal the following values:\nHemoglobin level: 6.9 g/dL (reference range, 13.5-17.5 g/dL)\nHematocrit: 40% (reference range, 41-50%)\nWhite blood cell count: 7000 cells/µL (reference range, 4000-11,000 cells/µL)\nPlatelet count: 177,000 cells/µL (reference range, 150,000-400,000 cells/µL)\nThe fecal occult blood test result is positive. All other laboratory values are unremarkable. An ECG shows sinus tachycardia and no ST-segment changes. Echocardiography reveals a left ventricular ejection fraction of 60%-65%. Esophagogastroduodenoscopy (EGD) is performed. Figure 1 shows similar results as were seen in this case in another patient. Colonoscopy is also performed. Figure 2 is an example of similar findings as were seen in this case in another patient.\nFigure 1.\nFigure 2.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1579251,
"choiceText": "Acute exacerbation of COPD",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579252,
"choiceText": "Acute gastrointestinal (GI) bleeding",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579253,
"choiceText": "Congestive heart failure",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579254,
"choiceText": "In-stent restenosis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579255,
"choiceText": "IBD",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 506967,
"questionText": "On the basis of these findings only, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Strange Stool Color and Fatigue in a Man With COPD and Atrial Fibrillation"
},
{
"authors": "Asim Kichloo, MD; Dushyant Singh Dahiya, MD; Farah Wani, MD; Khalil Kanjwal, MD",
"content": [
"Acute GI bleeding can be classified into the two following subtypes, according to the location of the bleeding and the presentation of the symptoms:",
"Upper GI bleeding usually presents with hematemesis or melena. Massive upper GI bleeding may present with hematochezia.",
"Lower GI bleeding typically presents with hematochezia. Rarely, patients with right-sided colonic bleeding may present with melena.",
"In this case, the patient presented to the ED with acute, sudden-onset worsening shortness of breath upon exertion, fatigue, and dark stools. Upon examination, he had tachycardia, hypotension, weak peripheral pulses, and cold and pale extremities. Laboratory investigations revealed low hemoglobin levels, and the fecal occult blood test was positive. These characteristic signs, symptoms, and test results favor a diagnosis of acute blood loss anemia from a GI source, which was later visualized on colonoscopy. In addition, the patient was taking aspirin, clopidogrel, and apixaban, which are known to increase the risk for GI bleeding.",
"Although this patient had a history of COPD and presented with worsening shortness of breath, he did not have increased cough, wheezing, or sputum production. Moreover, he did not require home oxygen and had no triggering factors. These findings make a diagnosis of acute exacerbation of COPD less likely.",
"Congestive heart failure was ruled out by the absence of orthopnea (no increase in the number of pillows to help relieve shortness of breath while lying down), paroxysmal nocturnal dyspnea, and peripheral edema. In addition, the echocardiogram showed a normal left ventricular ejection fraction.",
"In-stent restenosis has been reported in 3%-20% of patients who undergo PCI with stent placement and depends on the drug-eluting stent used.[1] It can occur within 3-12 months of the stent placement and may present with features of recurrent angina or myocardial infarction (MI). This patient did not have clinical features suggestive of angina or MI, and the ECG findings were unremarkable; thus, in-stent restenosis was unlikely.",
"Finally, although a positive family history of IBD predisposes the patient to IBD and requires aggressive screening, the results of his colonoscopy 2 years earlier were unremarkable. In addition, the findings on his most recent colonoscopy do not support a diagnosis of IBD.",
"The initial assessment and treatment of a patient who presents to the ED with suspected acute GI bleeding should focus on hemodynamic stability; however, other investigations should also occur in parallel. The goals are to determine the location of the bleeding (upper or lower GI tract), assess the severity of the bleeding, triage the patient to an appropriate setting, provide general supportive measures, and initiate resuscitation if necessary."
],
"date": "April 12, 2021",
"figures": [],
"markdown": "# Strange Stool Color and Fatigue in a Man With COPD and Atrial Fibrillation\n\n **Authors:** Asim Kichloo, MD; Dushyant Singh Dahiya, MD; Farah Wani, MD; Khalil Kanjwal, MD \n **Date:** April 12, 2021\n\n ## Content\n\n Acute GI bleeding can be classified into the two following subtypes, according to the location of the bleeding and the presentation of the symptoms:\nUpper GI bleeding usually presents with hematemesis or melena. Massive upper GI bleeding may present with hematochezia.\nLower GI bleeding typically presents with hematochezia. Rarely, patients with right-sided colonic bleeding may present with melena.\nIn this case, the patient presented to the ED with acute, sudden-onset worsening shortness of breath upon exertion, fatigue, and dark stools. Upon examination, he had tachycardia, hypotension, weak peripheral pulses, and cold and pale extremities. Laboratory investigations revealed low hemoglobin levels, and the fecal occult blood test was positive. These characteristic signs, symptoms, and test results favor a diagnosis of acute blood loss anemia from a GI source, which was later visualized on colonoscopy. In addition, the patient was taking aspirin, clopidogrel, and apixaban, which are known to increase the risk for GI bleeding.\nAlthough this patient had a history of COPD and presented with worsening shortness of breath, he did not have increased cough, wheezing, or sputum production. Moreover, he did not require home oxygen and had no triggering factors. These findings make a diagnosis of acute exacerbation of COPD less likely.\nCongestive heart failure was ruled out by the absence of orthopnea (no increase in the number of pillows to help relieve shortness of breath while lying down), paroxysmal nocturnal dyspnea, and peripheral edema. In addition, the echocardiogram showed a normal left ventricular ejection fraction.\nIn-stent restenosis has been reported in 3%-20% of patients who undergo PCI with stent placement and depends on the drug-eluting stent used.[1] It can occur within 3-12 months of the stent placement and may present with features of recurrent angina or myocardial infarction (MI). This patient did not have clinical features suggestive of angina or MI, and the ECG findings were unremarkable; thus, in-stent restenosis was unlikely.\nFinally, although a positive family history of IBD predisposes the patient to IBD and requires aggressive screening, the results of his colonoscopy 2 years earlier were unremarkable. In addition, the findings on his most recent colonoscopy do not support a diagnosis of IBD.\nThe initial assessment and treatment of a patient who presents to the ED with suspected acute GI bleeding should focus on hemodynamic stability; however, other investigations should also occur in parallel. The goals are to determine the location of the bleeding (upper or lower GI tract), assess the severity of the bleeding, triage the patient to an appropriate setting, provide general supportive measures, and initiate resuscitation if necessary.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1579251,
"choiceText": "Acute exacerbation of COPD",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579252,
"choiceText": "Acute gastrointestinal (GI) bleeding",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579253,
"choiceText": "Congestive heart failure",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579254,
"choiceText": "In-stent restenosis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579255,
"choiceText": "IBD",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 506967,
"questionText": "On the basis of these findings only, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Strange Stool Color and Fatigue in a Man With COPD and Atrial Fibrillation"
},
{
"authors": "Asim Kichloo, MD; Dushyant Singh Dahiya, MD; Farah Wani, MD; Khalil Kanjwal, MD",
"content": [
"A thorough clinical history and physical examination may be the key to identifying not only the probable cause of the bleeding but also the patient's current functional status. Physical examination findings that can point to hypovolemia include resting tachycardia (mild to moderate hypovolemia), orthostatic hypotension (blood loss ≥ 15%), and supine hypotension (blood loss ≥ 40%). Patients who are hemodynamically unstable require immediate resuscitation, and specific investigations to find the probable cause of bleeding should be deferred until after hemodynamic stability is achieved.",
"In cases of acute GI bleeding of abrupt onset, a thorough medication history becomes essential, particularly in patients who may already be at high risk because of guideline-oriented treatment for an underlying disease pathology. Laboratory investigations that should be obtained in patients with acute GI bleeding include a complete blood cell count, serum chemistries, liver tests, and coagulation studies. Once these steps are completed, additional diagnostic modalities, such as EGD or colonoscopy, can be used to find the probable cause of the GI bleeding.",
"In this case, initial assessment in the ED found the patient to be hemodynamically stable. Because his hemoglobin level was < 7 g/dL (6.9 g/dL), he was given a transfusion with a unit of packed red blood cells. A decision was made to perform EGD, which showed only mild gastritis, and colonoscopy, which revealed an aberrant bleeding artery in the right-sided colon that was cauterized during the procedure.",
"The next day, the patient reported feeling much better. His temperature was 98 °F (36.7 °C), heart rate was 84 beats/min, respiration rate was 12 breaths/min, and blood pressure was 116/80 mm Hg. His oxygen saturation was 98% on room air. Peripheral pulses were of good volume and palpable in all limbs. Repeated laboratory studies revealed a hemoglobin level of 7.7 g/dL.",
"The number of patients who are receiving anticoagulant or antiplatelet therapy to prevent cardiovascular or cerebrovascular mortality is increasing. However, the major downside to these therapies is the increased risk for GI or intracerebral bleeding.",
"GI bleeding is a serious but frequently encountered complication of antithrombotic therapy. The relative risk for upper GI bleeding, in particular, increases up to 10% in patients who are treated with oral anticoagulants or antiplatelet agents, and the annual risk for upper GI bleeding in such patients is 1.5%-4.5%.[2]Lower GI bleeding is usually less severe; however, patients are still at significant risk for lower GI bleeding with triple therapy (the combination of an anticoagulant plus two antiplatelet drugs).[3] Overall, GI bleeding is an acute life-threatening situation, with mortality ranging from 1% to 13%.[2]",
"The management of antithrombotic therapy after an episode of GI bleeding poses a significant dilemma. Restarting antithrombotic therapy could lead to recurrent bleeding; however, interrupting the treatment could increase the risk for thrombosis and adverse outcomes, owing to the underlying disease pathology. For example, in the United States, about 20%-30% of ischemic strokes are attributed to atrial fibrillation.[4]",
"In an observational cohort study with a median follow-up of 24.9 months, patients who did not restart therapy had a higher risk for ischemic events and death than those who did restart therapy, although the latter patients were more likely to have another episode of GI bleeding.[5] Patients who restarted therapy early had more bleeding events than later restarters; however, fewer ischemic events were reported. Furthermore, mortality rates did not significantly differ between the early and late restarters. No specific guidelines exist in the literature on starting anticoagulant or antiplatelet agents after PCI in patients with atrial fibrillation or on restarting these agents after an episode of GI bleeding.",
"Worldwide, nearly 3 million people undergo PCI each year.[4] Over the past decade, studies have explored the risks and benefits of using different combinations of antithrombotic agents after PCI. Recommendations for the initiation and use of antithrombotic therapy in patients with atrial fibrillation who undergo PCI can be summarized as follows[6]:",
"Low risk for stroke and bleeding: A direct oral anticoagulant (DOAC) plus a purinergic signaling receptor Y12 (P2Y12) inhibitor for 1 year after PCI, with a transition to a DOAC only after 1 year.",
"High risk for stroke and low risk for bleeding: Triple therapy with a DOAC, a P2Y12 inhibitor, and aspirin for the first month, with a transition to a DOAC plus a P2Y12 inhibitor after the first month and continued for 1 year, and then a transition to a DOAC only after 1 year.",
"Low risk for stroke and high risk for bleeding: A DOAC plus a P2Y12 inhibitor for the first 6 months and then a transition to a DOAC only after 6 months."
],
"date": "April 12, 2021",
"figures": [],
"markdown": "# Strange Stool Color and Fatigue in a Man With COPD and Atrial Fibrillation\n\n **Authors:** Asim Kichloo, MD; Dushyant Singh Dahiya, MD; Farah Wani, MD; Khalil Kanjwal, MD \n **Date:** April 12, 2021\n\n ## Content\n\n A thorough clinical history and physical examination may be the key to identifying not only the probable cause of the bleeding but also the patient's current functional status. Physical examination findings that can point to hypovolemia include resting tachycardia (mild to moderate hypovolemia), orthostatic hypotension (blood loss ≥ 15%), and supine hypotension (blood loss ≥ 40%). Patients who are hemodynamically unstable require immediate resuscitation, and specific investigations to find the probable cause of bleeding should be deferred until after hemodynamic stability is achieved.\nIn cases of acute GI bleeding of abrupt onset, a thorough medication history becomes essential, particularly in patients who may already be at high risk because of guideline-oriented treatment for an underlying disease pathology. Laboratory investigations that should be obtained in patients with acute GI bleeding include a complete blood cell count, serum chemistries, liver tests, and coagulation studies. Once these steps are completed, additional diagnostic modalities, such as EGD or colonoscopy, can be used to find the probable cause of the GI bleeding.\nIn this case, initial assessment in the ED found the patient to be hemodynamically stable. Because his hemoglobin level was < 7 g/dL (6.9 g/dL), he was given a transfusion with a unit of packed red blood cells. A decision was made to perform EGD, which showed only mild gastritis, and colonoscopy, which revealed an aberrant bleeding artery in the right-sided colon that was cauterized during the procedure.\nThe next day, the patient reported feeling much better. His temperature was 98 °F (36.7 °C), heart rate was 84 beats/min, respiration rate was 12 breaths/min, and blood pressure was 116/80 mm Hg. His oxygen saturation was 98% on room air. Peripheral pulses were of good volume and palpable in all limbs. Repeated laboratory studies revealed a hemoglobin level of 7.7 g/dL.\nThe number of patients who are receiving anticoagulant or antiplatelet therapy to prevent cardiovascular or cerebrovascular mortality is increasing. However, the major downside to these therapies is the increased risk for GI or intracerebral bleeding.\nGI bleeding is a serious but frequently encountered complication of antithrombotic therapy. The relative risk for upper GI bleeding, in particular, increases up to 10% in patients who are treated with oral anticoagulants or antiplatelet agents, and the annual risk for upper GI bleeding in such patients is 1.5%-4.5%.[2]Lower GI bleeding is usually less severe; however, patients are still at significant risk for lower GI bleeding with triple therapy (the combination of an anticoagulant plus two antiplatelet drugs).[3] Overall, GI bleeding is an acute life-threatening situation, with mortality ranging from 1% to 13%.[2]\nThe management of antithrombotic therapy after an episode of GI bleeding poses a significant dilemma. Restarting antithrombotic therapy could lead to recurrent bleeding; however, interrupting the treatment could increase the risk for thrombosis and adverse outcomes, owing to the underlying disease pathology. For example, in the United States, about 20%-30% of ischemic strokes are attributed to atrial fibrillation.[4]\nIn an observational cohort study with a median follow-up of 24.9 months, patients who did not restart therapy had a higher risk for ischemic events and death than those who did restart therapy, although the latter patients were more likely to have another episode of GI bleeding.[5] Patients who restarted therapy early had more bleeding events than later restarters; however, fewer ischemic events were reported. Furthermore, mortality rates did not significantly differ between the early and late restarters. No specific guidelines exist in the literature on starting anticoagulant or antiplatelet agents after PCI in patients with atrial fibrillation or on restarting these agents after an episode of GI bleeding.\nWorldwide, nearly 3 million people undergo PCI each year.[4] Over the past decade, studies have explored the risks and benefits of using different combinations of antithrombotic agents after PCI. Recommendations for the initiation and use of antithrombotic therapy in patients with atrial fibrillation who undergo PCI can be summarized as follows[6]:\nLow risk for stroke and bleeding: A direct oral anticoagulant (DOAC) plus a purinergic signaling receptor Y12 (P2Y12) inhibitor for 1 year after PCI, with a transition to a DOAC only after 1 year.\nHigh risk for stroke and low risk for bleeding: Triple therapy with a DOAC, a P2Y12 inhibitor, and aspirin for the first month, with a transition to a DOAC plus a P2Y12 inhibitor after the first month and continued for 1 year, and then a transition to a DOAC only after 1 year.\nLow risk for stroke and high risk for bleeding: A DOAC plus a P2Y12 inhibitor for the first 6 months and then a transition to a DOAC only after 6 months.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Strange Stool Color and Fatigue in a Man With COPD and Atrial Fibrillation"
},
{
"authors": "Asim Kichloo, MD; Dushyant Singh Dahiya, MD; Farah Wani, MD; Khalil Kanjwal, MD",
"content": [
"Risk stratification of patients with atrial fibrillation can be done using the CHA2DS2-VASc score (congestive heart failure, hypertension, age ≥ 75 years, diabetes mellitus, stroke or transient ischemic attack, vascular disease, age 65-74 years, sex category) to calculate stroke risk (a score ≥ 2 indicates high risk). The HAS-BLED score (hypertension, abnormal renal/liver function, stroke, bleeding history or predisposition, labile international normalized ratio, elderly [age ≥ 65 years], drug/alcohol use concomitantly) can be used to estimate the risk for bleeding in a patient who is receiving anticoagulant therapy (a score ≥ 3 indicates high risk).",
"When to restart antithrombotic therapy after an episode of acute GI bleeding is often a challenging decision. Results from the current literature strongly favor restarting antithrombotic therapy once the acute event has been managed; however, the optimal time to wait after the event to resume therapy remains unclear.[5,7] On the basis of the available literature, a period of approximately 14 days may provide the best balance among GI bleeding recurrence, thromboembolism, and mortality risks.[7]",
"In conclusion, triple therapy with a DOAC, a P2Y12 inhibitor, and aspirin is a very aggressive approach and carries a higher risk for GI bleeding and mortality than double therapy (an anticoagulant plus an antiplatelet agent), with no tradeoff in efficacy in patients with atrial fibrillation after PCI. However, in patients with a high stroke risk and a low bleeding risk, triple therapy can be used for up to 1 month before transitioning to a DOAC and a P2Y12 inhibitor, and ultimately a DOAC after 1 year.[4]",
"Overall, the patient in this case showed significant improvement throughout the course of his hospital stay. Thus, the decision was made to discharge him. Because the patient was at 46 days (> 30 days and < 1 year) after his PCI, therapy was de-escalated to clopidogrel and apixaban. His CHA2DS2-VASc score was 2, and his HAS-BLED score was 2. Follow-up was planned for 1 year after his PCI for further de-escalation of therapy."
],
"date": "April 12, 2021",
"figures": [],
"markdown": "# Strange Stool Color and Fatigue in a Man With COPD and Atrial Fibrillation\n\n **Authors:** Asim Kichloo, MD; Dushyant Singh Dahiya, MD; Farah Wani, MD; Khalil Kanjwal, MD \n **Date:** April 12, 2021\n\n ## Content\n\n Risk stratification of patients with atrial fibrillation can be done using the CHA2DS2-VASc score (congestive heart failure, hypertension, age ≥ 75 years, diabetes mellitus, stroke or transient ischemic attack, vascular disease, age 65-74 years, sex category) to calculate stroke risk (a score ≥ 2 indicates high risk). The HAS-BLED score (hypertension, abnormal renal/liver function, stroke, bleeding history or predisposition, labile international normalized ratio, elderly [age ≥ 65 years], drug/alcohol use concomitantly) can be used to estimate the risk for bleeding in a patient who is receiving anticoagulant therapy (a score ≥ 3 indicates high risk).\nWhen to restart antithrombotic therapy after an episode of acute GI bleeding is often a challenging decision. Results from the current literature strongly favor restarting antithrombotic therapy once the acute event has been managed; however, the optimal time to wait after the event to resume therapy remains unclear.[5,7] On the basis of the available literature, a period of approximately 14 days may provide the best balance among GI bleeding recurrence, thromboembolism, and mortality risks.[7]\nIn conclusion, triple therapy with a DOAC, a P2Y12 inhibitor, and aspirin is a very aggressive approach and carries a higher risk for GI bleeding and mortality than double therapy (an anticoagulant plus an antiplatelet agent), with no tradeoff in efficacy in patients with atrial fibrillation after PCI. However, in patients with a high stroke risk and a low bleeding risk, triple therapy can be used for up to 1 month before transitioning to a DOAC and a P2Y12 inhibitor, and ultimately a DOAC after 1 year.[4]\nOverall, the patient in this case showed significant improvement throughout the course of his hospital stay. Thus, the decision was made to discharge him. Because the patient was at 46 days (> 30 days and < 1 year) after his PCI, therapy was de-escalated to clopidogrel and apixaban. His CHA2DS2-VASc score was 2, and his HAS-BLED score was 2. Follow-up was planned for 1 year after his PCI for further de-escalation of therapy.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1579260,
"choiceText": "Continue aspirin, clopidogrel, and apixaban (triple therapy)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579261,
"choiceText": "De-escalate therapy to aspirin only",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579262,
"choiceText": "De-escalate therapy to clopidogrel and apixaban (dual therapy)",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579263,
"choiceText": "De-escalate therapy to apixaban only",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "For patients who have atrial fibrillation with a CHA<sub>2</sub>DS<sub>2</sub>-VASc score ≥ 2 (high risk for stroke) but a HAS-BLED score < 3 (low risk for bleeding), triple therapy with a DOAC, a P2Y<sub>12</sub> inhibitor, and aspirin is indicated for the first month after a PCI, with a transition to a DOAC plus a P2Y<sub>12</sub> inhibitor after 1 month. Double therapy is continued, with a transition to only a DOAC after 1 year. Thus, in this scenario, the therapy should be de-escalated to clopidogrel and apixaban after the first 30 days, with further de-escalation to only apixaban 1 year after the PCI.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 506969,
"questionText": "If the patient in this case had presented to the cardiology clinic for follow-up 45 days after his PCI and was on a regimen of aspirin, clopidogrel, and apixaban (CHA<sub>2</sub>DS<sub>2</sub>-VASc score of 3 and HAS-BLED score of 1), which of the following would be the next best step in management?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1579256,
"choiceText": "Continue aspirin, clopidogrel, and apixaban (triple therapy)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579257,
"choiceText": "De-escalate therapy to aspirin only",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579258,
"choiceText": "De-escalate therapy to clopidogrel and apixaban (dual therapy)",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579259,
"choiceText": "De-escalate therapy to apixaban only",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Because of the COVID-19 pandemic, many patients have been reluctant to keep elective follow-up appointments. Ideally, for patients who have atrial fibrillation with a CHA<sub>2</sub>DS<sub>2</sub>-VASc score ≥ 2 (high risk for stroke) but a HAS-BLED score < 3 (low risk for bleeding), triple therapy with a DOAC, a P2Y<sub>12</sub> inhibitor, and aspirin is indicated for the first month, with a transition to a DOAC plus a P2Y<sub>12</sub> inhibitor after the first month, and then a transition to only a DOAC after 1 year.<br><br>\r\n\r\nIn this scenario, the therapy was not de-escalated to a DOAC plus a P2Y<sub>12</sub> inhibitor after the first month, but luckily the patient had no GI bleeding. The next best step at this time would be to de-escalate the therapy to only a DOAC, as the patient presents at 1 year after his PCI.\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 506968,
"questionText": "The patient in this case presents to the cardiology clinic for follow-up 1 year after his PCI and is on a regimen of aspirin, clopidogrel, and apixaban (CHA<sub>2</sub>DS<sub>2</sub>-VASc score of 3 and HAS-BLED score of 1). He reports that he was not able to keep his follow-up appointment 1 month after his PCI because of personal issues and did not keep the later appointments because of the COVID-19 pandemic. He has had no complaints during this period and has been highly compliant with the aspirin, clopidogrel, and apixaban regimen. Which of the following is the next best step?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Strange Stool Color and Fatigue in a Man With COPD and Atrial Fibrillation"
},
{
"authors": "Asim Kichloo, MD; Dushyant Singh Dahiya, MD; Farah Wani, MD; Khalil Kanjwal, MD",
"content": [],
"date": "April 12, 2021",
"figures": [],
"markdown": "# Strange Stool Color and Fatigue in a Man With COPD and Atrial Fibrillation\n\n **Authors:** Asim Kichloo, MD; Dushyant Singh Dahiya, MD; Farah Wani, MD; Khalil Kanjwal, MD \n **Date:** April 12, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1579260,
"choiceText": "Continue aspirin, clopidogrel, and apixaban (triple therapy)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579261,
"choiceText": "De-escalate therapy to aspirin only",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579262,
"choiceText": "De-escalate therapy to clopidogrel and apixaban (dual therapy)",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579263,
"choiceText": "De-escalate therapy to apixaban only",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "For patients who have atrial fibrillation with a CHA<sub>2</sub>DS<sub>2</sub>-VASc score ≥ 2 (high risk for stroke) but a HAS-BLED score < 3 (low risk for bleeding), triple therapy with a DOAC, a P2Y<sub>12</sub> inhibitor, and aspirin is indicated for the first month after a PCI, with a transition to a DOAC plus a P2Y<sub>12</sub> inhibitor after 1 month. Double therapy is continued, with a transition to only a DOAC after 1 year. Thus, in this scenario, the therapy should be de-escalated to clopidogrel and apixaban after the first 30 days, with further de-escalation to only apixaban 1 year after the PCI.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 506969,
"questionText": "If the patient in this case had presented to the cardiology clinic for follow-up 45 days after his PCI and was on a regimen of aspirin, clopidogrel, and apixaban (CHA<sub>2</sub>DS<sub>2</sub>-VASc score of 3 and HAS-BLED score of 1), which of the following would be the next best step in management?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1579256,
"choiceText": "Continue aspirin, clopidogrel, and apixaban (triple therapy)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579257,
"choiceText": "De-escalate therapy to aspirin only",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579258,
"choiceText": "De-escalate therapy to clopidogrel and apixaban (dual therapy)",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579259,
"choiceText": "De-escalate therapy to apixaban only",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Because of the COVID-19 pandemic, many patients have been reluctant to keep elective follow-up appointments. Ideally, for patients who have atrial fibrillation with a CHA<sub>2</sub>DS<sub>2</sub>-VASc score ≥ 2 (high risk for stroke) but a HAS-BLED score < 3 (low risk for bleeding), triple therapy with a DOAC, a P2Y<sub>12</sub> inhibitor, and aspirin is indicated for the first month, with a transition to a DOAC plus a P2Y<sub>12</sub> inhibitor after the first month, and then a transition to only a DOAC after 1 year.<br><br>\r\n\r\nIn this scenario, the therapy was not de-escalated to a DOAC plus a P2Y<sub>12</sub> inhibitor after the first month, but luckily the patient had no GI bleeding. The next best step at this time would be to de-escalate the therapy to only a DOAC, as the patient presents at 1 year after his PCI.\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 506968,
"questionText": "The patient in this case presents to the cardiology clinic for follow-up 1 year after his PCI and is on a regimen of aspirin, clopidogrel, and apixaban (CHA<sub>2</sub>DS<sub>2</sub>-VASc score of 3 and HAS-BLED score of 1). He reports that he was not able to keep his follow-up appointment 1 month after his PCI because of personal issues and did not keep the later appointments because of the COVID-19 pandemic. He has had no complaints during this period and has been highly compliant with the aspirin, clopidogrel, and apixaban regimen. Which of the following is the next best step?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Strange Stool Color and Fatigue in a Man With COPD and Atrial Fibrillation"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1579251,
"choiceText": "Acute exacerbation of COPD",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579252,
"choiceText": "Acute gastrointestinal (GI) bleeding",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579253,
"choiceText": "Congestive heart failure",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579254,
"choiceText": "In-stent restenosis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579255,
"choiceText": "IBD",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 506967,
"questionText": "On the basis of these findings only, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1579260,
"choiceText": "Continue aspirin, clopidogrel, and apixaban (triple therapy)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579261,
"choiceText": "De-escalate therapy to aspirin only",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579262,
"choiceText": "De-escalate therapy to clopidogrel and apixaban (dual therapy)",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579263,
"choiceText": "De-escalate therapy to apixaban only",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "For patients who have atrial fibrillation with a CHA<sub>2</sub>DS<sub>2</sub>-VASc score ≥ 2 (high risk for stroke) but a HAS-BLED score < 3 (low risk for bleeding), triple therapy with a DOAC, a P2Y<sub>12</sub> inhibitor, and aspirin is indicated for the first month after a PCI, with a transition to a DOAC plus a P2Y<sub>12</sub> inhibitor after 1 month. Double therapy is continued, with a transition to only a DOAC after 1 year. Thus, in this scenario, the therapy should be de-escalated to clopidogrel and apixaban after the first 30 days, with further de-escalation to only apixaban 1 year after the PCI.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 506969,
"questionText": "If the patient in this case had presented to the cardiology clinic for follow-up 45 days after his PCI and was on a regimen of aspirin, clopidogrel, and apixaban (CHA<sub>2</sub>DS<sub>2</sub>-VASc score of 3 and HAS-BLED score of 1), which of the following would be the next best step in management?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1579256,
"choiceText": "Continue aspirin, clopidogrel, and apixaban (triple therapy)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579257,
"choiceText": "De-escalate therapy to aspirin only",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579258,
"choiceText": "De-escalate therapy to clopidogrel and apixaban (dual therapy)",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1579259,
"choiceText": "De-escalate therapy to apixaban only",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Because of the COVID-19 pandemic, many patients have been reluctant to keep elective follow-up appointments. Ideally, for patients who have atrial fibrillation with a CHA<sub>2</sub>DS<sub>2</sub>-VASc score ≥ 2 (high risk for stroke) but a HAS-BLED score < 3 (low risk for bleeding), triple therapy with a DOAC, a P2Y<sub>12</sub> inhibitor, and aspirin is indicated for the first month, with a transition to a DOAC plus a P2Y<sub>12</sub> inhibitor after the first month, and then a transition to only a DOAC after 1 year.<br><br>\r\n\r\nIn this scenario, the therapy was not de-escalated to a DOAC plus a P2Y<sub>12</sub> inhibitor after the first month, but luckily the patient had no GI bleeding. The next best step at this time would be to de-escalate the therapy to only a DOAC, as the patient presents at 1 year after his PCI.\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 506968,
"questionText": "The patient in this case presents to the cardiology clinic for follow-up 1 year after his PCI and is on a regimen of aspirin, clopidogrel, and apixaban (CHA<sub>2</sub>DS<sub>2</sub>-VASc score of 3 and HAS-BLED score of 1). He reports that he was not able to keep his follow-up appointment 1 month after his PCI because of personal issues and did not keep the later appointments because of the COVID-19 pandemic. He has had no complaints during this period and has been highly compliant with the aspirin, clopidogrel, and apixaban regimen. Which of the following is the next best step?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
948069 | /viewarticle/948069 | [
{
"authors": "Maurie Markman, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us .",
"A 58-year-old woman seeks medical attention after she discovered a new mass in her left axilla during a routine monthly breast self-examination while showering. She has not noted any changes in either of her breasts. The mass in her left axilla is not tender, and she has not felt any other abnormal masses, including in her right axilla. She reports no other symptoms and specifically has no pain anywhere in her body. She also does not have shortness of breath, fever, night sweats, fatigue, rash, or abdominal discomfort or bloating.",
"Fifteen years earlier, the patient was diagnosed with high-grade, stage 1 cervical cancer and underwent surgery and chemoradiation. She has been closely monitored since that time with physical examinations and abdominal CT, with no evidence of recurrent disease. The patient has not had any other surgical procedure, except for removal of two basal cell carcinomas on her neck 4 years ago. She has had yearly routine mammograms for at least the past 15 years.",
"The patient has hypertension, which has been well controlled with the same medications for the past 10 years. She also has a 25-year history of type 2 diabetes mellitus, which is currently managed with diet alone. She had a \"silent myocardial infarction\" sometime within the past 5 years but has had no cardiac symptoms and is not taking any cardiac medications. She smoked approximately one pack of cigarettes a day for less than 2 years when she was \"in her teens\" but has not had any tobacco products since that time.",
"Pancreatic cancer was diagnosed in the patient's father at age 49 years, and breast cancer was diagnosed in her aunt on her father's side at age 67 years. Her paternal grandmother is reported to have died in her 60s after diagnosis of a \"cancer in her stomach.\" No further information is available regarding either the actual diagnosis or the medical care provided to this individual.",
"To the best of the patient's knowledge, her mother's side of the family and her two brothers have no history of cancer. She has no sisters. Her mother is in her 80s and has mild dementia. The patient is not aware of any member of her family having undergone genetic testing."
],
"date": "March 30, 2021",
"figures": [],
"markdown": "# Pleural Effusion and an Axillary Mass in a Woman With Hypertension\n\n **Authors:** Maurie Markman, MD \n **Date:** March 30, 2021\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us .\nA 58-year-old woman seeks medical attention after she discovered a new mass in her left axilla during a routine monthly breast self-examination while showering. She has not noted any changes in either of her breasts. The mass in her left axilla is not tender, and she has not felt any other abnormal masses, including in her right axilla. She reports no other symptoms and specifically has no pain anywhere in her body. She also does not have shortness of breath, fever, night sweats, fatigue, rash, or abdominal discomfort or bloating.\nFifteen years earlier, the patient was diagnosed with high-grade, stage 1 cervical cancer and underwent surgery and chemoradiation. She has been closely monitored since that time with physical examinations and abdominal CT, with no evidence of recurrent disease. The patient has not had any other surgical procedure, except for removal of two basal cell carcinomas on her neck 4 years ago. She has had yearly routine mammograms for at least the past 15 years.\nThe patient has hypertension, which has been well controlled with the same medications for the past 10 years. She also has a 25-year history of type 2 diabetes mellitus, which is currently managed with diet alone. She had a \"silent myocardial infarction\" sometime within the past 5 years but has had no cardiac symptoms and is not taking any cardiac medications. She smoked approximately one pack of cigarettes a day for less than 2 years when she was \"in her teens\" but has not had any tobacco products since that time.\nPancreatic cancer was diagnosed in the patient's father at age 49 years, and breast cancer was diagnosed in her aunt on her father's side at age 67 years. Her paternal grandmother is reported to have died in her 60s after diagnosis of a \"cancer in her stomach.\" No further information is available regarding either the actual diagnosis or the medical care provided to this individual.\nTo the best of the patient's knowledge, her mother's side of the family and her two brothers have no history of cancer. She has no sisters. Her mother is in her 80s and has mild dementia. The patient is not aware of any member of her family having undergone genetic testing.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Pleural Effusion and an Axillary Mass in a Woman With Hypertension"
},
{
"authors": "Maurie Markman, MD",
"content": [
"The patient appears well and is in no acute distress. The patient is afebrile, with a blood pressure of 135/85 mm Hg, a respiratory rate of 16 breaths/min, and a pulse of 72 beats/min. Her weight is 148 lb (67 kg), and she has no reported recent weight loss.",
"Examination of the skin reveals no suspicious lesions. Scars from the previous removal of the basal cell carcinomas are noted, but no evidence suggests recurrence.",
"Results of the head and neck examination are unremarkable; specifically, no abnormal cervical lymphadenopathy is detected. The cardiac and chest examination results are normal. The lungs are clear to percussion and auscultation. The breast examination reveals no abnormal masses. The right axilla is unremarkable; however, a single 3 × 2 cm, nontender, firm, movable but partially fixed mass is noted in the left axilla.",
"The abdomen appears normal, with no ascites or enlargement of the liver. The pelvic examination reveals evidence of previous surgery and local radiation but no signs of recurrence of cervical cancer. The lymph nodes appear normal, except for the findings noted above. Results of the neurologic examination are unremarkable.",
"Complete blood cell count, serum electrolyte levels, renal function tests, and urinalysis are all normal. Liver function tests are normal except for a mildly elevated serum alkaline phosphatase level. The fecal occult blood test result is negative.",
"Chest radiography reveals a suspicious small left-sided pleural effusion. No other abnormalities are observed, and no prior chest radiographs are available to compare with the current findings.",
"Chest CT confirms the presence of a possible small pleural effusion, with no other abnormalities noted. The radiologist suggests it will not be possible to obtain fluid safely through an interventional procedure, owing to the limited (if any) amount of fluid present. Furthermore, the radiologist recommends PET/CT to look for other evidence of metastatic cancer in the lungs or elsewhere.",
"Bilateral mammograms reveal no suspicious abnormalities, and the results are unchanged from a previous examination 11 months earlier. Figure 1 shows a similar bilateral mammogram in another patient. Breast MRI shows no evidence of cancer. Figure 2 shows similar breast MRI findings in another patient.",
"Figure 1.",
"Figure 2.",
"CT of the abdomen and pelvis reveals no changes compared with a scan obtained 2 years earlier for follow-up of the previous diagnosis of cervical cancer. Specifically, no evidence suggests ascites or any pelvic masses.",
"An incisional biopsy sample is obtained from the left axillary mass. Light microscopy reveals a moderately well-differentiated adenocarcinoma. Immunostaining shows the cancer to be cytokeratin (CK) 7 positive and CK 20 negative (CK 7+/CK 20-, thyroid transcription factor 1 (TTF-1) negative, thyroglobulin negative, napsin A negative, and mammaglobin positive. The tumor is estrogen receptor positive (2% staining), progesterone receptor negative, and human epidermal growth factor receptor 2 (HER2) negative."
],
"date": "March 30, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/948/069/948069-Thumb1.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/948/069/948069-Thumb2.jpg"
}
],
"markdown": "# Pleural Effusion and an Axillary Mass in a Woman With Hypertension\n\n **Authors:** Maurie Markman, MD \n **Date:** March 30, 2021\n\n ## Content\n\n The patient appears well and is in no acute distress. The patient is afebrile, with a blood pressure of 135/85 mm Hg, a respiratory rate of 16 breaths/min, and a pulse of 72 beats/min. Her weight is 148 lb (67 kg), and she has no reported recent weight loss.\nExamination of the skin reveals no suspicious lesions. Scars from the previous removal of the basal cell carcinomas are noted, but no evidence suggests recurrence.\nResults of the head and neck examination are unremarkable; specifically, no abnormal cervical lymphadenopathy is detected. The cardiac and chest examination results are normal. The lungs are clear to percussion and auscultation. The breast examination reveals no abnormal masses. The right axilla is unremarkable; however, a single 3 × 2 cm, nontender, firm, movable but partially fixed mass is noted in the left axilla.\nThe abdomen appears normal, with no ascites or enlargement of the liver. The pelvic examination reveals evidence of previous surgery and local radiation but no signs of recurrence of cervical cancer. The lymph nodes appear normal, except for the findings noted above. Results of the neurologic examination are unremarkable.\nComplete blood cell count, serum electrolyte levels, renal function tests, and urinalysis are all normal. Liver function tests are normal except for a mildly elevated serum alkaline phosphatase level. The fecal occult blood test result is negative.\nChest radiography reveals a suspicious small left-sided pleural effusion. No other abnormalities are observed, and no prior chest radiographs are available to compare with the current findings.\nChest CT confirms the presence of a possible small pleural effusion, with no other abnormalities noted. The radiologist suggests it will not be possible to obtain fluid safely through an interventional procedure, owing to the limited (if any) amount of fluid present. Furthermore, the radiologist recommends PET/CT to look for other evidence of metastatic cancer in the lungs or elsewhere.\nBilateral mammograms reveal no suspicious abnormalities, and the results are unchanged from a previous examination 11 months earlier. Figure 1 shows a similar bilateral mammogram in another patient. Breast MRI shows no evidence of cancer. Figure 2 shows similar breast MRI findings in another patient.\nFigure 1.\nFigure 2.\nCT of the abdomen and pelvis reveals no changes compared with a scan obtained 2 years earlier for follow-up of the previous diagnosis of cervical cancer. Specifically, no evidence suggests ascites or any pelvic masses.\nAn incisional biopsy sample is obtained from the left axillary mass. Light microscopy reveals a moderately well-differentiated adenocarcinoma. Immunostaining shows the cancer to be cytokeratin (CK) 7 positive and CK 20 negative (CK 7+/CK 20-, thyroid transcription factor 1 (TTF-1) negative, thyroglobulin negative, napsin A negative, and mammaglobin positive. The tumor is estrogen receptor positive (2% staining), progesterone receptor negative, and human epidermal growth factor receptor 2 (HER2) negative.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1575616,
"choiceText": "Lung",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575617,
"choiceText": "Cervix",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575618,
"choiceText": "Stomach",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575619,
"choiceText": "Breast",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575620,
"choiceText": "Oropharynx",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 505791,
"questionText": "On the basis of these findings only, which is the most likely site of origin of this cancer?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Pleural Effusion and an Axillary Mass in a Woman With Hypertension"
},
{
"authors": "Maurie Markman, MD",
"content": [
"This case is a classic example of cancer of unknown primary site or origin (CUP). CUP represents approximately 5% of cancers diagnosed in the United States (50,000 to 60,000 cases each year), with various series reporting that the site of origin is not diagnosed in between 2% and 6% of all cancer cases.[1] Worldwide, the incidence of CUP is even higher, resulting from the limited availability of sophisticated (and expensive) diagnostic technology in many regions. The median age at diagnosis of CUP is 60 years, and men and women are equally likely to be affected.",
"A cancer is considered a CUP if, after routine clinical assessment, physical and laboratory examination, standard imaging studies, and routine pathologic evaluation (biopsy or surgical removal of a metastatic mass lesion), a site of origin cannot be defined. With the availability of more sophisticated imaging technologies (eg, MRI), the overall percentage of cancers that are defined as a CUP has been reduced. However, even at autopsy, the site of origin of such cancer is often unable to be determined if the location was unknown before the patient's death.",
"Several theories have been proposed for why a metastatic lesion becomes clinically evident despite the site of origin of the cancer remaining obscure. These include (1) very slow growth of the primary cancer compared with that of the metastasis; (2) spontaneous regression of the primary cancer; (3) a prominent vascular component of the cancer, which enhances the rate of spread; and (4) unique molecular events associated with the cancer, which result in rapid progression and the growth of metastatic lesions.",
"Approximately 60% of CUPs are adenocarcinomas (well or moderately well differentiated); 25%-30% are poorly differentiated (including poorly differentiated adenocarcinomas); 5% are completely undifferentiated, with no defining histologic features; 5% are squamous cell cancers; and approximately 1% are carcinomas, with evidence of neuroendocrine differentiation.[1]"
],
"date": "March 30, 2021",
"figures": [],
"markdown": "# Pleural Effusion and an Axillary Mass in a Woman With Hypertension\n\n **Authors:** Maurie Markman, MD \n **Date:** March 30, 2021\n\n ## Content\n\n This case is a classic example of cancer of unknown primary site or origin (CUP). CUP represents approximately 5% of cancers diagnosed in the United States (50,000 to 60,000 cases each year), with various series reporting that the site of origin is not diagnosed in between 2% and 6% of all cancer cases.[1] Worldwide, the incidence of CUP is even higher, resulting from the limited availability of sophisticated (and expensive) diagnostic technology in many regions. The median age at diagnosis of CUP is 60 years, and men and women are equally likely to be affected.\nA cancer is considered a CUP if, after routine clinical assessment, physical and laboratory examination, standard imaging studies, and routine pathologic evaluation (biopsy or surgical removal of a metastatic mass lesion), a site of origin cannot be defined. With the availability of more sophisticated imaging technologies (eg, MRI), the overall percentage of cancers that are defined as a CUP has been reduced. However, even at autopsy, the site of origin of such cancer is often unable to be determined if the location was unknown before the patient's death.\nSeveral theories have been proposed for why a metastatic lesion becomes clinically evident despite the site of origin of the cancer remaining obscure. These include (1) very slow growth of the primary cancer compared with that of the metastasis; (2) spontaneous regression of the primary cancer; (3) a prominent vascular component of the cancer, which enhances the rate of spread; and (4) unique molecular events associated with the cancer, which result in rapid progression and the growth of metastatic lesions.\nApproximately 60% of CUPs are adenocarcinomas (well or moderately well differentiated); 25%-30% are poorly differentiated (including poorly differentiated adenocarcinomas); 5% are completely undifferentiated, with no defining histologic features; 5% are squamous cell cancers; and approximately 1% are carcinomas, with evidence of neuroendocrine differentiation.[1]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1575616,
"choiceText": "Lung",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575617,
"choiceText": "Cervix",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575618,
"choiceText": "Stomach",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575619,
"choiceText": "Breast",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575620,
"choiceText": "Oropharynx",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 505791,
"questionText": "On the basis of these findings only, which is the most likely site of origin of this cancer?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Pleural Effusion and an Axillary Mass in a Woman With Hypertension"
},
{
"authors": "Maurie Markman, MD",
"content": [
"Immunohistochemical staining of biopsy material can be helpful in narrowing the possible anatomical sites of origin. The results are particularly relevant in the selection of therapeutic strategies and in ensuring that a rare, potentially highly curable cancer is not missed (eg, lymphoma, germ cell tumor).[2]",
"A critical initial test is examination of several CK subtypes that are more likely to be expressed in certain carcinomas than in others. For example, the CK 7+/CK 20- staining seen in this patient is characteristic of breast and lung cancers (among others), whereas CK 7+/CK 20+ staining would be expected in pancreatic, gastric, and urothelial cancers. A CK 7-/CK 20+ finding would be more suggestive of colon or mucinous ovarian cancer. Furthermore, approximately 70% of lung adenocarcinomas are TTF-1 positive and 60%-80% are napsin A positive. The negative findings in this patient's case make the diagnosis of metastatic lung cancer less likely.",
"Examination for the presence (or absence) of well-established biomarkers for breast cancer can potentially be helpful in suggesting the site of origin or in helping to define subsequent therapy. These markers include estrogen and progesterone receptors and HER2 overexpression. An additional biomarker, mammaglobin, has been reported to be expressed in 48% of breast cancers but is absent in cancers of the lung, gastrointestinal tract, ovary, and head and neck region.[2]",
"Of note, mammaglobin was found to be expressed in this patient. Although only 2% of the cells were reported to stain for the estrogen receptor, this finding is still considered positive and supports breast cancer as the correct diagnosis.",
"Recognized relevant prognostic factors in CUP include baseline performance status, the number and location of metastatic lesions, and the response to cytotoxic chemotherapy.",
"Unfortunately, the overall prognosis associated with a diagnosis of CUP is poor, with median survival in various series reported to be less than 6 months. However, important exceptions to this outcome include women who present with an isolated metastatic axillary mass, as described in this case.",
"Previous reports of axillary adenopathy as the initial presentation of cancer in women revealed that the majority had evidence of cancer in the breast at the time of subsequent mastectomy.[3,4] As a result, in the absence of other indications found during routine workup (eg, a single pulmonary lesion suggestive of a primary lung cancer, pathologic findings inconsistent with breast cancer), an isolated adenocarcinoma in the breast (with no evidence of metastatic cancer elsewhere) should be treated as either stage II or stage III breast cancer. Note that this recommendation specifically relates to female patients. If a male patient has CUP with an isolated axillary mass, it is generally assumed that the lung is the origin of the malignancy."
],
"date": "March 30, 2021",
"figures": [],
"markdown": "# Pleural Effusion and an Axillary Mass in a Woman With Hypertension\n\n **Authors:** Maurie Markman, MD \n **Date:** March 30, 2021\n\n ## Content\n\n Immunohistochemical staining of biopsy material can be helpful in narrowing the possible anatomical sites of origin. The results are particularly relevant in the selection of therapeutic strategies and in ensuring that a rare, potentially highly curable cancer is not missed (eg, lymphoma, germ cell tumor).[2]\nA critical initial test is examination of several CK subtypes that are more likely to be expressed in certain carcinomas than in others. For example, the CK 7+/CK 20- staining seen in this patient is characteristic of breast and lung cancers (among others), whereas CK 7+/CK 20+ staining would be expected in pancreatic, gastric, and urothelial cancers. A CK 7-/CK 20+ finding would be more suggestive of colon or mucinous ovarian cancer. Furthermore, approximately 70% of lung adenocarcinomas are TTF-1 positive and 60%-80% are napsin A positive. The negative findings in this patient's case make the diagnosis of metastatic lung cancer less likely.\nExamination for the presence (or absence) of well-established biomarkers for breast cancer can potentially be helpful in suggesting the site of origin or in helping to define subsequent therapy. These markers include estrogen and progesterone receptors and HER2 overexpression. An additional biomarker, mammaglobin, has been reported to be expressed in 48% of breast cancers but is absent in cancers of the lung, gastrointestinal tract, ovary, and head and neck region.[2]\nOf note, mammaglobin was found to be expressed in this patient. Although only 2% of the cells were reported to stain for the estrogen receptor, this finding is still considered positive and supports breast cancer as the correct diagnosis.\nRecognized relevant prognostic factors in CUP include baseline performance status, the number and location of metastatic lesions, and the response to cytotoxic chemotherapy.\nUnfortunately, the overall prognosis associated with a diagnosis of CUP is poor, with median survival in various series reported to be less than 6 months. However, important exceptions to this outcome include women who present with an isolated metastatic axillary mass, as described in this case.\nPrevious reports of axillary adenopathy as the initial presentation of cancer in women revealed that the majority had evidence of cancer in the breast at the time of subsequent mastectomy.[3,4] As a result, in the absence of other indications found during routine workup (eg, a single pulmonary lesion suggestive of a primary lung cancer, pathologic findings inconsistent with breast cancer), an isolated adenocarcinoma in the breast (with no evidence of metastatic cancer elsewhere) should be treated as either stage II or stage III breast cancer. Note that this recommendation specifically relates to female patients. If a male patient has CUP with an isolated axillary mass, it is generally assumed that the lung is the origin of the malignancy.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Pleural Effusion and an Axillary Mass in a Woman With Hypertension"
},
{
"authors": "Maurie Markman, MD",
"content": [
"In a female patient with negative mammographic findings, breast MRI can be helpful. In one series, 28 of 40 women (70%) with evidence of cancer in the axilla and a normal mammogram were found to have a breast abnormality on MRI.[5] Of note, and of considerable relevance to subsequent disease management, five of the 12 women with negative findings in this series underwent surgery, and in four of the cases no cancer was found. Although the number of participants in this series is limited, the absence of an MRI abnormality in the patient in this case can reasonably be considered in her future treatment plans.",
"Specifically, it might be suggested in this case that treatment include surgical removal of the axillary mass (if possible) followed by radiation to this area and the breast (rather than performing a mastectomy). Alternatively, treatment might begin with chemotherapy (a neoadjuvant approach) followed by surgery to remove any residual axillary mass and local/regional radiation or local/regional radiation alone. Adjuvant chemotherapy and/or hormonal therapy would then be administered.",
"The presence of a possible small pleural effusion is a concern because it potentially indicates more widespread metastatic disease, as does the mild elevation of the serum alkaline phosphatase level (eg, suggesting metastatic disease in bone or the liver). In the absence of other evidence of tumor spread, PET would not be unreasonable. A negative scan for evidence of metastatic disease would support a \"curative\" approach to the management of local disease in the axilla and presumably the breast, whereas a finding of other metastatic sites would lead to the conclusion that treatment should probably be delivered with more palliative intent.",
"The family history of cancer (father, paternal aunt with breast cancer, paternal grandmother with possible ovarian cancer) is intriguing and would suggest a role for genetic counseling and possibly genetic testing (eg, for BRCA mutation).",
"The patient in this case underwent PET. The only abnormality observed was in the left axilla. The axillary mass was subsequently resected. This was followed by curative radiation to both the axilla and left breast, adjuvant chemotherapy, and 5 years of hormonal therapy. The patient has showed no evidence of recurrence 2 years after completion of the hormonal treatment."
],
"date": "March 30, 2021",
"figures": [],
"markdown": "# Pleural Effusion and an Axillary Mass in a Woman With Hypertension\n\n **Authors:** Maurie Markman, MD \n **Date:** March 30, 2021\n\n ## Content\n\n In a female patient with negative mammographic findings, breast MRI can be helpful. In one series, 28 of 40 women (70%) with evidence of cancer in the axilla and a normal mammogram were found to have a breast abnormality on MRI.[5] Of note, and of considerable relevance to subsequent disease management, five of the 12 women with negative findings in this series underwent surgery, and in four of the cases no cancer was found. Although the number of participants in this series is limited, the absence of an MRI abnormality in the patient in this case can reasonably be considered in her future treatment plans.\nSpecifically, it might be suggested in this case that treatment include surgical removal of the axillary mass (if possible) followed by radiation to this area and the breast (rather than performing a mastectomy). Alternatively, treatment might begin with chemotherapy (a neoadjuvant approach) followed by surgery to remove any residual axillary mass and local/regional radiation or local/regional radiation alone. Adjuvant chemotherapy and/or hormonal therapy would then be administered.\nThe presence of a possible small pleural effusion is a concern because it potentially indicates more widespread metastatic disease, as does the mild elevation of the serum alkaline phosphatase level (eg, suggesting metastatic disease in bone or the liver). In the absence of other evidence of tumor spread, PET would not be unreasonable. A negative scan for evidence of metastatic disease would support a \"curative\" approach to the management of local disease in the axilla and presumably the breast, whereas a finding of other metastatic sites would lead to the conclusion that treatment should probably be delivered with more palliative intent.\nThe family history of cancer (father, paternal aunt with breast cancer, paternal grandmother with possible ovarian cancer) is intriguing and would suggest a role for genetic counseling and possibly genetic testing (eg, for BRCA mutation).\nThe patient in this case underwent PET. The only abnormality observed was in the left axilla. The axillary mass was subsequently resected. This was followed by curative radiation to both the axilla and left breast, adjuvant chemotherapy, and 5 years of hormonal therapy. The patient has showed no evidence of recurrence 2 years after completion of the hormonal treatment.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1575621,
"choiceText": "Pancreas",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575622,
"choiceText": "Breast",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575623,
"choiceText": "Colon",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575624,
"choiceText": "Oropharynx",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575625,
"choiceText": "Lung",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The lungs are generally assumed to be the site of origin of the cancer in a male patient who has CUP with an isolated axillary mass. In contrast, the majority of women with axillary adenopathy as the initial presentation of cancer were found to have evidence of cancer in the breast at the time of subsequent mastectomy.<sup>[3,4]</sup>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 505792,
"questionText": "In a man with an isolated axillary finding of adenocarcinoma, which is the most likely site of origin of the cancer?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1575630,
"choiceText": "CT",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575631,
"choiceText": "PET",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575632,
"choiceText": "MRI",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575633,
"choiceText": "Ultrasonography",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nBreast MRI can be helpful in a female patient with negative mammographic findings. In one series, MRI detected a breast abnormality in 28 of 40 women (70%) with evidence of cancer in the axilla and a normal mammogram.<sup>[5]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 505794,
"questionText": "\r\n\r\nWhich study is most likely to find an abnormality consistent with breast cancer in a woman with an adenocarcinoma in the axilla and a negative mammogram?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Pleural Effusion and an Axillary Mass in a Woman With Hypertension"
},
{
"authors": "Maurie Markman, MD",
"content": [],
"date": "March 30, 2021",
"figures": [],
"markdown": "# Pleural Effusion and an Axillary Mass in a Woman With Hypertension\n\n **Authors:** Maurie Markman, MD \n **Date:** March 30, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1575621,
"choiceText": "Pancreas",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575622,
"choiceText": "Breast",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575623,
"choiceText": "Colon",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575624,
"choiceText": "Oropharynx",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575625,
"choiceText": "Lung",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The lungs are generally assumed to be the site of origin of the cancer in a male patient who has CUP with an isolated axillary mass. In contrast, the majority of women with axillary adenopathy as the initial presentation of cancer were found to have evidence of cancer in the breast at the time of subsequent mastectomy.<sup>[3,4]</sup>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 505792,
"questionText": "In a man with an isolated axillary finding of adenocarcinoma, which is the most likely site of origin of the cancer?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1575630,
"choiceText": "CT",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575631,
"choiceText": "PET",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575632,
"choiceText": "MRI",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575633,
"choiceText": "Ultrasonography",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nBreast MRI can be helpful in a female patient with negative mammographic findings. In one series, MRI detected a breast abnormality in 28 of 40 women (70%) with evidence of cancer in the axilla and a normal mammogram.<sup>[5]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 505794,
"questionText": "\r\n\r\nWhich study is most likely to find an abnormality consistent with breast cancer in a woman with an adenocarcinoma in the axilla and a negative mammogram?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Pleural Effusion and an Axillary Mass in a Woman With Hypertension"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1575616,
"choiceText": "Lung",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575617,
"choiceText": "Cervix",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575618,
"choiceText": "Stomach",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575619,
"choiceText": "Breast",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575620,
"choiceText": "Oropharynx",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 505791,
"questionText": "On the basis of these findings only, which is the most likely site of origin of this cancer?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1575621,
"choiceText": "Pancreas",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575622,
"choiceText": "Breast",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575623,
"choiceText": "Colon",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575624,
"choiceText": "Oropharynx",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575625,
"choiceText": "Lung",
"correct": true,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The lungs are generally assumed to be the site of origin of the cancer in a male patient who has CUP with an isolated axillary mass. In contrast, the majority of women with axillary adenopathy as the initial presentation of cancer were found to have evidence of cancer in the breast at the time of subsequent mastectomy.<sup>[3,4]</sup>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 505792,
"questionText": "In a man with an isolated axillary finding of adenocarcinoma, which is the most likely site of origin of the cancer?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1575630,
"choiceText": "CT",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575631,
"choiceText": "PET",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575632,
"choiceText": "MRI",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1575633,
"choiceText": "Ultrasonography",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nBreast MRI can be helpful in a female patient with negative mammographic findings. In one series, MRI detected a breast abnormality in 28 of 40 women (70%) with evidence of cancer in the axilla and a normal mammogram.<sup>[5]</sup>",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 505794,
"questionText": "\r\n\r\nWhich study is most likely to find an abnormality consistent with breast cancer in a woman with an adenocarcinoma in the axilla and a negative mammogram?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
878375 | /viewarticle/878375 | [
{
"authors": "John G. Christensen, Jr, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 42-year-old woman presents with a history of chronic leg and lower back pain lasting several years. She has no history of flank pain or gross or microscopic hematuria. She does not report any fevers, appetite loss, weight loss, or obesity.",
"She is a nonsmoker and drinks a glass of wine with dinner 2-3 nights a week. She works as an office assistant and is not exposed to any solvents or chemicals. Her medical history is free of chronic illness, and she has no family history of renal tumors, skin lesions, seizures, or cognitive delay."
],
"date": "March 05, 2021",
"figures": [],
"markdown": "# A 42-Year-Old Office Assistant With Chronic Leg and Back Pain\n\n **Authors:** John G. Christensen, Jr, MD \n **Date:** March 05, 2021\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 42-year-old woman presents with a history of chronic leg and lower back pain lasting several years. She has no history of flank pain or gross or microscopic hematuria. She does not report any fevers, appetite loss, weight loss, or obesity.\nShe is a nonsmoker and drinks a glass of wine with dinner 2-3 nights a week. She works as an office assistant and is not exposed to any solvents or chemicals. Her medical history is free of chronic illness, and she has no family history of renal tumors, skin lesions, seizures, or cognitive delay.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A 42-Year-Old Office Assistant With Chronic Leg and Back Pain"
},
{
"authors": "John G. Christensen, Jr, MD",
"content": [
"The physical examination reveals a healthy-appearing, nonobese female. She has no axillary, cervical, or inguinal adenopathy. Her lung sounds are clear. Heart auscultation reveals regular rhythm with no murmurs. Abdominal examination findings are negative, with no tenderness or mass. No flank tenderness or mass is noted. Lower extremities are normal without edema.",
"Metabolic panel findings are normal, including normal creatinine levels, liver function test results, and calcium levels.",
"Laboratory studies reveal normal urinalysis without red blood cells or protein. A complete blood cell count reveals normal hemoglobin level, hematocrit level, and white blood cell count.",
"After structural issues were ruled out, a spinal MRI is eventually performed as part of the investigation into her leg and lower back pain. Findings prompt CT scanning with and without contrast. See Figures 1-2 below.",
"Figure 1.",
"Figure 2."
],
"date": "March 05, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/878/375/878375-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/878/375/878375-Thumb2.png"
}
],
"markdown": "# A 42-Year-Old Office Assistant With Chronic Leg and Back Pain\n\n **Authors:** John G. Christensen, Jr, MD \n **Date:** March 05, 2021\n\n ## Content\n\n The physical examination reveals a healthy-appearing, nonobese female. She has no axillary, cervical, or inguinal adenopathy. Her lung sounds are clear. Heart auscultation reveals regular rhythm with no murmurs. Abdominal examination findings are negative, with no tenderness or mass. No flank tenderness or mass is noted. Lower extremities are normal without edema.\nMetabolic panel findings are normal, including normal creatinine levels, liver function test results, and calcium levels.\nLaboratory studies reveal normal urinalysis without red blood cells or protein. A complete blood cell count reveals normal hemoglobin level, hematocrit level, and white blood cell count.\nAfter structural issues were ruled out, a spinal MRI is eventually performed as part of the investigation into her leg and lower back pain. Findings prompt CT scanning with and without contrast. See Figures 1-2 below.\nFigure 1.\nFigure 2.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1085390,
"choiceText": "Hyperdense renal cyst",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085392,
"choiceText": "Renal cell carcinoma",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085394,
"choiceText": "Oncocytoma",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085396,
"choiceText": "Angiomyolipoma\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 343771,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 42-Year-Old Office Assistant With Chronic Leg and Back Pain"
},
{
"authors": "John G. Christensen, Jr, MD",
"content": [
"The CT scan with and without contrast reveals a 2-cm, solid, enhancing, right lower pole exophytic mass confined to the kidney and no enlarged lymph nodes or signs of metastasis. No fat content by CT scan criteria is noted.",
"Only 20% of small solid renal masses that are suspicious for renal cell carcinoma (RCC) on CT scan are benign (oncocytoma or atypical, fat-poor angiomyolipoma); 60% are relatively indolent RCCs, and about 20% demonstrate potentially aggressive histologic features, making RCC the most likely diagnostic option above, given the findings presented.[1] The incidence of more aggressive cell types increases in lesions over 3 cm.[2] Other causes of renal mass include abscess, angiomyolipoma, urothelial carcinoma, metastatic lesions to kidney, infarct or scar, vascular malformations, and pseudotumor.",
"More than 50% of RCCs are now found incidentally in asymptomatic patients undergoing imaging for other purposes. Most of these are T1 (7 cm or smaller, confined to the kidney). The \"classic triad\" of flank pain, flank mass, and hematuria occurs in 10% of cases and is indicative of advanced disease.[3] The individual components are seen more frequently, with hematuria present in 40% of presentations, flank pain present in 40%, and a palpable mass present in 25%. Other presenting symptoms include weight loss, fever, hypertension, hypercalcemia, night sweats, malaise, abnormal liver function test results (not necessarily indicative of metastatic disease to the liver), and varicocele (especially left side due to spermatic vein compression).[3]",
"RCC occurs at an annual rate of about 17 new cases per 100,000 population in the United States, with an average age at diagnosis in the early 60s. Overall, about 35% of patients diagnosed with RCC eventually succumb to the disease. The stage at presentation strongly affects survival and cure rates.",
"The risk of developing RCC may be reduced through fruit, vegetable, and fatty fish consumption and by moderate alcohol consumption. Cigarette smoking doubles the risk for RCC and may contribute to as many as one third of all cases. Obesity is also a significant risk factor. Family history is also associated with increased risk for RCC. At least four hereditary syndromes are associated with RCC: von Hippel-Lindau syndrome, hereditary papillary renal carcinoma, familial renal oncocytoma associated with Birt-Hogg-Dube syndrome, and hereditary renal carcinoma.[3] Long-term dialysis, especially with acquired cystic disease of the kidney, is associated with an increased risk of developing RCC."
],
"date": "March 05, 2021",
"figures": [],
"markdown": "# A 42-Year-Old Office Assistant With Chronic Leg and Back Pain\n\n **Authors:** John G. Christensen, Jr, MD \n **Date:** March 05, 2021\n\n ## Content\n\n The CT scan with and without contrast reveals a 2-cm, solid, enhancing, right lower pole exophytic mass confined to the kidney and no enlarged lymph nodes or signs of metastasis. No fat content by CT scan criteria is noted.\nOnly 20% of small solid renal masses that are suspicious for renal cell carcinoma (RCC) on CT scan are benign (oncocytoma or atypical, fat-poor angiomyolipoma); 60% are relatively indolent RCCs, and about 20% demonstrate potentially aggressive histologic features, making RCC the most likely diagnostic option above, given the findings presented.[1] The incidence of more aggressive cell types increases in lesions over 3 cm.[2] Other causes of renal mass include abscess, angiomyolipoma, urothelial carcinoma, metastatic lesions to kidney, infarct or scar, vascular malformations, and pseudotumor.\nMore than 50% of RCCs are now found incidentally in asymptomatic patients undergoing imaging for other purposes. Most of these are T1 (7 cm or smaller, confined to the kidney). The \"classic triad\" of flank pain, flank mass, and hematuria occurs in 10% of cases and is indicative of advanced disease.[3] The individual components are seen more frequently, with hematuria present in 40% of presentations, flank pain present in 40%, and a palpable mass present in 25%. Other presenting symptoms include weight loss, fever, hypertension, hypercalcemia, night sweats, malaise, abnormal liver function test results (not necessarily indicative of metastatic disease to the liver), and varicocele (especially left side due to spermatic vein compression).[3]\nRCC occurs at an annual rate of about 17 new cases per 100,000 population in the United States, with an average age at diagnosis in the early 60s. Overall, about 35% of patients diagnosed with RCC eventually succumb to the disease. The stage at presentation strongly affects survival and cure rates.\nThe risk of developing RCC may be reduced through fruit, vegetable, and fatty fish consumption and by moderate alcohol consumption. Cigarette smoking doubles the risk for RCC and may contribute to as many as one third of all cases. Obesity is also a significant risk factor. Family history is also associated with increased risk for RCC. At least four hereditary syndromes are associated with RCC: von Hippel-Lindau syndrome, hereditary papillary renal carcinoma, familial renal oncocytoma associated with Birt-Hogg-Dube syndrome, and hereditary renal carcinoma.[3] Long-term dialysis, especially with acquired cystic disease of the kidney, is associated with an increased risk of developing RCC.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1085390,
"choiceText": "Hyperdense renal cyst",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085392,
"choiceText": "Renal cell carcinoma",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085394,
"choiceText": "Oncocytoma",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085396,
"choiceText": "Angiomyolipoma\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 343771,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 42-Year-Old Office Assistant With Chronic Leg and Back Pain"
},
{
"authors": "John G. Christensen, Jr, MD",
"content": [
"RCC subtypes include clear cell (roughly 75%), papillary, chromophobe, collecting duct, and unclassified.[1] The papillary and chromophobe subtypes may portend better survival. The Fuhrman cellular grade of clear cell carcinoma is an independent predictor of survival. Sarcomatoid features can be found in any subtype and are associated with a worse prognosis. Oncocytoma, which may be associated with a central star-shaped density on CT scanning, does not metastasize and is considered a benign renal mass.",
"The presence of fat in a renal mass on CT or MRI images is pathognomonic of benign angiomyolipoma. Otherwise, solid renal masses should be considered likely malignant (≥80%) and possibly aggressive (≥20%) and treated as such.",
"The TNM staging for RCC is as follows[3,4]:",
"T1—Tumor ≤7 cm, limited to kidney",
"T1a—Tumor ≤4 cm",
"T1b—Tumor >4 cm and ≤7 cm",
"T2—Tumor >7 cm but limited to kidney",
"T3—Tumor involves renal vein, inferior vena cava (IVC), or perirenal fat but contained within Gerota fascia",
"T4—Tumor invades beyond Gerota fascia",
"American Joint Committee on Cancer staging is as follows[3,4]:",
"Stage I—T1, N0M0",
"Stage II—T2, N0M0",
"Stage III—T3, N0M0 or T1-3, N1M0",
"Stage IV—T4, N0-1M0; any T with M1",
"Tumor size is a strong predictor of survival. The 5-year disease-specific survival by T stage for RCC is as follows[3]:",
"T1—95%",
"T2—88%",
"T3—59%",
"T4—20%",
"The Fuhrman Nuclear Grading System is an independent predictor of survival. In patients with T1 disease, the 5-year cancer-specific survival rates after surgery are as follows[5]:",
"Fuhrman Grade 1—91%",
"Fuhrman Grade 2—83%",
"Fuhrman Grade 3—60%",
"Fuhrman Grade 4—0%",
"The objectives of imaging a renal mass are to rule out benign angiomyolipoma (any fat density seen), to evaluate for locally invasive features, to study the involved anatomy (for surgical planning), and to determine the status of the uninvolved kidney.[3]",
"Contrast-enhanced CT scanning is the imaging procedure of choice for diagnosis and staging of renal masses when renal function is adequate. Typically, this is a CT scan of the abdomen and pelvis without and then with contrast; this may include a delayed urogram phase.[1,2,3] Contrast-enhanced MRI is an optional imaging modality for initial evaluation. MRI is also recommended if renal vein or IVC involvement is in question. Urinary calculi may not show up on MRI.",
"Renal ultrasonography can be useful in evaluating cystic masses if CT imaging is inconclusive; however, ultrasonography may miss isodense renal tumors or transitional cell tumors of the renal collecting system.[3] Angiomyolipomas are suspected based on the high echogenicity of fat; however, a CT scan is more definitive.",
"Intravenous pyelography is inadequate to evaluate a renal mass due to low sensitivity and specificity.[3] Bone scanning is not routinely performed unless bone pain, elevated alkaline phosphatase, or other suspicion of bony metastases is present. The role of PET scanning in RCC has yet to be determined.[4]",
"Brain MRI or CT scanning can be performed if clinical signs or symptoms are suspicious for brain metastases.[4] Chest imaging (radiography or CT scanning) should be routinely included in the workup of a solid renal mass."
],
"date": "March 05, 2021",
"figures": [],
"markdown": "# A 42-Year-Old Office Assistant With Chronic Leg and Back Pain\n\n **Authors:** John G. Christensen, Jr, MD \n **Date:** March 05, 2021\n\n ## Content\n\n RCC subtypes include clear cell (roughly 75%), papillary, chromophobe, collecting duct, and unclassified.[1] The papillary and chromophobe subtypes may portend better survival. The Fuhrman cellular grade of clear cell carcinoma is an independent predictor of survival. Sarcomatoid features can be found in any subtype and are associated with a worse prognosis. Oncocytoma, which may be associated with a central star-shaped density on CT scanning, does not metastasize and is considered a benign renal mass.\nThe presence of fat in a renal mass on CT or MRI images is pathognomonic of benign angiomyolipoma. Otherwise, solid renal masses should be considered likely malignant (≥80%) and possibly aggressive (≥20%) and treated as such.\nThe TNM staging for RCC is as follows[3,4]:\nT1—Tumor ≤7 cm, limited to kidney\nT1a—Tumor ≤4 cm\nT1b—Tumor >4 cm and ≤7 cm\nT2—Tumor >7 cm but limited to kidney\nT3—Tumor involves renal vein, inferior vena cava (IVC), or perirenal fat but contained within Gerota fascia\nT4—Tumor invades beyond Gerota fascia\nAmerican Joint Committee on Cancer staging is as follows[3,4]:\nStage I—T1, N0M0\nStage II—T2, N0M0\nStage III—T3, N0M0 or T1-3, N1M0\nStage IV—T4, N0-1M0; any T with M1\nTumor size is a strong predictor of survival. The 5-year disease-specific survival by T stage for RCC is as follows[3]:\nT1—95%\nT2—88%\nT3—59%\nT4—20%\nThe Fuhrman Nuclear Grading System is an independent predictor of survival. In patients with T1 disease, the 5-year cancer-specific survival rates after surgery are as follows[5]:\nFuhrman Grade 1—91%\nFuhrman Grade 2—83%\nFuhrman Grade 3—60%\nFuhrman Grade 4—0%\nThe objectives of imaging a renal mass are to rule out benign angiomyolipoma (any fat density seen), to evaluate for locally invasive features, to study the involved anatomy (for surgical planning), and to determine the status of the uninvolved kidney.[3]\nContrast-enhanced CT scanning is the imaging procedure of choice for diagnosis and staging of renal masses when renal function is adequate. Typically, this is a CT scan of the abdomen and pelvis without and then with contrast; this may include a delayed urogram phase.[1,2,3] Contrast-enhanced MRI is an optional imaging modality for initial evaluation. MRI is also recommended if renal vein or IVC involvement is in question. Urinary calculi may not show up on MRI.\nRenal ultrasonography can be useful in evaluating cystic masses if CT imaging is inconclusive; however, ultrasonography may miss isodense renal tumors or transitional cell tumors of the renal collecting system.[3] Angiomyolipomas are suspected based on the high echogenicity of fat; however, a CT scan is more definitive.\nIntravenous pyelography is inadequate to evaluate a renal mass due to low sensitivity and specificity.[3] Bone scanning is not routinely performed unless bone pain, elevated alkaline phosphatase, or other suspicion of bony metastases is present. The role of PET scanning in RCC has yet to be determined.[4]\nBrain MRI or CT scanning can be performed if clinical signs or symptoms are suspicious for brain metastases.[4] Chest imaging (radiography or CT scanning) should be routinely included in the workup of a solid renal mass.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A 42-Year-Old Office Assistant With Chronic Leg and Back Pain"
},
{
"authors": "John G. Christensen, Jr, MD",
"content": [
"Partial nephrectomy is the treatment of choice for T1a (≤4 cm) renal tumors unless anatomically not feasible (eg, hilar invasion). For T1b tumors (4-7 cm), radical nephrectomy is acceptable, but partial nephrectomy should be considered if complete resection can be achieved. Partial nephrectomy may be performed via open, laparoscopic, or robotic-assisted laparoscopic technique. Partial nephrectomy is unfortunately underused, with radical nephrectomy often performed for T1 lesions that are amenable to renal unit-sparing surgery.",
"Radical nephrectomy is acceptable for T1b (4-7 cm) tumors and is the treatment of choice for T2-4 tumors. However, with T1b tumors that are anatomically amenable to complete excision via partial nephrectomy, no survival or cure benefit is associated with performing radical nephrectomy. With radical nephrectomy instead of partial nephrectomy, the remaining kidney may be prone to hyperfiltration injury over time, and the patient is at risk for total renal loss in the event of trauma or asynchronous de-novo renal cancer. Radical nephrectomy for cytoreduction may improve survival in patients with metastatic disease. Radical nephrectomy can be performed by open or laparoscopic approach.",
"Active surveillance might be considered with a small asymptomatic renal mass (<4 cm) in elderly patients, those with high surgical risk, and those with limited life expectancy, provided slow growth (or no growth) is documented on serial imaging. A retrospective, single-institution review of 51 patients showed no metastatic spread with a median follow-up of 6 years; only 2 patients required surgical intervention for local progression or symptoms.[6] Periodic follow-up imaging is advised to assess growth rate, with possible intervention if a more aggressive clinical course is evident.[1,2,4] Regardless, active surveillance is not recommended for even very small renal tumors in most patients who are reasonable surgical candidates.",
"Thermoablation (radiofrequency or cryoablation) is a potentially less-invasive option for elderly or high-risk patients, especially those with tumors <4 cm. Thermoablation can be done as a percutaneous technique, and good long-term results have been obtained in patients with RCCs <4 cm who were poor surgical candidates.[7] Pretreatment tissue pathology confirmation by biopsy is strongly recommended if thermoablation is planned.[1,2,3] However, complete tumor eradication is more difficult to determine, additional treatments may be needed, and a higher rate of local tumor recurrence is associated with ablation techniques compared with surgery. Therefore, at present, thermoablation is not considered a first-line treatment in most patients.[3]",
"Percutaneous needle biopsy of a renal mass may be considered if the results may affect management.[1,2,4] Traditional concerns for false-negative results or needle tract seeding have been assuaged by new data that indicate that false-negative rates are lower than 1%, and needle tract seeding is actually exceedingly rare. Biopsy is more regularly becoming a part of decision making for small renal masses, particularly with masses <3 cm in elderly or infirm patients who may consider treatment only if cancer is confirmed. At this time, biopsy is not routinely indicated in healthy patients who may not accept the risk for tumor progression with conservative approaches. Likewise, biopsy is not helpful in elderly or infirm patients who may refuse any treatment regardless of biopsy results.",
"Examples where renal biopsy is recommended and may alter treatment include the following:",
"Suspicion of a metastatic lesion to kidney from another primary source",
"Suspicion of lymphoma",
"Possible abscess (although follow-up imaging alone may suffice)",
"Evaluation of questionable renal cysts in selected cases",
"An elderly or high-risk patient who may consider surgery or thermoablation only if RCC is confirmed",
"A surgical candidate who wishes to consider active surveillance or thermoablation and accepts the possible increased risk for tumor progression by avoiding standard therapy with partial or radical nephrectomy",
"For tissue confirmation prior to thermoablation",
"In the patient in this case, after the CT scan revealed a 2-cm, solid, enhancing, right renal mass suspicious for RCC, a chest x-ray was obtained, the results of which were negative. No further metastatic evaluation was ordered in the absence of suspicious symptoms or findings and the absence of bony lesions on her MRI and CT. The patient was counseled on further options and elected robotic-assisted laparoscopic right partial nephrectomy, which was performed the following week. She was discharged on postoperative day 2, and recovery was uneventful. Pathology revealed a Fuhrman grade 2/4 clear cell RCC, with negative margins and no sarcomatous elements (pT1aN0M0). Her chronic leg and lower back pain remained unchanged and are felt to be unrelated. Medical investigation into the causes and possible treatment is ongoing.",
"RCC recurrence occurs in 20%-40% of patients with clinically localized disease following surgery, typically within the first 3-5 years; however, recurrences more than 30 years later have been documented. Periodic follow-up monitoring is therefore recommended. For T1 tumors following partial nephrectomy, a baseline CT scan with and without contrast and chest radiography is planned for 3-6 months postoperatively; CT scanning or ultrasonography plus chest radiography is then planned annually for 3 years, and then as clinically indicated. For larger tumors (T2+), CT scanning and chest radiography are performed at baseline, and then CT scanning or ultrasonography plus chest radiography is performed every 6 months until year 3, then annually until year 5, and then as clinically indicated. Immunotherapy and surgery are available treatments for recurrent RCC.[5]"
],
"date": "March 05, 2021",
"figures": [],
"markdown": "# A 42-Year-Old Office Assistant With Chronic Leg and Back Pain\n\n **Authors:** John G. Christensen, Jr, MD \n **Date:** March 05, 2021\n\n ## Content\n\n Partial nephrectomy is the treatment of choice for T1a (≤4 cm) renal tumors unless anatomically not feasible (eg, hilar invasion). For T1b tumors (4-7 cm), radical nephrectomy is acceptable, but partial nephrectomy should be considered if complete resection can be achieved. Partial nephrectomy may be performed via open, laparoscopic, or robotic-assisted laparoscopic technique. Partial nephrectomy is unfortunately underused, with radical nephrectomy often performed for T1 lesions that are amenable to renal unit-sparing surgery.\nRadical nephrectomy is acceptable for T1b (4-7 cm) tumors and is the treatment of choice for T2-4 tumors. However, with T1b tumors that are anatomically amenable to complete excision via partial nephrectomy, no survival or cure benefit is associated with performing radical nephrectomy. With radical nephrectomy instead of partial nephrectomy, the remaining kidney may be prone to hyperfiltration injury over time, and the patient is at risk for total renal loss in the event of trauma or asynchronous de-novo renal cancer. Radical nephrectomy for cytoreduction may improve survival in patients with metastatic disease. Radical nephrectomy can be performed by open or laparoscopic approach.\nActive surveillance might be considered with a small asymptomatic renal mass (<4 cm) in elderly patients, those with high surgical risk, and those with limited life expectancy, provided slow growth (or no growth) is documented on serial imaging. A retrospective, single-institution review of 51 patients showed no metastatic spread with a median follow-up of 6 years; only 2 patients required surgical intervention for local progression or symptoms.[6] Periodic follow-up imaging is advised to assess growth rate, with possible intervention if a more aggressive clinical course is evident.[1,2,4] Regardless, active surveillance is not recommended for even very small renal tumors in most patients who are reasonable surgical candidates.\nThermoablation (radiofrequency or cryoablation) is a potentially less-invasive option for elderly or high-risk patients, especially those with tumors <4 cm. Thermoablation can be done as a percutaneous technique, and good long-term results have been obtained in patients with RCCs <4 cm who were poor surgical candidates.[7] Pretreatment tissue pathology confirmation by biopsy is strongly recommended if thermoablation is planned.[1,2,3] However, complete tumor eradication is more difficult to determine, additional treatments may be needed, and a higher rate of local tumor recurrence is associated with ablation techniques compared with surgery. Therefore, at present, thermoablation is not considered a first-line treatment in most patients.[3]\nPercutaneous needle biopsy of a renal mass may be considered if the results may affect management.[1,2,4] Traditional concerns for false-negative results or needle tract seeding have been assuaged by new data that indicate that false-negative rates are lower than 1%, and needle tract seeding is actually exceedingly rare. Biopsy is more regularly becoming a part of decision making for small renal masses, particularly with masses <3 cm in elderly or infirm patients who may consider treatment only if cancer is confirmed. At this time, biopsy is not routinely indicated in healthy patients who may not accept the risk for tumor progression with conservative approaches. Likewise, biopsy is not helpful in elderly or infirm patients who may refuse any treatment regardless of biopsy results.\nExamples where renal biopsy is recommended and may alter treatment include the following:\nSuspicion of a metastatic lesion to kidney from another primary source\nSuspicion of lymphoma\nPossible abscess (although follow-up imaging alone may suffice)\nEvaluation of questionable renal cysts in selected cases\nAn elderly or high-risk patient who may consider surgery or thermoablation only if RCC is confirmed\nA surgical candidate who wishes to consider active surveillance or thermoablation and accepts the possible increased risk for tumor progression by avoiding standard therapy with partial or radical nephrectomy\nFor tissue confirmation prior to thermoablation\nIn the patient in this case, after the CT scan revealed a 2-cm, solid, enhancing, right renal mass suspicious for RCC, a chest x-ray was obtained, the results of which were negative. No further metastatic evaluation was ordered in the absence of suspicious symptoms or findings and the absence of bony lesions on her MRI and CT. The patient was counseled on further options and elected robotic-assisted laparoscopic right partial nephrectomy, which was performed the following week. She was discharged on postoperative day 2, and recovery was uneventful. Pathology revealed a Fuhrman grade 2/4 clear cell RCC, with negative margins and no sarcomatous elements (pT1aN0M0). Her chronic leg and lower back pain remained unchanged and are felt to be unrelated. Medical investigation into the causes and possible treatment is ongoing.\nRCC recurrence occurs in 20%-40% of patients with clinically localized disease following surgery, typically within the first 3-5 years; however, recurrences more than 30 years later have been documented. Periodic follow-up monitoring is therefore recommended. For T1 tumors following partial nephrectomy, a baseline CT scan with and without contrast and chest radiography is planned for 3-6 months postoperatively; CT scanning or ultrasonography plus chest radiography is then planned annually for 3 years, and then as clinically indicated. For larger tumors (T2+), CT scanning and chest radiography are performed at baseline, and then CT scanning or ultrasonography plus chest radiography is performed every 6 months until year 3, then annually until year 5, and then as clinically indicated. Immunotherapy and surgery are available treatments for recurrent RCC.[5]\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1085398,
"choiceText": "Intravenous pyelography",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085400,
"choiceText": "CT scanning with and without contrast",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085402,
"choiceText": "Bone scanning ",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085404,
"choiceText": "PET scanning\r\n",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Contrast-enhanced CT scanning is the imaging procedure of choice for diagnosis and staging of renal masses when renal function is adequate. Typically, this is a CT scan of the abdomen and pelvis without and then with contrast; this may include a delayed urogram phase. MRI would be another option. Intravenous pyelography does not adequately evaluate renal masses. Bone scan is only indicated if signs or symptoms of bone metastasis are present. The role of PET scanning has not been established in the evaluation of a renal mass.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 343773,
"questionText": "Which of the following is the appropriate imaging study for an incidental, solid-appearing renal mass detected on abdominal ultrasonography?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1085406,
"choiceText": "Active surveillance",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085408,
"choiceText": "Thermoablation",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085410,
"choiceText": "Partial nephrectomy",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085412,
"choiceText": "Radical nephrectomy\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Partial nephrectomy is a standard of care for a T1a renal mass (≤4 cm). Radical nephrectomy is overused but is acceptable if tumor anatomy precludes complete removal by partial nephrectomy. Active surveillance or thermoablation can be considered, primarily in high-risk patients or patients with limited life expectancy due to age or other factors. Biopsy of a renal mass can be considered if it may change management and should be performed for tissue confirmation prior to thermoablation.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 343775,
"questionText": "Which of the following is the most appropriate next step in the management of a healthy, asymptomatic 52-year-old patient with a small (<4 cm), non‒fat-containing, solid renal mass incidentally discovered by contrast CT scanning?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 42-Year-Old Office Assistant With Chronic Leg and Back Pain"
},
{
"authors": "John G. Christensen, Jr, MD",
"content": [],
"date": "March 05, 2021",
"figures": [],
"markdown": "# A 42-Year-Old Office Assistant With Chronic Leg and Back Pain\n\n **Authors:** John G. Christensen, Jr, MD \n **Date:** March 05, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1085398,
"choiceText": "Intravenous pyelography",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085400,
"choiceText": "CT scanning with and without contrast",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085402,
"choiceText": "Bone scanning ",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085404,
"choiceText": "PET scanning\r\n",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Contrast-enhanced CT scanning is the imaging procedure of choice for diagnosis and staging of renal masses when renal function is adequate. Typically, this is a CT scan of the abdomen and pelvis without and then with contrast; this may include a delayed urogram phase. MRI would be another option. Intravenous pyelography does not adequately evaluate renal masses. Bone scan is only indicated if signs or symptoms of bone metastasis are present. The role of PET scanning has not been established in the evaluation of a renal mass.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 343773,
"questionText": "Which of the following is the appropriate imaging study for an incidental, solid-appearing renal mass detected on abdominal ultrasonography?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1085406,
"choiceText": "Active surveillance",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085408,
"choiceText": "Thermoablation",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085410,
"choiceText": "Partial nephrectomy",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085412,
"choiceText": "Radical nephrectomy\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Partial nephrectomy is a standard of care for a T1a renal mass (≤4 cm). Radical nephrectomy is overused but is acceptable if tumor anatomy precludes complete removal by partial nephrectomy. Active surveillance or thermoablation can be considered, primarily in high-risk patients or patients with limited life expectancy due to age or other factors. Biopsy of a renal mass can be considered if it may change management and should be performed for tissue confirmation prior to thermoablation.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 343775,
"questionText": "Which of the following is the most appropriate next step in the management of a healthy, asymptomatic 52-year-old patient with a small (<4 cm), non‒fat-containing, solid renal mass incidentally discovered by contrast CT scanning?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 42-Year-Old Office Assistant With Chronic Leg and Back Pain"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1085390,
"choiceText": "Hyperdense renal cyst",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085392,
"choiceText": "Renal cell carcinoma",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085394,
"choiceText": "Oncocytoma",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085396,
"choiceText": "Angiomyolipoma\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 343771,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1085398,
"choiceText": "Intravenous pyelography",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085400,
"choiceText": "CT scanning with and without contrast",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085402,
"choiceText": "Bone scanning ",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085404,
"choiceText": "PET scanning\r\n",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Contrast-enhanced CT scanning is the imaging procedure of choice for diagnosis and staging of renal masses when renal function is adequate. Typically, this is a CT scan of the abdomen and pelvis without and then with contrast; this may include a delayed urogram phase. MRI would be another option. Intravenous pyelography does not adequately evaluate renal masses. Bone scan is only indicated if signs or symptoms of bone metastasis are present. The role of PET scanning has not been established in the evaluation of a renal mass.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 343773,
"questionText": "Which of the following is the appropriate imaging study for an incidental, solid-appearing renal mass detected on abdominal ultrasonography?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1085406,
"choiceText": "Active surveillance",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085408,
"choiceText": "Thermoablation",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085410,
"choiceText": "Partial nephrectomy",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1085412,
"choiceText": "Radical nephrectomy\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Partial nephrectomy is a standard of care for a T1a renal mass (≤4 cm). Radical nephrectomy is overused but is acceptable if tumor anatomy precludes complete removal by partial nephrectomy. Active surveillance or thermoablation can be considered, primarily in high-risk patients or patients with limited life expectancy due to age or other factors. Biopsy of a renal mass can be considered if it may change management and should be performed for tissue confirmation prior to thermoablation.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 343775,
"questionText": "Which of the following is the most appropriate next step in the management of a healthy, asymptomatic 52-year-old patient with a small (<4 cm), non‒fat-containing, solid renal mass incidentally discovered by contrast CT scanning?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
946426 | /viewarticle/946426 | [
{
"authors": "Ankit Raiyani, MBBS, MD, DNB (Hematology)",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 62-year-old man is brought to the emergency department after the sudden onset of palpitations at rest, accompanied by dizziness and blackouts. The episode has lasted about 25 minutes. His heart rate is 190 beats/min, and his blood pressure is 90/60 mm Hg. The electrocardiographic findings are suggestive of ventricular tachycardia with low QRS voltage. Normal sinus rhythm is established with synchronized direct current cardioversion followed by administration of intravenous amiodarone.",
"Over the past 6 months, the patient has had a total of three transient episodes of sudden-onset palpitations that resolved spontaneously within a few seconds. He attributed these episodes to stress related to the COVID-19 pandemic and did not seek medical attention. The patient has also noticed lower limb edema, which is more pronounced after he stands for a long time. He reports that he bruises easily, even with trivial trauma. His wife has noticed subtle slurring in his speech for the past 6 months.",
"The patient's medical history includes irritable bowel syndrome (IBS) and diabetes mellitus, which was diagnosed 6 years earlier. He requires frequent modifications in the doses of oral hypoglycemic agents and insulin owing to episodes of hyperglycemia and hypoglycemia. He has been consulting a gastroenterologist for diarrhea-predominant IBS for the past year. He was taking an antidiarrheal (loperamide), an anticholinergic (dicyclomine), an antibiotic (rifaximin), a selective serotonin reuptake inhibitor (fluoxetine), and a fiber supplement, with less than satisfactory results. He does not have any other chronic illnesses that require long-term medications.",
"The patient denies recent fever, rashes, bleeding from any sites, and joint pain or swelling. He consumes alcohol in moderation and denies using illicit drugs. A detailed family history does not contribute significantly to the case at hand."
],
"date": "March 03, 2021",
"figures": [],
"markdown": "# Blackout at Rest and Slurring in a Man Afraid of COVID-19\n\n **Authors:** Ankit Raiyani, MBBS, MD, DNB (Hematology) \n **Date:** March 03, 2021\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 62-year-old man is brought to the emergency department after the sudden onset of palpitations at rest, accompanied by dizziness and blackouts. The episode has lasted about 25 minutes. His heart rate is 190 beats/min, and his blood pressure is 90/60 mm Hg. The electrocardiographic findings are suggestive of ventricular tachycardia with low QRS voltage. Normal sinus rhythm is established with synchronized direct current cardioversion followed by administration of intravenous amiodarone.\nOver the past 6 months, the patient has had a total of three transient episodes of sudden-onset palpitations that resolved spontaneously within a few seconds. He attributed these episodes to stress related to the COVID-19 pandemic and did not seek medical attention. The patient has also noticed lower limb edema, which is more pronounced after he stands for a long time. He reports that he bruises easily, even with trivial trauma. His wife has noticed subtle slurring in his speech for the past 6 months.\nThe patient's medical history includes irritable bowel syndrome (IBS) and diabetes mellitus, which was diagnosed 6 years earlier. He requires frequent modifications in the doses of oral hypoglycemic agents and insulin owing to episodes of hyperglycemia and hypoglycemia. He has been consulting a gastroenterologist for diarrhea-predominant IBS for the past year. He was taking an antidiarrheal (loperamide), an anticholinergic (dicyclomine), an antibiotic (rifaximin), a selective serotonin reuptake inhibitor (fluoxetine), and a fiber supplement, with less than satisfactory results. He does not have any other chronic illnesses that require long-term medications.\nThe patient denies recent fever, rashes, bleeding from any sites, and joint pain or swelling. He consumes alcohol in moderation and denies using illicit drugs. A detailed family history does not contribute significantly to the case at hand.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Blackout at Rest and Slurring in a Man Afraid of COVID-19"
},
{
"authors": "Ankit Raiyani, MBBS, MD, DNB (Hematology)",
"content": [
"Upon examination, the patient is alert and oriented but appears fatigued. He is afebrile. He has bilateral pitting pedal edema, which does not extend above the ankles, and periorbital edema. No icterus, lymphadenopathy, cyanosis, or clubbing is noted. Examination of the oral cavity shows macroglossia with teeth indentations. Skin examination findings are unremarkable except for the presence of ecchymoses.",
"Auscultation of the chest reveals a respiration rate of 24 breaths/min, with inspiratory crepitations at the bases of the lungs. His pulse is regular at 82 beats/min (after reverting to sinus rhythm), and his blood pressure is 108/64 mm Hg (supine) and 90/56 mm Hg (standing). His abdomen is distended but nontender. No hepatomegaly or splenomegaly is noted. A dull percussion note is elicited on the flanks. Neurologic examination findings are normal and reveal no focal deficits.",
"The patient's complete blood cell count is suggestive of normocytic anemia, with a hemoglobin level of 10.5 g/dL (reference range, 13.5-15.5 g/dL). The leukocyte count with differential and platelet count are within normal limits. Results of a peripheral smear examination are unremarkable.",
"The patient has an elevated serum creatinine level of 1.91 mg/dL (reference range, 0.9-1.3 mg/dL). Serum electrolyte levels (including sodium, potassium, calcium, and magnesium) are normal. Liver function test results are largely within normal limits, except for these serum protein values:",
"Total protein: 4.1 g/dL (reference range, 6.4-8.3 g/dL)",
"Albumin: 1.8 g/dL (reference range, 3.5-5 g/dL)",
"Globulin: 2.3 g/dL (reference range, 2.3-3.4 g/dL)",
"No monoclonal bands are detected on serum protein electrophoresis.",
"The findings on a two-dimensional echocardiogram suggest fair left ventricular systolic function, with a left ventricular ejection fraction of 60%. The chief findings are an interventricular septal thickness of 18 mm and grade 3 diastolic dysfunction. The patient has a very high N-terminal pro-brain natriuretic peptide (NT-proBNP) level of 24,924 pg/mL (reference range, < 300 pg/mL). His troponin I level is 0.38 ng/mL (reference range, < 0.03 ng/mL). Multiple short runs of ventricular premature complexes are detected by 24-hour ambulatory electrocardiographic (Holter) monitoring.",
"Urine examination reveals proteinuria without casts. No hematuria is detected. A 24-hour urinary protein loss of 7.1 g is noted (reference range, < 150 mg/d).",
"An ultrasonogram reveals marked mesenteric edema throughout the abdomen but no organomegaly or lymphadenopathy. An ultrasonogram of the pelvis shows bilateral bulky kidneys, with the loss of corticomedullary differentiation. No hydronephrosis or nephrolithiasis is observed."
],
"date": "March 03, 2021",
"figures": [],
"markdown": "# Blackout at Rest and Slurring in a Man Afraid of COVID-19\n\n **Authors:** Ankit Raiyani, MBBS, MD, DNB (Hematology) \n **Date:** March 03, 2021\n\n ## Content\n\n Upon examination, the patient is alert and oriented but appears fatigued. He is afebrile. He has bilateral pitting pedal edema, which does not extend above the ankles, and periorbital edema. No icterus, lymphadenopathy, cyanosis, or clubbing is noted. Examination of the oral cavity shows macroglossia with teeth indentations. Skin examination findings are unremarkable except for the presence of ecchymoses.\nAuscultation of the chest reveals a respiration rate of 24 breaths/min, with inspiratory crepitations at the bases of the lungs. His pulse is regular at 82 beats/min (after reverting to sinus rhythm), and his blood pressure is 108/64 mm Hg (supine) and 90/56 mm Hg (standing). His abdomen is distended but nontender. No hepatomegaly or splenomegaly is noted. A dull percussion note is elicited on the flanks. Neurologic examination findings are normal and reveal no focal deficits.\nThe patient's complete blood cell count is suggestive of normocytic anemia, with a hemoglobin level of 10.5 g/dL (reference range, 13.5-15.5 g/dL). The leukocyte count with differential and platelet count are within normal limits. Results of a peripheral smear examination are unremarkable.\nThe patient has an elevated serum creatinine level of 1.91 mg/dL (reference range, 0.9-1.3 mg/dL). Serum electrolyte levels (including sodium, potassium, calcium, and magnesium) are normal. Liver function test results are largely within normal limits, except for these serum protein values:\nTotal protein: 4.1 g/dL (reference range, 6.4-8.3 g/dL)\nAlbumin: 1.8 g/dL (reference range, 3.5-5 g/dL)\nGlobulin: 2.3 g/dL (reference range, 2.3-3.4 g/dL)\nNo monoclonal bands are detected on serum protein electrophoresis.\nThe findings on a two-dimensional echocardiogram suggest fair left ventricular systolic function, with a left ventricular ejection fraction of 60%. The chief findings are an interventricular septal thickness of 18 mm and grade 3 diastolic dysfunction. The patient has a very high N-terminal pro-brain natriuretic peptide (NT-proBNP) level of 24,924 pg/mL (reference range, < 300 pg/mL). His troponin I level is 0.38 ng/mL (reference range, < 0.03 ng/mL). Multiple short runs of ventricular premature complexes are detected by 24-hour ambulatory electrocardiographic (Holter) monitoring.\nUrine examination reveals proteinuria without casts. No hematuria is detected. A 24-hour urinary protein loss of 7.1 g is noted (reference range, < 150 mg/d).\nAn ultrasonogram reveals marked mesenteric edema throughout the abdomen but no organomegaly or lymphadenopathy. An ultrasonogram of the pelvis shows bilateral bulky kidneys, with the loss of corticomedullary differentiation. No hydronephrosis or nephrolithiasis is observed.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1568300,
"choiceText": "Protein-losing enteropathy (eg, celiac disease)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568301,
"choiceText": "Connective tissue disorder (eg, lupus nephritis)",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568302,
"choiceText": "Nephrotic syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568303,
"choiceText": "Systemic amyloidosis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568304,
"choiceText": "Diabetic nephropathy and autonomic neuropathy",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 503327,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Blackout at Rest and Slurring in a Man Afraid of COVID-19"
},
{
"authors": "Ankit Raiyani, MBBS, MD, DNB (Hematology)",
"content": [
"Systemic amyloidosis is a rare disease that occurs when an abnormal protein called amyloid builds up in vital organs and interferes with their normal function. Amyloid is not normally found in the body, but it can be formed from more than 30 different types of protein.[1]",
"Deposition of amyloid can occur under these conditions[1]:",
"With an abnormal protein (eg, hereditary amyloidosis and acquired systemic immunoglobulin light chain [AL] amyloidosis)",
"Owing to a prolonged overabundance of a normal protein (eg, reactive systemic [amyloid A, or AA] amyloidosis and beta-2 microglobulin dialysis-related amyloidosis)",
"Accompanying the aging process (eg, wild-type transthyretin amyloidosis [senile systemic amyloidosis] and atrial natriuretic peptide amyloidosis)",
"Amyloid fibril can be deposited in any soft tissue. The most commonly affected organs in systemic amyloidosis are the heart, kidneys, liver, skin, and nervous system.[1]",
"The degree of involvement varies among these organs, so each patient may have a unique set of symptoms. A high degree of clinical suspicion is required for a timely diagnosis, particularly in the early stages of the disease.",
"The two major types of systemic amyloidosis are the AL type and the AA type. The most frequent type of amyloidosis in high-income countries is AL amyloidosis.[1] AL amyloidosis may or may not be associated with a concurrent plasma cell dyscrasia, such as multiple myeloma or monoclonal gammopathy of unknown significance. AA amyloidosis may occur with chronic inflammatory conditions (eg, rheumatoid arthritis) or chronic infections (eg, tuberculosis).",
"In the patient in this case, recurrent cardiac arrhythmias, low voltage on an ECG, congestive heart failure, and diastolic dysfunction can be explained by amyloid deposition in the heart. Edema, periorbital swelling, and hypoproteinemia may be due to nephrotic-range proteinuria, which results from renal deposition of amyloid fibrils. Frequent loose bowel movements and postural hypotension may be caused by autonomic nervous system involvement. Macroglossia and the resultant slurring of speech may be attributed to amyloid deposition in the tongue. Easy bruising may be due to cutaneous involvement and/or acquired clotting factor X deficiency."
],
"date": "March 03, 2021",
"figures": [],
"markdown": "# Blackout at Rest and Slurring in a Man Afraid of COVID-19\n\n **Authors:** Ankit Raiyani, MBBS, MD, DNB (Hematology) \n **Date:** March 03, 2021\n\n ## Content\n\n Systemic amyloidosis is a rare disease that occurs when an abnormal protein called amyloid builds up in vital organs and interferes with their normal function. Amyloid is not normally found in the body, but it can be formed from more than 30 different types of protein.[1]\nDeposition of amyloid can occur under these conditions[1]:\nWith an abnormal protein (eg, hereditary amyloidosis and acquired systemic immunoglobulin light chain [AL] amyloidosis)\nOwing to a prolonged overabundance of a normal protein (eg, reactive systemic [amyloid A, or AA] amyloidosis and beta-2 microglobulin dialysis-related amyloidosis)\nAccompanying the aging process (eg, wild-type transthyretin amyloidosis [senile systemic amyloidosis] and atrial natriuretic peptide amyloidosis)\nAmyloid fibril can be deposited in any soft tissue. The most commonly affected organs in systemic amyloidosis are the heart, kidneys, liver, skin, and nervous system.[1]\nThe degree of involvement varies among these organs, so each patient may have a unique set of symptoms. A high degree of clinical suspicion is required for a timely diagnosis, particularly in the early stages of the disease.\nThe two major types of systemic amyloidosis are the AL type and the AA type. The most frequent type of amyloidosis in high-income countries is AL amyloidosis.[1] AL amyloidosis may or may not be associated with a concurrent plasma cell dyscrasia, such as multiple myeloma or monoclonal gammopathy of unknown significance. AA amyloidosis may occur with chronic inflammatory conditions (eg, rheumatoid arthritis) or chronic infections (eg, tuberculosis).\nIn the patient in this case, recurrent cardiac arrhythmias, low voltage on an ECG, congestive heart failure, and diastolic dysfunction can be explained by amyloid deposition in the heart. Edema, periorbital swelling, and hypoproteinemia may be due to nephrotic-range proteinuria, which results from renal deposition of amyloid fibrils. Frequent loose bowel movements and postural hypotension may be caused by autonomic nervous system involvement. Macroglossia and the resultant slurring of speech may be attributed to amyloid deposition in the tongue. Easy bruising may be due to cutaneous involvement and/or acquired clotting factor X deficiency.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1568300,
"choiceText": "Protein-losing enteropathy (eg, celiac disease)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568301,
"choiceText": "Connective tissue disorder (eg, lupus nephritis)",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568302,
"choiceText": "Nephrotic syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568303,
"choiceText": "Systemic amyloidosis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568304,
"choiceText": "Diabetic nephropathy and autonomic neuropathy",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 503327,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Blackout at Rest and Slurring in a Man Afraid of COVID-19"
},
{
"authors": "Ankit Raiyani, MBBS, MD, DNB (Hematology)",
"content": [
"After systemic amyloidosis, the second most probable diagnosis in the differential is diabetic nephropathy and autonomic neuropathy. Type 2 diabetes with poor glycemic control may cause end-organ damage. The heart, kidneys, peripheral and autonomic nervous systems, and blood vessels are among the most commonly affected organs.[2] Diabetic nephropathy can cause nephrotic-range proteinuria with declining renal function, which can lead to anasarca, heart failure, severe fatigue, and renal failure.[3,4] Autonomic neuropathy can explain this patient's symptoms of postural hypotension, palpitations, and frequent loose bowel movements. However, his easy bruising, recurrent cardiac arrhythmias, low voltage on an ECG, and macroglossia cannot be explained by diabetes complications.",
"Protein-losing enteropathy (PLE) is a condition in which an excess loss of proteins occurs through the gastrointestinal tract. PLE can be caused by more than 60 different conditions, including nearly all gastrointestinal diseases. It should be suspected in patients who have low serum protein levels and in whom other causes of hypoproteinemia have been ruled out.[5]",
"The leg swelling, periorbital puffiness, and low serum protein levels observed in this patient could be explained by PLE. Loose bowel movements can result from an underlying gastrointestinal condition. Palpitations can occur with the congestive heart failure associated with severe hypoproteinemia. However, the easy bruising, macroglossia, and cardiac arrhythmias observed in this patient are not usually associated with PLE.",
"Connective tissue disorders such as systemic lupus erythematosus can involve the kidneys. In lupus nephritis, the autoimmune response damages the renal tubules. Proteinuria develops in nearly all patients, and nephrotic-range proteinuria is observed in almost 50% of patients.[6] Loss of serum proteins in the urine can lead to anasarca, heart failure, severe fatigue, and renal failure.",
"Hypertension, hematuria, and granular casts in the urine develop in the majority of patients with lupus nephritis. These findings are absent in the patient in this case. In addition, this diagnosis cannot explain the other symptoms of the patient, including macroglossia, easy bruising, frequent loose bowel movements, and postural hypotension.",
"Similarly, nephrotic syndrome due to other conditions may result in anasarca, heart failure, severe fatigue, and renal failure. However, nephrotic syndrome does not cause arrhythmia, macroglossia, easy bruising, frequent loose bowel movements, and postural hypotension, which were observed in this patient.",
"The workup for systemic amyloidosis consists of these steps[1]:",
"Confirmation of the diagnosis",
"Classification of amyloidosis",
"Assessment of end-organ damage",
"The diagnosis is confirmed with biopsy of an affected organ (eg, skin, kidney, abdominal fat pad, or bone marrow trephine). Amyloid material stains with Congo red stain (Figure 1) and gives a characteristic apple-green birefringence on polarized microscopy (Figure 2). This finding is diagnostic of amyloid and is almost universally reported as evidence of amyloidosis.[7]",
"Figure 1.",
"Figure 2.",
"The classification of AL amyloidosis involves these studies:",
"Immunofixation electrophoresis",
"Serum free light chain assay",
"Bone marrow aspiration and biopsy",
"Whole body PET/CT scanning",
"These studies are used to classify AA amyloidosis:",
"C-reactive protein level, erythrocyte sedimentation rate, and ferritin level",
"Rheumatoid factor assay",
"Workup for tuberculosis",
"The assessment of end-organ damage includes these studies:",
"Serum creatinine level, estimated glomerular filtration rate, and 24-hour urine protein collection",
"Complete blood cell count, prothrombin time, and activated partial thromboplastin time",
"Liver function tests",
"ECG",
"NT-proBNP and troponin T/I levels",
"Fecal occult blood test",
"Nerve conduction study"
],
"date": "March 03, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/946/426/946426-Thumb1.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/946/426/946426-Thumb2.jpg"
}
],
"markdown": "# Blackout at Rest and Slurring in a Man Afraid of COVID-19\n\n **Authors:** Ankit Raiyani, MBBS, MD, DNB (Hematology) \n **Date:** March 03, 2021\n\n ## Content\n\n After systemic amyloidosis, the second most probable diagnosis in the differential is diabetic nephropathy and autonomic neuropathy. Type 2 diabetes with poor glycemic control may cause end-organ damage. The heart, kidneys, peripheral and autonomic nervous systems, and blood vessels are among the most commonly affected organs.[2] Diabetic nephropathy can cause nephrotic-range proteinuria with declining renal function, which can lead to anasarca, heart failure, severe fatigue, and renal failure.[3,4] Autonomic neuropathy can explain this patient's symptoms of postural hypotension, palpitations, and frequent loose bowel movements. However, his easy bruising, recurrent cardiac arrhythmias, low voltage on an ECG, and macroglossia cannot be explained by diabetes complications.\nProtein-losing enteropathy (PLE) is a condition in which an excess loss of proteins occurs through the gastrointestinal tract. PLE can be caused by more than 60 different conditions, including nearly all gastrointestinal diseases. It should be suspected in patients who have low serum protein levels and in whom other causes of hypoproteinemia have been ruled out.[5]\nThe leg swelling, periorbital puffiness, and low serum protein levels observed in this patient could be explained by PLE. Loose bowel movements can result from an underlying gastrointestinal condition. Palpitations can occur with the congestive heart failure associated with severe hypoproteinemia. However, the easy bruising, macroglossia, and cardiac arrhythmias observed in this patient are not usually associated with PLE.\nConnective tissue disorders such as systemic lupus erythematosus can involve the kidneys. In lupus nephritis, the autoimmune response damages the renal tubules. Proteinuria develops in nearly all patients, and nephrotic-range proteinuria is observed in almost 50% of patients.[6] Loss of serum proteins in the urine can lead to anasarca, heart failure, severe fatigue, and renal failure.\nHypertension, hematuria, and granular casts in the urine develop in the majority of patients with lupus nephritis. These findings are absent in the patient in this case. In addition, this diagnosis cannot explain the other symptoms of the patient, including macroglossia, easy bruising, frequent loose bowel movements, and postural hypotension.\nSimilarly, nephrotic syndrome due to other conditions may result in anasarca, heart failure, severe fatigue, and renal failure. However, nephrotic syndrome does not cause arrhythmia, macroglossia, easy bruising, frequent loose bowel movements, and postural hypotension, which were observed in this patient.\nThe workup for systemic amyloidosis consists of these steps[1]:\nConfirmation of the diagnosis\nClassification of amyloidosis\nAssessment of end-organ damage\nThe diagnosis is confirmed with biopsy of an affected organ (eg, skin, kidney, abdominal fat pad, or bone marrow trephine). Amyloid material stains with Congo red stain (Figure 1) and gives a characteristic apple-green birefringence on polarized microscopy (Figure 2). This finding is diagnostic of amyloid and is almost universally reported as evidence of amyloidosis.[7]\nFigure 1.\nFigure 2.\nThe classification of AL amyloidosis involves these studies:\nImmunofixation electrophoresis\nSerum free light chain assay\nBone marrow aspiration and biopsy\nWhole body PET/CT scanning\nThese studies are used to classify AA amyloidosis:\nC-reactive protein level, erythrocyte sedimentation rate, and ferritin level\nRheumatoid factor assay\nWorkup for tuberculosis\nThe assessment of end-organ damage includes these studies:\nSerum creatinine level, estimated glomerular filtration rate, and 24-hour urine protein collection\nComplete blood cell count, prothrombin time, and activated partial thromboplastin time\nLiver function tests\nECG\nNT-proBNP and troponin T/I levels\nFecal occult blood test\nNerve conduction study\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n\n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Blackout at Rest and Slurring in a Man Afraid of COVID-19"
},
{
"authors": "Ankit Raiyani, MBBS, MD, DNB (Hematology)",
"content": [
"Further studies were ordered for the patient in this case because of the high clinical suspicion of amyloidosis. A serum free light chain assay showed these results:",
"Kappa free light chains: 6.3 mg/L (reference range, 3.3-19.4 mg/L)",
"Lambda free light chains: 1360 mg/L (reference range, 5.71-26.3 mg/L)",
"Ratio of kappa/lambda: 0.0046 (reference range, 0.26-1.65)",
"Serum immunofixation detected a lambda light chain monoclonal band. Bone marrow examination revealed no evidence of a plasma cell disorder. The C-reactive protein level was normal, and the level of rheumatoid factor was within normal limits. Renal biopsy results were suggestive of deposition of amyloid material. On the basis of these findings, AL amyloidosis, also known as systemic light chain amyloidosis, was diagnosed.",
"The prognosis of the disease depends on the extent of cardiac involvement. Cardiac arrhythmias and cardiac failure are the most frequently implicated causes of decreased survival of patients with AL amyloidosis. Patients with extensive cardiac involvement have uniformly poor survival (9-15 months), even with the best available treatment.[8]",
"At present, no therapy directed toward elimination of the amyloid deposits is available. Hence, treatment of the disease addresses the underlying clonal plasma cell dyscrasia, with the aim of rapidly reducing production of amyloidogenic light chains to limit progressive damage to amyloidotic organs. Combination therapy regimens used for multiple myeloma are also effective in AL amyloidosis. There is no established standard combination. Bortezomib (a proteasome inhibitor) is the base drug in combination therapy and may be combined with dexamethasone (a corticosteroid), daratumumab, and/or other drugs.[9,10]",
"Autologous stem cell transplantation is the most effective treatment but is not tolerated in patients with major cardiac involvement. Only about 20% of patients are eligible. Eligible patients should undergo high-dose therapy with melphalan followed by autologous stem cell transplant to further enhance the response to treatment.[11,12] Unlike in multiple myeloma, prolonged maintenance therapy confers no advantage in primary amyloidosis.[13]",
"Many new molecules that target the amyloid deposits and interfere with amyloidogenesis are in trials. Some of the promising molecules that may improve the outcomes of patients with advanced disease include:",
"4′-Iodo-4′-deoxydoxorubicin",
"Doxycycline, the antibiotic[14]",
"Epigallocatechin gallate, a polyphenol from green tea[15]",
"CPHPC, a competitive inhibitor of amyloid P[16]",
"NEOD001, a monoclonal antibody against amyloid P[17]",
"The patient in this case underwent implantation of a cardioverter defibrillator to decrease the risk of sudden cardiac death from arrhythmia. He received four cycles of combination therapy, with significant improvement in quality of life. He had extensive cardiac involvement, so he was ineligible for high-dose melphalan therapy followed by autologous stem cell transplant. He is currently undergoing regular follow-up."
],
"date": "March 03, 2021",
"figures": [],
"markdown": "# Blackout at Rest and Slurring in a Man Afraid of COVID-19\n\n **Authors:** Ankit Raiyani, MBBS, MD, DNB (Hematology) \n **Date:** March 03, 2021\n\n ## Content\n\n Further studies were ordered for the patient in this case because of the high clinical suspicion of amyloidosis. A serum free light chain assay showed these results:\nKappa free light chains: 6.3 mg/L (reference range, 3.3-19.4 mg/L)\nLambda free light chains: 1360 mg/L (reference range, 5.71-26.3 mg/L)\nRatio of kappa/lambda: 0.0046 (reference range, 0.26-1.65)\nSerum immunofixation detected a lambda light chain monoclonal band. Bone marrow examination revealed no evidence of a plasma cell disorder. The C-reactive protein level was normal, and the level of rheumatoid factor was within normal limits. Renal biopsy results were suggestive of deposition of amyloid material. On the basis of these findings, AL amyloidosis, also known as systemic light chain amyloidosis, was diagnosed.\nThe prognosis of the disease depends on the extent of cardiac involvement. Cardiac arrhythmias and cardiac failure are the most frequently implicated causes of decreased survival of patients with AL amyloidosis. Patients with extensive cardiac involvement have uniformly poor survival (9-15 months), even with the best available treatment.[8]\nAt present, no therapy directed toward elimination of the amyloid deposits is available. Hence, treatment of the disease addresses the underlying clonal plasma cell dyscrasia, with the aim of rapidly reducing production of amyloidogenic light chains to limit progressive damage to amyloidotic organs. Combination therapy regimens used for multiple myeloma are also effective in AL amyloidosis. There is no established standard combination. Bortezomib (a proteasome inhibitor) is the base drug in combination therapy and may be combined with dexamethasone (a corticosteroid), daratumumab, and/or other drugs.[9,10]\nAutologous stem cell transplantation is the most effective treatment but is not tolerated in patients with major cardiac involvement. Only about 20% of patients are eligible. Eligible patients should undergo high-dose therapy with melphalan followed by autologous stem cell transplant to further enhance the response to treatment.[11,12] Unlike in multiple myeloma, prolonged maintenance therapy confers no advantage in primary amyloidosis.[13]\nMany new molecules that target the amyloid deposits and interfere with amyloidogenesis are in trials. Some of the promising molecules that may improve the outcomes of patients with advanced disease include:\n4′-Iodo-4′-deoxydoxorubicin\nDoxycycline, the antibiotic[14]\nEpigallocatechin gallate, a polyphenol from green tea[15]\nCPHPC, a competitive inhibitor of amyloid P[16]\nNEOD001, a monoclonal antibody against amyloid P[17]\nThe patient in this case underwent implantation of a cardioverter defibrillator to decrease the risk of sudden cardiac death from arrhythmia. He received four cycles of combination therapy, with significant improvement in quality of life. He had extensive cardiac involvement, so he was ineligible for high-dose melphalan therapy followed by autologous stem cell transplant. He is currently undergoing regular follow-up.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1568305,
"choiceText": "The AA type is the most common type of systemic amyloidosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568306,
"choiceText": "AL amyloidosis is always associated with multiple myeloma",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568307,
"choiceText": "Cardiac involvement is the most common cause of mortality in amyloidosis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568308,
"choiceText": "Renal biopsy is necessary for all patients with systemic amyloidosis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The most common type of systemic amyloidosis is AL type amyloidosis (65%-70%). AA amyloidosis is the second most common (10%-15%).<sup>[1]</sup><br><br>\r\nAL amyloidosis features deposition of abnormal light chains in the extracellular space in various organs. These abnormal light chains are produced by abnormal plasma cells. It is not necessary for these plasma cells to be present in high proportions in bone marrow. In fact, monoclonal gammopathy of unknown significance is more frequently associated with AL amyloidosis than multiple myeloma. <br><br>\r\nCardiac involvement is the most common cause of the mortality in patients with amyloidosis. The prognosis is determined by the extent of cardiac disease, among other factors. <br><br>\r\nFor the diagnosis of amyloidosis, a biopsy can be obtained from any accessible organ suspected to be affected by the disease. It is not necessary to take a biopsy from all the organs either to diagnose the disease or to check for end-organ damage.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 503328,
"questionText": "Which of the following statements is most accurate regarding amyloidosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1568309,
"choiceText": "Treatment of amyloidosis is directed toward removal of the amyloid fibrils from the affected organs",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568310,
"choiceText": "All patients with AL amyloidosis who are not eligible for stem cell transplant should receive combination therapy",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568311,
"choiceText": "Only high-risk patients with AL amyloidosis should undergo autologous stem cell transplant",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568312,
"choiceText": "Patient with extensive cardiac involvement will do well with high-dose melphalan therapy and autologous stem cell transplant",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "With currently available treatment options, it is not possible to remove amyloid fibrils from affected organs. Treatment is directed toward elimination of abnormal plasma cells and decreasing the production of amyloid light chain.<sup>[1]</sup> <br><br>\r\n\r\nAs in multiple myeloma, combination therapy is preferred for initial treatment.<sup>[10]</sup> Monotherapy is associated with high failure rates that waste crucial time. This delay may allow continued production of the light chains, causing further organ dysfunction.\r\n<br><br>\r\nAll patients who can tolerate high-dose melphalan therapy and autologous stem cell transplant should receive these treatments, which lead to deeper remissions with better long-term control of the disease.<sup>[11]</sup> However, patients who have extensive cardiac involvement are unable to tolerate the intensive therapy. For these high-risk patients, such therapy can result in worse outcomes, owing to increased treatment-related mortality.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 503329,
"questionText": "Which of the following is most accurate regarding the treatment of AL type amyloidosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Blackout at Rest and Slurring in a Man Afraid of COVID-19"
},
{
"authors": "Ankit Raiyani, MBBS, MD, DNB (Hematology)",
"content": [],
"date": "March 03, 2021",
"figures": [],
"markdown": "# Blackout at Rest and Slurring in a Man Afraid of COVID-19\n\n **Authors:** Ankit Raiyani, MBBS, MD, DNB (Hematology) \n **Date:** March 03, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1568305,
"choiceText": "The AA type is the most common type of systemic amyloidosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568306,
"choiceText": "AL amyloidosis is always associated with multiple myeloma",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568307,
"choiceText": "Cardiac involvement is the most common cause of mortality in amyloidosis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568308,
"choiceText": "Renal biopsy is necessary for all patients with systemic amyloidosis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The most common type of systemic amyloidosis is AL type amyloidosis (65%-70%). AA amyloidosis is the second most common (10%-15%).<sup>[1]</sup><br><br>\r\nAL amyloidosis features deposition of abnormal light chains in the extracellular space in various organs. These abnormal light chains are produced by abnormal plasma cells. It is not necessary for these plasma cells to be present in high proportions in bone marrow. In fact, monoclonal gammopathy of unknown significance is more frequently associated with AL amyloidosis than multiple myeloma. <br><br>\r\nCardiac involvement is the most common cause of the mortality in patients with amyloidosis. The prognosis is determined by the extent of cardiac disease, among other factors. <br><br>\r\nFor the diagnosis of amyloidosis, a biopsy can be obtained from any accessible organ suspected to be affected by the disease. It is not necessary to take a biopsy from all the organs either to diagnose the disease or to check for end-organ damage.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 503328,
"questionText": "Which of the following statements is most accurate regarding amyloidosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1568309,
"choiceText": "Treatment of amyloidosis is directed toward removal of the amyloid fibrils from the affected organs",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568310,
"choiceText": "All patients with AL amyloidosis who are not eligible for stem cell transplant should receive combination therapy",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568311,
"choiceText": "Only high-risk patients with AL amyloidosis should undergo autologous stem cell transplant",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568312,
"choiceText": "Patient with extensive cardiac involvement will do well with high-dose melphalan therapy and autologous stem cell transplant",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "With currently available treatment options, it is not possible to remove amyloid fibrils from affected organs. Treatment is directed toward elimination of abnormal plasma cells and decreasing the production of amyloid light chain.<sup>[1]</sup> <br><br>\r\n\r\nAs in multiple myeloma, combination therapy is preferred for initial treatment.<sup>[10]</sup> Monotherapy is associated with high failure rates that waste crucial time. This delay may allow continued production of the light chains, causing further organ dysfunction.\r\n<br><br>\r\nAll patients who can tolerate high-dose melphalan therapy and autologous stem cell transplant should receive these treatments, which lead to deeper remissions with better long-term control of the disease.<sup>[11]</sup> However, patients who have extensive cardiac involvement are unable to tolerate the intensive therapy. For these high-risk patients, such therapy can result in worse outcomes, owing to increased treatment-related mortality.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 503329,
"questionText": "Which of the following is most accurate regarding the treatment of AL type amyloidosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Blackout at Rest and Slurring in a Man Afraid of COVID-19"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1568300,
"choiceText": "Protein-losing enteropathy (eg, celiac disease)",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568301,
"choiceText": "Connective tissue disorder (eg, lupus nephritis)",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568302,
"choiceText": "Nephrotic syndrome",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568303,
"choiceText": "Systemic amyloidosis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568304,
"choiceText": "Diabetic nephropathy and autonomic neuropathy",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 503327,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1568305,
"choiceText": "The AA type is the most common type of systemic amyloidosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568306,
"choiceText": "AL amyloidosis is always associated with multiple myeloma",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568307,
"choiceText": "Cardiac involvement is the most common cause of mortality in amyloidosis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568308,
"choiceText": "Renal biopsy is necessary for all patients with systemic amyloidosis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The most common type of systemic amyloidosis is AL type amyloidosis (65%-70%). AA amyloidosis is the second most common (10%-15%).<sup>[1]</sup><br><br>\r\nAL amyloidosis features deposition of abnormal light chains in the extracellular space in various organs. These abnormal light chains are produced by abnormal plasma cells. It is not necessary for these plasma cells to be present in high proportions in bone marrow. In fact, monoclonal gammopathy of unknown significance is more frequently associated with AL amyloidosis than multiple myeloma. <br><br>\r\nCardiac involvement is the most common cause of the mortality in patients with amyloidosis. The prognosis is determined by the extent of cardiac disease, among other factors. <br><br>\r\nFor the diagnosis of amyloidosis, a biopsy can be obtained from any accessible organ suspected to be affected by the disease. It is not necessary to take a biopsy from all the organs either to diagnose the disease or to check for end-organ damage.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 503328,
"questionText": "Which of the following statements is most accurate regarding amyloidosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1568309,
"choiceText": "Treatment of amyloidosis is directed toward removal of the amyloid fibrils from the affected organs",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568310,
"choiceText": "All patients with AL amyloidosis who are not eligible for stem cell transplant should receive combination therapy",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568311,
"choiceText": "Only high-risk patients with AL amyloidosis should undergo autologous stem cell transplant",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1568312,
"choiceText": "Patient with extensive cardiac involvement will do well with high-dose melphalan therapy and autologous stem cell transplant",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "With currently available treatment options, it is not possible to remove amyloid fibrils from affected organs. Treatment is directed toward elimination of abnormal plasma cells and decreasing the production of amyloid light chain.<sup>[1]</sup> <br><br>\r\n\r\nAs in multiple myeloma, combination therapy is preferred for initial treatment.<sup>[10]</sup> Monotherapy is associated with high failure rates that waste crucial time. This delay may allow continued production of the light chains, causing further organ dysfunction.\r\n<br><br>\r\nAll patients who can tolerate high-dose melphalan therapy and autologous stem cell transplant should receive these treatments, which lead to deeper remissions with better long-term control of the disease.<sup>[11]</sup> However, patients who have extensive cardiac involvement are unable to tolerate the intensive therapy. For these high-risk patients, such therapy can result in worse outcomes, owing to increased treatment-related mortality.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 503329,
"questionText": "Which of the following is most accurate regarding the treatment of AL type amyloidosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
843821 | /viewarticle/843821 | [
{
"authors": "Dafina B. Kuzmanovska, MD, PhD",
"content": [
"Editor's Note:\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.",
"A 13-year-old boy presents to the emergency department (ED) with a history of epigastric pain, vomiting, malaise, polyuria, and a 12-lb weight loss during the past 3 months. His parents have brought him to the emergency department today because his pain and vomiting are worsening. They report no history of hematuria, hematemesis, fever, or chills. They also do not note any other associated symptoms, prior surgeries, or medical conditions.",
"The patient was previously seen by his pediatrician and is undergoing a work-up. Upper gastroendoscopy performed at a nearby hospital 2 weeks ago had revealed chronic gastritis with erosive changes in the antral region. Triple treatment for \nHelicobacter pylori, however, did not lead to any improvement. Abdominal ultrasonography also performed at that time showed mild nephrocalcinosis."
],
"date": "February 19, 2021",
"figures": [],
"markdown": "# Chronic Gastritis, a Lesion, and Weight Loss in a Teenager\n\n **Authors:** Dafina B. Kuzmanovska, MD, PhD \n **Date:** February 19, 2021\n\n ## Content\n\n Editor's Note:\nThe Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case you would like to suggest for a future Case Challenge, please contact us.\nA 13-year-old boy presents to the emergency department (ED) with a history of epigastric pain, vomiting, malaise, polyuria, and a 12-lb weight loss during the past 3 months. His parents have brought him to the emergency department today because his pain and vomiting are worsening. They report no history of hematuria, hematemesis, fever, or chills. They also do not note any other associated symptoms, prior surgeries, or medical conditions.\nThe patient was previously seen by his pediatrician and is undergoing a work-up. Upper gastroendoscopy performed at a nearby hospital 2 weeks ago had revealed chronic gastritis with erosive changes in the antral region. Triple treatment for \nHelicobacter pylori, however, did not lead to any improvement. Abdominal ultrasonography also performed at that time showed mild nephrocalcinosis.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Chronic Gastritis, a Lesion, and Weight Loss in a Teenager"
},
{
"authors": "Dafina B. Kuzmanovska, MD, PhD",
"content": [
"Upon physical examination, the child is thin and mildly ill-appearing. His temperature is 98.6°F (37°C); his pulse has a regular rhythm, with a rate of 80 beats/min; and his blood pressure is 120/70 mm Hg. The patient's respirations are regular and unlabored at 14 breaths/min.",
"The child is in mild distress secondary to his epigastric discomfort. The examination of the head and neck is normal, except that the oropharynx appears slightly dry. He has no dysmorphic facial features. His lungs are clear to auscultation, and normal respiratory effort is noted. The S1 and S2 heart sounds are normal, and no murmurs are detected. The abdomen is soft but tender to deep palpation in the epigastric region. The patient's extremities show no edema, and brisk capillary refill is noted. His skin is clear except in the gluteal region, where a nodular eczematous lesion is present (Figure 1).",
"Figure 1.",
"Figure 1.",
"Routine laboratory tests reveal a normal complete blood count and normal values for sodium, potassium, chloride, bicarbonate, and magnesium. The patient's blood urea nitrogen and serum creatinine values are elevated (22.4 mg/dL and 1.8 mg/dL, respectively). The calcium level is elevated at 14.4 mg/dL, which is confirmed with an ionized calcium level of 7.2 mg/dL. The phosphorus level is low, at 5 mg/dL. Hepatic aminotransferase values are slightly elevated (aspartate aminotransferase, 61 U/L; alanine aminotransferase, 201 U/L) and the bilirubin level is 0.7 mg/dL. A chest radiograph (Figure 2) is obtained.",
"Figure 2.",
"Figure 2.",
"The patient is hospitalized. During the hospital course, additional laboratory tests are performed. The thyroid hormone levels are in the normal range, but the parathyroid hormone level is low, at 10.91 pg/mL (normal range, 15-65 pg/mL). Vitamin D metabolites are not measured. The serum angiotensin-converting enzyme (ACE) level is normal, at 32.7 U/L (normal range, 12-42 U/L). The results of a purified protein derivative test are negative.",
"Urinalysis performed on several occasions shows a specific gravity of 1.003 and a pH of 5, with normal urinary sediment. Urinary culture findings are negative. On several occasions, marked hypercalciuria is observed, with a calcium level of 14 mg/kg and a urinary calcium/creatinine ratio (mmol/mmol) that ranges from 2.5 to 3.5. No glycosuria or aminoaciduria is noted.",
"Ultrasonography is performed, on which the parathyroid glands appear normal. Renal ultrasonography confirms mild nephrocalcinosis around the renal calices. A renal biopsy is performed. The specimen exhibits tubulointerstitial nephritis associated with tubular calcium deposits (Figure 3).",
"Figure 3.",
"Figure 3.",
"Other findings include interstitial infiltration by mononuclear cells, interstitial fibrosis, tubular necrosis, and atrophy. Dystrophic calcifications are present in some of the tubules.",
"Negative results are obtained for immunoglobulin (Ig) A, IgG, IgM, and C3 on immunofluorescence analysis. Immunohistochemical analysis reveals inflammatory cellular substrate CD68, macrophages, and lymphoid population. No glomerular abnormalities are evident."
],
"date": "February 19, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/843/821/843821-thumb-1.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/843/821/843821-thumb-2.jpg"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/843/821/843821-thumb-3.jpg"
}
],
"markdown": "# Chronic Gastritis, a Lesion, and Weight Loss in a Teenager\n\n **Authors:** Dafina B. Kuzmanovska, MD, PhD \n **Date:** February 19, 2021\n\n ## Content\n\n Upon physical examination, the child is thin and mildly ill-appearing. His temperature is 98.6°F (37°C); his pulse has a regular rhythm, with a rate of 80 beats/min; and his blood pressure is 120/70 mm Hg. The patient's respirations are regular and unlabored at 14 breaths/min.\nThe child is in mild distress secondary to his epigastric discomfort. The examination of the head and neck is normal, except that the oropharynx appears slightly dry. He has no dysmorphic facial features. His lungs are clear to auscultation, and normal respiratory effort is noted. The S1 and S2 heart sounds are normal, and no murmurs are detected. The abdomen is soft but tender to deep palpation in the epigastric region. The patient's extremities show no edema, and brisk capillary refill is noted. His skin is clear except in the gluteal region, where a nodular eczematous lesion is present (Figure 1).\nFigure 1.\nFigure 1.\nRoutine laboratory tests reveal a normal complete blood count and normal values for sodium, potassium, chloride, bicarbonate, and magnesium. The patient's blood urea nitrogen and serum creatinine values are elevated (22.4 mg/dL and 1.8 mg/dL, respectively). The calcium level is elevated at 14.4 mg/dL, which is confirmed with an ionized calcium level of 7.2 mg/dL. The phosphorus level is low, at 5 mg/dL. Hepatic aminotransferase values are slightly elevated (aspartate aminotransferase, 61 U/L; alanine aminotransferase, 201 U/L) and the bilirubin level is 0.7 mg/dL. A chest radiograph (Figure 2) is obtained.\nFigure 2.\nFigure 2.\nThe patient is hospitalized. During the hospital course, additional laboratory tests are performed. The thyroid hormone levels are in the normal range, but the parathyroid hormone level is low, at 10.91 pg/mL (normal range, 15-65 pg/mL). Vitamin D metabolites are not measured. The serum angiotensin-converting enzyme (ACE) level is normal, at 32.7 U/L (normal range, 12-42 U/L). The results of a purified protein derivative test are negative.\nUrinalysis performed on several occasions shows a specific gravity of 1.003 and a pH of 5, with normal urinary sediment. Urinary culture findings are negative. On several occasions, marked hypercalciuria is observed, with a calcium level of 14 mg/kg and a urinary calcium/creatinine ratio (mmol/mmol) that ranges from 2.5 to 3.5. No glycosuria or aminoaciduria is noted.\nUltrasonography is performed, on which the parathyroid glands appear normal. Renal ultrasonography confirms mild nephrocalcinosis around the renal calices. A renal biopsy is performed. The specimen exhibits tubulointerstitial nephritis associated with tubular calcium deposits (Figure 3).\nFigure 3.\nFigure 3.\nOther findings include interstitial infiltration by mononuclear cells, interstitial fibrosis, tubular necrosis, and atrophy. Dystrophic calcifications are present in some of the tubules.\nNegative results are obtained for immunoglobulin (Ig) A, IgG, IgM, and C3 on immunofluorescence analysis. Immunohistochemical analysis reveals inflammatory cellular substrate CD68, macrophages, and lymphoid population. No glomerular abnormalities are evident.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 838661,
"choiceText": "Complete Fanconi syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838663,
"choiceText": "Sarcoidosis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838665,
"choiceText": "IgA nephropathy",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838667,
"choiceText": "Bartter syndrome",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 263713,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Chronic Gastritis, a Lesion, and Weight Loss in a Teenager"
},
{
"authors": "Dafina B. Kuzmanovska, MD, PhD",
"content": [
"The clinical picture of this patient was dominated by nonspecific constitutional symptoms, such as fatigue, malaise, vomiting, abdominal cramps, and weight loss. He had no history of maculopapular rashes, erythema nodosum, arthritis, chronic lymphocytopenia, hepatomegaly, splenomegaly, lymphadenopathy, or uveitis. He also did not have any coughing or exertional dyspnea. The child did have vomiting and polyuria, which were caused by hypercalcemia.",
"The renal biopsy specimen indicated acute tubulointerstitial nephritis associated with tubular calcium deposits, without glomerular abnormalities. In addition, the chest radiograph demonstrated combined hilar lymphadenopathy and reticulonodular interstitial infiltrates in the upper lung zone (Figure 2).",
"Figure 2.",
"Figure 2.",
"The chest radiography findings, when considered along with the hypercalcemia, rash, and renal biopsy results, are consistent with stage 2 radiographic sarcoidosis.",
"Hypercalcemia associated with hypercalciuria and nephrocalcinosis is rare in childhood and may have many causes.[1] The most common cause is iatrogenic, followed by idiopathic infantile hypercalcemia in its mild or severe form (Williams syndrome).",
"Vitamin D intoxication is a rare cause of clinically manifested hypercalcemia, but it is associated with significant morbidity. It may be caused by endogenous synthesis of 1,25-dihydroxyvitamin D from subcutaneous fat necrosis and granulomatous disease or by excessive exogenous vitamin D intake. Hypercalcemia may also result from primary hyperparathyroidism or from increased levels of parathyroid hormone-related protein caused by certain malignancies. Finally, hypercalcemia may occur in patients with Jansen syndrome, hypophosphatemia, vitamin A intoxication, or blue-diaper syndrome, or it may occur in association with use of certain medications, most notably hydrochlorothiazide and other thiazide diuretics.[1,2]",
"An intact parathyroid hormone (PTH) level at the time of hypercalcemia is pivotal in narrowing the differential diagnosis. If the PTH level is high, the child must be thoroughly investigated for the cause of hyperparathyroidism and may require urgent surgical intervention. If the PTH level is low (as it was in this patient), additional calciotropic hormones may be assayed if appropriate testing is available. Identifying the abnormal calciotropic hormone might allow diagnosis of the specific cause, elucidation of the mechanism for the hypercalcemia, and optimal treatment.",
"Sarcoidosis is a multisystem disorder characterized by an increased cellular immune response to an unknown antigen and the formation of noncaseating granulomas in affected tissues. Although the lungs and lymph nodes are the predominant sites affected by sarcoidosis (75%-90%), other organs, such as the eyes, bone marrow, kidneys, liver, and spleen, may also be involved.[2,3] Cases of extrapulmonary sarcoidosis affecting the kidneys are rare; most such cases present with nephrocalcinosis or nephrolithiasis (3.6%). Renal failure is an extremely uncommon manifestation.[4,5]",
"Hypercalcemia in sarcoidosis is uncommon, occurring in approximately 10% of cases.[2,3] It is usually caused by the autonomous production of 1,25-dihydroxyvitamin D (calcitriol) by macrophages within the granuloma. These macrophages can convert 25-hydroxyvitamin D, produced by the liver, into calcitriol by possessing the 1-alpha-hydroxylase enzyme. Calcitriol then travels to the intestinal cells and promotes luminal absorption of calcium and phosphate into the circulation. Hypercalcemia is accompanied by hypercalciuria and, eventually, nephrocalcinosis (as seen in this case). Hypercalcemia may also eventually cause renal failure both by causing dehydration and by inducing renal vasoconstriction, thereby reducing the glomerular filtration rate.",
"Systemic corticosteroids can be used to treat hypercalcemia associated with sarcoidosis because they inhibit the production of calcitriol within the macrophages.[1,3,4]"
],
"date": "February 19, 2021",
"figures": [
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/843/821/843821-thumb-2.jpg"
}
],
"markdown": "# Chronic Gastritis, a Lesion, and Weight Loss in a Teenager\n\n **Authors:** Dafina B. Kuzmanovska, MD, PhD \n **Date:** February 19, 2021\n\n ## Content\n\n The clinical picture of this patient was dominated by nonspecific constitutional symptoms, such as fatigue, malaise, vomiting, abdominal cramps, and weight loss. He had no history of maculopapular rashes, erythema nodosum, arthritis, chronic lymphocytopenia, hepatomegaly, splenomegaly, lymphadenopathy, or uveitis. He also did not have any coughing or exertional dyspnea. The child did have vomiting and polyuria, which were caused by hypercalcemia.\nThe renal biopsy specimen indicated acute tubulointerstitial nephritis associated with tubular calcium deposits, without glomerular abnormalities. In addition, the chest radiograph demonstrated combined hilar lymphadenopathy and reticulonodular interstitial infiltrates in the upper lung zone (Figure 2).\nFigure 2.\nFigure 2.\nThe chest radiography findings, when considered along with the hypercalcemia, rash, and renal biopsy results, are consistent with stage 2 radiographic sarcoidosis.\nHypercalcemia associated with hypercalciuria and nephrocalcinosis is rare in childhood and may have many causes.[1] The most common cause is iatrogenic, followed by idiopathic infantile hypercalcemia in its mild or severe form (Williams syndrome).\nVitamin D intoxication is a rare cause of clinically manifested hypercalcemia, but it is associated with significant morbidity. It may be caused by endogenous synthesis of 1,25-dihydroxyvitamin D from subcutaneous fat necrosis and granulomatous disease or by excessive exogenous vitamin D intake. Hypercalcemia may also result from primary hyperparathyroidism or from increased levels of parathyroid hormone-related protein caused by certain malignancies. Finally, hypercalcemia may occur in patients with Jansen syndrome, hypophosphatemia, vitamin A intoxication, or blue-diaper syndrome, or it may occur in association with use of certain medications, most notably hydrochlorothiazide and other thiazide diuretics.[1,2]\nAn intact parathyroid hormone (PTH) level at the time of hypercalcemia is pivotal in narrowing the differential diagnosis. If the PTH level is high, the child must be thoroughly investigated for the cause of hyperparathyroidism and may require urgent surgical intervention. If the PTH level is low (as it was in this patient), additional calciotropic hormones may be assayed if appropriate testing is available. Identifying the abnormal calciotropic hormone might allow diagnosis of the specific cause, elucidation of the mechanism for the hypercalcemia, and optimal treatment.\nSarcoidosis is a multisystem disorder characterized by an increased cellular immune response to an unknown antigen and the formation of noncaseating granulomas in affected tissues. Although the lungs and lymph nodes are the predominant sites affected by sarcoidosis (75%-90%), other organs, such as the eyes, bone marrow, kidneys, liver, and spleen, may also be involved.[2,3] Cases of extrapulmonary sarcoidosis affecting the kidneys are rare; most such cases present with nephrocalcinosis or nephrolithiasis (3.6%). Renal failure is an extremely uncommon manifestation.[4,5]\nHypercalcemia in sarcoidosis is uncommon, occurring in approximately 10% of cases.[2,3] It is usually caused by the autonomous production of 1,25-dihydroxyvitamin D (calcitriol) by macrophages within the granuloma. These macrophages can convert 25-hydroxyvitamin D, produced by the liver, into calcitriol by possessing the 1-alpha-hydroxylase enzyme. Calcitriol then travels to the intestinal cells and promotes luminal absorption of calcium and phosphate into the circulation. Hypercalcemia is accompanied by hypercalciuria and, eventually, nephrocalcinosis (as seen in this case). Hypercalcemia may also eventually cause renal failure both by causing dehydration and by inducing renal vasoconstriction, thereby reducing the glomerular filtration rate.\nSystemic corticosteroids can be used to treat hypercalcemia associated with sarcoidosis because they inhibit the production of calcitriol within the macrophages.[1,3,4]\n\n ## Figures\n\n **Figure 2.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 838661,
"choiceText": "Complete Fanconi syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838663,
"choiceText": "Sarcoidosis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838665,
"choiceText": "IgA nephropathy",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838667,
"choiceText": "Bartter syndrome",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 263713,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Chronic Gastritis, a Lesion, and Weight Loss in a Teenager"
},
{
"authors": "Dafina B. Kuzmanovska, MD, PhD",
"content": [
"The true incidence and prevalence of sarcoidosis in children are unknown because of the rarity of the disease and the small number of reported cases in childhood. Most reported childhood cases have occurred in patients aged 13-15 years, but the disease has also been reported in very young children.",
"Two distinct forms of childhood sarcoidosis appear to exist. Older children usually present with a multisystem disease similar to the adult manifestation, with frequent lymphadenopathy and pulmonary involvement. They also show generalized signs and symptoms, such as fever and malaise. In contrast, early-onset childhood sarcoidosis is a unique form of the disease characterized by the triad of rash, uveitis, and arthritis, usually in patients who are younger than 4 years.[3]",
"Pulmonary disease and abnormal findings on chest radiography are more common in children with sarcoidosis who are aged 8-15 years; these findings occur in 94%-100% of patients in that age group, compared with 22% of those younger than 4 years. Bilateral hilar adenopathy is the most common finding on chest radiography in children; it occurs in almost all cases. It is typically symmetrical, although it may be unilateral in rare instances. Pulmonary parenchymal involvement is common and predominantly appears radiographically as an interstitial pattern; however, nodular, alveolar, and fibrotic patterns have also been described.",
"Other uncommon manifestations include pleural effusion, pneumothorax, pleural thickening, calcification, atelectasis, and cor pulmonale. Nearly half of all children with sarcoidosis demonstrate restrictive lung disease on static and dynamic pulmonary function tests, including a reduction in total lung capacity, forced vital capacity, functional residual capacity, and transfer factor. These changes are believed to be secondary to early alveolitis progressing to fibrosis. An obstructive ventilatory pattern has been reported in approximately 15% of children with sarcoidosis. Airway obstruction may be secondary to airway hyperactivity, intrabronchial sarcoid granuloma, hilar or mediastinal lymph node compression of the airways, or bronchiectasis.[2,3]",
"The serum ACE level is increased in 30%-80% of patients with sarcoidosis and may be a surrogate marker of the total granuloma burden. False-positive findings are noted in fewer than 20% of patients with other pulmonary disorders; however, the serum ACE level may be normal in patients with active disease.[3]",
"About 40%-70% of children with sarcoidosis have palpable peripheral lymph glands. The lymph nodes typically are firm, nontender, discrete, and freely movable. They do not ulcerate and do not form draining sinuses. The most frequently involved glands are the cervical, axillary, epitrochlear, and inguinal glands. In the neck, the posterior triangle nodes are affected more commonly than the nodes in the anterior triangle. The enlarged peripheral lymph nodes are the most accessible tissue for biopsy, providing a high diagnostic yield.[3]",
"Hepatosplenomegaly occurs in as many as 43% of children with sarcoidosis at some point in their clinical course; however, clinically significant hepatic dysfunction is rare. Mild elevation in biochemical liver function test values is common (as it was in this patient), but severe liver involvement is unusual in children.[3]",
"Ocular involvement is very common in children with sarcoidosis, and a complete ophthalmologic evaluation, including a slit-lamp examination, is crucial (particularly in young children). Any part of the eye or orbit may be affected. Anterior uveitis (also known as \"iritis\" or \"iridocyclitis\") is the most frequently observed lesion, occurring in about 58%-90% of early-onset sarcoidoses, compared with 24%-54% of sarcoidosis cases in older children.",
"Sarcoid-associated uveitis can be acute or chronic and may vary from an isolated iridocyclitis to a bilateral panuveitis syndrome. If left untreated, the disease may result in synechiae, corneal opacities, glaucoma, and, eventually, blindness.",
"Conjunctival granulomas are the second most common ocular manifestation in sarcoidosis. Other forms of ocular lesions include interstitial keratitis; band keratopathy (from calcium deposition); dacryocystitis; retinal vasculitis; lacrimal gland enlargement; choroiditis; and orbital infiltration, which may result in proptosis.[3]",
"Cutaneous involvement occurs in about 24%-40% of older children with sarcoidosis and in 77% of young children with sarcoidosis. Various cutaneous eruptions are frequently found on the face, but the trunk, extremities, and buttocks may also be involved. Skin lesions of sarcoidosis may include macules, papules, nodules, hyperpigmented lesions, hypopigmented lesions, ulcers, subcutaneous tumors, and erythema nodosum. Rarely, \"scar sarcoidosis,\" the infiltration of old scars with granuloma, may present in children.[3]",
"Renal involvement is not well characterized in published series of childhood sarcoidosis. Only 32 isolated cases of sarcoidosis with renal involvement have been reported in children since 1941. Histopathologic studies have revealed epithelioid granuloma formation, interstitial infiltration by mononuclear cells, interstitial fibrosis, tubulitis, tubular atrophy, mesangial hyperplasia, glomerular fibrosis, membranous nephropathy, and vascular involvement.[3,4]"
],
"date": "February 19, 2021",
"figures": [],
"markdown": "# Chronic Gastritis, a Lesion, and Weight Loss in a Teenager\n\n **Authors:** Dafina B. Kuzmanovska, MD, PhD \n **Date:** February 19, 2021\n\n ## Content\n\n The true incidence and prevalence of sarcoidosis in children are unknown because of the rarity of the disease and the small number of reported cases in childhood. Most reported childhood cases have occurred in patients aged 13-15 years, but the disease has also been reported in very young children.\nTwo distinct forms of childhood sarcoidosis appear to exist. Older children usually present with a multisystem disease similar to the adult manifestation, with frequent lymphadenopathy and pulmonary involvement. They also show generalized signs and symptoms, such as fever and malaise. In contrast, early-onset childhood sarcoidosis is a unique form of the disease characterized by the triad of rash, uveitis, and arthritis, usually in patients who are younger than 4 years.[3]\nPulmonary disease and abnormal findings on chest radiography are more common in children with sarcoidosis who are aged 8-15 years; these findings occur in 94%-100% of patients in that age group, compared with 22% of those younger than 4 years. Bilateral hilar adenopathy is the most common finding on chest radiography in children; it occurs in almost all cases. It is typically symmetrical, although it may be unilateral in rare instances. Pulmonary parenchymal involvement is common and predominantly appears radiographically as an interstitial pattern; however, nodular, alveolar, and fibrotic patterns have also been described.\nOther uncommon manifestations include pleural effusion, pneumothorax, pleural thickening, calcification, atelectasis, and cor pulmonale. Nearly half of all children with sarcoidosis demonstrate restrictive lung disease on static and dynamic pulmonary function tests, including a reduction in total lung capacity, forced vital capacity, functional residual capacity, and transfer factor. These changes are believed to be secondary to early alveolitis progressing to fibrosis. An obstructive ventilatory pattern has been reported in approximately 15% of children with sarcoidosis. Airway obstruction may be secondary to airway hyperactivity, intrabronchial sarcoid granuloma, hilar or mediastinal lymph node compression of the airways, or bronchiectasis.[2,3]\nThe serum ACE level is increased in 30%-80% of patients with sarcoidosis and may be a surrogate marker of the total granuloma burden. False-positive findings are noted in fewer than 20% of patients with other pulmonary disorders; however, the serum ACE level may be normal in patients with active disease.[3]\nAbout 40%-70% of children with sarcoidosis have palpable peripheral lymph glands. The lymph nodes typically are firm, nontender, discrete, and freely movable. They do not ulcerate and do not form draining sinuses. The most frequently involved glands are the cervical, axillary, epitrochlear, and inguinal glands. In the neck, the posterior triangle nodes are affected more commonly than the nodes in the anterior triangle. The enlarged peripheral lymph nodes are the most accessible tissue for biopsy, providing a high diagnostic yield.[3]\nHepatosplenomegaly occurs in as many as 43% of children with sarcoidosis at some point in their clinical course; however, clinically significant hepatic dysfunction is rare. Mild elevation in biochemical liver function test values is common (as it was in this patient), but severe liver involvement is unusual in children.[3]\nOcular involvement is very common in children with sarcoidosis, and a complete ophthalmologic evaluation, including a slit-lamp examination, is crucial (particularly in young children). Any part of the eye or orbit may be affected. Anterior uveitis (also known as \"iritis\" or \"iridocyclitis\") is the most frequently observed lesion, occurring in about 58%-90% of early-onset sarcoidoses, compared with 24%-54% of sarcoidosis cases in older children.\nSarcoid-associated uveitis can be acute or chronic and may vary from an isolated iridocyclitis to a bilateral panuveitis syndrome. If left untreated, the disease may result in synechiae, corneal opacities, glaucoma, and, eventually, blindness.\nConjunctival granulomas are the second most common ocular manifestation in sarcoidosis. Other forms of ocular lesions include interstitial keratitis; band keratopathy (from calcium deposition); dacryocystitis; retinal vasculitis; lacrimal gland enlargement; choroiditis; and orbital infiltration, which may result in proptosis.[3]\nCutaneous involvement occurs in about 24%-40% of older children with sarcoidosis and in 77% of young children with sarcoidosis. Various cutaneous eruptions are frequently found on the face, but the trunk, extremities, and buttocks may also be involved. Skin lesions of sarcoidosis may include macules, papules, nodules, hyperpigmented lesions, hypopigmented lesions, ulcers, subcutaneous tumors, and erythema nodosum. Rarely, \"scar sarcoidosis,\" the infiltration of old scars with granuloma, may present in children.[3]\nRenal involvement is not well characterized in published series of childhood sarcoidosis. Only 32 isolated cases of sarcoidosis with renal involvement have been reported in children since 1941. Histopathologic studies have revealed epithelioid granuloma formation, interstitial infiltration by mononuclear cells, interstitial fibrosis, tubulitis, tubular atrophy, mesangial hyperplasia, glomerular fibrosis, membranous nephropathy, and vascular involvement.[3,4]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Chronic Gastritis, a Lesion, and Weight Loss in a Teenager"
},
{
"authors": "Dafina B. Kuzmanovska, MD, PhD",
"content": [
"The treatment of sarcoidosis remains controversial.[2,5,6] Corticosteroids remain the cornerstone of therapy, but immunosuppressive, cytotoxic, and immunomodulatory agents have emerged as viable therapeutic options for patients who do not respond to or experience adverse effects from corticosteroids. The published data most extensively documents treatment with methotrexate, but favorable responses have been noted with leflunomide, azathioprine, and antimalarial and antimicrobial agents, as well as with tumor necrosis factor–alpha inhibitors. The dosage and the duration of corticosteroid therapy must often be individualized. Treatment is continued until the clinical manifestations of the disease resolve or show significant improvement.[2,5,6]",
"The patient in this case received prednisone, 1.5 mg/kg per day for 1 month, with gradual tapering of the dose over the following 4-5 months. Hypercalcemia and renal failure reversed completely, as did the pulmonary changes seen on radiography (Figure 4).",
"Figure 4.",
"Figure 4.",
"No recurrence was observed at 1-year follow-up. Renal nephrocalcinosis persisted, however, despite symptomatic and biochemical improvement. During corticosteroid therapy, measurement of the urinary beta-2-microglobulin concentration by sodium dodecyl sulfate polyacrylamide gel electrophoresis proved a valuable monitoring tool for assessing recovery of the tubular impairment.",
"Chest radiography obtained after 3 weeks of corticosteroid therapy showed resolution of the findings seen in Figure 2.",
"Figure 2.",
"Figure 2.",
"This patient represents a rare case of sarcoidosis presenting with acute renal failure and hypercalcemia as the initial manifestations. Sarcoidosis should be considered in the differential diagnosis of hypercalcemia and renal failure, occurring singly or in combination. Corticosteroids are useful for treatment and can lead to the reversal of hypercalcemia and renal failure and the resolution of pulmonary lesions. Renal nephrocalcinosis may persist despite symptomatic and biochemical improvement."
],
"date": "February 19, 2021",
"figures": [
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/843/821/843821-thumb-4.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/843/821/843821-thumb-2.jpg"
}
],
"markdown": "# Chronic Gastritis, a Lesion, and Weight Loss in a Teenager\n\n **Authors:** Dafina B. Kuzmanovska, MD, PhD \n **Date:** February 19, 2021\n\n ## Content\n\n The treatment of sarcoidosis remains controversial.[2,5,6] Corticosteroids remain the cornerstone of therapy, but immunosuppressive, cytotoxic, and immunomodulatory agents have emerged as viable therapeutic options for patients who do not respond to or experience adverse effects from corticosteroids. The published data most extensively documents treatment with methotrexate, but favorable responses have been noted with leflunomide, azathioprine, and antimalarial and antimicrobial agents, as well as with tumor necrosis factor–alpha inhibitors. The dosage and the duration of corticosteroid therapy must often be individualized. Treatment is continued until the clinical manifestations of the disease resolve or show significant improvement.[2,5,6]\nThe patient in this case received prednisone, 1.5 mg/kg per day for 1 month, with gradual tapering of the dose over the following 4-5 months. Hypercalcemia and renal failure reversed completely, as did the pulmonary changes seen on radiography (Figure 4).\nFigure 4.\nFigure 4.\nNo recurrence was observed at 1-year follow-up. Renal nephrocalcinosis persisted, however, despite symptomatic and biochemical improvement. During corticosteroid therapy, measurement of the urinary beta-2-microglobulin concentration by sodium dodecyl sulfate polyacrylamide gel electrophoresis proved a valuable monitoring tool for assessing recovery of the tubular impairment.\nChest radiography obtained after 3 weeks of corticosteroid therapy showed resolution of the findings seen in Figure 2.\nFigure 2.\nFigure 2.\nThis patient represents a rare case of sarcoidosis presenting with acute renal failure and hypercalcemia as the initial manifestations. Sarcoidosis should be considered in the differential diagnosis of hypercalcemia and renal failure, occurring singly or in combination. Corticosteroids are useful for treatment and can lead to the reversal of hypercalcemia and renal failure and the resolution of pulmonary lesions. Renal nephrocalcinosis may persist despite symptomatic and biochemical improvement.\n\n ## Figures\n\n **Figure 4.** \n \n\n**Figure 2.** \n \n\n\n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 838669,
"choiceText": "Endogenous synthesis of 1,25-dihydroxyvitamin D",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838671,
"choiceText": "Excessive exogenous vitamin D intake",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838673,
"choiceText": "Abnormal parathyroid function",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838675,
"choiceText": "Tumor-related factors",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838677,
"choiceText": "Iatrogenic",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Hypercalcemia in sarcoidosis is uncommon, occurring in approximately 10% of cases It is usually caused by autonomous production of 1,25-dihydroxyvitamin D (calcitriol) by macrophages within the granuloma. These macrophages can convert 25-hydroxyvitamin D, produced by the liver, into calcitriol by possessing the 1-alpha-hydroxylase enzyme. Calcitriol then travels to the intestinal cells and promotes luminal absorption of calcium and phosphate into the circulation. Hypercalcemia is accompanied by hypercalciuria and, eventually, nephrocalcinosis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 263715,
"questionText": "You are evaluating a patient whom you suspect has sarcoidosis and discover that the patient has hypercalcemia. Given the probability that sarcoidosis is present, which of the following is the best explanation for this patient's hypercalcemia?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 838679,
"choiceText": "Corticosteroids",
"correct": true,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838681,
"choiceText": "Fungicides",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838683,
"choiceText": "Antiviral drugs",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838685,
"choiceText": "Antibiotics",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Corticosteroids remain the cornerstone of therapy, but immunosuppressive, cytotoxic, and immunomodulatory agents have emerged as viable therapeutic options for patients who do not respond to or experience adverse effects from corticosteroids. Published data most extensively documents treatment with methotrexate, but favorable responses have been noted with leflunomide, azathioprine, and antimalarial and antimicrobial agents, as well as with tumor necrosis factor-alpha inhibitors.<br><br>The dosage and the duration of corticosteroid therapy must often be individualized. The treatment is continued until the clinical manifestations of the disease resolve or show significant improvement.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 263717,
"questionText": "You confirm the diagnosis of sarcoidosis in the patient described above. Which of the following choices would be best for treating this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Chronic Gastritis, a Lesion, and Weight Loss in a Teenager"
},
{
"authors": "Dafina B. Kuzmanovska, MD, PhD",
"content": [],
"date": "February 19, 2021",
"figures": [],
"markdown": "# Chronic Gastritis, a Lesion, and Weight Loss in a Teenager\n\n **Authors:** Dafina B. Kuzmanovska, MD, PhD \n **Date:** February 19, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 838669,
"choiceText": "Endogenous synthesis of 1,25-dihydroxyvitamin D",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838671,
"choiceText": "Excessive exogenous vitamin D intake",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838673,
"choiceText": "Abnormal parathyroid function",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838675,
"choiceText": "Tumor-related factors",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838677,
"choiceText": "Iatrogenic",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Hypercalcemia in sarcoidosis is uncommon, occurring in approximately 10% of cases It is usually caused by autonomous production of 1,25-dihydroxyvitamin D (calcitriol) by macrophages within the granuloma. These macrophages can convert 25-hydroxyvitamin D, produced by the liver, into calcitriol by possessing the 1-alpha-hydroxylase enzyme. Calcitriol then travels to the intestinal cells and promotes luminal absorption of calcium and phosphate into the circulation. Hypercalcemia is accompanied by hypercalciuria and, eventually, nephrocalcinosis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 263715,
"questionText": "You are evaluating a patient whom you suspect has sarcoidosis and discover that the patient has hypercalcemia. Given the probability that sarcoidosis is present, which of the following is the best explanation for this patient's hypercalcemia?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 838679,
"choiceText": "Corticosteroids",
"correct": true,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838681,
"choiceText": "Fungicides",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838683,
"choiceText": "Antiviral drugs",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838685,
"choiceText": "Antibiotics",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Corticosteroids remain the cornerstone of therapy, but immunosuppressive, cytotoxic, and immunomodulatory agents have emerged as viable therapeutic options for patients who do not respond to or experience adverse effects from corticosteroids. Published data most extensively documents treatment with methotrexate, but favorable responses have been noted with leflunomide, azathioprine, and antimalarial and antimicrobial agents, as well as with tumor necrosis factor-alpha inhibitors.<br><br>The dosage and the duration of corticosteroid therapy must often be individualized. The treatment is continued until the clinical manifestations of the disease resolve or show significant improvement.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 263717,
"questionText": "You confirm the diagnosis of sarcoidosis in the patient described above. Which of the following choices would be best for treating this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Chronic Gastritis, a Lesion, and Weight Loss in a Teenager"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 838661,
"choiceText": "Complete Fanconi syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838663,
"choiceText": "Sarcoidosis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838665,
"choiceText": "IgA nephropathy",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838667,
"choiceText": "Bartter syndrome",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 263713,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 838669,
"choiceText": "Endogenous synthesis of 1,25-dihydroxyvitamin D",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838671,
"choiceText": "Excessive exogenous vitamin D intake",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838673,
"choiceText": "Abnormal parathyroid function",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838675,
"choiceText": "Tumor-related factors",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838677,
"choiceText": "Iatrogenic",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Hypercalcemia in sarcoidosis is uncommon, occurring in approximately 10% of cases It is usually caused by autonomous production of 1,25-dihydroxyvitamin D (calcitriol) by macrophages within the granuloma. These macrophages can convert 25-hydroxyvitamin D, produced by the liver, into calcitriol by possessing the 1-alpha-hydroxylase enzyme. Calcitriol then travels to the intestinal cells and promotes luminal absorption of calcium and phosphate into the circulation. Hypercalcemia is accompanied by hypercalciuria and, eventually, nephrocalcinosis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 263715,
"questionText": "You are evaluating a patient whom you suspect has sarcoidosis and discover that the patient has hypercalcemia. Given the probability that sarcoidosis is present, which of the following is the best explanation for this patient's hypercalcemia?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 838679,
"choiceText": "Corticosteroids",
"correct": true,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838681,
"choiceText": "Fungicides",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838683,
"choiceText": "Antiviral drugs",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 838685,
"choiceText": "Antibiotics",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Corticosteroids remain the cornerstone of therapy, but immunosuppressive, cytotoxic, and immunomodulatory agents have emerged as viable therapeutic options for patients who do not respond to or experience adverse effects from corticosteroids. Published data most extensively documents treatment with methotrexate, but favorable responses have been noted with leflunomide, azathioprine, and antimalarial and antimicrobial agents, as well as with tumor necrosis factor-alpha inhibitors.<br><br>The dosage and the duration of corticosteroid therapy must often be individualized. The treatment is continued until the clinical manifestations of the disease resolve or show significant improvement.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 263717,
"questionText": "You confirm the diagnosis of sarcoidosis in the patient described above. Which of the following choices would be best for treating this patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
944870 | /viewarticle/944870 | [
{
"authors": "Catherine M. Divingian, MD, PhD; Mityanand Ramnarine, MD; Jeffrey Jordan, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us .",
"A 66-year-old woman presents to the emergency department (ED) directly from her nephrologist's office. She says, \"My kidney doctor told me that if I do not come in here, I'll die!\" She is asymptomatic, and an examination of all her systems is negative.",
"The patient has no history of sudden weight loss, fever, chills, nausea, vomiting, palpitations, focal neurologic or cognitive deficits, headache, dysuria, hematuria, polydipsia, and polyuria. She claims that she feels fine but is alarmed by her nephrologist's insistence that she go to the ED immediately.",
"The patient has a history of type 2 diabetes mellitus (DM2); stage IV chronic kidney disease (CKD); essential hypertension; and two basal ganglia strokes, which occurred 3 and 4 years earlier. She was told that she was not a candidate for dialysis, and her CKD has not progressed significantly over the past 3 years. A neurologist determined that her strokes were likely caused by previous drug and tobacco use. She has no history of any cardiac disease.",
"Her medications include insulin glargine (15 units every night), lisinopril (40 mg), and omeprazole (10 mg). She recalls that her most recent A1c was 8.9%, and her blood glucose level remains below 170 mg/dL. Her only surgery was the cesarean delivery of her daughter 30 years earlier.",
"The patient is a former smoker with a 45-pack-year history and was a heavy cocaine user until she had her most recent stroke 3 years prior. She currently does not take any illicit drugs and drinks only a glass or two of wine on weekends. She has no known drug allergies. Her family history is positive for DM2 on her mother's side of the family. Her father had a myocardial infarction in his late 70s."
],
"date": "February 02, 2021",
"figures": [],
"markdown": "# A Former Cocaine User Whose Specialist Told Her She's Dying\n\n **Authors:** Catherine M. Divingian, MD, PhD; Mityanand Ramnarine, MD; Jeffrey Jordan, MD \n **Date:** February 02, 2021\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us .\nA 66-year-old woman presents to the emergency department (ED) directly from her nephrologist's office. She says, \"My kidney doctor told me that if I do not come in here, I'll die!\" She is asymptomatic, and an examination of all her systems is negative.\nThe patient has no history of sudden weight loss, fever, chills, nausea, vomiting, palpitations, focal neurologic or cognitive deficits, headache, dysuria, hematuria, polydipsia, and polyuria. She claims that she feels fine but is alarmed by her nephrologist's insistence that she go to the ED immediately.\nThe patient has a history of type 2 diabetes mellitus (DM2); stage IV chronic kidney disease (CKD); essential hypertension; and two basal ganglia strokes, which occurred 3 and 4 years earlier. She was told that she was not a candidate for dialysis, and her CKD has not progressed significantly over the past 3 years. A neurologist determined that her strokes were likely caused by previous drug and tobacco use. She has no history of any cardiac disease.\nHer medications include insulin glargine (15 units every night), lisinopril (40 mg), and omeprazole (10 mg). She recalls that her most recent A1c was 8.9%, and her blood glucose level remains below 170 mg/dL. Her only surgery was the cesarean delivery of her daughter 30 years earlier.\nThe patient is a former smoker with a 45-pack-year history and was a heavy cocaine user until she had her most recent stroke 3 years prior. She currently does not take any illicit drugs and drinks only a glass or two of wine on weekends. She has no known drug allergies. Her family history is positive for DM2 on her mother's side of the family. Her father had a myocardial infarction in his late 70s.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A Former Cocaine User Whose Specialist Told Her She's Dying"
},
{
"authors": "Catherine M. Divingian, MD, PhD; Mityanand Ramnarine, MD; Jeffrey Jordan, MD",
"content": [
"The patient appears anxious but is otherwise in no acute distress. She is obese, with a body mass index (BMI) of 35.1 kg/m2. Her temperature is 98.1°F (36.7°C). Her heart rate is 53 beats/min, and her blood pressure is 194/65 mm Hg. No edema is noted in her extremities, and auscultation reveals no cardiac murmurs, rubs, or gallops.",
"Her respiration rate is 17 breaths/min, and her oxygen saturation is 98% on room air. Lung crackles, wheezing, or rhonchi are not audible. She is breathing comfortably without using accessory muscles. There is no costovertebral tenderness. Her abdomen is soft and nontender. She is interacting appropriately, and no focal neurologic deficits are evident. Cranial nerves II-XII are grossly intact.",
"Laboratory findings are significant for the following parameters:",
"Potassium: 5.7 mEq/L (reference range, 3.7-5.2 mEq/L)",
"Blood urea nitrogen (BUN): 49 mg/dL (reference range, 8-24 mg/dL)",
"Creatinine: 3.9 mg/dL (reference range, 0.9-1.3 mg/dL)",
"Estimated glomerular filtration rate (eGFR): 13 mL/min/1.73 m2 (reference range, 90-120 mL/min/1.73 m2)",
"Blood glucose: 164 mg/dL (reference range, 82-115 mg/dL)",
"The patient's baseline creatinine and glomerular filtration rate are not known, because this is her first presentation at this hospital and she has not brought records from her nephrologist. However, because her eGFR is below the lower-end cutoff for stage IV CKD, she is considered to have acute kidney injury superimposed on chronic renal failure. All values for the complete blood cell count are within normal limits. Urinalysis reveals no casts, blood cells, ketones, or proteins.",
"The patient's electrocardiogram (ECG) shows sinus bradycardia at 51 beats/min and second-degree Mobitz type 2 atrioventricular block.",
"Her heart rate is maintained between 45 and 53 beats/min. She states that her heart rate is usually much faster, typically in the 80s, when assessed during office visits. The chest radiograph (Figure 1) is unremarkable.",
"Figure 1."
],
"date": "February 02, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/944/870/944870-Thumb2.jpg"
}
],
"markdown": "# A Former Cocaine User Whose Specialist Told Her She's Dying\n\n **Authors:** Catherine M. Divingian, MD, PhD; Mityanand Ramnarine, MD; Jeffrey Jordan, MD \n **Date:** February 02, 2021\n\n ## Content\n\n The patient appears anxious but is otherwise in no acute distress. She is obese, with a body mass index (BMI) of 35.1 kg/m2. Her temperature is 98.1°F (36.7°C). Her heart rate is 53 beats/min, and her blood pressure is 194/65 mm Hg. No edema is noted in her extremities, and auscultation reveals no cardiac murmurs, rubs, or gallops.\nHer respiration rate is 17 breaths/min, and her oxygen saturation is 98% on room air. Lung crackles, wheezing, or rhonchi are not audible. She is breathing comfortably without using accessory muscles. There is no costovertebral tenderness. Her abdomen is soft and nontender. She is interacting appropriately, and no focal neurologic deficits are evident. Cranial nerves II-XII are grossly intact.\nLaboratory findings are significant for the following parameters:\nPotassium: 5.7 mEq/L (reference range, 3.7-5.2 mEq/L)\nBlood urea nitrogen (BUN): 49 mg/dL (reference range, 8-24 mg/dL)\nCreatinine: 3.9 mg/dL (reference range, 0.9-1.3 mg/dL)\nEstimated glomerular filtration rate (eGFR): 13 mL/min/1.73 m2 (reference range, 90-120 mL/min/1.73 m2)\nBlood glucose: 164 mg/dL (reference range, 82-115 mg/dL)\nThe patient's baseline creatinine and glomerular filtration rate are not known, because this is her first presentation at this hospital and she has not brought records from her nephrologist. However, because her eGFR is below the lower-end cutoff for stage IV CKD, she is considered to have acute kidney injury superimposed on chronic renal failure. All values for the complete blood cell count are within normal limits. Urinalysis reveals no casts, blood cells, ketones, or proteins.\nThe patient's electrocardiogram (ECG) shows sinus bradycardia at 51 beats/min and second-degree Mobitz type 2 atrioventricular block.\nHer heart rate is maintained between 45 and 53 beats/min. She states that her heart rate is usually much faster, typically in the 80s, when assessed during office visits. The chest radiograph (Figure 1) is unremarkable.\nFigure 1.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1560629,
"choiceText": "Surreptitious cocaine use",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560630,
"choiceText": "Hyperosmolar hyperglycemic syndrome",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560631,
"choiceText": "End-stage renal failure secondary to diabetes mellitus",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560632,
"choiceText": "Bradycardia, renal failure, atrioventricular nodal blockade, shock, and hyperkalemia syndrome",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560633,
"choiceText": "Chronic pancreatitis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 500823,
"questionText": "On the basis of only these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Former Cocaine User Whose Specialist Told Her She's Dying"
},
{
"authors": "Catherine M. Divingian, MD, PhD; Mityanand Ramnarine, MD; Jeffrey Jordan, MD",
"content": [
"Surreptitious cocaine use is unlikely in this case. Although some patients with cocaine overdose may have no symptoms - tachycardia, hypertension, and hyperthermia are common.[1] Whereas this patient has bradycardia and is normothermic.",
"Hyperosmolar hyperglycemic syndrome is marked by elevated glucose levels and possible sodium derangements; however, in contrast to the findings in this patient, the potassium level is typically normal in hyperosmolar hyperglycemic syndrome, and bradycardia is not expected.[2]",
"Patients with end-stage renal failure secondary to diabetes mellitus typically present with electrolyte abnormalities, particularly hyperkalemia, and elevated BUN and creatinine levels. However, they usually do not have bradycardia.[3,4]",
"Chronic pancreatitis is frequently associated with abdominal pain, nausea, vomiting, and steatorrhea and resulting fat-soluble vitamin deficiencies. Weight loss is also common.[5] The patient in this case reported none of these symptoms.",
"This patient has the classic presentation of bradycardia, renal failure, atrioventricular nodal blockade, shock, and hyperkalemia (BRASH) syndrome. The signs and symptoms may initially appear disjointed making the diagnosis challenging. Additionally, the syndrome has recently been recognized, with the first description being published in 2016; thus, the pathophysiology and treatment are still poorly understood, and the condition may go unrecognized.[6,7,8,9,10]",
"To mitigate morbidity and mortality, emergency medicine providers, in particular, must be able to recognize BRASH syndrome and intervene early. Identifying the syndrome accurately is important because advanced cardiac life support (ACLS) and standard resuscitation protocols may worsen outcomes. Patients with BRASH syndrome may have a poor response to typical 'cookbook' algorithms if they are applied individually.[6,7,8] Fortunately, in this case, a medical student who was working in the ED recognized the patient's syndrome, and appropriate interventions were started in the ED before she was admitted."
],
"date": "February 02, 2021",
"figures": [],
"markdown": "# A Former Cocaine User Whose Specialist Told Her She's Dying\n\n **Authors:** Catherine M. Divingian, MD, PhD; Mityanand Ramnarine, MD; Jeffrey Jordan, MD \n **Date:** February 02, 2021\n\n ## Content\n\n Surreptitious cocaine use is unlikely in this case. Although some patients with cocaine overdose may have no symptoms - tachycardia, hypertension, and hyperthermia are common.[1] Whereas this patient has bradycardia and is normothermic.\nHyperosmolar hyperglycemic syndrome is marked by elevated glucose levels and possible sodium derangements; however, in contrast to the findings in this patient, the potassium level is typically normal in hyperosmolar hyperglycemic syndrome, and bradycardia is not expected.[2]\nPatients with end-stage renal failure secondary to diabetes mellitus typically present with electrolyte abnormalities, particularly hyperkalemia, and elevated BUN and creatinine levels. However, they usually do not have bradycardia.[3,4]\nChronic pancreatitis is frequently associated with abdominal pain, nausea, vomiting, and steatorrhea and resulting fat-soluble vitamin deficiencies. Weight loss is also common.[5] The patient in this case reported none of these symptoms.\nThis patient has the classic presentation of bradycardia, renal failure, atrioventricular nodal blockade, shock, and hyperkalemia (BRASH) syndrome. The signs and symptoms may initially appear disjointed making the diagnosis challenging. Additionally, the syndrome has recently been recognized, with the first description being published in 2016; thus, the pathophysiology and treatment are still poorly understood, and the condition may go unrecognized.[6,7,8,9,10]\nTo mitigate morbidity and mortality, emergency medicine providers, in particular, must be able to recognize BRASH syndrome and intervene early. Identifying the syndrome accurately is important because advanced cardiac life support (ACLS) and standard resuscitation protocols may worsen outcomes. Patients with BRASH syndrome may have a poor response to typical 'cookbook' algorithms if they are applied individually.[6,7,8] Fortunately, in this case, a medical student who was working in the ED recognized the patient's syndrome, and appropriate interventions were started in the ED before she was admitted.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1560629,
"choiceText": "Surreptitious cocaine use",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560630,
"choiceText": "Hyperosmolar hyperglycemic syndrome",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560631,
"choiceText": "End-stage renal failure secondary to diabetes mellitus",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560632,
"choiceText": "Bradycardia, renal failure, atrioventricular nodal blockade, shock, and hyperkalemia syndrome",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560633,
"choiceText": "Chronic pancreatitis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 500823,
"questionText": "On the basis of only these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Former Cocaine User Whose Specialist Told Her She's Dying"
},
{
"authors": "Catherine M. Divingian, MD, PhD; Mityanand Ramnarine, MD; Jeffrey Jordan, MD",
"content": [
"BRASH syndrome must be distinguished from other conditions. Patients may present with moderate hyperkalemia at levels that are usually insufficient to cause bradycardia on an ECG. In this way, pure hyperkalemia can be ruled out. Patients who have atrioventricular nodal blockade attributable to overdose toxicity have a history of taking excess medication, whereas those with BRASH syndrome typically report taking medication as prescribed.[7]",
"BRASH syndrome is cyclical in nature. Each aspect of the pathophysiology works synergistically, resulting in escalating exacerbation if proper intervention is not started. A current model shows renal failure that leads to hyperkalemia, which then drives the bradycardia, worsening perfusion and contributing to cardiogenic shock. Any part of the cycle can be entered, depending on the triggering mechanism.[6,7] Most important, BRASH syndrome is considered to be at the intersection of hyperkalemia and atrioventricular nodal blockade, with their respective pathophysiologic effects impinging upon each other.[7]",
"The most common precipitant of BRASH syndrome is hypovolemia or medications that promote hyperkalemia or renal injury[7]; however, acute infectious processes can also be possible contributors. Implicated medications include angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs), which can cause renal failure and hyperkalemia under certain conditions. Beta-blockers can contribute to hyperkalemia, particularly if they are nonselective, and to bradycardia. Calcium channel blockers (CCBs) can also slow the heart rate.[7,8] This bradycardia, in turn, reduces renal perfusion.[6]",
"One case study described trimethoprim/sulfamethoxazole (TMP/SMX)–induced BRASH syndrome due to hyperkalemia, especially when TMP/SMX is combined with potassium-sparing diuretics and mineralocorticoid antagonists. The combination magnifies acute kidney injury and bradycardia.[9] Another case report suggested that novel coronavirus disease 19 (COVID-19) can give rise to BRASH syndrome, perhaps owing to the virus's ability to induce acute tubular necrosis from hypoperfusion. Another possible etiology could be the interaction of the coronavirus with angiotensin-converting enzyme-2 receptors in the heart, lung, or kidney.[10]",
"The approach to treating BRASH syndrome is critical. A common, and potentially disastrous, mistake is to focus narrowly on one feature of the syndrome at a time, rather than to approach management from a gestalt.[1,2] All aspects of BRASH syndrome need to be treated simultaneously to improve patient outcomes.",
"Treatment starts with finding the underlying etiology and attempting to reverse it, if at all possible. Consider withholding the patient's beta-blockers, CCBs, ACEIs, or ARBs, as any of these medications could have caused the syndrome. In this case the patient was taking lisinopril, which was discontinued.",
"Antibodies to digitalis may be required in case of toxicity. Empiric antibiotics can be started for likely infectious causes.[6,7,8,9,10] ED personnel who take a thorough medical history, identify potential sick contacts, and compile an accurate patient medication list will be able to determine the root cause and how to treat it.",
"Although administering bolus fluids may be tempting, treating possible hypoperfusion without addressing other factors can lead to over-resuscitation with fluids and can potentially result in acute respiratory distress syndrome. Instead, consider judicious volume resuscitation.[9] In this case, the patient appeared to be hypovolemic and was given sodium bicarbonate solution to treat her hyperkalemia as well. However, bicarbonate alone is insufficient to treat hyperkalemia. The patient was also given a beta agonist, short-acting insulin, and dextrose to lower serum potassium by shifting it into the intracellular compartment.[11]"
],
"date": "February 02, 2021",
"figures": [],
"markdown": "# A Former Cocaine User Whose Specialist Told Her She's Dying\n\n **Authors:** Catherine M. Divingian, MD, PhD; Mityanand Ramnarine, MD; Jeffrey Jordan, MD \n **Date:** February 02, 2021\n\n ## Content\n\n BRASH syndrome must be distinguished from other conditions. Patients may present with moderate hyperkalemia at levels that are usually insufficient to cause bradycardia on an ECG. In this way, pure hyperkalemia can be ruled out. Patients who have atrioventricular nodal blockade attributable to overdose toxicity have a history of taking excess medication, whereas those with BRASH syndrome typically report taking medication as prescribed.[7]\nBRASH syndrome is cyclical in nature. Each aspect of the pathophysiology works synergistically, resulting in escalating exacerbation if proper intervention is not started. A current model shows renal failure that leads to hyperkalemia, which then drives the bradycardia, worsening perfusion and contributing to cardiogenic shock. Any part of the cycle can be entered, depending on the triggering mechanism.[6,7] Most important, BRASH syndrome is considered to be at the intersection of hyperkalemia and atrioventricular nodal blockade, with their respective pathophysiologic effects impinging upon each other.[7]\nThe most common precipitant of BRASH syndrome is hypovolemia or medications that promote hyperkalemia or renal injury[7]; however, acute infectious processes can also be possible contributors. Implicated medications include angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs), which can cause renal failure and hyperkalemia under certain conditions. Beta-blockers can contribute to hyperkalemia, particularly if they are nonselective, and to bradycardia. Calcium channel blockers (CCBs) can also slow the heart rate.[7,8] This bradycardia, in turn, reduces renal perfusion.[6]\nOne case study described trimethoprim/sulfamethoxazole (TMP/SMX)–induced BRASH syndrome due to hyperkalemia, especially when TMP/SMX is combined with potassium-sparing diuretics and mineralocorticoid antagonists. The combination magnifies acute kidney injury and bradycardia.[9] Another case report suggested that novel coronavirus disease 19 (COVID-19) can give rise to BRASH syndrome, perhaps owing to the virus's ability to induce acute tubular necrosis from hypoperfusion. Another possible etiology could be the interaction of the coronavirus with angiotensin-converting enzyme-2 receptors in the heart, lung, or kidney.[10]\nThe approach to treating BRASH syndrome is critical. A common, and potentially disastrous, mistake is to focus narrowly on one feature of the syndrome at a time, rather than to approach management from a gestalt.[1,2] All aspects of BRASH syndrome need to be treated simultaneously to improve patient outcomes.\nTreatment starts with finding the underlying etiology and attempting to reverse it, if at all possible. Consider withholding the patient's beta-blockers, CCBs, ACEIs, or ARBs, as any of these medications could have caused the syndrome. In this case the patient was taking lisinopril, which was discontinued.\nAntibodies to digitalis may be required in case of toxicity. Empiric antibiotics can be started for likely infectious causes.[6,7,8,9,10] ED personnel who take a thorough medical history, identify potential sick contacts, and compile an accurate patient medication list will be able to determine the root cause and how to treat it.\nAlthough administering bolus fluids may be tempting, treating possible hypoperfusion without addressing other factors can lead to over-resuscitation with fluids and can potentially result in acute respiratory distress syndrome. Instead, consider judicious volume resuscitation.[9] In this case, the patient appeared to be hypovolemic and was given sodium bicarbonate solution to treat her hyperkalemia as well. However, bicarbonate alone is insufficient to treat hyperkalemia. The patient was also given a beta agonist, short-acting insulin, and dextrose to lower serum potassium by shifting it into the intracellular compartment.[11]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A Former Cocaine User Whose Specialist Told Her She's Dying"
},
{
"authors": "Catherine M. Divingian, MD, PhD; Mityanand Ramnarine, MD; Jeffrey Jordan, MD",
"content": [
"Focusing on bradycardia may cause the healthcare provider to start with atropine when following ACLS protocols. This drug may not be useful in BRASH syndrome, as the slowed heart rate is probably not because of poor vagal tone.[6,7] Furthermore, implementing the bradycardia protocol could lead to worsening morbidity or mortality.",
"One case demonstrated that ACLS protocols performed without consideration for the entire syndrome resulted in the death of an 80-year-old woman after she had undergone transcutaneous pacing and had received pressor support for hypotension. The author concluded that focusing on cardiogenic shock can worsen BRASH syndrome, especially in an elderly patient.[6] Although the patient in this case did not show signs of shock when she arrived at the ED, cardiogenic shock would have been the expected sequela, if she had not been adequately treated.[6] The patient's bradycardia was addressed with transcutaneous pacing when her heart rate dipped into the 40s. Importantly, untreated hyperkalemia can also result in 'failure to capture' with a pacemaker; this underscores the importance of pursuing a multifactorial approach to BRASH and simultaneous treatment of hyperkalemia and bradycardia.[12]",
"The patient in this case did not show ECG signs of hyperkalemia, as is the case in other patients with BRASH syndrome. In fact, ECG abnormalities of any type, including bradycardia, could be considered evidence of hyperkalemia. Calcium gluconate or chloride should be administered to stabilize the cardiac membranes; however, the effect is short-lived and more doses may be required. Insulin with dextrose can be important in mitigating hyperkalemia while reducing the effects of beta-blocker or CCB toxicity, especially in patients with elevated glucose levels. Epinephrine has a prolonged effect in reducing blood potassium levels and has the added benefit of positive chronotropic effects and potential improvement in renal perfusion.[7]",
"The treatment of hyperkalemia depends on the patient's presentation. Hypovolemia should be treated judiciously with sodium bicarbonate solution, which may help further mitigate the hyperkalemia. Loop diuretics should be used with caution, as they may worsen hypovolemia and exacerbate the acute kidney injury, even if they are useful in reducing potassium levels. Emergency dialysis should be considered as a last resort if the hyperkalemia is refractory to other treatments.[6,7,8,9,10] The patient in this case was treated with calcium gluconate. As mentioned above, she also received sodium bicarbonate solution for hypovolemia as well as a beta agonist and insulin with dextrose for hyperkalemia.",
"Each case requires consideration of an optimal approach to treat BRASH syndrome. Literature shows that a holistic approach to the syndrome can enhance patient outcomes.[6,7,8,9,10] In the patient in this case, the potential triggering medication, lisinopril, was withheld. Her hyperkalemia, hypovolemia, bradycardia, and worsening renal function were addressed as described above. She was given hydralazine to reduce her blood pressure. The patient remained hemodynamically stable and was admitted to the floor; she ultimately recovered."
],
"date": "February 02, 2021",
"figures": [],
"markdown": "# A Former Cocaine User Whose Specialist Told Her She's Dying\n\n **Authors:** Catherine M. Divingian, MD, PhD; Mityanand Ramnarine, MD; Jeffrey Jordan, MD \n **Date:** February 02, 2021\n\n ## Content\n\n Focusing on bradycardia may cause the healthcare provider to start with atropine when following ACLS protocols. This drug may not be useful in BRASH syndrome, as the slowed heart rate is probably not because of poor vagal tone.[6,7] Furthermore, implementing the bradycardia protocol could lead to worsening morbidity or mortality.\nOne case demonstrated that ACLS protocols performed without consideration for the entire syndrome resulted in the death of an 80-year-old woman after she had undergone transcutaneous pacing and had received pressor support for hypotension. The author concluded that focusing on cardiogenic shock can worsen BRASH syndrome, especially in an elderly patient.[6] Although the patient in this case did not show signs of shock when she arrived at the ED, cardiogenic shock would have been the expected sequela, if she had not been adequately treated.[6] The patient's bradycardia was addressed with transcutaneous pacing when her heart rate dipped into the 40s. Importantly, untreated hyperkalemia can also result in 'failure to capture' with a pacemaker; this underscores the importance of pursuing a multifactorial approach to BRASH and simultaneous treatment of hyperkalemia and bradycardia.[12]\nThe patient in this case did not show ECG signs of hyperkalemia, as is the case in other patients with BRASH syndrome. In fact, ECG abnormalities of any type, including bradycardia, could be considered evidence of hyperkalemia. Calcium gluconate or chloride should be administered to stabilize the cardiac membranes; however, the effect is short-lived and more doses may be required. Insulin with dextrose can be important in mitigating hyperkalemia while reducing the effects of beta-blocker or CCB toxicity, especially in patients with elevated glucose levels. Epinephrine has a prolonged effect in reducing blood potassium levels and has the added benefit of positive chronotropic effects and potential improvement in renal perfusion.[7]\nThe treatment of hyperkalemia depends on the patient's presentation. Hypovolemia should be treated judiciously with sodium bicarbonate solution, which may help further mitigate the hyperkalemia. Loop diuretics should be used with caution, as they may worsen hypovolemia and exacerbate the acute kidney injury, even if they are useful in reducing potassium levels. Emergency dialysis should be considered as a last resort if the hyperkalemia is refractory to other treatments.[6,7,8,9,10] The patient in this case was treated with calcium gluconate. As mentioned above, she also received sodium bicarbonate solution for hypovolemia as well as a beta agonist and insulin with dextrose for hyperkalemia.\nEach case requires consideration of an optimal approach to treat BRASH syndrome. Literature shows that a holistic approach to the syndrome can enhance patient outcomes.[6,7,8,9,10] In the patient in this case, the potential triggering medication, lisinopril, was withheld. Her hyperkalemia, hypovolemia, bradycardia, and worsening renal function were addressed as described above. She was given hydralazine to reduce her blood pressure. The patient remained hemodynamically stable and was admitted to the floor; she ultimately recovered.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1560634,
"choiceText": "Administer digitalis antibodies",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560635,
"choiceText": "Give glucagon",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560636,
"choiceText": "Start 5% dextrose in water (D5W) ½ normal saline",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560637,
"choiceText": "Order a renal vein ultrasonogram",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560638,
"choiceText": "Check for carotenoid overdose",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nDigitalis has been shown to be a potential contributor to BRASH syndrome.<sup>[7]</sup> In addition to discontinuation of his beta-blocker, administration of antibodies to digitalis would target the cause of the syndrome.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 500824,
"questionText": "A 72-year-old man presents to the ED with nausea and vomiting. He has a history of coronary artery disease, chronic atrial fibrillation, and diastolic heart failure. His medications include metoprolol succinate, digitalis, atorvastatin, and aspirin. His heart rate is 49 beats/min; blood pressure, 189/98 mm Hg; and respiration rate, 17 breaths/min. He is afebrile. He describes changes in his vision saying, “Everything looks yellow.” <br><br>\r\nAbnormal laboratory findings are noted - potassium level of 6.1 mEq/L (reference range, 3.7-5.2 mEq/L); creatinine level of 1.5 mg/dL (his baseline is 1.1 mg/dL); and BUN level of 30 mg/dL (reference range, 8-24 mg/dL). His ECG shows a new Mobitz type 2 atrioventricular block. <br><br>\r\nIn addition to discontinuation of his beta-blocker, which of the following steps would best address the management of his BRASH syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1560639,
"choiceText": "Calcium and lactulose",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560640,
"choiceText": "Calcium and sodium bicarbonate intravenous solution",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560641,
"choiceText": "Calcium, beta agonist, and sodium bicarbonate intravenous solution",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560642,
"choiceText": "Calcium, beta agonist, insulin, and sodium bicarbonate intravenous solution",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Although multiple approaches can be used to address hyperkalemia, calcium is important for stabilizing cardiac membranes. A beta agonist plus insulin, as well as sodium bicarbonate, can assist with volume resuscitation and help reduce potassium levels.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 500825,
"questionText": "Which of the following is most likely to be the best approach to reduce the potassium level of the patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Former Cocaine User Whose Specialist Told Her She's Dying"
},
{
"authors": "Catherine M. Divingian, MD, PhD; Mityanand Ramnarine, MD; Jeffrey Jordan, MD",
"content": [],
"date": "February 02, 2021",
"figures": [],
"markdown": "# A Former Cocaine User Whose Specialist Told Her She's Dying\n\n **Authors:** Catherine M. Divingian, MD, PhD; Mityanand Ramnarine, MD; Jeffrey Jordan, MD \n **Date:** February 02, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1560634,
"choiceText": "Administer digitalis antibodies",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560635,
"choiceText": "Give glucagon",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560636,
"choiceText": "Start 5% dextrose in water (D5W) ½ normal saline",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560637,
"choiceText": "Order a renal vein ultrasonogram",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560638,
"choiceText": "Check for carotenoid overdose",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nDigitalis has been shown to be a potential contributor to BRASH syndrome.<sup>[7]</sup> In addition to discontinuation of his beta-blocker, administration of antibodies to digitalis would target the cause of the syndrome.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 500824,
"questionText": "A 72-year-old man presents to the ED with nausea and vomiting. He has a history of coronary artery disease, chronic atrial fibrillation, and diastolic heart failure. His medications include metoprolol succinate, digitalis, atorvastatin, and aspirin. His heart rate is 49 beats/min; blood pressure, 189/98 mm Hg; and respiration rate, 17 breaths/min. He is afebrile. He describes changes in his vision saying, “Everything looks yellow.” <br><br>\r\nAbnormal laboratory findings are noted - potassium level of 6.1 mEq/L (reference range, 3.7-5.2 mEq/L); creatinine level of 1.5 mg/dL (his baseline is 1.1 mg/dL); and BUN level of 30 mg/dL (reference range, 8-24 mg/dL). His ECG shows a new Mobitz type 2 atrioventricular block. <br><br>\r\nIn addition to discontinuation of his beta-blocker, which of the following steps would best address the management of his BRASH syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1560639,
"choiceText": "Calcium and lactulose",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560640,
"choiceText": "Calcium and sodium bicarbonate intravenous solution",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560641,
"choiceText": "Calcium, beta agonist, and sodium bicarbonate intravenous solution",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560642,
"choiceText": "Calcium, beta agonist, insulin, and sodium bicarbonate intravenous solution",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Although multiple approaches can be used to address hyperkalemia, calcium is important for stabilizing cardiac membranes. A beta agonist plus insulin, as well as sodium bicarbonate, can assist with volume resuscitation and help reduce potassium levels.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 500825,
"questionText": "Which of the following is most likely to be the best approach to reduce the potassium level of the patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Former Cocaine User Whose Specialist Told Her She's Dying"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1560629,
"choiceText": "Surreptitious cocaine use",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560630,
"choiceText": "Hyperosmolar hyperglycemic syndrome",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560631,
"choiceText": "End-stage renal failure secondary to diabetes mellitus",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560632,
"choiceText": "Bradycardia, renal failure, atrioventricular nodal blockade, shock, and hyperkalemia syndrome",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560633,
"choiceText": "Chronic pancreatitis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 500823,
"questionText": "On the basis of only these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1560634,
"choiceText": "Administer digitalis antibodies",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560635,
"choiceText": "Give glucagon",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560636,
"choiceText": "Start 5% dextrose in water (D5W) ½ normal saline",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560637,
"choiceText": "Order a renal vein ultrasonogram",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560638,
"choiceText": "Check for carotenoid overdose",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nDigitalis has been shown to be a potential contributor to BRASH syndrome.<sup>[7]</sup> In addition to discontinuation of his beta-blocker, administration of antibodies to digitalis would target the cause of the syndrome.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 500824,
"questionText": "A 72-year-old man presents to the ED with nausea and vomiting. He has a history of coronary artery disease, chronic atrial fibrillation, and diastolic heart failure. His medications include metoprolol succinate, digitalis, atorvastatin, and aspirin. His heart rate is 49 beats/min; blood pressure, 189/98 mm Hg; and respiration rate, 17 breaths/min. He is afebrile. He describes changes in his vision saying, “Everything looks yellow.” <br><br>\r\nAbnormal laboratory findings are noted - potassium level of 6.1 mEq/L (reference range, 3.7-5.2 mEq/L); creatinine level of 1.5 mg/dL (his baseline is 1.1 mg/dL); and BUN level of 30 mg/dL (reference range, 8-24 mg/dL). His ECG shows a new Mobitz type 2 atrioventricular block. <br><br>\r\nIn addition to discontinuation of his beta-blocker, which of the following steps would best address the management of his BRASH syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1560639,
"choiceText": "Calcium and lactulose",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560640,
"choiceText": "Calcium and sodium bicarbonate intravenous solution",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560641,
"choiceText": "Calcium, beta agonist, and sodium bicarbonate intravenous solution",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1560642,
"choiceText": "Calcium, beta agonist, insulin, and sodium bicarbonate intravenous solution",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Although multiple approaches can be used to address hyperkalemia, calcium is important for stabilizing cardiac membranes. A beta agonist plus insulin, as well as sodium bicarbonate, can assist with volume resuscitation and help reduce potassium levels.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 500825,
"questionText": "Which of the following is most likely to be the best approach to reduce the potassium level of the patient?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
876162 | /viewarticle/876162 | [
{
"authors": "Caroline Tschibelu, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 26-year-old woman presents to the emergency department (ED) with confusion, agitation, sweating, and abnormal involuntary eye movement (diaphoresis and ocular clonus). The symptoms started the previous week; they were mild at first, and the patient attributed them to a heat wave in the city all week long.",
"The patient felt worse as the week went on and decided to come to the ED because she was not feeling better that morning. She started sweating profusely in the middle of the night, felt her leg muscles become stiff, and was increasingly nauseous. Her fiancé insisted she go to the ED as early as possible because she seemed agitated and confused, pacing around the apartment instead of taking a shower.",
"The patient's history is reviewed with her fiancé. She has a history of depression, for which she takes fluoxetine; her dose was increased by her psychiatrist 1 month ago. For migraines, she takes sumatriptan and ondansetron. Because her headaches have recently worsened, her neurologist started her on tramadol. She also has had a cough, for which she self-medicated with dextromethorphan. The remainder of her medical history is noncontributory.",
"She does not smoke, denies drugs and alcohol use, and has no allergies or family history of other significant illness."
],
"date": "January 20, 2021",
"figures": [],
"markdown": "# Abnormal Eye Movement and Agitated Delirium in a 26-Year-Old\n\n **Authors:** Caroline Tschibelu, MD \n **Date:** January 20, 2021\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 26-year-old woman presents to the emergency department (ED) with confusion, agitation, sweating, and abnormal involuntary eye movement (diaphoresis and ocular clonus). The symptoms started the previous week; they were mild at first, and the patient attributed them to a heat wave in the city all week long.\nThe patient felt worse as the week went on and decided to come to the ED because she was not feeling better that morning. She started sweating profusely in the middle of the night, felt her leg muscles become stiff, and was increasingly nauseous. Her fiancé insisted she go to the ED as early as possible because she seemed agitated and confused, pacing around the apartment instead of taking a shower.\nThe patient's history is reviewed with her fiancé. She has a history of depression, for which she takes fluoxetine; her dose was increased by her psychiatrist 1 month ago. For migraines, she takes sumatriptan and ondansetron. Because her headaches have recently worsened, her neurologist started her on tramadol. She also has had a cough, for which she self-medicated with dextromethorphan. The remainder of her medical history is noncontributory.\nShe does not smoke, denies drugs and alcohol use, and has no allergies or family history of other significant illness.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Abnormal Eye Movement and Agitated Delirium in a 26-Year-Old"
},
{
"authors": "Caroline Tschibelu, MD",
"content": [
"Upon physical examination, the patient has a blood pressure of 165/105 mm Hg, pulse of 128 beats/min, respiratory rate of 20 breaths/min, pulse oximetry of 98% on room air, and a temperature of 100.6°F (38.1°C).",
"The patient is a thin woman who seems agitated and restless but complies with the examination. The lung examination reveals clear breath sounds in all fields. Her heart has a regular rhythm, and no murmur is appreciated.",
"Upon neurologic evaluation, she is alert and oriented to date but not to time or place. Her speech is clear and fluent, with good repetition, comprehension, and naming. She recalls 1 out of 3 objects at 5 minutes. No tenderness or signs of trauma are found over the scalp and neck. No proptosis, lid swelling, conjunctival injection, or chemosis is observed.",
"The patient is able to identify a pen and a clock. She can count fingers and has an intact bitemporal visual field. Extraocular muscles are intact upon examination; she is able to look from right to left as well as up and down. Spontaneous right ocular clonus is observed. Her pupils are 2 mm and are reactive to light. Sensory examination of her face is unremarkable. Her tongue and uvula are midline, with a positive gag reflex. Her hearing test findings are symmetric. Shoulder-shrug findings are equal on both sides. Strength is 5/5 in the upper and lower extremities.",
"Sensory examination findings reveal symmetry to light touch, pinprick, temperature, vibration, and proprioception. The patient's reflexes are 2+, except in the lower extremities, where bilateral hyperreflexia is observed. She is able to perform rapid alternating movements. The remainder of her physical examination findings are unremarkable.",
"An ECG reveals normal sinus at a rate of 128 beats/min, without ST-T wave changes. Head CT is performed, and an example similar to the findings in this case is shown below.",
"Figure 1.",
"A urine pregnancy test result is negative. Laboratory analyses performed in the ED include a complete blood cell count, metabolic panel, hepatic panel with lipase, and troponin level. Laboratory test findings are remarkable for a white blood cell count of 12.4 × 103 cells/µL (reference range, 4.2-11.0 × 103 cells/µL), with 69% segmented neutrophils (54%-62%) and bandemia of 2% (3%-5%), and a hemoglobin level of 11.6 g/dL (reference range for women, 12-15 g/dL). Her troponin level is 0.5 ng/mL (reference range, 0-0.4 ng/mL). The remainder of laboratory test findings, including a toxicology screen and creatine phosphokinase level, were within normal limits.",
"The patient was given acetaminophen for the low-grade fever. Intravenous fluids were started, and she was admitted to the medicine floor."
],
"date": "January 20, 2021",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/876/162/876162-Thumb1.png"
}
],
"markdown": "# Abnormal Eye Movement and Agitated Delirium in a 26-Year-Old\n\n **Authors:** Caroline Tschibelu, MD \n **Date:** January 20, 2021\n\n ## Content\n\n Upon physical examination, the patient has a blood pressure of 165/105 mm Hg, pulse of 128 beats/min, respiratory rate of 20 breaths/min, pulse oximetry of 98% on room air, and a temperature of 100.6°F (38.1°C).\nThe patient is a thin woman who seems agitated and restless but complies with the examination. The lung examination reveals clear breath sounds in all fields. Her heart has a regular rhythm, and no murmur is appreciated.\nUpon neurologic evaluation, she is alert and oriented to date but not to time or place. Her speech is clear and fluent, with good repetition, comprehension, and naming. She recalls 1 out of 3 objects at 5 minutes. No tenderness or signs of trauma are found over the scalp and neck. No proptosis, lid swelling, conjunctival injection, or chemosis is observed.\nThe patient is able to identify a pen and a clock. She can count fingers and has an intact bitemporal visual field. Extraocular muscles are intact upon examination; she is able to look from right to left as well as up and down. Spontaneous right ocular clonus is observed. Her pupils are 2 mm and are reactive to light. Sensory examination of her face is unremarkable. Her tongue and uvula are midline, with a positive gag reflex. Her hearing test findings are symmetric. Shoulder-shrug findings are equal on both sides. Strength is 5/5 in the upper and lower extremities.\nSensory examination findings reveal symmetry to light touch, pinprick, temperature, vibration, and proprioception. The patient's reflexes are 2+, except in the lower extremities, where bilateral hyperreflexia is observed. She is able to perform rapid alternating movements. The remainder of her physical examination findings are unremarkable.\nAn ECG reveals normal sinus at a rate of 128 beats/min, without ST-T wave changes. Head CT is performed, and an example similar to the findings in this case is shown below.\nFigure 1.\nA urine pregnancy test result is negative. Laboratory analyses performed in the ED include a complete blood cell count, metabolic panel, hepatic panel with lipase, and troponin level. Laboratory test findings are remarkable for a white blood cell count of 12.4 × 103 cells/µL (reference range, 4.2-11.0 × 103 cells/µL), with 69% segmented neutrophils (54%-62%) and bandemia of 2% (3%-5%), and a hemoglobin level of 11.6 g/dL (reference range for women, 12-15 g/dL). Her troponin level is 0.5 ng/mL (reference range, 0-0.4 ng/mL). The remainder of laboratory test findings, including a toxicology screen and creatine phosphokinase level, were within normal limits.\nThe patient was given acetaminophen for the low-grade fever. Intravenous fluids were started, and she was admitted to the medicine floor.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1070044,
"choiceText": "Neuroleptic malignant syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070046,
"choiceText": "Malignant hyperthermia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070048,
"choiceText": "Serotonin syndrome",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070050,
"choiceText": "Anticholinergic toxicity",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070052,
"choiceText": "Meningitis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 338819,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Abnormal Eye Movement and Agitated Delirium in a 26-Year-Old"
},
{
"authors": "Caroline Tschibelu, MD",
"content": [
"Serotonin syndrome is a potentially life-threatening condition that occurs secondary to serotonin toxicity in the central and peripheral nervous systems. This can be due to a combination of serotonergic agents, an increase in therapeutic dosing of a serotonergic agent, and an overdose or inadvertent interactions of serotonergic agents. Serotonin syndrome is a clinical diagnosis; therefore, a careful and thorough history and physical and neurologic examinations are essential, as is a high level of suspicion.[1]",
"Serotonin syndrome results from excessive stimulation, or agonist activity at postsynaptic serotonin receptors; most often implicated is excessive binding at 5-HT2A and 5-HT1A receptors subtypes. Those two subtypes may be the predominant cause of symptoms.[2] Presenting symptoms can widely vary and range from mild to life-threatening.",
"Serotonin (5-HT) is produced in the neurons from L-tryptophan, and its concentration is regulated through feedback loops controlling its reuptake and metabolism. 5-HT receptors in the central nervous system regulate attention, behavior, temperature, the sleep/wake cycle, appetite, and muscle tone.[3]",
"5-HT receptors are also located in the peripheral nervous system; peripheral serotonin is produced by intestinal enterochromaffin cells and is involved in the regulation of gastrointestinal motility, uterine contraction, bronchoconstriction, and vascular tone. In addition, 5-HT in platelets promotes their aggregation.",
"No specific laboratory test is indicated to diagnose serotonin syndrome, and serotonin levels do not correlate with the severity of symptoms. The Hunter criteria are the most accurate diagnostic set available to diagnose serotonin syndrome, with 84% sensitivity and 97% specificity. The criteria require that a patient be taking a serotonergic agent and meet at least one of the following conditions[4]:",
"Spontaneous clonus",
"Inducible clonus with agitation or diaphoresis",
"Ocular clonus with agitation or diaphoresis",
"Tremor and hyperreflexia",
"Hypertonia, temperature > 100.4°F (38°C), and ocular or inducible clonus"
],
"date": "January 20, 2021",
"figures": [],
"markdown": "# Abnormal Eye Movement and Agitated Delirium in a 26-Year-Old\n\n **Authors:** Caroline Tschibelu, MD \n **Date:** January 20, 2021\n\n ## Content\n\n Serotonin syndrome is a potentially life-threatening condition that occurs secondary to serotonin toxicity in the central and peripheral nervous systems. This can be due to a combination of serotonergic agents, an increase in therapeutic dosing of a serotonergic agent, and an overdose or inadvertent interactions of serotonergic agents. Serotonin syndrome is a clinical diagnosis; therefore, a careful and thorough history and physical and neurologic examinations are essential, as is a high level of suspicion.[1]\nSerotonin syndrome results from excessive stimulation, or agonist activity at postsynaptic serotonin receptors; most often implicated is excessive binding at 5-HT2A and 5-HT1A receptors subtypes. Those two subtypes may be the predominant cause of symptoms.[2] Presenting symptoms can widely vary and range from mild to life-threatening.\nSerotonin (5-HT) is produced in the neurons from L-tryptophan, and its concentration is regulated through feedback loops controlling its reuptake and metabolism. 5-HT receptors in the central nervous system regulate attention, behavior, temperature, the sleep/wake cycle, appetite, and muscle tone.[3]\n5-HT receptors are also located in the peripheral nervous system; peripheral serotonin is produced by intestinal enterochromaffin cells and is involved in the regulation of gastrointestinal motility, uterine contraction, bronchoconstriction, and vascular tone. In addition, 5-HT in platelets promotes their aggregation.\nNo specific laboratory test is indicated to diagnose serotonin syndrome, and serotonin levels do not correlate with the severity of symptoms. The Hunter criteria are the most accurate diagnostic set available to diagnose serotonin syndrome, with 84% sensitivity and 97% specificity. The criteria require that a patient be taking a serotonergic agent and meet at least one of the following conditions[4]:\nSpontaneous clonus\nInducible clonus with agitation or diaphoresis\nOcular clonus with agitation or diaphoresis\nTremor and hyperreflexia\nHypertonia, temperature > 100.4°F (38°C), and ocular or inducible clonus\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1070044,
"choiceText": "Neuroleptic malignant syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070046,
"choiceText": "Malignant hyperthermia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070048,
"choiceText": "Serotonin syndrome",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070050,
"choiceText": "Anticholinergic toxicity",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070052,
"choiceText": "Meningitis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 338819,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Abnormal Eye Movement and Agitated Delirium in a 26-Year-Old"
},
{
"authors": "Caroline Tschibelu, MD",
"content": [
"Besides serotonin syndrome, other differential diagnoses were considered but excluded in this case. Neuroleptic malignant syndrome (NMS) is an idiopathic drug reaction to antipsychotics that has a presentation similar to that of serotonin syndrome; however, NMS presents with bradyreflexia, hyperpyrexia, and lead-pipe rigidity.[5] Myoclonus is rarely seen with NMS, and symptoms typically resolve in days, compared with 24 hours after removal of the offending agent in serotonin syndrome.[6] In addition, patients with NMS have a history of taking a neuroleptic agent (eg, haloperidol, chlorpromazine), atypical antipsychotics, or antiemetic drugs. For NMS, dantrolene is the most effective, evidence-based drug treatment available, whereas no evidence-based drug treatments are available for serotonin syndrome.",
"Malignant hyperthermia is a disorder of skeletal muscle that results from inhalation of halogenated anesthetics (eg, halothane, sevoflurane, desflurane, isoflurane), administration of depolarizing muscle relaxants (eg, succinylcholine), or stressors (eg, vigorous exercise, heat exposure).[7] Malignant hyperthermia is considered a hypermetabolic response of skeletal muscles, and affected patients may present with hyperthermia, tachycardia, tachypnea, increased carbon dioxide production or oxygen consumption, acidosis, hyperkalemia, muscle rigidity, and rhabdomyolysis. Malignant hyperthermia is treated with dantrolene, a specific antagonist that should be available wherever general anesthesia is administered.",
"Anticholinergic toxicity results from an overdose with an anticholinergic agent and may present with hyperthermia, agitation, altered mental status, mydriasis, dry mucous membranes, urinary retention, and decreased bowel sounds.[8] Patients have normal muscular tone and reflexes in anticholinergic poisoning, compared with serotonin syndrome; the treatment is physostigmine.",
"Patients with meningitis often have a history of headache, photophobia, neck stiffness, vomiting, and diplopia; they may also present with convulsions, abnormal movements, and/or posturing.",
"Serotonin syndrome may be distinguished from other causes of agitated delirium on the basis of neuromuscular findings. Patients with sympathomimetic toxicity or infections of the central nervous system typically lack these findings.",
"The medications most commonly involved in serotonin syndrome include selective serotonin reuptake inhibitors (SSRIs), serotonin norepinephrine reuptake inhibitors (SNRIs), monoamine oxidase inhibitors (MAOIs), opioids, cough medications (eg, dextromethorphan), and antibiotics.[9]",
"Specific drugs that have the potential to cause serotonin syndrome are as follows[1,6,7,8,9,10,11,12]:",
"SSRIs",
"Citalopram",
"Fluoxetine",
"Fluvoxamine",
"Olanzapine/fluoxetine",
"Paroxetine",
"SNRIs",
"Duloxetine",
"Sibutramine",
"Venlafaxine",
"Triptans",
"Almotriptan",
"Eletriptan",
"Frovatriptan",
"Naratriptan",
"Rizatriptan",
"Sumatriptan",
"Zolmitriptan",
"Miscellaneous",
"Buspirone",
"Carbamazepine",
"Cocaine",
"Cyclobenzaprine",
"Dextromethorphan",
"Ergot alkaloids",
"Fentanyl",
"5-Hydroxytryptophan",
"Linezolid",
"Lithium",
"L-Tryptophan",
"Meperidine",
"Methadone",
"Methamphetamine",
"Methylene blue",
"Metoclopramide",
"Mirtazapine",
"Ondansetron",
"Phenelzine",
"Selegiline",
"St John's wort",
"Tramadol",
"Tranylcypromine",
"Trazodone",
"Tricyclic antidepressants",
"Valproic acid",
"Avoid prescribing the following opioids, because they precipitate or worsen serotonin syndrome in patients already receiving SSRIs or MAOIs:",
"Tramadol",
"Methadone",
"Meperidine",
"Fentanyl",
"Opioids that have not been linked to serotonin syndrome include morphine, codeine, and hydrocodone; these should be administered if no alternative is available.[10]"
],
"date": "January 20, 2021",
"figures": [],
"markdown": "# Abnormal Eye Movement and Agitated Delirium in a 26-Year-Old\n\n **Authors:** Caroline Tschibelu, MD \n **Date:** January 20, 2021\n\n ## Content\n\n Besides serotonin syndrome, other differential diagnoses were considered but excluded in this case. Neuroleptic malignant syndrome (NMS) is an idiopathic drug reaction to antipsychotics that has a presentation similar to that of serotonin syndrome; however, NMS presents with bradyreflexia, hyperpyrexia, and lead-pipe rigidity.[5] Myoclonus is rarely seen with NMS, and symptoms typically resolve in days, compared with 24 hours after removal of the offending agent in serotonin syndrome.[6] In addition, patients with NMS have a history of taking a neuroleptic agent (eg, haloperidol, chlorpromazine), atypical antipsychotics, or antiemetic drugs. For NMS, dantrolene is the most effective, evidence-based drug treatment available, whereas no evidence-based drug treatments are available for serotonin syndrome.\nMalignant hyperthermia is a disorder of skeletal muscle that results from inhalation of halogenated anesthetics (eg, halothane, sevoflurane, desflurane, isoflurane), administration of depolarizing muscle relaxants (eg, succinylcholine), or stressors (eg, vigorous exercise, heat exposure).[7] Malignant hyperthermia is considered a hypermetabolic response of skeletal muscles, and affected patients may present with hyperthermia, tachycardia, tachypnea, increased carbon dioxide production or oxygen consumption, acidosis, hyperkalemia, muscle rigidity, and rhabdomyolysis. Malignant hyperthermia is treated with dantrolene, a specific antagonist that should be available wherever general anesthesia is administered.\nAnticholinergic toxicity results from an overdose with an anticholinergic agent and may present with hyperthermia, agitation, altered mental status, mydriasis, dry mucous membranes, urinary retention, and decreased bowel sounds.[8] Patients have normal muscular tone and reflexes in anticholinergic poisoning, compared with serotonin syndrome; the treatment is physostigmine.\nPatients with meningitis often have a history of headache, photophobia, neck stiffness, vomiting, and diplopia; they may also present with convulsions, abnormal movements, and/or posturing.\nSerotonin syndrome may be distinguished from other causes of agitated delirium on the basis of neuromuscular findings. Patients with sympathomimetic toxicity or infections of the central nervous system typically lack these findings.\nThe medications most commonly involved in serotonin syndrome include selective serotonin reuptake inhibitors (SSRIs), serotonin norepinephrine reuptake inhibitors (SNRIs), monoamine oxidase inhibitors (MAOIs), opioids, cough medications (eg, dextromethorphan), and antibiotics.[9]\nSpecific drugs that have the potential to cause serotonin syndrome are as follows[1,6,7,8,9,10,11,12]:\nSSRIs\nCitalopram\nFluoxetine\nFluvoxamine\nOlanzapine/fluoxetine\nParoxetine\nSNRIs\nDuloxetine\nSibutramine\nVenlafaxine\nTriptans\nAlmotriptan\nEletriptan\nFrovatriptan\nNaratriptan\nRizatriptan\nSumatriptan\nZolmitriptan\nMiscellaneous\nBuspirone\nCarbamazepine\nCocaine\nCyclobenzaprine\nDextromethorphan\nErgot alkaloids\nFentanyl\n5-Hydroxytryptophan\nLinezolid\nLithium\nL-Tryptophan\nMeperidine\nMethadone\nMethamphetamine\nMethylene blue\nMetoclopramide\nMirtazapine\nOndansetron\nPhenelzine\nSelegiline\nSt John's wort\nTramadol\nTranylcypromine\nTrazodone\nTricyclic antidepressants\nValproic acid\nAvoid prescribing the following opioids, because they precipitate or worsen serotonin syndrome in patients already receiving SSRIs or MAOIs:\nTramadol\nMethadone\nMeperidine\nFentanyl\nOpioids that have not been linked to serotonin syndrome include morphine, codeine, and hydrocodone; these should be administered if no alternative is available.[10]\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Abnormal Eye Movement and Agitated Delirium in a 26-Year-Old"
},
{
"authors": "Caroline Tschibelu, MD",
"content": [
"Most cases of serotonin syndrome are mild and can treated by withdrawal of the offending agent and supportive care, with complete resolution of the presenting symptoms.[1] Most cases of serotonin syndrome present for care within 6-24 hours of onset of symptoms and resolve within the following 24 hours.",
"Agitation and tremors can be treated with benzodiazepines (which are nonspecific 5-HT antagonists); however, in severe cases, patients may require neuromuscular paralysis, sedation, or intubation. Hyperthermia over 106°F (41.1°C) is usually a poor prognosis. Patients presenting with hyperthermia and severe muscle rigidity should be managed with antipyretics, neuromuscular paralysis, sedation, or intubation as indicated.[11]",
"Serotonin syndrome may be complicated by rhabdomyolysis, disseminated intravascular coagulation (DIC), hepatic or renal dysfunction, and lactic acidosis. Therefore, obtaining urinalysis, renal and hepatic function measurement, and a DIC profile should be part of management. Confirm or deny use of illicit or recreational drugs, especially in cases of intentional overdose, because this may complicate the clinical picture and delay diagnosis.",
"Cyproheptadine is the recognized therapy for serotonin syndrome. Cyproheptadine is a histamine-1 receptor antagonist with anticholinergic and antiserotonergic properties. It is taken orally, and the initial dose is 4-12 mg, repeated every 2 hours, and discontinued if the maximum dose of 32 mg is reached without symptom improvement.[12]",
"Although serotonin syndrome is rare, the case of Libby Zion in 1984 was instrumental in influencing and changing medicine in an unprecedented way. Zion was a patient who had been taking phenelzine, an antidepressant.[13] The therapeutic effects of phenelzine may continue for as long as 2 weeks after discontinuation. Zion was given meperidine for agitation, which led to deadly manifestations of serotonin syndrome. That case led to reforms in the grueling hours of medical residents across the United States.",
"Serotonin syndrome resolves over time if promptly diagnosed and appropriately managed. Thus, correctly diagnosing serotonin syndrome is important. Polypharmacy also increases the risk for serotonin syndrome; therefore, reconciling a patient's medications is important if serotonin syndrome is suspected. Remember that such medications as fluoxetine have a long half-life and may require 5-8 weeks to be cleared from the system; thus, additional serotonergic medications should be cautiously added.",
"The patient in this case was successfully managed by discontinuing the inciting agents and was treated with cyproheptadine and supportive care. After complete resolution of all symptoms, the patient was discharged (2 days after admission)."
],
"date": "January 20, 2021",
"figures": [],
"markdown": "# Abnormal Eye Movement and Agitated Delirium in a 26-Year-Old\n\n **Authors:** Caroline Tschibelu, MD \n **Date:** January 20, 2021\n\n ## Content\n\n Most cases of serotonin syndrome are mild and can treated by withdrawal of the offending agent and supportive care, with complete resolution of the presenting symptoms.[1] Most cases of serotonin syndrome present for care within 6-24 hours of onset of symptoms and resolve within the following 24 hours.\nAgitation and tremors can be treated with benzodiazepines (which are nonspecific 5-HT antagonists); however, in severe cases, patients may require neuromuscular paralysis, sedation, or intubation. Hyperthermia over 106°F (41.1°C) is usually a poor prognosis. Patients presenting with hyperthermia and severe muscle rigidity should be managed with antipyretics, neuromuscular paralysis, sedation, or intubation as indicated.[11]\nSerotonin syndrome may be complicated by rhabdomyolysis, disseminated intravascular coagulation (DIC), hepatic or renal dysfunction, and lactic acidosis. Therefore, obtaining urinalysis, renal and hepatic function measurement, and a DIC profile should be part of management. Confirm or deny use of illicit or recreational drugs, especially in cases of intentional overdose, because this may complicate the clinical picture and delay diagnosis.\nCyproheptadine is the recognized therapy for serotonin syndrome. Cyproheptadine is a histamine-1 receptor antagonist with anticholinergic and antiserotonergic properties. It is taken orally, and the initial dose is 4-12 mg, repeated every 2 hours, and discontinued if the maximum dose of 32 mg is reached without symptom improvement.[12]\nAlthough serotonin syndrome is rare, the case of Libby Zion in 1984 was instrumental in influencing and changing medicine in an unprecedented way. Zion was a patient who had been taking phenelzine, an antidepressant.[13] The therapeutic effects of phenelzine may continue for as long as 2 weeks after discontinuation. Zion was given meperidine for agitation, which led to deadly manifestations of serotonin syndrome. That case led to reforms in the grueling hours of medical residents across the United States.\nSerotonin syndrome resolves over time if promptly diagnosed and appropriately managed. Thus, correctly diagnosing serotonin syndrome is important. Polypharmacy also increases the risk for serotonin syndrome; therefore, reconciling a patient's medications is important if serotonin syndrome is suspected. Remember that such medications as fluoxetine have a long half-life and may require 5-8 weeks to be cleared from the system; thus, additional serotonergic medications should be cautiously added.\nThe patient in this case was successfully managed by discontinuing the inciting agents and was treated with cyproheptadine and supportive care. After complete resolution of all symptoms, the patient was discharged (2 days after admission).\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1070054,
"choiceText": "Serum serotonin levels correlate with the severity of symptoms",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070056,
"choiceText": "Thorough history and physical and neurologic examinations are the basis for diagnosis of serotonin syndrome",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070058,
"choiceText": "The Hunter criteria require spontaneous, inducible, or ocular clonus concurrently with tremor, hyperreflexia, and fever",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070060,
"choiceText": "Specific laboratory findings, such as creatine phosphokinase level, are used to confirm the diagnosis of serotonin syndrome",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "A thorough history and physical and neurologic examinations are essential for diagnosis. No specific laboratory test is indicated to diagnose serotonin syndrome, and serotonin levels do not correlate with the severity of symptoms. The Hunter criteria are the most accurate diagnostic set available to diagnose serotonin syndrome, with 84% sensitivity and 97% specificity. They require that a patient be taking a serotonergic agent and meet at least 1 of the following conditions<sup>[4]</sup>:<br>\r\n<ul>\r\n\t<li>Spontaneous clonus;</li>\r\n\t<li>Inducible clonus with agitation or diaphoresis;</li>\r\n\t<li>Ocular clonus with agitation or diaphoresis;</li>\r\n\t<li>Tremor and hyperreflexia; or</li>\r\n\t<li>Hypertonia, temperature > 100.4°F (38°C), and ocular or inducible clonus.</li>\r\n</ul>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 338821,
"questionText": "Which of the following is accurate regarding the workup for serotonin syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1070062,
"choiceText": "Dantrolene",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070064,
"choiceText": "Supportive care",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070066,
"choiceText": "Diazepam",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070068,
"choiceText": "Cyproheptadine",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "NMS is an idiopathic drug reaction to antipsychotics that has a presentation similar to that of serotonin syndrome and is characterized by bradyreflexia, hyperpyrexia, and lead-pipe rigidity. Symptoms typically resolve in days compared with 24 hours after removal of offending agent in serotonin syndrome. Patients with NMS have a history of taking a neuroleptic agent (eg, haloperidol, chlorpromazine), atypical antipsychotics, or antiemetic drugs. For NMS, dantrolene is the most effective, evidence-based drug treatment available.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 338823,
"questionText": "A 30-year-old man presents with a 7-month history of worsening hallucinations and delusions. Management initiated by his psychiatrist 1 month ago included risperidone, lithium, olanzapine, and lorazepam. He was brought to the ED because he had been in bed for 3 days in a row and was feeling sluggish, with a temperature of 106°F (41.1°C).<br><br>\r\n\r\nUpon examination, the patient is arousable but not oriented to date, time, or place. All extremities are rigid, and reflexes are decreased. His heart rate is 110 beats/min, respiratory rate is 24 breaths/min, and blood pressure is 130/80 mm Hg. No history of illicit drug use is reported.<br><br>\r\n\r\nWhich of the following is the most appropriate treatment for this patient's clinical presentation, after removal of the offending agent?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Abnormal Eye Movement and Agitated Delirium in a 26-Year-Old"
},
{
"authors": "Caroline Tschibelu, MD",
"content": [],
"date": "January 20, 2021",
"figures": [],
"markdown": "# Abnormal Eye Movement and Agitated Delirium in a 26-Year-Old\n\n **Authors:** Caroline Tschibelu, MD \n **Date:** January 20, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1070054,
"choiceText": "Serum serotonin levels correlate with the severity of symptoms",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070056,
"choiceText": "Thorough history and physical and neurologic examinations are the basis for diagnosis of serotonin syndrome",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070058,
"choiceText": "The Hunter criteria require spontaneous, inducible, or ocular clonus concurrently with tremor, hyperreflexia, and fever",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070060,
"choiceText": "Specific laboratory findings, such as creatine phosphokinase level, are used to confirm the diagnosis of serotonin syndrome",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "A thorough history and physical and neurologic examinations are essential for diagnosis. No specific laboratory test is indicated to diagnose serotonin syndrome, and serotonin levels do not correlate with the severity of symptoms. The Hunter criteria are the most accurate diagnostic set available to diagnose serotonin syndrome, with 84% sensitivity and 97% specificity. They require that a patient be taking a serotonergic agent and meet at least 1 of the following conditions<sup>[4]</sup>:<br>\r\n<ul>\r\n\t<li>Spontaneous clonus;</li>\r\n\t<li>Inducible clonus with agitation or diaphoresis;</li>\r\n\t<li>Ocular clonus with agitation or diaphoresis;</li>\r\n\t<li>Tremor and hyperreflexia; or</li>\r\n\t<li>Hypertonia, temperature > 100.4°F (38°C), and ocular or inducible clonus.</li>\r\n</ul>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 338821,
"questionText": "Which of the following is accurate regarding the workup for serotonin syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1070062,
"choiceText": "Dantrolene",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070064,
"choiceText": "Supportive care",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070066,
"choiceText": "Diazepam",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070068,
"choiceText": "Cyproheptadine",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "NMS is an idiopathic drug reaction to antipsychotics that has a presentation similar to that of serotonin syndrome and is characterized by bradyreflexia, hyperpyrexia, and lead-pipe rigidity. Symptoms typically resolve in days compared with 24 hours after removal of offending agent in serotonin syndrome. Patients with NMS have a history of taking a neuroleptic agent (eg, haloperidol, chlorpromazine), atypical antipsychotics, or antiemetic drugs. For NMS, dantrolene is the most effective, evidence-based drug treatment available.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 338823,
"questionText": "A 30-year-old man presents with a 7-month history of worsening hallucinations and delusions. Management initiated by his psychiatrist 1 month ago included risperidone, lithium, olanzapine, and lorazepam. He was brought to the ED because he had been in bed for 3 days in a row and was feeling sluggish, with a temperature of 106°F (41.1°C).<br><br>\r\n\r\nUpon examination, the patient is arousable but not oriented to date, time, or place. All extremities are rigid, and reflexes are decreased. His heart rate is 110 beats/min, respiratory rate is 24 breaths/min, and blood pressure is 130/80 mm Hg. No history of illicit drug use is reported.<br><br>\r\n\r\nWhich of the following is the most appropriate treatment for this patient's clinical presentation, after removal of the offending agent?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Abnormal Eye Movement and Agitated Delirium in a 26-Year-Old"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1070044,
"choiceText": "Neuroleptic malignant syndrome",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070046,
"choiceText": "Malignant hyperthermia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070048,
"choiceText": "Serotonin syndrome",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070050,
"choiceText": "Anticholinergic toxicity",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070052,
"choiceText": "Meningitis",
"correct": false,
"displayOrder": 5,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 338819,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1070054,
"choiceText": "Serum serotonin levels correlate with the severity of symptoms",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070056,
"choiceText": "Thorough history and physical and neurologic examinations are the basis for diagnosis of serotonin syndrome",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070058,
"choiceText": "The Hunter criteria require spontaneous, inducible, or ocular clonus concurrently with tremor, hyperreflexia, and fever",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070060,
"choiceText": "Specific laboratory findings, such as creatine phosphokinase level, are used to confirm the diagnosis of serotonin syndrome",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "A thorough history and physical and neurologic examinations are essential for diagnosis. No specific laboratory test is indicated to diagnose serotonin syndrome, and serotonin levels do not correlate with the severity of symptoms. The Hunter criteria are the most accurate diagnostic set available to diagnose serotonin syndrome, with 84% sensitivity and 97% specificity. They require that a patient be taking a serotonergic agent and meet at least 1 of the following conditions<sup>[4]</sup>:<br>\r\n<ul>\r\n\t<li>Spontaneous clonus;</li>\r\n\t<li>Inducible clonus with agitation or diaphoresis;</li>\r\n\t<li>Ocular clonus with agitation or diaphoresis;</li>\r\n\t<li>Tremor and hyperreflexia; or</li>\r\n\t<li>Hypertonia, temperature > 100.4°F (38°C), and ocular or inducible clonus.</li>\r\n</ul>",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 338821,
"questionText": "Which of the following is accurate regarding the workup for serotonin syndrome?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1070062,
"choiceText": "Dantrolene",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070064,
"choiceText": "Supportive care",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070066,
"choiceText": "Diazepam",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1070068,
"choiceText": "Cyproheptadine",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "NMS is an idiopathic drug reaction to antipsychotics that has a presentation similar to that of serotonin syndrome and is characterized by bradyreflexia, hyperpyrexia, and lead-pipe rigidity. Symptoms typically resolve in days compared with 24 hours after removal of offending agent in serotonin syndrome. Patients with NMS have a history of taking a neuroleptic agent (eg, haloperidol, chlorpromazine), atypical antipsychotics, or antiemetic drugs. For NMS, dantrolene is the most effective, evidence-based drug treatment available.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 338823,
"questionText": "A 30-year-old man presents with a 7-month history of worsening hallucinations and delusions. Management initiated by his psychiatrist 1 month ago included risperidone, lithium, olanzapine, and lorazepam. He was brought to the ED because he had been in bed for 3 days in a row and was feeling sluggish, with a temperature of 106°F (41.1°C).<br><br>\r\n\r\nUpon examination, the patient is arousable but not oriented to date, time, or place. All extremities are rigid, and reflexes are decreased. His heart rate is 110 beats/min, respiratory rate is 24 breaths/min, and blood pressure is 130/80 mm Hg. No history of illicit drug use is reported.<br><br>\r\n\r\nWhich of the following is the most appropriate treatment for this patient's clinical presentation, after removal of the offending agent?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
907561 | /viewarticle/907561 | [
{
"authors": "Ricardo Correa, MD; Sri Harsha Tella, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 28-year-old man presents to an endocrine clinic for evaluation of a broad spectrum of symptoms, which his family members suggested were most likely the result of a hormonal abnormality. He reports episodic heart palpitations and tremors that progressed to worsening fatigue and confusion over the past 6 months. When the episodes started about 6 months ago, they typically lasted for 30-60 seconds. At that time, he had six to 10 episodes when he was awake. He does not recall having such episodes at night. Changes in weather did not affect his symptoms.",
"The patient claims that he was mostly healthy throughout his life, except for a personality disorder that was treated with psychotherapy and medications about 5 years ago. He says that he has been \"free of the disease\" for at least 5 years and denies any other comorbidities. He has been worried that \"something is wrong\" over the past 6 months, despite trying his best to keep his body in good shape by spending 2-3 hours in the gym almost 7 days per week. He admits using a supplement over the past 6 months to gain muscle, because he felt his intense workouts did not help him much.",
"His family history is significant for type 2 diabetes mellitus and premature menopause in his mother. He said that he has no clue about the health of other family members."
],
"date": "January 11, 2021",
"figures": [],
"markdown": "# A Weightlifter With Palpitations, Tremors, and Confusion\n\n **Authors:** Ricardo Correa, MD; Sri Harsha Tella, MD \n **Date:** January 11, 2021\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 28-year-old man presents to an endocrine clinic for evaluation of a broad spectrum of symptoms, which his family members suggested were most likely the result of a hormonal abnormality. He reports episodic heart palpitations and tremors that progressed to worsening fatigue and confusion over the past 6 months. When the episodes started about 6 months ago, they typically lasted for 30-60 seconds. At that time, he had six to 10 episodes when he was awake. He does not recall having such episodes at night. Changes in weather did not affect his symptoms.\nThe patient claims that he was mostly healthy throughout his life, except for a personality disorder that was treated with psychotherapy and medications about 5 years ago. He says that he has been \"free of the disease\" for at least 5 years and denies any other comorbidities. He has been worried that \"something is wrong\" over the past 6 months, despite trying his best to keep his body in good shape by spending 2-3 hours in the gym almost 7 days per week. He admits using a supplement over the past 6 months to gain muscle, because he felt his intense workouts did not help him much.\nHis family history is significant for type 2 diabetes mellitus and premature menopause in his mother. He said that he has no clue about the health of other family members.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A Weightlifter With Palpitations, Tremors, and Confusion"
},
{
"authors": "Ricardo Correa, MD; Sri Harsha Tella, MD",
"content": [
"On physical examination, the patient had a blood pressure of 110/70 mm Hg, a heart rate of 65 beats/min, a respiratory rate of 16 breaths/min, and weight of 154.3 lb (70 kg) with a body mass index of 22 kg/m2. He had a well-built, muscular body and was calm and cooperative. His neck examination revealed a normal-sized thyroid, with no palpable nodules or lymph nodes. Heart and lung examination findings were unremarkable. His abdomen was soft, nontender, and nondistended, with no central adiposity. Neurologic examination findings were unremarkable. Genital examination revealed 25 mL of volume in both testes, with no masses and normal development of the penis.",
"Coincidentally, the patient experienced the typical episode of palpitations, tremors, fatigue, and confusion during his clinic visit. His blood glucose level was 88 mg/dL. He was offered a can of orange juice and a bag of crackers, which made his symptoms disappear. A fasting test was ordered, and he was given a glucometer to log his glucose level along with the time and day when he has episodes.",
"His significant fasting laboratory data included a white blood cell count of 7000 cells/µL, a hemoglobin level of 16.8 g/dL, a hematocrit of 49.5%, and a platelet count of 200,000 cells/µL. Blood chemistry revealed a blood glucose level of 75 mg/dL, normal electrolyte levels, normal liver function test results, and creatinine level of 1 mg/dL. His lipid panel revealed a total cholesterol level of 250 mg/dL, a triglyceride level of 150 mg/dL, a low-density lipoprotein cholesterol level of 180 mg/dL, and a high-density lipoprotein cholesterol level of 45 mg/dL.",
"His thyroid-stimulating hormone level was 1.4 mIU/L, his free thyroxine level was 1 µg/dL, his 8 AM cortisol level was 12 µg/dL, his insulinlike growth factor 1 level was 190 ng/mL, and his urine metanephrine levels were within the reference range. His 8 AM total testosterone level was 700 ng/dL, his follicle-stimulating hormone level was 4.3 IU/L, and his luteinizing hormone level was 3.6 IU/L. A review of his blood glucose logs over a couple of weeks revealed a blood glucose range of 77-130 mg/dL, including fasting and postmeal readings. He reported having six to 10 episodes of palpitations, tremor, fatigue, and confusion per day and checked his fingerstick glucose level at least four or five times per day."
],
"date": "January 11, 2021",
"figures": [],
"markdown": "# A Weightlifter With Palpitations, Tremors, and Confusion\n\n **Authors:** Ricardo Correa, MD; Sri Harsha Tella, MD \n **Date:** January 11, 2021\n\n ## Content\n\n On physical examination, the patient had a blood pressure of 110/70 mm Hg, a heart rate of 65 beats/min, a respiratory rate of 16 breaths/min, and weight of 154.3 lb (70 kg) with a body mass index of 22 kg/m2. He had a well-built, muscular body and was calm and cooperative. His neck examination revealed a normal-sized thyroid, with no palpable nodules or lymph nodes. Heart and lung examination findings were unremarkable. His abdomen was soft, nontender, and nondistended, with no central adiposity. Neurologic examination findings were unremarkable. Genital examination revealed 25 mL of volume in both testes, with no masses and normal development of the penis.\nCoincidentally, the patient experienced the typical episode of palpitations, tremors, fatigue, and confusion during his clinic visit. His blood glucose level was 88 mg/dL. He was offered a can of orange juice and a bag of crackers, which made his symptoms disappear. A fasting test was ordered, and he was given a glucometer to log his glucose level along with the time and day when he has episodes.\nHis significant fasting laboratory data included a white blood cell count of 7000 cells/µL, a hemoglobin level of 16.8 g/dL, a hematocrit of 49.5%, and a platelet count of 200,000 cells/µL. Blood chemistry revealed a blood glucose level of 75 mg/dL, normal electrolyte levels, normal liver function test results, and creatinine level of 1 mg/dL. His lipid panel revealed a total cholesterol level of 250 mg/dL, a triglyceride level of 150 mg/dL, a low-density lipoprotein cholesterol level of 180 mg/dL, and a high-density lipoprotein cholesterol level of 45 mg/dL.\nHis thyroid-stimulating hormone level was 1.4 mIU/L, his free thyroxine level was 1 µg/dL, his 8 AM cortisol level was 12 µg/dL, his insulinlike growth factor 1 level was 190 ng/mL, and his urine metanephrine levels were within the reference range. His 8 AM total testosterone level was 700 ng/dL, his follicle-stimulating hormone level was 4.3 IU/L, and his luteinizing hormone level was 3.6 IU/L. A review of his blood glucose logs over a couple of weeks revealed a blood glucose range of 77-130 mg/dL, including fasting and postmeal readings. He reported having six to 10 episodes of palpitations, tremor, fatigue, and confusion per day and checked his fingerstick glucose level at least four or five times per day.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1316254,
"choiceText": "Hypogonadism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316256,
"choiceText": "Insulinoma",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316258,
"choiceText": "Pseudohypoglycemia",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316260,
"choiceText": "Hyperviscosity",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 4,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 420079,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Weightlifter With Palpitations, Tremors, and Confusion"
},
{
"authors": "Ricardo Correa, MD; Sri Harsha Tella, MD",
"content": [
"In patients without diabetes, true hypoglycemic episodes are characterized by the Whipple triad of low plasma glucose, concurrent symptoms of hypoglycemia, and resolution of symptoms when the glucose level returns to normal.[1] Adrenergic symptoms of hypoglycemia are the first to appear and typically include palpitation, tremors, anxiety, and sweating. Adrenergic symptoms appear at blood glucose ranges of 40-60 mg/dL. Thereafter, if blood glucose continues to decrease, neuroglycopenic symptoms appear. These include confusion, syncope, seizure, and coma.[2]",
"The term \"clinical pseudohypoglycemia\" is used when patients—typically those with personality or other psychological disorders—report relief of hypoglycemia symptoms after eating despite having a blood glucose level within the normal range. Pseudohypoglycemia broadly falls under two categories: (1) normal blood glucose with hypoglycemia symptoms and (2) discrepancy between fingerstick and serum blood glucose levels. The first group includes patients with a personality disorder or other psychiatric disorder, including addiction problems, which lead to hypoglycemic symptoms that are relieved after eating. However, these patients do not manifest the typical Whipple triad. They have no evidence of blood glucose levels < 70 mg/dL during a symptomatic hypoglycemic episode. The patient in this case falls into this category.",
"The patient had a past medical history of personality disorder. He did not provide detailed information about his psychiatric illness, the treatment that was administered, or why that treatment was discontinued. He was fixated on fitness and achieving a \"macho\" look and was possibly using androgenic steroids along with other supplements, although laboratory tests did not confirm this suspicion."
],
"date": "January 11, 2021",
"figures": [],
"markdown": "# A Weightlifter With Palpitations, Tremors, and Confusion\n\n **Authors:** Ricardo Correa, MD; Sri Harsha Tella, MD \n **Date:** January 11, 2021\n\n ## Content\n\n In patients without diabetes, true hypoglycemic episodes are characterized by the Whipple triad of low plasma glucose, concurrent symptoms of hypoglycemia, and resolution of symptoms when the glucose level returns to normal.[1] Adrenergic symptoms of hypoglycemia are the first to appear and typically include palpitation, tremors, anxiety, and sweating. Adrenergic symptoms appear at blood glucose ranges of 40-60 mg/dL. Thereafter, if blood glucose continues to decrease, neuroglycopenic symptoms appear. These include confusion, syncope, seizure, and coma.[2]\nThe term \"clinical pseudohypoglycemia\" is used when patients—typically those with personality or other psychological disorders—report relief of hypoglycemia symptoms after eating despite having a blood glucose level within the normal range. Pseudohypoglycemia broadly falls under two categories: (1) normal blood glucose with hypoglycemia symptoms and (2) discrepancy between fingerstick and serum blood glucose levels. The first group includes patients with a personality disorder or other psychiatric disorder, including addiction problems, which lead to hypoglycemic symptoms that are relieved after eating. However, these patients do not manifest the typical Whipple triad. They have no evidence of blood glucose levels < 70 mg/dL during a symptomatic hypoglycemic episode. The patient in this case falls into this category.\nThe patient had a past medical history of personality disorder. He did not provide detailed information about his psychiatric illness, the treatment that was administered, or why that treatment was discontinued. He was fixated on fitness and achieving a \"macho\" look and was possibly using androgenic steroids along with other supplements, although laboratory tests did not confirm this suspicion.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1316254,
"choiceText": "Hypogonadism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316256,
"choiceText": "Insulinoma",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316258,
"choiceText": "Pseudohypoglycemia",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316260,
"choiceText": "Hyperviscosity",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 4,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 420079,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Weightlifter With Palpitations, Tremors, and Confusion"
},
{
"authors": "Ricardo Correa, MD; Sri Harsha Tella, MD",
"content": [
"In investigating this case, various endocrine conditions were ruled out, including a thyroid disorder, growth hormone deficiency, pheochromocytoma/paraganglioma syndrome, and adrenal insufficiency. He did not meet the criteria for insulinoma or true hypoglycemia because he did not demonstrate all of the Whipple triad. This was a challenging case because the patient presented with all the adrenergic and neuroglycopenic symptoms of hypoglycemia; however, his blood glucose and serum glucose levels did not support this.",
"Certain disorders and conditions can cause a discrepancy between capillary blood glucose levels and plasma glucose levels.[5,6,7,8] These patients present with a very low plasma glucose level, usually in the range of 20-30 mg/dL, without any symptoms. Causes in this group of patients can include the following:",
"Decreased glucose transport through the tissues and increased tissue extraction of glucose, such as in Raynaud phenomenon, acrocyanosis, and peripheral vascular disease",
"Increased glycolysis by leukocytes and red blood cells associated with a delay in interpreting blood samples, such as in leukemia and polycythemia vera",
"Hyperviscosity syndromes, such as hypertriglyceridemia, monoclonal gammopathy of undetermined significance, and Waldenström macroglobulinemia",
"Drugs that affect glucose meter readings, including high doses of vitamin C, dopamine, and mannitol",
"Patients may occasionally hold the meter upside down and report incorrect readings. When a discrepancy is observed between glucometer readings and actual symptoms or signs, a different site may be punctured to get a blood drop for testing (ie, ear lobe).",
"Tarasova and colleagues[5] proposed that this condition should be called \"artifactual hypoglycemia\" instead of pseudohypoglycemia.[5] The term \"artifactual\" was introduced in 1961 to describe low glucose levels in a patient with chronic myelogenous leukemia due to increased glycolysis by leukocytes after delayed preparation of a venous blood sample.[9] This term has not yet been applied to guidelines.",
"None of the above conditions applied to the patient in this case because he never had a documented episode of hypoglycemia (blood glucose level < 70 mg/dL)."
],
"date": "January 11, 2021",
"figures": [],
"markdown": "# A Weightlifter With Palpitations, Tremors, and Confusion\n\n **Authors:** Ricardo Correa, MD; Sri Harsha Tella, MD \n **Date:** January 11, 2021\n\n ## Content\n\n In investigating this case, various endocrine conditions were ruled out, including a thyroid disorder, growth hormone deficiency, pheochromocytoma/paraganglioma syndrome, and adrenal insufficiency. He did not meet the criteria for insulinoma or true hypoglycemia because he did not demonstrate all of the Whipple triad. This was a challenging case because the patient presented with all the adrenergic and neuroglycopenic symptoms of hypoglycemia; however, his blood glucose and serum glucose levels did not support this.\nCertain disorders and conditions can cause a discrepancy between capillary blood glucose levels and plasma glucose levels.[5,6,7,8] These patients present with a very low plasma glucose level, usually in the range of 20-30 mg/dL, without any symptoms. Causes in this group of patients can include the following:\nDecreased glucose transport through the tissues and increased tissue extraction of glucose, such as in Raynaud phenomenon, acrocyanosis, and peripheral vascular disease\nIncreased glycolysis by leukocytes and red blood cells associated with a delay in interpreting blood samples, such as in leukemia and polycythemia vera\nHyperviscosity syndromes, such as hypertriglyceridemia, monoclonal gammopathy of undetermined significance, and Waldenström macroglobulinemia\nDrugs that affect glucose meter readings, including high doses of vitamin C, dopamine, and mannitol\nPatients may occasionally hold the meter upside down and report incorrect readings. When a discrepancy is observed between glucometer readings and actual symptoms or signs, a different site may be punctured to get a blood drop for testing (ie, ear lobe).\nTarasova and colleagues[5] proposed that this condition should be called \"artifactual hypoglycemia\" instead of pseudohypoglycemia.[5] The term \"artifactual\" was introduced in 1961 to describe low glucose levels in a patient with chronic myelogenous leukemia due to increased glycolysis by leukocytes after delayed preparation of a venous blood sample.[9] This term has not yet been applied to guidelines.\nNone of the above conditions applied to the patient in this case because he never had a documented episode of hypoglycemia (blood glucose level < 70 mg/dL).\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A Weightlifter With Palpitations, Tremors, and Confusion"
},
{
"authors": "Ricardo Correa, MD; Sri Harsha Tella, MD",
"content": [
"Although rare, insulinomas are often considered by physicians dealing with patients who present with hypoglycemic symptoms. Insulinomas are the most common functioning endocrine neoplasms of the pancreas, with an estimated incidence of 1-4 cases per million population per year. Less than 10% are reported to metastasize.[10]",
"In patients with insulinoma, episodes of hyperinsulinemic hypoglycemia cause various adrenergic and neuroglycopenic symptoms that usually emerge in the fasting state.[11] Another clinical characteristic of patients with insulinomas is weight gain due to frequent eating in order to prevent hypoglycemic events. Although the patient in this case experienced symptomatic hypoglycemic events that respond to food, he never demonstrated objective evidence of low blood sugar. Absence of the Whipple triad rendered further workup for insulinoma inappropriate.",
"Hyperviscosity syndromes should be included in the differential diagnoses of patients with hypoglycemic episodes. On the basis of the history and detailed laboratory data, the patient in this case did not have polycythemia or leukemia. Moreover, he was evaluated with multiple laboratory readings, which failed to show any blood glucose level < 70 mg/dL.",
"The other differential diagnosis to consider in this clinical scenario is hypogonadism. Although hypogonadism usually presents with fatigue and low libido, some patients can present with flushing and mood alterations. The patient in this case never complained of low libido. Hypogonadism is not related to hypoglycemia or pseudohypoglycemia. This patient had a high risk for hypogonadism due to the exogenous supplements that he was using to increase his muscle mass. However, further workup on this patient yielded normal testosterone, follicle-stimulating hormone, and luteinizing hormone levels.",
"The patient did not have typical symptoms of Raynaud phenomenon, and his physical examination did not support any connective tissue disorder. Workup was not initiated for connective tissue disorders because the possibility of these disorders presenting with only symptoms of hypoglycemia is highly unlikely. The patient's history also clearly included that he never had any issues with the weather changes. Acrocyanosis and Eisenmenger syndrome can be ruled out because he never had issues with skin color changes and could perform regular high-intensity exercise without any issues.",
"The effect of drugs on the patient's blood glucose levels was not an appropriate differential diagnosis in this case because such substances as high-dose vitamin C, dopamine, mannitol, and acetaminophen falsely lower blood glucose levels beyond normal readings. This patient never had blood glucose levels < 70 mg/dL; thus, drug-induced pseudohypoglycemia was ruled out. Other less possible causes of severe acidosis and high-flow oxygen were not appropriate for this patient because he was not critically ill.",
"The patient in this case was instructed to stop taking supplements and injections and was referred for a detailed psychiatric evaluation. His symptoms of hypoglycemia disappeared after receiving treatment from his psychiatrist for 8 months."
],
"date": "January 11, 2021",
"figures": [],
"markdown": "# A Weightlifter With Palpitations, Tremors, and Confusion\n\n **Authors:** Ricardo Correa, MD; Sri Harsha Tella, MD \n **Date:** January 11, 2021\n\n ## Content\n\n Although rare, insulinomas are often considered by physicians dealing with patients who present with hypoglycemic symptoms. Insulinomas are the most common functioning endocrine neoplasms of the pancreas, with an estimated incidence of 1-4 cases per million population per year. Less than 10% are reported to metastasize.[10]\nIn patients with insulinoma, episodes of hyperinsulinemic hypoglycemia cause various adrenergic and neuroglycopenic symptoms that usually emerge in the fasting state.[11] Another clinical characteristic of patients with insulinomas is weight gain due to frequent eating in order to prevent hypoglycemic events. Although the patient in this case experienced symptomatic hypoglycemic events that respond to food, he never demonstrated objective evidence of low blood sugar. Absence of the Whipple triad rendered further workup for insulinoma inappropriate.\nHyperviscosity syndromes should be included in the differential diagnoses of patients with hypoglycemic episodes. On the basis of the history and detailed laboratory data, the patient in this case did not have polycythemia or leukemia. Moreover, he was evaluated with multiple laboratory readings, which failed to show any blood glucose level < 70 mg/dL.\nThe other differential diagnosis to consider in this clinical scenario is hypogonadism. Although hypogonadism usually presents with fatigue and low libido, some patients can present with flushing and mood alterations. The patient in this case never complained of low libido. Hypogonadism is not related to hypoglycemia or pseudohypoglycemia. This patient had a high risk for hypogonadism due to the exogenous supplements that he was using to increase his muscle mass. However, further workup on this patient yielded normal testosterone, follicle-stimulating hormone, and luteinizing hormone levels.\nThe patient did not have typical symptoms of Raynaud phenomenon, and his physical examination did not support any connective tissue disorder. Workup was not initiated for connective tissue disorders because the possibility of these disorders presenting with only symptoms of hypoglycemia is highly unlikely. The patient's history also clearly included that he never had any issues with the weather changes. Acrocyanosis and Eisenmenger syndrome can be ruled out because he never had issues with skin color changes and could perform regular high-intensity exercise without any issues.\nThe effect of drugs on the patient's blood glucose levels was not an appropriate differential diagnosis in this case because such substances as high-dose vitamin C, dopamine, mannitol, and acetaminophen falsely lower blood glucose levels beyond normal readings. This patient never had blood glucose levels < 70 mg/dL; thus, drug-induced pseudohypoglycemia was ruled out. Other less possible causes of severe acidosis and high-flow oxygen were not appropriate for this patient because he was not critically ill.\nThe patient in this case was instructed to stop taking supplements and injections and was referred for a detailed psychiatric evaluation. His symptoms of hypoglycemia disappeared after receiving treatment from his psychiatrist for 8 months.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1316126,
"choiceText": "Raynaud phenomenon",
"correct": true,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316128,
"choiceText": "Hyperviscosity syndromes",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316130,
"choiceText": "Use of vitamin C",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316132,
"choiceText": "Eisenmenger syndrome\r\n",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Patients with Raynaud phenomenon usually have vasoconstriction in the distal phalanges that cause a false reading of blood glucose levels. If the patient has symptoms, serum glucose levels should be rechecked. The prevalence of Raynaud phenomenon is 3%-5% in the general population. The prevalence is much higher than hyperviscosity syndrome, use of high-dose vitamin C, and Eisenmenger syndrome.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 420049,
"questionText": "Which of the following is the most common cause of discrepancy between capillary glucose and serum glucose levels?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1316134,
"choiceText": "Symptoms of hyperglycemia ",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316136,
"choiceText": "Decreased insulin levels ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316138,
"choiceText": "Relief of the symptoms after eating something",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316140,
"choiceText": "Increased plasma glucose",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The Whipple triad consists of fasting hypoglycemia symptoms, a plasma glucose level < 45 mg/dL (measured at the time of symptoms), and symptoms that are relieved by administration of glucose, raising plasma glucose levels to normal levels. This triad was described by Whipple in the 1930s. Insulin levels are not included in the triad.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 420051,
"questionText": "Which of the following is part of the Whipple triad?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Weightlifter With Palpitations, Tremors, and Confusion"
},
{
"authors": "Ricardo Correa, MD; Sri Harsha Tella, MD",
"content": [],
"date": "January 11, 2021",
"figures": [],
"markdown": "# A Weightlifter With Palpitations, Tremors, and Confusion\n\n **Authors:** Ricardo Correa, MD; Sri Harsha Tella, MD \n **Date:** January 11, 2021\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1316126,
"choiceText": "Raynaud phenomenon",
"correct": true,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316128,
"choiceText": "Hyperviscosity syndromes",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316130,
"choiceText": "Use of vitamin C",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316132,
"choiceText": "Eisenmenger syndrome\r\n",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Patients with Raynaud phenomenon usually have vasoconstriction in the distal phalanges that cause a false reading of blood glucose levels. If the patient has symptoms, serum glucose levels should be rechecked. The prevalence of Raynaud phenomenon is 3%-5% in the general population. The prevalence is much higher than hyperviscosity syndrome, use of high-dose vitamin C, and Eisenmenger syndrome.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 420049,
"questionText": "Which of the following is the most common cause of discrepancy between capillary glucose and serum glucose levels?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1316134,
"choiceText": "Symptoms of hyperglycemia ",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316136,
"choiceText": "Decreased insulin levels ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316138,
"choiceText": "Relief of the symptoms after eating something",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316140,
"choiceText": "Increased plasma glucose",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The Whipple triad consists of fasting hypoglycemia symptoms, a plasma glucose level < 45 mg/dL (measured at the time of symptoms), and symptoms that are relieved by administration of glucose, raising plasma glucose levels to normal levels. This triad was described by Whipple in the 1930s. Insulin levels are not included in the triad.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 420051,
"questionText": "Which of the following is part of the Whipple triad?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A Weightlifter With Palpitations, Tremors, and Confusion"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1316254,
"choiceText": "Hypogonadism",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316256,
"choiceText": "Insulinoma",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316258,
"choiceText": "Pseudohypoglycemia",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316260,
"choiceText": "Hyperviscosity",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 4,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 420079,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1316126,
"choiceText": "Raynaud phenomenon",
"correct": true,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316128,
"choiceText": "Hyperviscosity syndromes",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316130,
"choiceText": "Use of vitamin C",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316132,
"choiceText": "Eisenmenger syndrome\r\n",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Patients with Raynaud phenomenon usually have vasoconstriction in the distal phalanges that cause a false reading of blood glucose levels. If the patient has symptoms, serum glucose levels should be rechecked. The prevalence of Raynaud phenomenon is 3%-5% in the general population. The prevalence is much higher than hyperviscosity syndrome, use of high-dose vitamin C, and Eisenmenger syndrome.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 420049,
"questionText": "Which of the following is the most common cause of discrepancy between capillary glucose and serum glucose levels?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1316134,
"choiceText": "Symptoms of hyperglycemia ",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316136,
"choiceText": "Decreased insulin levels ",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316138,
"choiceText": "Relief of the symptoms after eating something",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1316140,
"choiceText": "Increased plasma glucose",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The Whipple triad consists of fasting hypoglycemia symptoms, a plasma glucose level < 45 mg/dL (measured at the time of symptoms), and symptoms that are relieved by administration of glucose, raising plasma glucose levels to normal levels. This triad was described by Whipple in the 1930s. Insulin levels are not included in the triad.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 420051,
"questionText": "Which of the following is part of the Whipple triad?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
941704 | /viewarticle/941704 | [
{
"authors": "Avnish Sandhu, DO; Pranatharthi Chandrasekar, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us .",
"A 60-year-old woman with a history of uncontrolled diabetes, hypertension, and chronic obstructive pulmonary disease (COPD) presents during the winter with progressively worsening shortness of breath over the past 4 days. Associated symptoms include fever, chest pain, runny nose, sore throat, productive cough with hemoptysis, and diarrhea. She says she has not had night sweats, weight loss, or swelling of the lower extremities. About 1 week earlier, her husband also had coldlike symptoms.",
"The patient has a family history of diabetes and hypertension. She started smoking at age 20 years and smokes one pack of cigarettes per day. She drinks alcohol occasionally and denies any illicit drug use. She has no history of incarceration, homelessness, or recent travel."
],
"date": "December 02, 2020",
"figures": [],
"markdown": "# Dyspnea, Fever, Hemoptysis, and Diabetes in a Tobacco User\n\n **Authors:** Avnish Sandhu, DO; Pranatharthi Chandrasekar, MD \n **Date:** December 02, 2020\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us .\nA 60-year-old woman with a history of uncontrolled diabetes, hypertension, and chronic obstructive pulmonary disease (COPD) presents during the winter with progressively worsening shortness of breath over the past 4 days. Associated symptoms include fever, chest pain, runny nose, sore throat, productive cough with hemoptysis, and diarrhea. She says she has not had night sweats, weight loss, or swelling of the lower extremities. About 1 week earlier, her husband also had coldlike symptoms.\nThe patient has a family history of diabetes and hypertension. She started smoking at age 20 years and smokes one pack of cigarettes per day. She drinks alcohol occasionally and denies any illicit drug use. She has no history of incarceration, homelessness, or recent travel.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Dyspnea, Fever, Hemoptysis, and Diabetes in a Tobacco User"
},
{
"authors": "Avnish Sandhu, DO; Pranatharthi Chandrasekar, MD",
"content": [
"Her blood pressure is 110/75 mm/Hg, heart rate is 115 beats/min, and respiration rate is 38 breaths/min. Her temperature is 101.7°F (38.7°C). She is noted to be hypoxic, with an oxygen saturation of 88% on room air. Consequently, a non-rebreather mask is placed on the patient. She remains tachypneic on the non-rebreather mask, requires intubation, and is placed on a mechanical ventilator. Soon thereafter, supraventricular tachycardia develops. She receives two doses of adenosine, and the underlying rhythm is identified as atrial fibrillation.",
"The physical examination reveals dry oral mucosa with dried blood. Results of the cardiac examination are consistent with tachycardia and irregular rhythm. Upon lung examination, breath sounds are rhonchorous bilaterally, with diminished air entry on the right side. Her abdomen is soft, nontender, and nondistended, with normal bowel sounds and no rebound, guarding, or signs of peritoneal inflammation.",
"A comprehensive metabolic panel and a complete blood cell count reveal the following findings:",
"Serum creatinine level: 2.13 mg/dL (reference range, 0.7-1.2 mg/dL)",
"Aspartate aminotransferase level: 147 U/L (reference range, 5-30 U/L), with normal alkaline phosphatase and alanine aminotransferase levels",
"White blood cell count: 16 × 109/L (reference range, 4.5-11.0 × 109/L)",
"Hemoglobin level: 15.9 g/dL (reference range, 13.5-17.5 g/dL)",
"Serum lactate level: 4.2 mmol/L (reference range, 0.5-1 mmol/L)",
"Troponin I level: 0.5 ng/mL (reference range, 0-0.4 ng/mL)",
"Blood glucose level: 428 mg/dL (reference range, 74-106 mg/dL)",
"A CT scan of the chest shows a large area of consolidation in the right lower lobe with trace effusion and bilateral scattered ground-glass opacities (Figures 1 and 2). An ECG reveals atrial fibrillation, a normal axis, and diffuse ST segment elevation (Figure 3).",
"Figure 1.",
"Figure 2.",
"Figure 3.",
"A transthoracic echocardiogram demonstrates a reduced ventricular ejection fraction of 40%, with increased left ventricular wall thickness and a small pericardial effusion.",
"A real-time polymerase chain reaction (PCR) assay performed on a nasopharyngeal swab specimen is negative for SARS-CoV-2. Acid-fast bacilli smears from three endotracheal specimens are negative. Blood culture, respiratory culture with Gram staining, and a respiratory viral panel are ordered.",
"Fluid resuscitation is immediately started, and because of concerns about severe sepsis, therapy is initiated with intravenous vancomycin, ceftriaxone, and azithromycin."
],
"date": "December 02, 2020",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/941/704/941704-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/941/704/941704-Thumb2.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/941/704/941704-Thumb3.png"
}
],
"markdown": "# Dyspnea, Fever, Hemoptysis, and Diabetes in a Tobacco User\n\n **Authors:** Avnish Sandhu, DO; Pranatharthi Chandrasekar, MD \n **Date:** December 02, 2020\n\n ## Content\n\n Her blood pressure is 110/75 mm/Hg, heart rate is 115 beats/min, and respiration rate is 38 breaths/min. Her temperature is 101.7°F (38.7°C). She is noted to be hypoxic, with an oxygen saturation of 88% on room air. Consequently, a non-rebreather mask is placed on the patient. She remains tachypneic on the non-rebreather mask, requires intubation, and is placed on a mechanical ventilator. Soon thereafter, supraventricular tachycardia develops. She receives two doses of adenosine, and the underlying rhythm is identified as atrial fibrillation.\nThe physical examination reveals dry oral mucosa with dried blood. Results of the cardiac examination are consistent with tachycardia and irregular rhythm. Upon lung examination, breath sounds are rhonchorous bilaterally, with diminished air entry on the right side. Her abdomen is soft, nontender, and nondistended, with normal bowel sounds and no rebound, guarding, or signs of peritoneal inflammation.\nA comprehensive metabolic panel and a complete blood cell count reveal the following findings:\nSerum creatinine level: 2.13 mg/dL (reference range, 0.7-1.2 mg/dL)\nAspartate aminotransferase level: 147 U/L (reference range, 5-30 U/L), with normal alkaline phosphatase and alanine aminotransferase levels\nWhite blood cell count: 16 × 109/L (reference range, 4.5-11.0 × 109/L)\nHemoglobin level: 15.9 g/dL (reference range, 13.5-17.5 g/dL)\nSerum lactate level: 4.2 mmol/L (reference range, 0.5-1 mmol/L)\nTroponin I level: 0.5 ng/mL (reference range, 0-0.4 ng/mL)\nBlood glucose level: 428 mg/dL (reference range, 74-106 mg/dL)\nA CT scan of the chest shows a large area of consolidation in the right lower lobe with trace effusion and bilateral scattered ground-glass opacities (Figures 1 and 2). An ECG reveals atrial fibrillation, a normal axis, and diffuse ST segment elevation (Figure 3).\nFigure 1.\nFigure 2.\nFigure 3.\nA transthoracic echocardiogram demonstrates a reduced ventricular ejection fraction of 40%, with increased left ventricular wall thickness and a small pericardial effusion.\nA real-time polymerase chain reaction (PCR) assay performed on a nasopharyngeal swab specimen is negative for SARS-CoV-2. Acid-fast bacilli smears from three endotracheal specimens are negative. Blood culture, respiratory culture with Gram staining, and a respiratory viral panel are ordered.\nFluid resuscitation is immediately started, and because of concerns about severe sepsis, therapy is initiated with intravenous vancomycin, ceftriaxone, and azithromycin.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1545572,
"choiceText": "\r\nPulmonary infarction with acute pulmonary embolism\r\n",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545573,
"choiceText": "Pulmonary tuberculosis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545574,
"choiceText": "Influenza pneumonia with secondary bacterial pneumonia, complicated by myopericarditis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545575,
"choiceText": "Aspiration pneumonia with acute myocardial infarction",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 495853,
"questionText": "On the basis of these findings only, what is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Dyspnea, Fever, Hemoptysis, and Diabetes in a Tobacco User"
},
{
"authors": "Avnish Sandhu, DO; Pranatharthi Chandrasekar, MD",
"content": [
"Influenza viruses are generally known to infect the respiratory system and cause primary viral pneumonia. This patient presented during the winter with symptoms of fever, cough, sore throat, and diarrhea, along with hemoptysis and significant shortness of breath that required intubation.",
"Other possibilities include pulmonary hemorrhage with acute pulmonary embolism, pulmonary tuberculosis, and aspiration pneumonia with acute myocardial infarction. Pulmonary embolism with hemorrhage was excluded by the chest CT scan. Pulmonary tuberculosis was considered, given the right lower lobe consolidation; however, the patient had no risk factors for tuberculosis, such as recent travel or a history of incarceration, and no weight loss or night sweats. In addition, the acute onset of symptoms and the negative acid-fast bacilli smears militate against the diagnosis of tuberculosis. Aspiration pneumonia with acute myocardial infarction was excluded, as she had no risk factors for aspiration, such as loss of consciousness or altered mental status. An acute ischemic event was ruled out, given that her transthoracic echocardiogram showed no wall motion abnormality and her ECG revealed diffuse ST segment elevation with atrial fibrillation. These findings are not consistent with acute myocardial infarction.",
"Her respiratory viral panel PCR assay was positive for influenza A H3 subtype. A sputum culture with Gram staining was positive for methicillin-resistant Staphylococcus aureus, and a blood culture was positive for S aureus.",
"Because this patient has uncontrolled diabetes and COPD, she is at risk for complications from influenza. The following features of her illness fit the diagnostic criteria for influenza-associated myopericarditis[1]:",
"Positive clinical features, such as chest pain, shortness of breath, and tachyarrhythmia",
"An ECG showing diffuse ST segment elevation",
"An elevated cardiac enzyme (troponin I) level",
"A transthoracic echocardiogram showing a reduced ejection fraction with left ventricular wall thickness and pericardial effusion",
"A positive influenza A polymerase chain reaction test in the respiratory specimen",
"Influenza viruses are commonly known to cause secondary bacterial pneumonia,[2] but they may be associated with syndromes that affect other organ systems, such as the cardiovascular, central nervous system, renal, musculoskeletal, ocular, hematologic, hepatic, and endocrine systems.[3] Viral infections of the respiratory tract facilitate bacterial adherence by disrupting the epithelial lining; decrease mucociliary activity; and increase immunosuppression, which affects both innate and acquired immune responses, resulting in bacterial overgrowth.[2]",
"Streptococcus pneumoniae and S aureus are two common pathogens involved in secondary bacterial pneumonia following influenza virus infection.[2] In a retrospective and prospective cohort study conducted in 35 adult intensive care units among 683 critically ill patients with confirmed or probable 2009 influenza A (H1N1), Rice and colleagues[4] identified 207 patients with bacterial co-infection. Among these patients, cultures were positive for S aureus in 54 patients (26%) and for S pneumoniae in 19 (9.2%). Increased mortality was observed among those with S aureus co-infection."
],
"date": "December 02, 2020",
"figures": [],
"markdown": "# Dyspnea, Fever, Hemoptysis, and Diabetes in a Tobacco User\n\n **Authors:** Avnish Sandhu, DO; Pranatharthi Chandrasekar, MD \n **Date:** December 02, 2020\n\n ## Content\n\n Influenza viruses are generally known to infect the respiratory system and cause primary viral pneumonia. This patient presented during the winter with symptoms of fever, cough, sore throat, and diarrhea, along with hemoptysis and significant shortness of breath that required intubation.\nOther possibilities include pulmonary hemorrhage with acute pulmonary embolism, pulmonary tuberculosis, and aspiration pneumonia with acute myocardial infarction. Pulmonary embolism with hemorrhage was excluded by the chest CT scan. Pulmonary tuberculosis was considered, given the right lower lobe consolidation; however, the patient had no risk factors for tuberculosis, such as recent travel or a history of incarceration, and no weight loss or night sweats. In addition, the acute onset of symptoms and the negative acid-fast bacilli smears militate against the diagnosis of tuberculosis. Aspiration pneumonia with acute myocardial infarction was excluded, as she had no risk factors for aspiration, such as loss of consciousness or altered mental status. An acute ischemic event was ruled out, given that her transthoracic echocardiogram showed no wall motion abnormality and her ECG revealed diffuse ST segment elevation with atrial fibrillation. These findings are not consistent with acute myocardial infarction.\nHer respiratory viral panel PCR assay was positive for influenza A H3 subtype. A sputum culture with Gram staining was positive for methicillin-resistant Staphylococcus aureus, and a blood culture was positive for S aureus.\nBecause this patient has uncontrolled diabetes and COPD, she is at risk for complications from influenza. The following features of her illness fit the diagnostic criteria for influenza-associated myopericarditis[1]:\nPositive clinical features, such as chest pain, shortness of breath, and tachyarrhythmia\nAn ECG showing diffuse ST segment elevation\nAn elevated cardiac enzyme (troponin I) level\nA transthoracic echocardiogram showing a reduced ejection fraction with left ventricular wall thickness and pericardial effusion\nA positive influenza A polymerase chain reaction test in the respiratory specimen\nInfluenza viruses are commonly known to cause secondary bacterial pneumonia,[2] but they may be associated with syndromes that affect other organ systems, such as the cardiovascular, central nervous system, renal, musculoskeletal, ocular, hematologic, hepatic, and endocrine systems.[3] Viral infections of the respiratory tract facilitate bacterial adherence by disrupting the epithelial lining; decrease mucociliary activity; and increase immunosuppression, which affects both innate and acquired immune responses, resulting in bacterial overgrowth.[2]\nStreptococcus pneumoniae and S aureus are two common pathogens involved in secondary bacterial pneumonia following influenza virus infection.[2] In a retrospective and prospective cohort study conducted in 35 adult intensive care units among 683 critically ill patients with confirmed or probable 2009 influenza A (H1N1), Rice and colleagues[4] identified 207 patients with bacterial co-infection. Among these patients, cultures were positive for S aureus in 54 patients (26%) and for S pneumoniae in 19 (9.2%). Increased mortality was observed among those with S aureus co-infection.\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1545572,
"choiceText": "\r\nPulmonary infarction with acute pulmonary embolism\r\n",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545573,
"choiceText": "Pulmonary tuberculosis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545574,
"choiceText": "Influenza pneumonia with secondary bacterial pneumonia, complicated by myopericarditis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545575,
"choiceText": "Aspiration pneumonia with acute myocardial infarction",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 495853,
"questionText": "On the basis of these findings only, what is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Dyspnea, Fever, Hemoptysis, and Diabetes in a Tobacco User"
},
{
"authors": "Avnish Sandhu, DO; Pranatharthi Chandrasekar, MD",
"content": [
"Cardiovascular complications of influenza are often unrecognized. Common cardiovascular complications related to influenza virus infection include exacerbation of underlying heart disease, such as ischemic heart disease or heart failure.[3] An uncommon cardiovascular complication is myocarditis, with an incidence of approximately 11% and in-hospital mortality of 24%.[5,6] The inflammation can extend to the pericardium, leading to myopericarditis. During the H1N1 influenza pandemic in 2009, 58 cases of associated myocarditis were identified worldwide; of these cases, fulminant myocarditis occurred in 36 patients (62%).[6]",
"The diagnosis of myocarditis is based on clinical symptoms and diagnostic findings.[1] The clinical symptoms of myocarditis include chest pain, dyspnea, and syncope. These symptoms generally begin a few days after an influenzalike illness. The diagnostic findings in myocarditis/myopericarditis are:",
"Serologic tests that reveal elevated cardiac enzyme (troponin and creatine kinase-MB) levels without evidence of an acute ischemic event[1]",
"Transthoracic echocardiography or cardiovascular MRI that shows cardiac dysfunction, diffuse wall thickening, reduced ejection fraction, decreased wall motion, small cardiac chamber size, and pericardial effusion[1,7]",
"An abnormal ECG that shows diverse changes such as atrioventricular block, widened QRS complex, reduced R-wave height, abnormal Q wave, diffuse ST segment elevation, atrial fibrillation, supraventricular tachycardia, or ventricular fibrillation[1,8]",
"An endomyocardial biopsy that reveals cellular infiltration of mononuclear cells; cardiomyocyte rupture, fusion, and disappearance; and interstitial edema along with fibril formation (negative histopathologic examination results do not exclude the possibility of myocarditis, given the frequency of false-negative results)[1,9,10]",
"A PCR assay of a respiratory specimen that is positive for viral infection or a convalescent-phase viral antibody titer that is four times higher than the acute-phase titer[1]",
"The pathophysiology of influenza-associated myocarditis is not completely understood. Direct viral invasion of the endocardium and an exaggerated immune response caused by severe influenza virus infection, with increasing interleukin levels[1,8,10] and an elevated tumor necrosis factor-alpha level, can result in myocardial injury.[3,9,11]",
"The management of myocarditis depends on treating the underlying cause, such as viral infection, along with treating the cardiac dysfunction and maintaining hemodynamic stability.[1] Oseltamivir is an oral neuraminidase inhibitor approved for the treatment of influenza in patients who are symptomatic for 48 hours or less. However, treatment should be started in patients who are hospitalized with influenza regardless of the duration of symptoms.[12] Early treatment with a neuraminidase inhibitor is the standard of care based on an observational study, because it decreases symptom duration.[13,14] Patients with influenza-related fulminant myocarditis usually require arteriovenous extracorporeal membrane oxygenation, an intra-aortic balloon pump, or percutaneous cardiac devices.[1,5] Although myocarditis is a rare complication of influenza, it should be rapidly identified in patients infected with influenza virus, as often these patients can develop fulminant myocarditis that requires circulatory support. Prompt initiation of such support is key to these patients' recovery.[5]",
"Identifying patients who are at high risk for complications of influenza is imperative, and early initiation of empiric treatment, if influenza is suspected, is warranted in such patients.[10] The following persons are at high risk for complications[12]:",
"Children aged < 5 years and adults aged ≥ 65 years",
"Persons with chronic pulmonary disease (asthma), cardiovascular disease (excludes patients with a sole diagnosis of hypertension), chronic kidney disease, hematologic disease (eg, sickle cell disease), metabolic disorders (eg, diabetes mellitus), or chronic neurologic conditions (eg, stroke or epilepsy)",
"Persons with immunosuppression, including patients with HIV infection",
"Women who are pregnant or postpartum (within 2 weeks after delivery)",
"Persons with extreme obesity (body mass index of ≥ 40 kg/m2)",
"Patients in facilities (nursing homes, group homes)",
"Children and adolescents up to 18 years of age receiving aspirin- or salicylate-containing medication who are at risk for Reye syndrome after influenza virus infection"
],
"date": "December 02, 2020",
"figures": [],
"markdown": "# Dyspnea, Fever, Hemoptysis, and Diabetes in a Tobacco User\n\n **Authors:** Avnish Sandhu, DO; Pranatharthi Chandrasekar, MD \n **Date:** December 02, 2020\n\n ## Content\n\n Cardiovascular complications of influenza are often unrecognized. Common cardiovascular complications related to influenza virus infection include exacerbation of underlying heart disease, such as ischemic heart disease or heart failure.[3] An uncommon cardiovascular complication is myocarditis, with an incidence of approximately 11% and in-hospital mortality of 24%.[5,6] The inflammation can extend to the pericardium, leading to myopericarditis. During the H1N1 influenza pandemic in 2009, 58 cases of associated myocarditis were identified worldwide; of these cases, fulminant myocarditis occurred in 36 patients (62%).[6]\nThe diagnosis of myocarditis is based on clinical symptoms and diagnostic findings.[1] The clinical symptoms of myocarditis include chest pain, dyspnea, and syncope. These symptoms generally begin a few days after an influenzalike illness. The diagnostic findings in myocarditis/myopericarditis are:\nSerologic tests that reveal elevated cardiac enzyme (troponin and creatine kinase-MB) levels without evidence of an acute ischemic event[1]\nTransthoracic echocardiography or cardiovascular MRI that shows cardiac dysfunction, diffuse wall thickening, reduced ejection fraction, decreased wall motion, small cardiac chamber size, and pericardial effusion[1,7]\nAn abnormal ECG that shows diverse changes such as atrioventricular block, widened QRS complex, reduced R-wave height, abnormal Q wave, diffuse ST segment elevation, atrial fibrillation, supraventricular tachycardia, or ventricular fibrillation[1,8]\nAn endomyocardial biopsy that reveals cellular infiltration of mononuclear cells; cardiomyocyte rupture, fusion, and disappearance; and interstitial edema along with fibril formation (negative histopathologic examination results do not exclude the possibility of myocarditis, given the frequency of false-negative results)[1,9,10]\nA PCR assay of a respiratory specimen that is positive for viral infection or a convalescent-phase viral antibody titer that is four times higher than the acute-phase titer[1]\nThe pathophysiology of influenza-associated myocarditis is not completely understood. Direct viral invasion of the endocardium and an exaggerated immune response caused by severe influenza virus infection, with increasing interleukin levels[1,8,10] and an elevated tumor necrosis factor-alpha level, can result in myocardial injury.[3,9,11]\nThe management of myocarditis depends on treating the underlying cause, such as viral infection, along with treating the cardiac dysfunction and maintaining hemodynamic stability.[1] Oseltamivir is an oral neuraminidase inhibitor approved for the treatment of influenza in patients who are symptomatic for 48 hours or less. However, treatment should be started in patients who are hospitalized with influenza regardless of the duration of symptoms.[12] Early treatment with a neuraminidase inhibitor is the standard of care based on an observational study, because it decreases symptom duration.[13,14] Patients with influenza-related fulminant myocarditis usually require arteriovenous extracorporeal membrane oxygenation, an intra-aortic balloon pump, or percutaneous cardiac devices.[1,5] Although myocarditis is a rare complication of influenza, it should be rapidly identified in patients infected with influenza virus, as often these patients can develop fulminant myocarditis that requires circulatory support. Prompt initiation of such support is key to these patients' recovery.[5]\nIdentifying patients who are at high risk for complications of influenza is imperative, and early initiation of empiric treatment, if influenza is suspected, is warranted in such patients.[10] The following persons are at high risk for complications[12]:\nChildren aged < 5 years and adults aged ≥ 65 years\nPersons with chronic pulmonary disease (asthma), cardiovascular disease (excludes patients with a sole diagnosis of hypertension), chronic kidney disease, hematologic disease (eg, sickle cell disease), metabolic disorders (eg, diabetes mellitus), or chronic neurologic conditions (eg, stroke or epilepsy)\nPersons with immunosuppression, including patients with HIV infection\nWomen who are pregnant or postpartum (within 2 weeks after delivery)\nPersons with extreme obesity (body mass index of ≥ 40 kg/m2)\nPatients in facilities (nursing homes, group homes)\nChildren and adolescents up to 18 years of age receiving aspirin- or salicylate-containing medication who are at risk for Reye syndrome after influenza virus infection\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Dyspnea, Fever, Hemoptysis, and Diabetes in a Tobacco User"
},
{
"authors": "Avnish Sandhu, DO; Pranatharthi Chandrasekar, MD",
"content": [
"The influenza vaccine is approved for all persons aged ≥ 6 months and should be given yearly during each influenza season.[15] The composition of the influenza virus changes annually; hence, the vaccine is modified each year to best match the circulating viruses. For the 2020-2021 season, the options are a quadrivalent vaccine that protects against four strains of influenza virus (A/Guangdong-Maonan/SWL1536/2019H1N1 pdm 09, A/Hong Kong/2671/2019 [H3N2]) and two B viruses (B/Washington/02/209 [Victoria] and B/Phuket/3073/2013-like [Yamagata lineage]); and a trivalent vaccine that protects against three strains of influenza virus (A/Guangdon-Maonan/SWL1536/2019 [H1N1 pdm 09], A/Hong Kong/2671/2019 [H3N2]) and B virus (B/Washington/02/209 [Victoria lineage]). The Centers for Disease Control and Prevention (CDC) recommends any licensed, age-appropriate influenza vaccine for all persons. The high-dose vaccine, which contains four times the quantity of antigen, is reserved for adults age 65 years or older.[16]",
"Considering COVID-19 in patients who present with influenzalike illness is vital, because symptoms of influenza often overlap with those of COVID-19. Both illnesses can present with fever, cough, sore throat, muscle ache, headache, diarrhea, and shortness of breath. COVID-19 has a longer incubation period than that of influenza (1-14 days vs 1-4 days).[17] The secondary complications of both diseases are similar.[18,19] Of note, COVID-19 and influenza A can occur together.[20]",
"The patient in this case completed a 5-day course of oseltamivir, was extubated on day 5 of her admission, and was discharged a few days later to complete a 2-week course of intravenous vancomycin for uncomplicated methicillin-resistant S aureus bacteremia and pneumonia. She did not require any cardiac intervention or circulatory support for myopericarditis."
],
"date": "December 02, 2020",
"figures": [],
"markdown": "# Dyspnea, Fever, Hemoptysis, and Diabetes in a Tobacco User\n\n **Authors:** Avnish Sandhu, DO; Pranatharthi Chandrasekar, MD \n **Date:** December 02, 2020\n\n ## Content\n\n The influenza vaccine is approved for all persons aged ≥ 6 months and should be given yearly during each influenza season.[15] The composition of the influenza virus changes annually; hence, the vaccine is modified each year to best match the circulating viruses. For the 2020-2021 season, the options are a quadrivalent vaccine that protects against four strains of influenza virus (A/Guangdong-Maonan/SWL1536/2019H1N1 pdm 09, A/Hong Kong/2671/2019 [H3N2]) and two B viruses (B/Washington/02/209 [Victoria] and B/Phuket/3073/2013-like [Yamagata lineage]); and a trivalent vaccine that protects against three strains of influenza virus (A/Guangdon-Maonan/SWL1536/2019 [H1N1 pdm 09], A/Hong Kong/2671/2019 [H3N2]) and B virus (B/Washington/02/209 [Victoria lineage]). The Centers for Disease Control and Prevention (CDC) recommends any licensed, age-appropriate influenza vaccine for all persons. The high-dose vaccine, which contains four times the quantity of antigen, is reserved for adults age 65 years or older.[16]\nConsidering COVID-19 in patients who present with influenzalike illness is vital, because symptoms of influenza often overlap with those of COVID-19. Both illnesses can present with fever, cough, sore throat, muscle ache, headache, diarrhea, and shortness of breath. COVID-19 has a longer incubation period than that of influenza (1-14 days vs 1-4 days).[17] The secondary complications of both diseases are similar.[18,19] Of note, COVID-19 and influenza A can occur together.[20]\nThe patient in this case completed a 5-day course of oseltamivir, was extubated on day 5 of her admission, and was discharged a few days later to complete a 2-week course of intravenous vancomycin for uncomplicated methicillin-resistant S aureus bacteremia and pneumonia. She did not require any cardiac intervention or circulatory support for myopericarditis.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1545576,
"choiceText": "Positive endomyocardial biopsy",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545577,
"choiceText": "Clinical features of chest pain, dyspnea, and arrhythmia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545578,
"choiceText": "ECG findings consistent with diffuse ST segment elevation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545579,
"choiceText": "Elevated cardiac enzyme level",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "A positive endomyocardial biopsy helps to confirm the diagnosis of myocarditis and is part of the diagnostic criteria. However, negative biopsy results do not exclude the diagnosis of myocarditis, given that false-negative results are common. Influenza virus replication in cardiac tissue is not well recognized in humans and in animal models of influenza-associated myocarditis<sup>[5,9,10]</sup>; therefore, biopsy is not required for the diagnosis of myocarditis. The other choices (elevated cardiac enzyme levels, clinical features, and ECG changes) are part of the diagnostic criteria for myocarditis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 495854,
"questionText": "Of the following diagnostic criteria, which is <i>least important</i> for a diagnosis of myocarditis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1545580,
"choiceText": "A 50-year-old with isolated hypertension",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545581,
"choiceText": "A 35-year-old with diabetes mellitus",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545582,
"choiceText": "A 25-year-old with no significant medical history",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545583,
"choiceText": "A 45-year-old with recurrent sinusitis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Recognizing patients who are at risk for complications from influenza is important. Of the choices listed above, patients with diabetes are at the highest risk for complications from influenza. Although cardiovascular disease increases the risk for influenza complications, hypertension alone is not a risk factor. Early empiric treatment is appropriate in high-risk patients who are suspected of having influenza.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 495855,
"questionText": "Of the following patients, which has the highest risk for complications from influenza? ",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Dyspnea, Fever, Hemoptysis, and Diabetes in a Tobacco User"
},
{
"authors": "Avnish Sandhu, DO; Pranatharthi Chandrasekar, MD",
"content": [],
"date": "December 02, 2020",
"figures": [],
"markdown": "# Dyspnea, Fever, Hemoptysis, and Diabetes in a Tobacco User\n\n **Authors:** Avnish Sandhu, DO; Pranatharthi Chandrasekar, MD \n **Date:** December 02, 2020\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1545576,
"choiceText": "Positive endomyocardial biopsy",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545577,
"choiceText": "Clinical features of chest pain, dyspnea, and arrhythmia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545578,
"choiceText": "ECG findings consistent with diffuse ST segment elevation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545579,
"choiceText": "Elevated cardiac enzyme level",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "A positive endomyocardial biopsy helps to confirm the diagnosis of myocarditis and is part of the diagnostic criteria. However, negative biopsy results do not exclude the diagnosis of myocarditis, given that false-negative results are common. Influenza virus replication in cardiac tissue is not well recognized in humans and in animal models of influenza-associated myocarditis<sup>[5,9,10]</sup>; therefore, biopsy is not required for the diagnosis of myocarditis. The other choices (elevated cardiac enzyme levels, clinical features, and ECG changes) are part of the diagnostic criteria for myocarditis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 495854,
"questionText": "Of the following diagnostic criteria, which is <i>least important</i> for a diagnosis of myocarditis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1545580,
"choiceText": "A 50-year-old with isolated hypertension",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545581,
"choiceText": "A 35-year-old with diabetes mellitus",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545582,
"choiceText": "A 25-year-old with no significant medical history",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545583,
"choiceText": "A 45-year-old with recurrent sinusitis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Recognizing patients who are at risk for complications from influenza is important. Of the choices listed above, patients with diabetes are at the highest risk for complications from influenza. Although cardiovascular disease increases the risk for influenza complications, hypertension alone is not a risk factor. Early empiric treatment is appropriate in high-risk patients who are suspected of having influenza.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 495855,
"questionText": "Of the following patients, which has the highest risk for complications from influenza? ",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Dyspnea, Fever, Hemoptysis, and Diabetes in a Tobacco User"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1545572,
"choiceText": "\r\nPulmonary infarction with acute pulmonary embolism\r\n",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545573,
"choiceText": "Pulmonary tuberculosis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545574,
"choiceText": "Influenza pneumonia with secondary bacterial pneumonia, complicated by myopericarditis",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545575,
"choiceText": "Aspiration pneumonia with acute myocardial infarction",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 495853,
"questionText": "On the basis of these findings only, what is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1545576,
"choiceText": "Positive endomyocardial biopsy",
"correct": true,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545577,
"choiceText": "Clinical features of chest pain, dyspnea, and arrhythmia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545578,
"choiceText": "ECG findings consistent with diffuse ST segment elevation",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545579,
"choiceText": "Elevated cardiac enzyme level",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "A positive endomyocardial biopsy helps to confirm the diagnosis of myocarditis and is part of the diagnostic criteria. However, negative biopsy results do not exclude the diagnosis of myocarditis, given that false-negative results are common. Influenza virus replication in cardiac tissue is not well recognized in humans and in animal models of influenza-associated myocarditis<sup>[5,9,10]</sup>; therefore, biopsy is not required for the diagnosis of myocarditis. The other choices (elevated cardiac enzyme levels, clinical features, and ECG changes) are part of the diagnostic criteria for myocarditis.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 495854,
"questionText": "Of the following diagnostic criteria, which is <i>least important</i> for a diagnosis of myocarditis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1545580,
"choiceText": "A 50-year-old with isolated hypertension",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545581,
"choiceText": "A 35-year-old with diabetes mellitus",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545582,
"choiceText": "A 25-year-old with no significant medical history",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1545583,
"choiceText": "A 45-year-old with recurrent sinusitis",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Recognizing patients who are at risk for complications from influenza is important. Of the choices listed above, patients with diabetes are at the highest risk for complications from influenza. Although cardiovascular disease increases the risk for influenza complications, hypertension alone is not a risk factor. Early empiric treatment is appropriate in high-risk patients who are suspected of having influenza.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 495855,
"questionText": "Of the following patients, which has the highest risk for complications from influenza? ",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
939915 | /viewarticle/939915 | [
{
"authors": "Joshua J. Solano, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians, but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please email us at [email protected] with the subject line \"Case Challenge Suggestion.\" We look forward to hearing from you.",
"An 83-year-old man was found on the bathroom floor of his apartment after he had fallen about 24 hours earlier. He reports that he had been short of breath on the day of his fall. He went to the bathroom to urinate, felt dizzy, and then \"blacked out.\" After he struck his head on the edge of the bathtub, he was unable to get up owing to weakness. He remained on his right side, wedged between the toilet and the bathtub.",
"His daughter, who usually calls him daily, says that she went to his house because he had not answered the phone. She found him on the bathroom floor and called 911. Emergency medical services (EMS) providers brought him to the emergency department (ED).",
"The EMS providers report that his initial vital signs were an oxygen saturation of 85% on room air, a respiration rate of 28 breaths/min, a blood pressure of 185/120 mm Hg, and a heart rate of 124 beats/min. His blood glucose level was 435 mg/dL. The EMS providers found no blood at the scene.",
"The patient has moderate dyspnea and a headache. He denies any pain in his chest, neck, back, or extremities. He does report feeling very achy and weak. He denies any dysuria. He has missed all his medications over the past 24 hours.",
"His medical history includes coronary artery disease with the placement of two stents, congestive heart failure with an ejection fraction of 35%, atrial fibrillation, insulin-dependent diabetes mellitus, obesity, stage 3 chronic kidney disease, neuropathy, and hyperlipidemia. He had an appendectomy in the remote past. He has no advance directives.",
"His medications include carvedilol (25 mg twice daily), furosemide (40 mg twice daily), lisinopril (40 mg once daily), insulin glargine (20 units once daily), aspirin (324 mg once daily), warfarin (2.5 mg once daily), and simvastatin (20 mg once daily). He takes fish oil as a supplement.",
"The patient lives alone and is able to complete all activities of daily living. He denies smoking, drinking, or using illicit drugs."
],
"date": "October 31, 2024",
"figures": [],
"markdown": "# An Elderly Man Blacks Out in His Bathroom\n\n **Authors:** Joshua J. Solano, MD \n **Date:** October 31, 2024\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians, but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please email us at [email protected] with the subject line \"Case Challenge Suggestion.\" We look forward to hearing from you.\nAn 83-year-old man was found on the bathroom floor of his apartment after he had fallen about 24 hours earlier. He reports that he had been short of breath on the day of his fall. He went to the bathroom to urinate, felt dizzy, and then \"blacked out.\" After he struck his head on the edge of the bathtub, he was unable to get up owing to weakness. He remained on his right side, wedged between the toilet and the bathtub.\nHis daughter, who usually calls him daily, says that she went to his house because he had not answered the phone. She found him on the bathroom floor and called 911. Emergency medical services (EMS) providers brought him to the emergency department (ED).\nThe EMS providers report that his initial vital signs were an oxygen saturation of 85% on room air, a respiration rate of 28 breaths/min, a blood pressure of 185/120 mm Hg, and a heart rate of 124 beats/min. His blood glucose level was 435 mg/dL. The EMS providers found no blood at the scene.\nThe patient has moderate dyspnea and a headache. He denies any pain in his chest, neck, back, or extremities. He does report feeling very achy and weak. He denies any dysuria. He has missed all his medications over the past 24 hours.\nHis medical history includes coronary artery disease with the placement of two stents, congestive heart failure with an ejection fraction of 35%, atrial fibrillation, insulin-dependent diabetes mellitus, obesity, stage 3 chronic kidney disease, neuropathy, and hyperlipidemia. He had an appendectomy in the remote past. He has no advance directives.\nHis medications include carvedilol (25 mg twice daily), furosemide (40 mg twice daily), lisinopril (40 mg once daily), insulin glargine (20 units once daily), aspirin (324 mg once daily), warfarin (2.5 mg once daily), and simvastatin (20 mg once daily). He takes fish oil as a supplement.\nThe patient lives alone and is able to complete all activities of daily living. He denies smoking, drinking, or using illicit drugs.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "An Elderly Man Blacks Out in His Bathroom"
},
{
"authors": "Joshua J. Solano, MD",
"content": [
"Initial vital signs in the ED are as follows:",
"Temperature: 95.7°F (35.4°C)",
"Heart rate: 125 beats/min",
"Respiration rate: 22 breaths/min",
"Blood pressure, 175/120 mm Hg",
"Pulse oximetry reveals an oxygen saturation of 90% on 2 L/min of oxygen by nasal cannula. The patient's weight is 231.5 lb (105 kg), height is 5 ft 9 in (175 cm), and body mass index is 34.3 kg/m2.",
"The patient is awake and able to converse but is in mild respiratory distress and appears uncomfortable. He has a nonbleeding abrasion to the right side of the head and an underlying 2 × 2 cm hematoma. His mucous membranes are dry. Mild jugular venous distension is noted.",
"The cervical spine is nontender, but mild paraspinal tenderness is noted upon palpation. The patient has a regular pulse and no murmurs. In both lower extremities, 2+ pitted edema is noted. Bilateral crackles are audible throughout the lung fields. No abdominal tenderness, distension, or masses are detected. Several bullae are noted on the right side of the torso and right upper extremity. The patient has full range of motion of the extremities without pain, pulses are 2+ throughout, and sensation to light touch is diminished in a stocking and glove distribution at the level of the forearms and at the ankles.",
"All compartments are soft. No midline tenderness of the thoracic or lumbar spine is observed, but tenderness is noted along the right lateral thoracic and lumbar regions. The neurologic examination shows that the patient is alert and oriented × 4, cranial nerves II-XII are intact, and upper and lower extremity strength is 5/5.",
"A complete blood cell count shows normal values.",
"A comprehensive metabolic panel reveals the following abnormal values:",
"Potassium: 5.5 mEq/L (reference range, 3.7-5.2 mEq/L)",
"Carbon dioxide: 18 mEq/L (reference range, 23-29 mEq/L)",
"Blood urea nitrogen: 80 mg/dL (reference range, 8-24 mg/dL)",
"Creatinine: 3.5 mg/dL (reference range, 0.9-1.3 mg/dL)",
"Glucose: 465 mg/dL (reference range, < 160 mg/dL)",
"Aspartate aminotransferase: 80 IU/L (reference range, 6-34 IU/L)",
"Alanine aminotransferase: 75 IU/L (reference range, 20-60 IU/L)",
"His brain natriuretic peptide (BNP) level is 850 pg/mL (reference range, < 450 pg/mL). His troponin level and international normalized ratio (INR) are within reference ranges. His prothrombin time is 25 seconds (reference range, 11-12.5 s [>1.5-2 times control value for those receiving anticoagulant therapy]). His partial thromboplastin time is 29 seconds (reference range, 60-70 s [1.5-2.5 times control for those receiving anticoagulant therapy]). His creatine phosphokinase (CPK) level is 4500 IU/L (reference range, 55-170 units/L).",
"The urine is amber and appears hazy. Urinalysis reveals the following abnormalities:",
"Specific gravity: 1.040 (reference range, 1.002-1.030)",
"Blood: 3+",
"Protein: 3+",
"Glucose level: > 1000 mg/d (reference range, 0-15 mg/dL)",
"The urinalysis also revealed a trace level of ketones and no red blood cells, WBCs, bacteria, or epithelial cells.",
"An electrocardiogram (ECG) is obtained (Figure 1).",
"Figure 1.",
"Non-contrast CT scans of the head (Figures 2-4) and neck (Figure 5) are performed.",
"Figure 2.",
"Figure 3.",
"Figure 4.",
"Figure 5.",
"A point-of-care ultrasound examination of the lungs is performed (Figure 6).",
"Figure 6.",
"Point-of-care echocardiography is performed (Figures 7 and 8).",
"Figure 7.",
"Figure 8.",
"A chest radiograph is obtained (Figure 9).",
"Figure 9."
],
"date": "October 31, 2024",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/939/915/Figure 1 - Copy.jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/939/915/Figure 2 - Copy.jpg"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/939/915/Figure 3 - Copy.jpg"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/939/915/Figure 4 - Copy.jpg"
},
{
"caption": "Figure 5.",
"image_url": "https://img.medscapestatic.com/article/939/915/Figure 5 - Copy.jpg"
},
{
"caption": "Figure 6.",
"image_url": "https://img.medscapestatic.com/article/939/915/Figure 6 - Copy.gif"
},
{
"caption": "Figure 7.",
"image_url": "https://img.medscapestatic.com/article/939/915/Figure 7 - Copy.gif"
},
{
"caption": "Figure 8.",
"image_url": "https://img.medscapestatic.com/article/939/915/Figure 8 - Copy_(1).gif"
},
{
"caption": "Figure 9.",
"image_url": "https://img.medscapestatic.com/article/939/915/Figure 9 - Copy.jpg"
}
],
"markdown": "# An Elderly Man Blacks Out in His Bathroom\n\n **Authors:** Joshua J. Solano, MD \n **Date:** October 31, 2024\n\n ## Content\n\n Initial vital signs in the ED are as follows:\nTemperature: 95.7°F (35.4°C)\nHeart rate: 125 beats/min\nRespiration rate: 22 breaths/min\nBlood pressure, 175/120 mm Hg\nPulse oximetry reveals an oxygen saturation of 90% on 2 L/min of oxygen by nasal cannula. The patient's weight is 231.5 lb (105 kg), height is 5 ft 9 in (175 cm), and body mass index is 34.3 kg/m2.\nThe patient is awake and able to converse but is in mild respiratory distress and appears uncomfortable. He has a nonbleeding abrasion to the right side of the head and an underlying 2 × 2 cm hematoma. His mucous membranes are dry. Mild jugular venous distension is noted.\nThe cervical spine is nontender, but mild paraspinal tenderness is noted upon palpation. The patient has a regular pulse and no murmurs. In both lower extremities, 2+ pitted edema is noted. Bilateral crackles are audible throughout the lung fields. No abdominal tenderness, distension, or masses are detected. Several bullae are noted on the right side of the torso and right upper extremity. The patient has full range of motion of the extremities without pain, pulses are 2+ throughout, and sensation to light touch is diminished in a stocking and glove distribution at the level of the forearms and at the ankles.\nAll compartments are soft. No midline tenderness of the thoracic or lumbar spine is observed, but tenderness is noted along the right lateral thoracic and lumbar regions. The neurologic examination shows that the patient is alert and oriented × 4, cranial nerves II-XII are intact, and upper and lower extremity strength is 5/5.\nA complete blood cell count shows normal values.\nA comprehensive metabolic panel reveals the following abnormal values:\nPotassium: 5.5 mEq/L (reference range, 3.7-5.2 mEq/L)\nCarbon dioxide: 18 mEq/L (reference range, 23-29 mEq/L)\nBlood urea nitrogen: 80 mg/dL (reference range, 8-24 mg/dL)\nCreatinine: 3.5 mg/dL (reference range, 0.9-1.3 mg/dL)\nGlucose: 465 mg/dL (reference range, < 160 mg/dL)\nAspartate aminotransferase: 80 IU/L (reference range, 6-34 IU/L)\nAlanine aminotransferase: 75 IU/L (reference range, 20-60 IU/L)\nHis brain natriuretic peptide (BNP) level is 850 pg/mL (reference range, < 450 pg/mL). His troponin level and international normalized ratio (INR) are within reference ranges. His prothrombin time is 25 seconds (reference range, 11-12.5 s [>1.5-2 times control value for those receiving anticoagulant therapy]). His partial thromboplastin time is 29 seconds (reference range, 60-70 s [1.5-2.5 times control for those receiving anticoagulant therapy]). His creatine phosphokinase (CPK) level is 4500 IU/L (reference range, 55-170 units/L).\nThe urine is amber and appears hazy. Urinalysis reveals the following abnormalities:\nSpecific gravity: 1.040 (reference range, 1.002-1.030)\nBlood: 3+\nProtein: 3+\nGlucose level: > 1000 mg/d (reference range, 0-15 mg/dL)\nThe urinalysis also revealed a trace level of ketones and no red blood cells, WBCs, bacteria, or epithelial cells.\nAn electrocardiogram (ECG) is obtained (Figure 1).\nFigure 1.\nNon-contrast CT scans of the head (Figures 2-4) and neck (Figure 5) are performed.\nFigure 2.\nFigure 3.\nFigure 4.\nFigure 5.\nA point-of-care ultrasound examination of the lungs is performed (Figure 6).\nFigure 6.\nPoint-of-care echocardiography is performed (Figures 7 and 8).\nFigure 7.\nFigure 8.\nA chest radiograph is obtained (Figure 9).\nFigure 9.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4.** \n \n\n**Figure 5.** \n \n\n**Figure 6.** \n \n\n**Figure 7.** \n \n\n**Figure 8.** \n.gif) \n\n**Figure 9.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1536910,
"choiceText": "Angioedema",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536911,
"choiceText": "Pneumonia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536912,
"choiceText": "Congestive heart failure exacerbation",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536913,
"choiceText": "Pulmonary embolism",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 492807,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "An Elderly Man Blacks Out in His Bathroom"
},
{
"authors": "Joshua J. Solano, MD",
"content": [
"Respiratory distress is common in the ED, especially among older adults, and accounts for 4 million visits each year in the United States.[1] Rapid treatment of acute dyspnea in the ED relies on an organized evaluation that starts with airway, breathing, and circulation. At the same time, pertinent information is gathered and therapeutic interventions are applied. Dyspnea can be categorized based on the oxygen level of the patient.",
"This patient presents with dyspnea and significant hypoxia after he had been on the floor for approximately 24 hours. The differential diagnosis for acute dyspnea with hypoxia in adults is broad. It most commonly includes viral or bacterial pneumonia, pulmonary embolism, pulmonary edema, acute respiratory distress syndrome, asthma exacerbation, congestive heart failure exacerbation, and chronic obstructive pulmonary disease (COPD) exacerbation. Other less common but important considerations include pneumothorax, pleural effusion, foreign body aspiration, anaphylaxis, angioedema, neurologic disorders, and epiglottitis.",
"Causes of acute dyspnea without hypoxia include pericardial effusion, metabolic acidosis from multiple etiologies (eg, rhabdomyolysis, diabetic ketoacidosis, aspirin toxicity, sepsis), severe anemia, neurologic conditions, panic attacks, vocal cord paralysis, and acute myocardial infarction. Chronic dyspnea with hypoxia can result from tumors or malignancy, COPD, bronchiectasis, tuberculosis, idiopathic pulmonary fibrosis, and pulmonary arterial hypertension.",
"Limited medical history can complicate the assessment of acute dyspnea in the ED.",
"In general, the workup includes a chest radiograph, a complete blood cell count, a basic metabolic panel, an ECG, and other tests depending on the circumstances, such as CT angiography of the chest, ventilation-perfusion scanning, arterial blood gas measurement, ultrasonography, measurement of troponin levels, and measurement of BNP and N-terminal pro b-type natriuretic peptide (NT-proBNP) levels.",
"Ultrasonography has become a helpful test in the care of patients with acute dyspnea owing to its ability to rapidly detect life-threatening conditions.[2,3,4] The evaluation of the heart and lungs is key. This patient's echocardiogram reveals a significantly reduced ejection fraction without pericardial effusion (see Figures 7 and 8).",
"Figure 7.",
"Figure 8."
],
"date": "October 31, 2024",
"figures": [
{
"caption": "Figure 7.",
"image_url": "https://img.medscapestatic.com/article/939/915/Figure 7 - Copy.gif"
},
{
"caption": "Figure 8.",
"image_url": "https://img.medscapestatic.com/article/939/915/Figure 8 - Copy_(1).gif"
}
],
"markdown": "# An Elderly Man Blacks Out in His Bathroom\n\n **Authors:** Joshua J. Solano, MD \n **Date:** October 31, 2024\n\n ## Content\n\n Respiratory distress is common in the ED, especially among older adults, and accounts for 4 million visits each year in the United States.[1] Rapid treatment of acute dyspnea in the ED relies on an organized evaluation that starts with airway, breathing, and circulation. At the same time, pertinent information is gathered and therapeutic interventions are applied. Dyspnea can be categorized based on the oxygen level of the patient.\nThis patient presents with dyspnea and significant hypoxia after he had been on the floor for approximately 24 hours. The differential diagnosis for acute dyspnea with hypoxia in adults is broad. It most commonly includes viral or bacterial pneumonia, pulmonary embolism, pulmonary edema, acute respiratory distress syndrome, asthma exacerbation, congestive heart failure exacerbation, and chronic obstructive pulmonary disease (COPD) exacerbation. Other less common but important considerations include pneumothorax, pleural effusion, foreign body aspiration, anaphylaxis, angioedema, neurologic disorders, and epiglottitis.\nCauses of acute dyspnea without hypoxia include pericardial effusion, metabolic acidosis from multiple etiologies (eg, rhabdomyolysis, diabetic ketoacidosis, aspirin toxicity, sepsis), severe anemia, neurologic conditions, panic attacks, vocal cord paralysis, and acute myocardial infarction. Chronic dyspnea with hypoxia can result from tumors or malignancy, COPD, bronchiectasis, tuberculosis, idiopathic pulmonary fibrosis, and pulmonary arterial hypertension.\nLimited medical history can complicate the assessment of acute dyspnea in the ED.\nIn general, the workup includes a chest radiograph, a complete blood cell count, a basic metabolic panel, an ECG, and other tests depending on the circumstances, such as CT angiography of the chest, ventilation-perfusion scanning, arterial blood gas measurement, ultrasonography, measurement of troponin levels, and measurement of BNP and N-terminal pro b-type natriuretic peptide (NT-proBNP) levels.\nUltrasonography has become a helpful test in the care of patients with acute dyspnea owing to its ability to rapidly detect life-threatening conditions.[2,3,4] The evaluation of the heart and lungs is key. This patient's echocardiogram reveals a significantly reduced ejection fraction without pericardial effusion (see Figures 7 and 8).\nFigure 7.\nFigure 8.\n\n ## Figures\n\n **Figure 7.** \n \n\n**Figure 8.** \n.gif) \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1536910,
"choiceText": "Angioedema",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536911,
"choiceText": "Pneumonia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536912,
"choiceText": "Congestive heart failure exacerbation",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536913,
"choiceText": "Pulmonary embolism",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 492807,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "An Elderly Man Blacks Out in His Bathroom"
},
{
"authors": "Joshua J. Solano, MD",
"content": [
"The Bedside Lung Ultrasonography in Emergency (BLUE) protocol is useful for patients with undifferentiated disorders.[5] It involves multiple assessments of the lungs for lung sliding, A lines, B lines, consolidations, and effusions, as well as deep venous thrombosis. The lung sliding seen in Figure 10 signifies that the visceral and parietal pleura of the lung are moving against each other, and no air is observed in the potential space; thus, a pneumothorax is ruled out at that site. A lines are a form of reverberation artifact that appear as horizontal lines parallel to the pleural lines; this finding signifies that the lung is aerated without fluid or consolidation (Figure 11). B lines are a form of artifact that spread from the pleural line and propagate to the end of the frame at least 12 cm down on the sonogram and represent the presence of fluid in alveoli (see Figure 6). Consolidations and effusions appear as areas of anechoic fluid collection.",
"Figure 10.",
"Figure 11.",
"Figure 6.",
"In this patient, several important history points, physical examination findings, and data help narrow the differential diagnosis and allow for the implementation of treatment. He is notably hypoxic, requires oxygen, and denies any history of pertinent pulmonary disorders. These findings tend to exclude the causes of chronic dyspnea. The lack of a smoking history reduces the likelihood of COPD. The absence of a fever, cough, defined infiltrate on the chest radiograph, leukocytosis, and lactic acidosis makes viral or bacterial pneumonia less likely.",
"The patient has a history of atrial fibrillation and is taking warfarin. His INR is in the therapeutic range, which makes pulmonary embolism much less likely. If he had a history of noncompliance and subtherapeutic INRs, pulmonary embolism would be more of a consideration. In addition, the patient's abnormal chest radiograph, significant bilateral pitting edema, and lung crackles reduce the likelihood of pulmonary embolism. The absence of stridor, wheezing, and urticaria tends to exclude angioedema, asthma exacerbation, and anaphylaxis. The lack of reported upper airway or lower facial or neck trauma makes a foreign body (from an aspirated tooth, for instance), tracheal injury, or obstruction from aspirated blood much less likely. The presence of jugular venous distension points to such causes as pericardial effusion (less likely owing to the degree of hypoxia), tension pneumothorax (unlikely because of bilateral breath sounds and ruled out on the chest radiograph), and congestive heart failure.",
"This patient has a history of congestive heart failure with pitting edema on examination, crackles in the lung fields, a chest radiograph with pulmonary edema, a point-of-care lung sonogram with B lines, and a point-of-care echocardiogram with a reduced ejection fraction.[6,7]"
],
"date": "October 31, 2024",
"figures": [
{
"caption": "Figure 10.",
"image_url": "https://img.medscapestatic.com/article/939/915/Figure 10 - Copy.gif"
},
{
"caption": "Figure 11.",
"image_url": "https://img.medscapestatic.com/article/939/915/Figure 11 - Copy.gif"
},
{
"caption": "Figure 6.",
"image_url": "https://img.medscapestatic.com/article/939/915/Figure 6 - Copy.gif"
}
],
"markdown": "# An Elderly Man Blacks Out in His Bathroom\n\n **Authors:** Joshua J. Solano, MD \n **Date:** October 31, 2024\n\n ## Content\n\n The Bedside Lung Ultrasonography in Emergency (BLUE) protocol is useful for patients with undifferentiated disorders.[5] It involves multiple assessments of the lungs for lung sliding, A lines, B lines, consolidations, and effusions, as well as deep venous thrombosis. The lung sliding seen in Figure 10 signifies that the visceral and parietal pleura of the lung are moving against each other, and no air is observed in the potential space; thus, a pneumothorax is ruled out at that site. A lines are a form of reverberation artifact that appear as horizontal lines parallel to the pleural lines; this finding signifies that the lung is aerated without fluid or consolidation (Figure 11). B lines are a form of artifact that spread from the pleural line and propagate to the end of the frame at least 12 cm down on the sonogram and represent the presence of fluid in alveoli (see Figure 6). Consolidations and effusions appear as areas of anechoic fluid collection.\nFigure 10.\nFigure 11.\nFigure 6.\nIn this patient, several important history points, physical examination findings, and data help narrow the differential diagnosis and allow for the implementation of treatment. He is notably hypoxic, requires oxygen, and denies any history of pertinent pulmonary disorders. These findings tend to exclude the causes of chronic dyspnea. The lack of a smoking history reduces the likelihood of COPD. The absence of a fever, cough, defined infiltrate on the chest radiograph, leukocytosis, and lactic acidosis makes viral or bacterial pneumonia less likely.\nThe patient has a history of atrial fibrillation and is taking warfarin. His INR is in the therapeutic range, which makes pulmonary embolism much less likely. If he had a history of noncompliance and subtherapeutic INRs, pulmonary embolism would be more of a consideration. In addition, the patient's abnormal chest radiograph, significant bilateral pitting edema, and lung crackles reduce the likelihood of pulmonary embolism. The absence of stridor, wheezing, and urticaria tends to exclude angioedema, asthma exacerbation, and anaphylaxis. The lack of reported upper airway or lower facial or neck trauma makes a foreign body (from an aspirated tooth, for instance), tracheal injury, or obstruction from aspirated blood much less likely. The presence of jugular venous distension points to such causes as pericardial effusion (less likely owing to the degree of hypoxia), tension pneumothorax (unlikely because of bilateral breath sounds and ruled out on the chest radiograph), and congestive heart failure.\nThis patient has a history of congestive heart failure with pitting edema on examination, crackles in the lung fields, a chest radiograph with pulmonary edema, a point-of-care lung sonogram with B lines, and a point-of-care echocardiogram with a reduced ejection fraction.[6,7]\n\n ## Figures\n\n **Figure 10.** \n \n\n**Figure 11.** \n \n\n**Figure 6.** \n \n\n\n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "An Elderly Man Blacks Out in His Bathroom"
},
{
"authors": "Joshua J. Solano, MD",
"content": [
"The patient's treatment must be tailored to the underlying cause of the dyspnea. For example, attempting to treat a tension pneumothorax with intubation would result in cardiac arrest. In this case, the treatment of acute pulmonary edema from congestive heart failure exacerbation required bilevel positive airway pressure (BiPAP) with supplemental oxygen, nitrates, and a diuretic. This patient had a complicating factor: rhabdomyolysis, as evidenced by his elevated CPK level, blood in the urine, and myalgia. The rhabdomyolysis probably results from his being on the floor for a prolonged period. In such patients, all compartments should be checked to make sure that the cause of the rhabdomyolysis is not a compartment syndrome.",
"In addition, this patient has sustained a traumatic head injury and is receiving anticoagulation therapy with warfarin. Thus, a non-contrast head CT scan is required to rule out intracranial bleeding owing to the patient's advanced age, head trauma, and long-term use of anticoagulants and antiplatelet agents. A non-contrast cervical spine CT scan was also performed because of the patient's age and head trauma.",
"Currently, no clinical decision rule can effectively rule out cervical fracture in older adults, even in the absence of pain and tenderness. The rest of the physical examination results are reassuring for a lack of other traumatic injuries, which are common in older patients after a ground-level fall.",
"After the workup, the patient was treated with intravenous (IV) nitroglycerin and BiPAP. His condition improved initially, and he was admitted to the intensive care unit. However, his hospital course was complicated by worsening renal failure and fluid overload. After a discussion of the goals of care, the patient was transferred to hospice care and died."
],
"date": "October 31, 2024",
"figures": [],
"markdown": "# An Elderly Man Blacks Out in His Bathroom\n\n **Authors:** Joshua J. Solano, MD \n **Date:** October 31, 2024\n\n ## Content\n\n The patient's treatment must be tailored to the underlying cause of the dyspnea. For example, attempting to treat a tension pneumothorax with intubation would result in cardiac arrest. In this case, the treatment of acute pulmonary edema from congestive heart failure exacerbation required bilevel positive airway pressure (BiPAP) with supplemental oxygen, nitrates, and a diuretic. This patient had a complicating factor: rhabdomyolysis, as evidenced by his elevated CPK level, blood in the urine, and myalgia. The rhabdomyolysis probably results from his being on the floor for a prolonged period. In such patients, all compartments should be checked to make sure that the cause of the rhabdomyolysis is not a compartment syndrome.\nIn addition, this patient has sustained a traumatic head injury and is receiving anticoagulation therapy with warfarin. Thus, a non-contrast head CT scan is required to rule out intracranial bleeding owing to the patient's advanced age, head trauma, and long-term use of anticoagulants and antiplatelet agents. A non-contrast cervical spine CT scan was also performed because of the patient's age and head trauma.\nCurrently, no clinical decision rule can effectively rule out cervical fracture in older adults, even in the absence of pain and tenderness. The rest of the physical examination results are reassuring for a lack of other traumatic injuries, which are common in older patients after a ground-level fall.\nAfter the workup, the patient was treated with intravenous (IV) nitroglycerin and BiPAP. His condition improved initially, and he was admitted to the intensive care unit. However, his hospital course was complicated by worsening renal failure and fluid overload. After a discussion of the goals of care, the patient was transferred to hospice care and died.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1536914,
"choiceText": "A lines",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536915,
"choiceText": "B lines",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536916,
"choiceText": "Lung sliding",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536917,
"choiceText": "Consolidation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "B lines would be the expected ultrasound pattern for acute pulmonary edema, as mentioned in the BLUE protocol. B lines are a form of artifact that spread from the pleural line and propagate to the end of the frame at least 12 cm down on the sonogram and represent the presence of fluid in the alveoli. They have also been observed in viral pneumonia, especially coronavirus disease 2019 (COVID-19).",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 492808,
"questionText": "Which of the following ultrasound patterns in the lungs is associated with acute pulmonary edema?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1536918,
"choiceText": "CT angiogram of the chest",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536919,
"choiceText": "CT scan of the abdomen and pelvis with IV contrast",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536920,
"choiceText": "Cardiac magnetic resonance imaging scan",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536921,
"choiceText": "Ventilation-perfusion scan of the chest",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "If chest radiography was clear and the sonogram did not show pulmonary edema, pulmonary embolism would be a consideration. Given this patient’s profound chronic kidney disease and rhabdomyolysis, a ventilation-perfusion scan of the chest would be a better choice than a CT angiogram of the chest because of the renal implications of giving contrast dye to a patient who has reduced filtering capacity.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 492809,
"questionText": "If this patient had clear lungs, a normal chest radiograph, a bedside sonogram with A lines with normal sliding, and a mildly diminished ejection fraction, which of the following should be the most likely next choice for an imaging modality?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "An Elderly Man Blacks Out in His Bathroom"
},
{
"authors": "Joshua J. Solano, MD",
"content": [],
"date": "October 31, 2024",
"figures": [],
"markdown": "# An Elderly Man Blacks Out in His Bathroom\n\n **Authors:** Joshua J. Solano, MD \n **Date:** October 31, 2024\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1536914,
"choiceText": "A lines",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536915,
"choiceText": "B lines",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536916,
"choiceText": "Lung sliding",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536917,
"choiceText": "Consolidation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "B lines would be the expected ultrasound pattern for acute pulmonary edema, as mentioned in the BLUE protocol. B lines are a form of artifact that spread from the pleural line and propagate to the end of the frame at least 12 cm down on the sonogram and represent the presence of fluid in the alveoli. They have also been observed in viral pneumonia, especially coronavirus disease 2019 (COVID-19).",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 492808,
"questionText": "Which of the following ultrasound patterns in the lungs is associated with acute pulmonary edema?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1536918,
"choiceText": "CT angiogram of the chest",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536919,
"choiceText": "CT scan of the abdomen and pelvis with IV contrast",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536920,
"choiceText": "Cardiac magnetic resonance imaging scan",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536921,
"choiceText": "Ventilation-perfusion scan of the chest",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "If chest radiography was clear and the sonogram did not show pulmonary edema, pulmonary embolism would be a consideration. Given this patient’s profound chronic kidney disease and rhabdomyolysis, a ventilation-perfusion scan of the chest would be a better choice than a CT angiogram of the chest because of the renal implications of giving contrast dye to a patient who has reduced filtering capacity.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 492809,
"questionText": "If this patient had clear lungs, a normal chest radiograph, a bedside sonogram with A lines with normal sliding, and a mildly diminished ejection fraction, which of the following should be the most likely next choice for an imaging modality?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "An Elderly Man Blacks Out in His Bathroom"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1536910,
"choiceText": "Angioedema",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536911,
"choiceText": "Pneumonia",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536912,
"choiceText": "Congestive heart failure exacerbation",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536913,
"choiceText": "Pulmonary embolism",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 492807,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1536914,
"choiceText": "A lines",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536915,
"choiceText": "B lines",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536916,
"choiceText": "Lung sliding",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536917,
"choiceText": "Consolidation",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "B lines would be the expected ultrasound pattern for acute pulmonary edema, as mentioned in the BLUE protocol. B lines are a form of artifact that spread from the pleural line and propagate to the end of the frame at least 12 cm down on the sonogram and represent the presence of fluid in the alveoli. They have also been observed in viral pneumonia, especially coronavirus disease 2019 (COVID-19).",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 492808,
"questionText": "Which of the following ultrasound patterns in the lungs is associated with acute pulmonary edema?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1536918,
"choiceText": "CT angiogram of the chest",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536919,
"choiceText": "CT scan of the abdomen and pelvis with IV contrast",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536920,
"choiceText": "Cardiac magnetic resonance imaging scan",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1536921,
"choiceText": "Ventilation-perfusion scan of the chest",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "If chest radiography was clear and the sonogram did not show pulmonary edema, pulmonary embolism would be a consideration. Given this patient’s profound chronic kidney disease and rhabdomyolysis, a ventilation-perfusion scan of the chest would be a better choice than a CT angiogram of the chest because of the renal implications of giving contrast dye to a patient who has reduced filtering capacity.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 492809,
"questionText": "If this patient had clear lungs, a normal chest radiograph, a bedside sonogram with A lines with normal sliding, and a mildly diminished ejection fraction, which of the following should be the most likely next choice for an imaging modality?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
939533 | /viewarticle/939533 | [
{
"authors": "Melba Estrella, MD; Alan Snyder; John Plante; Dirk M. Elston, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians, but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please email us at [email protected] with the subject line \"Case Challenge Suggestion.\" We look forward to hearing from you.",
"A 38-year-old man presents with a relapsing pruritic rash of 3 years' duration on his buttocks. He has no significant past medical history. Initially, he noticed several small, itchy, red bumps on his upper buttocks that increased in number and size concurrently with the appearance of blisters. The blisters tended to break open after scratching.",
"The rash first appeared after the patient adopted a dog from a shelter. He suspected that he might have contracted an infection from the dog and self-treated with an over-the-counter topical antimicrobial ointment, with no improvement. He later sought medical attention from his primary care provider, who prescribed a topical corticosteroid cream. Although multiple applications of the topical corticosteroid resulted in improvement, flares would arise when the cream was discontinued.",
"The patient states that the rash seems to be progressively worsening, mainly during warm weather, but he cannot identify specific triggers. He denies further dissemination of the lesions but recalls having had a similar milder version of the rash on both of his ankles, which subsided after he switched from ankle-cut socks to extra–low-cut socks.",
"The patient has no other rashes. He denies pain and recent fever or chills, travel, infections, and changes in weight. He is an otherwise healthy radiology technician who lives with his wife and dog. He has not been exposed to a family member or other contact with a similar rash. He changes daily into a clean uniform provided by his workplace and denies the use of new or borrowed clothing. The patient has no known medical allergies and is not taking medication. His immunizations are up to date."
],
"date": "November 15, 2024",
"figures": [],
"markdown": "# A 38-Year-Old Radiology Technician With a Blistering, Itchy Rash\n\n **Authors:** Melba Estrella, MD; Alan Snyder; John Plante; Dirk M. Elston, MD \n **Date:** November 15, 2024\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians, but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please email us at [email protected] with the subject line \"Case Challenge Suggestion.\" We look forward to hearing from you.\nA 38-year-old man presents with a relapsing pruritic rash of 3 years' duration on his buttocks. He has no significant past medical history. Initially, he noticed several small, itchy, red bumps on his upper buttocks that increased in number and size concurrently with the appearance of blisters. The blisters tended to break open after scratching.\nThe rash first appeared after the patient adopted a dog from a shelter. He suspected that he might have contracted an infection from the dog and self-treated with an over-the-counter topical antimicrobial ointment, with no improvement. He later sought medical attention from his primary care provider, who prescribed a topical corticosteroid cream. Although multiple applications of the topical corticosteroid resulted in improvement, flares would arise when the cream was discontinued.\nThe patient states that the rash seems to be progressively worsening, mainly during warm weather, but he cannot identify specific triggers. He denies further dissemination of the lesions but recalls having had a similar milder version of the rash on both of his ankles, which subsided after he switched from ankle-cut socks to extra–low-cut socks.\nThe patient has no other rashes. He denies pain and recent fever or chills, travel, infections, and changes in weight. He is an otherwise healthy radiology technician who lives with his wife and dog. He has not been exposed to a family member or other contact with a similar rash. He changes daily into a clean uniform provided by his workplace and denies the use of new or borrowed clothing. The patient has no known medical allergies and is not taking medication. His immunizations are up to date.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "A 38-Year-Old Radiology Technician With a Blistering, Itchy Rash"
},
{
"authors": "Melba Estrella, MD; Alan Snyder; John Plante; Dirk M. Elston, MD",
"content": [
"The skin examination reveals two poorly to well-demarcated linear plaques composed of multiple coalescing erythematous papules with punctate erosions, some of which exhibit sanguineous crusting. Slightly perceptible edema and overlying thin scaling are also present. Both lesions conform to a band-like rash confined to the posterior aspect of the waistline and upper buttocks, with sparing of the intergluteal cleft (Figures 1 and 2).",
"Figure 1.",
"Figure 2.",
"Associated moderate pruritus is also present. The regional lymph nodes are nonpalpable, and no additional rashes are noted. The rest of the physical examination findings are unremarkable.",
"The patient undergoes patch testing with the Thin-layer Rapid Use Epicutaneous Test (TRUE Test) baseline series kit and swabs for viral and bacterial culture. The results of all tests are negative."
],
"date": "November 15, 2024",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/939/533/939533-Thumb1_(1).jpg"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/939/533/939533-Thumb2_(1)_(1).jpg"
}
],
"markdown": "# A 38-Year-Old Radiology Technician With a Blistering, Itchy Rash\n\n **Authors:** Melba Estrella, MD; Alan Snyder; John Plante; Dirk M. Elston, MD \n **Date:** November 15, 2024\n\n ## Content\n\n The skin examination reveals two poorly to well-demarcated linear plaques composed of multiple coalescing erythematous papules with punctate erosions, some of which exhibit sanguineous crusting. Slightly perceptible edema and overlying thin scaling are also present. Both lesions conform to a band-like rash confined to the posterior aspect of the waistline and upper buttocks, with sparing of the intergluteal cleft (Figures 1 and 2).\nFigure 1.\nFigure 2.\nAssociated moderate pruritus is also present. The regional lymph nodes are nonpalpable, and no additional rashes are noted. The rest of the physical examination findings are unremarkable.\nThe patient undergoes patch testing with the Thin-layer Rapid Use Epicutaneous Test (TRUE Test) baseline series kit and swabs for viral and bacterial culture. The results of all tests are negative.\n\n ## Figures\n\n **Figure 1.** \n.jpg) \n\n**Figure 2.** \n_(1).jpg) \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1535597,
"choiceText": "Herpes simplex virus infection",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535598,
"choiceText": "Atopic dermatitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535599,
"choiceText": "Plaque psoriasis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535600,
"choiceText": "Contact dermatitis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 492329,
"questionText": "On the basis of these findings only, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 38-Year-Old Radiology Technician With a Blistering, Itchy Rash"
},
{
"authors": "Melba Estrella, MD; Alan Snyder; John Plante; Dirk M. Elston, MD",
"content": [
"Herpes simplex virus infection can affect almost any area of the skin or mucous membranes and presents with localized blistering. Isolation of the virus in tissue culture confirms the diagnosis.[1] In this case, the viral and bacterial cultures were negative. Although atopic dermatitis can occur on any part of the body, it would not remain as focal and symmetric over time, as the eruption seen in this patient has been—with the exception of flexural presentations, which were not observed in this case.",
"Plaque psoriasis may cause large, itchy, and erythematous demarcated scaly plaques confined to areas of pressure. However, in contrast to the thin scaling on this patient's plaques and mild edema, psoriasis displays bumpy red plaques with silvery thick scales that when removed elicit pinpoint bleeding, commonly known as the Auspitz sign. The punctate erosions in this case could potentially resemble the remnants of pinpoint bleeding, but because they were formed in the presence of vesiculation, it would be extremely unlikely for this presentation to be psoriasis. Thus, contact dermatitis is the diagnosis of exclusion.",
"Contact dermatitis is an inflammatory response of the skin to environmental insults that acutely manifests with pruritic skin lesions and varying degrees of erythema, edema, scaling, and vesicles. Contact dermatitis may be classified as allergic or irritant. Allergic contact dermatitis is a delayed type of hypersensitivity reaction induced by a lymphocyte-mediated response after skin contact with sensitized allergens.[2] Irritant contact dermatitis is a non–immune-mediated inflammatory response by mediators of epidermal cells that react to direct chemical insults on the skin. Because allergic and irritant contact dermatitis often overlap in clinical presentations, identifying the correct trigger of the reaction is essential.",
"The linear distribution of the rash in this case strongly suggests a reaction to the elastic waistband of the patient's underwear. Rubber-containing products, such as elastic waistbands, can be associated with bleached rubber syndrome, conventional allergic contact dermatitis to rubber antioxidants and accelerators, and even irritant dermatitis.[2] No reliable diagnostic tests for irritant contact dermatitis are available; thus, the diagnosis in this case relies mainly on the exclusion of allergic contact dermatitis and appropriate clinical interventions.[3]",
"For reasons not yet clearly understood, many patients can become sensitized to certain components found in the molecules of natural rubber (latex) or synthetic rubber; however, they are more likely to become sensitized to the many chemicals used in the process of rubber manufacturing. These chemicals make up a wide list of allergens ranging from vulcanizing to accelerator agents; the latter is the most common of these allergens. A detailed list of these chemicals is available at DermNet NZ.[4] About 1%-5% of the general population exhibits rubber allergy as a reaction either to the components of rubber or to its manufacturing resins.[2]"
],
"date": "November 15, 2024",
"figures": [],
"markdown": "# A 38-Year-Old Radiology Technician With a Blistering, Itchy Rash\n\n **Authors:** Melba Estrella, MD; Alan Snyder; John Plante; Dirk M. Elston, MD \n **Date:** November 15, 2024\n\n ## Content\n\n Herpes simplex virus infection can affect almost any area of the skin or mucous membranes and presents with localized blistering. Isolation of the virus in tissue culture confirms the diagnosis.[1] In this case, the viral and bacterial cultures were negative. Although atopic dermatitis can occur on any part of the body, it would not remain as focal and symmetric over time, as the eruption seen in this patient has been—with the exception of flexural presentations, which were not observed in this case.\nPlaque psoriasis may cause large, itchy, and erythematous demarcated scaly plaques confined to areas of pressure. However, in contrast to the thin scaling on this patient's plaques and mild edema, psoriasis displays bumpy red plaques with silvery thick scales that when removed elicit pinpoint bleeding, commonly known as the Auspitz sign. The punctate erosions in this case could potentially resemble the remnants of pinpoint bleeding, but because they were formed in the presence of vesiculation, it would be extremely unlikely for this presentation to be psoriasis. Thus, contact dermatitis is the diagnosis of exclusion.\nContact dermatitis is an inflammatory response of the skin to environmental insults that acutely manifests with pruritic skin lesions and varying degrees of erythema, edema, scaling, and vesicles. Contact dermatitis may be classified as allergic or irritant. Allergic contact dermatitis is a delayed type of hypersensitivity reaction induced by a lymphocyte-mediated response after skin contact with sensitized allergens.[2] Irritant contact dermatitis is a non–immune-mediated inflammatory response by mediators of epidermal cells that react to direct chemical insults on the skin. Because allergic and irritant contact dermatitis often overlap in clinical presentations, identifying the correct trigger of the reaction is essential.\nThe linear distribution of the rash in this case strongly suggests a reaction to the elastic waistband of the patient's underwear. Rubber-containing products, such as elastic waistbands, can be associated with bleached rubber syndrome, conventional allergic contact dermatitis to rubber antioxidants and accelerators, and even irritant dermatitis.[2] No reliable diagnostic tests for irritant contact dermatitis are available; thus, the diagnosis in this case relies mainly on the exclusion of allergic contact dermatitis and appropriate clinical interventions.[3]\nFor reasons not yet clearly understood, many patients can become sensitized to certain components found in the molecules of natural rubber (latex) or synthetic rubber; however, they are more likely to become sensitized to the many chemicals used in the process of rubber manufacturing. These chemicals make up a wide list of allergens ranging from vulcanizing to accelerator agents; the latter is the most common of these allergens. A detailed list of these chemicals is available at DermNet NZ.[4] About 1%-5% of the general population exhibits rubber allergy as a reaction either to the components of rubber or to its manufacturing resins.[2]\n\n ## Figures\n\n \n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1535597,
"choiceText": "Herpes simplex virus infection",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535598,
"choiceText": "Atopic dermatitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535599,
"choiceText": "Plaque psoriasis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535600,
"choiceText": "Contact dermatitis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 492329,
"questionText": "On the basis of these findings only, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 38-Year-Old Radiology Technician With a Blistering, Itchy Rash"
},
{
"authors": "Melba Estrella, MD; Alan Snyder; John Plante; Dirk M. Elston, MD",
"content": [
"Many patients with an apparent allergy to elasticated clothing are not allergic to the elastic itself but rather to the subproducts that result from laundering the elasticated clothing with chlorine bleach.[5,6] Bleached rubber contact dermatitis, also known as \"bleached rubber syndrome,\" is a common type of allergic contact dermatitis that results from allergy to bleached rubber compounds.[6,7] Jordan and Bourlas[6] first described this syndrome in 1975. In a case series of six patients who were allergic to elastic underwear, the investigators demonstrated that the main cause of the syndrome in all the study participants was N,N-dibenzylcarbamyl chloride, the resultant product from the interaction of the accelerator agent zinc dibenzyldithiocarbamate with chlorine laundry bleach.",
"Repeated bleaching in theory causes greater availability of carbamate compounds, which enhance the allergenicity of the elastic. This increase in allergenicity could help explain the progressive worsening of this patient's rash.",
"The first step in the diagnosis of allergic contact dermatitis is to determine whether the lesions resolve after avoidance of the offending agent. If the rash persists despite avoidance and empirical topical treatment, patch testing is indicated. Patients with suspected allergic contact dermatitis who have a negative reaction on the initial patch test should undergo additional testing. A patch test is the most useful and cost-effective diagnostic tool to identify allergic contact dermatitis; the sensitivity and specificity range from 70%-80%.[8,9] A commonly used patch test is the TRUE Test baseline series kit, which includes 27 single antigens and eight mixes of allergens that are frequently associated with allergic contact dermatitis, as well as a negative control.",
"If a patient reacts positively to a rubber mix on the baseline series kit, patch testing for rubber compounds is the next step.[10,11] Kits that contain broken-down rubber ingredients are used to further assess the allergy in question. Uter and colleagues[11] suggested that if the allergy remains strongly suspected despite a negative baseline series patch test, a rubber series kit is warranted to avoid false-negative results. The TRUE Test 5 Rubber Panel kit is a commercially available rubber series kit that contains ubiquitous chemicals used in rubber manufacturing, such as accelerator agents.",
"A reading of a rubber series patch test in this patient was performed 48 hours after application, then again after 72 and 96 hours. No reaction was visible.",
"Further questioning about the patient's laundering practices revealed that his wife washed his white clothes with bleach. This finding is consistent with his past history of a similar rash on the ankles that resolved with the use of new socks. Because patch testing typically does not detect carbamyl chloride, the diagnosis was made clinically in this patient."
],
"date": "November 15, 2024",
"figures": [],
"markdown": "# A 38-Year-Old Radiology Technician With a Blistering, Itchy Rash\n\n **Authors:** Melba Estrella, MD; Alan Snyder; John Plante; Dirk M. Elston, MD \n **Date:** November 15, 2024\n\n ## Content\n\n Many patients with an apparent allergy to elasticated clothing are not allergic to the elastic itself but rather to the subproducts that result from laundering the elasticated clothing with chlorine bleach.[5,6] Bleached rubber contact dermatitis, also known as \"bleached rubber syndrome,\" is a common type of allergic contact dermatitis that results from allergy to bleached rubber compounds.[6,7] Jordan and Bourlas[6] first described this syndrome in 1975. In a case series of six patients who were allergic to elastic underwear, the investigators demonstrated that the main cause of the syndrome in all the study participants was N,N-dibenzylcarbamyl chloride, the resultant product from the interaction of the accelerator agent zinc dibenzyldithiocarbamate with chlorine laundry bleach.\nRepeated bleaching in theory causes greater availability of carbamate compounds, which enhance the allergenicity of the elastic. This increase in allergenicity could help explain the progressive worsening of this patient's rash.\nThe first step in the diagnosis of allergic contact dermatitis is to determine whether the lesions resolve after avoidance of the offending agent. If the rash persists despite avoidance and empirical topical treatment, patch testing is indicated. Patients with suspected allergic contact dermatitis who have a negative reaction on the initial patch test should undergo additional testing. A patch test is the most useful and cost-effective diagnostic tool to identify allergic contact dermatitis; the sensitivity and specificity range from 70%-80%.[8,9] A commonly used patch test is the TRUE Test baseline series kit, which includes 27 single antigens and eight mixes of allergens that are frequently associated with allergic contact dermatitis, as well as a negative control.\nIf a patient reacts positively to a rubber mix on the baseline series kit, patch testing for rubber compounds is the next step.[10,11] Kits that contain broken-down rubber ingredients are used to further assess the allergy in question. Uter and colleagues[11] suggested that if the allergy remains strongly suspected despite a negative baseline series patch test, a rubber series kit is warranted to avoid false-negative results. The TRUE Test 5 Rubber Panel kit is a commercially available rubber series kit that contains ubiquitous chemicals used in rubber manufacturing, such as accelerator agents.\nA reading of a rubber series patch test in this patient was performed 48 hours after application, then again after 72 and 96 hours. No reaction was visible.\nFurther questioning about the patient's laundering practices revealed that his wife washed his white clothes with bleach. This finding is consistent with his past history of a similar rash on the ankles that resolved with the use of new socks. Because patch testing typically does not detect carbamyl chloride, the diagnosis was made clinically in this patient.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "A 38-Year-Old Radiology Technician With a Blistering, Itchy Rash"
},
{
"authors": "Melba Estrella, MD; Alan Snyder; John Plante; Dirk M. Elston, MD",
"content": [
"History-taking before patch testing identifies potential allergens to which patients have been exposed that should be included in the test. Once patch testing is completed, additional history-taking helps determine the clinical significance of the findings.[9] Note that some garments are washed with sodium hypochlorite immediately after manufacture, which causes structural changes in some elastics.[12] Because this practice could potentially cloud the clinical picture if the patient denies washing clothes with bleach, a detailed history before patch testing is key in evaluating patients with suspected bleached rubber syndrome.",
"Mid- or high-potency topical corticosteroids are the mainstay of treatment to relieve the inflammatory signs of contact dermatitis. Although antihistamines may not relieve associated pruritus, they are usually prescribed. If more than 20% of the skin surface is involved, systemic corticosteroids are recommended.[8]",
"The definitive management of allergic contact dermatitis is the detection and removal of the offending allergen. Nonchlorine bleach is safe to use, but all elasticated clothing that has been previously exposed to chlorine bleach must be discarded. Patients should be followed up by a dermatologist to assess for the recurrence of dermatitis.",
"This patient was treated with a regimen of high-potency topical corticosteroids that was tapered over several weeks. After 3 months of follow-up, the lesions had cleared, and he had no signs of recurrence at 8 months."
],
"date": "November 15, 2024",
"figures": [],
"markdown": "# A 38-Year-Old Radiology Technician With a Blistering, Itchy Rash\n\n **Authors:** Melba Estrella, MD; Alan Snyder; John Plante; Dirk M. Elston, MD \n **Date:** November 15, 2024\n\n ## Content\n\n History-taking before patch testing identifies potential allergens to which patients have been exposed that should be included in the test. Once patch testing is completed, additional history-taking helps determine the clinical significance of the findings.[9] Note that some garments are washed with sodium hypochlorite immediately after manufacture, which causes structural changes in some elastics.[12] Because this practice could potentially cloud the clinical picture if the patient denies washing clothes with bleach, a detailed history before patch testing is key in evaluating patients with suspected bleached rubber syndrome.\nMid- or high-potency topical corticosteroids are the mainstay of treatment to relieve the inflammatory signs of contact dermatitis. Although antihistamines may not relieve associated pruritus, they are usually prescribed. If more than 20% of the skin surface is involved, systemic corticosteroids are recommended.[8]\nThe definitive management of allergic contact dermatitis is the detection and removal of the offending allergen. Nonchlorine bleach is safe to use, but all elasticated clothing that has been previously exposed to chlorine bleach must be discarded. Patients should be followed up by a dermatologist to assess for the recurrence of dermatitis.\nThis patient was treated with a regimen of high-potency topical corticosteroids that was tapered over several weeks. After 3 months of follow-up, the lesions had cleared, and he had no signs of recurrence at 8 months.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1535601,
"choiceText": "Natural latex proteins",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535602,
"choiceText": "Synthetic latex polymers",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535603,
"choiceText": "Rubber manufacturing accelerators",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535604,
"choiceText": "Bleached rubber compounds",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Patients can become sensitized to components found in natural rubber (latex) or synthetic rubber; however, they are more likely to become sensitized to the chemicals used in the process of rubber manufacturing, particularly accelerator agents.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 492330,
"questionText": "Which of the following is most likely to cause allergic contact dermatitis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1535605,
"choiceText": "Repeat patch testing using a rubber series kit",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535606,
"choiceText": "Perform patch testing using samples of the patient's underwear",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535607,
"choiceText": "Perform a repeat open application test",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535608,
"choiceText": "Perform a punch biopsy",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nIf allergy remains strongly suspected despite a negative baseline series patch test, a rubber series kit is warranted to avoid false-negative results.<sup type=\"ref\">[11]</sup> In this patient, the negative results of the rubber series kit obviated the need to repeat the test.<br/><br/>\r\n\r\nMany known allergens, such as those commonly found in cosmetic products, are not included in patch testing kits. Thus, referral to a specialist for customized patch testing would be useful to confirm the diagnosis in this patient.<br/><br/>\r\n\r\nAn open application test, also known as a "repeat open application test," is performed after a mildly positive patch test to determine whether the reaction is clinically significant.<sup type=\"ref\">[13]</sup> The allergen in question is openly and repeatedly applied to a small area of the skin, which is observed for a reaction at regular intervals within the first hour of testing and after 3-4 days.<sup type=\"ref\">[14]</sup> This test is most appropriate for "leave-on" consumer products suspected to contain low-level contact allergens.<br/><br/>\r\n\r\nA skin biopsy can exclude other conditions, such as psoriasis. The histologic finding of spongiotic dermatitis is an important clue to the diagnosis of allergic contact dermatitis.<sup type=\"ref\">[15]</sup> Because the offending agent had been identified in this patient, a skin biopsy was not necessary.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 492331,
"questionText": "Of the following tests, which would best help to confirm this patient's diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 38-Year-Old Radiology Technician With a Blistering, Itchy Rash"
},
{
"authors": "Melba Estrella, MD; Alan Snyder; John Plante; Dirk M. Elston, MD",
"content": [],
"date": "November 15, 2024",
"figures": [],
"markdown": "# A 38-Year-Old Radiology Technician With a Blistering, Itchy Rash\n\n **Authors:** Melba Estrella, MD; Alan Snyder; John Plante; Dirk M. Elston, MD \n **Date:** November 15, 2024\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1535601,
"choiceText": "Natural latex proteins",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535602,
"choiceText": "Synthetic latex polymers",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535603,
"choiceText": "Rubber manufacturing accelerators",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535604,
"choiceText": "Bleached rubber compounds",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Patients can become sensitized to components found in natural rubber (latex) or synthetic rubber; however, they are more likely to become sensitized to the chemicals used in the process of rubber manufacturing, particularly accelerator agents.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 492330,
"questionText": "Which of the following is most likely to cause allergic contact dermatitis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1535605,
"choiceText": "Repeat patch testing using a rubber series kit",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535606,
"choiceText": "Perform patch testing using samples of the patient's underwear",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535607,
"choiceText": "Perform a repeat open application test",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535608,
"choiceText": "Perform a punch biopsy",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nIf allergy remains strongly suspected despite a negative baseline series patch test, a rubber series kit is warranted to avoid false-negative results.<sup type=\"ref\">[11]</sup> In this patient, the negative results of the rubber series kit obviated the need to repeat the test.<br/><br/>\r\n\r\nMany known allergens, such as those commonly found in cosmetic products, are not included in patch testing kits. Thus, referral to a specialist for customized patch testing would be useful to confirm the diagnosis in this patient.<br/><br/>\r\n\r\nAn open application test, also known as a "repeat open application test," is performed after a mildly positive patch test to determine whether the reaction is clinically significant.<sup type=\"ref\">[13]</sup> The allergen in question is openly and repeatedly applied to a small area of the skin, which is observed for a reaction at regular intervals within the first hour of testing and after 3-4 days.<sup type=\"ref\">[14]</sup> This test is most appropriate for "leave-on" consumer products suspected to contain low-level contact allergens.<br/><br/>\r\n\r\nA skin biopsy can exclude other conditions, such as psoriasis. The histologic finding of spongiotic dermatitis is an important clue to the diagnosis of allergic contact dermatitis.<sup type=\"ref\">[15]</sup> Because the offending agent had been identified in this patient, a skin biopsy was not necessary.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 492331,
"questionText": "Of the following tests, which would best help to confirm this patient's diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "A 38-Year-Old Radiology Technician With a Blistering, Itchy Rash"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1535597,
"choiceText": "Herpes simplex virus infection",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535598,
"choiceText": "Atopic dermatitis",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535599,
"choiceText": "Plaque psoriasis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535600,
"choiceText": "Contact dermatitis",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 492329,
"questionText": "On the basis of these findings only, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1535601,
"choiceText": "Natural latex proteins",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535602,
"choiceText": "Synthetic latex polymers",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535603,
"choiceText": "Rubber manufacturing accelerators",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535604,
"choiceText": "Bleached rubber compounds",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Patients can become sensitized to components found in natural rubber (latex) or synthetic rubber; however, they are more likely to become sensitized to the chemicals used in the process of rubber manufacturing, particularly accelerator agents.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 492330,
"questionText": "Which of the following is most likely to cause allergic contact dermatitis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1535605,
"choiceText": "Repeat patch testing using a rubber series kit",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535606,
"choiceText": "Perform patch testing using samples of the patient's underwear",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535607,
"choiceText": "Perform a repeat open application test",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1535608,
"choiceText": "Perform a punch biopsy",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "\r\nIf allergy remains strongly suspected despite a negative baseline series patch test, a rubber series kit is warranted to avoid false-negative results.<sup type=\"ref\">[11]</sup> In this patient, the negative results of the rubber series kit obviated the need to repeat the test.<br/><br/>\r\n\r\nMany known allergens, such as those commonly found in cosmetic products, are not included in patch testing kits. Thus, referral to a specialist for customized patch testing would be useful to confirm the diagnosis in this patient.<br/><br/>\r\n\r\nAn open application test, also known as a "repeat open application test," is performed after a mildly positive patch test to determine whether the reaction is clinically significant.<sup type=\"ref\">[13]</sup> The allergen in question is openly and repeatedly applied to a small area of the skin, which is observed for a reaction at regular intervals within the first hour of testing and after 3-4 days.<sup type=\"ref\">[14]</sup> This test is most appropriate for "leave-on" consumer products suspected to contain low-level contact allergens.<br/><br/>\r\n\r\nA skin biopsy can exclude other conditions, such as psoriasis. The histologic finding of spongiotic dermatitis is an important clue to the diagnosis of allergic contact dermatitis.<sup type=\"ref\">[15]</sup> Because the offending agent had been identified in this patient, a skin biopsy was not necessary.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 492331,
"questionText": "Of the following tests, which would best help to confirm this patient's diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
842258 | /viewarticle/842258 | [
{
"authors": "Winston W. Tan, MD; Matthew Tan",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 63-year-old woman presents with a chronic cough. She was in her usual state of health until 3 months ago, when she developed a dry cough with fever. She was initially treated with antibiotics for 2 weeks. The cough improved, and the fever resolved. However, the dry cough returned.",
"The patient reports recent several instances of hemoptysis, as well as a 5-lb weight loss that she attributes to her recent diet change and exercise. She also describes chest pain, shortness of breath, dyspnea, and significant lower back pain.",
"Her medical history is significant for hypertension and diabetes. Her family history includes a father who had congestive heart failure at age 73 years. The patient gets her eyes checked regularly. She has never seen a pulmonary specialist. She reports aches and pains that vary, depending on how much physical activity she gets. She has had a hysterectomy. She is married and denies smoking, although she reports a history of continued secondhand smoke exposure."
],
"date": "October 16, 2020",
"figures": [],
"markdown": "# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\n\n **Authors:** Winston W. Tan, MD; Matthew Tan \n **Date:** October 16, 2020\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 63-year-old woman presents with a chronic cough. She was in her usual state of health until 3 months ago, when she developed a dry cough with fever. She was initially treated with antibiotics for 2 weeks. The cough improved, and the fever resolved. However, the dry cough returned.\nThe patient reports recent several instances of hemoptysis, as well as a 5-lb weight loss that she attributes to her recent diet change and exercise. She also describes chest pain, shortness of breath, dyspnea, and significant lower back pain.\nHer medical history is significant for hypertension and diabetes. Her family history includes a father who had congestive heart failure at age 73 years. The patient gets her eyes checked regularly. She has never seen a pulmonary specialist. She reports aches and pains that vary, depending on how much physical activity she gets. She has had a hysterectomy. She is married and denies smoking, although she reports a history of continued secondhand smoke exposure.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old"
},
{
"authors": "Winston W. Tan, MD; Matthew Tan",
"content": [
"Physical examination reveals the following:",
"Blood pressure: 124/58 mm Hg",
"Temperature: 98.3°F (36.8°C)",
"Heart rate: 85 beats/min",
"Examination of her neck reveals enlarged supraclavicular lymph nodes. Examination of her breasts reveals no distinct nodules, lumps, discharge, skin retraction, or axillary adenopathy. Her abdomen is soft, benign, and nontender. Neurologically, cranial nerves II through XII are grossly intact.",
"Upon evaluation of the lungs, wheezing and atelectasis are observed. Increased work of breathing is also noted. A chest radiograph is subsequently ordered."
],
"date": "October 16, 2020",
"figures": [],
"markdown": "# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\n\n **Authors:** Winston W. Tan, MD; Matthew Tan \n **Date:** October 16, 2020\n\n ## Content\n\n Physical examination reveals the following:\nBlood pressure: 124/58 mm Hg\nTemperature: 98.3°F (36.8°C)\nHeart rate: 85 beats/min\nExamination of her neck reveals enlarged supraclavicular lymph nodes. Examination of her breasts reveals no distinct nodules, lumps, discharge, skin retraction, or axillary adenopathy. Her abdomen is soft, benign, and nontender. Neurologically, cranial nerves II through XII are grossly intact.\nUpon evaluation of the lungs, wheezing and atelectasis are observed. Increased work of breathing is also noted. A chest radiograph is subsequently ordered.\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 831357,
"choiceText": "Sarcoidosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831359,
"choiceText": "Lung cancer",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831361,
"choiceText": "Tuberculosis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831363,
"choiceText": "Pneumonia \r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 261411,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old"
},
{
"authors": "Winston W. Tan, MD; Matthew Tan",
"content": [
"Lung cancer is often insidious, failing to produce clear symptoms until advanced disease. A high index of suspicion is required to properly identify this disease in most patients. In this case, weight loss, hemoptysis, and a history of secondhand smoke exposure, along with a low-grade fever and irregularities upon lung evaluation, warranted an investigation for lung cancer. Subsequently, CT revealed a 1.3-cm left upper lobe complex nodule (Figure 1).",
"Figure 1.",
"The patient underwent a left upper lobectomy with mediastinal lymph node dissection for a 1.5-cm poorly differentiated squamous cancer of lung, with 1 (station 5) of 18 lymph nodes positive with a microscopic focus of cancer. She was subsequently treated with adjuvant chemoradiation therapy, consisting of cisplatin and docetaxel concurrent with radiation. However, chemotherapy was stopped after a few doses owing to complications.",
"The patient later developed a seizure and was hospitalized; MRI of the brain was negative for metastatic disease but suggested possible temporal lobe inflammation. Her cerebrospinal fluid was positive for herpes. She was started on phenytoin and valacyclovir.",
"She completed radiation therapy to 6120 cGy. Additional planned chemotherapy was delayed owing to the patient's debility. She also experienced an outbreak of shingles. Serial follow-up every 4 months showed that disease was in complete remission, with a stable postradiation residual scar in the left lung.",
"Figure 2.",
"Figure 3.",
"Six years later, CT revealed a new enhancing mass in the medial right upper lobe (adjacent to the mediastinum) that was suspicious for metastatic or new primary lung cancer (Figure 2). A brain scan was negative for metastases. PET revealed uptake in the expected area and indeterminate uptake in a right hilar node (Figure 3), but was otherwise negative. Pulmonary function tests revealed showed an FEV1 of 1.45 L, or 65% of predicted. The diffusing capacity of the lung for carbon monoxide (DLCO) was 42%. Saturation was normal at rest but decreased to 92% with exercise.",
"Endobronchial ultrasonography did not reveal any specific abnormality. The mucosa was friable. A right hilar lymph node was sampled, but no lymphoid elements were obtained. Nothing specific for the tumor area was seen.",
"Figure 4.",
"A CT-guided biopsy was nondiagnostic. Surgical exploration yielded a small cell carcinoma that was unresectable owing to mediastinal invasion and bleeding (Figure 4). The patient started palliative chemotherapy with carboplatin/etoposide, with etoposide given orally on days 2 and 3. She completed four cycles of this chemotherapy and tolerated chemotherapy well overall.",
"Follow-up CT showed minimal residual density in the area of the prior lesion. As a result of excellent response, she was referred for proton therapy, because standard radiation was not feasible owing to prior dosing.",
"Induction chemotherapy was followed by consolidation radiation. The patient subsequently underwent proton radiation to the residual chest mass. She experienced a seizure; she was dehydrated, and was started on anticonvulsant and became stable. MRI of the brain revealed an area of right anterior temporal encephalomalacia. She is doing well currently and is under active surveillance for her cancer."
],
"date": "October 16, 2020",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/842/258/842258-Thumb1a.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/842/258/842258-Thumb2a.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/842/258/842258-Thumb3a.png"
},
{
"caption": "Figure 4.",
"image_url": "https://img.medscapestatic.com/article/842/258/842258-Thumb4a.png"
}
],
"markdown": "# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\n\n **Authors:** Winston W. Tan, MD; Matthew Tan \n **Date:** October 16, 2020\n\n ## Content\n\n Lung cancer is often insidious, failing to produce clear symptoms until advanced disease. A high index of suspicion is required to properly identify this disease in most patients. In this case, weight loss, hemoptysis, and a history of secondhand smoke exposure, along with a low-grade fever and irregularities upon lung evaluation, warranted an investigation for lung cancer. Subsequently, CT revealed a 1.3-cm left upper lobe complex nodule (Figure 1).\nFigure 1.\nThe patient underwent a left upper lobectomy with mediastinal lymph node dissection for a 1.5-cm poorly differentiated squamous cancer of lung, with 1 (station 5) of 18 lymph nodes positive with a microscopic focus of cancer. She was subsequently treated with adjuvant chemoradiation therapy, consisting of cisplatin and docetaxel concurrent with radiation. However, chemotherapy was stopped after a few doses owing to complications.\nThe patient later developed a seizure and was hospitalized; MRI of the brain was negative for metastatic disease but suggested possible temporal lobe inflammation. Her cerebrospinal fluid was positive for herpes. She was started on phenytoin and valacyclovir.\nShe completed radiation therapy to 6120 cGy. Additional planned chemotherapy was delayed owing to the patient's debility. She also experienced an outbreak of shingles. Serial follow-up every 4 months showed that disease was in complete remission, with a stable postradiation residual scar in the left lung.\nFigure 2.\nFigure 3.\nSix years later, CT revealed a new enhancing mass in the medial right upper lobe (adjacent to the mediastinum) that was suspicious for metastatic or new primary lung cancer (Figure 2). A brain scan was negative for metastases. PET revealed uptake in the expected area and indeterminate uptake in a right hilar node (Figure 3), but was otherwise negative. Pulmonary function tests revealed showed an FEV1 of 1.45 L, or 65% of predicted. The diffusing capacity of the lung for carbon monoxide (DLCO) was 42%. Saturation was normal at rest but decreased to 92% with exercise.\nEndobronchial ultrasonography did not reveal any specific abnormality. The mucosa was friable. A right hilar lymph node was sampled, but no lymphoid elements were obtained. Nothing specific for the tumor area was seen.\nFigure 4.\nA CT-guided biopsy was nondiagnostic. Surgical exploration yielded a small cell carcinoma that was unresectable owing to mediastinal invasion and bleeding (Figure 4). The patient started palliative chemotherapy with carboplatin/etoposide, with etoposide given orally on days 2 and 3. She completed four cycles of this chemotherapy and tolerated chemotherapy well overall.\nFollow-up CT showed minimal residual density in the area of the prior lesion. As a result of excellent response, she was referred for proton therapy, because standard radiation was not feasible owing to prior dosing.\nInduction chemotherapy was followed by consolidation radiation. The patient subsequently underwent proton radiation to the residual chest mass. She experienced a seizure; she was dehydrated, and was started on anticonvulsant and became stable. MRI of the brain revealed an area of right anterior temporal encephalomalacia. She is doing well currently and is under active surveillance for her cancer.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n**Figure 4.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 831357,
"choiceText": "Sarcoidosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831359,
"choiceText": "Lung cancer",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831361,
"choiceText": "Tuberculosis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831363,
"choiceText": "Pneumonia \r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 261411,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old"
},
{
"authors": "Winston W. Tan, MD; Matthew Tan",
"content": [
"Non-small cell lung cancer accounts for approximately 85% of all lung cancers. Histologically, it is divided into adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Patients with non-small cell lung cancer require a complete staging work-up to evaluate the extent of disease because stage plays a major role in determining the choice of treatment.[1]",
"The patient in this case has the typical presentation of chronic cough. Typically, a cough that is initially thought to be an infection is noted. A chronic cough without improvement of symptoms despite treatment for infection should prompt further evaluation for potential lung mass. CT of the chest is often used as a diagnostic tool to clarify the suspicion of a lung mass.[2]",
"Because of the importance of stage in the therapeutic decision-making process, all patients must undergo proper staging of disease. A complete staging work-up should be performed to evaluate the extent of disease. In the United States, the standard staging work-up includes the following:",
"CT of the chest and upper abdomen",
"Complete blood count with differential",
"Serum chemistry studies, including creatinine, electrolytes, and calcium",
"Alkaline phosphate",
"Aspartate aminotransferase",
"Pulmonary function testing",
"Mediastinoscopy (if surgical resection is considered)",
"The information obtained from these tests guides additional testing (eg, imaging studies). Invasive staging procedures (eg, mediastinoscopy, mediastinotomy) may be required to assess mediastinal lymph nodes in patients who may undergo surgical resection. PET may be useful in detecting affected nodes, which may influence decisions about operability.",
"Paraneoplastic syndromes are more likely to occur in small cell lung cancer than in non-small cell lung cancer. Patients are at risk for the following:",
"Cushing syndrome",
"Lambert-Eaton myasthenic syndrome (Onset of proximal lower-extremity weakness is gradual; proximal upper-extremity weakness is usually less noticeable; the syndrome may be worse in the morning and improve during the day; although extraocular muscle involvement is uncommon, ptosis is often found)",
"Hypercalcemia (usually occurs with squamous cell carcinoma)",
"Syndrome of inappropriate antidiuretic hormone secretion",
"Enlargement of the extremities and painful, swollen joints (hypertrophic osteoarthropathy)"
],
"date": "October 16, 2020",
"figures": [],
"markdown": "# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\n\n **Authors:** Winston W. Tan, MD; Matthew Tan \n **Date:** October 16, 2020\n\n ## Content\n\n Non-small cell lung cancer accounts for approximately 85% of all lung cancers. Histologically, it is divided into adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Patients with non-small cell lung cancer require a complete staging work-up to evaluate the extent of disease because stage plays a major role in determining the choice of treatment.[1]\nThe patient in this case has the typical presentation of chronic cough. Typically, a cough that is initially thought to be an infection is noted. A chronic cough without improvement of symptoms despite treatment for infection should prompt further evaluation for potential lung mass. CT of the chest is often used as a diagnostic tool to clarify the suspicion of a lung mass.[2]\nBecause of the importance of stage in the therapeutic decision-making process, all patients must undergo proper staging of disease. A complete staging work-up should be performed to evaluate the extent of disease. In the United States, the standard staging work-up includes the following:\nCT of the chest and upper abdomen\nComplete blood count with differential\nSerum chemistry studies, including creatinine, electrolytes, and calcium\nAlkaline phosphate\nAspartate aminotransferase\nPulmonary function testing\nMediastinoscopy (if surgical resection is considered)\nThe information obtained from these tests guides additional testing (eg, imaging studies). Invasive staging procedures (eg, mediastinoscopy, mediastinotomy) may be required to assess mediastinal lymph nodes in patients who may undergo surgical resection. PET may be useful in detecting affected nodes, which may influence decisions about operability.\nParaneoplastic syndromes are more likely to occur in small cell lung cancer than in non-small cell lung cancer. Patients are at risk for the following:\nCushing syndrome\nLambert-Eaton myasthenic syndrome (Onset of proximal lower-extremity weakness is gradual; proximal upper-extremity weakness is usually less noticeable; the syndrome may be worse in the morning and improve during the day; although extraocular muscle involvement is uncommon, ptosis is often found)\nHypercalcemia (usually occurs with squamous cell carcinoma)\nSyndrome of inappropriate antidiuretic hormone secretion\nEnlargement of the extremities and painful, swollen joints (hypertrophic osteoarthropathy)\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old"
},
{
"authors": "Winston W. Tan, MD; Matthew Tan",
"content": [
"The standard treatment for stage I and II disease is surgical resection. In stage IIIA, chemotherapy is indicated, as is surgical resection in selected patients. Standard treatment of stage IIIb is chemoradiation. Stage IV requires cisplatin-based chemotherapy or surgical resection if a solitary metastatic lesion with resectable primary tumor is present.[3,4,5]",
"This patient underwent resection of the cancer. Owing to her residual disease and because her lymph nodes were positive, she was treated with chemoradiation. Surgical resection is the primary modality of treatment for early stage non-small cell lung cancer.[6]",
"Close surveillance of patients with cancer should be the standard after completion of therapy. This patient had a contralateral hilar recurrence 6 years later. When a patient has a recurrence, it must be determined whether it is the same cancer or another primary cancer. This patient had another primary cancer, specifically small cell cancer of the lung. Biopsy must be done of a new recurrence, because it could be an entirely different cancer.",
"Approximately 60%-70% of patients with small cell lung cancer have clinically disseminated or extensive disease at presentation. Extensive-stage small cell lung cancer is incurable. When given combination chemotherapy, patients with extensive-stage disease have a complete response rate of more than 20% and a median survival longer than 7 months; however, only 2% are alive at 5 years.",
"For individuals with limited-stage disease that is treated with combination chemotherapy plus chest radiation, a complete response rate of 80% and survival of 17 months have been reported; 12%-15% of patients are alive at 5 years.[1]",
"Recommendations from the National Comprehensive Cancer Network (NCCN) regarding cancer surveillance in survivors of non-small cell lung cancer include the following:",
"History and physical examination, and chest CT with or without contrast, every 6-12 months for 2 years, then history and physical examination and noncontrast chest CT annually",
"Assessment of smoking status at each visit, with counseling and referral for smoking cessation as needed",
"Other NCCN recommendations for long-term follow-up care include the following:",
"Immunization: Annual influenza vaccination, pneumococcal vaccination with revaccination as appropriate, herpes zoster vaccination",
"Counseling regarding health promotion and wellness (eg, regular physical activity, healthy diet)",
"Routine health monitoring",
"Several important points should be remembered:",
"Persistent cough despite treatment should prompt further diagnostic testing for lung mass.",
"Nonsmokers can develop lung cancer.",
"Neurologic symptoms in patients with lung cancer do not always mean brain metastasis. Although brain metastasis should be ruled out, other causes could be found, such as encephalomalacia.",
"Biopsy of recurrent cancer should be redone, especially if the time to recurrence is more than a few years. A separate cancer can be found in a patient previously cured of their cancer.",
"Several factors may increase the likelihood of a primary cancer resulting in a secondary cancer. A \"field effect\" is noted in certain types of cancers, particularly in the areas of respiratory tract. In smokers, this is especially true in such areas as the head and neck, throat, laryngeal, esophageal area, and tongue. Because the body's immune system is vulnerable to the development of the first cancer, it may be more susceptible to the development of a second cancer."
],
"date": "October 16, 2020",
"figures": [],
"markdown": "# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\n\n **Authors:** Winston W. Tan, MD; Matthew Tan \n **Date:** October 16, 2020\n\n ## Content\n\n The standard treatment for stage I and II disease is surgical resection. In stage IIIA, chemotherapy is indicated, as is surgical resection in selected patients. Standard treatment of stage IIIb is chemoradiation. Stage IV requires cisplatin-based chemotherapy or surgical resection if a solitary metastatic lesion with resectable primary tumor is present.[3,4,5]\nThis patient underwent resection of the cancer. Owing to her residual disease and because her lymph nodes were positive, she was treated with chemoradiation. Surgical resection is the primary modality of treatment for early stage non-small cell lung cancer.[6]\nClose surveillance of patients with cancer should be the standard after completion of therapy. This patient had a contralateral hilar recurrence 6 years later. When a patient has a recurrence, it must be determined whether it is the same cancer or another primary cancer. This patient had another primary cancer, specifically small cell cancer of the lung. Biopsy must be done of a new recurrence, because it could be an entirely different cancer.\nApproximately 60%-70% of patients with small cell lung cancer have clinically disseminated or extensive disease at presentation. Extensive-stage small cell lung cancer is incurable. When given combination chemotherapy, patients with extensive-stage disease have a complete response rate of more than 20% and a median survival longer than 7 months; however, only 2% are alive at 5 years.\nFor individuals with limited-stage disease that is treated with combination chemotherapy plus chest radiation, a complete response rate of 80% and survival of 17 months have been reported; 12%-15% of patients are alive at 5 years.[1]\nRecommendations from the National Comprehensive Cancer Network (NCCN) regarding cancer surveillance in survivors of non-small cell lung cancer include the following:\nHistory and physical examination, and chest CT with or without contrast, every 6-12 months for 2 years, then history and physical examination and noncontrast chest CT annually\nAssessment of smoking status at each visit, with counseling and referral for smoking cessation as needed\nOther NCCN recommendations for long-term follow-up care include the following:\nImmunization: Annual influenza vaccination, pneumococcal vaccination with revaccination as appropriate, herpes zoster vaccination\nCounseling regarding health promotion and wellness (eg, regular physical activity, healthy diet)\nRoutine health monitoring\nSeveral important points should be remembered:\nPersistent cough despite treatment should prompt further diagnostic testing for lung mass.\nNonsmokers can develop lung cancer.\nNeurologic symptoms in patients with lung cancer do not always mean brain metastasis. Although brain metastasis should be ruled out, other causes could be found, such as encephalomalacia.\nBiopsy of recurrent cancer should be redone, especially if the time to recurrence is more than a few years. A separate cancer can be found in a patient previously cured of their cancer.\nSeveral factors may increase the likelihood of a primary cancer resulting in a secondary cancer. A \"field effect\" is noted in certain types of cancers, particularly in the areas of respiratory tract. In smokers, this is especially true in such areas as the head and neck, throat, laryngeal, esophageal area, and tongue. Because the body's immune system is vulnerable to the development of the first cancer, it may be more susceptible to the development of a second cancer.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 831365,
"choiceText": "Adenocarcinoma",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831367,
"choiceText": "Squamous cell carcinoma",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831369,
"choiceText": "Large-cell carcinoma",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831371,
"choiceText": "None of the above\r\n",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The most common metabolic abnormality associated with non-small cell lung cancer is hypercalcemia, which usually occurs with squamous cell carcinoma and results from secretion of parathyroid hormone-related peptide by the tumor. This can be distinguished from hyperparathyroidism by confirmation of normal serum parathyroid hormone levels.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 261413,
"questionText": "Which of the following is most commonly associated with hypercalcemia in patients with non-small cell lung cancer?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 831373,
"choiceText": "Smoke exposure",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831375,
"choiceText": "Family history",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831377,
"choiceText": "Poor diet",
"correct": true,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831379,
"choiceText": "Chemical exposure",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Smoking is the most well-recognized risk factor for lung cancer. Even secondhand exposure carries a significant risk. In addition, exposure to certain gases (eg, radon), asbestos, and other chemicals may increase the risk for lung cancer. Likewise, a family history of lung cancer increases risk for the disease.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 261415,
"questionText": "Which of the following is <i>not</i> considered a primary risk factor for lung cancer?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old"
},
{
"authors": "Winston W. Tan, MD; Matthew Tan",
"content": [],
"date": "October 16, 2020",
"figures": [],
"markdown": "# Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old\n\n **Authors:** Winston W. Tan, MD; Matthew Tan \n **Date:** October 16, 2020\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 831365,
"choiceText": "Adenocarcinoma",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831367,
"choiceText": "Squamous cell carcinoma",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831369,
"choiceText": "Large-cell carcinoma",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831371,
"choiceText": "None of the above\r\n",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The most common metabolic abnormality associated with non-small cell lung cancer is hypercalcemia, which usually occurs with squamous cell carcinoma and results from secretion of parathyroid hormone-related peptide by the tumor. This can be distinguished from hyperparathyroidism by confirmation of normal serum parathyroid hormone levels.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 261413,
"questionText": "Which of the following is most commonly associated with hypercalcemia in patients with non-small cell lung cancer?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 831373,
"choiceText": "Smoke exposure",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831375,
"choiceText": "Family history",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831377,
"choiceText": "Poor diet",
"correct": true,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831379,
"choiceText": "Chemical exposure",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Smoking is the most well-recognized risk factor for lung cancer. Even secondhand exposure carries a significant risk. In addition, exposure to certain gases (eg, radon), asbestos, and other chemicals may increase the risk for lung cancer. Likewise, a family history of lung cancer increases risk for the disease.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 261415,
"questionText": "Which of the following is <i>not</i> considered a primary risk factor for lung cancer?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Antibiotic-Resistant Cough and Back Pain in a 63-Year-Old"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 831357,
"choiceText": "Sarcoidosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831359,
"choiceText": "Lung cancer",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831361,
"choiceText": "Tuberculosis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831363,
"choiceText": "Pneumonia \r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 261411,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 831365,
"choiceText": "Adenocarcinoma",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831367,
"choiceText": "Squamous cell carcinoma",
"correct": true,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831369,
"choiceText": "Large-cell carcinoma",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831371,
"choiceText": "None of the above\r\n",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "The most common metabolic abnormality associated with non-small cell lung cancer is hypercalcemia, which usually occurs with squamous cell carcinoma and results from secretion of parathyroid hormone-related peptide by the tumor. This can be distinguished from hyperparathyroidism by confirmation of normal serum parathyroid hormone levels.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 261413,
"questionText": "Which of the following is most commonly associated with hypercalcemia in patients with non-small cell lung cancer?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 831373,
"choiceText": "Smoke exposure",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831375,
"choiceText": "Family history",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831377,
"choiceText": "Poor diet",
"correct": true,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 831379,
"choiceText": "Chemical exposure",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Smoking is the most well-recognized risk factor for lung cancer. Even secondhand exposure carries a significant risk. In addition, exposure to certain gases (eg, radon), asbestos, and other chemicals may increase the risk for lung cancer. Likewise, a family history of lung cancer increases risk for the disease.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 261415,
"questionText": "Which of the following is <i>not</i> considered a primary risk factor for lung cancer?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
938423 | /viewarticle/938423 | [
{
"authors": "Timothy D. Murphy, MD",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us .",
"A 5-year-old girl with a long-standing history of severe asthma and eczema presented to a pediatric pulmonary and sleep medicine clinic. Her asthma was stabilized with an inhaled corticosteroid (fluticasone, 88 µg, inhaled twice daily), albuterol sulfate (180 µg, inhaled as needed), and ipratropium bromide (34 µg, inhaled as needed). Her skin condition improved with a moderately aggressive regimen of hydrating bleach baths, moisturizing lotions, nonsedating antihistamines, and as-needed use of topical hydrocortisone or triamcinolone, pimecrolimus, and mupirocin.",
"Her asthma remained stable for a year but then progressed to the extent that the dosage of inhaled fluticasone was increased to 220 µg twice daily. Bronchoscopy revealed only mild bronchomalacia of the left mainstem bronchus (Figure 1), diffuse mild inflammation, and increased secretions.",
"Figure 1.",
"Montelukast (5 mg daily) and nasal fluticasone (50 µg) were added to her regimen. In addition, diphenhydramine (25 mg) was prescribed to be used as needed for excessive itchiness, eczema flares, and allergic asthma flares.",
"The patient remained well and was followed up in the clinic approximately every 3 months, owing to the complexity of her condition. After 6 months, significant weight gain and an increasing body mass index (BMI) were noted. She met with a dietitian, who recommended weight loss strategies. From the age of 7-8 years, the patient demonstrated a modest weight loss from the changes in her diet. However, symptoms of fatigue, excessive daytime sleepiness (EDS), and inattention in school developed over a 1- to 2-month period, and her weight started to increase rapidly despite the dietary intervention.",
"Her daytime sleepiness seemed to be progressive, and she would fall asleep suddenly even when she wanted to be awake. Concerned about the emerging symptoms of inattention, autistic features, fatigue, and sleepiness, the girl's parents are seeking further medical advice."
],
"date": "October 09, 2020",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/938/423/938423-Thumb1.jpg"
}
],
"markdown": "# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\n\n **Authors:** Timothy D. Murphy, MD \n **Date:** October 09, 2020\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us .\nA 5-year-old girl with a long-standing history of severe asthma and eczema presented to a pediatric pulmonary and sleep medicine clinic. Her asthma was stabilized with an inhaled corticosteroid (fluticasone, 88 µg, inhaled twice daily), albuterol sulfate (180 µg, inhaled as needed), and ipratropium bromide (34 µg, inhaled as needed). Her skin condition improved with a moderately aggressive regimen of hydrating bleach baths, moisturizing lotions, nonsedating antihistamines, and as-needed use of topical hydrocortisone or triamcinolone, pimecrolimus, and mupirocin.\nHer asthma remained stable for a year but then progressed to the extent that the dosage of inhaled fluticasone was increased to 220 µg twice daily. Bronchoscopy revealed only mild bronchomalacia of the left mainstem bronchus (Figure 1), diffuse mild inflammation, and increased secretions.\nFigure 1.\nMontelukast (5 mg daily) and nasal fluticasone (50 µg) were added to her regimen. In addition, diphenhydramine (25 mg) was prescribed to be used as needed for excessive itchiness, eczema flares, and allergic asthma flares.\nThe patient remained well and was followed up in the clinic approximately every 3 months, owing to the complexity of her condition. After 6 months, significant weight gain and an increasing body mass index (BMI) were noted. She met with a dietitian, who recommended weight loss strategies. From the age of 7-8 years, the patient demonstrated a modest weight loss from the changes in her diet. However, symptoms of fatigue, excessive daytime sleepiness (EDS), and inattention in school developed over a 1- to 2-month period, and her weight started to increase rapidly despite the dietary intervention.\nHer daytime sleepiness seemed to be progressive, and she would fall asleep suddenly even when she wanted to be awake. Concerned about the emerging symptoms of inattention, autistic features, fatigue, and sleepiness, the girl's parents are seeking further medical advice.\n\n ## Figures\n\n **Figure 1.** \n \n\n\n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Rapid Weight Gain in an Excessively Sleepy Girl With Asthma"
},
{
"authors": "Timothy D. Murphy, MD",
"content": [
"The patient has fallen asleep at school nearly every day for the past 1-2 months and falls into a deep sleep unless she is kept active. At home, she is taking more naps during the day, falling asleep in the car, and struggling with schoolwork. Her grades have dropped significantly over the past few months. Her parents report that she does not awaken during the night. No snoring, choking, snorting, gasping, or apnea is noted. She sleeps an average of 9-10 hours per night but is restless and tosses and turns frequently in her sleep.",
"Her family history is notable for obesity, obstructive sleep apnea (OSA) that requires continuous positive airway pressure (CPAP) in her father, and narcolepsy in an uncle and a grandfather.",
"On physical examination, she has mild to moderate obesity (BMI of 23.89 kg/m2 [the 98th percentile for age]) and enlarged tonsils (2-3+). She has difficulty with focusing and staying awake in the clinic.",
"She is referred to a pediatric otolaryngologist for consideration of nocturnal polysomnography (NPSG) or an adenotonsillectomy. The otolaryngologist notes that she has not tolerated nasal fluticasone well, that she is a chronic mouth breather, and that her tonsils are enlarged (3+). An NPSG is ordered to help clarify matters.",
"The NPSG demonstrates the following:",
"A respiratory disturbance index and an apnea-hypopnea index (AHI) of 6.2 per hour",
"Sleep latency of 0.5 minutes and rapid eye movement (REM) latency of 0.5 minutes",
"A sleep efficiency of 87.5%",
"18.2% of total sleep time in stage N1, 36.4% in N2, 29.9% in N3, and 15.5% in REM sleep",
"An arousal index of 18.6",
"A periodic leg movement index of 6.3",
"Multiple periods of wakefulness scattered throughout the night and six REM periods"
],
"date": "October 09, 2020",
"figures": [],
"markdown": "# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\n\n **Authors:** Timothy D. Murphy, MD \n **Date:** October 09, 2020\n\n ## Content\n\n The patient has fallen asleep at school nearly every day for the past 1-2 months and falls into a deep sleep unless she is kept active. At home, she is taking more naps during the day, falling asleep in the car, and struggling with schoolwork. Her grades have dropped significantly over the past few months. Her parents report that she does not awaken during the night. No snoring, choking, snorting, gasping, or apnea is noted. She sleeps an average of 9-10 hours per night but is restless and tosses and turns frequently in her sleep.\nHer family history is notable for obesity, obstructive sleep apnea (OSA) that requires continuous positive airway pressure (CPAP) in her father, and narcolepsy in an uncle and a grandfather.\nOn physical examination, she has mild to moderate obesity (BMI of 23.89 kg/m2 [the 98th percentile for age]) and enlarged tonsils (2-3+). She has difficulty with focusing and staying awake in the clinic.\nShe is referred to a pediatric otolaryngologist for consideration of nocturnal polysomnography (NPSG) or an adenotonsillectomy. The otolaryngologist notes that she has not tolerated nasal fluticasone well, that she is a chronic mouth breather, and that her tonsils are enlarged (3+). An NPSG is ordered to help clarify matters.\nThe NPSG demonstrates the following:\nA respiratory disturbance index and an apnea-hypopnea index (AHI) of 6.2 per hour\nSleep latency of 0.5 minutes and rapid eye movement (REM) latency of 0.5 minutes\nA sleep efficiency of 87.5%\n18.2% of total sleep time in stage N1, 36.4% in N2, 29.9% in N3, and 15.5% in REM sleep\nAn arousal index of 18.6\nA periodic leg movement index of 6.3\nMultiple periods of wakefulness scattered throughout the night and six REM periods\n\n ## Figures\n\n \n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1529064,
"choiceText": "Behavioral insomnia of childhood\r\n",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529065,
"choiceText": "Pediatric chronic obstructive pulmonary disease",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529066,
"choiceText": "Delayed sleep phase disorder",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529067,
"choiceText": "Narcolepsy",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 490073,
"questionText": "On the basis of these findings only, what is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Rapid Weight Gain in an Excessively Sleepy Girl With Asthma"
},
{
"authors": "Timothy D. Murphy, MD",
"content": [
"This case is very challenging because the patient had the findings of and met the criteria for OSA, periodic limb movement disorder (PLMD)/restless legs syndrome (RLS), and hypersomnolence. She also had several historical findings that were highly suggestive of narcolepsy with cataplexy. These included a strong family history of narcolepsy, a history of the sudden onset of sleep and greatly increased sleep pressure, and rapid weight gain. A critical finding was a nocturnal sleep-onset REM sleep period (SOREMP). A nocturnal SOREMP (defined as REM sleep within 15 minutes of falling asleep) has a very high specificity for narcolepsy with cataplexy in adults and children.[1,2] However, the importance of the nocturnal SOREMP was not initially noted in her evaluation and management.",
"OSA and PLMD were initially diagnosed, and the otolaryngologist performed an adenotonsillectomy. The patient returned to the pediatric pulmonary and sleep medicine clinic after the procedure. At 3 weeks after the surgery, her somnolence improved very little. She had been gaining weight more rapidly and symptoms of apparent instability in her asthma were noted.",
"Further history-taking revealed a complex set of interactions around eating (some involved her father catering to her desire for higher-carbohydrate foods), increased sedentary behavior, and a history suggestive of vocal cord dysfunction. She was having \"asthma attacks\" characterized by rapid onset with inspiratory stridor and rapid resolution at the onset of activity. Her family was willing to make changes in their diet and to encourage activity, and they sought help for the vocal cord dysfunction from a speech and language pathologist.",
"Despite these measures, her weight gain rapidly progressed and the daytime fatigue and sleepiness continued. The pediatrician referred her to the neurologist who had interpreted the first NPSG. His history presented a differential diagnosis of narcolepsy, primary hypersomnolence, persistent OSA, and PLMD. He recommended a second NPSG with a multiple sleep latency test (MSLT), to be done immediately following the NPSG to assess her sleepiness more formally. His history documented that she felt as if she was \"going to fall\" when she laughed. He also noted that her father had OSA (treated with CPAP) and that she had an uncle and a grandfather with narcolepsy.",
"The second NPSG revealed the following:",
"A respiratory disturbance index of 1.4 (improved)",
"Sleep latency of 2.5 minutes and REM latency of 68.5 minutes",
"A sleep efficiency of 68.3%",
"31.6% of total sleep time in stage N1, 43.8% in N2, 20% in N3, and 4.6% in REM sleep",
"An arousal index of 23.5 (increased)",
"A periodic leg movement index of 5.9 (slightly lower)",
"\"3 REM periods, 2 of them were very brief,\" and a period of wakefulness after sleep onset of 180.5 minutes (increased)",
"The MSLT showed a mean sleep latency calculated at 9.5 minutes and no sleep onset–associated REM sleep (REM sleep within 20 minutes of sleep onset).",
"The neurologist provisionally diagnosed narcolepsy (vs hypersomnolence). He prescribed methylphenidate and then gradually increased the dose. Despite slightly improved daytime alertness, the patient started to develop more classic findings of cataplexy. The patient's mother brought her back to the pediatric pulmonary and sleep medicine clinic. Methylphenidate was discontinued and therapy with modafinil was initiated.",
"When the patient was 9 years old, sodium oxybate was added to her regimen and her condition finally stabilized. Her therapy was complicated by the treatment of her inattention with dextroamphetamine and levoamphetamine (Adderall) and the effects of all of her therapy on her weight. Her rapid weight gain was followed by an equally rapid weight loss, and these changes finally settled into her currently stable pattern of tracking around the 75th percentile after starting sodium oxybate (Figure 2).",
"Figure 2."
],
"date": "October 09, 2020",
"figures": [
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/938/423/938423-Thumb2.jpg"
}
],
"markdown": "# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\n\n **Authors:** Timothy D. Murphy, MD \n **Date:** October 09, 2020\n\n ## Content\n\n This case is very challenging because the patient had the findings of and met the criteria for OSA, periodic limb movement disorder (PLMD)/restless legs syndrome (RLS), and hypersomnolence. She also had several historical findings that were highly suggestive of narcolepsy with cataplexy. These included a strong family history of narcolepsy, a history of the sudden onset of sleep and greatly increased sleep pressure, and rapid weight gain. A critical finding was a nocturnal sleep-onset REM sleep period (SOREMP). A nocturnal SOREMP (defined as REM sleep within 15 minutes of falling asleep) has a very high specificity for narcolepsy with cataplexy in adults and children.[1,2] However, the importance of the nocturnal SOREMP was not initially noted in her evaluation and management.\nOSA and PLMD were initially diagnosed, and the otolaryngologist performed an adenotonsillectomy. The patient returned to the pediatric pulmonary and sleep medicine clinic after the procedure. At 3 weeks after the surgery, her somnolence improved very little. She had been gaining weight more rapidly and symptoms of apparent instability in her asthma were noted.\nFurther history-taking revealed a complex set of interactions around eating (some involved her father catering to her desire for higher-carbohydrate foods), increased sedentary behavior, and a history suggestive of vocal cord dysfunction. She was having \"asthma attacks\" characterized by rapid onset with inspiratory stridor and rapid resolution at the onset of activity. Her family was willing to make changes in their diet and to encourage activity, and they sought help for the vocal cord dysfunction from a speech and language pathologist.\nDespite these measures, her weight gain rapidly progressed and the daytime fatigue and sleepiness continued. The pediatrician referred her to the neurologist who had interpreted the first NPSG. His history presented a differential diagnosis of narcolepsy, primary hypersomnolence, persistent OSA, and PLMD. He recommended a second NPSG with a multiple sleep latency test (MSLT), to be done immediately following the NPSG to assess her sleepiness more formally. His history documented that she felt as if she was \"going to fall\" when she laughed. He also noted that her father had OSA (treated with CPAP) and that she had an uncle and a grandfather with narcolepsy.\nThe second NPSG revealed the following:\nA respiratory disturbance index of 1.4 (improved)\nSleep latency of 2.5 minutes and REM latency of 68.5 minutes\nA sleep efficiency of 68.3%\n31.6% of total sleep time in stage N1, 43.8% in N2, 20% in N3, and 4.6% in REM sleep\nAn arousal index of 23.5 (increased)\nA periodic leg movement index of 5.9 (slightly lower)\n\"3 REM periods, 2 of them were very brief,\" and a period of wakefulness after sleep onset of 180.5 minutes (increased)\nThe MSLT showed a mean sleep latency calculated at 9.5 minutes and no sleep onset–associated REM sleep (REM sleep within 20 minutes of sleep onset).\nThe neurologist provisionally diagnosed narcolepsy (vs hypersomnolence). He prescribed methylphenidate and then gradually increased the dose. Despite slightly improved daytime alertness, the patient started to develop more classic findings of cataplexy. The patient's mother brought her back to the pediatric pulmonary and sleep medicine clinic. Methylphenidate was discontinued and therapy with modafinil was initiated.\nWhen the patient was 9 years old, sodium oxybate was added to her regimen and her condition finally stabilized. Her therapy was complicated by the treatment of her inattention with dextroamphetamine and levoamphetamine (Adderall) and the effects of all of her therapy on her weight. Her rapid weight gain was followed by an equally rapid weight loss, and these changes finally settled into her currently stable pattern of tracking around the 75th percentile after starting sodium oxybate (Figure 2).\nFigure 2.\n\n ## Figures\n\n **Figure 2.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1529064,
"choiceText": "Behavioral insomnia of childhood\r\n",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529065,
"choiceText": "Pediatric chronic obstructive pulmonary disease",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529066,
"choiceText": "Delayed sleep phase disorder",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529067,
"choiceText": "Narcolepsy",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 490073,
"questionText": "On the basis of these findings only, what is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Rapid Weight Gain in an Excessively Sleepy Girl With Asthma"
},
{
"authors": "Timothy D. Murphy, MD",
"content": [
"This case illustrates some of the challenges facing clinicians who care for a \"sleepy child.\" In the evolution of this child's care, multiple diagnoses were made and treated. The failure of her symptoms to respond to treatment resulted in further evaluation (and reevaluation of the data), which finally led to the diagnosis (narcolepsy with cataplexy) and her ultimate improvement and stabilization.",
"Hypersomnolence may be primary or it may be secondary to a poor night's sleep. The most common conditions seen in a pediatric sleep clinic that might lead to daytime sleepiness include sleep apnea, behavioral insomnia of childhood, restless sleeping (or, when more extreme, pediatric RLS), and delayed sleep phase disorder (DSPD). The latter is much more common in teenagers, with a prevalence of up to 7% in this age group.[3] However, youths with daytime hypersomnolence due to DSPD do not typically fall asleep easily at bedtime, as this patient did. Moreover, DSPD is unusual in an 8-year-old.",
"An insufficient quantity of sleep can usually be diagnosed on the basis of the history alone, but actigraphy is occasionally used when the history does not exclude difficulty in falling asleep or a circadian rhythm sleep-wake disorder.[4] Actigraphy was not included in this patient's workup.",
"Pediatric RLS is primarily diagnosed on the basis of history, but the use of strict criteria (which include that the child \"relates a description in his or her own words\" of leg discomfort) may lead to missing the diagnosis in children who can benefit from treatment but are unable to verbalize their feelings. Suboptimal levels of serum ferritin are associated with restless sleep in children, as is improvement with iron therapy. The use of dopaminergic medications typically requires a higher standard for the diagnosis of RLS and a failure to respond to iron therapy.[5,6] Published data regarding autism and attention-deficit/hyperactivity disorder (ADHD) increasingly suggest complex links between iron metabolism and brain function, including during sleep.[7,8] This patient's movements in bed and her behavioral and learning struggles led to the investigation of her iron stores and ferritin levels and a trial of treatment for RLS.",
"Hypersomnolence is associated with OSA more commonly in adults than in children. \"Hyperactivity\" or symptoms of ADHD are more frequently observed in children with OSA, although some sleepiness is still noted.[9] Most sleep centers consider an obstructive AHI of fewer than 1 event per hour (some use a threshold of 1.5) to be normal.[10] More pragmatically, the absolute score is useful in choosing a diagnostic billing code, but clinical decision-making also factors in the age of the patient and the severity of observed symptoms, considered formally or as a gestalt.[11]",
"This patient had a positive AHI, which is diagnostic of OSA, and underwent adenotonsillectomy without significant improvement. She was also treated with iron and vitamin C, without significant changes in her daytime sleepiness or her apparent sleep quality. Furthermore, her clinical care was complicated by the MSLT result, which documented hypersomnolence but not narcolepsy.",
"The diagnosis of narcolepsy was based primarily on clinical factors. Despite the positive AHI, snoring, leg movements, and low ferritin level, her condition did not improve after the adenotonsillectomy and iron therapy. As her case progressed, she developed more classic symptoms of cataplexy, such as feeling as if she would fall with laughter and falling asleep rapidly in conjunction with strong emotions. These findings, along with the rapid weight gain, pointed toward the diagnosis.",
"Some confusion along the path toward a diagnosis is common in narcolepsy. Comorbidities, including PLMD, RLS, and OSA, may be found in association with narcolepsy and can delay the diagnosis,[12] as certainly happened in this patient.",
"Narcolepsy affects about 1 in 2000 people. Two types are recognized: type 1 narcolepsy (previously referred to as narcolepsy with cataplexy) and type 2 narcolepsy (narcolepsy without cataplexy). Type 1 narcolepsy is considered an adult diagnosis by many pediatricians, but it frequently develops during adolescence, and onset after age 40 years is uncommon. Children may first present with a resumption of prolonged naps rather than prolonged nighttime sleep; nocturnal sleep is often somewhat disturbed initially. Cataplexy, multiple short naps during the day, hypnagogic hallucinations, and sleep-onset REM periods may be absent in young children, and repeated NPSGs and MSLTs over months to years may be required to make the diagnosis.",
"Although a retrospective analysis of sleep histories often reveals hypersomnolence for years prior to the diagnosis, it can be easily missed in the first decade of life.[13] Type 1 narcolepsy is caused by the loss of orexin neuropeptides, which are mediators of central nervous system (CNS) control of energy metabolism and maintenance of sleep-wake states. Rapid weight gain and precocious puberty can occur in children with type 1 narcolepsy. This patient's rapid weight gain started to make more sense once the diagnosis was made.[14]",
"In type 1 narcolepsy, the lack of consistent REM sleep at night leads to the intrusion of REM sleep features into the waking state. The diagnostic features include the tetrad of daytime sleepiness, cataplexy, hypnagogic hallucinations, and sleep paralysis. Specific questioning is usually required to elicit the history; only cataplexy is specific for narcolepsy. Patients often present initially with hypersomnolence alone, and other diagnostic findings may emerge over time.",
"The etiology of narcolepsy is unclear. The lack of orexin may be related to autoimmune disease or infectious diseases. Most patients with type 1 narcolepsy have HLA DQB1 (0602 allele), the gene complex that encodes for proteins on the surface of T cells. Additionally, some infections (most notably H1N1 influenza, as well as some vaccines for it) are associated with clusters of type 1 narcolepsy and reduced orexin levels.[15,16,17] However, measurement of cerebrospinal fluid (CSF) levels of orexin is not required to make the diagnosis of narcolepsy.",
"The diagnosis of type 1 narcolepsy can be clinically made in a child with a clear history of cataplexy, EDS, and an otherwise normal neurologic examination. In the absence of cataplexy, an NPSG followed by an MSLT can be used to make the diagnosis of narcolepsy. \"Secondary narcolepsy\" in the setting of CNS diseases such as hypothalamic tumors or arteriovenous malformations, following cerebrovascular accidents, or in association with multiple sclerosis or Niemann-Pick disease type C has been reported, but alternative causes of narcolepsy are vanishingly rare in childhood. The primary challenge is to rule out other sleep disorders causing the EDS; as in this patient, that may be difficult."
],
"date": "October 09, 2020",
"figures": [],
"markdown": "# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\n\n **Authors:** Timothy D. Murphy, MD \n **Date:** October 09, 2020\n\n ## Content\n\n This case illustrates some of the challenges facing clinicians who care for a \"sleepy child.\" In the evolution of this child's care, multiple diagnoses were made and treated. The failure of her symptoms to respond to treatment resulted in further evaluation (and reevaluation of the data), which finally led to the diagnosis (narcolepsy with cataplexy) and her ultimate improvement and stabilization.\nHypersomnolence may be primary or it may be secondary to a poor night's sleep. The most common conditions seen in a pediatric sleep clinic that might lead to daytime sleepiness include sleep apnea, behavioral insomnia of childhood, restless sleeping (or, when more extreme, pediatric RLS), and delayed sleep phase disorder (DSPD). The latter is much more common in teenagers, with a prevalence of up to 7% in this age group.[3] However, youths with daytime hypersomnolence due to DSPD do not typically fall asleep easily at bedtime, as this patient did. Moreover, DSPD is unusual in an 8-year-old.\nAn insufficient quantity of sleep can usually be diagnosed on the basis of the history alone, but actigraphy is occasionally used when the history does not exclude difficulty in falling asleep or a circadian rhythm sleep-wake disorder.[4] Actigraphy was not included in this patient's workup.\nPediatric RLS is primarily diagnosed on the basis of history, but the use of strict criteria (which include that the child \"relates a description in his or her own words\" of leg discomfort) may lead to missing the diagnosis in children who can benefit from treatment but are unable to verbalize their feelings. Suboptimal levels of serum ferritin are associated with restless sleep in children, as is improvement with iron therapy. The use of dopaminergic medications typically requires a higher standard for the diagnosis of RLS and a failure to respond to iron therapy.[5,6] Published data regarding autism and attention-deficit/hyperactivity disorder (ADHD) increasingly suggest complex links between iron metabolism and brain function, including during sleep.[7,8] This patient's movements in bed and her behavioral and learning struggles led to the investigation of her iron stores and ferritin levels and a trial of treatment for RLS.\nHypersomnolence is associated with OSA more commonly in adults than in children. \"Hyperactivity\" or symptoms of ADHD are more frequently observed in children with OSA, although some sleepiness is still noted.[9] Most sleep centers consider an obstructive AHI of fewer than 1 event per hour (some use a threshold of 1.5) to be normal.[10] More pragmatically, the absolute score is useful in choosing a diagnostic billing code, but clinical decision-making also factors in the age of the patient and the severity of observed symptoms, considered formally or as a gestalt.[11]\nThis patient had a positive AHI, which is diagnostic of OSA, and underwent adenotonsillectomy without significant improvement. She was also treated with iron and vitamin C, without significant changes in her daytime sleepiness or her apparent sleep quality. Furthermore, her clinical care was complicated by the MSLT result, which documented hypersomnolence but not narcolepsy.\nThe diagnosis of narcolepsy was based primarily on clinical factors. Despite the positive AHI, snoring, leg movements, and low ferritin level, her condition did not improve after the adenotonsillectomy and iron therapy. As her case progressed, she developed more classic symptoms of cataplexy, such as feeling as if she would fall with laughter and falling asleep rapidly in conjunction with strong emotions. These findings, along with the rapid weight gain, pointed toward the diagnosis.\nSome confusion along the path toward a diagnosis is common in narcolepsy. Comorbidities, including PLMD, RLS, and OSA, may be found in association with narcolepsy and can delay the diagnosis,[12] as certainly happened in this patient.\nNarcolepsy affects about 1 in 2000 people. Two types are recognized: type 1 narcolepsy (previously referred to as narcolepsy with cataplexy) and type 2 narcolepsy (narcolepsy without cataplexy). Type 1 narcolepsy is considered an adult diagnosis by many pediatricians, but it frequently develops during adolescence, and onset after age 40 years is uncommon. Children may first present with a resumption of prolonged naps rather than prolonged nighttime sleep; nocturnal sleep is often somewhat disturbed initially. Cataplexy, multiple short naps during the day, hypnagogic hallucinations, and sleep-onset REM periods may be absent in young children, and repeated NPSGs and MSLTs over months to years may be required to make the diagnosis.\nAlthough a retrospective analysis of sleep histories often reveals hypersomnolence for years prior to the diagnosis, it can be easily missed in the first decade of life.[13] Type 1 narcolepsy is caused by the loss of orexin neuropeptides, which are mediators of central nervous system (CNS) control of energy metabolism and maintenance of sleep-wake states. Rapid weight gain and precocious puberty can occur in children with type 1 narcolepsy. This patient's rapid weight gain started to make more sense once the diagnosis was made.[14]\nIn type 1 narcolepsy, the lack of consistent REM sleep at night leads to the intrusion of REM sleep features into the waking state. The diagnostic features include the tetrad of daytime sleepiness, cataplexy, hypnagogic hallucinations, and sleep paralysis. Specific questioning is usually required to elicit the history; only cataplexy is specific for narcolepsy. Patients often present initially with hypersomnolence alone, and other diagnostic findings may emerge over time.\nThe etiology of narcolepsy is unclear. The lack of orexin may be related to autoimmune disease or infectious diseases. Most patients with type 1 narcolepsy have HLA DQB1 (0602 allele), the gene complex that encodes for proteins on the surface of T cells. Additionally, some infections (most notably H1N1 influenza, as well as some vaccines for it) are associated with clusters of type 1 narcolepsy and reduced orexin levels.[15,16,17] However, measurement of cerebrospinal fluid (CSF) levels of orexin is not required to make the diagnosis of narcolepsy.\nThe diagnosis of type 1 narcolepsy can be clinically made in a child with a clear history of cataplexy, EDS, and an otherwise normal neurologic examination. In the absence of cataplexy, an NPSG followed by an MSLT can be used to make the diagnosis of narcolepsy. \"Secondary narcolepsy\" in the setting of CNS diseases such as hypothalamic tumors or arteriovenous malformations, following cerebrovascular accidents, or in association with multiple sclerosis or Niemann-Pick disease type C has been reported, but alternative causes of narcolepsy are vanishingly rare in childhood. The primary challenge is to rule out other sleep disorders causing the EDS; as in this patient, that may be difficult.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Rapid Weight Gain in an Excessively Sleepy Girl With Asthma"
},
{
"authors": "Timothy D. Murphy, MD",
"content": [
"The treatment of narcolepsy focuses first on attempts to reduce the EDS pharmacologically; timed naps or increased time in bed is not usually sufficient to reduce the EDS. Although many medications have been used to treat EDS, clinicians typically start with caffeine (usually inadequate) and then move to stronger stimulants, such as methylphenidate or amphetamine and dextroamphetamine in combination.",
"Failure of these agents might then lead to the use of modafinil (prescription without the failure of other therapies is often difficult). Monitoring of response and fairly frequent visits are required at this point. A selective serotonin reuptake inhibitor, such as fluoxetine, is often added to the regimen of patients with classic cataplexy. As was the case for this patient, the use of medications that might affect mood, attention, learning, and sleep requires close attention and collaboration between specialists in sleep medicine, neurology, and behavioral and general pediatrics.",
"In some patients, including this patient, sodium oxybate (gamma-hydroxybutyrate [GHB]) is required to treat the cataplexy and to lead to better daytime functioning.[18] The exact mechanism of action is unknown, but the evening dosing of GHB is associated with improved REM sleep at night, perhaps relieving the intrusion of REM during daytime wake periods associated with type 1 narcolepsy. Unfortunately, GHB is associated with abuse — it is often called the \"date rape drug\" — and is now tightly regulated. Prescription in the United States is limited to one US pharmacy, and a sleep physician is typically required to obtain and use this medication.",
"The finding of EDS requires exploration of nocturnal problems with sleep, including RLS, OSA, and behavioral insomnia that affects daytime functioning. Narcolepsy can be diagnosed as the cause of EDS on the basis of careful history-taking as well as the results of an NPSG and an MSLT."
],
"date": "October 09, 2020",
"figures": [],
"markdown": "# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\n\n **Authors:** Timothy D. Murphy, MD \n **Date:** October 09, 2020\n\n ## Content\n\n The treatment of narcolepsy focuses first on attempts to reduce the EDS pharmacologically; timed naps or increased time in bed is not usually sufficient to reduce the EDS. Although many medications have been used to treat EDS, clinicians typically start with caffeine (usually inadequate) and then move to stronger stimulants, such as methylphenidate or amphetamine and dextroamphetamine in combination.\nFailure of these agents might then lead to the use of modafinil (prescription without the failure of other therapies is often difficult). Monitoring of response and fairly frequent visits are required at this point. A selective serotonin reuptake inhibitor, such as fluoxetine, is often added to the regimen of patients with classic cataplexy. As was the case for this patient, the use of medications that might affect mood, attention, learning, and sleep requires close attention and collaboration between specialists in sleep medicine, neurology, and behavioral and general pediatrics.\nIn some patients, including this patient, sodium oxybate (gamma-hydroxybutyrate [GHB]) is required to treat the cataplexy and to lead to better daytime functioning.[18] The exact mechanism of action is unknown, but the evening dosing of GHB is associated with improved REM sleep at night, perhaps relieving the intrusion of REM during daytime wake periods associated with type 1 narcolepsy. Unfortunately, GHB is associated with abuse — it is often called the \"date rape drug\" — and is now tightly regulated. Prescription in the United States is limited to one US pharmacy, and a sleep physician is typically required to obtain and use this medication.\nThe finding of EDS requires exploration of nocturnal problems with sleep, including RLS, OSA, and behavioral insomnia that affects daytime functioning. Narcolepsy can be diagnosed as the cause of EDS on the basis of careful history-taking as well as the results of an NPSG and an MSLT.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1529068,
"choiceText": "Narcolepsy without cataplexy (type 2 narcolepsy) is associated with increased orexin neuropeptide levels",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529069,
"choiceText": "Childhood narcolepsy is characterized by multiple brief naps during the day",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529070,
"choiceText": "Narcolepsy is associated with the loss of orexin neuropeptides",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529071,
"choiceText": "Measurement of orexin levels in the CSF is required for the diagnosis of narcolepsy",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Levels of orexin neuropeptides in the CNS are reduced, not increased, in all forms of narcolepsy. Children more frequently present with prolonged daytime sleep, and multiple naps are typically seen in older patients. The diagnosis can be made by a careful history-taking that documents cataplexy, which is explained only by type 1 narcolepsy. Measurement of CSF levels of orexin is usually related to research only and typically is not used clinically in diagnosing narcolepsy.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 490074,
"questionText": "Which of the following is most accurate regarding narcolepsy in children?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1529072,
"choiceText": "Timed or planned naps to reduce sleep pressure, and amphetamine and dextroamphetamine for stimulant therapy during the day\r\n",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529073,
"choiceText": "Modafinil as a daytime stimulant, fluoxetine for cataplexy, and sodium oxybate to improve REM efficiency",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529074,
"choiceText": "Caffeine as a morning stimulant and sodium oxybate (gamma-hydroxybutyrate [GHB]) used at night to consolidate non-REM sleep",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529075,
"choiceText": "Methylphenidate to reduce cataplexy, fluoxetine to reduce depressive symptoms, and sodium oxybate to prolong REM latency",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Caffeine is usually an inadequate stimulant for patients with narcolepsy. The daytime use of methylphenidate or amphetamine and dextroamphetamine in combination does not adequately reduce cataplexy and does not address the problem with REM sleep at night. Modafinil is a more reliable daytime stimulant, and fluoxetine helps reduce cataplexy. The use of sodium oxybate in the evening in divided doses is intended to consolidate REM sleep and may reduce REM latency; non-REM sleep is not related to the daytime difficulties associated with narcolepsy.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 490075,
"questionText": "Which of the following is typically required in the treatment of type 1 narcolepsy?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Rapid Weight Gain in an Excessively Sleepy Girl With Asthma"
},
{
"authors": "Timothy D. Murphy, MD",
"content": [],
"date": "October 09, 2020",
"figures": [],
"markdown": "# Rapid Weight Gain in an Excessively Sleepy Girl With Asthma\n\n **Authors:** Timothy D. Murphy, MD \n **Date:** October 09, 2020\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1529068,
"choiceText": "Narcolepsy without cataplexy (type 2 narcolepsy) is associated with increased orexin neuropeptide levels",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529069,
"choiceText": "Childhood narcolepsy is characterized by multiple brief naps during the day",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529070,
"choiceText": "Narcolepsy is associated with the loss of orexin neuropeptides",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529071,
"choiceText": "Measurement of orexin levels in the CSF is required for the diagnosis of narcolepsy",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Levels of orexin neuropeptides in the CNS are reduced, not increased, in all forms of narcolepsy. Children more frequently present with prolonged daytime sleep, and multiple naps are typically seen in older patients. The diagnosis can be made by a careful history-taking that documents cataplexy, which is explained only by type 1 narcolepsy. Measurement of CSF levels of orexin is usually related to research only and typically is not used clinically in diagnosing narcolepsy.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 490074,
"questionText": "Which of the following is most accurate regarding narcolepsy in children?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1529072,
"choiceText": "Timed or planned naps to reduce sleep pressure, and amphetamine and dextroamphetamine for stimulant therapy during the day\r\n",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529073,
"choiceText": "Modafinil as a daytime stimulant, fluoxetine for cataplexy, and sodium oxybate to improve REM efficiency",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529074,
"choiceText": "Caffeine as a morning stimulant and sodium oxybate (gamma-hydroxybutyrate [GHB]) used at night to consolidate non-REM sleep",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529075,
"choiceText": "Methylphenidate to reduce cataplexy, fluoxetine to reduce depressive symptoms, and sodium oxybate to prolong REM latency",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Caffeine is usually an inadequate stimulant for patients with narcolepsy. The daytime use of methylphenidate or amphetamine and dextroamphetamine in combination does not adequately reduce cataplexy and does not address the problem with REM sleep at night. Modafinil is a more reliable daytime stimulant, and fluoxetine helps reduce cataplexy. The use of sodium oxybate in the evening in divided doses is intended to consolidate REM sleep and may reduce REM latency; non-REM sleep is not related to the daytime difficulties associated with narcolepsy.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 490075,
"questionText": "Which of the following is typically required in the treatment of type 1 narcolepsy?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Rapid Weight Gain in an Excessively Sleepy Girl With Asthma"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1529064,
"choiceText": "Behavioral insomnia of childhood\r\n",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529065,
"choiceText": "Pediatric chronic obstructive pulmonary disease",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529066,
"choiceText": "Delayed sleep phase disorder",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529067,
"choiceText": "Narcolepsy",
"correct": true,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 490073,
"questionText": "On the basis of these findings only, what is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1529068,
"choiceText": "Narcolepsy without cataplexy (type 2 narcolepsy) is associated with increased orexin neuropeptide levels",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529069,
"choiceText": "Childhood narcolepsy is characterized by multiple brief naps during the day",
"correct": false,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529070,
"choiceText": "Narcolepsy is associated with the loss of orexin neuropeptides",
"correct": true,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529071,
"choiceText": "Measurement of orexin levels in the CSF is required for the diagnosis of narcolepsy",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Levels of orexin neuropeptides in the CNS are reduced, not increased, in all forms of narcolepsy. Children more frequently present with prolonged daytime sleep, and multiple naps are typically seen in older patients. The diagnosis can be made by a careful history-taking that documents cataplexy, which is explained only by type 1 narcolepsy. Measurement of CSF levels of orexin is usually related to research only and typically is not used clinically in diagnosing narcolepsy.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 490074,
"questionText": "Which of the following is most accurate regarding narcolepsy in children?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1529072,
"choiceText": "Timed or planned naps to reduce sleep pressure, and amphetamine and dextroamphetamine for stimulant therapy during the day\r\n",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529073,
"choiceText": "Modafinil as a daytime stimulant, fluoxetine for cataplexy, and sodium oxybate to improve REM efficiency",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529074,
"choiceText": "Caffeine as a morning stimulant and sodium oxybate (gamma-hydroxybutyrate [GHB]) used at night to consolidate non-REM sleep",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1529075,
"choiceText": "Methylphenidate to reduce cataplexy, fluoxetine to reduce depressive symptoms, and sodium oxybate to prolong REM latency",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Caffeine is usually an inadequate stimulant for patients with narcolepsy. The daytime use of methylphenidate or amphetamine and dextroamphetamine in combination does not adequately reduce cataplexy and does not address the problem with REM sleep at night. Modafinil is a more reliable daytime stimulant, and fluoxetine helps reduce cataplexy. The use of sodium oxybate in the evening in divided doses is intended to consolidate REM sleep and may reduce REM latency; non-REM sleep is not related to the daytime difficulties associated with narcolepsy.",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 490075,
"questionText": "Which of the following is typically required in the treatment of type 1 narcolepsy?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
904350 | /viewarticle/904350 | [
{
"authors": "Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO",
"content": [
"Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.",
"A 49-year-old man with a significant medical history of alcohol abuse, tobacco dependence, and pancreatitis presents to the emergency department (ED) with abdominal pain that has lasted for 3 days. The abdominal pain has been intermittent, achy, and located in the periumbilical region. Associated symptoms have included nausea and vomiting, with several episodes of watery, brown diarrhea.",
"The patient reports a history of alcohol abuse, stating that he has ingested at least 1 pint a day since he was a teenager. He states that this pain feels different from the pain associated with his last bout of pancreatitis."
],
"date": "October 02, 2020",
"figures": [],
"markdown": "# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\n\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \n **Date:** October 02, 2020\n\n ## Content\n\n Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.\nA 49-year-old man with a significant medical history of alcohol abuse, tobacco dependence, and pancreatitis presents to the emergency department (ED) with abdominal pain that has lasted for 3 days. The abdominal pain has been intermittent, achy, and located in the periumbilical region. Associated symptoms have included nausea and vomiting, with several episodes of watery, brown diarrhea.\nThe patient reports a history of alcohol abuse, stating that he has ingested at least 1 pint a day since he was a teenager. He states that this pain feels different from the pain associated with his last bout of pancreatitis.\n\n ## Figures\n\n \n*Page 1 of 6*",
"pagination": {
"current_page": 1,
"total_pages": 6
},
"questionnaire": [],
"title": "Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old"
},
{
"authors": "Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO",
"content": [
"Upon arrival to the ED, the patient has a temperature of 97.9°F (36.6°C), a heart rate of 91 beats/min, a respiratory rate of 23 breaths/min, blood pressure of 113/85 mm Hg, and 98% saturation on room air.",
"Upon physical examination, he appears uncomfortable and is lying on his right side; he is slightly diaphoretic, with dry oral mucosa. Abdominal examination reveals a soft abdomen with apparent tenderness to palpation in the epigastric and periumbilical region, with minimal left upper-quadrant pain. His abdominal pain appears out of proportion to the physical examination findings.",
"His laboratory values are as follows:",
"White blood cell count: 13,000 cells/µL (reference range, 4,000-11,000 cells/µL)",
"Hemoglobin level: 14.1 g/dL (reference range, 13.5-17.5 g/dL)",
"Hematocrit: 39% (reference range, 41%-50%)",
"Platelet count: 506,000 cells/µL (reference range, 150,000-400,000 cells/µL)",
"Aspartate aminotransferase level: 126 U/L (reference range, 6-34 IU/L)",
"Alanine aminotransferase level: 81 U/L (reference range, 7-55 U/L)",
"Amylase level: 125 U/L (reference range, 30-110 U/L)",
"Lipase level: 419 U/L (reference range, 0-160 U/L)",
"Gamma glutamyltransferase level: 58 U/L (reference range, 8-38 U/L)",
"Lactate dehydrogenase level: 175 U/L (reference range, 140-280 U/L)",
"Lactic acid level: 0.7 mmol/L (reference range, 0.5-2.2 mmol/L)",
"Glucose level: 102 mg/dL (reference range, <100 mg/dL)",
"Rectal examination findings are negative for occult blood. All other laboratory values are unremarkable, including alcohol level. Subsequent CT of the abdomen/pelvis with intravenous contrast was performed (Figures 1-3).",
"Figure 1.",
"Figure 2.",
"Figure 3."
],
"date": "October 02, 2020",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/904/350/904350-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/904/350/904350-Thumb2.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/904/350/904350-Thumb3.png"
}
],
"markdown": "# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\n\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \n **Date:** October 02, 2020\n\n ## Content\n\n Upon arrival to the ED, the patient has a temperature of 97.9°F (36.6°C), a heart rate of 91 beats/min, a respiratory rate of 23 breaths/min, blood pressure of 113/85 mm Hg, and 98% saturation on room air.\nUpon physical examination, he appears uncomfortable and is lying on his right side; he is slightly diaphoretic, with dry oral mucosa. Abdominal examination reveals a soft abdomen with apparent tenderness to palpation in the epigastric and periumbilical region, with minimal left upper-quadrant pain. His abdominal pain appears out of proportion to the physical examination findings.\nHis laboratory values are as follows:\nWhite blood cell count: 13,000 cells/µL (reference range, 4,000-11,000 cells/µL)\nHemoglobin level: 14.1 g/dL (reference range, 13.5-17.5 g/dL)\nHematocrit: 39% (reference range, 41%-50%)\nPlatelet count: 506,000 cells/µL (reference range, 150,000-400,000 cells/µL)\nAspartate aminotransferase level: 126 U/L (reference range, 6-34 IU/L)\nAlanine aminotransferase level: 81 U/L (reference range, 7-55 U/L)\nAmylase level: 125 U/L (reference range, 30-110 U/L)\nLipase level: 419 U/L (reference range, 0-160 U/L)\nGamma glutamyltransferase level: 58 U/L (reference range, 8-38 U/L)\nLactate dehydrogenase level: 175 U/L (reference range, 140-280 U/L)\nLactic acid level: 0.7 mmol/L (reference range, 0.5-2.2 mmol/L)\nGlucose level: 102 mg/dL (reference range, <100 mg/dL)\nRectal examination findings are negative for occult blood. All other laboratory values are unremarkable, including alcohol level. Subsequent CT of the abdomen/pelvis with intravenous contrast was performed (Figures 1-3).\nFigure 1.\nFigure 2.\nFigure 3.\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n\n*Page 2 of 6*",
"pagination": {
"current_page": 2,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1281940,
"choiceText": "Splenic vein thrombosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281942,
"choiceText": "Superior mesenteric vein thrombosis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281944,
"choiceText": "Mesenteric arterial thrombosis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281946,
"choiceText": "Septic pylephlebitis\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 408509,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old"
},
{
"authors": "Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO",
"content": [
"Acute mesenteric vein thrombosis (MVT) is a rare but extremely important cause of mesenteric intestinal ischemia. In this patient, CT of the abdomen/pelvis with intravenous contrast revealed a filling defect that was consistent with acute thrombosis within the superior mesenteric vein (SMV), which extends approximately 3 cm cephalad to the portosplenic confluence. Other associated findings on these images included peripancreatic fat stranding and peripancreatic fluid consistent with acute pancreatitis (Figures 1-3).",
"Figure 1.",
"Figure 2.",
"Figure 3.",
"Pancreatitis results in a vast spectrum of both arterial and venous complications. The vascular complications involved in pancreatitis are major causes of morbidity and mortality. The venous complications result from thrombosis of the splenic vein and, less commonly, the portal vein and the SMV, as seen in the patient in this case. Prompt recognition is of paramount importance and requires a high index of clinical suspicion because aggressive therapy and anticoagulation can limit progression of the potential devastating consequences.",
"Patients with acute pancreatitis can present with portal vein thrombosis, splenic vein thrombosis, or (less commonly) superior MVT. Clinical research has shown that an isolated venous thrombosis to only the SMV, without simultaneous involvement of either the portal vein or the splenic vein, is rare. This vascular complication is important because of the increased risk for mesenteric ischemia and bowel infarction if not recognized.[1]",
"MVT is considered a rare condition, with only 1 case per 5000-15000 inpatient admissions per year; it accounts for roughly 6%-9% of all cases of acute mesenteric ischemia.[2] In a systematic review of 3692 patients from 1966 to 2002, MVT was the cause of acute mesenteric ischemia in about 3% of patients.[3]"
],
"date": "October 02, 2020",
"figures": [
{
"caption": "Figure 1.",
"image_url": "https://img.medscapestatic.com/article/904/350/904350-Thumb1.png"
},
{
"caption": "Figure 2.",
"image_url": "https://img.medscapestatic.com/article/904/350/904350-Thumb2.png"
},
{
"caption": "Figure 3.",
"image_url": "https://img.medscapestatic.com/article/904/350/904350-Thumb3.png"
}
],
"markdown": "# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\n\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \n **Date:** October 02, 2020\n\n ## Content\n\n Acute mesenteric vein thrombosis (MVT) is a rare but extremely important cause of mesenteric intestinal ischemia. In this patient, CT of the abdomen/pelvis with intravenous contrast revealed a filling defect that was consistent with acute thrombosis within the superior mesenteric vein (SMV), which extends approximately 3 cm cephalad to the portosplenic confluence. Other associated findings on these images included peripancreatic fat stranding and peripancreatic fluid consistent with acute pancreatitis (Figures 1-3).\nFigure 1.\nFigure 2.\nFigure 3.\nPancreatitis results in a vast spectrum of both arterial and venous complications. The vascular complications involved in pancreatitis are major causes of morbidity and mortality. The venous complications result from thrombosis of the splenic vein and, less commonly, the portal vein and the SMV, as seen in the patient in this case. Prompt recognition is of paramount importance and requires a high index of clinical suspicion because aggressive therapy and anticoagulation can limit progression of the potential devastating consequences.\nPatients with acute pancreatitis can present with portal vein thrombosis, splenic vein thrombosis, or (less commonly) superior MVT. Clinical research has shown that an isolated venous thrombosis to only the SMV, without simultaneous involvement of either the portal vein or the splenic vein, is rare. This vascular complication is important because of the increased risk for mesenteric ischemia and bowel infarction if not recognized.[1]\nMVT is considered a rare condition, with only 1 case per 5000-15000 inpatient admissions per year; it accounts for roughly 6%-9% of all cases of acute mesenteric ischemia.[2] In a systematic review of 3692 patients from 1966 to 2002, MVT was the cause of acute mesenteric ischemia in about 3% of patients.[3]\n\n ## Figures\n\n **Figure 1.** \n \n\n**Figure 2.** \n \n\n**Figure 3.** \n \n\n\n*Page 3 of 6*",
"pagination": {
"current_page": 3,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1281940,
"choiceText": "Splenic vein thrombosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281942,
"choiceText": "Superior mesenteric vein thrombosis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281944,
"choiceText": "Mesenteric arterial thrombosis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281946,
"choiceText": "Septic pylephlebitis\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 408509,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old"
},
{
"authors": "Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO",
"content": [
"Many risk factors for MVT are recognized, including direct injury (eg, abdominal trauma, splenectomy, intra-abdominal inflammatory processes), venous congestion/stasis (eg, congestive heart failure, portal hypertension, cirrhosis), and hypercoagulable conditions (eg, protein C/S deficiency, antithrombin III deficiency, factor V Leiden mutation, pancreatic/colon carcinoma, oral contraceptive use, polycythemia vera, heparin-induced thrombocytopenia, lupus anticoagulant/anti-phospholipid syndrome).[4] In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.[5]",
"Acute occlusion of the mesenteric vein results in increased resistance within the mesenteric venous bed, leading to decreased perfusion pressure.[3] As flow stagnates in the mesenteric vein, increased venous pressure results in an efflux of fluid into the tissues, leading to bowel-wall edema. If the clinical progression continues, venous return from the bowel wall is completely occluded, and the end result is bowel ischemia.[3] Integrity of the bowel mucosa is lost and bacteria can translocate, leading to lactic acidosis, sepsis, multiorgan failure, and eventually death.[2]",
"MVT can occur acutely, subacutely, or chronically. The clinical features vary, depending on the location of the thrombus within the splanchnic vasculature.[3] Acute MVT, similar to other forms of acute mesenteric ischemia, presents most often as a colicky periumbilical pain that is often out of proportion to the physical examination findings. However, the onset of venous thrombosis, compared with arterial thrombosis, is often less sudden and dull, with as many as 75% of patients presenting after 2 days of abdominal pain.[3]",
"Alternatively, chronic mesenteric venous thrombosis often presents with portal hypertension and variceal hemorrhage.[2] In general, peritoneal signs are absent, unless the venous thrombosis goes untreated and the bowel becomes ischemic, in which case peritoneal signs develop.",
"In a retrospective study, 31 patients diagnosed with MVT from 1985-1999 were reviewed.[4] Approximately 84% of patients presented with abdominal pain, with 16% presenting with peritoneal signs. Common overall symptoms included diarrhea (42%), nausea and vomiting (32%), lower gastrointestinal bleeding (19%), fatigue (16%), and upper gastrointestinal bleeding (10%). Furthermore, only 22 patients were initially treated with heparin. Five patients were found to have peritonitis and underwent exploratory laparotomy, with the ultimate goal to prevent or limit gangrenous bowel, with an additional five patients later undergoing surgery for the development of ischemic bowel. Seven of the 31 patients died within 30 days, secondary to complications from infarcted bowel and multisystemic organ failure. Overall, 19 of the 24 survivors were treated with long-term anticoagulation, with 88% of those surviving long-term.",
"Differentiating between ischemia secondary to MVT and ischemia secondary to a mesenteric arterial thrombosis is important. MVT presents in the setting of thrombophilia or an inflammatory abdominal process, whereas mesenteric arterial ischemia presents in the setting of cardiac disease, low-flow states, and atrial fibrillation.[1] Similar to all forms of mesenteric ischemia, no clinical features are specific to MVT. As such, a clinician must have a high index of suspicion in order to make an early diagnosis and avoid the complications of an undiagnosed MVT."
],
"date": "October 02, 2020",
"figures": [],
"markdown": "# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\n\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \n **Date:** October 02, 2020\n\n ## Content\n\n Many risk factors for MVT are recognized, including direct injury (eg, abdominal trauma, splenectomy, intra-abdominal inflammatory processes), venous congestion/stasis (eg, congestive heart failure, portal hypertension, cirrhosis), and hypercoagulable conditions (eg, protein C/S deficiency, antithrombin III deficiency, factor V Leiden mutation, pancreatic/colon carcinoma, oral contraceptive use, polycythemia vera, heparin-induced thrombocytopenia, lupus anticoagulant/anti-phospholipid syndrome).[4] In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.[5]\nAcute occlusion of the mesenteric vein results in increased resistance within the mesenteric venous bed, leading to decreased perfusion pressure.[3] As flow stagnates in the mesenteric vein, increased venous pressure results in an efflux of fluid into the tissues, leading to bowel-wall edema. If the clinical progression continues, venous return from the bowel wall is completely occluded, and the end result is bowel ischemia.[3] Integrity of the bowel mucosa is lost and bacteria can translocate, leading to lactic acidosis, sepsis, multiorgan failure, and eventually death.[2]\nMVT can occur acutely, subacutely, or chronically. The clinical features vary, depending on the location of the thrombus within the splanchnic vasculature.[3] Acute MVT, similar to other forms of acute mesenteric ischemia, presents most often as a colicky periumbilical pain that is often out of proportion to the physical examination findings. However, the onset of venous thrombosis, compared with arterial thrombosis, is often less sudden and dull, with as many as 75% of patients presenting after 2 days of abdominal pain.[3]\nAlternatively, chronic mesenteric venous thrombosis often presents with portal hypertension and variceal hemorrhage.[2] In general, peritoneal signs are absent, unless the venous thrombosis goes untreated and the bowel becomes ischemic, in which case peritoneal signs develop.\nIn a retrospective study, 31 patients diagnosed with MVT from 1985-1999 were reviewed.[4] Approximately 84% of patients presented with abdominal pain, with 16% presenting with peritoneal signs. Common overall symptoms included diarrhea (42%), nausea and vomiting (32%), lower gastrointestinal bleeding (19%), fatigue (16%), and upper gastrointestinal bleeding (10%). Furthermore, only 22 patients were initially treated with heparin. Five patients were found to have peritonitis and underwent exploratory laparotomy, with the ultimate goal to prevent or limit gangrenous bowel, with an additional five patients later undergoing surgery for the development of ischemic bowel. Seven of the 31 patients died within 30 days, secondary to complications from infarcted bowel and multisystemic organ failure. Overall, 19 of the 24 survivors were treated with long-term anticoagulation, with 88% of those surviving long-term.\nDifferentiating between ischemia secondary to MVT and ischemia secondary to a mesenteric arterial thrombosis is important. MVT presents in the setting of thrombophilia or an inflammatory abdominal process, whereas mesenteric arterial ischemia presents in the setting of cardiac disease, low-flow states, and atrial fibrillation.[1] Similar to all forms of mesenteric ischemia, no clinical features are specific to MVT. As such, a clinician must have a high index of suspicion in order to make an early diagnosis and avoid the complications of an undiagnosed MVT.\n\n ## Figures\n\n \n*Page 4 of 6*",
"pagination": {
"current_page": 4,
"total_pages": 6
},
"questionnaire": [],
"title": "Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old"
},
{
"authors": "Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO",
"content": [
"Treatment for MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal exams. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence. If evidence of clinical deterioration and bowel infarction is present, surgical intervention is necessary. Broad-spectrum antibiotics are generally reserved for the setting of pylephlebitis, septic thrombophlebitis, and sepsis secondary to bacterial translocation from an infarcted bowel.[2]",
"Initiation of anticoagulation remains the cornerstone of treatment and should not be delayed.[6]Research has shown that once a patient is transitioned to oral anticoagulation, treatment should continue for 3-6 months, unless a thrombophilia has been diagnosed. After anticoagulation, most MVTs partially or completely recanalize, with one study showing recanalization in 80% of patients who received anticoagulation.[7] However, the recurrence rate has been reported at 15%.",
"Acute MVT carries a better prognosis than acute mesenteric ischemia. In one systematic review of nearly 3700 cases of acute mesenteric ischemia from 1966 to 2002, the mortality rate of those patients with MVT was 44%, compared with as much as 89% for those patients with advancement to mesenteric ischemia.[8] However, with increasing physician awareness, the use of contrast-enhanced CT to investigate abdominal pain in combination with anticoagulation has improved outcomes in these patients. In more modern studies, the mortality rate of acute MVT is down to 20%, with the most common cause of death being sepsis and multiorgan failure.[8]",
"In conclusion, acute superior MVT is a rare but important cause of mesenteric intestinal ischemia. It requires a high index of clinical suspicion. Rapid recognition and aggressive therapy are of extreme importance in order to prevent ischemic and infarcted bowel, sepsis, multiorgan failure, and eventual death. The 49-year-old man in this case had nonnecrotizing, alcohol-induced acute pancreatitis, complicated by acute superior MVT.",
"The patient in this case was eventually transitioned to rivaroxaban and discharged on day 4. Since his discharge, he has entered into alcohol rehabilitation and remains compliant with his anticoagulation."
],
"date": "October 02, 2020",
"figures": [],
"markdown": "# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\n\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \n **Date:** October 02, 2020\n\n ## Content\n\n Treatment for MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal exams. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence. If evidence of clinical deterioration and bowel infarction is present, surgical intervention is necessary. Broad-spectrum antibiotics are generally reserved for the setting of pylephlebitis, septic thrombophlebitis, and sepsis secondary to bacterial translocation from an infarcted bowel.[2]\nInitiation of anticoagulation remains the cornerstone of treatment and should not be delayed.[6]Research has shown that once a patient is transitioned to oral anticoagulation, treatment should continue for 3-6 months, unless a thrombophilia has been diagnosed. After anticoagulation, most MVTs partially or completely recanalize, with one study showing recanalization in 80% of patients who received anticoagulation.[7] However, the recurrence rate has been reported at 15%.\nAcute MVT carries a better prognosis than acute mesenteric ischemia. In one systematic review of nearly 3700 cases of acute mesenteric ischemia from 1966 to 2002, the mortality rate of those patients with MVT was 44%, compared with as much as 89% for those patients with advancement to mesenteric ischemia.[8] However, with increasing physician awareness, the use of contrast-enhanced CT to investigate abdominal pain in combination with anticoagulation has improved outcomes in these patients. In more modern studies, the mortality rate of acute MVT is down to 20%, with the most common cause of death being sepsis and multiorgan failure.[8]\nIn conclusion, acute superior MVT is a rare but important cause of mesenteric intestinal ischemia. It requires a high index of clinical suspicion. Rapid recognition and aggressive therapy are of extreme importance in order to prevent ischemic and infarcted bowel, sepsis, multiorgan failure, and eventual death. The 49-year-old man in this case had nonnecrotizing, alcohol-induced acute pancreatitis, complicated by acute superior MVT.\nThe patient in this case was eventually transitioned to rivaroxaban and discharged on day 4. Since his discharge, he has entered into alcohol rehabilitation and remains compliant with his anticoagulation.\n\n ## Figures\n\n \n*Page 5 of 6*",
"pagination": {
"current_page": 5,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1281948,
"choiceText": "Pancreatic and inflammatory bowel disease",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281950,
"choiceText": "Portal hypertension",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281952,
"choiceText": "Factor V Leiden mutation",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281954,
"choiceText": "Splenectomy",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281956,
"choiceText": "Gastric sleeve",
"correct": false,
"displayOrder": 5,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281958,
"choiceText": "All of the above\r\n",
"correct": true,
"displayOrder": 6,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "MVT has many associated risk factors, including direct injury, venous congestive/stasis, and hypercoagulable conditions. The patient in this case had an extensive history of alcohol abuse and pancreatitis. In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 408511,
"questionText": "Which of the following is considered a risk factor for the development of MVT?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1281960,
"choiceText": "Broad-spectrum antibiotic use is contraindicated at this point",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281962,
"choiceText": "Surgical consultation is unnecessary at this point",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281964,
"choiceText": "Anticoagulation should be delayed until further investigation is done",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281966,
"choiceText": "Bowel rest and fluid resuscitation should be promptly initiated",
"correct": true,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Treatment of MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal examinations. In this particular case, the patient is septic and has evidence of an intra-abdominal source in the setting of SMV thrombosis. If evidence suggests clinical deterioration and bowel infarction, surgical intervention is necessary.<br><br>\r\n\r\nIn this case, the patient has voluntary guarding and an elevated lactic acid level, making an emergent surgical consult necessary. Broad-spectrum antibiotics are generally reserved for patients with pylephlebitis, those with septic thrombophlebitis, and those with sepsis secondary to bacterial translocation from an infarcted bowel.\r\n<br><br>\r\nInitiation of anticoagulation remains the cornerstone of treatment and should not be delayed. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence.\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 408513,
"questionText": "A 53-year-old man with a significant medical history of pancreatitis presents to the ED with nausea, vomiting, and abdominal pain. His vital signs are notable for a heart rate of 113 beats/min, respiratory rate of 24 breaths/min, and a blood pressure of 96/50 mm Hg, with a temperature of 101.3°F (38.5°C). Abdominal examination reveals diffuse tenderness to palpation with voluntary guarding. Laboratory values are notable for a lactic acid level of 4.6 mmol/L, neutrophil-predominant leukocytosis of 19 × 10<sup>9</sup> cells/L, and a lipase level of 459 U/L. CT of the abdomen/pelvis reveals superior MVT. \r\n<br><br>\r\nWhich of the following is accurate regarding his treatment?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old"
},
{
"authors": "Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO",
"content": [],
"date": "October 02, 2020",
"figures": [],
"markdown": "# Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old\n\n **Authors:** Gregory Taylor, DO; Michael Semple, DO; Matthew Warpinski, DO \n **Date:** October 02, 2020\n\n ## Content\n\n \n\n ## Figures\n\n \n*Page 6 of 6*",
"pagination": {
"current_page": 6,
"total_pages": 6
},
"questionnaire": [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1281948,
"choiceText": "Pancreatic and inflammatory bowel disease",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281950,
"choiceText": "Portal hypertension",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281952,
"choiceText": "Factor V Leiden mutation",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281954,
"choiceText": "Splenectomy",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281956,
"choiceText": "Gastric sleeve",
"correct": false,
"displayOrder": 5,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281958,
"choiceText": "All of the above\r\n",
"correct": true,
"displayOrder": 6,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "MVT has many associated risk factors, including direct injury, venous congestive/stasis, and hypercoagulable conditions. The patient in this case had an extensive history of alcohol abuse and pancreatitis. In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 408511,
"questionText": "Which of the following is considered a risk factor for the development of MVT?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1281960,
"choiceText": "Broad-spectrum antibiotic use is contraindicated at this point",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281962,
"choiceText": "Surgical consultation is unnecessary at this point",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281964,
"choiceText": "Anticoagulation should be delayed until further investigation is done",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281966,
"choiceText": "Bowel rest and fluid resuscitation should be promptly initiated",
"correct": true,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Treatment of MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal examinations. In this particular case, the patient is septic and has evidence of an intra-abdominal source in the setting of SMV thrombosis. If evidence suggests clinical deterioration and bowel infarction, surgical intervention is necessary.<br><br>\r\n\r\nIn this case, the patient has voluntary guarding and an elevated lactic acid level, making an emergent surgical consult necessary. Broad-spectrum antibiotics are generally reserved for patients with pylephlebitis, those with septic thrombophlebitis, and those with sepsis secondary to bacterial translocation from an infarcted bowel.\r\n<br><br>\r\nInitiation of anticoagulation remains the cornerstone of treatment and should not be delayed. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence.\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 408513,
"questionText": "A 53-year-old man with a significant medical history of pancreatitis presents to the ED with nausea, vomiting, and abdominal pain. His vital signs are notable for a heart rate of 113 beats/min, respiratory rate of 24 breaths/min, and a blood pressure of 96/50 mm Hg, with a temperature of 101.3°F (38.5°C). Abdominal examination reveals diffuse tenderness to palpation with voluntary guarding. Laboratory values are notable for a lactic acid level of 4.6 mmol/L, neutrophil-predominant leukocytosis of 19 × 10<sup>9</sup> cells/L, and a lipase level of 459 U/L. CT of the abdomen/pelvis reveals superior MVT. \r\n<br><br>\r\nWhich of the following is accurate regarding his treatment?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
],
"title": "Alcohol Abuse and Unusual Abdominal Pain in a 49-Year-Old"
}
] | [
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1281940,
"choiceText": "Splenic vein thrombosis",
"correct": false,
"displayOrder": 1,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281942,
"choiceText": "Superior mesenteric vein thrombosis",
"correct": true,
"displayOrder": 2,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281944,
"choiceText": "Mesenteric arterial thrombosis",
"correct": false,
"displayOrder": 3,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281946,
"choiceText": "Septic pylephlebitis\r\n",
"correct": false,
"displayOrder": 4,
"explanation": "",
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "",
"displayOrder": 1,
"displayType": 1,
"horizontal": false,
"introduction": "",
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 408509,
"questionText": "Based only on these findings, which of the following is the most likely diagnosis?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1281948,
"choiceText": "Pancreatic and inflammatory bowel disease",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281950,
"choiceText": "Portal hypertension",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281952,
"choiceText": "Factor V Leiden mutation",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281954,
"choiceText": "Splenectomy",
"correct": false,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281956,
"choiceText": "Gastric sleeve",
"correct": false,
"displayOrder": 5,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281958,
"choiceText": "All of the above\r\n",
"correct": true,
"displayOrder": 6,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "MVT has many associated risk factors, including direct injury, venous congestive/stasis, and hypercoagulable conditions. The patient in this case had an extensive history of alcohol abuse and pancreatitis. In pancreatitis, the pathogenesis involves local venous congestion/stasis and spasm, with mass effect from the inflamed pancreas and damage to the wall of the veins by pancreatic enzymes.",
"displayOrder": 2,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 408511,
"questionText": "Which of the following is considered a risk factor for the development of MVT?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
},
{
"answered": false,
"answeredCorrectly": false,
"branch": false,
"choices": [
{
"branchPath": null,
"choiceId": 1281960,
"choiceText": "Broad-spectrum antibiotic use is contraindicated at this point",
"correct": false,
"displayOrder": 1,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281962,
"choiceText": "Surgical consultation is unnecessary at this point",
"correct": false,
"displayOrder": 2,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281964,
"choiceText": "Anticoagulation should be delayed until further investigation is done",
"correct": false,
"displayOrder": 3,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
},
{
"branchPath": null,
"choiceId": 1281966,
"choiceText": "Bowel rest and fluid resuscitation should be promptly initiated",
"correct": true,
"displayOrder": 4,
"explanation": null,
"hideLabel": false,
"selected": false,
"totalAbsoluteResponseCount": 0,
"totalResponses": "0"
}
],
"discussion": "Treatment of MVT is mainly conservative, involving systemic anticoagulation, bowel rest, fluid resuscitation, and serial abdominal examinations. In this particular case, the patient is septic and has evidence of an intra-abdominal source in the setting of SMV thrombosis. If evidence suggests clinical deterioration and bowel infarction, surgical intervention is necessary.<br><br>\r\n\r\nIn this case, the patient has voluntary guarding and an elevated lactic acid level, making an emergent surgical consult necessary. Broad-spectrum antibiotics are generally reserved for patients with pylephlebitis, those with septic thrombophlebitis, and those with sepsis secondary to bacterial translocation from an infarcted bowel.\r\n<br><br>\r\nInitiation of anticoagulation remains the cornerstone of treatment and should not be delayed. The ultimate goal is to prevent extension of the thrombus, avoid intestinal infarction, and prevent recurrence.\r\n",
"displayOrder": 3,
"displayType": 1,
"horizontal": false,
"introduction": null,
"matrixQuestions": [],
"mutuallyExclusive": false,
"poll": true,
"professions": [],
"questionId": 408513,
"questionText": "A 53-year-old man with a significant medical history of pancreatitis presents to the ED with nausea, vomiting, and abdominal pain. His vital signs are notable for a heart rate of 113 beats/min, respiratory rate of 24 breaths/min, and a blood pressure of 96/50 mm Hg, with a temperature of 101.3°F (38.5°C). Abdominal examination reveals diffuse tenderness to palpation with voluntary guarding. Laboratory values are notable for a lactic acid level of 4.6 mmol/L, neutrophil-predominant leukocytosis of 19 × 10<sup>9</sup> cells/L, and a lipase level of 459 U/L. CT of the abdomen/pelvis reveals superior MVT. \r\n<br><br>\r\nWhich of the following is accurate regarding his treatment?",
"questionTypeId": 1,
"required": false,
"responseText": null,
"score": false,
"showAnsTable": true,
"showQuestion": true,
"showResult": true,
"specialties": [],
"totalResponses": 0,
"viewResults": false
}
] |
Subsets and Splits
No saved queries yet
Save your SQL queries to embed, download, and access them later. Queries will appear here once saved.